Please set your exam date
Genito-Urinary System Disorders
Study Questions
Dialysis
Explanation
A)This statement is incorrect. Hemodialysis does not use the peritoneal membrane as a filter. Hemodialysis involves the use of a machine that filters the blood outside the body, not the peritoneal membrane.
B) This statement is incorrect. Continuous ambulatory peritoneal dialysis (CAPD) uses the peritoneal membrane as a filter during manual exchanges of dialysate fluid, not with a machine like automated peritoneal dialysis (APD).
C) This statement is accurate. Automated peritoneal dialysis (APD) uses a machine to perform exchanges of dialysate solution through the peritoneal membrane.
D) This statement is incorrect. Peritoneal dialysis uses the peritoneal membrane as a filter. It involves the instillation and drainage of dialysate fluid into the abdominal cavity through a catheter.
Explanation
A) The client's symptoms of dizziness and weakness may indicate hypotension (low blood pressure). The nurse should first check the client's blood pressure and pulse rate to assess for hypotension before implementing further interventions.
B) This statement is incorrect. Administering an antiemetic medication would not address the reported symptoms of dizziness and weakness, which may be related to changes in blood pressure.
C) This statement is incorrect. Increasing the rate of fluid removal during dialysis may exacerbate the client's symptoms of dizziness and weakness and may lead to hypotension (low blood pressure).
D) This statement is incorrect. Elevating the client's legs may help improve blood flow, but it does not address the underlying cause of the reported symptoms. The nurse should first check the client's blood pressure and pulse rate to assess for hypotension before implementing further interventions.
Explanation
A) This statement is incorrect. The catheter dressing should be changed regularly as per the healthcare provider's instructions, but it is not typically changed every week.
B) This statement is incorrect. The routine use of antibiotic ointment is not recommended, as it can lead to antibiotic resistance and is not necessary for all clients on peritoneal dialysis.
C) To reduce the risk of infection, the client should avoid touching the catheter site with clean hands. Maintaining proper hand hygiene is essential to prevent infection.
D) This statement is incorrect. Cleaning the catheter site with hydrogen peroxide is not recommended, as it can be too harsh and irritating to the skin. Instead, the site should be cleaned with mild soap and water or as instructed by the healthcare provider.
Explanation
A) This statement is incorrect. Increasing the dialysis session duration would not address the client's muscle cramps and may lead to further fluid and electrolyte imbalances.
B) Muscle cramps during hemodialysis can be caused by the cooling effect of the dialysate solution. Increasing the temperature of the dialysate can help alleviate the cramps.
C) This statement is incorrect. Decreasing the dialysate solution flow rate may not directly address the muscle cramps and may not be indicated unless there are other clinical indications to do so.
D) This statement is incorrect. Administering an anticoagulant medication is not relevant to address muscle cramps. Muscle cramps during hemodialysis are often caused by the cooling effect of the dialysate solution. Increasing the temperature of the dialysate can help alleviate the cramps.
Explanation
A) This statement is incorrect. Erythropoietin-stimulating agents (ESAs) are not used to prevent infections during dialysis. They are used to address anemia by stimulating red blood cell production.
B) This statement is accurate. Erythropoietin-stimulating agents (ESAs) stimulate the bone marrow to produce more red blood cells, addressing anemia commonly associated with chronic kidney disease and dialysis.
C) This statement is incorrect. Erythropoietin-stimulating agents (ESAs) do not reduce the risk of blood clot formation. They are specific to stimulating the production of red blood cells.
D) This statement is incorrect. Erythropoietin-stimulating agents (ESAs) do not enhance kidney function and filtration. They target the production of red blood cells to address anemia associated with ESRD and dialysis.
Explanation
A) This statement is incorrect. Cloudy dialysate drainage may indicate infection or peritonitis, and the nurse should not simply document the finding and continue monitoring without further assessment.
B) This statement is incorrect. Administering an antibiotic medication without a definitive diagnosis is not appropriate. The nurse should assess the client further to determine the cause of the cloudy drainage.
C) This statement is incorrect. Increasing the dialysis exchange frequency would not address the issue of cloudy dialysate drainage and may not be indicated without a proper assessment.
D) This statement is correct. Cloudy dialysate drainage may indicate infection or peritonitis. The nurse should check the client's vital signs and assess for signs of abdominal pain or tenderness, as this requires immediate evaluation.
Explanation
A) This statement is accurate. Clients on hemodialysis should limit their protein intake to reduce the workload on the kidneys and minimize waste buildup. Excess protein intake can lead to the accumulation of urea and other waste products, which can be challenging for the compromised kidneys to eliminate.
B) This statement is incorrect. While clients on hemodialysis may need to limit sodium intake to manage fluid retention and blood pressure, the primary nutrient that requires limitation in their diet is protein.
C) This statement is incorrect. Clients on hemodialysis may need to monitor their calcium intake, but it is not the primary nutrient that requires limitation in their diet. Calcium levels may be affected by the use of phosphate binders and the avoidance of high-phosphorus foods, but protein restriction is more critical.
D) This statement is incorrect. Iron intake may need to be managed for clients with anemia, which is common in end-stage renal disease (ESRD) and dialysis. However, protein restriction remains a more significant dietary consideration for clients on hemodialysis.
QUESTIONS
Explanation
A) This statement is incorrect. Hypertension (high blood pressure) is a common complication of kidney disease, but it is not the primary indication for initiating dialysis. Dialysis is primarily indicated to address the impaired filtration and waste removal functions of the kidneys, which can lead to electrolyte imbalances like hyperkalemia.
B) This statement is incorrect. Hypercalcemia (elevated calcium levels) is not a primary indication for initiating dialysis. While calcium imbalances can be associated with kidney disease, hyperkalemia takes precedence as a more critical indication for dialysis initiation.
C) This statement is accurate. Hyperkalemia (elevated potassium levels) is a critical indication for initiating dialysis. Dialysis helps remove excess potassium from the bloodstream when the kidneys are unable to do so, preventing potentially life-threatening complications.
D) This statement is incorrect. Hypokalemia (low potassium levels) is not an indication for initiating dialysis. In fact, dialysis may lead to a reduction in potassium levels, and clients on dialysis are more likely to experience hyperkalemia.
Explanation
A) This statement is incorrect. Dialysis does not restore normal kidney function. Instead, it serves as a substitute for impaired kidney function, helping to maintain fluid and electrolyte balance.
B) This statement is incorrect. Dialysis is not a surgical procedure to transplant a healthy kidney. Kidney transplantation is a separate procedure that involves replacing a damaged kidney with a healthy one from a living or deceased donor.
C) This statement is incorrect. Dialysis may help manage complications of CKD and prolong life, but it does not prevent the progression of the underlying kidney disease. CKD is a chronic and progressive condition that may eventually require dialysis or kidney transplantation.
D) This statement is accurate. Dialysis is the process of removing waste products, excess fluids, and toxins from the blood when the kidneys are no longer able to perform these functions adequately.
Explanation
A) This statement is incorrect. Hypokalemia (low potassium levels) is not an indication for initiating dialysis. In AKI, electrolyte imbalances can occur, but hyperkalemia is more likely due to impaired kidney function.
B) This statement is incorrect. Hyponatremia (low sodium levels) is not a primary indication for initiating dialysis in AKI. It can occur due to fluid shifts, but the primary concern in AKI is the accumulation of waste products like urea, leading to uremia.
C) This statement is incorrect. Hypernatremia (high sodium levels) is not a primary indication for initiating dialysis in AKI. Hypernatremia is rare in AKI and usually occurs when there is a significant loss of free water compared to sodium intake.
D) Uremia, which is characterized by elevated levels of urea and other waste products in the blood, is a critical indication for initiating dialysis in clients with acute kidney injury. Dialysis helps remove these toxic substances from the bloodstream.
Explanation
A) This statement is incorrect. Hypermagnesemia (elevated magnesium levels) can be a concern in ESRD, but it is not a primary indication for initiating dialysis. Magnesium levels can be managed through dietary restrictions and medications without the need for dialysis.
B) This statement is incorrect. Hyperphosphatemia (elevated phosphorus levels) is a common issue in ESRD, but it is not a primary indication for initiating dialysis. Clients with ESRD may receive phosphate binders to control phosphorus levels without necessarily needing immediate dialysis.
C) This statement is incorrect. Hyperkalemia (elevated potassium levels) is a concern in ESRD, but it is not the primary indication described in the scenario. While hyperkalemia may occur with fluid overload, the primary concern in this case is the hypervolemia and its associated symptoms.
D) Hypervolemia (severe fluid overload) is a critical indication for initiating dialysis in clients with end-stage renal disease. Dialysis helps remove excess fluid from the body and can relieve symptoms such as pulmonary edema and hypertension.
Explanation
A) This statement is incorrect. Hypernatremia (high sodium levels) is not the primary indication for initiating dialysis in this case. Metabolic acidosis and the inability of the kidneys to excrete acids are the primary concerns.
B) This statement is incorrect. Hyperkalemia (elevated potassium levels) may occur in CKD, but it is not the primary indication described in the scenario. Metabolic acidosis is the primary concern leading to the need for dialysis.
C) This statement is incorrect. Hypocalcemia (low calcium levels) can be a complication of CKD, but it is not the primary indication for initiating dialysis in this scenario. Metabolic acidosis and its associated symptoms take precedence.
D) Severe metabolic acidosis, which results from the kidneys' inability to adequately excrete acids and regulate pH balance, is a critical indication for initiating dialysis in clients with CKD.
Explanation
A) This statement is incorrect. Hypercalcemia (elevated calcium levels) can be a concern in ESRD, but it is not the primary indication for initiating dialysis in this scenario. Pruritus is more commonly associated with uremia and high levels of other waste products.
B) This statement is incorrect. Hypervolemia (fluid overload) can be a concern in ESRD, but it is not the primary indication described in the scenario. The persistent pruritus is more likely related to uremia and the accumulation of toxins.
C) This statement is incorrect. Hyperkalemia (elevated potassium levels) is not the primary indication described in the scenario. While hyperkalemia may occur in ESRD, the primary concern leading to the need for dialysis in this case is the uremia and its associated symptoms.
D) Uremia, which is the accumulation of urea and other waste products in the blood, can lead to various complications, including pruritus. Dialysis helps remove these waste products from the bloodstream and may alleviate the itching associated with uremia.
Explanation
A) This statement is incorrect. Hypoglycemia (low blood glucose) is not the primary indication for initiating dialysis. Hypoglycemia can occur in certain situations, but it is not the primary concern in this case.
B) This statement is incorrect. Hyperkalemia (elevated potassium levels) can be a concern in AKI, but it is not the primary indication described in the scenario. The primary concern in AKI with decreased GFR is the impaired filtration and waste removal, leading to the need for dialysis.
C) This statement is incorrect. Hypernatremia (high sodium levels) is not a primary indication for initiating dialysis in AKI. Hypernatremia is rare in AKI and usually occurs when there is a significant loss of free water compared to sodium intake.
D) A significantly decreased glomerular filtration rate (GFR) indicates that the kidneys' ability to filter waste products and excess fluids from the blood is severely impaired. Dialysis can help support kidney function and remove waste products when the GFR is critically low.
Explanation
A) This statement is incorrect. Hyperkalemia (elevated potassium levels) can be a concern in ESRD, but it is not the primary indication described in the scenario. While hyperkalemia may occur in ESRD, the primary concern leading to the need for dialysis is the uremia and its associated symptoms.
B) This statement is incorrect. Hypophosphatemia (low phosphorus levels) can be a concern in ESRD, but it is not the primary indication for initiating dialysis in this case. Uremia and its associated symptoms are the primary concerns leading to the need for dialysis.
C) Uremia, which is characterized by elevated levels of urea and other waste products in the blood, is a critical indication for initiating dialysis in clients with end-stage renal disease. Dialysis helps remove these toxic substances from the bloodstream and may alleviate symptoms like fatigue, weakness, and decreased urine output.
D) This statement is incorrect. Hyponatremia (low sodium levels) is not the primary indication for initiating dialysis in this scenario. Uremia and the accumulation of waste products are the primary concerns that require dialysis to address.
QUESTIONS
Explanation
A) This statement is incorrect. Hemodialysis does not involve the removal of the peritoneal membrane; that description is characteristic of peritoneal dialysis.
B) This statement is accurate. Hemodialysis uses a machine called a dialyzer to filter blood outside the body, removing waste products and excess fluid before returning the clean blood to the patient.
C) This statement is incorrect. Hemodialysis does not rely on a catheter inserted into the bladder; that description is characteristic of urinary catheterization.
D) This statement is incorrect. Hemodialysis does not use a pump to circulate dialysate through the intestines; that description is characteristic of peritoneal dialysis.
Explanation
A) This statement is incorrect. Increasing the rate of fluid removal during dialysis may worsen the client's symptoms of lightheadedness and dizziness, as it can lead to further drops in blood pressure.
B) This statement is incorrect. Administering an antihypertensive medication is not appropriate in this situation, as the client is experiencing symptoms of low blood pressure, not high blood pressure.
C) This statement is accurate. Feeling lightheaded and dizzy during hemodialysis may be a sign of hypotension (low blood pressure), and the nurse should assess the client's blood pressure and pulse rate to determine if intervention is needed.
D) This statement is incorrect. Elevating the client's legs may promote blood flow, but it does not address the immediate issue of lightheadedness and dizziness. Assessing the client's blood pressure and pulse rate is the priority to determine the appropriate intervention.
Explanation
A) This statement is accurate. Clients on hemodialysis should limit their protein intake to reduce the workload on the kidneys and minimize waste buildup. Excess protein intake can lead to the accumulation of urea and other waste products, which can be challenging for the compromised kidneys to eliminate.
B) This statement is incorrect. While clients on hemodialysis may need to limit sodium intake to manage fluid retention and blood pressure, the primary nutrient that requires limitation in their diet is protein.
C) This statement is incorrect. Clients on hemodialysis may need to monitor their calcium intake, but it is not the primary nutrient that requires limitation in their diet. Calcium levels may be affected by the use of phosphate binders and the avoidance of high-phosphorus foods, but protein restriction is more critical.
D) This statement is incorrect. Iron intake may need to be managed for clients with anemia, which is common in end-stage renal disease (ESRD) and dialysis. However, protein restriction remains a more significant dietary consideration for clients on hemodialysis.
Explanation
A) This statement is incorrect. Increasing the dialysis session duration would not address the client's muscle cramps and may lead to further fluid and electrolyte imbalances.
B) This statement is accurate. Muscle cramps during hemodialysis are often caused by the cooling effect of the dialysate solution. Increasing the temperature of the dialysate can help alleviate the cramps.
C) This statement is incorrect. Decreasing the dialysate solution flow rate may not directly address the muscle cramps and may impact the effectiveness of the dialysis treatment.
D) This statement is incorrect. Administering an anticoagulant medication is not indicated for muscle cramps during hemodialysis. Anticoagulants are used to prevent blood clots during the procedure but would not alleviate muscle cramps.
Explanation
A)This statement is incorrect. Administering an analgesic for the headache may provide temporary relief, but it does not address the underlying issue of fluid overload and elevated blood pressure.
B) This statement is incorrect. Notifying the healthcare provider about the blood pressure changes is important, but assessing for fluid overload and taking appropriate actions should be the nurse's priority.
C) This statement is accurate. Headache and restlessness during hemodialysis, along with elevated blood pressure, may indicate fluid overload. The nurse should assess the client's weight and fluid intake during the dialysis session to determine if there is excessive fluid retention.
D) This statement is incorrect. Increasing the dialysate solution flow rate may not be appropriate without further assessment of the client's fluid status. It could worsen the fluid overload and further increase blood pressure.
Explanation
A) This statement is incorrect. Serum calcium levels are not directly related to ESA therapy for anemia management. ESA therapy focuses on increasing red blood cell production.
B) This statement is incorrect. Blood urea nitrogen (BUN) levels are indicators of kidney function and may be monitored for other reasons in a client on hemodialysis. However, they are not directly related to ESA therapy for anemia management.
C) This statement is accurate. During ESA therapy, the nurse should closely monitor the client's hemoglobin and hematocrit levels. ESAs stimulate the production of red blood cells and can increase hemoglobin and hematocrit levels. Regular monitoring is essential to prevent anemia or excessive increases in these values.
D) This statement is incorrect. Serum potassium levels may be monitored for a client on hemodialysis due to the potential for electrolyte imbalances, but they are not the primary concern during ESA therapy for anemia management.
Explanation
A) This statement is accurate. Palpating for a thrill or vibration over the AV fistula site is a critical assessment to ensure proper functioning. A thrill indicates adequate blood flow through the fistula, which is essential for effective hemodialysis.
B) This statement is incorrect. Auscultating for bruits over the radial artery is not related to the AV fistula assessment. The bruit is the sound of blood flow in the fistula, which is best assessed directly over the fistula site.
C) This statement is incorrect. Checking for distal pulses in the lower extremities is not related to the assessment of an AV fistula. The AV fistula is typically created in the upper extremity.
D) This statement is incorrect. Assessing for swelling and tenderness in the neck is not related to the AV fistula assessment. Swelling and tenderness may be related to other issues but are not specific to AV fistula functioning.
Explanation
A) This statement is incorrect. Monitoring hemoglobin levels is essential for clients with ESRD and during hemodialysis, but it is not directly related to the administration of heparin.
B) This statement is accurate. While a drop in platelet count is not uncommon during heparin administration, the nurse should closely monitor the client's platelet count to detect any significant changes or potential complications related to heparin-induced thrombocytopenia.
C) This statement is incorrect. Monitoring blood glucose levels is important, especially for clients with diabetes or those at risk of hypoglycemia during dialysis, but it is not specifically related to heparin administration.
D) This statement is incorrect. Monitoring blood urea nitrogen (BUN) levels is crucial for clients with ESRD, but it is not directly related to the administration of heparin during hemodialysis.
QUESTIONS
Explanation
A) This statement is incorrect. Peritoneal dialysis does not use a machine to filter blood outside of the body; that description is characteristic of hemodialysis.
B) This statement is incorrect. Peritoneal dialysis does not involve the removal of the peritoneal membrane; instead, it uses the peritoneal membrane in the abdomen to filter waste.
C) This statement is accurate. Peritoneal dialysis uses the peritoneal membrane in the abdomen as a semipermeable membrane to filter waste products and excess fluids from the blood.
D) This statement is incorrect. Peritoneal dialysis does not require a catheter to be inserted into the bladder. Instead, it uses a catheter to infuse and drain dialysate into and out of the peritoneal cavity.
Explanation
A) This statement is incorrect. While administering an antibiotic may be necessary if peritonitis is confirmed, it should not be done without obtaining a sample for testing first.
B) This statement is incorrect. Measuring vital signs and assessing for pain are essential aspects of client assessment, but they may not provide enough information to determine the cause of the cloudy drainage.
C) This statement is incorrect. Clamping the catheter may be necessary if peritonitis is suspected, but it should not be done without first obtaining a sample of the drainage for testing.
D) This statement is accurate. Cloudy drainage from the catheter site may indicate peritonitis, which is an infection of the peritoneal cavity. Obtaining a sample of the drainage for culture and sensitivity testing can help identify the presence of infection and guide appropriate treatment.
Explanation
A) This statement is incorrect. Serum calcium levels are not directly related to ESA therapy for anemia management. ESA therapy focuses on increasing red blood cell production.
B) This statement is incorrect. Blood urea nitrogen (BUN) levels are indicators of kidney function and may be monitored for other reasons in a client on peritoneal dialysis. However, they are not directly related to ESA therapy for anemia management.
C) This statement is accurate. During ESA therapy, the nurse should closely monitor the client's hemoglobin and hematocrit levels. ESAs stimulate the production of red blood cells and can increase hemoglobin and hematocrit levels. Regular monitoring is essential to prevent anemia or excessive increases in these values.
D) This statement is incorrect. Serum potassium levels may be monitored for a client on peritoneal dialysis due to the potential for electrolyte imbalances, but they are not the primary concern during ESA therapy for anemia management.
Explanation
A) This statement is incorrect. Infection is not a rare complication of peritoneal dialysis. It is a common risk that requires proactive measures to prevent.
B) This statement is incorrect. While infections can occur and may be treatable with antibiotics, it is essential to focus on prevention and maintaining aseptic technique.
C) This statement is incorrect. Taking antibiotics regularly to prevent infection is not the standard practice for clients on peritoneal dialysis. Antibiotics are typically prescribed to treat infections when they occur, not as a preventive measure.
D) This statement is accurate. Infection is a significant risk for clients on peritoneal dialysis due to the direct access to the peritoneal cavity through the catheter. Strict aseptic technique is crucial to prevent infections.
Explanation
A) This statement is incorrect. Administering an analgesic for the abdominal pain may provide temporary relief, but it does not address the underlying cause of the symptoms.
B) This statement is incorrect. Measuring blood pressure and pulse rate is essential for client assessment, but it may not provide enough information to determine the cause of the symptoms.
C) This statement is accurate. Abdominal pain and fever in a client on peritoneal dialysis may indicate peritonitis, which can result from infection or catheter issues. The nurse should first check the catheter for kinks or obstructions to ensure proper drainage and prevent complications.
D) This statement is incorrect. Notifying the healthcare provider about the symptoms is important, but the nurse should first assess the catheter for possible issues to determine if immediate intervention is needed.
Explanation
A) This statement is incorrect. Peritoneal dialysis does not require extended hospital stays, as it can be performed at home.
B) This statement is incorrect. While some modifications to daily activities may be necessary, peritoneal dialysis does not generally require clients to limit their daily activities or avoid physical exertion.
C) This statement is accurate. Peritoneal dialysis is a form of dialysis that can be performed by the client at home, allowing them to continue with their daily activities without the need for hospitalization or daily clinic visits.
D) This statement is incorrect. Peritoneal dialysis is performed by the client at home, not at the outpatient clinic every day. The client may visit the clinic for periodic follow-up and assessment, but the actual dialysis is performed at home.
Explanation
A) This statement is accurate. Hypertonic dialysate has a higher concentration of glucose, which results in increased fluid removal from the client's peritoneal cavity. This type of dialysate is often used for more effective ultrafiltration.
B) This statement is incorrect. Infusing hypertonic dialysate does not result in decreased urine output. Peritoneal dialysis is a process of exchanging fluids and waste products through the peritoneal membrane, but it does not directly affect urine production.
C) This statement is incorrect. Infusing hypertonic dialysate would not lead to hydration overload, as it causes fluid to be removed from the body.
D) This statement is incorrect. Hypertonic dialysate would not cause hypotension. In fact, it may lead to a decrease in blood pressure due to fluid removal, but it would not be considered a primary cause of hypotension.
Explanation
A) This statement is incorrect. Increasing the intake of potassium-rich foods is not related to managing constipation. In fact, clients on peritoneal dialysis may need to restrict potassium intake due to the potential for electrolyte imbalances.
B) This statement is accurate. Constipation can be a common issue for clients on peritoneal dialysis due to the presence of glucose in the dialysate, which can draw fluid into the peritoneal cavity and lead to decreased bowel movement. Administering a stool softener as needed can help alleviate constipation.
C) This statement is incorrect. Decreasing fluid intake during dialysis is not recommended for managing constipation. Fluid intake should be maintained as prescribed to achieve adequate ultrafiltration.
D) This statement is incorrect. Encouraging the client to consume dairy products is not directly related to managing constipation. While calcium intake may be important for bone health in clients with ESRD, it is not a primary intervention for constipation.
QUESTIONS
Explanation
A. Incorrect. Protein intake is essential for maintaining body functions, but clients on dialysis may need to adjust their protein intake based on their individual needs and dialysis prescription.
B. Incorrect. Clients on dialysis may need to limit their sodium intake to manage fluid retention and blood pressure.
C. Correct. Clients on dialysis often need to avoid potassium-rich foods to prevent hyperkalemia, as the kidneys are unable to adequately remove excess potassium from the blood.
D. Incorrect. Clients on dialysis typically need to restrict their phosphorus intake to prevent complications related to high phosphorus levels, such as bone disease and cardiovascular issues.
Explanation
A. Correct. Monitoring the client's blood pressure and heart rate is a priority during dialysis to assess the client's hemodynamic status and detect any potential complications, such as hypotension or arrhythmias.
B. Incorrect. While assisting with dietary s is important, it is not the priority during the dialysis procedure.
C. Incorrect. Providing emotional support is essential, but the nurse's priority during dialysis is to monitor the client's vital signs and ensure their safety during the procedure.
D. Incorrect. Administering prescribed intravenous medications may be necessary during dialysis, but it is not the priority action stated in this question.
Explanation
A. Incorrect. Using sterile technique when handling the catheter is essential to prevent infection. Clients and caregivers should be taught the proper aseptic technique for catheter care.
B. Incorrect. Alcohol wipes can dry out the skin and are not recommended for cleaning the catheter insertion site. A more appropriate solution is provided in the correct answer.
C. Correct. Changing the dressing over the catheter daily using clean gloves helps maintain a clean and dry site, reducing the risk of infection during peritoneal dialysis.
D. Incorrect. The catheter should not be immersed in water during bathing or showering, as this can introduce pathogens and increase the risk of infection.
Explanation
A. Incorrect. Limiting fluid intake is important for some clients with renal issues, but clients on dialysis typically need to maintain adequate hydration due to fluid removal during the procedure.
B. Correct. Clients on dialysis often need to consume plenty of fluids to compensate for the fluid removal that occurs during dialysis treatment, preventing dehydration and maintaining hemodynamic stability.
C. Incorrect. Increasing salt intake is not recommended for clients on dialysis, as it can contribute to fluid retention and worsen hypertension.
D. Incorrect. Limiting fluid intake only on the day of dialysis treatment is not sufficient to maintain overall hydration and may lead to imbalances and complications between dialysis sessions.
Explanation
A. Correct. Avoiding heavy lifting can help prevent trauma or dislodgement of the peritoneal catheter, which can be a risk factor for infection or complications.
B. Correct. Cleaning the catheter exit site with soap and water daily helps maintain cleanliness and reduce the risk of infection.
C. Incorrect. The dressing around the catheter insertion site should be changed more frequently than weekly, ideally every 2-3 days, to ensure proper hygiene and reduce the risk of infection.
D. Correct. Notifying the healthcare provider about any redness or drainage at the catheter site is essential, as these can be signs of infection or other complications that require prompt evaluation and treatment.
Explanation
A. Incorrect. Warming the dialysate fluid to body temperature before instilling it into the peritoneal cavity is a standard procedure in continuous ambulatory peritoneal dialysis (CAPD. .
B. Correct. Performing the exchanges in a clean, dry environment free from pets is crucial to prevent contamination and reduce the risk of infection during CAPD.
C. Incorrect. Using tap water to cleanse the catheter insertion site before the exchange is not recommended. The catheter exit site should be cleaned with an appropriate antiseptic solution as instructed by the healthcare provider.
D. Incorrect. While daily dressing changes are important, using sterile technique for catheter dressing changes may not be necessary, as the dressing does not directly contact the peritoneal cavity during CAPD exchanges.
Explanation
A. Correct. Using the arm with the AV fistula for blood pressure measurements can compress the vascular access and compromise blood flow. It is important to avoid using the fistula arm for blood pressure measurements and venipuncture.
B. Incorrect. The AV fistula should not be used for intravenous catheter insertion to prevent potential damage and infection to the access site.
C. Incorrect. Self-cannulation of the AV graft is typically performed by healthcare professionals, and clients should not attempt to self-cannulate their vascular access.
D. Incorrect. If an AV fistula starts bleeding, the client should not apply pressure to the site. Instead, they should immediately elevate the arm and apply pressure to the bleeding site with a clean cloth or bandage while seeking medical attention.
QUESTIONS
Explanation
A. Incorrect. Increasing the dialysate temperature can lead to vasodilation and potentially exacerbate hypotension during dialysis.
B. Correct. Limiting fluid removal during dialysis is essential to prevent excessive fluid loss, which can cause hypotension and potentially lead to intradialytic hypotension.
C. Incorrect. Encouraging a high-sodium diet is not the primary intervention to prevent dialysis-related hypotension. It may be recommended for some clients to manage hyponatremia, but fluid management is more critical.
D. Incorrect. Administering intravenous hypertonic saline during dialysis is not a routine intervention to prevent hypotension. It may be used in specific cases, but fluid management is the primary approach.
Explanation
A. Incorrect. Collecting a sample of the effluent for culture and sensitivity testing may be necessary, but notifying the healthcare provider about the finding should be done first.
B. Incorrect. Stopping the exchange immediately may be necessary in some cases, but the nurse should first communicate the finding to the healthcare provider for further assessment and guidance.
C. Correct. Cloudy dialysate effluent may indicate peritonitis, an infection of the peritoneal cavity, which requires immediate attention and treatment by the healthcare provider.
D. Incorrect. Encouraging the client to perform another exchange without further assessment can potentially exacerbate any underlying issue causing the cloudy effluent.
Explanation
A. Incorrect. While administering an antiepileptic medication may be necessary if the client is experiencing seizures, it is essential to identify the underlying cause first.
B. Correct. The client's severe headache, confusion, and seizures may be indicative of dialysis disequilibrium syndrome, which is a complication of rapid solute removal during hemodialysis. Hypoglycemia can also present with similar symptoms, so assessing blood glucose levels is crucial to differentiate between the two conditions.
C. Incorrect. Documenting the findings and monitoring the client's condition are important, but addressing the acute symptoms and potential cause should be the priority.
D. Incorrect. Checking the client's pre-dialysis weight is not the priority when the client is experiencing severe neurological symptoms. Immediate assessment and intervention are needed.
Explanation
A. Incorrect. Administering a calcium channel blocker is not the first-line intervention for muscle cramps during dialysis.
B. Incorrect. Slowing down the blood flow rate during dialysis may be necessary in some cases, but it is not the first action to address muscle cramps.
C. Correct. Muscle cramps during dialysis can be caused by electrolyte imbalances, such as low potassium levels. Offering the client a sports drink with electrolytes can help alleviate the cramps.
D. Incorrect. Applying a heating pad to the affected muscles is not recommended during dialysis, as it may cause burns or worsen the cramps.
Explanation
A. Incorrect. Administering a prescribed analgesic may be necessary, but it is not the priority when the client is experiencing sudden chest pain and dyspnea.
B. Correct. The sudden onset of chest pain and dyspnea can be indicative of potential complications, such as dialysis-related hypotension, cardiac issues, or fluid overload. Assessing the client's blood pressure and heart rate is the priority to identify any acute changes or abnormalities.
C. Incorrect. Monitoring the client's weight is important to assess fluid status, but it is not the immediate priority when the client presents with acute chest pain and dyspnea.
D. Incorrect. Placing the client in a semi-Fowler's position may be appropriate for respiratory distress, but the nurse should first assess the client's vital signs and overall condition before implementing positioning changes.
Explanation
A. Incorrect. Instructing the client to increase fluid intake may not address the underlying cause of abdominal pain and fever in a client on peritoneal dialysis.
B. Incorrect. Assisting the client with a peritoneal fluid exchange is not the priority when the client is experiencing abdominal pain and fever, as it may exacerbate the symptoms.
C. Incorrect. Administering an over-the-counter pain reliever may provide temporary relief, but it does not address the underlying cause of the symptoms.
D. Correct. Abdominal pain and fever in a client on peritoneal dialysis may indicate peritonitis, an infection of the peritoneal cavity. Obtaining a peritoneal fluid sample for testing is essential to confirm the diagnosis and initiate appropriate treatment promptly.
Explanation
A. Incorrect. Offering hard candies or mints may provide temporary relief from the metallic taste, but it does not address the underlying cause.
B. Correct. A persistent metallic taste in the mouth can be caused by various factors, such as dietary changes, medication side effects, or biochemical imbalances. Assessing the client's recent dietary and medication changes can help identify the potential cause.
C. Incorrect. Providing an oral rinse may offer temporary relief, but it does not address the underlying cause of the metallic taste.
D. Incorrect. Administering an antiemetic medication is not indicated for a metallic taste in the mouth, as it is not associated with nausea or vomiting.
Explanation
A. Correct. Applying pressure to the bleeding site is the first action to control the bleeding and prevent excessive blood loss.
B. Incorrect. Elevating the arm above heart level may not be effective in controlling bleeding from the access site and could cause unnecessary discomfort.
C. Incorrect. Administering a prescribed antiplatelet medication is not the first action to take when the client experiences bleeding from the access site, as it may further increase bleeding risk.
D. Incorrect. While checking the client's platelet count is important, it is not the first action to address active bleeding. Applying pressure to the bleeding site takes priority to control the bleeding.
QUESTIONS
Nephrotic Syndrome
Explanation
A. Correct. Nephrotic syndrome is characterized by increased protein loss in the urine, leading to hypoalbuminemia and a weakened immune system. Clients with nephrotic syndrome are at a higher risk of infection, so the priority nursing intervention is to assess for signs of infection and initiate appropriate treatment promptly.
B. Incorrect. While monitoring blood glucose levels is essential in some conditions, it is not the priority for a client with nephrotic syndrome.
C. Incorrect. Dietary education may be necessary, but increasing protein intake is not appropriate for clients with nephrotic syndrome due to the increased protein loss in the urine.
D. Incorrect. Diuretics may be used to manage edema in nephrotic syndrome, but the priority intervention is to assess for infection, as it poses a more immediate threat to the client's health.
Explanation
A. Incorrect. Corticosteroids should be taken with food to reduce the risk of gastrointestinal side effects.
B. Incorrect. While corticosteroids may improve proteinuria over time, it is unlikely to see an immediate improvement after starting the medication.
C. Correct. Corticosteroids can suppress the immune system and increase the risk of infection, so the client should avoid crowded places and contact with individuals who are sick to minimize the risk of infections.
D. Incorrect. Corticosteroids do not specifically affect potassium levels, so there is no need for a diet high in potassium to offset potential electrolyte imbalances.
Explanation
A. Incorrect. Restricting fluid intake may not be appropriate for clients with nephrotic syndrome, as they may already have reduced fluid intake due to decreased glomerular filtration.
B. Incorrect. Elevating the client's legs can help reduce edema, but a low-sodium diet is a more direct and essential intervention for managing fluid retention in nephrotic syndrome.
C. Correct. A low-sodium diet is crucial in managing edema in nephrotic syndrome. Sodium intake can lead to fluid retention, and reducing sodium intake helps decrease edema.
D. Incorrect. Monitoring blood glucose levels is important for clients with diabetes, but it is not directly related to managing edema in nephrotic syndrome.
Explanation
A. Incorrect. Frothy, foamy urine is not characteristic of increased glucose levels in the urine.
B. Incorrect. While blood in the urine may cause changes in urine color, it does not result in frothy, foamy appearance.
C. Correct. Nephrotic syndrome is characterized by increased protein excretion in the urine (proteinuriA. . The presence of protein in the urine can cause it to appear frothy and foamy.
D. Incorrect. Creatinine levels reflect kidney function, but they do not cause changes in urine appearance.
Explanation
A. Correct. ACE inhibitors are commonly prescribed in nephrotic syndrome to reduce proteinuria by dilating blood vessels and decreasing pressure in the glomerulus. This helps preserve kidney function and slow the progression of kidney damage.
B. Incorrect. ACE inhibitors are not primarily used to manage blood glucose levels in diabetes, although they may have some impact on blood pressure control in clients with both diabetes and nephrotic syndrome.
C. Incorrect. ACE inhibitors do not directly impact calcium absorption or bone health in nephrotic syndrome.
D. Incorrect. ACE inhibitors do not specifically increase potassium excretion. In fact, they may lead to potassium retention, so clients may need to be cautious about potassium intake while on ACE inhibitors.
Explanation
A. Correct. Diuretics can lead to potassium loss, potentially causing hypokalemia. Monitoring serum potassium levels is essential to prevent complications related to potassium imbalances.
B. Incorrect. Diuretics may affect blood glucose levels indirectly, but their primary impact is not related to glucose control.
C. Incorrect. Diuretics do not directly impact calcium levels
in nephrotic syndrome.
D. Incorrect. While monitoring blood pressure is important in nephrotic syndrome, it is not the primary focus when clients are on diuretic therapy.
Explanation
A. Incorrect. While increased proteinuria can increase the risk of clot formation in the urinary tract, anticoagulant therapy is not typically prescribed for this reason in nephrotic syndrome.
B. Incorrect. Anticoagulants are not primarily used to reduce inflammation and pain associated with kidney damage.
C. Incorrect. Anticoagulants do not directly impact the risk of infection related to hypoalbuminemia.
D. Correct. Nephrotic syndrome can cause damage to the glomerular capillaries, leading to clot formation. Anticoagulant therapy is prescribed to prevent clot formation in the kidneys and reduce the risk of complications such as renal vein thrombosis.
QUESTIONS
Explanation
A. Incorrect. Hematuria (blood in the urinE. and dysuria (painful urination) are not characteristic manifestations of nephrotic syndrome. Instead, they may indicate other kidney conditions or infections.
B. Incorrect. While clients with nephrotic syndrome may experience increased urine output (polyuriA. and nighttime urination (nocturiA. due to fluid imbalances, these are not the primary clinical manifestations.
C. Correct. Frothy, foamy urine output is a classic sign of nephrotic syndrome due to the presence of excessive protein (proteinuriA. in the urine. This foamy appearance is caused by the high levels of protein, mainly albumin, in the urine.
D. Incorrect. Suprapubic tenderness and urgency are not typical manifestations of nephrotic syndrome and may indicate other urinary tract or bladder issues.
Explanation
A. Incorrect. Increased renal blood flow and fluid overload would lead to excessive urine output and reduced edema, which is not consistent with nephrotic syndrome.
B. Incorrect. Excessive sodium excretion and dehydration would lead to reduced fluid retention and edema, which is not consistent with nephrotic syndrome.
C. Correct. Nephrotic syndrome is characterized by glomerular damage, leading to increased permeability of the glomerular capillaries and loss of protein (mainly albumin) in the urine. This results in decreased oncotic pressure in the blood vessels, leading to edema in various parts of the body.
D. Incorrect. Elevated blood pressure and vascular leakage would lead to a different set of clinical manifestations, not characteristic of nephrotic syndrome.
Explanation
A. Correct. Periorbital edema is a common manifestation of nephrotic syndrome, especially in the morning after fluid accumulation overnight. Elevated blood pressure and headache may accompany this edema, indicating fluid retention and hypertension, which are frequently associated with nephrotic syndrome.
B. Incorrect. Yellowish discoloration of the skin and sclera (jaundicE. is not a typical manifestation of nephrotic syndrome and is more indicative of liver dysfunction or bile flow obstruction.
C. Incorrect. Pain and tenderness over the lower back are not directly related to periorbital edema and may suggest a separate issue, such as musculoskeletal pain.
D. Incorrect. Shortness of breath and crackles in the lungs are not specific to nephrotic syndrome and may suggest other respiratory or cardiac issues.
Explanation
A. Incorrect. Elevated blood pressure and fluid overload are more indicative of fluid retention and hypertension in nephrotic syndrome, not hypoalbuminemia.
B. Correct. Hypoalbuminemia, a common feature of nephrotic syndrome, results from the loss of albumin (a protein) in the urine. Low albumin levels can lead to muscle weakness and fatigue due to decreased oncotic pressure in the blood vessels, resulting in fluid shifting from the blood vessels to the interstitial spaces.
C. Incorrect. Hyperactivity and restlessness are not typical manifestations of hypoalbuminemia and nephrotic syndrome.
D. Incorrect. Pallor and cold extremities are not directly related to hypoalbuminemia and are not specific to nephrotic syndrome.
Explanation
A. Incorrect. Elevated platelet count and clotting factors are not characteristic of nephrotic syndrome. Clients with nephrotic syndrome tend to have normal platelet counts.
B. Incorrect. Decreased blood viscosity and enhanced blood flow would not directly lead to an increased risk of thromboembolic events in nephrotic syndrome.
C. Incorrect. While impaired liver function may impact clotting factors, it is not a common manifestation of nephrotic
syndrome.
D. Correct. Nephrotic syndrome is associated with a loss of anticoagulant proteins, particularly antithrombin III, in the urine. This loss of anticoagulant proteins contributes to a state of hypercoagulability, increasing the risk of thromboembolic events, such as deep vein thrombosis and pulmonary embolism.
Explanation
A. Incorrect. Abdominal distension and discomfort are not typical manifestations of a urinary tract infection, even in the presence of proteinuria.
B. Correct. Nephrotic syndrome often results in hypoalbuminemia due to significant protein loss in the urine. Hypoalbuminemia leads to decreased oncotic pressure in the blood vessels, causing fluid to leak into the peritoneal cavity and resulting in abdominal distension and discomfort, known as ascites.
C. Incorrect. Hyperkalemia may occur in chronic kidney disease, including nephrotic syndrome, but it is not directly related to abdominal distension and discomfort.
D. Incorrect. Renal vein thrombosis is a complication of nephrotic syndrome but is not typically associated with acute abdominal distension and discomfort.
Explanation
A. Incorrect. While increased cholesterol synthesis in the liver can contribute to hyperlipidemia, it is not the primary reason for elevated lipid levels in nephrotic syndrome.
B. Incorrect. Impaired fat absorption in the small intestine is not a significant factor contributing to hyperlipidemia in nephrotic syndrome.
C. Correct. Nephrotic syndrome results in increased protein loss, including proteins involved in lipid transport and metabolism. Reduced clearance of lipids by the kidneys leads to elevated lipid levels in the bloodstream.
D. Incorrect. Elevated blood glucose levels and insulin resistance are not directly related to hyperlipidemia in nephrotic syndrome.
QUESTIONS
Explanation
A. Incorrect. While a renal biopsy may provide information about kidney function and glomerular filtration rate, its primary purpose in diagnosing nephrotic syndrome is to identify the specific histopathological changes in the kidney, which can help confirm the diagnosis and guide treatment decisions.
B. Incorrect. The response to diuretic therapy can be monitored through other means, such as assessing urine output and fluid balance. A renal biopsy is not performed primarily to evaluate the response to diuretics.
C. Incorrect. Renal biopsy is not typically used to evaluate the extent of renal inflammation and infection. Other imaging or laboratory tests are more suitable for assessing renal inflammation and infection.
D. Correct. A renal biopsy is the definitive diagnostic procedure for nephrotic syndrome. It allows the pathologist to examine a small tissue sample from the kidney and identify the specific histopathological changes, such as glomerular changes, that confirm the diagnosis.
Explanation
A. Incorrect. Decreased serum albumin levels may contribute to fluid overload and hypertension in nephrotic syndrome, but they are not the primary indicators of these complications.
B. Incorrect. A decreased serum albumin level alone does not confirm the presence of proteinuria, which requires additional tests, such as a 24-hour urine collection for protein quantification.
C. Incorrect. Decreased serum albumin levels are not directly related to the presence of renal vein thrombosis, although nephrotic syndrome can increase the risk of thromboembolic events.
D. Correct. In nephrotic syndrome, the glomerular damage results in significant proteinuria, leading to decreased serum albumin levels. The loss of albumin in the urine contributes to hypoalbuminemia, a hallmark feature of nephrotic syndrome.
Explanation
A. Incorrect. Glomerular filtration rate and kidney function are typically assessed through blood tests, such as serum creatinine and blood urea nitrogen (BUN) levels. A 24-hour urine collection is not used to assess these parameters.
B. Incorrect. The presence of glucose and ketones in the urine is typically assessed using a urinalysis or dipstick test. A 24-hour urine collection is not used to determine glucose and ketone levels.
C. Correct. A 24-hour urine collection measures the amount of protein excreted in the urine over a 24-hour period. This test is essential in diagnosing and monitoring nephrotic syndrome, as significant proteinuria is a hallmark feature of the condition.
D. Incorrect. The concentration of electrolytes in the urine is not typically assessed through a 24-hour urine collection. Urinary electrolyte levels are more commonly evaluated through spot urine samples or blood tests.
Explanation
A. Incorrect. Monitoring lipid levels is not primarily aimed at identifying liver dysfunction in clients with nephrotic syndrome.
B. Incorrect. While nephrotic syndrome can lead to secondary diabetes mellitus in some cases, monitoring lipid levels is not a direct indicator of diabetes.
C. Correct. Nephrotic syndrome is associated with increased levels of lipids, including cholesterol and triglycerides, in the blood (hyperlipidemiA. . Monitoring lipid levels helps detect this common complication of nephrotic syndrome and informs treatment decisions.
D. Incorrect. Monitoring lipid levels is not directly related to evaluating electrolyte imbalances in clients with nephrotic syndrome. Electrolyte imbalances are typically assessed through separate blood tests.
QUESTIONS
Explanation
A. Correct. Diuretics are commonly used to manage edema in clients with nephrotic syndrome. They help increase urine output and reduce fluid retention, which can alleviate severe edema and fluid overload.
B. Incorrect. Restricting fluid intake is not typically recommended for clients with nephrotic syndrome, as it may lead to dehydration and worsen the hypoalbuminemia.
C. Incorrect. While adequate protein intake is essential, a high-protein diet may not be appropriate for clients with nephrotic syndrome due to increased protein loss in the urine.
D. Incorrect. Monitoring blood glucose levels is important, but it is not directly related to managing edema and hypoalbuminemia in nephrotic syndrome.
Explanation
A. Incorrect. Corticosteroids should be taken with food to reduce the risk of gastrointestinal side effects.
B. Incorrect. While corticosteroids may improve proteinuria over time, it is unlikely to see an immediate improvement after starting the medication.
C. Correct. Corticosteroids can suppress the immune system and increase the risk of infection, so the client should avoid crowded places and contact with individuals who are sick to minimize the risk of infections.
D. Incorrect. Corticosteroids do not specifically affect potassium levels, so there is no need for a diet high in potassium to offset potential electrolyte imbalances.
Explanation
A. Incorrect. Increasing sodium intake would worsen edema and fluid retention in clients with nephrotic syndrome, as sodium contributes to fluid retention.
B. Incorrect. While protein intake may need to be adjusted in nephrotic syndrome, a low-protein diet is not typically indicated, as clients may already have protein loss in the urine.
C. Incorrect. Encouraging fluid restriction is not recommended in nephrotic syndrome, as it may lead to dehydration and worsen edema due to hypoalbuminemia.
D. Correct. A low-sodium diet is crucial in managing edema in nephrotic syndrome. Sodium intake can lead to fluid retention, and reducing sodium intake helps decrease edema.
Explanation
A. Correct. ACE inhibitors are commonly prescribed in nephrotic syndrome to reduce proteinuria by dilating blood vessels and decreasing pressure in the glomerulus. This helps preserve kidney function and slow the progression of kidney damage.
B. Incorrect. ACE inhibitors are not primarily used to manage blood glucose levels in diabetes, although they may have some impact on blood pressure control in clients with both diabetes and nephrotic syndrome.
C. Incorrect. ACE inhibitors do not directly impact calcium absorption or bone health in nephrotic syndrome.
D. Incorrect. ACE inhibitors do not specifically increase potassium excretion. In fact, they may lead to potassium retention, so clients may need to be cautious about potassium intake while on ACE inhibitors.
Explanation
A. Incorrect. Elevated platelet count and clotting factors are not characteristic of nephrotic syndrome. Clients with nephrotic syndrome tend to have normal platelet counts.
B. Incorrect. Decreased blood viscosity and enhanced blood flow would not directly lead to an increased risk of thromboembolic events in nephrotic syndrome.
C. Incorrect. While impaired liver function may impact clotting factors, it is not a common manifestation of nephrotic syndrome.
D. Correct. Nephrotic syndrome is associated with a loss of anticoagulant proteins, particularly antithrombin III, in the urine. This loss of anticoagulant proteins contributes to a state of hypercoagulability, increasing the risk of thromboembolic events, such as deep vein thrombosis and pulmonary embolism.
Explanation
A. Incorrect. While increased cholesterol synthesis in the liver can contribute to hyperlipidemia, it is not the primary reason for elevated lipid levels in nephrotic syndrome.
B. Incorrect. Impaired fat absorption in the small intestine is not a significant factor contributing to hyperlipidemia in nephrotic syndrome.
C. Correct. Nephrotic syndrome results in increased protein loss, including proteins involved in lipid transport and metabolism. Reduced clearance of lipids by the kidneys leads to elevated lipid levels in the bloodstream.
D. Incorrect. Elevated blood glucose levels and insulin resistance are not directly related to hyperlipidemia in nephrotic syndrome.
QUESTIONS
Explanation
A. Correct. Monitoring blood pressure regularly is essential for clients with nephrotic syndrome, as they are at risk of hypertension due to fluid retention.
B. Incorrect. Restricting fluid intake is not typically recommended for clients with nephrotic syndrome, as it may lead to dehydration and worsen edema due to hypoalbuminemia.
C. Correct. Clients with nephrotic syndrome are at increased risk of infections due to immunosuppression from protein loss in the urine. Reporting any signs of infection is crucial to ensure timely intervention.
D. Correct. Daily weight monitoring is essential for clients with nephrotic syndrome to assess for fluid retention. Sudden weight changes can indicate worsening edema and fluid overload.
Explanation
A. Incorrect. Increased urine output and dehydration are not common side effects of corticosteroid therapy. Instead, clients may experience fluid retention and edema due to the medication's effects.
B. Correct. Corticosteroids can cause increased appetite, leading to weight gain, which is a common side effect that clients should be aware of.
C. Incorrect. Frequent bruising and prolonged bleeding are not typical side effects of corticosteroids. Instead, clients on corticosteroid therapy may experience increased susceptibility to infections and impaired wound healing.
D. Incorrect. Corticosteroids are more likely to cause fluid retention and increased blood pressure, leading to potential hypertension, rather than low blood pressure and dizziness.
Explanation
A. Incorrect. While protein intake may need to be adjusted in nephrotic syndrome, increasing protein intake is not typically recommended, as clients may already have significant protein loss in the urine.
B. Incorrect. Limiting potassium-rich foods is not a primary dietary concern in nephrotic syndrome. Clients should consume a balanced diet unless instructed otherwise by their healthcare provider.
C. Correct. A low-sodium diet is crucial in managing fluid retention and edema in clients with nephrotic syndrome. Sodium intake contributes to fluid retention, so reducing sodium intake helps decrease edema.
D. Incorrect. Restricting fluid intake is not typically recommended in nephrotic syndrome, as it may lead to dehydration and worsen fluid imbalances due to hypoalbuminemia.
Explanation
A. Incorrect. While some clients on ACE inhibitors may need to be cautious about potassium intake, this instruction is not universally applicable to all clients with nephrotic syndrome on this medication.
B. Incorrect. ACE inhibitors should be taken with food to reduce the risk of gastrointestinal side effects.
C. Incorrect. Monitoring blood glucose levels is important, but it is not directly related to ACE inhibitor use in nephrotic syndrome.
D. Correct. ACE inhibitors can cause a drop in blood pressure, leading to dizziness, especially when changing positions (orthostatic hypotension). Clients should be instructed to change positions slowly to prevent falls and injuries.
Explanation
A. Incorrect. While some clients may be at increased risk of certain infections, avoiding close contact with family members is not practical and not recommended in general.
B. Correct. Good hand hygiene is essential in reducing the risk of infections in clients with nephrotic syndrome, as they are immunocompromised due to protein loss in the urine. Regular handwashing with soap and water, especially before meals and after using the bathroom, can help prevent the spread of pathogens.
C. Incorrect. Avoiding outdoor activities and crowded places is not necessary for all clients with nephrotic syndrome and may negatively impact their quality of life.
D. Incorrect. While physical activity is generally beneficial for overall health, it is not directly related to enhancing the immune system's response in clients with nephrotic syndrome.
Explanation
A. Incorrect. While monitoring urine output and kidney function is important in nephrotic syndrome, it is not directly related to addressing skin breakdown.
B. Correct. Skin breakdown in clients with nephrotic syndrome can lead to an increased risk of infection. The nurse should assess the affected skin areas for signs of infection, such as redness, warmth, swelling, and drainage.
C. Incorrect. Providing pain medication may be necessary for managing discomfort, but the priority is to prevent infection and promote wound healing.
D. Incorrect. While reducing edema is important, it is not the immediate priority in managing skin breakdown and preventing infection.
Explanation
A. Correct. Immunosuppressive medications are prescribed in nephrotic syndrome to reduce inflammation in the kidneys and prevent further damage, including kidney scarring. They help slow the progression of the disease and preserve kidney function.
B. Incorrect. Immunosuppressive medications are not primarily used to address fluid overload or improve urinary output in nephrotic syndrome.
C. Incorrect. While some immunosuppressive medications may have an impact on blood glucose levels, they are not typically used to manage diabetes in nephrotic syndrome.
D. Incorrect. Immunosuppressive medications do not directly alleviate pain and discomfort associated with edema in nephrotic syndrome. Other interventions, such as diuretics, are used for managing edema.
QUESTIONS
Acute renal failure
Explanation
A. Incorrect. Acute renal failure is not a chronic condition; it is an acute condition that develops rapidly and is typically reversible with prompt treatment.
B. Incorrect. While long-term uncontrolled diabetes can lead to chronic kidney disease, acute renal failure is not caused by chronic kidney damage related to diabetes.
C. Correct. Acute renal failure, also known as acute kidney injury (AKI), is characterized by a sudden and temporary loss of kidney function. It is often caused by factors such as decreased blood flow to the kidneys, kidney damage, or obstruction of the urinary tract.
D. Incorrect. While the statement is partially true, it does not capture the acute and sudden nature of acute renal failure. The inability of the kidneys to filter waste products from the blood is one of the manifestations of AKI.
Explanation
A. Incorrect. Elevated blood pressure is not typically an initial assessment finding in acute renal failure. In fact, it is more common to see low blood pressure (hypotension) due to decreased blood flow to the kidneys.
B. Correct. One of the hallmark manifestations of acute renal failure is decreased urine output (oliguriA. or even no urine output (anuriA. . This is often accompanied by low blood pressure as a result of decreased kidney function.
C. Incorrect. Acute renal failure usually leads to changes in blood pressure and urine output. Stable blood pressure and urine output are not typical initial assessment findings in this condition.
D. Incorrect. High blood sugar levels and frequent urination are not directly related to acute renal failure. These symptoms are more characteristic of diabetes mellitus.
Explanation
A. Correct. Hypertension (high blood pressurE. is a significant risk factor for the development of acute renal failure. Elevated blood pressure can damage the blood vessels in the kidneys and impair kidney function.
B. Incorrect. Osteoporosis is not directly related to the development of acute renal failure. Osteoporosis is a condition characterized by weak and brittle bones.
C. Incorrect. While type 2 diabetes is a risk factor for chronic kidney disease, it is not a common risk factor for the development of acute renal failure.
D. Incorrect. Seasonal allergies are not associated with an increased risk of acute renal failure.
Explanation
A. Incorrect. Hypotension and tachycardia are more commonly associated with fluid depletion, not fluid overload.
B. Incorrect. Dry mucous membranes and decreased skin turgor are signs of dehydration, which is not indicative of fluid overload.
C. Correct. Fluid overload in acute renal failure can lead to pulmonary congestion and edema in the extremities. Crackles in the lungs (rales) are auscultated when there is fluid accumulation in the lung tissue, and edema in the extremities is visible swelling caused by excessive fluid retention.
D. Incorrect. Hypoactive bowel sounds and constipation are not directly related to fluid overload in acute renal failure.
Explanation
A. Incorrect. While protein intake may need to be adjusted in acute renal failure, increasing protein intake is not typically recommended during the acute phase, as it may place additional stress on the kidneys.
B. Correct. Limiting potassium-rich foods is essential for clients with acute renal failure, as impaired kidney function can lead to hyperkalemia (high potassium levels), which can be life-threatening.
C. Incorrect. A high-sodium diet is not recommended in acute renal failure, as it can exacerbate fluid retention and fluid overload.
D. Incorrect. Fluid restriction is not typically recommended in acute renal failure, especially if the client is experiencing fluid depletion and dehydration.
Explanation
A. Incorrect. Loop diuretics are used to increase urine output, not decrease it. They help reduce fluid overload and prevent dehydration.
B. Incorrect. Loop diuretics typically lead to a decrease in blood pressure, not an increase. They are often prescribed to address hypertension in acute renal failure.
C. Incorrect. Loop diuretics promote the excretion of sodium and water from the kidneys, not their reabsorption.
D. Correct. Loop diuretics are prescribed in acute renal failure to increase urine output and promote fluid excretion. This helps reduce fluid overload and decrease edema.
Explanation
A. Correct. In acute renal failure, when the kidneys are unable to excrete acids properly, metabolic acidosis can occur. Administering bicarbonate intravenously helps raise the pH levels and correct the acid-base imbalance.
B. Incorrect. Encouraging the client to consume more acidic foods would worsen metabolic acidosis and is not a suitable intervention.
C. Incorrect. Increasing fluid intake is not a specific intervention for correcting metabolic acidosis. The focus should be on addressing the underlying acid-base imbalance.
D. Incorrect. Promoting shallow breathing to retain carbon dioxide is not a recommended intervention for correcting metabolic acidosis. Respiratory acidosis and metabolic acidosis are different types of acid-base imbalances with distinct causes and treatments.
Explanation
A. Incorrect. While administering prescribed medications is important, the priority in acute renal failure is to closely monitor the client's intake and output to assess kidney function and fluid balance.
B. Correct. Monitoring intake and output is a priority nursing intervention in acute renal failure. Accurate assessment of urine output helps determine the client's kidney function and the effectiveness of treatment.
C. Incorrect. Providing emotional support is essential, but it is not the priority over monitoring kidney function and fluid balance.
D. Incorrect. Preventing infection and complications is important, but it is not the priority over assessing kidney function in acute renal failure.
QUESTIONS
Explanation
A. Incorrect. While long-term use of NSAIDs can contribute to kidney damage and chronic kidney disease, it is not the primary cause of acute renal failure.
B. Incorrect. Acute renal failure is a sudden and abrupt loss of kidney function, and it is distinct from chronic kidney disease, which develops gradually over time.
C. Correct. Acute renal failure is characterized by a rapid and sudden decline in kidney function, often caused by a sudden decrease in blood flow to the kidneys (prerenal), kidney injury (intrinsiC. , or obstruction of the urinary tract (postrenal).
D. Incorrect. While UTIs and kidney stones can cause kidney injury, they are not the exclusive causes of acute renal failure, which can have various underlying etiologies.
Explanation
A. Correct. Dehydration is a significant risk factor for prerenal acute renal failure. Insufficient fluid intake or excessive fluid loss (e.g., vomiting, diarrheA. can lead to decreased blood volume and decreased blood flow to the kidneys, impairing kidney function.
B. Incorrect. A UTI can cause kidney injury but is not specifically associated with prerenal acute renal failure.
C. Incorrect. Chronic kidney disease (CKD. is a risk factor for the development of intrinsic acute renal failure, but it is not directly related to prerenal causes.
D. Incorrect. Diabetes mellitus is a risk factor for chronic kidney disease, but it is not a specific risk factor for prerenal acute renal failure.
Explanation
A. Incorrect. Hypovolemia is associated with prerenal acute renal failure, not intrinsic acute renal failure.
B. Correct. Glomerulonephritis is one of the common causes of intrinsic acute renal failure. It is characterized by inflammation of the glomeruli in the kidneys, which can lead to kidney damage and impaired function.
C. Incorrect. Prostate enlargement is associated with postrenal acute renal failure due to urinary tract obstruction, not intrinsic causes.
D. Incorrect. Urinary tract obstruction is also associated with postrenal acute renal failure, not intrinsic causes.
Explanation
A. Correct. Nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen, are known to cause kidney damage and are a common cause of intrinsic acute renal failure, especially when used in high doses or for extended periods.
B. Incorrect. Loop diuretics, such as furosemide, are not typically associated with intrinsic acute renal failure.
C. Incorrect. Metformin is not a common cause of intrinsic acute renal failure. However, it is contraindicated in individuals with severe kidney impairment.
D. Incorrect. While ciprofloxacin and other antibiotics may have renal-related side effects, they are not a common cause of intrinsic acute renal failure.
Explanation
A. Incorrect. Hypertension is a risk factor for prerenal acute renal failure, not postrenal.
B. Incorrect. While a UTI can cause kidney injury, it is not directly related to postrenal acute renal failure.
C. Correct. An enlarged prostate, also known as benign prostatic hyperplasia (BPH), can cause obstruction of the urinary tract and lead to postrenal acute renal failure. The obstruction prevents urine flow, causing pressure buildup in the kidneys and impairing kidney function.
D. Incorrect. Chronic kidney disease (CKD. is a risk factor for intrinsic acute renal failure, not postrenal.
Explanation
A. Correct. Hypertension, or high blood pressure, is a significant risk factor for the development of acute renal failure. Chronic hypertension can lead to kidney damage and impaired kidney function over time.
B. Incorrect. Seasonal allergies, osteoarthritis, and anemia are not direct risk factors for acute renal failure.
C. Incorrect. Osteoarthritis is not directly related to acute renal failure.
D. Incorrect. While anemia can be associated with chronic kidney disease, it is not a specific risk factor for acute renal failure.
Explanation
A. Correct. Angiotensin-converting enzyme (ACE. inhibitors can contribute to prerenal acute renal failure, especially in clients with preexisting cardiovascular disease. These medications may cause vasodilation and decrease blood flow to the kidneys, leading to impaired kidney function.
B. Incorrect. Beta-blockers are not directly associated with prerenal acute renal failure.
C. Incorrect. Calcium channel blockers are not typically associated with prerenal acute renal failure.
D. Incorrect. Thiazide diuretics may cause electrolyte imbalances and metabolic disturbances, but they are not a common cause of prerenal acute renal failure.
QUESTIONS
Explanation
A. Incorrect. Increased glomerular filtration rate (GFR) would lead to increased urine output, not decreased urine output.
B. Incorrect. Obstruction of the urethra would cause postrenal acute renal failure and may lead to urinary retention, but it would not cause decreased urine output in prerenal or intrinsic acute renal failure.
C. Correct. In prerenal and intrinsic acute renal failure, impaired blood flow to the kidneys reduces the perfusion of nephrons, leading to decreased urine output.
D. Incorrect. Excessive fluid intake may contribute to fluid overload and decreased urine output in prerenal acute renal failure, but it is not the primary pathophysiological process that leads to decreased urine output.
Explanation
A. Incorrect. Constipation and abdominal pain are not typical manifestations of the fluid and electrolyte imbalance seen in acute renal failure.
B. Correct. Acute renal failure can lead to imbalances in electrolytes, particularly potassium and sodium. Muscle weakness and fatigue are common manifestations of these electrolyte imbalances.
C. Incorrect. Decreased heart rate and blood pressure are more commonly associated with fluid volume depletion in prerenal acute renal failure, rather than electrolyte imbalances.
D. Incorrect. Increased respiratory rate and depth are not typically associated with acute renal failure or its fluid and electrolyte imbalances.
Explanation
A. Incorrect. Elevated creatinine levels are not specific to dehydration and fluid deficit, although dehydration can contribute to prerenal acute renal failure.
B. Incorrect. Elevated creatinine levels do not suggest normal kidney function. Instead, they indicate impaired kidney function and acute kidney injury.
C. Correct. Creatinine is a waste product produced by muscles and excreted by the kidneys. Elevated creatinine levels are a reliable indicator of acute kidney injury and impaired kidney function.
D. Incorrect. Elevated creatinine levels can be seen in both acute and chronic kidney diseases, but they are not exclusively seen in chronic kidney disease.
Explanation
A. Incorrect. Increased heart rate and blood pressure are more commonly associated with metabolic alkalosis, not metabolic acidosis.
B. Correct. Muscle twitching and irritability are common clinical manifestations of metabolic acidosis. Acidosis can lead to an increase in excitability of nerve cells, causing muscle twitching and irritability.
C. Incorrect. Excessive thirst and frequent urination are not typically associated with metabolic acidosis.
D. Incorrect. Warm, flushed skin and headache are not directly related to metabolic acidosis.
Explanation
A. Incorrect. Muscle weakness and fatigue are manifestations of hyperkalemia, but they are not the most critical indicators of severe hyperkalemia.
B. Incorrect. Tingling sensations in the extremities are not the most critical indicator of severe hyperkalemia.
C. Correct. The most critical manifestation of severe hyperkalemia is an irregular heart rhythm (dysrhythmiA. , which can be life-threatening.
D. Incorrect. Excessive thirst and dry mucous membranes are not specific to hyperkalemia and are not the most critical indicators of severe hyperkalemia.
Explanation
A. Incorrect. Increased urine output and polyuria are not associated with uremia. In fact, acute renal failure often leads to decreased urine output (oliguria or anuriA. .
B. Incorrect. Hypertension and bradycardia are not typical manifestations of uremia.
C. Correct. Uremia is a condition characterized by the buildup of waste products and toxins in the blood due to impaired kidney function. Clinical manifestations of uremia include confusion (encephalopathy), nausea and vomiting, and pericarditis (inflammation of the pericardium, the sac surrounding the heart).
D. Incorrect. Decreased respiratory rate and shallow breathing are not directly associated with uremia.
Explanation
A. Incorrect. Decreased blood volume and hypovolemia may contribute to prerenal acute renal failure, but they are not the primary pathophysiological processes that lead to edema in acute renal failure.
B. Incorrect. Increased vascular permeability and leakage of fluid into tissues are not the primary mechanisms of edema in acute renal failure.
C. Correct. In acute renal failure, the impaired filtration and reduced excretion of fluid by the kidneys lead to fluid retention and edema in various parts of the body.
D. Incorrect. Excessive fluid intake and fluid overload may contribute to fluid retention and edema in prerenal acute renal failure, but they are not the primary pathophysiological process in acute renal failure.
Explanation
A. Incorrect. Bradypnea (slow respiratory ratE. is not typically associated with acute renal failure.
B. Correct. Kussmaul respirations are rapid and deep respirations seen in metabolic acidosis, a common complication of acute renal failure. The body tries to compensate for the acidosis by increasing the elimination of carbon dioxide through rapid and deep breathing.
C. Incorrect. Dyspnea and crackles in the lungs are not directly related to acute renal failure.
D. Incorrect. Increased respiratory rate and shallow breathing are not typical respiratory manifestations of acute renal failure.
QUESTIONS
Explanation
A. Incorrect. A complete blood count (CBC. provides information about the number and types of blood cells but does not assess kidney function.
B. Correct. Serum creatinine level is a commonly used blood test to assess kidney function. Elevated levels of creatinine in the blood indicate impaired glomerular filtration and decreased kidney function.
C. Incorrect. Urinalysis provides information about the presence of substances such as protein, blood, and glucose in the urine but does not directly assess GFR.
D. Incorrect. Renal ultrasound is an imaging test that provides information about the structure of the kidneys but does not directly measure GFR.
Explanation
A. Correct. A renal ultrasound is an imaging test that uses sound waves to create images of the kidneys. It can help identify kidney stones, obstructions, and other structural abnormalities in the urinary tract.
B. Incorrect. The renal ultrasound does not directly measure the glomerular filtration rate (GFR), which is typically assessed through blood tests.
C. Incorrect. A renal ultrasound does not provide information about the number and types of blood cells in the bloodstream.
D. Incorrect. While a renal ultrasound can visualize the blood vessels in the kidneys, its primary purpose is to assess kidney structure, not blood flow.
Explanation
A. Incorrect. Fasting is not typically required before a renal biopsy.
B. Incorrect. The renal biopsy does not directly measure the glomerular filtration rate (GFR), which is usually assessed through blood tests.
C. Correct. A renal biopsy is a procedure in which a needle is inserted through the skin and into the kidneys to obtain a small tissue sample for examination. This allows for a direct assessment of kidney tissue and helps identify the cause of kidney dysfunction.
D. Incorrect. While a renal biopsy can provide information about the kidney's structure, its primary purpose is to obtain a tissue sample for histological examination, not to assess blood flow.
Explanation
A. Incorrect. Withholding food and drink for 24 hours is not necessary for a CT scan with contrast dye.
B. Correct. Before a CT scan with contrast dye, it is essential to assess the client for allergies, especially to iodine and shellfish. Contrast dyes used in CT scans contain iodine, and clients with allergies to iodine or shellfish may have an allergic reaction to the contrast dye.
C. Incorrect. While administering intravenous fluids may be beneficial in certain situations, it is not a specific precaution for a CT scan with contrast dye.
D. Incorrect. Removing jewelry and metallic objects is a standard precaution for all imaging procedures, but it is not specific to a CT scan with contrast dye.
Explanation
A. Incorrect. Unlike computed tomography (CT) scans, MRI scans do not typically require the ingestion of a contrast solution.
B. Incorrect. The MRI scan does not directly measure the glomerular filtration rate (GFR), which is typically assessed through blood tests.
C. Incorrect. A renal biopsy involves inserting a needle through the back to obtain a tissue sample from the kidneys, not an MRI scan.
D. Correct. Before an MRI scan, clients need to remove all metal objects and devices, including jewelry, piercings, hearing aids, and certain medical implants. Metal can interfere with the MRI's magnetic field and cause safety concerns during the procedure.
Explanation
A. Incorrect. Fasting is not typically required before a renal nuclear scan.
B. Incorrect. The renal nuclear scan does not directly measure the glomerular filtration rate (GFR), which is typically assessed through blood tests.
C. Incorrect. A renal nuclear scan does not involve inserting a catheter into the bladder to obtain a urine sample.
D. Correct. A renal nuclear scan, also known as a renal scintigraphy, involves injecting a small amount of radioactive material intravenously. The radioactive material is taken up by the kidneys, and the scan creates images that assess kidney function and blood flow.
QUESTIONS
Explanation
A. Incorrect. While fluid restriction may be necessary in certain cases of acute renal failure, it should be prescribed and monitored by the healthcare provider based on the client's specific needs.
B. Incorrect. A high-protein diet can put additional strain on the kidneys, and it is not recommended for clients with acute renal failure.
C. Incorrect. Over-the-counter diuretics may not be safe for clients with acute renal failure and can lead to further electrolyte imbalances.
D. Correct. The nurse's best response is to encourage the client to follow their healthcare provider's instructions and avoid medications that may harm the kidneys. Compliance with prescribed treatment plans and avoiding nephrotoxic medications are essential to support kidney function and prevent further damage.
Explanation
A. Incorrect. Hemodialysis is not a procedure for kidney transplantation.
B. Correct. Hemodialysis is a treatment that helps remove waste products, toxins, and excess fluids from the blood when the kidneys are not functioning properly. It helps maintain the body's internal environment and prevent complications of acute renal failure.
C. Incorrect. While hemodialysis can improve kidney function temporarily, its primary purpose is to provide kidney support and replace some of the kidney's functions.
D. Incorrect. The description provided refers to the insertion of a urinary catheter for bladder drainage, not hemodialysis.
Explanation
A. Incorrect. Continuous renal replacement therapy (CRRT) provides gradual and continuous removal of waste products and excess fluids from the blood, but it may not be as rapid as intermittent hemodialysis.
B. Incorrect. CRRT typically requires continuous sessions, which may last 24 hours or more. Intermittent hemodialysis involves shorter but more frequent sessions.
C. Correct. One of the primary advantages of CRRT is that it does not require the use of anticoagulants to prevent blood clotting in the machine. This reduces the risk of bleeding and other complications associated with anticoagulant use during hemodialysis.
D. Incorrect. The cost of CRRT and intermittent hemodialysis can vary based on the healthcare setting and the client's needs. The cost-effectiveness depends on individual factors and resource availability.
Explanation
A. Incorrect. Cloudy dialysis fluid may indicate infection or peritonitis, which requires immediate attention and intervention.
B. Correct. Cloudy dialysis fluid may indicate infection or peritonitis, which can be a severe complication of peritoneal dialysis. The nurse should stop the procedure immediately and notify the healthcare provider for further assessment and management.
C. Incorrect. Administering antibiotics without a proper diagnosis and healthcare provider's order is not appropriate.
D. Incorrect. Increasing the dwell time would not address the issue of cloudy dialysis fluid and potential infection.
Explanation
A. Incorrect. Increasing the rate of dialysis may further lower the client's blood pressure and worsen the situation.
B. Incorrect. Administering an antihypertensive medication during a hypotensive episode could exacerbate the client's low blood pressure.
C. Correct. The nurse's priority action is to stop the dialysis procedure immediately and notify the healthcare provider of the significant drop in blood pressure. The client may be experiencing a hypotensive episode, which requires prompt evaluation and intervention.
D. Incorrect. Increasing the client's
fluid intake is not appropriate during a hypotensive episode, as it may not rapidly improve blood pressure and could lead to fluid overload.
Explanation
A. Correct. Loop diuretics can cause potassium loss and potentially lead to hypokalemia. The nurse should monitor the client's serum potassium levels frequently to assess for any imbalances.
B. Incorrect. While loop diuretics can be given intravenously for rapid action, the administration route depends on the client's condition and the healthcare provider's order.
C. Incorrect. Loop diuretics are used to promote diuresis and fluid removal from the body. Encouraging fluid restriction while on diuretic therapy may exacerbate dehydration and electrolyte imbalances.
D. Incorrect. The timing of loop diuretic administration is determined by the healthcare provider's order and the client's specific needs. Taking diuretics at bedtime may result in increased nighttime urination and sleep disruption.
QUESTIONS
Explanation
A. Incorrect. Increasing sodium intake would exacerbate fluid retention and worsen the client's fluid overload.
B. Correct. Limiting fluid intake to the prescribed amount helps manage fluid balance in clients with acute renal failure, especially those experiencing fluid overload.
C. Incorrect. Rapid administration of intravenous fluids may worsen fluid overload and increase the risk of edema and hypertension.
D. Incorrect. Encouraging the client to drink water freely would exacerbate fluid overload and impair the body's ability to eliminate excess fluids.
Explanation
A. Correct. Bananas and oranges are high-potassium fruits that the client should avoid on a potassium-restricted diet.
B. Incorrect. Bread and pasta are not typically high in potassium and are usually acceptable in a potassium-restricted diet.
C. Incorrect. Eggs and cheese are not significant sources of potassium and are usually allowed in a potassium-restricted diet.
D. Incorrect. Chicken and fish are sources of protein and do not have high potassium content that would require restriction in most cases.
Explanation
A. Incorrect. Encouraging the client to sit up in a chair for extended periods can increase pressure on certain areas and contribute to skin breakdown.
B. Incorrect. Applying a heating pad to areas at risk for skin breakdown can lead to thermal injury and exacerbate skin issues.
C. Correct. Regular repositioning and skin assessments are essential in preventing pressure ulcers and maintaining skin integrity in clients with acute renal failure who may be bedridden or have limited mobility.
D. Incorrect. Adhesive tape can cause skin irritation and damage when removed, especially in clients at risk for impaired skin integrity.
Explanation
A. Incorrect. Encouraging a low-carbohydrate diet is not the appropriate intervention for correcting metabolic acidosis.
B. Correct. Sodium bicarbonate is an alkalizing agent that can help correct metabolic acidosis by increasing the body's bicarbonate levels, which buffers excess acids.
C. Incorrect. Fluid restriction would not directly correct metabolic acidosis and may be detrimental to the client's overall fluid balance.
D. Incorrect. Deep breathing exercises are not specific interventions for correcting metabolic acidosis.
Explanation
A. Correct. Encouraging the client to perform active range-of-motion exercises can help prevent complications of immobility, such as muscle wasting and joint contractures.
B. Incorrect. Elevating the head of the bed primarily benefits respiratory function and does not directly address the complications of immobility.
C. Incorrect. Limiting fluid intake would not prevent complications of immobility and may lead to dehydration.
D. Incorrect. Administering pain medication before passive range-of-motion exercises is not a standard practice and does not directly prevent complications of immobility.
Explanation
:
A. Incorrect. Cheese and yogurt are high in phosphate and should be avoided in a low-phosphate diet.
B. Incorrect. Beans and lentils are also high in phosphate and are not suitable for a low-phosphate diet.
C. Incorrect. Eggs and poultry are significant sources of phosphate and are not recommended in a low-phosphate diet.
D. Correct. Fresh fruits and vegetables are generally low in phosphate and are suitable for a low-phosphate diet. These foods can help meet the client's nutritional needs while adhering to the dietary restriction.
Explanation
A. Incorrect. Muscle cramps in acute renal failure are often related to electrolyte imbalances, including high potassium levels. Encouraging the consumption of potassium-rich foods would exacerbate the issue.
B. Incorrect. Muscle relaxants may not be appropriate for all clients, and the underlying cause of the muscle cramps should be addressed first.
C. Correct. Applying warm compresses to the affected muscles can help relax muscle tension and provide relief from muscle cramps.
D. Incorrect. Gentle stretching exercises may not be appropriate for a client experiencing muscle cramps, as stretching could exacerbate the discomfort.
Explanation
A. Correct. Erythropoietin-stimulating agents (ESAs) are commonly used to treat anemia in clients with renal failure. These medications stimulate the production of red blood cells and help manage anemia associated with kidney dysfunction.
B. Incorrect. Anticoagulants such as heparin are not used to treat anemia; they are prescribed to prevent blood clotting and thrombosis.
C. Incorrect. Loop diuretics are used to promote diuresis and manage fluid overload in clients with acute renal failure; they do not treat anemia.
D. Incorrect. Antihypertensive agents are prescribed to manage hypertension and do not treat anemia in clients with renal failure.
QUESTIONS
Chronic renal failure
Explanation
A. Incorrect. Being physically active and maintaining a healthy weight can actually reduce the risk of chronic renal failure, as it helps to control blood pressure and blood sugar levels, which are risk factors for kidney disease.
B. Incorrect. Having a family history of kidney disease can increase the risk of chronic renal failure, as genetics can play a role in the development of kidney problems.
C. Incorrect. Consuming a high-sodium diet can actually be harmful to the kidneys, as it can lead to hypertension and contribute to kidney damage.
D. Correct. Conditions such as hypertension and diabetes are well-established risk factors for chronic renal failure. These conditions can cause damage to the blood vessels and filtering units of the kidneys over time, leading to kidney dysfunction.
Explanation
A. Incorrect. The volume of urine produced in 24 hours is measured through a different test called the 24-hour urine collection, not the GFR test.
B. Incorrect. The GFR test does not assess blood glucose levels; it is primarily used to evaluate kidney function.
C. Correct. The GFR test measures how well the kidneys are filtering waste and fluids from the blood. It is an important indicator of kidney function and is commonly used to stage chronic renal failure.
D. Incorrect. The GFR test does not specifically measure the excretion of potassium and sodium in the urine; instead, it focuses on overall kidney function and filtration rate.
Explanation
A. Incorrect. While chronic renal failure is often irreversible, the rate of decline in kidney function can vary depending on the underlying cause and the effectiveness of treatment and management.
B. Incorrect. While appropriate lifestyle changes and medications can improve the client's quality of life and slow the progression of the disease, chronic renal failure is a chronic condition that may require ongoing management.
C. Incorrect. Chronic renal failure is generally not curable, but proper management can help stabilize the condition and slow the progression of kidney damage.
D. Correct. The prognosis for chronic renal failure can vary widely depending on factors such as the cause of kidney disease, the stage of kidney damage, and the client's response to treatment. Early intervention, such as controlling blood pressure and blood sugar levels, can help slow the progression of kidney damage and improve long-term outcomes.
Explanation
A. Correct. An increase in blood pressure readings can be an early indication of fluid retention in a client with chronic renal failure. Fluid overload can lead to hypertension as the kidneys struggle to excrete excess fluids.
B. Incorrect. Shortness of breath and crackles in the lungs are signs of fluid overload but are considered more advanced symptoms. These indicate that fluid has accumulated in the lungs, leading to pulmonary edema.
C. Incorrect. Decreased serum potassium levels (hypokalemiA. are not typically associated with fluid overload. Instead, chronic renal failure often leads to hyperkalemia due to impaired potassium excretion.
D. Incorrect. Rapid weight loss over a few days is not indicative of fluid retention; rather, it may suggest dehydration or inadequate caloric intake.
Explanation
A. Incorrect. While assessing vital signs and blood pressure is important, it is not the first action when the client reports cloudy dialysate effluent during an exchange.
B. Correct. Cloudy dialysate effluent may indicate peritonitis, an infection of the peritoneal cavity. Obtaining a sample of the effluent for testing is the first action to determine if an infection is present and requires immediate treatment.
C. Incorrect. Instructing the client to stop the exchange immediately may be necessary if there are signs of infection or other complications, but obtaining a sample of the effluent should be done first to determine the cause.
D. Incorrect. Providing the client with an analgesic is not the priority when the client reports cloudy dialysate effluent; the focus is on identifying the cause of the cloudiness.
Explanation
A. Incorrect. Reducing protein intake can lead to calcium loss and bone fractures in clients with chronic renal failure, as it may affect
bone health.
B. Correct. Limiting protein intake is a common dietary recommendation for clients with chronic renal failure to reduce the workload on the kidneys and slow the progression of kidney damage. Protein metabolism produces waste products that the kidneys must filter and excrete, and reducing protein intake can help alleviate this burden on the already compromised kidneys.
C. Incorrect. Decreasing protein intake may not necessarily improve appetite or overall nutritional status, as protein is essential for maintaining body functions and tissue repair.
D. Incorrect. While reducing protein intake can result in fewer waste products being generated, the primary reason for limiting protein intake in chronic renal failure is to reduce the strain on the kidneys, not solely to decrease waste production.
QUESTIONS
Explanation
A. Incorrect. Smoking and tobacco use are harmful to the kidneys and can increase the risk of chronic renal failure.
B. Incorrect. While genetic factors may play a role in some cases of chronic renal failure, lifestyle changes can significantly impact the risk and progression of kidney disease.
C. Incorrect. While a history of kidney stones may be associated with an increased risk of kidney damage, it is not a primary risk factor for chronic renal failure.
D. Correct. Conditions such as hypertension and diabetes are two of the leading causes of chronic renal failure. Uncontrolled high blood pressure and elevated blood sugar levels can damage the blood vessels and filtering units of the kidneys, leading to chronic kidney disease over time.
Explanation
A. Incorrect. Age is a non-modifiable risk factor for chronic renal failure. While the risk of kidney disease may increase with age, it is not something that individuals can control or change.
B. Incorrect. Gender is also a non-modifiable risk factor, as both males and females can develop chronic renal failure. It does not impact an individual's ability to modify their risk.
C. Correct. Smoking is a modifiable risk factor for chronic renal failure. Smoking can damage blood vessels, leading to reduced blood flow to the kidneys and an increased risk of kidney disease.
D. Incorrect. Family history of kidney disease is a non-modifiable risk factor. While individuals cannot change their family history, they can modify other lifestyle factors, such as smoking, to reduce their overall risk of kidney disease.
Explanation
A. Incorrect. Hyperthyroidism is not a known risk factor for chronic renal failure. However, uncontrolled thyroid disease may contribute to cardiovascular issues that can impact kidney health.
B. Incorrect. Peptic ulcer disease is not a risk factor for chronic renal failure.
C. Incorrect. Chronic obstructive pulmonary disease (COPD. is not directly associated with an increased risk of chronic renal failure. However, chronic illnesses can place additional stress on the kidneys over time.
D. Correct. Hypertension, or high blood pressure, is a significant risk factor for chronic renal failure. Long-term uncontrolled hypertension can damage the blood vessels in the kidneys, leading to chronic kidney disease.
Explanation
A. Incorrect. Diabetes is strongly associated with an increased risk of chronic renal failure. Chronic kidney disease related to diabetes is known as diabetic nephropathy.
B. Correct. Diabetes is a leading cause of chronic renal failure. Uncontrolled high blood sugar levels can damage the blood vessels in the kidneys over time, leading to kidney disease.
C. Incorrect. Both Type 1 and Type 2 diabetes are associated with an increased risk of chronic renal failure. It is essential for individuals with either type of diabetes to manage their blood sugar levels to reduce the risk of kidney complications.
D. Incorrect. Chronic renal failure can be caused by various factors, but diabetes is a significant and common cause of kidney disease, especially in individuals with uncontrolled diabetes.
Explanation
A. Incorrect. Antibiotics are generally safe and are not known to be a risk factor for chronic renal failure.
B. Incorrect. Antihypertensive medications are essential for managing high blood pressure and reducing the risk of kidney damage in individuals with hypertension. They are not considered a risk factor for chronic renal failure.
C. Correct. Proton pump inhibitors (PPIs) are commonly used to treat conditions such as acid reflux and peptic ulcers. Prolonged and high-dose use of PPIs has been associated with an increased risk of kidney disease, including acute interstitial nephritis and chronic kidney disease.
D. Incorrect. Antipyretics such as acetaminophen are generally safe when used appropriately and are not considered a risk factor for chronic renal failure.
Explanation
A. Incorrect. Cardiovascular disease can impact kidney health. The heart and kidneys are closely connected, and conditions that affect the heart can also have implications for kidney function.
B. Incorrect. High cholesterol levels can contribute to cardiovascular disease, and cardiovascular disease is a significant risk factor for chronic renal failure. Therefore, high cholesterol indirectly impacts kidney health.
C. Correct. Cardiovascular disease, including conditions like heart failure or atherosclerosis, can lead to decreased blood flow to the kidneys, impairing kidney function and contributing to chronic renal failure.
D. Incorrect. High blood pressure is a well-established risk factor for chronic renal failure. Uncontrolled hypertension can damage the blood vessels in the kidneys, leading to kidney dysfunction over time.
QUESTIONS
Explanation
A. Correct. Fatigue and weakness are early clinical manifestations of chronic renal failure, often due to anemia and the accumulation of waste products in the blood.
B. Incorrect. Hematuria may be present in some cases of kidney dysfunction, but it is not typically an early symptom of chronic renal failure.
C. Incorrect. Shortness of breath and chest pain are more likely to be associated with fluid overload or cardiac issues, which may occur in advanced stages of chronic renal failure.
D. Incorrect. Hyperkalemia is a complication of chronic renal failure but may not be an early clinical manifestation. It is more likely to occur as kidney function declines and potassium excretion becomes impaired.
Explanation
A. Incorrect. Pruritus (itching) is a common symptom of chronic renal failure and is related to the buildup of waste products and toxins in the blood, leading to skin irritation.
B. Correct. Pruritus is a common and distressing symptom of chronic renal failure, caused by the retention of uremic toxins in the blood. These toxins can irritate the skin and lead to itching.
C. Incorrect. While medications can sometimes cause pruritus as a side effect, it is not the primary cause of itching in clients with chronic renal failure.
D. Incorrect. Persistent pruritus in a client with chronic renal failure is not necessarily indicative of an allergic reaction to medications. It is more likely related to the buildup of waste products in the blood.
Explanation
A. Incorrect. Administering an antiemetic medication may help relieve nausea, but it is not the priority action in a client with chronic renal failure experiencing anorexia and nausea.
B. Incorrect. Encouraging the client to increase protein intake is not appropriate if they are experiencing anorexia and nausea. Protein intake may need to be adjusted based on the client's symptoms and kidney function.
C. Incorrect. While assessing serum electrolyte levels is important in chronic renal failure, it is not the priority action in this situation. The client's anorexia and nausea require immediate attention.
D. Correct. Monitoring the client's weight and fluid intake is the priority action when the client is experiencing anorexia and nausea. These symptoms may indicate fluid and electrolyte imbalances that need to be addressed promptly.
Explanation
A. Correct. Increased blood pressure readings can be an early clinical manifestation of fluid overload in clients with chronic renal failure. Fluid retention can lead to hypertension as the kidneys struggle to excrete excess fluids.
B. Incorrect. Hyperkalemia may occur in chronic renal failure, but it is not an early clinical manifestation of fluid overload.
C. Incorrect. Dry and cracked skin is more commonly associated with dehydration rather than fluid overload.
D. Incorrect. Polyuria is not typically associated with fluid overload. Instead, it may be present in early stages of chronic renal failure due to the inability of the kidneys to concentrate urine properly.
Explanation
A. Incorrect. Applying compression stockings may help reduce swelling but does not address the underlying cause. Additionally, compression stockings should not be used if the client has arterial insufficiency.
B. Incorrect. Elevation may provide temporary relief from swelling, but it does not address the underlying cause of fluid retention
in chronic renal failure.
C. Correct. The nurse should measure the client's blood pressure and pulse rate to assess for fluid overload and possible hypertension, which can be associated with chronic renal failure.
D. Incorrect. Assessing the client's daily protein intake is not the priority when the client presents with swelling in the ankles and legs. Fluid retention is a more immediate concern that requires assessment and intervention.
Explanation
A. Incorrect. Applying a heating pad may provide temporary relief for muscle cramps, but it does not address the underlying cause.
B. Correct. Muscle cramps in clients with chronic renal failure can be caused by dehydration and electrolyte imbalances. Encouraging the client to increase fluid intake can help alleviate muscle cramps and maintain adequate hydration.
C. Incorrect. While calcium supplements may be prescribed in certain situations, they are not the first-line intervention for muscle cramps in chronic renal failure.
D. Incorrect. Educating the client about potassium-rich foods is important for managing potassium levels, but it is not the priority in this situation. Muscle cramps are more likely related to fluid and electrolyte imbalances rather than potassium intake.
Explanation
A. Incorrect. Peripheral edema and weight gain are more commonly associated with fluid retention in later stages of chronic renal failure when the kidneys are unable to effectively remove excess fluids from the body.
B. Incorrect. Frothy urine and increased urination may indicate proteinuria, a condition where excessive protein is excreted in the urine. While proteinuria can be a symptom of kidney dysfunction, it is not an early symptom.
C. Incorrect. Hypertension and headache can be associated with chronic renal failure, but they are not specific to early stages of kidney dysfunction.
D. Correct. Fatigue and decreased appetite are early clinical manifestations of kidney dysfunction in chronic renal failure. The kidneys play a vital role in filtering waste products and toxins from the blood, and when kidney function is compromised, it can lead to a buildup of waste products in the body, causing fatigue and decreased appetite.
Explanation
A. Incorrect. Excess production of calcium in the body is not a typical cause of bone pain in chronic renal failure.
B. Correct. Chronic renal failure can lead to impaired phosphorus excretion, resulting in elevated levels of phosphorus in the blood. High phosphorus levels can lead to bone demineralization, weakening the bones and causing bone pain.
C. Incorrect. While some medications used in the management of chronic renal failure may have side effects, frequent bone pain is not commonly associated with these medications.
D. Incorrect. Kidney dysfunction in chronic renal failure does not typically lead to low levels of calcium in the bones. Instead, it can lead to abnormalities in phosphorus levels, which affect bone health.
Explanation
A. Correct. Peripheral neuropathy, characterized by tingling sensations or "pins and needles" in the hands and feet, is a common neurological complication of chronic renal failure. Uremic toxins build up in the blood when the kidneys are unable to adequately filter waste products, leading to nerve damage and peripheral neuropathy.
B. Incorrect. Increased blood flow to the extremities is not typically associated with the "pins and needles" sensation described by the client.
C. Incorrect. Adequate nerve conduction related to calcium levels would not cause the "pins and needles" sensation; instead, disturbances in calcium levels can lead to other neurological symptoms.
D. Incorrect. Hypokalemia, or low potassium levels, can cause muscle weakness or cramps but is not typically associated with peripheral neuropathy.
Explanation
A. Incorrect. Hyperkalemia, or high potassium levels, can cause muscle weakness and potentially cardiac arrhythmias, but it is not typically associated with difficulty concentrating or irritability.
B. Incorrect. Hyponatremia, or low sodium levels, can cause neurological symptoms such as confusion and headache, but it is not typically associated with muscle cramps.
C. Incorrect. Hypocalcemia, or low calcium levels, can cause muscle cramps and neurological symptoms, but it is not specifically associated with difficulty concentrating and irritability.
D. Correct. Hyperphosphatemia, or high phosphorus levels, is common in chronic renal failure due to impaired kidney function. Elevated phosphorus levels can lead to the binding of calcium, resulting in decreased ionized calcium in the blood. This can cause neuromuscular irritability, difficulty concentrating, and muscle cramps.
Explanation
A. Incorrect. Proteinuria, or the presence of excessive protein in the urine, may be a symptom of kidney dysfunction, but it is not directly related to periorbital edema and swelling of the ankles and feet.
B. Incorrect. Hypokalemia, or low potassium levels, may cause muscle weakness and other symptoms but is not associated with the specific edema described.
C. Incorrect. Hypernatremia, or high sodium levels, may lead to symptoms such as thirst and confusion but does not typically cause peripheral edema.
D. Correct. Periorbital edema (swelling around the eyes) and edema in the ankles and feet are classic signs of fluid overload in chronic renal failure. The impaired kidney function in chronic renal failure leads to the retention of fluid and sodium in the body, resulting in edema.
Explanation
A. Incorrect. Increasing the intake of potassium-rich foods may not be appropriate, especially if the client's potassium levels are already elevated due to chronic renal failure. High potassium levels can lead to muscle cramps.
B. Incorrect. While regular weight-bearing exercises are beneficial for overall health, they may not specifically address or alleviate muscle cramps in chronic renal failure.
C. Correct. Engaging in stretching exercises before bedtime can help reduce the frequency of muscle cramps in clients with chronic renal failure. Stretching can help relax and lengthen muscles, reducing the risk of cramping.
D. Incorrect. Taking over-the-counter calcium supplements without proper evaluation of calcium levels can be dangerous and may contribute to other imbalances in chronic renal failure.
Explanation
A. Incorrect. Severe anemia in chronic renal failure is characterized by low hemoglobin levels, not elevated levels.
B. Incorrect. Chronic renal failure can lead to decreased red blood cell production, resulting in a reduced red blood cell count.
C. Correct. Chronic renal failure often leads to decreased production of erythropoietin, a hormone that stimulates red blood cell production. This deficiency results in low hematocrit levels and severe anemia.
D. Incorrect. Chronic renal failure is not typically associated with elevated platelet counts; in fact, it can lead to platelet dysfunction and an increased risk of bleeding.
QUESTIONS
Explanation
A. Correct. The GFR test measures how well the kidneys are filtering waste and fluids from the blood. It is an essential indicator of kidney function and is commonly used to diagnose and stage chronic renal failure.
B. Incorrect. The volume of urine produced in 24 hours is measured through a different test called the 24-hour urine collection, not the GFR test.
C. Incorrect. While the GFR test is used to assess kidney function, it is not specific to diagnosing particular kidney diseases like glomerulonephritis.
D. Incorrect. The GFR test does not specifically assess the excretion of potassium and sodium in the urine; instead, it focuses on overall kidney function and filtration rate.
Explanation
A. Incorrect. A GFR value of 50 mL/min/1.73m² indicates some level of kidney dysfunction, not normal kidney function.
B. Incorrect. A GFR value of 50 mL/min/1.73m² indicates moderate kidney dysfunction, not mild impairment.
C. Correct. A GFR value of 50 mL/min/1.73m² is considered to represent moderate kidney dysfunction. This level of GFR indicates that the kidneys are not effectively filtering waste and fluids from the blood.
D. Incorrect. While a GFR value of 50 mL/min/1.73m² indicates kidney dysfunction, it does not represent severe kidney damage. Severe kidney dysfunction would have a much lower GFR value.
Explanation
A. Incorrect. Converting the creatinine level to micromoles per liter is not necessary for the GFR calculation.
B. Incorrect. While a 24-hour urine sample can be used to measure creatinine clearance, it is not required for the GFR calculation, which can be estimated using formulas.
C. Incorrect. Calculating the body surface area is not necessary for the GFR calculation.
D. Correct. The GFR can be estimated using formulas that include the serum creatinine level, such as the Modification of Diet in Renal Disease (MDRD. formula or the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.
Explanation
A. Incorrect. Fasting is not required for a GFR test.
B. Incorrect. While staying hydrated is essential for overall health, there are no specific hydration requirements before a GFR test.
C. Incorrect. While dietary changes may be necessary for other tests, such as creatinine clearance, there are no specific dietary restrictions for the GFR test.
D. Correct. There are no special preparations needed for a GFR test. The test can be done at any time, regardless of food intake or hydration status.
Explanation
A. Incorrect. A GFR value of 10 mL/min/1.73m² indicates severe kidney dysfunction, not mild impairment.
B. Correct. A GFR value of 10 mL/min/1.73m² is considered very low and indicates severe kidney dysfunction. At this level, the kidneys are severely damaged and unable to effectively filter waste and fluids from the blood.
C. Incorrect. A GFR value of 10 mL/min/1.73m² is much lower than the threshold for moderate kidney dysfunction.
D. Incorrect. A GFR value of 10 mL/min/1.73m² is far below the normal range and indicates significant kidney dysfunction, not normal kidney function.
Explanation
A. Incorrect. While a GFR value of 60 mL/min/1.73m² is within the normal range for some populations, it is considered below the normal range for adults and indicates some level of kidney dysfunction.
B. Correct. A GFR value of 60 mL/min/1.73m² indicates mild kidney impairment. While it may not be severely compromised, it still represents some level of kidney dysfunction.
C. Incorrect. A GFR value of 60 mL/min/1.73m² is not considered moderate kidney dysfunction. It is within the mild impairment range.
D. Incorrect. A GFR value of 60 mL/min/1.73m² is not indicative of severely damaged kidneys. Severe kidney dysfunction would have a much lower GFR value.
Explanation
A. Incorrect. Pain medication is not typically administered for a GFR test as the test itself is not painful.
B. Correct. The GFR test is painless and non-invasive. It involves a blood test to measure creatinine levels and does not cause discomfort.
C. Incorrect. While relaxation techniques can be helpful for other procedures, they are not necessary for the GFR test as it does not cause discomfort.
D. Incorrect. Reassuring the client about the brief and tolerable nature of discomfort would be misleading, as the GFR test does not cause discomfort.
QUESTIONS
Explanation
A. Incorrect. In chronic renal failure, the kidneys may have difficulty processing excess protein, so protein intake should be limited to reduce the workload on the kidneys.
B. Correct. Limiting fluid intake is crucial in managing chronic renal failure. The kidneys' reduced ability to filter waste products can lead to fluid retention and electrolyte imbalances, so restricting fluid intake helps prevent overload and complications.
C. Incorrect. In chronic renal failure, high-potassium foods should be limited to prevent hyperkalemia, a condition in which potassium levels in the blood become too high.
D. Incorrect. Foods high in phosphorus should be restricted in chronic renal failure because the kidneys may have difficulty excreting excess phosphorus, leading to hyperphosphatemia, which can contribute to bone and mineral disorders.
Explanation
A. Incorrect. Phosphate binders are not used to reduce calcium absorption. They are specifically prescribed to control phosphate levels in the blood.
B. Correct. Phosphate binders are medications that bind to dietary phosphorus in the digestive tract, preventing its absorption and reducing phosphate levels in the blood. This helps manage hyperphosphatemia, a common complication in chronic renal failure.
C. Incorrect. Phosphate binders do not improve iron absorption or manage anemia. They are not related to iron metabolism.
D. Incorrect. Phosphate binders do not affect potassium excretion. They are specific to phosphate control in the body and do not impact potassium levels.
Explanation
A. Incorrect. While proper medication adherence can help prevent drug interactions, it is not the primary reason for advising clients to take medications as prescribed in chronic renal failure.
B. Incorrect. Medication adherence may or may not directly impact the cost of treatment, but the main reason for consistent use is to manage the condition effectively.
C. Correct. Adhering to medication regimens in chronic renal failure is crucial for slowing the progression of kidney damage. Medications are prescribed to control blood pressure, manage complications, and reduce the strain on the kidneys.
D. Incorrect. Medication adherence is essential, but it does not eliminate the need for dietary restrictions in chronic renal failure. Dietary modifications are also a vital part of managing the condition effectively.
Explanation
A. Incorrect. ESA therapy is not directly related to dehydration or thirst. It is used to manage anemia by stimulating red blood cell production.
B. Correct. ESA therapy can increase red blood cell production, which may elevate blood pressure. Regular blood pressure monitoring is essential to ensure it remains within a safe range.
C. Incorrect. Increased appetite and weight gain are not typical side effects of ESA therapy.
D. Incorrect. ESA therapy is not associated with an increased risk of bleeding or restrictions on engaging in strenuous activities. It is used to manage anemia and improve overall blood cell counts.
Explanation
A. Incorrect. Encouraging the client to drink 3 liters of fluid daily may be excessive and can contribute to fluid overload in individuals on hemodialysis. Fluid intake needs to be limited and closely monitored.
B. Correct. Monitoring the vascular access site is crucial to detect early signs of infection or clotting, which can lead to serious complications such as sepsis or thrombosis.
C. Incorrect. Phosphate binders are used to control phosphate levels in the blood and are generally taken with meals, not specifically before hemodialysis sessions.
D. Incorrect. Promoting a high-potassium diet is not appropriate for individuals on hemodialysis, as it can lead to hyperkalemia. Clients on hemodialysis typically need to restrict potassium intake.
Explanation
A. Incorrect. Encouraging the client to drink more fluids may not immediately resolve the cloudy dialysate drainage. The nurse needs to assess the client's dialysis technique and the potential cause of the cloudiness.
B. Incorrect. Administering intravenous antibiotics is not the initial intervention for cloudy dialysate drainage. First, the nurse should assess the client's technique and position during dialysis.
C. Correct. Cloudy dialysate drainage may indicate improper dialysate exchange, infection, or other complications. The
nurse should first assess the client's dialysis technique and ensure proper positioning to identify the cause.
D. Incorrect. Discontinuing peritoneal dialysis should be considered if there is clear evidence of infection or other serious complications, but it is not the initial intervention for cloudy drainage without further assessment.
Explanation
A. Incorrect. Calcitriol is not given to enhance appetite or improve nutrition. Its primary role is in regulating calcium and phosphate levels.
B. Incorrect. Calcitriol does not directly impact urine output or prevent kidney stones.
C. Incorrect. While some medications may be prescribed to manage blood pressure in chronic renal failure, calcitriol is not one of them.
D. Correct. Calcitriol is the active form of vitamin D and plays a crucial role in regulating calcium and phosphate levels in the body. It helps maintain bone health by promoting the absorption of calcium from the digestive tract and preventing bone demineralization.
Explanation
A. Correct. ACE inhibitors are commonly prescribed to manage hypertension and fluid overload in clients with chronic renal failure. These medications help relax blood vessels, reduce fluid retention, and lower blood pressure.
B. Incorrect. Phosphate binders are prescribed to control phosphate levels, but they do not directly address fluid overload and hypertension.
C. Incorrect. Erythropoietin-stimulating agents (ESA. are used to manage anemia in chronic renal failure and do not specifically address hypertension or fluid overload.
D. Incorrect. Potassium-sparing diuretics may not be the first for managing fluid overload and hypertension in chronic renal failure, especially if the client has elevated potassium levels. ACE inhibitors are a more suitable option in this scenario.
QUESTIONS
Explanation
A. Correct. Touching the dialysis catheter site increases the risk of infection, and clients receiving peritoneal dialysis must practice meticulous catheter care to minimize this risk.
B. Incorrect. While daily weight monitoring is essential for clients on peritoneal dialysis, it is not specifically related to peritoneal dialysis care.
C. Incorrect. Peritoneal dialysis is a home-based treatment, and the client performs the dialysis exchanges themselves. There is no need for frequent visits to the dialysis center.
D. Incorrect. Pain medication is not typically needed before starting a peritoneal dialysis exchange, as the procedure itself is not painful. Proper technique and sterile care are the main focus of peritoneal dialysis education.
Explanation
A. Correct. In chronic renal failure, limiting protein intake is essential to reduce the workload on the kidneys and slow the progression of kidney damage.
B. Incorrect. Increasing sodium intake is not recommended in chronic renal failure, as it can lead to fluid retention and hypertension.
C. Incorrect. While potassium intake may need to be adjusted based on blood levels, there is no indication to consume potassium-rich foods to prevent deficiency.
D. Incorrect. Fluid restrictions are typically necessary in chronic renal failure to prevent fluid overload and related complications.
Explanation
A. Incorrect. While physical activity is essential for overall health, the client's fatigue may be related to anemia, not lack of physical activity.
B. Correct. Fatigue and lethargy are common symptoms of anemia, which is a common complication of chronic renal failure. Iron supplements can help address anemia-related fatigue.
C. Incorrect. Increasing protein intake may not directly address the underlying cause of the client's fatigue, which is likely anemia.
D. Incorrect. Caffeine-containing beverages can contribute to fluid overload and hypertension in chronic renal failure and are not a suitable intervention for addressing fatigue.
Explanation
A. Correct. Phosphate binders are most effective when taken with meals because they bind to dietary phosphorus, preventing its absorption in the digestive tract.
B. Incorrect. While constipation can be a side effect of some phosphate binders, drinking plenty of fluids is not directly related to this issue.
C. Incorrect. Phosphate binders should be taken with meals, and calcium supplements should be taken separately to prevent interactions between the two medications.
D. Incorrect. Phosphate binders do not typically lower potassium levels, and monitoring potassium intake is not specifically related to their use.
Explanation
A. Incorrect. Dairy products are high in potassium and should be limited in clients at risk for hyperkalemia.
B. Incorrect. Fruits and vegetables are also high in potassium and should be limited in clients with chronic renal failure and hyperkalemia risk.
C. Correct. Nuts and seeds are rich sources of potassium and should be restricted in the diet of clients at risk for hyperkalemia.
D. Incorrect. Poultry is a good protein source, but the type of protein is not the main concern for clients at risk for hyperkalemia; it is the overall potassium content of the diet that needs to be reduced.
Explanation
A. Incorrect. While dietary modifications are often necessary in chronic renal failure, this response does not address the client's concerns about lifestyle impact.
B. Correct. Hemodialysis requires a significant time commitment, and clients must plan their activities around the dialysis schedule. It is important for the client to understand the need for regular dialysis sessions to manage their condition effectively.
C. Incorrect. While hemodialysis does require regular sessions, it should not necessarily limit a client's ability to travel or participate in social events. Many individuals on hemodialysis can adjust their activities and still engage in meaningful experiences.
D. Incorrect.
Physical activity is generally encouraged in clients with chronic renal failure, as it contributes to overall well-being. Hemodialysis may increase energy levels and improve the client's ability to engage in physical activity.
Explanation
A. Incorrect. Calcium-based phosphate binders should not be taken with milk or calcium-rich foods, as this can lead to an excessive calcium load and increase the risk of hypercalcemia.
B. Incorrect. Calcium-based phosphate binders are most effective when taken with meals to bind to dietary phosphorus.
C. Incorrect. While vitamin D plays a role in calcium metabolism, its supplementation is not directly related to the use of calcium-based phosphate binders.
D. Correct. Constipation is a common side effect of calcium-based phosphate binders. Increasing fluid intake can help alleviate constipation and promote bowel regularity.
Questions
End-stage renal disease
Explanation
A. This is incorrect because ESRD is not a reversible condition. Once the kidneys have reached this stage, their ability to function is permanently lost, and treatment focuses on managing the condition and replacing kidney function through dialysis or transplantation.
B. This is correct. ESRD is the final stage of chronic kidney disease, where the kidneys have lost their ability to function adequately to sustain life. At this stage, the client requires renal replacement therapy such as dialysis or kidney transplantation to survive.
C. This is incorrect because ESRD is not a temporary condition caused by an infection; it is a chronic and irreversible condition.
D. This is incorrect because ESRD is not a condition where the kidneys can recover with proper management. Once the kidneys have reached end-stage, their ability to function is permanently compromised.
Explanation
A. This is incorrect because while kidney transplantation is an essential treatment option for ESRD, it is not the only option. Dialysis (hemodialysis or peritoneal dialysis) is also a viable treatment to replace kidney function for clients who are not transplant candidates or awaiting transplantation.
B. This is correct. Dialysis is the primary treatment for ESRD, providing renal replacement therapy by removing waste products and excess fluid from the blood. Kidney transplantation is another treatment option for eligible candidates who may benefit from a functioning kidney.
C. This is incorrect because effective treatment options, such as dialysis and kidney transplantation, are available for ESRD. There is ongoing research and development in nephrology, but new therapies have not replaced the standard treatments.
D. This is incorrect because ESRD is a severe condition where the kidneys have permanently lost their ability to function, and treatment options such as dialysis or transplantation are necessary to sustain life.
Explanation
A. This is correct. Family history of diabetes is a significant risk factor for the development of ESRD. Diabetes is one of the leading causes of ESRD, and individuals with a family history of diabetes are at increased risk of kidney complications.
B. This is incorrect because being physically active and maintaining a healthy lifestyle do not increase the risk of ESRD. In fact, a healthy lifestyle can help reduce the risk of developing kidney disease.
C. This is incorrect because having a history of frequent kidney stones is not associated with a decreased risk of ESRD. In some cases, recurrent kidney stones may lead to chronic kidney disease, which can progress to ESRD.
D. This is incorrect because high blood pressure (hypertension) is a significant risk factor for the development and progression of ESRD. Uncontrolled hypertension can lead to damage to the blood vessels in the kidneys, contributing to kidney disease.
Explanation
A. This is correct. Clients with ESRD need to limit their fluid intake to prevent fluid overload, which can lead to swelling, shortness of breath, and heart-related issues.
B. This is incorrect. Protein intake needs to be monitored and adjusted, but it is not restricted entirely. Protein is essential for the body, and malnutrition should be avoided in clients with ESRD. However, high protein intake can put additional strain on the kidneys, so moderation is key.
C. This is correct. Clients with ESRD should avoid foods high in potassium, as elevated potassium levels can lead to life-threatening cardiac arrhythmias. Limiting potassium intake helps maintain potassium levels within a safe range.
D. This is correct. Consuming foods low in phosphorus is crucial for clients with ESRD. High phosphorus levels can lead to complications such as bone disease, so managing phosphorus intake is essential.
Explanation
A. This is correct. Hemodialysis is a renal replacement therapy that uses a dialysis machine to remove waste products, toxins, and excess fluid from the bloodstream when the kidneys are no longer able to do so effectively.
B. This is incorrect. While hemodialysis may have some effect on blood pressure, its primary purpose is to replace kidney function in filtering waste products
and maintaining fluid balance.
C. This is incorrect. Hemodialysis does not stimulate the kidneys to produce more urine. It directly filters the blood to remove toxins and fluid.
D. This is incorrect. Hemodialysis does not involve surgical replacement of damaged kidneys. It is a non-surgical procedure performed in a dialysis center using a dialysis machine.
Explanation
A. This is incorrect. Peritoneal dialysis is typically performed at home, providing more flexibility and convenience for clients compared to hemodialysis, which requires regular visits to a dialysis center.
B. This is correct. Peritoneal dialysis is performed at home, which allows clients to have more control over their treatment schedule. It can be done during the day or overnight, providing greater flexibility for clients to continue with their daily activities.
C. This is incorrect. Peritoneal dialysis involves the insertion of a catheter into the peritoneal cavity, not the bladder. The catheter allows the dialysis solution to be infused and drained from the peritoneal cavity.
D. This is incorrect. While peritoneal dialysis does carry some risk of infection, it is generally considered to have a lower risk of infection compared to hemodialysis, where blood is exposed to an external machine.
Explanation
A. This is incorrect. While kidney transplantation does require the use of immunosuppressant medications to prevent organ rejection, it eliminates the need for dialysis and provides a better chance of long-term survival compared to dialysis alone.
B. This is incorrect. While there is a risk of infection after kidney transplantation, the overall risk of infection is generally higher in clients on long-term dialysis.
C. This is incorrect. Kidney transplantation is associated with improved quality of life compared to dialysis. Transplant recipients often experience increased energy, better dietary freedom, and a decreased reliance on medical appointments compared to dialysis patients.
D. This is correct. Kidney transplantation offers the best chance for long-term survival and eliminates the need for ongoing dialysis. It provides improved quality of life and potential freedom from dietary restrictions, fluid restrictions, and the time-consuming dialysis procedure.
Questions
Explanation
A. This is incorrect. While acute kidney injury (AKI) can contribute to the development of ESRD, it is not the primary cause. ESRD typically results from chronic kidney diseases that progress over time, such as diabetes and hypertension.
B. This is correct. The most common causes of ESRD are diabetes mellitus and uncontrolled hypertension. These conditions can lead to chronic kidney disease and eventual kidney failure if not well managed.
C. This is incorrect. While kidney stones can cause kidney damage and contribute to kidney disease, they are not a common cause of ESRD.
D. This is incorrect. While genetic factors and family history may play a role in some cases of kidney disease, they are not the primary causes of ESRD. ESRD is most commonly associated with chronic conditions like diabetes and hypertension.
Explanation
A. This is incorrect. While adequate fluid intake is essential for kidney health, increasing fluid intake is not a solution for worsening kidney function. The client should follow the healthcare provider's recommendations for fluid intake based on their kidney function and medical history.
B. This is correct. NSAIDs, such as ibuprofen and naproxen, can be harmful to the kidneys, especially when used for extended periods or in high doses. Avoiding these medications can help protect the kidneys and prevent further damage, especially in individuals with chronic kidney disease.
C. This is incorrect. Regularly consuming foods high in potassium can be detrimental to individuals with compromised kidney function. High potassium levels can be harmful to the kidneys, and clients with kidney disease may need to restrict their potassium intake to protect their kidneys.
D. This is incorrect. High-intensity exercise may not be suitable for all individuals with kidney disease, and the client should consult their healthcare provider before engaging in any exercise program. While regular physical activity can be beneficial for overall health, the type and intensity of exercise should be individualized based on the client's medical condition and fitness level.
Explanation
A. This is correct. Polycystic kidney disease (PKD. is a genetic disorder, and individuals with a family history of PKD have a higher risk of developing the condition. It can be inherited from one or both parents, and the mutated gene responsible for PKD affects the development of fluid-filled cysts in the kidneys.
B. This is incorrect. While exposure to certain environmental toxins can contribute to kidney damage, it is not the cause of PKD.
C. This is incorrect. PKD is not an autoimmune disorder; it is a genetic disorder characterized by the growth of cysts in the kidneys.
D. This is incorrect. PKD is not caused by chronic kidney infections; it is a genetic condition that results in the formation of cysts within the kidney tissue.
Explanation
A. This statement is reassuring. The client's history of kidney stones in the past does not directly contribute to their current diagnosis of ESRD if the stones were successfully treated. However, it may still be relevant to their overall kidney health and risk factors.
B. This statement is concerning. Family history of kidney stones and a sister with ESRD may indicate a genetic predisposition to kidney disease and warrants further evaluation.
C. This statement is positive. Changing the diet to avoid kidney stones is a proactive step to protect kidney health and reduce the risk of kidney damage.
D. This statement requires further evaluation by the nurse. While hypertension and diabetes are well-known risk factors for ESRD, the absence of kidney stones does not rule out other potential causes or risk factors for the client's current diagnosis.
Explanation
A. This is correct. High blood pressure is a significant risk factor for the progression of chronic kidney disease. Regularly monitoring blood pressure and maintaining it within the recommended target range can help slow the decline in kidney function and reduce the risk of complications associated with kidney disease.
B. This is incorrect. Regular exercise and maintaining a healthy weight are generally beneficial for overall health, including cardiovascular health. However, they do not increase the risk of CKD progression. In fact, they may help improve blood pressure control and reduce the risk of kidney disease progression.
C. This is incorrect. Increasing dietary intake of sodium and protein can be harmful to individuals with kidney disease. High sodium intake can contribute to fluid retention and increased blood pressure, while excessive protein intake can place additional stress on the kidneys. Clients with CKD are often advised to follow a low-sodium and moderate-protein diet to protect kidney function.
D. This is incorrect. Smoking and regular alcohol consumption can have harmful effects on the kidneys and overall health. Smoking is a risk factor for kidney disease progression, and excessive alcohol consumption can contribute to high blood pressure and other health issues that may worsen kidney function.
Explanation
A. This is incorrect. A history of cardiovascular disease can increase the risk of developing ESRD. Cardiovascular disease and kidney disease often share common risk factors, such as hypertension and diabetes, which can contribute to the progression of both conditions.
B. This is incorrect. While the chronic use of certain medications can potentially harm the kidneys, it is not a common risk factor for the development of ESRD. Medications like NSAIDs are more directly associated with kidney injury and acute kidney damage rather than the development of ESRD.
C. This is correct. Cardiovascular disease is a significant risk factor for the development of ESRD. Chronic kidney disease and cardiovascular disease often coexist and share common risk factors. Cardiovascular disease can lead to impaired blood flow to the kidneys, contributing to kidney damage and dysfunction.
D. This is incorrect. While having a family history of gout can be associated with an increased risk of kidney stones and kidney damage, it is not a common risk factor for the development of ESRD.
Explanation
A. This is incorrect. Herbal supplements are not always safe, and some can have adverse effects on kidney function, especially if used in excessive amounts or in combination with certain medications.
B. This is correct. Regular use of herbal supplements can potentially interact with medications, including those prescribed for kidney disease, and worsen kidney function. Some herbal supplements may have diuretic properties or may be metabolized by the kidneys, leading to potential complications for individuals with ESRD.
C. This is incorrect. Herbal supplements are not regulated by the U.S. Food and Drug Administration (FDA. , and their safety and efficacy may vary. Some herbal supplements have been associated with adverse effects on kidney health and may not be as benign as the client assumes.
D. This is incorrect. Herbal supplements should not be considered as replacements for prescribed medications in managing ESRD. The client should always consult with their healthcare provider before starting or continuing the use of herbal supplements to ensure they are safe and appropriate for their medical condition.
Questions
Explanation
A. This is incorrect. ESRD leads to decreased urine output and excessive thirst due to impaired kidney function, not increased urine output.
B. This is correct. Swelling of the legs and ankles, also known as edema, is a common symptom of ESRD. Kidney failure causes fluid retention and electrolyte imbalances, leading to edema in the lower extremities and other body parts.
C. This is incorrect. Clients with ESRD often experience poor appetite and unintended weight loss due to the accumulation of waste products in the body.
D. This is incorrect. ESRD is often associated with hypertension and other cardiovascular complications. Clients with ESRD may experience symptoms such as high blood pressure, shortness of breath, and chest pain.
Explanation
A. This is not the priority assessment for this client. Skin rash and itching are common in ESRD due to the accumulation of waste products in the bloodstream, but it is not the most critical finding among the options given.
B. This is not the priority assessment for this client. Numbness and tingling in extremities can be related to neuropathy, which can occur in ESRD, but it is not the most critical finding among the options given.
C. This is the priority assessment for the client with ESRD. Decreased urine output is a significant symptom of kidney failure and requires immediate attention. It may indicate worsening kidney function or complications that need to be addressed promptly.
D. This is not the priority assessment for this client. While increased blood pressure can be a complication of ESRD, decreased urine output takes precedence in this situation.
Explanation
A. This is correct. ESRD often leads to hypertension and increased cardiovascular risk due to fluid retention, electrolyte imbalances, and activation of the renin-angiotensin-aldosterone system.
B. This is incorrect. Clients with ESRD are at increased risk for bone fractures and calcium imbalances due to impaired calcium and phosphorus metabolism, leading to bone demineralization and increased fracture risk.
C. This is incorrect. ESRD is not associated with improved vision or eye health; in fact, clients with ESRD may experience eye complications, such as retinopathy, due to the effects of diabetes and hypertension on the retina.
D. This is incorrect. ESRD can affect the gastrointestinal system, leading to complications such as nausea, vomiting, and gastrointestinal bleeding due to the accumulation of waste products and electrolyte imbalances.
Explanation
A. This is incorrect. Administering a bolus of IV fluid may worsen fluid overload and electrolyte imbalances in the client with ESRD. It is not an appropriate intervention for muscle cramps and twitching.
B. This is incorrect. Vigorous physical exercise may exacerbate muscle cramps and twitching in clients with ESRD. Encouraging moderate physical activity is more appropriate.
C. This is correct. Muscle cramps and twitching in clients with ESRD are often associated with elevated phosphate levels in the blood. Phosphate-binding medications can help reduce phosphate levels and alleviate these symptoms.
D. This is incorrect. While dietary protein intake may need to be adjusted for clients with ESRD, restricting protein intake to minimal levels can lead to malnutrition and other complications. It is not an appropriate intervention for muscle cramps and twitching.
Explanation
A. This is correct. Hemodialysis is performed to remove waste products and excess fluids from the body, but there is a risk of fluid overload during the procedure. It is essential for the client to be monitored for signs of fluid retention, such as swelling and shortness of breath.
B. This is incorrect. Hemodialysis typically reduces fluid overload and may lead to decreased appetite and weight loss, not weight gain.
C. This is incorrect. Hemodialysis is used to manage fluid and electrolyte imbalances, including blood pressure regulation. While blood pressure may fluctuate during the dialysis procedure, it is not a common complication to increase blood pressure.
D. This is incorrect. Hemodialysis is used to regulate potassium levels in clients with ESRD, as high potassium levels can be dangerous. It is more common for potassium levels to be reduced during hemodialysis, not increased.
Explanation
A. This statement is accurate. ESA therapy can sometimes cause an increase in blood pressure, and the client should monitor their blood pressure regularly to ensure it is well-controlled.
B. This statement is accurate. ESA therapy can increase the risk of blood clots, and clients should be vigilant for signs of blood clots or shortness of breath, as it may indicate a potential complication.
C. This statement is accurate. Iron supplements are often prescribed along with ESA to enhance their effectiveness in treating anemia. Iron helps in the production of red blood cells.
D. This statement is incorrect. There is no evidence to suggest that clients on ESA therapy should avoid vaccinations. In fact, vaccination is important for clients with ESRD to protect against infections, which can be particularly dangerous for individuals with compromised kidney function.
Explanation
A. This is correct. Peritoneal dialysis involves the insertion of a catheter into the peritoneal cavity, and there is a risk of bleeding at the insertion site. The nurse should closely monitor for any signs of hemorrhage or infection at the catheter site.
B. This is incorrect. Hypoglycemia and blood glucose fluctuations are not common complications of peritoneal dialysis. However, clients with diabetes may need adjustments in their diabetes management during peritoneal dialysis.
C. This is incorrect. Electrolyte imbalances and fluid overload are potential complications of both hemodialysis and peritoneal dialysis. While electrolyte imbalances can occur with peritoneal dialysis, hemorrhage at the catheter insertion site is a more specific concern for this type of dialysis.
D. This is incorrect. Impaired respiratory function and lung collapse are not typical complications of peritoneal dialysis. These are more commonly associated with other respiratory conditions and not directly related to peritoneal dialysis.
Questions
Explanation
A. This statement is incorrect. Dialysis does not regenerate damaged kidney tissues; it only serves to replace some kidney functions that are lost in ESRD.
B. This statement is correct. Dialysis is a treatment that helps to remove waste products and excess fluids from the body when the kidneys are unable to perform these functions adequately due to ESRD.
C. This statement is incorrect. Dialysis is not a kidney transplant procedure; it is a method of artificially filtering the blood to perform some functions of the kidneys.
D. This statement is incorrect. Dialysis is not a medication-based treatment; it is a mechanical process to cleanse the blood outside the body.
Explanation
A. This statement is correct. The two main types of dialysis are peritoneal dialysis and intermittent hemodialysis. Peritoneal dialysis uses the peritoneal cavity as a natural filter, and intermittent hemodialysis is performed using a machine to filter the blood.
B. This statement is incorrect. Dialysis can be performed both in a hospital setting and at home, depending on the type of dialysis chosen by the client and their healthcare provider.
C. This statement is incorrect. There are two main types of dialysis, as mentioned in option A, not just one.
D. This statement is incorrect. Dialysis is a common and effective treatment option for ESRD when kidney function has significantly declined. It can improve the quality of life and extend survival for many clients with ESRD.
Explanation
A. This is incorrect. Peritoneal dialysis typically helps manage fluid and blood pressure imbalances in clients with ESRD.
B. This is incorrect. While blood clots and clotting disorders can be potential complications of ESRD, they are not specifically associated with peritoneal dialysis.
C. This is correct. Peritonitis is a severe and potentially life-threatening complication of peritoneal dialysis. It occurs when the peritoneal cavity, used for dialysis, becomes infected, leading to inflammation and infection at the catheter insertion site.
D. This is incorrect. Electrolyte imbalances and fluid overload can occur with both peritoneal dialysis and hemodialysis. However, peritonitis is a specific complication unique to peritoneal dialysis.
Explanation
A. This is incorrect. Abdominal pain and discomfort are not typical complications of hemodialysis.
B. This is incorrect. Muscle cramps and twitching are more commonly associated with ESRD itself or other types of dialysis, such as peritoneal dialysis.
C. This is incorrect. Hemodialysis is intended to remove excess fluids and waste products from the body, leading to decreased urine output, not increased urine output and excessive thirst.
D. This is correct. Hypotension and low blood pressure are common complications of hemodialysis. During the procedure, the rapid removal of fluids can cause a drop in blood pressure, leading to symptoms such as dizziness and lightheadedness.
Explanation
A. This is incorrect. Increasing the dialysis flow rate can exacerbate the client's symptoms and lead to further complications, such as hypotension and cramping.
B. This is not the most appropriate action to address the client's current symptoms of nausea and vomiting during the procedure. Assessing weight gain between dialysis sessions is essential for overall fluid management but may not directly address the acute symptoms.
C. This is correct. Administering an antiemetic medication can help alleviate nausea and vomiting during the dialysis procedure. Antiemetics can prevent or reduce these symptoms, making the dialysis session more tolerable for the client.
D. This is incorrect. Increasing fluid intake during dialysis may not be appropriate, as the goal of hemodialysis is to remove excess fluids from the body. Encouraging increased fluid intake could lead to fluid overload and worsen the client's symptoms.
Explanation
A. This is correct. In CAPD, the peritoneal cavity is used as a dialysate exchange site, and an indwelling catheter remains in place. Regularly inspecting the skin and exit site for signs of infection is essential to minimize the risk of peritonitis and other complications.
B. This is not the most appropriate aspect to focus on in CAPD. Daily fluid intake is not limited in CAPD; instead, the fluid exchange process occurs multiple times throughout the day to remove waste and excess fluids from the body.
C. This is incorrect. Subcutaneous heparin is not typically used in CAPD, as it is a form of anticoagulation therapy and not a standard component of peritoneal dialysis treatment.
D. This is incorrect. The catheter should remain connected to the drainage bag at all times, even during sleep. Disconnecting the catheter can disrupt the dialysate exchange process and increase the risk of infection and other complications.
Explanation
A. This is not directly related to the client's successful home-based peritoneal dialysis. While companionship is essential for many clients, it is not a critical factor for dialysis treatment.
B. This is not the most appropriate factor to assess for home-based peritoneal dialysis. Availability of transportation is crucial for clients who may need to travel for hemodialysis sessions, not for clients undergoing peritoneal dialysis at home.
C. This is correct. Access to a reliable electricity source is crucial for home-based peritoneal dialysis since the peritoneal dialysis machine requires electricity to function properly. The machine helps with the exchange of dialysate, which is necessary for effective treatment.
D. This is not directly related to home-based peritoneal dialysis. While proximity to a local hospital or medical facility is always important for any client, it is not a primary factor for choosing home-based peritoneal dialysis as a treatment option.
Questions
A client with end-stage renal disease (ESRD. is considering renal transplantation as a treatment option. The client asks the nurse about the advantages of this procedure. Which response by the nurse is accurate?
Explanation
A. This statement is incorrect. Renal transplantation is not always temporary; it can provide long-term relief and improve the client's quality of life.
B. This statement is incorrect. While renal transplantation is beneficial, recipients will need to take lifelong immunosuppressive medications to prevent organ rejection.
C. This statement is correct. Renal transplantation is a treatment that can provide immediate relief from the symptoms of ESRD and restore normal kidney function, allowing the client to lead a more normal life.
D. This statement is incorrect. Renal transplantation is not limited to clients with a specific genetic predisposition; it is a treatment option considered for any eligible client with ESRD.
A nurse is providing preoperative education to a client who is scheduled for a renal transplant. The client asks about the source of the donated kidney. Which response by the nurse is accurate?
Explanation
A. This statement is correct. Renal transplantation can involve kidneys from deceased donors who have chosen to donate their organs after their passing.
B. This statement is incorrect. While living donors can donate kidneys, in this scenario, the kidney is from a deceased donor.
C. This statement is incorrect. The donor could be deceased or living, but the kidney in this scenario is from a deceased donor.
D. This statement is incorrect. While genetic matching can be considered in living donor scenarios, it does not apply to deceased donor situations.
A nurse is discussing living donor kidney transplantation with a client who has a family member willing to donate a kidney. The client expresses concerns about the potential risks to the living donor. What should the nurse explain to the client about the evaluation process for living donors?
Explanation
A. This statement is correct. Living donors undergo a comprehensive physical and psychological evaluation to ensure they are in good health and at minimal risk for complications after the surgery.
B. This statement is incorrect. While genetic matching can be considered in some cases, it is not the primary factor in the evaluation process for living donors.
C. This statement is incorrect. Living donors can be unrelated individuals, such as friends or even altruistic donors, as long as they meet the necessary health criteria.
D. This statement is incorrect. Blood type compatibility is essential for a successful transplant, but it is not the only consideration in the evaluation process for living donors.
A client with ESRD has found a suitable living kidney donor. The client asks the nurse about the surgical procedure for the kidney transplant. Which response by the nurse is accurate?
Explanation
A. This statement is incorrect. In living donor kidney transplantation, the donor's kidney is surgically removed and transplanted directly into the recipient's body during the same surgical procedure.
B. This statement is incorrect. While both the donor and recipient will undergo surgeries simultaneously, they will be in separate operating rooms.
C. This statement is correct. During the kidney transplant, the donor's kidney is placed in the recipient's lower abdomen, and the recipient's native kidneys, if present and non-functional, may be removed or left in place, depending on the circumstances.
D. This statement is incorrect. The donor's kidney is typically transplanted into the lower abdomen on the opposite side from the recipient's native failed kidney to ensure proper blood supply and surgical access.
Explanation
A. This statement is correct. Immunosuppressive medications are crucial after a renal transplant to prevent the body's immune system from attacking and rejecting the transplanted kidney.
B. This statement is not directly related to the need for immunosuppressive medications. While infection prevention is essential, immunosuppressive medications serve a different purpose.
C. This statement is incorrect. Immunosuppressive medications are not directly related to complications during surgery or wound healing.
D. This statement is incorrect. Immunosuppressive medications are not intended to improve the function of native kidneys. Their primary purpose is to prevent rejection of the transplanted kidney.
Explanation
A. This statement is incorrect. While all surgeries carry some risk, a preemptive transplant is not associated with increased risks of surgical complications and infection compared to a transplant after dialysis initiation.
B. This statement is incorrect. Regardless of the timing of the transplant, recipients will need to take immunosuppressive medications to prevent rejection.
C. This statement is correct. Preemptive transplantation can offer better long-term outcomes, including improved survival rates and a higher likelihood of success compared to a transplant performed after dialysis initiation.
D. This statement is incorrect. Preemptive transplantation is considered as an option for eligible candidates who have ESRD but have not yet started dialysis.
Explanation
A. This statement is correct. Graft rejection is a significant concern after renal transplantation. If the transplanted kidney is rejected by the recipient's immune system, it can lead to organ failure and the need for additional treatment options.
B. This statement is not the most critical complication to prioritize in the client's education. While incisional pain and discomfort are common after surgery, they are typically managed effectively with pain medications and wound care.
C. This statement is important to discuss, but it is not the most critical complication. Clients will be educated on infection prevention strategies and will undergo regular monitoring for infections.
D. This statement is important to address, but it is not the highest priority. Short-term complications related to immunosuppressive medications can be managed, and the benefits of preventing graft rejection outweigh the risks associated with these medications.
Questions
Explanation
A. This response is not appropriate. Telling the client to ignore their feelings can invalidate their emotions and may lead to further distress.
B. This response is the correct approach. Acknowledging the client's emotions as normal and suggesting joining a support group allows the client to connect with others who can empathize with their experiences and provide emotional support.
C. This response is not helpful. Encouraging the client to be more positive dismisses their genuine feelings and does not address their emotional needs.
D. This response is not supportive. Encouraging the client to talk less to their family about their feelings can lead to feelings of isolation and may hinder the client from seeking the support they need.
Explanation
A. This intervention is not appropriate. Discouraging the client from expressing negative emotions can invalidate their feelings and may lead to a lack of emotional support.
B. This intervention is the correct approach. Validating the client's feelings and providing a nonjudgmental environment can help the client feel heard and understood, fostering a therapeutic relationship.
C. This intervention is not helpful. Avoiding the client's feelings does not address their emotional needs and may make the client feel isolated.
D. This intervention is not appropriate. Encouraging the client to focus solely on the physical benefits of dialysis ignores the emotional impact of the treatment and does not address the client's feelings of anger and frustration.
Explanation
A. This option is not appropriate. Encouraging the client to avoid researching their condition and treatments may lead to increased anxiety due to lack of knowledge and understanding.
B. This option is correct. Deep breathing exercises and mindfulness techniques are evidence-based strategies to manage anxiety and stress during medical appointments. These techniques can help the client stay calm and focused during discussions with healthcare providers.
C. This option is not helpful. Limiting interactions with healthcare providers may result in inadequate support and education for the client, leading to increased anxiety and uncertainty.
D. This option is not appropriate. Encouraging the client to stop discussing their concerns with family members can isolate the client emotionally and prevent them from receiving much-needed emotional support.
Explanation
A. This response is not helpful. Telling the client that their feelings are unwarranted may invalidate their emotions and not address their concerns.
B. This response is appropriate. Validating the client's feelings while reassuring them of their family's support can help the client feel understood and less burdened by their emotions.
C. This response is not appropriate. Encouraging the client to hide their feelings from their family can lead to emotional suppression and may hinder open communication.
D. This response is not appropriate. Encouraging the client to rely more on friends than family for support may not be practical or address the client's feelings of guilt and burden.
Explanation
A. This statement is incorrect. Limiting potassium intake is not primarily related to preventing dehydration and electrolyte imbalances.
B. This statement is incorrect. While reducing potassium intake can be beneficial for kidney function, it is not the primary reason for limiting potassium in clients with ESRD.
C. This statement is incorrect. Although adequate calcium intake is essential for bone health, it is not the main reason for limiting potassium in ESRD clients.
D. This statement is correct. Clients with ESRD have impaired kidney function, which can lead to decreased potassium excretion. Excess potassium in the bloodstream can result in dangerous heart rhythm disturbances (arrhythmias) and muscle weakness. Limiting dietary potassium helps prevent these complications and maintain a safe level of potassium in the body.
Explanation
A. This statement is incorrect. Iron supplements do not directly improve kidney function or slow down the progression of ESRD.
B. This statement is incorrect. While adequate calcium and vitamin D are essential for bone health, iron supplements are not primarily used for this purpose.
C. This statement is correct. Iron supplements are prescribed to clients with ESRD experiencing anemia due to decreased red blood cell production. Iron is necessary for the production of hemoglobin, the protein responsible for carrying oxygen in the blood. Supplementing with iron can help improve red blood cell production and alleviate anemia symptoms.
D. This statement is incorrect. Iron supplements are not specifically used to prevent dangerous blood clots.
Explanation
A. This statement is incorrect. While phosphate binders may be prescribed to manage phosphorus levels, they do not protect the kidneys or slow down the progression of ESRD.
B. This statement is not the primary reason for prescribing phosphate binders. While they may influence calcium absorption, their main role is to control phosphorus levels.
C. This statement is not the main purpose of phosphate binders. While managing phosphorus levels may have some effect on blood pressure and heart health, the primary rationale for using phosphate binders is to reduce the elevated phosphorus levels in the blood.
D. This statement is correct. In clients with ESRD, impaired kidney function can lead to increased phosphorus levels in the blood (hyperphosphatemiA. . Phosphate binders are prescribed to lower the absorption of dietary phosphorus, thus reducing the phosphorus level in the blood. Maintaining appropriate phosphorus levels is essential for bone and muscle health and can help prevent complications associated with hyperphosphatemia.
Questions
Explanation
A. Encouraging the client to share their feelings with friends and family is essential, but connecting with individuals experiencing similar challenges in a support group can provide the client with additional understanding and emotional support.
B. This is the correct answer. Support groups provide an opportunity for clients with ESRD to share their experiences, learn coping strategies from others, and realize they are not alone in their struggles, which can alleviate feelings of isolation and provide emotional support.
C. Advising the client to limit social interactions can exacerbate feelings of isolation and loneliness, which is not helpful in providing appropriate support.
D. While it is essential to reassure the client that feeling overwhelmed is normal, attending a support group can provide them with practical strategies for coping with these emotions.
Explanation
A. Telling the client they must accept their condition without resistance may invalidate their emotions and not allow them to express their feelings freely.
B. While positivity is essential, avoiding focusing on negative emotions may hinder therapeutic communication and the client's ability to express their true feelings.
C. This is the correct answer. Therapeutic communication involves active listening and providing a safe space for the client to express their feelings openly. The nurse's statement acknowledges the client's emotions and offers support.
D. Encouraging the client to think about positive aspects and avoid dwelling on the negative may not allow the client to process and express their feelings genuinely.
Explanation
A. Encouraging the client to avoid talking about their feelings may suppress their emotions and prevent them from seeking appropriate support.
B. This is the correct answer. Depression and feelings of hopelessness require professional mental health intervention. Referring the client to a mental health professional allows for specialized support and counseling to address their emotional needs.
C. While physical exercise can be beneficial for mental health, it is not the primary intervention for addressing clinical depression and feelings of hopelessness.
D. Encouraging the client to rely solely on family for emotional support may not be sufficient to address the severity of their emotional concerns. Professional counseling and therapy are necessary to address clinical depression.
Explanation
A. Avoiding addressing stressors can lead to emotional suppression and may increase feelings of burden and isolation, not providing effective coping strategies.
B. Suppressing emotions is not a healthy coping mechanism and may lead to increased stress and emotional strain over time.
C. This is the correct answer. Deep breathing exercises and mindfulness techniques are evidence-based stress management strategies that can help the client manage stress more effectively and promote emotional well-being.
D. While physical activity is essential for overall health, excessive physical activity may not address the root cause of stress and can lead to physical exhaustion.
Explanation
A. Encouraging the client to ignore their financial situation does not address their distress and may hinder them from seeking appropriate financial support.
B. This is the correct answer. Referring the client to a financial counselor can help them explore financial assistance options, budgeting strategies, and potential resources to alleviate their financial difficulties.
C. Suggesting the client borrow money from friends or family may not be a practical solution, and it does not address the root cause of the client's financial distress.
D. While it may be true that financial struggles are common in ESRD, simply acknowledging this fact does not offer practical solutions or support to the client in managing their financial difficulties.
Explanation
A. Instructing the client to avoid adhering strictly to the dialysis schedule can be detrimental to their health and may lead to complications associated with missed treatments.
B. Encouraging the client to skip dialysis sessions is not appropriate as it can worsen their condition and lead to serious health consequences.
C. This is the correct answer. Recognizing and reporting signs of infection or complications is crucial for clients on dialysis. Early detection and management of potential issues can help prevent further complications and ensure the client's well-being.
D. Advising the client to avoid monitoring their fluid and dietary intake can lead to fluid overload and worsen their ESRD condition.
Explanation
A. Criticizing the client's lack of compliance is not an effective approach and may lead to increased feelings of frustration and disengagement.
B. Offering rewards and incentives may not address the underlying reasons for the client's lack of motivation and may not be a sustainable strategy.
C. Telling the client that adherence is essential regardless of their feelings may not address the barriers they are experiencing and can be perceived as dismissive of their concerns.
D. This is the correct answer. Listening to the client's concerns and exploring strategies together allows the nurse to identify potential barriers to adherence and develop personalized solutions that are meaningful to the client. Collaborative goal-setting enhances the client's motivation and promotes ownership of their treatment plan.
Questions
Benign prostatic hyperplasia
Explanation
A. Dysuria can be associated with urinary tract infections but is not a typical symptom of BPH.
B. Hematuria may indicate other urological conditions but is not a primary symptom of BPH.
C. This is the correct answer. Urinary frequency, especially during the night (nocturiA. , is a common symptom of BPH. It occurs due to the enlarged prostate compressing the urethra and obstructing urine flow.
D. Rectal pain and discomfort are not typical symptoms of BPH.
Explanation
A. Young age is not a risk factor for developing BPH. BPH is more common in older men, typically over the age of 50.
B. This is the correct answer. Family history of BPH is considered a risk factor, suggesting a genetic predisposition to developing the condition.
C. High intake of dairy products is not a well-established risk factor for BPH. However, some studies have suggested a potential link between calcium intake and BPH risk, but more research is needed.
D. A sedentary lifestyle may contribute to overall health issues but is not a specific risk factor for BPH.
Explanation
A. This is the correct answer. Difficulty starting a urine stream is a common symptom of BPH and occurs because the enlarged prostate compresses the urethra, obstructing the flow of urine.
B. Bladder spasms causing urinary retention are not a typical symptom of BPH.
C. Excessive fluid intake may lead to increased urinary frequency, but it is not directly related to difficulty starting a urine stream in BPH.
D. An enlarged bladder compressing the urethra is not a common symptom of BPH. Instead, it is the enlarged prostate that causes the obstruction.
Explanation
A. This is the correct answer. When a urinary catheter is in place, there is a risk of urinary tract infection due to the introduction of bacteria into the urinary tract.
B. Increased urine output is not a typical complication related to a urinary catheter. The catheter helps drain urine from the bladder, but it does not increase urine production.
C. Reduced bladder pressure may occur when a catheter is draining urine from the bladder, but it is not a complication to monitor for specifically.
D. Improved urine flow is an intended outcome of relieving urinary retention with the catheter, not a complication.
Explanation
A. Limiting fluid intake in the morning is not likely to be helpful in reducing nighttime awakenings caused by urinary frequency and nocturia.
B. Limiting fluid intake in the afternoon is not likely to be helpful in reducing nighttime awakenings caused by urinary frequency and nocturia.
C. This is the correct answer. Limiting fluid intake in the evening can help reduce the volume of urine produced during the night, thereby decreasing nocturia and nighttime awakenings.
D. Limiting fluid intake at night may cause dehydration and is not recommended. Instead, the client should focus on reducing evening fluid intake to minimize nighttime urine production.
Questions
Explanation
A. Acute urinary retention is characterized by the sudden inability to pass urine, resulting in severe pain and discomfort. Difficulty starting a urine stream and a weak urine flow are characteristic of obstructive voiding symptoms, not acute urinary retention.
B. Urinary incontinence refers to the involuntary loss of urine and is not associated with difficulty starting a urine stream or a weak urine flow.
C. Stress urinary incontinence is a type of urinary incontinence characterized by urine leakage during activities that increase intra-abdominal pressure, such as coughing, sneezing, or laughing. It is not related to the symptoms described in the question.
D. This is the correct answer. Difficulty starting a urine stream and a weak urine flow are obstructive voiding symptoms commonly seen in clients with BPH due to the enlargement of the prostate gland, which obstructs the urethra.
Explanation
A. Increased urinary frequency is a common symptom of BPH, but it is not directly related to bladder outlet obstruction. It is a result of reduced bladder capacity due to the obstruction.
B. Nocturia is the need to wake up at night to urinate and can be caused by reduced bladder capacity and increased urine production at night due to BPH. However, it is not as indicative of bladder outlet obstruction as difficulty emptying the bladder.
C. Hematuria (blood in the urinE. can be a sign of various urinary tract disorders but is not a specific symptom of bladder outlet obstruction.
D. This is the correct answer. Difficulty emptying the bladder is a hallmark symptom of bladder outlet obstruction caused by an enlarged prostate in BPH.
Explanation
A. Urinary urgency is a common symptom of BPH but not necessarily a complication.
B. This is the correct answer. Erectile dysfunction (ED. is a potential complication of BPH. The enlarged prostate can compress the prostatic nerves and affect erectile function.
C. Stress urinary incontinence is not a typical complication of BPH. It is more commonly associated with other conditions, such as weakened pelvic floor muscles.
D. Increased urine output is not a typical complication of BPH. BPH primarily affects the outflow of urine, resulting in obstructive voiding symptoms.
Explanation
A. Overflow urinary incontinence is characterized by constant or frequent dribbling of urine due to the bladder's inability to empty fully. It is not specifically related to postvoid dribbling.
B. Stress urinary incontinence is the involuntary loss of urine during activities that increase intra-abdominal pressure, such as coughing, sneezing, or laughing. It is not directly related to postvoid dribbling.
C. This is the correct answer. Postvoid dribbling refers to the leakage of urine that occurs immediately after completing urination. It is often seen in clients with BPH due to the enlarged prostate obstructing the urethra, leading to incomplete bladder emptying and residual urine left in the urethra.
D. Urinary urgency is the sudden and strong desire to urinate and is not specifically related to postvoid dribbling.
Explanation
A. This is the correct answer. Urinary retention refers to the inability to completely empty the bladder, leading to a sensation of fullness in the lower abdomen and difficulty voiding.
B. Urinary urgency is the sudden and strong desire to urinate.
C. Urinary frequency is the need to urinate more often than usual.
D. Nocturia is the need to wake up at night to urinate.
Explanation
A. Reduced urine output is not a contributing factor to recurrent UTIs. In BPH, the urinary flow is obstructed, leading to incomplete bladder emptying and residual urine in the bladder, which can increase the risk of UTIs.
B. Increased fluid intake is not directly related to the risk of recurrent UTIs in BPH.
C. Decreased prostate size is not associated with recurrent UTIs in BPH.
D. This is the correct answer. Residual urine in the bladder after voiding provides a breeding ground for bacteria, increasing the risk of UTIs. In BPH, the enlarged prostate obstructs the urethra, leading to incomplete bladder emptying and the presence of residual urine, which contributes to recurrent UTIs.
Explanation
A. Alpha-blockers do not directly reduce the size of the prostate gland. They work by relaxing the smooth muscles of the bladder neck and prostate, improving urinary flow and reducing obstructive voiding symptoms.
B. This is the correct answer. Alpha-blockers are commonly prescribed for BPH to relax the smooth muscles of the bladder neck and prostate, relieving the obstruction and improving urine flow.
C. Inhibiting the production of dihydrotestosterone (DHT) is the mechanism of action of 5-alpha reductase inhibitors, not alpha-blockers. DHT plays a role in prostate enlargement, and inhibiting its production can reduce the size of the prostate over time.
D. Alpha-blockers do not enhance urine production by the kidneys. They primarily focus on relaxing the smooth muscles to improve urinary flow.
Questions
A client with lower urinary tract symptoms (LUTS) seeks medical advice. The nurse anticipates that the initial diagnostic evaluation for BPH will likely include:
Explanation
A. This is the correct answer. A digital rectal examination (DRE. is typically the first step in the diagnostic evaluation of BPH. During a DRE, the healthcare provider can assess the size, shape, and consistency of the prostate gland to identify any enlargement or abnormalities.
B. The prostate-specific antigen (PSA. test is used to screen for prostate cancer, not specifically for BPH. While elevated PSA levels can be seen in both conditions, the DRE is usually the initial step for BPH evaluation.
C. Transrectal ultrasound (TRUS) is a diagnostic test used to assess the prostate gland's size and characteristics in more detail. It is often performed in conjunction with other tests, but it is not typically the initial step in the diagnostic evaluation of BPH.
D. A urinalysis is a general test used to assess the urine's appearance, specific gravity, and the presence of blood, proteins, and other substances. While it can provide information about kidney function and potential urinary tract infections, it is not specific to BPH.
A nurse is preparing a client for a transrectal ultrasound (TRUS) to evaluate the prostate gland. What information should the nurse provide to the client about the procedure?
Explanation
A. A transrectal ultrasound (TRUS) is a diagnostic imaging procedure that uses sound waves to create images of the prostate gland. It does not involve a biopsy of the prostate gland.
B. Fasting is not necessary for a transrectal ultrasound (TRUS). It is a non-invasive procedure and does not require any special preparation, such as fasting.
C. While a clean bowel is preferable for a transrectal ultrasound, it does not typically require an enema. The client may be asked to empty the rectum with a bowel movement before the procedure.
D. This is the correct answer. During a transrectal ultrasound (TRUS), a lubricated probe is inserted into the rectum to obtain images of the prostate gland. Some clients may experience mild discomfort or pressure during the procedure, but it is generally well-tolerated.
A client with suspected BPH is scheduled for a prostate-specific antigen (PS
Explanation
A. The prostate-specific antigen (PSA. test is not specific to BPH diagnosis. Elevated PSA levels can be seen in both BPH and prostate cancer, but it is not used solely for BPH diagnosis.
B. This is the correct answer. The PSA test is primarily used as a screening tool for prostate cancer. Elevated PSA levels may indicate the presence of prostate cancer and can prompt further evaluation.
C. The PSA test is not used to assess renal function. It is specifically related to prostate health and prostate cancer screening.
D. The evaluation of urinary flow rate is typically done through urodynamic studies and flowmetry tests, not the PSA test.
A nurse is reviewing the results of a client's urinalysis as part of the diagnostic evaluation for BPH. Which finding should the nurse expect to be associated with BPH?
Explanation
A. The presence of glucose in the urine is indicative of diabetes mellitus and is not directly related to BPH.
B. An elevated white blood cell count in the urine may indicate a urinary tract infection or inflammation but is not specific to BPH.
C. The presence of bacteria in the urine is indicative of a urinary tract infection and is not specific to BPH.
D. This is the correct answer. Hematuria (blood in the urinE. can be associated with BPH due to irritation or trauma to the urinary tract caused by the enlarged prostate. Hematuria may be gross (visiblE. or microscopic and should be further evaluated to determine its cause.
Explanation
A. Increased urine output is not a contributing factor to recurrent UTIs. In BPH, the urinary flow is obstructed, leading to incomplete bladder emptying and residual urine in the bladder, which can increase the risk of UTIs.
B. This is the correct answer. Residual urine in the bladder after voiding provides a breeding ground for bacteria, increasing the risk of UTIs. In BPH, the enlarged prostate obstructs the urethra, leading to incomplete bladder emptying and the presence of residual urine, which contributes to recurrent UTIs.
C. Decreased fluid intake may contribute to urinary stasis and an increased risk of UTIs, but it is not specific to BPH.
D. Reduced bladder capacity is not a contributing factor to recurrent UTIs in BPH.
Explanation
A. A urodynamic study is not used to determine the size of the prostate gland. It is primarily focused on assessing bladder and urinary function.
B. A urodynamic study is not used to assess renal function and kidney health. It is a diagnostic test focused on evaluating the lower urinary tract and bladder function.
C. This is the correct answer. A urodynamic study is a diagnostic test used to evaluate the pressure and flow of urine during voiding. It provides valuable information about the lower urinary tract's function, including bladder capacity, detrusor muscle activity, and the presence of any obstructions or abnormalities.
D. A urodynamic study is not used to evaluate the bladder's capacity directly, but it does assess bladder function during voiding.
Explanation
A. Stress urinary incontinence is the involuntary loss of urine due to activities that increase intra-abdominal pressure, such as coughing or sneezing. It is not related to the symptoms described in the question.
B. Overflow urinary incontinence is characterized by a constant dribbling of urine due to an overdistended bladder. It is typically seen in conditions that obstruct urine flow, such as BPH, but it does not present as difficulty starting the urine stream and a weak flow.
C. This is the correct answer. Difficulty starting the urine stream and a weak urinary flow are common symptoms of urinary retention, a condition in which the bladder does not fully empty during voiding due to an obstruction, such as an enlarged prostate in BPH.
D. Urge urinary incontinence is characterized by a sudden, strong urge to urinate, followed by involuntary urine loss. It is not related to the symptoms described in the question.
Questions
Explanation
A. Radiation therapy is not a first-line treatment for BPH. It is primarily used for certain types of cancer treatment.
B. Hormone therapy may be used for advanced cases of BPH, but it is not typically the initial management.
C. This is the correct answer. Watchful waiting, also known as active surveillance, is often the initial management for mild to moderate BPH. It involves close monitoring of symptoms and the prostate's size without immediate intervention unless symptoms worsen or complications arise.
D. Invasive surgery is usually reserved for severe cases of BPH that do not respond to conservative management or when complications occur.
Explanation
A. This is the correct answer. Alpha-blockers are commonly prescribed as the first-line medication for BPH. They relax the smooth muscles in the prostate and bladder neck, improving urinary flow and reducing LUTS.
B. Antibiotics are prescribed if the client has a urinary tract infection, but they do not directly address BPH symptoms.
C. Diuretics are not typically used to treat BPH.
D. Anticholinergics are used to treat overactive bladder symptoms, which are not specific to BPH-related LUTS.
Explanation
A. Transurethral resection of the prostate (TURP) is a surgical procedure that removes only a portion of the enlarged prostate gland, not the entire gland.
B. This is a potential benefit of TURP, but the primary purpose of the procedure is to reduce the size of the prostate to relieve urinary obstruction and improve urinary flow.
C. This is the correct answer. TURP is performed to reduce the size of the prostate gland, which is causing urinary obstruction due to BPH.
D. TURP does not have a direct impact on fertility, as it does not affect the production or release of sperm.
Explanation
A. Relaxing the smooth muscles in the bladder neck is the action of alpha-blockers, not 5-alpha reductase inhibitors.
B. This is the correct answer. 5-alpha reductase inhibitors work by blocking the enzyme 5-alpha reductase, which converts testosterone into dihydrotestosterone (DHT). DHT is involved in the growth of the prostate gland, and reducing its levels can help shrink the prostate and improve urinary flow in BPH.
C. Inhibiting bacterial growth in the prostate gland is the action of antibiotics, not 5-alpha reductase inhibitors.
D. Contracting the prostate gland is not a desired effect in BPH management.
Explanation
A. Limiting fluid intake to avoid urinary urgency is not necessary after a TURP. Adequate hydration is essential for promoting urinary flow and preventing urinary tract infections.
B. This is the correct answer. After a TURP, sexual activity is usually restricted for at least two weeks to allow for proper healing and to reduce the risk of complications, such as bleeding or infection.
C. Restricting walking and physical activity is not necessary after a TURP. Encouraging early ambulation is important for preventing complications and promoting recovery.
D. Avoiding sitting for extended periods is not a specific activity restriction after a TURP.
Explanation
A. Prostate massage is not recommended for clients with urinary retention due to BPH. It can cause the spread of infection or worsen inflammation.
B. The double voiding technique is used to empty the bladder more completely, but it may not be effective in cases of urinary retention.
C. This is the correct answer. Catheterization is often necessary to relieve urinary retention in clients with BPH. It involves inserting a catheter into the bladder to drain the urine.
D. Pelvic floor exercises are helpful for strengthening pelvic muscles but are not a primary intervention for relieving urinary retention.
Explanation
A. Preventing recurrent urinary tract infections is not the primary purpose of combination therapy with an alpha-blocker and a 5-alpha reductase inhibitor.
B. While some improvement in erectile function may occur with alpha-blockers, the primary purpose of the combination therapy is not to address erectile dysfunction.
C. This is the correct answer. The combination of an alpha-blocker and a 5-alpha reductase inhibitor is used to enhance the effects of both medications. Alpha-blockers help relieve urinary symptoms quickly by relaxing the smooth muscles of the prostate and bladder neck, while 5-alpha reductase inhibitors work over time to shrink the prostate and improve urinary flow.
D. Reducing the risk of urinary incontinence is not the primary goal of combination therapy with these medications.
Questions
Explanation
A. This is the correct answer. Difficulty starting the urinary stream and a feeling of incomplete bladder emptying are common symptoms of urinary retention, a complication of BPH. In BPH, the enlarged prostate obstructs the flow of urine from the bladder, leading to incomplete emptying and retention.
B. Hematuria, or blood in the urine, is not typically associated with BPH but may occur in other conditions affecting the urinary tract.
C. Stress incontinence is the involuntary loss of urine during activities that increase intra-abdominal pressure, such as coughing or sneezing, and is not specific to BPH.
D. Urgency is the sudden and strong need to urinate, and it is not specifically associated with BPH.
Explanation
A. While urinary tract infections can occur in clients with BPH, they do not typically present with severe pain in the lower abdomen, groin, and testicles.
B. Testicular cancer does not typically cause pain in the lower abdomen and is not directly related to BPH.
C. This is the correct answer. Severe pain in the lower abdomen, groin, and testicles can be indicative of kidney stones, which may occur as a complication of BPH. Urinary retention and stasis in the bladder can lead to the formation of stones.
D. Prostate cancer may cause symptoms similar to BPH, but sudden severe pain in the lower abdomen, groin, and testicles is not a typical presentation of prostate cancer.
Explanation
A. Decreased urine production is not a common complication of BPH. Instead, BPH leads to urinary retention and incomplete bladder emptying.
B. This is the correct answer. BPH can lead to urinary retention, allowing bacteria to multiply and colonize the prostate, increasing the risk of recurrent UTIs.
C. Increased bladder capacity is not a complication of BPH. Instead, the enlarged prostate obstructs the flow of urine, leading to urinary retention and incomplete emptying.
D. Inadequate fluid intake may contribute to UTIs, but the primary reason for recurrent UTIs in BPH is the bacterial colonization of the prostate due to urinary retention.
Explanation
A. This is the correct answer. The client's symptoms of difficulty starting the urinary stream and a weak urine flow, along with a distended bladder and a firm, enlarged prostate on digital rectal examination, suggest acute urinary retention, which is a complication of BPH.
B. Chronic kidney disease is not directly related to the physical findings described in the scenario.
C. Urethral stricture may cause difficulty in starting the urinary stream, but it would not typically present with a distended bladder and an enlarged prostate.
D. Prostate cancer may have similar symptoms to BPH but would not present with acute urinary retention and a distended bladder.
Explanation
A. Chronic kidney disease is not directly related to hematuria in clients with BPH. Hematuria is not a typical symptom of kidney disease.
B. While urinary tract infections may cause hematuria, it is more commonly associated with bladder stones in clients with BPH.
C. Prostate cancer may cause hematuria, but it is less common than other potential complications.
D. This is the correct answer. Hematuria in clients with BPH may be due to the presence of bladder stones. Urinary retention and stasis can lead to the formation of stones in the bladder, which may cause bleeding and hematuria.
Explanation
A. This is the correct answer. Nocturia and frequent nighttime urination in clients with BPH are often due to decreased bladder capacity. BPH causes obstruction of the urinary outflow, leading to incomplete bladder emptying during the day and increased urine volume at night.
B. Nocturnal enuresis refers to involuntary nighttime urination in children and is not relevant to this scenario.
C. While hormonal changes may play a role in the development of BPH, they are not directly related to nocturia and frequent nighttime urination.
D. Urinary retention may cause decreased frequency of urination rather than nocturia and frequent nighttime urination.
Explanation
A. This is the correct answer. In cases of acute urinary retention, immediate relief is achieved through catheterization to drain the bladder and relieve the obstruction caused by the enlarged prostate.
B. Medications to reduce bladder spasms may be used as an adjunct to catheterization in managing urinary retention but are not the primary intervention for relieving the obstruction.
C. Invasive surgical intervention may be considered for persistent or severe cases of BPH, but it is not the initial step in managing acute urinary retention.
D. Increased fluid intake may be beneficial for overall bladder health but will not directly relieve the obstruction causing acute urinary retention.
Questions
Explanation
A. This statement is correct. Caffeinated beverages can irritate the bladder and worsen BPH symptoms, so it's best to avoid them.
B. This statement is incorrect. Limiting fluid intake, especially in the evening, can help reduce nighttime urination in clients with BPH.
C. This statement is correct. Pelvic floor exercises, such as Kegel exercises, can help strengthen the pelvic muscles and improve urine flow in BPH.
D. This statement is incorrect. Over-the-counter cold medications containing decongestants can worsen BPH symptoms by constricting blood vessels, including those in the prostate, and can lead to urinary retention.
Explanation
A. Encouraging the client to increase fluid intake would be inappropriate in this case, as the client already has a distended bladder and difficulty starting the urinary stream, which are signs of urinary retention.
B. While assisting the client in finding a comfortable position for voiding is important, it will not relieve the current urinary retention.
C. Teaching the client relaxation techniques is beneficial for overall health, but it will not address the immediate issue of urinary retention.
D. This is the correct answer. Catheterization is necessary to relieve urinary retention and drain the distended bladder.
Explanation
A. Resuming normal activities immediately after a TURP is not recommended. The client should gradually resume activities as advised by the healthcare provider.
B. This is the correct answer. After a TURP, the client is at risk of developing a UTI due to catheter use and bladder manipulation. The nurse should monitor for signs of infection, such as fever, dysuria, or cloudy urine.
C. Avoiding all fluid intake for 24 hours is not appropriate, as it can lead to dehydration and other complications. Adequate hydration is essential for postoperative recovery.
D. Administering anticoagulant medications may not be necessary after a TURP unless specifically ordered by the healthcare provider. The nurse should follow the prescribed medication regimen and monitor for bleeding complications.
Explanation
A. Scheduling a follow-up appointment in two years is too long of an interval for a client with BPH. Regular follow-up is essential for monitoring the condition and adjusting the treatment plan as needed.
B. This is the correct answer. Clients with BPH should have regular follow-up appointments, typically every six months, to monitor symptoms and treatment effectiveness.
C. Skipping follow-up appointments, even if the client is feeling better, is not advisable. Regular monitoring is essential to ensure optimal management of BPH.
D. Waiting for new symptoms to arise before seeking a follow-up appointment may delay necessary interventions and could lead to worsening of symptoms.
Explanation
A. Dry mouth is not a common side effect of alpha-blocker medications used to treat BPH
.
B. Constipation is not a common side effect of alpha-blocker medications used to treat BPH.
C. While alpha-blockers can cause a decrease in blood pressure, they are often used to treat hypertension, so this answer is incorrect.
D. This is the correct answer. Alpha-blocker medications used to treat BPH can cause a sudden drop in blood pressure, leading to dizziness. Clients should be educated about this potential side effect and advised to change positions slowly to minimize the risk of falls.
Explanation
A. Clamping the catheter is not recommended, as it can cause urinary retention and obstruct urine flow.
B. Cleansing around the catheter insertion site with alcohol is not recommended, as it may cause skin irritation. The site should be cleaned with mild soap and water.
C. Securing the catheter to the leg with a safety pin is not recommended, as it may cause trauma to the catheter and increase the risk of infection.
D. This is the correct answer. Clients should be instructed to report any signs of catheter blockage or leakage to their healthcare provider. Catheter blockage can lead to urinary retention, and leakage may indicate a problem with the catheter or the drainage system.
Explanation
A. Increasing calcium intake is not specifically indicated for managing urinary frequency and urgency in clients with BPH.
B. Limiting fluid intake, especially in the evening, may help reduce nighttime urination, but it is not advisable to restrict fluids excessively, as dehydration can lead to other health problems.
C. This is the correct answer. Caffeine and alcohol are diuretics that can increase urine production and exacerbate urinary frequency and urgency in clients with BPH. Recommending the avoidance of these substances may help alleviate symptoms.
D. Eating a high-protein diet is not specifically indicated for managing urinary frequency and urgency in clients with BPH.
Questions
A client asks the nurse, "What is Benign Prostatic Hyperplasia?" Which response by the nurse is most appropriate?
Explanation
A) This statement is not correct. BPH is a non-cancerous condition, not a malignant tumor.
B) This is the correct answer. BPH is characterized by the enlargement of the prostate gland, which is non-cancerous and benign.
C) This statement is not correct. BPH is not an infection of the prostate gland but rather an enlargement.
D) This statement is not correct. BPH does not involve the absence of the prostate gland; it is an enlargement of the gland.
A nurse is reviewing the diagnostic tests used to confirm BPH in a client. Which test directly assesses the size and shape of the prostate gland?
Explanation
A) This is the correct answer. A digital rectal exam (DRE) involves the insertion of a gloved, lubricated finger into the rectum to feel the size, shape, and texture of the prostate gland. It helps assess for enlargement and any abnormalities.
B) The prostate-specific antigen (PSA) blood test measures the level of PSA in the blood, which may be elevated in various prostate conditions, including BPH. However, it does not directly assess the size and shape of the prostate gland.
C) Transrectal ultrasound (TRUS) uses sound waves to create images of the prostate gland and is used to assess the prostate's size and identify any abnormalities.
D) Urinalysis is a urine test that evaluates the urine's physical and chemical properties but does not directly assess the size and shape of the prostate gland.
Renal calculus
Explanation
A. This is not the correct answer. Renal calculi are not bacterial infections but rather solid masses that form from mineral and acid salts in the kidneys.
B. This is the correct answer. Renal calculi, commonly known as kidney stones, are solid masses formed from mineral and acid salts that accumulate in the kidneys.
C. Renal calculi are not benign tumors. They are distinct from tumors and do not have the same characteristics.
D. Renal calculi are not blood clots. Blood clots can block the urinary tract, but they are not the same as kidney stones.
Explanation
A. Excessive water intake is not a risk factor for kidney stones. In fact, adequate hydration is encouraged to prevent kidney stone formation.
B. Low dietary calcium intake is not a common risk factor for kidney stones. In some cases, excessive calcium supplementation may be a risk factor, but dietary calcium is generally not a concern.
C. This is the correct answer. Family history, a diet high in protein and salt, and dehydration are common risk factors for kidney stones.
D. Kidney stones are not mostly caused by consuming too many fruits and vegetables. Fruits and vegetables are generally considered beneficial for kidney health.
Explanation
A. Citrus fruits are generally not a concern for calcium oxalate stones. They are a good source of citrate, which may actually help prevent stone formation.
B. Dairy products are not specifically associated with calcium oxalate stones. However, high-calcium supplements might increase the risk, not dietary calcium from dairy products.
C. Red meat is not a significant concern for calcium oxalate stones. It is more associated with uric acid stones.
D. This is the correct answer. Leafy green vegetables are high in oxalates, which can contribute to calcium oxalate stone formation. Clients with calcium oxalate stones should limit their intake of these vegetables.
Explanation
A. Severe back pain can be a symptom of kidney stones, but it is not the most common one.
B. This is the correct answer. Hematuria, or blood in the urine, is the most common symptom of kidney stones. The blood may be visible or microscopic.
C. Frequent urination can be a symptom of kidney stones, but it is not the most common one.
D. Sudden weight loss is not a symptom commonly associated with kidney stones.
Explanation
A. Calcium oxalate stones may cause pain, but they do not typically radiate to the groin. They are more likely to cause localized pain in the back or side.
B. This is the correct answer. Uric acid stones can cause sudden and severe pain that radiates from the back to the groin. The pain is often described as colicky and is associated with restlessness.
C. Struvite stones are typically associated with urinary tract infections and may not cause the sudden and severe pain described in the question.
D. Cystine stones are rare and are more likely to cause chronic, dull pain rather than sudden and severe pain.
Explanation
A. Avoiding all dairy products is not a recommended prevention strategy for kidney stones. In fact, adequate dietary calcium may be beneficial for reducing the risk of certain types of stones.
B. Increasing dietary calcium intake, especially from food sources, may help prevent certain types of kidney stones, such as calcium oxalate stones.
C. Reducing fluid intake is not a recommended prevention strategy for kidney stones. Inadequate hydration can actually increase the risk of stone formation.
D. This is the correct answer. Drinking plenty of water and staying hydrated is one of the most effective ways to prevent kidney stones. Adequate hydration helps dilute urine and reduce the concentration of minerals that can lead to stone formation.
Explanation
A. ESWL is a non-invasive procedure, and it does not require a hospital stay. It is typically performed on an outpatient basis.
B. This is not entirely accurate. ESWL is a non-invasive procedure that does not require general anesthesia. Instead, the client may be given sedation or local anesthesia.
C. It is essential to maintain adequate hydration after ESWL to help pass the broken-up stone fragments. Avoiding all fluids for 24 hours is not recommended and may lead to dehydration.
D. This is the correct answer. ESWL uses shock waves to break up kidney stones, and the client will need to remain still during the procedure to ensure precise targeting of the stones. The procedure is usually painless, but some discomfort may be experienced during the process.
Questions
Explanation
A. Excessive consumption of fruits and vegetables is not a primary cause of kidney stones. Some specific types of fruits and vegetables may contribute to stone formation, but it is not a general cause.
B. While genetic factors and family history can play a role in kidney stone formation, they are not the primary cause. The presence of minerals and salts in the urine is the main contributing factor.
C. An overactive bladder and frequent urination are not direct causes of kidney stone formation. They may be related to other urinary conditions but not to the formation of kidney stones.
D. This is the correct answer. Kidney stones are formed when certain minerals and salts in the urine form solid crystals that can clump together and grow into stones.
Explanation
A. This is the correct answer. High dietary calcium intake is a common risk factor for certain types of kidney stones, particularly calcium oxalate stones. However, dietary calcium intake from food sources is not typically associated with an increased risk of kidney stones. Calcium supplements, on the other hand, may contribute to stone formation.
B. A low protein diet is not a significant risk factor for kidney stones. High-protein diets may be associated with an increased risk, but low protein intake is not a concern.
C. Adequate water consumption is essential to prevent kidney stones. Dehydration is a risk factor for stone formation, but excessive water consumption alone is not a significant risk factor.
D. While a sedentary lifestyle may be associated with other health risks, it is not a primary risk factor for kidney stones.
Explanation
A. This is the correct answer. Calcium oxalate stones are common, and limiting the intake of foods high in oxalate, such as spinach, nuts, and certain other vegetables and fruits, can help reduce the risk of stone recurrence.
B. Increasing the intake of red meat and fish is not recommended to prevent calcium oxalate stones. In fact, high intake of animal protein may increase the risk of certain types of stones, such as uric acid stones.
C. Consuming carbonated beverages is not recommended to improve kidney function or prevent kidney stones. Some carbonated beverages may contain phosphoric acid, which can contribute to stone formation.
D. Avoiding dairy products is not recommended to prevent calcium oxalate stone formation. In fact, adequate dietary calcium intake from food sources may help reduce the risk of these stones.
Explanation
A. This is not entirely accurate. While family history can be a risk factor for kidney stones, there are still preventive measures that individuals can take to reduce their risk.
B. Avoiding all calcium-rich foods and beverages is not recommended for preventing kidney stones. In fact, adequate dietary calcium from food sources is generally beneficial for kidney health and may help reduce the risk of certain types of stones.
C. This is the correct answer. Maintaining a healthy weight and drinking plenty of water are important lifestyle factors that can help reduce the risk of kidney stones. Adequate hydration helps prevent the concentration of minerals in the urine, reducing the likelihood of stone formation.
D. Surgery is not the only treatment option for kidney stones. Depending on the size and type of stone, other treatment options, such as lithotripsy or medication, may be considered.
Explanation
A. Uric acid stones may cause pain, but they do not typically present with costovertebral angle tenderness. Uric acid stones are more likely to be associated with gout and hyperuricemia.
B. Calcium oxalate stones are common and can cause pain, but they do not typically cause costovertebral angle tenderness. They are more likely to cause localized pain in the back or side.
C. This is the correct answer. Struvite stones, also known as infection stones, can cause severe pain that radiates to the back and lower abdomen. They are often associated with urinary tract infections, and the presence of an infection can lead to costovertebral angle tenderness.
D. Cystine stones are rare and are more likely to cause chronic, dull pain rather than sudden and severe pain with tenderness.
Explanation
A. Smoking cessation is important for overall health, but it is not a primary lifestyle factor related to kidney stone formation.
B. Increased alcohol consumption is not recommended as a preventive measure for kidney stones. In fact, excessive alcohol intake can lead to dehydration, which is a risk factor for stone formation.
C. Regular exercise can be beneficial for overall health, but it is not a primary lifestyle factor related to kidney stone formation.
D. This is the correct answer. A high sodium diet can increase the excretion of calcium in the urine, leading to a higher risk of calcium-based kidney stones. Reducing sodium intake can help prevent stone formation.
Explanation
A. Limiting fluid intake is not recommended to prevent kidney stones. Adequate hydration is essential to prevent stone formation. Dehydration can lead to a higher concentration of minerals in the urine, increasing the risk of stones.
B. Including more foods high in oxalate is not recommended to prevent kidney stones, especially if the client has a history of calcium oxalate stones. Limiting the intake of oxalate-rich foods is a preventive measure.
C. Avoiding all dairy products is not recommended to prevent kidney stones. In fact, adequate dietary calcium intake from food sources may help reduce the risk of certain types of stones, such as calcium oxalate stones.
D. This is the correct answer. Staying hydrated and drinking plenty of water throughout the day is one of the most effective ways to prevent kidney stones. Adequate hydration helps dilute urine and reduce the concentration of minerals that can lead to stone formation.
Questions
Explanation
A. Sharp, stabbing pain in the lower abdomen is not typically associated with kidney stones. Kidney stone pain is usually felt in the back and flank regions of the body.
B. This is the correct answer. The pain caused by kidney stones is often described as a dull ache in the upper back and flank region, usually on the affected side where the kidney is located.
C. Burning sensation during urination is more commonly associated with urinary tract infections or inflammation of the urethra, not kidney stones.
D. Constant, generalized abdominal discomfort is not a specific symptom of kidney stones. Kidney stone pain is usually more localized to the back and flank regions.
Explanation
A. Fever and chills are more commonly associated with a urinary tract infection, which can sometimes be a complication of kidney stones. However, the severe pain described is more likely related to the presence of the stone itself.
B. This is the correct answer. Blood in the urine, also known as hematuria, is a common symptom of kidney stones. As the stone moves through the urinary tract, it may cause irritation and small blood vessels may be damaged, resulting in blood in the urine.
C. Difficulty starting the urine stream is not a specific symptom of kidney stones. It may be seen in other urinary conditions but is not typically associated with stones.
D. The frequent urge to urinate may be experienced if the stone causes irritation in the bladder, but it is not the most common symptom associated with kidney stones.
Explanation
A. This is the correct answer. Kidney stone pain is often described as colicky, which means it comes and goes in waves of severe pain. The pain can be intense and cramp-like, causing the client to writhe or be restless.
B. Gnawing pain is not typically associated with kidney stones. Gnawing pain is often described as a persistent, dull ache that can be more chronic in nature.
C. Stabbing pain is sharp and localized and is not typically used to describe kidney stone pain.
D. Numbing pain refers to a loss of sensation, which is not characteristic of kidney stone pain.
Explanation
A. Diarrhea and abdominal cramping are not typically associated with kidney stone pain. These symptoms are more commonly seen in gastrointestinal disorders.
B. Painful and frequent urination may occur if the stone causes irritation in the bladder or urethra, but it is not a direct symptom of kidney stone pain.
C. Fatigue and generalized weakness are not specific symptoms of kidney stone pain. They may be associated with other medical conditions but are not directly related to renal calculus.
D. This is the correct answer. Nausea and vomiting are common symptoms that may accompany kidney stone pain, especially if the stone causes obstruction in the urinary tract. The pain and irritation can trigger a reflex that leads to nausea and vomiting.
Explanation
A. Limiting fluid intake to 1 liter per day is not recommended to prevent kidney stone formation. Adequate hydration is essential to
help prevent stone formation, as it helps dilute the urine and reduce the concentration of minerals that can lead to stone formation.
B. Decreasing dietary fiber intake is not a preventive measure for kidney stones. In fact, increasing dietary fiber intake can be beneficial for overall health.
C. Reducing calcium intake from all sources is not recommended to prevent kidney stones. In some cases, reducing dietary calcium intake can actually increase the risk of certain types of kidney stones.
D. This is the correct answer. Increasing citric acid intake can help prevent certain types of kidney stones, such as calcium oxalate stones. Citric acid helps to bind calcium in the urine, reducing the risk of stone formation. Citric acid can be found in citrus fruits and juices, and the nurse may advise the client to include more of these foods in their diet.
Explanation
A. Pain relief is important in managing kidney stone pain, but potassium citrate is not primarily prescribed for this purpose.
B. Acid-base balance regulation may be one of the functions of potassium citrate, but it is not the primary purpose when prescribed to a client with renal calculus.
C. Urinary tract infection treatment is not the primary purpose of potassium citrate. While it may have some benefits in preventing certain types of urinary tract infections associated with stones, its primary purpose is not to treat infections.
D. This is the correct answer. Potassium citrate is prescribed to help dissolve certain types of kidney stones, particularly calcium oxalate stones and uric acid stones. It works by increasing the pH of the urine, making it more alkaline and less conducive to stone formation.
Explanation
A. Extracorporeal shock wave lithotripsy (ESWL) does not typically require general anesthesia. It is usually done under sedation or with the use of local anesthesia.
B. The procedure does not involve the insertion of a scope into the urinary tract. ESWL is a non-invasive procedure that uses shock waves to break up the stone from outside the body.
C. This is the correct answer. ESWL involves the use of high-energy shock waves that are focused on the stone to break it up into smaller fragments. The fragments are then passed out of the body through the urine.
D. A urinary catheter is not typically required after ESWL. The client may be encouraged to drink plenty of fluids to help flush out the stone fragments, but a catheter is not usually needed.
Questions
Explanation
A. Sharp, stabbing pain in the lower abdomen is not typically associated with kidney stones. Kidney stone pain is usually felt in the back and flank regions of the body.
B. This is the correct answer. The pain caused by kidney stones is often described as a dull ache in the upper back and flank region, usually on the affected side where the kidney is located.
C. Burning sensation during urination is more commonly associated with urinary tract infections or inflammation of the urethra, not kidney stones.
D. Constant, generalized abdominal discomfort is not a specific symptom of kidney stones. Kidney stone pain is usually more localized to the back and flank regions.
Explanation
A. Fever and chills are more commonly associated with a urinary tract infection, which can sometimes be a complication of kidney stones. However, the severe pain described is more likely related to the presence of the stone itself.
B. This is the correct answer. Blood in the urine, also known as hematuria, is a common symptom of kidney stones. As the stone moves through the urinary tract, it may cause irritation and small blood vessels may be damaged, resulting in blood in the urine.
C. Difficulty starting the urine stream is not a specific symptom of kidney stones. It may be seen in other urinary conditions but is not typically associated with stones.
D. The frequent urge to urinate may be experienced if the stone causes irritation in the bladder, but it is not the most common symptom associated with kidney stones.
Explanation
A. This is the correct answer. Kidney stone pain is often described as colicky, which means it comes and goes in waves of severe pain. The pain can be intense and cramp-like, causing the client to writhe or be restless.
B. Gnawing pain is not typically associated with kidney stones. Gnawing pain is often described as a persistent, dull ache that can be more chronic in nature.
C. Stabbing pain is sharp and localized and is not typically used to describe kidney stone pain.
D. Numbing pain refers to a loss of sensation, which is not characteristic of kidney stone pain.
Explanation
A. Diarrhea and abdominal cramping are not typically associated with kidney stone pain. These symptoms are more commonly seen in gastrointestinal disorders.
B. Painful and frequent urination may occur if the stone causes irritation in the bladder or urethra, but it is not a direct symptom of kidney stone pain.
C. Fatigue and generalized weakness are not specific symptoms of kidney stone pain. They may be associated with other medical conditions but are not directly related to renal calculus.
D. This is the correct answer. Nausea and vomiting are common symptoms that may accompany kidney stone pain, especially if the stone causes obstruction in the urinary tract. The pain and irritation can trigger a reflex that leads to nausea and vomiting.
Explanation
A. Limiting fluid intake to 1 liter per day is not recommended to prevent kidney stone formation. Adequate hydration is essential to
help prevent stone formation, as it helps dilute the urine and reduce the concentration of minerals that can lead to stone formation.
B. Decreasing dietary fiber intake is not a preventive measure for kidney stones. In fact, increasing dietary fiber intake can be beneficial for overall health.
C. Reducing calcium intake from all sources is not recommended to prevent kidney stones. In some cases, reducing dietary calcium intake can actually increase the risk of certain types of kidney stones.
D. This is the correct answer. Increasing citric acid intake can help prevent certain types of kidney stones, such as calcium oxalate stones. Citric acid helps to bind calcium in the urine, reducing the risk of stone formation. Citric acid can be found in citrus fruits and juices, and the nurse may advise the client to include more of these foods in their diet.
Explanation
A. Pain relief is important in managing kidney stone pain, but potassium citrate is not primarily prescribed for this purpose.
B. Acid-base balance regulation may be one of the functions of potassium citrate, but it is not the primary purpose when prescribed to a client with renal calculus.
C. Urinary tract infection treatment is not the primary purpose of potassium citrate. While it may have some benefits in preventing certain types of urinary tract infections associated with stones, its primary purpose is not to treat infections.
D. This is the correct answer. Potassium citrate is prescribed to help dissolve certain types of kidney stones, particularly calcium oxalate stones and uric acid stones. It works by increasing the pH of the urine, making it more alkaline and less conducive to stone formation.
Explanation
A. Extracorporeal shock wave lithotripsy (ESWL) does not typically require general anesthesia. It is usually done under sedation or with the use of local anesthesia.
B. The procedure does not involve the insertion of a scope into the urinary tract. ESWL is a non-invasive procedure that uses shock waves to break up the stone from outside the body.
C. This is the correct answer. ESWL involves the use of high-energy shock waves that are focused on the stone to break it up into smaller fragments. The fragments are then passed out of the body through the urine.
D. A urinary catheter is not typically required after ESWL. The client may be encouraged to drink plenty of fluids to help flush out the stone fragments, but a catheter is not usually needed.
Questions
Explanation
A. While increasing fluid intake can help with the passage of small stones, it is not likely to dissolve larger stones. The primary benefit of increased fluid intake is to help prevent the formation of new stones.
B. Drinking more fluids may help alleviate some discomfort, but the primary goal is not pain reduction.
C. This is the correct answer. Adequate fluid intake can help prevent the formation of new kidney stones by diluting the urine and reducing the concentration of minerals that can contribute to stone formation.
D. While adequate fluid intake can help reduce the risk of urinary tract infections, it is not the primary reason for recommending increased fluid intake in clients with kidney stones.
Explanation
A. This is a correct statement. Drinking plenty of water is important to help flush out any stone fragments that may have resulted from the procedure.
B. This is a correct statement. Strenuous activities should be avoided for a few days after the procedure to allow for proper healing.
C. This is a correct statement. It is common to have some blood in the urine for a short time after ureteroscopy due to irritation and manipulation of the urinary tract during the procedure.
D. This statement is not correct. After the procedure, the client may be advised to follow a specific diet that is low in certain minerals (such as oxalate and calcium) that can contribute to stone formation. The nurse should provide specific dietary guidelines and restrictions to the client.
Explanation
A. Extracorporeal shock wave lithotripsy (ESWL) is typically used for smaller stones that can be broken up into smaller fragments and passed more easily. It is not usually recommended for large stones.
B. This is the correct answer. Percutaneous nephrolithotomy (PCNL) is a procedure used to remove larger kidney stones. It involves making a small incision in the back and inserting a nephroscope to directly visualize and remove the stone.
C. Ureteroscopy with laser lithotripsy is used for stones in the ureter, not in the kidney itself.
D. Cystoscopy with stent placement is used for conditions involving the lower urinary tract, such as the urethra and bladder, and is not typically used to remove kidney stones.
Explanation
A. Alpha-blockers do not directly reduce inflammation in the urinary tract. They primarily work by relaxing the smooth muscle of the ureters, which can help ease the passage of kidney stones through the urinary tract.
B. Alpha-blockers do not dissolve kidney stones. They assist with stone passage by relaxing the ureters.
C. This is the correct answer. Alpha-blockers are prescribed to relax the smooth muscle of the ureters, allowing the stone to pass more easily through the urinary tract.
D. Alpha-blockers do not have a direct effect on preventing bacterial growth in the urinary tract. They are not antibiotics.
Explanation
A. Reducing calcium intake is not typically recommended for uric acid stones. In fact, low calcium intake can increase the risk of other types of kidney stones.
B. Increasing consumption of red meat and shellfish is not recommended for uric acid stones. These foods are high in purines, which can increase uric acid levels in the body.
C. This is the correct answer. Uric acid stones are formed from high levels of uric acid in the urine. Purine-rich foods can contribute to elevated uric acid levels, so limiting these foods is important in managing uric acid stones.
D. Increasing intake of oxalate-rich foods is not specifically relevant to uric acid stones. Oxalate-rich foods are associated with calcium oxalate stones, not uric acid stones.
Explanation
A. Thiazide diuretics do not directly increase the excretion of uric acid. They are primarily used to reduce calcium excretion and prevent the formation of calcium-based stones.
B. This is the correct answer. Thiazide diuretics help reduce the excretion of calcium in the urine, which can be beneficial in preventing the formation of certain types of kidney stones, particularly calcium oxalate stones.
C. Thiazide diuretics do not directly increase the pH of the urine. They primarily reduce calcium excretion.
D. Thiazide diuretics do not dissolve existing kidney stones. They are used to prevent stone formation, not to treat existing stones.
Explanation
A. This is the correct answer. After percutaneous nephrolithotomy (PCNL), the client may experience urinary retention due to swelling and irritation around the bladder or urethra from the procedure. The nurse should monitor the client for signs of urinary retention, such as difficulty urinating or a distended bladder, and take appropriate measures to relieve the obstruction.
B. Hyperkalemia is not directly related to PCNL. It may occur in certain medical conditions but is not a common complication of this procedure.
C. Hypoglycemia is not related to PCNL. It is a condition related to low blood sugar levels and is not a typical complication of kidney stone removal.
D. Hypertension is not directly related to PCNL. While some clients with hypertension may be at increased risk for kidney stones, hypertension is not a common complication of PCNL itself.
Questions
Explanation
A. This statement is not correct. Adequate fluid intake is essential to help prevent kidney stones. Restricting fluid intake can increase the concentration of minerals in the urine and promote stone formation.
B. This statement is not correct. While calcium oxalate stones are common, reducing calcium intake is not recommended for most people. In fact, a low-calcium diet may increase the risk of other types of kidney stones.
C. This statement is not correct. Fruits and vegetables contain valuable nutrients and should not be avoided. However, some fruits and vegetables are high in oxalate, which may contribute to the formation of calcium oxalate stones. The key is to consume a balanced diet and drink plenty of fluids.
D. This is the correct answer. Adequate fluid intake is crucial in preventing kidney stones. It helps dilute the urine and reduce the concentration of minerals that can lead to stone formation.
Explanation
A. This statement is not correct. If a client has calcium oxalate stones, they should limit foods high in oxalate, such as spinach and nuts, to reduce the risk of stone formation.
B. This is the correct answer. Calcium oxalate stones are the most common type of kidney stone. Reducing dietary calcium intake can help prevent the formation of calcium oxalate stones. However, it is important to note that not all clients with kidney stones should reduce their calcium intake, as calcium is essential for bone health and other bodily functions.
C. Avoiding foods high in purines is more relevant to the prevention of uric acid stones, not calcium oxalate stones.
D. While reducing sodium and processed foods can be beneficial for overall health, it is not a specific dietary modification for preventing calcium oxalate stones.
Explanation
A. This statement is not correct. Limiting intake of calcium is not necessary for the prevention of uric acid stones. In fact, low calcium intake can increase the risk of other types of stones.
B. This is the correct answer. Uric acid stones are formed from high levels of uric acid in the urine. Purine-rich foods can contribute to elevated uric acid levels, so avoiding these foods is important in managing uric acid stones.
C. Increasing consumption of oxalate-rich foods like spinach is not relevant to preventing uric acid stones.
D. Reducing fluid intake is not recommended for preventing any type of kidney stone. Adequate fluid intake is essential for kidney health and preventing stone formation.
Explanation
A. This statement is not correct. Vitamin C supplements may increase the risk of calcium oxalate stones in some individuals.
B. This is the correct answer. High doses of vitamin C can be metabolized into oxalate in the body
, which can contribute to the formation of calcium oxalate stones. For individuals with a history of calcium oxalate stones, it is best to limit vitamin C supplements.
C. Taking vitamin C supplements in large doses is not recommended, especially for individuals prone to kidney stones.
D. Vitamin C supplements do have an effect on kidney stone formation, particularly for those at risk of calcium oxalate stones.
Explanation
A. Avoiding foods high in oxalate is more relevant to the prevention of calcium oxalate stones, not struvite stones.
B. Limiting intake of purine-rich foods is more relevant to the prevention of uric acid stones, not struvite stones.
C. This statement is not correct. Reducing calcium intake is not recommended for struvite stones. In fact, calcium is an essential nutrient for overall health.
D. This is the correct answer. Struvite stones are composed of magnesium, ammonium, and phosphate. Limiting the intake of high-phosphorus foods can help prevent the formation of these stones.
Explanation
A. Thiazide diuretics do not directly increase the excretion of uric acid. They are primarily used to reduce calcium excretion and prevent the formation of calcium-based stones.
B. This is the correct answer. Thiazide diuretics help reduce the excretion of calcium in the urine, which can be beneficial in preventing the formation of certain types of kidney stones, particularly calcium oxalate stones.
C. Thiazide diuretics do not directly increase the pH of the urine. They primarily reduce calcium excretion.
D. Thiazide diuretics do not dissolve existing kidney stones. They are used to prevent stone formation, not to treat existing stones.
Explanation
A. This is the correct answer. After percutaneous nephrolithotomy (PCNL), the client may experience urinary retention due to swelling and irritation around the bladder or urethra from the procedure. The nurse should monitor the client for signs of urinary retention, such as difficulty urinating or a distended bladder, and take appropriate measures to relieve the obstruction.
B. Hyperkalemia is not directly related to PCNL. It may occur in certain medical conditions but is not a common complication of this procedure.
C. Hypoglycemia is not related to PCNL. It is a condition related to low blood sugar levels and is not a typical complication of kidney stone removal.
D. Hypertension is not directly related to PCNL. While some clients with hypertension may be at increased risk for kidney stones, hypertension is not a common complication of PCNL itself.
Questions
Explanation
A. This statement is not correct. Adequate fluid intake is essential in preventing kidney stones. Reducing fluid intake can increase the concentration of minerals in the urine and promote stone formation.
B. This statement is not correct. A high-protein diet can contribute to the formation of certain types of kidney stones, such as uric acid stones. It is not recommended as a preventive measure.
C. This statement is not correct. Dairy products are an important source of calcium, which is needed for overall health. However, individuals with calcium oxalate stones may need to limit high-oxalate foods in their diet.
D. This is the correct answer. Adequate fluid intake helps dilute urine and reduces the concentration of minerals that can lead to stone formation.
Explanation
A. This statement is not correct. Limiting calcium intake is not recommended for preventing calcium oxalate stones. In fact, adequate dietary calcium can help reduce the risk of stone formation.
B. This statement is not correct. Foods high in oxalate, such as spinach and nuts, should be limited to prevent calcium oxalate stones.
C. This statement is not correct. Fruits and vegetables are essential for overall health and should not be avoided. However, some fruits and vegetables are high in oxalate, which may contribute to calcium oxalate stone formation.
D. This is the correct answer. Reducing sodium intake can be beneficial for kidney health, as high sodium intake can increase calcium excretion in the urine and promote stone formation. Additionally, processed foods may contain high levels of sodium and should be limited.
Explanation
A. This statement is not correct. Potassium citrate does not dissolve existing kidney stones. It is used to prevent the formation of certain types of stones, particularly calcium oxalate stones.
B. This is the correct answer. Potassium citrate is an alkalizing agent that helps reduce the acidity of urine. By making the urine less acidic, it can help prevent the formation of certain types of stones, such as uric acid stones.
C. Potassium citrate does not increase calcium levels in the body. It may help prevent the formation of calcium oxalate stones, but it does not affect overall calcium levels.
D. Potassium citrate does not decrease urine output. It primarily works to reduce urine acidity and prevent stone formation.
Explanation
A. This statement is not correct. Increasing dairy product intake may provide calcium, which is important for overall health, but it is not a specific dietary modification to prevent struvite stones.
B. This is the correct answer. Struvite stones are composed of magnesium, ammonium, and phosphate. Limiting the intake of high-phosphorus foods can help prevent the formation of these stones.
C. Avoiding foods high in purines is more relevant to the prevention of uric acid stones, not struvite stones.
D. Limiting fluid intake is
not recommended for the prevention of struvite stones. Adequate fluid intake is essential in preventing stone formation.
Explanation
A. Allopurinol does not directly increase urine output. It is not a diuretic and is not used for that purpose.
B. Allopurinol does not dissolve existing kidney stones. It is primarily used to prevent the formation of uric acid stones, not to treat existing stones.
C. This is the correct answer. Allopurinol is a medication used to reduce the production of uric acid in the body. By lowering uric acid levels, it can help prevent the formation of uric acid stones.
D. Allopurinol does not increase the excretion of calcium. It is used specifically to address uric acid levels and prevent uric acid stone formation.
Explanation
A. This is the correct answer. After a ureteroscopy, the client may experience postoperative urinary retention due to swelling or irritation in the urethra or bladder. The nurse should monitor for signs of urinary retention and take appropriate measures to address it.
B. Hyperkalemia is not directly related to ureteroscopy. It may occur in certain medical conditions but is not a common complication of this procedure.
C. Hypertension is not directly related to ureteroscopy. While some clients with hypertension may be at increased risk for kidney stones, hypertension is not a common complication of the procedure itself.
D. Hypoglycemia is not related to ureteroscopy. It is a condition related to low blood sugar levels and is not a typical complication of kidney stone removal.
Explanation
A. Thiazide diuretics can lead to decreased calcium excretion in the urine, which may be beneficial for some clients with kidney stones. They are used to reduce the excretion of calcium and prevent the formation of calcium-based stones.
B. Hypernatremia is not directly related to thiazide diuretic use. Thiazide diuretics primarily affect sodium excretion in the urine, but they do not typically cause hypernatremia.
C. This is the correct answer. Thiazide diuretics can cause hypokalemia (low potassium levels) as they increase potassium excretion in the urine.
D. Thiazide diuretics do not cause hypermagnesemia. They do not have a significant effect on magnesium excretion in the urine.
Questions
Transurethral resection of the prostate
Explanation
A. Discharging a client on the same day of TURP surgery is not common due to the need for monitoring and management of postoperative complications.
B. A hospital stay of about a week is more extended than usual for TURP surgery, which typically requires a shorter stay.
C. This is the correct answer. Most clients who undergo TURP can expect to stay in the hospital for 2 to 3 days for close postoperative monitoring and management of any complications.
D. Discharging a client on the same day of surgery is not standard practice for TURP, as immediate postoperative monitoring is necessary.
Explanation
A. Educating the client about postoperative care instructions is essential, but it is not the primary responsibility related to informed consent.
B. This is the correct answer. The nurse's primary responsibility is to ensure that the client is adequately informed about the risks, benefits, and alternatives to the surgery and that they provide voluntary and informed consent. The nurse witnesses the client's signature on the consent form to verify that the client understands and agrees to the procedure.
C. Explaining the surgical procedure is part of the informed consent process, but witnessing the client's signature is the primary responsibility related to informed consent.
D. Ensuring the client is medically fit for the surgery is crucial, but it is not the primary responsibility related to informed consent.
Explanation
A. Administering pain relief may be necessary, but the nurse's first action should be to notify the healthcare provider about the client's severe pain and other concerning symptoms.
B. This is the correct answer. Severe lower abdominal pain, difficulty urinating, and the presence of blood clots in the urine may indicate postoperative complications after TURP. The nurse should notify the healthcare provider immediately for further evaluation and intervention.
C. Encouraging the client to drink more fluids may be helpful, but it is not the first action when the client experiences severe pain and other concerning symptoms.
D. Deep breathing exercises can help manage pain, but the nurse should first address the client's acute symptoms and notify the healthcare provider for appropriate intervention.
Explanation
A. This is the correct answer. TURP can cause temporary sexual dysfunction due to the proximity of the prostate to the nerves and blood vessels that control sexual function. However, in many cases, sexual function improves over time as the surgical site heals.
B. While sexual dysfunction can occur after TURP, it is not a common complication, and there are potential treatment options available.
C. TURP can have an impact on sexual function, and it is essential for the client to be aware of this possibility.
D. Sexual dysfunction after TURP is typically temporary and not a permanent outcome.
Explanation
A. Resuming regular activities immediately after discharge may not be advisable, as the client needs time to recover and heal from the surgical procedure.
B. While the client may need to limit certain activities, waiting for a week before resuming any activities is not necessary in most cases.
C. Avoiding all physical activities is not necessary, and it may lead to deconditioning and delayed recovery.
D. This is the correct answer. The client should gradually resume their regular activities as they tolerate, but they should avoid heavy lifting and strenuous exercises for a few weeks to promote healing and prevent complications after TURP.
Questions
Explanation
A. Increasing fluid intake may not be necessary before TURP surgery and could lead to over-distension of the bladder, making catheterization difficult.
B. Limiting fluid intake is not recommended as the client needs adequate hydration before surgery to support the body's normal functions.
C. This is the correct answer. Emptying the bladder completely before TURP surgery helps reduce the risk of infection and prevents complications during the procedure.
D. Kegel exercises are beneficial for pelvic floor muscle strengthening but are not specifically required before TURP surgery.
Explanation
A. Sharing personal experiences of other clients may not be appropriate, as each individual's experience is unique, and it may not alleviate the client's anxiety.
B. Avoiding discussing the surgical procedure can increase the client's anxiety, as they may feel uninformed and uncertain about the surgery.
C. While explaining the surgical procedure is important, listening to the client's concerns and providing emotional support are equally crucial in alleviating anxiety.
D. This is the correct answer. Actively listening to the client's concerns allows the nurse to understand their fears and provide appropriate emotional support, which can help alleviate anxiety before TURP surgery.
Explanation
A. This is the correct answer. Informing the healthcare provider about the client's anticoagulant medication is crucial before surgery, as it can affect the surgical plan and potential bleeding risks during TURP.
B. Withholding all medications, including anticoagulants, should only be done under the direction of the healthcare provider and anesthesia team. Abruptly stopping anticoagulants can lead to significant medical risks.
C. Continuing the anticoagulant as prescribed may pose a bleeding risk during surgery, so it is essential to involve the healthcare provider in the decision.
D. Administering a blood-thinning agent to counteract the anticoagulant effects is not appropriate and can lead to complications. The healthcare provider should decide on the management of anticoagulation therapy before surgery.
Explanation
A. General anesthesia may not be necessary for TURP surgery, as it is typically performed using regional anesthesia like spinal or epidural anesthesia.
B. This is the correct answer. TURP surgery is usually done using spinal anesthesia, which numbs the lower part of the body, allowing the client to remain awake during the procedure while avoiding pain and discomfort.
C. The of anesthesia is usually determined before the day of the surgery based on the client's medical history and surgical plan.
D. Local anesthesia alone may not be sufficient for pain relief during TURP surgery, as it involves a more extensive procedure that requires regional anesthesia to achieve better pain control.
Explanation
A. While the client's marital status and family support are important aspects of the client's life, they are not directly related to the client's readiness for TURP surgery.
B. The client's dietary preferences and meal schedule are important for overall health but are not the priority during the preoperative assessment for TURP.
C. This is the correct answer. The nurse should prioritize assessing the client's allergies and medication history to identify any potential risks or adverse reactions during the surgical procedure and anesthesia.
D. The client's educational background and employment status may not be directly relevant to TURP surgery and are not the priority during the preoperative assessment.
Explanation
A. Erectile dysfunction may be a concern after TURP, but it is not the most common postoperative complication.
B. Incontinence can occur after TURP, but it is not the most common postoperative complication.
C. This is the correct answer. Hematuria, or blood in the urine, is the most common postoperative concern for clients undergoing TURP. It is expected for a short period after the surgery and should gradually improve.
D. Retrograde ejaculation may occur after TURP, but it is not the most common postoperative complication.
Explanation
A. Keeping the catheter in place for at least two weeks after TURP is not typical. The duration of catheterization varies depending on the client's recovery and ability to urinate.
B. The catheter is often necessary after TURP to drain the bladder and prevent urinary retention. It is usually removed once the client can urinate normally without difficulty.
C. This is the correct answer. The catheter will remain in place until the client can urinate normally without difficulty, which typically occurs once the swelling and inflammation in the urinary tract subside.
D. Removing the catheter the day after surgery may not be appropriate, as the client may still have difficulty urinating due to the effects of the surgery. The removal of the catheter is based on the client's ability to urinate comfortably and effectively.
Questions
Explanation
A. While anesthesia can cause irritation, it is not the primary reason for removing dentures before TURP surgery.
B. This is the correct answer. Removing dentures reduces the risk of aspiration (inhaling fluids or secretions) during surgery, which can lead to serious complications.
C. While some hospitals may have policies about removing dentures, the main concern here is the safety and prevention of aspiration.
D. Leaving dentures in place during surgery may not interfere with surgical instruments directly, but the main concern is the risk of aspiration.
Explanation
A. This is the correct answer. Bladder perforation is a significant complication that requires immediate attention. The nurse should inform the surgical team to address the situation promptly.
B. Notifying the client's family about the complication is not the immediate action. The priority is to inform the surgical team and manage the situation.
C. While documentation is essential, it is not the immediate action required in this critical situation.
D. Administering pain medication may be necessary, but the priority is to address the bladder perforation and involve the surgical team to manage the complication.
Explanation
A. Maintaining strict fluid restrictions may not be necessary during TURP surgery and can lead to dehydration.
B. Preventing dehydration is essential, but the primary reason for fluid intake and output monitoring is to detect potential complications related to fluid overload or imbalance.
C. While proper irrigation of the surgical site is essential, fluid intake and output monitoring serve a broader purpose of assessing overall fluid balance and preventing complications.
D. This is the correct answer. Monitoring fluid intake and output during TURP surgery allows the nurse to assess for signs of fluid overload or imbalance, which can occur due to irrigation fluids and potential bleeding.
Explanation
A. Administering pain medication may not be appropriate for these symptoms, as the client's condition requires immediate attention and assessment.
B. This is the correct answer. The sudden onset of tachycardia, hypotension, and confusion indicates a potential complication or adverse reaction that requires immediate intervention from the surgical and anesthesia teams.
C. Reassuring the client is important, but it is not the priority when the client is experiencing concerning symptoms.
D. Initiating a rapid infusion of intravenous fluids may not be appropriate without a proper assessment and evaluation of the client's condition. The priority is to inform the surgical and anesthesia teams to address the situation promptly.
Explanation
A. The prone position with the abdomen elevated is not the appropriate position for TURP surgery.
B. The supine position with the legs elevated is not the appropriate position for TURP surgery.
C. This is the correct answer. The lithotomy position with the feet in stirrups is the standard position for TURP surgery, as it provides access to the urinary tract for the procedure.
D. The lateral position with the affected side up is not the appropriate position for TURP surgery, as it does not provide the necessary access to the urinary tract.
Questions
Explanation
A. While anesthesia can cause irritation, it is not the primary reason for removing dentures before TURP surgery.
B. This is the correct answer. Removing dentures reduces the risk of aspiration (inhaling fluids or secretions) during surgery, which can lead to serious complications.
C. While some hospitals may have policies about removing dentures, the main concern here is the safety and prevention of aspiration.
D. Leaving dentures in place during surgery may not interfere with surgical instruments directly, but the main concern is the risk of aspiration.
Explanation
A. This is the correct answer. Bladder perforation is a significant complication that requires immediate attention. The nurse should inform the surgical team to address the situation promptly.
B. Notifying the client's family about the complication is not the immediate action. The priority is to inform the surgical team and manage the situation.
C. While documentation is essential, it is not the immediate action required in this critical situation.
D. Administering pain medication may be necessary, but the priority is to address the bladder perforation and involve the surgical team to manage the complication.
Explanation
A. Maintaining strict fluid restrictions may not be necessary during TURP surgery and can lead to dehydration.
B. Preventing dehydration is essential, but the primary reason for fluid intake and output monitoring is to detect potential complications related to fluid overload or imbalance.
C. While proper irrigation of the surgical site is essential, fluid intake and output monitoring serve a broader purpose of assessing overall fluid balance and preventing complications.
D. This is the correct answer. Monitoring fluid intake and output during TURP surgery allows the nurse to assess for signs of fluid overload or imbalance, which can occur due to irrigation fluids and potential bleeding.
Explanation
A. Administering pain medication may not be appropriate for these symptoms, as the client's condition requires immediate attention and assessment.
B. This is the correct answer. The sudden onset of tachycardia, hypotension, and confusion indicates a potential complication or adverse reaction that requires immediate intervention from the surgical and anesthesia teams.
C. Reassuring the client is important, but it is not the priority when the client is experiencing concerning symptoms.
D. Initiating a rapid infusion of intravenous fluids may not be appropriate without a proper assessment and evaluation of the client's condition. The priority is to inform the surgical and anesthesia teams to address the situation promptly.
Explanation
A. The prone position with the abdomen elevated is not the appropriate position for TURP surgery.
B. The supine position with the legs elevated is not the appropriate position for TURP surgery.
C. This is the correct answer. The lithotomy position with the feet in stirrups is the standard position for TURP surgery, as it provides access to the urinary tract for the procedure.
D. The lateral position with the affected side up is not the appropriate position for TURP surgery, as it does not provide the necessary access to the urinary tract.
Questions
Explanation
A. This is the correct answer. The priority intervention for suspected UTI is to administer prescribed antibiotics to treat the infection and prevent its spread.
B. While increased fluid intake is essential, it is not the priority when the client is exhibiting signs of a UTI. Antibiotics should be given to address the infection promptly.
C. Monitoring vital signs and urine output is important, but the priority is to treat the infection with antibiotics.
D. Applying warm compresses to the abdomen may provide some comfort but does not address the underlying UTI.
Explanation
A. While encouraging fluid intake is important, severe pain during urination and inability to void after TURP surgery require further evaluation and intervention by the healthcare provider.
B. This is the correct answer. Severe pain and inability to void after TURP surgery may indicate a complication or urinary retention that requires immediate attention from the healthcare provider.
C. Documenting the client's complaints is essential, but the nurse should not delay notifying the healthcare provider about the client's symptoms.
D. Instructing the client to perform Kegel exercises is not the priority when the client is experiencing severe pain and inability to void after TURP surgery. The client's symptoms require prompt evaluation and intervention.
Explanation
A. While maintaining hydration is important, the priority is to address the continuous bright red bleeding from the urinary catheter by notifying the healthcare provider immediately.
B. Clamping the catheter may obstruct urine flow and worsen the situation. The nurse should not intervene without healthcare provider guidance.
C. Administering fresh frozen plasma may be necessary in some situations, but it is not the immediate action for addressing continuous bleeding from the urinary catheter.
D. This is the correct answer. Continuous bright red bleeding from the urinary catheter after TURP surgery may indicate bleeding complications that require immediate intervention and evaluation by the healthcare provider.
Explanation
A. Administering diuretics may be necessary, but the priority is to improve respiratory distress and oxygenation by elevating the head of the bed and providing oxygen therapy.
B. This is the correct answer. The priority intervention for signs of fluid overload is to improve respiratory function and oxygenation by elevating the head of the bed and providing oxygen therapy as needed.
C. Encouraging the client to limit fluid intake is not the priority when the client is experiencing signs of fluid overload. The focus should be on improving respiratory function.
D. Restricting sodium intake may be appropriate in some cases, but the priority is to address the respiratory distress associated with fluid overload.
Explanation
A. This is the correct answer. Encouraging the client to perform pelvic floor exercises, also known as Kegel exercises, can help strengthen the pelvic floor muscles and improve urinary control after TURP surgery.
B. Applying a condom catheter may not address the underlying issue of urinary incontinence after TURP surgery. It is more appropriate for managing male urinary incontinence in other contexts.
C. Inserting an indwelling urinary catheter for continuous drainage is not the first-line intervention for urinary incontinence after TURP surgery. It may increase the risk of complications such as infection and should be used judiciously.
D. Administering an anticholinergic medication may be appropriate in some cases, but it is not
the primary intervention for urinary incontinence after TURP surgery. Pelvic floor exercises are a non-pharmacological approach to address the issue.
Explanation
A. Assessing pain level and administering pain medication is important, but the priority during the immediate postoperative period is to monitor vital signs and assess for signs of hemorrhage or other complications.
B. This is the correct answer. Monitoring vital signs and assessing for signs of hemorrhage, such as continuous bright red bleeding, tachycardia, and hypotension, is essential to detect and address any complications promptly.
C. Evaluating the client's urinary output and catheter patency is important but may not be the immediate priority if there are concerns about hemorrhage or other complications.
D. Assessing the client's surgical incision for signs of infection is essential, but it may not be the immediate priority during the immediate postoperative period. The focus should be on assessing vital signs and for signs of bleeding or other complications.
Questions
Explanation
A. Resuming driving the day after TURP surgery may not be safe, as the client may still be recovering from the effects of anesthesia and the procedure.
B. This is the correct answer. The client should avoid driving for at least six to eight weeks after TURP surgery to ensure proper healing and prevent complications.
C. The removal of the catheter may not be the only factor affecting the client's ability to drive safely. The nurse should advise the client to wait for six to eight weeks before resuming driving.
D. Avoiding driving for just one week may not be sufficient for proper recovery after TURP surgery.
Explanation
A. This is the correct answer. Administering pain medication as prescribed by the healthcare provider is the most appropriate intervention to manage postoperative pain after TURP surgery.
B. Deep breathing exercises are helpful for preventing respiratory complications, but they may not be sufficient for managing postoperative pain.
C. Applying a heating pad to the surgical site is not recommended as it may increase the risk of bleeding and other complications.
D. While distractions can provide some comfort, they may not be enough to effectively manage postoperative pain. Pain medication is the primary intervention.
Explanation
A. Cleaning the catheter with alcohol wipes may irritate the urethra and increase the risk of infection. The catheter should not be cleaned with alcohol wipes.
B. Flushing the catheter with sterile water may introduce pathogens into the urinary tract and increase the risk of infection. The catheter should not be flushed with sterile water.
C. This is the correct answer. Keeping the catheter bag below the level of the bladder prevents urine from flowing back into the bladder, reducing the risk of infection.
D. The catheter should not be replaced weekly unless there is a specific indication for catheter change. Catheter replacement should be done according to the healthcare provider's instructions and protocols.
Explanation
A. While erectile dysfunction can occur after TURP surgery, it is not accurate to describe it as a "common" complication. The actual incidence varies among individuals.
B. This is the correct answer. Erectile dysfunction is a possible complication after TURP surgery due to the proximity of nerves involved in erectile function. However, it is often temporary and resolves within a few months as the body heals.
C. TURP surgery can have an impact on erectile function due to its proximity to the nerves and structures involved in sexual function.
D. It is not appropriate for the nurse to dismiss the client's concerns. Erectile dysfunction is a valid concern for many clients undergoing TURP surgery.
Explanation
A. Increasing fluid intake is important, but excessive fluid consumption may put additional stress on the bladder and cause discomfort. The client should maintain adequate fluid intake without overhydration.
B. Limiting protein intake is not typically necessary after TURP surgery unless there are specific medical reasons for such restrictions.
C. This is not an appropriate recommendation. Foods that are high in fiber and whole grains are beneficial for overall health, including gastrointestinal function.
D. This is the correct answer. Consuming caffeine and alcohol in moderation is recommended after TURP surgery. These substances can act as diuretics, increasing the need to urinate and potentially causing discomfort for the client.
Explanation
A. Encouraging the client to delay voiding may lead to urinary retention and increase the risk of complications. This is not an appropriate intervention for urinary urgency and frequency after TURP surgery.
B. Limiting fluid intake may lead to dehydration and affect the overall health of the client. Adequate fluid intake is important for proper healing and preventing complications after TURP surgery.
C. This is the correct answer. Anticholinergic medications can help reduce urinary urgency and frequency by relaxing the bladder muscles and reducing bladder spasms.
D. Kegel exercises are helpful for strengthening the pelvic floor muscles but may not be the best intervention for addressing urinary urgency and frequency after TURP surgery. Anticholinergic medications are more appropriate in this case.
A nurse is providing preoperative education to a client scheduled for a Transurethral Resection of the Prostate (TURP). The client asks, "What is the purpose of this procedure?" Which response by the nurse is most appropriate?
Explanation
A) This response is not accurate. TURP is primarily performed for benign prostatic hyperplasia (BPH) or prostate enlargement and not for prostate cancer removal.
B) This is the correct answer. TURP is a surgical procedure that involves removing a portion of the prostate gland to alleviate urinary symptoms caused by BPH, such as urinary frequency, urgency, and difficulty in urination.
C) This statement is not accurate. TURP is a therapeutic procedure, not a diagnostic one.
D) This response is incorrect. TURP is a surgical procedure and does not involve catheter insertion for drainage.
A client scheduled for a TURP expresses concerns about potential complications after the surgery. Which complication should the nurse prioritize when providing preoperative education?
Explanation
A) This is the correct answer. Infection is a significant concern after TURP surgery due to the potential introduction of bacteria during the procedure or through catheterization. It can lead to urinary tract infections or systemic infections if not managed promptly.
B) Anemia may be a concern in some cases, but infection is a more immediate and potentially serious complication to address.
C) Weight gain and muscle weakness are not typical complications associated with TURP surgery.
A nurse is providing discharge instructions to a client after TURP surgery. The client asks, "When can I resume normal activities like heavy lifting and strenuous exercises?" What is the nurse's best response?
Explanation
A) Resuming heavy lifting and strenuous exercises immediately after TURP surgery can lead to complications such as bleeding or wound disruption.
B) This is the correct answer. The client should avoid heavy lifting and strenuous exercises for at least six to eight weeks after surgery to allow for proper healing and to prevent complications.
C) Resuming heavy lifting and strenuous exercises just two days after surgery is not recommended as the body needs time to heal.
D) Avoiding heavy lifting and strenuous exercises for one week may not be sufficient for proper healing after TURP surgery.
Exams on Genito-Urinary System Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Introduction to genitourinary disorders
- The genitourinary system, encompassing the urinary and reproductive systems, plays a critical role in maintaining fluid balance, eliminating waste products, and facilitating human reproduction.
- Genitourinary disorders encompass a spectrum of conditions affecting the kidneys, bladder, ureters, reproductive organs, and associated structures.
- In the realm of nursing, a comprehensive understanding of genitourinary disorders is essential for assessment, diagnosis, treatment, and patient education.
- This Study Guide delves into various genitourinary disorders, offering nursing students and professionals a comprehensive resource to enhance their knowledge and clinical competence.
- By addressing key concepts, assessment techniques, therapeutic interventions, and patient-centered care strategies, this guide aims to equip nurses with the tools to excel in managing genitourinary disorders and promoting positive patient outcomes.
Dialysis
Introduction to dialysis
- Dialysis is a process of removing waste and excess fluid from the blood when the kidneys are not able to do so adequately.
- It is a life-saving treatment for people with end-stage renal disease (ESRD) or acute kidney injury (AKI). There are two main types of dialysis: hemodialysis and peritoneal dialysis.
- Both types have advantages and disadvantages, and the depends on various factors such as patient preference, medical condition, availability, and cost.
- Dialysis is a life-sustaining medical procedure that serves as a vital lifeline for individuals with impaired kidney function.
- Its significance lies in its ability to replicate the essential functions of the kidneys, allowing patients to maintain a relatively normal life despite the challenges posed by kidney failure or chronic kidney disease (CKD).
- This revolutionary medical technique has transformed the landscape of nephrology, significantly enhancing the quality of life and longevity of countless patients worldwide.
- The kidneys play a critical role in filtering waste products and excess fluids from the bloodstream.
- However, when these essential organs become compromised due to various factors such as diabetes, hypertension, or genetic disorders, they lose their ability to function optimally.
- This often results in a dangerous accumulation of toxins and fluids in the body, leading to a myriad of life-threatening complications.
- Dialysis serves as an artificial means to replace the lost kidney function, ensuring that waste products are efficiently removed, and fluid balance is maintained within safe limits.
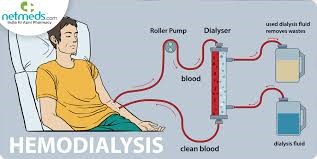
Indications for dialysis
- Dialysis is indicated for patients who have irreversible kidney failure or acute kidney injury that cannot be managed by conservative measures.
- Some of the common indications for dialysis are:
- Uremia: a condition of high levels of urea and other waste products in the blood that cause symptoms such as nausea, vomiting, fatigue, confusion, seizures, coma, and bleeding.
- Volume overload: a condition of excess fluid in the body that causes symptoms such as edema, shortness of breath, hypertension, heart failure, and pulmonary edema.
- Electrolyte imbalance: a condition of abnormal levels of electrolytes such as sodium, potassium, calcium, phosphate, and bicarbonate in the blood that cause symptoms such as muscle weakness, arrhythmias, tetany, seizures, and acidosis or alkalosis.
- Intoxication: a condition of poisoning by drugs or toxins that are dialyzable such as ethylene glycol, methanol, salicylates, lithium, and some antibiotics.
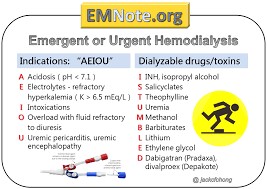
Hemodialysis
- Hemodialysis is a type of dialysis that uses an artificial kidney (dialyzer) to filter the blood outside the body.
- The blood is pumped from the patient's vascular access (a surgically created connection between an artery and a vein) to the dialyzer, where it passes through a semipermeable membrane that allows waste and fluid to move across but retains blood cells and proteins.
- The dialysate (a solution of water and electrolytes) flows on the opposite side of the membrane and creates a concentration gradient that facilitates the removal of waste and fluid from the blood.
- The cleansed blood is then returned to the patient's circulation.
- Hemodialysis is usually performed three times a week for about four hours per session in a dialysis center or hospital.
- However, some patients may opt for home hemodialysis or more frequent or longer sessions depending on their preference and medical condition.
- Hemodialysis requires careful monitoring of vital signs, fluid balance, electrolytes, blood pressure, anticoagulation, and complications such as hypotension, cramps, infection, clotting, air embolism, and hemolysis.

Peritoneal dialysis
- Peritoneal dialysis is a type of dialysis that uses the peritoneum (the lining of the abdominal cavity) as a natural filter to remove waste and fluid from the blood.
- The peritoneum is rich in blood vessels and has a large surface area that allows diffusion of waste and fluid across its membrane.
- A catheter is inserted into the peritoneal cavity through a small incision in the abdomen and connected to a bag of dialysate. The dialysate is infused into the peritoneal cavity and left there for a certain period of time (dwell time) during which waste and fluid move from the blood to the dialysate. The dialysate is then drained out of the peritoneal cavity and replaced with fresh dialysate.
- Peritoneal dialysis can be performed at home or at work by the patient or a caregiver.
- There are two main types of peritoneal dialysis: continuous ambulatory peritoneal dialysis (CAPD) and automated peritoneal dialysis (APD).
- CAPD involves four to five exchanges of dialysate per day, each lasting about 30 to 40 minutes. APD involves using a machine (cycler) that performs several exchanges of dialysate overnight while the patient sleeps.
- Peritoneal dialysis requires regular assessment of weight, fluid balance, electrolytes, glucose, infection, catheter function, and complications such as peritonitis, leakage, hernia, malnutrition, and encapsulating peritoneal sclerosis.
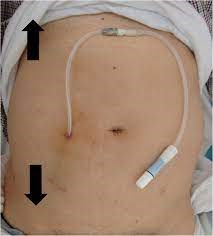
Patient Education and Lifestyle Modification
- Patients undergoing dialysis need to receive education and support on how to cope with their condition and maintain their quality of life. Some of the topics that need to be covered are:
- Diet: Patients need to follow a diet that is low in sodium, potassium, phosphorus, and fluid to prevent complications such as hypertension, hyperkalemia, hyperphosphatemia, and volume overload. They also need to consume adequate protein, calories, vitamins, and minerals to prevent malnutrition and anemia. A registered dietitian can help plan a suitable diet for each patient based on their blood tests and preferences.
- Medications: Patients need to take medications as prescribed by their doctor to treat their underlying kidney disease and associated conditions such as hypertension, diabetes, anemia, bone disease, and infection. They also need to avoid certain medications that are nephrotoxic or not dialyzable such as nonsteroidal anti-inflammatory drugs (NSAIDs), metformin, and some antibiotics. They need to inform their doctor and pharmacist of all the medications they are taking, including over-the-counter drugs, herbal remedies, and supplements.
- Fluid management: Patients need to monitor their fluid intake and output and weigh themselves daily to prevent fluid overload or dehydration. They need to limit their fluid intake to the amount prescribed by their doctor, which is usually the urine output plus 500 to 1000 ml per day. They also need to avoid foods that are high in water content such as soups, ice cream, fruits, and vegetables. They need to report any signs of fluid imbalance such as edema, shortness of breath, dry mouth, thirst, or dizziness to their doctor or nurse.
- Exercise: Patients need to engage in regular physical activity to improve their cardiovascular health, muscle strength, mood, and energy level. They need to consult with their doctor or physiotherapist before starting an exercise program and choose activities that are suitable for their condition and preferences. They need to avoid exercises that involve high impact, heavy lifting, or contact sports that may injure their vascular access or peritoneal catheter. They need to drink enough fluids before, during, and after exercise to prevent dehydration.
- Smoking cessation: Patients need to quit smoking as it increases the risk of cardiovascular disease, infection, and poor wound healing. They need to seek help from their doctor or nurse on how to quit smoking and use nicotine replacement therapy or other medications if needed. They also need to avoid exposure to secondhand smoke.
- Alcohol consumption: Patients need to limit their alcohol intake as it may interfere with their medications, fluid balance, electrolytes, and blood pressure. They need to follow the guidelines of no more than one drink per day for women and two drinks per day for men. One drink is equivalent to 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of liquor. They also need to avoid binge drinking or drinking on an empty stomach.
- Sexual function: Patients may experience changes in their sexual function and desire due to hormonal imbalance, fatigue, depression, anxiety, body image issues, or medication side effects. They need to communicate with their partner about their feelings and needs and seek counseling or medical treatment if needed. They also need to practice safe sex and use contraception if they do not want to get pregnant or father a child.

Complications of dialysis
- Dialysis is a life-saving treatment for patients with end-stage renal disease, but it also carries some risks and potential complications.
- Some of the common complications of dialysis are:
- Hypotension: This is a drop in blood pressure that can occur during or after dialysis, especially if too much fluid is removed or the patient has a low blood volume. Symptoms include dizziness, nausea, vomiting, cramps, headache, chest pain, and shortness of breath.
- To prevent or treat hypotension, the nurse should monitor the patient's vital signs, adjust the fluid removal rate, administer saline or hypertonic solutions, elevate the patient's legs, and stop or slow down the dialysis if needed.
- Muscle cramps: These are painful spasms of the muscles that can occur during or after dialysis, usually in the legs or feet. The exact cause is not clear, but it may be related to fluid shifts, electrolyte imbalances, or nerve irritation.
- To prevent or treat muscle cramps, the nurse should ensure adequate hydration, avoid excessive fluid removal, correct electrolyte abnormalities, massage the affected muscles, apply heat or cold packs, and administer antispasmodic medications if prescribed.
- Infection: This is a serious complication that can affect the access site (fistula, graft, or catheter), the bloodstream, or other organs. Infection can be caused by bacteria, fungi, or viruses that enter through the access site or during dialysis. Symptoms include fever, chills, redness, swelling, pain, pus, drainage, or foul odor at the access site, and signs of sepsis or organ dysfunction.
- To prevent or treat infection, the nurse should follow strict aseptic technique when handling the access site and dialysis equipment, inspect and clean the access site regularly, change dressings as needed, administer antibiotics or antifungal medications if prescribed, and monitor for signs of infection and report them promptly.
- Anaemia: This is a low level of red blood cells (RBCs) or haemoglobin in the blood that can result from chronic kidney disease or dialysis. Anaemia can cause fatigue, weakness, pallor, shortness of breath, chest pain, and increased risk of cardiovascular complications.
- To prevent or treat anaemia, the nurse should monitor the patient's haematocrit and haemoglobin levels regularly
- administer erythropoietin-stimulating agents (ESAs) or iron supplements if prescribed
- educate the patient on dietary sources of iron and folate.
- Bone and mineral disorders: These are abnormalities in calcium, phosphorus, parathyroid hormone (PTH), and vitamin D metabolism that can occur in patients with chronic kidney disease or dialysis. These disorders can cause bone loss, fractures, joint pain, itching, calcification of soft tissues and blood vessels (vascular calcification), and increased risk of cardiovascular complications.
- To prevent or treat bone and mineral disorders, the nurse should monitor the patient's serum calcium, phosphorus, PTH, and vitamin D levels regularly. They should also administer phosphate binders, calcium supplements, vitamin D analogues, or calcimimetics if prescribed.
- They should educate the patient on dietary restrictions of phosphorus and calcium.
- Hypotension: This is a drop in blood pressure that can occur during or after dialysis, especially if too much fluid is removed or the patient has a low blood volume. Symptoms include dizziness, nausea, vomiting, cramps, headache, chest pain, and shortness of breath.
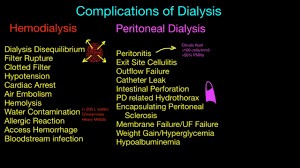
Summary
- Dialysis is a treatment that replaces some of the functions of the kidneys by removing waste and excess fluid from the blood.
- There are two main types of dialysis: haemodialysis and peritoneal dialysis.
- Haemodialysis uses an artificial kidney (dialyzer) that filters the blood through a semipermeable membrane.
- Peritoneal dialysis uses the lining of the abdomen (peritoneum) as a natural filter that exchanges fluid and solutes with a dialysate solution.
- Both types of dialysis require an access site that allows blood or fluid to flow in and out of the body.
- The dialysis modality depends on various factors such as:
- patient preference,
- medical condition,
- lifestyle,
- availability,
- cost.
- Nurses play a vital role in ensuring the safety, efficacy, and quality of life of dialysis patients by providing pre-dialysis assessment, intradialytic intervention, post-dialysis evaluation, psychosocial support, education, and infection control.

Conclusion
- Dialysis is a complex and challenging treatment that requires careful nursing care and monitoring.
- Two primary types of dialysis, hemodialysis, and peritoneal dialysis, have emerged as effective approaches, offering patients based on their individual medical conditions and lifestyle preferences.
- Additionally, the advent of home-based and more patient-friendly dialysis modalities has provided a sense of independence and empowerment for individuals undergoing treatment.
- However, dialysis also presents challenges that must be acknowledged and addressed. Patients face potential side effects, lifestyle adjustments, and emotional burdens due to their chronic medical conditions.
- Furthermore, the financial implications of long-term dialysis can be burdensome, highlighting the need for equitable access to healthcare and affordable treatment options.
- Nurses play a vital role in ensuring the safety, efficacy, and quality of life of dialysis patients by providing pre-dialysis assessment, intradialytic intervention, post-dialysis evaluation, psychosocial support, education, and infection control.
- Nurses should also be aware of the potential complications of dialysis and how to prevent or manage them effectively.
Nephrotic Syndrome
Introduction to Nephrotic Syndrome
- Nephrotic syndrome is a condition that results from damage to the glomeruli, the tiny blood vessels in the kidneys that filter waste and excess water from the blood.
- Normally, the glomeruli keep blood protein (mainly albumin) from leaking into the urine, as it is needed to maintain the right amount of fluid in the body.
- When the glomeruli are damaged, they allow too much protein to escape into the urine, leading to nephrotic syndrome.
- Nephrotic syndrome can be caused by many diseases and conditions that affect the kidneys, such as:
- Diabetes
- lupus
- amyloidosis
- minimal change disease
- focal segmental glomerulosclerosis
- membranous nephropathy.
- Nephrotic syndrome is a kidney disorder that causes your body to lose too much protein in your urine. It can lead to swelling, high cholesterol, blood clots, infections, and kidney failure.
- The underlying cause of nephrotic syndrome determines the prognosis and treatment of the condition.

Clinical Manifestations and Symptoms
The main signs and symptoms of nephrotic syndrome are:
- Proteinuria: The presence of large amounts of protein in the urine (>3.5 g per day or >40 mg per hour in children), which can make the urine foamy or frothy.
- Hypoalbuminemia: The low level of albumin in the blood (<3.5 g/dL), which can cause fluid to leak out of the blood vessels into the tissues.
- Edema: The swelling of body parts due to fluid accumulation, especially in the ankles, feet, legs, face, and around the eyes. Edema can also affect the abdomen (ascites) and the lungs (pleural effusion).
- Hyperlipidemia: The high level of cholesterol and triglycerides in the blood, which can increase the risk of cardiovascular disease.
- Weight gain: The increase in body weight due to fluid retention and increased fat deposits.
- Fatigue: The feeling of tiredness and weakness due to low protein levels and anemia.
- Loss of appetite: The reduced desire to eat due to nausea, abdominal discomfort, or altered taste sensation.
- Blood clots: The formation of clots in the blood vessels due to loss of proteins that prevent clotting, such as antithrombin III. Blood clots can cause serious complications such as pulmonary embolism (clot in the lung) or deep vein thrombosis (clot in the leg).
- Infections: The increased susceptibility to infections due to loss of immunoglobulins (antibodies) and complement proteins that fight against bacteria and viruses.
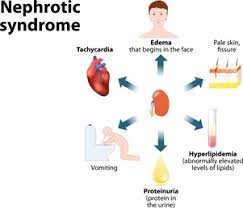
Diagnostic Evaluation
The diagnosis of nephrotic syndrome is based on:
- Urine test: To check for proteinuria, which is usually confirmed by a 24-hour urine collection or a spot urine sample with a protein-to-creatinine ratio.
- Blood test: To measure albumin, cholesterol, triglycerides, blood urea nitrogen (BUN), creatinine, electrolytes, glucose, and complete blood count (CBC). These tests can help assess the severity of nephrotic syndrome and its complications.
- Kidney biopsy: To obtain a small sample of kidney tissue for microscopic examination. This can help identify the cause and type of glomerular damage and guide treatment decisions.
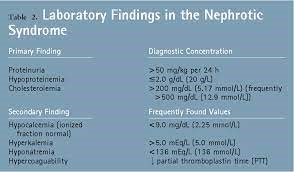
Management and Treatment
The treatment of nephrotic syndrome depends on:
- The underlying cause: Some causes of nephrotic syndrome are treatable with specific medications or interventions, such as diabetes (with insulin or oral hypoglycemic agents), lupus (with corticosteroids or immunosuppressants), or blood clot (with anticoagulants).
- The severity of symptoms: Some symptoms of nephrotic syndrome are manageable with supportive measures, such as edema (with diuretics or fluid restriction), hyperlipidemia (with statins or dietary modification), or infections (with antibiotics or prophylaxis).
- The response to treatment: Some patients with nephrotic syndrome may respond well to corticosteroids or immunosuppressants, which can reduce inflammation and proteinuria. Others may require more aggressive treatments such as plasmapheresis (removal of plasma from the blood) or dialysis (removal of waste products from the blood).
The management of nephrotic syndrome involves both non-pharmacological and pharmacological approaches. Here are the key aspects of treatment:
- Non-pharmacological Management:
a. Dietary Modifications: Reducing salt intake can help manage edema by minimizing fluid retention. A low-sodium diet is often recommended. Additionally, dietary changes to control cholesterol and triglyceride levels may be advised.
b. Fluid Management: In some cases, fluid intake may need to be restricted to prevent fluid overload and further edema.
c. Rest and Physical Activity: Adequate rest and appropriate levels of physical activity can help manage symptoms and promote overall well-being.
d. Infection Prevention: Since nephrotic syndrome can increase the risk of infections, especially in children, steps to prevent infections such as vaccinations and hygiene measures are essential.
- Pharmacological Treatment:
a. Corticosteroids: Corticosteroids, such as prednisone, are the mainstay of treatment for many cases of nephrotic syndrome. They help reduce inflammation in the kidneys, which can lead to decreased proteinuria and improved kidney function.
b. Immunosuppressants: In cases where corticosteroids alone are not effective, or if the underlying cause of nephrotic syndrome is an immune-related condition, immunosuppressive medications like cyclophosphamide or mycophenolate mofetil may be prescribed to suppress the immune system and reduce kidney inflammation.
c. Diuretics: Diuretics, commonly known as water pills, may be used to help control edema by promoting urine output and reducing fluid retention.
d. ACE Inhibitors or ARBs: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are blood pressure medications that also have protective effects on the kidneys. They can help reduce proteinuria and slow the progression of kidney damage.
e. Statins: Statins may be prescribed to manage elevated cholesterol levels in nephrotic syndrome.
- Treatment of Complications:
a. Blood Clot Prevention: Individuals with nephrotic syndrome are at an increased risk of blood clot formation. Medications to prevent blood clots, such as anticoagulants, may be prescribed when necessary.
b. Treatment of Infections: Prompt treatment of infections is essential to prevent complications and exacerbation of kidney damage.
- Monitoring and Follow-up:
Regular check-ups with a healthcare provider are crucial to monitor kidney function, blood pressure, and response to treatment. Adjustments to the treatment plan may be made based on the individual's condition and response to therapy.

Nursing Care and Patient Education
The nursing care and patient education for nephrotic syndrome include:
- Monitoring vital signs, especially blood pressure and weight, to detect changes in fluid status and cardiovascular risk.
- Assessing urine output and appearance, to evaluate proteinuria and renal function.
- Measuring edema, using a tape measure or a pitting scale, to monitor fluid retention and response to diuretics.
- Checking laboratory results, such as albumin, cholesterol, BUN, creatinine, and electrolytes, to identify abnormalities and complications.
- Administering medications, such as corticosteroids, immunosuppressants, diuretics, statins, anticoagulants, or antibiotics, as prescribed by the physician. Monitoring for side effects and adverse reactions, such as infection, bleeding, or hyperglycemia.
- Providing dietary education, such as limiting sodium intake (to <2 g per day), reducing saturated fat and cholesterol intake (to <7% and <200 mg per day, respectively), increasing protein intake (to 0.8-1 g per kg per day), and avoiding alcohol and caffeine. Encouraging adequate fluid intake (to 1.5 L per day or as prescribed).
- Promoting skin care, such as applying moisturizers, avoiding scratching, and preventing pressure ulcers. Educating the patient on how to prevent skin infections and report signs of infection, such as redness, warmth, swelling, or pus.
- Encouraging physical activity, such as walking, swimming, or cycling, to improve circulation, muscle strength, and mood. Advising the patient to avoid strenuous exercise or activities that increase the risk of injury or bleeding.
- Providing emotional support, such as listening to the patient's concerns, fears, and frustrations. Offering reassurance, information, and resources. Referring the patient to a counselor or a support group if needed.

Summary
- Nephrotic syndrome is a kidney disorder that causes excessive protein loss in the urine.
- It can lead to swelling, high cholesterol, blood clots, infections, and kidney failure.
- It can be caused by many diseases and conditions that damage the glomeruli. The diagnosis is based on urine test, blood test, and kidney biopsy.
- The treatment depends on the underlying cause, the severity of symptoms, and the response to treatment.
- The nursing care and patient education focus on monitoring vital signs, urine output, edema, and laboratory results; administering medications; providing dietary education; promoting skin care; encouraging physical activity; and providing emotional support.
- Nephrotic syndrome is a multifaceted kidney disorder with diverse underlying causes and complex clinical manifestations.
- Early detection, accurate diagnosis, and timely and appropriate intervention are crucial in mitigating its impact and preventing long-term complications.
- Ongoing research and advances in treatment modalities offer hope for improved outcomes and quality of life for individuals living with nephrotic syndrome.
Conclusion
- Nephrotic syndrome is a complex and potentially serious kidney disorder characterized by the abnormal excretion of protein in the urine, low levels of proteins in the blood, edema (swelling), and elevated cholesterol and triglyceride levels.
- It can affect individuals of all ages, but it is more prevalent in children, particularly between the ages of 2 and 6.
- The condition results from damage to the glomeruli, which are the tiny filtering units within the kidneys responsible for removing waste products and excess fluids from the blood.
- Various underlying causes can lead to nephrotic syndrome, including primary glomerular diseases such as minimal change disease, focal segmental glomerulosclerosis, and membranous nephropathy, as well as secondary causes like diabetes, lupus, and certain infections.
- Clinically, nephrotic syndrome presents with hallmark symptoms such as significant edema, particularly around the eyes, ankles, and feet, along with foamy urine due to the excessive protein loss.
- Patients may also experience fatigue, weight gain, and a heightened risk of infections and blood clots.
- Diagnosis is based on a combination of clinical presentation, urine analysis revealing proteinuria, and blood tests indicating hypoalbuminemia and hyperlipidemia. A kidney biopsy is often necessary to identify the specific underlying cause and guide appropriate treatment.
- Treatment for nephrotic syndrome primarily focuses on managing the symptoms, reducing proteinuria, and preventing complications. Corticosteroids are the mainstay of therapy for many primary glomerular diseases, with additional immunosuppressive agents used for more severe or refractory cases. Diuretics are commonly prescribed to alleviate edema, while ACE inhibitors or angiotensin receptor blockers are used to control blood pressure and reduce proteinuria.
- Despite advances in treatment, some cases of nephrotic syndrome may progress to chronic kidney disease, leading to end-stage renal failure and requiring dialysis or kidney transplantation. Long-term monitoring and management are essential to preserve kidney function and improve the overall quality of life for affected individuals.
- Nurses can help patients with nephrotic syndrome achieve optimal outcomes and quality of life by collaborating with the health care team and empowering the patients to manage their condition.
Acute renal failure
Introduction to Acute Renal Failure
- Acute renal failure (ARF), also known as acute kidney injury (AKI), is a sudden loss of kidney function due to damage or dysfunction of the kidneys.
- It can affect anyone, but it is more common in hospitalized patients, especially those in critical care units.
- Acute renal failure is defined as a rapid decline in glomerular filtration rate (GFR), which is the rate at which the kidneys filter blood and remove waste products.
- GFR is measured by serum creatinine, which is a waste product of muscle metabolism. A normal GFR is about 90 to 120 mL/min/1.73 m2.
- ARF is diagnosed when there is an increase in serum creatinine of 0.3 mg/dL or more within 48 hours, or a decrease in urine output of less than 0.5 mL/kg/hour for 6 hours or more.
- ARF can be classified into three categories, depending on the site of the problem:
- Prerenal ARF: This occurs when there is reduced blood flow to the kidneys, resulting in decreased GFR. This can be caused by conditions such as dehydration, hypovolemia, heart failure, shock, sepsis, or renal artery stenosis.
- Intrinsic ARF: This occurs when there is damage to the kidney tissue itself, resulting in impaired filtration and tubular function. This can be caused by conditions such as acute tubular necrosis (ATN), acute interstitial nephritis (AIN), glomerulonephritis, vasculitis, or contrast-induced nephropathy.
- Postrenal ARF: This occurs when there is an obstruction to the urine flow from the kidneys, resulting in increased pressure and backflow of urine into the kidney. This can be caused by conditions such as kidney stones, benign prostatic hyperplasia (BPH), tumors, blood clots, or neurogenic bladder.
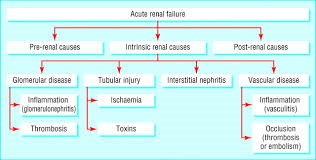
Etiology
The most common causes of ARF vary depending on the category and the setting.
In general, prerenal ARF accounts for about 60% to 70% of cases, intrinsic ARF accounts for about 25% to 40% of cases, and postrenal ARF accounts for about 5% to 10% of cases.
Some of the specific causes of each category are:
- Prerenal ARF: Hypovolemia (due to hemorrhage, vomiting, diarrhea, burns), hypotension (due to septic shock, cardiogenic shock, anaphylactic shock), heart failure (due to myocardial infarction, arrhythmias, valvular disease), renal artery stenosis (due to atherosclerosis, fibromuscular dysplasia), hepatorenal syndrome (due to liver cirrhosis), drugs that affect renal perfusion (such as nonsteroidal anti-inflammatory drugs [NSAIDs], angiotensin-converting enzyme inhibitors [ACEIs], angiotensin receptor blockers [ARBs])
- Intrinsic ARF: Acute tubular necrosis (ATN) (due to ischemia from prerenal causes or nephrotoxins such as antibiotics [aminoglycosides], antivirals [acyclovir], antifungals [amphotericin B], chemotherapeutic agents [cisplatin], contrast media [iodinated]), acute interstitial nephritis (AIN) (due to allergic reactions to drugs such as antibiotics [penicillins], anticonvulsants [phenytoin], diuretics [furosemide], NSAIDs [ibuprofen] or infections such as streptococcal pharyngitis, cytomegalovirus [CMV], etc.), glomerulonephritis (due to immune-mediated diseases such as lupus nephritis, post-streptococcal glomerulonephritis, IgA nephropathy), vasculitis (due to systemic diseases such as granulomatosis with polyangiitis,
microscopic polyangiitis, polyarteritis nodosa), thrombotic microangiopathy (due to disorders such as hemolytic uremic syndrome [HUS], thrombotic thrombocytopenic purpura [TTP])
- Postrenal ARF: Kidney stones (due to hypercalcemia, hyperuricemia, hyperoxaluria), benign prostatic hyperplasia (BPH) (due to hormonal changes in aging men), tumors (such as bladder cancer, prostate cancer, cervical cancer), blood clots (due to trauma, surgery, anticoagulation), neurogenic bladder (due to spinal cord injury, multiple sclerosis, diabetes mellitus)
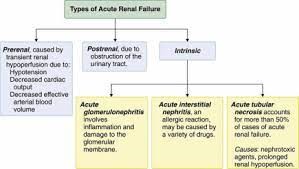
Pathophysiology and Clinical Presentation
- The pathophysiology and clinical presentation of ARF depend on the category and the severity of the condition.
- In general, ARF leads to the accumulation of waste products and fluid in the body, resulting in metabolic acidosis, hyperkalemia, hyponatremia, hyperphosphatemia, hypocalcemia, uremia, edema, and hypertension.
- ARF also affects other organ systems, such as the cardiovascular system (causing arrhythmias, pericarditis), the respiratory system (causing pulmonary edema, pleural effusion), the hematologic system (causing anemia, bleeding tendency), the gastrointestinal system (causing nausea, vomiting, anorexia), the nervous system (causing confusion, lethargy, seizures), and the skin (causing pruritus, uremic frost).
- Some of the specific pathophysiological mechanisms and clinical manifestations of each category are:
I. Prerenal ARF: The reduced blood flow to the kidneys triggers a series of compensatory mechanisms to maintain GFR and renal perfusion.
- These include activation of the renin-angiotensin-aldosterone system (RAAS), which causes vasoconstriction of the efferent arterioles and increased sodium and water reabsorption; stimulation of the sympathetic nervous system (SNS), which causes vasoconstriction of the afferent arterioles and increased cardiac output; and release of antidiuretic hormone (ADH), which causes increased water reabsorption.
- These mechanisms result in oliguria (<400 mL/day), low urine sodium (<20 mEq/L), high urine osmolality (>500 mOsm/kg), high urine specific gravity (>1.020), and low fractional excretion of sodium (<1%).
- The clinical presentation of prerenal ARF is usually related to the underlying cause of hypoperfusion. For example:
- patients with hypovolemia may present with tachycardia, hypotension, dry mucous membranes, poor skin turgor
- patients with heart failure may present with dyspnea, orthopnea, jugular venous distension, crackles
- patients with septic shock may present with fever, chills, tachycardia, hypotension, and altered mental status.
II. Intrinsic ARF: The damage to the kidney tissue causes inflammation, necrosis, and apoptosis of the renal cells. This leads to impairment of the glomerular filtration barrier and tubular function.
- Depending on the site and extent of injury:
- there may be leakage of protein and blood into the urine (proteinuria and hematuria),
- loss of sodium and water into the urine (hyponatremia and hypovolemia),
- decreased reabsorption of bicarbonate and increased production of hydrogen ions (metabolic acidosis),
- decreased reabsorption of potassium and increased secretion of potassium into the urine (hypokalemia or hyperkalemia),
- decreased reabsorption of phosphate and increased secretion of phosphate into the urine (hyperphosphatemia),
- decreased production of erythropoietin (anemia),
- and decreased activation of vitamin D (hypocalcemia).
- The clinical presentation of intrinsic ARF is usually related to the type and severity of kidney injury. For example,
- patients with ATN may present with oliguria or anuria (<100 mL/day), high urine sodium (>40 mEq/L), low urine osmolality (<350 mOsm/kg), low urine specific gravity (<1.010), and high fractional excretion of sodium (>2%)
- patients with AIN may present with fever, rash, eosinophilia, and pyuria patients with glomerulonephritis may present with hematuria, proteinuria, edema, and hypertension
- patients with vasculitis may present with hematuria, proteinuria, purpura, and arthralgia
- patients with thrombotic microangiopathy may present with hemolytic anemia, thrombocytopenia, fever, and neurologic symptoms.
III. Postrenal ARF: The obstruction to the urine flow causes increased pressure and backflow of urine into the kidney. This leads to compression and dilation of the renal tubules and vessels. This impairs GFR and renal perfusion. Depending on the level and duration of obstruction, there may be various degrees of impairment in kidney function, which is known as postrenal acute renal failure (ARF).
- Postrenal ARF, also referred to as obstructive nephropathy, occurs when there is a blockage or obstruction in the urinary tract that prevents the normal flow of urine from the kidneys to the bladder.
- The obstruction can occur at any level of the urinary tract, including the ureters, bladder, or urethra.
- Some common causes of postrenal ARF include kidney stones, tumors, enlarged prostate gland in men, urinary tract infections, and certain congenital abnormalities.
- Common clinical presentations of post-renal AKI include:
- Decreased urine output (oliguria): One of the hallmark signs of post-renal AKI is a reduction in the amount of urine produced. The urine output may be significantly lower than normal or even absent in severe cases. This occurs because the obstruction prevents urine from flowing freely out of the kidneys.
- Flank pain: Patients with post-renal AKI may experience pain in the sides of their abdomen, known as flank pain. The pain can be dull, aching, or sharp and may be localized to one or both sides depending on the location of the obstruction.
- Urinary retention: In cases where the obstruction occurs in the lower urinary tract, such as in the bladder or urethra, patients may have difficulty passing urine. This can result in urinary retention, leading to a feeling of fullness or discomfort in the lower abdomen.
- Signs of uremia: As the kidney function is impaired, waste products and toxins that are normally eliminated in the urine can build up in the bloodstream. This can lead to uremia, a condition characterized by elevated levels of waste products in the blood. Signs of uremia may include nausea, vomiting, loss of appetite, fatigue, confusion, and altered mental status.
- Fluid and electrolyte imbalances: Post-renal AKI can disrupt the normal balance of fluids and electrolytes in the body. This can lead to symptoms such as edema (swelling), especially in the legs and ankles, as well as imbalances in sodium, potassium, and other essential electrolytes.
- Systemic symptoms: In severe cases, post-renal AKI can cause systemic symptoms such as fever, chills, and signs of infection if the obstruction is related to a urinary tract infection or kidney stones.
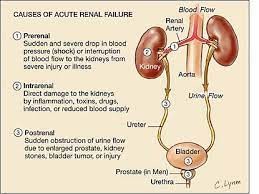
Diagnostic tests and imaging
- The diagnosis of acute renal failure is based on the history, physical examination, laboratory tests, and imaging studies.
- The following tests and imaging may be used to diagnose acute renal failure:
- Serum creatinine and BUN: These are blood tests that measure the levels of creatinine and urea in the blood. Creatinine is a waste product of muscle metabolism that is normally filtered by the kidneys. Urea is a waste product of protein metabolism that is normally excreted by the kidneys. A rise in serum creatinine and BUN indicates a decrease in kidney function. The ratio of BUN to creatinine can help differentiate prerenal from intrinsic causes of acute renal failure. A ratio greater than 20:1 suggests prerenal causes, whereas a ratio less than 10:1 suggests intrinsic causes
- Urine output: This is a measure of how much urine is produced in 24 hours. A normal urine output is about 1.5 liters per day for adults. A urine output less than 0.5 ml/kg/hour for more than 6 hours indicates oliguria, which is a sign of acute renal failure.
- Urine tests: These include urinalysis, urine electrolytes, urine osmolality, urine specific gravity, and urine sediment examination. Urinalysis can reveal abnormalities such as proteinuria, hematuria, pyuria, or casts that suggest kidney damage or infection. Urine electrolytes can help assess tubular function and differentiate prerenal from intrinsic causes of acute renal failure. Urine osmolality and specific gravity can help assess the concentration ability of the kidneys and differentiate prerenal from intrinsic causes of acute renal failure. Urine sediment examination can help identify cellular or crystalline components that indicate glomerular or tubular injury.
- Blood tests: These include serum electrolytes, blood gas analysis, complete blood count (CBC), and other tests depending on the suspected cause of acute renal failure. Serum electrolytes can reveal imbalances such as hyperkalemia, hyponatremia, hyperphosphatemia, hypocalcemia, or hypermagnesemia that result from impaired kidney function. Blood gas analysis can reveal metabolic acidosis due to accumulation of acids or loss of bicarbonate by the kidneys. CBC can reveal anemia due to decreased erythropoietin production by the kidneys or blood loss.
- Other tests may include liver function tests, coagulation studies, lactate dehydrogenase (LDH), haptoglobin, antinuclear antibody (ANA), antineutrophil cytoplasmic antibody (ANCA), complement levels, serum protein electrophoresis, blood cultures, or drug levels.
- Imaging tests: These include renal ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), or renal scintigraphy.
- Renal ultrasound is the preferred imaging modality for renal assessment, as it can provide valuable information such as kidney size, shape, echogenicity, blood flow, and presence of obstruction, cysts, masses, or stones.
- CT or MRI can provide more detailed information on the renal parenchyma, vessels, and collecting system, and can help identify causes such as renal artery stenosis or thrombosis, renal vein thrombosis, pyelonephritis, abscess, infarction, or tumor.
- Renal scintigraphy can help evaluate renal perfusion and function using radioactive tracers that are filtered by the kidneys.
- Biopsy: This is a procedure that involves removing a small sample of kidney tissue for microscopic examination. A biopsy can help confirm the diagnosis and determine the cause and extent of kidney damage in cases of acute renal failure that are unexplained or refractory to treatment. A biopsy can also help differentiate acute from chronic kidney injury by assessing the degree of fibrosis and scarring in the kidney tissue.
Management and treatment
- The management and treatment of acute renal failure depend on the cause and severity of the condition, as well as the presence of complications and comorbidities.
- The general goals of management and treatment are to:
- Restore renal perfusion and function
- Correct or eliminate any reversible causes of kidney injury
- Provide supportive care to prevent or treat complications
- Preserve residual kidney function and prevent progression to chronic kidney disease
- The specific interventions may include:
- Fluid resuscitation: This involves administering intravenous (IV) fluids to restore fluid volume and blood pressure in patients with acute renal failure due to hypovolemia or hypotension. Isotonic crystalloids such as normal saline or lactated Ringer's solution are preferred over colloids as they have no clear renal or mortality benefit and may increase the risk of bleeding or infection. The amount and rate of fluid administration should be guided by the patient's hemodynamic status, urine output, serum creatinine, and BUN levels. Fluid overload should be avoided as it can worsen edema, pulmonary congestion, and heart failure.
- Diuretics: These are medications that increase urine output by inhibiting sodium and water reabsorption in the kidneys. Diuretics may be used to treat fluid overload in patients with acute renal failure who are oliguric or anuric. Loop diuretics such as furosemide (Lasix) or bumetanide (Bumex) are preferred over thiazide diuretics as they are more effective in patients with low GFR. Diuretics should be used with caution as they can cause dehydration, electrolyte imbalances, ototoxicity, or nephrotoxicity. The dose and frequency of diuretics should be adjusted according to the patient's response and laboratory values.
- Discontinuation of Nephrotoxic medications: These are medications that can cause or worsen kidney injury by affecting the blood flow to the kidneys or by directly damaging the kidney cells. Nephrotoxic medications should be discontinued or avoided in patients with acute renal failure whenever possible. Some examples of nephrotoxic medications include:
- nonsteroidal anti-inflammatory drugs (NSAIDs), aminoglycosides,
- amphotericin B,
- vancomycin,
- contrast media,
- cyclosporine,
- tacrolimus,
- cisplatin,
- and methotrexate.
- Drug dose adjustment: This involves modifying the dose or frequency of medications that are eliminated by the kidneys according to the patient's renal function. Drugs that are renally excreted may accumulate in patients with acute renal failure and cause toxicity or adverse effects. The degree of dose adjustment depends on the drug's pharmacokinetics, therapeutic index, and toxicity profile. Some examples of drugs that require dose adjustment in patients with acute renal failure include:
- digoxin,
- lithium,
- gabapentin,
- metformin,
- warfarin.
- Dialysis: This is a process that removes waste products and excess fluid from the blood using a machine (hemodialysis) or the abdomen (peritoneal dialysis). Dialysis may also be indicated in patients with acute renal failure who have chronic kidney disease, volume overload, or drug overdose. The timing and modality of dialysis should be individualized based on the patient's clinical condition, preferences, and availability of resources.
-
Dialysis may be indicated in patients with acute renal failure who have life-threatening complications such as:
- severe hyperkalemia,
- metabolic acidosis,
- uremic encephalopathy,
- pericarditis,
- pulmonary edema that is unresponsive to medical therapy.
- Renal replacement therapy: This is a term that encompasses dialysis and kidney transplantation as methods of replacing kidney function in patients with end-stage renal disease. Renal replacement therapy may be initiated in individuals with nephrotic syndrome who progress to end-stage renal disease (ESRD). ESRD refers to the advanced stage of kidney disease where the kidneys can no longer function adequately to sustain life, necessitating the need for renal replacement therapy.

Nursing Interventions and Supportive Care
- Nursing interventions for ARF depend on the cause, stage, and severity of the condition, as well as the patient's individual needs and preferences.
- Some of the general nursing interventions for ARF include:
- Monitoring and managing fluid and electrolyte balance: The nurse should assess the patient's fluid status by measuring intake and output, daily weight, vital signs, central venous pressure (CVP), and urine specific gravity. The nurse should also monitor the patient's serum electrolyte levels, especially potassium, sodium, calcium, magnesium, and phosphorus, and report any abnormalities to the physician. The nurse should administer intravenous fluids or blood products as ordered, and adjust the rate and type of fluid according to the patient's response. The nurse should also restrict fluid intake if indicated, and educate the patient on signs of fluid overload or dehydration.
- Optimizing nutrition: The nurse should consult with a dietitian to provide a suitable diet for the patient with ARF. The diet should be low in protein, sodium, potassium, phosphorus, and fluids, but high in calories, vitamins, and minerals. The nurse should also monitor the patient's nutritional status by checking serum albumin, prealbumin, transferrin, and nitrogen balance. The nurse should encourage oral intake if possible, or administer enteral or parenteral nutrition as ordered. The nurse should also supplement the patient with vitamins and minerals as needed.
- Ensuring medication safety: The nurse should be aware of the potential nephrotoxic effects of some medications, such as aminoglycosides, nonsteroidal anti-inflammatory drugs (NSAIDs), contrast agents, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs). The nurse should avoid or minimize the use of these medications in patients with ARF, or adjust the dosage and frequency according to the patient's renal function. The nurse should also monitor the patient's serum drug levels and report any signs of toxicity to the physician. The nurse should also administer medications that can help improve renal function or prevent complications, such as diuretics, vasodilators, antihypertensives, bicarbonates, calcium gluconate, insulin, albuterol, kayexalate, or dialysis solutions.

Summary
- ARF is a serious condition that requires prompt diagnosis and treatment.
- The main goals of treatment are to correct or eliminate the underlying cause of kidney damage, restore renal function, prevent or treat complications, and support the patient's recovery.
- Preventive measures, such as avoiding nephrotoxic medications, managing underlying medical conditions, and maintaining good hydration, can play a vital role in reducing the risk of acute renal failure.
- Advances in medical knowledge and technology continue to improve our understanding and management of acute renal failure.
- However, the prevention of this condition remains a key goal, emphasizing the importance of public health awareness, early detection of kidney dysfunction, and multidisciplinary collaboration in patient care.
- Nursing interventions for ARF are based on the patient's individual needs and preferences, but generally include monitoring and managing fluid and electrolyte balance, optimizing nutrition, and ensuring medication safety.
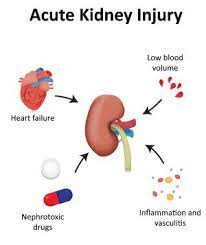
Conclusion
- Acute renal failure, also known as acute kidney injury (AKI), is a serious and potentially life-threatening condition characterized by a rapid and abrupt decline in kidney function.
- It can arise from various underlying causes, including reduced blood flow to the kidneys (prerenal), damage to the kidney tissue (intrinsic renal), or obstruction of the urinary tract (postrenal).
- The clinical presentation of acute renal failure varies, but common features include decreased urine output, alterations in fluid and electrolyte balance, signs of uremia, and potential systemic symptoms.
- Timely recognition and diagnosis are crucial to initiate appropriate interventions and prevent further damage to the kidneys.
- Management of acute renal failure involves addressing the underlying cause, optimizing hemodynamic status, and providing supportive care to maintain fluid and electrolyte balance.
- In some cases, temporary renal replacement therapy, such as dialysis, may be necessary to support kidney function until recovery occurs.
- While many cases of acute renal failure are reversible with prompt and appropriate treatment, some patients may progress to more severe forms of kidney injury or chronic kidney disease.
- Acute renal failure is a critical condition that demands timely and comprehensive evaluation to determine the cause and implement appropriate interventions.
- Its successful management requires a multidimensional approach, including identifying and treating the underlying cause, providing supportive care, and closely monitoring kidney function. By addressing acute renal failure with diligence and diligence, healthcare professionals can improve patient outcomes and contribute to the prevention and management of kidney diseases more effectively.
- Nurses play a vital role in the care and management of patients with ARF. They provide supportive interventions that can help improve renal function or prevent complications.
- They also educate the patient on self-care and prevention strategies that can reduce the risk of future kidney damage.
- By applying evidence-based nursing practice and collaborating with other healthcare professionals, nurses can help improve the outcomes and quality of life of patients with ARF.
Chronic renal failure
Introduction to chronic renal failure
- Chronic renal failure (CRF) is the end result of a gradual, progressive loss of kidney function due to various causes such as:
- chronic infections
- high blood pressure
- vascular diseases
- obstructive processes
- collagen diseases
- nephrotoxic agents
- endocrine diseases such as diabetes mellitus
- CRF can lead to serious complications, such as high blood pressure, anemia, weak bones, nerve damage, and heart disease.
- It is a systemic disease that affects all body systems and leads to uremia, a condition where the end products of protein metabolism accumulate in the blood.
- CRF is also referred to as chronic kidney disease (CKD) and has five stages based on the glomerular filtration rate (GFR), with stage 5 being the most severe and requiring renal replacement therapy.
- Early detection and treatment of CRF can help prevent or delay the progression of kidney disease and reduce the risk of kidney failure, which requires dialysis or a kidney transplant to sustain life.
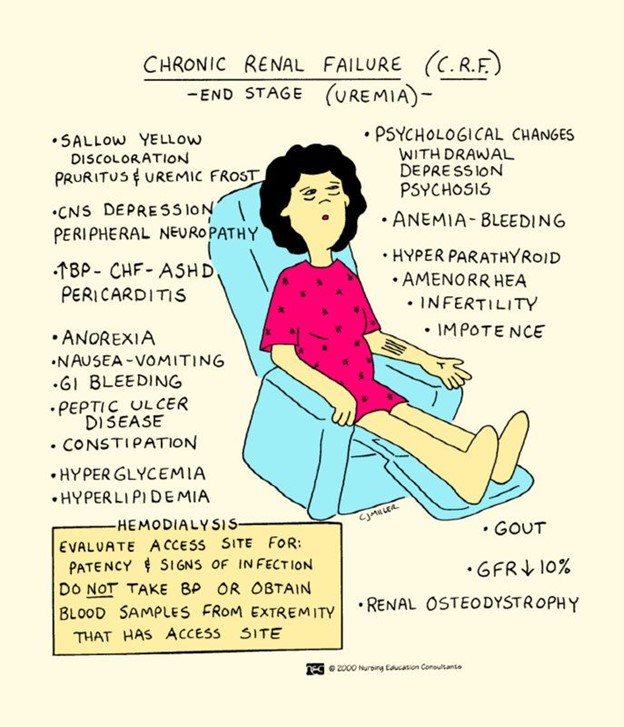
Etiology and risk factors
- The most common causes of CRF are diabetes mellitus and hypertension, which account for about two-thirds of the cases.
- Diabetes Mellitus: Diabetes is the leading cause of chronic kidney disease worldwide. Prolonged high blood sugar levels in diabetes can damage the small blood vessels and filters in the kidneys, leading to impaired kidney function over time.
- Hypertension (High Blood Pressure): Uncontrolled high blood pressure puts strain on the blood vessels in the kidneys, leading to their gradual deterioration and eventual failure.
- Other causes include:
- Glomerulonephritis: This term refers to inflammation of the glomeruli, which are the tiny filters in the kidneys responsible for filtering waste and fluids from the blood. Chronic inflammation can lead to scarring and impaired kidney function.
- Pyelonephritis: This is a type of kidney infection that, if left untreated or recurrent, can cause damage to the kidney tissues and impair their function.
- Nephrosclerosis: This condition involves the hardening and narrowing of the blood vessels in the kidneys, often caused by high blood pressure or aging. The reduced blood flow can damage the kidney tissues and lead to CRF.
- Renal Calculi (Kidney Stones): When kidney stones block the flow of urine and cause repeated obstructions, they can damage the kidneys and lead to chronic kidney disease.
- Systemic Lupus Erythematosus (SLE): SLE is an autoimmune disease that can affect various organs, including the kidneys. Immune system abnormalities may cause inflammation and damage to kidney tissues.
- Aminoglycosides: These are a class of antibiotics that, when used inappropriately or at high doses, can be toxic to the kidneys and lead to CRF.
- Hyperparathyroidism: Overactive parathyroid glands can disrupt calcium and phosphorus balance in the body, leading to kidney damage over time.
- Risk Factors for Developing CRF:
- Older Age: As people age, the risk of developing chronic kidney disease increases. The kidneys naturally undergo some decline in function with age.
- Family History: A family history of kidney disease may increase an individual's risk of developing CRF, indicating a possible genetic predisposition.
- Smoking: Smoking has been linked to the progression of kidney disease, as it can worsen blood vessel damage and decrease blood flow to the kidneys.
- Obesity: Obesity is associated with an increased risk of diabetes and hypertension, both of which are major causes of CRF.
- Dyslipidemia: Abnormal levels of lipids (cholesterol and triglycerides) in the blood can contribute to kidney damage and the progression of CRF.
- Cardiovascular Disease: Conditions like heart disease and atherosclerosis can affect kidney health due to decreased blood flow and increased strain on the kidneys.
- Exposure to Nephrotoxins: Certain medications, environmental toxins, and substances like heavy metals can be harmful to the kidneys and contribute to CRF development.
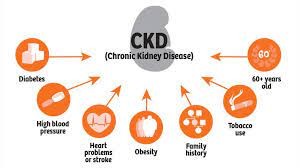
Clinical manifestations and symptoms
- The clinical manifestations and symptoms of CRF depend on the stage of the disease and the degree of uremia.
- They may be nonspecific and vary from person to person. Some of the common signs and symptoms are:
- Fatigue, weakness, anorexia, nausea, vomiting, weight loss
- Pruritus, dry skin, uremic frost
- Edema, hypertension, dyspnea, chest pain
- Anemia, bleeding tendency, bruising
- Confusion, lethargy, seizures, coma
- Polyuria, oliguria, anuria
- Hematuria, proteinuria
- Nocturia, dysuria
- Flank pain
- Bone pain, fractures
- Muscle cramps, restless leg syndrome
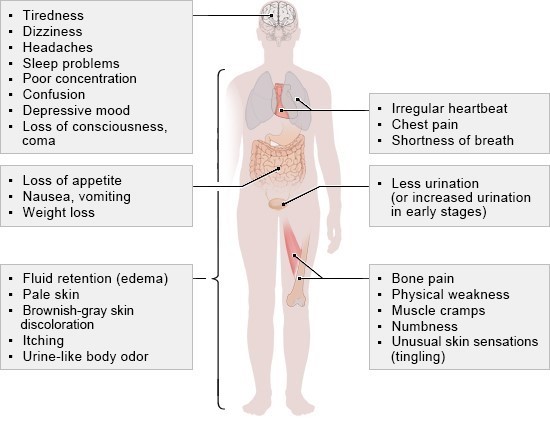
Diagnostic Evaluation and GFR Calculation
- The diagnosis of CRF is based on the presence of kidney damage or decreased GFR for three or more months.
- The GFR can be estimated by using serum creatinine level and other factors such as age, sex, race, and body size.
- The most commonly used formula is the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation:
- GFR = 141 x min (Scr/κ, 1)^α x max(Scr/κ , 1)^-1.209 x 0.993^Age x 1.018 [if female] x 1.159 [if black] where Scr is serum creatinine in mg/dL, κ is 0.7 for females and 0.9 for males,α is -0.329 for females and -0.411 for males, min indicates the minimum of Scr/κ or 1, and max indicates the maximum of Scr/κ or 1.
- The stages of CKD are defined by the GFR as follows:
Stage 1: GFR ≥90 mL/min/1.73 m2 with evidence of kidney damage
Stage 2: GFR 60-89 mL/min/1.73 m2 with evidence of kidney damage
Stage 3a: GFR 45-59 mL/min/1.73 m2
Stage 3b: GFR 30-44 mL/min/1.73 m2
Stage 4: GFR 15-29 mL/min/1.73 m2
Stage 5: GFR <15 mL/min/1.73 m2 or on dialysis
- Other diagnostic tests that may be performed include:
- Blood tests: to measure electrolytes, blood urea nitrogen (BUN), calcium, phosphorus, parathyroid hormone (PTH), albumin, hemoglobin, hematocrit, platelets, coagulation factors
- Urine tests: to measure urine volume, specific gravity, osmolality, pH, sodium, potassium
- Urine culture: to rule out infection
- Urine protein electrophoresis: to identify the type of proteinuria
- Renal ultrasound: to assess the size and shape of the kidneys and detect any obstruction or cysts
- CT scan or MRI: to provide more detailed images of the kidneys and detect any masses or lesions. They can reveal structural changes, such as cysts, tumors, or kidney stones, that may be contributing to kidney damage.
- Kidney biopsy: to obtain a tissue sample for histological examination and diagnosis of the underlying cause

Management and Treatment
- The management and treatment of CRF aim to slow down the progression of the disease, prevent or treat the complications, and improve the quality of life of the patients.
- The main strategies include:
- Control of blood pressure: The target blood pressure for most patients with CKD is <140/90 mmHg, or <130/80 mmHg if there is significant proteinuria.
- Antihypertensive drugs that block the renin-angiotensin-aldosterone system (RAAS), such as angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs), are preferred as they have renal-protective effects.
- However, they should be used with caution in patients with hyperkalemia, bilateral renal artery stenosis, or pregnancy.
- Other antihypertensive drugs that may be used include calcium channel blockers, beta-blockers, diuretics, and alpha-blockers.
- Control of blood glucose: The target glycemic control for patients with diabetes and CKD is a hemoglobin A1c (HbA1c) level of <7%.
- However, this may vary depending on the individual risk-benefit ratio. Oral hypoglycemic agents that are safe and effective in CKD include metformin, sulfonylureas, dipeptidyl peptidase-4 inhibitors, and sodium-glucose cotransporter-2 inhibitors. Insulin therapy may be required in some cases.
- The dose and frequency of these agents may need to be adjusted according to the renal function.
- Control of dyslipidemia: The target lipid levels for patients with CKD are a low-density lipoprotein cholesterol (LDL-C) level of <100 mg/dL, or <70 mg/dL if there is a high cardiovascular risk.
- Statins are the first-line drugs for lowering LDL-C and reducing cardiovascular events in CKD.
- However, they should be avoided in patients with advanced CKD (stage 4 or 5) or on dialysis, as they have no proven benefit and may increase the risk of adverse effects.
- Other lipid-lowering drugs that may be used include ezetimibe, fibrates, niacin, and omega-3 fatty acids.
- Correction of anemia: The target hemoglobin level for patients with CKD is 10-12 g/dL.
- Anemia in CKD is mainly due to the reduced production of erythropoietin (EPO) by the kidneys.
- The treatment of anemia includes iron supplementation (oral or intravenous), EPO-stimulating agents (ESAs), and blood transfusions.
- Iron supplementation is indicated if the serum ferritin level is <100 ng/mL or the transferrin saturation is <20%.
- ESAs are indicated if the hemoglobin level is <10 g/dL and the iron status is adequate.
- Blood transfusions are indicated if the hemoglobin level is <7 g/dL or there are signs of tissue hypoxia.
- Management of mineral and bone disorders: The target levels for patients with CKD are a serum calcium level of 8.4-9.5 mg/dL, a serum phosphorus level of 2.7-4.6 mg/dL, and a serum PTH level of 2-9 times the upper limit of normal.
- Mineral and bone disorders in CKD are due to the impaired excretion of phosphorus, reduced synthesis of vitamin D, and increased secretion of PTH by the parathyroid glands.
- The treatment of mineral and bone disorders includes phosphate binders (such as calcium carbonate, calcium acetate, sevelamer, lanthanum carbonate, or iron-based binders), vitamin D analogs (such as calcitriol, paricalcitol, or doxercalciferol), and calcimimetics (such as cinacalcet).
- Dietary restriction of phosphorus intake and regular exercise are also recommended.
- Management of acid-base disorders: The target serum bicarbonate level for patients with CKD is 22-26 mEq/L.
- Acid-base disorders in CKD are due to the reduced ability of the kidneys to excrete hydrogen ions and reabsorb bicarbonate ions.
- The treatment of acid-base disorders includes sodium bicarbonate supplementation (oral or intravenous) and correction of any underlying causes such as dehydration, infection, or respiratory failure.
- Management of fluid and electrolyte disorders: The target fluid balance for patients with CKD is a weight gain of <5% between dialysis sessions or a urine output of >500 mL/day. Fluid and electrolyte disorders in CKD.
- Diet: A dietitian can help plan a diet that meets the nutritional needs of the patient while limiting the intake of sodium, potassium, phosphorus, protein, and fluid. This can help reduce the workload on the kidneys and prevent further damage.
- Lifestyle: Smoking cessation, regular exercise, weight management, stress reduction, and avoiding nephrotoxic substances (such as NSAIDs, contrast agents, herbal remedies) can help improve the overall health of the patient and slow down the progression of CRF.
- Dialysis: This is a procedure that uses a machine or a membrane to filter the blood and remove waste products and excess fluid.
- It is usually indicated when the kidney function falls below 10% to 15% of normal or when the patient develops life-threatening complications such as uremia, hyperkalemia, or pulmonary edema.
- There are two types of dialysis: hemodialysis and peritoneal dialysis. These depends on the patient's preference, medical condition, availability, and suitability.
- Kidney transplantation: This is a surgery that involves replacing a diseased kidney with a healthy one from a donor. It can restore normal kidney function and improve the quality of life of the patient. However, it also carries risks such as rejection, infection, and side effects of immunosuppressive drugs.
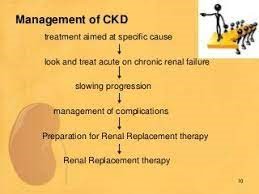
Nursing Care and Patient Education
- The nursing care and patient education for CRF aim to provide holistic support to the patient and family, monitor the patient's condition and response to treatment, prevent complications, and promote self-care and adherence.
- Some of the nursing interventions include:
- Assessing the patient's history, physical examination, laboratory tests, vital signs, fluid balance, nutritional status, mental status, pain level, skin integrity, and potential complications.
- Administering medications as prescribed and monitoring for adverse effects.
- Providing dialysis care as ordered and ensuring proper access to site care, infection control, anticoagulation therapy, and complication management.
- Educating the patient and family about the disease process, treatment options, dietary restrictions, fluid intake, medication regimen, signs and symptoms of complications, when to seek medical attention and available resources and support groups.
- Encouraging the patient to participate in self-care activities such as daily hygiene, oral care, skin care, exercise, relaxation techniques, hobbies, and social interactions.
- Providing emotional support and counseling to the patient and family to cope with the stressors and challenges of living with CRF.

Summary
- CRF is a serious condition that affects multiple body systems and functions. It can be caused by various diseases that damage the kidneys over time.
- The management and treatment of CRF depend on the stage of the disease, the underlying cause, and the presence of complications.
- The main goals are to prevent the progression of the disease, manage symptoms, and prevent complications.
- The nursing care and patient education for CRF aim to provide holistic support to the patient and family, monitor the patient's condition and response to treatment, prevent complications, and promote self-care and adherence.
- It's essential to recognize and manage these risk factors early on to reduce the likelihood of chronic kidney disease development and its progression.
- Regular health checkups, maintaining a healthy lifestyle, and controlling conditions like diabetes and hypertension can help in preventing CRF or delaying its onset.
- Moreover, if an individual is at higher risk due to family history or other factors, proactive monitoring of kidney function is advisable to catch any issues at an early stage and intervene appropriately.
Conclusion
- CRF is a challenging condition that requires multidisciplinary collaboration and individualized care.
- Chronic Kidney Disease (CKD) is a significant and increasingly prevalent health condition worldwide, characterized by the progressive and irreversible decline in kidney function over an extended period.
- CKD poses a significant burden on individuals, families, and healthcare systems due to its potential to lead to end-stage renal disease (ESRD) requiring dialysis or kidney transplantation.
- The prevalence of CKD has been steadily rising, largely due to the increasing incidence of risk factors such as diabetes, hypertension, obesity, and aging populations.
- Early detection and intervention are vital in managing CKD effectively, as the condition often develops silently with few noticeable symptoms in its early stages.
- CKD is classified into five stages based on the estimated glomerular filtration rate (eGFR) and the presence of kidney damage.
- Each stage represents varying degrees of kidney function impairment, ranging from mild (Stage 1) to severe (Stage 5), known as ESRD.
- Patients with CKD are at increased risk of developing cardiovascular complications, bone disorders, anemia, and other related comorbidities.
- Preventive measures play a pivotal role in tackling CKD, with lifestyle modifications, regular health check-ups, and the management of underlying conditions being essential in reducing the risk of disease progression.
- Additionally, early identification of CKD allows for interventions to slow down its progression and preserve kidney function.
- The management of CKD includes comprehensive care, focusing on blood pressure control, glycemic control (in diabetic patients), proteinuria reduction, and the use of medications to address complications and coexisting conditions.
- Diet and lifestyle modifications, including a low-sodium diet, regular physical activity, and smoking cessation, can also contribute to better outcomes.
- In advanced stages of CKD, renal replacement therapies such as dialysis or kidney transplantation become necessary.
- Kidney transplantation offers the best long-term outcomes and quality of life for eligible candidates with ESRD, but access to transplantation remains a challenge due to organ shortage and logistical barriers.
- By addressing CKD comprehensively through early detection, proper management, and education, healthcare professionals and policymakers can make significant strides in enhancing the lives of individuals living with this challenging condition.
- Nurses play a vital role in providing quality care and education to patients with CRF and their families.
- By applying evidence-based practice, nurses can help improve the outcomes and quality of life of patients with CRF.
Treatment
4tyq34y354a3ygt
End-stage renal disease
Introduction to End-Stage Renal Disease
- EndStage Renal Disease (ESRD) is the final stage of chronic kidney disease (CKD) characterized by a significant loss of kidney function.
- ESRD results in the inability to adequately filter waste products and excess fluids from the blood.
- This condition necessitates advanced medical interventions, such as dialysis or kidney transplantation, to sustain the patient's life.
- ESRD is a serious and life-altering condition that poses various challenges for individuals living with it.
- Healthcare professionals play a crucial role in understanding and managing ESRD to provide effective care and support patients through their healthcare journey.
- Enhancing knowledge about ESRD is essential in improving patient outcomes and enhancing their overall quality of life.
Causes and Risk Factors
- Chronic Kidney Disease (CKD): Having a history of CKD significantly increases the risk of progressing to ESRD.
- Diabetes Mellitus: Diabetes, especially poorly controlled, is a leading cause of ESRD.
- Hypertension: Chronic and uncontrolled high blood pressure is a major risk factor for developing ESRD.
- Glomerulonephritis: Inflammatory conditions affecting the kidney's glomeruli can lead to kidney damage and ESRD.
- Polycystic Kidney Disease (PKD): A genetic disorder characterized by the growth of fluidfilled cysts in the kidneys, increasing the risk of ESRD.
- Age: The risk of ESRD increases with age, particularly for individuals over 60 years old.
- Family History: A family history of kidney disease or ESRD may indicate a genetic predisposition.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, and Native Americans, have a higher risk of ESRD.
- Cardiovascular Disease: Conditions like heart disease and atherosclerosis contribute to ESRD risk.
- Obesity: Being overweight or obese increases the likelihood of developing kidney disease and ESRD.
- Smoking: Smoking is associated with a higher risk of kidney disease progression to ESRD.
- Nephrolithiasis: Kidney stones and recurrent urinary tract infections can lead to chronic kidney damage and ESRD.
- Autoimmune Disorders: Autoimmune conditions like systemic lupus erythematosus (SLE) may cause kidney inflammation and ESRD.
- Medications: Certain drugs, such as nonsteroidal antiinflammatory drugs (NSAIDs) and some antibiotics, can cause kidney damage and increase the risk of ESRD.
- Excessive Analgesic Use: Overuse of pain medications, especially analgesics, can lead to kidney damage and ESRD.
- Occupational Exposure: Working in environments with potential nephrotoxic substances increases the risk of kidney disease and ESRD.
- HIV Infection: People with HIV have a higher risk of developing kidney disease and ESRD due to the virus's impact on the kidneys.
- Obstructive Uropathy: Conditions causing urinary tract obstructions can lead to kidney damage and ESRD.
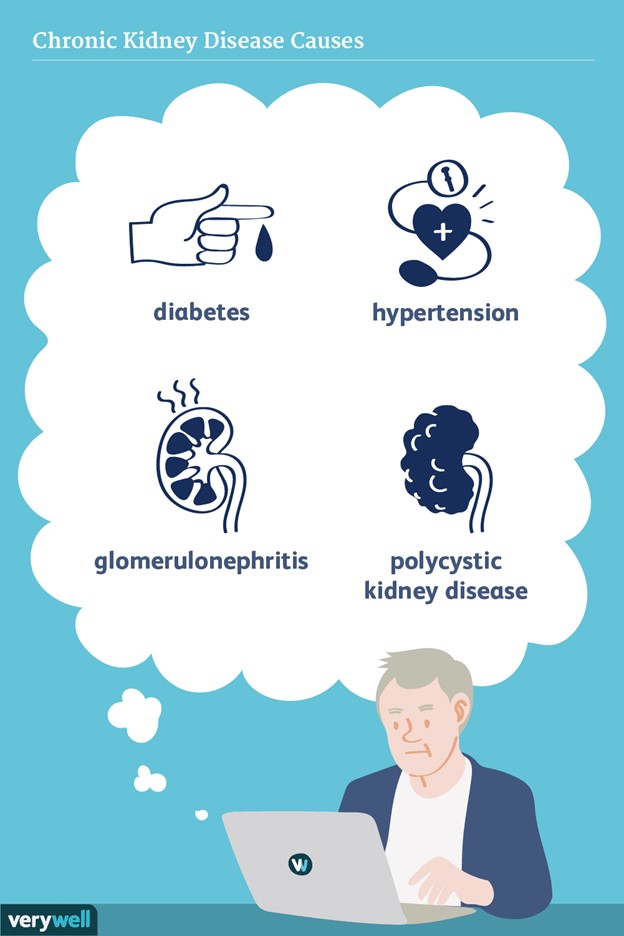
Clinical Features and Complications
- ESRD affects multiple organ systems and leads to various signs and symptoms such as:
- Fluid and electrolyte imbalances: edema, hypertension, dysrhythmias, hyperkalemia, hyponatremia, hypocalcemia, hyperphosphatemia, metabolic acidosis.
- Hematologic disorders: anemia, bleeding tendencies, infection risk.
- Cardiovascular disorders: heart failure, coronary artery disease, pericarditis, peripheral vascular disease.
- Respiratory disorders: pulmonary edema, pleural effusion, uremic pneumonitis.
- Gastrointestinal disorders: nausea, vomiting, anorexia, gastritis, peptic ulcer disease, constipation.
- Neurologic disorders: encephalopathy, neuropathy, seizures, coma.
- Musculoskeletal disorders: renal osteodystrophy, bone pain, fractures.
- Endocrine disorders: insulin resistance, hyperglycemia, hyperlipidemia.
- Dermatologic disorders: pruritus, uremic frost.
- Reproductive disorders: infertility, impotence.
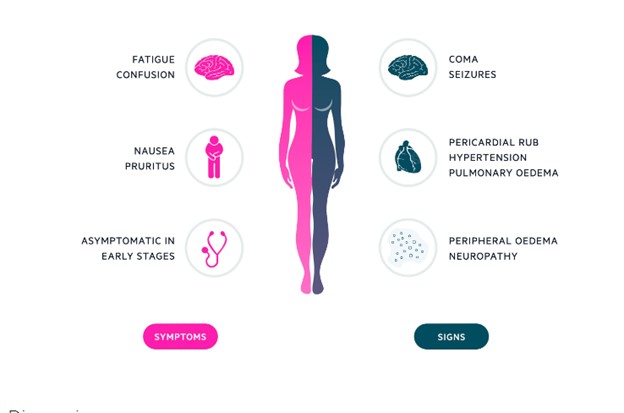
Dialysis as a Treatment Option
- Dialysis is a process that removes waste products and excess fluid from the blood by using a semipermeable membrane.
- There are two types of dialysis: hemodialysis and peritoneal dialysis.
- Hemodialysis uses an artificial kidney machine that pumps blood through a dialyzer (filter) that exchanges waste products and electrolytes with a dialysate (solution).
- Hemodialysis is usually performed three times a week for about four hours each session in a dialysis center or at home.
- Hemodialysis requires vascular access through an arteriovenous fistula (surgically created connection between an artery and a vein), an arteriovenous graft (synthetic tube connecting an artery and a vein), or a central venous catheter (inserted into a large vein in the neck or chest).
- Hemodialysis complications include hypotension, muscle cramps, infection, clotting, air embolism, and hemolysis.
- Peritoneal dialysis uses the peritoneum (lining of the abdominal cavity) as a natural membrane that exchanges waste products and electrolytes with a dialysate that is infused into the abdominal cavity through a catheter.
- Peritoneal dialysis can be performed continuously or intermittently at home or at work.
- Peritoneal dialysis requires a peritoneal catheter that is surgically implanted into the abdomen.
- Peritoneal dialysis complications include peritonitis (infection of the peritoneum), leakage, hernia, malnutrition, and hyperglycemia.
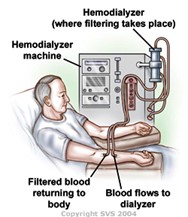
Renal Transplantation and Living Donor Options
- Renal transplantation is the surgical implantation of a healthy kidney from a donor (living or deceased) into a recipient with ESRD.
- Renal transplantation is the preferred treatment option for ESRD as it offers better quality of life, lower mortality, and lower cost than dialysis.
- Renal transplantation requires immunosuppressive therapy to prevent rejection of the transplanted kidney.
- Renal transplantation complications include acute or chronic rejection, infection, malignancy, cardiovascular disease, and recurrence of original kidney disease.
- Living donor options include related (genetically or emotionally) or unrelated (altruistic) donors who are willing and medically suitable to donate one of their kidneys.
- Living donor options have advantages such as shorter waiting time, better matching, longer graft survival, and lower rejection rate than deceased donor options.
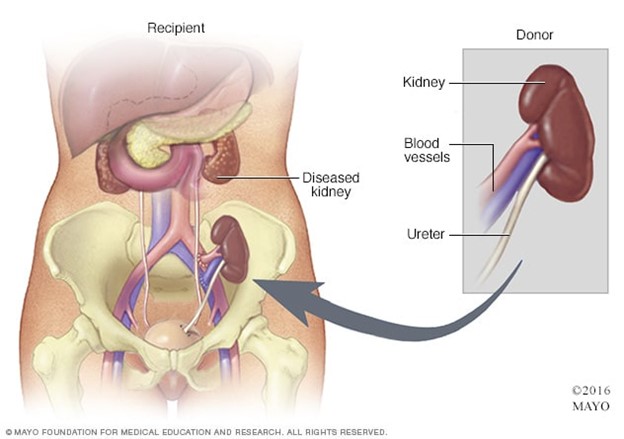
Psychological and Social Impact
- Emotional Distress: ESRD diagnosis can lead to feelings of shock, fear, anxiety, and depression due to the uncertainty of the future and the need for life-altering treatments.
- Quality of Life: ESRD can negatively affect a person's quality of life, leading to limitations in daily activities, social interactions, and employment opportunities.
- Social Isolation: ESRD patients may withdraw from social activities due to fatigue, dietary restrictions, and the need for frequent medical appointments.
- Financial Burden: The cost of ESRD treatments, medications, and potential loss of income can create financial stress for patients and their families.
- Family and Caregiver Stress: Family members and caregivers may experience increased stress due to their role in supporting and caring for the patient.
- Coping Challenges: ESRD patients and their families may struggle with coping with the challenges of managing a chronic and life-threatening condition.
- Sexual Dysfunction: ESRD and its treatments may lead to sexual dysfunction, affecting intimate relationships and adding to emotional distress.
- Adherence Difficulties: Compliance with complex treatment regimens and dietary restrictions can be challenging for ESRD patients, impacting treatment effectiveness.
Nursing Support and Coping Strategies
- Nursing support for patients with ESRD and their families involves providing holistic care that addresses their physical, psychological, social, and spiritual needs.
- Nursing support includes:
- Assessing the patient's and family's knowledge, beliefs, values, preferences, expectations, coping skills, and support systems.
- Educating the patient and family about ESRD, its causes, complications, treatment options, self-care measures, and available resources.
- Encouraging the patient and family to participate in decision-making and care planning.
- Providing emotional support and counseling to the patient and family to help them cope with their feelings and concerns.
- Referring the patient and family to appropriate health care professionals and community agencies for further assistance .
- Advocating for the patient's and family's rights and interests .
- Collaborating with the interdisciplinary health care team to ensure coordinated and comprehensive care for the patient and family.
- Coping strategies for patients with ESRD and their families include:
- Seeking information and education about ESRD and its management.
- Maintaining a positive attitude and outlook on life.
- Expressing and sharing feelings and concerns with others who are supportive and understanding.
- Seeking professional help if experiencing severe psychological distress or suicidal thoughts.
- Joining a support group or peer network for patients with ESRD or their families.
- Engaging in enjoyable activities and hobbies that provide relaxation and distraction.
- Practicing healthy lifestyle habits such as eating well, exercising regularly, sleeping adequately, avoiding smoking and alcohol

Summary
- ESRD is the final stage of chronic kidney disease (CKD), marked by a significant loss of kidney function and the need for advanced medical interventions.
- Diabetes, hypertension, glomerulonephritis, and polycystic kidney disease are common causes and risk factors for ESRD.
- ESRD presents with clinical features like fluid and electrolyte imbalances, uremia, anemia, and cardiovascular complications.
- Treatment options for ESRD include dialysis (hemodialysis and peritoneal dialysis) and kidney transplantation.
- The psychological and social impact of ESRD can lead to emotional distress, body image issues, social isolation, and financial burden for patients and their families.
- Support services, patient education, and social work involvement are essential in addressing the psychosocial challenges of living with ESRD.
- ESRD patients may experience sexual dysfunction and adherence difficulties, requiring a comprehensive care approach.
- Quality of life can be affected due to limitations in daily activities and employment opportunities.
- Early detection and patient-centered care are crucial in improving outcomes and enhancing the overall well-being of individuals with ESRD.
- Healthcare professionals play a vital role in providing holistic care, empowering patients to cope with the challenges of ESRD, and supporting them throughout their healthcare journey.
Conclusion
- ESRD represents a critical stage of chronic kidney disease, necessitating advanced medical interventions for the management of kidney failure.
- The psychological and social impact of ESRD can significantly affect patients' emotional wellbeing and quality of life.
- Holistic care, including psychosocial support, patient education, and social work involvement, is essential in addressing the challenges faced by individuals with ESRD.
- Early detection, patient-centered care, and comprehensive treatment options are crucial in improving outcomes and enhancing overall well-being.
- Healthcare professionals play a pivotal role in providing compassionate care and support, empowering ESRD patients to lead fulfilling lives despite the challenges of their condition.
- By addressing the multifaceted aspects of ESRD, healthcare providers can positively impact patients' lives and contribute to improved longterm outcomes for individuals living with this condition.
Benign prostatic hyperplasia
Introduction
- BPH is a condition that occurs when the prostate gland enlarges, potentially slowing or blocking the urine stream
- BPH is common in older men and can cause lower urinary tract symptoms (LUTS) such as frequency, urgency, hesitancy, incontinence, incomplete emptying, dribbling, nocturia, weak stream, straining, hematuria, and frequent UTIs
- BPH is not cancerous and does not increase the risk of prostate cancer
- The exact cause of BPH is unknown, but it may be related to hormonal changes, genetic factors, lifestyle factors, and inflammation
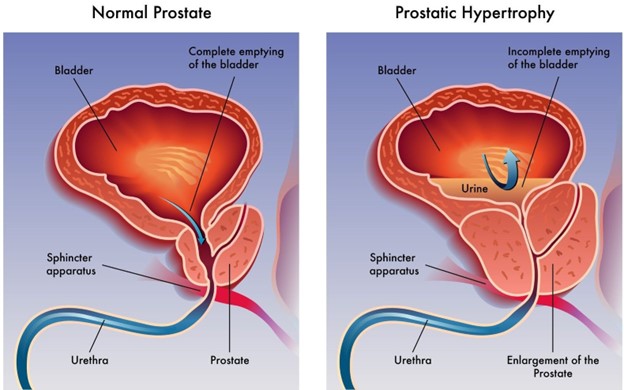
Clinical Presentation and Symptoms
- The symptoms of BPH vary depending on the degree of prostate enlargement and bladder outlet obstruction
- The most common symptom are LUTS which affects the storage and emptying of urine
- Storage symptoms include frequency, urgency, nocturia, incontinence, and overflow incontinence
- Emptying symptoms include hesitancy, weak stream, intermittency, dribbling, incomplete emptying, and straining
- Other symptoms may include hematuria, urinary retention, bladder stones, bladder diverticula, hydronephrosis, renal insufficiency, and recurrent UTIs

Diagnostic Evaluation
- The diagnosis of BPH is based on the history, physical examination, symptom assessment, laboratory tests, and imaging studies
- The history should include the onset, duration, severity, and impact of LUTS on the quality of life of the client
- The physical examination should include a digital rectal exam (DRE) to palpate the size, shape, consistency, and tenderness of the prostate gland
- The symptom assessment should include the International Prostate Symptom Score (IPSS) or the American Urological Association Symptom Index (AUASI) to quantify the severity of LUTS and their effect on the client's well-being
- The laboratory tests should include a urinalysis and culture to rule out UTI or hematuria; a complete blood count (CBC) to check for infection or anemia; a blood urea nitrogen (BUN) and creatinine to assess renal function; and a prostate-specific antigen (PSA) to screen for prostate cancer or monitor treatment response
- The imaging studies may include a transrectal ultrasound (TRUS) with or without biopsy to measure the prostate volume and rule out prostate cancer; a postvoid residual (PVR) measurement to evaluate bladder emptying; a uroflowmetry to measure the urine flow rate; a cystoscopy to visualize the urethra and bladder; and a urodynamic study to assess bladder pressure and function
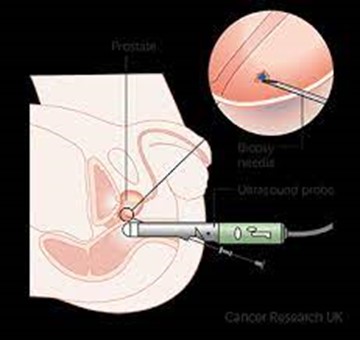
Management and Treatment
- Watchful waiting: This means monitoring the condition without any active treatment, but making some lifestyle changes such as drinking less fluids at night, avoiding caffeine and alcohol, and urinating when you feel the urge. This option is suitable for men with mild or moderate symptoms who are not bothered by them.
- Medications: There are two main types of drugs that can help reduce the size of the prostate or relax the muscles around it, thus improving the urine flow. They are alpha-blockers (such as tamsulosin, alfuzosin, or doxazosin) and 5-alpha reductase inhibitors (such as finasteride or dutasteride). These medications can have side effects such as dizziness, low blood pressure, sexual dysfunction, or breast enlargement. They may also interact with other drugs, so it is important to consult with your doctor before taking them.
- Minimally invasive procedures: These are techniques that use heat, lasers, or implants to destroy or shrink some of the prostate tissue, thus relieving the obstruction. They are usually done under local anesthesia and have a shorter recovery time than surgery. Some of the examples are transurethral microwave therapy (TUMT), transurethral needle ablation (TUNA), water vapor therapy (Rezum), or prostatic urethral lift (UroLift). These procedures may have risks such as bleeding, infection, urinary retention, or erectile dysfunction.
- Surgery: This is the most effective option for men with severe symptoms or complications such as urinary retention, kidney damage, bladder stones, or recurrent urinary tract infections. Surgery involves removing part or all of the prostate gland through an incision in the abdomen or the urethra. The most common type of surgery is transurethral resection of the prostate (TURP), which uses an electric loop to cut and remove the excess tissue. Other types of surgery are open prostatectomy, holmium laser enucleation of the prostate (HoLEP), or robot-assisted laparoscopic prostatectomy (RALP). Surgery can have complications such as bleeding, infection, urinary incontinence, retrograde ejaculation, or erectile dysfunction.
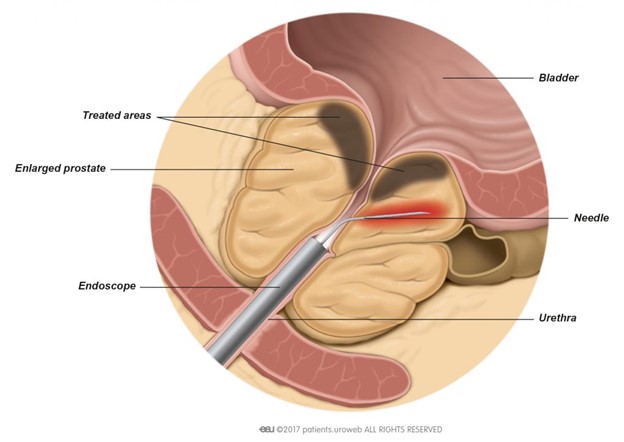
Complications
- Urinary retention: Inability to completely empty the bladder, leading to discomfort and increased risk of urinary tract infections.
- Urinary tract infections (UTIs): Stagnant urine in the bladder can lead to bacterial growth and recurrent infections.
- Bladder stones: Residual urine in the bladder can precipitate the formation of bladder stones, causing pain and further obstruction.
- Hematuria: Presence of blood in the urine due to irritation and inflammation of the bladder or urinary tract.
- Acute kidney injury: Severe or prolonged urinary retention can cause back pressure on the kidneys, leading to kidney dysfunction.
- Bladder diverticula: Chronic pressure from urine retention can cause weak areas in the bladder wall, leading to pouchlike outpouchings called diverticula.
- Hydroureter and hydronephrosis: Dilatation of the ureters and kidneys due to urine backflow from the bladder obstruction.
- Renal insufficiency: Longterm obstruction and impaired kidney function can lead to chronic kidney disease and renal failure.
- Urinary incontinence: Overflow incontinence may occur when the bladder is constantly full, leading to involuntary urine leakage.
- Recurrent UTIs: BPHrelated urinary retention and incomplete bladder emptying increase the risk of recurrent urinary tract infections.
- Bladder damage: Prolonged bladder distension may lead to weakening of the bladder muscle and loss of its contractile function.
- Urinary stones: BPH can increase the risk of developing urinary stones due to urine stasis and altered urinary pH.
- Sexual dysfunction: BPH and its treatments may impact sexual function, leading to erectile dysfunction or ejaculatory disturbances.
- Emotional and psychological impact: BPH-related complications and symptoms can affect the patient's quality of life, causing anxiety, depression, or social isolation.
Nursing Considerations and Patient Education
- Assess for lower urinary tract symptoms (LUTS) such as frequency, urgency, hesitancy, incontinence, incomplete emptying, dribbling, nocturia, diminished stream, straining, hematuria
- Use the International Prostate Symptom Score to determine the severity of manifestations and their effect on the patient's quality of life
- Perform digital rectal exam to palpate for enlarged smooth prostate
- Obtain urinalysis and culture, CBC, BUN and creatinine, prostate-specific antigen (PSA), culture, and sensitivity of prostatic fluid as indicated
- Administer medications such as 5alpha reductase inhibitors (finasteride) or alpha-blocking agents (tamsulosin) as prescribed
- Monitor for adverse effects of medications such as impotence, decreased libido, breast enlargement, orthostatic hypotension, dizziness, headache
- Educate patient about medication adherence, potential teratogenic effects of finasteride, and the need for regular followup
- Provide information about surgical options such as transurethral resection of the prostate (TURP), transurethral incision of the prostate (TUIP), laser prostatectomy, or prostatectomy if medications are ineffective or contraindicated
- Prepare patient for surgery and postoperative care such as continuous bladder irrigation, catheter care, pain management, prevention of infection and bleeding
- Encourage patient to avoid drinking large amounts of fluid at one time, urinate as soon as urge is felt, avoid bladder stimulants (alcohol, caffeine), avoid medications that decrease bladder tone (anticholinergics, decongestants, antihistamines)
- Advise patient that frequent ejaculation releases retained prostatic fluids and may decrease the size of the prostate
- Promote physical activity and healthy diet to reduce risk factors such as smoking, obesity, diabetes, heart disease
Summary
- Benign prostatic hyperplasia (BPH) is a common condition in older men that involves enlargement of the prostate gland and causes urinary dysfunction.
- BPH can lead to complications such as infection, retention, kidney damage, bladder stones, and bladder diverticula.
- BPH can be treated with medications or surgery depending on the severity of symptoms and the patient's preference.
- Nursing care involves assessment, education, medication administration, and postoperative care.
- Patients should be advised to follow lifestyle modifications to improve urinary function and prevent recurrence.
Conclusion
- Benign Prostatic Hyperplasia (BPH) is a prevalent condition that affects aging men and can lead to significant urinary symptoms and complications.
- Timely recognition of BPH and appropriate management are crucial in improving the patient's quality of life and preventing potential complications.
- Nurses play a vital role in assessing, educating, and implementing comprehensive care strategies for patients with BPH.
- By understanding the pathophysiology, treatment options, and potential complications of BPH, healthcare professionals can optimize patient outcomes and enhance overall wellbeing.
- Patientcentered care, evidence-based practice, and effective communication are key components in managing BPH and supporting patients throughout their healthcare journey.
- With a focus on early intervention and tailored care, healthcare providers can make a positive impact on the lives of patients with BPH, promoting better urinary health and overall health outcomes.
Renal calculus
Introduction to Renal Calculus
- Renal calculus, commonly known as kidney stones, is a prevalent urological condition that affects millions of individuals worldwide.
- These stones are solid masses formed within the kidneys due to the crystallization of minerals and salts in the urine.
- Renal calculus presents a significant health challenge, causing pain, urinary obstruction, and potential complications if left untreated.
- This introduction aims to provide an overview of renal calculus, including its causes, symptoms, diagnostic approaches, and the crucial role of nursing care in its management.
- By understanding the complexities of renal calculus, healthcare professionals can enhance their ability to provide comprehensive care and support for patients affected by this condition.
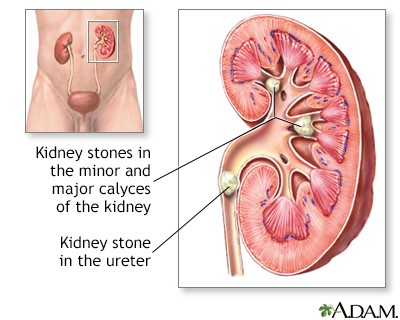
Etiology and Risk Factors
- The etiology of renal calculus is multifactorial and involves genetic, metabolic, environmental, dietary, and lifestyle factors
- Some of the risk factors for renal calculus are:
- Family or personal history of renal calculus
- Dehydration or low fluid intake
- High intake of animal protein, sodium, oxalate, or calcium
- Low intake of citrate or magnesium
- Obesity or diabetes mellitus
- Hyperparathyroidism or gout
- Urinary tract infection or stasis
- Medications such as diuretics, antacids, or vitamin C supplements
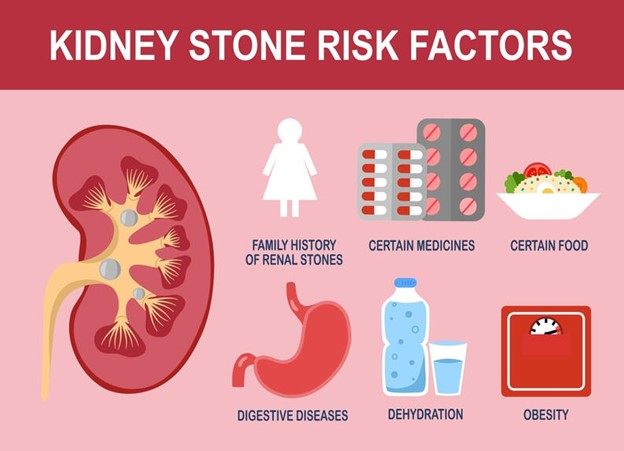
Clinical Manifestations and Symptoms
The clinical manifestations and symptoms of renal calculus depend on the size, location, and movement of the stone
- The most common symptom of renal calculus is renal colic, which is a sudden and severe pain in the flank, back, or abdomen that radiates to the groin or genitalia
- Other symptoms of renal calculus are:
- Hematuria or blood in the urine
- Dysuria or painful urination
- Frequency or urgency of urination
- Nausea or vomiting
- Fever or chills
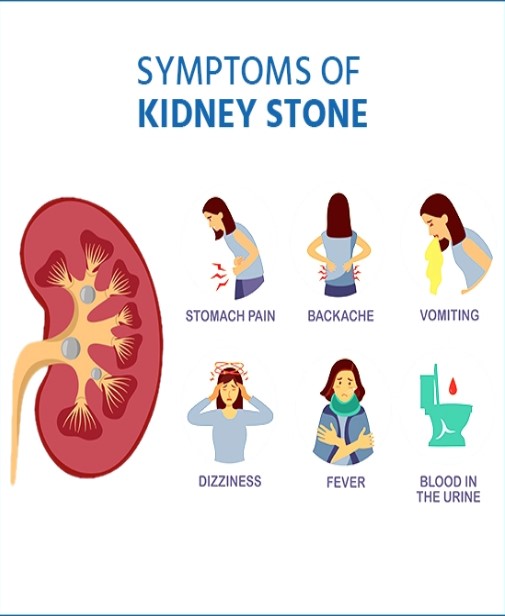
Diagnostic Evaluation
- The diagnostic evaluation of renal calculus involves a combination of history taking, physical examination, laboratory tests, and imaging studies
- Some of the diagnostic tests for renal calculus are:
- Urinalysis to detect hematuria, infection, pH, specific gravity, and crystals
- Urine culture and sensitivity to identify the causative organism and antibiotic susceptibility in case of infection
- Serum chemistry to measure electrolytes, calcium, phosphorus, uric acid, creatinine, and blood urea nitrogen levels
- Complete blood count to detect leukocytosis or anemia in case of infection or bleeding
- Imaging studies such as ultrasound, plain abdominal xray (KUB), intravenous pyelogram (IVP), computed tomography (CT) scan, or magnetic resonance imaging (MRI) to visualize the size, shape, location, and number of stones
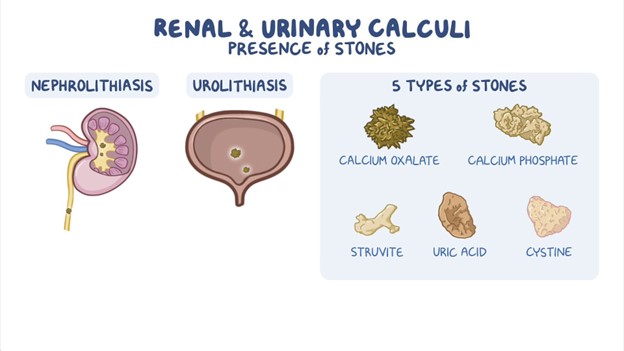
Management and Treatment
- The management and treatment of renal calculus aim to relieve pain, facilitate stone passage, prevent infection, and prevent recurrence
- Some of the management and treatment options for renal calculus are:
- Analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids to reduce pain and inflammation
- Antispasmodics such as hyoscyamine or oxybutynin to relax the smooth muscle of the ureter and facilitate stone passage
- Antibiotics such as ciprofloxacin or nitrofurantoin to treat or prevent infection
- Fluid therapy to increase urine output and dilute urine concentration
- Dietary modifications such as increasing fluid intake; reducing intake of animal protein, sodium, oxalate, or calcium; increasing intake of citrate or magnesium; and adjusting pH according to stone type
- Lithotripsy such as extracorporeal shock wave lithotripsy (ESWL) or percutaneous nephrolithotomy (PCNL) to break up large stones into smaller fragments that can be passed in the urine
- Surgery such as ureteroscopy (URS), cystoscopy (CS), or open surgery to remove stones that are too large, impacted, infected, or causing obstruction

Prevention Strategies and Lifestyle Modifications
- The prevention strategies and lifestyle modifications for renal calculus aim to reduce the risk factors and recurrence of stone formation
- Some of the prevention strategies and lifestyle modifications for renal calculus are:
- Drinking at least 2.5 liters of fluid per day to maintain urine output above 2 liters per day
- Avoiding dehydration and excessive sweating
- Limiting intake of animal protein, sodium, oxalate, or calcium according to stone type
- Increasing intake of citrate or magnesium according to stone type
- Adjusting pH according to stone type
- Maintaining a healthy weight and avoiding obesity
- Controlling blood glucose and blood pressure levels
- Treating underlying conditions such as hyperparathyroidism or gout
- Taking medications such as thiazide diuretics, potassium citrate, allopurinol, or antibiotics as prescribed to prevent stone formation
Nursing Care and Patient Education
- The nursing care and patient education for renal calculus involve providing physical and emotional support, monitoring vital signs and urine output, administering medications and fluids, teaching selfcare measures, and providing discharge instructions
- Some of the nursing care and patient education for renal calculus are:
- Assessing pain level and location and administering analgesics as prescribed
- Encouraging fluid intake and offering oral or intravenous fluids as ordered
- Straining urine and inspecting for stone passage
- Collecting urine specimens for urinalysis, culture, and sensitivity as ordered
- Monitoring vital signs, especially temperature, pulse, and blood pressure
- Observing for signs of infection such as fever, chills, leukocytosis, or positive urine culture
- Educating the patient about the etiology, risk factors, symptoms, diagnosis, treatment, and prevention of renal calculus
- Instructing the patient to drink adequate fluids; follow dietary modifications; take medications as prescribed; report any changes in pain, urine color, or urine output; and seek medical attention if symptoms worsen or persist
- Referring the patient to a urologist or nephrologist for followup care and stone analysis
Summary
- Renal calculus is a common urologic disorder that can cause significant morbidity and complications if not treated promptly and effectively
- Renal calculus is caused by the crystallization of minerals and organic substances in the urine due to various genetic, metabolic, environmental, dietary, and lifestyle factors
- Renal calculus can present with renal colic, hematuria, dysuria, frequency, urgency, nausea, vomiting, fever, or chills depending on the size, location, and movement of the stone
- Renal calculus can be diagnosed by history taking, physical examination, laboratory tests, and imaging studies that can reveal the size, shape, location, and number of stones
- Renal calculus can be managed by analgesics, antispasmodics, antibiotics, fluid therapy, dietary modifications, lithotripsy, or surgery depending on the severity and type of the stone
- Renal calculus can be prevented by drinking adequate fluids; limiting intake of animal protein, sodium, oxalate, or calcium; increasing intake of citrate or magnesium; adjusting pH according to stone type; maintaining a healthy weight; controlling blood glucose and blood pressure levels; treating underlying conditions; and taking medications as prescribed
Conclusion
- Renal calculus is a challenging condition that requires comprehensive knowledge and skills from nurses to provide optimal care and education for patients.
- Nurses play a vital role in relieving pain, facilitating stone passage, preventing infection, preventing recurrence, and promoting health and well-being for patients with renal calculus.
- Their expertise in managing the condition and offering holistic care significantly impacts patient outcomes and quality of life.
- Through diligent monitoring, timely interventions, and patient education, nurses contribute to the successful management and long-term prevention of renal calculus.
- The compassionate and attentive care provided by nurses plays a crucial role in supporting patients throughout their journey with renal calculus, fostering a positive and comforting healthcare experience.
Transurethral resection of the prostate
Introduction
- Transurethral Resection of the Prostate (TURP) is a common surgical procedure for treating benign prostatic hyperplasia (BPH) in aging men.
- BPH causes prostate gland enlargement, resulting in urinary obstruction and lower urinary tract symptoms.
- TURP effectively relieves urinary obstruction and improves urinary flow, restoring normal voiding function.
- The procedure significantly enhances the patient's quality of life by reducing bothersome urinary symptoms.
- This introduction provides an overview of TURP, its purpose, and its role in managing BPH.
- Nursing care plays a crucial role in ensuring successful patient outcomes throughout the perioperative period and recovery.
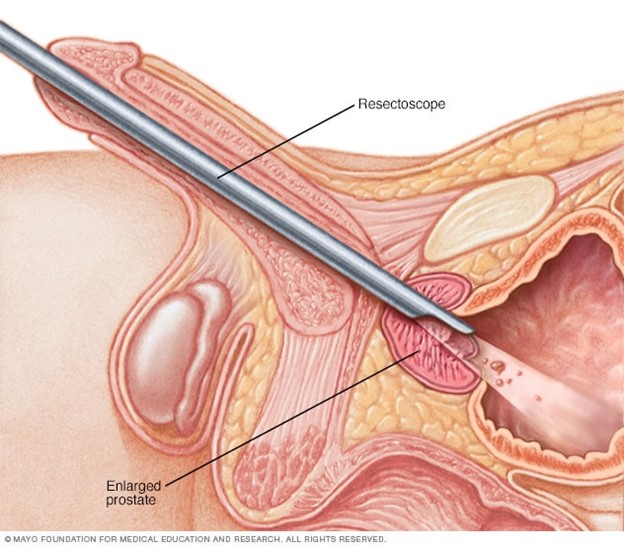
Preoperative Nursing Care
- Assess the patient's medical history, physical exam, urine culture, blood tests, and prostate-specific antigen (PSA) level
- Teach the patient about the procedure, risks, benefits, and alternatives
- Instruct the patient to fast for 8 hours before the surgery and to stop taking anticoagulants or antiplatelets as advised by the doctor
- Administer antibiotics prophylactically to prevent infection
- Prepare the patient for anesthesia (general or spinal) and insert an intravenous (IV) line for fluid and medication administration
Intraoperative Considerations
- Monitor the patient's vital signs, oxygen saturation, electrocardiogram (ECG), and urine output during the surgery
- Assist the surgeon with the insertion of the resectoscope through the urethra and the removal of prostate tissue using an electrical wire loop
- Irrigate the bladder with sterile fluid to wash out blood clots and tissue fragments during and after the surgery
- Insert a threeway urinary catheter with a balloon to drain urine and provide continuous bladder irrigation (CBI) after the surgery
- Be prepared to manage potential bleeding and fluid electrolyte imbalances.
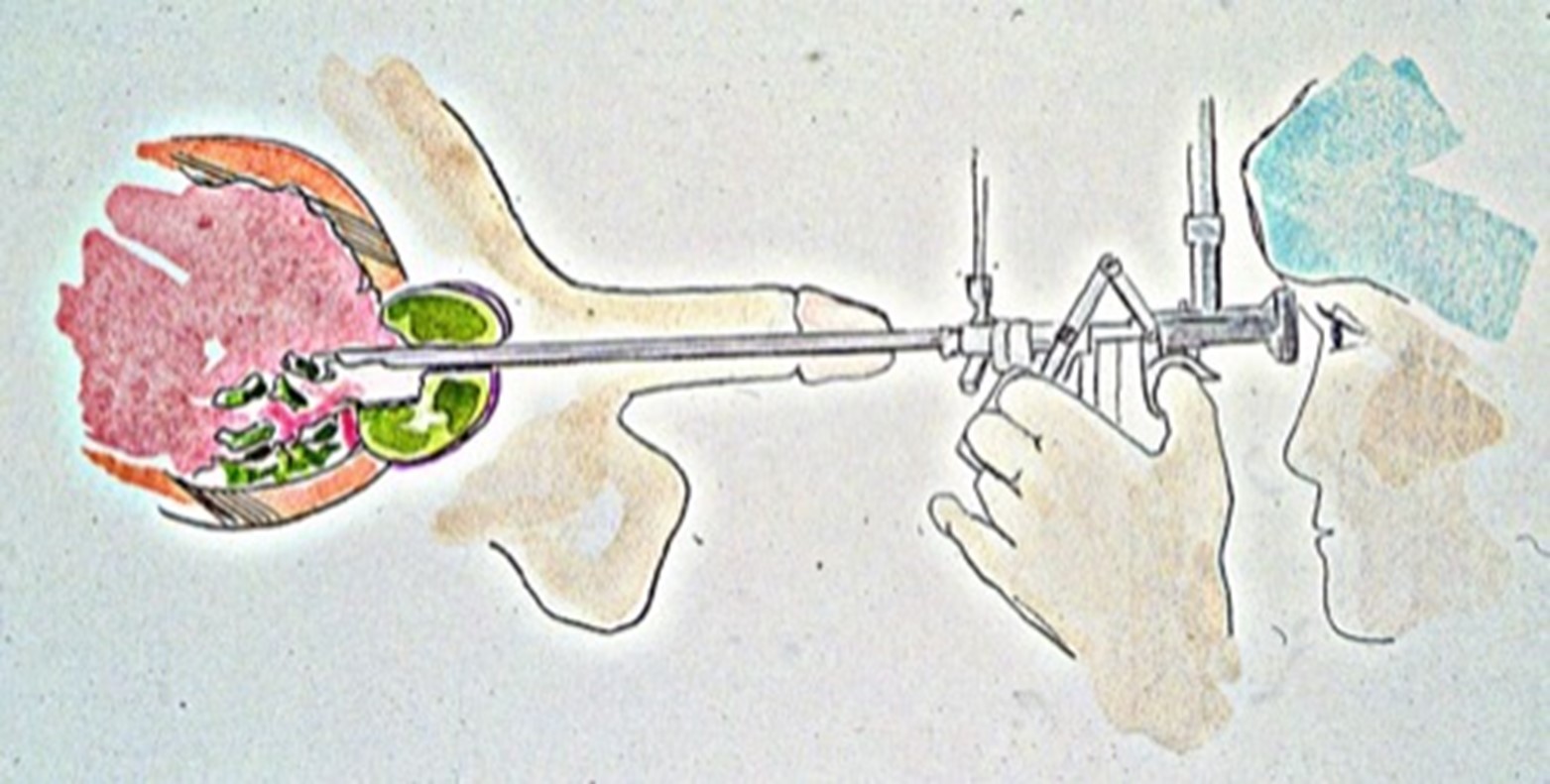
Postoperative Nursing Care
- Transfer the patient to the recovery room and monitor for signs of bleeding, infection, shock, or fluid overload
- Maintain CBI as ordered and regulate the flow rate to keep the urine clear or slightly pink
- Clamp and unclamp the catheter intermittently to prevent bladder spasms and promote clot removal
- Administer analgesics, antispasmodics, antiemetics, and antibiotics as prescribed
- Encourage fluid intake of at least 2 liters per day unless contraindicated
- Remove the catheter when there is no significant bleeding or clots in the urine, usually after 24 to 48 hours

Complications and Nursing Interventions
- Hemorrhage: monitor for bright red bleeding, increased clots, decreased urine output, or signs of shock; notify the doctor; increase CBI flow rate; administer fluids and blood transfusions as ordered
- Infection: monitor for fever, chills, dysuria, hematuria, or foulsmelling urine; notify the doctor; obtain urine culture; administer antibiotics as ordered
- Bladder injury: monitor for abdominal pain, distension, or leakage of urine around the catheter; notify the doctor; prepare for possible cystoscopy or surgical repair
- Electrolyte abnormalities: monitor for hyponatremia due to absorption of irrigating fluid; notify the doctor; restrict fluids; administer diuretics or hypertonic saline as ordered
- Erectile dysfunction: monitor for changes in sexual function; notify the doctor; provide emotional support; refer to counseling or treatment options as needed
- Retrograde ejaculation: monitor for dry orgasm or cloudy urine after ejaculation; notify the doctor; provide reassurance that this is not harmful and does not affect sexual pleasure; educate about fertility options if desired
Patient Education and Recovery Guidelines
- Educate the patient about the expected outcomes and possible complications of TURP
- Instruct the patient to avoid strenuous activities, heavy lifting, driving, sexual intercourse, constipation, or straining for 4 to 6 weeks after the surgery
- Instruct the patient to drink plenty of fluids, avoid caffeine and alcohol, and take stool softeners as needed to prevent dehydration and constipation
- Instruct the patient to report any signs of infection, bleeding, urinary retention, or incontinence to the doctor
- Instruct the patient to follow up with the doctor for regular check-ups and PSA
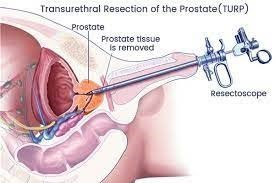
Summary
- Transurethral Resection of the Prostate (TURP) is a surgical procedure for treating benign prostatic hyperplasia (BPH).
- It involves the removal of excess prostate tissue using a resectoscope inserted through the urethra.
- TURP is performed to relieve urinary obstruction and improve urinary flow in men with BPH.
- Preoperative care includes patient assessment, medication administration, and obtaining informed consent.
- Intraoperative considerations involve anesthesia administration, monitoring, and assisting the surgeon.
- Postoperative care focuses on monitoring vital signs, catheter care, pain management, and preventing complications.
- Potential complications include hemorrhage, urinary tract infection, bladder spasms, and fluid electrolyte imbalances.
- Patient education covers self-care after TURP, including catheter care and incision care.
- Recovery guidelines advise avoiding strenuous activities and attending follow-up appointments.
- Overall, TURP is an effective procedure for improving urinary function and quality of life in men with BPH.
Conclusion
- Transurethral Resection of the Prostate (TURP) is a well-established surgical intervention for benign prostatic hyperplasia (BPH).
- It offers significant relief from urinary obstruction and improved urinary flow in affected individuals.
- TURP is a safe and effective procedure when performed by skilled surgeons and supported by comprehensive nursing care.
- Proper preoperative, intraoperative, and postoperative management is crucial to ensure successful outcomes and minimize complications.
- Patient education plays a vital role in promoting adherence to recovery guidelines and fostering optimal postoperative recovery.
- With its proven benefits and positive impact on patients' quality of life, TURP remains a valuable option in managing BPH.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Genito-Urinary System Disorders
This filled cannot be empty

