LPN ATI mental Health
Total Questions : 49
Showing 25 questions, Sign in for moreA nurse is caring for a client who escapes anxiety-causing thoughts by ignoring their existence. The nurse should recognize this behavior as which of the following defense mechanisms?
Explanation
Repression is a defense mechanism that involves pushing distressing or anxiety-provoking thoughts, memories, or impulses into the unconscious mind. By repressing these thoughts, the individual can avoid dealing with the associated anxiety or discomfort. In the given scenario, the client escapes from anxiety-causing thoughts by ignoring their existence, which aligns with the concept of repression.
Denial, another defense mechanism, involves refusing to acknowledge the existence of a distressing reality or truth. However, in this case, the client is not denying the existence of the thoughts but rather ignoring or avoiding them.
Splitting is a defense mechanism characterized by the inability to integrate positive and negative qualities of oneself or others into a cohesive whole. It is not applicable in this situation.
Sublimation is a defense mechanism in which individuals redirect their unacceptable impulses into more socially acceptable outlets. It involves channeling potentially harmful or unacceptable desires into constructive behaviors. The given scenario does not reflect sublimation as the individual is not redirecting their anxiety into a productive activity or behavior.
A nurse is reinforcing discharge teaching with a client who has several new prescriptions for psychotropic medications. The client tells the nurse that she has always had trouble following a medication regimen. Which of the following responses should the nurse make?
Explanation
The response "Let's work together to devise a schedule that is convenient for you on a daily basis" demonstrates a collaborative and patient-centered approach. It acknowledges the client's difficulty in following a medication regimen and suggests finding a solution that works for the client's lifestyle and needs. By involving the client in the process and considering their preferences and challenges, the nurse can increase the chances of medication adherence.
The response "You really should work hard to stay on the schedule we establish here" may come across as judgmental and may not address the underlying reasons for the client's difficulty in medication adherence. It does not promote a collaborative and supportive environment.
The response "I wouldn't worry about what you've done in the past. You'll do just fine this time" dismisses the client's concerns and does not provide practical strategies to improve medication adherence. It does not address the client's specific challenge or offer any support.
The response "Why do you find it difficult to take your medications if they improve your condition?" is a probing question that seeks to understand the client's reasons for struggling with medication adherence. While it may be important to explore the underlying reasons, it should be followed by a supportive and collaborative approach to finding solutions.
A nurse is caring for a newly admitted female client who has depression and refuses to get out of bed, dress, or participate in group therapy. Which of the following is an appropriate nursing response?
Explanation
The response "I will assist you in getting out of bed and getting dressed" demonstrates a supportive and therapeutic approach. It acknowledges the client's current state and offers assistance to engage in self-care activities. By providing support and actively participating in the client's care, the nurse can promote motivation, engagement, and a sense of empowerment.
The response "You can remain in bed until you feel well enough to join the milieu" may enable the client's depressive behaviors and reinforce the avoidance of activities. It does not encourage participation or provide support for the client to engage in therapeutic activities.
The response "The unit rules state that clients may not remain in bed" focuses on enforcing rules rather than addressing the client's underlying emotional state and needs. It may increase resistance and hinder the therapeutic relationship.
The response "If you don't participate in your care, you will not get better" may be perceived as blaming or judgmental. It may increase the client's guilt or sense of failure and does not provide practical support or encouragement.
A nurse is caring for a client who reports a state of Increasing anxiety and the inability to sleep and concentrate. Which of the following is an appropriate response by the nurse?
Explanation
The response "It sounds like you're having a difficult time" acknowledges the client's distress and validates their experience. It demonstrates empathy and shows the nurse's willingness to listen and provide support. This response encourages the client to express their feelings and concerns further, facilitating open communication and a therapeutic relationship.
The response "Why do you think you are so anxious?" may come across as confrontational or intrusive. It puts the client on the spot and may make them feel defensive or uncomfortable. It is important to create a supportive environment where the client feels safe to share their experiences without judgment.
The response "Everyone has trouble sleeping at times" minimizes the client's concerns and may invalidate their feelings. It does not address the client's anxiety or offer any support or guidance.
The response "Have you talked to your provider about this yet?" is a helpful question to explore whether the client has sought professional help. However, it should be used after acknowledging the client's difficulties and showing empathy. It can be part of a conversation about accessing appropriate care and resources.
A nurse is caring for a client in an acute care mental health unit who was involuntarily admitted for 72 hr after attacking a neighbor. To keep the client in the hospital when the initial time to hold the client expires, which of the following must be determined?
Explanation
When a client is involuntarily admitted to a mental health unit, there is typically a specific time frame, such as 72 hours, during which they can be held involuntarily for evaluation and
treatment. At the end of this initial hold period, further determination is required to determine if continued hospitalization is necessary.
The primary consideration for extending the client's stay is whether they continue to pose a danger to themselves or others. This determination is based on a comprehensive assessment of the client's mental state, behavior, and potential for harm. If the client still exhibits signs of being a threat to themselves or others, the healthcare team may decide to continue their hospitalization to ensure their safety and the safety of others.
The other options listed are not the primary criteria for determining the need for continued hospitalization:
● Whether the client is unwilling to accept that treatment is needed: While the client's willingness to accept treatment is an important factor, it is not the sole determinant for extending their stay. Even if the client recognizes the need for treatment, if they are still a danger to themselves or others, their hospitalization may be prolonged.
● Whether the client is financially incapable of paying for prescribed medications: Financial considerations do not directly impact the decision to extend the client's stay. The focus is on their safety and the need for continued psychiatric assessment and treatment.
● Whether the client is unable to make arrangements to stay with someone: The client's living arrangements or ability to stay with someone outside of the hospital are not the main factors in determining the need for extended hospitalization. The key consideration is whether the client continues to pose a danger to themselves or others.
A nurse observes that a client is sitting alone in her room crying. As the nurse approaches, she states, "I'm feeling really down and don't want to talk to anyone right now." Which of the following responses is appropriate for the nurse?
Explanation
The appropriate response for the nurse in this situation would be: "I'll just sit here with you for a few minutes then."
This response acknowledges the client's expressed desire not to talk and respects their boundaries. It shows support and presence by offering companionship without pressuring the client to discuss their feelings. The nurse's willingness to sit with the client demonstrates empathy and provides a sense of comfort and reassurance.
The other options are not as appropriate:
1. "It might help you feel better if you talk about it." This response disregards the client's stated preference not to talk and may create a sense of pressure or intrusiveness. It is important to respect the client's autonomy and readiness to share their feelings.
2. "Why are you feeling so down?" This response directly asks the client to explain their feelings, which they have already indicated they do not want to discuss. It can be seen as intrusive and may make the client feel uncomfortable or defensive.
3. "I understand. I've felt like that before, too." While empathy is important, this response brings the focus back to the nurse's own experiences, potentially diverting the attention from the client. It is important for the nurse to remain focused on the client's needs and create a supportive environment for them to express their feelings if they choose to do so.
A nurse is caring for a client who has a major depressive disorder. Which of the following actions should the nurse take when developing a relationship with the client?
Explanation
It is important for the nurse to establish and maintain appropriate professional boundaries with the client. This includes respecting the client's personal space and privacy. By maintaining appropriate boundaries, the nurse ensures a therapeutic and professional relationship that focuses on the client's needs and promotes their well-being.
The other options are not appropriate when developing a relationship with the client:
1. Share personal information to help the client feel comfortable: While it is important to build rapport and create a supportive environment, sharing personal information may blur professional boundaries and divert the focus from the client to the nurse. The therapeutic relationship should primarily revolve around the client's needs and experiences.
2. Develop an emotional commitment to the client: While empathy and compassion are essential in providing care, it is important for the nurse to maintain professional objectivity. Developing an emotional commitment can make it challenging for the nurse to maintain appropriate boundaries and could lead to potential ethical issues.
3. He reminds the nurse of a personal friend or relative: It is important for the nurse to remain unbiased and treat each client as an individual. Drawing comparisons or associations with personal acquaintances can influence the nurse's objectivity and professionalism in providing care.
A nurse observes that a client is sitting alone in her room crying. As the nurse approaches, she states, "I'm feeling really down and don't want to talk to anyone right now." Which of the following responses is appropriate for the nurse?
Explanation
This response acknowledges the client's expressed desire not to talk and respects their boundaries. It shows support and presence by offering companionship without pressuring the client to discuss their feelings. The nurse's willingness to sit with the client demonstrates empathy and provides a sense of comfort and reassurance.
The other options are not as appropriate:
1. "It might help you feel better if you talk about it." This response disregards the client's stated preference not to talk and may create a sense of pressure or intrusiveness. It is important to respect the client's autonomy and readiness to share their feelings.
2. "Why are you feeling so down?" This response directly asks the client to explain their feelings, which they have already indicated they do not want to discuss. It can be seen as intrusive and may make the client feel uncomfortable or defensive.
3. "I understand. I've felt like that before, too." While empathy is important, this response brings the focus back to the nurse's own experiences, potentially diverting the attention from the client. It is important for the nurse to remain focused on the client's needs and create a supportive environment for them to express their feelings if they choose to do so.
A nurse working in a long-term care facility is admitting a client who has dementia.
Nurses Notes
Client has a flat affect. Client's speech is rambling and the client frequently loses their train of thoughts. While speaking, the client constantly taps their right foot. Client is unable to sit still and frequently exhibits wandering behavior and becomes agitated when attempts are made to redirect their activity.
Which of the following interventions should the nurse include in the plan of care?
Select all that apply.
Explanation
From the given information, the nurse should include the following interventions in the plan of care for the client with dementia:
● Obtain client's weight weekly: Regular weight monitoring helps assess the client's nutritional status and detect any significant changes that may require intervention.
● Offer the client finger foods for meals: Finger foods can be easier for the client to handle and consume independently, promoting independence and self-feeding.
● Encourage the client to take deep breaths when feeling agitated: Deep breathing exercises can help the client manage their agitation and promote relaxation.
● Assess client's memory every shift: Regular assessment of the client's memory allows for monitoring any changes or decline, which helps in planning appropriate interventions and providing necessary support.
The following interventions should be avoided:
● Speak loudly when addressing the client: Speaking loudly may cause confusion or agitation in the client. Instead, it is recommended to use a calm and reassuring tone of voice.
● Give long tasks at a time to the client: Clients with dementia often have difficulty with concentration and memory. Providing long tasks may overwhelm them and contribute to their frustration. Breaking tasks into smaller, manageable steps is more appropriate.
● Turn the client's TV on at night when they are unable to sleep: It is generally recommended to create a quiet and calming environment for sleep. The TV may interfere with the client's sleep and contribute to increased agitation or confusion.
A nurse is discussing legal exceptions to client confidentiality with nursing staff. Which of the following statements by a staff member indicates an understanding?
Explanation
The statement "Providers are required to warn individuals if the client threatens harm" demonstrates an understanding of the legal exception known as the duty to warn or protect. It means that if a client expresses an intent to harm themselves or others, healthcare providers have a legal obligation to take appropriate actions, which may include notifying potential victims or authorities.
Incorrect:
1. "The legal requirement for client confidentiality does not apply if the client is deceased." - This statement is incorrect. Client confidentiality extends even after a client's death, and healthcare professionals are still expected to maintain confidentiality regarding the client's health information.
2. "Staff members are required to divulge information regarding a client's hospitalization to a client's employer." - This statement is incorrect. Healthcare professionals are required to maintain client confidentiality and cannot disclose a client's health information to their employer without the client's explicit consent or as mandated by specific legal requirements.
3. "Healthcare workers can use client confidentiality for their own legal defense." - This statement is incorrect. Client confidentiality is meant to protect the client's privacy and
maintain trust. It cannot be used by healthcare workers as a defense mechanism in legal matters.
A nurse is assisting in the admission process for a client who has a history of violent behavior. The client stands up and begins clenching her fists and arguing with the nurse. Which of the following actions is the priority?
Explanation
The priority action in this situation is to set behavioral limits for the client. This is important for maintaining a safe environment for the client, other staff members, and other clients. By setting limits, the nurse establishes clear boundaries and expectations for behavior, helping to prevent the escalation of aggression or violence.
Let's examine why the other choices are incorrect:
A. Exploring the truth of the client's statements: While it is important to listen to and validate the client's concerns, in this particular situation, where the client is becoming agitated and confrontational, addressing the truth of their statements is not the priority. The immediate concern is ensuring safety and de-escalating the situation.
B. Establishing a therapeutic nurse-client relationship: Developing a therapeutic relationship is crucial for providing effective care, but it may not be the immediate priority when a client is displaying aggressive or violent behavior. Safety takes precedence in such situations, and setting behavioral limits is necessary before establishing a therapeutic relationship can effectively occur.
D. Showing the client around the unit and introducing her to other clients: This action is inappropriate during an agitated and confrontational episode. It is important to first
address the client's behavior and ensure the safety of all individuals involved before engaging in social activities or introductions.
A nurse is caring for a client who is scheduled for electroconvulsive therapy In 1 hr. The client asks the nurse, "Can I refuse today's treatment?" Which of the following responses should the nurse make?
Explanation
Clients have the right to make informed decisions about their own healthcare, including the right to refuse treatment. It is important to respect the client's autonomy and honor their decision if they choose to refuse the treatment. The nurse should provide the client with information about the potential benefits and risks of the treatment, as well as any alternatives, and support the client in making an informed decision.
Let's examine why the other choices are incorrect:
A. "You will be discharged sooner if you have the prescribed ECT treatments." This statement does not address the client's right to refuse treatment and instead focuses on potential consequences of refusing. It is important to respect the client's autonomy and prioritize their right to make decisions about their own healthcare.
C. "You are admitted to a mental health facility and must follow the provider's orders." While clients in a mental health facility may have certain treatment plans, including ECT, it is still important to respect their right to refuse treatment. Admitting to a facility does not negate the client's right to make decisions about their own care.
D. "You have already signed the consent form, so you cannot refuse today's treatment." Signing a consent form does not mean that the client loses their right to refuse treatment. Consent forms are signed to acknowledge that the client has been provided with information about the treatment and has agreed to undergo it voluntarily. However, the client still has the right to change their mind and refuse the treatment at any time.
A nurse is caring for a client following the recent, sudden death of his partner. The client says, "I feel paralyzed and can't seem to cope with work or family responsibilities anymore." Which of the following types of crisis is the client demonstrating?
Explanation
A situational crisis is a type of crisis that occurs in response to a specific event or situation that disrupts a person's usual coping mechanisms. In this case, the sudden death of the client's partner has caused significant distress and an inability to cope with work and family responsibilities. The client's feelings of paralysis and inability to function indicate a response to the specific situation they are facing.
Incorrect:
B- Developmental crisis refers to crises that arise during normal stages of growth and development, such as adolescence or midlife crisis.
C- A maturational crisis involves a crisis that occurs as a result of the normal process of aging and the associated challenges and changes that come with it.
D- Adventitious crisis refers to crises that arise from unpredictable, uncommon events that are out of the ordinary, such as natural disasters or accidents.
A nurse is caring for a client who has generalized anxiety disorder. The client is consistently late for appointments and ignores household chores. The client states, "I'm just too stressed. I need to be taken care of. The nurse should identify this behavior as the maladaptive use of which of the following defense mechanisms?
Explanation
Regression is a defense mechanism that involves reverting to an earlier stage of development or behaving in a way that is characteristic of an earlier developmental level in response to stress or anxiety. It is a way for individuals to cope with overwhelming emotions or situations by retreating to a previous, more comfortable state.
In the scenario described, the client's behavior of consistently being late for appointments and ignoring household chores while expressing the need to be taken care of indicates a regressive response to stress. By relying on others to take care of their responsibilities, the client is seeking a sense of security and support, similar to how they may have relied on others in the past, such as during childhood.
Inc
A- Repression involves the unconscious blocking of unacceptable thoughts or impulses from conscious awareness.
B- Introjection is the internalization of values or qualities of another person or group.
C- Dissociation is a defense mechanism that involves detaching oneself from reality or the present moment to avoid emotional distress.
A nurse is assisting with the admission assessment for a cilent who is receiving treatment following a situational crisis. Which of the following actions is the nurse's priority?
Explanation
Determining if the client has thoughts of self-harm: This is the priority action for the nurse in this situation. Assessing the client's risk of self-harm or suicide is crucial to determine the level of immediate intervention required. It helps identify the severity of the crisis and enables the nurse to implement appropriate measures to ensure the client's safety.
In the context of a client with generalized anxiety disorder who is exhibiting signs of distress and seeking to be taken care of, it is essential to assess for suicidal ideation or intent. Clients with mental health disorders, especially when experiencing high levels of stress, may be at an increased risk of self-harm or suicide. Therefore, it is vital for the nurse to prioritize the assessment of the client's safety and risk of self-harm in order to provide appropriate care and interventions.
Incorrect:
A- Asking the client to identify the cause of the crisis: While it is important to gather information about the cause of the crisis to understand the client's situation, it is not the nurse's priority at this moment. Assessing the client's safety and immediate risk of self-harm takes precedence.
C- Identifying if friends or family are available to help: While social support from friends and family can be valuable in managing a crisis, it is not the nurse's priority in this situation. The immediate concern is to assess the client's safety and risk of self-harm.
D-Identifying the client's coping skills: Assessing the client's coping skills is an important aspect of the overall assessment process, but it is not the priority at this moment. The nurse needs to first ensure the client's safety and address any immediate risks.
A nurse is caring for an older adult client admitted to the hospital following a cerebrovascular accident. The client's daughter tells the nurse, "I wish I could stay with my father, but I need to go home to my family." Which of the following responses should the nurse make?
Explanation
The response "You are feeling drawn in two different directions" acknowledges the daughter's conflicting feelings and validates her emotions. It demonstrates empathy and understanding of her situation. It can help the daughter feel heard and supported and opens up an opportunity for further conversation about her concerns and possible solutions.
The other options are less appropriate:
A- "Don't worry. We'll take good care of your father while you are gone." While this response reassures the daughter about her father's care, it does not address her emotional conflict or provide support for her own needs and concerns.
B- "Perhaps you could stay here and just call your family to see how they are doing." This response minimizes the daughter's situation and does not fully acknowledge her need to be with her own family. It may overlook the emotional strain and responsibilities she may have outside of the hospital.
C-"There's nothing you can do here. You should go home to your family." This response dismisses the daughter's feelings and implies that her presence is not necessary or valuable. It does not consider her desire to support her father or the importance of maintaining a connection with him during his hospitalization.
A nurse is assisting with the court-ordered admission of a client to a substance-abuse program. The client states, "You are all angry at me and wish you could go out and have a drink." The client's response is an example of which of the following defense mechanisms?
Explanation
Projection is a defense mechanism where an individual attributes their own undesirable thoughts, feelings, or impulses onto someone else. In this case, the client is projecting their own desire to go out and have a drink onto the nurse and others involved in their care. They are attributing their own feelings to others in an attempt to avoid acknowledging or taking responsibility for their own desires.
A- Reaction-formation is a defense mechanism where an individual expresses the opposite of their true feelings or impulses.
B- Compensation is a defense mechanism where an individual tries to make up for their perceived deficiencies by excelling in another area.
D- Identification is a defense mechanism where an individual models their behavior after someone they admire.
A nurse at an urgent care center is caring for a client who sustained minor injuries during a street fight in which two of the client's friends were stabbing victims. The client tells the nurse that he doesn't remember anything that happened after he and his friends first saw the suspects in the stabbing. Which of the following defense mechanisms is the client demonstrating?
Explanation
Dissociation is a defense mechanism in which a person disconnects from their thoughts, feelings, memories, or sense of identity as a way to cope with overwhelming or traumatic experiences. In this case, the client's inability to remember anything that happened after seeing the suspects in the stabbing is a form of dissociation. It is a way for the client to psychologically distance themselves from the traumatic event and protect themselves from the emotional distress associated with it.
A- Projection is a defense mechanism where an individual attributes their own undesirable thoughts, feelings, or impulses onto someone else.
C- Repression is a defense mechanism where disturbing or unacceptable thoughts, memories, or feelings are pushed into the unconscious mind.
D- Sublimation is a defense mechanism where unacceptable impulses or emotions are redirected into socially acceptable activities.
A nurse is caring for a client following major spinal surgery who is reporting pain. The client's partner tells the nurse, "I wish I could do something to make my wife feel better." Which of the following responses should the nurse make?
Explanation
The appropriate response for the nurse in this situation is to acknowledge the partner's concern and empathize with their feelings. By stating, "It must be very difficult for you to see your wife in pain," the nurse acknowledges the partner's emotions and shows understanding and empathy. This response validates the partner's feelings and demonstrates support and compassion.
B- "We're doing everything we can to keep your wife comfortable" may be a true statement, but it does not directly address the partner's expressed wish to do something to help. It may not fully address the emotional aspect of the partner's statement.
C- "I wish there was more that I could do to relieve your wife's pain, too" is a genuine response that expresses empathy. It acknowledges the partner's desire to help and implies that the nurse shares the same sentiment. This response shows understanding and support.
D- "I'm sure your wife will begin to feel better soon" dismisses the partner's concern and does not address their expressed wish to alleviate their wife's pain. It may not fully acknowledge the partner's emotions or provide the support they need in that moment.
A nurse is caring for a client who begins to make sexual advances towards him. Which of the following is an appropriate statement by the nurse?
Explanation
The appropriate response by the nurse in this situation is to set clear boundaries and remove themselves from the situation. By stating, "I'm going to leave now and I'll return in one hour to spend time with you then," the nurse establishes that the inappropriate behavior is not acceptable and that they will return later to continue providing care within professional boundaries.
A- "I'm sure that you don't intend to behave this way, so I'm going to ignore this behavior" is not an appropriate response. Ignoring the behavior can potentially enable or encourage further inappropriate advances, and it does not address the issue directly.
B- "I'm curious as to why you are behaving this way. Can you please explain it to me?" places the responsibility on the client to explain their behavior, which is not appropriate or necessary in this situation. It may also encourage further discussion of the inappropriate behavior.
C- "I'm very flattered, but I am married and cannot engage in this behavior" personalizes the situation and may give the wrong impression that the nurse's marital status is the reason for rejecting the advances. It is important to maintain professional boundaries and not involve personal factors in the response.
A nurse is caring for an older adult client who has dementia and is agitated. The client says, "I have to go home and see my mother." The nurse replies, "You miss your mother." Which of the following therapeutic techniques is the nurse using?
Explanation
Validation is a technique used to acknowledge and validate the emotions and experiences of individuals with dementia, even if their thoughts or perceptions do not align with reality. In this scenario, the nurse responds by saying, "You miss your mother," which shows understanding and empathy toward the client's emotions. The nurse is validating the client's feelings rather than attempting to correct or redirect their thoughts.
A. Orientation to reality involves providing factual information and attempting to reorient individuals with dementia to the present time, place, and situation.
B. Remotivation is a technique used to stimulate memories and engage individuals with dementia in meaningful activities.
D. Guided imagery involves using vivid language and descriptive prompts to guide individuals into imagining pleasant or calming scenes.
The nurse is caring for a client who has been admitted Involuntarily for psychiatric treatment. Which of the following Information about involuntary commitment should the nurse provide the client's family?
Explanation
Involuntary commitment refers to the legal process by which an individual is admitted to a psychiatric facility for treatment against their will. The decision to involuntarily commit someone is typically based on the assessment that their behavior poses a risk of harm to themselves or others. Therefore, it is important for the nurse to inform the client's family that the reason for the involuntary commitment is the client's behavior being a threat to their own safety or the safety of others.
A."A psychiatrist determines that the client's behavior is irrational." This statement is incorrect because irrational behavior alone is not sufficient grounds for involuntary commitment.
Involuntary commitment is typically based on the assessment that the individual's behavior poses a risk of harm to themselves or others, rather than solely on the basis of irrational behavior.
B. "The client is unable to manage the affairs necessary for daily life." While the inability to manage daily affairs may be a factor considered in the overall assessment of a client's condition, it is not the sole criterion for involuntary commitment. Involuntary commitment is primarily focused on the risk of harm posed by the individual's behavior, rather than their ability to manage daily life tasks.
D. "The client has been accused of breaking the law." Accusations of breaking the law are not the basis for involuntary commitment. Involuntary commitment is based on the assessment that the individual's behavior presents a risk of harm to themselves or others. Legal issues are addressed separately through the legal system and are not directly related to the criteria for involuntary commitment.
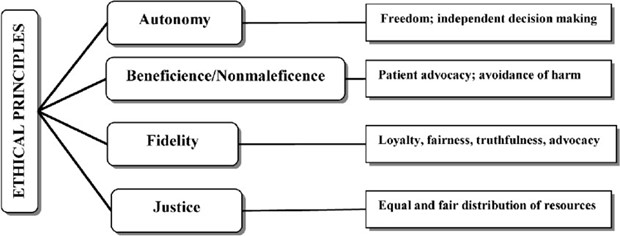
A nurse on an inpatient mental health unit is caring for a group of clients. Which of the following actions by the nurse demonstrates the ethical concept of autonomy?
Explanation
Autonomy is the ethical principle that upholds an individual's right to make decisions about their own care and treatment. Respecting autonomy means acknowledging and honoring a person's right to make choices based on their own values, beliefs, and preferences. By importing a client's wishes to refuse prescribed treatments, the nurse is recognizing and respecting the client's autonomy. This shows that the nurse values the client's right to make decisions about their own healthcare and supports their choice, even if it may differ from what the nurse may recommend.
Incorrect:
A. Spending extra time to calm an agitated client demonstrates the ethical principle of beneficence, which is the duty to promote the well-being and welfare of the client.
B. Ensuring that a client understands expectations for group participation relates to the ethical principle of fidelity, which involves maintaining trust and keeping promises to the client.
C. Describing the adverse effects of a client's medications is important for informed consent and promoting understanding, but it does not directly involve the client's autonomy unless it is accompanied by a discussion of the client's choices and preferences regarding medication.
A nurse on a mental health unit is participating in a community meeting with a group of clients. Which of the following actions should the nurse take?
Explanation
Respecting and honoring the autonomy of the clients is important in a mental health setting. Allowing clients to determine the boundaries of the nurse-client relationship empowers them to have control over their own treatment and fosters a sense of autonomy. It encourages clients to express their needs, preferences, and comfort levels in the therapeutic relationship, which can contribute to a more collaborative and effective treatment process.
The other options mentioned are not appropriate actions for the nurse to take:
A. Orienting clients to their responsibilities on the unit is an important task, but it is not specific to the context of a community meeting. It is more relevant during individual client orientations or at the beginning of their admission.
B. Focusing on client weaknesses to increase adaptation is not a therapeutic approach. It is important to focus on clients' strengths and support their growth and development rather than emphasizing weaknesses.
C. Planning to discuss any topic presented by clients can be unfeasible or not relevant in a community meeting. It is essential to have structure and purpose in group discussions to facilitate meaningful interactions.
A nurse is caring for a client with whom he has developed a therapeutic relationship and who will be discharged later in the day. The client thanks the nurse for his help during the hospitalization. Which of the following responses should the nurse make?
Explanation
Asking the client how they feel about being discharged encourages open communication and provides an opportunity for the client to express their emotions and thoughts about leaving the
hospital. It shows that the nurse values the client's perspective and allows for further discussion and support if needed. This response promotes client-centered care and acknowledges the client's experience during the hospitalization.
The other options are less appropriate:
A. "I know you will do well living out in the community" assumes the client's feelings and may not accurately reflect their experience or emotions about the discharge.
B. "I will send you a note in a few weeks" focuses on the nurse's future action rather than actively engaging with the client's expression of gratitude.
C. "Aren't you excited about being discharged today?" assumes the client's emotional state and may not consider the potential range of emotions the client could be experiencing.
Sign Up or Login to view all the 49 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

