Please set your exam date
Immediate Newborn Care
Study Questions
Newborns’ Basic Needs
A nurse is caring for a newborn who was delivered 30 minutes ago.
The newborn is placed skin-to-skin with the mother and covered with a dry cloth and a hat.
What is the primary purpose of this intervention?
Explanation
The correct answer is choice B. To prevent hypothermia in the newborn.This is because newborns are at a higher risk of losing heat through various mechanisms, such as evaporation, conduction, convection, and radiation.Placing the newborn skin-to-skin with the mother and covering with a dry cloth and a hat helps to conserve heat and prevent cold stress.
Choice A is wrong because promoting bonding between the mother and the newborn is not the primary purpose of this intervention, although it is a beneficial outcome.
Choice C is wrong because stimulating the newborn’s respiratory effort is not the primary purpose of this intervention, although it may help to reduce apnea and bradycardia.
Choice D is wrong because facilitating early initiation of breastfeeding is not the primary purpose of this intervention, although it may enhance lactation and milk transfer.

A nurse is assessing a newborn who has not cried or breathed spontaneously since birth.
The nurse rubs the newborn’s back and feet, but there is no response.
What is the next action that the nurse should take?
Explanation
The correct answer is choice C. Provide positive pressure ventilation with a bag and mask.
This is because the newborn has not established spontaneous breathing and needs immediate respiratory support.According to the NRP 7th edition, positive pressure ventilation should be initiated within the first minute of life for non-breathing or gasping newborns.
Choice A is wrong because chest compressions are only indicated if the heart rate is below 60 beats per minute after 30 seconds of effective ventilation.
Choice B is wrong because oxygen via nasal cannula is not an appropriate method of delivering oxygen to a non-breathing newborn.
Choice D is wrong because suctioning the newborn’s mouth and nose with a bulb syringe may cause bradycardia and delay ventilation.
The normal respiratory rate for a newborn is 30 to 60 breaths per minute.The normal heart rate for a newborn is 100 to 160 beats per minute.

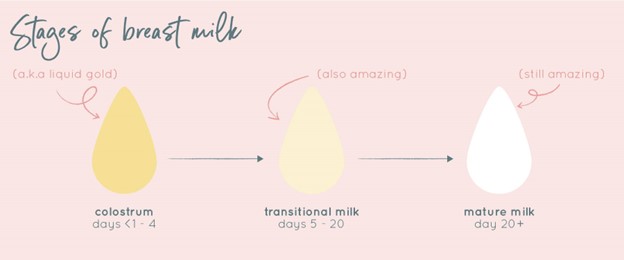
A nurse is teaching a new mother about the benefits of colostrum, the first breast milk.
Which of the following statements by the mother indicates an understanding of the teaching?
Explanation
The correct answer is choice B. Colostrum will protect my baby from getting sick.This is because colostrum contains antibodies and white blood cells that help strengthen the baby’s immune system and fight off infections.Colostrum also coats the baby’s intestines and prevents harmful bacteria from being absorbed.
Choice A is wrong because colostrum does not directly affect the baby’s growth or strength.
It does provide ideal nutrition for a newborn, but it is not the only factor that influences growth and development.
Choice C is wrong because colostrum does not make the baby sleep better at night.It does have a laxative effect that helps the baby clear meconium (the first poop) and reduces the risk of jaundice, but this does not affect sleep quality.
Choice D is wrong because colostrum does not prevent the baby from having allergies.It does contain some factors that may help modulate the immune response and reduce inflammation, but it cannot guarantee that the baby will not develop any allergic reactions
A nurse is administering prophylactic eye ointment and vitamin K injection to a newborn within 1 hour of birth.
What are the rationales for these interventions? (Select all that apply.)
Explanation
The correct answer is choice A and B. The rationale for these interventions are:
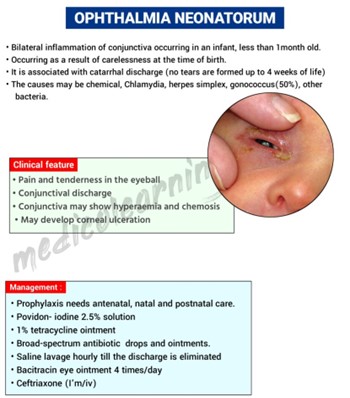
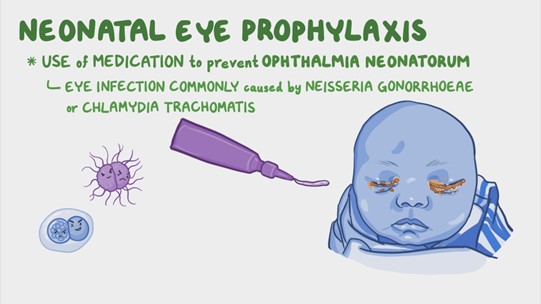
• Choice A: To prevent ophthalmia neonatorum caused by gonorrhea or chlamydia.
This is a serious eye infection that can lead to blindness if untreated.Prophylactic eye ointment, such as erythromycin, is given to the newborn within 1 hour of birth to prevent this infection.
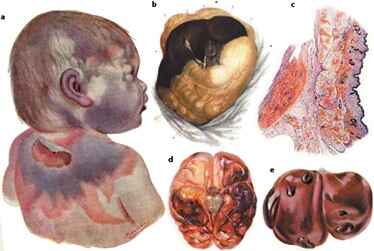
• Choice B: To prevent hemorrhagic disease of the newborn caused by vitamin K deficiency.
This is a bleeding disorder that can occur due to low levels of vitamin K, which is essential for blood clotting.
Newborns are at risk of vitamin K deficiency because their colon is sterile and they do not produce enough of it.Vitamin K injection is given to the newborn within 1 hour of birth to prevent this disease.
• Choice C: To prevent retinopathy of prematurity caused by oxygen toxicity.
This is incorrect because retinopathy of prematurity is a condition that affects premature infants who receive high levels of oxygen therapy.
It causes abnormal blood vessel growth in the retina, which can lead to vision loss.
This intervention is not relevant for a term newborn who does not need oxygen therapy.
• Choice D: To prevent neonatal jaundice caused by bilirubin accumulation.
This is incorrect because neonatal jaundice is a common condition that occurs when the newborn
Erythromycin Eye Ointment
A nurse is preparing to administer erythromycin eye ointment to a newborn.
What is the purpose of this intervention?
Explanation
The correct answer is choice B. To prevent ophthalmia neonatorum, a serious eye infection caused by gonorrhea or chlamydia.Erythromycin eye ointment is an antibiotic that kills bacteria and is used to prevent neonatal conjunctivitis, which can lead to blindness if untreated.Erythromycin is the only approved agent available in the United States for prevention of ophthalmia neonatorum.
Choice A is wrong because erythromycin eye ointment does not prevent dryness and irritation of the eyes.It is used to treat bacterial eye infections like bacterial conjunctivitis, bacterial keratitis, blepharitis and infectious uveitis.
Choice C is wrong because erythromycin eye ointment does not prevent retinopathy of prematurity, a condition that can lead to blindness in premature infants.Retinopathy of prematurity is caused by abnormal growth of blood vessels in the retina and is not related to bacterial infection.
Choice D is wrong because erythromycin eye ointment does not prevent conjunctivitis, a common eye infection in newborns.
Conjunctivitis can be caused by viruses, fungi, parasites or allergens, which erythromycin cannot treat.Erythromycin only prevents conjunctivitis caused by gonorrhea or chlamydia.
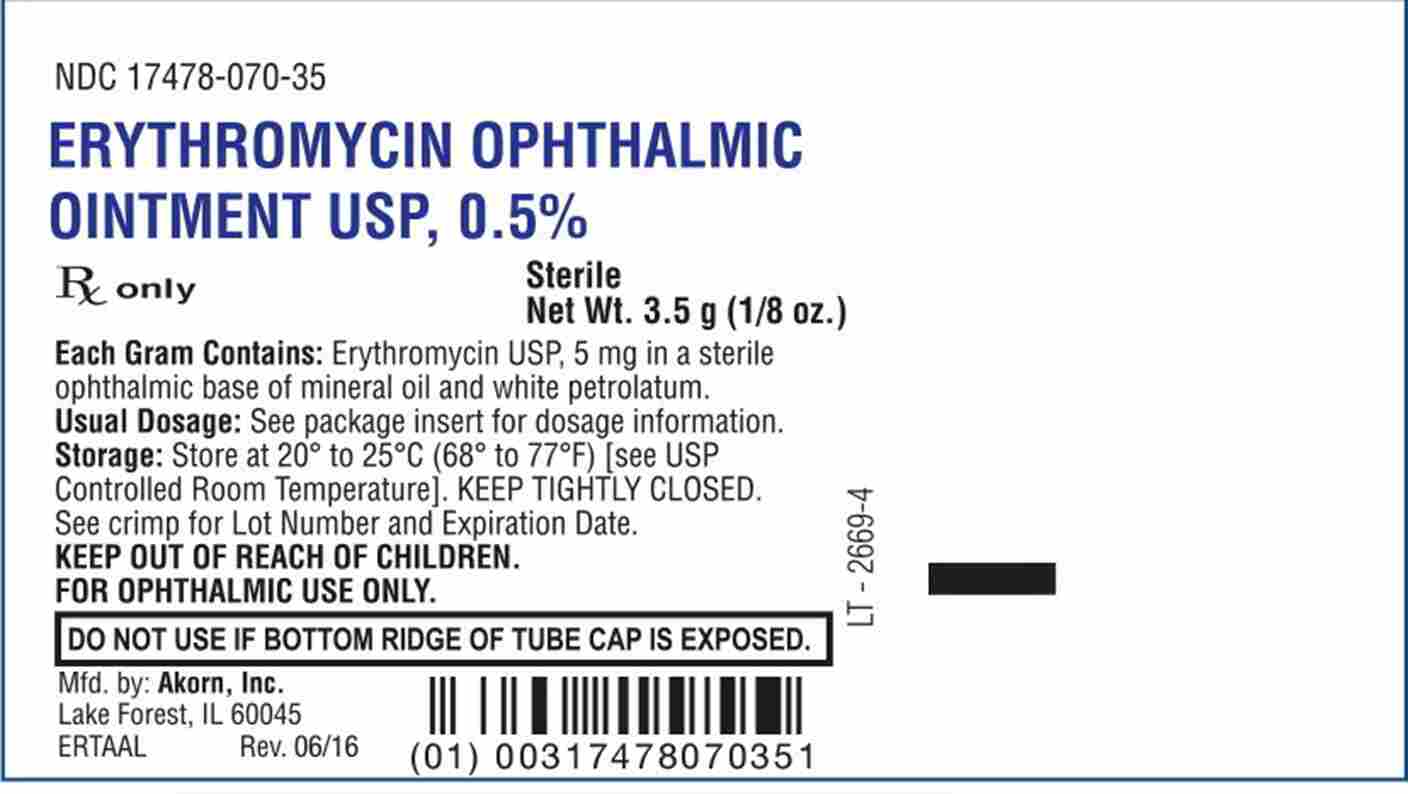
A nurse is checking the medication label of erythromycin eye ointment before applying it to a newborn’s eyes.
What information should the nurse verify on the label? (Select all that apply)
Explanation
The correct answer is choice A, B and C. The nurse should verify the name, dose and expiry date of the medication on the label before applying it to a newborn’s eyes.
This is to ensure that the medication is appropriate, safe and effective for the intended purpose.
Choice D is wrong because the route of administration of the medication is already known.Erythromycin eye ointment is applied to the lower eyelids of the newborn’s eyes.
Choice E is wrong because the frequency of administration of the medication is also already known.Erythromycin eye ointment is usually applied once soon after birth.
Erythromycin eye ointment is used for the prevention of neonatal conjunctivitis, which is an eye infection caused by bacteria that can enter the baby’s eyes during childbirth.It can cause serious complications such as blindness if left untreated.
A nurse is applying erythromycin eye ointment to a newborn’s eyes.
How much ointment should the nurse squeeze into the lower conjunctival sac of each eye?
Explanation
The correct answer is choice B. 0.5 cm.According to the PEDIATRIC NEWBORN MEDICINE CLINICAL PRACTICE GUIDELINES, a thin strip of erythromycin eye ointment should be applied to the lower conjunctival sac of each eye of the newborn within 24 hours after birth.
The length of the strip should be approximately 0.5 cm (or 1/4 inch).This is done to prevent neonatal conjunctivitis, also known as ophthalmia neonatorum, which is a serious eye infection caused by bacteria such as Neisseria gonorrhoeae.
Choice A is wrong because 0.25 cm is too short and may not provide adequate coverage of the eye.
Choice C is wrong because 1 cm is too long and may cause excessive ointment to spill out of the eye.
Choice D is wrong because 2 cm is way too long and may cause irritation and discomfort to the eye.
The normal range for erythromycin eye ointment application is 0.5 cm to 1 cm, but the recommended dose is 0.5 cm.
A nurse is applying erythromycin eye ointment to a newborn’s eyes.
What should the nurse do after applying the ointment?
Explanation
The correct answer is choice B. Do not rub or wipe the eyes after applying the ointment.This is because rubbing or wiping the eyes can cause irritation and remove the ointment from the conjunctival sac, where it is supposed to act against bacterial infections.
Choice A is wrong because rubbing or wiping the eyes gently does not spread the ointment evenly and can cause harm to the newborn’s eyes.
Choice C is wrong because rinsing the eyes with sterile saline solution can wash away the ointment and reduce its effectiveness.
Choice D is wrong because covering the eyes with sterile gauze pads can interfere with eye-to-eye contact between the newborn and parents, which is important for bonding and attachment.
A nurse is teaching a new mother about erythromycin eye ointment for her newborn.
What should the nurse include in the teaching? (Select all that apply)
Explanation
The correct answer is choice A and E.The ointment should be administered within 1-2 hours of birth to be effective and may cause minor ocular irritation or redness that lasts for 24-48 hours.
Choice B is wrong because the ointment does not affect the newborn’s ability to see.The ointment may cause temporary blurred vision, but this does not impair the newborn’s vision development.
Choice C is wrong because the ointment does not increase the risk of bleeding if the newborn is also given vitamin K injection.Vitamin K injection is given to prevent bleeding disorders in newborns and has no interaction with erythromycin ointment.
Choice D is wrong because the ointment is not required by law in all states of the United States to prevent eye infections in newborns.
Some states have laws that mandate the use of erythromycin ointment for newborns, but others do not.However, it is recommended by the American Academy of Pediatrics and the Centers for Disease Control and Prevention as a standard of care.
Vitamin K Injection
A nurse is preparing to administer vitamin K injection to a newborn.
Which of the following actions should the nurse take before drawing up the medication?
Explanation
The correct answer is choice C. Check the medication label for the name, dose, expiry date and route of administration.
This is a standard precaution that should be taken before administering any medication to ensure patient safety and avoid medication errors.
Choice A is wrong because checking the newborn’s blood type and Rh factor is not necessary before giving vitamin K injection.
Vitamin K is not a blood product and does not depend on blood compatibility.
Choice B is wrong because checking the newborn’s bilirubin level and jaundice score is not relevant to vitamin K injection.Vitamin K is given to prevent vitamin K deficiency bleeding (VKDB), which is a serious condition that can cause bleeding in the brain or other organs.
Bilirubin level and jaundice score are indicators of neonatal jaundice, which is a common condition that causes yellowing of the skin and eyes due to excess bilirubin in the blood.
Choice D is wrong because checking the newborn’s weight and length measurements is not required before giving vitamin K injection.The recommended dose of vitamin K for newborns weighing more than 1500 g is 1 mg as a single intramuscular injection within 6 hours of birth.For preterm infants weighing less than 1500 g, the dose is 0.3 mg/kg to 0.5 mg/kg.
The dose does not depend on the exact weight or length of the newborn.
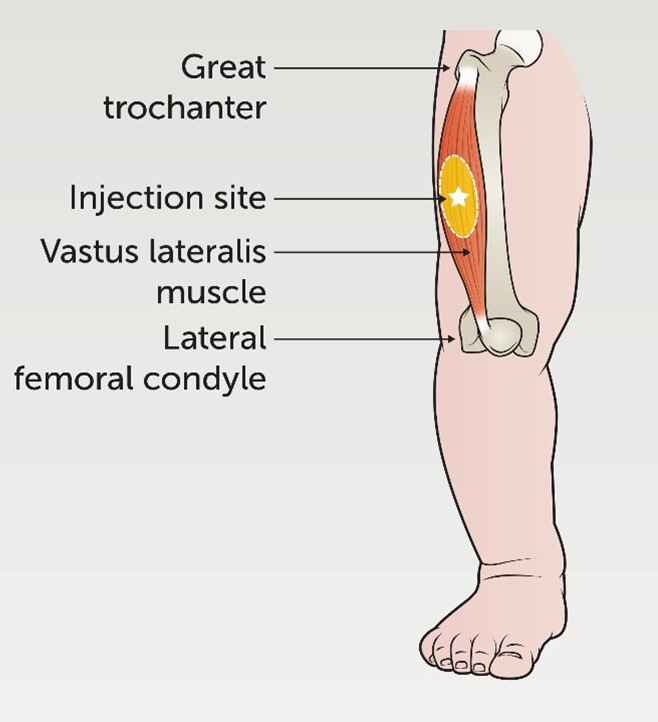
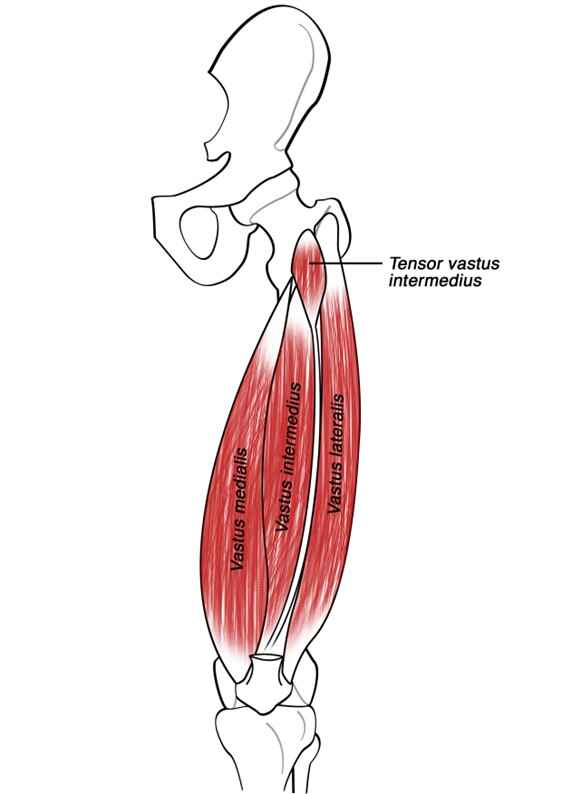
A nurse is administering vitamin K injection to a newborn using the vastus lateralis muscle as the injection site.
Which of the following techniques should the nurse use to ensure proper needle placement?
Explanation
The correct answer is choice B. Locate the greater trochanter and the lateral femoral condyle and use the middle third of this line.This technique ensures proper needle placement in the vastus lateralis muscle, which is the preferred site for vitamin K injection in newborns.Vitamin K is given to prevent vitamin K deficiency bleeding (VKDB), which can cause serious bleeding problems in newborns.
Choice A is wrong because dividing the thigh into thirds horizontally and vertically and using the outer middle third of the thigh is a technique for locating the dorsogluteal site, which is not recommended for newborns.
Choice C is wrong because palpating the anterior iliac spine and the mid-patella and using the lateral aspect of this line is a technique for locating the rectus femoris site, which is an alternative site for vitamin K injection in newborns but not as preferred as the vastus lateralis site.
Choice D is wrong because identifying the midpoint of a line drawn from the anterior superior iliac spine to the pubic tubercle and using this point is a technique for locating the ventrogluteal site, which is not recommended for newborns.
A nurse has administered vitamin K injection to a newborn.
Which of the following statements by the nurse indicates an understanding of the rationale for this intervention?
Explanation
The correct answer is choice A. This injection will help prevent your baby from developing a bleeding disorder caused by low vitamin K levels.
Vitamin K is essential for the synthesis of clotting factors in the liver.
Newborns have low levels of vitamin K because it does not cross the placenta well and they have limited gut flora to produce it.
Therefore, they are at risk of vitamin K deficiency bleeding (VKDB), which can cause serious and potentially fatal hemorrhages.To prevent VKDB, the American Academy of Pediatrics recommends a single intramuscular dose of 1 mg of vitamin K to all newborn infants within 6 hours of birth.
Choice B is wrong because vitamin K does not boost the immune system or protect from infections.
Choice C is wrong because vitamin K does not stimulate liver function or metabolism.
Choice D is wrong because vitamin K does not increase appetite or growth.
A nurse is caring for a newborn who did not receive vitamin K injection at birth due to parental refusal.
Which of the following signs and symptoms should alert the nurse to a possible vitamin K deficiency bleeding (VKDB)?
Explanation
The correct answer is choice A.Petechiae, ecchymosis, or oozing from puncture sites are signs and symptoms of vitamin K deficiency bleeding (VKDB) in newborns.VKDB is a rare form of bleeding disorder that affects newborns and young infants due to low stores of vitamin K at birth.Vitamin K is a substance that our body needs to form clots and to stop bleeding.
Choice B is wrong because pallor, tachycardia, or poor perfusion are signs of anemia or shock, which can have many causes other than VKDB.
Choice C is wrong because jaundice, dark urine, or clay-colored stools are signs of liver disease or biliary obstruction, which can affect vitamin K absorption but are not specific for VKDB.
Choice D is wrong because hypoglycemia, lethargy, or jitteriness are signs of low blood sugar or neonatal abstinence syndrome, which are not related to VKDB.
Hypoglycemia
A nurse is caring for a newborn who was born to a mother with diabetes mellitus.
The nurse should monitor the newborn for which of the following signs of hypoglycemia?
Explanation
The correct answer is choice D. All of the above.
Hypoglycemia is a condition where the blood sugar level is too low.It can cause various signs and symptoms in newborns, such as jitteriness, weak cry, seizures, and more.
Choice A is wrong because jitteriness is not the only sign of hypoglycemia in newborns.
It is one of the possible signs, but not the only one.
Choice B is wrong because a weak cry is not the only sign of hypoglycemia in newborns.
It is one of the possible signs, but not the only one.
Choice C is wrong because seizures are not the only sign of hypoglycemia in newborns.
They are one of the possible signs, but not the only one.
Some of the risk factors for hypoglycemia in newborns are being born to a mother with diabetes, being small or large for gestational age, being preterm, having infection, or having metabolic or hormonal disorders.The normal range of blood sugar for newborns is usually between 47 and 150 mg/dL.
A nurse is teaching a mother about prevention and recognition of hypoglycemia in her newborn.
Which of the following statements by the mother indicates an understanding of the teaching?
Explanation
The correct answer is choice D. All of the above.
The mother demonstrates an understanding of the teaching by stating that she should feed her baby every 2 to 3 hours, check her baby’s blood glucose level if he is not feeding well, and keep her baby warm and close to her.
These are all measures to prevent and recognize hypoglycemia in newborns.
Hepatitis B Vaccine
A nurse is preparing to administer hepatitis B vaccine to a newborn.
Which syringe, needle, and injection site should the nurse use?
Explanation
The correct answer is choice B. 1 ml syringe, 25-gauge needle, vastus lateralis muscle.This is because the vastus lateralis muscle is the preferred site for intramuscular injections in infants, and a 25-gauge needle is appropriate for the viscosity of the hepatitis B vaccine.A 1 ml syringe can deliver the required dose of 0.5 ml for newborns.
Choice A is wrong because the anterolateral aspect of upper thigh is not a recommended site for intramuscular injections in infants.
Choice C is wrong because the deltoid muscle is not well developed in infants and may not have enough muscle mass to absorb the vaccine.
Choice D is wrong because the ventrogluteal muscle is not a recommended site for intramuscular injections in infants, and a 23-gauge needle may cause more pain and tissue damage than a 25-gauge needle.
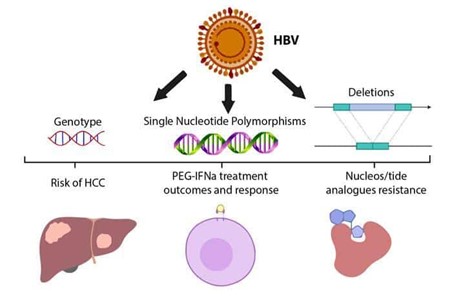
A client who is pregnant asks the nurse if she needs to get vaccinated against hepatitis B virus (HBV).
What is the best response by the nurse?
Explanation
The correct answer is A.“Yes, you need to get vaccinated because HBV can be transmitted from mother to child during pregnancy or delivery.” This statement is correct because HBV is a blood-borne virus that can infect the fetus through the placenta or during birth.Vaccination can prevent HBV infection and its complications, such as chronic liver disease or cancer.
Statement B is wrong because HBV is a serious disease that affects the liver and can cause inflammation, scarring, cirrhosis, or failure.
Statement C is wrong because although HBV can cause chronic liver disease or cancer in later life, this is not the main reason for vaccination during pregnancy.The main reason is to prevent transmission to the baby.
Statement D is wrong because HBV is not only spread through contact with infected blood or body fluids, but also through sexual contact, sharing needles, or from mother to child.
Normal ranges for HBV tests are:
• HBsAg (hepatitis B surface antigen): negative
• Anti-HBs (antibody to hepatitis B surface antigen): positive after vaccination
• Anti-HBc (antibody to hepatitis B core antigen): negative
• HBeAg (hepatitis B e antigen): negative
• Anti-HBe (antibody to hepatitis B e antigen): positive after recovery
• HBV DNA: undetectable
A nurse is reviewing the immunization schedule for hepatitis B vaccine with a parent of a 2-month-old infant.
The nurse informs the parent that the infant should receive the second dose of the vaccine at what age?
Explanation
The correct answer is choice C. The infant should receive the second dose of the hepatitis B vaccine at 4 months of age.This is based on the recommended 3-dose vaccine series for infants, which includes a birth dose, a second dose at 1 month, and a third dose at 6 months.The 4-dose combination vaccine series, which includes a pentavalent or hexavalent vaccine, also requires a birth dose, followed by doses at 6 weeks, 4 months, and 6 months.
Choice A is wrong because 1 month is too early for the second dose.The minimum interval between the first and second doses is 4 weeks.
Choice B is wrong because 2 months is also too early for the second dose.The minimum interval between the first and second doses is 4 weeks, and the second dose should be given at least 8 weeks after the first dose.
Choice D is wrong because 6 months is too late for the second dose.The second dose should be given at least 8 weeks after the first dose, and the third dose should be given at least 8 weeks after the second dose and at least 16 weeks after the first dose.
A client who has been exposed to hepatitis B virus (HBV) asks the nurse what he can do to prevent infection.
The nurse explains that the client can receive which of the following interventions? (Select all that apply)
Explanation
The correct answer is choice A and B.
Hepatitis B vaccine and hepatitis B immune globulin (HBIG) are the recommended interventions for a person who has been exposed to hepatitis B virus (HBV) through a distinct, identifiable exposure to blood or body fluids that contain blood.Hepatitis B vaccine provides active immunity by stimulating the production of antibodies against HBV, while HBIG provides passive immunity by giving temporary antibodies from another source.
Choice C is wrong because antiviral medication is not indicated for postexposure prophylaxis of HBV, but rather for the treatment of chronic HBV infection.
Choice D is wrong because antibiotics are not effective against viral infections such as HBV.
Choice E is wrong because blood transfusion is not a preventive measure for HBV infection, but rather a potential source of exposure to HBV and other bloodborne pathogens.
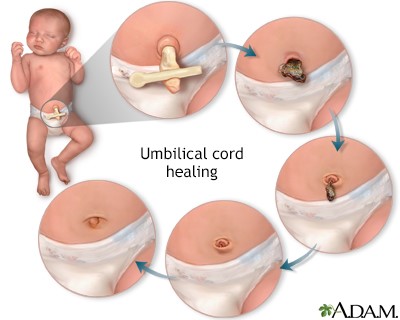
Umbilical cord care
A nurse is teaching a new mother how to care for her baby’s umbilical cord stump at home.
Which of the following instructions should the nurse include? (Select all that apply.)
Explanation
The correct answer is choice B and C.The nurse should instruct the new mother to keep the cord stump above the diaper level to prevent irritation and infectionand to change the diapers frequently and check for signs of wetness or soiling around the cord stump.
Choice A is wrong because applying antiseptic solution to the cord stump is not necessary and may delay healing.The stump should be kept dry and clean with gauze and water only.
Choice D is wrong because giving the baby tub baths with mild soap and water may cause the cord stump to get wet and increase the risk of infection.The baby should be given sponge baths until the cord stump falls off.
Choice E is correct but not part of the question.The nurse should tell the mother to report any signs of infection such as redness, swelling, foul odor, or purulent drainage to the health care provider, but this is not an instruction on how to care for the cord stump at home.
A nurse is assessing a newborn’s umbilical cord after delivery.
What is the normal number of vessels in the cord?
Explanation
The correct answer is choice C. Three.The normal number of vessels in the umbilical cord is three: one umbilical vein and two umbilical arteries.The umbilical vein carries oxygenated blood and nutrients from the placenta to the fetus, while the umbilical arteries carry deoxygenated blood and waste products from the fetus to the placenta.
Choice A is wrong because one vessel in the umbilical cord is not enough to support the fetal circulation.Choice B is wrong because two vessels in the umbilical cord is a condition called two-vessel cord or single umbilical artery, which can be associated with some birth defects or growth problems.Choice D is wrong because four vessels in the umbilical cord is not a normal variation and can cause complications such as cord prolapse or knotting.The normal range of the umbilical cord length is 50-60 cm and the diameter is 1-2 cm.
A nurse is monitoring a newborn’s temperature and notes that it is 97.2°F (36.2°C).
What is the most appropriate action for the nurse to take?
Explanation
The correct answer is choice A. Recheck the temperature in 15 minutes.The normal temperature range for newborn babies is between 96.8°F and 100.3°F, with the average being 98.6°F.A rectal reading is the most accurate way to take a baby’s temperature.A fever is considered to be a temperature of 100.4°F or higher.If a baby is under 3 months old and has a fever of 100.4°F or higher, it requires urgent care and a pediatrician should be called immediately.
However, if the baby’s temperature is slightly below the normal range, it may not be a cause for concern.It could be due to being wrapped up tightly in a blanket, in a very warm room, very active, cuddling a hot water bottle, wearing a lot of clothes or having a bath.Therefore, the nurse should recheck the temperature in 15 minutes after allowing the baby to cool down for a few minutes.
Choice B is wrong because notifying the health care provider immediately is not necessary unless the baby has a fever of 100.4°F or higher or other signs of illness.
Choice C is wrong because placing the newborn under a radiant warmer is not appropriate unless the baby has hypothermia
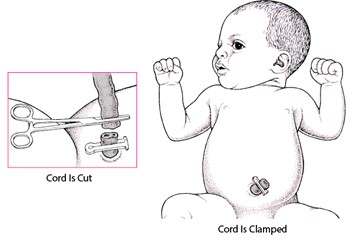
A nurse is preparing to clamp and cut a newborn’s umbilical cord with sterile instruments.
When should the nurse perform this procedure?
Explanation
The correct answer is choice A. The nurse should clamp and cut the newborn’s umbilical cord within 1 to 3 minutes after birth.This is because delaying the cord clamping for longer than 3 minutes may increase the risk of jaundice in the baby.
Jaundice is a condition where the skin and eyes turn yellow due to high levels of bilirubin in the blood.
Bilirubin is a waste product that is normally removed by the liver, but in newborns, the liver may not be fully developed yet.
Choice B is wrong because waiting for 5 to 10 minutes after birth to clamp and cut the cord may not have any significant benefits for the baby compared to clamping within 1 to 3 minutes.Choice C is wrong because waiting for 15 to 20 seconds after birth to clamp and cut the cord is too early and may deprive the baby of some blood, oxygen, and nutrients that are still flowing from the placenta.Choice D is wrong because waiting for 30 to 45 minutes after birth to clamp and cut the cord is too late and may expose the baby to infection or bleeding from the cord.
The umbilical cord is a vital connection between the baby and the placenta during pregnancy and delivery.
It delivers oxygen and nutrients to the baby and removes waste products from the baby’s blood.
After birth, the cord continues to function for a few minutes until it stops pulsing.The optimal time to clamp and cut the cord depends on various factors, such as the baby’s gestational age, health condition, and risk of jaundice.
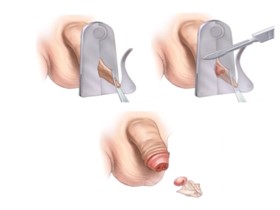
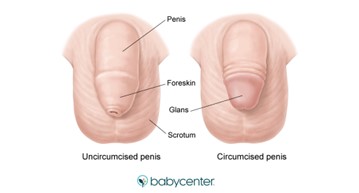
Circumcision care
A nurse is caring for a newborn who has just undergone circumcision using the Gomco clamp method.
What should the nurse do to prevent the diaper from sticking to the penis?
Explanation
The correct answer is choice A. Apply petroleum jelly with each diaper change for at least 24 hours.This will prevent the diaper from sticking to the penis and causing irritation or infection.The Gomco clamp method involves using a steel bell that protects the glans penis during the circumcision and does not leave any foreign body at the site afterwards.
Choice B is wrong because a sterile dressing is not necessary and may interfere with the healing process.
Choice C is wrong because antibiotic ointment is not recommended and may cause allergic reactions or resistance.
Choice D is wrong because cold compresses are not effective and may cause discomfort or tissue damage.

A nurse is teaching a new mother about circumcision care at home.
What should the nurse include in the teaching? (Select all that apply.)
Explanation
The correct answer is choice B and C. The nurse should include in the teaching that the mother should observe for signs of bleeding, infection or delayed healing, and seek medical attention if signs of complications are present.
These are important steps to prevent and treat any possible problems after circumcision.
Choice A is wrong because tub baths are not harmful for circumcision healing.According to wikiHow, sponge baths are recommended for newborns, but older children or adolescents may shower or take a tub bath for comfort.
Choice D is wrong because pulling back the remaining foreskin can cause pain and bleeding.
The foreskin should be left alone until it heals completely.According to Verywell Family, skin adhering to the glans can cause penile adhesion and may require surgery.
Choice E is wrong because oral sucrose solution is not an effective pain relief for circumcision.
According to Mayo Clinic, oral sucrose solution may help reduce crying during minor procedures, but it does not reduce pain signals in the brain or spinal cord.
Other methods of pain relief, such as acetaminophen, topical anesthetic cream or a pacifier dipped in sugar water, may be more helpful.
A nurse is assisting the practitioner with a circumcision using the Mogen clamp method.
What should the nurse do during the procedure?
Explanation
The correct answer is choice A. Comfort and maintain the newborn’s safety by holding his hands and legs securely.This is because the Mogen clamp method does not directly protect the glans during the procedureand requires the safe placement of the clamp to avoid injuring the glans.
Therefore, the nurse should help immobilize the newborn and prevent any sudden movements that could cause harm.
Choice B is wrong because monitoring the newborn’s vital signs and oxygen saturation continuously is not necessary for this procedure.The Mogen clamp method is fast and does not leave a foreign body at the circumcision site.
Choice C is wrong because applying a topical anesthetic cream to the penis 30 minutes before the procedure is not effective for pain relief.The Mogen clamp method requires local anesthesia, such as lidocaine injection or dorsal penile nerve block.
Choice D is wrong because providing oral sucrose solution to the newborn using a pacifier or syringe is not sufficient for pain management.The Mogen clamp method requires local anesthesia, such as lidocaine injection or dorsal penile nerve block.Oral sucrose solution can be used as an adjunctive measure, but not as a sole intervention.
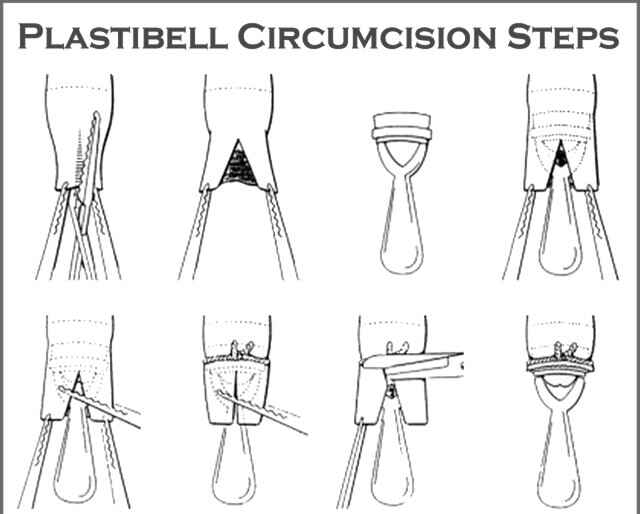
The nurse has just assisted with a circumcision using a Plastibell device and notices that there is a yellowish exudate on the glans penis of an infant on his second day after circumcision.
The nurse should:
Explanation
The correct answer is choice C. Recognize this as an expected finding.
The yellowish exudate on the glans penis of an infant on his second day after circumcision is a normal sign of healing and does not indicate infection.
It should not be washed off or treated with antibiotic ointment as this may interfere with the healing process or cause irritation.
The nurse should only notify the physician if there are signs of bleeding, swelling, redness, foul odor, or pus.
Choice A is wrong because notifying the physician immediately is not necessary unless there are signs of infection or complications.
Choice B is wrong because washing off the exudate with warm water may remove the protective layer of tissue that forms over the glans penis and cause bleeding or pain.
Choice D is wrong because applying an antibiotic ointment may cause allergic reactions, skin irritation, or resistance to the antibiotic.
The Plastibell device does not require any special care other than keeping the area clean and dry.
More questions on this topic
A nurse is assessing a newborn’s vital signs at 1 hour of age.
Which of the following findings should the nurse report to the provider?
Explanation
The correct answer is choice C. A temperature of 36°C (96.8°F) is below the normal range for a newborn, which is 36.5°C to 37.5°C (97.7°F to 99.5°F).
A low temperature can indicate hypothermia, infection, or hypoglycemia, and should be reported to the provider.
Choice A is wrong because a heart rate of 140/min is within the normal range for a newborn, which is 120 to 160/min.
Choice B is wrong because a respiratory rate of 50/min is within the normal range for a newborn, which is 30 to 60/min.
Choice D is wrong because a blood pressure of 60/40 mm Hg is within the normal range for a newborn, which is 50 to 75/30 to 45 mm Hg.
A nurse is preparing to administer hepatitis B vaccine to a newborn whose mother is hepatitis B surface antigen negative (HBsAg-).
Which of the following actions should the nurse take?
Explanation
The correct answer is choice B. Give the vaccine intramuscularly in the anterolateral thigh.
This is because the anterolateral thigh is the recommended site for intramuscular injections in infants less than 12 months of age.
It has a large muscle mass and minimal risk of injury to nerves or blood vessels.
Choice A is wrong because informed consent is not required for routine immunizations, unless the parent or guardian requests more information or declines the vaccine.
Choice C is wrong because hepatitis B immune globulin (HBIG) is only indicated for newborns whose mothers are hepatitis B surface antigen positive (HBsAg+), as they have a high risk of acquiring the infection from their mothers.
Choice D is wrong because there is no need to delay giving the vaccine until after breastfeeding is established.
Breastfeeding does not interfere with the vaccine’s effectiveness or safety, and it does not increase the risk of adverse reactions.
A nurse is performing an initial assessment of a newborn who was delivered vaginally at term with no complications.
Which of the following findings should alert the nurse to a potential problem?
Explanation
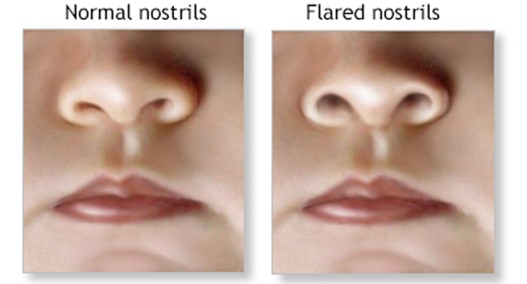
The correct answer is choice C. Nasal flaring and grunting are signs of respiratory distress in a newborn and should alert the nurse to a potential problem.
The nurse should monitor the newborn’s respiratory rate, oxygen saturation, and chest movements, and notify the provider if the symptoms persist or worsen.
Choice A is wrong because molding of the head is a normal finding in a newborn who was delivered vaginally.
It is caused by the pressure of the birth canal on the skull bones and usually resolves within a few days.
Choice B is wrong because acrocyanosis of hands and feet is a normal finding in a newborn during the first 24 hours of life.
It is caused by poor peripheral circulation and does not indicate hypoxia or cyanosis.
Choice D is wrong because vernix caseosa on skin folds is a normal finding in a newborn.
It is a white, cheesy substance that protects the skin from amniotic fluid and helps with thermoregulation.
It usually disappears within a few days.
A nurse is caring for a newborn who has received erythromycin eye ointment as prophylaxis for ophthalmia neonatorum.
What should the nurse monitor for as a potential adverse reaction to this medication?
Explanation
The correct answer is choice A. Hypersensitivity.Erythromycin eye ointment is an antibiotic that can cause allergic reactions in some newborns, such as irritation, redness, swelling, or cloudy eyes.
This is a potential adverse reaction to this medication that the nurse should monitor for.
Choice B. Glaucoma is wrong because glaucoma is a condition that causes increased pressure in the eye and can damage the optic nerve.
It is not caused by erythromycin eye ointment.
Choice C. Cataracts is wrong because cataracts are a condition that causes clouding of the lens of the eye and can impair vision.
It is not caused by erythromycin eye ointment.
Choice D. Strabismus is wrong because strabismus is a condition that causes misalignment of the eyes and can affect depth perception.
It is not caused by erythromycin eye ointment.
Erythromycin eye ointment is used to prevent ophthalmia neonatorum, which is an infection of the eye surface that affects newborns within the first month of life.It can be caused by bacteria such as chlamydia or gonorrhea that can enter the baby’s eyes during childbirth and cause permanent damage to the corneas.Erythromycin eye ointment can help prevent vision loss caused by these bacteria.
A nurse is administering erythromycin eye ointment to a newborn who has a history of allergic reaction to penicillin.
What should the nurse do before applying the ointment?
Explanation
The correct answer is choice B. Check if there is any cross-sensitivity between erythromycin and penicillin.Erythromycin is a macrolide antibiotic that can be used to treat bacterial eye infections in newborns and adults.
Penicillin is a beta-lactam antibiotic that can cause allergic reactions in some people.
Cross-sensitivity means that a person who is allergic to one type of antibiotic may also be allergic to another type of antibiotic that has a similar structure or mechanism of action.Erythromycin and penicillin have different structures and mechanisms of action, but there is still a small chance of cross-sensitivity between them.
Therefore, the nurse should check if the newborn has any history of allergic reaction to penicillin before applying the erythromycin eye ointment.
Choice A is wrong because asking the mother if she has any allergies to antibiotics is not enough to determine if the newborn is at risk of an allergic reaction to erythromycin.
The newborn may have inherited or developed an allergy to penicillin or erythromycin that the mother does not have.
Choice C is wrong because applying a small amount of ointment on the skin to test for allergic reaction is not a reliable method to diagnose an allergy.Skin testing can cause false positive or false negative results, and it may also trigger a severe allergic reaction in some cases.
Choice D is wrong because administering an antihistamine to prevent anaphylaxis is not appropriate for a newborn who has not been exposed to the allergen yet.
An antihistamine is a medication that blocks the effects of histamine, a chemical that causes allergic symptoms.
Anaphylaxis is a life-threatening allergic reaction that involves multiple organ systems and requires immediate medical attention.An antihistamine cannot prevent anaphylaxis, and it may also cause side effects such as drowsiness, dry mouth, or low blood pressure in a newborn.
A nurse is reviewing laboratory results for a newborn who received vitamin K injection at birth.
Which of the following coagulation factors should be activated by vitamin K?
Explanation
The correct answer is choice A.Factor II, also known as prothrombin, is one of the coagulation factors that are activated by vitamin K.Vitamin K is a cofactor for the carboxylation of specific glutamic acid groups in coagulation factors II, VII, IX, and X.
This process is essential for the activation of these factors in the coagulation cascade.
Choice B is wrong because factor V is not a vitamin K-dependent coagulation factor.
Factor V is activated by thrombin and acts as a cofactor for factor Xa in the conversion of prothrombin to thrombin.
Choice C is wrong because factor VIII is not a vitamin K-dependent coagulation factor.
Factor VIII is activated by thrombin and acts as a cofactor for factor IXa in the activation of factor X.
Choice D is wrong because factor XI is not a vitamin K-dependent coagulation factor.
Factor XI is activated by factor XIIa and activates factor IX in the intrinsic pathway of coagulation.
Normal ranges for coagulation factors are:
• Factor II: 70-120% of normal activity
• Factor V: 50-150% of normal activity
• Factor VIII: 50-150% of normal activity
• Factor IX: 50-150% of normal activity
• Factor X: 70-140% of normal activity
• Factor XI: 70-150% of normal activity
A nurse is caring for a newborn who has early-onset VKDB due to maternal use of anticoagulants during pregnancy.
Which of the following interventions should the nurse anticipate for this newborn?
Explanation
The correct answer is choice A. Administer fresh frozen plasma.This is because fresh frozen plasma contains clotting factors that can help stop the bleeding caused by vitamin K deficiency.Vitamin K is needed for the synthesis of clotting factors in the liver, but newborns have low levels of vitamin K and may develop vitamin K deficiency bleeding (VKDB) if they do not receive prophylaxis at birth.VKDB can manifest as bleeding in various sites, such as the skin, mucous membranes, umbilicus, gastrointestinal tract, or central nervous system.
Choice B is wrong because packed red blood cells do not contain clotting factors and will not correct the underlying deficiency of vitamin K.
Choice C is wrong because intravenous immunoglobulin is used to treat immune-mediated thrombocytopenia, not vitamin K deficiency.
Choice D is wrong because recombinant erythropoietin is used to stimulate red blood cell production in anemia, not to treat bleeding disorders.
Early-onset VKDB occurs within 24 hours of birth and is associated with maternal use of drugs that interfere with vitamin K metabolism, such as anticoagulants, anticonvulsants, or antituberculosis drugs.
These drugs induce the enzymes that break down vitamin K in the fetal liver
A nurse is assessing a newborn who has late-onset VKDB due to exclusive breastfeeding and inadequate oral vitamin K supplementation.
Which of the following findings should indicate a possible intracranial hemorrhage to the nurse?
Explanation
The correct answer is choice A. Bulging fontanelle.
A bulging fontanelle is a sign of increased intracranial pressure, which can be caused by intracranial hemorrhage.
Late-onset VKDB is a condition that occurs in infants who have low levels of vitamin K, which is essential for blood clotting.Most cases of late-onset VKDB present with intracranial hemorrhage.
Choice B. Sunken eyes is wrong because it is a sign of dehydration, not intracranial hemorrhage.
Choice C. Mottled skin is wrong because it is a sign of poor circulation or shock, not intracranial hemorrhage.
Choice D. Flaring nostrils is wrong because it is a sign of respiratory distress, not intracranial hemorrhage.
Normal ranges for vitamin K plasma concentrations are 0.2 to 3.2 ng/mL for adults and 0.15 to 1.5 ng/mL for infants.
A nurse is assessing a newborn who has hypoglycemia due to perinatal asphyxia.
Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
The correct answer is choice A, C, D, and E.Hypoglycemia due to perinatal asphyxia can cause various neurological signs in the newborn, such as irregular respirations, apnea, eye-rolling, and lethargy.
These signs indicate inadequate oxygenation and glucose delivery to the brain.Cyanosis is not a specific sign of hypoglycemia, but rather a sign of poor oxygenation that can occur due to other causes.
Therefore, choice B is wrong.
Choice A is correct because irregular respirations can result from hypoglycemia due to perinatal asphyxia.Hypoglycemia can impair the respiratory center in the brainstem and cause irregular breathing patterns.
Choice C is correct because apnea can result from hypoglycemia due to perinatal asphyxia.
Apnea is defined as a pause in breathing
A nurse is caring for a preterm newborn who has hypoglycemia due to inadequate gluconeogenesis.
The nurse should understand that this condition occurs because preterm newborns have limited stores of which of the following substances?
Explanation
The correct answer is choice A. Glycogen.Preterm newborns have limited stores of glycogen, which is a substance made from glucose that is stored in the liver and muscle cells to be used later for energy.When blood glucose levels are low, the hormone glucagon signals the cells to convert glycogen back into glucose and release it into the bloodstream.However, preterm newborns have a reduced ability to produce glucagon and to use gluconeogenesis, which is the process of making new glucose from other sources.Therefore, they are at risk of hypoglycemia, which is a condition where blood glucose levels are too low to support normal brain function.
Choice B is wrong because glucose is the sugar that travels through the blood to fuel the cells, not a substance that is stored for later use.
Choice C is wrong because insulin is a hormone that helps cells absorb glucose from the blood, not a substance that is stored for later use.
Choice D is wrong because glucagon is a hormone that triggers the release of glucose from the liver and muscle cells, not a substance that is stored for later use.
A nurse is educating a group of college students about hepatitis B virus (HBV) transmission and prevention.
The nurse should emphasize that the most common modes of transmission are which of the following? (Select all that apply)
Explanation
The correct answer is choice A, B, C, D and E.All of these are possible modes of transmission for hepatitis B virus (HBV), which is a viral infection that attacks the liver and can cause both acute and chronic disease.The virus is most commonly transmitted from mother to child during birth and delivery, as well as through contact with blood or other body fluids during sex with an infected partner, unsafe injections or exposures to sharp instruments.
Choice A is correct because unprotected sexual contact can expose a person to the blood, semen, or vaginal fluids of an infected partner.
Choice B is correct because sharing drugs, needles, or “works” when using drugs can expose a person to the blood of an infected person.
Choice C is correct because poor infection control practices in medical settings can expose a person to contaminated needles or syringes or sharp objects that have been used on an infected person.
Choice D is correct because sharing of blood sugar (diabetes) testing equipment can expose a person to the blood of an infected person.
Choice E is correct because needle sticks or sharps exposures on the job can expose a person to the blood of an infected
A nurse is caring for a client who has chronic hepatitis B infection and is taking lamivudine (Epivir).
The nurse should monitor the client for which of the following adverse effects?
Explanation
The correct answer is choice B. Lactic acidosis.
Lamivudine (Epivir) is a nucleoside reverse transcriptase inhibitor (NRTI) used to treat chronic hepatitis B infection and HIV infection.
One of the rare but serious adverse effects of lamivudine is lactic acidosis, which is a condition where the blood becomes too acidic due to the accumulation of lactate.Lactic acidosis can cause symptoms such as nausea, vomiting, abdominal pain, muscle weakness, rapid breathing, and low blood pressure.
Choice A is wrong because pancreatitis is not a common side effect of lamivudine.
Pancreatitis is an inflammation of the pancreas that can cause severe abdominal pain, nausea, vomiting, and fever.Pancreatitis is more likely to occur with other NRTIs such as didanosine (Videx) or stavudine (Zerit).
Choice C is wrong because hypothyroidism is not a common side effect of lamivudine.
Hypothyroidism is a condition where the thyroid gland does not produce enough thyroid hormones, which regulate the metabolism and energy levels of the body.
Hypothyroidism can cause symptoms such as fatigue, weight gain, cold intolerance, dry skin, hair loss, and depression.
Hypothyroidism is more likely to occur with other drugs that interfere with thyroid function such as amiodarone (Cordarone) or lithium
A nurse is educating a new mother about umbilical cord care and how to prevent omphalitis, sepsis, and tetanus.
Which of the following statements by the mother indicates an understanding of the teaching?
Explanation
The correct answer is choice A.Washing hands before and after handling the cord stump can prevent the transmission of bacteria that can cause omphalitis, sepsis, and tetanus.
Choice B is wrong because applying petroleum jelly or ointment to the cord stump can delay its drying and increase the risk of infection.
Choice C is wrong because using hydrogen peroxide to clean the cord stump can damage the healthy tissue and delay healing.
Choice D is wrong because folding down the diaper below the cord stump can expose it to urine and feces, which can contaminate it and cause infection.
The normal range for umbilical cord separation is 5 to 15 days after birth.
A postpartum nurse instructs a new mother in how to bathe her newborn.
Which statement by the mother indicates a need for further instruction?
Explanation
The correct answer is choice B.“I should bathe him before a feeding so he won’t spit up.” This statement indicates a need for further instruction because it is not advisable to bathe a newborn infant before a feeding, as this may cause hypoglycemia or cold stress.The mother should bathe the infant after a feeding or between feedings when the infant is alert and comfortable.
Choice A is wrong because it is correct to use a clean cloth and warm water to wash around the umbilical cord.This helps prevent infection and promotes drying of the cord stump.
Choice C is wrong because it is correct to avoid getting water in the infant’s ears or eyes.This helps prevent ear infections and eye irritation.
Choice D is wrong because it is correct to dry the infant thoroughly and dress him warmly after bathing.
This helps prevent heat loss
The nurse is caring for a newborn who was circumcised using a Gomco clamp 12 hours ago and notes that there is a small amount of blood on his diaper where his penis rests against it.
The most appropriate nursing action would be to:
Explanation
The correct answer is choice C. Document this as a normal finding.According to the American Academy of Family Physicians, bleeding from the dorsal slit after circumcision using a Gomco clamp is usually minimal and will stop once the clamp is in place.
Therefore, a small amount of blood on the diaper 12 hours after the procedure is not a cause for concern and does not require any intervention.
Choice A is wrong because applying gentle pressure to stop bleeding is not necessary and may cause more trauma to the wound.
Choice B is wrong because changing the diaper more frequently may also disturb the healing process and increase the risk of infection.Choice D is wrong because notifying the physician is not indicated unless there is excessive or persistent bleeding, signs of infection, or other complications.
The nurse is teaching parents how to care for their son’s circumcision site after discharge from hospital using petroleum jelly and gauze dressing method.
Which statement by parents indicates that they need further instruction?
Explanation
The correct answer is choice B. Washing the penis with soap and water daily can irritate the circumcision site and delay healing.
The parents should only use warm water to gently clean the area and pat it dry.
They should avoid using soap, alcohol, or peroxide on the wound.
Choice A is wrong because changing the diaper every 3 to 4 hours is recommended to prevent infection and keep the area clean and dry.
Choice C is wrong because applying petroleum jelly on the penis with each diaper change can protect the wound from sticking to the diaper and reduce friction.
Choice D is wrong because calling the doctor if they see any signs of infection, such as redness, swelling, pus, foul odor, or fever, is a correct action.
Exams on Immediate Newborn Care
Custom Exams
Login to Create a Quiz
Click here to loginImmediate Newborn Care
Lessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Login to View Immediate Newborn Care Study Video
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the basic needs of a newborn immediately after birth.
- Identify the steps of immediate care at birth according to WHO guidelines.
- Explain the rationale and procedure for administering erythromycin eye ointment and vitamin K injection to newborns.
- List the signs and symptoms of hypoglycemia in newborns and the appropriate interventions.
- Discuss the importance and schedule of hepatitis B vaccination for newborns.
- Demonstrate proper umbilical cord care and circumcision care for newborns.
Introduction
- Immediate newborn care refers to the essential interventions that are provided to a newborn within the first hour of life.
- These interventions aim to support the newborn’s transition from intrauterine to extrauterine life, prevent complications and infections, and promote bonding and breastfeeding.
- Immediate newborn care is crucial for reducing neonatal mortality and morbidity, especially in low-resource settings.

Newborns’ Basic Needs
- Newborns have four basic needs immediately after birth: warmth, breathing, feeding and protection.
- Warmth: Newborns are prone to heat loss through conduction, convection, evaporation and radiation. To prevent hypothermia, they should be dried thoroughly, placed skin-to-skin with the mother, covered with a dry cloth and a hat, and delayed bathing until 24 hours after birth or until the cord falls off.
- Breathing: Newborns need to establish effective respiration after birth. They should be stimulated by rubbing their back or feet, and suctioned gently if necessary. If they do not breathe or cry within 30 seconds, they should receive positive pressure ventilation with a bag and mask.
- Feeding: Newborns need to receive colostrum, the first breast milk, within the first hour of life. Colostrum is rich in antibodies, nutrients and growth factors that protect the newborn from infections and promote growth and development. Breastfeeding also helps the mother’s uterus contract and reduces postpartum bleeding.
- Protection: Newborns need to be protected from infections and injuries. They should receive routine immunizations, such as hepatitis B vaccine, within 24 hours of birth. They should also receive prophylactic eye ointment (erythromycin) and vitamin K injection within 1 hour of birth. Their umbilical cord should be clamped and cut with sterile instruments, and kept dry and clean until it falls off. If they undergo circumcision, they should receive appropriate pain relief and wound care.
Erythromycin Eye Ointment
- Erythromycin eye ointment is a topical antibiotic that is applied to the lower conjunctival sac of each eye of the newborn within 1 hour of birth.
- The purpose of this intervention is to prevent ophthalmia neonatorum, a serious eye infection caused by gonorrhea or chlamydia that can lead to blindness if untreated.
- The procedure for administering erythromycin eye ointment is as follows:
- Wash your hands and wear gloves.
- Check the medication label for the name, dose, expiry date and route of administration.
- Gently open one eye of the newborn and squeeze about 0.5 cm of ointment into the lower conjunctival sac from the inner to the outer canthus.
- Repeat with the other eye.
- Do not rub or wipe the eyes after applying the ointment.
- Dispose of the used tube in a sharps container and remove your gloves.
- Wash your hands again and document the medication administration.
Vitamin K Injection
- Vitamin K injection is an intramuscular injection that is given to the newborn within 1 hour of birth.
- The purpose of this intervention is to prevent hemorrhagic disease of the newborn (HDN), a rare but potentially fatal bleeding disorder caused by vitamin K deficiency.
- Vitamin K is essential for blood clotting, but it is not produced by the newborn’s immature liver or gut bacteria until several days or weeks after birth. Breast milk also contains low levels of vitamin K compared to formula milk.
- The procedure for administering vitamin K injection is as follows:
- Wash your hands and wear gloves, apron, mask and eye protection.
- Check the medication label for the name, dose, expiry date and route of administration.
- Draw up 0.5 mg (0.5 ml) of vitamin K into a 1 ml syringe with a 25-gauge needle.
- Expel any air bubbles from the syringe and recap the needle.
- Identify an appropriate injection site on the anterolateral aspect of the middle or lower third of the thigh.
- Cleanse the skin with an alcohol swab and let it dry.
- Hold the syringe at a 90-degree angle to the skin and insert the needle quickly and firmly into the muscle.
- Aspirate for blood return. If none, inject the medication slowly over 5 seconds. If blood return is present, withdraw the needle slightly and aspirate again before injecting.
- Withdraw the needle swiftly and apply gentle pressure to the injection site with a dry cotton ball. Do not massage or rub the site.
- Dispose of the used syringe and needle in a sharps container and remove your personal protective equipment (PPE).
- Wash your hands again and document the medication administration.
Hypoglycemia
- Hypoglycemia is a condition where blood glucose levels fall below 40 mg/dl in term newborns or below 30 mg/dl in preterm newborns.
- Hypoglycemia can cause brain damage or death if untreated. It can occur due to various risk factors such as prematurity, intrauterine growth restriction (IUGR), maternal diabetes, perinatal asphyxia or sepsis.
- Signs and symptoms of hypoglycemia in newborns include twitching, irregular respirations, jitteriness, weak or high-pitched cry, cyanosis, lethargy, seizures or eye-rolling.
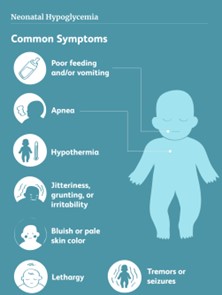
- Interventions for hypoglycemia include monitoring blood glucose levels at least every 4 hours for at-risk newborns or whenever signs are present; ensuring early and frequent feeding with breast milk or formula; providing intravenous glucose infusion if oral feeding is ineffective or contraindicated; maintaining skin-to-skin contact with mother; keeping warm; treating any underlying causes; educating parents on prevention and recognition of hypoglycemia; referring to a pediatrician if needed
Hepatitis B Vaccine
- Hepatitis B vaccine is an intramuscular injection that protects against hepatitis B virus (HBV), which can cause chronic liver disease or cancer in later life.
- HBV can be transmitted from mother to child during pregnancy or delivery, or through contact with infected blood or body fluids.
- The vaccine is given in three doses: the first dose within 24 hours of birth; the second dose at 1 month of age; and the third dose at 6 months of age.
- The procedure for administering hepatitis B vaccine is similar to that of vitamin K injection, except that it uses a different syringe (0.5 ml), needle (23-gauge) and injection site (anterolateral aspect of upper thigh).
Umbilical cord care
- Umbilical cord care refers to keeping the cord stump clean and dry until it falls off naturally within 10 to 14 days after birth.
- Umbilical cord care prevents infection or bleeding from the cord stump or umbilicus. Infection can cause omphalitis (inflammation of umbilical tissues), sepsis (bloodstream infection) or tetanus (a serious bacterial disease).
- Umbilical cord care includes clamping and cutting the cord with sterile instruments within 1 to 3 minutes after birth; applying antiseptic such as chlorhexidine solution or alcohol swab once daily until it falls off; keeping it above diaper level; changing diapers frequently; avoiding tub baths until it falls off; checking for signs of infection such as moistness, redness, purulent drainage or foul odor; seeking medical attention if signs are present.
Circumcision care
- Circumcision care refers to caring for the penis after surgical removal of the foreskin (a fold of skin covering the glans).
- -Circumcision care prevents complications such as bleeding, infection, swelling, adhesions or meatal stenosis (narrowing of the urethral opening).
- -Circumcision care includes applying petroleum jelly with each diaper change for at
- Circumcision care includes applying petroleum jelly with each diaper change for at least 24 hours after circumcision to prevent the diaper from sticking to the penis; avoiding tub baths until the circumcision heals completely; observing for signs of bleeding, infection or delayed healing such as persistent oozing, redness, swelling or pus; seeking medical attention if signs are present.
- Circumcision care also involves providing pain relief to the newborn before, during and after the procedure. Pain relief methods include oral sucrose solution, topical anesthetic cream, dorsal penile nerve block or acetaminophen.
Conclusion
- Immediate newborn care is a vital component of neonatal nursing care that can save lives and improve outcomes for newborns and their mothers.
- Immediate newborn care consists of four basic elements: warmth, breathing, feeding and protection.
- Immediate newborn care also involves administering prophylactic medications (erythromycin eye ointment and vitamin K injection), monitoring for hypoglycemia, immunizing against hepatitis B, caring for the umbilical cord and the circumcision site if applicable.
- Immediate newborn care requires knowledge, skills and competence of the nurse, as well as effective communication and education of the parents.
Summary
- Newborns have four basic needs immediately after birth: warmth, breathing, feeding and protection.
- Warmth is maintained by drying, skin-to-skin contact, covering and delaying bathing.
- Breathing is established by stimulation, suctioning and ventilation if needed.
- Feeding is initiated by breastfeeding within the first hour of life.
- Protection is provided by immunizations (hepatitis B), prophylactic medications (erythromycin eye ointment and vitamin K injection), umbilical cord care and circumcision care if applicable.
- Hypoglycemia is a common complication that can be prevented by early and frequent feeding and monitored by blood glucose levels and signs and symptoms.
- Erythromycin eye ointment prevents ophthalmia neonatorum caused by gonorrhea or chlamydia.
- Vitamin K injection prevents hemorrhagic disease of the newborn caused by vitamin K deficiency.
- Hepatitis B vaccine prevents chronic liver disease or cancer caused by hepatitis B virus.
- Umbilical cord care prevents infection or bleeding from the cord stump or umbilicus.
- Circumcision care prevents complications such as bleeding, infection, swelling, adhesions or meatal stenosis.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Immediate Newborn Care
This filled cannot be empty

