Please set your exam date
Care of Patients with Chronic Illnesses
Study Questions
Introduction to Care of Patients with Chronic Illnesses
A nurse is assessing a client with chronic obstructive pulmonary disease (COPD). Which finding would indicate a potential complication of the disease?
Explanation
Cyanosis of the lips and nail beds is a sign of hypoxemia, which indicates inadequate oxygenation of the blood. This is a potential complication of COPD, as the disease causes airflow obstruction and impaired gas exchange. Cyanosis requires immediate intervention to improve oxygen delivery and prevent tissue damage.
Incorrect options:
A) Barrel-shaped chest - This is a common finding in clients with COPD, as the disease causes hyperinflation of the lungs and increased anteroposterior diameter of the chest. It is not a sign of a complication, but rather a chronic adaptation to the disease.
B) Clubbing of the fingers - This is a possible finding in clients with COPD, as the disease causes chronic hypoxia and stimulation of vascular endothelial growth factor, leading to thickening and widening of the distal phalanges. It is not a sign of a complication, but rather a long-term effect of the disease.
D) Wheezes on auscultation - This is an expected finding in clients with COPD, as the disease causes narrowing of the airways and increased airway resistance. It is not a sign of a complication, but rather a characteristic manifestation of the disease.
A client with rheumatoid arthritis (RA) is prescribed methotrexate, a disease-modifying antirheumatic drug (DMARD). What should the nurse include in the teaching plan for this client?
Explanation
The client should be advised to avoid drinking alcohol while taking methotrexate, as this can increase the risk of hepatotoxicity and liver damage. Methotrexate is metabolized by the liver and can cause elevated liver enzymes and inflammation. The client should also have regular liver function tests while taking this medication.
Incorrect options:
A) "You should take this medication with food or milk to prevent stomach upset." - This is not a correct statement, as methotrexate should be taken on an empty stomach, at least one hour before or two hours after meals, to enhance absorption and effectiveness.
C) "You should monitor your blood pressure regularly while taking this medication." - This is not a relevant statement, as methotrexate does not affect blood pressure. However, the client should monitor their blood counts regularly while taking this medication, as methotrexate can cause bone marrow suppression and anemia.
D) "You should take this medication every day for optimal results." - This is not a correct statement, as methotrexate is usually taken once a week for RA. Taking it more frequently can increase the risk of adverse effects and toxicity.
A nurse is caring for a client with diabetes mellitus who has peripheral neuropathy. Which intervention would be most appropriate for this client?
Explanation
The client with peripheral neuropathy should inspect their feet daily for any injuries or infections, as they may have reduced sensation and pain perception in their lower extremities. This can lead to delayed detection and treatment of wounds, ulcers, or infections, which can result in serious complications such as gangrene and amputation.
Incorrect options:
A) Applying heating pads to the affected areas - This is not an appropriate intervention, as heating pads can cause burns or skin damage in clients with peripheral neuropathy, who may not feel the heat or pain. The client should avoid exposing their feet to extreme temperatures and use warm water instead of hot water for bathing.
B) Massaging the affected areas with lotion - This is not an appropriate intervention, as massaging can cause friction or injury to the affected areas, especially if there are any open wounds or ulcers. The client should apply moisturizer to their feet after bathing, but avoid applying it between the toes, where fungal infections can occur.
D) Wearing tight-fitting socks and shoes - This is not an appropriate intervention, as tight-fitting socks and shoes can impair circulation and cause pressure ulcers or blisters in the affected areas. The client should wear well-fitting, comfortable, and protective footwear, and change their socks daily.
A client with multiple sclerosis (MS) is experiencing fatigue and muscle weakness. Which strategy would be most helpful for the client to conserve energy and prevent exacerbation of symptoms?
Explanation
The client with MS should plan activities that require more energy for the morning, when they are likely to have more strength and endurance. Fatigue and muscle weakness tend to worsen as the day progresses, especially in warm or humid weather. The client should also prioritize and pace their activities, and take rest breaks as needed.
Incorrect options:
A) Performing exercises that target the affected muscles - This is not a helpful strategy, as overexertion of the affected muscles can aggravate fatigue and weakness. The client should perform exercises that are moderate, low-impact, and well-tolerated, such as stretching, yoga, or swimming.
C) Taking frequent naps throughout the day - This is not a helpful strategy, as frequent naps can disrupt the sleep cycle and interfere with nighttime sleep quality. The client should aim for seven to eight hours of uninterrupted sleep at night, and limit naps to 20 to 30 minutes in the afternoon if needed.
D) Increasing fluid and caffeine intake - This is not a helpful strategy, as excessive fluid intake can cause bladder problems, such as urgency, frequency, or incontinence, which are common in clients with MS. Caffeine intake can also worsen these symptoms, as well as cause dehydration, insomnia, or anxiety.
Understanding Chronic Illnesses
A nurse is caring for a client with chronic obstructive pulmonary disease (COPD). Which intervention is most appropriate to promote oxygenation in this client?
Explanation
Pursed-lip breathing is a technique that helps to slow down the breathing rate, reduce air trapping, and improve gas exchange in clients with COPD. It also helps to relieve dyspnea and anxiety.
Incorrect options:
B) Administer oxygen via nasal cannula at 6 L/min. - This is an incorrect intervention, as clients with COPD are at risk of developing oxygen-induced hypercapnia, a condition where high levels of oxygen reduce the drive to breathe and cause carbon dioxide retention. Oxygen therapy should be administered cautiously and titrated to maintain a target oxygen saturation of 88-92% in clients with COPD.
C) Position the client in a supine position with the head elevated. - This is an incorrect intervention, as a supine position can increase the pressure on the diaphragm and impair lung expansion, worsening dyspnea and hypoxemia in clients with COPD. A semi-Fowler's or high-Fowler's position is preferred, as it allows for maximal lung expansion and reduces the work of breathing.
D) Instruct the client to cough forcefully every hour. - This is an incorrect intervention, as forceful coughing can increase airway resistance, cause bronchospasm, and increase dyspnea in clients with COPD. A more effective coughing technique is to use huff coughing, which involves exhaling forcefully through an open mouth while making a "huff" sound.
A client with type 2 diabetes mellitus is prescribed metformin, a biguanide antidiabetic agent. The nurse should instruct the client to monitor for which adverse effect of this medication?
Explanation
Lactic acidosis is a rare but potentially fatal complication of metformin therapy, especially in clients with renal impairment, liver disease, heart failure, or alcohol abuse. It occurs when metformin accumulates in the body and causes an increase in lactate production and a decrease in lactate clearance, leading to metabolic acidosis. Symptoms of lactic acidosis include nausea, vomiting, abdominal pain, hyperventilation, muscle weakness, and confusion.
Incorrect options:
A) Hypoglycemia - This is an incorrect option, as metformin does not cause hypoglycemia by itself. However, hypoglycemia may occur if metformin is combined with other antidiabetic agents that lower blood glucose levels, such as sulfonylureas or insulin.
C) Pancreatitis - This is an incorrect option, as metformin does not cause pancreatitis. However, pancreatitis may occur as a complication of diabetes mellitus or as an adverse effect of other antidiabetic agents, such as glucagon-like peptide-1 (GLP-1) agonists or dipeptidyl peptidase-4 (DPP-4) inhibitors.
D) Hepatotoxicity - This is an incorrect option, as metformin does not cause hepatotoxicity. However, hepatotoxicity may occur as a complication of diabetes mellitus or as an adverse effect of other antidiabetic agents, such as thiazolidinediones or alpha-glucosidase inhibitors.
A client with rheumatoid arthritis (RA) is scheduled for a joint replacement surgery. The nurse should teach the client to discontinue which medication before the surgery to prevent bleeding complications?
Explanation
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that is commonly used to treat pain and inflammation in clients with RA. However, NSAIDs can also inhibit platelet aggregation and prolong bleeding time, increasing the risk of hemorrhage during and after surgery. Therefore, ibuprofen should be discontinued at least 7 days before the surgery.
Incorrect options:
A) Prednisone - This is an incorrect option, as prednisone is a corticosteroid that is used to suppress inflammation and immune responses in clients with RA. Prednisone does not affect bleeding time or platelet function. However, prednisone can increase the risk of infection and delay wound healing, so it should be tapered gradually before the surgery to avoid adrenal insufficiency and withdrawal symptoms.
B) Methotrexate - This is an incorrect option, as methotrexate is a disease-modifying antirheumatic drug (DMARD) that is used to slow down the progression of joint damage and reduce inflammation in clients with RA. Methotrexate does not affect bleeding time or platelet function. However, methotrexate can increase the risk of infection and bone marrow suppression, so it should be discontinued at least 2 weeks before the surgery.
D) Hydroxychloroquine - This is an incorrect option, as hydroxychloroquine is an antimalarial drug that is used to treat mild to moderate RA. Hydroxychloroquine does not affect bleeding time or platelet function. However, hydroxychloroquine can cause ocular toxicity, so it should be monitored regularly by an ophthalmologist.
A client with chronic kidney disease (CKD) is receiving hemodialysis three times a week. The nurse should assess the client for which potential complication of hemodialysis?
Explanation
Disequilibrium syndrome is a neurological complication of hemodialysis that occurs when the rate of solute removal from the blood exceeds the rate of solute removal from the brain, creating an osmotic gradient that causes fluid to shift into the brain cells, resulting in cerebral edema. Symptoms of disequilibrium syndrome include headache, nausea, vomiting, restlessness, confusion, and seizures. It usually occurs during or shortly after the first few dialysis sessions or when there is a large decrease in blood urea nitrogen (BUN) levels.
Incorrect options:
A) Hyperkalemia - This is an incorrect option, as hyperkalemia is a common complication of CKD that occurs when the kidneys are unable to excrete excess potassium. Hemodialysis helps to lower potassium levels by removing it from the blood. However, hyperkalemia may occur between dialysis sessions if the client consumes foods high in potassium or takes medications that increase potassium levels, such as angiotensin-converting enzyme (ACE) inhibitors or potassium-sparing diuretics.
B) Hypertension - This is an incorrect option, as hypertension is a common complication of CKD that occurs when the kidneys are unable to regulate fluid and sodium balance. Hemodialysis helps to lower blood pressure by removing excess fluid and sodium from the blood. However, hypertension may occur between dialysis sessions if the client consumes foods high in sodium or fluid or takes medications that increase blood pressure, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids.
C) Hypocalcemia - This is an incorrect option, as hypocalcemia is a common complication of CKD that occurs when the kidneys are unable to activate vitamin D and promote calcium absorption from the gut. Hemodialysis helps to correct hypocalcemia by adding calcium to the dialysate solution. However, hypocalcemia may occur between dialysis sessions if the client consumes foods low in calcium or takes medications that lower calcium levels, such as phosphate binders or bisphosphonates.
Assessment and Diagnosis of Chronic Illnesses
A nurse is assessing a client who has chronic obstructive pulmonary disease (COPD). Which of the following findings should the nurse report to the provider?
Explanation
Purulent sputum production indicates a possible infection, which can exacerbate COPD and lead to respiratory failure. The nurse should report this finding to the provider and obtain a sputum culture for further evaluation.
Incorrect options:
A) Barrel-shaped chest - This is a common finding in clients with COPD, due to chronic hyperinflation of the lungs. It does not require immediate intervention.
B) Clubbing of the fingers - This is a sign of chronic hypoxia, which is often seen in clients with COPD. It does not indicate an acute complication.
C) Increased respiratory rate - This is a compensatory mechanism for clients with COPD, who have impaired gas exchange and reduced lung capacity. It does not necessarily indicate a worsening of the condition.
A client with diabetes mellitus is scheduled for a hemoglobin A1c test. The client asks the nurse what this test measures. How should the nurse respond?
Explanation
Hemoglobin A1c (HbA1c) is a test that reflects the percentage of hemoglobin that is glycosylated, or attached to glucose molecules, in the red blood cells. It provides an estimate of the average blood glucose level over the past 3 months, as red blood cells have a lifespan of about 120 days. The higher the HbA1c level, the poorer the glycemic control.
Incorrect options:
B) "It measures your blood glucose level at the time of the test." - This is not correct, as HbA1c does not reflect the current blood glucose level, but rather the average over a period of time. A fasting blood glucose test or a random blood glucose test would measure the blood glucose level at the time of the test.
C) "It measures your ability to produce insulin in response to glucose." - This is not correct, as HbA1c does not measure insulin production or secretion. A C-peptide test or an oral glucose tolerance test would measure insulin function.
D) "It measures your risk of developing diabetic complications." - This is not correct, as HbA1c does not directly measure the risk of diabetic complications, but rather indicates the degree of glycemic control, which affects the risk of complications. Other factors, such as blood pressure, cholesterol levels, and kidney function, also influence the risk of diabetic complications.
A nurse is caring for a client who has rheumatoid arthritis (RA). The client reports increased joint pain and stiffness in the morning. Which of the following interventions should the nurse suggest to the client?
Explanation
Performing gentle range-of-motion exercises after waking up can help reduce joint stiffness and improve mobility for clients with RA. The exercises should be done slowly and carefully, without forcing or overextending the joints.
Incorrect options:
A) Apply cold packs to the affected joints before getting out of bed. - This is not correct, as cold packs are more effective for acute inflammation and swelling, which are not typical features of RA. Cold packs can also increase joint stiffness and discomfort.
C) Take nonsteroidal anti-inflammatory drugs (NSAIDs) before bedtime. - This is not correct, as NSAIDs are more effective when taken regularly throughout the day, rather than only at night. NSAIDs can also cause gastrointestinal irritation and bleeding, especially when taken on an empty stomach or before lying down.
D) Avoid weight-bearing activities until noon. - This is not correct, as avoiding weight-bearing activities can lead to muscle weakness and joint deformity in clients with RA. Weight-bearing activities should be done in moderation and with proper support and alignment.
A client with hypertension is prescribed a thiazide diuretic. The nurse instructs the client to monitor their potassium level and report any signs of hypokalemia. Which of the following signs should the nurse include in the teaching?
Explanation
Muscle cramps are a sign of hypokalemia, or low potassium level, which can occur as a side effect of thiazide diuretics. Potassium is an electrolyte that is essential for muscle contraction and nerve conduction. Hypokalemia can cause muscle weakness, spasms, and cramps, as well as cardiac arrhythmias and dysrhythmias.
Incorrect options:
B) Constipation - This is not a sign of hypokalemia, but rather a sign of hypercalcemia, or high calcium level, which can also occur as a side effect of thiazide diuretics. Calcium is an electrolyte that is involved in muscle contraction and blood clotting. Hypercalcemia can cause constipation, abdominal pain, kidney stones, and bone pain.
C) Dry mouth - This is not a sign of hypokalemia, but rather a sign of dehydration, which can occur as a result of fluid loss from diuretic therapy. Dehydration can cause dry mouth, thirst, decreased urine output, and increased heart rate and blood pressure.
D) Nausea - This is not a sign of hypokalemia, but rather a sign of hyponatremia, or low sodium level, which can also occur as a side effect of thiazide diuretics. Sodium is an electrolyte that is important for fluid balance and nerve function. Hyponatremia can cause nausea, vomiting, headache, confusion, and seizures.
Collaborative Care and Management of Chronic Illnesses
A nurse is caring for a client with chronic obstructive pulmonary disease (COPD) who is experiencing dyspnea and anxiety. Which intervention should the nurse implement first?
Explanation
The nurse should follow the ABC (airway, breathing, circulation) priority framework when caring for a client with respiratory distress. The first intervention should be to assess the client's vital signs and oxygen saturation to determine the severity of the condition and the need for further interventions.
Incorrect options:
A) Administer oxygen therapy as prescribed. - This is an important intervention, but not the first one. The nurse should assess the client's oxygen saturation before administering oxygen therapy, as too much or too little oxygen can be harmful for a client with COPD.
B) Teach the client pursed-lip breathing technique. - This is a helpful intervention, but not the first one. The nurse should assess the client's respiratory status before teaching any breathing techniques, as some clients may not be able to perform them due to severe dyspnea or anxiety.
D) Provide reassurance and a calm environment for the client. - This is a supportive intervention, but not the first one. The nurse should address the client's physical needs before providing emotional support, as anxiety can be exacerbated by dyspnea and hypoxia.
A client with type 2 diabetes mellitus is scheduled for a colonoscopy. The client asks the nurse how to manage their blood glucose levels on the day of the procedure. What is the best response by the nurse?
Explanation
The client with type 2 diabetes mellitus who is undergoing a colonoscopy may need to adjust their oral antidiabetic medication dose, as they will be fasting before and after the procedure and may receive sedatives or analgesics that can affect their blood glucose levels. The best response by the nurse is to advise the client to contact their health care provider for specific instructions on how to adjust their medication dose, as this may vary depending on the type and dosage of medication, the duration of fasting, and the client's blood glucose levels.
Incorrect options:
A) "You should take your usual dose of oral antidiabetic medication in the morning before the procedure." - This is an incorrect response, as taking the usual dose of oral antidiabetic medication without eating can cause hypoglycemia, which can be dangerous for the client.
B) "You should check your blood glucose levels frequently and drink clear liquids with sugar if they are low." - This is an incorrect response, as drinking clear liquids with sugar can interfere with the bowel preparation and affect the quality of the colonoscopy. The client should follow the instructions for bowel preparation and avoid any liquids that are not clear or contain red or purple dye.
C) "You should skip your oral antidiabetic medication on the day of the procedure and resume it after you eat." - This is an incorrect response, as skipping oral antidiabetic medication can cause hyperglycemia, which can increase the risk of complications during and after the procedure.
A nurse is conducting a home visit for a client with rheumatoid arthritis (RA). The nurse observes that the client has difficulty opening jars and bottles due to joint stiffness and pain. Which assistive device should the nurse recommend to the client?
Explanation
A jar opener is an assistive device that can help a client with RA open jars and bottles more easily by providing leverage and reducing strain on the joints. A jar opener can improve the client's independence and quality of life by facilitating activities of daily living.
Incorrect options:
B) A reacher - This is an assistive device that can help a client with RA reach objects that are high or low without bending or stretching. However, it does not address the specific problem of opening jars and bottles.
C) A walker - This is an assistive device that can help a client with RA maintain balance and stability while walking. However, it does not address the specific problem of opening jars and bottles.
D) A cane - This is an assistive device that can help a client with RA reduce pressure and pain on the affected joints while walking. However, it does not address the specific problem of opening jars and bottles.
A client with chronic kidney disease (CKD) is receiving hemodialysis three times a week. The client reports feeling depressed and hopeless about their condition. Which statement by the nurse demonstrates empathy and compassion?
Explanation
The nurse should demonstrate empathy and compassion when caring for a client with CKD who is feeling depressed and hopeless. Empathy is the ability to understand and share the feelings of another person, while compassion is the willingness to help alleviate their suffering. The nurse should acknowledge the client's feelings, validate their emotions, and offer support and encouragement.
Incorrect options:
A) "You should be grateful that you have access to dialysis. Many people with CKD don't have that option." - This statement does not demonstrate empathy or compassion, but rather minimizes the client's feelings and implies that they are ungrateful or selfish.
B) "You have a chronic condition that requires lifelong treatment. You need to accept that and move on." - This statement does not demonstrate empathy or compassion, but rather dismisses the client's feelings and implies that they are weak or irrational.
C) "You are not alone in this situation. There are many people who have CKD and cope well with dialysis." - This statement does not demonstrate empathy or compassion, but rather compares the client to others and implies that they are abnormal or inadequate.
Psychosocial Considerations in Chronic Illness Care
A nurse is assessing a client who has been diagnosed with rheumatoid arthritis. Which of the following findings is most indicative of psychosocial distress related to the chronic illness?
Explanation
Frustration and anger are common emotional responses to chronic illness, especially when the disease affects the client's ability to perform daily activities, maintain social relationships, and cope with uncertainty. These emotions can interfere with the client's adherence to treatment, self-care, and quality of life. The nurse should acknowledge the client's feelings, provide emotional support, and refer the client to appropriate resources, such as counseling, support groups, or stress management techniques.
Incorrect options:
A) The client reports difficulty sleeping due to joint pain and stiffness. - This is a physical finding, not a psychosocial one. However, poor sleep quality can affect the client's mood, energy, and immune function, so the nurse should address this issue and suggest strategies to improve sleep hygiene and comfort.
C) The client has a history of depression and anxiety prior to the diagnosis. - This is a risk factor for developing psychosocial distress related to chronic illness, but it is not a finding in itself. The nurse should assess the client for signs and symptoms of depression and anxiety, such as low mood, hopelessness, excessive worry, nervousness, or changes in appetite or weight. The nurse should also monitor the client for suicidal ideation or behavior and provide appropriate interventions as needed.
D) The client requests information about the prognosis and treatment options for the disease. - This is a positive finding, as it indicates that the client is interested in learning more about the disease and participating in decision-making. The nurse should provide accurate and honest information, clarify any misconceptions, and address any concerns or questions that the client may have.
A client with multiple sclerosis is admitted to the hospital for an exacerbation of symptoms. The client tells the nurse that they feel hopeless and worthless because they cannot work or take care of their family anymore. How should the nurse respond?
Explanation
The client is experiencing low self-esteem and negative self-image due to the loss of roles and functions caused by chronic illness. The nurse should use positive reinforcement and affirmations to help the client recognize their worth and value as a person, regardless of their disease status or limitations. The nurse should also encourage the client to identify their strengths and abilities, such as hobbies, interests, skills, or talents, that they can still enjoy or develop.
Incorrect options:
B) "You are not hopeless. There are many treatments available that can help you manage your symptoms." - This response is dismissive of the client's feelings and may sound unrealistic or insensitive. While providing information about treatments is important, it should not be done without acknowledging and validating the client's emotions first.
C) "You are not alone. There are many people who care about you and want to help you." - This response is supportive but does not address the core issue of low self-esteem and negative self-image. The nurse should also help the client explore their own sense of identity and worth beyond their relationships with others.
D) "You are not helpless. There are many things that you can do to improve your condition and well-being." - This response is empowering but may sound patronizing or demanding if the client is feeling overwhelmed or discouraged by their situation. The nurse should also respect the client's pace and readiness to make changes or take action.
A nurse is caring for a client who has end-stage renal disease (ESRD) and requires hemodialysis three times a week. The client tells the nurse that they are tired of living this way and wish they could just die. What is the best initial action by the nurse?
Explanation
The client is expressing suicidal ideation, which is a medical emergency that requires immediate assessment and intervention. The nurse should first ask the client if they have a plan to harm themselves or others, as this indicates the level of risk and urgency. The nurse should also assess the client for other signs and symptoms of suicidal behavior, such as giving away possessions, saying goodbye, withdrawing from others, or having a history of previous attempts. The nurse should ensure the client's safety, provide emotional support, and notify the health care provider and the mental health team as soon as possible.
Incorrect options:
B) Explore the reasons behind the client's wish to die. - This is an important step in understanding the client's perspective and addressing their underlying issues, such as depression, hopelessness, grief, or loss of control. However, it should not be done before ensuring the client's safety and assessing their risk of suicide.
C) Inform the health care provider about the client's statement. - This is a necessary action, but not the best initial one. The nurse should first assess the client's risk of suicide and ensure their safety before contacting the health care provider and the mental health team.
D) Educate the client about the benefits of hemodialysis and the risks of discontinuing it. - This is an inappropriate action, as it ignores the client's feelings and may sound judgmental or coercive. The nurse should not try to persuade or convince the client to change their mind without first acknowledging and validating their emotions and exploring their reasons for wanting to die.
A client with chronic obstructive pulmonary disease (COPD) is admitted to the hospital for an acute exacerbation. The client has a history of smoking for 40 years and has tried to quit several times without success. The client tells the nurse that they are ashamed of themselves and feel guilty for causing their own illness. How should the nurse respond?
Explanation
The client is experiencing self-blame and guilt for contributing to their chronic illness through smoking. The nurse should use motivational interviewing techniques to help the client overcome their ambivalence and resistance to quitting smoking. The nurse should express empathy, avoid confrontation or criticism, elicit the client's own reasons for quitting, highlight the discrepancies between the client's goals and behaviors, and support the client's self-efficacy and autonomy. The nurse should also provide information about the benefits of quitting smoking, such as reducing symptoms, preventing complications, improving lung function, increasing life expectancy, saving money, and enhancing well-being.
Incorrect options:
A) "You should not feel ashamed or guilty. Smoking is an addiction that is hard to overcome." - This response is empathetic but may sound dismissive or minimizing of the client's feelings. The nurse should acknowledge and validate the client's emotions before providing reassurance or information.
B) "You should feel ashamed and guilty. Smoking is a harmful habit that you could have avoided." - This response is judgmental and blaming, which can damage the therapeutic relationship and increase the client's defensiveness or resistance to quitting smoking. The nurse should avoid using words such as "should" or "must" that imply obligation or pressure.
C) "You can still quit smoking if you want to. There are many resources available to help you." - This response is supportive but may sound presumptuous or premature if the client is not ready or willing to quit smoking. The nurse should assess the client's stage of change and readiness to quit before offering resources or assistance.
Complications and Comorbidities in Chronic Illnesses
A nurse is caring for a client with chronic obstructive pulmonary disease (COPD) who has developed cor pulmonale. Which assessment finding is most indicative of this complication?
Explanation
Cor pulmonale is a condition in which the right side of the heart fails due to increased pressure in the pulmonary arteries, caused by chronic lung disease. This results in fluid retention and venous congestion, leading to distended neck veins and peripheral edema.
Incorrect options:
A) Clubbing of the fingers and toes - This is a sign of chronic hypoxia, which may be present in clients with COPD, but does not necessarily indicate cor pulmonale.
C) Wheezes and crackles in the lung fields - These are signs of airway obstruction and fluid accumulation in the lungs, which are common in clients with COPD, but do not directly reflect the status of the right heart.
D) Cyanosis of the lips and nail beds - This is a sign of poor oxygenation, which may occur in clients with COPD, but does not indicate the presence of cor pulmonale.
A client with type 2 diabetes mellitus is admitted to the hospital with diabetic ketoacidosis (DKA). The nurse recognizes that which factor is most likely to have precipitated this complication?
Explanation
DKA is a life-threatening condition in which the body produces excess ketones due to a lack of insulin, resulting in metabolic acidosis, dehydration, and electrolyte imbalance. The most common triggers for DKA are acute stress or infection, which increase the body's demand for insulin and glucose.
Incorrect options:
A) Insufficient insulin administration - This is a possible cause of DKA, but not the most likely one, as clients with type 2 diabetes mellitus usually have some endogenous insulin production and may not require exogenous insulin therapy.
B) Excessive carbohydrate intake - This may cause hyperglycemia, but not DKA, as carbohydrates do not produce ketones when metabolized.
C) Prolonged physical activity - This may lower blood glucose levels, but not cause DKA, as exercise increases insulin sensitivity and glucose uptake by the muscles.
A client with rheumatoid arthritis (RA) is prescribed methotrexate, a disease-modifying antirheumatic drug (DMARD). Which statement by the client indicates a need for further teaching?
Explanation
Methotrexate is a potent immunosuppressant and cytotoxic agent that can cause serious adverse effects, such as bone marrow suppression, hepatotoxicity, pulmonary toxicity, and teratogenicity. The client should be instructed to monitor their blood counts, liver function tests, chest x-rays, and pregnancy tests regularly, and report any signs of infection, bleeding, jaundice, cough, or dyspnea. Blood pressure monitoring is not directly related to methotrexate therapy.
Incorrect options:
A) "I will take folic acid supplements to prevent side effects." - This is a correct statement, as folic acid supplementation can reduce the risk of methotrexate-induced hematologic toxicity and mucositis.
B) "I will avoid drinking alcohol while taking this medication." - This is a correct statement, as alcohol consumption can increase the risk of methotrexate-induced liver damage.
D) "I will use contraception to prevent pregnancy while taking this medication." - This is a correct statement, as methotrexate is contraindicated in pregnancy due to its potential teratogenic effects on the fetus.
A client with systemic lupus erythematosus (SLE) is experiencing a flare-up of symptoms. The nurse anticipates that the client may develop which complication related to SLE?
Explanation
Glomerulonephritis is a common complication of SLE, as the autoimmune disorder causes inflammation and damage to the glomeruli, the filtering units of the kidneys. This can lead to proteinuria, hematuria, hypertension, edema, and renal failure.
Incorrect options:
B) Thyroid storm - This is a rare complication of hyperthyroidism, not SLE. It is characterized by a severe exacerbation of thyroid hormone effects, such as fever, tachycardia, agitation, and delirium.
C) Pancreatitis - This is an inflammation of the pancreas, which can be caused by various factors, such as gallstones, alcohol abuse, trauma, or medications. It is not directly related to SLE.
D) Peptic ulcer disease - This is a condition in which ulcers form in the lining of the stomach or duodenum, due to erosion by gastric acid and pepsin. It can be caused by Helicobacter pylori infection, nonsteroidal anti-inflammatory drugs (NSAIDs), stress, or smoking. It is not directly related to SLE.
Ethical and Legal Considerations in Chronic Illness Care
A nurse is caring for a client who has terminal cancer and has expressed a wish to die at home. The client's family members are reluctant to honor this wish and insist that the client should stay in the hospital. What is the best action for the nurse to take in this situation?
Explanation
The nurse should respect the client's autonomy and right to self-determination, but also acknowledge the family's concerns and emotions. Referring the client and the family to a palliative care team can help to facilitate communication, provide education, address psychosocial and spiritual needs, and coordinate care options that are acceptable to both parties.
Incorrect options:
A) Respect the client's autonomy and advocate for their preference to die at home. - This option may seem respectful, but it does not consider the family's perspective or provide any support or guidance for them. The nurse should not act as a mediator or arbitrator between the client and the family, but rather involve a multidisciplinary team that can address their needs holistically.
B) Explain to the client that dying at home is not feasible and persuade them to stay in the hospital. - This option is disrespectful and paternalistic, as it disregards the client's wishes and imposes the nurse's own judgment on them. The nurse should not assume that dying at home is not feasible, as there may be resources and services available to assist with home-based palliative care. The nurse should also not coerce or manipulate the client into changing their decision, as this violates their autonomy and dignity.
D) Ask the client to reconsider their decision and respect the family's wishes. - This option is also disrespectful and paternalistic, as it implies that the client's decision is wrong or irrational, and that the family's wishes are more important or valid. The nurse should not pressure or guilt-trip the client into complying with the family's preferences, as this undermines their autonomy and dignity.
A client with chronic obstructive pulmonary disease (COPD) has signed a do-not-resuscitate (DNR) order and has requested no further interventions for their condition. The client develops acute respiratory distress and asks the nurse for help. What is the most appropriate response by the nurse?
Explanation
The nurse should respect the client's DNR order, which means that they do not want CPR or other life-sustaining measures in case of cardiac or respiratory arrest. However, this does not mean that they do not want any treatment or comfort care for their condition. The nurse should provide palliative interventions, such as oxygen and morphine, to relieve the client's symptoms and suffering.
Incorrect options:
A) "I'm sorry, but you have signed a DNR order, so I cannot do anything for you." - This option is insensitive and unethical, as it implies that the nurse has abandoned the client and does not care about their well-being. The nurse has a duty to provide compassionate care to all clients, regardless of their code status or prognosis.
B) "I will call your doctor and see if they can change your DNR order." - This option is inappropriate and unethical, as it disregards the client's wishes and autonomy. The nurse should not attempt to change or revoke the client's DNR order without their consent, unless there is evidence of a change of mind or new information that may affect their decision.
D) "I will initiate cardiopulmonary resuscitation (CPR) if you stop breathing." - This option is inappropriate and unethical, as it violates the client's DNR order and autonomy. The nurse should not perform CPR or other life-sustaining measures on a client who has explicitly refused them, unless there is evidence of a change of mind or new information that may affect their decision.
A nurse is conducting a home visit for a client who has diabetes mellitus type 2. The nurse observes that the client has several empty bottles of soda, candy wrappers, and fast food containers in their kitchen. The nurse also notes that the client has poor foot hygiene and several ulcers on their toes. What is the most ethical way for the nurse to address these issues with the client?
Explanation
The nurse should respect the client's autonomy and right to self-determination, but also encourage them to take responsibility for their health and well-being. The nurse should use a client-centered and motivational approach, which involves asking open-ended questions, expressing empathy, and exploring the client's feelings, beliefs, and goals. This can help to elicit the client's own reasons for change and enhance their readiness and confidence.
Incorrect options:
A) "You are not taking good care of yourself. You need to follow a healthy diet and check your feet every day." - This option is judgmental and authoritarian, as it criticizes the client's behavior and tells them what to do. The nurse should not use blame, shame, or guilt to influence the client's decisions, as this can damage the therapeutic relationship and increase the client's resistance and defensiveness.
B) "You are putting yourself at risk of serious complications. You should stop drinking soda, eating candy, and ordering fast food." - This option is fear-based and prescriptive, as it warns the client of the negative consequences of their behavior and gives them specific instructions. The nurse should not use scare tactics or coercion to influence the client's decisions, as this can undermine the client's autonomy and dignity.
C) "You have the right to make your own choices, but I am concerned about your health. Can we talk about your diet and foot care?" - This option is respectful and caring, but it is also somewhat passive and vague. The nurse should not use a but-statement, as this can negate or diminish the first part of the sentence. The nurse should also be more specific and direct in addressing the issues with the client, rather than asking for permission or implying a request.
A client with chronic kidney disease (CKD) has been informed that they need dialysis to maintain their renal function. The client refuses dialysis and states that they want to die naturally. The client's spouse disagrees with this decision and urges the nurse to convince the client to accept dialysis. What is the most legal way for the nurse to handle this situation?
Explanation
The nurse should respect the client's right to refuse treatment, as long as they are competent, informed, and voluntary in making their decision. The nurse should inform the spouse of this right and explain that it is a legal obligation to honor the client's wishes. The nurse should also provide emotional support and education to both parties, but not interfere with or influence their decision.
Incorrect options:
B) Inform the client that dialysis is the only option to prolong their life and that their decision will affect their spouse. - This option is inappropriate and unethical, as it disregards the client's wishes and autonomy. The nurse should not pressure or manipulate the client into accepting treatment by using false or exaggerated information or appealing to their emotions.
C) Inform both parties that dialysis is a standard of care for CKD and that they should consult a lawyer before making a final decision. - This option is irrelevant and unhelpful, as it does not address the ethical or legal aspects of the situation. The nurse should not imply that dialysis is mandatory or superior to other options, as this may bias or confuse the parties. The nurse should also not suggest legal action or involvement, as this may escalate or complicate the situation.
D) Inform both parties that dialysis is a personal choice and that they should seek counseling or mediation before making a final decision. - This option is respectful and supportive, but it is also unnecessary and potentially harmful
Communication and Therapeutic Relationships in Chronic Illness Care
A nurse is caring for a client who has chronic obstructive pulmonary disease (COPD) and is experiencing dyspnea. Which of the following actions should the nurse take to facilitate effective communication with the client?
Explanation
The nurse should use gestures and nonverbal cues, such as nodding, smiling, and eye contact, to supplement verbal communication with the client who has dyspnea. This helps to convey empathy, understanding, and interest, as well as reduce the need for the client to speak excessively.
Incorrect options:
A) Ask open-ended questions that require detailed responses. - This is an incorrect action, as asking open-ended questions that require detailed responses can increase the client's dyspnea and anxiety, as well as decrease the client's oxygenation.
C) Speak loudly and clearly to ensure the client can hear the nurse. - This is an incorrect action, as speaking loudly and clearly can be perceived as shouting or aggressive by the client, which can impair the therapeutic relationship and increase the client's stress level.
D) Interrupt the client frequently to save time and energy. - This is an incorrect action, as interrupting the client frequently can be disrespectful and rude, which can damage the rapport and trust between the nurse and the client.
A client who has diabetes mellitus is admitted to the hospital for a foot ulcer. The client tells the nurse that they have been feeling depressed and hopeless about their condition. Which of the following responses by the nurse demonstrates therapeutic communication?
Explanation
The nurse demonstrates therapeutic communication by using an open-ended statement that invites the client to express their feelings and concerns. The nurse also shows empathy, respect, and genuineness by offering to listen attentively.
Incorrect options:
A) "You should be more optimistic. Things could be worse." - This is a nontherapeutic response that minimizes the client's feelings and implies that the client is wrong or ungrateful for feeling depressed and hopeless.
B) "Why do you feel depressed and hopeless? You have a lot to live for." - This is a nontherapeutic response that uses a closed-ended question that can make the client feel defensive or guilty for feeling depressed and hopeless. The nurse also makes an assumption about the client's life without exploring their perspective.
C) "I understand how you feel. I have a family member who has diabetes too." - This is a nontherapeutic response that uses false reassurance and self-disclosure that can shift the focus away from the client and their feelings.
A nurse is conducting a health history interview with a client who has rheumatoid arthritis. The nurse notices that the client is grimacing and rubbing their hands. Which of the following statements by the nurse is appropriate at this time?
Explanation
The nurse uses an appropriate statement that acknowledges the client's pain and explores its impact on their quality of life and coping strategies. This helps to assess the client's physical, emotional, and social needs, as well as provide support and education.
Incorrect options:
A) "You seem to be in pain. Would you like some medication?" - This is an inappropriate statement that assumes that the client wants medication without assessing their pain level, preference, or history of medication use.
B) "How long have you had rheumatoid arthritis? What treatments have you tried?" - This is an inappropriate statement that ignores the client's pain and continues with the interview without addressing their comfort or needs.
C) "Let's take a break from the interview. I will come back later when you are feeling better." - This is an inappropriate statement that terminates the interview prematurely and may make the client feel dismissed or abandoned.
A client who has cancer is receiving palliative care at home. The client's spouse tells the nurse that they are overwhelmed by the caregiving responsibilities and feel guilty for wanting some time for themselves. Which of the following statements by the nurse reflects the use of empathy?
Explanation
The nurse reflects the use of empathy by recognizing and validating the spouse's feelings and situation, without judging or offering advice.
Incorrect options:
A) "You have been doing a great job caring for your spouse. You deserve some time for yourself." - This is a statement that reflects the use of praise, which can be helpful in some situations, but does not demonstrate empathy or address the spouse's feelings of guilt.
B) "You should not feel guilty for wanting some time for yourself. It is normal to feel that way." - This is a statement that reflects the use of reassurance, which can be counterproductive in some situations, as it can minimize or dismiss the spouse's feelings of guilt.
D) "You need to take care of yourself too. Have you considered respite care or hospice services?" - This is a statement that reflects the use of information, which can be beneficial in some situations, but does not demonstrate empathy or explore the spouse's feelings or needs.
Collaborative Care in the Community Setting
A nurse is caring for a client who has a history of recurrent urinary tract infections (UTIs). Which of the following actions should the nurse take to prevent UTIs in this client?
Explanation
The nurse should teach the client to urinate before and after sexual intercourse, as this can help flush out any bacteria that may have entered the urinary tract during sexual activity, reducing the risk of UTIs.
Incorrect options:
A) Encourage the client to drink cranberry juice daily. - This is an incorrect option, as there is insufficient evidence to support the use of cranberry juice for preventing or treating UTIs. Cranberry juice may also interact with some medications, such as warfarin, and increase the risk of bleeding.
B) Instruct the client to wipe from back to front after urination. - This is an incorrect option, as wiping from back to front can introduce bacteria from the anal area into the urethra, increasing the risk of UTIs. The client should be instructed to wipe from front to back after urination and bowel movements.
D) Advise the client to limit fluid intake to 1.5 L per day. - This is an incorrect option, as limiting fluid intake can reduce urine output and allow bacteria to multiply in the urinary tract, increasing the risk of UTIs. The client should be advised to drink at least 2 L of water per day, or more if advised by the health care provider, to promote adequate hydration and urinary elimination.
A nurse is conducting a home visit for a client who has diabetes mellitus and hypertension. The nurse notices that the client has several empty bottles of soda and bags of chips on the kitchen counter. Which of the following statements should the nurse make?
Explanation
The nurse should use an open-ended question to assess the client's dietary habits and preferences, as well as any barriers or challenges that may affect their food choices. This can help the nurse identify areas for education and intervention, and provide individualized and client-centered care.
Incorrect options:
A) "You should avoid eating these foods, as they can worsen your blood sugar and blood pressure levels." - This is an incorrect option, as it is a directive statement that may sound judgmental or accusatory, and may elicit resistance or defensiveness from the client. The nurse should avoid using "should" statements and instead use motivational interviewing techniques to elicit change talk from the client.
C) "These foods are high in calories, sugar, and sodium, which can have negative effects on your health." - This is an incorrect option, as it is an informative statement that may not address the client's readiness or motivation for change. The nurse should avoid providing information without first assessing the client's knowledge level and interest in learning.
D) "I can refer you to a dietitian who can help you plan a balanced diet that meets your nutritional needs." - This is an incorrect option, as it is a premature action that may not reflect the client's goals or preferences. The nurse should avoid making referrals without first exploring the client's needs and expectations.
A nurse is collaborating with a social worker to provide care for a client who has schizophrenia and lives alone in a low-income housing complex. The social worker reports that the client has been missing appointments and not taking medications as prescribed. Which of the following actions should the nurse take first?
Explanation
The nurse should use the nursing process to provide care for clients with mental health disorders. The first step of the nursing process is assessment, which involves collecting data about the client's physical, psychological, social, and environmental factors that may affect their health and well-being. By visiting the client at home, the nurse can directly observe the client's mental status and living conditions, and identify any potential problems or needs.
Incorrect options:
A) Contact the client's family members and ask them to check on the client regularly. - This is an incorrect option, as it is an intervention that should be implemented after assessing the client and determining their level of support and involvement from family members. The nurse should also respect the client's privacy and autonomy, and obtain their consent before contacting their family members.
B) Arrange for a home health aide to visit the client daily and administer medications. - This is an incorrect option, as it is an intervention that should be implemented after assessing the client and determining their level of functioning and adherence to medications. The nurse should also consider the client's preferences and resources, and collaborate with them to develop a realistic and individualized plan of care.
C) Call the client and express concern about their well-being and adherence to treatment. - This is an incorrect option, as it is an intervention that should be implemented after assessing the client and determining their level of engagement and motivation for treatment. The nurse should also avoid using confrontational or coercive language, and instead use therapeutic communication techniques to establish rapport and trust with the client.
A nurse is providing discharge teaching to a client who has chronic obstructive pulmonary disease (COPD) and uses supplemental oxygen at home. Which of the following instructions should the nurse include in the teaching?
Explanation
The nurse should instruct the client to avoid smoking or being near open flames while using oxygen, as this can pose a serious fire hazard and risk of injury. The nurse should also advise the client to keep a fire extinguisher nearby and post "no smoking" signs in their home.
Incorrect options:
A) "You should keep your oxygen flow rate between 2 to 4 L/min." - This is an incorrect option, as the oxygen flow rate should be prescribed by the health care provider based on the client's condition and oxygen saturation level. The nurse should instruct the client to follow the prescribed oxygen flow rate and not adjust it without consulting the health care provider.
B) "You should use a humidifier with your oxygen therapy." - This is an incorrect option, as the use of a humidifier with oxygen therapy depends on the type of oxygen delivery device and the client's comfort level. The nurse should instruct the client to follow the manufacturer's instructions for using a humidifier with their oxygen device, and monitor for signs of dryness or irritation in their nose or mouth.
D) "You should check your oxygen saturation level every 4 hours." - This is an incorrect option, as the frequency of checking the oxygen saturation level depends on the client's stability and response to oxygen therapy. The nurse should instruct the client to check their oxygen saturation level as directed by the health care provider, and report any changes or concerns.
Documentation and Evaluation in Chronic Illness Care
A nurse is assessing a client with chronic obstructive pulmonary disease (COPD). Which finding should the nurse document as an expected outcome of the client's plan of care?
Explanation
The goal of care for a client with COPD is to maintain adequate oxygenation and prevent complications. An oxygen saturation of 95% on room air indicates that the client is receiving enough oxygen without supplemental oxygen therapy.
Incorrect options:
B) Respiratory rate of 28 breaths per minute - This is an abnormal finding, as a normal respiratory rate for an adult is 12 to 20 breaths per minute. A respiratory rate of 28 breaths per minute indicates tachypnea, which may be a sign of respiratory distress or hypoxemia in a client with COPD.
C) Barrel-shaped chest on inspection - This is an abnormal finding, as a normal chest shape is elliptical, with a transverse diameter that is twice the anteroposterior diameter. A barrel-shaped chest, where the chest appears rounded and enlarged, is a result of chronic hyperinflation of the lungs due to COPD. It is not an expected outcome of the client's plan of care.
D) Clubbing of the fingers on palpation - This is an abnormal finding, as normal fingernails have a 160-degree angle between the nail and the nail bed. Clubbing of the fingers, where the angle increases to 180 degrees or more and the nail bed becomes soft and spongy, is a sign of chronic hypoxia due to COPD or other lung diseases. It is not an expected outcome of the client's plan of care.
A client with type 2 diabetes mellitus is scheduled for a hemoglobin A1c test. The client asks the nurse what this test measures. How should the nurse respond?
Explanation
A hemoglobin A1c test measures the percentage of hemoglobin molecules that have glucose attached to them. Hemoglobin molecules have a lifespan of about 120 days, so this test reflects the average blood glucose level over the past three months. It is used to monitor the long-term glycemic control and effectiveness of diabetes management.
Incorrect options:
B) "It measures your blood glucose level at the time of the test." - This is an incorrect statement, as this describes a random blood glucose test, which measures the blood glucose level at any time of the day, regardless of when the last meal was eaten.
C) "It measures your blood glucose level after fasting for eight hours." - This is an incorrect statement, as this describes a fasting blood glucose test, which measures the blood glucose level after not eating or drinking anything except water for at least eight hours.
D) "It measures your blood glucose level after eating a carbohydrate-rich meal." - This is an incorrect statement, as this describes a postprandial blood glucose test, which measures the blood glucose level one to two hours after eating a meal.
A nurse is evaluating a client's response to pain medication. Which question should the nurse ask to assess the intensity of the client's pain?
Explanation
The most reliable and valid method to assess pain intensity is to use a numeric rating scale, where zero means no pain and ten means the worst possible pain. This allows the nurse to quantify and document the client's pain level and monitor changes over time.
Incorrect options:
B) "How does your pain affect your daily activities?" - This is a question that assesses pain interference, which is how pain affects the client's physical, psychological, and social functioning. It does not directly measure pain intensity.
C) "What words would you use to describe your pain?" - This is a question that assesses pain quality, which is how the client perceives and expresses their pain sensation. It does not directly measure pain intensity.
D) "What do you think is causing your pain?" - This is a question that assesses pain etiology, which is the underlying cause or source of the pain. It does not directly measure pain intensity.
A client with rheumatoid arthritis is prescribed methotrexate, a disease-modifying antirheumatic drug (DMARD). Which statement by the client indicates a need for further teaching?
Explanation
The client should be instructed to avoid alcohol while taking methotrexate, as alcohol can increase the risk of liver toxicity and damage. Methotrexate can also impair the immune system and increase the risk of infection, so the client should report any signs of infection, such as fever, sore throat, or cough, to their doctor. Methotrexate can also affect the blood cell counts and kidney function, so the client should have regular blood tests to monitor these parameters. Folic acid supplements can help reduce the side effects of methotrexate, such as nausea, mouth ulcers, and hair loss.
Incorrect options:
A) "I will take folic acid supplements as prescribed by my doctor." - This is a correct statement, as folic acid supplements can help reduce the side effects of methotrexate, such as nausea, mouth ulcers, and hair loss.
C) "I will report any signs of infection to my doctor." - This is a correct statement, as methotrexate can impair the immune system and increase the risk of infection, so the client should report any signs of infection, such as fever, sore throat, or cough, to their doctor.
D) "I will have regular blood tests to monitor my liver and kidney function." - This is a correct statement, as methotrexate can affect the liver and kidney function, so the client should have regular blood tests to monitor these parameters.
Exams on Care of Patients with Chronic Illnesses
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction to Care of Patients with Chronic Illnesses
- Understanding Chronic Illnesses
- Assessment and Diagnosis of Chronic Illnesses
- Collaborative Care and Management of Chronic Illnesses
- Psychosocial Considerations in Chronic Illness Care
- Complications and Comorbidities in Chronic Illnesses
- Ethical and Legal Considerations in Chronic Illness Care
- Communication and Therapeutic Relationships in Chronic Illness Care
- Collaborative Care in the Community Setting
- Documentation and Evaluation in Chronic Illness Care
- Conclusion
- Summary
Notes Highlighting is available once you sign in. Login Here.
Objectives
- To define chronic illnesses and their impact on patients and society
- To describe the assessment and diagnosis process for patients with chronic illnesses
- To identify the principles and strategies of collaborative care and management for patients with chronic illnesses
- To discuss the psychosocial considerations in caring for patients with chronic illnesses
- To recognize the common complications and comorbidities in patients with chronic illnesses
- To examine the ethical and legal considerations in caring for patients with chronic illnesses
- To demonstrate effective communication and therapeutic relationships in caring for patients with chronic illnesses
- To apply the concepts of collaborative care in the community setting for patients with chronic illnesses
- To document and evaluate the outcomes of care for patients with chronic illnesses
Introduction to Care of Patients with Chronic Illnesses
- Chronic illnesses are conditions that last longer than 3 months and require ongoing medical attention or limit activities of daily living
- Examples of chronic illnesses include diabetes, hypertension, heart failure, arthritis, asthma, cancer, dementia, depression, etc.
- Chronic illnesses affect about 60% of adults in the United States and are the leading cause of death and disability
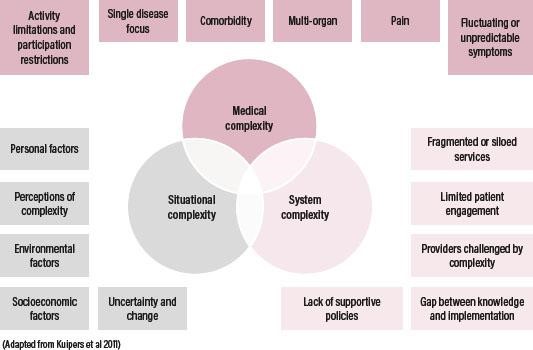
- Chronic illnesses pose significant challenges to patients, families, health care providers, and the health care system
- Care of patients with chronic illnesses requires a holistic, patient-centered, and interdisciplinary approach that focuses on promoting quality of life, preventing complications, and enhancing self-management
Understanding Chronic Illnesses
- Chronic illnesses are influenced by multiple factors, such as genetics, environment, lifestyle, behavior, culture, socioeconomic status, etc.
- Chronic illnesses have different trajectories and stages, such as stable, acute exacerbation, progressive deterioration, terminal phase, etc.
- Chronic illnesses have various effects on patients' physical, psychological, social, and spiritual well-being
- Patients with chronic illnesses experience different responses and coping mechanisms, such as denial, anger, depression, acceptance, adaptation, etc.

- Patients with chronic illnesses have diverse needs and preferences for information, education, support, and decision making
Assessment and Diagnosis of Chronic Illnesses
- Assessment of patients with chronic illnesses involves collecting comprehensive data about their history, physical examination, laboratory tests, diagnostic procedures, functional status, quality of life, etc.
- Diagnosis of patients with chronic illnesses involves identifying the specific type and severity of the condition, as well as the presence of any complications or comorbidities
- Assessment and diagnosis of patients with chronic illnesses should be done in collaboration with the patient and the health care team
- Assessment and diagnosis of patients with chronic illnesses should be done periodically to monitor changes and evaluate outcomes
Collaborative Care and Management of Chronic Illnesses
- Collaborative care and management of patients with chronic illnesses involves developing a plan of care that is individualized, evidence-based, goal-oriented, and patient-centered care.
- Collaborative care and management of patients with chronic illnesses involves implementing interventions that address the physical, psychological, social, and spiritual aspects of care
- Collaborative care and management of patients with chronic illnesses involves evaluating the effectiveness, safety, and satisfaction of the interventions
- Collaborative care and management of patients with chronic illnesses involves modifying the plan of care as needed based on the patient's condition, response, and feedback
Psychosocial Considerations in Chronic Illness Care
- Psychosocial considerations in caring for patients with chronic illnesses include assessing and addressing the patient's emotional, cognitive, behavioral, and relational issues that may affect their coping and adaptation to their condition
- Psychosocial considerations in caring for patients with chronic illnesses include providing education, counseling, referrals, and resources to help the patient manage their stress, anxiety, depression, grief, loss, isolation, stigma, etc.
- Psychosocial considerations in caring for patients with chronic illnesses include involving the patient's family, friends, and support groups in their care and providing them with information, education, support, and respite as needed
- Psychosocial considerations in caring for patients with chronic illnesses include promoting the patient's autonomy, dignity, self-esteem, hope, and spirituality.
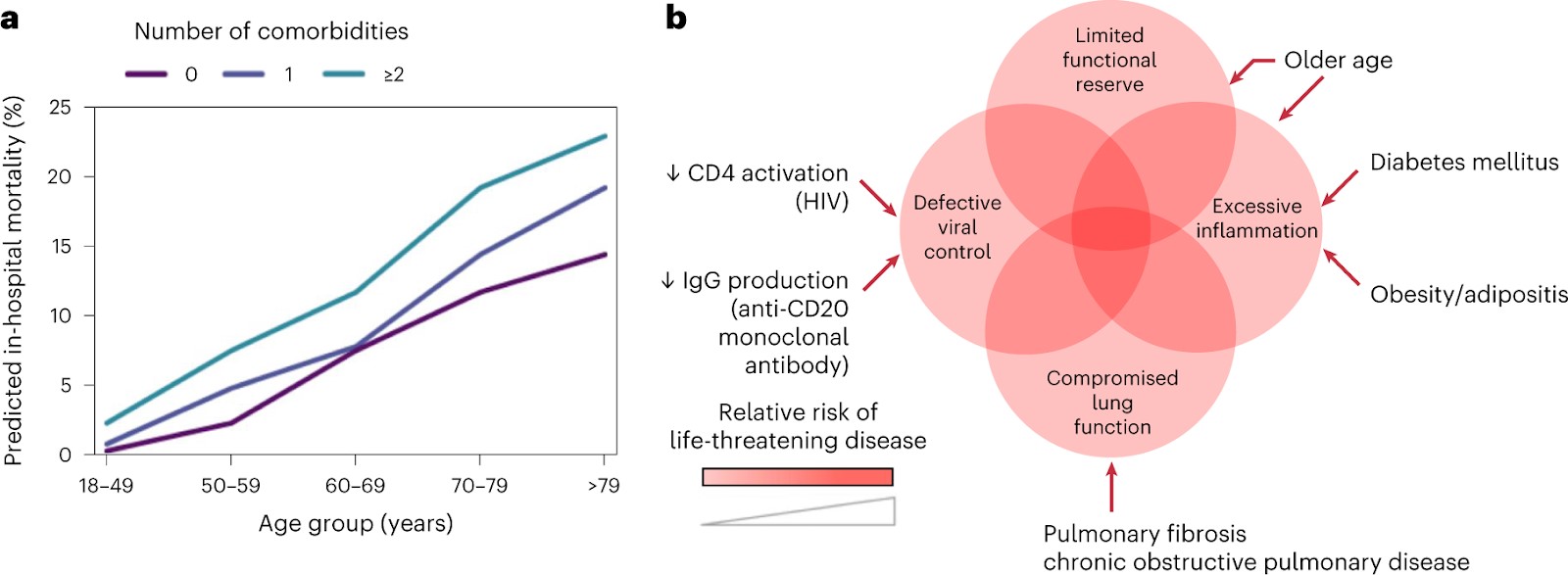
Complications and Comorbidities in Chronic Illnesses
- Complications are problems that arise from or are worsened by a chronic illness or its treatment
- Comorbidities are other conditions that coexist with a chronic illness or increase its risk or severity
- Examples of complications and comorbidities in patients with chronic illnesses include
a) infections
b) bleeding
c) pain
d) ulcers
e) fractures
f) renal failure
g) stroke
- Complications and comorbidities in patients with chronic illnesses can affect their prognosis, quality of life, and mortality
- Complications and comorbidities in patients with chronic illnesses can be prevented or managed by early detection, treatment adherence, lifestyle modification, risk reduction,
and symptom management
Ethical and Legal Considerations in Chronic Illness Care
- Ethical and legal considerations in caring for patients with chronic illnesses include respecting the patient's rights, values, beliefs, and preferences
- Ethical and legal considerations in caring for patients with chronic illnesses include ensuring the patient's informed consent, confidentiality, privacy, and security
- Ethical and legal considerations in caring for patients with chronic illnesses include facilitating the patient's advance directives, living wills, power of attorney, and organ donation
- Ethical and legal considerations in caring for patients with chronic illnesses include advocating for the patient's best interests, welfare, and access to care
- Ethical and legal considerations in caring for patients with chronic illnesses include addressing any ethical dilemmas, conflicts, or concerns that may arise in the course of care
Communication and Therapeutic Relationships in Chronic Illness Care
- Communication and therapeutic relationships in caring for patients with chronic illnesses involve establishing rapport, trust, and empathy with the patient
- Communication and therapeutic relationships in caring for patients with chronic illnesses involve using effective communication skills, such as active listening, open-ended questions, clarification, reflection, summarization.
- Communication and therapeutic relationships in caring for patients with chronic illnesses involve using appropriate communication strategies, such as motivational interviewing, teach-back method, shared decision making.
- Communication and therapeutic relationships in caring for patients with chronic illnesses involve using suitable communication tools and aids, such as charts, diagrams, models, videos.
- Communication and therapeutic relationships in caring for patients with chronic illnesses involve communicating respectfully, sensitively, and honestly with the patient
Collaborative Care in the Community Setting
- Collaborative care in the community setting for patients with chronic illnesses involves providing care that is accessible, affordable, coordinated, continuous, and comprehensive
- Collaborative care in the community setting for patients with chronic illnesses involves collaborating with other health care providers, such as primary care providers, specialists, pharmacists, nurses, social workers.
- Collaborative care in the community setting for patients with chronic illnesses involves collaborating with other community resources, such as home health agencies, hospice services, senior centers, support groups.
- Collaborative care in the community setting for patients with chronic illnesses involves educating and empowering the patient and their caregivers to self-manage their condition and prevent complications
- Collaborative care in the community setting for patients with chronic illnesses involves following up and monitoring the patient's progress and outcomes
Documentation and Evaluation in Chronic Illness Care
- Documentation and evaluation in caring for patients with chronic illnesses involve recording and reporting the patient's data, interventions, outcomes, and feedback
- Documentation and evaluation in caring for patients with chronic illnesses involve using standardized formats, terminologies, abbreviations, and symbols
- Documentation and evaluation in caring for patients with chronic illnesses involve using electronic health records, databases, registries.
- Documentation and evaluation in caring for patients with chronic illnesses involve using quality indicators, measures, benchmarks.
- Documentation and evaluation in caring for patients with chronic illnesses involve using evidence-based practice, research, guidelines, protocols.
Conclusion
- Care of patients with chronic illnesses is a complex and challenging task that requires a holistic, patient-centered, and interdisciplinary approach
- Care of patients with chronic illnesses aims to promote quality of life, prevent complications, and enhance self-management
- Care of patients with chronic illnesses involves various aspects of care, such as assessment, diagnosis, collaborative care, management, psychosocial considerations, complications, comorbidities, ethical and legal considerations, communication, therapeutic relationships, collaborative care in the community setting, documentation, and evaluation
Summary
- Chronic illnesses are conditions that last longer than 3 months and require ongoing medical attention or limit activities of daily living
- Care of patients with chronic illnesses requires a holistic, patient-centered, and interdisciplinary approach that focuses on promoting quality of life, preventing complications, and enhancing self-management
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Care of Patients with Chronic Illnesses
This filled cannot be empty

