South Tampa University, Exam 3 Pharmacology
Total Questions : 48
Showing 25 questions, Sign in for more
A patient with diabetes has been administered 38 units of NPH insulin at 7:00 AM. By 1:00 PM, the patient has been away from the nursing unit for 2 hours and missed lunch while waiting for a chest X-ray.
What is the most appropriate action for the nurse to prevent hypoglycemia?
Explanation
Choice A rationale:
Requesting that the patient eat lunch first if testing is further delayed is the most appropriate action to prevent hypoglycemia for the following reasons:
1. Timing of NPH Insulin Peak:
NPH insulin is an intermediate-acting insulin with a peak action time of 4-12 hours after administration.
In this case, the patient received NPH insulin at 7:00 AM, meaning its peak effect is likely to occur between 11:00 AM and 5:00 PM.
Delaying lunch beyond 1:00 PM significantly increases the risk of hypoglycemia as the insulin's action peaks without adequate food intake to balance glucose levels.
2. Ensuring Consistent Mealtimes:
Consistency in meal timing is crucial for managing blood glucose levels in diabetic patients. Delaying meals can disrupt the balance between insulin and glucose, leading to hypoglycemia.
Prioritizing lunch at the usual time, even amidst testing delays, helps maintain a more predictable glucose pattern.
3. Addressing Acute Hypoglycemia Risk:
Hypoglycemia is a serious complication of diabetes that can occur if blood glucose levels fall too low. Symptoms can include shakiness, sweating, dizziness, confusion, and even loss of consciousness.
Promptly addressing potential delays in food intake is essential to prevent hypoglycemia and its associated risks.
Rationales for other choices:
Choice B: Discontinuing the evening dose of insulin does not address the immediate risk of hypoglycemia due to the missed lunch. It could lead to hyperglycemia later in the day or overnight.
Choice C: Saving the lunch tray for later may not be feasible if testing is significantly delayed. It also does not prevent hypoglycemia in the immediate timeframe.
Choice D: While a glass of orange juice can provide a quick source of glucose, it is a short-term solution and does not replace a balanced meal. It could also lead to a rapid rise in blood glucose followed by a subsequent drop.
What specific administration techniques should the nurse employ when administering NPH insulin?
Explanation
Choice A Rationale:
NPH insulin can be mixed with certain other insulins, such as regular insulin, to achieve different effects and better control blood glucose levels. Therefore, stating that it should never be mixed with another insulin is incorrect.
Choice C rationale:
NPH insulin is an intermediate-acting insulin that can be administered at various times of the day, depending on the individual's needs and blood glucose patterns. It is not restricted to bedtime administration only.
Choice D rationale:
When mixing NPH insulin with another insulin, the order of mixing does not significantly affect its action. The crucial aspect is to ensure proper mixing of the insulins before administration.
Choice B rationale:
NPH insulin is a suspension, meaning the insulin particles are not fully dissolved in the liquid. Therefore, it's essential to roll the vial gently between the palms to evenly distribute the insulin particles throughout the solution. This ensures that the patient receives the correct dose and prevents injection of an uneven mixture, which could lead to unpredictable blood glucose levels.
Key points to remember:
NPH insulin is an intermediate-acting insulin that starts working within 1 to 2 hours, peaks in 4 to 12 hours, and lasts for 12 to 18 hours.
It can be mixed with regular insulin to provide both short-acting and longer-acting insulin coverage. Always follow the specific instructions provided by the insulin manufacturer and healthcare provider. Proper mixing of NPH insulin is crucial for accurate dosing and optimal glucose control.

What order should the nurse anticipate?
Explanation
Choice A rationale:
Glucagon directly addresses the underlying issue of severe hypoglycemia: In a patient with Type 1 diabetes mellitus, a blood glucose level of 40 mg/dL signifies a critical condition known as severe hypoglycemia. This condition occurs when blood sugar levels drop dangerously low, depriving the brain and other vital organs of glucose, their primary source of energy. Glucagon, a hormone that acts opposite to insulin, is the most effective and rapid treatment for severe hypoglycemia. It works by stimulating the liver to release stored glucose into the bloodstream, quickly raising blood sugar levels and restoring normal brain function.
Rationale for other choices:
Choice B: Give orange juice: While orange juice contains carbohydrates that can raise blood sugar, it is not ideal for treating severe hypoglycemia due to its slower absorption rate compared to glucagon. In an unconscious patient, there's also a risk of aspiration if given orally.
Choice C: Perform CPR: CPR is not indicated in this scenario as the patient has a pulse. CPR is a lifesaving technique that is only used when a person's heart has stopped beating.
Choice D: Give insulin: Insulin, which lowers blood glucose, would be contraindicated in this situation as the patient is already experiencing severe hypoglycemia. Administering insulin would further decrease blood sugar levels, worsening the patient's condition.
Key points to remember:
Severe hypoglycemia is a medical emergency that requires prompt treatment with glucagon.
Glucagon is the only medication that can effectively and quickly raise blood glucose levels in severe hypoglycemia. It's crucial to administer glucagon as soon as possible to prevent irreversible brain damage or even death.
Healthcare professionals should be proficient in recognizing the signs and symptoms of severe hypoglycemia and administering glucagon appropriately.
Explanation
Choice A rationale:
Erythromycin ointment does not have moisturizing properties. Its primary purpose is to prevent bacterial infection, not to provide moisture to the eyes.
While some ointments may have a slight moisturizing effect, this is not the main reason for using erythromycin ointment in newborns.
If moisture is the primary concern, other products specifically designed to lubricate the eyes would be more appropriate.
Choice B rationale:
Chemical conjunctivitis is typically caused by exposure to irritants such as chlorine in swimming pools or strong chemicals. Erythromycin ointment is not effective in preventing chemical conjunctivitis.
In fact, it could potentially worsen the irritation if used in cases of chemical conjunctivitis.
If chemical conjunctivitis is suspected, flushing the eyes with water or saline solution and seeking medical attention would be the appropriate course of action.
Choice D rationale:
Erythromycin ointment is an antibiotic, but it is not typically used to treat active infections in newborns.
If a newborn has a suspected eye infection, a healthcare provider would likely prescribe a different antibiotic eye drop or ointment that is more effective in treating the specific infection.
However, erythromycin ointment can be used as a prophylactic measure to prevent eye infections, which is why it is commonly administered to newborns shortly after birth.
Choice C rationale:
Erythromycin ointment is primarily used to prevent eye infections in newborns.
It is effective against a variety of bacteria that can cause conjunctivitis, including Neisseria gonorrhoeae (the bacteria that causes gonorrhea) and Chlamydia trachomatis (the bacteria that causes chlamydia).
These bacteria can be passed from the mother to the baby during childbirth, and if left untreated, they can cause serious eye infections that can lead to vision loss.
By applying erythromycin ointment to the newborn's eyes shortly after birth, the risk of these infections can be significantly reduced.
Explanation
Choice A rationale:
Fever is not a common side effect of metformin. While it's possible for a minority of patients to experience a mild fever as their bodies adjust to the medication, it's not considered a typical or expected adverse effect.
Fevers typically occur due to infections or inflammation, and metformin does not directly cause either of these processes.
If a patient taking metformin develops a fever, it's crucial to rule out other potential causes, such as infections or other medications, before attributing it to metformin.
Choice B rationale:
Insomnia is also not a common side effect of metformin. In fact, some studies have suggested that metformin may even have a positive effect on sleep quality in some individuals.
While sleep disturbances can occur with any medication, they are not specifically associated with metformin.
If a patient experiences insomnia while taking metformin, it's essential to consider other potential factors, such as stress, anxiety, or other medications, that could be contributing to sleep problems.
Choice C rationale:
Bitter or metallic taste is a very common side effect of metformin, experienced by approximately 30-40% of patients. This taste disturbance is thought to be caused by metformin's interaction with taste receptors on the tongue.
The taste is often described as metallic, bitter, or similar to the taste of pennies.
While it can be unpleasant, it's generally not considered a serious side effect and does not usually require discontinuation of the medication.
Some strategies to manage the metallic taste include: Taking metformin with meals or snacks to mask the taste.
Chewing sugar-free gum or sucking on hard candy after taking the medication. Rinsing the mouth with water or mouthwash after taking the medication.
Switching to an extended-release formulation of metformin, which may have a less pronounced metallic taste.
Choice D rationale:
Seizures are a rare but serious side effect of metformin.
They are most likely to occur in patients with underlying kidney problems or those taking certain other medications that can interact with metformin.
If a patient taking metformin experiences a seizure, it's critical to seek immediate medical attention.
The RN is aware that a long-term side effect of amiodarone is:
Explanation
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
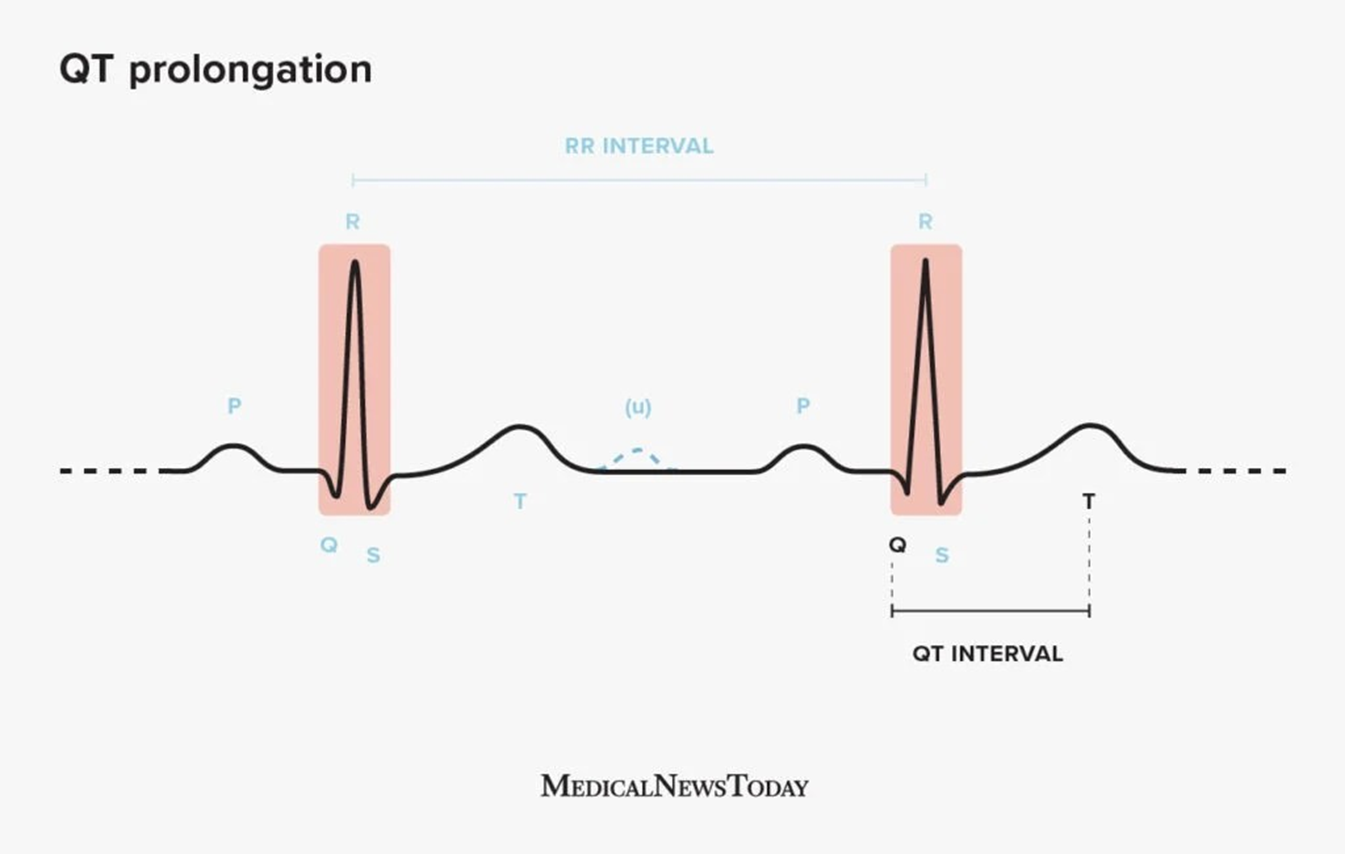
Choice D rationale:
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
The client is having excessive urine output.
Which medication should the nurse anticipate administering?
Explanation
Choice A rationale:
Prednisolone is a corticosteroid that has anti-inflammatory and immunosuppressant effects. It does not have a direct effect on urine output.
While it may be used in some cases of head trauma to reduce inflammation, it would not be the first-line choice to address excessive urine output.
Prolonged use of prednisolone can have adverse effects such as fluid retention, weight gain, hypertension, and hyperglycemia.
Choice B rationale:
Corticotropin (ACTH) is a hormone that stimulates the adrenal glands to produce cortisol. Cortisol has a variety of effects, including increasing blood pressure and blood sugar levels.
It does not have a direct effect on urine output and would not be used to address this issue.
ACTH can have significant side effects, including fluid retention, electrolyte imbalances, and mood changes.
Choice C rationale:
Vasopressin is a hormone that regulates fluid balance in the body. It works by increasing water reabsorption in the kidneys, which can help to reduce urine output.
It is the most appropriate medication to administer to a client with excessive urine output following head trauma.
Vasopressin can be administered intravenously or subcutaneously. It is important to monitor the client's fluid intake and output closely when administering vasopressin, as it can lead to fluid overload if not used carefully.
Choice D rationale:
Calciferol is a form of vitamin D that helps to regulate calcium and phosphorus levels in the body. It does not have a direct effect on urine output.
It would not be used to address excessive urine output in a client with head trauma.
Excessive doses of calciferol can lead to hypercalcemia, which can cause kidney stones, bone pain, and other serious problems.
What is the rationale for rotating insulin injection sites?
Explanation
Choice A rationale:
Insulin resistance is a condition in which the body's cells become less responsive to insulin, requiring more insulin to maintain normal blood glucose levels.
It's primarily caused by factors such as obesity, physical inactivity, and genetic predisposition. Rotating injection sites does not directly address these underlying causes of insulin resistance.
It can help ensure consistent insulin absorption, but it's not the primary mechanism for preventing insulin resistance.
Choice B rationale:
Allergic reactions to insulin are rare but can occur.
They typically manifest as localized symptoms at the injection site, such as redness, swelling, itching, or pain.
In severe cases, systemic reactions like hives, difficulty breathing, or anaphylaxis can occur.
Rotating injection sites might reduce the risk of localized allergic reactions by preventing repeated exposure to insulin in the same area of skin.
However, it does not prevent systemic allergic reactions, which are immune-mediated and not dependent on the injection site.
Choice C rationale:
Lipodystrophy is a condition characterized by abnormal changes in fat distribution under the skin. It can occur as a complication of repeated insulin injections at the same site.
There are two main types of lipodystrophy:
Lipohypertrophy: This involves the accumulation of excess fatty tissue at injection sites, creating visible lumps or bumps. Lipoatrophy: This involves the loss of fatty tissue at injection sites, leading to depressions or indentations in the skin.
Both lipohypertrophy and lipoatrophy can interfere with insulin absorption, leading to unpredictable blood glucose control.
Rotating injection sites helps to prevent lipodystrophy by distributing insulin injections over a wider area of skin, reducing the likelihood of repeated trauma to the same tissue.

Choice D rationale:
Insulin shock, also known as hypoglycemia, is a condition that occurs when blood glucose levels drop too low.
It can be caused by several factors, including excessive insulin dosing, missed meals, or increased physical activity. Rotating injection sites does not directly affect the risk of insulin shock.
It's essential for individuals using insulin to monitor their blood glucose levels regularly, adjust insulin doses as needed, and follow a balanced diet and exercise plan to prevent hypoglycemia.
A newly diagnosed client with type I diabetes was admitted to the ICU with the diagnosis of diabetic ketoacidosis.
After being transferred to the med/surg unit, he asks if he can receive today’s NPH and regular insulin the same way to avoid being “stuck” since there is still an IV access.
Which information should be included in the nurse’s response?
Explanation
Rationale for A:
Regular insulin is the only insulin formulation that can be safely administered intravenously. It is a rapid-acting insulin that starts working within 15 minutes and peaks in 1-2 hours, making it ideal for urgent glucose control in situations like diabetic ketoacidosis.
NPH insulin is an intermediate-acting insulin that is not suitable for IV administration. It is designed to be absorbed slowly over several hours, and injecting it intravenously could lead to unpredictable and potentially dangerous fluctuations in blood glucose levels.
Subcutaneous (SQ) injection is the standard route of administration for both regular and NPH insulin outside of acute care settings. This route allows for a more gradual and consistent absorption of insulin, which is essential for maintaining stable blood glucose control.
The patient's transfer to the med/surg unit indicates that their condition has stabilized and no longer requires the aggressive glucose control that is achieved with an IV insulin infusion. Therefore, it is appropriate to transition them to SQ insulin injections.
Rationale for B:
While mixing insulins can potentially alter their absorption rates and action profiles, the primary concern with mixing NPH and regular insulin is not an increased risk of hypoglycemia. It is the incompatibility of the formulations for IV administration.
Rationale for C:
NPH and regular insulin can be mixed together for subcutaneous injection, but they are not compatible for intravenous administration.
Rationale for D:
While NPH insulin can be administered as part of an IV insulin drip in the ICU, this is typically done in specific situations where a continuous infusion of both rapid-acting and intermediate-acting insulin is required. It is not the standard practice for NPH insulin administration.
Explanation
Choice A rationale:
Severe acidemia: A pH of 6.9 indicates severe acidemia, a condition where the blood is too acidic. Sodium bicarbonate is an alkalizing agent that can help raise the blood pH back to a normal range.
Rapid correction: Intravenous (IVP) administration of sodium bicarbonate allows for rapid correction of acidemia, which is crucial in severe cases to prevent life-threatening complications.
Buffering action: Sodium bicarbonate acts as a buffer, accepting excess hydrogen ions (H+) in the blood and converting them into water and carbon dioxide (CO2), which can be exhaled.
Specific indications: Sodium bicarbonate is typically used in cases of severe acidemia caused by metabolic acidosis, such as diabetic ketoacidosis or lactic acidosis. It may also be considered in cases of respiratory acidosis, but other interventions like ventilatory support are often prioritized.
Choice B rationale:
Calcium carbonate is not a direct treatment for acidemia: It is primarily used as an antacid to neutralize stomach acid and as a calcium supplement for bone health. While it can have a mild alkalizing effect, it is not as effective as sodium bicarbonate in rapidly correcting severe acidemia.
Choice C rationale:
Alkalemia: A pH of 7.6 indicates alkalemia, a condition where the blood is too alkaline. Administration of sodium bicarbonate in this situation would worsen the alkalemia and potentially lead to serious complications.
Choice D rationale:
Hyponatremia: Low serum sodium levels do not directly require treatment with sodium bicarbonate. Sodium bicarbonate is primarily used to address acid-base imbalances, not electrolyte imbalances.
Explanation
Choice A rationale:
It is not recommended to take levothyroxine with food as it can interfere with its absorption.
Food, particularly those containing calcium or iron, can bind to levothyroxine in the gastrointestinal tract, reducing the amount of medication that is absorbed into the bloodstream.
This can lead to decreased effectiveness of the medication.
It's generally advised to take levothyroxine on an empty stomach, at least 30-60 minutes before breakfast, to ensure optimal absorption.
Choice B rationale:
Taking levothyroxine first thing in the morning, on an empty stomach, is the most effective way to ensure its absorption and consistent hormone levels throughout the day.
This aligns with the body's natural rhythm of thyroid hormone production, which typically peaks in the morning hours.
Taking the medication consistently at the same time each day helps maintain stable thyroid hormone levels, which is crucial for managing hypothyroidism effectively.
Choice C rationale:
Relief of symptoms with levothyroxine therapy often takes several weeks, not just one week.
It takes time for the body to adjust to the medication and for thyroid hormone levels to reach a therapeutic range.
Patients should be counseled to have patience and continue taking the medication as prescribed, even if they don't experience immediate symptom relief.
They should also be monitored regularly by their healthcare provider to assess their response to treatment and make any necessary adjustments to the dosage.
Choice D rationale:
Doubling the dose of levothyroxine without consulting a healthcare provider is dangerous and can lead to serious health consequences.
Overdosing on levothyroxine can cause hyperthyroidism, which can manifest as rapid heart rate, anxiety, tremors, weight loss, and other health problems.
It's essential to follow the prescribed dosage and not make any changes without the guidance of a healthcare professional.
Explanation
Choice A rationale:
Insulin lispro is a rapid-acting insulin that begins to work within 15 minutes of injection. If administered 15 minutes after eating, it may not be able to effectively control the rise in blood glucose levels that occurs after a meal. This could lead to hyperglycemia, which can have negative short-term and long-term health consequences.
Administering insulin lispro 15 minutes after eating would delay its action and potentially lead to suboptimal blood glucose control. It's crucial to match the timing of insulin administration with the meal to ensure optimal glucose management.
Choice C rationale:
Administering insulin lispro 10 minutes after eating would also delay its action. While not as delayed as 15 minutes, it still wouldn't align with the peak of meal-related glucose absorption, potentially leading to suboptimal glucose control.
Choice D rationale:
Insulin lispro has a shorter duration of action compared to regular insulin. Administering it 30 minutes before eating could lead to hypoglycemia, a condition characterized by low blood glucose levels. Hypoglycemia can cause a variety of symptoms, including shakiness, sweating, dizziness, confusion, and even loss of consciousness.
It's essential to closely align the timing of rapid-acting insulins like insulin lispro with mealtimes to minimize the risk of hypoglycemia.
The patient inquires, “What is the mechanism of action of this medication in managing my diabetes?” How should the nurse respond?
Explanation
Choice A rationale:
Glipizide does not directly enhance glucose transport into the muscles. This action is primarily mediated by insulin, which increases the expression of glucose transporter proteins (GLUT4) on muscle cell membranes, facilitating glucose uptake.
While glipizide can indirectly improve glucose transport into muscles by increasing insulin levels, it's not the primary mechanism of action.
Choice B rationale:
Glipizide does not directly facilitate glucose utilization by body cells. This process also largely depends on insulin, which activates intracellular pathways that promote glucose metabolism and energy production.
Although glipizide can indirectly enhance glucose utilization by increasing insulin availability, it's not the main mechanism responsible for its glucose-lowering effects.
Choice C rationale:
Glipizide does not boost glucose levels. In fact, it has the opposite effect, lowering blood glucose levels by stimulating insulin secretion.
Elevating glucose levels would be counterproductive in diabetes management, as the goal is to maintain blood glucose within a healthy range.
Choice D rationale (correct answer):
Glipizide belongs to a class of medications called sulfonylureas, which act primarily by stimulating insulin secretion from pancreatic beta cells.
Insulin is a hormone that plays a crucial role in regulating blood glucose levels. It promotes glucose uptake by various tissues, including muscles, liver, and adipose tissue, and it inhibits glucose production by the liver.
By triggering insulin release, glipizide effectively lowers blood glucose levels. This helps to prevent the long-term complications of diabetes, such as damage to blood vessels, nerves, and organs.
Explanation
Choice A rationale:
COPD (Chronic Obstructive Pulmonary Disease) is a chronic lung disease that causes airflow obstruction. While labetalol can cause some bronchoconstriction, it is generally considered safe for use in patients with COPD. However, it's essential to monitor respiratory status closely, especially in those with severe COPD.
Choice B rationale:
Narrow-angle glaucoma is an eye condition characterized by increased intraocular pressure (IOP) due to impaired drainage of aqueous humor. Labetalol can exacerbate this condition by further increasing IOP through its beta-blocking effects. This can lead to acute angle-closure glaucoma, a medical emergency that can result in permanent vision loss.
Specific mechanisms by which labetalol can increase IOP:
Reduced aqueous humor production: Beta-blockers like labetalol can decrease the production of aqueous humor, the fluid that maintains eye pressure. While this might seem beneficial, a significant reduction can lead to anterior chamber shallowing, which can mechanically block the drainage angle and trigger angle closure.
Impaired uveoscleral outflow: Beta-blockers can also impair the uveoscleral outflow pathway, an alternative route for aqueous humor drainage that becomes more important in glaucoma patients. This can further contribute to IOP elevation.
Vasoconstriction of ciliary blood vessels: Labetalol's alpha-blocking effects can cause vasoconstriction of the ciliary blood vessels, which supply blood to the ciliary body responsible for aqueous humor production. This can reduce blood flow and indirectly hinder aqueous humor drainage.
Pupillary dilation: Beta-blockers can cause pupillary dilation, which can mechanically narrow the anterior chamber angle and obstruct aqueous humor outflow.
Therefore, labetalol is generally contraindicated in patients with known narrow-angle glaucoma.
Choice C rationale:
Hypertension (high blood pressure) is one of the primary indications for labetalol. It is an effective antihypertensive medication that works by blocking beta receptors, leading to decreased heart rate, contractility, and blood pressure.
Choice D rationale:
Tachycardia (fast heart rate) can also be treated with labetalol due to its beta-blocking effects. It helps to slow down the heart rate and restore a normal rhythm.
The patient has been prescribed morphine sulfate IV 4 mg every 5-30 minutes as needed until chest pain subsides.
The last dose of 4 mg was administered 15 minutes ago, and the patient is still complaining of chest pain and showing signs of increased respiratory effort.
The nurse observes a heart rate of 82 beats per minute, a respiratory rate of 18 breaths per minute, and a blood pressure of 135/88 mm Hg. What should the nurse do next?
Explanation
Choice A rationale:
Requesting an order for morphine sulfate IV 2 mg over 1-5 minutes would not be appropriate at this time for several reasons: The patient has already received a dose of 4 mg 15 minutes ago, and it has not been effective in relieving the chest pain.
The patient is showing signs of increased respiratory effort, which could be a sign of respiratory depression. Administering an additional dose of morphine could worsen the respiratory depression.
The patient's heart rate is 82 beats per minute, which is within the normal range.
The patient's blood pressure is 135/88 mm Hg, which is also within the normal range.
Choice C rationale:
Administering naloxone (Narcan) to counteract respiratory depression would not be appropriate at this time because the patient is not showing signs of severe respiratory depression. Naloxone is a medication that is used to reverse the effects of opioid overdose. It is typically only used in situations where the patient is experiencing life-threatening respiratory depression.
Choice D rationale:
Administering morphine sulfate IV 4 mg over 1-5 minutes would not be appropriate for the reasons listed above. It could worsen the patient's respiratory depression and potentially lead to other complications.
Choice B is the best answer because it is the most conservative and safest option. By withholding the next dose of morphine and informing the provider about the patient's symptoms, the nurse can ensure that the patient receives the appropriate care and that any potential complications are avoided.
Explanation
Choice A rationale:
Hypertension is not a primary contraindication for mannitol use. While it's important to monitor blood pressure during mannitol administration, it's not the most concerning factor in this scenario.
Mannitol can even be used cautiously in hypertensive patients with conditions like intracranial hypertension or acute renal failure, where its benefits may outweigh the potential risks of exacerbating hypertension.
Choice B rationale:
Mannitol is actually indicated for the treatment of increased intracranial pressure (ICP). It works by drawing fluid from the brain tissues into the bloodstream, thereby reducing pressure within the skull.
Therefore, a patient with ICP would not be a concern for mannitol administration; rather, they would be a potential candidate for its use.
Choice D rationale:
While fluid volume overload can be a concern with mannitol use, it's typically managed with careful monitoring and fluid restriction.
The more significant concern in this scenario is congestive heart failure (CHF).
Choice C rationale:
Mannitol is contraindicated in patients with congestive heart failure (CHF). Here's why:
Increased Circulating Volume: Mannitol is an osmotic diuretic, meaning it draws fluid from the tissues into the bloodstream, increasing circulating blood volume. This can overload the already compromised heart in CHF patients, leading to worsening heart failure and pulmonary edema.
Elevated Blood Pressure: Mannitol can also cause a transient increase in blood pressure due to its osmotic effects. This can further strain the heart and worsen CHF symptoms.
Renal Impairment: CHF patients often have impaired renal function, which can reduce their ability to excrete mannitol effectively. This can lead to fluid retention and electrolyte imbalances, further complicating CHF management.
In summary, administering mannitol to a patient with CHF could potentially lead to:
Exacerbation of heart failure symptoms Pulmonary edema
Worsening renal function Electrolyte imbalances Increased risk of mortality
Therefore, it's crucial to avoid mannitol use in patients with CHF and to closely monitor fluid status and electrolytes in those who must receive it for other indications.
Explanation
Choice A rationale:
Oxytocin is a hormone that stimulates uterine contractions. It is not a tocolytic, which is a medication that inhibits uterine contractions. In fact, oxytocin is often used to induce labor or to augment labor that is progressing slowly.
It acts on the myofibrils in the uterine muscle, causing them to contract more forcefully and frequently. This leads to cervical dilation and effacement, and ultimately to the birth of the baby.
Oxytocin is typically administered as an intravenous (IV) infusion. The dosage is carefully titrated to achieve the desired effect on the uterus.
It is important to note that oxytocin can have serious side effects, including uterine hyperstimulation, fetal distress, and postpartum hemorrhage. Therefore, it should only be used under the close supervision of a healthcare provider.
Choice B rationale:
Magnesium sulfate is a tocolytic that is often used to prevent preterm labor. It works by relaxing the smooth muscle of the uterus.
It is typically administered as an IV infusion. The dosage is carefully monitored to ensure that the magnesium level in the blood does not become too high.
Side effects of magnesium sulfate can include flushing, nausea, vomiting, and headache. In rare cases, it can also cause serious complications such as respiratory depression and cardiac arrest.
Choice C rationale:
Nifedipine is a calcium channel blocker that is sometimes used as a tocolytic. It works by relaxing the smooth muscle of the uterus and blood vessels.
It is typically administered as an oral tablet. Side effects of nifedipine can include headache, dizziness, flushing, and low blood pressure.
Choice D rationale:
Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) that is sometimes used as a tocolytic. It works by inhibiting the production of prostaglandins, which are substances that promote uterine contractions.
It is typically administered as an oral tablet or suppository. Side effects of indomethacin can include nausea, vomiting, heartburn, and diarrhea.
Explanation
Choice A rationale:
Dopamine was once considered a first-line vasopressor for cardiogenic shock. However, recent studies have shown that it is associated with increased mortality compared to norepinephrine.
Dopamine has dose-dependent effects on dopamine receptors, beta receptors, and alpha receptors. At low doses (1-5 mcg/kg/min), it primarily stimulates dopamine receptors, leading to renal vasodilation and increased urine output. At moderate doses (5-10 mcg/kg/min), it stimulates beta receptors, resulting in increased heart rate and contractility. At high doses (>10 mcg/kg/min), it stimulates alpha receptors, causing vasoconstriction.
The main concern with dopamine is its potential to cause arrhythmias, particularly at higher doses. This is due to its effects on beta receptors, which can increase heart rate and myocardial oxygen demand.
Additionally, dopamine can cause tachyphylaxis, meaning that its effects can diminish over time, requiring higher doses to achieve the same effect.
Choice B rationale:
Norepinephrine is a potent alpha-adrenergic agonist that causes vasoconstriction, leading to an increase in blood pressure. It has minimal effects on beta receptors, so it is less likely to cause tachycardia and arrhythmias compared to dopamine.
Norepinephrine also has some inotropic effects, meaning that it can increase the strength of contraction of the heart muscle.
Studies have shown that norepinephrine is associated with improved survival rates in patients with cardiogenic shock compared to dopamine.
It is generally well-tolerated, with the most common side effects being hypertension and peripheral vasoconstriction.
Choice C rationale:
Epinephrine is a potent alpha- and beta-adrenergic agonist that causes vasoconstriction, increased heart rate, and increased contractility.
It is typically used as a second-line agent in cardiogenic shock, after norepinephrine has failed to achieve adequate blood pressure.
Epinephrine can cause significant tachycardia and arrhythmias, so it should be used with caution in patients with underlying heart disease.
Choice D rationale:
Vasopressin is a hormone that causes vasoconstriction by acting on V1 receptors in vascular smooth muscle. It is sometimes used as an adjunct to norepinephrine in patients with refractory cardiogenic shock.
Vasopressin has the potential to cause coronary vasoconstriction, so it should be used with caution in patients with coronary artery disease.
What would be the most appropriate response from the nurse?
Explanation
Rationale for Choice A:
It is not recommended to always consume levothyroxine with food. In fact, food can interfere with the absorption of levothyroxine, leading to decreased efficacy of the medication.
Consuming levothyroxine with food can decrease its absorption by up to 30%, which can significantly impact its ability to manage hypothyroidism symptoms.
Certain foods, such as those high in fiber, calcium, or iron, can be particularly problematic, as they can bind to levothyroxine in the gut and further reduce its absorption.
While taking levothyroxine with a small amount of food may be necessary for some individuals who experience gastrointestinal side effects, it's generally recommended to take it on an empty stomach for optimal absorption.
Rationale for Choice B:
Milk is not an ideal beverage to take with levothyroxine, as it can also interfere with absorption. Milk contains calcium, which can bind to levothyroxine and reduce its absorption.
It's best to avoid consuming milk or other calcium-rich beverages within a few hours of taking levothyroxine.
Rationale for Choice C:
Similar to milk, juice and crackers are not ideal choices to take with levothyroxine.
Juice, especially those high in acidity, can affect the absorption of levothyroxine in the gut.
Crackers, often made with refined grains, can be high in fiber, which can also interfere with absorption.
Rationale for Choice D:
Taking levothyroxine on an empty stomach, typically 30-60 minutes before breakfast, is generally recommended to ensure optimal absorption.
This allows the medication to be absorbed more efficiently in the small intestine without being affected by the presence of food.
By taking levothyroxine on an empty stomach, patients can maximize its effectiveness in treating hypothyroidism.
Explanation
Choice A rationale:
Uncontrolled diabetes mellitus: Corticosteroids can have a hyperglycemic effect, meaning they can raise blood sugar levels. This makes them generally unsuitable for use in patients with uncontrolled diabetes mellitus. In fact, corticosteroids might even worsen glycemic control in these patients. While corticosteroids might be used in some cases of diabetes mellitus, such as to treat diabetic retinopathy or nephropathy, they would be used cautiously and with close monitoring of blood sugar levels.
Choice B rationale:
A recent diagnosis of lung cancer: Corticosteroids are not a primary treatment for lung cancer. They might be used in some cases to help manage symptoms or side effects of other treatments, such as chemotherapy or radiation therapy. However, they would not typically be used as a first-line treatment for lung cancer itself.
Choice C rationale:
Acute exacerbation of COPD: Corticosteroids are a mainstay of treatment for acute exacerbations of COPD. They work by reducing inflammation in the airways, which helps to improve airflow and relieve symptoms such as wheezing, shortness of breath, and chest tightness. Corticosteroids can be given orally, intravenously, or by inhalation. The dose and duration of treatment will depend on the severity of the exacerbation.
Choice D rationale:
Chronic asthma: Corticosteroids are often used as a long-term control medication for chronic asthma. However, they are typically used at lower doses than those used for acute exacerbations of COPD. Inhaled corticosteroids are the preferred form of treatment for chronic asthma, as they deliver the medication directly to the airways and have fewer systemic side effects.
The nurse is aware that which insulins are long-acting and should be administered once daily at bedtime? (Select all that apply.)
Explanation
Choice A rationale:
Insulin glargine (Lantus) is a long-acting insulin analog that is designed to provide a steady, basal level of insulin throughout the day.
It has a duration of action of approximately 24 hours, so it is typically administered once daily at bedtime.
This helps to control blood glucose levels overnight and during the early morning hours, when the risk of hypoglycemia is highest.
Key characteristics of Insulin Glargine (Lantus):
Onset: 1-2 hours
Peak: No pronounced peak Duration: Approximately 24 hours
Administration: Once daily at bedtime
Choice B rationale:
Lispro (Humalog) is a rapid-acting insulin analog that is designed to be taken with meals to help control blood glucose spikes after eating.
It has a onset of action of approximately 15 minutes and a duration of action of 2-4 hours.
Because of its rapid onset and short duration of action, lispro is not typically used as a basal insulin. Key characteristics of Lispro (Humalog):
Onset: 15 minutes
Peak: 30-90 minutes
Duration: 2-4 hours
Administration: With meals
Choice C rationale:
Insulin detemir (Levemir) is another long-acting insulin analog that is similar to insulin glargine in terms of its duration of action.
It is typically administered once daily at bedtime to provide basal insulin coverage. Key characteristics of Insulin Detemir (Levemir):
Onset: 1-2 hours
Peak: No pronounced peak
Duration: Approximately 18-24 hours Administration: Once daily at bedtime Question 23.
The nurse receives an order for insulin: NPH (Humulin NPH) 10 units to be administered intravenously daily at 7:00am.
What action should the nurse take?
A. Administer the dose but ensure that if mixed with another Humulin-R insulin, to draw the regular insulin up first.
B. Give the drug subcutaneously rather than IV
C. Review the insulin order with the prescriber and pharmacy.
D. Administer the insulin ordered mixed in 50 ML of 0.9%NS IV Piggyback (not to infuse faster than 1/2 hour or 30 minutes).
The correct answer is C. Review the insulin order with the prescriber and pharmacy.
Rationale for Choice A:
Intravenous administration of NPH insulin is not recommended. It is an intermediate-acting insulin that is designed to be absorbed slowly from the subcutaneous tissue. IV administration can lead to rapid and unpredictable changes in blood glucose levels, which can be dangerous.
Mixing NPH insulin with regular insulin does not change the route of administration. Both insulins should still be given subcutaneously.
Rationale for Choice B:
Subcutaneous administration of NPH insulin is the correct route. This allows for slow and steady absorption of the insulin, which helps to prevent blood glucose fluctuations.
However, the nurse should still clarify the order with the prescriber and pharmacy. This is because IV insulin orders are unusual and may be a mistake.
Rationale for Choice D:
Adding NPH insulin to a 50 mL IV piggyback is not a safe practice. This would dilute the insulin and make it even more difficult to control the rate of infusion.
IV insulin infusions are typically administered using a dedicated insulin pump. This allows for precise control of the infusion rate and helps to prevent hypoglycemia.
Rationale for Choice C:
Reviewing the insulin order with the prescriber and pharmacy is the safest course of action. This will help to ensure that the order is correct and that the insulin is administered safely.
The prescriber may have meant to order regular insulin instead of NPH insulin. Regular insulin can be given intravenously, but it requires careful monitoring of blood glucose levels.
The pharmacy can also double-check the order and ensure that the correct insulin is dispensed.
Explanation
Choice A rationale:
Propylthiouracil (PTU) is a thionamide medication that inhibits the synthesis of thyroid hormones. It is the preferred drug for presurgical treatment of Graves' disease because it effectively lowers thyroid hormone levels and reduces the risk of thyroid storm, a life-threatening complication that can occur during or after surgery.
PTU acts by blocking the enzyme thyroid peroxidase, which is essential for the production of thyroid hormones. It also inhibits the conversion of thyroxine (T4) to triiodothyronine (T3), the more active form of thyroid hormone. This results in a decrease in circulating levels of both T4 and T3, leading to a reduction in the symptoms of hyperthyroidism.
PTU is typically started at a dose of 100-300 mg daily, divided into two or three doses. The dose is then adjusted based on the patient's response and thyroid hormone levels. The goal of treatment is to achieve a euthyroid state, which means that the thyroid hormone levels are within the normal range.
PTU is generally well-tolerated, but it can cause some side effects, including skin rash, itching, nausea, vomiting, abdominal pain, joint pain, and hair loss. In rare cases, it can also cause serious side effects, such as liver damage and agranulocytosis (a decrease in white blood cells).
Choice B rationale:
Liotrix (Thyrolar) is a combination of synthetic T4 and T3 hormones. It is not used for presurgical treatment of Graves' disease because it can worsen the symptoms of hyperthyroidism.
Choice C rationale:
Propranolol (Inderal) is a beta-blocker medication that can be used to control the symptoms of hyperthyroidism, such as tachycardia, tremor, and anxiety. However, it does not lower thyroid hormone levels and is not used for presurgical treatment of Graves' disease.
Choice D rationale:
Levothyroxine sodium (Synthroid) is a synthetic T4 hormone. It is used to treat hypothyroidism, but it is not used for presurgical treatment of Graves' disease.
Explanation
Choice A rationale:
Respiratory distress is not a direct side effect of metformin. While metformin can cause a rare condition called lactic acidosis, which can lead to rapid breathing, respiratory distress is not a primary concern with metformin use.
Respiratory distress typically involves difficulty breathing due to other causes such as asthma, pneumonia, heart failure, or chronic obstructive pulmonary disease (COPD).
Choice B rationale:
Seizures are not a known side effect of metformin.
Seizures are typically associated with neurological conditions, such as epilepsy, or metabolic disturbances such as hypoglycemia or electrolyte imbalances.
Metformin does not directly affect the central nervous system in a way that would increase the risk of seizures.
Choice C rationale:
Lactic acidosis:
This is a rare but serious condition that can occur with metformin use.
It happens when lactic acid builds up in the bloodstream, causing the blood to become too acidic. Symptoms of lactic acidosis include:
Rapid breathing Nausea and vomiting Abdominal pain Muscle weakness Unusual sleepiness Feeling cold
Risk factors for lactic acidosis in patients taking metformin include:
Kidney disease Congestive heart failure Liver disease Dehydration
Excessive alcohol intake Recent surgery or heart attack
It's important to note that lactic acidosis is rare, occurring in about 3 to 10 cases per 100,000 people taking metformin per year.
Renal failure:
Metformin is primarily eliminated by the kidneys.
If kidney function is impaired, metformin can build up in the body, increasing the risk of lactic acidosis. Additionally, metformin can potentially cause kidney damage in rare cases, further worsening kidney function. It's crucial to monitor kidney function regularly in patients taking metformin.
Choice D rationale:
Hyperglycemia (high blood sugar) is not a side effect of metformin.
In fact, metformin is a medication used to lower blood sugar levels in people with type 2 diabetes. It works by:
Decreasing the amount of glucose produced by the liver Improving the body's sensitivity to insulin
Slowing the absorption of glucose from the intestines
Explanation
Choice A rationale:
Incorrect. Insulin pumps should be removed before bathing or swimming to prevent damage to the device. Water can enter the pump through the infusion set or through the battery compartment, causing it to malfunction. This can lead to inaccurate insulin delivery, which can result in hyperglycemia or hypoglycemia.
Additionally, the adhesive that holds the infusion set in place may not stick well to wet skin, which can increase the risk of the infusion set falling out.
It is important to note that some insulin pumps are now waterproof and can be worn while bathing or swimming. However, it is still important to check the manufacturer's instructions before doing so.
Choice B rationale:
Correct. Even though insulin pumps deliver insulin continuously, people who use them still need to monitor their blood glucose levels regularly. This is because many factors can affect blood glucose levels, such as food intake, exercise, stress, and illness.
Monitoring blood glucose levels allows people to adjust their insulin doses as needed to keep their blood glucose levels within a target range.
Recommended frequency of blood glucose monitoring:
Before meals and snacks Two hours after meals At bedtime
Before and after exercise During times of illness or stress
Whenever they feel symptoms of hypoglycemia or hyperglycemia
Choice C rationale:
Incorrect. People who use insulin pumps still need to count carbohydrates. This is because the amount of insulin that is needed to cover a meal depends on the amount of carbohydrates in the meal.
The insulin pump can be programmed to deliver different amounts of insulin for different meals, snacks, and corrections based on carbohydrate intake. This allows for more precise insulin dosing and better blood glucose control.
Choice D rationale:
Incorrect. Insulin pumps are not designed to help people lose weight. They are designed to help people manage their blood glucose levels.
While some people may lose weight when they start using an insulin pump, this is usually due to improved blood glucose control rather than the pump itself.
The patient’s vital signs are: T=99.1, HR=80, BP=109/62, RR=18, SPO2=97%. What should the nurse do first?
Explanation
Choice A rationale:
Hypoglycemia is a critical consideration: The patient's symptoms of lethargy, diaphoresis, and combativeness, along with recent insulin administration, raise a strong suspicion of hypoglycemia (low blood sugar). Hypoglycemia can quickly progress to coma and seizures if not promptly treated, making it a high priority to assess and address.
Bedside glucose testing is rapid and reliable: A bedside finger stick blood glucose test is a quick, non-invasive, and accurate way to determine the patient's blood sugar level. It provides immediate results, allowing for prompt intervention if hypoglycemia is confirmed.
Other assessments and interventions can follow: Once hypoglycemia is ruled out or confirmed, the nurse can proceed with other assessments and interventions as needed.
Choice B rationale:
Insulin administration without blood sugar confirmation is dangerous: Administering insulin without first checking the patient's blood sugar could worsen hypoglycemia if it is already present. This could lead to severe complications, including neurological damage or even death.
Insulin timing is not a priority: While the next dose of insulin may be due, its administration is not the most urgent priority in this situation. Addressing the patient's immediate symptoms and potential hypoglycemia takes precedence.
Choice C rationale:
Naloxone is not indicated for hypoglycemia: Naloxone is an opioid antagonist used to reverse opioid overdose. It has no effect on hypoglycemia and would not be appropriate in this case.
Choice D rationale:
Oxygen therapy may not address the underlying issue: While oxygen therapy can be beneficial for patients with respiratory distress, it does not address the potential hypoglycemia in this case. If the patient's lethargy and combativeness are due to low blood sugar, oxygen therapy alone would not be sufficient treatment.
Oxygen saturation is already within normal limits: The patient's oxygen saturation (SPO2) is 97%, indicating that their oxygenation is currently adequate. Oxygen therapy would not be indicated unless there were signs of hypoxia.
Sign Up or Login to view all the 48 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

