Please set your exam date
Pain Management During Labor
Study Questions
Introduction
A nurse is caring for a client who is in labor and requests nonpharmacological pain relief measures.
Which of the following actions should the nurse take? (Select all that apply.).
Explanation
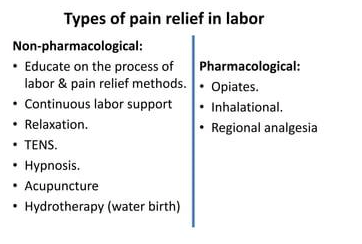
These are all nonpharmacological pain relief measures that the nurse can take for a client who is in labor.
• aromatherapy can help the client relax and cope with the pain by stimulating the olfactory system and influencing the limbic system.
• sacral counterpressure can relieve back pain caused by posterior fetal position by applying firm pressure on the sacrum during contractions.
• effleurage is a form of light rhythmic stroking of the abdomen that can distract the client from the pain and increase endorphin production.
• continuous labor support can reduce anxiety, fear, and stress, and enhance the client’s sense of control and confidence.

A nurse is reviewing the options for pharmacologic analgesia with a client who is in the first stage of labor.
Which of the following statements by the nurse is appropriate?
Explanation
Nitrous oxide is a self-administered inhaled analgesic that can reduce anxiety and pain perception during labor.It has a rapid onset and offset, and does not cause respiratory depression in the mother or the baby.
A nurse is preparing a client for a cesarean delivery and explains the procedure for spinal anesthesia.
Which of the following information should the nurse include?
Explanation
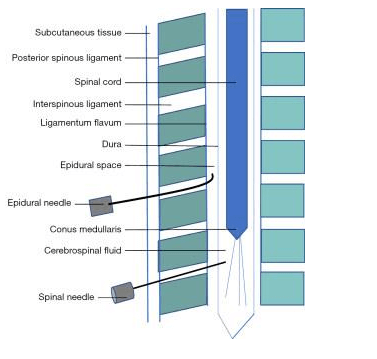
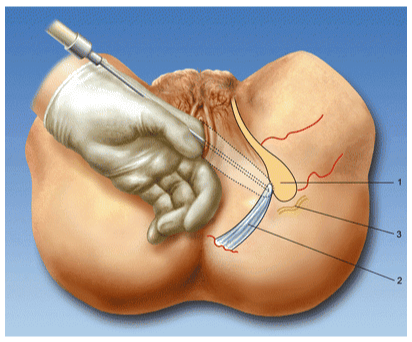
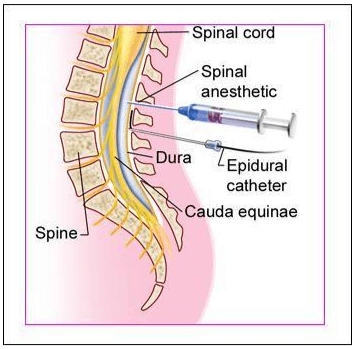
This is a description of spinal anesthesia, which is the safest form of anesthesia for cesarean delivery.Spinal anesthesia involves inserting a needle into the subarachnoid space and injecting a local anesthetic and/or a narcotic into the cerebrospinal fluid.
A lumbar puncture involves making a small puncture in the dura mater and allowing a small amount of cerebrospinal fluid to leak out for analysis.
A lumbar puncture does not involve injecting any medication or blocking any pain sensations.
A nurse is assessing a client who is receiving epidural analgesia during labor.
Which of the following findings should the nurse report to the provider?
Explanation
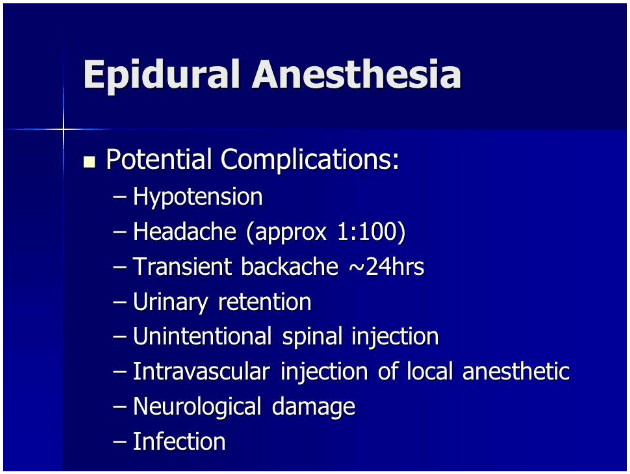
This finding should be reported to the provider because it indicates a possible infection, which can be a complication of epidural anesthesia.
A nurse is caring for a client who has opioid use disorder and is in labor.
Which of the following actions should the nurse take to provide individualized pain management for this client? (Select all that apply.).
Explanation
The nurse should consult with a substance use disorder specialist to determine the best pain management plan for the client who has opioid use disorder and is in labor.
The nurse should also monitor the client and the fetus closely for signs of withdrawal, which can occur due to reduced opioid intake during labor or due to the administration of opioid antagonists.
Nonpharmacologic Pain Management During Labor
A nurse is caring for a woman who is in active labor and wants to use water immersion as a nonpharmacologic pain management method.
What should the nurse do before assisting the woman into the tub?
Explanation
The nurse should monitor the fetal well-being and maternal progress before assisting the woman into the tub.Water immersion during labor may be associated with decreased pain or use of anesthesia and decreased duration of labor, but it should not prevent or inhibit other elements of care.
A nurse is teaching a childbirth preparation class about the benefits of upright positioning during labor.
What should the nurse include in the teaching? (Select all that apply.)
Explanation
These are the benefits of upright positioning during labor:
• It improves blood flow to the uterus and placenta, which means better oxygen supply to the baby.
• It reduces pressure on the sacrum and perineum, which means less pain and discomfort for the mother.
• It increases pelvic diameter and fetal descent, which means shorter and more effective contractionsand easier delivery.
A nurse is providing continuous labor support to a woman who is experiencing back pain due to a posterior fetal position.
What nonpharmacologic technique can the nurse use to relieve the pain?
Explanation
Sacral pressure is a nonpharmacologic technique that can relieve back pain due to a posterior fetal position by applying firm pressure to the lower back with a fist, tennis ball, or other object.
This can help counteract the pressure of the fetal head on the sacrum and reduce discomfort.
A nurse is instructing a woman in labor to use relaxation techniques to cope with pain.
What are some examples of relaxation techniques that the nurse can suggest? (Select all that apply.)
Explanation
Breathing exercises, progressive muscle relaxation, guided imagery, and aromatherapy are all examples of relaxation techniques that can help a woman in labor cope with pain.
These techniques can reduce stress, anxiety, and muscle tension, and enhance the release of endorphins, which are natural painkillers.
A nurse is explaining the gate control theory of pain to a woman in labor who wants to use cutaneous stimulation as a nonpharmacologic pain management method.
What should the nurse say about how cutaneous stimulation works?
Explanation
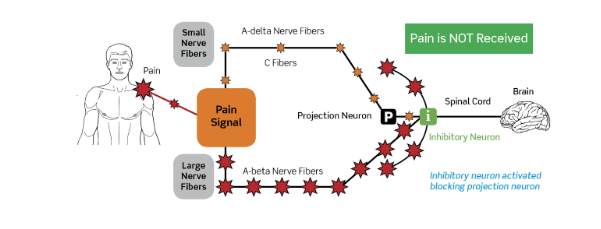
This is based on thegate control theory of pain, which describes how non-painful sensations can override and reduce painful sensations.According to this theory, there are neurological “gates” in the spinal cord that decide which pain signals pass through and which are kept out.When non-painful stimuli, such as cutaneous stimulation, activate large-diameter nerve fibers, they can close the gates and block the transmission of pain signals from small-diameter nerve fibers.
This reduces the perception of pain in the brain.
Pharmacologic Pain Management During Labor
A nurse is caring for a client who is in labor and requests systemic analgesia.
Which of the following medications can the nurse administer intravenously to provide sedation, anxiolysis, and analgesia during labor?
Explanation
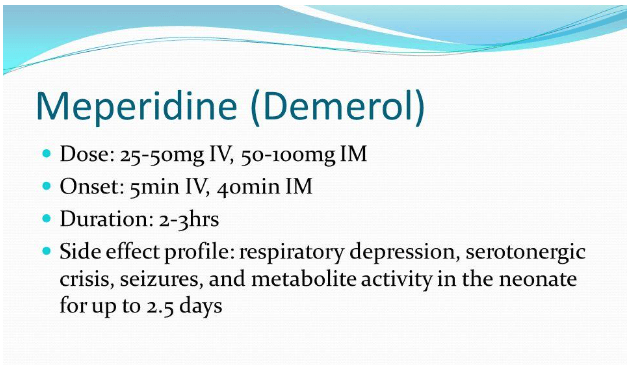
Meperidine is an opioid that can be administered intravenously to provide sedation, anxiolysis, and analgesia during labor.It provides pain relief that is superior to nitrous oxide but inferior to regional anesthesia.
A client who is in labor asks the nurse about the benefits and limitations of inhaled analgesia.
Which of the following statements should the nurse include in the teaching?
Explanation
inhaled analgesia, such as nitrous oxide, is self-administered by the client through a mask or mouthpiece.The client needs to coordinate the inhalation with the onset of contractions and may need assistance from a support person to hold the mask or mouthpiece.
A nurse is reviewing the medical record of a client who is in labor and has a history of asthma.
The nurse should identify that which of the following pharmacologic pain management methods is contraindicated for this client?
Explanation
Inhaled analgesia is contraindicated for this client because it can cause bronchospasm and hypoxia in patients with asthma.
Normal ranges for blood pressure are 90/60 to 120/80 mmHg, for fetal heart rate are 110 to 160 beats per minute, and for bladder function are urine output of at least 30 mL/hour.
A nurse is preparing to administer fentanyl to a client who is in labor and has severe pain.
Which of the following actions should the nurse take to prevent adverse effects on the fetus?
Explanation
Administer the medication immediately after a contraction.This is because fentanyl can cross the placenta and cause respiratory depression in the fetus, so it should be given when the placental blood flow is lowest, which is right after a contraction.
A nurse is caring for a client who is in labor and has received meperidine for pain relief.
Which of the following findings should alert the nurse to a possible adverse effect of the medication?
Explanation
This is a sign ofrespiratory depression, which is a possible adverse effect of meperidine.Meperidine is an opioid analgesic that can slow or stop breathing, and cause death in some cases.
A nurse is preparing to administer epidural anesthesia to a client in labor.
What is the minimum cervical dilation required before inserting the catheter into the epidural space?
Explanation
The correct answer is Choice B.
Choice A rationale: A cervical dilation of 2 cm is not sufficient for the insertion of an epidural catheter. The cervix needs to be dilated more to ensure that the catheter can be inserted without causing injury or discomfort to the patient. Furthermore, administering epidural anesthesia too early in labor can potentially slow down the labor process.
Choice B rationale: A cervical dilation of 4 cm is generally considered the minimum dilation required before inserting the catheter into the epidural space. At this stage, the labor is established and the risk of slowing down the labor process is minimal. The epidural space can be accessed safely and the catheter can be inserted without causing injury or discomfort to the patient.
Choice C rationale: While a cervical dilation of 6 cm is more than sufficient for the insertion of an epidural catheter, it is not necessary to wait until the cervix is dilated to this extent before administering epidural anesthesia. Waiting until the cervix is dilated to 6 cm could result in unnecessary pain and discomfort for the patient.
Choice D rationale: A cervical dilation of 8 cm is well into the active phase of labor and is often considered too late for the administration of epidural anesthesia. At this stage, the labor is progressing rapidly and there may not be enough time to administer the anesthesia and achieve adequate pain relief before the baby is born.
A nurse is caring for a client who received spinal anesthesia for a cesarean delivery.
The nurse should monitor the client for which of the following potential complications of spinal anesthesia?
Explanation
A potential complication of spinal anesthesia is postdural puncture headache (PDPH), which occurs when cerebrospinal fluid leaks through the puncture site and causes low pressure in the subarachnoid space.
This can result in a severe headache that worsens when sitting or standing and improves when lying down.PDPH usually occurs within 24 to 48 hours after the spinal anesthesia and can last for days or weeks.
A nurse is educating a client about the advantages of combined spinal-epidural (CSE) anesthesia over epidural or spinal anesthesia alone.
Which of the following statements by the client indicates understanding of the teaching?
Explanation
This statement indicates that the client understands the advantages of CSE anesthesia over epidural or spinal anesthesia alone.CSE anesthesia combines the rapid onset and reliable blockade of spinal anesthesia with the ability to extend and adjust the analgesia through epidural catheterization.This makes CSE anesthesia suitable for procedures that require timely, effective, and prolonged pain relief, such as labor and delivery, abdominal surgery, and lower extremity orthopedic surgery.
A nurse is assisting an anesthesiologist with performing dural puncture epidural (DPE) anesthesia for a client in labor.
What is the purpose of intentionally puncturing the dura mater with a needle in this technique?
Explanation
The purpose of intentionally puncturing the dura mater with a needle in this technique is to allow cerebrospinal fluid to leak into the epidural space and enhance the spread of local anesthetics.This technique is a modification of the combined spinal epidural technique, which involves injecting medication into both the epidural and the subarachnoid spaces.The dural puncture epidural technique aims to avoid the side effects of the combined spinal epidural technique, such as hypotension, pruritus, and urinary retention.
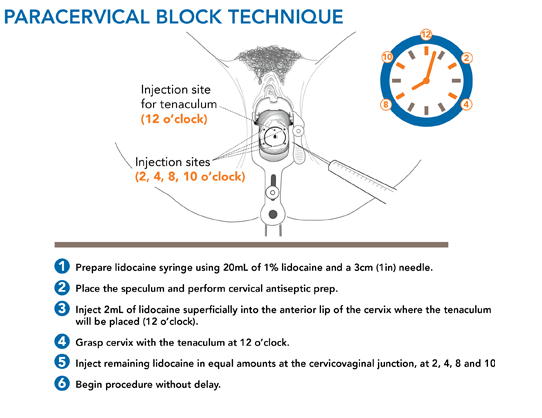
A nurse is planning to administer paracervical block to a client in labor.
Which of the following areas should the nurse inject local anesthetics into?
Explanation
The paracervical area at 3 o’clock and 9 o’clock positions.This is because a paracervical block is an anesthetic procedure in which a local anesthetic is injected into between two and six sites at a depth of 3–7 mm alongside the vaginal portion of the cervix in the vaginal fornices.The injection sites are usually at 10 o’clock, 8 o’clock, 2 and 4 o’clock positions, but for labor pain relief, the 3 o’clock and 9 o’clock positions are preferred.
Nursing Interventions for Pain Management During Labor
A nurse is assessing a client’s pain during labor using a numerical rating scale.
The client reports a pain level of 8 out of 10.
What is the nurse’s priority action?
Explanation
According to the article by Carvalho and Mhyre, pain scales such as the numerical rating scale are unidimensional and lack many characteristics of an ideal psychometric pain instrument in a labor setting.
They also state that “the most important question for laboring women is not ‘How much does it hurt?’ but rather ‘How are you coping?’”.Therefore, the nurse’s priority action is to assess the woman’s coping skills and provide comfort measures such as relaxation, breathing techniques, massage, heat or cold application, etc
A nurse is educating a client about nonpharmacologic methods of pain management during labor.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Aromatherapy is a nonpharmacologic method of pain management during labor that uses scented oils or candles to stimulate the senses and distract the woman from the pain.Aromatherapy can also help reduce anxiety and stress during labor.
A nurse is administering an epidural analgesia to a client in labor.
Which of the following actions should the nurse take?
Explanation
Obtaining informed consent is an essential step before administering epidural analgesia to a client in labor.The nurse should explain the procedure, benefits, risks, and alternatives to the client and obtain her written consent.
A nurse is evaluating a client’s satisfaction with pain management during labor.
Which of the following tools should the nurse use?
Explanation
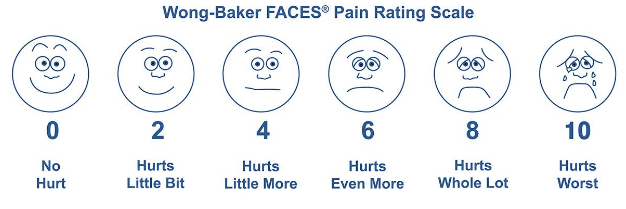
This is a pain assessment tool that combines pictures and numbers for pain ratings.
It can be used in adults and children over age 3.
Six faces depict different expressions, ranging from happy to extremely upset.
Each is assigned a numerical rating between 0 (smiling) and 10 (crying).To use it, the patient can point to the picture that best represents the degree and intensity of their pain.
A nurse is providing continuous labor support to a client in labor.
Which of the following actions should the nurse take? (Select all that apply.).
Explanation
These are all actions that the nurse should take to provide continuous labor support to a client in labor.According to the Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN), continuous labor support from a registered nurse (RN) is critical to achieve improved birth outcomes.Continuous labor support includes encouraging the client to drink clear fluids and ice chips, assisting the client with ambulation and position changes, providing feedback and reinforcement to the client and her partner, and massaging the client’s back and shoulders during contractions.
Summary
A nurse is reviewing nonpharmacologic methods of pain relief with a pregnant client who is in early labor.
The client states that she wants to try aromatherapy during labor but does not know which essential oils are safe to use.
Which of the following oils should the nurse recommend?
Explanation
Lavender is a safe and effective essential oil to use during labor for pain relief and relaxation.According to Evidence Based Birth, lavender may also help reduce anxiety, nausea and the length of labor.
A nurse is assisting a client who is in active labor and plans to use hypnosis as a nonpharmacologic method of pain relief.
Which of the following actions should the nurse take to facilitate this method?
Explanation
hypnosis for pain relief during labor involves entering into a state of self-hypnosis that alters the perception of potentially painful sensations.By focusing on a pleasant image or memory, the client can enhance the effect of hypnosis and reduce the need for pharmacological analgesia.
A nurse is caring for a client who is in transition phase of labor and reports feeling nauseated and lightheaded.
The nurse suspects that the client is hyperventilating due to rapid breathing.
Which of the following findings supports this suspicion?
Explanation
are common symptoms of hyperventilation.Hyperventilation is rapid or deep breathing that reduces the amount of carbon dioxide in the blood.This causes the blood vessels that supply the brain to narrow, leading to lightheadedness and tingling sensations.
A nurse is teaching a childbirth education class about nonpharmacological measures for pain management during labor.
Which of the following techniques should the nurse include as an example of gate control theory?
Explanation
Acupressure is an example of gate control theory of pain, which describes how non-painful sensations can override and reduce painful sensations.Acupressure involves applying pressure to specific points on the body to stimulate large-diameter nerve fibers that can block the transmission of pain signals from smaller-diameter nerve fibers.
A nurse is caring for a client who is receiving pudendal block anesthesia for a vaginal delivery.
Which of the following outcomes should the nurse expect?
Explanation
a pudendal nerve block is a form of local anesthesia that blocks the pudendal nerve, which innervates the perineum, vulva, and vagina.A pudendal nerve block is commonly used to relieve pain during the delivery of baby by forceps, vaginal repairs, and anorectal surgeries.
A nurse is administering nitrous oxide to a client who is in labor.
Which of the following actions should the nurse take?
Explanation
The nurse should take all of the following actions when administering nitrous oxide to a client who is in labor:
Instruct the client to hold the mask over her mouth and nose during contractions.This allows the client to self-administer the gas and control the amount and timing of inhalation.
Monitor the client’s oxygen saturation level continuously.Nitrous oxide can cause hypoxia and respiratory depression if used in high concentrations or for prolonged periods.
Ensure that there is adequate ventilation in the room.Nitrous oxide is a greenhouse gas and can have negative environmental and occupational effects if not properly scavenged.
A nurse is caring for a client who is in labor and has received epidural anesthesia for pain relief.
Which of the following interventions should the nurse perform to prevent hypotension?
Explanation
epidural anesthesia can cause vasodilation and decrease venous return, leading to hypotension.IV fluids can help maintain blood volume and prevent hypotension.
A nurse is caring for a client who is in labor and has received spinal anesthesia for pain relief.
The client reports a severe headache that worsens when sitting up.
Which of the following actions should the nurse take?
Explanation
the client has a spinal headache, which is caused by leakage of cerebrospinal fluid (CSF) through the dural hole created by the needle.Lying flat can reduce the pressure gradient between the brain and the spinal cord and decrease the headache pain.
A nurse is caring for a client who is in labor and has received nitrous oxide for pain relief.
Which of the following are potential adverse effects of this method? (Select all that apply.).
Explanation
Dizziness and headache are potential adverse effects of nitrous oxide for pain relief during labor.Nitrous oxide can also cause nausea, vomiting, drowsiness, reduced awareness, and mask phobia.
A nurse is caring for a child who is receiving morphine via a patient-controlled analgesia (PCA) pump after abdominal surgery.
Which of the following actions should the nurse take? (Select all that apply.)
Explanation
The nurse should assess the child’s pain level using a numeric rating scale and check the PCA pump settings with another nurse.
These actions ensure that the child is receiving adequate pain relief and that the PCA pump is functioning properly and safely.
A nurse is caring for a client who is in active labor and requests pain medication.
Which of the following factors should the nurse consider when choosing a pharmacological pain management method? (Select all that apply.)
Explanation
These are the factors that the nurse should consider when choosing a pharmacological pain management method for a client who is in active labor.
- the client’s preference and birth plan should be respected and supported by the nurse.The client may have specific wishes or expectations about the type and timing of pain medication, and the nurse should discuss these with the client and provide information and education as needed.
- the stage and duration of labor affect the type and effectiveness of pharmacological pain management methods.For example, parenteral opioids provide pain relief that is superior to nitrous oxide but inferior to regional anesthesia.However, opioids may cause adverse effects such as nausea, vomiting, sedation and respiratory depression in both the mother and the fetus.Therefore, opioids are usually given in early labor and avoided in late labor or close to delivery.Regional anesthesia, such as epidural or spinal anesthesia, provides the most effective pain relief but may also have some drawbacks such as hypotension, pruritus, urinary retention and prolonged second stage of labor.Therefore, regional anesthesia may not be suitable for clients who have contraindications or who are in advanced labor.
- the fetal heart rate and position may influence the choice of pharmacological pain management method.For example, regional anesthesia may cause maternal hypotension, which can reduce uteroplacental blood flow and cause fetal bradycardia.Therefore, regional anesthesia should be used with caution in clients who have fetal distress or nonreassuring fetal heart rate patterns.Additionally, some fetal positions, such as occiput posterior or transverse lie, may cause more severe back pain that may not be relieved by regional anesthesia alone.In such cases, other methods such as sterile water injections or pudendal block may be helpful.
A nurse is reviewing informed consent with a client who is scheduled for a cesarean delivery with spinal anesthesia.
Which of the following statements by the client indicates a need for further teaching?
Explanation
Spinal anesthesia does not affect blood loss or blood pressure during a cesarean delivery.It only blocks pain sensations from the lower part of the body by injecting medication into the cerebrospinal fluid.
A nurse is caring for a client who is in active labor and requests pain medication.
Which of the following factors should the nurse consider when choosing a systemic analgesic? (Select all that apply.).
Explanation
The stage and phase of labor and the fetal heart rate and pattern are important factors that the nurse should consider when choosing a systemic analgesic for a client who is in active labor.Systemic analgesics can cross the placenta and affect the fetus, so the nurse should monitor the fetal heart rate and pattern for any signs of distress or changes.The stage and phase of labor can influence the timing and effectiveness of systemic analgesics, as well as the risk of adverse effects on the mother and the fetus.For example, systemic analgesics given too early in labor may prolong labor, whereas systemic analgesics given too late in labor may cause respiratory depression in the newborn.
Normal ranges for maternal vital signs are: blood pressure 110/60 to 140/90 mm Hg, pulse 60 to 100 beats per minute, respiratory rate 12 to 20 breaths per minute, and temperature 36.5 to 37.5°C (97.7 to 99.5°F).
Normal ranges for fetal heart
A nurse is caring for a client who is receiving intrathecal opioid analgesia during labor.
Which of the following medications should the nurse have available as an antidote in case of respiratory depression?
Explanation
Naloxone is an opioid antagonist that can reverse the respiratory depression caused by intrathecal opioid analgesia.Flumazenil is an antidote for benzodiazepine overdose, not opioid overdose.Protamine sulfate is an antidote for heparin overdose, not opioid overdose.Vitamin K is an antidote for warfarin overdose, not opioid overdose.
A nurse is caring for a client who is receiving nitrous oxide for pain relief during labor.
Which of the following are advantages of this method? (Select all that apply.).
Explanation
Nitrous oxide hasrapid onset and offsetand it allows the client tocontrol the dosageby self-administering the gas through a mask or mouthpiece.
Exams on Pain Management During Labor
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Explain the physiology of labor pain and its sources
-
Describe the benefits and risks of nonpharmacologic and pharmacologic pain management options during labor
-
Identify the indications, contraindications, and potential complications of regional anesthesia techniques during labor
-
Discuss the nursing interventions and patient education for pain management during labor
-
Evaluate the effectiveness and patient satisfaction of pain management during labor
Introduction
Pain perception and preferences for pain management are unique to each woman in labor. Pain management during labor affects the maternal experience, outcomes, and satisfaction. Uncontrolled pain can lead to anxiety and adverse postnatal effects. Therefore, creating a supportive and nurturing environment should be a priority throughout the perinatal period. Nurses are in a key position to help patients understand the options and make informed choices about pain management during labor.
Pharmacologic Pain Management During Labor
Pharmacologic pain management methods are techniques that involve medications or invasive procedures to relieve pain during labor. They aim to reduce pain intensity, modify pain perception, or block pain transmission.
Some of the benefits of pharmacologic methods are that they provide effective, consistent, and predictable pain relief for most women, they do not require active participation from the woman or her support person, and they can be adjusted according to the woman’s needs.
Some of the limitations are that they may have adverse effects on the mother or the fetus, they may interfere with maternal-fetal bonding, they may require additional monitoring or interventions, and they may not be available or acceptable in some cultures or settings.
Some examples of pharmacologic pain management methods are:
Systemic analgesics: These are medications that are administered orally, intramuscularly, or intravenously to provide sedation, anxiolysis, and analgesia during labor.
Systemic analgesics include opioids (such as meperidine, fentanyl, or morphine), antiemetics (such as promethazine), and benzodiazepines (such as diazepam).
Systemic analgesics provide pain relief that is superior to nitrous oxide but inferior to regional anesthesia.
Systemic analgesics can also reduce anxiety, nausea, vomiting, and shivering during labor.
However, systemic analgesics may cause maternal respiratory depression, hypotension, drowsiness, confusion, or pruritus.
Systemic analgesics may also cross the placenta and cause fetal respiratory depression, bradycardia, decreased variability, or neurobehavioral changes.
Systemic analgesics should be used with caution in women with asthma, cardiac disease, renal disease, liver disease, or opioid use disorder.
Systemic analgesics should also be timed carefully to avoid peak effects at delivery.
-
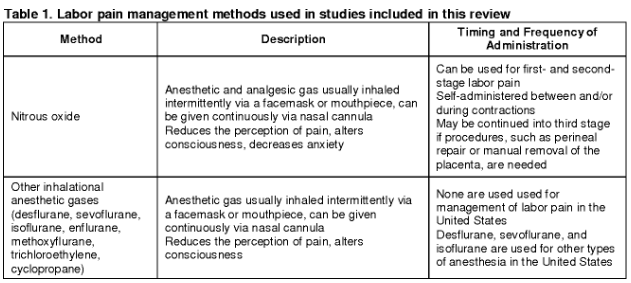
Inhaled analgesia: This is a method that involves inhaling a mixture of nitrous oxide (N2O) and oxygen (O2) through a mask or mouthpiece to provide self-administered analgesia during labor.
Inhaled analgesia provides mild to moderate pain relief that is comparable to parenteral opioids but less than regional anesthesia.
Inhaled analgesia can also reduce anxiety, nausea, vomiting, and shivering during labor.
However, inhaled analgesia may cause maternal dizziness, headache, drowsiness, nausea, vomiting, or dry mouth.
Inhaled analgesia may also have negative environmental impact as a greenhouse gas.
Inhaled analgesia should be used with caution in women with vitamin B12 deficiency, pulmonary disease, bowel obstruction, or pneumothorax.
Inhaled analgesia should also be discontinued at least 30 minutes before delivery to avoid neonatal depression.
Regional anesthesia: This is a method that involves injecting local anesthetics into specific regions of the body to block nerve impulses from reaching the brain.
Regional anesthesia provides the most effective pharmacologic analgesia during labor and is used in nearly three-fourths of labors in the United States.
Regional anesthesia can also reduce stress hormones, blood pressure, cardiac workload, and blood loss during labor.
However, regional anesthesia may cause maternal hypotension, bradycardia, fever, itching, urinary retention, or headache.
Regional anesthesia may also prolong the second stage of labor, increase the need for oxytocin augmentation or instrumental delivery, or interfere with maternal-fetal bonding.
Regional anesthesia should be performed by an anesthesiologist or a certified registered nurse anesthetist under strict aseptic technique.
Regional anesthesia should also be accompanied by adequate hydration, monitoring of vital signs and fetal heart rate, and prevention of supine hypotension syndrome by placing a wedge under the right hip.
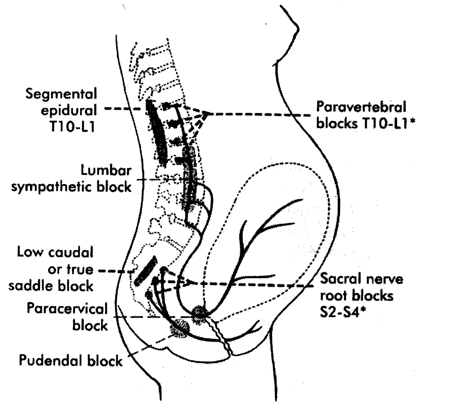
Some examples of regional anesthesia techniques are:
-
Epidural anesthesia: This involves placing a small catheter into the epidural space between L3-L4 or L4-L5 vertebrae through which local anesthetics (such as bupivacaine) and opioids (such as fentanyl) are administered continuously or intermittently.
Epidural anesthesia provides lack of sensation from the level at umbilicus to thighs.
Epidural anesthesia requires at least 4 cm of cervical dilation before insertion.
-
Spinal anesthesia: This involves injecting local anesthetics (such as bupivacaine) and opioids (such as fentanyl) into the subarachnoid space between L3-L4 or L4-L5 vertebrae through which local anesthetics (such as bupivacaine) and opioids (such as fentanyl) are injected once or twice.
Spinal anesthesia provides lack of sensation from the nipples to the feet.
Spinal anesthesia is used mainly for cesarean delivery or forceps delivery.
-
Combined spinal-epidural (CSE) anesthesia: This involves placing a small catheter into the epidural space and then injecting local anesthetics and opioids into the subarachnoid space through a needle that passes through the catheter.
CSE anesthesia combines the advantages of both epidural and spinal anesthesia, such as rapid onset, dense block, and prolonged duration.
CSE anesthesia can also provide better sacral coverage and less motor block than epidural or spinal anesthesia alone.
-
Dural puncture epidural (DPE) anesthesia: This involves placing a small catheter into the epidural space and then intentionally puncturing the dura mater with a needle to create a small hole.
DPE anesthesia allows cerebrospinal fluid to leak into the epidural space, which enhances the spread and effectiveness of local anesthetics administered through the catheter.
DPE anesthesia can provide faster onset, lower dose requirement, and better sacral coverage than epidural anesthesia alone.
-
Paracervical block: This involves injecting local anesthetics (such as lidocaine) into the paracervical area at 3 o’clock and 9 o’clock positions.
Paracervical block provides lack of sensation from the cervix to the lower vagina.
Paracervical block is used mainly for pain relief during the first stage of labor or for cervical dilation before instrumental delivery.
-
Pudendal block: This involves injecting local anesthetics (such as lidocaine) into the pudendal nerve near the ischial spine on both sides.
Pudendal block provides lack of sensation from the lower vagina to the perineum.
Pudendal block is used mainly for pain relief during the second stage of labor or for episiotomy repair.
Nursing Interventions for Pain Management During Labor
Nurses play a vital role in providing pain management during labor. Some of the nursing interventions for pain management during labor are:
-
Assessing pain: Nurses should assess pain regularly using valid and reliable tools, such as numerical rating scales, visual analog scales, or behavioral observation scales. Nurses should also assess pain location, quality, intensity, duration, frequency, and aggravating or relieving factors. Nurses should document pain assessment findings and communicate them to other members of the health care team.
-
Educating patients: Nurses should educate patients about the physiology of labor pain, the options and benefits and risks of nonpharmacologic and pharmacologic pain management methods, and the expected outcomes and potential complications of pain management during labor. Nurses should also respect patients’ preferences and choices regarding pain management and involve them in decision making.
-
Providing nonpharmacologic methods: Nurses should provide nonpharmacologic methods according to patients’ needs and preferences. Nurses should assist patients with continuous labor support, water immersion, upright positioning, relaxation techniques, cutaneous stimulation, or other methods that are available and acceptable. Nurses should also monitor patients’ responses and satisfaction with nonpharmacologic methods and adjust them as needed.
-
Administering pharmacologic methods: Nurses should administer pharmacologic methods according to orders and protocols. Nurses should ensure informed consent, adequate hydration, proper positioning, aseptic technique, correct dosage and route, appropriate timing, and safe administration of pharmacologic methods. Nurses should also monitor patients’ vital signs, fetal heart rate, level of consciousness, level of analgesia, motor function, urinary output, and adverse effects of pharmacologic methods. Nurses should also report any abnormal findings or complications to the health care provider and intervene accordingly.
- Evaluating pain management: Nurses should evaluate pain management regularly using valid and reliable tools, such as numerical rating scales, visual analog scales, or behavioral observation scales. Nurses should also evaluate patients’ satisfaction, comfort, and coping with pain management during labor. Nurses should document pain management evaluation findings and communicate them to other members of the health care team. Nurses should also provide feedback, reinforcement, and encouragement to patients and their support persons regarding pain management during labor.
Conclusion
Pain management during labor is an important aspect of maternal care that affects the maternal experience, outcomes, and satisfaction. Pain perception and preferences for pain management are unique to each woman in labor. Therefore, nurses and health care providers must be knowledgeable about the various pain management modalities and help each woman make informed choices consistent with her personal preferences. Nurses play a vital role in providing pain management during labor by assessing, educating, providing, administering, and evaluating pain management methods.
Summary
-
Pain perception and preferences for pain management are unique to each woman in labor.
-
Pain management during labor affects the maternal experience, outcomes, and satisfaction.
-
Pain management during labor can be divided into nonpharmacologic and pharmacologic methods.
-
Nonpharmacologic methods include continuous labor support, water immersion, upright positioning, relaxation techniques, and cutaneous stimulation.
-
Nonpharmacologic methods are safe, inexpensive, easy to use, have no adverse effects on the mother or the fetus, and can be used in any setting.
-
Nonpharmacologic methods may not provide adequate pain relief for some women, they require active participation from the woman or her support person, and they may not be available or acceptable in some cultures or settings.
-
Pharmacologic methods include systemic analgesics, inhaled analgesia, and regional anesthesia.
-
Pharmacologic methods provide effective, consistent, and predictable pain relief for most women, they do not require active participation from the woman or her support person, and they can be adjusted according to the woman’s needs.
-
Pharmacologic methods may have adverse effects on the mother or the fetus, they may interfere with maternal-fetal bonding, they may require additional monitoring or interventions, and they may not be available or acceptable in some cultures or settings.
-
Regional anesthesia techniques include epidural anesthesia, spinal anesthesia, combined spinal-epidural anesthesia, dural puncture epidural anesthesia, paracervical block, and pudendal block.
-
Regional anesthesia techniques provide lack of sensation in specific regions of the body by blocking nerve impulses from reaching the brain.
-
Regional anesthesia techniques may cause maternal hypotension, bradycardia, fever, itching, urinary retention, or headache.
-
Regional anesthesia techniques may also prolong the second stage of labor, increase the need for oxytocin augmentation or instrumental delivery, or interfere with maternal-fetal bonding.
-
Regional anesthesia techniques should be performed by an anesthesiologist or a certified registered nurse anesthetist under strict aseptic technique.
-
Regional anesthesia techniques should also be accompanied by adequate hydration, monitoring of vital signs and fetal heart rate, and prevention of supine hypotension syndrome by placing a wedge under the right hip.
-
Nurses play a vital role in providing pain management during labor by assessing, educating, providing, administering, and evaluating pain management methods.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Pain Management During Labor
This filled cannot be empty

