Please set your exam date
Pre-term Labor
Study Questions
Introduction
A nurse is educating a pregnant client about pre-term labor.
Which of the following is a correct statement about pre-term birth?
Explanation
Pre-term birth can result in long-term developmental disabilities.This is because pre-term babies are born before their organs and systems are fully developed and may face complications such as respiratory distress, bleeding in the brain, infection, and jaundice.
Choice A is wrong because pre-term birth occursbefore37 weeks of gestation, not after.Choice B is wrong because pre-term birth isassociatedwith increased neonatal morbidity and mortality.Choice D is wrong because pre-term birth can be caused byvariousfactors, such as infection, multiple pregnancy, cervical insufficiency, placental abruption, and maternal conditions.
It is not always induced by medical complications.
Normal ranges for gestational age are 37 to 42 weeks.Normal ranges for hemoglobin are 11 to 16 g/dL for pregnant women.
A client asks a nurse about the potential consequences of pre-term labor.
Which of the following is an accurate response?
Explanation
Pre-term labor can lead to neonatal morbidity and mortality.Pre-term labor is defined as labor that occurs before 37 weeks of gestation.Pre-term infants are at risk for various complications, such as respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, sepsis, and death.
Choice A is wrong because pre-term labor does pose risks to the infant, as explained above.
Choice C is wrong because pre-term labor occurs before 40 weeks of gestation, not after.The normal term of pregnancy is 40 weeks.
Choice D is wrong because pre-term labor can be caused by various factors, not only obstetric complications.Some of the risk factors for pre-term labor include multiple gestation, infection, cervical insufficiency, placental abruption, preeclampsia, and maternal stress.
A nurse is discussing pre-term labor with a pregnant client.
Which of the following statements accurately describes pre-term labor?
Explanation
Preterm labor involves irregular uterine contractions without cervical changes.This is because preterm labor is defined as labor that occurs before 37 weeks of gestation with regular contractions and cervical changes.
Irregular contractions without cervical changes are more likely to be Braxton Hicks contractions, which are normal and do not indicate labor.
Choice A is wrong because preterm labor can be spontaneous or induced.
Spontaneous preterm labor occurs without a known cause or risk factor, while induced preterm labor is done for medical
A nurse is providing education about pre-term labor to a group of pregnant clients.
Which of the following statements about pre-term labor is correct?
Explanation
Pre-term labor can lead to neonatal morbidity and mortality.Pre-term labor is defined as labor that occurs before 37 weeks of gestation.Pre-term birth is the leading cause of death among children under 5 years of age.Pre-term babies may face a lifetime of disability, including learning disabilities and visual and hearing problems.
Choice A is wrong because pre-term labor is more likely to occur before 40 weeks of gestation, not after.
Choice B is wrong because pre-term labor does have an impact on the baby’s long-term health, such as increased risk of infections, bleeding in the brain, and respiratory distress syndrome.
Choice C is wrong because pre-term labor does not always require medical induction.Sometimes, pre-term labor can be stopped or delayed with medications or bed rest.
Causes and Risk Factors
A nurse is caring for a client who is at 32 weeks of gestation and has pre-term labor.
Which of the following infections can increase the risk of pre-term labor?
Explanation
Bacterial vaginosis is the most common vaginal infection in women of reproductive age and it increases the risk of preterm labor.It is caused by an imbalance of the normal vaginal flora and can lead to intra-amniotic infection, which can trigger inflammation and uterine contractions.
Choice B. Candidiasis is wrong because it is a fungal infection that does not increase the risk of preterm labor.
It can cause itching, burning, and discharge, but it does not affect the amniotic fluid or the fetus.
Choice C. Gonorrhea is wrong because it is a bacterial infection that can cause pelvic inflammatory disease, which can increase the risk of preterm labor, but it is not as common as bacterial vaginosis.
Gonorrhea can also cause neonatal conjunctivitis if transmitted during delivery.
Choice D. Syphilis is wrong because it is a bacterial infection that can cause congenital syphilis if transmitted during pregnancy, but it does not increase the risk of preterm labor.
Syphilis can cause serious complications such as stillbirth, neonatal death, or neurologic damage.
A nurse is reviewing the medical history of a client who is at 28 weeks of gestation and has pre-term labor.
Which of the following conditions can cause placental abnormalities that can lead to pre-term labor?
Explanation
Preeclampsia.Preeclampsia is a condition that can cause placental abnormalities that can lead to pre-term labor.Preeclampsia is characterized by high blood pressure and proteinuria in pregnant women after 20 weeks of gestation.
Preeclampsia can affect the blood flow to the placenta and cause placental insufficiency, which is a reduced ability of the placenta to deliver oxygen and nutrients to the fetus.Placental insufficiency can trigger pre-term labor as a way of protecting the fetus from further hypoxia and growth restriction.
Choice A. Diabetes mellitus is wrong because diabetes mellitus does not directly cause placental abnormalities
A nurse is assessing a client who is at 30 weeks of gestation and has pre-term labor.
Which of the following findings can indicate cervical insufficiency?
Explanation
Cervical length of less than 2.5 cm.This can indicate cervical insufficiency, a condition in which the cervix begins to dilate and efface prematurely, leading to preterm labor.A normal cervical length is about 4 cm.
Choice A is wrong because cervical dilation of 4 cm or more is not a sign of cervical insufficiency, but rather of active labor.
Choice B is wrong because cervical effacement of 80% or more is also a sign of active labor, not cervical insufficiency.Choice D is wrong because cervical funneling is not a finding that can indicate cervical insufficiency by itself, but rather a complication that can result from it.Cervical funneling is when the internal os (the opening of the cervix inside the uterus) widens while the external os (the opening of the cervix outside the uterus) remains closed.
A nurse is educating a client who is at 26 weeks of gestation and has pre-term labor about the risk factors for pre-term labor.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The client should limit their physical activity and stress as much as possible, as these are risk factors for pre-term labor.
Some additional explanations are:
• Choice A is correct because smoking and drinking alcohol during pregnancy can increase the risk of pre-term labor and birth, as well as other complications for the mother and the baby.
• Choice B is correct because any signs of vaginal bleeding or fluid leakage can indicate a problem with the pregnancy, such as placenta previa or premature rupture of membranes, which can lead to pre-term labor and birth.
The client should report these symptoms to their provider immediately.
• Choice D is correct because drinking plenty of fluids and eating a balanced diet can help prevent dehydration and malnutrition, which can also contribute to pre-term labor and birth.The client should also avoid caffeine, artificial sweeteners, and foods that may cause foodborne illness.
Normal ranges for gestational age are 37 to 42 weeks.Pre-term labor is defined as regular contractions that result in the opening of the cervix before 37 weeks of pregnancy.Pre-term birth is the delivery of a baby before 37 weeks of pregnancy.
A nurse is evaluating a client who is at 34 weeks of gestation and has pre-term labor.
Which of the following fetal factors can contribute to pre-term labor?
Explanation
Fetal aneuploidy, which means having an abnormal number of chromosomes, can contribute to pre-term labor.This is because fetal abnormalities are associated with 30% of preterm deliveries.
Choice A is wrong because fetal macrosomia, which means having a large baby, is not a risk factor for pre-term labor.In fact, it may increase the risk of post-term delivery.
Choice C is wrong because fetal distress, which means the baby is not getting enough oxygen or nutrients, is not a cause of pre-term labor, but rather a complication that may occur during labor and delivery.
Choice D is wrong because fetal hydrops, which means having excess fluid in the body tissues, is not a direct cause of pre-term labor, but rather a symptom of other conditions that may affect the baby’s health.
Normal ranges for gestational age are 37 to 42 weeks.Pre-term labor occurs when regular contractions result in the opening of the cervix after week 20 and before week 37 of pregnancy.
Signs and Symptoms
A nurse is assessing a pregnant client who is at risk for pre-term labor.
Which sign or symptom should the nurse prioritize when determining the need for immediate intervention?
Explanation
Regular uterine contractions occurring every 20 minutes.This is a sign of preterm labor, which is labor that begins before 37 weeks of pregnancy.
Preterm labor can lead to premature birth and complications for the baby.
Choice B is wrong because low back pain lasting for 15 minutes is not a specific sign of preterm labor.
It could be caused by other factors, such as posture, muscle strain, or kidney infection.
Choice C is wrong because a change in vaginal discharge with a mild increase in amount is not a sign of preterm labor.
It is normal for pregnant women to have some vaginal discharge throughout pregnancy.
However, if the discharge is watery, bloody, or has a foul odor, it could indicate a problem and should be reported to the provider.
Choice D is wrong because decreased fetal movement is not a sign of preterm labor.
It could be a sign of fetal distress or other complications.
Pregnant women should monitor their baby’s movements daily and contact their provider if they notice any changes or concerns.
A client at 32 weeks of gestation presents with regular uterine contractions occurring every 7 minutes and lasting for 45 seconds.
Which additional sign or symptom should the nurse expect to assess?
Explanation
Lower abdominal cramping or pressure is one of the signs and symptoms of preterm labor.
Preterm labor occurs when regular contractions begin to open your cervix before 37 weeks of pregnancy.A full-term pregnancy should last about 40 weeks.
B. Low back pain.Statement is wrong because low back pain is also a sign and symptom of preterm labor.
C. Change in vaginal discharge.Statement is wrong because change in vaginal discharge, such as leaking fluid or bleeding, is also a sign and symptom of preterm labor.
D. Rupture of membranes.Statement is wrong because rupture of membranes, or breaking of water, is also a sign and symptom of preterm labor.
If you think you might be having preterm labor, you should call your doctor or go to the hospital to be evaluated.
A nurse is assessing a pregnant client who is at risk for pre-term labor.
Which signs or symptoms should the nurse consider as a potential indicator of imminent labor?
Explanation
Change in vaginal discharge, including increased amount, color, or consistency.This can indicate that the client is losing the mucus plug or experiencing a premature rupture of membranes, which are signs of imminent labor.
Choice A is wrong because regular uterine contractions every 10 minutes lasting for 30 seconds are not indicative of imminent labor.They could be Braxton Hicks contractions, which are irregular and painless contractions that occur throughout pregnancy.
Choice B is wrong because low back pain and pelvic pressure are common discomforts of pregnancy and do not necessarily mean that the client is in labor.
Choice D is wrong because decreased fetal movement is not a sign of imminent labor.It could be a sign of fetal distress or hypoxia and should be reported to the provider.
Normal ranges for vaginal discharge during pregnancy are clear or white in color, thin or milky in consistency, and mild or odorless in smell.
Any changes from these ranges should be evaluated by the provider.
A nurse is assessing a pregnant client who is at risk for pre-term labor.
Which symptom should the nurse consider as a potential warning sign indicating the need for immediate medical attention?
Explanation
Regular uterine contractions occurring every 20 minutes are a sign of preterm labor that requires immediate medical attention.Preterm labor is any labor that occurs from 20 weeks through 36 weeks of pregnancy.If preterm labor can’t be stopped, the baby will be born early and may have health problems.
Choice B is wrong because mild lower abdominal cramping is a normal symptom of pregnancy and does not indicate preterm labor.
Choice C is wrong because low back pain lasting for 10 minutes is not a specific symptom of preterm labor and may be caused by other factors such as posture or muscle strain.
Choice D is wrong because a change in vaginal discharge with a mild increase in amount is also a normal symptom of pregnancy and does not indicate preterm labor.However, if the discharge is watery, bloody, or has a foul odor, it may be a sign of infection or placental problems and should be reported to the doctor.
Assessment
A nurse is assessing a pregnant client at 28 weeks of gestation.
Which finding should the nurse prioritize as a potential sign of pre-term labor?
Explanation
Mild lower abdominal cramping is a sign of preterm laborand should be prioritized as a potential complication.Preterm labor occurs when regular contractions begin to open your cervix before 37 weeks of pregnancy.
A full-term pregnancy should last about 40 weeks.
Choice B is wrong because a change in vaginal discharge color is not a specific sign of preterm labor.
It could be due to other factors such as infection or normal hormonal changes.
Choice C is wrong because a brief episode of low back pain is not a sign of preterm labor.
It could be due to posture, muscle strain or other causes.
Choice D is wrong because occasional fetal hiccups are not a sign of preterm labor.
They are normal movements of the fetus and do not indicate any distress or danger.
A nurse is performing a physical examination on a client who is at 30 weeks of gestation and has pre-term labor.
Which of the following findings indicates fetal distress?
Explanation
Fetal heart rate decelerations indicate fetal distress because they reflect a decrease in blood flow or oxygen to the fetus.
Choice A is wrong because a fetal heart rate of 150/min is within the normal range of 110-160 bpm.Choice B is wrong because a fetal heart rate variability of 10/min is considered moderate and reassuring.Choice D is wrong because fetal heart rate accelerations are a sign of fetal well-being and indicate that the fetus is responding to stimuli.
A nurse is performing a speculum examination on a client who is at 26 weeks of gestation and has pre-term labor.
Which of the following findings indicates a positive FFN test?
Explanation
Bluish-white secretions.
This indicates a positive FFN test, which means that the fetal fibronectin protein has been released into the cervical secretions.Fetal fibronectin is a protein that helps keep the amniotic sac attached to the lining of the uterus.A positive FFN test means that there is a higher risk of preterm labor.
Choice A is wrong because yellow-green discharge could indicate an infection, not preterm labor.
Choice B is wrong because bloody show is a sign of cervical dilation, not preterm labor.
Choice C is wrong because sticky mucus plug is a normal part of pregnancy, not preterm labor.
A negative FFN test means that there is a less than 1% chance of preterm labor within the next 2 weeks.The FFN test is used to rule out preterm labor and avoid unnecessary treatments.It is approved for use in women with symptoms of preterm labor who are 24 to 35 weeks pregnant.
A nurse is assessing a client for pre-term labor.
Which of the following assessments should the nurse prioritize?
Explanation
Performing a speculum examination of the vagina and cervix.
This is because a speculum examination can help determine the presence of cervical dilation, effacement, or infection, which are signs of pre-term labor.
A speculum examination can also detect the presence of fetal fibronectin, which is a protein that indicates an increased risk of pre-term delivery.
Choice A is wrong because obtaining a detailed history of previous pregnancies is not a priority assessment for pre-term labor.
While it can provide some information about the client’s risk factors, it does not indicate the current status of the pregnancy or the cervix.
Choice B is wrong because checking the fetal heart rate and activity is not a priority assessment for pre-term labor.
While it can provide some information about the fetal well-being, it does not indicate the presence or absence of contractions or cervical changes.
Choice D is wrong because performing laboratory tests, such as urine culture, is not a priority assessment for pre-term labor.
While it can help identify possible infections that may contribute to pre-term labor, it does not provide immediate results or indicate the current status of the cervix.
A nurse is performing a physical examination on a client suspected of pre-term labor.
Which assessment finding should the nurse report immediately?
Explanation
A positive fetal fibronectin test (FFN) indicates that the fetal membrane has been disrupted and labor may occur within the next 7 to 14 days.
This is a sign of preterm labor that should be reported immediately.
Choice A is wrong because elevated blood glucose level is not a sign of preterm labor, but a possible complication of gestational diabetes.
Choice B is wrong because thinning of the cervix (also called effacement) is a normal process that occurs during late pregnancy and labor.
It does not necessarily indicate preterm labor.
Choice D is wrong because abdominal tenderness is not a specific sign of preterm labor.
It could be caused by other factors such as constipation, gas, or stretching of the ligaments.
Some of the signs and symptoms of preterm labor include:
• Regular or frequent sensations of abdominal tightening (contractions) every 10 minutes or more often
• Change in vaginal discharge (leaking fluid or bleeding from the vagina)
• Feeling of pressure in the pelvis (hip) area
• Low, dull backache
• Cramps that feel like menstrual cramps
• Abdominal cramps with or without diarrhea
A nurse is caring for a client in pre-term labor.
Which intervention should the nurse prioritize to improve blood flow to the placenta and fetus?
Explanation
The correct answer is choice B. Administering tocolytics.Tocolytics are drugs that inhibit uterine contractions and can delay preterm labor for a short time.This can allow time for the administration of antenatal corticosteroids and transfer to a tertiary care facility if necessary.
Choice A is wrong because administering intravenous fluids does not improve blood flow to the placenta and fetus.It may also increase the risk of pulmonary edema in women with preterm labor.
Choice C is wrong because administering corticosteroids does not improve blood flow to the placenta and fetus.Corticosteroids are given to enhance fetal lung maturity and reduce the risk of neonatal complications such as respiratory distress syndrome, intracranial hemorrhage, and necrotizing enterocolitis.
However, they do not stop preterm labor.
Choice D is wrong because providing emotional support does not improve blood flow to the placenta and fetus.Emotional support is important for women with preterm labor, but it is not a priority intervention to prevent fetal hypoxia or acidosis.
A client at 28 weeks of gestation is experiencing pre-term labor.
Which intervention should the nurse anticipate to enhance fetal lung maturity?
Explanation
Administering corticosteroids.Corticosteroids are drugs that can speed up the development of the baby’s lungs and reduce the risk of respiratory distress syndrome and other complications of preterm birth.They are usually given to pregnant women who are at risk of preterm delivery between 24 0/7 weeks and 33 6/7 weeks of gestation.
Choice A is wrong because administering intravenous fluids does not enhance fetal lung maturity.
It may be used to treat dehydration or prevent hypotension, but it has no effect on the baby’s lungs.
Choice B is wrong because administering tocolytics does not enhance fetal lung maturity.
Tocolytics are drugs that can delay preterm labor for a short time, but they do not improve the baby’s lung function.
Choice D is wrong because providing emotional support does not enhance fetal lung maturity.
It may help the mother cope with stress and anxiety, but it does not affect the baby’s lungs.
Fetal lung maturity is the condition of the baby’s lungs being able to breathe normally after birth.It involves several developmental processes, such as the formation of alveoli, bronchi, and surfactant.
Fetal lungs are usually mature by 36 weeks of gestation, but some babies may need steroids to speed up lung development if they are at risk of preterm birth.
A nurse is monitoring a client in pre-term labor for signs of fetal lung maturity enhancement.
Which medication should the nurse anticipate administering?
Explanation
Betamethasone is a corticosteroid that can be given to pregnant women who are at risk of preterm labor to enhance fetal lung maturity and reduce the risk of respiratory distress syndrome in the newborn.
Betamethasone stimulates the production of surfactant, a substance that helps the lungs expand and prevents them from collapsing.
Choice A is wrong because magnesium sulfate is used to prevent seizures in women with preeclampsia or eclampsia, not to enhance fetal lung maturity.
Choice B is wrong because nifedipine is a calcium channel blocker that can be used to relax the uterine muscles and inhibit contractions in preterm labor, but it does not affect fetal lung development.
Choice D is wrong because ampicillin is an antibiotic that can be used to treat infections that may cause preterm labor, such as chorioamnionitis or group B streptococcus, but it does not have any direct effect on fetal lung maturation.
A client at 32 weeks of gestation is diagnosed with pre-term labor.
Which intervention should the nurse prioritize to reduce uterine activity?
Explanation
Administering tocolytics.Tocolytics are drugs that inhibit uterine contractions and can delay preterm labor for a short time.This can allow time for the administration of corticosteroids and transfer to a tertiary care facility if necessary.
Choice A is wrong because administering intravenous fluids does not reduce uterine activity.It may be used to correct dehydration or electrolyte imbalance, which can be risk factors for preterm labor.
Choice C is wrong because administering corticosteroids does not reduce uterine activity.It may be used to enhance fetal lung maturity and reduce the risk of neonatal complications such as respiratory distress syndrome, intracranial hemorrhage, and necrotizing enterocolitis.
Choice D is wrong because administering antibiotics does not reduce uterine activity.It may be used to treat infections that can trigger preterm labor, such as bacterial vaginosis or chorioamnionitis.
A nurse is caring for a client in pre-term labor and suspects an infection.
Which assessment finding would support this suspicion?
Explanation
A decrease in fetal heart rate can indicate fetal distress due to infection, hypoxia, or cord compression.
Normal fetal heart rate is between 110 and 160 beats per minute.
Choice B. Increased uterine contractions is wrong because it is a normal sign of pre-term labor and does not necessarily indicate infection.
Choice C. Decreased fluid intake is wrong because it is not a specific sign of infection and can have other causes such as nausea, vomiting, or decreased thirst.
Choice D. Decreased cervical changes is wrong because it is also not a specific sign of infection and can indicate ineffective contractions or cervical incompetence.
A client with pre-term labor is at 28 weeks of gestation.
Which intervention should the nurse prioritize to monitor fetal well-being?
Explanation
Monitoring cervical changes.
This is because cervical changes indicate the progress of labor and the risk of preterm delivery.
Preterm labor is defined as regular uterine contractions with cervical dilation and effacement before 37 weeks of gestation.
The nurse should assess the cervical length, dilation, effacement, and position frequently to determine the need for interventions to stop or delay labor.
Choice A is wrong because monitoring vital signs is not specific to fetal well-being.
Vital signs can reflect maternal health, infection, or complications, but they do not directly measure fetal status.
Choice C is wrong because monitoring fluid intake and output is not specific to fetal well-being.
Fluid balance can affect maternal hydration, electrolytes, and blood pressure, but it does not directly measure fetal status.
Choice D is wrong because monitoring maternal preference is not specific to fetal well-being.
Maternal preference can affect the comfort, satisfaction, and coping of the mother, but it does not directly measure fetal status.
A nurse is caring for a client who has preterm labor.
Which manifestation should the nurse identify as a complication of preterm labor?
Explanation
Haemorrhage due to placental abruption.
Placental abruption is a serious complication of preterm labor that occurs when the placenta separates from the wall of the uterus before delivery.This can cause heavy bleeding and endanger the life of both the mother and the baby.
Choice A is wrong because increased fetal movement is not a complication of preterm labor.In fact, decreased fetal movement may indicate fetal distress.
Choice B is wrong because decreased uterine contractions are not a complication of preterm labor.Preterm labor is defined as regular contractions that result in the opening of the cervix before 37 weeks of pregnancy.
Choice D is wrong because increased cervical dilation is not a complication of preterm labor, but a sign of it.Cervical dilation indicates that the cervix is preparing for delivery and may lead to preterm birth.
A nurse is caring for a newborn who was born prematurely.
Which finding should the nurse report as a potential complication of prematurity?
Explanation
Hypoglycemia due to low glycogen stores.
Premature newborns have low glycogen stores and are at risk of developing hypoglycemia, which can cause seizures, brain damage, or death.
The nurse should monitor the blood glucose levels of the newborn and report any signs of hypoglycemia, such as jitteriness, lethargy, poor feeding, or temperature instability.
Choice A is wrong because increased bilirubin levels, not decreased, are a potential complication of prematurity.
Bilirubin is a waste product of red blood cell breakdown that can accumulate in the blood and cause jaundice, a yellowing of the skin and eyes.
Premature newborns have immature livers that cannot process bilirubin effectively and may need phototherapy to reduce the levels.
Choice B is wrong because decreased fat stores, not increased, are a potential complication of prematurity.
Fat stores provide insulation and energy for the newborn and help maintain body temperature.
Premature newborns have less subcutaneous fat and are prone to heat loss and cold stress, which can affect their metabolism and oxygen consumption.
Choice D is wrong because absence of mature lung surfactant, not presence, is a potential complication of prematurity.
Surfactant is a substance that reduces the surface tension of the alveoli and prevents them from collapsing during expiration.
Premature newborns have insufficient surfactant production and may develop respiratory distress syndrome, which is characterized by tachypnea, grunting, retractions, and cyanosis.
A nurse is assessing a preterm newborn and notes the presence of retinopathy of prematurity (ROP).
Which intervention should the nurse anticipate in the plan of care?
Explanation
Scheduling regular eye examinations.
Retinopathy of prematurity (ROP) is an eye disease that can happen in babies who are premature or who weigh less than 3 pounds at birth.ROP happens when abnormal blood vessels grow in the retina, which can cause vision loss or blindness.
The best way to prevent and treat ROP is to monitor the retinal development and detect any signs of abnormal blood vessel growth early.This can be done by regular eye examinations by an ophthalmologist.Some babies with mild ROP may get better without treatment, but some may need laser treatment, eye injections, or surgery to stop the abnormal blood vessels and prevent retinal detachment.
Choice A is wrong because antibiotics are not used to treat ROP.
Antibiotics are used to treat infections, which are not the cause of ROP.
Choice B is wrong because phototherapy is not used to treat ROP.
Phototherapy is used to treat jaundice, which is a condition where the skin and eyes turn yellow due to high levels of bilirubin in the blood.
Jaundice is not related to ROP.
Choice C is wrong because surfactant is not used to treat ROP.
Surfactant is a substance that helps the lungs function properly by reducing the surface tension of the air sacs.
Surfactant may be given to premature babies who have respiratory distress syndrome, which is a lung problem that can affect their oxygen levels.However, surfactant does not directly affect the retina or the blood vessels in the eye.
A nurse is caring for a client who is at risk for developing intraventricular hemorrhage (IVH).
Which action should the nurse take to reduce the client's risk?
Explanation
Maintaining a neutral head position.This action can help reduce the client’s risk of intraventricular hemorrhage (IVH) by preventing fluctuations in intracranial pressure that could rupture blood vessels in the brain.
Choice A is wrong because encouraging early ambulation can increase the risk of IVH by causing changes in blood pressure and cerebral perfusion.
Choice B is wrong because administering medications to induce hypercoagulability can increase the risk of IVH by promoting thrombosis and impairing blood flow to the brain.
Choice C is wrong because monitoring the client’s blood glucose levels is not directly related to the prevention of IVH, although it may be important for other reasons such as avoiding hypoglycemia or hyperglycemia.
Nursing Interventions
A client is being assessed for pre-term labor.
The nurse performs a digital examination of the cervix and finds it to be 3 cm dilated, 60% effaced, and at -2 station.
What should the nurse interpret from these findings?
Explanation
The client is at risk for pre-term birth.Pre-term labor occurs when regular contractions begin to open your cervix before 37 weeks of pregnancy.A full-term pregnancy should last about 40 weeks.The client’s cervix is 3 cm dilated, 60% effaced, and at -2 station, which indicates that the cervix is thinning and opening, and the baby is moving down the birth canal.These are signs of early labor, which can progress to active labor and delivery if not stopped.
Choice A is wrong because the client is not in active labor.Active labor is when the cervix is 6 cm or more dilated, and contractions are stronger and closer together.
Choice B is wrong because the client is not in labor.Labor is when the cervix begins to open and the baby moves down the birth canal due to regular contractions.
Choice C is wrong because the client is not experiencing early labor.Early labor is when the cervix is up to 6 cm dilated, and contractions are mild and irregular.
Complications and Outcomes
A nurse is caring for a client who is experiencing pre-term labor at 32 weeks of gestation.
The client’s cervix is 3 cm dilated and 80% effaced.
The nurse should anticipate administering which medication to suppress uterine contractions?
Explanation
Nifedipine.Nifedipine is a medication that can slow or stop contractions of the uterus and may prevent labor for 2 to 7 days.It works by relaxing smooth muscles and inhibiting uterine wall contractions.It can prolong delivery by up to 48 hours, allowing for proper lung development in the fetus.
Choice A is wrong because magnesium sulfate is not a tocolytic drug, but a medication that can prevent seizures and reduce the risk of cerebral palsy in preterm babies.
Choice B is wrong because betamethasone is not a tocolytic drug, but a corticosteroid that can help promote the baby’s lung maturity.
Choice D is wrong because indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) that can inhibit prostaglandin synthesis and reduce uterine contractions.However, it has serious side effects such as oligohydramnios (low amniotic fluid), premature closure of the ductus arteriosus (a blood vessel in the baby’s heart), and bleeding problems.Therefore, it is not recommended for use after 32 weeks of gestation.
Patient Education and Discharge Planning
A nurse is caring for a client who has preterm labor.
Which finding should the nurse report as a potential complication of preterm labor?
Explanation
Necrotizing enterocolitis (NEC) is a potential complication of preterm labor that affects the intestines of premature infants.NEC can cause inflammation, infection and tissue death in the bowel, leading to serious problems such as perforation, sepsis and shock.NEC usually occurs within the first two weeks of life and requires immediate medical attention.
Choice A is wrong because decreased fetal heart rate is not a complication of preterm labor, but a sign of fetal distress that may indicate a problem with the placenta, umbilical cord or fetus.
Choice C is wrong because hypothermia due to low fat stores is not a complication of preterm labor, but a common condition of premature infants who have difficulty maintaining their body temperature due to their immature skin and lack of subcutaneous fat.
Choice D is wrong because increased amniotic fluid production is not a complication of preterm labor, but a condition called polyhydramnios that may occur in pregnancies with multiple fetuses, diabetes, fetal anomalies or infections.Polyhydramnios can increase the risk of preterm labor, but it is not a consequence of it.
A nurse is teaching a pregnant client about pre-term labor.
Which activity should the nurse advise the client to avoid?
Explanation
Heavy lifting can increase the risk of preterm labor by putting stress on the uterus and cervix.
The nurse should advise the client to avoid heavy lifting and other strenuous activities during pregnancy.
Choice B is wrong because drinking plenty of fluids is important for pregnant women to prevent dehydration, which can also trigger preterm labor.
The nurse should encourage the client to drink at least eight glasses of water a day.
Choice C is wrong because taking prenatal vitamins is beneficial for pregnant women and their babies.Prenatal vitamins provide essential nutrients such as folic acid, iron, calcium, and vitamin D that support fetal growth and development.
The nurse should instruct the client to take prenatal vitamins as prescribed by their health care provider.
Choice D is wrong because reporting decrease in fetal movement is a sign of possible fetal distress or complications.The nurse should advise the client to monitor their baby’s movements and call their health care provider if they notice any changes or concerns.
A client at 34 weeks of gestation is at risk for pre-term labor.
Which instruction should the nurse include in the client's education?
Explanation
Perform fetal kick counts daily.
Fetal kick counts are a way of monitoring the baby’s well-being and detecting any signs of distress.They can also help identify preterm labor, as a decrease in fetal movement may indicate uterine contractions or placental insufficiency.
Choice B is wrong because strenuous exercise can increase the risk of preterm labor by causing dehydration, uterine irritability, or cervical changes.Women at risk for preterm labor should avoid vigorous physical activity and limit moderate exercise to 30 minutes per day.
Choice C is wrong because caffeine can stimulate uterine contractions and reduce blood flow to the placenta, which can lead to preterm labor or fetal growth restriction.Women at risk for preterm labor should limit their caffeine intake to less than 200 mg per day.
Choice D is wrong because participating in support groups may not have a direct effect on preventing preterm labor, although it may help reduce stress and anxiety, which are potential risk factors for preterm birth.Women at risk for preterm labor should seek emotional and social support from their health care providers, family, friends, or community resources.
A nurse is providing discharge teaching to a client who experienced pre-term labor.
Which statement by the client indicates understanding of the instructions?
Explanation
“I will report any decrease in fetal movement.” This statement indicates that the client understands the importance of monitoring fetal well-being and seeking medical attention if there are signs of fetal distress.Decreased fetal movement can indicate problems with the placenta, cord, or fetus that may require intervention.
Choice B is wrong because engaging in sexual intercourse can stimulate uterine contractions and increase the risk of preterm labor.
Women who have experienced preterm labor should avoid sexual activity until they reach term.
Choice C is wrong because breastfeeding a preterm infant can provide many benefits, such as reducing the risk of infection, enhancing bonding, and improving neurodevelopmental outcomes.
Women who have preterm infants should be encouraged and supported to breastfeed or express breast milk for their babies.
Choice D is wrong because ignoring signs or symptoms of preterm labor can lead to delayed treatment and increased complications for both mother and baby.Women who have experienced preterm labor should be educated about the warning signs of preterm labor, such as regular contractions, pelvic pressure, vaginal bleeding, fluid leakage, or low back pain, and instructed to call their healthcare provider or go to the hospital if they occur.
A nurse is instructing a client on how to recognize pre-term labor.
Which signs should the nurse include?
Explanation
Uterine contractions are a sign of preterm labor, which occurs when the cervix begins to open before 37 weeks of pregnancy.
Preterm labor can lead to premature birth and complications for the baby.
Choice B is wrong because increased fetal movement is not a sign of preterm labor.
Fetal movement may vary throughout pregnancy and does not indicate labor.
Choice C is wrong because urinary frequency is a common symptom of pregnancy, especially in the third trimester.
It is caused by the pressure of the growing uterus on the bladder and does not indicate labor.
Choice D is wrong because decreased vaginal discharge is not a sign of preterm labor.
In fact, some women may notice an increase in vaginal discharge or a change in its color or consistency as a sign of labor.This is called the mucus plug or bloody show and it means that the cervix is dilating and preparing for delivery.
Normal ranges for uterine contractions are about 10 to 15 minutes apart and last for 30 to 60 seconds.
If contractions are more frequent, regular, or painful, they may indicate preterm labor and require medical attention.
More questions on Preterm Labor
A client in pre-term labor is being discharged from the hospital.
What should the nurse include in the client's discharge plan?
Explanation
A. Referral to community services for support.
A client in preterm labor who is being discharged from the hospital needs to have a discharge plan that includes education, follow-up care, and support services.A referral to community services for support can help the client cope with the stress and anxiety of preterm labor, access resources such as home health care or social workers, and prevent complications or recurrence of preterm labor.
B. Encouragement to smoke in moderation is wrong because smoking is harmful for both the mother and the baby.
Smoking can increase the risk of preterm labor, low birth weight, placental abruption, and sudden infant death syndrome (SIDS).Smoking should be avoided completely during pregnancy and after delivery.
C. Instructions for heavy lifting and strenuous exercise is wrong because these activities can trigger uterine contractions and increase the risk of preterm labor.
A client in preterm labor should rest as much as possible and avoid physical exertion.The client should also avoid sexual intercourse, which can stimulate the cervix and cause bleeding or infection.
D. Recommendation to avoid kangaroo care is wrong because kangaroo care is a method of holding a newborn skin-to-skin with the mother or father.
Kangaroo care can have many benefits for preterm babies, such as improving temperature regulation, breathing, heart rate, feeding, bonding, and growth.Kangaroo care can also reduce stress and pain for both the baby and the parent.
A client in pre-term labor is being discharged from the hospital.
What should the nurse include in the client's discharge plan?
Explanation
A. Referral to community services for support.
Referral to community services for support is an important part of the discharge plan for a client in preterm labor.Community services can provide education, counseling, home visits, and other resources to help the client cope with preterm labor and prevent complications.
B. Encouragement to smoke in moderation.Statement is wrong because smoking is harmful for the unborn baby and can increase the risk of preterm labor.Smoking should be avoided completely during pregnancy and the client should be advised to quit or seek help to quit.
C. Instructions for heavy lifting and strenuous exercise.Statement is wrong because heavy lifting and strenuous exercise can trigger contractions and worsen preterm labor.The client should be instructed to rest as much as possible and avoid activities that may cause uterine irritation or bleeding.
D. Recommendation to avoid kangaroo care.Statement is wrong because kangaroo care, or skin-to-skin contact with the baby, is beneficial for both the mother and the baby after birth.Kangaroo care can help regulate the baby’s temperature, heart rate, breathing, and blood sugar levels, as well as promote bonding, breastfeeding, and infection prevention.The client should be encouraged to practice kangaroo care as soon as possible after delivery.
A nurse is preparing to administer betamethasone (Celestone) to a client who is at 31 weeks of gestation and has pre-term labor.
What is the purpose of this medication?
Explanation
To promote fetal lung maturity.Betamethasone (Celestone) is a type of corticosteroid that can help reduce the risk of respiratory distress syndrome and other complications in preterm infants by accelerating the development of their lungs.It is recommended for pregnant women between 24 0/7 weeks and 36 6/7 weeks of gestation who are at risk of preterm delivery within 7 days.
Choice A is wrong because betamethasone does not suppress uterine contractions.
It has no effect on the cause of preterm labor.
Choice B is wrong because betamethasone does not prevent infection.
It may actually increase the risk of infection by suppressing the immune system.
Choice D is wrong because betamethasone does not reduce maternal blood pressure.
It may actually cause hypertension and hyperglycemia as side effects.
A nurse is preparing to administer betamethasone (Celestone) to a client who is at 31 weeks of gestation and has pre-term labor.
What is the purpose of this medication?
Explanation
To promote fetal lung maturity.Betamethasone (Celestone) is a type of corticosteroid that can help reduce the risk of respiratory distress syndrome and other complications in preterm infants by accelerating the development of their lungs.It is recommended for pregnant women between 24 0/7 weeks and 36 6/7 weeks of gestation who are at risk of preterm delivery within 7 days.
Choice A is wrong because betamethasone does not suppress uterine contractions.
It has no effect on the cause of preterm labor.
Choice B is wrong because betamethasone does not prevent infection.
It may actually increase the risk of infection by suppressing the immune system.
Choice D is wrong because betamethasone does not reduce maternal blood pressure.
It may actually cause hypertension and hyperglycemia as side effects.
A nurse is monitoring a client who is at 29 weeks of gestation and has pre-term labor.
The client is receiving magnesium sulfate IV infusion.
Which of the following are expected adverse effects of this medication? (Select all that apply)
Explanation
Magnesium sulfate IV infusion can cause various adverse effects such asflushing,headache,nauseaanddrowsiness.
These are common and expected side effects of this medication.
Choice A is wrong because magnesium sulfate IV infusion does not causediarrhea.Diarrhea is a possible side effect of oral magnesium sulfate, which is used as a laxative.
However, oral magnesium sulfate is not used to treat pre-term labor or prevent seizures.
Normal ranges of magnesium in the blood are 1.7 to 2.2 mg/dL for adults.
Magnesium sulfate IV infusion is used to treat hypomagnesemia (low levels of magnesium in the blood) or to prevent seizures in pregnant women with pre-eclampsia, eclampsia or toxemia.
A nurse is teaching a client who is at 27 weeks of gestation and has pre-term labor about the signs and symptoms of true labor versus false labor.
Which of the following information should the nurse include in the teaching?
Explanation
True labor contractions cause cervical dilation and effacement.
This means that the cervix opens up and thins out to prepare for the baby’s passage through the birth canal.
Cervical changes can be measured by a pelvic exam.
Choice A is wrong because true labor contractions are regular and do not subside with rest.False labor contractions are irregular and may stop when you change position or activity level.
Choice B is wrong because false labor contractions are usually felt in the front of the abdomen, not in the lower back.True labor contractions may start in the back and radiate to the abdomen.
Choice D is wrong because false labor contractions do not increase in intensity with ambulation.True labor contractions may become stronger and closer together when you walk.
Normal ranges for cervical dilation and effacement vary depending on the stage of labor, but generally, full dilation is 10 cm and full effacement is 100%.
A nurse is caring for a client who is at 33 weeks of gestation and has pre-term labor.
The client reports a sudden gush of fluid from her vagina.
Which of the following actions should the nurse take first?
Explanation
Assess fetal heart rate and activity.
The nurse should identify that a client who reports a sudden gush of fluid from her vagina is at risk forpremature rupture of membranes (PROM), which can lead toinfection,cord prolapse, andfetal distress.Therefore, the priority action is to assess the fetal heart rate and activity to monitor for signs of hypoxia or distress.
Choice B is wrong because performing a nitrazine test on the fluid is not the first action.A nitrazine test can confirm the presence of amniotic fluid by detecting its alkaline pH, but it is not as urgent as assessing the fetal well-being.
Choice C is wrong because administering oxytocin (Pitocin) IV infusion is contraindicated in this situation.Oxytocin is used to induce or augment labor, but it can causeuterine hyperstimulation,fetal distress, andplacental abruptionif given to a client who has PROM.
Choice D is wrong because placing the client in Trendelenburg position is not recommended for a client who has PROM.Trendelenburg position can increase the risk ofcord prolapseandaspirationin this situation.
A nurse is planning discharge teaching for a client who is at 25 weeks of gestation and has pre-term labor that was successfully stopped with tocolytic therapy.
Which of the following instructions should the nurse include in the teaching?
Explanation
Report any increase in vaginal discharge to the provider.This is because an increase in vaginal discharge can indicate an infection, which can trigger preterm labor or cause complications for the mother and the baby.
Choice A is wrong because sexual intercourse is not contraindicated for women who have preterm labor that was successfully stopped with tocolytic therapy, unless they have other risk factors such as placenta previa or ruptured membranes.
Choice B is wrong because drinking at least 3 L of fluids per day is not necessary for women who have preterm labor that was successfully stopped with tocolytic therapy, unless they have dehydration or oligohydramnios.
Choice D is wrong because pelvic floor exercises are not recommended for women who have preterm labor that was successfully stopped with tocolytic therapy, as they can increase uterine activity and cause contractions.
Tocolytic therapy is the use of drugs to delay delivery for a short time (up to 48 hours) if a woman begins labor too early in her pregnancy.
The purpose of tocolytic therapy is to allow time for the administration of corticosteroids or other medicine.
A nurse is caring for a pregnant client at 36 weeks of gestation who reports low back pain and pelvic pressure.
Which intervention should the nurse implement first?
Explanation
Assess fetal heart rate using a Doppler device.
This is because low back pain and pelvic pressure at 36 weeks of gestation may indicate preterm labor, which can affect the fetal well-being.Therefore, the nurse should assess the fetal heart rate as a priority to determine if the fetus is in distress or not.
Choice A is wrong because tocolytic medication is used to stop uterine contractions, not to relieve low back pain and pelvic pressure.Choice B is wrong because resting in a side-lying position may help with blood circulation and reduce supine hypotensive syndrome, but it does not address the possible cause of low back pain and pelvic pressure.Choice D is wrong because assessing vaginal discharge for any change may indicate infection, rupture of membranes, or cervical dilation, but it is not as urgent as assessing fetal heart rate.
Some interventions for preventing and treating low back pain and pelvic pressure during pregnancy include exercise, water-based exercise, acupuncture, osteomanipulative therapy, craniosacral therapy, and pelvic support belts.
However, these interventions should be discussed with the health care provider before starting them.
A client at 28 weeks of gestation presents with bleeding from the vagina.
Which assessment finding should the nurse prioritize?
Explanation
Regular uterine contractions occurring every 15 minutes.
This finding suggests that the client may have placental abruption, which is a serious complication that requires immediate medical attention.Placental abruption is the premature separation of the placenta from the uterine wall, which can cause heavy bleeding, pain, and fetal distress.
Choice B is wrong because low back pain and pelvic pressure are common symptoms of preterm labor, which is not as urgent as placental abruption.
Choice C is wrong because a change in vaginal discharge is not a specific sign of any complication and may be normal in pregnancy.
Choice D is wrong because rupture of membranes is not a priority finding in this case, unless it is associated with infection or cord prolapse.
A nurse is caring for a client who is at 32 weeks of gestation and reports lower abdominal cramping.
Which of the following actions should the nurse take first?
Explanation
Assess the client’s vital signs.
The nurse should first assess the client’s vital signs to determine the severity of the situation and identify any signs of infection, bleeding, or shock.
The nurse should also monitor the fetal heart rate to assess fetal well-being.
Choice B is wrong because a sterile vaginal exam is not indicated for a client who reports lower abdominal cramping and may increase the risk of infection or rupture of membranes.
Choice C is wrong because administering tocolytic medication is not the first action the nurse should take.
Tocolytic medication may be used to inhibit uterine contractions and prolong pregnancy, but only after assessing the client’s and fetus’s condition and obtaining a prescription from the provider.
Choice D is wrong because monitoring the fetal heart rate is not the first action the nurse should take.
Monitoring the fetal heart rate is important to assess fetal well-being, but it does not take priority over assessing the client’s vital signs.
A nurse is teaching a client who is at risk for pre-term labor about the signs and symptoms to report to the provider.
Which of the following should the nurse include in the teaching?
Explanation
All of the above.The nurse should include all of these signs and symptoms in the teaching as they may indicate pre-term labor.Pre-term labor occurs when regular contractions begin to open the cervix before 37 weeks of pregnancy.
Choice A is wrong because decreased fetal movement is not a normal sign of pre-term labor, but it may indicate fetal distress or other complications.
Choice B is wrong because increased vaginal discharge is not a normal sign of pre-term labor, but it may indicate infection or rupture of membranes.
Choice C is wrong because pelvic pressure is not a normal sign of pre-term labor, but it may indicate cervical dilation or descent of the fetus.
A nurse is reviewing the medical record of a client who is at 34 weeks of gestation and has pre-term labor.
Which of the following findings is a risk factor for pre-term labor?
Explanation
History of urinary tract infections.According to the Mayo Clinic, untreated vaginal infections, such as urinary tract infections or sexually transmitted infections, are risk factors for preterm labor.
These infections can cause inflammation and irritation of the cervix, which can trigger contractions and cervical dilation.
Choice B is wrong because maternal age of 25 years is not a risk factor for preterm labor.In fact, women younger than 18 or older than 35 are more likely to have a preterm delivery.
Choice C is wrong because singleton pregnancy is not a risk factor for preterm labor.On the contrary, being pregnant with twins, triplets, or more (called "multiple gestations") is associated with a higher risk of preterm labor and birth.
Choice D is wrong because cervical length of 3 cm is not a risk factor for preterm labor.A short cervix (less than 2.5 cm) or a cervix that shortens in the second trimester instead of the third trimester is a risk factor for preterm delivery.A normal cervical length ranges from 3 to 5 cm during pregnancy.
A nurse is admitting a client who is at 30 weeks of gestation and has pre-term labor.
Which of the following medications should the nurse anticipate administering to prevent fetal respiratory distress syndrome?
Explanation
Betamethasone is a corticosteroid that is given to pregnant women who are at risk of preterm delivery to enhance fetal lung maturity and prevent respiratory distress syndrome.It is usually given in two doses, 24 hours apart, and takes effect within 24 hours of administration.
Choice B.Magnesium sulfate is wrong because it is used to prevent seizures in women with severe preeclampsia or eclampsia, not to prevent respiratory distress syndrome.
Choice C.Nifedipine is wrong because it is a calcium channel blocker that is used to inhibit uterine contractions and prolong pregnancy in women with preterm labor, not to prevent respiratory distress syndrome.
Choice D.Indomethacin is wrong because it is a nonsteroidal anti-inflammatory drug that is used to inhibit prostaglandin synthesis and reduce uterine activity in women with preterm labor, not to prevent respiratory distress syndrome.However, it can also cause premature closure of the ductus arteriosus in the fetus and should be avoided after 32 weeks of gestation.
Normal ranges for gestational age are 37 to 42 weeks.
Preterm labor is defined as regular uterine contractions with cervical changes.
A nurse is evaluating a client who is at 28 weeks of gestation and has pre-term labor.
Which of the following findings indicates that the client’s condition is improving?
Explanation
Decreased frequency and intensity of contractions indicates that the client’s condition is improving.Preterm labor occurs when regular contractions result in the opening of your cervix before 37 weeks of pregnancy.
If preterm labor can’t be stopped, your baby will be born early and may have health problems.
Choice B is wrong because increased cervical dilation and effacement means that the cervix is thinning and opening more, which are signs of labor progression.
Choice C is wrong because increased amount and color of vaginal discharge may indicate infection, bleeding, or rupture of membranes, which are complications of preterm labor.
Choice D is wrong because decreased fetal heart rate variability means that the baby’s heart rate is not changing much, which may indicate fetal distress or hypoxia.A normal fetal heart rate variability is between 6 and 25 beats per minute.
A nurse is providing discharge instructions to a client who had pre-term labor at 32 weeks of gestation and was prescribed bed rest at home.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
“I will call my doctor if I have more than four contractions in an hour.” This statement indicates that the client understands the signs of preterm labor and when to seek medical attention.Preterm labor is defined as having regular contractions and cervical changes before 37 weeks of gestation.More than four contractions in an hour may indicate that preterm labor is occurring and requires prompt evaluation.
Choice A is wrong because drinking at least eight glasses of water every day is not a specific instruction for preventing preterm labor.However, dehydration can trigger contractions and should be avoided.
Choice B is wrong because lying on the back with a pillow under the knees can reduce blood flow to the uterus and the baby.This position can also increase the risk of blood clots in the legs.A better position is lying on the left side, which improves circulation and reduces pressure on the cervix.
Choice C is wrong because avoiding sexual intercourse until reaching term is not necessary for most women with a history of preterm labor.Sexual activity does not cause preterm labor or premature rupture of membranes (PROM).However, some women may be advised to abstain from sex if they have certain conditions, such as placenta previa or a short cervix.
A nurse is caring for a client who is at 33 weeks of gestation and has pre-term labor that has not responded to tocolytic therapy.
The client’s cervix is dilated to 4 cm and she is experiencing regular contractions every 3 minutes.
Which of the following interventions should the nurse include in the plan of care?
Explanation
Prepare for an emergency cesarean section.This is because the client has pre-term labor that has not responded to tocolytic therapy, which are drugs that are used to delay delivery for a short time.The client’s cervix is dilated to 4 cm and she is experiencing regular contractions every 3 minutes, which are signs of active labor.The baby is at 33 weeks of gestation, which is premature and may have complications such as respiratory distress syndrome or bleeding in the brain.
Therefore, the client needs an emergency cesarean section to deliver the baby as soon as possible and prevent further risks.
Choice A is wrong because administering magnesium sulfate intravenously is a type of tocolytic therapy that the client has already failed.Magnesium sulfate may also have side effects such as nausea, vomiting, flushing, headache, and muscle weakness.
Choice C is wrong because placing the client in Trendelenburg position, which is lying on the back with the feet elevated above the head, is not recommended for preterm labor.This position may increase the risk of aspiration, decrease cardiac output, and impair gas exchange.
Choice D is wrong because administering antibiotics prophylactically is not indicated for preterm labor unless there is evidence of infection in the uterus or membranes.
Antibiotics may also cause allergic reactions or bacterial resistance
A nurse is administering terbutaline to a client who is at 31 weeks of gestation and has pre-term labor.
Which of the following findings should the nurse monitor as an adverse effect of this medication?
Explanation
Tachycardia.
Terbutaline is a medication that can be used to stop or delay preterm labor by relaxing the uterine muscles.However, it can also cause serious side effects for both the mother and the baby.One of the most common side effects of terbutaline is tachycardia, which means a fast or irregular heartbeat.This can lead to chest pain, palpitations, shortness of breath, and even cardiac arrhythmias or ischemia.
Therefore, the nurse should monitor the mother’s heart rate and rhythm closely when administering terbutaline.
Choice A is wrong because terbutaline does not cause hypotension, which means low blood pressure.In fact, terbutaline can increase blood pressure by constricting blood vessels.
Choice C is wrong because terbutaline does not cause hyperglycemia, which means high blood sugar.However, terbutaline can interfere with insulin secretion and glucose metabolism in some cases, especially in diabetic mothers.
Therefore, the nurse should monitor the mother’s blood sugar levels when administering terbutaline.
Choice D is wrong because terbutaline does not cause hypokalemia, which means low potassium levels in the blood.However, terbutaline can cause a temporary increase in potassium levels in the baby, which can affect the baby’s heart function.
Therefore, the nurse should monitor the baby’s heart rate and rhythm when administering terbutaline.
Normal ranges for heart rate are 60 to 100 beats per minute for adults and 120 to 160 beats per minute for fetuses.
Normal ranges for blood pressure aretypically between 90/60 mmHg and 120/80 mmHg.
A nurse is caring for a client who is at 35 weeks of gestation and has pre-term labor with intact membranes and no signs of infection.
The provider prescribes indomethacin to inhibit prostaglandin synthesis and suppress uterine contractions.
Which of the following laboratory tests should the nurse monitor while the client is receiving this medication?
Explanation
Creatinine clearance.
Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) that inhibits prostaglandin synthesis and suppresses uterine contractions.However, it can also causerenal failurein the fetus and the mother by reducing renal blood flow and glomerular filtration rate.
Therefore, the nurse should monitor the creatinine clearance, which is a measure of renal function, while the client is receiving this medication.
Choice A is wrong because indomethacin does not affect platelet count or coagulation.
Choice C is wrong because indomethacin does not affect liver function tests.
Choice D is wrong because indomethacin does not affect blood glucose levels.
Normal ranges for creatinine clearance are 88-128 mL/min for women and 97-137 mL/min for men.Normal ranges for platelet count are 150,000-450,000 cells/mm3.
Normal ranges for liver function tests vary depending on the specific test, but some common ones are: alanine aminotransferase (ALT) 7-55 U/L, aspartate aminotransferase (AST) 8-48 U/L, alkaline phosphatase (ALP) 45-115 U/L, total bilirubin 0.1-1.2 mg/dL.
A nurse is assessing a client for pre-term labor.
Which diagnostic test should the nurse anticipate being ordered for this client?
Explanation
Ultrasound.
An ultrasound can help determine the gestational age, fetal growth, placental location, and amniotic fluid volume of the fetus.
These factors can affect the risk of pre-term labor and delivery.
An ultrasound can also detect cervical changes that may indicate pre-term labor.
Choice B is wrong because a blood count is not specific for pre-term labor.
It may be done to check for anemia, infection, or other conditions that may affect the pregnancy, but it does not directly assess the risk of pre-term labor.
Choice C is wrong because a urine culture is not specific for pre-term labor.
It may be done to check for urinary tract infection, which can cause pre-term labor, but it does not directly assess the risk of pre-term labor.
Choice D is wrong because an amniocentesis is not usually done for pre-term labor.
It may be done to check for fetal lung maturity, chromosomal abnormalities, or infections, but it is an invasive procedure that carries some risks and complications.
It does not directly assess the risk of pre-term labor.
A nurse is assessing a client for pre-term labor.
Which assessment finding would be most concerning and require immediate intervention?
Explanation
Infection on speculum examination.
Infection is a major cause of preterm labor and can lead to serious complications for the mother and the fetus.
Infection can be detected by a speculum examination that shows signs of inflammation, such as erythema, edema, discharge, or odor.
Infection can also be confirmed by laboratory tests, such as culture, gram stain, or polymerase chain reaction.Infection should be treated promptly with antibiotics and other supportive measures.
Choice B. Bleeding on speculum examination is wrong because bleeding is not a direct cause of preterm labor, but rather a sign of other conditions that may increase the risk of preterm labor, such as placenta previa, placental abruption, or cervical trauma.Bleeding should be evaluated further to determine the source and severity of the hemorrhage and to manage any complications.
Choice C. Positive fetal fibronectin test (FFN) is wrong because a positive FFN test indicates the presence of fetal fibronectin in the cervical or vaginal secretions, which is a marker of increased risk of preterm labor, but not a definitive marker.
A nurse is caring for a client who is at 32 weeks of gestation and has signs of pre-term labor.
Which of the following tests should the nurse anticipate to confirm ROM?
Explanation
Nitrazine paper test.
This test involves putting a drop of fluid obtained from the vagina onto paper strips containing nitrazine dye.
The strips change color depending on the pH of the fluid.The strips will turn blue if the pH is greater than 6.0, which indicates the presence of amniotic fluid.This test can help confirm rupture of membranes (ROM) in pregnancy, especially when preterm labor is suspected.
Choice B. Ferning test.This test involves examining a sample of vaginal fluid under a microscope and looking for a fern-like pattern that is formed by dried amniotic fluid crystals.This test can also help confirm ROM, but it is less reliable than the nitrazine test because other substances such as cervical mucus, semen, or blood can also cause ferning.
Choice C. Amniotic fluid index.This test involves measuring the amount of amniotic fluid in the uterus using ultrasound.This test can help assess the fetal well-being and detect conditions such as oligohydramnios (low amniotic fluid) or polyhydramnios (high amniotic fluid).This test cannot confirm ROM by itself, but it can be used in combination with other tests to evaluate the status of the pregnancy.
Choice D. Biophysical profile.This test involves using ultrasound and a fetal monitor to assess the fetal heart rate, breathing, movement, muscle tone, and amniotic fluid volume.
A nurse is reviewing the history of a client who is at 28 weeks of gestation and has pre-term labor.
Which of the following factors increases the risk of pre-term labor?
Explanation
A cervical cerclage is a procedure that involves placing stitches around the cervix to prevent it from opening prematurely.This procedure is usually done for women who have a history of cervical insufficiency or a short cervix, which are risk factors for preterm labor.
Choice A is wrong because history of gestational diabetes is not a risk factor for preterm labor.
Gestational diabetes is a condition that causes high blood sugar during pregnancy and can affect the health of the mother and the baby, but it does not increase the risk of preterm labor.
Choice C is wrong because history of recurrent urinary tract infections (UTIs) is a risk factor for preterm labor.
UTIs are infections that affect the urinary system and can cause symptoms such as pain, burning, or frequent urination.
UTIs can also spread to the kidneys or the uterus and cause inflammation or infection that can trigger preterm labor.
Choice D is wrong because history of assisted reproductive technology (ART) is a risk factor for preterm labor.
ART refers to any medical procedure that helps with conception, such as in vitro fertilization (IVF).
ART can increase the risk of preterm labor because it can result in multiple gestations (twins, triplets, or more), which put more strain on the uterus and can cause it to contract prematurely.ART can also cause complications such as placenta previa or rupture of the uterus, which can lead to preterm labor.
A nurse is performing a digital examination on a client who is at 34 weeks of gestation and has pre-term labor.
Which of the following findings indicates cervical effacement?
Explanation
Cervix is shortened and thinned.This indicates cervical effacement, which is the thinning and softening of the cervix in preparation for childbirth.Cervical effacement is measured in percentages, from 0% (no effacement) to 100% (fully effaced).
Choice A is wrong because cervix is soft and pliable does not necessarily mean it is effaced.The cervix can soften before it thins and shortens.
Choice C is wrong because cervix is dilated and open indicates cervical dilation, which is the opening of the cervix.Cervical dilation is measured in centimeters, from 0 cm (closed) to 10 cm (fully dilated).
Cervical dilation and effacement are related, but not the same.
Choice D is wrong because cervix is posterior and high indicates the position of the cervix in relation to the vagina.The cervix can move from posterior (back) to anterior (front) and from high to low as labor progresses.
The position of the cervix does not indicate effacement.
A nurse is reviewing the laboratory results of a client who is at 29 weeks of gestation and has pre-term labor.
Which of the following results indicates an infection that can trigger pre-term labor?
Explanation
A white blood cell count of 12,000/mm3 indicates an infection that can trigger pre-term labor.The normal range for white blood cell count in pregnancy is 5.7-15.0×10 9 /L, which is equivalent to 5,700-15,000/mm3.
A count above this range suggests an inflammatory response to an infection.
Choice B is wrong because a hemoglobin level of 11 g/dL is within the normal range for pregnancy, which is 10-14 g/dL.
Choice C is wrong because a platelet count of 250,000/mm3 is within the normal range for pregnancy, which is 150,000-400,000/mm3.
Choice D is wrong because a blood glucose level of 90 mg/dL is within the normal range for pregnancy, which is 70-110 mg/dL.
A nurse is reviewing the ultrasound report of a client who is at 31 weeks of gestation and has pre-term labor.
Which of the following findings indicates oligohydramnios?
Explanation
Amniotic fluid index of 4 cm indicates oligohydramnios, which means too little amniotic fluid.This can cause fetal growth restriction, cord compression, and congenital anomalies.
Choice B is wrong because amniotic fluid index of 8 cm is within the normal range of 5 to 25 cm.
Choice C is wrong because amniotic fluid index of 12 cm is also within the normal range and close to the median value of 14 cm.
Choice D is wrong because amniotic fluid index of 16 cm is also within the normal range and does not indicate oligohydramnios.
A nurse is preparing to perform an amniocentesis on a client who is at 27 weeks of gestation and has pre-term labor.
Which of the following actions should the nurse take before the procedure?
Explanation
Instruct the client to empty her bladder.This is because a full bladder can interfere with the insertion of the needle and increase the risk of injury to the bladder or the uterus.Emptying the bladder also reduces discomfort during the procedure.
Choice A is wrong because administering tocolytic medication to stop contractions is not necessary before amniocentesis.Tocolytic medication can have side effects and should only be used when there is a clear indication of preterm labor.
Choice C is wrong because obtaining informed consent from the client is not a nursing action, but a medical one.The nurse can assist in providing information and answering questions, but the final consent should be obtained by the doctor who will perform the procedure.
Choice D is wrong because monitoring fetal heart rate and activity is not a specific action before amniocentesis, but a routine part of prenatal care.Fetal heart rate and activity can be affected by many factors, such as maternal position, fetal sleep cycle, or maternal blood sugar level.
Monitoring them before amniocentesis does not provide any useful information for the procedure.
A nurse is teaching a client who is at 25 weeks of gestation and has pre-term labor about the purpose and side effects of magnesium sulfate therapy.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
This medication will help relax my uterus and stop contractions.
Magnesium sulfate is a tocolytic, a medication used to suppress uterine contractions and delay preterm delivery.The exact mechanism through which magnesium sulfate inhibits contractions is unknown, but researchers believe it likely works by lowering calcium levels in the uterine muscles.
Choice A is wrong because magnesium sulfate is not used to prevent seizures in case of preeclampsia.
Preeclampsia is a condition characterized by high blood pressure and protein in the urine during pregnancy.Magnesium sulfate may be used to treat seizures if they occur with eclampsia, which is a severe complication of preeclampsia.
Choice B is wrong because magnesium sulfate does not help mature the baby’s lungs in case of preterm birth.
Magnesium sulfate may have some neuroprotective effects for the baby, but it does not affect lung development.Steroids are usually given to pregnant women at risk of preterm delivery to help accelerate fetal lung maturation.
Choice D is wrong because magnesium sulfate does not lower blood pressure in case it gets too high.
Magnesium sulfate may have some vasodilatory effects, but it is not used as an antihypertensive agent.Other medications, such as hydralazine or labetalol, are used to treat high blood pressure during pregnancy.
A client at 30 weeks of gestation is experiencing pre-term labor.
Which intervention should the nurse anticipate to suppress uterine contractions?
Explanation
Tocolytics are a category of drugs used to delay the labor process.These may be used in situations when a pregnant person begins showing signs of preterm labor —which is any time before 37 weeks of completed pregnancy.Tocolytics may help delay labor by two to seven days.
Some possible explanations for the other choices are:
• Choice A. Administering intravenous fluids.
This is not a correct answer because intravenous fluids are not effective in suppressing uterine contractions.They may be used to correct dehydration or electrolyte imbalance, which can sometimes trigger preterm labor, but they are not a primary intervention for preterm labor.
• Choice C. Administering corticosteroids.
This is not a correct answer because corticosteroids are not tocolytics.They do not stop or slow down uterine contractions, but they help accelerate fetal lung maturity and reduce the risk of neonatal respiratory distress syndrome and other complications of prematurity.
Corticosteroids are often given along with tocolytics, but they have a different function and mechanism of action.
• Choice D. Administering antibiotics.
This is not a correct answer because antibiotics are not tocolytics.They may be used to treat infections that can cause or complicate preterm labor, such as chorioamnionitis or group B streptococcus, but they do not directly affect uterine contractions.
Antibiotics may be given along with tocolytics, but they have a different function.
A nurse is providing education to a client and her partner about pre-term labor.
Which intervention should the nurse include in the teaching plan to address possible outcomes and complications?
Explanation
Corticosteroids are given to pregnant women who are at risk of preterm labor to help mature the lungs of the fetus and reduce the risk of respiratory distress syndrome and other complications.Corticosteroids also have a protective effect on the brain and reduce the risk of bleeding and cerebral palsy.
Choice A is wrong because administering intravenous fluids is not a specific intervention to address possible outcomes and complications of preterm labor.Intravenous fluids may be given to correct dehydration or electrolyte imbalance, but they do not prevent or treat preterm labor.
Choice B is wrong because administering tocolytics is an intervention to delay preterm labor, not to address possible outcomes and complications.
Tocolytics are drugs that inhibit uterine contractions and prolong pregnancy for a short period of time, usually 24 to 48 hours, to allow for the administration of corticosteroids or the transfer of the mother to a facility with neonatal intensive care.
A nurse is monitoring a client who is receiving terbutaline for pre-term labor.
Which of the following findings should the nurse report to the provider as a potential adverse effect of the medication?
Explanation
Terbutaline can cause low potassium levels in the blood, which can lead to muscle weakness, cramps, and cardiac arrhythmias.
This is a potential adverse effect of the medication that should be reported to the provider.
Choice A is wrong because tachycardia is a common side effect of terbutaline that does not usually require medical attention.
Terbutaline works by stimulating beta-adrenergic receptors, which can increase the heart rate.
Choice B is wrong because hypotension is not a typical side effect of terbutaline.Terbutaline can actually cause elevated blood pressure in some cases.
Choice C is wrong because hyperglycemia is not a common side effect of terbutaline.Terbutaline can cause transient hyperglycemia in pregnant women, but this is not a reason to stop the medication.
Normal ranges for potassium are 3.5-5.0 mEq/L and for blood glucose are 70-110 mg/dL.
A nurse is administering betamethasone to a client who is in pre-term labor at 28 weeks of gestation.
The nurse should explain that the purpose of this medication is to:
Explanation
Betamethasone is a corticosteroid that is given to pregnant women who are at risk of preterm delivery to enhance fetal lung maturity.Betamethasone stimulates the production of surfactant, a substance that lubricates the lungs and prevents them from collapsing when the baby breathes.This reduces the risk of respiratory distress syndrome and other complications in preterm infants.
Choice A is wrong because betamethasone does not reduce inflammation in the uterus.
Choice C is wrong because betamethasone does not prevent infection in the amniotic fluid.
Choice D is wrong because betamethasone does not increase blood flow to the placenta.
Normal ranges for gestational age are 37 to 42 weeks.
Preterm birth is defined as delivery before 37 weeks of gestation.Antenatal corticosteroids are recommended for women between 24 and 34 weeks of gestation who are at risk of preterm delivery within 7 days, and may be considered for women at 23 weeks of gestation or between 34 and 37 weeks of gestation depending on the clinical scenario.
A nurse is reviewing the laboratory results of a client who is in pre-term labor and has received indomethacin.
Which of the following findings should the nurse monitor for as a potential complication of the medication?
Explanation
Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) that can cause renal impairment and elevated serum creatinine levels in both the mother and the fetus.This can lead to oligohydramnios, reduced fetal urine output, and fetal renal failure.
Therefore, the nurse should monitor the serum creatinine levels of the client and the fetus as a potential complication of indomethacin.
Choice A is wrong because indomethacin does not affect the platelet count.It may increase the risk of bleeding due to its antiplatelet effect, but it does not cause thrombocytopenia.
Choice C is wrong because indomethacin does not cause anemia or decrease the hematocrit.It may cause gastrointestinal bleeding or ulceration, which could lead to anemia, but this is not a common or direct effect of the medication.
Choice D is wrong because indomethacin does not cause hyperkalemia or increase the serum potassium levels.It may cause hyponatremia due to its effect on renal sodium excretion, but it does not affect potassium balance.
A nurse is caring for a client who is receiving magnesium sulfate for pre-term labor.
Which of the following assessments should the nurse perform to evaluate the therapeutic effect of the medication?
Explanation
The therapeutic effect of magnesium sulfate is to inhibit uterine contractions and prevent or delay preterm labor.
By assessing uterine activity, the nurse can evaluate if the medication is working or not.
Choice A is wrong because measuring urine output is not directly related to the therapeutic effect of magnesium sulfate, but rather to monitor for toxicity and renal function.
Choice B is wrong because checking deep tendon reflexes is also not directly related to the therapeutic effect of magnesium sulfate, but rather to monitor for neuromuscular effects and toxicity.
Choice D is wrong because monitoring blood pressure is not directly related to the therapeutic effect of magnesium sulfate, but rather to monitor for cardiovascular effects and toxicity.
A nurse is preparing to administer nifedipine to a client who is in pre-term labor.
The nurse should withhold the medication and notify the provider if the client has which of the following conditions?
Explanation
Nifedipine is a calcium channel blocker that is used to relax uterine contractions and postpone preterm labor.However, it can also lower blood pressure and cause side effects such as headache, dizziness, flushing, and palpitations.Therefore, it should be avoided in clients who have cardiac disease or other conditions that affect the heart function.
Choice A is wrong because asthma is not a contraindication for nifedipine.Nifedipine does not affect the airways or cause bronchospasm.
Choice B is wrong because diabetes mellitus is not a contraindication for nifedipine.Nifedipine does not affect blood glucose levels or insulin secretion.
Choice C is wrong because hypertension is not a contraindication for nifedipine.In fact, nifedipine can be used to treat high blood pressure as well as preterm labor.However, blood pressure should be monitored closely during nifedipine therapy to avoid hypotension.
A nurse is educating a client who is at risk for pre-term labor about measures to prevent it from occurring.
Which of the following instructions should the nurse include?
Explanation
Drinking enough water can help prevent dehydration, which can trigger preterm labor contractions.Dehydration can also cause low amniotic fluid levels, which can affect fetal growth and development.
Choice A is wrong because avoiding sexual intercourse until term is not necessary for most women at risk for preterm labor.Sexual activity does not cause preterm labor unless there are other complications, such as placenta previa or cervical insufficiency.
Choice C is wrong because lying down when feeling contractions may not stop preterm labor.If a woman has regular contractions that cause cervical change, she should seek medical attention as soon as possible.Lying down may also reduce blood flow to the uterus and placenta, which can affect fetal oxygenation.
Choice D is wrong because taking aspirin for pelvic pain is not recommended for pregnant women.Aspirin can increase the risk of bleeding and affect fetal blood circulation.
Pelvic pain may be a sign of preterm labor or other complications, so it should be evaluated by a health care provider
A nurse is reviewing the medication history of a client who is in pre-term labor and has a history of peptic ulcer disease.
The nurse should recognize that which of the following medications is contraindicated for this client?
Explanation
Indomethacin is contraindicated for this client because it is a nonsteroidal anti-inflammatory drug (NSAID) that can irritate or inflame the lining of the stomach and small intestine.This can worsen the client’s peptic ulcer disease, which is a condition where open sores develop on the inner surface of the stomach or small intestine due to acid erosion.
Indomethacin can also interact with other medications that the client may be taking for pre-term labor or peptic ulcer disease.
Choice A is wrong because magnesium sulfate is not contraindicated for this client.It is a medication that can relax the smooth muscles of the uterus and prevent pre-term labor contractions.
Choice B is wrong because betamethasone is not contraindicated for this client.It is a corticosteroid that can help mature the fetal lungs and reduce the risk of respiratory distress syndrome in pre-term infants.
Choice D is wrong because terbutaline is not contraindicated for this client.
A nurse is evaluating the fetal heart rate tracing of a client who is in pre-term labor and receiving magnesium sulfate.
The nurse should identify that which of the following patterns indicates a potential adverse effect of the medication on the fetus?
Explanation
According to the search results, magnesium sulfate can have a negative effect on the fetal heart rate (FHR) by lowering the baseline, decreasing the variability, and reducing the reactivity or acceleration pattern.Absent variability means that there is no fluctuation in the FHR and it indicates fetal hypoxia or acidosis.
This is a potential adverse effect of magnesium sulfate on the fetus and requires immediate intervention.
Choice A.Accelerations is wrong because accelerations are transient increases in the FHR that indicate fetal well-being.They are not affected by magnesium sulfate.
Choice B.Early decelerations is wrong because early decelerations are decreases in the FHR that occur with uterine contractions and are caused by fetal head compression.They are benign and do not indicate fetal distress.They are not associated with magnesium sulfate.
Choice C.Variable decelerations is wrong because variable decelerations are abrupt decreases in the FHR that vary in shape, duration, and timing and are caused by umbilical cord compression.
They may or may not indicate fetal compromise.
A nurse is caring for a client who is in pre-term labor and receiving magnesium sulfate therapy.
The nurse should monitor the client for which of the following adverse effects of magnesium sulfate?
Explanation
Magnesium sulfate is a drug that is used to prevent seizures associated with pre-eclampsia and to stop preterm labor.However, it can also cause adverse effects such as respiratory depression, which is a condition where the breathing rate becomes too slow and shallow.
Respiratory depression can be life-threatening for both the mother and the baby, so the nurse should monitor the client’s respiratory rate and oxygen saturation closely.
Choice A is wrong because magnesium sulfate can cause hypotension, not hypertension.Hypotension is low blood pressure, which can lead to dizziness, fainting, and shock.
Choice B is wrong because magnesium sulfate can cause hyporeflexia, not hyperreflexia.Hyporeflexia is a reduced or absent reflex response, which can indicate magnesium toxicity.
The nurse should check the client’s deep tendon reflexes regularly and stop the infusion if they are absent.
Choice D is wrong because magnesium sulfate can cause bradycardia, not tachycardia.
Bradycardia is a slow heart rate, which can reduce the blood flow to vital organs.
A nurse is planning care for a pre-term infant who is in an incubator.
Which of the following interventions should the nurse include to promote bonding between the infant and the parents?
Explanation
Encouraging the parents to touch and talk to the infant through the incubator ports can promote bonding between the infant and the parents.Bonding is the intense attachment that develops between parents and their baby, and it is essential for the baby’s social and cognitive development.Touch and communication are some of the ways that babies bond with their parents.
Choice B is wrong because limiting the parents’ visitation time can disrupt the bonding process and make the parents feel less involved in their baby’s care.
Choice C is wrong because eye contact is another way of bonding with babies, and it can help them feel secure and loved.
Choice D is wrong because holding and feeding the infant are also important ways of bonding, and they should not be restricted unless medically necessary.
A nurse is caring for a client who is experiencing pre-term labor at 32 weeks of gestation and has been prescribed betamethasone.
Which of the following outcomes should the nurse expect from this medication?
Explanation
It will increase fetal lung maturity.
Betamethasone is a type of corticosteroid that is given to pregnant women who are at risk of preterm delivery between 24 and 34 weeks of gestation.It helps to improve neonatal outcomes by reducing the incidence of respiratory distress syndrome and other complications.Betamethasone works by stimulating the production and release of surfactant, a substance that lubricates the lungs and prevents them from collapsing when the baby breathes.
Choice A is wrong because betamethasone does not affect maternal blood pressure.
Choice C is wrong because betamethasone does not reduce uterine contractions.
Choice D is wrong because betamethasone does not prevent neonatal infection.
A nurse is assessing a client who is in pre-term labor and has received one dose of terbutaline subcutaneously.
Which of the following findings should the nurse report to the provider?
Explanation
Blood pressure of 150/90 mmHg.This is because terbutaline can causeelevated blood pressureas a side effect.
The nurse should report this finding to the provider as it may indicate hypertension or a hypertensive crisis.
Choice A is wrong because a heart rate of 110/min is not abnormal for a person who has received terbutaline.Terbutaline can causefast or pounding heartbeatsas a common side effect.
Choice C is wrong because a blood glucose of 90 mg/dL is within the normal range of 70-130 mg/dL before meals.Terbutaline can causetransient hyperglycemia(high blood sugar) as a serious side effect, but this is not the case here.
Choice D is wrong because a temperature of 37°C (98.6°F) is normal for a human being.Terbutaline does not cause fever or hypothermia as a side effect.
A nurse is evaluating the understanding of a client who is at risk for pre-term labor and has been instructed to perform daily home uterine activity monitoring (HUAM).
Which of the following statements by the client indicates a need for further teaching?
Explanation
Lying on one’s back with knees bent while using the monitor is not recommended for women at risk of preterm labor, as it can put pressure on the inferior vena cava, a major vein leading back to the heart.This can cause low blood pressure and reduce blood flow to the uterus and the baby.A better position is to lie on one’s side with a pillow at the back for support.
Choice A is correct because emptying the bladder before applying the monitor can reduce interference from urine contractions and make the readings more accurate.
Choice C is correct because pressing the event marker every time one feels a contraction can help record the frequency and duration of uterine activity.
Choice D is correct because using the monitor for at least 1 hour twice a day can provide sufficient data on uterine contractions and help detect early signs of preterm labor.
A nurse is admitting a client who is in pre-term labor at 34 weeks of gestation and has ruptured membranes and oligohydramnios.
Which of the following actions should the nurse take first?
Explanation
This is because assessing fetal heart rate is the most important action to take first when a client has prelabor rupture of membranes (PROM) at 34 weeks of gestation and oligohydramnios.Fetal heart rate can indicate fetal well-being, distress, or infection.Oligohydramnios can increase the risk of umbilical cord compression and fetal hypoxia.
Choice A is wrong because administering IV fluids is not the first priority in this situation.IV fluids may be given to prevent dehydration, enhance uterine blood flow, or augment labor, but they are not as urgent as assessing fetal heart rate.
Choice B is wrong because obtaining a urine specimen is not the first priority in this situation.A urine specimen may be obtained to check for infection, proteinuria, or glucose levels, but they are not as urgent as assessing fetal heart rate.
Choice D is wrong because inserting an indwelling urinary catheter is not the first priority in this situation.An indwelling urinary catheter may be inserted to monitor fluid balance, prevent bladder distension, or reduce the risk of infection, but they are not as urgent as assessing fetal heart rate.
Normal ranges for fetal heart rate are 110 to 160 beats per minute.Oligohydramnios is defined as an amniotic fluid index of less than 5 cm.
A nurse is providing education to a client who had pre-term labor and was prescribed indomethacin.
Which of the following information should the nurse include in the teaching?
Explanation
“This medication can cause premature closure of your baby’s ductus arteriosus.”
Indomethacin is a NSAID that can prevent the synthesis of prostaglandins, which are involved in preterm contractions.However, it can also cause constrictive effects on the fetal ductus arteriosus, which can lead to cardiac complications and oligohydramnios.The dosage and duration of indomethacin treatment should be carefully monitored.
Choice B is wrong because indomethacin does not increase the risk of postpartum hemorrhage.In fact, it may reduce the risk of bleeding by inhibiting platelet aggregation.
Choice C is wrong because indomethacin does not cause jaundice in the baby.
Jaundice is caused by high levels of bilirubin in the blood, which can be due to various factors such as blood group incompatibility, infection, or liver problems.
Choice D is wrong because indomethacin does not increase blood pressure during labor.It may actually lower blood pressure by dilating blood vessels.
Normal ranges for indomethacin dosage are 25 to 50 mg orally every 6 hours or 100 mg rectally every 12 hours for up to 48 hours.
Normal ranges for fetal ductus arteriosus diameter are 1.5 to 4 mm before 28 weeks of gestation and 1 to 3 mm after 28 weeks of gestation.
A nurse is caring for a client who is in pre-term labor.
Which of the following maternal complications is most likely to occur due to prolonged bed rest?
Explanation
Thromboembolism.
Prolonged bed rest increases the risk of venous stasis and blood clot formation in the lower extremities, which can lead to pulmonary embolism if the clot dislodges and travels to the lungs.
This is a life-threatening complication that requires immediate treatment.
Choice B. Placental abruption is wrong because it is not caused by bed rest, but by trauma, hypertension, cocaine use, or other factors that can cause the placenta to separate from the uterine wall.
Choice C. Uterine atony is wrong because it is not caused by bed rest, but by overdistension of the uterus, prolonged labor, infection, or other factors that can impair the contraction of the uterine muscles after delivery.
Choice D. Infection is wrong because it is not caused by bed rest, but by poor hygiene, invasive procedures, or other factors that can introduce microorganisms into the reproductive tract.
Normal ranges for maternal heart rate are 60-100 beats per minute and blood pressure are 110-140/60-90 mm Hg.
Normal range for fetal heart rate is 110-160 beats per minute.
A nurse is assessing a pre-term newborn who was born at 28 weeks of gestation.
Which of the following findings indicates a possible diagnosis of respiratory distress syndrome (RDS)?
Explanation
All of the above.
Respiratory distress syndrome (RDS) is a condition that affects preterm newborns who have immature lungs and lack sufficient surfactant.
Surfactant is a substance that helps keep the alveoli open and prevents them from collapsing.
Without enough surfactant, the newborn has difficulty breathing and may develop hypoxia and acidosis.
Choice A is wrong because tachypnea and grunting are signs of respiratory distress, but they are not specific to RDS.
They can also be caused by other conditions such as transient tachypnea of the newborn, pneumonia, or congenital heart defects.
Choice B is wrong because bradycardia and cyanosis are also signs of respiratory distress, but they are not specific to RDS.
They can also be caused by other conditions such as hypothermia, hypoglycemia, or sepsis.
Choice C is wrong because apnea and nasal flaring are also signs of respiratory distress, but they are not specific to RDS.
They can also be caused by other conditions such as intracranial ...
A nurse is teaching a client who is pregnant about the risk factors for pre-term labor.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The client should not limit their physical activity and rest as much as possible, unless advised by their provider.Excessive rest and inactivity can increase the risk of blood clots and decrease blood circulation, which can affect the placenta and the fetus.The client should follow the recommended guidelines for physical activity during pregnancy, unless they have a medical condition that requires bed rest or reduced activity.
Choice A is wrong because smoking and drinking alcohol during pregnancy are known risk factors for preterm labor and birth.Smoking can reduce blood flow to the placenta and affect fetal growth and development, while alcohol can cause fetal alcohol spectrum disorders and other complications.
Choice B is wrong because reporting any vaginal bleeding or fluid leakage to the provider is important to prevent or treat preterm labor and birth.Bleeding can indicate placenta previa or placental abruption, which are serious conditions that can cause premature delivery or fetal distress.Fluid leakage can indicate rupture of membranes, which can increase the risk of infection and preterm labor.
Choice D is wrong because drinking plenty of fluids and eating a balanced diet are beneficial for the health of the mother and the fetus.Dehydration can cause uterine contractions and trigger preterm labor, while malnutrition can affect fetal growth and development.A balanced diet can also help prevent or manage conditions like diabetes, high blood pressure, and anemia, which are risk factors for preterm labor and birth.
A nurse is reviewing the laboratory results of a pre-term newborn who was born at 32 weeks of gestation.
Which of the following values indicates a potential complication of necrotizing enterocolitis (NEC)?
Explanation
White blood cell count 25,000/mm3.
This indicates a potential complication of necrotizing enterocolitis (NEC), which is the death of intestinal tissue in premature or sick newborns.A high white blood cell count can be a sign of infection or inflammation in the bowel, which are common features of NEC.
Choice A is wrong because hematocrit 45% is within the normal range for newborns.
Hematocrit measures the percentage of red blood cells in the blood.
A low hematocrit can indicate blood loss or anemia, which can be complications of NEC, but a normal hematocrit does not rule out NEC.
Choice B is wrong because platelets 150,000/mm3 is also within the normal range for newborns.
Platelets are cells that help the blood clot.A low platelet count can indicate a consumption coagulopathy, which is a bleeding disorder that can occur in severe cases of NEC.
However, a normal platelet count does not exclude NEC.
Choice D is wrong because blood glucose 80 mg/dL is also within the normal range for newborns.
Blood glucose measures the amount of sugar in the blood.
A low blood glucose can indicate hypoglycemia, which can be caused by sepsis or other conditions that mimic NEC, but a normal blood glucose does not eliminate NEC.
A nurse is planning care for a pre-term newborn who has a diagnosis of intraventricular hemorrhage (IVH).
Which of the following interventions should the nurse include in the plan?
Explanation
Monitor vital signs and neurological status frequently.
This is because intraventricular hemorrhage (IVH) is a common and serious complication of prematurity that can lead to hydrocephalus, cerebral palsy, and developmental delays.Monitoring vital signs and neurological status can help detect changes in intracranial pressure, bleeding, and infection.
Choice B is wrong because antibiotics are not indicated for IVH unless there is evidence of infection.
Choice C is wrong because elevating the head of the bed to 30 degrees can increase the risk of IVH by reducing cerebral perfusion pressure and causing venous congestion.
Choice D is wrong because supplemental oxygen is not recommended for IVH unless there is hypoxia or respiratory distress.Excessive oxygen can cause oxidative stress and vasoconstriction, which can worsen IVH.
A nurse is caring for a pre-term newborn who has a patent ductus arteriosus (PDA).
Which of the following medications should the nurse expect to administer to close the ductus arteriosus?
Explanation
Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) that helps close the ductus arteriosus, a blood vessel connecting two arteries of the heart (aorta and pulmonary artery) in fetus.This drug is effective only among premature babies.
Choice B.Prostaglandin E1 is wrong because it is used to keep the ductus arteriosus open in some congenital heart defects that require surgery.
Choice C.Furosemide is wrong because it is a diuretic that reduces fluid retention and blood pressure, but does not affect the ductus arteriosus.
Choice D.Digoxin is wrong because it is a cardiac glycoside that strengthens the heart muscle contractions and regulates the heart rhythm, but does not affect the ductus arteriosus.
A nurse is evaluating the effectiveness of magnesium sulfate therapy for a client who is in pre-term labor.
Which of the following findings indicates that the therapy is successful?
Explanation
Magnesium sulfate is a tocolytic drug that inhibits uterine activity and relaxes smooth muscles.The goal of magnesium sulfate therapy for a client who is in pre-term labor is to stop or reduce the frequency and intensity of contractions.
Choice B is wrong because the client’s blood pressure decreases to within normal limits.
Magnesium sulfate is not an antihypertensive drug and does not lower blood pressure.It is used to prevent seizures in clients with preeclampsia or eclampsia.
Choice C is wrong because the client’s deep tendon reflexes are 2+.
This is a normal finding and does not indicate the effectiveness of magnesium sulfate therapy.A decrease or loss of deep tendon reflexes may indicate magnesium toxicity, which is a serious complication that requires immediate intervention.
Choice D is wrong because the client’s urine output increases to more than 30 mL/hr.
This is also a normal finding and does not indicate the effectiveness of magnesium sulfate therapy.A decrease in urine output may indicate renal impairment or magnesium toxicity, which are both adverse effects of the drug.
The normal range for serum magnesium level is 1.5 to 2.5 mEq/L or 1.8 to 3 mg/dL.The therapeutic range for magnesium sulfate management is 5 to 8 mg/dL.
A nurse is providing discharge teaching to a client who delivered a pre-term newborn at 34 weeks of gestation.
Which of the following instructions should the nurse include in the teaching?
Explanation
Pre-term newborns are at risk of apnea of prematurity, which is a pause in breathing for more than 20 seconds or less than 20 seconds with bradycardia or cyanosis.An apnea monitor can detect and alert the parents of any episodes of apnea and help them intervene promptly.
Choice A is wrong because breastfeeding is beneficial for pre-term newborns and can provide them with antibodies, nutrients, and bonding with the mother.Breastfeeding should be encouraged as soon as the newborn is medically stable and able to suck and swallow.
Choice C is wrong because keeping the newborn in a warm environment at all times can lead to overheating, dehydration, and increased metabolic rate.Pre-term newborns have difficulty regulating their body temperature and need to be dressed appropriately for the ambient temperature.They should also be monitored for signs of cold stress or heat stress.
Choice D is wrong because delaying immunizations until the newborn reaches term gestation can expose the newborn to preventable infections that ...
A nurse is assessing a pre-term newborn who has retinopathy of prematurity (ROP).
Which of the following manifestations should the nurse expect to observe?
Explanation
Leukocoria (white pupils) is a symptom of retinopathy of prematurity (ROP), an eye disease that can happen in premature babies.ROP happens when abnormal blood vessels grow on the retina, the light-sensitive layer of tissue in the back of the eye.
Choice B is wrong because strabismus (crossed eyes) is not a symptom of ROP, but a possible complication that can occur later in life.
Choice C is wrong because nystagmus (involuntary eye movements) is not a symptom of ROP, but another possible complication that can occur later in life.
Choice D is wrong because it includes choices B and C, which are incorrect.
Normal ranges for gestational age and birth weight are 38 to 42 weeks and 5.5 to 10 pounds, respectively.Babies born before 31 weeks or weighing less than 3 pounds are at risk for ROP.
A nurse is administering betamethasone to a client who is at risk for pre-term labor at 30 weeks of gestation.
Which of the following outcomes should the nurse monitor for in the newborn?
Explanation
Betamethasone is a corticosteroid that is given to pregnant women who are at risk of preterm labor to improve neonatal outcomes.Betamethasone stimulates the production of surfactant, a substance that lubricates the lungs and prevents them from collapsing after birth.This reduces the risk of respiratory distress syndrome, a common complication of preterm birth.
Choice B is wrong because betamethasone does not decrease the risk of infection in the newborn.In fact, it may increase the risk of maternal and neonatal infections by suppressing the immune system.
Choice C is wrong because betamethasone does not increase blood glucose levels in the newborn.However, it may cause transient hyperglycemia in the mother, which should be monitored and treated if necessary.
Choice D is wrong because betamethasone does not decrease the risk of bleeding in the newborn.It may increase the risk of intraventricular hemorrhage, a type of bleeding in the brain, if given before 24 weeks of gestation.Therefore, it should be used with caution in this population and only after a family’s decision regarding resuscitation.
Exams on Pre-term Labor
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define pre-term labor and its causes and risk factors
- Identify the signs and symptoms of pre-term labor and how to assess them
- Describe the nursing interventions and medications for pre-term labor and their rationales
- Explain the complications and outcomes of pre-term labor for the mother and the fetus
- Discuss the patient education and discharge planning for pre-term labor
- Apply the nursing process and critical thinking to case scenarios involving pre-term labor
Introduction
- Pre-term labor is the onset of regular uterine contractions with cervical changes before 37 weeks of gestation
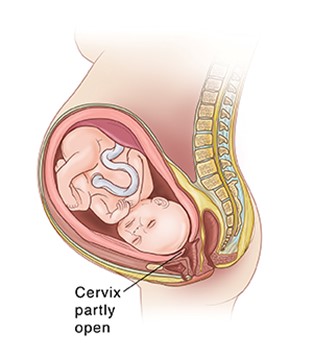
- Pre-term labor can lead to pre-term birth, which is the delivery of a live-born infant before 37 weeks of gestation
- Pre-term birth is a major cause of neonatal morbidity and mortality, as well as long-term developmental disabilities
- Pre-term labor can be spontaneous or induced by medical or obstetric complications
Causes and Risk Factors
- The exact causes of pre-term labor are unknown, but some possible factors include:
- Infection or inflammation of the genital tract, such as bacterial vaginosis, chorioamnionitis, or urinary tract infection
- Multiple gestation, such as twins or triplets
- Placental abnormalities, such as placenta previa or abruption
- Uterine anomalies, such as fibroids or septum
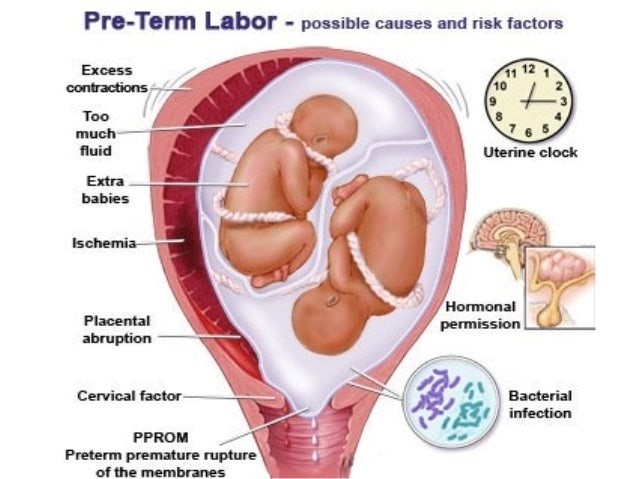
-
- Cervical insufficiency, which is the inability of the cervix to remain closed during pregnancy
- History of pre-term birth or cervical surgery
- Maternal age less than 18 or more than 35 years
- Maternal medical conditions, such as diabetes, hypertension, preeclampsia, or anemia
- Maternal lifestyle factors, such as smoking, alcohol use, drug abuse, or stress

-
- Fetal factors, such as congenital anomalies, intrauterine growth restriction, or fetal distress
Signs and Symptoms
- The signs and symptoms of pre-term labor may include:
- Regular uterine contractions that occur at least every 10 minutes and last for more than 30 seconds
- Lower abdominal cramping or pressure
- Low back pain or pelvic pressure
- Change in vaginal discharge, such as increased amount, color, or consistency
- Bleeding or spotting from the vagina
- Rupture of membranes (ROM), which is the leakage of amniotic fluid from the vagina
- Decreased fetal movement

Assessment
- The assessment of pre-term labor includes:
- Obtaining a detailed history of the current pregnancy and any previous pregnancies, including any complications or interventions
- Performing a physical examination of the vital signs, abdomen, cervix, and fetal heart rate and activity
- Performing a speculum examination of the vagina and cervix to check for infection, bleeding, or ROM
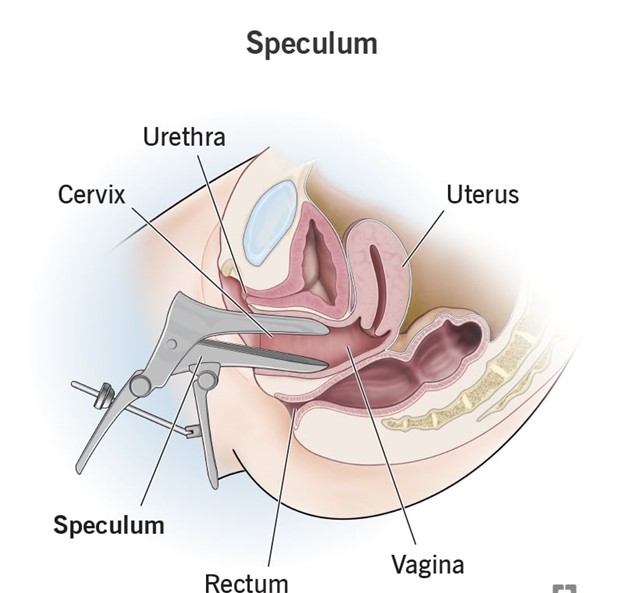
-
- Performing a digital examination of the cervix to check for dilation (opening), effacement (thinning), and station (position) of the fetus in relation to the pelvis
- Performing laboratory tests, such as urine culture, blood count, glucose level, and coagulation profile
- Performing diagnostic tests, such as ultrasound, fetal fibronectin test (FFN), or amniocentesis
Nursing Interventions
- The nursing interventions for pre-term labor depend on the gestational age, cervical status, fetal condition, and maternal preference. Some possible interventions include:
- Providing bed rest in a lateral position to reduce uterine activity and improve blood flow to the placenta and fetus
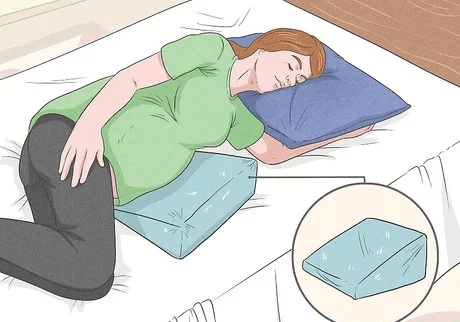
- Monitoring vital signs, uterine contractions, cervical changes, fetal heart rate and activity, and fluid intake and output
- Administering intravenous fluids to maintain hydration and prevent dehydration-induced contractions
- Administering medications to suppress uterine contractions (tocolytics), such as magnesium sulfate, nifedipine, indomethacin, or terbutaline. These medications have various side effects and contraindications that need to be monitored closely.
- Administering medications to enhance fetal lung maturity (corticosteroids), such as betamethasone or dexamethasone. These medications are given intramuscularly between 24 and 34 weeks of gestation and have a maximum effect after 48 hours.
- Administering antibiotics to treat infection or prophylactically if ROM has occurred. Some common antibiotics are ampicillin, erythromycin, or clindamycin.
- Providing emotional support and education to the mother and her partner or family about the causes, signs, and treatments of pre-term labor and the possible outcomes and complications for the mother and the fetus
- Preparing for delivery if pre-term labor is inevitable or if the risks of continuing the pregnancy outweigh the benefits. The mode of delivery depends on the gestational age, fetal presentation, and maternal and fetal condition. The delivery may be vaginal or cesarean.
Complications and Outcomes
- The complications and outcomes of pre-term labor vary depending on the gestational age, fetal condition, and neonatal care. Some possible complications and outcomes include:
- For the mother:
- Hemorrhage due to placental abruption or uterine atony
- Infection due to ROM or invasive procedures
- Thromboembolism due to prolonged bed rest or hypercoagulability
- Psychological distress due to anxiety, guilt, or grief
- For the fetus:
- Respiratory distress syndrome (RDS) due to immature lungs and surfactant deficiency
- For the mother:
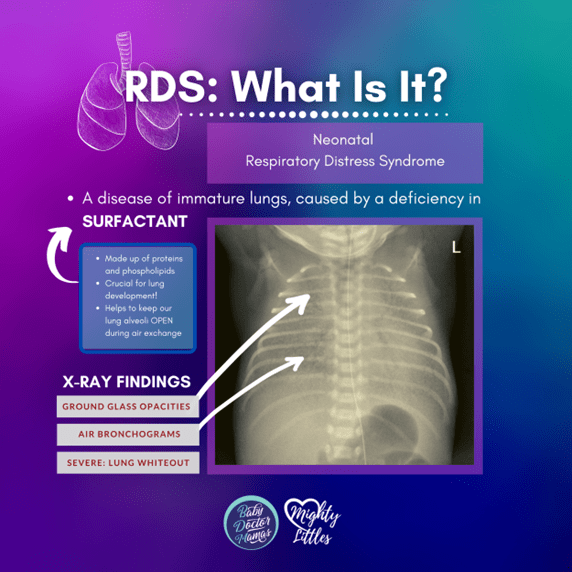
-
-
- Intraventricular hemorrhage (IVH) due to fragile blood vessels in the brain
- Necrotizing enterocolitis (NEC) due to ischemia and inflammation of the bowel
- Retinopathy of prematurity (ROP) due to abnormal growth of blood vessels in the retina
- Sepsis due to infection or immune deficiency
- Patent ductus arteriosus (PDA) due to failure of closure of the fetal shunt between the aorta and pulmonary artery
- Jaundice due to increased bilirubin production and decreased excretion
- Hypothermia due to large surface area and low fat stores
- Hypoglycemia due to low glycogen stores and increased glucose demand
-
Patient Education and Discharge Planning
The patient education and discharge planning for pre-term labor include:
- Teaching the mother how to recognize and report the signs and symptoms of pre-term labor and when to seek medical attention
- Advising the mother to avoid activities that may trigger or worsen pre-term labor, such as heavy lifting, strenuous exercise, sexual intercourse, smoking, alcohol use, or drug abuse
- Encouraging the mother to follow a balanced diet, drink plenty of fluids, take prenatal vitamins, and avoid caffeine
- Instructing the mother on how to perform fetal kick counts daily and report any decrease in fetal movement
- Providing information and resources on breastfeeding, kangaroo care (skin-to-skin contact), and bonding with the pre-term infant
- Referring the mother to community services or support groups for pre-term infants and their families
Summary
- Pre-term labor is the onset of regular uterine contractions with cervical changes before 37 weeks of gestation
- Pre-term labor can be spontaneous or induced by medical or obstetric complications
- Pre-term labor can lead to pre-term birth, which is a major cause of neonatal morbidity and mortality
- The signs and symptoms of pre-term labor may include regular uterine contractions, lower abdominal cramping or pressure, low back pain or pelvic pressure, change in vaginal discharge, bleeding or spotting from the vagina, rupture of membranes, or decreased fetal movement
- The assessment of pre-term labor includes obtaining a detailed history, performing a physical examination, performing a speculum examination, performing a digital examination, performing laboratory tests, and performing diagnostic tests
- The nursing interventions for pre-term labor depend on the gestational age, cervical status, fetal condition, and maternal preference. Some possible interventions include providing bed rest in a lateral position, monitoring vital signs and fetal status, administering intravenous fluids, administering medications to suppress uterine contractions or enhance fetal lung maturity, administering antibiotics to treat infection or prophylactically if ROM has occurred, providing emotional support and education, and preparing for delivery if pre-term labor is inevitable or if the risks of continuing the pregnancy outweigh the benefits
- The complications and outcomes of pre-term labor vary depending on the gestational age, fetal condition, and neonatal care. Some possible complications and outcomes include hemorrhage, infection, thromboembolism, psychological distress, respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, retinopathy of prematurity, sepsis, patent ductus arteriosus, jaundice, hypothermia, and hypoglycemia for the mother and the fetus
- The patient education and discharge planning for pre-term labor include teaching the mother how to recognize and report the signs and symptoms of pre-term labor and when to seek medical attention, advising the mother to avoid activities that may trigger or worsen pre-term labor, encouraging the mother to follow a balanced diet and take prenatal vitamins, instructing the mother on how to perform fetal kick counts daily, providing information and resources on breastfeeding, kangaroo care, and bonding with the pre-term infant, and referring the mother to community services or support groups for pre-term infants and their families
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Pre-term Labor
This filled cannot be empty

