ATI Adult Medical Surgical 2019
Total Questions : 97
Showing 25 questions, Sign in for moreA nurse is caring for a female client who has toxic shock syndrome.
Which of the following findings should the nurse expect?
Explanation

Toxic shock syndrome (TSS) is a life-threatening condition caused by bacterial toxins.
Common symptoms include high fever, low blood pressure, headache, rapid heartbeat, nausea and vomiting, muscle pain, malaise, confusion, and rashes on the soles and palms.
A generalized rash resembling a sunburn is one of the possible signs and symptoms of TSS.
A. Elevated platelet count: TSS does not cause an elevated platelet count.
B. Decreased total bilirubin: TSS does not cause a decrease in total bilirubin levels.
C. Hypertension: TSS causes low blood pressure (hypotension), not high blood pressure (hypertension).
A nurse is providing instructions about foot care for a client who has peripheral arterial disease.
The nurse should identify which of the following statements by the client indicates an understanding of the teaching.
Explanation
“I rest in my recliner with my feet elevated for about an hour every afternoon.” Elevating the feet can help improve blood flow and reduce swelling.
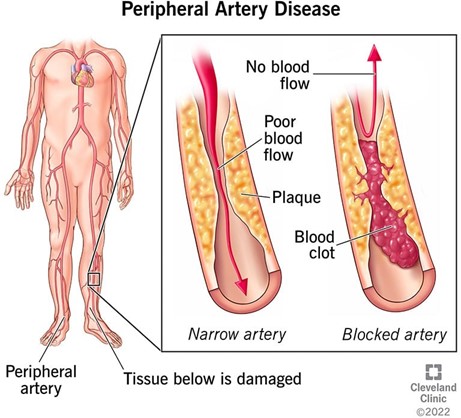
B. “l apply a lubricating lotion to the cracked areas on the soles of my feet every morning.” While moisturizing the feet is important, it is not specific to peripheral arterial disease.
C. “I soak my feet in hot water before trimming my toenails.” Soaking the feet in hot water is not recommended for people with peripheral arterial disease.
D. “I use my heating pad on a low setting to keep my feet warm.” While keeping the feet warm is important, using a heating pad is not recommended as it can cause burns.
A nurse is assessing a client who has a pressure ulcer.
Which of the following findings should the nurse expect as an indication the wound is healing?
Explanation
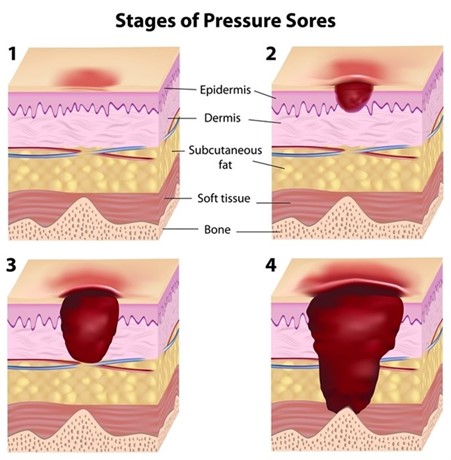
Granulation tissue is new connective tissue and tiny blood vessels that form on the surfaces of a wound during the healing process.
The presence of dark red granulation tissue is a sign that the wound is healing.
B.Light yellow exudate: Light yellow exudate may indicate the presence of infection and is not a sign of healing.
C. Dry brown eschar: Dry brown eschar is dead tissue that needs to be removed for the wound to heal properly.
D.Wound tissue firm to palpation: Wound tissue firm to palpation is not a specific sign of healing.
A nurse is caring for a client in diabetic ketoacidosis (DKA).
Which of the following is the priority intervention by the nurse?
Explanation

The correct answer isChoice D.
Choice A rationale:Checking potassium levels is important in the management of DKA, but it is not the priority intervention.The priority intervention is to restore intravascular volume with fluid resuscitation
Choice B rationale:Bicarbonate infusion is not the priority intervention in the management of DKA.It is used only in severe cases of metabolic acidosis
Choice C rationale:Initiation of a continuous IV insulin infusion is an important intervention in the management of DKA, but it is not the priority intervention.The priority intervention is to restore intravascular volume with fluid resuscitation
Choice D rationale:Administering 0.9% sodium chloride is the priority intervention in the management of DKA.It is used to restore intravascular volume and correct electrolyte imbalances
A nurse is providing discharge teaching to a client following a modified left radical mastectomy with a breast expander.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
“I should expect less than 25 mL of secretions per day in the drainage devices.” After a mastectomy with breast reconstruction using a tissue expander, you may go home with drains in your chest to remove extra fluid.
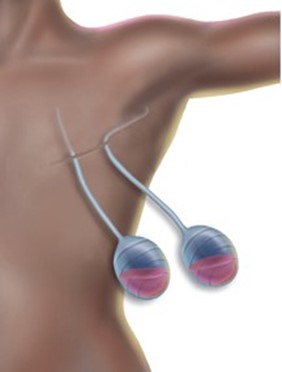
Choice A is wrong because performing strength-building arm exercises using a 15-pound weight is not recommended.
Choice B is wrong because waiting 2 months before additional saline can be added to the breast expander is not accurate.
Choice C is wrong because keeping the left arm flexed at the elbow as much as possible is not recommended.
A nurse is teaching a client about the use of an incentive spirometer.
Which of the following instructions should the nurse include in the teaching?
Explanation

After inhaling deeply using an incentive spirometer, you should hold your breath for 3 to 5 seconds before exhaling.
Choice A is wrong because exhaling slowly through pursed lips is not an instruction for using an incentive spirometer.
Choice C is wrong because placing hands on the upper abdomen during inhalation is not an instruction for using an incentive spirometer.
Choice D is wrong because positioning the mouthpiece.5 cm (1 in) from the mouth is not an instruction for using an incentive spirometer.
A nurse is assessing a client who has a new diagnosis of diverticulitis and reports that he uses multiple complementary and alternative healing therapies.
Which of the following complementary therapies should the nurse identify as contraindicated for the client?
Explanation
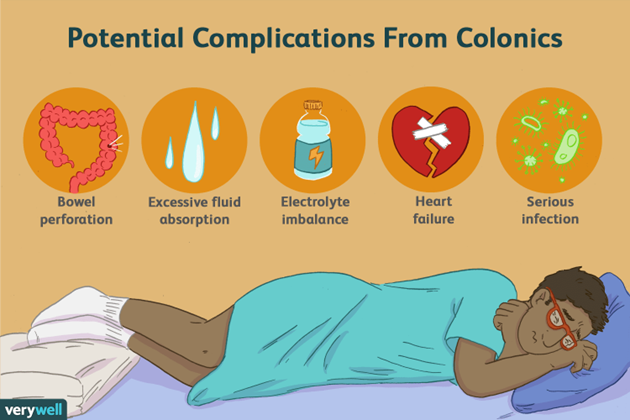
Colonics, also known as colonic irrigation or colon hydrotherapy, involves flushing the colon with fluids to remove waste and is not recommended for individuals with diverticulitis.
Choice A is wrong because acupuncture is not a contraindication for a client with diverticulitis.
Choice B is wrong because saw palmetto is not a contraindication for a client with diverticulitis.
Choice D is wrong because guided imagery is not a contraindication for a client with diverticulitis.
A nurse is providing discharge teaching to a client who has an impaired immune system due to chemotherapy.
Which of the following information should the nurse include in the teaching?
Explanation
The nurse should instruct the client to wash their perineal area two times each day with antimicrobial soap.
This is important because chemotherapy can weaken the immune system, making the client more susceptible to infections.
Choice B is wrong because washing a toothbrush in a dishwasher once a month is not an effective way to prevent infection.
Choice C is wrong because changing a pet’s litter box daily could expose the client to harmful bacteria and should be avoided.
Choice D is wrong because changing the water in a drinking glass every 4 hours is not necessary for preventing infection.
A nurse in a provider's office is caring for a client who has total vision loss and is the handler of a service dog.
Which of the following actions should the nurse take to show consideration for the client and the service animal?
Explanation
The nurse should consult the client before approaching the dog.
Service dogs are working animals and it is important to respect their role and the handler’s wishes.
Choice A is wrong because petting the dog briefly to demonstrate acceptance could distract the dog from its duties.
Choice C is wrong because offering the dog a bowl of water without consulting the client first could interfere with the dog’s training or schedule.
Choice D is wrong because commanding the dog to sit while talking with the client could confuse the dog and disrupt its training.
A nurse is planning care for a client who has upper gastrointestinal bleeding due to a peptic ulcer.
Which of the following actions should the nurse plan to take?
Explanation
The nurse should plan to insert a large-bore nasogastric tube for a client who has upper gastrointestinal bleeding due to a peptic ulcer.

This allows for gastric lavage and can help diagnose the source of bleeding.
Choice A is wrong because a 22-gauge IV line may be too small for rapid fluid resuscitation.
Choice B is wrong because ketorolac is a nonsteroidal anti-inflammatory drug (NSAID) that can increase the risk of gastrointestinal bleeding.
Choice C is wrong because nitroprusside is a vasodilator used to treat hypertensive emergencies and is not typically used for upper gastrointestinal bleeding.
A nurse is planning care for a client who has left-sided hemiplegia following a stroke.
Which of the following actions should the nurse include in the plan of care?
Explanation
The nurse should provide the client with a short-handled teacher.
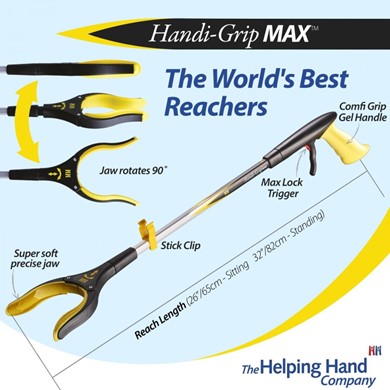
This can help the client to reach and grasp objects without having to overextend or strain their unaffected arm.
Choice B is also correct.
The nurse should place a plate guard on the client’s meal tray.
This can help prevent food from spilling off the plate and make it easier for the client to eat with one hand.
Choice C is wrong because reminding the client to use a cane on his left side while ambulating could be unsafe as the client’s left side is affected by hemiplegia.
Choice D is wrong because positioning the bedside table on the client’s left side could make it difficult for the client to reach items on the table.
A nurse is planning the discharge of a client who had an ischemic stroke.
The nurse should ensure that the client is discharged with which of the following types of pharmacologic therapy?
Explanation
The nurse should ensure that the client is discharged with antithrombotic pharmacologic therapy.
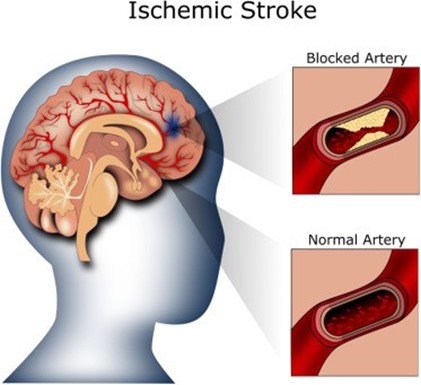
Antithrombotic medications help prevent blood clots from forming and can reduce the risk of another ischemic stroke.
Choice B is wrong because diuretics are used to treat fluid retention and high blood pressure and are not typically used for stroke prevention.
Choice C is wrong because anticonvulsants are used to prevent seizures and are not typically used for stroke prevention.
Choice D is wrong because opioid analgesics are used to treat pain and are not typically used for stroke prevention.
A nurse is caring for a client in the emergency department who experienced a full-thickness burn injury to the lower torso 1 hr ago.
Which of the following findings should the nurse expect?
Explanation

A full-thickness burn injury can result in fluid loss and low blood volume (hypovolemia), which can lead to hypotension.
Choice A, Urinary diuresis, is not the correct answer because it refers to increased production of urine and is not a common symptom of a full-thickness burn injury.
Choice C, Decreased respiratory rate, is not the correct answer because it refers to a decrease in the number of breaths per minute and is not a common symptom of a full-thickness burn injury.
Choice D, Bradycardia, is not the correct answer because it refers to a slow heart rate and is not a common symptom of a full-thickness burn injury.
A nurse is completing discharge teaching with a client who has a peripherally inserted central catheter (PICC) line in the left arm.
Which of the following instructions should the nurse include in the teaching?
Explanation
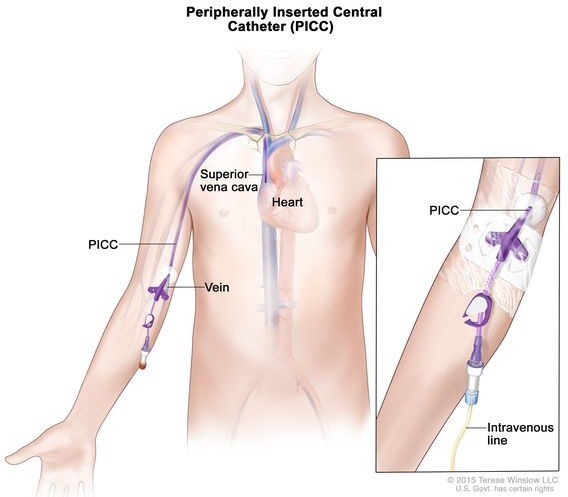
A 10-mL syringe is the minimum size that should be used to flush a PICC line to prevent damage to the catheter.
Choice A, Clean the insertion site using 20 mL of hydrogen peroxide, is not the correct answer because hydrogen peroxide should not be used to clean the insertion site of a PICC line.
Choice B, Changing the catheter dressing daily, is not the correct answer because the catheter dressing should be changed every 3 to 7 days or as directed by a healthcare provider.
Choice D, Do not elevate the arm above the level of the heart, is not the correct answer because there is no restriction on elevating the arm above the level of the heart with a PICC line.
A nurse is monitoring a client's heart rhythm following the insertion of a permanent pacemaker.
Which of the following images should the nurse expect?
Explanation
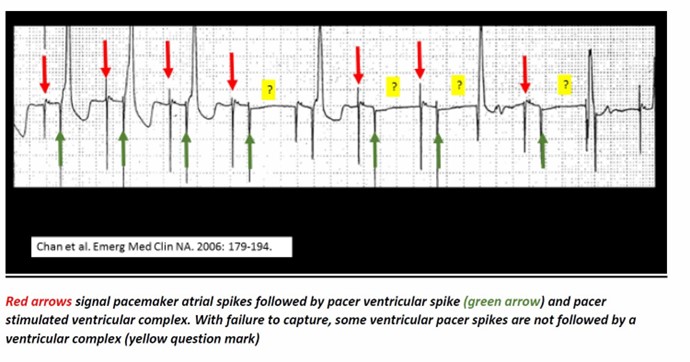
A pacemaker sends electrical signals to the heart to regulate the heartbeat.
On an electrocardiogram (ECG), these signals appear as small spikes followed by a QRS complex, which represents the contraction of the ventricles.
Choice A, A regular sinus rhythm, is not the correct answer because a regular sinus rhythm is a normal heart rhythm that originates from the sinoatrial (SA) node and does not involve a pacemaker.
Choice B, A chaotic, irregular rhythm, is not the correct answer because a pacemaker is designed to regulate the heartbeat and prevent chaotic or irregular rhythms.
Choice C, the Absence of any electrical activity, is not the correct answer because a pacemaker sends electrical signals to the heart to regulate its activity.
A nurse is teaching a client who has endometriosis about the adverse effects of leuprolide.
Which of the following manifestations should the nurse include in the teaching?
Explanation
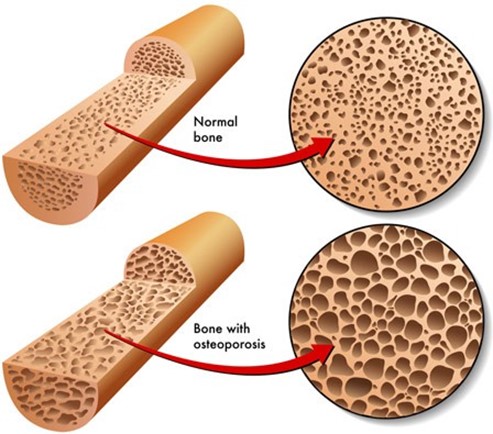
Leuprolide can cause bone loss, which can lead to osteoporosis and an increased risk of bone fractures.
Choice A, Pallor, is not the correct answer because pallor (pale skin) is not a common side effect of leuprolide.
Choice B, Increased appetite, is not the correct answer because increased appetite is not a common side effect of leuprolide.
Choice D, Hypoglycemia, is not the correct answer because hypoglycemia (low blood sugar) is not a common side effect of leuprolide.
A nurse is monitoring a client who is receiving 2 units of packed RBCs.
Which of the following manifestations indicates a hemolytic transfusion reaction?
Explanation
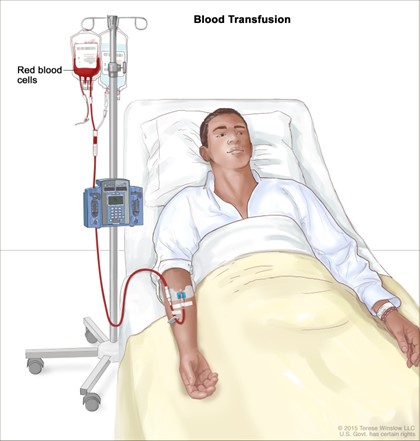
A hemolytic transfusion reaction is a serious complication that can occur after a blood transfusion.
The reaction occurs when the red blood cells that were given during the transfusion are destroyed by the person’s immune system.
Early acute hemolytic transfusion reactions are typically characterized by fever, which may be accompanied by rigors (chills).
Choice A: Mild cases are also typically characterized by abdominal, back, flank, or chest pain.
Choice B: Bradycardia is not an answer because it is not mentioned as a symptom of hemolytic transfusion reaction in my sources.
Choice C: Hypertension is not an answer because it is not mentioned as a symptom of hemolytic transfusion reaction in my sources.
A nurse finds a client in bed, unresponsive and breathing.
Which of the following actions should the nurse take first?
Explanation
The first step when finding an unresponsive person is to check their breathing by tilting their head back and looking and feeling for breaths.
When a person is unresponsive, their muscles relax and their tongue can block their airway so they can no longer breathe.
Tilting their head back opens the airway by pulling the tongue forward.
Palpating for the client’s carotid pulse is a way to check if the client has a pulse and is still breathing.
Choice A: Initiating cardiac monitoring for the client is not an answer because it is not mentioned as the first action to take in my sources.
Choice B: Apply a blood pressure cuff is not an answer because it is not mentioned as the first action to take in my sources.
Choice D: Establishing an IV access is not an answer because it is not mentioned as the first action to take in my sources.
A nurse in a provider's office is teaching a client about the self-management of GERD.
Which of the following instructions should the nurse include?
Explanation

One of the lifestyle changes that doctors recommend for managing symptoms of gastroesophageal reflux disease (GERD) is elevating the head during sleep by placing a foam wedge or extra pillows under the head and upper back to incline the body and raising the head off the bed 6 to 8 inches.
Choice A: “Increase your caloric intake by 250 calories per day” is not an answer because it is not mentioned as a self-management strategy for GERD in my sources.
Choice B: “Lie down for 30 minutes after each meal” is not an answer because it is not mentioned as a self-management strategy for GERD in my sources.
Choice C: “Eat a light meal 1 hour before bedtime” is not an answer because it is not mentioned
A nurse in an emergency department is reviewing a client's ECG reading.
Which of the following findings should the nurse identify as an indication that the client has first-degree heart block?
Explanation
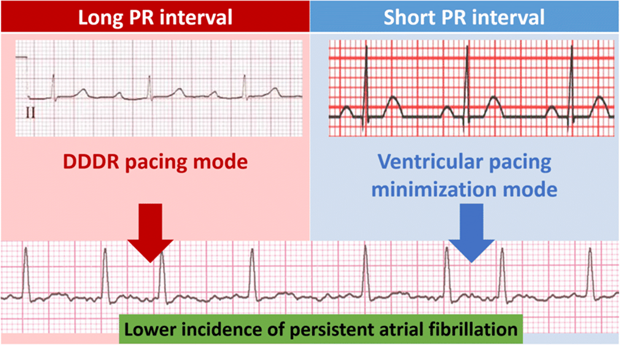
First-degree heart block is a type of atrioventricular (AV) block that involves the consistent prolongation of the PR interval (defined as >0.20 seconds) due to delayed conduction via the atrioventricular node.
This is seen on an ECG as a PR interval greater than 200 ms in length.
Choice B: Nondiscernible P waves are not an answer because it is not mentioned as a characteristic of first-degree heart block in my sources.
Choice C: More P waves than QRS complexes is not an answer because it is not mentioned as a characteristic of first-degree heart block in my sources.
Choice D: No correlation between P and QRS waves is not an answer because it is not mentioned as a characteristic of first-degree heart block in my sources.
A nurse is assessing a client who has heart failure.
Which of the following client statements should indicate to the nurse that the client needs a referral for cardiac rehabilitation?
Explanation
“I’m too tired to brush my teeth.” This statement indicates that the client is experiencing fatigue, which is a common symptom of heart failure.
Fatigue can significantly impact a person’s ability to perform daily activities and can be an indication that the client needs a referral for cardiac rehabilitation 1.
Choice A is not the correct answer because weighing oneself daily is a recommended self-monitoring technique for clients with heart failure.
Choice B is not the correct answer because while feeling unhappy can be a symptom of heart failure, it does not necessarily indicate a need for cardiac rehabilitation.
Choice D is not the correct answer because eating a low-sodium diet is a recommended dietary change for clients with heart failure.
A nurse is caring for a client who has cancer.
The client tells the nurse, "I would prefer to try vitamins and minerals instead of chemotherapy." Which of the following responses should the nurse make?
Explanation
“You should ask your provider about your plan.” The client has expressed a preference for trying vitamins and minerals instead of chemotherapy.
The nurse should encourage the client to discuss their treatment plan with their provider to ensure that they receive the most appropriate care.
Choice B is not the correct answer because while it is important for the client to be informed about their treatment options, the nurse’s primary responsibility is to encourage the client to discuss their concerns with their provider.
Choice C is not the correct answer because it is not within the nurse’s scope of practice to make definitive statements about the effectiveness of holistic treatments.
Choice D is not the correct answer because it is not within the nurse’s scope of practice to make definitive statements about the best way to treat cancer.
A nurse is caring for a client who has bounding pulses, crackles on auscultation, and pink frothy secretions when receiving suctioning.
The nurse should recognize these assessment findings as indicating which of the following?
Explanation
“Fluid volume excess.” Bounding pulses, crackles on auscultation, and pink frothy secretions when receiving suctioning are all signs of fluid volume excess.
Fluid volume excess can occur when the heart is unable to pump blood efficiently, causing fluid to build up in the lungs.
Choice A is not the correct answer because the increased cardiac output would not cause these symptoms.
Choice B is not the correct answer because pleural effusion refers to a buildup of fluid between the layers of tissue that line the lungs and chest cavity, which would not cause these symptoms.
Choice D is not the correct answer because aspiration refers to the inhalation of food, liquid, or other substances into the lungs, which would not cause these symptoms.
A nurse is caring for a client who has just returned from surgery with an external fixator to the left tibia.
Which of the following assessment findings requires immediate intervention by the nurse?
Explanation
“The client’s capillary refill in the left toe is 6 seconds.” Capillary refill time is the time it takes for blood to return to the capillaries after pressure has been applied to the skin.

A normal capillary refill time is less than 2 seconds.
A capillary refill time of 6 seconds indicates poor blood flow to the left toe and requires immediate intervention by the nurse.
Choice B is not the correct answer because while a pain level of 7 on a scale from 0 to 10 at the operative site is concerning, it does not require immediate intervention by the nurse.
Choice C is not the correct answer because an oral temperature of 38.3° C (100.9° F) is only slightly elevated and does not require immediate intervention by the nurse.
Choice D is not the correct answer because while 100 mL of blood in a closed-suction drain may be concerning, it does not necessarily require immediate intervention by the nurse.
A nurse is caring for a client who is receiving continuous bladder irrigation following a transurethral resection of the prostate.
The client reports bladder spasms and the nurse observes decreased urinary output.
Which of the following actions should the nurse take?
Explanation
“Flush the catheter manually with 0.9% sodium chloride.” The client is receiving continuous bladder irrigation following a transurethral resection of the prostate and reports bladder spasms and decreased urinary output.
These symptoms may indicate that the catheter is blocked with blood clots.
Flushing the catheter manually with 0.9% sodium chloride can help to remove any blood clots and restore urinary output.
Choice A is not the correct answer because removing the indwelling urinary catheter would not address the underlying issue of blood clots blocking the catheter.
Choice B is not the correct answer because decreasing traction on the catheter would not address the underlying issue of blood clots blocking the catheter.
Choice C is not the correct answer because while ibuprofen may provide some pain relief, it would not address the underlying issue of blood clots blocking the catheter.
Sign Up or Login to view all the 97 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

