Please set your exam date
End-of-life Care and Palliative Care
Study Questions
Introduction to End-of-Life Care and Palliative Care
A nurse is providing end-of-life care for a client who has terminal cancer. The nurse notices that the client's breathing is becoming shallow and irregular. What is the most appropriate action for the nurse to take?
Explanation
D) is the correct answer because staying with the client and providing reassurance can help reduce anxiety and promote comfort during the dying process.
A) is incorrect because oxygen administration is not indicated for clients who are dying unless they have signs of hypoxia or dyspnea.
B) is incorrect because elevating the head of the bed may not improve breathing and may cause discomfort for the client.
C) is incorrect because notifying the physician is not a priority action unless there is a change in the client's condition or wishes.
A client with advanced heart failure is admitted to the hospital for symptom management. The client expresses a desire to receive palliative care instead of aggressive treatments.
What is the best response by the nurse?
Explanation
B) is the correct answer because it reflects the definition and goal of palliative care, which is to provide holistic care for clients with serious illnesses regardless of their prognosis.
A) is incorrect because palliative care can be initiated at any stage of an illness, not only at the end of life.
C) is incorrect because palliative care does not mean giving up on treatment or accepting death, but rather focusing on comfort and quality of life.
D) is incorrect because palliative care does not interfere with current medications and therapies, but rather complements them.
A nurse is part of an interdisciplinary team that provides palliative care for clients with various illnesses.
What is the primary role of the nurse in this team?
Explanation
D) is the correct answer because assessing clients' needs and preferences is the foundation of nursing practice and guides all other interventions in palliative care.
A) is incorrect because prescribing medications and treatments is usually done by physicians or advanced practice nurses, not by registered nurses.
B) is incorrect because coordinating care and communicating with other team members and family members is a shared responsibility among all team members, not only by nurses.
C) is incorrect because providing emotional and spiritual support and counseling is also a shared responsibility among all team members, not only by nurses.
A client who has end-stage renal disease decides to discontinue dialysis and receive hospice care at home. The client's family members are having difficulty accepting the client's decision and ask the nurse to convince the client to change their mind.
What is the most appropriate response by the nurse?
Explanation
D) is the correct answer because it respects the client's autonomy and right to make informed decisions, while also offering support and education for the family members.
A) is incorrect because it may sound dismissive or insensitive to the family members' feelings and concerns.
B) is incorrect because it may sound coercive or judgmental of the client's decision.
C) is incorrect because it may sound biased or disrespectful of the client's decision.
A client who has a terminal illness asks the nurse about the difference between end-of-life care and palliative care. What is the most accurate explanation by the nurse?
Explanation
B) is the correct answer because it reflects the definitions and scopes of end-of-life care and palliative care, as explained in the introduction.
A) is incorrect because end-of-life care and palliative care are not the same thing, but rather end-of-life care is a subset of palliative care.
C) is incorrect because end-of-life care is not defined by a specific prognosis, but rather by the signs and symptoms of imminent death.
D) is incorrect because palliative care does not focus on curing the illness or prolonging life, but rather on improving quality of life and relieving suffering.
Understanding End-of-Life Care and Palliative Care
A nurse is caring for a client who has terminal cancer and is receiving palliative care at home. The client's spouse asks the nurse what palliative care means. Which of the following responses should the nurse make?
A) "Palliative care is a type of care that focuses on relieving your loved one's pain and symptoms, as well as providing emotional and spiritual support for both of you."
B) "Palliative care is a type of care that helps your loved one prepare for death by withdrawing any life-sustaining treatments and medications."
C) "Palliative care is a type of care that aims to cure your loved one's cancer by using aggressive treatments and interventions."
D) "Palliative care is a type of care that involves hospice services and requires your loved one to have a life expectancy of six months or less."
Explanation
Palliative care is a holistic approach to care that focuses on improving the quality of life for clients with serious illnesses and their families. It addresses physical, emotional, social, and spiritual needs, and can be provided at any stage of illness, along with curative treatments.
Option B is incorrect because palliative care does not necessarily involve withdrawing treatments or medications, unless they are causing more harm than benefit.
Option C is incorrect because palliative care does not aim to cure the disease, but rather to manage the symptoms and enhance comfort.
Option D is incorrect because palliative care is not the same as hospice care, which is a specific type of palliative care for clients who have a life expectancy of six months or less and have decided to forego curative treatments.
A client who has advanced heart failure is admitted to the hospital for symptom management. The client tells the nurse that he does not want any resuscitation measures if his heart stops. Which of the following actions should the nurse take?
A) Respect the client's wishes and document them in the medical record.
B) Inform the client that he needs to have a written advance directive to refuse resuscitation.
C) Encourage the client to reconsider his decision and discuss the benefits of resuscitation.
D) Notify the health care provider and request a referral to a palliative care team.
Explanation
The nurse should notify the health care provider and request a referral to a palliative care team, which can help the client and his family explore his goals of care, preferences, values, and beliefs regarding end-of-life care. The palliative care team can also assist with completing an advance directive, which is a legal document that specifies the client's wishes for medical treatment in case he becomes unable to communicate them.
Option A is incorrect because respecting the client's wishes is not enough; the nurse should also ensure that they are communicated to the health care team and documented in an advance directive.
Option B is incorrect because although an advance directive is recommended, it is not required; the client can verbally express his wishes to his health care provider, who can then write a do-not-resuscitate (DNR) order.
Option C is incorrect because it is not appropriate for the nurse to impose her own values or opinions on the client; rather, she should respect his autonomy and support his decision.
A nurse is providing education to a group of nursing students about end-of-life care. Which of the following statements by a nursing student indicates an understanding of the teaching?
Explanation
End-of-life care is based on the ethical principles of beneficence (doing good) and nonmaleficence (doing no harm), which guide the health care team in providing compassionate and respectful care that alleviates suffering and promotes dignity for dying clients.
Option A is incorrect because end-of-life care can be provided in various settings, such as hospitals, nursing homes, or home health agencies, depending on the client's needs and preferences.
Option C is incorrect because informed consent is not required for end-of-life care; however, it may be needed for specific treatments or procedures that are part of end-of-life care, such as pain medication, blood transfusions, or organ donation.
Option D is incorrect because end-of-life care does not necessarily include interventions such as artificial nutrition and hydration, which may be considered futile or burdensome for some clients; rather, the decision to use or withhold these interventions should be based on the client's wishes, values, and goals of care.
A client who has a terminal illness and is receiving hospice care at home has a prescription for morphine sulfate 10 mg PO every 4 hr PRN for pain. The client's family member tells the nurse that the client is experiencing increased pain and asks if he can give him more morphine.
Which of the following responses should the nurse make?
Explanation
The nurse should instruct the family member to call the hospice nurse first to get an order for a higher dose of morphine, if needed. The hospice nurse can assess the client's pain level, vital signs, and response to the medication, and adjust the dose accordingly.
Option A is incorrect because although respiratory rate is one of the factors to monitor when administering opioids, it is not the only one; other factors include level of consciousness, oxygen saturation, and presence of adverse effects. Moreover, the family member should not increase the dose of morphine without consulting the hospice nurse.
Option B is incorrect because although respiratory depression is a potential side effect of opioids, it is not a common cause of death in clients receiving palliative care; rather, opioids are considered safe and effective for managing pain and dyspnea in dying clients, as long as they are prescribed and administered appropriately.
Option D is incorrect because tolerance and dependence are not major concerns in clients receiving palliative care; rather, the goal is to provide adequate pain relief and comfort for the client.
A client who has a do-not-resuscitate (DNR) order is admitted to the hospital for pneumonia. The client's condition deteriorates and he becomes unresponsive. The nurse notices that his heart rate is dropping and his blood pressure is low.
Which of the following actions should the nurse take?
Explanation
The nurse should continue to provide comfort measures and emotional support to the client, as well as respect his DNR order, which means that no resuscitation measures should be attempted if he experiences cardiac or respiratory arrest.
Option A is incorrect because initiating CPR and calling a code blue would violate the client's DNR order and his right to refuse treatment.
Option B is incorrect because administering oxygen via nasal cannula may be considered a form of resuscitation, depending on the client's wishes and goals of care; moreover, monitoring his vital signs may not be necessary or beneficial at this stage of his illness. Option C is incorrect because notifying the health care provider and the client's family of his status may not be a priority at this time; rather, the nurse should focus on providing compassionate care to the client until he dies.
Communication and Advance Care Planning
A nurse is caring for a client who has terminal cancer and is receiving palliative care at home. The client's spouse tells the nurse that they do not want to discuss advance directives with the client because they are afraid of upsetting them.
Which of the following responses should the nurse make?
Explanation
The nurse should encourage the spouse to communicate with the client about their preferences for end-of-life care, and express their love and support. This can help the client feel more comfortable and respected, and reduce the risk of conflicts or regrets later on.
Answer A is incorrect because it does not respect the client's autonomy or right to make informed decisions about their own care.
Answer C is incorrect because it may delay or prevent important conversations that need to happen before the client's condition worsens.
Answer D is incorrect because it violates the client's legal and ethical rights, and may cause resentment or anger from the client.
A client who has a terminal illness tells the nurse that they want to have a do-not-resuscitate (DNR) order in their medical record. The nurse knows that the client's family is opposed to this decision and has tried to persuade the client to change their mind.
Which of the following actions should the nurse take?
Explanation
The nurse should document the client's decision in the medical record and notify the health care team, as this is part of their professional responsibility and legal obligation. The nurse should also respect and support the client's autonomy and right to self-determination, even if it differs from their own or their family's values or beliefs.
Answer A is incorrect because it may cause conflict or distress for both the client and their family, and it is not within the nurse's scope of practice to mediate such issues.
Answer C is incorrect because it may imply that the nurse does not respect or accept the client's decision, and it may interfere with their dignity or quality of life.
Answer D is incorrect because it may suggest that the nurse thinks that there is something wrong with the client's decision, or that they need to be convinced otherwise.
A nurse is providing education to a group of clients who have chronic illnesses about advance care planning. Which of the following information should the nurse include in the teaching?
Explanation
Advance care planning can be revised or updated at any time by the client or their designated surrogate, as long as they have decision-making capacity and communicate their wishes clearly. This allows for flexibility and adaptation to changing circumstances or preferences.
Answer A is incorrect because advance care planning is recommended for all adults, regardless of their health status or prognosis, as it can help them prepare for future situations and ensure that their values and goals are respected.
Answer B is incorrect because advance care planning involves more than just making decisions about life-sustaining treatments and organ donation; it also includes expressing one's values, beliefs, preferences, fears, hopes, and expectations for end-of-life care, as well as identifying a surrogate decision-maker and communicating with one's family and health care team.
Answer C is incorrect because advance care planning does not require a written document, although it is advisable to have one; it can also be done verbally or through other means, such as videos or audio recordings.
A client who has a progressive neurological disorder tells the nurse that they want to have a physician-assisted death (PAD) when their condition becomes intolerable. The nurse is uncomfortable with this request and does not agree with the client's decision.
Which of the following responses should the nurse make?
Explanation
The nurse should acknowledge the client's decision and express empathy and understanding, without imposing their own values or judgments. The nurse should also explore the client's reasons, feelings, concerns, and expectations for having a PAD, and provide information, education, and support as needed.
Answer A is incorrect because it may make the client feel rejected, guilty, or ashamed, and it does not address the client's needs or concerns.
Answer C is incorrect because it may make the client feel invalidated, stigmatized, or patronized, and it does not respect the client's autonomy or dignity.
Answer D is incorrect because it may make the client feel abandoned, isolated, or betrayed, and it does not facilitate communication or continuity of care.
A nurse is reviewing the medical record of a client who has end-stage renal disease and is receiving palliative care. The nurse notes that the client has an advance directive that states that they do not want dialysis or any other form of renal replacement therapy.
However, the nurse also notes that the client's spouse is the designated surrogate decision-maker and has consented to start dialysis for the client.
Which of the following actions should the nurse take?
Explanation
The nurse should inform the health care provider of the discrepancy between the client's advance directive and the spouse's consent, and request clarification on how to proceed. The health care provider should then discuss the situation with the spouse and explain their role and responsibilities as a surrogate decision-maker, as well as the benefits and burdens of dialysis for the client. The health care provider should also try to resolve any conflicts or misunderstandings that may exist between the client's wishes and the spouse's beliefs or values.
Answer A is incorrect because it does not respect the client's advance directive or their right to self-determination, and it may cause harm or suffering to the client.
Answer B is incorrect because it may delay or complicate the decision-making process, and it may not be necessary unless there is a serious ethical dilemma or legal dispute that cannot be resolved by other means.
Answer C is incorrect because it is not within the nurse's scope of practice to educate or persuade the spouse about the client's advance directive or its implications; this should be done by the health care provider or another qualified professional.
A client who has a terminal illness and is receiving palliative care expresses a wish to die at home. The client's family members are reluctant to agree, as they are concerned about their ability to provide care and cope with the situation. Which of the following actions should the nurse take?
Explanation
The nurse should explore the reasons for the family's reluctance and provide education and support, as this can help address their concerns and fears, and facilitate decision-making that respects the client's wishes and values. The nurse should also inform the family about the availability and benefits of home hospice care, which can provide medical, nursing, social, spiritual, and bereavement services for the client and the family at home.
Incorrect answers:
A) The nurse should not respect the client's wish and arrange for home hospice care without involving the family in the decision, as this may cause conflict and resentment among the family members, and compromise the quality of care and comfort for the client. The nurse should respect the client's autonomy, but also consider the family's perspectives and needs, and promote effective communication and collaboration among all parties.
C) The nurse should not suggest a compromise and recommend a palliative care unit in a hospital or facility without exploring the client's preferences and goals of care, as this may disregard
the client's autonomy and dignity. The nurse should respect the client's wish to die at home, unless there are compelling reasons to suggest otherwise, such as safety issues or lack of resources.
D) The nurse should not refer the client and the family to a social worker or a chaplain for counseling without first assessing their needs and preferences, as this may imply that the nurse is avoiding or delegating the issue, or imposing unwanted services on them. The nurse should provide emotional support and reassurance to the client and the family, and offer referrals to other professionals or resources as appropriate.
A client who has chronic obstructive pulmonary disease (COPD) and is receiving palliative care develops a fever of 38.5°C (101.3°F), productive cough, and increased dyspnea. The nurse suspects that the client has a respiratory infection. Which of the following actions should the nurse take?
Explanation
T
he nurse should initiate antibiotic therapy as prescribed for a client who has COPD and develops signs of a respiratory infection, such as fever, productive cough, and increased dyspnea. Antibiotics can help treat the infection and prevent complications such as sepsis or respiratory failure.
Incorrect answers:
A) The nurse should not obtain a sputum culture and sensitivity test for a client who has COPD and develops signs of a respiratory infection, as this is not necessary or appropriate in palliative care. The goal of palliative care is to relieve symptoms and improve quality of life, not to diagnose or cure diseases. A sputum culture and sensitivity test may cause discomfort or distress for
the client, and delay treatment.
B) The nurse should not administer acetaminophen as prescribed for a client who has COPD
and develops signs of a respiratory infection, as this is not sufficient or effective in managing
the condition. Acetaminophen may help reduce fever, but it does not address the underlying cause of infection or relieve other symptoms such as cough or dyspnea.
D) The nurse should not increase fluid intake as tolerated for a client who has COPD and develops signs of a respiratory infection, as this may worsen dyspnea or cause fluid overload. Fluid intake should be individualized
Symptom Management in Palliative Care
A nurse is caring for a client who has terminal cancer and is experiencing severe pain. The client has a prescription for morphine sulfate 10 mg IV every 4 hr PRN for pain. The nurse notes that the client's pain level is 8/10 on a numeric rating scale and administers the medication. Which of the following actions should the nurse take next?
Explanation
The nurse should monitor the client's respiratory rate and level of consciousness after administering an opioid analgesic, as these are indicators of potential adverse effects such as respiratory depression and sedation. This is a priority action according to the airway, breathing, circulation (ABC) framework.
Incorrect answers:
A) The nurse should assess the client's pain level after 15 min, but this is not the priority action. The nurse should first ensure that the client's airway and breathing are not compromised by the medication.
B) The nurse should document the administration and the client's response, but this is not the priority action. Documentation is important, but it does not take precedence over monitoring for adverse effects.
D) The nurse should educate the client about nonpharmacological pain relief methods, but this is not the priority action. Education is part of holistic care, but it does not address the immediate need of managing pain and preventing complications.
A client who has advanced amyotrophic lateral sclerosis (ALS) is receiving palliative care at home. The client has dysphagia and is at risk for aspiration. The client's spouse asks the nurse how to prevent aspiration when feeding the client. Which of the following responses should the nurse make?
Explanation
The nurse should instruct the spouse to position the client upright during and after feeding, as this facilitates swallowing and reduces the risk of aspiration. This is an evidence-based practice that promotes safety and comfort for the client.
Incorrect answers:
A) The nurse should not advise the spouse to thicken liquids to a honey-like consistency before giving them to the client, as this may increase the difficulty of swallowing and cause choking or aspiration. The appropriate consistency of liquids depends on the individual client's needs and preferences, and should be determined by a speech-language pathologist.
C) The nurse should not suggest that the spouse offer small bites of soft foods and encourage chewing well, as this may be too challenging for a client who has dysphagia due to ALS. The client may have impaired oral motor function and muscle weakness that prevent effective chewing and swallowing. The appropriate texture of foods depends on the individual client's needs and preferences, and should be determined by a speech-language pathologist.
D) The nurse should not recommend that the spouse check the client's mouth for pocketing of food after each bite, as this may be invasive and uncomfortable for
the client. The spouse should observe for signs of difficulty swallowing or aspiration, such as coughing, choking, drooling, or changes in voice quality.
Psychosocial and Spiritual Care
A nurse is caring for a client who is receiving palliative care for terminal cancer. The client expresses anger and resentment about their condition and questions the meaning of life. How should the nurse respond?
Explanation
The nurse should use open-ended questions to explore the client's feelings and beliefs about their condition and the meaning of life. This can help the client to express their emotions, identify their sources of strength and hope, and cope with their situation.
Incorrect options:
A) "You have every right to feel angry. This is not fair." - This is an empathic statement, but it does not encourage further communication or exploration of the client's feelings. It may also reinforce the client's negative emotions and sense of hopelessness.
B) "I understand how you feel. I have lost many loved ones to cancer." - This is an attempt to show empathy, but it is not appropriate to share personal experiences or compare the client's situation to others. This may make the client feel invalidated or minimized.
C) "Maybe you should talk to a spiritual counselor. They can help you find some peace." - This is a suggestion that may be helpful for some clients, but it should not be imposed on the client without assessing their willingness or preference for spiritual support. It may also imply that the nurse is avoiding the client's feelings or imposing their own beliefs.
A client who is in hospice care for end-stage heart failure tells the nurse that they are afraid of dying and what will happen after death. Which intervention is most appropriate for the nurse to implement?
Explanation
The nurse should assess the client's spiritual beliefs and values and provide support that is consistent with them. This can help the client to cope with their fears, find comfort and hope, and achieve a sense of closure.
Incorrect options:
A) Provide reassurance that death is a natural part of life and that they will not suffer. - This is a general statement that may not address the client's specific concerns or questions about death and the afterlife. It may also contradict the client's beliefs or expectations.
C) Administer prescribed sedatives or analgesics to relieve the client's anxiety or pain. - This is an intervention that may be necessary to manage the client's physical symptoms, but it does not address the underlying psychological or spiritual issues that are causing the fear of dying.
D) Refer the client to a mental health professional for counseling and therapy. - This is an intervention that may be beneficial for some clients, but it should not be done without assessing the client's readiness or preference for this type of support. It may also imply that the nurse is unable to handle the client's emotions or that the fear of dying is abnormal.
A nurse is conducting a psychosocial assessment of a client who has been diagnosed with a terminal illness. Which question should the nurse ask to assess the client's social support system?
Explanation
The nurse should ask about the people that the client can count on for help or comfort, such as family members, friends, neighbors, or community groups. This can help to identify the client's social support system, which is an important factor in coping with a terminal illness.
Incorrect options:
B) "How do you spend your free time when you are not in treatment?" - This is a question that can assess the client's hobbies, interests, or activities, but it does not directly address their social support system.
C) "What are some of the goals that you have for yourself and your family?" - This is a question that can assess the client's hopes, dreams, or plans, but it does not directly address their social support system.
D) "How do you cope with stress or difficult emotions?" - This is a question that can assess the client's coping strategies, but it does not directly address their social support system.
A client who is receiving palliative care for advanced lung cancer tells the nurse that they have lost their faith in God and feel abandoned and alone. Which response by the nurse is most appropriate?
Explanation
The nurse should acknowledge the client's feelings and use open-ended questions to explore their faith and how it has changed. This can help the client to express their doubts, fears, or anger, and to find meaning and hope in their situation.
Incorrect options:
B) "Don't say that. God loves you and has a plan for you. You just need to trust Him." - This is a response that may reflect the nurse's own beliefs, but it does not respect the client's feelings or perspective. It may also make the client feel guilty, judged, or misunderstood.
C) "Maybe you should try to pray more or read some inspirational books. They might help you feel better." - This is a response that may suggest some possible sources of comfort or guidance, but it does not address the client's feelings or concerns. It may also imply that the client is not doing enough to maintain their faith or that their faith is the cause of their distress.
D) "I can see that this is very hard for you. Would you like me to contact a chaplain or a spiritual leader for you?" - This is a response that may offer some professional support, but it does not explore the client's faith or how it has changed. It may also be premature or unwanted by the client without assessing their readiness or preference for spiritual assistance.
A nurse is providing education to a client who is considering hospice care for end-of-life care. Which statement by the nurse is accurate?
Explanation
Hospice care is a type of palliative care that provides comprehensive services to meet the needs of clients who are terminally ill and have a life expectancy of six months or less. Hospice care aims to improve the quality of life of clients and their families by providing pain and symptom management, emotional and spiritual support, bereavement counseling, and other services.
Incorrect options:
A) "Hospice care focuses on curing your disease and prolonging your life as much as possible." - This is an inaccurate statement, as hospice care does not focus on curing the disease or prolonging life, but rather on enhancing comfort and dignity.
C) "Hospice care requires that you give up all other treatments and medications for your condition." - This is an inaccurate statement, as hospice care does not require that clients give up all other treatments or medications, but rather that they accept that their condition is incurable and that they do not seek aggressive or futile interventions.
D) "Hospice care can only be provided in a hospital or a nursing home setting." - This is an inaccurate statement, as hospice care can be provided in various settings, including the client's home, a hospice facility, an assisted living facility, or a hospital.
Ethical and Legal Considerations in End-of-Life Care
A nurse is caring for a client who has terminal cancer and is receiving hospice care at home. The client's spouse asks the nurse to administer a higher dose of morphine to the client to hasten death. What is the nurse's best response?
Explanation
The nurse should empathize with the spouse's grief, but refuse to administer a higher dose of morphine to the client to hasten death. This would be considered active euthanasia, which is illegal and violates the ethical principles of beneficence and nonmaleficence.
Incorrect options:
B) "I will contact the hospice physician and ask for a prescription for a higher dose of morphine." - This is an incorrect response, as the nurse should not seek a prescription for a higher dose of morphine without the client's consent and without a valid indication. This could also be seen as an attempt to facilitate euthanasia.
C) "I will report you to the authorities for requesting euthanasia." - This is an incorrect response, as the nurse should not threaten or intimidate the spouse for expressing their feelings. The nurse should provide support and education to the spouse and respect their right to autonomy.
D) "I will discuss your request with the client and respect their wishes." - This is an incorrect response, as the nurse should not involve the client in a decision that is illegal and unethical. The nurse should protect the client's rights and dignity and advocate for their best interests.
A client who has amyotrophic lateral sclerosis (ALS) has an advance directive that states they do not want any life-sustaining measures, including artificial nutrition and hydration, if they become unable to make decisions for themselves. The client's family disagrees with this decision and asks the nurse to insert a feeding tube in the client. What should the nurse do?
A) Insert the feeding tube in the client, as the family has the right to make decisions for the client.
B) Refuse to insert the feeding tube in the client, as the advance directive is legally binding and must be honored.
C) Consult with the ethics committee and seek a resolution that respects both the client's and the family's wishes.
D) Ask the physician to override the advance directive and order artificial nutrition and hydration for the client.
Explanation
The nurse should respect the client's autonomy and follow their advance directive, which is a legal document that expresses their wishes regarding end-of-life care. The nurse should not insert a feeding tube in the client, as this would violate their right to self-determination and informed consent.
Incorrect options:
A) Insert the feeding tube in the client, as the family has the right to make decisions for the client. - This is an incorrect option, as the family does not have the right to make decisions for the client that are contrary to their advance directive. The family should be educated about the purpose and scope of the advance directive and supported in coping with their emotions.
C) Consult with the ethics committee and seek a resolution that respects both
the client's and the family's wishes. - This is an incorrect option, as there is no need to consult with the ethics committee when there is a clear advance directive that states the client's wishes. The ethics committee can be involved if there is a conflict or uncertainty about the interpretation or validity of the advance directive.
D) Ask the physician to override the advance directive and order artificial nutrition and hydration for the client. - This is an incorrect option, as the physician cannot override the advance directive without the client's consent or a court order. The physician should respect the client's autonomy and follow their advance directive.
A nurse is providing palliative care to a client who has end-stage heart failure. The client tells the nurse that they want to donate their organs after death. What should the nurse do?
Explanation
Rationale: The nurse should document the client's request and notify the organ Procurement organization, which is responsible for evaluating the client's eligibility, obtaining consent, and coordinating the donation process. The nurse should respect
the client's autonomy and support their decision.
Incorrect options:
A) Encourage the client to discuss their decision with their family and obtain their consent. - This is an incorrect option, as the client does not need their family's consent to donate their organs. The client has the right to make decisions about their own body and health care. The nurse should encourage the client to inform their family of their decision, but not pressure them to do so.
B) Inform the client that they are not eligible for organ donation due to their medical condition. - This is an incorrect option, as the nurse is not qualified to determine
the client's eligibility for organ donation. The nurse should not discourage or misinform the client about organ donation. The nurse should refer the client to the organ procurement organization, which will assess the client's suitability and availability of organs.
D) Explain the process and risks of organ donation to the client and obtain their informed consent. - This is an incorrect option, as the nurse is not responsible for obtaining informed consent for organ donation. The nurse should provide general information and education to the client about organ donation, but not go into details or risks that are beyond their scope of Practice. The nurse should refer the client to the organ procurement organization, which will obtain informed consent from the client or their designated representative.
A client who has a do-not-resuscitate (DNR) order is admitted to the hospital with pneumonia. The client develops respiratory distress and requires intubation and mechanical ventilation. The nurse notices that the DNR order is not documented in the electronic health record (EHR). What should the nurse do?
Explanation
Rationale: The nurse should verify the DNR order with the client or their surrogate decision-maker and document it in the EHR before proceeding. The nurse should ensure that the DNR order is clear, current, and consistent with the client's wishes and goals of care. The nurse should also communicate the DNR order to other members of the health care team.
Incorrect options:
A) Intubate and ventilate the client, as the DNR order is not valid without documentation in the EHR. - This is an incorrect option, as intubating and ventilating the client would violate their right to refuse treatment and die naturally. The DNR order is valid even if it is not documented in the EHR, as long as it is written by a physician and signed by the client or their surrogate decision-maker.
B) Contact the physician who wrote the DNR order and ask them to enter it in the EHR as soon as possible. - This is an incorrect option, as contacting the physician who wrote the DNR order would delay providing appropriate care to the client. The nurse should verify and document the DNR order themselves, as they are accountable for following it.
C) Refuse to intubate and ventilate the client, as the DNR order is valid regardless of documentation in the EHR. - This is an incorrect option, as refusing to intubate and ventilate the client without verifying and documenting the DNR order would put the nurse at risk of legal liability and professional misconduct. The nurse should ensure that there is evidence of the DNR order in the EHR before acting on it.
Family and Caregiver Support
A nurse is assessing a client who is a caregiver for his spouse with Alzheimer's disease. The nurse notices that the client has lost weight, appears fatigued, and reports feeling overwhelmed. What is the priority nursing intervention for this client?
Explanation
Rationale: The client is showing signs of caregiver stress, which can lead to depression and increased risk of suicide. The priority nursing intervention is to assess the client's mental health status and provide appropriate referrals and interventions as needed.
Incorrect options:
A) Refer the client to a support group for caregivers. - This is an appropriate intervention, as support groups can provide emotional and social support, as well as information and resources, for caregivers. However, this is not the priority intervention, as the client's mental health needs to be addressed first.
B) Educate the client on the stages and progression of Alzheimer's disease. - This is an appropriate intervention, as education can help the client understand and cope with the challenges of caring for a spouse with Alzheimer's disease. However, this is not the priority intervention, as the client's mental health needs to be addressed first.
C) Arrange for respite care services for the client's spouse. - This is an appropriate intervention, as respite care can provide temporary relief and assistance for caregivers, allowing them to rest and attend to their own needs. However, this is not the priority intervention, as the client's mental health needs to be addressed first.
A client who is a single parent of three children tells the nurse that they have been feeling stressed and overwhelmed lately. The client says that they have no one to help them with childcare or household chores. Which of the following statements by the nurse is most appropriate?
Explanation
Rationale: The client is experiencing chronic stress, which can have negative effects on their physical and mental health. The nurse should suggest professional counseling services, which can provide emotional support, coping strategies, and referrals to other resources that may help the client.
Incorrect options:
A) "You should try to find some time for yourself every day." - This is a helpful suggestion, as self-care is important for reducing stress and enhancing well-being. However, this statement may not be realistic or feasible for the client, who may not have any available time or resources to do so.
B) "You are doing a great job managing everything on your own." - This is a supportive statement, as it acknowledges the client's efforts and challenges. However, this statement may not address the client's needs or concerns, and may imply that they do not need any help or assistance.
C) "You need to prioritize your tasks and delegate what you can." - This is a practical suggestion, as prioritizing and delegating tasks can help reduce stress and workload. However, this statement may not be helpful or appropriate for the client, who may not have anyone to delegate to or may feel guilty or inadequate for doing so.
A nurse is caring for a client who has terminal cancer and has decided to stop treatment and enter hospice care. The client's family members express anger and disbelief at the client's decision. How should the nurse respond?
Explanation
Rationale: The nurse should use active listening and empathy skills to acknowledge and validate the family members' feelings, without judging or dismissing them. The nurse should also avoid giving advice or opinions that may conflict with the client's wishes.
Incorrect options:
A) "I understand how you feel, but you have to respect your loved one's wishes." - This statement may sound patronizing or insensitive, as it implies that the nurse knows how the family members feel and that they are not respecting the client's wishes. The nurse should avoid using "but" statements, as they can negate or minimize the previous statement.
C) "Why are you angry? Don't you want your loved one to be comfortable?" - This statement may sound accusatory or defensive, as it questions the family members' motives and emotions. The nurse should avoid using "why" questions, as they can sound confrontational or judgmental.
D) "You should talk to your loved one and try to change their mind." - This statement may sound disrespectful or inappropriate, as it suggests that the nurse does not support the client's decision and that the family members should persuade the client otherwise. The nurse should avoid giving unsolicited advice or opinions that may interfere with the client's autonomy and dignity.
A client who is a refugee from a war-torn country tells the nurse that they have nightmares, flashbacks, and difficulty sleeping. The client says that they do not want to talk about their past experiences or seek any help. What is the best response by the nurse?
Explanation
Rationale: The nurse should use a trauma-informed approach, which involves providing safety, trust, choice, collaboration, and empowerment to the client. The nurse should express empathy and compassion, without assuming or labeling the client's diagnosis or condition. The nurse should also offer options and resources, without imposing or forcing them on the client.
Incorrect options:
A) "You are suffering from post-traumatic stress disorder (PTSD). You need to see a psychiatrist as soon as possible." - This statement may sound alarming or stigmatizing, as it labels the client's condition and prescribes a specific treatment without involving the client in the decision-making process. The nurse should avoid making assumptions or diagnoses based on limited information.
B) "You have been through a lot of trauma. It is normal to have these symptoms. They will go away with time." - This statement may sound dismissive or minimizing, as it normalizes the client's symptoms and does not acknowledge the impact or severity of their trauma. The nurse should avoid making generalizations or predictions about the client's recovery.
D) "You are in denial. You have to face your past and deal with it. Otherwise, you will never heal." - This statement may sound harsh or blaming, as it criticizes the client's coping mechanism and implies that they are responsible for their own healing. The nurse should avoid using guilt-tripping or shaming tactics that may damage the therapeutic relationship.
A nurse is conducting a home visit for a client who has a newborn baby. The nurse observes that the client's partner is verbally abusive and controlling towards the client. The partner does not allow the client to leave the house or talk to anyone without their permission. The partner also refuses to let the nurse talk to the client privately. What is the most appropriate action by the nurse?
Explanation
Rationale: The nurse should recognize that the client is in an abusive relationship and may be at risk of harm or retaliation if they try to leave or seek help. The nurse should provide discreet and confidential support to the client, without alerting or provoking the partner. The nurse should also give the client information and resources that may help them escape or cope with their situation.
Incorrect options:
A) Confront the partner and tell them that their behavior is unacceptable and abusive. - This action may be dangerous or counterproductive, as it may escalate the partner's anger or violence towards the client or the nurse. The nurse should avoid confronting or challenging the partner, as this may jeopardize their safety or trust.
B) Ignore the partner and focus on providing education and care to the client and the baby. - This action may be ineffective or unethical, as it may ignore or enable the partner's abuse towards the client. The nurse should not overlook or disregard signs of domestic violence, as this can put the client and the baby at further risk.
C) Report the partner to the authorities for domestic violence and child abuse. - While reporting the partner to the authorities may be necessary in some cases, it is not the most appropriate immediate action for the nurse in this situation. The nurse should prioritize the safety and well-being of the client and the baby and provide them with resources to seek help and support.
The nurse's primary responsibility is to ensure the safety and well-being of the client and the baby. By giving the client a phone number for a domestic violence hotline and asking them to call when they are safe, the nurse provides them with a confidential resource that can offer guidance, support, and help in planning a safe exit from the abusive situation. It allows the client to reach out for assistance when they feel ready and secure enough to do so.
Bereavement and Grief Support
A nurse is caring for a client who has just experienced the loss of a spouse. Which of the following actions should the nurse take to facilitate the grieving process?
Explanation
Rationale: The nurse should encourage the client to express their feelings and emotions, as this can help them cope with the loss and work through the stages of grief. Suppressing or denying emotions can prolong or complicate the grieving process.
Incorrect options:
B) Advise the client to avoid reminders of their spouse for a while. - This is an incorrect action, as avoiding reminders of the spouse can hinder the acceptance of the loss and delay the resolution of grief. The nurse should help the client to acknowledge and honor the memories of their spouse, not avoid them.
C) Suggest the client to join a support group as soon as possible. - This is an incorrect action, as joining a support group may not be appropriate or helpful for every client. The nurse should assess the client's readiness and willingness to participate in a support group, and respect their preferences and choices. Some clients may prefer individual counseling or informal support from family and friends.
D) Tell the client that time will heal their pain and sorrow. - This is an incorrect action, as telling the client that time will heal their pain and sorrow can minimize or invalidate their feelings and experiences. The nurse should acknowledge and empathize with the client's pain and sorrow, and avoid clichés or platitudes that may sound insensitive or dismissive.
A client is receiving hospice care at home for terminal cancer. The client's family members are present and providing care. A nurse visits the client regularly to monitor their condition and provide support. The nurse observes that the family members are showing signs of anticipatory grief, such as anxiety, depression, anger, and guilt. Which of the following interventions should the nurse implement to assist the family members?
Explanation
Rationale: The nurse should provide opportunities for the family members to share their feelings and concerns, as this can help them cope with anticipatory grief and prepare for the impending loss. The nurse should listen actively and empathically, and validate their emotions.
Incorrect options:
A) Encourage the family members to focus on the positive aspects of the situation. - This is an incorrect intervention, as encouraging the family members to focus on the positive aspects of the situation can deny or minimize their negative emotions and experiences. The nurse should acknowledge and respect both positive and negative aspects of the situation, and avoid imposing unrealistic optimism or expectations on the family members.
B) Educate the family members about the signs and stages of dying. - This is an incorrect intervention, as educating the family members about the signs and stages of dying may not be helpful or appropriate at this time. The nurse should assess the family members' level of knowledge and understanding about the dying process, and provide information only if they request it or consent to it. Some family members may not be ready or willing to learn about this topic, as it may increase their anxiety or distress.
C) Refer the family members to a mental health professional for counseling. - This is an incorrect intervention, as referring the family members to a mental health professional for counseling may not be necessary or beneficial for every family member. The nurse should assess the family members' coping skills and resources, and offer referrals only if they indicate a need or interest in counseling. Some family members may prefer other sources of support, such as spiritual leaders, friends, or community groups.
A nurse is conducting a bereavement follow-up call with a client who lost their partner six months ago. The client reports that they still feel sad and lonely, but they have resumed some of their normal activities, such as going to work, socializing with friends, and volunteering at a local shelter. The client also says that they have started dating someone new, but they feel guilty about it. How should the nurse respond?
Explanation
Rationale: The nurse should respond in a way that acknowledges and validates the client's feelings, and reassures them that they are coping well with their loss. The nurse should also help the client to understand that dating someone new does not mean that they are betraying or forgetting their partner, and that they have the right to pursue happiness and intimacy.
Incorrect options:
A) "It sounds like you are moving on with your life. That's good." - This is an incorrect response, as it implies that the client is leaving their partner behind or erasing their memory. The nurse should avoid using the term "moving on", as it can sound insensitive or dismissive of the client's grief. The nurse should use the term "moving forward" instead, as it conveys a sense of continuity and respect for the past relationship.
B) "It's normal to feel guilty about dating someone new. You should talk to your partner's family and friends about it." - This is an incorrect response, as it suggests that the client needs permission or approval from their partner's family and friends to date someone new. The nurse should respect the client's autonomy and privacy, and avoid interfering with their personal decisions. The nurse should also avoid implying that the client's guilt is normal or justified, as it can reinforce their negative feelings and beliefs.
D) "It's too soon to date someone new. You should wait until you are completely over your partner." - This is an incorrect response, as it imposes a rigid timeline or expectation on the client's grieving process. The nurse should recognize that grief is individual and variable, and that there is no right or wrong time to date someone new. The nurse should also avoid implying that the client will ever be completely over their partner, as this can deny or minimize the significance of their past relationship.
A client is admitted to the hospital for a surgical procedure. The client tells the nurse that they are worried about the surgery, as they have a history of complications from anesthesia. The client also reveals that they lost their sibling a year ago due to a surgical error. The nurse suspects that the client is experiencing unresolved grief. Which of the following findings supports this suspicion?
Explanation
Rationale: The nurse should suspect that the client is experiencing unresolved grief if they avoid talking about their sibling or the surgery, as this can indicate denial, repression, or isolation of their feelings and thoughts. Unresolved grief can interfere with the client's emotional and physical well-being, and increase their risk of complications from surgery.
Incorrect options:
A) The client expresses anger and resentment towards the health care system. - This is not a finding that supports the suspicion of unresolved grief, as expressing anger and resentment towards the health care system can be a normal and healthy reaction to the loss of a sibling due to a surgical error. Anger is one of the stages of grief, and expressing it can help the client cope with the injustice and pain of the loss.
B) The client keeps a photo of their sibling on their bedside table. - This is not a finding that supports the suspicion of unresolved grief, as keeping a photo of their sibling on their bedside table can be a positive and adaptive way of honoring and remembering their sibling. Maintaining a connection with the deceased loved one can help the client accept and integrate the loss into their life.
C) The client requests a visit from a chaplain before the surgery. - This is not a finding that supports the suspicion of unresolved grief, as requesting a visit from a chaplain before the surgery can be a sign of spiritual coping and seeking comfort and guidance from a higher power. Spirituality can be an important source of support and meaning for the client during times of stress and uncertainty.
Cultural Competence in End-of-Life Care
A nurse is caring for a client who is terminally ill and has expressed a wish to die at home. The client's family members are reluctant to honor this wish, as they are concerned about the quality of care and the emotional burden. What is the best action for the nurse to take in this situation?
Explanation
Rationale: The nurse should explore the cultural and religious beliefs of the client and the family members regarding end-of-life care, as these may influence their preferences and expectations. The nurse should also respect the client's autonomy and dignity, but also acknowledge the family's role and involvement in decision-making. The nurse should facilitate open communication and provide information and support to both the client and the family, while avoiding imposing their own values or judgments.
Incorrect options:
A) Respect the client's autonomy and arrange for hospice care at home. - This option may be appropriate if the client's wish is consistent with their cultural and religious beliefs, and if the family members are supportive or agreeable. However, this option does not address the potential conflict or misunderstanding between the client and the family, nor does it consider their emotional needs.
B) Educate the family members about the benefits of palliative care in a hospital setting. - This option may be informative, but it may also be perceived as dismissive or insensitive to the client's wish or to the family's concerns. The nurse should not assume that palliative care in a hospital setting is superior or preferable to home care, as this may depend on various factors, including cultural and religious beliefs.
C) Encourage the family members to discuss their feelings and concerns with the client. - This option may be helpful, but it may also be premature or inappropriate if the nurse has not explored the cultural and religious beliefs of the client and the family first. The nurse should not assume that direct communication is always desirable or acceptable, as some cultures may value indirect or nonverbal communication, or may defer to elders or authorities in decision-making.
A nurse is conducting a cultural assessment of a client who has recently immigrated from India. The client reports that they practice Hinduism and follow a vegetarian diet. Which question should the nurse ask next to obtain more information about the client's dietary preferences?
Explanation
Rationale: The nurse should ask if the client eats eggs or dairy products, as this can help to determine what type of vegetarian diet they follow. Some vegetarians may consume eggs or dairy products (lacto-ovo vegetarians), while others may avoid them (vegan vegetarians). The nurse should also be aware that some Hindus may consider eggs as non-vegetarian, while others may not.
Incorrect options:
B) "Do you have any food allergies or intolerances?" - This question is relevant, but it is not specific to the client's cultural background or religious beliefs. The nurse should ask this question after obtaining more information about the client's dietary preferences based on their culture and religion.
C) "Do you fast on certain days or occasions?" - This question is pertinent, but it is not directly related to the client's vegetarian diet. The nurse should ask this question after establishing what type of vegetarian diet the client follows, as fasting may affect their nutritional intake and needs.
D) "Do you use any herbs or spices in your cooking?" - This question is interesting, but it is not essential to understand the client's dietary preferences. The nurse should ask this question after exploring what foods the client eats or avoids based on their culture and religion.
A nurse is providing end-of-life care to a client who identifies as Jewish. The client's spouse asks the nurse to remove all medical equipment from the room before the client dies, as they believe that this will allow the soul to depart peacefully. How should the nurse respond to this request?
Explanation
Rationale: The nurse should acknowledge and accommodate the spouse's request, as it is based on the client's cultural and religious beliefs. The nurse should also recognize that the spouse is acting as the client's advocate and surrogate decision-maker, as some Jewish traditions may assign this role to the closest family member. The nurse should collaborate with the interdisciplinary team and follow the ethical principles of beneficence, nonmaleficence, autonomy, and justice.
Incorrect options:
A) "I'm sorry, but I cannot do that. It is against hospital policy to remove medical equipment without a doctor's order." - This response is insensitive and dismissive of the spouse's request and the client's beliefs. The nurse should not use hospital policy as an excuse to deny or delay culturally competent care.
B) "I understand your request, but I need to check with the client first. It is their right to decide what kind of care they want to receive." - This response is respectful of the client's autonomy, but it may not be appropriate or feasible in this situation. The client may not be able to communicate their wishes or preferences, or they may have delegated this responsibility to their spouse. The nurse should not assume that the spouse's request is contrary to the client's wishes or best interests.
C) "I respect your request, but I need to explain the risks and benefits of removing the medical equipment. It may affect the client's comfort and safety." - This response is informative and
concerned for the client's well-being, but it may not be necessary or helpful in this situation. The spouse may already be aware of the risks and benefits of removing the medical equipment, or they may value their religious beliefs over their medical outcomes. The nurse should not try to persuade or dissuade the spouse from their request.
A nurse is working with a client who has a terminal illness and has chosen not to pursue any aggressive treatments. The client's culture values collectivism and harmony, and the client has expressed a desire to avoid any conflicts or disagreements with their family members. The nurse notices that some of the family members are unhappy or unsupportive of the client's decision. What is an appropriate nursing intervention for this situation?
Explanation
Rationale: The nurse should arrange a family meeting with the client and the health care team to discuss the goals of care and address any concerns or questions, as this can help to facilitate communication, understanding, and consensus among all parties involved. The nurse should also acknowledge and respect the client's culture, which values collectivism and harmony, and avoid creating or exacerbating any conflicts or disagreements within the family.
Incorrect options:
B) Provide individual counseling sessions for the family members who are unhappy or unsupportive of the client's decision and offer emotional support. - This intervention may be beneficial, but it may not be sufficient or effective in resolving the issue. The nurse should also consider the client's culture, which values collectivism and harmony, and involve all family members in the care planning or decision-making process.
C) Suggest alternative treatments or therapies for the client that may be more acceptable or appealing to the family members who are unhappy or unsupportive. - This intervention may be inappropriate or unethical, as it may undermine or disregard the client's decision and autonomy. The nurse should not try to influence or coerce the client or the family members into accepting any treatments or therapies that are not consistent with their goals, values, or beliefs.
D) Respect the client's decision and avoid involving the family members who are unhappy or unsupportive in the care planning or decision-making process. - This intervention may be respectful of the client's decision
Legal and Documentation Considerations in End-of-Life Care
A nurse is caring for a client who has a terminal illness and has expressed a wish to die at home. The client's family is supportive of this decision and has arranged for hospice care. What is the nurse's priority action in this situation?
Explanation
Rationale: The nurse's priority action in this situation is to review the client's advance directives and code status with the family, as these documents indicate the client's preferences and wishes regarding end-of-life care and resuscitation measures. The nurse should ensure that the family understands and respects the client's choices and that they have a copy of these documents available at home.
Incorrect options:
B) Assess the client's pain level and administer analgesics as prescribed. - This is an important action, but not the priority in this situation. The nurse should assess and manage the client's pain and other symptoms as part of palliative care, but this should be done after reviewing the advance directives and code status with the family.
C) Provide emotional support and counseling to the client and the family. - This is an important action, but not the priority in this situation. The nurse should provide emotional support and counseling to the client and the family as part of holistic care, but this should be done after reviewing the advance directives and code status with the family.
D) Educate the client and the family about the signs and symptoms of impending death. - This is an important action, but not the priority in this situation. The nurse should educate the client and the family about what to expect as death approaches, such as changes in breathing, circulation, consciousness, and skin color, but this should be done after reviewing the advance directives and code status with the family.
A client who has end-stage renal disease has decided to discontinue dialysis treatments. The client has a living will that states no artificial hydration or nutrition should be provided in case of a terminal condition. The client's spouse asks the nurse if they can give the client some ice chips or water to moisten their mouth. What is the best response by the nurse?
Explanation
Rationale: The best response by the nurse is to inform the spouse that they cannot give any ice chips or water to the client, as this would constitute artificial hydration and nutrition, which is against the client's living will. However, the nurse should also offer an alternative way of providing comfort to the client, such as using a moist sponge or swab to gently clean their mouth. This would help to relieve dryness and prevent cracking of the lips and tongue.
Incorrect options:
A) "Yes, you can give them some ice chips or water, as this will not prolong their life or interfere with their decision." - This is an incorrect response, as giving ice chips or water to a terminally ill client who has refused artificial hydration or nutrition would be unethical and potentially harmful. Ice chips or water could cause aspiration pneumonia, fluid overload, electrolyte imbalance, or increased blood pressure in a client who has end-stage renal disease.
B) "No, you cannot give them any ice chips or water, as this will violate their living will and cause them more discomfort." - This is a partially correct response, as giving ice chips or water to a terminally ill client who has refused artificial hydration or nutrition would violate their living will. However, this response does not offer any alternative way of providing comfort to the client, such as using a moist sponge or swab to gently clean their mouth.
C) "Yes, you can give them some ice chips or water, but only if they ask for it or indicate that they are thirsty." - This is an incorrect response, as giving ice chips or water to a terminally ill client who has refused artificial hydration or nutrition would be unethical and potentially harmful, regardless of whether they ask for it or not. Ice chips or water could cause aspiration pneumonia, fluid overload, electrolyte imbalance, or increased blood pressure in a client who has end-stage renal disease.
A nurse is reviewing the medical record of a client who has a do-not-resuscitate (DNR) order. The nurse notes that the order was written by the physician after consulting with the client's health care proxy, who is the client's adult daughter. The nurse also notes that the client is alert and oriented and has not expressed any objections to the DNR order.
What is the appropriate action by the nurse in this situation?
Explanation
Rationale: The appropriate action by the nurse in this situation is to confirm the DNR order with
the client and document the conversation in the medical record. The nurse should ensure that
the client understands what a DNR order means and that they agree with it. The nurse should
also respect the client's right to change their mind at any time and revoke the DNR order if they wish.
Incorrect options:
B) Contact the physician and request that the DNR order be revoked, as the client has not given consent. - This is an inappropriate action, as it would violate the client's autonomy and dignity. The nurse should not assume that the client has not given consent, as they may have discussed their wishes with their health care proxy or physician beforehand. The nurse should confirm the DNR order with the client instead of requesting its revocation.
C) Respect the DNR order and provide palliative care to the client, as the health care proxy has authority to make decisions. - This is a partially correct action, as the nurse should respect the DNR order and provide palliative care to the client. However, the nurse should not rely solely on the health care proxy's authority to make decisions, asthe client is alert and oriented and may have their own preferences and opinions. The nurse should confirm the DNR order with the client as well.
A nurse is caring for a client who has a do-not-resuscitate (DNR) order in place. The client's spouse asks the nurse to perform cardiopulmonary resuscitation (CPR) if the client stops breathing. Which action should the nurse take?
Explanation
Rationale: The nurse should respect the client's autonomy and right to self-determination, and ask the client to confirm their wishes regarding the DNR order. The client has the right to change or revoke their DNR order at any time, as long as they are competent and able to communicate.
Incorrect options:
A) Inform the spouse that the nurse is legally obligated to follow the DNR order. - This is an incorrect action, as it does not address the client's wishes or involve them in the decision-making process. The nurse should not assume that the spouse has the authority to make decisions for the client, unless there is evidence of a durable power of attorney for health care.
C) Notify the health care provider of the spouse's request. - This is an incorrect action, as it does not respect the client's autonomy or involve them in the decision-making process. The health care provider cannot change or revoke the DNR order without the client's consent, unless there is evidence of a court order or an advance directive that states otherwise.
D) Suggest the spouse to contact a lawyer to revoke the DNR order. - This is an incorrect action, as it does not respect the client's autonomy or involve them in the decision-making process. The spouse does not need a lawyer to revoke the DNR order, as long as the client is competent and able to communicate.
A client is admitted to the hospital with terminal cancer and expresses a wish to die at home. The client has an advance directive that states they do not want any life-sustaining treatments. Which statement by the nurse indicates an understanding of legal and ethical principles related to end-of-life care?
Explanation
Rationale: The nurse should refer the client to a hospice program that can provide them with palliative care at home, as this aligns with their wish to die at home and their advance directive that states they do not want any life-sustaining treatments. Hospice care focuses on improving the quality of life and comfort of clients who have a life expectancy of six months or less.
Incorrect options:
A) "I will make sure that your advance directive is followed by all members of your health care team." - This is a correct statement, but it does not indicate an understanding of legal and ethical principles related to end-of-life care. The nurse has a legal and ethical duty to follow the client's advance directive, but this does not address their wish to die at home or their need for palliative care.
B) "I will consult with your family members before making any decisions about your care." - This is an incorrect statement, as it violates the client's autonomy and right to self-determination. The nurse should respect the client's wishes and decisions regarding their end-of-life care, unless there is evidence of a durable power of attorney for health care or a court order that states otherwise.
C) "I will administer pain medication as needed, even if it may hasten your death." - This is an incorrect statement, as it implies that the nurse intends to cause or hasten the client's death, which is illegal and unethical. The nurse should administer pain medication as needed, following the principle of double effect, which states that an action that has both good and bad effects is morally permissible if the good effect is intended and outweighs
the bad effect.
A nurse is reviewing a client's medical record and notices that there is no documentation of informed consent for a surgical procedure that was performed earlier that day. Which action should the nurse take?
Explanation
Rationale: The nurse should report the incident to the risk management department, as this is a serious breach of legal and ethical principles that could result in legal action or disciplinary measures. The risk management department is responsible for identifying, analyzing, and minimizing risks that could harm clients, staff, or the organization.
Incorrect options:
B) Document the incident in the client's medical record. - This is an incorrect action, as it does not address the issue or prevent further harm. The nurse should not document anything in the client's medical record that is not related to their care or treatment, as this could be used as evidence in a lawsuit or investigation.
C) Contact the health care provider who performed the procedure. - This is an incorrect action, as it does not address the issue or prevent further harm. The nurse should not confront or accuse the health care provider who performed the procedure, as this could create conflict or hostility. The nurse should report the incident to the appropriate authority, such as the risk management department or the nursing supervisor.
D) Notify the client's family members of the incident. - This is an incorrect action, as it does not address the issue or prevent further harm. The nurse should not disclose any information about the client's care or treatment to anyone who is not authorized to receive it, unless there is a legal obligation or a valid consent from the client.
A client who has a terminal illness tells the nurse that they want to end their life by taking an overdose of medication. The client asks the nurse to help them obtain and administer the medication. Which response by the nurse is appropriate?
Explanation
Rationale: The nurse should empathize with the client's situation, but refuse to help them with their request to end their life by taking an overdose of medication. The nurse should explain that it is against their scope of practice and code of ethics to assist the client in ending their life, as this violates the principle of nonmaleficence, which states that nurses should do no harm or allow harm to occur.
Incorrect options:
A) "I understand that you are suffering, but I cannot help you with that. It is illegal and unethical for me to assist you in ending your life." - This is an incorrect response, as it does not show empathy or compassion for the client's situation. The nurse should not use legal or ethical terms that may sound harsh or judgmental to
the client.
B) "I respect your decision, but I cannot help you with that. It is against my personal and professional values to assist you in ending your life." - This is an incorrect response, as it does not show empathy or compassion for the client's situation. The nurse should not use personal or professional values that may sound biased or insensitive to
the client.
D) "I appreciate your honesty, but I cannot help you with that. It is against my moral and religious beliefs to assist you in ending your life." - This is an incorrect response, as it does not show empathy or compassion for the client's situation. The nurse should not use moral or religious beliefs that may sound intolerant or disrespectful to
the client.
Exams on End-of-life Care and Palliative Care
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Introduction to End-of-Life Care and Palliative Care
- Understanding End-of-Life Care and Palliative Care
- Communication and Advance Care Planning
- Symptom Management in Palliative Care
- Psychosocial and Spiritual Care
- Ethical and Legal Considerations in End-of-Life Care
- Family and Caregiver Support
- Bereavement and Grief Support
- Cultural Competence in End-of-Life Care
- Legal and Documentation Considerations in End-of-Life Care
- Conclusion
- Summary
Notes Highlighting is available once you sign in. Login Here.
Introduction to End-of-Life Care and Palliative Care
-
End-of-life care is the care provided to patients who are in the last stages of life and have a terminal illness that cannot be cured.
-
Palliative care is the care that focuses on improving the quality of life of patients and their families who are facing serious or life-threatening illnesses, regardless of the stage of the disease or the need for other therapies.
-
Both end-of-life care and palliative care aim to relieve physical, emotional, social, and spiritual suffering and to respect the dignity and preferences of patients and their families.

Understanding End-of-Life Care and Palliative Care
- End-of-life care and palliative care are based on the following principles:
-
Affirming life and regarding dying as a normal process
-
Providing holistic care that addresses the needs of the patient and the family
-
Supporting the patient's right to self-determination and informed decision making
-
Enhancing the patient's comfort and well-being
-
Offering a support system to help the patient and the family cope
-
Collaborating with an interdisciplinary team of health care professionals
-
Applying evidence-based practice and ethical standards
Communication and Advance Care Planning
-
Communication is a key component of end-of-life care and palliative care, as it helps to establish trust, rapport, and understanding between the patient, the family, and the health care team.
-
Communication skills that are essential for end-of-life care and palliative care include:
-
Active listening
-
Empathy
-
Open-ended questions
-
Reflection
-
Clarification
-
Summarization
-
Validation
-
Silence
- Communication challenges that may arise in end-of-life care and palliative care include:
-
Language barriers
-
Cultural differences
-
Emotional distress
-
Cognitive impairment
-
Conflicting values or beliefs
-
Family dynamics or conflicts
- Strategies to overcome communication challenges include:
-
Using interpreters or translators when needed
-
Being respectful and sensitive to cultural diversity
-
Providing emotional support and reassurance
-
Assessing the patient's mental status and capacity to make decisions
-
Exploring the patient's and the family's values, goals, and preferences
-
Resolving or mediating conflicts in a respectful and collaborative manner
- Advance care planning is the process of discussing and documenting the patient's wishes and preferences for future medical care, especially in the event that the patient becomes unable to communicate or make decisions.
- Advance care planning involves:
-
-
Identifying a health care proxy or surrogate decision maker who can act on behalf of the patient if needed
-
Completing an advance directive or living will that specifies the patient's preferences for life-sustaining treatments, such as cardiopulmonary resuscitation (CPR), mechanical ventilation, artificial nutrition and hydration, dialysis, etc.
-
Completing a do-not-resuscitate (DNR) order or a do-not-intubate (DNI) order if the patient does not want CPR or mechanical ventilation in case of cardiac or respiratory arrest
-
Completing a physician orders for life-sustaining treatment (POLST) form that summarizes the patient's wishes for medical interventions in various scenarios, such as comfort measures only, limited interventions, or full treatment
-
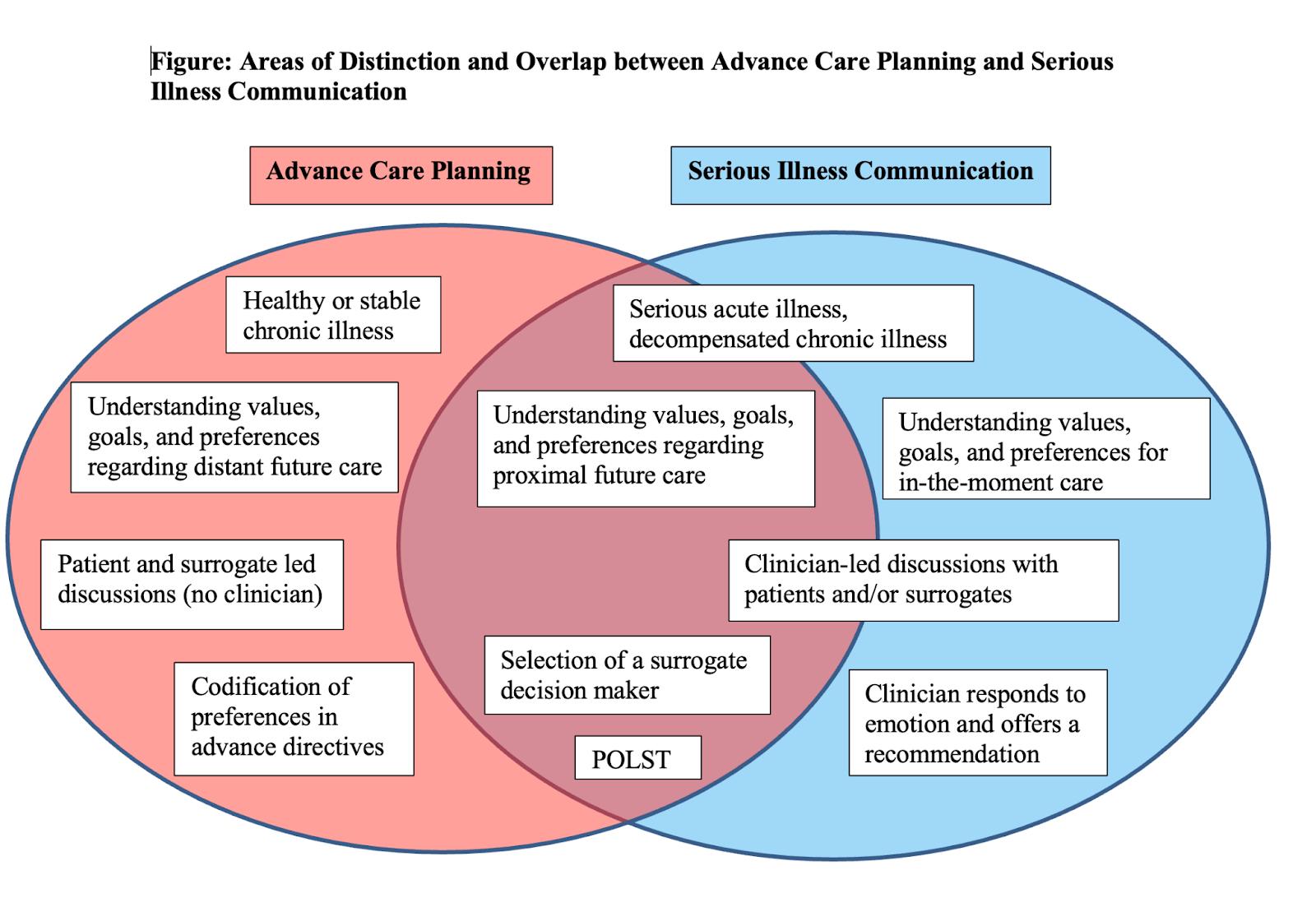
Symptom Management in Palliative Care
- Symptom management is a major aspect of palliative care, as it aims to relieve physical discomfort and improve functional status and quality of life for patients with serious or life-threatening illnesses.
- Common symptoms that require management in palliative care include:
-
Pain
-
Dyspnea (shortness of breath)
-
Nausea and vomiting
-
Constipation or diarrhea
-
Anorexia or cachexia (loss of appetite or weight)
-
Fatigue or weakness
-
Anxiety or depression
-
Delirium or confusion
- Symptom management strategies include:
-
Assessing the type, intensity, frequency, duration, location, and impact of symptoms using standardized tools, such as numerical rating scales, visual analog scales, faces pain scales, etc.
-
Identifying and treating the underlying causes of symptoms when possible, such as infections, obstructions, bleeding, etc.
-
Using pharmacological interventions, such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, anticholinergics, antiemetics, laxatives, etc., according to the principles of pain management (by mouth if possible; by clock; by ladder; for individual; with attention to detail)
-
Using nonpharmacological interventions, such as relaxation techniques, massage therapy, music therapy, aromatherapy.
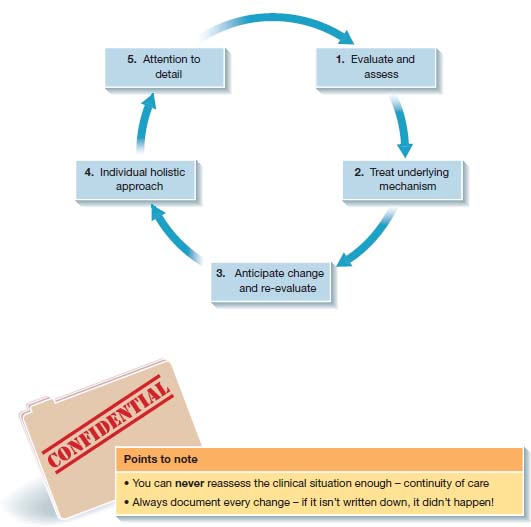
Psychosocial and Spiritual Care
- Psychosocial and spiritual care is another important component of palliative care that addresses the emotional, social, and existential needs of the patients and their families.
- Psychosocial and spiritual care helps to cope with the stressors, challenges, and losses associated with serious or terminal illnesses, such as fear, anger, guilt, sadness, loneliness, isolation, hopelessness, helplessness, regret, unresolved conflicts, loss of meaning or purpose, and loss of faith or identity.
- Psychosocial and spiritual care interventions include providing:
-
emotional support
-
validation
-
reassurance
-
education
-
information
-
referrals to community resources or support groups
-
crisis intervention
-
grief counseling
-
legacy work (such as life review or reminiscence)
-
rituals or ceremonies (such as prayer or meditation)
-
addressing spiritual or religious beliefs or practices
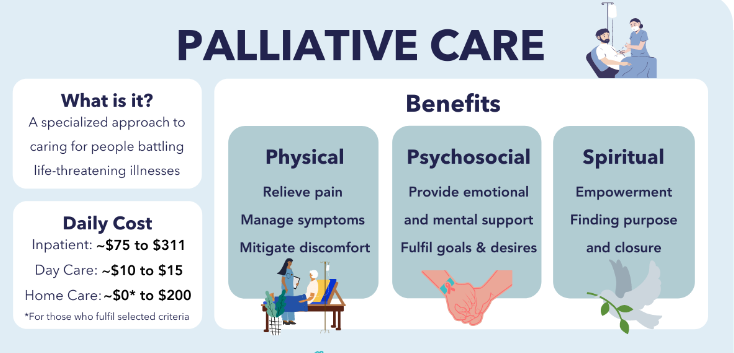
Ethical and Legal Considerations in End-of-Life Care
- Ethical and legal considerations in end-of-life care involve applying ethical principles
(such as autonomy, beneficence, non-maleficence, and justice) and legal standards (such as informed consent, confidentiality, and accountability) to decision-making processes regarding end-of-life issues, such as withholding or withdrawing life-sustaining treatments, providing palliative sedation, managing requests for hastened death, and resolving conflicts or dilemmas among the patients, their families, and the health care team.
- Ethical and legal considerations in end-of-life care require respecting the patient's
- rights
-
values
-
preferences
-
professional obligations
-
codes of conduct
-
scope of practice of the health care providers
- Ethical and legal considerations in end-of-life care also involve consulting with ethics committees, legal counsel, or other experts when needed.
Family and Caregiver Support
- Family and caregiver support is a vital part of end-of-life care and palliative care that recognizes the impact of serious or terminal illnesses on the family system and the role of family members and caregivers in providing care and comfort to the patients.
- Family and caregiver support includes assessing the needs, strengths, and resources of the family and caregivers, such as:
-
their physical, emotional, social, financial, and spiritual well-being,
-
their coping skills,
-
their knowledge and skills in caregiving,
-
their availability and willingness to provide care,
-
their access to support services or respite care.
- Family and caregiver support also includes providing education, guidance, assistance, encouragement, recognition, and appreciation to the family and caregivers, as well as involving them in decision-making, care planning, and care delivery.
- Family and caregiver support also includes addressing the potential challenges, risks, and burdens of caregiving, such as caregiver stress, burnout, fatigue, depression, anxiety, isolation, guilt, resentment, grief, or compassion fatigue.

Bereavement and Grief Support
- Bereavement and grief support is an essential component of end-of-life care and palliative care that acknowledges the normal and natural responses to loss and helps the bereaved cope with the death of a loved one.
- Bereavement and grief support includes providing information about the stages, tasks, and manifestations of grief, such as:
-
shock
-
denial
-
anger
-
bargaining
-
depression
-
acceptance
-
and finding meaning or growth.
- Bereavement and grief support also includes providing:
-
emotional support,
-
validation,
-
empathy,
-
comfort,
-
and companionship to the bereaved,
-
as well as facilitating expressions of grief, such as crying, talking, writing, or creating art or memorials.
- Bereavement and grief support also includes identifying and addressing the risk factors for complicated grief, such as:
-
sudden or traumatic death,
-
ambiguous loss,
-
multiple losses,
-
lack of social support,
-
pre-existing mental health issues,
-
or unresolved conflicts or guilt.
- Bereavement and grief support also includes offering referrals to professional counseling, support groups, or other resources when needed.
Cultural Competence in End-of-Life Care
- Cultural competence in end-of-life care is the ability to provide culturally appropriate
and respectful care to patients and their families who have diverse cultural backgrounds,
beliefs, values, practices, and preferences regarding end-of-life issues.
- Cultural competence in end-of-life care involves being aware of one's own cultural biases and assumptions and avoiding stereotypes or judgments based on cultural differences.
- Cultural competence in end-of-life care also involves being knowledgeable about the cultural norms and expectations of the patients and their families and being sensitive to their communication styles, verbal and non-verbal cues, body language, eye contact, touching, silence, and use of interpreters or translators.
- Cultural competence in end-of-life care also involves being respectful of the patient's
and family's wishes and choices regarding end-of-life issues, such as disclosure of diagnosis or prognosis, involvement of family members or elders in decision-making,
use of traditional or alternative therapies or healers, expression of emotions or grief,
rituals or ceremonies before or after death, disposition of the body or organs,
or funeral arrangements.
Legal and Documentation Considerations in End-of-Life Care
-
Legal and documentation considerations in end-of-life care involve following the legal requirements and standards or documenting and reporting the patient's status, care plan, interventions, outcomes, and death in a timely and accurate manner.
-
Legal and documentation considerations in end-of-life care include:
-
obtaining informed consent from the patient or surrogate decision-maker for any medical treatments or procedures that are offered or performed;
- documenting any advance directives or code status orders that are established or revised;
-
recording any changes in the patient's condition or goals of care;
-
any ethical or legal issues or conflicts that arise;
-
reporting any adverse events or errors that occur; completing any required forms or certificates for pronouncing or certifying death;
-
and ensuring proper identification and handling of the body.
-
Conclusion
- End-of-life care and palliative care are important aspects of nursing practice that aim to provide comfort, dignity and quality of life for patients with terminal illnesses and their families.
-
End-of-life care involves managing the physical, psychological, social and spiritual needs of patients who are dying, as well as providing support for their caregivers and loved ones.
-
Palliative care is a holistic approach that focuses on relieving pain and suffering, enhancing well-being and facilitating communication and decision-making for patients with life-limiting conditions and their families.
-
Nurses play a vital role in providing end-of-life care and palliative care by assessing the needs and preferences of patients and families, collaborating with the interdisciplinary team, advocating for patient rights and autonomy, and delivering compassionate and culturally sensitive care.
-
Nurses should also be aware of their own values, beliefs and emotions regarding death and dying, and seek professional and personal support to cope with the challenges and stressors of end-of-life care and palliative care.
Summary
-
End-of-life care and palliative care are both approaches to provide comfort and support to patients with life-limiting illnesses and their families.
-
End-of-life care is the care given in the final days or hours of a patient's life, when death is imminent or expected. Palliative care is the care given throughout the course of a serious or chronic illness, regardless of the prognosis or stage of the disease.
-
The goals of end-of-life care and palliative care are to relieve physical, emotional, social, and spiritual suffering; respect the patient's values, preferences, and goals; enhance the quality of life; and facilitate a peaceful death.
-
Nurses play a vital role in providing end-of-life care and palliative care by assessing and managing symptoms, communicating effectively, providing education and counseling, coordinating care, advocating for the patient's wishes, and supporting bereavement.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on End-of-life Care and Palliative Care
This filled cannot be empty

