Exam Review
Mental and Behavioral Health Nursing Exam
Total Questions : 78
Showing 78 questions, Sign in for moreA nurse is teaching a group of clients regarding the use of naltrexone in treating alcoholism. What would the nurse teach about the effectiveness of this drug?
Explanation
A) Incorrect. Naltrexone does not primarily target withdrawal symptoms. It works by blocking the pleasurable effects of alcohol, reducing the reinforcement that leads to craving.
B) Correct. Naltrexone is an opioid antagonist that reduces the craving for alcohol. It does this by blocking the opioid receptors in the brain, which are involved in the pleasurable effects of
alcohol consumption.
C) Incorrect. Naltrexone is not primarily used to manage anxiety. Its main purpose is to help individuals reduce or stop their alcohol intake.
D) Incorrect. Naltrexone is not primarily used to treat depressive symptoms. Its focus is on reducing alcohol cravings.

A client diagnosed with bipolar disorder has recently started taking lamotrigine as part of their medication regimen. Which of the following would be an essential teaching point to include regarding the medication?
Explanation
A) Incorrect. While monitoring sodium levels can be important for clients on certain
medications, it is not a primary concern with lamotrigine. The main concern is the potential for a serious rash.
B) Correct. Lamotrigine is associated with a risk of a severe skin reaction called Stevens Johnson syndrome. If a client experiences any rash while taking lamotrigine, it is crucial to notify a
healthcare provider immediately.
C) Incorrect. While monitoring weight and potential changes in appetite are important aspects of overall health, it is not a specific teaching point for lamotrigine.
D) Incorrect. While it is important for individuals of childbearing age to discuss pregnancy plans and contraceptive methods with their healthcare provider, it is not the primary teaching point specific to lamotrigine.
When a client diagnosed with schizophrenia was discharged 6 months ago, haloperidol was prescribed. The client now says, "I stopped taking those pills. They made me feel like a robot." What are common side effects the nurse should validate with the client?
Explanation
A) Correct. Haloperidol, a first-generation antipsychotic, commonly causes side effects like sedation (drowsiness) and extrapyramidal symptoms, including muscle stiffness.
B) Incorrect. Sweating, nausea, and diarrhea are not typically associated with haloperidol.
C) Incorrect. Mild fever, sore throat, and skin rash are not common side effects of haloperidol.
D) Incorrect. Headache, watery eyes, and runny nose are not common side effects of haloperidol.
The nurse is obtaining the mental health history of a newly admitted client diagnosed with schizophrenia. The client's family reports the client is hearing voices and cannot stay focused on the topic of a discussion. Which thought disturbance is the client demonstrating?
Explanation
A) Incorrect. Delusions of reference involve a belief that everyday events, objects, or other people have a particular and unusual significance. This is not described in the scenario.
B) Incorrect. Tangentiality is a thought disorder where the individual goes off on tangents and never returns to the original point or idea. This is not described in the scenario.
C) Incorrect. Neologism refers to the creation of new words or phrases that have meaning only to the person using them. This is not described in the scenario.
D) Correct. Loose associations are characterized by a disruption in the logical progression of thought, where thoughts become disorganized and may seem unrelated or loosely connected.
The nurse is admitting a client with the diagnosis of schizophreniform disorder. What should the nurse expect to find?
Explanation
A) Incorrect. The ability to accomplish activities of daily living is not specific to the diagnosis of schizophreniform disorder.
B) Incorrect. The client's emotional state or demeanor is not a specific indicator of schizophreniform disorder.
C) Correct. Schizophreniform disorder is characterized by the presence of hallucinations,
delusions, and other psychotic symptoms for less than six months. It is considered a provisional diagnosis while the condition is still in its early stages.
D) Incorrect. Euphoria and excessive energy are not specific features of schizophreniform disorder.
A client diagnosed with bipolar I disorder is in a manic state, rushing about the unit, and talking regularly with a flight of ideas. What is the most therapeutic intervention?
Explanation
A) Incorrect. Isolating the client in his room may escalate the situation or make the client feel isolated and misunderstood.
B) Incorrect. Asking the client to stop talking may be perceived as confrontational and could potentially agitate the client further.
C) Correct. Speaking slowly and in a quiet voice can help the client focus and may reduce the flight of ideas. This calm approach can be grounding for the client.
D) Incorrect. Encouraging the client to talk more may exacerbate the flight of ideas and the manic state.
A nurse is providing discharge teaching to a client who has bipolar disorder and will be discharged with a prescription for lithium. What information should be included in the teaching? (Select all that apply.)
Explanation
A) Incorrect. While it's important to avoid dehydration, this option is not specific to lithium use.
B) Correct. Lithium can cause dehydration, so it's crucial for the client to drink adequate fluids daily.
C) Correct. A low sodium diet is important while taking lithium, as high sodium levels can affect lithium absorption and potentially lead to toxicity.
D) Correct. Routine blood work is necessary to monitor lithium levels and ensure the client's levels remain within the therapeutic range.
E) Incorrect. Dependency is not a common concern with lithium.
The nurse is obtaining the mental health history of a newly admitted client diagnosed with schizophrenia. The client's family reports the client is hearing voices and cannot stay focused on the topic of a discussion.
Which thought disturbance is the client demonstrating?
Explanation
A) Incorrect. Delusions of reference involve a belief that everyday events, objects, or other people have a particular and unusual significance. This is not described in the scenario.
B) Incorrect. Tangentiality is a thought disorder where the individual goes off on tangents and never returns to the original point or idea. This is not described in the scenario.
C) Incorrect. Neologism refers to the creation of new words or phrases that have meaning only to the person using them. This is not described in the scenario.
D) Correct. Loose associations are characterized by a disruption in the logical progression of thought, where thoughts become disorganized and may seem unrelated or loosely connected.
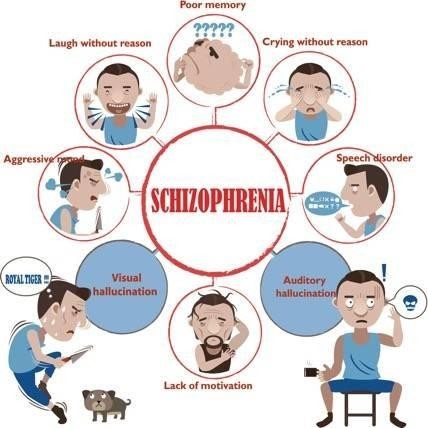
A nurse is caring for a client diagnosed with schizophrenia following a recent suicide attempt. Which of the following actions should the nurse take?
Explanation
A) Incorrect. Placing metal utensils on the client's meal tray may pose a safety risk, especially considering the recent suicide attempt.
B) Incorrect. Assigning the client to a private room may be beneficial for privacy, but the more immediate concern is ensuring the safety of the client by inspecting personal belongings.
C) Correct. Inspecting the client's personal belongings is crucial to remove any potentially harmful items that the client may use to harm themselves.
D) Incorrect. Tucking bedcovers over the client's hands and arms is not a specific intervention related to the recent suicide attempt.
The client is experiencing a manic episode. Which of the following activities will be included in the plan of care?
Explanation
A) Correct. Encouraging participation in physical activities can help channel excess energy and agitation associated with manic episodes.
B) Incorrect. Group card games may not provide an outlet for the high energy level typically seen in a manic episode.
C) Incorrect. While Bingo is a social activity, it may not be sufficient to address the high energy and potential restlessness seen in a manic episode.
D) Incorrect. Creating a new interactive game may not be feasible or appropriate in the acute setting, and it may not effectively address the client's current needs.
An adolescent tells the school nurse, "My friend threatened to take an overdose of pills." The nurse talks to the friend who verbalized the suicide threat. What is the most critical question for the nurse to ask?
Explanation
A) Incorrect. While understanding the reasons behind the suicidal thoughts is important, in this immediate situation, assessing access to means (medications) is crucial.
B) Correct. This question assesses the immediate risk by determining if the friend has access to the means (medications) to carry out the overdose.
C) Incorrect. While substance use is a risk factor, it may not directly address the immediate threat of overdose with pills.
D) Incorrect. While family issues can contribute to emotional distress, the most pressing concern is the immediate risk of overdose.
A female client staggers to day treatment smelling strongly of alcohol. She uses the defense mechanism "rationalization" when approached by the nurse and questioned about her recent alcohol consumption. How is this expressed?
Explanation
A) Incorrect. This statement is a straightforward denial rather than rationalization.
B) Incorrect. This response is an example of avoidance or distraction, not rationalization.
C) Correct. Rationalization involves offering logical or reasonable explanations to justify behaviors or actions that might otherwise be unacceptable. In this case, the client is rationalizing her alcohol consumption as a means to relax and cope with the day treatment.
D) Incorrect. This statement reflects a defensive response but is not an example of rationalization.
A client is showing symptoms of alcohol intoxication. What question should the nurse ask first?
Explanation
A) Incorrect. While understanding if the client is experiencing a relapse is important, knowing the timing of the last drink is crucial for assessing the level of intoxication.
B) Correct. Knowing the time of the last drink helps the nurse gauge the current level of alcohol in the client's system, which is crucial in assessing and managing alcohol intoxication.
C) Incorrect. While understanding the duration of the client's problem with alcohol is important, it is not the most immediate concern when the client is showing symptoms of intoxication.
D) Incorrect. Asking about liver problems is relevant but not the first priority when the client is exhibiting signs of alcohol intoxication.
A client has been diagnosed with major depression and placed on amitriptyline. Which is a side effect of amitriptyline?
Explanation
A) Correct. Amitriptyline, like other tricyclic antidepressants, can cause orthostatic hypotension, which is a drop in blood pressure when changing position from lying to standing.
B) Incorrect. Diarrhea is not a common side effect of amitriptyline.
C) Incorrect. Weight gain is more commonly associated with amitriptyline, not weight loss.
D) Incorrect. Excessive salivation is not a typical side effect of amitriptyline.
A client receiving risperidone reports severe muscle stiffness at 1030. By 1200, the client has difficulty swallowing food and is drooling. The client is diaphoretic. By 1600, vital signs are as follows Temperature 102.8 F pulse 110 beats/minute, respirations 26 breaths/minute, and blood pressure 150/90 mmHg.
What is the nurse's best analysis and action?
Explanation
A) Incorrect. Reverse isolation is not indicated in this situation. The client's symptoms are likely due to a side effect of the medication, not an infectious process.
B) Incorrect. While it may be necessary to withhold the next dose of medication, the client's symptoms require more immediate attention.
C) Incorrect. The client's symptoms are indicative of a serious adverse reaction, and dietary changes would not address the issue.
D) Correct. The client's symptoms, including severe muscle stiffness, difficulty swallowing, drooling, diaphoresis, and elevated vital signs, are indicative of neuroleptic malignant syndrome (NMS), a potentially life-threatening side effect of antipsychotic medications like risperidone.
The nurse should notify the healthcare provider immediately for further guidance and intervention.
A newly admitted client has a diagnosis of schizoaffective disorder. Based on this diagnosis, the nurse would expect to find which of the following symptoms?
Explanation
A) Correct. Schizoaffective disorder is characterized by a combination of symptoms of schizophrenia (such as delusions and hallucinations) and mood disorders (such as depression or mania).
B) Incorrect. Waxy flexibility and catatonic excitement are more commonly associated with catatonic schizophrenia, not schizoaffective disorder.
C) Incorrect. Bizarre mannerisms and hostility may be seen in various psychiatric disorders but are not specific to schizoaffective disorder.
D) Incorrect. While agitation and ideas of reference can occur in schizoaffective disorder, they are not the defining features of this diagnosis.
A client is showing symptoms of alcohol intoxication. What question should the nurse ask first?
Explanation
A) Incorrect. While understanding if the client is experiencing a relapse is important, knowing the timing of the last drink is crucial for assessing the level of intoxication.
B) Correct. Knowing the time of the last drink helps the nurse gauge the current level of alcohol in the client's system, which is crucial in assessing and managing alcohol intoxication.
C) Incorrect. While understanding the duration of the client's problem with alcohol is important, it is not the most immediate concern when the client is showing symptoms of intoxication.
D) Incorrect. Asking about liver problems is relevant but not the first priority when the client is exhibiting signs of alcohol intoxication.
A physician has prescribed an antidepressant medication for a 15yearold client. Which statement would be appropriate for inclusion in medication teaching?
Explanation
A) Incorrect. This statement does not provide relevant information about the medication or potential risks.
B) Incorrect. This statement is not accurate and may cause unnecessary concern or confusion for the client.
C) Correct. Adolescents and young adults prescribed with antidepressant medications should be informed about the potential increased risk of suicidal thoughts or behaviors, especially in the early stages of treatment. This information is important for the client's safety and allows for appropriate monitoring.
D) Incorrect. Doubling the dose if a dose is missed is not a safe or appropriate practice. The client should be instructed on what to do if they miss a dose according to their healthcare provider's instructions.
The nurse receives report on a male client diagnosed with schizoaffective disorder and is informed that the client's verbal communication includes "circumstantiality." What intervention is most therapeutic when caring for this client?
Explanation
A) Incorrect. Allowing the client to continue at his own pace may not effectively address the issue of circumstantiality and could lead to prolonged, tangential conversations.
B) Correct. Redirecting the conversation can help the client refocus and stay on topic, which can be particularly helpful for someone experiencing circumstantiality.
C) Incorrect. Stopping the client and telling him how his conversation sounds to others may be perceived as confrontational and could potentially be distressing for the client.
D) Incorrect. Reflecting is a useful communication technique, but it may not be the most effective intervention for addressing circumstantiality in this scenario.
A client is prescribed risperidone 4 mg PO twice daily. After the client is caught cheeking medications, liquid medication is prescribed. Available is risperidone 0.5 mg/mL. How many milliliters would be administered daily?
(Write the number only, do not include the label Record the answer to the nearest whole number. Do not use a trailing zero.)
Explanation
- The client needs to take 8 mg of risperidone per day in liquid form.
- The concentration of the liquid medication is 0.5 mg/mL.
- To calculate the daily dose in milliliters, divide the total milligrams by the concentration.
- 8 mg / 0.5 mg/mL = 16 mL
- The answer is 16. This is the number of milliliters that would be administered daily.
What client population is at risk of developing tardive dyskinesia?
Explanation
A) Correct. Tardive dyskinesia is a side effect of long-term neuroleptic (antipsychotic) treatment. It is characterized by involuntary, repetitive movements, particularly of the face and tongue. This condition is more commonly seen in clients who have been on neuroleptics for extended periods.
B) Incorrect. Discontinuing neuroleptic treatment may lead to withdrawal symptoms or symptom recurrence, but it does not directly increase the risk of developing tardive dyskinesia.
C) Incorrect. Neuroleptic malignant syndrome (NMS) is a different side effect associated with neuroleptic medications, characterized by hyperthermia, autonomic dysregulation, altered mental status, and generalized muscle rigidity.
D) Incorrect. Monoamine oxidase inhibitors (MAOIs) are a different class of medications and are not associated with the development of tardive dyskinesia.
The nurse is caring for a client who is withdrawing from long-term use of opioids. The nurse will monitor using a Clinical Opioid Withdrawal Scale (COWS). Which of the following cluster of symptoms would indicate to the nurse the client was withdrawing from opioids?
Explanation
A) Correct. These symptoms are indicative of opioid withdrawal. Opioid withdrawal symptoms include sweating (diaphoresis), goosebumps (piloerection), tremors, irritability, insomnia, and gastrointestinal symptoms like nausea and vomiting.
B) Incorrect. These symptoms are more indicative of withdrawal from substances like alcohol or benzodiazepines, rather than opioids.
C) Incorrect. These symptoms are not specific to opioid withdrawal and may be seen in various conditions.
D) Incorrect. This cluster of symptoms is not characteristic of opioid withdrawal.
An 80 year-old client, together with his daughter, arrived at the medical surgical unit for diagnostic confirmation and management of probable delirium. Which statement by the client's daughter best supports the diagnosis?
Explanation
A) Incorrect. While aging can contribute to cognitive changes, it is not the primary factor in the acute onset of delirium.
B) Correct. This statement highlights the acute and rapid onset of behavioral changes, which is characteristic of delirium. Delirium is an acute confessional state characterized by alterations in cognition, attention, and level of consciousness. It often has a sudden onset.
C) Incorrect. Chronic forgetfulness may be indicative of dementia or other cognitive disorders, but it does not support the acute onset seen in delirium.
D) Incorrect. Independence and living alone do not directly relate to the acute onset of delirium.
A nurse is planning to run a group for clients diagnosed with paranoia and schizophrenia on an acute care mental health unit. Which of the following actions should the nurse plan to take to create a therapeutic environment?
Explanation
A) Incorrect. While discussing various topics is important, providing continuity of care is more crucial in creating a therapeutic environment for clients with paranoia and schizophrenia.
B) Incorrect. Focusing on client strengths rather than weaknesses is generally a more effective approach in mental health care.
C) Correct. Providing continuity of care by assigning the same staff helps build trust and a sense of security for clients, especially those with paranoia and schizophrenia.
D) Incorrect. While it's important to establish boundaries, allowing the client to solely determine them may not always be in their best interest.
A nurse is preparing to administer fluoxetine 80 mg PO daily. Available is fluoxetine 40 mg/5mL. How many mL should the nurse administer per dose?
(Write the number only, do not include the label. Record the answer to the nearest whole number. Do not use a trailing zero)
Explanation
Dose (mL) = Desired dose (mg) / Available dose (mg/mL) Plugging in the values from the question, we get:
Dose (mL) = 80 mg / (40 mg / 5 mL) Simplifying the fraction, we get:
Dose (mL) = 80 mg / 8 mg/mL Dividing both sides by 8, we get:
Dose (mL) = 10 mL
Therefore, the nurse should administer 10 mL of fluoxetine per dose.
A newly admitted client diagnosed with paranoid schizophrenia is super vigilant and constantly scans the environment. The client states, "I saw doctors talking in the hall. They were plotting to kill me." Which of the following does the nurse correctly identify as this behavior?
Explanation
A) Correct. An idea of reference is a false belief that ordinary events, objects, or behaviors of others have a particular and unusual meaning directly pertaining to oneself. In this case, the client believes that the doctors' conversation in the hall is about them.
B) Incorrect. A delusion of infidelity involves a false belief that one's partner is being unfaithful.
C) Incorrect. Auditory hallucinations involve hearing things that are not present.
D) Incorrect. Echolalia is the repetition of another person's words.
A nurse is providing teaching for a client who has schizophrenia and a new prescription for risperidone. Which of the following statements should the nurse include in the teaching?
Explanation
B) Correct. Risperidone can lead to an increased risk of hypertension, so it's important for the client to monitor their blood pressure regularly. This is crucial information for the client's safety and wellbeing.
A) Incorrect. While maintaining proper fluid and fiber intake is generally important for overall health, it's not directly related to risperidone.
C) Incorrect. There is no specific indication for weekly blood checks for electrolyte imbalances with risperidone.
D) Incorrect. While addressing weight concerns can be important, it's not a direct result of risperidone use.
A nurse is providing teaching for a client who has schizophrenia and a new prescription for risperidone. Which of the following statements should the nurse include in the teaching?
Explanation
A) Incorrect. While maintaining proper nutrition is important, this statement is not directly related to the use of risperidone.
B) Correct. Risperidone, an atypical antipsychotic, can be associated with metabolic side effects, including hypertension. Therefore, monitoring blood pressure is important.
C) Incorrect. While regular monitoring of blood parameters may be necessary for some medications, it is not a specific requirement for risperidone.
D) Incorrect. While weight changes can occur with risperidone, there is no specific indication to increase caloric intake in this context.
The mother of a 20yearold woman recently diagnosed with paranoid schizophrenia asks the nurse what causes schizophrenia. The nurse recognizes which of the following are implicated in the etiology of schizophrenia?
Explanation
A) Incorrect. Thyroxine is a hormone produced by the thyroid gland and is not directly implicated in the etiology of schizophrenia.
B) Incorrect. Erythropoietin is a hormone that stimulates the production of red blood cells and is not directly implicated in the etiology of schizophrenia.
C) Correct. Glutamate, an excitatory neurotransmitter, has been implicated in the development of schizophrenia. Abnormalities in glutamate signaling have been identified in individuals with schizophrenia.
D) Incorrect. While serotonin abnormalities have been associated with mood disorders such as depression, they are not considered a primary factor in the etiology of schizophrenia.
A nurse is providing teaching for a client who has schizophrenia and a new prescription for risperidone. Which of the following statements should the nurse include in the teaching?
Explanation
A) Incorrect. While maintaining proper nutrition is important, this statement is not directly related to the use of risperidone.
B) Correct. Risperidone, an atypical antipsychotic, can be associated with metabolic side effects, including hypertension. Therefore, monitoring blood pressure is important.
C) Incorrect. While regular monitoring of blood parameters may be necessary for some medications, it is not a specific requirement for risperidone.
D) Incorrect. While weight changes can occur with risperidone, there is no specific indication to increase caloric intake in this context.
A client has been admitted to a psychiatric mental health facility in a manic state. The client's spouse accompanies the client to the facility and informs the nurse that the client has been displaying manic symptoms for the past 2 weeks. The spouse reports that the client has not slept for the past 2 days, and that the client has not eaten anything for at least 3 days.
Which would be the priority nursing diagnosis for this client?
Explanation
A) Incorrect. While the client's sleep disturbance and lack of selfcare may contribute to
ineffective health maintenance, the more immediate concern is addressing the risk of imbalanced nutrition.
B) Incorrect. While clients in a manic state may exhibit hyperactivity and impulsivity, there is no indication in the scenario that the client poses an immediate risk for other-directed violence.
C) Correct. The client's reported lack of sleep and refusal to eat for an extended period raises concerns about nutritional deficits and dehydration. This is the most immediate and pressing issue to address.
D) Incorrect. While the client's manic state may increase the risk of impulsive behavior, there is no specific indication in the scenario that the client is at immediate risk for suicide.
A client was admitted to the intensive care unit after a single car accident in which he struck a cement wall. He is now responsive and wants to be discharged within the next couple of days. Which of the following are priorities for screening? (Select all that apply)
Explanation
A) Correct. Given the nature of the accident, there is a high risk for traumatic brain injury. This should be a priority for screening and assessment.
B) Incorrect. While chronic pain may be a concern, it is not directly related to the recent accident and is not a priority for screening at this time.
C) Incorrect. Sexual dysfunction is not directly related to the recent accident and is not a priority for screening at this time.
D) Correct. The client's request for early discharge and the recent traumatic event raise concerns about potential depression. Screening for depression is important.
E) Incorrect. Effective coping strategies are important, but they are not a priority for screening in this scenario.
F) Correct. Given the recent accident and the client's expressed desire for early discharge, there may be an increased risk for suicide. This should be a priority for screening and assessment.
A nurse is caring for a client who exhibits manifestations of major depressive disorder. The provider wants to rule out any other medical conditions that may be contributing or causing the symptoms. Which diagnostic test should the nurse expect to be ordered?
Explanation
A) Incorrect. While kidney function is important for overall health, it is not the primary focus for ruling out medical conditions contributing to major depressive disorder.
B) Correct. Thyroid function can significantly impact mood and energy levels. Abnormalities in thyroid function can sometimes present with symptoms similar to depression, so a thyroid panel (including TSH, T3, and T4 levels) is an important test to consider.
C) Incorrect. While liver function is important for overall health, it is not the primary focus for ruling out medical conditions contributing to major depressive disorder.
D) Incorrect. A urinalysis with culture is not a standard test for ruling out medical conditions contributing to major depressive disorder. It is more relevant for assessing urinary tract infections or kidney function.
A client is admitted to the emergency department after using ecstasy. The nurse identifies this drug as belonging to what class?
Explanation
A) Correct. Ecstasy, also known as MDMA (3,4methylenedioxymethamphetamine), belongs to the hallucinogen class of drugs. It produces altered perceptions and sensations.
B) Incorrect. Hypnotics are drugs that promote sleep.
C) Incorrect. Opioids are a class of drugs that include substances like heroin and prescription pain medications.
D) Incorrect. Sedatives are drugs that calm or soothe and can also induce sleep.
When assessing a client immediately following electroconvulsive therapy (ECT), the nurse expects what side effect in a client?
Explanation
A) Correct. Confusion is a common side effect following ECT. It is usually temporary and gradually resolves.
B) Incorrect. Long-term memory impairment is a potential side effect of ECT, but it is not immediate and is more of a concern with repeated sessions.
C) Incorrect. Feeling full of energy would not be an expected immediate side effect of ECT.
D) Incorrect. Numbness and tingling in the extremities are not typically associated with ECT.

A client is admitted to the hospital for alcohol intoxication. The family reports that he is a heavy drinker and has been admitted several times for alcohol detoxification. When can the nurse expect to observe the first symptoms of withdrawal?
Explanation
A. 24 hours is a long time for alcohol withdrawal symptoms to occur.
B. Alcohol withdrawal symptoms typically begin within 6 to 8 hours after the last drink for
individuals with a history of heavy alcohol use. These symptoms can range from mild anxiety and tremors to more severe symptoms like seizures and delirium tremens. It's crucial for
healthcare providers to monitor and manage alcohol withdrawal symptoms, as they can be life- threatening in severe cases.
C. Alcohol withdrawal symptoms occur within 6 to 8 hours, not 18 hours.
D. Alcohol withdrawal symptoms occur within 6 to 8 hours, not 72 hours.
The nurse is caring for a client diagnosed with premenstrual dysphoric disorder. What is the primary manifestation of this disorder?
Explanation
A. Loss of appetite can be a symptom of PMDD, but it is not the primary manifestation.
B. Insomnia can be a symptom of PMDD, but it is not the primary manifestation.
C. Emotional lability, or rapid and intense mood swings, is a primary manifestation of PMDD.
D. Anxiety can be a symptom of PMDD, but it is not the primary manifestation.
A client diagnosed with bipolar II disorder has a problem statement of impaired social
interactions related to egocentrism. Which short-term correctly written outcome is an appropriate expectation for this client problem?
Explanation
A. This outcome is specific, measurable, and timebound. It addresses the client's impaired social interactions and sets a realistic expectation for improvement within a short timeframe.
B. While this outcome is specific, it may not be achievable within a short timeframe and may not directly address the issue of egocentrism.
C. This outcome focuses on verbalization but may not necessarily lead to actual interaction or address the issue of egocentrism.
D. While this outcome is relevant, it is not as specific or timebound as option A.
The nurse states in report that the client is experiencing positive symptoms of schizophrenia. What symptoms would the nurse receiving report expect to observe?
Explanation
A. Flat affect (lack of emotional expression) and hygiene needs are negative symptoms, not positive symptoms.
B. Social isolation and anhedonia (inability to experience pleasure) are also negative symptoms, not positive symptoms.
C. Positive symptoms involve the presence of abnormal experiences or behaviors that are not present in healthy individuals. Hallucinations (perceiving things that aren't there) and delusions (strongly held false beliefs) are examples of positive symptoms.
D. Withdrawal (lack of interest or participation in social activities) and avolition (lack of motivation) are negative symptoms, not positive symptoms.
What intervention is a priority when the client is experiencing auditory hallucinations?
Explanation
A. While understanding precipitating factors is important, it is not the immediate priority when the client is actively experiencing hallucinations.
B. Distracting the client may not address the underlying cause of the hallucinations, which should be the priority.
C. Determining the content of the hallucinations can provide important information for assessment and intervention.
D. Dismissing the client's experience can be alienating and unhelpful.
A client with schizophrenia has received standard antipsychotics for a year. His hallucinations are less intrusive, but the client remains apathetic, has poverty of thought, cannot work, and is socially isolated.
To address these symptoms, the nurse might expect the psychiatrist to prescribe which medication?
Explanation
A. Haloperidol is a first-generation antipsychotic and may not be as effective in addressing the negative symptoms (e.g., apathy, poverty of thought) as second-generation antipsychotics.
B. Olanzapine is a second-generation antipsychotic known to be effective in treating both positive and negative symptoms of schizophrenia.
C. Diphenhydramine is not typically used as a primary treatment for schizophrenia.
D. Chlorpromazine is a first-generation antipsychotic and may not be as effective in addressing the negative symptoms as second-generation antipsychotics.
What intervention is a priority when the client is experiencing auditory hallucinations?
Explanation
A. While understanding precipitating factors is important, it is not the immediate priority when the client is actively experiencing hallucinations.
B. Distracting the client may not address the underlying cause of the hallucinations, which should be the priority.
C. Determining the content of the hallucinations can provide important information for assessment and intervention.
D. Dismissing the client's experience can be alienating and unhelpful.
What are the possible physiological changes in the brain of a client diagnosed with Alzheimer's disease? (Select all that apply)
Explanation
A. Brain atrophy is a common physiological change in the brain of individuals with Alzheimer's disease.
B. An overabundance of plaques, specifically amyloid beta, is a characteristic feature of Alzheimer's disease.
C. An overabundance of tangles, specifically tau protein, is also a characteristic feature of Alzheimer's disease.
D. Enlargement of the hippocampus is not typically associated with Alzheimer's disease; rather, it tends to shrink.
E. Enlarged cerebral cortex is not a typical physiological change in Alzheimer's disease; it actually tends to shrink.
A client diagnosed with schizophrenia is experiencing delusions of persecution. How would the client express feeling persecuted?
Explanation
A. This option describes a feeling of burden, but it doesn't specifically address persecution.
B. This option describes a delusion involving a familial relationship with a public figure, but it doesn't specifically address persecution.
C. This option describes a command hallucination, which can be related to violence, but it doesn't directly address feeling persecuted.
D. This option directly addresses the feeling of persecution by believing a powerful agency is actively seeking to harm the client.
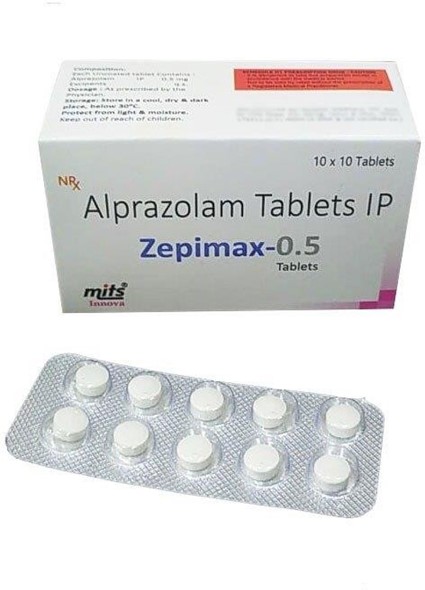
A client asks the nurse to give her information regarding the detoxification process of alprazolam. What is the best response by the nurse?
Explanation
A. This option is too vague and doesn't provide specific guidance about the detoxification process for alprazolam.
B. Frequency of usage is one factor, but it's not the only consideration in the detoxification process.
C. A planned reduction is necessary to safely taper off alprazolam and minimize withdrawal symptoms.
D. This option provides the best guidance, emphasizing the importance of a gradual and controlled tapering process for alprazolam.
The nurse observes a client drooling during mealtime. The client complains that his tongue feels swollen, and his jaw feels tight. What is the first action by the nurse?
Explanation
A. While medication review may be necessary, the immediate concern is the client's current symptoms and potential need for urgent intervention.
B. Encouraging the client to eat more slowly does not address the urgent nature of the client's symptoms.
C. "Assessment security" is not a standard term or intervention. It does not provide specific guidance for addressing the client's symptoms.
D. Given the client's complaints of swelling and tightness, along with difficulty swallowing, further assessment is needed to determine the cause. This information should be reported to the provider promptly.
Which of the following is the most therapeutic response by the nurse when a client states, "I no longer need my medication since I do not hear voices"?
Explanation
A. This response may be seen as evading the client's statement. It's important to provide a more direct response.
B. This response may come across as controlling or confrontational, which may not promote open communication.
C. This response is a good therapeutic technique as it encourages the client to reflect on past experiences with stopping medication.
D. This response provides a clear and factual statement about the purpose of the prescribed medication, encouraging the client to understand its importance.
A client with chronic alcoholism has been found to have Wernicke encephalopathy. What is this irreversible complication characterized by?
Explanation
A. Wernicke encephalopathy is caused by thiamine (Vitamin B1) deficiency, but it is not characterized by thiamine deficiency itself.
B. Wernicke encephalopathy is characterized by lesions in the hypothalamus and mammillary bodies in the brain.
C. While cognitive impairment may be present, this is not the primary characteristic of Wernicke encephalopathy.
D. Double vision and rapid eye movement are symptoms of Wernicke encephalopathy, but they are not the irreversible complication itself.
The nurse is caring for a client with poor self-esteem. What intervention would be important for the nurse to include in the plan of care?
Explanation
A. Encouraging descriptions of perceived failures may further exacerbate the client's poor self- esteem and is not a therapeutic intervention.
B. While setting limits is important in managing behavior, it may not directly address the underlying issue of poor self-esteem.
C. Providing activities that can be accomplished can help boost the client's confidence and self- esteem.
D. Teaching aggressive communication skills is not appropriate and may contribute to further negative self-perception.
A 70yearold client is admitted to the locked psychiatric unit, diagnosed with delirium. Later in the day, he tries to get out of the locked unit several times. He yells, "I have to leave and get to my barber. I see him every Wednesday. Let me out!"
Which of the following would be the most therapeutic response by the nurse?
Explanation
A. This response does not directly address the client's concern and may be perceived as dismissive.
B. This response does not provide a clear explanation for the locked door and may not effectively address the client's agitation.
C. This response provides a clear and honest explanation for the locked door, ensuring the client's safety, which is the priority.
D. This response acknowledges the situation but does not provide a clear explanation for the locked door.
Benztropine is ordered as needed (PRN) for a client taking haloperidol after being diagnosed with schizoaffective disorder.
Which of the following assessments by the nurse would indicate a need for this medication?
Explanation
A. Increasing aggression may be an indication for a PRN medication, but benztropine specifically targets extrapyramidal symptoms (EPS).
B. Elevated blood pressure is not a direct indication for benztropine; it is used to address EPS.
C. Complaints of dizziness may not be directly related to EPS, which is the target of benztropine.
D. Benztropine is an anticholinergic medication used to manage extrapyramidal symptoms (EPS) associated with antipsychotic medications like haloperidol.
During the admission interview for a client with schizophrenia, the nurse asks the client "tell me the names of the medications you are currently taking. The client responds, medications, abbreviations, deviations, mediations." The nurse will document which form of speech pattern the client is demonstrating?
Explanation
A. Neologisms are new words or expressions created by the individual, often with personal meaning only they understand.
B. Echolalia is the repetition of words or phrases spoken by others, often without apparent understanding.
C. Pressured speech is rapid and continuous speech without pauses, often difficult to interrupt.
D. Clang association is the meaningless rhyming of words, often driven by sound rather than meaning.
While caring for a depressed client, a nurse would evaluate the need for suicide precautions under which circumstance?
Explanation
A. Agitation can be a sign of distress, but sudden cheerfulness may be indicative of a decision to act on suicidal thoughts, as the individual may feel relieved to have made a decision.
B. Sudden cheerfulness can be a concerning sign, as it may indicate that the client has made a decision to carry out suicidal thoughts.
C. Psychomotor retardation is a symptom of depression and may not necessarily indicate imminent risk of suicide.
D. Not attending group therapy may be a sign of withdrawal or isolation, but it does not directly indicate immediate suicidal risk.
A client on the mental health unit has disorganized type schizophrenia. The nurse observes blunted affect and social isolation. He occasionally curses or calls another client a "jerk" without provocation. The nurse asks the client how he is feeling, and he responds, "Everybody picks on me. They frobitz me." The client's communication exhibits ______________
Explanation
A. Neologisms are new words or expressions created by the individual, often with personal meaning only they understand. "Frobitz" is an example of a neologism.
B. Loose associations involve a lack of logical connection between thoughts and ideas, leading to disjointed or incoherent speech.
C. Delusional thinking involves holding false beliefs that are resistant to reason or contradictory to evidence.
D. Circumstantial speech involves excessive and unnecessary detail before getting to the point of a conversation.
The nurse is caring for a client who has become increasingly agitated. He is pacing in the hallway and shouting at other clients. What is the priority action of the nurse?
Explanation
A. Attempting to deescalate the client is important, but ensuring immediate safety is the top priority.
B. Continuing to observe the client may lead to a further escalation of the situation. Safety measures should be taken first.
C. While offering medications may be necessary, ensuring safety is the immediate priority before any interventions are implemented.
D. Ensuring the safety of the client and others is the priority in situations of escalating agitation.
While conducting an admission interview with a client, the nurse suspects the client may be in alcohol withdrawal. Which screening tool can help the nurse identify the severity of withdrawal symptoms?
Explanation
A. The Michigan Alcohol Screening Test (MAST) is a tool used to screen for alcohol abuse or dependence, but it does not specifically assess withdrawal symptoms.
B. The CAGE questionnaire is used to screen for alcohol abuse, but it does not assess withdrawal symptoms.
C. The Clinical Institute Withdrawal Assessment for Alcohol (CIWA) is a validated tool used to assess the severity of alcohol withdrawal symptoms. It includes various criteria such as agitation, tremor, and hallucinations.
D. The Delirium Rating Scale (DMSE) is used to assess the severity of delirium, which can be caused by various factors including alcohol withdrawal, but it is not specific to alcohol withdrawal.
The nurse is monitoring a client who abuses alcohol for signs of alcohol withdrawal delirium. The nurse would monitor for which symptoms?
Explanation
A. These symptoms are not characteristic of alcohol withdrawal delirium.
B. Alcohol withdrawal delirium is characterized by symptoms such as hypertension, disorientation, and hallucinations.
C. Hypotension and bradycardia are not typically associated with alcohol withdrawal delirium. They may be seen in other types of alcohol withdrawal.
D. These symptoms are not specific to alcohol withdrawal delirium. They may be present in other forms of alcohol withdrawal.
Which statement made by the nurse would be most appropriate to an elderly client who is confused, has no history of dementia and is hospitalized for an acute urinary tract infection?
Explanation
A. This statement may cause unnecessary distress to the client and is not necessarily true in this situation.
B. While the confusion may be temporary, this statement may not provide enough reassurance or information.
C. This statement may not be accurate or helpful in addressing the client's concerns about confusion.
D. This statement provides reassurance and offers a positive outlook, indicating that the confusion is likely to improve as the client's condition gets better.
A nurse in the emergency department is implementing a plan of care for an older adult client who is experiencing delirium tremens. Which of the following actions should the nurse take first?
Explanation
A. Administering diazepam may be part of the treatment plan for delirium tremens, but ensuring adequate hydration and addressing potential electrolyte imbalances is the first priority.
B. Raising the side rails is important for safety, but it is not the highest priority action at this time.
C. Obtaining a medical history is important for comprehensive care, but in this urgent situation, addressing fluid and electrolyte balance is the first priority.
D. Starting intravenous fluids is crucial for rehydration and addressing potential electrolyte imbalances, which is the priority in this emergency situation.
An older adult in the middle and late stages of Alzheimer's forgets where the bathroom is and has episodes of incontinence. Which intervention should the nurse suggest to the client's family?
Explanation
A. Labeling the bathroom door can provide a visual cue to help the older adult locate the bathroom, which may reduce episodes of incontinence.

B. Taking the older adult to the bathroom hourly is a good strategy, but it may not always be feasible or effective in preventing accidents.
C. Using disposable adult briefs may be necessary at times, but it should not be the first line intervention.
D. Limiting oral fluids to 1000 mL/day may lead to dehydration and is not an appropriate intervention for addressing incontinence.
An older adult in the middle and late stages of Alzheimer's forgets where the bathroom is and has episodes of incontinence. Which intervention should the nurse suggest to the client's family?
Explanation
A. Labeling the bathroom door can provide a visual cue to help the older adult locate the bathroom, which may reduce episodes of incontinence.
B. Taking the older adult to the bathroom hourly is a good strategy, but it may not always be feasible or effective in preventing accidents.
C. Using disposable adult briefs may be necessary at times, but it should not be the first line intervention.
D. Limiting oral fluids to 1000 mL/day may lead to dehydration and is not an appropriate intervention for addressing incontinence.
Which nursing documentation entry accurately describes a client's use of confabulation?
Explanation
Confabulation involves the fabrication of details or events to fill in gaps in memory. In this case, the client is expressing happiness about a trip to the park that did not actually occur, which is an example of confabulation.
A client is hospitalized following a suicide attempt after breaking up with her significant other.
The client says to the nurse, "When I get out of here, I'm going to try this again, and next time I'll get it right?" Which is the best response by the nurse?
Explanation
A. While providing reassurance is important, this response does not directly address the client's statement about future attempts.
B. This response may minimize the seriousness of the client's statement and is not the best way to address the situation.
C. This response directly addresses the client's statement, seeking clarification on her plans. It is important to assess the level of risk and ensure the client's safety.
D. While expressing empathy and highlighting the client's positive qualities can be helpful, it may not directly address the immediate concern of the client's statement about future attempts.
A nurse suspects the client is experiencing delirium. Which of the following assessment findings would support the nurse's suspicion?
Explanation
A. Delirium is characterized by a fluctuating level of consciousness, which can include periods of hypervigilance.
B. A slow onset of confusion and agitation is more characteristic of dementia rather than delirium.
C. A decrease in output and vital signs may indicate a different condition, but it is not specific to delirium.
D. Delirium is characterized by an acute onset and is typically short-lived, usually lasting days to weeks. Symptoms lasting longer than a month would suggest a different diagnosis.
A client with schizophrenia has begun a new prescription of clozapine. The nurse should assess the result of which laboratory study to monitor for adverse effects?
Explanation
A. Kidney function studies While monitoring kidney function is important for clients on certain medications, it is not the primary laboratory test for monitoring clozapine. Clozapine is associated with agranulocytosis, which affects white blood cell count.
B. Red blood cell count Monitoring red blood cell count is not the primary concern when a client is prescribed clozapine. The main concern with clozapine is agranulocytosis, which affects white blood cells.
C. Liver function studies While liver function is important to monitor with some medications, it is not the primary laboratory test for monitoring clozapine. The primary concern with clozapine is agranulocytosis, which affects white blood cell count.
D. White blood cell count Clozapine is associated with agranulocytosis, a potentially life- threatening condition characterized by a severe decrease in white blood cells. Regular
monitoring of white blood cell count is crucial to detect and prevent this adverse effect. This test should be performed before starting clozapine and regularly throughout treatment. If the white blood cell count drops significantly, clozapine may need to be discontinued. This makes it the
most important laboratory study to monitor when a client is prescribed clozapine.
A 28-year old male admitted with catatonic schizophrenia has been mute and motionless for several days while at home prior to admission. He still appears stuporous in the hospital. Which nursing intervention would be an initial priority?
Explanation
A. Orienting the client to the unit While orientation is important, the client's prolonged
immobility and stupor necessitate a physical assessment first to ensure there are no underlying medical issues contributing to this state.
B. Reinforcing reality with the client The client's catatonic state may make it difficult to effectively communicate or engage in reality orientation at this point. Addressing potential physical issues is the initial priority.
C. Establishing a nonthreatening relationship Building a therapeutic relationship is crucial, but given the client's current state, assessing for physical problems takes precedence.
D. Assessing the client for physical problems The client's prolonged catatonic state requires an
immediate physical assessment to rule out any underlying medical conditions contributing to his condition.
A client diagnosed with major depressive disorder is considering cognitive behavioral therapy. The client asks the nurse how this therapy would help alleviate depressive thoughts. What is the best response by the nurse?
Explanation
A. "This therapy helps you learn to think more positively, and thereby reduce depressive
thoughts and symptoms." Cognitive behavioral therapy (CBT) aims to identify and challenge negative thought patterns and replace them with more positive and realistic thinking, which can help alleviate symptoms of depression.
B. "In this therapy, you will explore past events and analyze how these events have affected your behavior and thoughts." This description is more characteristic of psychodynamic therapy, not cognitive behavioral therapy.
C. "This type of therapy focuses on how you use defense mechanisms to feel more comfortable and content." This description aligns more with psychodynamic therapy, not cognitive behavioral therapy.
D. "The purpose of this therapy is to determine how to get psychological needs met through
interpersonal relationships." This statement does not accurately describe cognitive behavioral
therapy, which primarily focuses on identifying and changing maladaptive thought patterns and behaviors.
A client diagnosed with major depressive disorder with psychotic features hears voices commanding self harm. The client refuses to commit to developing a plan for safety. What should be the nurse's priority intervention at this time?
Explanation
A. Placing the client on one-on-one observation while monitoring for suicidal ideations Given that the client is experiencing auditory hallucinations commanding self harm and is refusing to commit to a safety plan, one-on-one observation is necessary to ensure the client's safety. This
intervention provides constant monitoring and allows for immediate intervention if self harm is attempted.
B. Conducting 15minute checks to ensure safety While conducting regular safety checks is
important, in this case, more continuous monitoring is required due to the severity of the client's symptoms.
C. Encouraging the client to verbalize feelings related to suicide While encouraging communication is essential, in this urgent situation, immediate safety measures take precedence.
D. Completing a room search to ensure there are no harmful objects available to the client
Ensuring the environment is safe is important, but it should be done in conjunction with one-on- one observation to provide the highest level of safety for the client.
An adult in the emergency department states, "Everything I see appears to be waving. I am outside my body looking at myself. I think I'm losing my mind." Vital signs are slightly elevated. What does the nurse suspect?
Explanation
A. A schizophrenic episode Schizophrenic episodes are characterized by a complex interplay of symptoms including delusions, hallucinations, disorganized thinking, and altered perceptions. While the client is experiencing altered perceptions, the sudden onset and specific description are more indicative of hallucinogen ingestion.
B. Hallucinogen ingestion The client's description of altered perception, feeling outside of their own body, and visual distortions are indicative of hallucinogen ingestion. This class of substances can cause profound alterations in perception, leading to hallucinations and distorted sensory experiences. The slightly elevated vital signs may be a physiological response to the effects of the hallucinogen.
C. Opium intoxication Opium is an opioid and its effects are characterized by sedation, respiratory depression, and miosis (pupil constriction). The client's description of altered perception and feeling outside of their body are not typical of opium intoxication.
D. Cocaine overdose Cocaine is a stimulant and its effects are characterized by increased heart rate, blood pressure, and hyperarousal. The client's description of altered perception and feeling outside of their body are not typical of cocaine overdose.
A client is admitted with tachycardia, hypertension, restlessness, agitation, and admits substance use. Which substance would be most likely to cause these symptoms?
Explanation
A. A depressant Depressants typically slow down the central nervous system, leading to
symptoms like sedation, slowed heart rate, and reduced blood pressure. The symptoms described in the question, such as tachycardia, hypertension, restlessness, and agitation, are not
characteristic of depressant use.
B. An opioid Opioids primarily lead to central nervous system depression, resulting in symptoms like respiratory depression, sedation, and decreased heart rate. The symptoms described in the question, such as tachycardia and restlessness, are not typical of opioid use.
C. A stimulant Stimulants, such as amphetamines or cocaine, lead to increased activity in the central nervous system, resulting in symptoms like tachycardia, hypertension, restlessness, and agitation. These symptoms align with the presentation described in the question.
D. An inhalant Inhalants can lead to a variety of effects, including dizziness, confusion, and sometimes increased heart rate. However, they are not typically associated with the specific symptoms of tachycardia, hypertension, restlessness, and agitation described in the question.
The nurse is admitting a client with a dual diagnosis of major depressive disorder and alcohol abuse. What is the primary intervention?
Explanation
A. Administer thiamine intramuscular (IM) Administering thiamine is important, especially in
clients with alcohol abuse, to prevent or treat potential Wernicke Korsakoff syndrome. However, the primary intervention when admitting a client is addressing immediate physical and psychological needs, such as personal hygiene.
B. Assist the client with personal hygiene needs This is the primary intervention upon admission.
It addresses the client's immediate physical and psychological wellbeing and helps establish a therapeutic rapport.
C. Place the client on continuous observation While observation may be necessary for safety, it is not the primary intervention in this scenario. Addressing personal hygiene needs takes precedence.
D. Explain milieu therapy Milieu therapy is an important aspect of a comprehensive treatment plan, but it is not the primary intervention upon admission. Immediate physical care and safety are the initial priorities.
A client is showing early signs of dementia. The client's spouse asks, "What may I expect next?" What is the nurse's best response?
Explanation
A. "He may begin to try to cover recognition of his memory loss by creating events." As
dementia progresses, individuals may experience confabulation, which involves creating false memories to compensate for memory loss. This is a common symptom seen in the middle stages of dementia.
B. "He may have difficulty in a motor skill such as walking." While motor skills may be affected in the later stages of dementia, it is not typically one of the early signs.
C. "The inability to communicate with speech comes immediately after the early signs." This statement is not accurate. Communication difficulties may occur in later stages, but it is not an immediate progression from early signs.
D. "He may not recognize you and other people who have been in his life." This symptom, known as agnosia, may occur in later stages of dementia, but it is not one of the early signs.
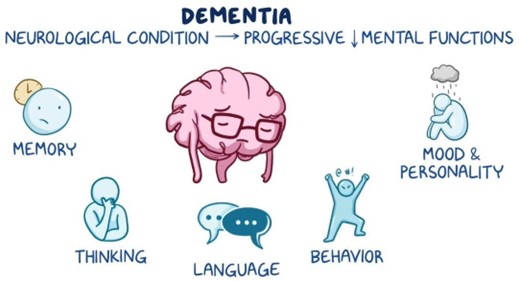
During the admission process, an elderly client is asked to present their license for identification purposes. The client gives the admission personnel their glasses. This is an example of which of the following symptoms of dementia?
Explanation
A. Anhedonia is a symptom commonly associated with depression, characterized by a decreased ability to experience pleasure or interest in activities.
B. Aphasia is a language disorder that affects the ability to communicate. It may involve difficulty in speaking, understanding language, reading, or writing. This is not demonstrated in the scenario.
C. Akathisia is a side effect of some antipsychotic medications characterized by a feeling of inner restlessness and the need to move constantly. It is not demonstrated in the scenario.
D. Agnosia is a symptom of dementia characterized by the inability to recognize familiar objects, people, or places, despite the senses being intact. In this scenario, the client's inability to recognize that their glasses are not a form of identification indicates agnosia.
A client has been prescribed lithium for long-term maintenance of bipolar disorder diagnosis. Which statement by the client shows an understanding of the medication?
Explanation
A. "Lab work is only needed at the start of taking the medication." This statement is incorrect. Regular monitoring of lithium levels and kidney function through lab work is crucial for ensuring the medication's effectiveness and preventing potential toxicity.
B. "Once I feel better, I will not need to take this medication anymore." This statement is incorrect. Lithium is typically prescribed for long-term maintenance in bipolar disorder to prevent relapses and stabilize mood.
C. "There is a chance I may become addicted to this medication." This statement is incorrect. Lithium is not addictive. It is a mood stabilizer used to manage bipolar disorder.
D. "I need to be aware of situations that may cause dehydration." This statement demonstrates an understanding of an important consideration with lithium. Dehydration can lead to an increase in lithium levels in the body, potentially leading to toxicity. It's important for clients taking lithium to stay well hydrated and be cautious in situations that may lead to dehydration.
The spouse of a client diagnosed recently with a mood disorder calls the nurse therapist to report a change in the client's mood. The spouse states, "My spouse is clearly in a better mood than usual. I would say my spouse seems mildly elated. They are functioning fine at work and home. My spouse is energetic, up and doing things at 500 a.m. and really confident again. It seems fantastic, but unusual. Is this something to worry about?"
Which potential response by the nurse accurately assesses the situation?
Explanation
A. "It sounds as though the antidepressants are working well. Just ask the client if the client is experiencing any side effects and let me know." This response does not adequately address the change in mood and the potential for hypomania. It assumes the change is solely due to the antidepressants.
B. "I'm concerned. Sometimes depressed people seem contented when they have decided to commit suicide. Let's schedule an appointment for tomorrow." While it's important to assess for suicidality, the description provided does not indicate immediate suicidal intent. The client's behavior is more indicative of hypomania.
C. "Since the client is eating, sleeping, and not behaving inappropriately, there's nothing to worry about. Just let me know if the client starts getting irritable or has trouble sleeping." This response downplays the significance of the mood change and does not address the potential for hypomania.
D. "The client sounds hypomanic. Let's schedule an appointment for this week for an evaluation. The client may need additional or different medication." This response correctly identifies the potential for hypomania and takes appropriate action by scheduling an evaluation. Adjusting the client's medication may be necessary to address the change in mood.
The nurse is teaching about obstacles to maintaining recovery. Which of the following statements would indicate to the nurse a greater risk for relapse? (Select all that apply.)
Explanation
A. "I don't have a problem, I can quit when, where and how I want to." This statement reflects denial and overconfidence, which are common obstacles to recovery. It suggests a lack of recognition of the seriousness of the addiction.
B. "I am not going to let my family and friends know I have an addiction and give them this burden." This statement indicates a reluctance to seek support from loved ones, which can hinder the recovery process. Keeping the addiction, a secret can lead to isolation and make it more
challenging to maintain recovery.
C. "I will start Alcoholic Anonymous meetings in two weeks when I am settled after discharge." This statement shows proactive planning and willingness to engage in support groups, which can be a positive step towards recovery.
D. "I know I am an addict, and it will take hard work and a higher power to help me." This statement reflects self-awareness and a recognition of the effort required for recovery. The
mention of a higher power suggests a willingness to engage in a spiritual or faith based approach to recovery, which can be beneficial for some individuals.
E. "I don't know how I am going to get through this but will take it one day at a time with my family." This statement acknowledges the challenges ahead and expresses a willingness to take recovery one step at a time with the support of family. It reflects a realistic and hopeful approach to the recovery process.
Which statement provides the best rationale for why a nurse should closely monitor a severely depressed client during antidepressant therapy?
Explanation
A. "As depression lifts, physical energy becomes available to carry out suicide." This statement highlights a critical consideration in the care of severely depressed clients. When a client's depression starts to improve due to antidepressant therapy, there may be a period where they have increased energy but have not yet gained full relief from their depressive thoughts. This can potentially increase the risk of carrying out suicidal thoughts or plans.
B. "Suicide may be precipitated by a variety of internal and external events." While this statement is true, it does not specifically address the importance of monitoring a client during antidepressant therapy.
C. "Suicidal clients have difficulty using social supports." This statement acknowledges a potential challenge for clients who are experiencing suicidal thoughts, but it does not directly relate to the need for close monitoring during antidepressant therapy.
D. "Suicide is an impulsive act that has no warning." This statement is not entirely accurate. While some suicides can be impulsive, many individuals give warning signs or exhibit changes in behavior before attempting suicide.
The nurse is building a discharge teaching plan with a client diagnosed with substance use disorder. Which of the following relapse prevention strategies will be included in the teaching? (Select all that apply)
Explanation
A. Establish a healthy sleeping, eating, and exercise routine This is an important relapse prevention strategy as it promotes physical and emotional wellbeing. A structured routine helps maintain stability and reduces the risk of returning to substance use.
B. Prevent overscheduling and becoming fatigued and exhausted. Reach out to reconnect with old buddies to test strength in resistance This statement includes potential triggers for relapse (reconnecting with old buddies) and does not align with effective relapse prevention strategies.
C. Have a friend or counselor number to call when having doubts This is a valuable strategy as it provides the client with a support system and someone to reach out to during moments of doubt or vulnerability.
D. Attend outpatient and community support groups for addiction Support groups provide a sense of community, understanding, and accountability for individuals in recovery. They offer a safe space to share experiences and coping strategies, making them an essential part of relapse prevention.
Sign Up or Login to view all the 78 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

