Please set your exam date
Care Of The Older Adult
Study Questions
Introduction
(Select all that apply.).
Explanation
The correct answer isA, B, C, and D.
The nurse should consider the older adults’ preferences and interests, cultural and ethnic backgrounds, cognitive and functional abilities, and income and education levels when designing a health promotion program for them.
These factors can affect the older adults’ motivation, participation, adherence, and outcomes of the program.For example, the nurse should tailor the program to match the older adults’ needs, values, beliefs, and expectations; assess their cognitive and functional status and provide appropriate interventions; and consider their financial and educational resources and barriers.
Choice E is wrong because the older adults’ age and gender are not sufficient factors to consider when designing a health promotion program.
Age and gender are not homogeneous categories that determine the health status or behavior of older adults.Rather, they are influenced by multiple biological, psychological, social, and environmental factors that vary among individuals.
Therefore, the nurse should not rely on stereotypes or assumptions based on age and gender alone.
A client who is 75 years old tells the nurse that he feels lonely and isolated since his wife died last year.He says he has no friends or family nearby and rarely leaves his home.
Which of the following interventions should the nurse suggest to help the client cope with his situation? (Select all that apply.).
Explanation
The correct answer is A, C, and E.
These interventions are aimed at helping the client cope with his situation by providing new opportunities for social connection, companionship, and support.According to the APA, loneliness is a cognitive discomfort or uneasiness from perceiving oneself to be alone.It can be caused by various factors such as physical isolation, lack of close confidants, personality factors, psychological disorders, cultural factors, or relationship loss.Loneliness can have negative effects on the physical and mental health of older adults, such as increased risk of cardiovascular disease, depression, anxiety, cognitive decline, and mortality.
Choice B is wrong because referring the client to a home health aide for assistance with daily activities does not address his emotional needs or help him cope with his loneliness.
It may even increase his sense of dependency and isolation.
Choice D is wrong because teaching the client some relaxation techniques to reduce stress and anxiety may be helpful for his mental well-being, but it does not address the root cause of his loneliness or help him establish meaningful social relationships.
Some nursing interventions for loneliness are:.
• Determining the patient’s available support system such as family and friends and nurturing their relationships to counteract loneliness.
• Providing therapy or counseling for the patient to address their emotional needs and coping skills.
• Supporting the patient to improve the quality of their existing relationships, working on their attitudes, expectations and skills around relationships.
• Providing new opportunities for social connection, such as group activities, volunteering, or online communities.
• Using psychological therapies such as mindfulness, lessons on friendship, robotic pets, and social facilitation software to reduce loneliness.
Normal ranges for vital signs in older adults are:.
• Temperature: 36.1°C to 36.8°C (97°F to 98.2°F).
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: less than 120/80 mm Hg.
A nurse is caring for an older adult client who has mild cognitive impairment. The client asks the nurse, “What day is it today?” Which of the following responses should the nurse give?
Explanation
The correct answer is A.
“It’s Monday, June 3rd.” The nurse should give the client factual and specific information to orient them to time and place.This can help reduce confusion and anxiety for the client who has mild cognitive impairment.
Choice B is wrong because it is dismissive and does not address the client’s question.
Choice C is wrong because it is sarcastic and may make the client feel ashamed or embarrassed.
Choice D is wrong because it is vague and does not provide direct information to the client.
Mild cognitive impairment (MCI) is a mild decline in single or multiple cognitive domains, while global cognition and basic activities of daily living remain intact.Nurses play an important role in early detection of MCI and providing care to maintain maximum independence for persons with MCI.Some of the nursing interventions for MCI include:.
• Assessing the patient’s environment and surroundings for the presence of hazards and removing them.
• Providing cues and reminders to help the patient remember important information and tasks.
• Encouraging the patient to engage in physical, cognitive, and social activities that can stimulate brain function and delay cognitive decline.
• Educating the patient and family about MCI, its causes, risk factors, symptoms, diagnosis, treatment, and prognosis.
• Referring the patient to appropriate resources and support services such as memory clinics, support groups, or counseling.
A nurse is conducting a physical assessment of an older adult client who has multiple chronic conditions.The client says, “I’m so tired of taking all these pills and going to all these appointments. What’s the point?” Which of the following statements should the nurse make?
Explanation
The correct answer is D.“Tell me more about what’s bothering you.” This statement demonstrates the nurse’s empathy, respect, and active listening skills, which are essential for effective communication with older adult clients.It also invites the client to express their feelings and concerns, which can help the nurse assess the client’s mental health, coping strategies, and social support.
Choice A is wrong because it is dismissive of the client’s feelings and does not address the underlying issues.It may also imply that the client has no reason to feel hopeless or depressed, which can make them feel misunderstood or judged.
Choice B is wrong because it is not empathetic but rather sympathetic.
Saying “I understand how you feel” may sound insincere or patronizing, especially if the nurse has not experienced the same situation as the client.It may also discourage the client from sharing more details about their feelings.
Choice C is wrong because it is threatening and coercive.
It may make the client feel guilty or fearful about their health condition, which can increase their stress and anxiety.It may also undermine the client’s autonomy and dignity, which are important for older adults.
Normal ranges for vital signs in older adults are similar to those in younger adults, except for blood pressure, which tends to increase with age due to arterial stiffness.The normal range for systolic blood pressure in older adults is 120-140 mmHg, and for diastolic blood pressure is 60-90 mmHg.
A nurse is educating an older adult client about sexuality and aging.Which of the following information should the nurse include?
Explanation
The correct answer isC.
Sexual expression and satisfaction are possible at any age.
This is because sexuality is not only about physical function, but also about feelings, desires, identity, intimacy and connection.Aging does not necessarily diminish these aspects of sexuality, and many older adults enjoy an active and fulfilling sex life.
Choice A is wrong because it assumes that sexual interest and activity decline with age for everyone, which is not true.Some older adults may experience a decrease in sexual desire or frequency due to various factors, such as health conditions, medications, stress, relationship issues or personal preferences, but others may maintain or even increase their sexual interest and activity as they age.
Choice B is wrong because it ignores the fact that aging does bring some physical changes that can affect sexual function and response.
For example, the vagina can become shorter, narrower and less lubricated, which can make vaginal penetration painful or uncomfortable for some women.
Men may experience erectile dysfunction or reduced firmness or size of their erections.These changes do not mean that sex is impossible or undesirable, but they may require some adjustments or alternative ways of expressing sexuality.
Choice D is wrong because it implies that sexual problems and concerns are inevitable with age, which is not true.
While some older adults may face challenges or difficulties in their sexual lives, others may not have any problems or concerns at all.
Moreover, many sexual problems and concerns can be prevented, treated or managed with the help of health care providers, counselors or therapists.Older adults should not accept sexual dissatisfaction as a normal part of aging, but rather seek help and support if they need it.
Physiological Changes with Aging
A nurse is assessing the skin of an older adult client. Which of the following findings is a normal age-related change in the integumentary system?
Explanation
The correct answer isD.
Decreased perspiration.This is because the sweat glands become less active with aging, resulting in reduced sweating and dryness of the skin.Decreased perspiration can also affect the body’s ability to regulate its temperature and may cause heat intolerance.
Choice A is wrong becauseincreased skin vascularityis not a normal age-related change in the integumentary system.In fact, the blood vessels in the skin become thinner and less elastic, resulting in decreased perfusion and a paler skin tone.
Choice B is wrong becausedecreased skin fragilityis not a normal age-related change in the integumentary system.On the contrary, the skin becomes thinner, less elastic, and more prone to splitting, cracking, and infections due to reduced collagen and elastin production, decreased mitosis in the epidermis, and lowered immunity.
Choice C is wrong becauseincreased sebaceous gland activityis not a normal age-related change in the integumentary system.Rather, the sebaceous glands produce less sebum, which contributes to the dryness and loss of moisture in the skin.
Normal ranges for some of the parameters related to the integumentary system are:.
• Skin thickness: varies depending on body location, but generally ranges from 0.5 mm to 4 mm.
• Skin elasticity: measured by the Cutometer device, which uses negative pressure to lift the skin and calculate its elasticity.
A higher value indicates more elastic skin.The average elasticity value for young adults is 0.82, while for older adults it is 0.57.
• Skin moisture: measured by the Corneometer device, which uses electrical capacitance to assess the hydration level of the stratum corneum (the outermost layer of the skin).
A higher value indicates more hydrated skin.The average moisture value for young adults is 62.8, while for older adults it is 51.3.
• Perspiration: measured by the Evaporimeter device, which uses a humidity sensor to detect the amount of water vapor lost from the skin surface.
A higher value indicates more perspiration.The average perspiration value for young adults is 13.9 g/m2/h, while for older adults it is 9.8 g/m2/h.
A nurse is teaching a group of older adults about the respiratory system changes that occur with aging. Which of the following statements should the nurse include? (Select all that apply.).
Explanation
The correct answer is A, B, C, and E.These statements reflect the respiratory system changes that occur with aging, such as decreased respiratory muscle strength, decreased lung elasticity and recoil, decreased cough and gag reflexes, and decreased ciliary action and mucus production.
These changes can impair gas exchange, increase the risk of infections, and reduce exercise capacity.
Choice D is wrong because it states the opposite of what happens with aging.
Vital capacity is the maximum amount of air that can be exhaled after a maximum inhalation.
Residual volume is the amount of air that remains in the lungs after a maximum exhalation.With aging, vital capacity decreases and residual volume increases due to the loss of lung elasticity and airway closure.
This reduces the amount of fresh air that can enter the lungs and increases the amount of stale air that remains in the lungs.
A nurse is caring for an older adult client who has dry skin and complains of feeling cold.
Which of the following statements should the nurse make?
Explanation
The correct answer is D.
“You should apply moisturizer to your skin after bathing.” This statement is based on the fact that dry skin is a common problem among older adults, especially in cold or dry weather.Applying moisturizer after bathing can help to lock in the moisture and prevent further water loss from the skin.
Choice A is wrong because drinking more water may not be enough to hydrate the skin if the skin barrier is impaired or damaged.Drinking water is important for overall health, but it does not directly affect the moisture content of the skin.
Choice B is wrong because avoiding soap and hot water when bathing may not be sufficient to prevent dry skin.
Soap can strip the natural oils from the skin, but so can hot water.It is recommended to use mild, non-soap cleansers and warm water instead of hot water when bathing.
Choice C is wrong because wearing layers of clothing to keep warm may not address the underlying cause of feeling cold.Older adults may feel cold more than usual due to various factors, such as thinning of the skin, decreased blood circulation, reduced muscle mass, or hormonal changes.
Wearing layers of clothing may help to maintain body temperature, but it does not treat the cause of feeling cold.
Normal ranges for skin moisture and body temperature vary depending on individual factors, such as age, health status, environment, and activity level.
However, some general guidelines are:.
• Skin moisture: The skin should feel soft and smooth, not rough or scaly.
The skin should not have cracks, flakes, or redness.The skin should have a normal color, not pale or grayish.
• Body temperature: The normal body temperature for adults is around 98.6°F (37°C), but it can vary slightly depending on the time of day, activity level, and other factors.A body temperature below 95°F (35°C) is considered hypothermia and requires immediate medical attention.
A nurse is educating an older adult client about the changes in hair and nails that occur with aging. Which of the following statements should the nurse expect the client to make?
Explanation
The correct answer is A.“I may notice my hair becoming thinner and grayer as I age.” This statement reflects the common changes in hair that occur with aging, such as reduced melanin production, slower growth rate, and smaller hair strands.
Choice B is wrong because nails do not grow faster and stronger with age, but rather more slowly and may become dull and brittle.
Choice C is wrong because hair does not become more oily and curly with age, but rather drier and finer.
Choice D is wrong because nails do not become smoother and shinier with age, but rather yellowed and opaque.
Normal ranges for hair and nail growth vary depending on factors such as genetics, nutrition, health conditions, and environmental exposure.
However, some general estimates are:.
• Fingernails grow about 3 mm per month and toenails grow about 1 mm per month.
• Hair grows about 0.5 inches per month and loses about 50 to 100 strands per day.
• Hair color changes from about 30% gray at age 50 to about 50% gray at age 70.
A nurse is reviewing the chest x-ray of an older adult client. Which of the following findings is a normal age-related change in the thorax?
Explanation
The correct answer is A.
Increased anteroposterior diameter.
This is a normal age-related change in the thorax that results from changes in the bones and muscles of the chest and spine.The ribcage becomes less flexible and more rounded, which increases the front-to-back dimension of the chest.
This can affect the lung function and breathing capacity of older adults.
Choice B is wrong because decreased kyphosis means reduced curvature of the spine, which is not a normal age-related change.In fact, kyphosis tends to increase with aging due to osteoporosis and vertebral compression fractures.
Choice C is wrong because increased lung expansion means greater ability to fill the lungs with air, which is not a normal age-related change.In fact, lung expansion tends to decrease with aging due to loss of elasticity and shape of the air sacs (alveoli) and weakening of the respiratory muscles.
Choice D is wrong because decreased calcification means reduced deposition of calcium in the tissues, which is not a normal age-related change.In fact, calcification tends to increase with aging, especially in the costal cartilages that connect the ribs to the sternum.
This can make the chest wall more rigid and less compliant.
Normal ranges for anteroposterior diameter vary depending on age, sex, height and weight, but generally it should be less than the transverse diameter (the side-to-side dimension of the chest).
A ratio of anteroposterior to transverse diameter greater than 0.9 is considered abnormal and may indicate chronic obstructive pulmonary disease (COPD).
A nurse is assessing a client who is 75 years old. Which of the following findings is most likely related to the decreased contractile strength of the myocardium in older adults?
Explanation
The correct answer is B. Decreased stroke volume.
Stroke volume is the amount of blood pumped by the left ventricle of the heart in one contraction.
The contractile strength of the myocardium determines how much blood is ejected with each beat.As people age, the myocardium becomes less elastic and less responsive to catecholamines, which can reduce the contractile force and lower the stroke volume.
Choice A is wrong because increased heart rate is not related to the decreased contractile strength of the myocardium, but rather to the decreased responsiveness of the baroreceptors, which regulate blood pressure.Older adults may have higher resting heart rates and lower maximum heart rates than younger adults.
Choice C is wrong because increased cardiac output is not related to the decreased contractile strength of the myocardium, but rather to the increased blood volume and cardiac workload that may occur with aging.Cardiac output is the product of stroke volume and heart rate, so a lower stroke volume would tend to decrease cardiac output.
Choice D is wrong because decreased peripheral resistance is not related to the decreased contractile strength of the myocardium, but rather to the decreased elasticity and increased stiffness of the arterial walls that may occur with aging.
Peripheral resistance is the opposition to blood flow caused by friction between the blood and the vessel walls.A higher peripheral resistance would increase the afterload on the heart and reduce the stroke volume.
Normal ranges for stroke volume are 60 to 100 mL/beat for men and 50 to 90 mL/beat for women.
Normal ranges for heart rate are 60 to 100 beats per minute for adults.
Normal ranges for cardiac output are 4 to 8 L/min for adults.
Normal ranges for peripheral resistance are 800 to 1200 dynes/sec/cm-for adults.
A nurse is teaching a group of older adults about the effects of aging on the cardiovascular system. Which of the following statements should the nurse include? (Select all that apply.).
Explanation
The correct answer is A, D, and E.
Here is why:.
A. “You may experience dizziness when you stand up quickly.” This is true because aging causes the arteries and arterioles to become less elastic and less able to adjust the blood pressure quickly when the posture changes.This can lead to a drop in blood pressure when standing up, which can cause dizziness or fainting.
D. “Your blood vessels may become stiffer and narrower.” This is true because aging causes the walls of the arteries and arterioles to become thicker and stiffer, which reduces their compliance and increases the resistance to blood flow.This can lead to high blood pressure, atherosclerosis, and other cardiovascular diseases.
E. “Your heart may skip some beats or have extra beats.” This is true because aging causes changes in the electrical system of the heart, which can result in arrhythmias such as atrial fibrillation, premature ventricular contractions, or sinus bradycardia.These can cause irregular heartbeats that may be felt as palpitations or skipped beats.
B. “Your blood pressure may drop when you are resting.” This is false because aging does not cause a decrease in blood pressure at rest.
In fact, aging tends to increase the systolic blood pressure (the pressure when the heart contracts) due to the stiffening of the arteries.The diastolic blood pressure (the pressure when the heart relaxes) may remain normal or decrease slightly, resulting in a widened pulse pressure (the difference between systolic and diastolic pressures).
C. “Your heart may beat faster when you exercise.” This is false because aging does not cause an increase in heart rate during exercise.
In fact, aging tends to decrease the maximum heart rate that can be achieved during exercise due to the reduced responsiveness of the heart to adrenergic stimuli.The older heart also takes longer to recover after exercise.
Normal ranges for blood pressure are less than 120/80 mmHg for adults of any age.Normal ranges for heart rate are 60-100 beats per minute for adults of any age, but the maximum heart rate decreases with age according to the formula 220 minus age.
A nurse is caring for a client who has dysphagia due to decreased esophageal motility.
Which of the following actions should the nurse take?
Explanation
The correct answer is B.
Instruct the client to tuck their chin when swallowing.
This action helps to prevent aspiration by closing off the airway and directing food and liquid into the esophagus.It also reduces the risk of food getting stuck in the throat or chest.
Choice A is wrong because thin liquids are more difficult to swallow and control for clients who have dysphagia due to decreased esophageal motility.They can easily enter the airway and cause choking or pneumonia.
Choice C is wrong because hot or spicy foods can irritate the esophagus and worsen the symptoms of dysphagia.They can also trigger reflux, which can damage the esophageal lining and cause narrowing or inflammation.
Choice D is wrong because elevating the head of the bed to 30 degrees during meals is not enough to prevent aspiration or regurgitation.The client should be sitting upright at 90 degrees or higher to facilitate swallowing and gravity.
Normal ranges for esophageal motility are:.
• Lower esophageal sphincter pressure: 10 to 45 mm Hg.
• Peristaltic amplitude: 30 to 180 mm Hg.
• Peristaltic duration: 2.5 to 6 seconds.
• Peristaltic velocity: 2 to 4.5 cm/s.
A nurse is reviewing the laboratory results of a client who is 80 years old.The nurse notes that the client has low levels of iron, calcium and vitamin B12. Which of the following statements by the client indicates an understanding of this finding?
Explanation
The correct answer is A.
“I need to eat more foods that are rich in these nutrients.” This statement indicates that the client understands that low levels of iron, calcium and vitamin B12 can be caused by inadequate dietary intake of these nutrients.Iron, calcium and vitamin B12 are mainly found in animal-based foods, such as meat, eggs, milk and cheese.A diet lacking in these foods can lead to vitamin deficiency anemia, which is a condition where the body produces fewer and larger red blood cells that cannot carry enough oxygen.
Choice B is wrong because supplements may not be necessary or sufficient to correct these deficiencies.
Supplements can also interact with other medications or have side effects.The client should consult with their healthcare provider before taking any supplements.
Choice C is wrong because gastric acid inhibitors can actually worsen vitamin B12 deficiency.
Gastric acid inhibitors are medications that reduce the amount of stomach acid produced.However, stomach acid is needed to release vitamin B12 from food and to help it bind to a protein called intrinsic factor, which is essential for its absorption in the intestines.
Therefore, taking gastric acid inhibitors can impair vitamin B12 absorption and lead to deficiency.
Choice D is wrong because reducing dairy consumption can further lower calcium intake.
Dairy products are a good source of calcium, which is a mineral that helps build and maintain strong bones and teeth.Calcium deficiency can lead to osteoporosis, which is a condition where the bones become weak and brittle.
Normal ranges for iron, calcium and vitamin B12 in the blood are:.
• Iron: 50 to 170 micrograms per deciliter (mcg/dL) for men; 40 to 150 mcg/dL for women.
• Calcium: 8.5 to 10.2 milligrams per deciliter (mg/dL).
• Vitamin B12: 200 to 900 picograms per milliliter (pg/mL).
A nurse is administering medications to a client who is 65 years old. The nurse knows that older adults are at increased risk for adverse drug reactions due to which of the following physiological changes?
Explanation
The correct answer is C.
Decreased liver function.Older adults are at increased risk for adverse drug reactions due to various physiological changes that affect the absorption, distribution, metabolism and excretion of drugs.One of these changes is the reduction in liver blood flow, size, drug-metabolizing enzyme content and function.This can result in slower or decreased metabolism of drugs, leading to higher plasma concentrations and increased risk of toxicity.
Choice A is wrong because older adults have decreased renal clearance, not increased.This means that drugs that are eliminated by the kidneys may accumulate in the body and cause adverse effects.
Choice B is wrong because older adults have decreased plasma protein levels, not increased.This means that drugs that are bound to plasma proteins may have higher free fractions and increased pharmacological effects.
Choice D is wrong because older adults have increased permeability of the blood-brain barrier, not decreased.This means that drugs that cross the blood-brain barrier may have enhanced central nervous system effects in older adults.
Normal ranges for liver function tests vary depending on the laboratory and the method used, but some common values are:.
• Alanine aminotransferase (ALT): 7-55 U/L.
• Aspartate aminotransferase (AST): 8-48 U/L.
• Alkaline phosphatase (ALP): 45-115 U/L.
• Total bilirubin: 0.1-1.2 mg/dL.
• Albumin: 3.5-5 g/dL.
Musculoskeletal System
A nurse is assessing a client who has osteoporosis. Which of the following findings should the nurse expect?
Explanation
The correct answer is D. Decreased height.
Osteoporosis is a condition that causes bones to become weak and brittle, making them more prone to fractures.One of the symptoms of osteoporosis is loss of height over time, due to compression or collapse of the vertebrae in the spine.
Choice A is wrong because osteoporosis causes decreased bone density, not increased.
Bone density is a measure of how much mineral is in the bone tissue.Low bone density means the bones are weaker and more likely to break.
Choice B is wrong because osteoporosis does not affect muscle mass directly.
Muscle mass is the amount of muscle tissue in the body.Muscle mass can decrease with age, inactivity, or certain diseases, but it is not directly related to bone health.
Choice C is wrong because osteoporosis does not cause decreased joint mobility, or the ability to move the joints freely.
Joint mobility can be affected by arthritis, injury, inflammation, or other conditions, but it is not a symptom of osteoporosis.
Normal ranges for bone density vary depending on age, sex, and ethnicity.
A common test for bone density is the dual-energy X-ray absorptiometry (DEXA) scan, which compares the patient’s bone density to that of a healthy young adult of the same sex.
The result is expressed as a T-score, which can range from normal (-1 or above) to osteopenia (-1 to -2.5) to osteoporosis (-2.5 or below).
A nurse is teaching a group of older adults about the effects of aging on the neurological system. Which of the following statements should the nurse include as correct? (Select all that apply.).
Explanation
The correct answer is A, B, and D.These statements reflect some of the effects of aging on the neurological system, such as slower reaction time, difficulty with learning new things, and loss of some of the sense of smell and taste.
Choice C is wrong because the number of neurotransmitters in the brain decreases with age, not increases.
Neurotransmitters are chemicals that help nerve cells communicate with each other.
Choice E is wrong because oxygen delivery to the brain cells decreases with age, not increases.
This is due to reduced blood flow and oxygen saturation in the brain.
Normal ranges for some of the neurological functions that change with age are:.
• Reaction time: increases from about 0.2 seconds in young adults to about 0.3 seconds in older adults.
• Learning ability: declines by about 10% per decade after age 40.
• Sense of smell: decreases by about 50% by age 80.
• Sense of taste: decreases by about 20% by age 70.
A nurse is caring for a client who has presbyopia. The client asks the nurse what this condition means. Which of the following responses should the nurse give?
Explanation
The correct answer isC.
It means that you have difficulty focusing on close objects due to changes in your lenses.Presbyopia is a natural, often annoying part of aging that affects your eyes’ ability to focus on nearby objects.It is caused by a hardening of the lens of your eye, which occurs with aging.
As your lens becomes less flexible, it can no longer change shape to focus on close-up images.As a result, these images appear out of focus.
Choice A is wrong because it describes glaucoma, a condition that causes increased pressure in your eyes that can damage your optic nerve and lead to vision loss.
Choice B is wrong because it describes cataracts, a condition that causes cloudy areas in your lenses that can impair your vision and make it difficult to see colors and details.
Choice D is wrong because it describes macular degeneration, a condition that causes damage to your retina that can cause loss of central vision and affect your ability to read, drive and recognize faces.
Normal ranges for presbyopia vary depending on the individual, but it usually becomes noticeable in your early to mid-40s and continues to worsen until around age 65.
You can correct the condition with eyeglasses or contact lenses.You might also consider surgery.
A nurse is performing a hearing test on a client who has presbycusis. The client asks the nurse what this condition means. Which of the following responses should the nurse give?
Explanation
The correct answer is B.
“It means that you have decreased ability to hear high-pitched sounds due to changes in your inner ear.” Presbycusis is the medical term for age-related hearing loss, which is the gradual and irreversible loss of hearing in both ears as a result of agingIt affects the ability to hear high-frequency sounds, such as speech, more than low-frequency sounds, such as background noisePresbycusis is caused by a combination of genetic, environmental and physiological factors that damage the inner ear or the auditory nerve over time.
Choice A is wrong because it describes tinnitus, which is a condition where you hear ringing or buzzing sounds in your ears that are not caused by external sources.Tinnitus can occur with presbycusis, but it is not the same thing.
Choice C is wrong because it describes otitis media, which is a condition where you have inflammation or infection in your middle ear that can cause pain, fever and temporary hearing loss.Otitis media is not related to aging and can be treated with antibiotics or surgery.
Choice D is wrong because it describes cerumen impaction, which is a condition where you have excess wax or foreign objects in your ear canal that can block your hearing.Cerumen impaction is not related to aging and can be removed by a doctor or a nurse.
Normal ranges for hearing vary depending on the frequency and the method of testing, but generally, a hearing threshold of 25 decibels (dB) or lower is considered normal for adults.A hearing threshold of 26 to 40 dB is considered mild hearing loss, 41 to 55 dB is considered moderate hearing loss, 56 to 70 dB is considered moderately severe hearing loss, 71 to 90 dB is considered severe hearing loss, and above 90 dB is considered profound hearing loss.
A nurse is educating a client who has anosmia about safety precautions at home. Which of the following instructions should the nurse give?
Explanation
The correct answer isA.
Use a smoke detector and carbon monoxide detector in every room.This is because anosmia is a loss of sense of smell that can be caused by many health-related conditions.People with anosmia might miss important warning odors such as smoke from a fire or natural gas leaks, which can pose a serious risk to their safety.
Therefore, using detectors in every room can help alert them to potential dangers and prevent accidents.
Choice B is wrong becauseavoiding using spices or herbs to enhance the flavor of foodis not a safety precaution, but rather a personal preference.
Some people with anosmia may find spices or herbs helpful to improve their appetite and enjoyment of food, while others may not.
It depends on the individual’s taste buds and preferences.
Choice C is wrong becausedrinking plenty of fluids to prevent dehydration and dry mouthis not specific to anosmia, but rather a general health advice for everyone.
Dehydration and dry mouth can affect anyone, regardless of their sense of smell, and can have various causes and consequences.
Drinking fluids can help maintain hydration and oral health, but it does not prevent or treat anosmia.
Choice D is wrong becausewearing protective eyewear when working with chemicals or dustis not directly related to anosmia, but rather to the protection of the eyes.Anosmia can be caused by toxic chemicals or environments that can damage the olfactory nerves or the brain, but wearing eyewear does not prevent this from happening.
It only protects the eyes from irritation or injury.
Wearing eyewear when working with chemicals or dust is a good practice for anyone, not just people with anosmia.
Genitourinary System
A nurse is assessing a client who is 75 years old and has a history of benign prostatic hyperplasia. Which of the following findings should the nurse expect?
Explanation
The correct answer is C. Decreased bladder capacity.
This is because benign prostatic hyperplasia (BPH) is a condition in which the prostate gland enlarges and compresses the urethra, the tube that carries urine out of the bladder.This can cause difficulty in emptying the bladder completely, leading to increased frequency and urgency of urination, especially at night.The bladder may also lose its elasticity and ability to hold urine as it becomes overstretched.
Choice A is wrong because BPH causes increased urinary frequency, not decreased.This is due to the reduced bladder capacity and the residual urine that remains in the bladder after urination.
Choice B is wrong because BPH does not affect urine concentration directly.However, some medications used to treat BPH, such as diuretics, may increase urine concentration by removing excess fluid from the body.
Choice D is wrong because BPH does not cause increased kidney size.However, untreated BPH can lead to complications such as urinary tract infections, bladder stones, and kidney damage due to backflow of urine or obstruction of urine flow.
Some additional information:.
• BPH is a common condition that affects about half of men over 50 and up to 90% of men over 80.
• BPH is not the same as prostate cancer, but it can have similar symptoms.Therefore, it is important to have regular check-ups and screenings to rule out cancer.
• BPH can be diagnosed by a physical exam, a rectal exam, a urine test, a blood test for prostate-specific antigen (PSA), and other tests such as ultrasound, cystoscopy, or urodynamic testing.
• BPH can be treated by medications, surgery, or other procedures depending on the severity of symptoms, the size of the prostate, and the presence of complications or other health conditions.
• BPH can be prevented or managed by maintaining a healthy lifestyle, such as exercising regularly, drinking enough fluids, avoiding caffeine and alcohol, and eating a balanced diet rich in fruits, vegetables, and protein.
A nurse is teaching a group of older adults about the effects of aging on the reproductive system. Which of the following statements should the nurse include as correct?
(Select all that apply.).
Explanation
The correct answer isA, C, D, and E.
Here is why:.
• Choice A is correct because women may experiencevaginal dryness and atrophy due to decreased estrogen levelsafter menopause.
This can cause pain during sexual activity and increase the risk of vaginal infections and irritation.
• Choice B is wrong because men may have difficulty achieving erection due todecreasedtestosterone levels, not increased.
Testosterone is the hormone that stimulates sexual desire and erectile function in men, and it declines with age.
• Choice C is correct because women may havecessation of menstruation and decreased fertility due to decreased ovarian functionafter menopause.
The ovaries stop producing estrogen and progesterone, and stop releasing eggs.
This means that women can no longer become pregnant naturally after menopause.
• Choice D is correct because men may havedecreased sperm production and quality due to decreased testicular functionwith age.
The testicles shrink in size and produce less sperm, which may also have lower motility and more abnormalities.
This can affect male fertility and sexual performance.
• Choice E is correct because both genders may havedelayed sexual response due to decreased blood flow and nerve sensitivitywith age.
The blood vessels and nerves that supply the genital organs become less efficient, resulting in longer time to achieve arousal, orgasm, and erection.
This can also affect sexual satisfaction and pleasure.
Normal ranges for reproductive hormones vary depending on age, gender, and laboratory methods.
However, some general values are:.
• Estrogen: 15 to 350 pg/mL for women; 10 to 40 pg/mL for men.
• Progesterone: 0.1 to 0.3 ng/mL for women; less than 1 ng/mL for men.
• Testosterone: 300 to 1000 ng/dL for men; 15 to 70 ng/dL for women.
A nurse is caring for a client who is 80 years old and has a urinary tract infection.The client reports feeling thirsty and having a headache.
Which of the following statements should the nurse make?
Explanation
The correct answer is A.“You should drink more fluids to prevent dehydration.” Dehydration is a common complication of urinary tract infections (UTIs) in the elderly, and it can cause headaches, confusion, fatigue, and increased risk of infection.Drinking more fluids can help flush out the bacteria from the urinary tract and prevent further complications.
Choice B is wrong because limiting fluid intake can worsen dehydration and kidney function.
Choice C is wrong because caffeinated beverages do not cause bladder irritation, although they may increase urine frequency.
Choice D is wrong because checking urine color and odor is not a reliable way to monitor for infection, as these can be affected by other factors such as diet, medication, or hydration status.
Normal ranges for urine output are about 800 to 2000 mL per day for adults, depending on fluid intake and other factors.Normal urine color is pale yellow to amber, and normal urine odor is mild and slightly aromatic.
A nurse is providing education to a client who is 65 years old and has erectile dysfunction. The client asks about the use of sildenafil (Viagra).
Which of the following statements should the nurse make?
Explanation
The correct answer is C.
“You may experience flushing, headache and nasal congestion as side effects.” Sildenafil (Viagra) is a medication that belongs to a group of drugs called phosphodiesterase 5 (PDE5) inhibitors.It works by relaxing the muscles and blood vessels in the penis, allowing more blood to flow and causing an erection when sexually stimulated.However, it can also cause some common side effects such as flushing, headache and nasal congestion.
These are usually mild and temporary, but they can be bothersome for some people.
Choice A is wrong because sildenafil is not a medication that can be taken as needed before sexual activity.It should be taken about an hour before sexual activity, and not more than once a day.
Taking it too often or too close to sexual activity can increase the risk of side effects or interactions with other drugs.
Choice B is wrong because sildenafil is not contraindicated for people who have a history of heart disease.However, it should be used with caution and under medical supervision, as it can lower blood pressure and interact with some medications that are used to treat heart conditions, such as nitrates and riociguat.
People who have heart disease should consult their doctor before taking sildenafil and follow their instructions carefully.
Choice D is wrong because sildenafil does not interact with grapefruit juice or alcohol.However, grapefruit juice and alcohol can affect the absorption and metabolism of sildenafil, which can make it less effective or increase the risk of side effects.
Therefore, it is advisable to limit or avoid grapefruit juice and alcohol while taking sildenafil.
Normal ranges: Sildenafil comes in different doses, ranging from 25 mg to 100 mg.The usual starting dose is 50 mg, but it can be adjusted depending on the response and tolerance of the individual.
The maximum dose is 100 mg per day.Sildenafil should not be taken more than once a day or within 24 hours of taking another PDE5 inhibitor.
A nurse is conducting a health screening for a group of older adults at a community center. The nurse notices that one of the women has sagging breasts and asks her about her breast health. Which of the following responses should the nurse expect from the woman?
Explanation
The correct answer is A.
“I have noticed that my breasts have become smaller and less firm as I age.” This is a normal and expected change in the breasts of older women, as the ligaments that support the breast tissue stretch and lose elasticity over time, and the breast fullness is compromised by the loss of fat and mammary ducts.Gravity, smoking, sunburn, and weight fluctuations can also contribute to breast sagging.
Choice B is wrong because it is not a response that reflects the woman’s awareness of her breast health, but rather a personal preference or difficulty.Wearing a supportive bra can help maintain breast shape and lift, but it cannot prevent or reverse sagging.
Choice C is wrong because it is not a response that indicates the woman has noticed any changes in her breasts due to aging, but rather a preventive measure that she performs to check for any abnormalities.Performing monthly breast self-examinations is recommended for all women, regardless of age or breast size.
Choice D is wrong because it is not a response that shows the woman has observed any changes in her breasts as she ages, but rather a screening tool that she uses to detect any signs of breast cancer.Having regular mammograms is advised for women over 40 years old, or earlier if they have a family history or other risk factors for breast cancer.
Normal ranges for breast size and shape vary widely among women, and there is no standard or ideal way that breasts should look.
However, some women may experience psychological distress or low self-esteem due to sagging breasts, and may seek cosmetic surgery to improve their appearance.Breast lift surgery can remove excess skin and lift the breasts to a higher position on the chest wall, and may also involve inserting implants to increase the volume of the breasts.
However, this procedure has risks and complications, and may not guarantee lasting results.
Therefore, women should consult with their doctors before deciding to undergo breast lift surgery.
Endocrine System
A nurse is assessing a client who has decreased thyroid function due to aging. Which of the following findings should the nurse expect?
Explanation
The correct answer isD. Dry skin.
Decreased thyroid function due to aging, also known as hypothyroidism, is a condition where the thyroid gland does not produce enough thyroid hormones.
Thyroid hormones regulate the body’s metabolism, temperature, and other functions.When there is not enough thyroid hormone, the body’s processes slow down and cause various symptoms.
Some of the symptoms of hypothyroidism in the elderly are:.
• Fatigue.
• Weight gain.
• Cold intolerance.
• Constipation.
• Dry skin.
• Hair loss.
• Muscle weakness.
• Joint pain.
• Depression.
• Memory problems.
Dry skin is a common symptom of hypothyroidism because thyroid hormones affect the skin’s moisture and elasticity.Low thyroid hormone levels can reduce the production of natural oils and cause the skin to become dry, flaky, and itchy.
Choice A is wrong becausetachycardia, or fast heart rate, is not a symptom of hypothyroidism.In fact, hypothyroidism can causebradycardia, or slow heart rate, because thyroid hormones affect the heart’s contractility and rhythm.
Choice B is wrong becauseweight lossis not a symptom of hypothyroidism.
On the contrary, hypothyroidism can causeweight gainbecause thyroid hormones regulate the body’s metabolism and energy expenditure.Low thyroid hormone levels can reduce the basal metabolic rate and cause the body to store more fat.
Choice C is wrong becauseheat intoleranceis not a symptom of hypothyroidism.
Instead, hypothyroidism can causecold intolerancebecause thyroid hormones affect the body’s temperature regulation and thermogenesis.Low thyroid hormone levels can reduce the production of heat and cause the body to feel cold.
The normal ranges for thyroid function tests are:.
• TSH: 0.4 - 4.0 mIU/L.
• Free T4: 0.8 - 1.8 ng/dL.
• Free T3: 2.3 - 4.2 pg/mL.
However, these ranges may vary depending on the laboratory and the population.Some studies suggest that the upper limit of normal for TSH may be higher in older adults.
Therefore, it is important to interpret thyroid function tests in the context of clinical symptoms and other factors.
A nurse is teaching a client who has diabetes mellitus about the effects of aging on the endocrine system. Which of the following statements should the nurse include?
(Select all that apply.).
Explanation
The correct answer is A, B, and C.
Here is why:.
• A.“You may need to increase your insulin dosage as you get older.” This is true because ageing can impair insulin secretion and action, leading to increased insulin resistance and reduced glucose tolerance.Additionally, ageing can affect the absorption, metabolism, and excretion of insulin and other medications, which may require dose adjustments.
• B.“You may experience more episodes of hypoglycemia as you get older.” This is true because ageing can impair the counter-regulatory response to hypoglycemia, which is the release of hormones such as glucagon, epinephrine, cortisol, and growth hormone that raise blood glucose levels.Older adults with diabetes may also have reduced awareness of hypoglycemic symptoms, such as sweating, trembling, hunger, and confusion.
• C.“You may have less energy and feel more tired as you get older.” This is true because ageing can reduce the production and activity of several hormones that affect energy metabolism, such as thyroid hormones, growth hormone, and sex hormones.
These hormones regulate basal metabolic rate, muscle mass, fat distribution, and physical performance.Reduced energy levels can also affect glucose control and quality of life in older adults with diabetes.
• D.“You may develop osteoporosis due to decreased growth hormone production.” This is false because osteoporosis is mainly caused by decreased estrogen or testosterone production in women and men, respectively.
Estrogen and testosterone are important for maintaining bone mass and preventing bone resorption.Growth hormone has a minor role in bone metabolism compared to sex hormones.
• E.“You may have difficulty coping with stress due to decreased cortisol production.” This is false because cortisol production does not decrease with ageing.
Cortisol is the main stress hormone that helps the body adapt to various challenges.In fact, ageing can increase cortisol levels due to chronic inflammation, psychological stress, or impaired feedback regulation.Elevated cortisol levels can have negative effects on glucose control, cardiovascular health, and cognitive function in older adults with diabetes.
Normal ranges for some hormones in older adults are:.
• Thyroid-stimulating hormone: 0.4–4.0 mIU/L.
• Free thyroxine: 9–19 pmol/L.
• Growth hormone: < 5 ng/mL.
• Insulinlike growth factor 1: 50–216 ng/mL.
• Cortisol: 5–25 mcg/dL.
• Testosterone: 300–1000 ng/dL (men), 15–70 ng/dL (women).
• Estradiol: < 20 pg/mL (men), < 10 pg/mL (women).
A nurse is caring for a client who has a wound infection. The nurse knows that aging affects the immune system in which of the following ways?
Explanation
The correct answer is A.
“Your wound may take longer to heal because of decreased inflammatory response.” Aging affects the immune system in several ways, such as:.
• The immune system becomes less able to distinguish self from nonself, which increases the risk of autoimmune disorders.
• Macrophages, which ingest bacteria and other foreign cells, destroy them more slowly, which may contribute to the higher incidence of cancer among older people.
• T cells, which remember antigens they have previously encountered, respond less quickly to them.There are also fewer white blood cells capable of responding to new antigens.
• The production of B and T cells in bone marrow and thymus is reduced, which affects the adaptive immunity.
• The function of lymph nodes and spleen is impaired, which reduces the ability to mount an effective immune response.
These changes result in a decreased inflammatory response, which is essential for wound healing.Inflammation helps to clear the infection, recruit immune cells, and promote tissue repair.
Therefore, older people may have slower wound healing due to aging of the immune system.
Choice B is wrong because aging does not increase nerve sensitivity.In fact, nerve endings may deteriorate with age, leading to reduced sensation and pain perception.
Choice C is wrong because aging does not decrease platelet aggregation.
Platelets are blood cells that help with clotting and prevent bleeding.Platelet function may be altered by aging, but not necessarily reduced.
Choice D is wrong because aging does not increase blood flow.Blood flow may decrease with age due to various factors, such as atherosclerosis, hypertension, and diabetes.Reduced blood flow may impair wound healing by limiting oxygen and nutrient delivery to the injured tissue.
A nurse is educating a client who is at risk for developing infections due to aging. The nurse should explain that aging affects the immune system by causing which of the following changes?
Explanation
The correct answer is C.
“Your T-cells become less effective and respond slower to antigens.”.
Some possible explanations for the answer are:.
• T-cells are a type of white blood cell that help the immune system fight infections by recognizing and destroying foreign invaders such as bacteria, viruses and cancer cells.
• Aging affects the immune system by causing several changes in the production, function and diversity of T-cells.These changes include thymic involution, mitochondrial dysfunction, genetic and epigenetic alterations, loss of proteostasis, reduction of the T-cell receptor (TCR) repertoire, naive-memory imbalance, T-cell senescence and lack of effector plasticity.
• Thymic involution is the gradual shrinking of the thymus gland, which is where T-cells mature and learn to distinguish self from non-self.This leads to a decrease in the number and quality of naive T-cells, which are essential for responding to new antigens.
• Mitochondrial dysfunction is the impairment of the energy-producing organelles in the cells, which affects the survival, activation and differentiation of T-cells.Aging causes oxidative stress, DNA damage and reduced autophagy in the mitochondria, which compromise their function and induce apoptosis or cell death.
• Genetic and epigenetic alterations are changes in the DNA sequence or expression of genes that regulate T-cell development, activation and function.Aging causes accumulation of mutations, chromosomal abnormalities and epigenetic modifications such as DNA methylation and histone acetylation in T-cells, which affect their gene expression and signaling pathways.
• Loss of proteostasis is the disruption of the balance between protein synthesis, folding, trafficking and degradation in the cells, which affects the quality and quantity of proteins involved in T-cell function.Aging causes increased protein misfolding, aggregation and degradation in T-cells, which impair their antigen recognition, cytokine production and cell cycle regulation.
• Reduction of the TCR repertoire is the decrease in the diversity and specificity of the receptors that recognize antigens on the surface of T-cells.
Aging causes clonal expansion of memory T-cells and contraction.
A nurse is reviewing the laboratory results of a client who has decreased adrenal function due to aging. Which of the following values should the nurse expect to find?
Explanation
The correct answer is B. Decreased sodium level.
This is because decreased adrenal function due to aging can lead to lower levels of aldosterone, a hormone that regulates sodium and potassium balance in the body.Lower aldosterone levels can cause sodium loss and potassium retention, resulting in hyponatremia (low sodium) and hyperkalemia (high potassium).
Choice A is wrong because decreased adrenal function due to aging can cause lower levels of cortisol, a hormone that regulates glucose metabolism and stress response.Lower cortisol levels can cause hypoglycemia (low glucose) and impaired ability to cope with stress.
Choice C is wrong because decreased adrenal function due to aging can cause higher levels of potassium, as explained above.
Choice D is wrong because decreased adrenal function due to aging can cause lower levels of glucose, as explained above.
Normal ranges for sodium, potassium, cortisol and glucose are:.
• Sodium: 135-145 mEq/L.
• Potassium: 3.5-5.0 mEq/L.
• Cortisol: 5-25 mcg/dL (morning); 3-16 mcg/dL (afternoon).
• Glucose: 70-110 mg/dL (fasting); <140 mg/dL (2 hours after meal).
Functional Status
A nurse is assessing the functional status of an older adult client using the Katz Index of Independence in Activities of Daily Living (ADLs).
Which of the following tasks is included in this tool?
Explanation
The correct answer isD.
Dressing.According to the Katz Index of Independence in Activities of Daily Living (ADLs), dressing is one of the six tasks that are used to assess the functional status of older adults.The other five tasks are bathing, toileting, transferring, continence, and feeding.These tasks are considered basic ADLs that reflect the client’s ability to perform self-care independently.
Choice A is wrong because preparing meals is not included in the Katz ADLs.Preparing meals is an example of an instrumental activity of daily living (IADL), which involves more complex skills such as using transportation, managing finances, and taking medications.
Choice B is wrong because taking medications is also an IADL, not a basic ADL.Taking medications requires cognitive abilities such as memory, judgment, and problem-solving.
Choice C is wrong because using transportation is another IADL, not a basic ADL.Using transportation involves planning, organizing, and navigating in the environment.
The Katz ADLs are scored from 0 to 6, with 6 indicating complete independence, 4 indicating moderate impairment, and 2 or less indicating severe functional impairment.The Katz ADLs are useful for measuring the client’s functional status across different settings and professionals.However, they have some limitations such as a ceiling effect, a fixed hierarchy of tasks, and a lack of sensitivity to changes in the level of assistance needed.
A nurse is planning interventions to improve the functional status of an older adult client who has arthritis and lives alone. Which of the following interventions should the nurse include?
(Select all that apply.).
Explanation
The correct answer isA, B, and D.
These interventions are aimed at improving the functional status of an older adult client who has arthritis and lives alone by providing social support, enhancing mobility and safety, and facilitating self-care.
• Choice A is correct because joining a support group for people with arthritis can help the client cope with the emotional and psychological aspects of the chronic condition, as well as provide peer education and resources.
• Choice B is correct because teaching the client how to use a walker and a shower chair can improve the client’s mobility, balance, and independence in performing activities of daily living (ADLs), as well as prevent falls and injuries.
• Choice D is correct because referring the client to a home health aide for assistance with ADLs can reduce the client’s burden and stress, as well as promote self-care and hygiene.
• Choice C is wrong because limiting fluid intake to prevent edema is not a recommended intervention for arthritis, as it can lead to dehydration, electrolyte imbalance, and kidney problems.The client should be encouraged to drink adequate fluids to maintain hydration and joint lubrication.
• Choice E is wrong because prescribing a low-dose aspirin regimen for pain relief is not within the scope of nursing practice, as it requires a physician’s order.
Moreover, aspirin may not be the most appropriate analgesic for arthritis, as it can cause gastrointestinal bleeding, allergic reactions, and interactions with other medications.The nurse should assess the client’s pain level and administer prescribed pain medications as needed.
Normal ranges for fluid intake are about 2 to 3 liters per day for adults, depending on age, weight, activity level, and climate.
Normal ranges for pain level are subjective, but generally a score of 0 to 3 on a 0 to 10 scale indicates mild pain, 4 to 6 indicates moderate pain, and 7 to 10 indicates severe pain.
A nurse is evaluating the functional status of an older adult client who has dementia and lives with a caregiver. The nurse asks the caregiver how the client manages instrumental activities of daily living (IADLs).
Which of the following statements by the caregiver indicates that the client needs assistance with IADLs?
Explanation
The correct answer is A.“He sometimes forgets to turn off the stove after cooking.”
This statement indicates that the client needs assistance with IADLs, which are tasks that allow an individual to live independently in a community and to take care of themselves and their home.They include cooking, cleaning, transportation, laundry, managing finances, and meal preparation.They require more complex planning and thinking than activities of daily living (ADLs), which are basic self-care tasks like bathing.
Choice B is wrong because watching TV and reading magazines are not IADLs, but leisure activities that do not affect the client’s ability to live independently.
Choice C is wrong because having trouble getting in and out of bed is not an IADL, but an ADL that involves functional mobility.
Choice D is wrong because getting confused when talking on the phone is not an IADL, but a communication problem that may affect the client’s social participation.
A nurse is educating an older adult client and a caregiver about the Lawton Instrumental Activities of Daily Living (IADLs) Scale. Which of the following statements by the nurse is appropriate?
Explanation
The correct answer isC.
“This scale evaluates your ability to perform complex tasks such as managing finances, shopping and doing housework.”.
According to the Lawton Instrumental Activities of Daily Living (IADL) Scale, it is an 8-item questionnaire that measures a person’s ability to engage in more complex activities that are necessary for functioning in community settings.
These activities include:.
• Using a telephone.
• Shopping.
• Food preparation.
• Housekeeping.
• Laundry.
• Mode of transportation.
• Responsibility for own medications.
• Ability to handle finances.
The scale can be administered by proxy, through interview, or as a self-report, and it can be scored from 0 (low function, dependent) to 8 (high function, independent) for women, and 0 to 5 for men.
Choice A is wrong because it describes basic tasks such as bathing, dressing and feeding, which are not part of the IADL scale.These tasks are measured by another scale called the Katz Index of Activities of Daily Living (ADL).
Choice B is wrong because it refers to cognitive function and memory skills, which are not directly assessed by the IADL scale.However, cognitive impairment may affect a person’s ability to perform IADLs.
Choice D is wrong because it relates to depression and anxiety, which are not the focus of the IADL scale.However, depression and anxiety may also affect a person’s ability to perform IADLs.
A nurse is caring for an older adult client who has multiple chronic diseases and takes several medications.
The nurse recognizes that these factors can affect the functional status of the client by:.
Explanation
The correct answer is A.
Increasing the risk of complications, adverse effects and polypharmacy.
Older adults with multiple chronic diseases and medications have more complex health and social care needs than those with fewer or no chronic conditions.They are more likely to experience functional limitations, such as difficulty with activities of daily living, mobility, safety and independence.They are also more likely to have complications from their diseases, adverse effects from their medications, and polypharmacy (the use of multiple medications that may interact with each other or cause harm).
Choice B is wrong because older adults with multiple chronic diseases and medications may have more need for assistive devices and adaptive equipment to help them cope with their functional limitations and improve their quality of life.
Choice C is wrong because older adults with multiple chronic diseases and medications may have reduced mobility, safety and independence due to their functional limitations and increased risk of falls, injuries and hospitalizations.
Choice D is wrong because older adults with multiple chronic diseases and medications may have more impact from environmental and psychosocial factors, such as socioeconomic status, education, health literacy, access to care, social support and caregiver burden.
Normal ranges for functional status can be measured by various tools, such as the Katz Index of Independence in Activities of Daily Living, the Lawton Instrumental Activities of Daily Living Scale, the Short Physical Performance Battery, the Timed Up and Go Test, and the Barthel Index.
These tools assess different domains of function, such as self-care, mobility, balance, strength and endurance.
The scores can range from 0 (complete dependence or impairment) to 100 (complete independence or performance) depending on the tool.
Cognitive Conditions
A nurse is assessing an older adult client who has been admitted to the hospital with pneumonia.
The nurse suspects that the client has developed delirium based on which of the following findings?
Explanation
The correct answer is B.
The client has a decreased level of consciousness and is difficult to arouse.
This is a sign of delirium, which is a fast-developing type of confusion that affects attention and awareness.
Delirium is often caused by a combination of factors, such as infection, medication, surgery or dehydration.
Delirium is more common in older adults, especially those with dementia or other chronic conditions.
Choice A is wrong because difficulty remembering recent events and conversations is more likely a sign of dementia, which is a slow and progressive decline in memory and other thinking skills.
Dementia can also increase the risk of delirium, but it is not the same condition.
Choice C is wrong because having a history of Alzheimer’s disease and taking donepezil daily does not necessarily mean that the client has delirium.
Alzheimer’s disease is a type of dementia that affects memory, language and behavior.
Donepezil is a medication that can help improve cognitive function in some people with Alzheimer’s disease.
However, neither Alzheimer’s disease nor donepezil can cause delirium by themselves.
Choice D is wrong because having a normal blood pressure and pulse rate does not rule out delirium.
Delirium can affect people with normal vital signs, as well as those with abnormal ones.
Delirium is more related to brain function than to cardiovascular function.
Normal ranges for blood pressure are less than 120/80 mmHg for systolic/diastolic pressure, and for pulse rate are 60 to 100 beats per minute.
However, these ranges may vary depending on age, health status and other factors.
A nurse is planning care for an older adult client who is at risk for developing delirium due to a urinary tract infection.
Which of the following interventions should the nurse include in the plan?
(Select all that apply.).
Explanation
The correct answer isA, C, and E.
Here is why:.
A. Administer antibiotics as prescribed.This is correct because antibiotics are the main treatment for urinary tract infections (UTIs), which can cause delirium in older adults.Antibiotics can help clear the infection and reduce the inflammation that affects the brain function.
B. Restrict fluids to prevent fluid overload.This is incorrect because restricting fluids can worsen dehydration, which is a risk factor for delirium.Fluids help flush out bacteria from the urinary tract and prevent constipation, which can also contribute to delirium.Older adults should drink enough fluids to keep their urine clear or pale yellow.
C. Provide frequent reorientation and reassurance.This is correct because delirium causes confusion, anxiety, and reduced awareness of surroundings.Reorientation and reassurance can help the person feel more secure and calm, and reduce the risk of agitation or wandering.Reorientation can include reminding the person of their name, date, time, and place, and using familiar objects or pictures.
D. Use restraints to prevent injury or wandering.This is incorrect because restraints can increase the risk of delirium by causing physical discomfort, emotional distress, and sensory deprivation.Restraints can also lead to complications such as pressure ulcers, infections, or injuries from struggling.Restraints should only be used as a last resort when other measures have failed to ensure safety.
E. Encourage family members to stay with the client.This is correct because family members can provide emotional support, comfort, and familiarity to the person with delirium.Family members can also help with communication, monitoring, and care coordination.Family involvement can reduce the duration and severity of delirium.
References:.
:Delirium - Symptoms and causes - Mayo Clinic.
:Urinary Tract Infection Induced Delirium in Elderly Patients: A Systematic Review - PMC Journal List.
:Urinary tract infections and dementia | Alzheimer’s Society.
:What is Delirium and its causes and related conditions?.
A nurse is caring for an older adult client who has delirium and is experiencing hallucinations.
Which of the following statements should the nurse make to the client?
Explanation
The correct answer is C. “I know this is scary for you.
I am here to help you.” This statement shows empathy and reassurance to the client who has delirium and is experiencing hallucinations.
The nurse should also use a calm and soothing voice, maintain eye contact, and orient the client to reality.
Choice A is wrong because it is dismissive and invalidating of the client’s experience.
It can also increase the client’s anxiety and agitation.
Choice B is wrong because it can encourage the client to focus on the hallucinations and reinforce their delusions.
It can also make the client more fearful and confused.
Choice D is wrong because it is unrealistic and unhelpful.
The client cannot ignore the hallucinations that are distressing to them.
They also need support and intervention to address the underlying cause of delirium.
Delirium is a disturbance of consciousness and a change in cognition that develop rapidly over a short period.
It can be caused by various factors such as medical conditions, medications, substance use or withdrawal, infections, dehydration, pain, or emotional stress.
Delirium can manifest as hyperactive, hypoactive, or mixed type, with different levels of arousal, psychomotor activity, and mood.
Nursing interventions for delirium include assessing the patient’s cognitive and functional ability, using non-pharmacological methods such as multi-component interventions, family involvement, and light therapy, and recognizing delirium as a medical emergency that requires frequent monitoring and advocacy.
General measures to support cerebral function, such as hydration, nourishment, and oxygen, are also important.
Physical restraints are used only as a last resort.
For more information on delirium nursing diagnosis and care management, please refer to these sources:.
A nurse is evaluating the effectiveness of interventions for an older adult client who has delirium.
Which of the following statements by the client indicates an improvement in the condition?
Explanation
The correct answer is C.
“I remember that you are my nurse and your name is Lisa.” This statement indicates an improvement in the condition of delirium, which is a temporary mental state characterized by confusion, anxiety, incoherent speech, and hallucinations.
Delirium can be caused by various factors, such as fever, infection, medication, surgery, or alcohol or drug use or withdrawal.
Delirium can have different types: hyperactive, hypoactive, or mixed.
Delirium can be distinguished from dementia by its acute and fluctuating onset, reduced awareness of surroundings, and poor thinking skills.
Choice A is wrong because “I don’t know where I am or what day it is.” indicates a lack of orientation to time and place, which is a sign of delirium.
Choice B is wrong because “I feel so sleepy all the time.
I just want to rest.” indicates a hypoactive type of delirium, which is characterized by reduced activity, sluggishness, and drowsiness.
Choice D is wrong because “I still hear voices sometimes, but they are not as loud.” indicates a presence of hallucinations, which is a symptom of delirium.
Normal ranges for cognitive function in older adults depend on various factors, such as age, education, culture, and health status.
However, some general indicators of normal cognition include being able to recall recent events, recognize familiar people and places, communicate clearly and coherently, and perform daily activities independently.
References:.
• Delirium - Symptoms and causes - Mayo Clinic.
• Delirium in elderly adults: diagnosis, prevention and treatment.
A nurse is educating a group of family caregivers about delirium in older adults.
Which of the following information should the nurse include in the teaching?
Explanation
The correct answer is B.
Delirium is a reversible condition that can be cured with proper treatment.
Delirium is a serious change in mental abilities that results in confused thinking and a lack of awareness of one’s surroundings.It usually comes on fast and can be caused by various factors, such as infection, medication, surgery, or alcohol or drug use or withdrawal.Delirium can often be prevented and treated by addressing the underlying causes and providing supportive care.
Choice A is wrong because delirium is not a chronic condition that causes progressive cognitive decline.
That description fits dementia, which is different from delirium.Dementia is a gradual loss of memory and other thinking skills due to damage or loss of brain cells.
Choice C is wrong because delirium is not a normal part of aging that does not require any intervention.
Delirium is a medical emergency that needs prompt attention and treatment.Delirium can have serious consequences, such as functional decline, institutionalization, and death.
Choice D is wrong because delirium is not a genetic condition that runs in families.Delirium is not inherited, but rather triggered by environmental factors or medical conditions that affect the brain.
Normal ranges for mental status assessment in older adults are based on standardized tools, such as the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA).
These tools measure various aspects of cognition, such as orientation, memory, attention, language, and executive function.
The MMSE has a maximum score of 30, and the MoCA has a maximum score of 26.
A score below 24 on the MMSE or below 18 on the MoCA may indicate cognitive impairment.
However, these tools are not diagnostic of delirium or dementia, and should be interpreted in the context of the patient’s history and clinical presentation.
Dementia
A nurse is caring for a client with Alzheimer’s disease who has difficulty remembering recent events.
Which of the following interventions is appropriate for the nurse to implement?
Explanation
The correct answer is B.
Provide the client with a calendar and a clock to promote orientation.This intervention helps the client with Alzheimer’s disease to maintain a sense of reality and reduce confusion by providing cues for time and date.
Choice A is wrong because asking the client to repeat information several times to enhance retention may increase frustration and anxiety for the client, as he or she may not be able to recall the information due to impaired memory.
Choice C is wrong because avoiding using reminiscence therapy as it may increase confusion is not supported by evidence.Reminiscence therapy is a type of intervention that involves recalling and sharing past experiences with others, which can improve mood, cognition, and socialization for clients with Alzheimer’s disease.
Choice D is wrong because correcting the client’s mistakes or inaccuracies to improve memory may also cause frustration and agitation for the client, as he or she may not be aware of the errors or may feel criticized or embarrassed.
Normal ranges for cognitive function can be assessed using tools such as the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA), which measure orientation, attention, memory, language, and executive function.
The MMSE has a maximum score of 30, with scores below 24 indicating cognitive impairment.The MoCA has a maximum score of 30, with scores below 26 indicating mild cognitive impairment.
A. Ask the client to repeat information several times to enhance retention.
B. Provide the client with a calendar and a clock to promote orientation.
C. Avoid using reminiscence therapy as it may increase confusion.
D. Correct the client’s mistakes or inaccuracies to improve memory.
A nurse is conducting a health history for a client who is suspected of having vascular dementia.
Which of the following factors should the nurse ask about?
(Select all that apply.).
Explanation
The correct answer isA, C and E.
These are the factors that the nurse should ask about when suspecting vascular dementia.
Vascular dementia is caused by different conditions that interrupt the flow of blood and oxygen supply to the brain and damage blood vessels in the brain.People with vascular dementia almost always have abnormalities in the brain that can be seen on MRI scans.These abnormalities can include evidence of prior strokes, which are often small and sometimes without noticeable symptoms.
Choice Ais correct becausehypertension(high blood pressure) is one of the risk factors for vascular dementia, as it can damage the small blood vessels in the brain and reduce blood flow.Controlling blood pressure may help lower the chances of developing vascular dementia.
Choice Bis wrong becausefamily history of Alzheimer’s diseaseis not a factor for vascular dementia, but for Alzheimer’s disease, which is a different type of dementia.Alzheimer’s disease is caused by abnormal protein deposits in the brain, not by impaired blood flow.
Choice Cis correct becausetransient ischemic attacks(TIAs), also known as mini-strokes, are another risk factor for vascular dementia, as they can damage brain cells and affect cognition.TIAs are temporary episodes of reduced blood flow to the brain, causing symptoms similar to a stroke but lasting only a few minutes or hours.
Choice Dis wrong becauseexposure to environmental toxinsis not a factor for vascular dementia, but for other types of dementia, such as Lewy body dementia or Parkinson’s disease dementia.These types of dementia are caused by abnormal protein deposits in the brain or nerve cell damage, not by impaired blood flow.
Choice Eis correct becausediabetes mellitusis another risk factor for vascular dementia, as it can damage the blood vessels and increase the risk of stroke and heart disease.Controlling blood sugar may help lower the chances of developing vascular dementia.
Sources:.
:Vascular Dementia: Causes, Symptoms, and Treatments | National Institute on Aging.
:Vascular dementia - Symptoms & causes - Mayo Clinic.
:causes of vascular dementia - NHS - NHS.
A. History of hypertension B.
Family history of Alzheimer’s disease C.
History of transient ischemic attacks D.
Exposure to environmental toxins E.
History of diabetes mellitus
A nurse is teaching a family caregiver about validation therapy for a client with Lewy body dementia who often hallucinates.
Which of the following statements by the caregiver indicates understanding of the teac
Explanation
The correct answer is A.
“I should acknowledge my loved one’s feelings and try to redirect their attention.” This statement indicates understanding of validation therapy, which is a way to approach older adults with empathy and understanding.
Validation therapy focuses on helping the person work through the emotions behind challenging behaviors, such as hallucinations, by listening, acknowledging, and rephrasing their feelings.Validation therapy also involves using reminiscence, sensory stimulation, and redirection to engage the person in a meaningful way.
Choice B is wrong because it contradicts validation therapy.
Confronting the person’s hallucinations and explaining that they are not real can increase their anxiety, confusion, and agitation.It can also damage the trust and rapport between the caregiver and the person with dementia.
Choice C is wrong because it also goes against validation therapy.
Ignoring the person’s hallucinations and changing the topic of conversation can make them feel dismissed, invalidated, and isolated.It can also prevent them from expressing and resolving their emotions.
Choice D is wrong because it is not part of validation therapy.
Agreeing with the person’s hallucinations and pretending that you see them too can reinforce their delusions and make them more persistent.It can also confuse the person and make them doubt your honesty and credibility.
Lewy body dementia is a progressive dementia that results from protein deposits in nerve cells of the brain.
It affects movement, thinking skills, mood, memory, and behavior.It is characterized by fluctuating cognition, visual hallucinations, parkinsonian symptoms, sleep disturbances, and autonomic dysfunction.
A. “I should acknowledge my loved one’s feelings and try to redirect their attention.” B.
“I should confront my loved one’s hallucinations and explain that they are not real.” C.
“I should ignore my loved one’s hallucinations and change the topic of conversation.” D.
“I should agree with my loved one’s hallucinations and pretend that I see them too.”
A nurse is planning care for a client with frontotemporal dementia who exhibits disinhibited and inappropriate behaviors.
Which of the following interventions should the nurse include in the plan?
Explanation
The correct answer is B.
Provide positive reinforcement when the client behaves appropriately.This is because positive reinforcement can help increase the frequency of desired behaviors and reduce the occurrence of inappropriate behaviors in clients with frontotemporal dementia (FTD) who exhibit disinhibition.Disinhibition is a common symptom of behavioral variant FTD (bvFTD), which is characterized by a deterioration in cognition and social behavior.
Choice A is wrong because restricting the client’s social interactions to prevent embarrassment can lead to social isolation, depression, and loss of self-esteem.Clients with FTD need social support and stimulation to maintain their quality of life.
Choice C is wrong because using physical restraints when the client becomes agitated or aggressive can increase the risk of injury, infection, and psychological distress.Physical restraints should only be used as a last resort when other interventions have failed and the client poses a serious threat to themselves or others.
Choice D is wrong because administering antipsychotic medications to control the client’s impulses can have adverse effects such as sedation, extrapyramidal symptoms, metabolic syndrome, and increased mortality.Antipsychotic medications should be used with caution and only when non-pharmacological interventions are insufficient or contraindicated.
Normal ranges for vital signs, blood tests, and other parameters are not applicable in this question.
A. Restrict the client’s social interactions to prevent embarrassment.
B. Provide positive reinforcement when the client behaves appropriately.
C. Use physical restraints when the client becomes agitated or aggressive.
D. Administer antipsychotic medications to control the client’s impulses.
A nurse is evaluating the effectiveness of cognitive stimulation therapy for a client with mild dementia.
Which of the following outcomes indicates that the therapy is beneficial?
Explanation
The correct answer isA.
The client reports improved mood and self-esteem.Cognitive stimulation therapy (CST) is a short-term programme for people with mild to moderate dementia that involves a wide range of activities aiming to stimulate thinking and memory, such as discussion, word games, puzzles, music and creative tasks.CST can improve certain aspects of dementia, such as memory, problem-solving, communication, quality of life, and mood.
Therefore, if the client reports improved mood and self-esteem after CST, it indicates that the therapy is beneficial.
Choice B is wrong because CST does not directly target independence in activities of daily living (ADLs), although it may have some indirect effects on functional abilities.
Choice C is wrong because CST is not designed to treat delirium or depression, which are different conditions from dementia.
Delirium is an acute state of confusion that can have various causes and requires medical attention.
Depression is a mood disorder that can affect anyone and may co-occur with dementia.Both delirium and depression may need different interventions than CST.
Choice D is wrong because CST does not specifically enhance executive function and attention, which are higher-order cognitive skills that involve planning, organizing, inhibiting, switching and focusing.Executive function and attention may be impaired in dementia, but they are not the main focus of CST.
Depression
A nurse is assessing an older adult client who has depression. Which of the following symptoms would the nurse expect to find? (Select all that apply.).
Explanation
The correct answer isB, C, D, and E.
These are common symptoms of depression in older adults, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Choice A is wrong becauseincreased appetite and weight gainare not typical signs of depression in older adults.In fact,decreased appetite and weight lossare more likely to occur in depressed older adults.
Normal ranges for appetite and weight vary depending on the individual’s height, body mass index, health status, and dietary needs.However, a general guideline is that older adults should consume about 30 calories per kilogram of body weight per day, and maintain a healthy weight that is neither too high nor too low.
A nurse is planning to screen an older adult client for depression using the Geriatric Depression Scale (GDS).
Which of the following statements is true about this tool?
Explanation
The Geriatric Depression Scale (GDS) is a screening tool used to identify symptoms of depression in older adults.
It was originally developed by J.A.Yesavage and colleagues in 1982.
It consists of questions that assess a person’s level of enjoyment, interest, social interactions, and more.
• Choice A is correct because the GDS consists of 30 yes/no questions that assess the client’s mood and cognitive function.
• Choice B is correct because the GDS has a cut-off score of 10, indicating a high risk of depression.A score of 0 to 9 indicates normal mood, while a score of 10 to 19 indicates mild depression and a score of 20 to 30 indicates severe depression.
• Choice C is correct because the GDS can be administered by the nurse, the client or a family member.
The GDS is a self-report instrument that uses a “yes/no” format, which makes it easy to complete by different people.
• Choice D is correct because the GDS takes about 15 minutes to complete and score.The GDS is a brief and simple tool that can be used in various settings, such as acute, long-term, and community settings.
• Choice E is correct because it summarizes all the previous choices.
Therefore, the GDS is a valid and reliable tool for screening depression in older adults.It has several advantages, such as being specific for psychiatric rather than somatic symptoms, being appropriate for healthy as well as medically ill adults and those with mild to moderate cognitive impairments, and being available in different forms and languages.
A nurse is providing psychoeducation to an older adult client who has depression and is prescribed an antidepressant medication.
Which of the following statements should the nurse include?
Explanation
The correct answer isE.
All of the above.
Here is why:.
• Choice A is wrong because antidepressant medications usually takeseveral weeksto show their full effects on mood and functioning.
Telling the client that they should start feeling better within a few days might create unrealistic expectations and discourage adherence to the treatment plan.
• Choice B is correct because alcohol can interact with antidepressant medications and cause adverse effects such as increased sedation, impaired coordination, increased risk of bleeding, and decreased effectiveness of the medication.
The client should avoid drinking alcohol while taking this medication to prevent these complications and optimize their recovery.
• Choice C is correct because stopping antidepressant medications abruptly can cause withdrawal symptoms such as nausea, headache, dizziness, anxiety, and mood swings.
The client should not stop taking this medication without consulting their doctor, who can advise them on how to taper off the medication safely and monitor their response.
• Choice D is correct because some antidepressant medications can cause stomach upset, nausea, or vomiting as side effects.
The client should take this medication with food to prevent or reduce these symptoms and improve their tolerance of the medication.
Therefore, the nurse should include all of these statements when providing psychoeducation to the client who has depression and is prescribed an antidepressant medication.
A nurse is providing cognitive-behavioral therapy (CBT) to an older adult client who has depression.“I can challenge my negative thoughts and replace them with more realistic ones.”.
Which of the following statements by the client indicates a positive outcome of the therapy?
Explanation
The correct answer isE.
All of the above.Cognitive-behavioral therapy (CBT) is a type of psychotherapy that helps you recognize and replace negative or unhelpful thought and behavior patterns that contribute to depression.CBT involves practical problem-solving and homework assignments to help you cope with or recover from challenging mental health conditions.
Some of the skills that CBT teaches you are:.
• Challenging your negative thoughts and replacing them with more realistic ones.This can help you reduce the cognitive distortions that make you feel hopeless, worthless, or guilty.
• Identifying the triggers that make you feel depressed and avoiding them.This can help you reduce the exposure to stressful or harmful situations that worsen your mood.
• Expressing your feelings and needs to others in a respectful way.This can help you improve your communication and interpersonal skills, and increase your social support.
• Setting realistic goals and rewarding yourself for achieving them.This can help you increase your motivation, self-esteem, and sense of accomplishment.
Choice A is wrong because it is only one of the skills that CBT teaches you, not the only one.
Choice B is wrong for the same reason.
Choice C is wrong for the same reason.
Choice D is wrong for the same reason.
Choice E is correct because it includes all of the skills that CBT teaches you.
Normal ranges for depression are not applicable here, as depression is not measured by a single scale or test.
However, some of the common tools that are used to assess depression are:.
• The Hamilton Rating Scale for Depression (HAM-D), which ranges from 0 (no depression) to 52 (severe depression).
• The Beck Depression Inventory (BDI), which ranges from 0 (no depression) to 63 (extreme depression).
• The Patient Health Questionnaire-9 (PHQ-9), which ranges from 0 (no depression) to 27 (severe depression).
A. “I can challenge my negative thoughts and replace them with more realistic ones.” B.
“I can identify the triggers that make me feel depressed and avoid them.” C.
“I can express my feelings and needs to others in a respectful way.” D.
“I can set realistic goals and reward myself for achieving them.” E.
All of the above
A nurse is providing social support and counseling to an older adult client who has depression and lives alone.
Which of the following interventions would be most appropriate for the nurse to implement?
Explanation
The correct answer isE.
All of the above.
Here is why:.
• Encouraging the client to join a support group or a community center for older adults is an appropriate intervention because it can help the client reduce social isolation, increase social support, and enhance self-esteem and coping skills.
• Arranging for home health care services or respite care for the client is an appropriate intervention because it can help the client maintain independence, safety, and quality of life at home, as well as provide relief for caregivers who may be stressed or overwhelmed.
• Educating the client about the signs and symptoms of depression and when to seek help is an appropriate intervention because it can help the client recognize and monitor their own mental health status, increase their awareness of available resources, and empower them to seek professional help when needed.
• Referring the client to a psychiatrist or a psychologist for further evaluation and treatment is an appropriate intervention because it can help the client access evidence-based pharmacological and psychological therapies for depression, such as antidepressant medications and cognitive-behavioral therapy.
Choice A is wrong because it is not enough to address the multifaceted needs of older adults with depression.
Choice B is wrong because it does not address the psychological aspects of depression.
Choice C is wrong because it does not address the social aspects of depression.
Choice D is wrong because it does not address the physical aspects of depression.
Normal ranges for depression screening tools vary depending on the tool used, but generally a higher score indicates a higher risk or severity of depression.For example, on the Geriatric Depression Scale (GDS), a score of 0 to 4 indicates normal mood, 5 to 8 indicates mild depression, 9 to 11 indicates moderate depression, and 12 or more indicates severe depression.On the Nurses’ Global Assessment of Suicide Risk (NGASR), a score of 0 to 3 indicates low risk, 4 to 6 indicates moderate risk, 7 to 9 indicates high risk, and 10 or more indicates extreme risk.
Psychosocial Changes
A nurse is assessing an older adult client who has recently retired from work.
Which of the following statements by the client indicates a positive psychosocial adjustment to retirement?
Explanation
The correct answer is B.
“I have more time to spend with my family and friends now.” This statement indicates a positive psychosocial adjustment to retirement because it shows that the client is enjoying the benefits of having more leisure time and social support.
The client is also likely to have a higher sense of well-being and life satisfaction.
Choice A is wrong because it suggests that the client is experiencing a loss of identity and purpose in life, which can lead to depression, anxiety, and low self-esteem.
The client may benefit from finding new ways to contribute to society, such as volunteering, mentoring, or pursuing hobbies.
Choice C is wrong because it implies that the client is bored and lacks direction, which can also affect their mental health negatively.
The client may need to structure their days and set small goals to stay motivated and engaged.
Choice D is wrong because it indicates that the client is missing their work environment and the challenges it provided, which can make them feel isolated and unfulfilled.
The client may need to find new sources of stimulation and challenge, such as learning new skills, taking classes, or finding an “encore” job.
According to some sources, adjusting to retirement can be a stressful process that involves going through stages of emotions, finding new purpose and meaning, managing stress, anxiety, and depression, looking after one’s health, and embracing change.Psychosocial interventions can support retirement well-being and adjustment by providing guidance, support, and coping skills.
A nurse is planning interventions for an older adult client who is preparing for retirement.
Which of the following interventions should the nurse include?
(Select all that apply.).
Explanation
The correct answer isA, C, and D.These interventions are consistent with the recommendations for retirement planning for older adults, which include setting realistic goals, seeking alternative income sources if needed, and maintaining a balanced schedule of activities that provide stimulation, satisfaction and purpose.
Choice B is wrong because it suggests the client to reduce social contacts and focus on personal interests.This is not a healthy intervention for older adults, as social isolation can lead to depression, cognitive decline, and poor quality of life.Older adults should be encouraged to join social groups or clubs that share common interests or values, as this can enhance their well-being and sense of belonging.
Choice E is wrong because it recommends the client to join social groups or clubs that share common interests or values.
While this is a good suggestion for older adults in general, it is not specific to retirement planning.Retirement planning involves preparing for the financial, emotional, and physical aspects of leaving work and transitioning to a new phase of life.
Joining social groups or clubs may be part of the retirement plan, but it is not an intervention that the nurse should include in the planning process.
A nurse is providing education to an older adult client who is considering retirement.
Which of the following statements by the nurse is appropriate?
Explanation
The correct answer is D.
“Retirement can be facilitated by planning ahead for retirement goals, finances and lifestyle.” This statement by the nurse is appropriate because it acknowledges the client’s autonomy and encourages the client to prepare for a successful transition to retirement.Planning ahead can help the client cope with the potential challenges and opportunities of retirement, such as income changes, social support, health issues, leisure activities, and personal identity.
Choice A is wrong because it does not provide any education or guidance to the client.
It merely states a possible psychological outcome of retirement, which may not be relevant or helpful to the client’s situation.
Choice B is wrong because it defines retirement rather than educates the client about it.
It also implies that retirement is a passive or negative event that may occur against the client’s will, which may not be accurate or empowering.
Choice C is wrong because it focuses only on the positive aspects of retirement and ignores the potential challenges or difficulties that the client may face.
It also assumes that the client has the resources and interest to pursue these activities, which may not be true.
Normal ranges for retirement age vary depending on the country, profession, and personal circumstances of the individual.However, some common factors that influence retirement age are life expectancy, health status, financial security, social security benefits, and personal preferences.
A nurse is evaluating an older adult client who has retired from work six months ago.
Which of the following statements by the client indicates a need for further intervention?
Explanation
The correct answer is C.
“I have been feeling depressed and lonely since I left my job.” This statement by the client indicates a need for further intervention because it suggests that the client is experiencing depression, which is a serious mood disorder that can affect the way a person feels, acts, and thinks.
Depression is not a normal part of aging, and it can be treated with counseling, medication, or other forms of therapy.
Depression can be caused by various factors, such as changes in the brain, life events, medical conditions, or substance use.
Depression in older adults may be difficult to recognize because they may have different symptoms than younger people.
For some older adults with depression, sadness is not their main symptom.They could instead be feeling more of a numbness or a lack of interest in activities.
Choice A is wrong because “I have joined a book club and a gardening club in my neighborhood.” This statement by the client indicates that the client is engaging in social and recreational activities that can enhance their well-being and prevent isolation.Social support and meaningful activities are important factors for healthy aging and mental health.
Choice B is wrong because “I have been taking online courses to learn new skills and hobbies.” This statement by the client indicates that the client is pursuing lifelong learning and personal growth, which can also improve their cognitive function and self-esteem.Learning new skills and hobbies can help older adults cope with life transitions and challenges, as well as provide them with a sense of purpose and achievement.
Choice D is wrong because “I have been volunteering at a local animal shelter twice a week.” This statement by the client indicates that the client is contributing to their community and caring for others, which can also boost their mood and self-worth.Volunteering can provide older adults with opportunities to connect with others, share their skills and talents, and make a positive difference in the world.
A nurse is caring for an older adult client who has retired from work due to health reasons.
Which of the following statements by the nurse demonstrates empathy and respect for the client?
Explanation
The correct answer isC.
“You can still find meaning and purpose in life after retirement.”.
This statement by the nurse demonstrates empathy and respect for the client because it acknowledges the client’s potential to cope with the transition and to pursue new goals and interests.Empathy is the ability to understand the personal experience of the patient without bonding with them, and it includes three dimensions: emotional, cognitive, and behavioral.Empathy is an important communication skill for a health professional, as it helps to elicit therapeutic change and to comprehend the needs of the health care users.
Choice A is wrong because it assumes how the client feels and may not reflect their actual emotions.
It also does not offer any support or encouragement to the client.
Choice B is wrong because it shows a lack of empathy and respect for the client’s situation.
It implies that the client should not have any negative feelings about retiring early and that they should be satisfied with what they have.
Choice D is wrong because it dismisses the client’s feelings and challenges as a normal part of aging.
It does not acknowledge the impact of retirement on the client’s identity and well-being.
Normal ranges for empathy vary depending on the context, culture, and profession of the health care provider.However, some studies have suggested that empathy scores tend to decline during medical training and practice, and that higher levels of empathy are associated with better patient satisfaction, adherence, and outcomes.
Therefore, it is important for health professionals to develop and maintain empathetic skills through education, training, and self-care.
Social Isolation
A nurse is assessing an older adult client who lives alone and has no relatives nearby. The nurse suspects that the client is experiencing social isolation.
Which of the following findings support this suspicion?
(Select all that apply.).
Explanation
The correct answer is A and D.
The client reports feeling lonely and depressed most of the time, and the client rarely attends social activities or events in the neighborhood.These are both signs of social isolation and loneliness, which are important, yet neglected, social determinants of the health of older adults.Social isolation is an objective absence or lack of social contact with others, whereas loneliness is defined as an undesirable subjective experience of unfulfilled social contacts and/or needs.Both can have serious negative effects on physical and mental health, such as cognitive decline, depression, heart disease, and even death.
Choice B is wrong because having difficulty hearing and wearing a hearing aid does not necessarily mean that the client is socially isolated or lonely.Hearing loss can be a risk factor for social isolation and loneliness, but it can be mitigated by using assistive devices, communicating effectively, and seeking support.
Choice C is wrong because having a history of hypertension and diabetes mellitus does not indicate that the client is socially isolated or lonely.
These are chronic conditions that can affect the quality of life of older adults, but they are not directly related to social isolation or loneliness.However, social isolation and loneliness can worsen these conditions by affecting blood pressure, immune system, and self-care.
Choice E is wrong because having poor hygiene and grooming habits does not imply that the client is socially isolated or lonely.
Poor hygiene and grooming habits can be a result of various factors, such as depression, dementia, physical disability, or lack of resources.
They can also affect the client’s self-esteem and social interactions, but they are not necessarily caused by social isolation or loneliness.
Normal ranges for blood pressure are less than 120/80 mmHg for adults, and for blood glucose are 70 to 100 mg/dL for fasting plasma glucose.
A nurse is planning interventions to prevent or reduce social isolation in older adult clients.
Which of the following interventions are appropriate for this purpose?
(Select all that apply.).
Explanation
The correct answer is A, B, C and D.These interventions are appropriate for preventing or reducing social isolation in older adult clients because they address the factors that can contribute to social isolation and loneliness, such as loss of social network, support system, preferences, interests, abilities, values, hearing, vision or mobility.
Choice E is wrong because restricting the clients’ access to media or technology that may cause stress or anxiety is not an effective way to prevent or reduce social isolation.Media or technology can be a source of information, communication and entertainment for older adults, and can help them stay connected with their family, friends and community.
Instead of restricting access, the nurse should help the clients use media or technology safely and appropriately, and provide them with alternative sources of positive stimulation.
Normal ranges for social isolation and loneliness are difficult to define because they are subjective and context-dependent experiences.However, some indicators of social isolation and loneliness include having few or no social contacts, feeling unhappy or dissatisfied with one’s social relationships, feeling disconnected from others or society, and having low levels of social support.Social isolation and loneliness can have serious negative impacts on the physical and mental health of older adults, such as increased risks of depression, cognitive decline, cardiovascular disease and mortality.
Therefore, it is important to assess and intervene for these conditions in older adult clients.
A nurse is caring for an older adult client who has been admitted to the hospital for pneumonia.
The client tells the nurse that he feels isolated and lonely since his wife died a year ago.
Which of the following responses by the nurse is appropriate?
Explanation
The correct answer is A.
“I’m sorry for your loss.
How have you been coping with your grief?.” This response by the nurse is appropriate because it acknowledges the client’s feelings, expresses empathy, and invites the client to share more about his situation.
This can help the client feel supported and validated.
Choice B is wrong because it minimizes the client’s loss and implies that he should not feel sad or lonely.
This can make the client feel dismissed and misunderstood.
Choice C is wrong because it assumes that the client feels comforted by the presence of the staff, who are not his family or friends.
This can make the client feel isolated and patronized.
Choice D is wrong because it suggests that the client should find new relationships to replace his wife, which can be insensitive and unrealistic.
This can make the client feel pressured and guilty.
A nurse is conducting a home visit for an older adult client who has mild cognitive impairment and lives with her daughter. The daughter tells the nurse that she is worried about her mother’s social isolation because she does not have any friends or hobbies.
Which of the following statements by the nurse is appropriate?
Explanation
The correct answer is A.
“Maybe you can enroll your mother in a day care program where she can interact with other older adults.” This statement by the nurse is appropriate because it suggests a possible solution to the client’s social isolation that is respectful of her preferences and needs.A day care program can provide opportunities for socialization, stimulation, and support for older adults with mild cognitive impairment.
Choice B is wrong because it assumes that the client can learn new skills or activities, which may not be realistic or enjoyable for her.
Choice C is wrong because it places the burden of socialization on the daughter’s friends or relatives, who may not be interested or available to spend time with the client.
Choice D is wrong because it does not address the client’s social isolation, but only provides a change of scenery.
Social isolation is a common problem among older adults, especially those who live alone or have cognitive impairment.It can lead to depression, anxiety, loneliness, and poor quality of life.Therefore, it is important for nurses to assess the social needs of older adult clients and provide appropriate interventions to enhance their social well-being.
Sexuality
A nurse is assessing the sexuality of an older adult client.
Which of the following statements by the client indicates a need for further education?
Explanation
The correct answer isD.
“I don’t need to worry about sexually transmitted infections at my age.” This statement indicates a need for further education because older adults are still at risk of contracting sexually transmitted infections (STIs) if they are sexually active and do not use protection.According to the National Institute on Aging, STIs can affect anyone who is sexually active, regardless of age, and some STIs may not have any symptoms.Therefore, older adults should use condoms or other barrier methods to prevent STIs, and get tested regularly if they have multiple partners or a new partner.
Choice A is wrong because it is a correct statement.
“I know that my sexual response may be slower or less intense as I age.” This statement shows that the client has realistic expectations about the normal changes in sexual function that occur with aging.As people age, their bodies change, and their sexual response may take longer or require more stimulation.This does not mean that they cannot enjoy sex or intimacy, but they may need to adapt to these changes and communicate with their partner.
Choice B is wrong because it is not necessarily a sign of a need for education.
“I sometimes feel depressed or anxious about my sexual performance.” This statement reflects the client’s emotional state, which can affect their sexuality and intimacy.Some older adults may feel insecure about their aging bodies, their sexual abilities, or their attractiveness to their partner.
These feelings are normal and understandable, but they can also interfere with sexual satisfaction and intimacy.
The client may benefit from counseling or therapy to address these feelings, but they do not indicate a lack of knowledge about sexuality.
Choice C is wrong because it is a correct statement.
“I use lubricants and different positions to make sex more comfortable.” This statement shows that the client is aware of some strategies to cope with the physical changes that can affect sexual comfort in older adults.For example, vaginal dryness is a common problem for older women, especially after menopause, and it can make sex painful or uncomfortable.Using lubricants can help reduce friction and increase pleasure.Similarly, changing positions can help avoid discomfort or injury caused by arthritis or other conditions that affect mobility or flexibility.
Normal ranges for sexual activity and satisfaction vary widely among older adults, depending on their individual preferences, health status, relationship status, and other factors.
There is no one right way to express sexuality or intimacy in older age, as long as it is safe, consensual, and enjoyable for both partners.
A nurse is planning interventions to enhance the sexuality of an older adult couple.
Which of the following interventions should the nurse include?
(Select all that apply.).
Explanation
The correct answer is A, B, and C.
These interventions are appropriate for enhancing the sexuality of an older adult couple because they address the effects of aging, chronic diseases, medications, and environmental factors on sexual function and intimacy.
The nurse should educate the couple about the normal physiological changes that occur with aging, such as decreased vaginal lubrication, erectile dysfunction, and longer refractory periods.
The nurse should also inform the couple about how certain medical conditions (such as diabetes, hypertension, arthritis, or depression) and medications (such as antihypertensives, antidepressants, or antihistamines) can affect sexual desire, arousal, and performance.
The nurse should encourage the couple to explore alternative ways of expressing intimacy and affection, such as cuddling, kissing, caressing, or oral stimulation.
The nurse should also provide the couple with a private, comfortable and safe environment for sexual activity, such as a quiet room with adequate lighting, temperature, and ventilation.
Choice D is wrong because prescribing medications or devices to improve sexual performance or satisfaction is not within the scope of nursing practice.
The nurse should refer the couple to a physician or a sex therapist if they need pharmacological or mechanical interventions for sexual dysfunction.
Choice E is wrong because discouraging the couple from discussing their sexual concerns or expectations is contrary to promoting healthy sexuality and intimacy.
The nurse should facilitate open and honest communication between the couple and their health care providers about their sexual needs, preferences, and goals.
The nurse should also provide the couple with accurate and reliable information and resources about sexuality in older adults.
Normal ranges for sexual function and satisfaction vary widely among individuals and couples depending on their age, health status, lifestyle, relationship quality, and personal values.
Therefore, the nurse should not impose any rigid or unrealistic standards or expectations on the couple.
Instead, the nurse should respect the couple’s autonomy and dignity and support them in achieving their optimal level of sexual well-being.
A nurse is caring for an older adult client who has a history of depression and low self-esteem.
The client tells the nurse, “I don’t feel attractive or desirable anymore. I don’t think anyone would want to have sex with me.” How should the nurse respond?
Explanation
The correct answer is B.
“Why do you say that?.
What makes you feel that way?.” This is an open-ended question that encourages the client to express their feelings and thoughts, and shows empathy and respect from the nurse.
The nurse can then explore the factors that contribute to the client’s low self-esteem and depression, and provide appropriate interventions and referrals.
Choice A is wrong because it is a false reassurance that does not address the client’s underlying issues.
It may also make the client feel invalidated or patronized.
Choice C is wrong because it dismisses the client’s sexual needs and implies that they are not important.
Sexuality is a basic human need and a source of pleasure and intimacy for many people, regardless of age.
Choice D is wrong because it suggests that the client’s appearance is the cause of their low self-esteem and depression, and that changing it will solve their problems.
This may reinforce the client’s negative self-image and make them feel more insecure.
Older adults who have depression and low self-esteem may benefit from nursing interventions such as:.
• Providing a safe and supportive environment that promotes trust and rapport.
• Assessing for risk factors and signs of depression, such as loss of interest, hopelessness, guilt, insomnia, appetite changes, suicidal ideation, etc.
• Assessing for physical, psychological, social, and environmental factors that may affect the client’s self-esteem and sexual function, such as chronic illness, medication side effects, cognitive impairment, abuse, isolation, stigma, etc.
• Educating the client about depression and its treatment options, including medication, psychotherapy, counseling, support groups, etc.
• Encouraging the client to participate in activities that enhance their mood, self-esteem, and social interaction, such as exercise, hobbies, volunteering, etc.
• Encouraging the client to express their feelings and concerns, and listening actively and empathically.
• Helping the client identify their strengths and achievements, and challenging their negative thoughts and beliefs about themselves.
• Helping the client set realistic and attainable goals, and providing positive feedback and reinforcement.
• Respecting the client’s sexual needs and preferences, and providing information and resources on sexual health and safety.
• Referring the client to appropriate professionals or agencies for further assessment and intervention if needed.
A nurse is teaching an older adult client about the myths and stereotypes that affect sexuality in later life.
Which of the following statements by the client indicates an understanding of the teachi
Explanation
The correct answer isA.
“I guess I shouldn’t let my age or society’s expectations limit my sexual expression.” This statement indicates that the client has a positive and realistic attitude about sexuality in later life, and does not let ageist sexual stereotypes affect their sexual health and wellness.
Choice B is wrong because it reflects a myth that sex is not important or appropriate for older adults.This myth can lead to internalized stigma and reduced sexual activity, which can have negative consequences for physical and mental health.
Choice C is wrong because it implies that the decline in sexual interest and ability is inevitable and unavoidable.
This is another myth that can discourage older adults from seeking help or exploring alternatives for their sexual problems.In fact, many factors can affect sexual function and satisfaction, such as medications, chronic conditions, lifestyle habits, relationship issues, etc., and some of them can be modified or treated.
Choice D is wrong because it suggests that older adults can only have sex with someone of the same age and marital status as them.
This is a stereotype that limits the diversity and expression of sexuality in later life.Older adults can have sex with anyone they choose, as long as it is consensual and safe.
A nurse is evaluating the effectiveness of interventions to enhance the sexuality of an older adult client.
Which of the following outcomes would indicate that the interventions were successful?
Explanation
The correct answer is A.
The client reports increased sexual satisfaction and enjoyment.This outcome would indicate that the interventions were successful in enhancing the sexuality of an older adult client, which is the way we experience and express ourselves sexually.Sexuality is often affected by one’s emotional and physical state, and normal aging brings physical changes that can sometimes interfere with the ability to have and enjoy sex.
Therefore, interventions that aim to improve sexual satisfaction and enjoyment are relevant and important for older adults.
Choice B is wrong because increased sexual response and function are not necessarily indicators of enhanced sexuality, as they may not reflect the feelings, desires, actions, and identity of the older adult client.Sexual response and function can also be influenced by physiological factors such as menopause, erectile dysfunction, or chronic health conditions, which may require medical treatment rather than nursing interventions.
Choice C is wrong because increased sexual identity and orientation are not outcomes of interventions to enhance sexuality, but rather aspects of one’s personal and social identity that are usually established earlier in life.
Sexual identity and orientation are not affected by aging or health conditions, and do not need to be improved or changed by nursing interventions.
Choice D is wrong because increased sexual feelings and desires are not sufficient to measure the effectiveness of interventions to enhance sexuality, as they may not translate into sexual satisfaction and enjoyment.Sexual feelings and desires can also vary depending on the context, the partner, the mood, or other factors that are not related to the interventions.
The normal ranges for sexual activity in older adults depend on various factors such as personal preferences, health status, relationship status, availability of partner, social norms, and cultural values.
There is no single or standard definition of what constitutes normal or healthy sexuality for older adults.
However, some general guidelines for promoting sexual health in older adults are:.
• Communicate openly and honestly with your partner about your sexual needs and expectations.
• Use lubricants, pillows, or other aids to make sex more comfortable and enjoyable.
• Explore different ways of expressing intimacy and affection.
Nursing Interventions
A nurse is assessing an older adult client who reports feeling lonely and isolated since retiring from work.
Which of the following questions should the nurse ask to assess the client’s psychosocial changes?
Explanation
The correct answer is A.
How do you spend your time during the day?.
This question is relevant to assess the client’s psychosocial changes because it can reveal the client’s level of activity, engagement, and satisfaction with their daily routine.Older adults may face various psychosocial challenges that can affect their well-being and social relationships, such as isolation, loss of identity, mistrust, guilt, and financial anxiety.
Asking about the client’s daily activities can help the nurse identify any signs of depression, anxiety, loneliness, boredom, or cognitive impairment that may require further intervention.
Choice B is wrong because it is not directly related to the client’s psychosocial changes.
Asking about hobbies or interests may provide some information about the client’s personality and preferences, but it does not address the client’s current emotional or social state.
Choice C is wrong because it is too specific and may not capture the full extent of the client’s social network and support.
Asking about friends or family members may indicate the client’s level of connectedness and attachment, but it does not explore the quality or frequency of those relationships.
Choice D is wrong because it is too broad and may not elicit useful information for the nurse.
Asking about coping strategies may be helpful to assess the client’s resilience and adaptability, but it does not focus on the client’s present psychosocial issues or needs.
Normal ranges for psychosocial changes in older adults are difficult to define, as they depend on various factors such as culture, personality, life experiences, health status, and environmental conditions.However, some general indicators of healthy psychosocial functioning in older adults include:.
• Having a positive self-image and a sense of purpose.
• Maintaining social contacts and meaningful relationships.
• Engaging in enjoyable and stimulating activities.
• Expressing emotions appropriately and seeking help when needed.
• Accepting changes and losses with grace and dignity.
• Demonstrating wisdom and integrity.
A nurse is planning care for an older adult client who has arthritis, hypertension and mild cognitive impairment.
Which of the following interventions should the nurse include in the care plan to promote health and wellness in this client?
(Select all that apply.).
Explanation
The correct answer is A, B, C and E.
Here is why:.
• Choice A is correct because range-of-motion exercises can help improve the mobility and flexibility of the joints affected by arthritis.
They can also reduce stiffness and pain, especially after long periods of inactivity.Some examples of range-of-motion exercises for knee arthritis are ball kicks, glute kicks, knee flexion exercises, and hamstring stretch.
• Choice B is correct because monitoring the client’s blood pressure and medication adherence is essential for managing hypertension, which is a common chronic condition among older adults.
Hypertension can increase the risk of cardiovascular complications, such as stroke and heart failure.Medication adherence can help lower blood pressure and prevent adverse effects from drug interactions or overdosing.
• Choice C is correct because providing the client with a calendar and a clock to orient them to time and date can help with mild cognitive impairment, which is a decline in memory and thinking skills that is not severe enough to interfere with daily life.
Mild cognitive impairment can affect the ability to remember appointments, events, or tasks.A calendar and a clock can serve as memory aids and reminders for the client.
• Choice D is wrong because referring the client to a social worker for financial assistance is not directly related to promoting health and wellness in this client.
While financial stress can affect the mental and physical health of older adults, it is not a priority intervention for this client who has arthritis, hypertension and mild cognitive impairment.The nurse should focus on interventions that address the client’s specific health needs and goals.
• Choice E is correct because teaching the client relaxation techniques and coping skills can help reduce stress and anxiety, which can worsen arthritis pain and inflammation, as well as blood pressure.
Relaxation techniques can include deep breathing, meditation, progressive muscle relaxation, or guided imagery.Coping skills can include positive self-talk, problem-solving, or seeking social support.
Normal ranges for blood pressure are:.
• Systolic: less than 120 mm Hg.
• Diastolic: less than 80 mm Hg.
A nurse is educating an older adult client and their caregiver about the normal aging process and health promotion strategies. The nurse wants to empower the client to participate in decision-making and self-care.
Which of the following statements should the nurse make?
Explanation
The correct answer is B.
“You have the right to make your own choices about your health care and lifestyle.” This statement reflects the principle ofautonomy, which means respecting the client’s right to self-determination and decision-making.The nurse should empower the client to participate in their own care and promote their dignity and independence.
Choice A is wrong because it implies that the client should be passive and obedient, which does not respect their autonomy or preferences.
Choice C is wrong because it suggests that the client is dependent and helpless, which does not foster their self-esteem or confidence.
Choice D is wrong because it indicates that the client has no control or influence over their health condition, which does not encourage their coping or adaptation.
Normal aging is a gradual process that involves changes in all body systems, but does not necessarily lead to disability or disease.Health promotion strategies for older adults include maintaining physical activity, nutrition, hydration, immunization, social interaction, cognitive stimulation, and safety.The nurse should also be aware of the psychosocial needs of older adults, such as resolving conflicts between integrity and despair, according to Erikson’s theory of development.
A nurse is evaluating the outcomes of interventions for an older adult client who has diabetes, depression and hearing loss. The nurse wants to support the dignity, autonomy and quality of life of the client.
Which of the following statements should the nurse make?
Explanation
The correct answer is B.
“You have done a great job managing your blood sugar levels and taking your medications.” This statement supports the dignity, autonomy and quality of life of the client by acknowledging their efforts and achievements in managing their chronic conditions.
It also reinforces positive behaviors and encourages self-care.
Choice A is wrong because it expresses pity and sympathy, which can undermine the client’s dignity and self-esteem.
It also does not address the client’s depression or hearing loss.
Choice C is wrong because it implies that the client is not doing enough to cope with their depression and hearing loss.
It also does not respect the client’s preferences and choices regarding their social activities.
Choice D is wrong because it is too directive and does not consider the client’s autonomy or reasons for not wearing their hearing aid.
It also does not address the client’s diabetes or depression.
Some of the nursing interventions for an older adult client who has diabetes, depression and hearing loss are:.
• Assessing the client’s physical, mental, emotional, social, and spiritual needs and providing individualized care.
• Promoting safety and preventing falls and injuries by removing environmental hazards, providing assistive devices, and educating the client on fall prevention strategies.
• Improving gas exchange and respiratory function by monitoring vital signs, oxygen saturation, breath sounds, and respiratory symptoms; administering oxygen therapy as prescribed; encouraging deep breathing and coughing exercises; and promoting hydration.
• Managing hypothermia by monitoring temperature, skin color, and sensation; providing warm clothing, blankets, and fluids; and avoiding exposure to cold environments.
• Promoting adequate sleep and improving sleep patterns by assessing sleep quality and quantity; providing a quiet, dark, and comfortable environment; avoiding caffeine, alcohol, and nicotine before bedtime; encouraging relaxation techniques; and avoiding daytime naps.
• Restoring bowel function and managing constipation by assessing bowel habits, stool characteristics, and abdominal distension; encouraging a high-fiber diet, adequate fluid intake, and regular exercise; administering laxatives or enemas as prescribed; and educating the client on bowel health.
• Preventing aspiration by assessing swallowing ability, oral hygiene, and dentition; providing soft, moist, and easy-to-chew foods; elevating the head of the bed during and after meals; instructing the client to tilt their head forward when swallowing; and monitoring for signs of aspiration such as coughing, choking, or wheezing.
• Preventing fluid imbalance by assessing fluid intake and output, weight changes, skin turgor, mucous membranes, and edema; encouraging adequate fluid intake according to the client’s needs and preferences; administering intravenous fluids as prescribed; and educating the client on signs of dehydration or fluid overload.
A. “I’m sorry that you have to deal with these health problems.
It must be hard for you.” B.
“You have done a great job managing your blood sugar levels and taking your medications.” C.
“You should be more active and socialize more with other people.
It will make you feel better.” D.
“You need to wear your hearing aid at all times.
It will help you communicate better.”
More questions on the topic
A nurse is reviewing the medication list of an older adult client who takes several medications for different health problems.
The nurse recognizes that polypharmacy in older adults can increase the risk of which of the following?
Explanation
The correct answer is A.
Adverse drug reactions.
Polypharmacy, which refers to the effects of taking multiple medications concurrently to manage coexisting health problems, is common among older adults.
It is defined as the regular use of at least five medications.
Polypharmacy can lead to an increase in geriatric syndromes, decrease in functional outcomes, and increased mortality.
One of the major risks of polypharmacy is adverse drug reactions, which are harmful or unintended effects of a medication that occur at normal doses.
Adverse drug reactions can result from drug-drug interactions, drug-disease interactions, drug-age interactions, or inappropriate prescribing.
Adverse drug reactions can cause symptoms such as confusion, dizziness, falls, bleeding, or organ damage.
They can also lead to hospitalizations, increased health care costs, and reduced quality of life.
Choice B is wrong because medication adherence, which is the extent to which patients take medications as prescribed by their health care providers, can actually decrease with polypharmacy.
This is because taking multiple medications can be complex, costly, and burdensome for older adults, especially if they have cognitive impairment or low health literacy.
Medication adherence can also be influenced by patients’ beliefs, preferences, and expectations about their medications.
Choice C is wrong because drug-drug interactions are not a risk of polypharmacy per se, but rather a cause of adverse drug reactions.
Drug-drug interactions occur when two or more drugs affect each other’s pharmacokinetics (absorption, distribution, metabolism, excretion) or pharmacodynamics (mechanism of action, efficacy, toxicity).
Drug-drug interactions can alter the therapeutic effects or safety of a medication.
Choice D is wrong because therapeutic effects are the intended or desired effects of a medication that benefit the patient’s health condition.
Therapeutic effects can decrease with polypharmacy due to drug-drug interactions that reduce the efficacy of a medication.
Therapeutic effects can also be diminished by prescribing cascade, which is a phenomenon where a new medication is prescribed to treat a symptom that is actually an adverse drug reaction of another medication.
Normal ranges for blood pressure are.
≤120/80.
mmHg for normal,.
120−129/80.
mmHg for elevated,.
130−139/80−89.
mmHg for stage 1 hypertension, and.
≥140/90.
mmHg for stage 2 hypertension.
A nurse is assessing an older adult client who has a history of falls.
Which of the following findings should the nurse identify as a risk factor for falls in older adults?
Explanation
The correct answer isD.
All of the above.All of these findings are risk factors for falls in older adults, according to the literature.
Some explanations for why each choice is a risk factor are:.
A. Orthostatic hypotension: This is a condition where blood pressure drops too much when getting up from lying down or sitting, causing dizziness, lightheadedness, or fainting.This can affect balance and increase the chance of falling.
B. Urinary frequency: This is a condition where one needs to urinate often, sometimes urgently.This can cause rushed movement to the bathroom, especially at night, which can lead to tripping, slipping, or losing balance.
C. Visual impairment: This is a condition where one has reduced or distorted vision, such as due to cataracts, glaucoma, macular degeneration, or diabetic retinopathy.This can affect depth perception, contrast sensitivity, and ability to detect obstacles or hazards in the environment.
Some normal ranges for these conditions are:.
• Orthostatic hypotension: A normal blood pressure change when standing up is less than 20 mmHg systolic (top number) or 10 mmHg diastolic (bottom number).
Orthostatic hypotension is defined as a drop of at least 20 mmHg systolic or 10 mmHg diastolic within 3 minutes of standing.
• Urinary frequency: A normal urinary frequency is about 4 to 6 times per day, depending on fluid intake and other factors.
Urinary frequency is considered abnormal if it is more than 8 times per day or more than 2 times per night.
• Visual impairment: A normal visual acuity is 20/20 or better with or without correction.
Visual impairment is defined as a visual acuity of 20/40 or worse in the better-seeing eye with best correction possible.
A nurse is providing discharge instructions to an older adult client who had a hip replacement surgery.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The correct answer is A.
“I will use a walker until I can walk without pain.” This statement indicates a need for further teaching because the client should use a walker or other assistive device until they have regained their balance, flexibility and strength, not just until the pain subsides.Using a walker too long or too little can affect the healing process and the stability of the new hip joint.
Choice B is correct because the client should avoid crossing their legs or bending their hip more than 90 degrees to prevent dislocating the new hip joint.
Choice C is correct because the client should sleep on their back with a pillow between their legs to keep the hip in a neutral position and prevent excessive internal or external rotation.
Choice D is correct because the client should apply ice to their hip if it becomes swollen or inflamed to reduce pain and inflammation.The client should also elevate their leg and notify their healthcare provider if they notice any signs of infection, such as fever, chills, redness, warmth or drainage from the incision site.
Normal ranges for hip replacement surgery recovery vary depending on the individual and the type of surgery, but some general guidelines are:.
• The client should be able to walk with a cane or crutches within 2 to 4 weeks after surgery.
• The client should be able to resume most daily activities within 6 to 12 weeks after surgery.
• The client should avoid high-impact activities, such as running, jumping or contact sports, for at least 6 months after surgery.
• The client should have regular follow-up visits with their healthcare provider and physical therapist to monitor their progress and adjust their treatment plan as needed.
The nurse is caring for an elderly patient who has been admitted with pneumonia.
The nurse knows that elderly patients are at increased risk for respiratory infections because of which of the following factors?
(Select all that apply.).
Explanation
The correct answer is A, B and C.
These are the factors that increase the risk of respiratory infections in elderly patients:.
• Decreased immune response: Elderly patients have a weaker immune system that makes them more susceptible to viral and bacterial infections.They also have a poor response to respiratory vaccines.
• Decreased chest wall compliance: Elderly patients have reduced elasticity of the lungs and chest wall, which makes it harder for them to breathe and expel mucus.
• Decreased alveolar surface area: Elderly patients have fewer and larger alveoli, which reduces the gas exchange area and oxygen diffusion capacity.
Choice D is wrong because decreased oxygen saturation is not a risk factor, but a consequence of respiratory infections.
Choice E is wrong because decreased bronchial dilation is not a specific factor for elderly patients, but a common feature of obstructive lung diseases.
Normal ranges for oxygen saturation are 95-100% and for bronchial dilation are variable depending on the type and severity of the disease.
The nurse is assessing an elderly patient’s skin turgor and notes that it is poor.
The nurse understands that this finding may be due to which of the following reasons?
Explanation
The correct answer is A.
Dehydration.
Poor skin turgor means that the skin takes longer to return to its normal position after being pinched or pulled.
This is a sign of dehydration, which means the body does not have enough fluid.
Dehydration can be caused by not drinking enough water, vomiting, diarrhea, fever, diabetes, or other conditions that affect fluid balance.
Choice B is wrong because malnutrition does not directly affect skin turgor.
Malnutrition means the body does not get enough nutrients from food.
This can cause various problems, such as weight loss, muscle wasting, poor wound healing, and infections.
However, malnutrition does not cause the skin to lose its elasticity.
Choice C is wrong because loss of subcutaneous fat does not cause poor skin turgor.
Subcutaneous fat is the layer of fat under the skin that helps insulate the body and store energy.
As people age, they tend to lose some subcutaneous fat, especially in the face and hands.
This can make the skin look thinner and more wrinkled, but it does not affect how quickly the skin snaps back after being pinched.
Choice D is wrong because reduced collagen fibers do not cause poor skin turgor.
Collagen is a protein that gives the skin its strength and structure.
As people age, they produce less collagen, which can make the skin sag and lose firmness.
However, collagen does not affect the skin’s ability to retain water and return to its normal shape after being stretched.
Normal ranges for skin turgor vary depending on the age and location of the skin.
In general, healthy skin should return to its normal position within 2 seconds after being pinched.
In children and young adults, skin turgor can be tested on the abdomen or forearm.In elderly people, skin turgor can be tested on the clavicle (collar bone), sternum (breastbone), forehead, or inner thigh.These sites are less affected by skin wrinkling and aging.
The nurse is teaching an elderly patient about nail care and hygiene. The nurse should instruct the patient to do which of the following?
(Select all that apply.).
Explanation
The correct answer isA, B, and E.
The nurse should instruct the patient to do the following:.
• Trim nails straight across and file edges smoothly.
• Soak nails in warm water before trimming to soften them.
• Report any signs of infection or inflammation around nails.
These are good practices for nail hygiene and health, especially for the elderly who may have dry, brittle or thickened nails.Trimming nails straight across and filing them prevents ingrown nails and reduces the risk of injury or infection.Soaking nails in warm water makes them easier to cut and less likely to crack or split.Reporting any signs of infection or inflammation around nails is important to prevent complications and get appropriate treatment.
Choice C is wrong because using a metal nail file or scissors to cut nails can damage the nail plate and cause splitting or tearing.Choice D is wrong because applying a clear nail polish to protect nails from cracking is unnecessary and may worsen nail health by trapping moisture and bacteria under the polish.
To maintain healthy nails, the elderly should also scrub the underside of their nails with soap and water, moisturize their nails and cuticles, avoid biting or chewing their nails, eat nutritious foods rich in calcium and vitamins B and C, and use sterilized nail grooming tools.
:Fingernail Care for the Elderly - assisting hands-il-wi.com:Fingernails: Do’s and don’ts for healthy nails - Mayo Clinic:Nail Hygiene | CDC - Centers for Disease Control and Prevention.
A nurse is planning care for an older adult client who has constipation due to decreased intestinal motility.
Which of the following interventions should the nurse include in the plan?
Explanation
Encourage fluid intake of at least 2 L/day.
This is because adequate hydration can help soften the stool and facilitate its passage through the intestines.Fluid intake should be increased gradually to avoid fluid overload or electrolyte imbalance.
Choice B is wrong because alow-fiber dietcan contribute to constipation by reducing the bulk and water content of the stool.
Fiber helps retain water in the stool and stimulate peristalsis.A high-fiber diet is recommended for clients who have constipation.
Choice C is wrong because astimulant laxativeshould not be used daily or for a long period of time, as it can cause dependence, dehydration, electrolyte imbalance, and damage to the intestinal mucosa.Stimulant laxatives should be used only as a last resort when other measures fail.
Choice D is wrong becausephysical activitycan help prevent constipation by increasing intestinal motility and blood flow.Physical activity should be encouraged for clients who have constipation, unless contraindicated by other conditions.
Normal ranges for fluid intake are about 2 to 3 L/day for adults, depending on age, weight, activity level, and climate.Normal ranges for fiber intake are about 25 to 38 g/day for adults, depending on age and sex.
A nurse is evaluating a client who is 70 years old for signs of dehydration.
Which of the following findings should the nurse expect?
Explanation
The correct answer is D.
Decreased mental status.Dehydration in elderly people can cause confusion, disorientation, or drowsiness due to the loss of water and electrolytes from the body.
These symptoms can affect the cognitive function and alertness of the client.Dehydration can also lead to complications such as kidney problems, electrolyte imbalances, or low blood pressure.
Choice A is wrong because increased skin turgor is not a sign of dehydration.
Skin turgor is the ability of the skin to return to its normal shape after being pinched or pulled.Dehydration causes decreased skin turgor, meaning the skin stays tented or wrinkled after being pinched.
Choice B is wrong because decreased pulse rate is not a sign of dehydration.Dehydration causes increased pulse rate, as the heart has to work harder to pump blood to the vital organs when there is less fluid in the body.
Choice C is wrong because increased urine output is not a sign of dehydration.Dehydration causes decreased urine output, as the kidneys try to conserve water and produce more concentrated urine.
The urine may also be darker in color than normal.
Normal ranges for fluid intake and output vary depending on age, weight, activity level, and health status.
However, a general guideline is to drink at least eight 8-ounce glasses of water per day and produce at least 30 mL of urine per hour.
A nurse is educating a client who is 60 years old about strategies to prevent orthostatic hypotension. Which of the following instructions should the nurse include?
(Select all that apply.).
Explanation
The correct answer is A, B, and D.These are some of the strategies to prevent orthostatic hypotension, which is a sudden drop in blood pressure caused by a change in posture, such as when a person stands up quickly.
Some explanations for the other choices are:.
• Choice C is wrong because drinking caffeinated beverages can cause dehydration, which can worsen orthostatic hypotension by reducing the fluid volume in the blood vessels.
• Choice E is wrong because increasing salt intake can raise blood pressure, but it can also cause fluid retention, which can strain the heart and kidneys.People with hypertension, heart failure, or kidney disease should limit their salt intake.
Some normal ranges for blood pressure are:.
• Systolic blood pressure (the top number) should be less than 120 mmHg for most adults.
• Diastolic blood pressure (the bottom number) should be less than 80 mmHg for most adults.
• Orthostatic hypotension is diagnosed when there is a drop of 20 mmHg or more in systolic blood pressure or 10 mmHg or more in diastolic blood pressure within 2 to 5 minutes of standing.
A nurse is caring for an older adult client who reports feeling cold most of the time.
The nurse knows that this is most likely due to which of the following physiological changes with aging?
Explanation
The correct answer is A.
Decreased metabolic rate.This is because the metabolic rate is the amount of energy that the body uses to maintain its functions, and it tends to decline with age due to various factors, such as loss of muscle mass, reduced activity, hormonal changes, and decreased thyroid function.
A lower metabolic rate means that the body produces less heat and therefore feels colder more easily.
Choice B is wrong because increased blood pressure is not a normal physiological change with aging, but rather a risk factor for cardiovascular diseases that can be influenced by lifestyle, genetics, and other factors.
Choice C is wrong because increased sweat gland activity is not a normal physiological change with aging, but rather a sign of hyperhidrosis, which is a condition that causes excessive sweating due to overactive sweat glands.Sweat glands actually decrease in number and function with age, which can impair thermoregulation and increase the risk of heat-related illnesses.
Choice D is wrong because decreased body fat is not a normal physiological change with aging, but rather a result of malnutrition, illness, or other causes.Body fat actually tends to increase with age, especially in the abdominal region, due to hormonal changes, reduced physical activity, and lower metabolic rate.
Body fat can act as an insulator and help maintain body temperature.
Normal ranges for metabolic rate vary depending on age, sex, body size, activity level, and other factors.
A general estimate for resting metabolic rate (RMR) is 10 calories per kilogram of body weight per day for men and 9 calories per kilogram of body weight per day for women.
However, this may not reflect the actual metabolic rate of an individual, as it does not account for the effects of food intake, exercise, or environmental factors.
Therefore, it is better to measure metabolic rate using indirect calorimetry or other methods that can capture these variables.
A nurse is assessing an older adult client who has sarcopenia.
The nurse knows that this condition is characterized by which of the following?
Explanation
The correct answer isB.
Loss of muscle mass and strength.Sarcopenia is a condition that affects older adults and causes a progressive decline in skeletal muscle mass, strength, and function.This can lead to an increased risk of falls, fractures, disability, and mortality.
Choice A is wrong because the loss of bone mass and strength is calledosteoporosis, not sarcopenia.Osteoporosis is a condition that affects the density and quality of bones, making them more prone to fracture.
Choice C is wrong because loss of joint flexibility and range of motion is calledarthritis, not sarcopenia.
Arthritis is a term that refers to inflammation of the joints, which can cause pain, stiffness, swelling, and reduced mobility.
Choice D is wrong because loss of skin elasticity and moisture is calledskin aging, not sarcopenia.
Skin aging is a process that involves changes in the structure and function of the skin, such as wrinkles, sagging, dryness, and decreased wound healing.
Normal ranges for muscle mass and strength vary depending on age, sex, body size, and physical activity level.However, some general indicators of sarcopenia include:.
• A muscle mass index (muscle mass divided by height squared) below 7.26 kg/m2 for men and 5.45 kg/m2 for women.
• A handgrip strength below 30 kg for men and 20 kg for women.
• A gait speed below 0.8 m/s for both sexes.
A nurse is planning care for an older adult client who has impaired tactile sensation due to aging.
Which of the following interventions should the nurse include?
(Select all that apply.).
Explanation
The correct answer isA, B, and C.
These interventions are appropriate for a client who has impaired tactile sensation due to aging.
• Ais correct because monitoring the client’s skin for signs of injury or infection can help prevent complications such as pressure ulcers, burns, or infections that might go unnoticed by the client due to reduced sensitivity.
• Bis correct because teaching the client to avoid exposure to extreme temperatures can protect the client from thermal injuries such as frostbite or heatstroke that might not be felt by the client due to diminished thermoreception.
• Cis correct because encouraging the client to use assistive devices for mobility and balance can enhance the client’s safety and independence by compensating for the loss of proprioception and kinesthesia that might impair the client’s coordination and stability.
• Dis wrong because providing the client with sensory stimulation such as massage or music is not directly related to impaired tactile sensation due to aging.While sensory stimulation might have other benefits for the client’s well-being, it does not address the specific problem of reduced touch perception.
• Eis wrong because advising the client to wear loose-fitting clothing and shoes is not helpful for a client who has impaired tactile sensation due to aging.In fact, loose-fitting clothing and shoes might increase the risk of falls or injuries by creating friction or slipping off the client’s body.
Normal ranges for tactile sensation vary depending on the type of stimulus, the location of the skin, and the method of testing.
However, some general guidelines are:.
• Vibration sense: normal threshold is less than 10 μm at 30 Hz on the fingertip.
• Temperature sense: normal threshold is less than 1°C difference between two stimuli on the forearm.
• Pressure sense: normal threshold is less than 10 g/mm2 on the fingertip.
• Pain sense: normal threshold is less than 0.5 g/mm2 on the fingertip.
The nurse is caring for an older adult client who has been diagnosed with benign prostatic hyperplasia (BPH). The client asks the nurse what causes this condition.
What is the best response by the nurse?
Explanation
The correct answer is B.
It is caused by a hormonal imbalance that stimulates the growth of prostate tissue.
• Choice A is wrong because BPH is not caused by an infection of the prostate gland.Prostate infections are called prostatitis and have different symptoms and treatments than BPH.
• Choice C is wrong because BPH is not caused by a genetic mutation that triggers abnormal cell division in the prostate.Prostate cancer is a malignant condition that involves uncontrolled cell growth in the prostate, but it is not the same as BPH.
• Choice D is wrong because BPH is not caused by an autoimmune disorder that attacks and damages the prostate tissue.Autoimmune disorders are conditions where the immune system mistakenly attacks healthy cells in the body, but they are not known to cause BPH.
The exact cause of BPH is unknown, but it is believed to be related to aging and hormonal changes in older men.The prostate gland grows throughout a man’s life, but it usually does not cause problems until later in life.Some factors that may increase the risk of BPH include family history, diabetes, heart problems, obesity, and prostate cancer.
BPH can cause symptoms such as difficulty urinating, frequent or urgent urination, weak or interrupted urine stream, dribbling at the end of urination, incomplete bladder emptying, nocturia (urination at night), urinary incontinence (leakage of urine), urinary retention (inability to urinate), blood in urine, and painful urination.These symptoms can affect the quality of life and lead to complications such as urinary tract infections, bladder stones, bladder damage, kidney problems, and acute urinary retention.
BPH can be diagnosed by a physical exam, medical history, and various tests such as urinalysis, urodynamic test, prostate-specific antigen (PSA) test, post-void residual test, and cystoscopy.
The treatment options depend on the severity of symptoms, the size of the prostate, and other health conditions.They include medications, surgery, and other procedures such as laser therapy or microwave therapy.Some natural treatments such as lifestyle changes, dietary supplements, and herbal remedies may also help with mild symptoms of BPH.
Normal ranges for some tests related to BPH are:.
• PSA test: The normal range for PSA levels is 0 to 4 nanograms per milliliter (ng/mL) of blood.
However, this range may vary depending on age, race, and other factors.Higher PSA levels may indicate prostate cancer or other prostate problems such as BPH or prostatitis.
• Post-void residual test: The normal range for post-void residual volume is less than 50 milliliters (mL) of urine.Higher volumes may indicate urinary retention or bladder dysfunction due to BPH or other causes.
• Urodynamic test: The normal range for urodynamic parameters such as bladder pressure, urine flow rate, and bladder capacity may vary depending on age, gender, and other factors.Abnormal values may indicate bladder obstruction or dysfunction due to BPH or other causes.
References:.
:What is Benign prostatic hyperplasia and its possible symptoms ….
The nurse is teaching an older adult client who has menopause about hormone replacement therapy (HRT). The client asks about the benefits and risks of HRT.
What should the nurse include in the teaching?
Explanation
The correct answer is A.
HRT can relieve hot flashes, vaginal dryness and mood swings, but it can also increase the risk of breast cancer, stroke and blood clots.This answer is based on the evidence from various studies that have shown the benefits and risks of HRT.
Choice B is wrong because HRT cannot prevent osteoporosis, heart disease and dementia, and it does not cause weight gain, acne and hair loss.These are common misconceptions about HRT that are not supported by scientific research.
Choice C is wrong because HRT does not have a significant effect on sexual function, skin elasticity and memory, and it does not lower the immune system, blood pressure and blood sugar.These are also myths about HRT that have no basis in reality.
Choice D is wrong because HRT can improve sleep quality, energy levels and mood, but it can also cause or worsen headaches, nausea and bloating.These are some of the possible side effects of HRT that vary depending on the type, dose and duration of the therapy.
Normal ranges for estrogen and progesterone levels depend on the stage of menopause, the type of HRT and the individual factors of each woman.
Generally, estrogen levels range from 10 to 50 pg/mL (picograms per milliliter) and progesterone levels range from 0.1 to 25 ng/mL (nanograms per milliliter) in postmenopausal women.
The nurse is reviewing the laboratory results of an older adult client who has a urinary tract infection (UTI).
Which of the following findings should alert the nurse to a possible complication of UTI in older adults?
(Select all that apply.).
Explanation
The correct answer isA, D, and E.
Here is why:.
A. Elevated white blood cell count.
This is a sign of infection and inflammation in the body, which can be caused by a UTI.An elevated white blood cell count can also indicate a complication of UTI such as pyelonephritis (kidney infection) or sepsis (blood infection).
D. Altered mental status.
This is a common symptom of UTI in older adults, especially those with dementia or other cognitive impairments.UTIs can cause confusion, agitation, delirium, or behavioral changes in the elderly due to the effects of infection and inflammation on the brain.
E. Positive urine culture.
This is the definitive test to diagnose a UTI, as it identifies the type and number of bacteria present in the urine.A positive urine culture confirms the presence of a UTI and guides the appropriate antimicrobial treatment.
The other choices are wrong because:.
•.
B. Decreased serum creatinine level.
This is not a sign of UTI or its complications.
Serum creatinine is a measure of kidney function, and it usually increases when the kidneys are damaged or impaired.A decreased serum creatinine level may indicate other conditions such as liver disease, muscle wasting, or malnutrition.
•.
C. Increased urine specific gravity.
This is not a sign of UTI or its complications.
Urine specific gravity is a measure of urine concentration, and it usually increases when the body is dehydrated or has high levels of solutes in the urine.An increased urine specific gravity may indicate other conditions such as diabetes mellitus, heart failure, or dehydration.
Normal ranges for some of these tests are:.
• White blood cell count: 4,000 to 11,000 cells per microliter (mcL) of blood.
• Serum creatinine: 0.6 to 1.2 milligrams per deciliter (mg/dL) for men and 0.5 to 1.1 mg/dL for women.
• Urine specific gravity: 1.005 to 1.030.
The nurse is caring for an older adult client who has an infection and a fever of 38°C (100.4°F).
The nurse should monitor the client for which of the following complications?
Explanation
The correct answer is D.
Delirium.
The nurse should monitor the client for delirium, which is a state of acute mental confusion that can be caused by fever, infection, dehydration, or medications.
Delirium can affect the client’s cognition, attention, orientation, memory, and behavior.It can also increase the risk of falls, complications, and mortality.
Choice A is wrong because dehydration is not a complication of fever, but rather a possible cause of fever.
Dehydration occurs when the body loses more fluid than it takes in, and it can impair the body’s ability to regulate its temperature.Dehydration is more common and dangerous in older adults because they have a lower volume of water in their bodies, a weaker thirst response, and may have conditions or medications that increase fluid loss.
Choice B is wrong because hypothermia is not a complication of fever, but rather a condition of abnormally low body temperature.
Hypothermia can occur when the body loses heat faster than it can produce it, such as in cold weather or water exposure.Hypothermia can affect the brain, heart, and other organs, and can lead to death if not treated promptly.
Choice C is wrong because seizures are not a common complication of fever in older adults.
Seizures are sudden episodes of abnormal electrical activity in the brain that can cause changes in movement, sensation, behavior, or consciousness.
Seizures can have various causes, such as head injury, stroke, infection, or epilepsy.
Fever-induced seizures are more likely to occur in young children than in older adults.
The nurse is providing discharge instructions to an older adult client who has diabetes mellitus and is taking oral hypoglycemic agents.
The nurse should advise the client to do which of the following?
Explanation
The correct answer is D.
Report any signs of infection or delayed wound healing.
This is because oral hypoglycemic agents lower the blood glucose level, but they do not prevent the complications of diabetes mellitus, such as impaired wound healing and increased susceptibility to infections.Therefore, the client should be advised to monitor for any signs of infection, such as fever, redness, swelling, or pus, and report them to the health care provider promptly.
Choice A is wrong because checking blood glucose levels at least four times a day is not necessary for most clients who are taking oral hypoglycemic agents.
The frequency of blood glucose monitoring depends on the type and dose of medication, the level of glycemic control, and the presence of other factors that may affect blood glucose, such as illness or stress.The client should follow the individualized plan prescribed by the health care provider regarding blood glucose monitoring.
Choice B is wrong because drinking plenty of fluids and avoiding caffeine is not specific to clients who are taking oral hypoglycemic agents.
This is a general recommendation for all clients who have diabetes mellitus, as dehydration and caffeine can worsen hyperglycemia and increase the risk of diabetic ketoacidosis or hyperosmolar hyperglycemic state.However, this alone is not sufficient to manage diabetes mellitus and prevent complications.
Choice C is wrong because eating small, frequent meals and avoiding simple sugars is also a general recommendation for all clients who have diabetes mellitus, as this can help to maintain a stable blood glucose level and prevent hypoglycemia or hyperglycemia.
However, this alone is not sufficient to manage diabetes mellitus and prevent complications.The client should also follow a balanced diet that includes complex carbohydrates, protein, fiber, and healthy fats, and consult with a dietitian or a diabetes educator for individualized dietary guidance.
The nurse is assessing an older adult client who has osteoporosis and reports frequent falls.
The nurse should ask the client about which of the following factors that could contribute to falls?
(Select all that apply.).
Explanation
The correct answer isA, B, C, and E.
The nurse should ask the client about medications, vision problems, home environment, and urinary incontinence as these are all factors that could contribute to falls in older adults.
• Medicationscan increase the risk of falls because they can cause side effects such as drowsiness, dizziness, confusion, or low blood pressure.Some medications that can increase the risk of falls include sedatives, antidepressants, antihypertensives, diuretics, and anticholinergics.
• Vision problemscan impair the ability to see obstacles, judge depth and distance, or adjust to changes in light.Some vision problems that can increase the risk of falls include cataracts, glaucoma, macular degeneration, and diabetic retinopathy.
• Home environmentcan pose safety hazards that can cause tripping, slipping, or losing balance.Some home hazards that can increase the risk of falls include loose rugs, clutter, poor lighting, slippery floors, uneven surfaces, and lack of handrails or grab bars.
• Urinary incontinencecan lead to rushed movements to the bathroom or frequent nighttime trips that can increase the risk of falls.Urinary incontinence can be caused by various factors such as bladder infections, prostate problems, pelvic floor weakness, or medication side effects.
Choice D is wrong because thyroid function is not a direct factor that contributes to falls in older adults.However, thyroid disorders such as hyperthyroidism or hypothyroidism can affect other factors such as muscle strength, bone density, heart rate, or blood pressure that can indirectly increase the risk of falls.
Normal ranges for thyroid function tests vary depending on the laboratory and the method used.However, a common reference range for thyroid-stimulating hormone (TSH) is 0.4 to 4.0 mIU/L and for free thyroxine (FT4) is 0.8 to 1.8 ng/dL.
A nurse is reviewing the results of a functional status assessment for an older adult client using the Katz Index of Independence in Activities of Daily Living (ADLs). The nurse notes that the client scored 4 out of 6 on this tool.
What does this score indicate?
Explanation
The correct answer is B.
The client needs assistance with two ADLs.This is because the Katz Index of Independence in Activities of Daily Living (ADLs) is a tool that measures the client’s ability to perform six basic ADLs independently: bathing, dressing, toileting, transferring, continence, and feeding.The score ranges from 0 to 6, with 6 indicating complete independence, 4 indicating moderate impairment, and 2 or less indicating severe dependence.The score is based on the number of ADLs that the client can perform without supervision, direction, personal assistance, or total care.
Therefore, a score of 4 out of 6 means that the client needs assistance with two ADLs.
Choice A is wrong because it implies that the client is independent in all ADLs, which would require a score of 6 out of 6.
Choice C is wrong because it implies that the client is dependent on others for all ADLs, which would require a score of 0 out of 6.
Choice D is wrong because it implies that the client has difficulty with four ADLs, which would require a score of 2 out of 6.
The normal range for the Katz Index of Independence in Activities of Daily Living (ADLs) depends on the setting and population of the client.For example, one study found that the average score for residents in skilled nursing facilities was 3.1 out of 6.Another study found that the hierarchy of difficulty of the six ADLs from least to greatest was: eating, maintaining continence, transferring, toileting, dressing, and bathing.
A nurse is conducting a functional status assessment for an older adult client using the Lawton Instrumental Activities of Daily Living (IADLs) Scale. The nurse asks the client about his ability to use transportation.
Which of the following questions is appropriate for this domain?
Explanation
The correct answer is A.“Do you drive your own car or use public transportation?.” This question is appropriate for the domain ofmode of transportation, which is one of the eight areas of occupational performance assessed by the Lawton Instrumental Activities of Daily Living (IADLs) Scale.The scale evaluates a person’s ability to engage in more complex activities thought necessary for functioning in community settings.
Choice B is wrong because it is not related to the domain of mode of transportation, but rather to the domain ofability to use a telephone.The scale asks about the person’s ability to operate a telephone, dial numbers, and answer calls.
Choice C is wrong because it is not related to the domain of mode of transportation, but rather to the domain ofshopping.The scale asks about the person’s ability to take care of all shopping needs independently, shop for small purchases, or need assistance with shopping.
Choice D is wrong because it is not related to the domain of mode of transportation, but rather to the domain ofmobility.The scale does not assess mobility directly, but it may be inferred from the person’s ability to travel by public transportation or car.
The Lawton IADLs Scale has a summary score that ranges from 0 (low function, dependent) to 8 (high function, independent) for women, and 0 to 5 for men.The score identifies areas of need in regard to care and support.
A nurse is implementing interventions to improve the functional status of an older adult client who has diabetes and hypertension.
Which of the following interventions should the nurse include?
(Select all that apply.).
Explanation
The correct answer isA, B, C and E.These interventions are consistent with the best practices for optimizing functional status in the elderly.
Some explanations for the choices are:.
• Choice A is correct because physical activity and exercise can help maintain muscle strength, joint mobility, balance and coordination, which are essential for functional independence and quality of life.
• Choice B is correct because adequate nutrition and hydration can prevent malnutrition, dehydration and electrolyte imbalance, which can impair physical and cognitive function and increase the risk of complications.
• Choice C is correct because managing chronic diseases and medications can prevent complications, adverse effects and polypharmacy, which can affect functional status and increase the need for health care services.
• Choice D is wrong because providing assistive devices and adaptive equipment is not an intervention to improve functional status, but rather to enhance mobility, safety and independence for patients who already have functional limitations.
The question asks for interventions to improve functional status, not to compensate for it.
• Choice E is correct because modifying the environment can reduce hazards, improve accessibility and facilitate self-care, which can promote functional independence and prevent injuries or falls.
The normal ranges for blood glucose and blood pressure for older adults with diabetes and hypertension are:.
• Blood glucose: 80-130 mg/dL before meals and less than 180 mg/dL after meals.
• Blood pressure: less than 140/90 mmHg or individualized based on comorbidities and risk factors.
A nurse is reviewing the medication list of an older adult client who has delirium.
Which of the following medications can contribute to delirium in older adults?
Explanation
The correct answer is B.
Diphenhydramine.Diphenhydramine is an antihistamine and sedative medication that can causedeliriumin older adults, especially when used in high doses or for a long time.Delirium is a serious change in mental abilities that results in confused thinking and reduced awareness of the surroundings.It can be caused by various factors, such as infections, medications, surgery, or alcohol or drug use or withdrawal.Delirium can have serious consequences, such as increased risk of falls, complications, and death.
Choice A is wrong because acetaminophen is a pain reliever and fever reducer that does not usually cause delirium in older adults.
However, acetaminophen overdose can cause liver damage and altered mental status.
Choice C is wrong because metformin is an oral medication that lowers blood sugar levels in people with type 2 diabetes.
Metformin does not typically cause delirium in older adults.
However, metformin can cause a rare but serious condition called lactic acidosis, which can cause confusion and other symptoms.
Choice D is wrong because lisinopril is an angiotensin-converting enzyme (ACE) inhibitor that lowers blood pressure and prevents heart failure.
Lisinopril does not usually cause delirium in older adults.
However, lisinopril can cause a rare but serious condition called angioedema, which can cause swelling of the face, tongue, or throat and difficulty breathing.
Normal ranges for some relevant laboratory tests are:.
• Albumin: 3.5-5.0 g/dL.
• Potassium: 3.5-5.0 mEq/L.
• Total cholesterol: <200 mg/dL.
• Hemoglobin: 13.5-17.5 g/dL for men; 12.0-15.5 g/dL for women.
A nurse is performing a mental status examination on an older adult client who has delirium.
Which of the following tools can the nurse use to assess the client’s attention span and concentration?
Explanation
The correct answer is D.
Digit Span Test (DST).
The DST is a tool that can be used to assess the client’s attention span and concentration by asking them to repeat a series of digits forward and backward (Martin, 1990).
The DST is part of the Mini-Mental State Examination (MMSE), which is a broader tool that covers other domains of cognitive functioning, such as orientation, memory, language, and visuospatial skills (Folstein et al., 1975).
Choice A is wrong because the MMSE is not a specific tool for attention span and concentration, but rather a general screening tool for cognitive impairment.
Choice B is wrong because the Confusion Assessment Method (CAM) is a tool that can be used to diagnose delirium, but not to assess attention span and concentration.
The CAM focuses on four features of delirium: acute onset and fluctuating course, inattention, disorganized thinking, and altered level of consciousness (Inouye et al., 1990).
Choice C is wrong because the Clock Drawing Test (CDT) is a tool that can be used to assess visuospatial skills and executive function, but not attention span and concentration.
The CDT requires the client to draw a clock face with numbers and hands indicating a specific time (Shulman et al., 1986).
Normal ranges for the DST vary depending on the age and education level of the client, but generally a score of 5 or more digits forward and 4 or more digits backward is considered normal (Martin, 1990).
A nurse is providing discharge instructions to an older adult client who has recovered from delirium and their family caregiver.
Which of the following recommendations should the nurse make to prevent recurrence of delirium?
(Select all that apply.).
Explanation
The correct answer isA, B and D.
Here is why:.
• Following up with the primary care provider regularly can help detect and treat any medical conditions that may cause or contribute to delirium, such as infections, electrolyte imbalances, or medication side effects.
• Avoiding alcohol and tobacco use can prevent delirium caused by intoxication or withdrawal, as well as improve overall health and cognitive function.
• Engaging in physical and mental activities daily can help maintain brain health, prevent cognitive decline, and reduce stress and boredom that may trigger delirium.
Choice C is wrong because taking over-the-counter sleeping pills as needed can increase the risk of delirium, especially in older adults.Sleeping pills can cause confusion, drowsiness, memory impairment, and falls that may lead to delirium.Instead of sleeping pills, it is better to have good sleep habits such as uninterrupted sleep, avoiding caffeine and naps, and having a regular bedtime routine.
Choice E is wrong because wearing glasses and hearing aids if prescribed can help prevent delirium, not cause it.Sensory impairment such as poor vision and hearing can make a person more prone to delirium, as they may feel disoriented, isolated, or misunderstood.Wearing glasses and hearing aids can help improve communication, orientation, and awareness of surroundings.
Delirium is a serious change in mental abilities that results in confused thinking and a lack of awareness of one’s surroundings.It usually comes on fast and can be caused by various factors such as fever, infection, surgery, medication, or emotional distress.
Delirium can often be prevented.
The nurse is caring for a patient who has had a spinal cord injury at level C5-C6 as a result of an automobile accident. The patient suddenly develops severe hypertension, throbbing headache, blurred vision, and bradycardia.
What is the priority nursing intervention?
Explanation
The correct answer is C.
Check for bladder distention or fecal impaction.
Autonomic dysreflexia is a disorder of autonomic nervous system dysregulation that occurs in patients with a spinal cord injury above T6.
It is caused by an exaggerated reflex response of the sympathetic nervous system due to an irritating stimulus below the spinal cord injury.It leads to severe hypertension and is a medical emergency.
Bladder or bowel distension are the most common triggers of autonomic dysreflexia.
Therefore, the priority nursing intervention is to check for bladder distention or fecal impaction and relieve them as soon as possible.
This can help to eliminate the stimulus and lower the blood pressure.
Choice A is wrong because administering antihypertensive medication as prescribed may not be effective or appropriate for autonomic dysreflexia.
The hypertension is caused by a reflex mechanism and not by a primary cardiovascular disorder.Moreover, antihypertensive drugs may cause hypotension once the stimulus is removed.
Choice B is wrong because elevating the head of bed to 90 degrees may not be enough to lower the blood pressure.It may also increase the risk of orthostatic hypotension once the stimulus is removed.However, sitting the patient upright and loosening any tight clothing are recommended as initial steps to reduce the blood pressure.
Choice D is wrong because applying a cooling blanket to lower body temperature is not indicated for autonomic dysreflexia.There is no evidence that body temperature is elevated or contributes to the hypertension in this condition.A cooling blanket may also cause vasoconstriction and worsen the hypertension.
Normal ranges for blood pressure vary depending on age, sex, and other factors.
However, a general guideline is that systolic blood pressure should be less than 120 mm Hg and diastolic blood pressure should be less than 80 mm Hg for most adults.
Normal ranges for heart rate also vary depending on age, activity level, and other factors.
However, a general guideline is that resting heart rate should be between 60 and 100 beats per minute for most adults.
References:.
The nurse is assessing a patient who has been diagnosed with multiple sclerosis (MS).
Which of the following findings is most consistent with this condition?
Explanation
Intention tremors and nystagmus.These are some of the common symptoms of multiple sclerosis (MS), a condition that affects the central nervous system and causes communication problems between the brain and the rest of the body.Intention tremors are involuntary shaking movements that occur when a person tries to perform a precise action, such as reaching for an object or writing.Nystagmus is a condition where the eyes make repetitive, uncontrolled movements, often resulting in reduced vision and depth perception.
Choice A is wrong because muscle atrophy and fasciculations are more typical of motor neuron diseases, such as amyotrophic lateral sclerosis (ALS), which affect the nerve cells that control voluntary muscle movements.
Choice C is wrong because flaccid paralysis and areflexia are signs of lower motor neuron lesions, which can be caused by spinal cord injuries, peripheral nerve disorders, or Guillain-Barré syndrome.
Choice D is wrong because hyperactive reflexes and spasticity are signs of upper motor neuron lesions, which can be caused by stroke, traumatic brain injury, or cerebral palsy.
Normal ranges for some of the symptoms mentioned are:.
• Intention tremors: none or minimal.
• Nystagmus: none or minimal.
• Muscle atrophy: none or minimal.
• Fasciculations: none or minimal.
• Flaccid paralysis: none or minimal.
• Areflexia: absent or reduced reflexes.
• Hyperactive reflexes: normal or slightly increased reflexes.
• Spasticity: normal or slightly increased muscle tone.
A. Muscle atrophy and fasciculations B.
Intention tremors and nystagmus C.
Flaccid paralysis and areflexia D.
Hyperactive reflexes and spasticity
A nurse is providing discharge teaching for a patient who had a seizure disorder and is prescribed phenytoin (Dilantin).
Which of the following instructions should the nurse include?
(Select all that apply.).
Explanation
The correct answer is B, C, and E.
Phenytoin (Dilantin) is an anticonvulsant medication that is used to control seizures.
It can have several side effects, some of which are serious and require medical attention.
Here are some explanations for each choice:.
A. Avoid drinking grapefruit juice while taking this medication.
This iswrongbecause grapefruit juice does not interact with phenytoin.However, grapefruit juice can affect the levels of other medications, such as statins, calcium channel blockers, and some antidepressants.
B. Brush your teeth gently with a soft-bristled toothbrush.This isrightbecause phenytoin can causegingival hyperplasia, which is an overgrowth of the gums that can lead to bleeding, infection, and difficulty chewing.
To prevent this, patients should practice good oral hygiene, avoid alcohol and tobacco, and see a dentist regularly.
A. Avoid drinking grapefruit juice while taking this medication B.
Brush your teeth gently with a soft-bristled toothbrush C.
Wear a medical alert bracelet or necklace at all times D.
Stop taking this medication if you develop a rash or fever E.
Have your blood levels checked regularly as directed by your provider
A nurse is caring for an older adult client who has depression and reports having chronic pain in his lower back.
Which of the following actions should the nurse take?
Explanation
The correct answer isD.
All of the above.
The nurse should take all of the actions listed to provide effective pain management for the older adult client who has depression and chronic pain in his lower back.
• Choice Ais correct because assessing the pain using a valid and reliable pain scale is essential for determining the severity and impact of pain, as well as monitoring the response to treatment.
• Choice Bis correct because administering analgesic medications as prescribed can help reduce pain and improve function.
The nurse should also monitor for effectiveness and side effects, especially in older adults who may have altered drug metabolism, polypharmacy, and increased risk of adverse events.
• Choice Cis correct because providing non-pharmacological interventions can enhance pain relief, reduce medication use, and address the biopsychosocial aspects of pain.
Massage, heat or cold therapy, relaxation techniques, and distraction are some examples of non-pharmacological interventions that can be used for chronic pain in older adults.
• Choice Dis correct because it includes all of the above actions, which are part of a multimodal approach to pain management that is recommended by clinical guidelines.
4 7 A multimodal approach can improve pain outcomes, reduce side effects, and address the complex needs of older adults with chronic pain.
A. Assess the location, intensity, quality and duration of the pain using a pain scale B.
Administer analgesic medications as prescribed and monitor for effectiveness and side effects C.
Provide non-pharmacological interventions such as massage, heat or cold therapy, relaxation techniques or distraction D.
All of the above
A nurse is evaluating an older adult client who has depression after four weeks of treatment with an antidepressant medication.
Which of the following findings would indicate that the medication is effective?
Explanation
The correct answer is D.
All of the above.
This is because all of these findings indicate that the client has experienced an improvement in mood, energy, appetite, sleep, interest and participation in social activities and hobbies, which are common signs of depression recovery.
Choice A is wrong because it only covers some of the symptoms of depression, such as mood, energy, appetite and sleep, but not others, such as interest and participation in social activities and hobbies.
Choice B is wrong because it only measures the client’s depression level using standardized scales, such as the Geriatric Depression Scale (GDS) or the Patient Health Questionnaire (PHQ-9), but not their actual functioning and quality of life.
Choice C is wrong because it only reflects the client’s interest and participation in social activities and hobbies, which are important aspects of depression recovery, but not their mood, energy, appetite, sleep or depression level.
The GDS and the PHQ-9 are both valid and reliable tools for screening and measuring depression in older adults.
The GDS is a 15-item questionnaire that asks the client to answer yes or no to questions about their mood, satisfaction, hopelessness, helplessness, worthlessness, guilt, agitation, withdrawal and suicidal thoughts.
The PHQ-9 is a 9-item questionnaire that asks the client to rate how often they have experienced symptoms of depression in the past two weeks, such as depressed mood, anhedonia, insomnia or hypersomnia, fatigue, appetite or weight changes, concentration problems, feelings of worthlessness or guilt.
A. The client reports an improvement in mood, energy, appetite and sleep B.
The client scores lower on the Geriatric Depression Scale (GDS) or the Patient Health Questionnaire (PHQ-9) C.
The client shows more interest and participation in social activities and hobbies D.
All of the above
A nurse is educating an older adult client who has depression about the benefits of physical activity and exercise.
Which of the following statements should the nurse include?
(Select all that apply.).
Explanation
The correct answer isA, B, C, D and E.
All of these statements are true and should be included in the nurse’s education.
Physical activity and exercise have many benefits for older adults with depression, such as:.
• Increasing the levels ofserotonin and endorphins, which are natural mood boosters that can help reduce depression symptoms.
• Improvingcardiovascular health, muscle strength, balance and flexibility, which can prevent or delay chronic diseases, reduce the risk of falls and injuries, and enhance functional ability.
• Reducingstress, anxiety, pain and inflammation, which can worsen depression and affect physical health.
• Enhancingself-esteem, confidence and sense of accomplishment, which can improve self-image, social interaction and coping skills.
• Helping tosleep better at night and feel more refreshed in the morning, which can improve mood, energy and cognitive function.
Choice A is correct because physical activity and exercise can increase the levels of serotonin and endorphins, which are natural mood boosters that can help reduce depression symptoms.
Choice B is correct because physical activity and exercise can improve cardiovascular health, muscle strength, balance and flexibility, which can prevent or delay chronic diseases, reduce the risk of falls and injuries, and enhance functional ability.
Choice C is correct because physical activity and exercise can reduce stress, anxiety, pain and inflammation.
A. Physical activity and exercise can increase your levels of serotonin and endorphins, which are natural mood boosters B.
Physical activity and exercise can improve your cardiovascular health, muscle strength, balance and flexibility C.
Physical activity and exercise can reduce your stress, anxiety, pain and inflammation D.
Physical activity and exercise can enhance your self-esteem, confidence and sense of accomplishment E.
Physical activity and exercise can help you sleep better at night and feel more refreshed in the morning
According to Erikson’s psychosocial theory, what is the main developmental task of older adults?
Explanation
The correct answer is C.
Ego integrity vs despair.
According to Erikson’s psychosocial theory, older adults face the challenge of looking back on their lives and evaluating their accomplishments and failures.
If they feel satisfied with their life course, they achieve a sense of ego integrity, which is a feeling of wholeness and coherence.
If they feel regretful or dissatisfied, they experience despair, which is a sense of hopelessness and bitterness.
Choice A is wrong because trust vs mistrust is the first stage of Erikson’s theory, which occurs in infancy.
It involves developing a basic sense of trust in oneself and others based on the quality of caregiving.
Choice B is wrong because generativity vs stagnation is the seventh stage of Erikson’s theory, which occurs in middle adulthood.
It involves contributing to society and the next generation through work, parenting, or other activities.
Choice D is wrong because identity vs role confusion is the fifth stage of Erikson’s theory, which occurs in adolescence.
It involves developing a stable and coherent sense of self and one’s role in society.
Normal ranges for Erikson’s stages are:.
• Trust vs mistrust: birth to 18 months.
• Autonomy vs shame and doubt: 18 months to 3 years.
• Initiative vs guilt: 3 to 6 years.
• Industry vs inferiority: 6 to 12 years.
• Identity vs role confusion: 12 to 18 years.
• Intimacy vs isolation: 18 to 40 years.
• Generativity vs stagnation: 40 to 65 years.
• Ego integrity vs despair: 65 years and older.
What are some of the environmental factors that can influence the psychosocial changes in older adults?
Explanation
The correct answer is C.
Living arrangements and social support.
This is because living arrangements and social support are some of the environmental factors that can influence the psychosocial changes in older adults.Psychosocial changes refer to the changes in mental and emotional well-being, social relationships, and roles that occur as people age.Environmental factors are the external conditions or circumstances that affect a person’s life.
Choice A is wrong because physical health and functional status are not environmental factors, but rather biological factors that affect the aging process.Physical health and functional status can influence the psychosocial changes in older adults, but they are not part of the environment.
Choice B is wrong because cognitive conditions and memory loss are also not environmental factors, but rather neurological factors that affect the brain function of older adults.Cognitive conditions and memory loss can also influence the psychosocial changes in older adults, but they are not part of the environment.
Choice D is wrong because hormonal changes and sensory impairments are also not environmental factors, but rather physiological factors that affect the body function of older adults.Hormonal changes and sensory impairments can also influence the psychosocial changes in older adults, but they are not part of the environment.
Living arrangements and social support are environmental factors because they depend on the availability, accessibility, and quality of housing, transportation, community services, family networks, and social interactions that older adults have in their surroundings.Living arrangements and social support can influence the psychosocial changes in older adults by affecting their sense of independence, identity, belonging, security, and satisfaction.
Therefore, living arrangements and social support are some of the environmental factors that can influence the psychosocial changes in older adults.
A nurse is conducting a psychosocial assessment of an older adult client who has recently retired from work.
Which of the following questions should the nurse ask?
(Select all that apply.).
Explanation
The correct answer isA, B, C, D, and E.
All of these questions are relevant for conducting a psychosocial assessment of an older adult client who has recently retired from work.A psychosocial assessment is a process for learning about a client’s problems and needs, so that together you can create therapy goals and a plan for recovery.The information-gathering process should allow you to learn more about the client as a person, beyond just a diagnosis.
• Choice A is correct because it explores how the client feels about their retirement, which can be a major life transition that affects their identity, self-esteem, and sense of purpose.
• Choice B is correct because it assesses the client’s interests and hobbies, which can provide sources of enjoyment, stimulation, and meaning in their life.
• Choice C is correct because it evaluates the client’s social support network, which can influence their mental health, well-being, and coping skills.
• Choice D is correct because it identifies the client’s stressors and challenges, which can affect their mood, functioning, and quality of life.
• Choice E is correct because it examines the client’s physical and mental health issues, which can impact their ability to perform daily activities, manage their emotions, and adhere to treatment plans.
A comprehensive geriatric assessment is a multidimensional process designed to assess the functional ability, health (physical, cognitive, and mental), and socioenvironmental situation of older people.The comprehensive geriatric assessment specifically and thoroughly evaluates functional and cognitive abilities, social support, financial status, and environmental factors, as well as physical and mental health.Ideally, a regular examination of older patients incorporates many aspects of the comprehensive geriatric assessment, making the two approaches very similar.
A nurse is teaching an older adult client about the benefits of social interaction for health and well-being.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The correct answer is D.
“Social interaction can help me avoid stress and anxiety.” This statement indicates a need for further teaching because social interaction does not necessarily help older adults avoid stress and anxiety.
In fact, some social situations may cause or increase stress and anxiety for some people, especially if they are negative, unpleasant, or conflictual.
Therefore, the nurse should explain to the client that social interaction can help them cope with stress and anxiety, but not avoid them altogether.
Choice A is correct because social interaction can help lower blood pressure and cholesterol levels by reducing the effects of stress hormones and promoting physical activity.
Choice B is correct because social interaction can help boost the immune system by enhancing positive emotions, increasing antibody production, and reducing inflammation.
Choice C is correct because social interaction can help improve memory and learning ability by stimulating brain regions involved in cognition, communication, and social perception.
Normal ranges for blood pressure are less than 120/80 mmHg for adults, and normal ranges for cholesterol are less than 200 mg/dL for total cholesterol, less than 100 mg/dL for LDL cholesterol, and more than 40 mg/dL for HDL cholesterol.
A nurse is assessing an older adult client who has been diagnosed with depression and social isolation.
Which of the following questions should the nurse ask to determine the possible causes of the client’s condition?
Explanation
The correct answer is D.
All of the above.
The nurse should ask all of these questions to assess the possible causes of the client’s condition.
Depression and social isolation in older adults can be triggered by various factors, such as:.
• Losses or changes in life, such as death of a spouse, retirement, relocation, or chronic illness.
• Lack of social support or contact with family, friends, or neighbors, which can lead to loneliness and reduced self-esteem.
• Decreased engagement or interest in activities or hobbies that provide meaning, pleasure, or stimulation, which can affect mood and cognitive function.
By asking these questions, the nurse can identify the specific factors that contribute to the client’s depression and social isolation, and provide appropriate interventions to address them.
For example, the nurse can:.
• Provide emotional support and empathy to the client and help them cope with their losses or changes.
• Encourage the client to maintain or increase their social interactions and connections with others who share similar interests or experiences.
• Assist the client to resume or find new activities or hobbies that suit their abilities and preferences, and provide positive feedback and reinforcement.
A nurse is implementing interventions to prevent or reduce social isolation in older adult clients who live in a long-term care facility.
Which of the following interventions are appropriate for this setting?
(Select all that apply.).
Explanation
These interventions are appropriate for reducing social isolation in older adult clients who live in a long-term care facility because they provide opportunities for social interaction, support, comfort and familiarity.
Choice A is correct because group activities such as games, music, art or exercise can foster a sense of belonging, enjoyment and engagement among older adults.Group activities can also improve physical and mental health, cognitive function and well-being.
Choice B is correct because encouraging family members or volunteers to visit or call the clients regularly can enhance the quality and quantity of social relationships, which can reduce loneliness and isolation.Family members or volunteers can also provide emotional support, companionship and practical assistance to the clients.
Choice C is correct because creating a homelike environment that promotes comfort, safety and privacy can increase the clients’ satisfaction, autonomy and dignity.A homelike environment can also facilitate social interactions among the clients and the staff by providing common areas, personal belongings and familiar objects.
Choice D is correct because assigning consistent staff members who are familiar with the clients’ needs and preferences can improve the continuity and quality of care, as well as the trust and rapport between the clients and the staff.Consistent staff members can also recognize and respond to the clients’ social needs and preferences, and provide personalized interventions.
Choice E is incorrect because providing feedback or recognition for the clients’ achievements or contributions may not be effective in reducing social isolation, unless it is combined with other interventions that promote social interaction and support.Feedback or recognition alone may not address the underlying causes of social isolation, such as lack of meaningful relationships, low self-esteem or poor health.
Normal ranges for social isolation and loneliness are difficult to define, as they depend on various factors such as individual characteristics, cultural norms and measurement tools.However, some indicators of social isolation include having few or no social contacts, participating in few or no social activities, feeling disconnected from others or society, and having low levels of perceived social support.Some indicators of loneliness include feeling unhappy about one’s social situation, feeling left out or unwanted, lacking companionship or intimacy, and having low levels of perceived belongingness or connectedness.
A nurse is providing education to a group of older adults about sexuality and aging.
Which of the following information should the nurse include?
Explanation
The correct answer is B.
Older adults may experience changes in sexual response or function due to physiological factors.This is because aging can affect the sex organs, hormones, blood flow, and nerve signals that are involved in sexual arousal and performance.These changes do not mean that older adults cannot enjoy a satisfying sex life, but they may require some adjustments or treatments to overcome any difficulties.
Choice A is wrong because older adults have the same need for intimacy and affection as younger adults, and sexuality is an important component of emotional and physical intimacy that can enhance well-being and quality of life.
Choice C is wrong because older adults with chronic diseases or disabilities can still have sexual activity, as long as they are comfortable and safe.They may need to consult with their health care providers about any precautions or modifications they should make to accommodate their conditions.
Choice D is wrong because older adults are not at lower risk for sexually transmitted infections (STIs) than younger adults.In fact, older adults may be more vulnerable to STIs due to lower immune function, thinner vaginal tissues, lack of condom use, and other factors.
Therefore, older adults should practice safe sex and get tested regularly for STIs.
Normal ranges for sexual response or function vary widely depending on the individual, the partner, the situation, and other factors.
There is no one standard or ideal way to experience sexuality and intimacy in older adulthood.The most important thing is to communicate openly with one’s partner and health care provider about any concerns or preferences, and to seek help if needed.
A nurse is caring for an older adult client who has erectile dysfunction due to diabetes mellitus.
The client asks the nurse what he can do to improve his sexual function.
Which of the following responses should the nurse give?
Explanation
You can do any of the above options, depending on your preference and medical condition.
Erectile dysfunction (ED) is the inability to get and maintain an erection for sexual activity.
It can be caused by physical or psychological factors, or both.
ED can affect your self-esteem, stress level and relationship quality.
There are different treatment options for ED, and they work in different ways.
Some of the most common ones are:.
• Oral medicationssuch as sildenafil (Viagra), tadalafil (Cialis), vardenafil (Levitra) or avanafil (Stendra).
These drugs enhance the effects of nitric oxide, a chemical that relaxes the muscles in the penis and increases blood flow.
You need to take them before sexual activity, and they only work if you are sexually stimulated.
They are not safe for everyone, especially if you have heart problems, low blood pressure, liver disease or certain eye conditions.They can also cause side effects such as headache, flushing, nasal congestion or indigestion.
• Penile self-injectionssuch as alprostadil (Caverject, Edex) or papaverine (OraVerse).
These are shots of medicine that you inject into the base or side of your penis with a fine needle.
They cause an erection by dilating the blood vessels in the penis.
The erection lasts about 20 to 30 minutes, and you need to use them only when needed.They can cause side effects such as bleeding, pain, priapism (a prolonged and painful erection) or fibrous tissue formation.
• Alprostadil urethral suppository(Muse).
This is a tiny pellet of medicine that you insert into your urethra (the tube that carries urine out of the body) with a special device.
It works by expanding the blood vessels in the penis and causing an erection.
The erection lasts about 30 to 60 minutes, and you need to use it only when needed.It can cause side effects such as burning, pain, bleeding or infection.
• Vacuum erection device(VED).
This is a plastic tube that you place over your penis and pump out the air to create a vacuum.
This draws blood into the penis and causes an erection.
You then slide a rubber ring around the base of your penis to keep the blood in place.
The erection lasts as long as the ring is on, up to 30 minutes.
You need to use it only when needed.It can cause side effects such as bruising, numbness, pain or difficulty ejaculating.
• Penile implant surgery.
This is a procedure where inflatable or bendable devices are surgically placed on both sides of your penis.
You can control when and how long you have an erection by inflating or deflating the devices with a pump or a switch.This is a permanent solution for ED, but it requires surgery and has risks of infection, mechanical failure or erosion.
Other treatment options for ED include hormone therapy, psychotherapy, lifestyle changes and natural remedies.
However, these may not be as effective or safe as the ones mentioned above.
The best treatment option for you depends on your personal preference, medical condition, cost and availability.
You should talk to your doctor about the benefits and risks of each option and choose the one that suits you best.
A nurse is assessing the risk factors for sexually transmitted infections (STIs) in older adult clients.
Which of the following factors should the nurse consider?
(Select all that apply.).
Explanation
The correct answer isA, B, C and D.
These are all factors that can increase the risk of sexually transmitted infections (STIs) in older adult clients.
A. Decreased immune system function with aging.This can make older adults more susceptible to infections and less able to fight them off.
B. Lack of knowledge or awareness about STIs.
Older adults may not have received adequate education or information about STIs, their symptoms, prevention and treatment.They may also have misconceptions or stigma about STIs that prevent them from seeking help or testing.
C. Reduced use of condoms or other barrier methods.
Older adults may not perceive themselves as at risk of STIs or may not know how to use condoms correctly or consistently.They may also face barriers such as cost, availability, embarrassment or partner resistance to using condoms.
D. Increased number of sexual partners or casual encounters.
Older adults may have more opportunities for sexual activity due to factors such as divorce, widowhood, online dating, travel or retirement.They may also engage in sexual behaviors that expose them to multiple or unknown partners, such as sex work, drug use or group sex.
Choice E is wrong becauseincreased vaginal dryness or atrophy with menopauseis not a risk factor for STIs in older adult clients.
While this condition can cause discomfort, pain or bleeding during sexual intercourse, it does not increase the likelihood of acquiring or transmitting an STI.However, it may affect the quality of life and sexual satisfaction of older women and their partners, and may require medical attention or lubrication products.
: Johnson BK.
Sexually transmitted infections and older adults.J Gerontol Nurs 2013;39(11):53-60.: World Health Organization (WHO).
Sexually transmitted infections (STIs).2022 Aug 22.: Journal of Gerontological Nursing (JGN).
Sexually Transmitted Infections and Older Adults.
2013 Sep 18.
Exams on Care Of The Older Adult
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction
- Physiological Changes with Aging
- Cardiovascular System
- Musculoskeletal System
- Genitourinary System
- Endocrine System
- Functional Status
- Cognitive Conditions
- Dementia
- Depression
- Psychosocial Changes
- Social Isolation
- Sexuality
- Nursing Interventions
- Conclusion
- Summary
- More questions on the topic
Notes Highlighting is available once you sign in. Login Here.
Objectives
By the end of these notes, you should be able to:
- Define older adult and ageism
- Identify myths and stereotypes about older adults
- List the developmental tasks of older adults
- Explain the physiological changes with aging in different body systems
- Assess the functional status and cognitive conditions of older adults
- Identify the psychosocial changes that occur in older adults
- Describe the nursing interventions for promoting health and wellness in older adults
Introduction
Older adults are persons age 65 and over.

They are a diverse group of individuals with different backgrounds, experiences, preferences, needs and abilities. Older adults face many challenges and opportunities as they age, such as coping with retirement, social isolation, chronic illnesses, functional decline, cognitive impairment, depression and loss. Older adults also have many strengths and resources, such as wisdom, resilience, spirituality, family support and community involvement.
Ageism is discrimination against people because of increasing age. It can lead to negative attitudes, stereotypes and behaviors towards older adults that affect their self-esteem, dignity, quality of life and access to health care. Some common myths and stereotypes about older adults are:
- They are ill, disabled and unattractive
- They are forgetful, confused, rigid, boring, unfriendly and poor
- They are unable to learn and understand new information
- They are not interested in sex or sexual activities
These myths and stereotypes are not true for most older adults and can be harmful to their well-being. Nurses need to respect the individuality and diversity of older adults and provide holistic, person-centered care that meets their physical, psychological, social and spiritual needs.
Physiological Changes with Aging
Aging is a natural process that involves gradual changes in the structure and function of different body systems. These changes vary from person to person depending on genetic factors, lifestyle factors, environmental factors and disease processes. Some of the normal physiological changes with aging in different body systems are:
Integumentary System
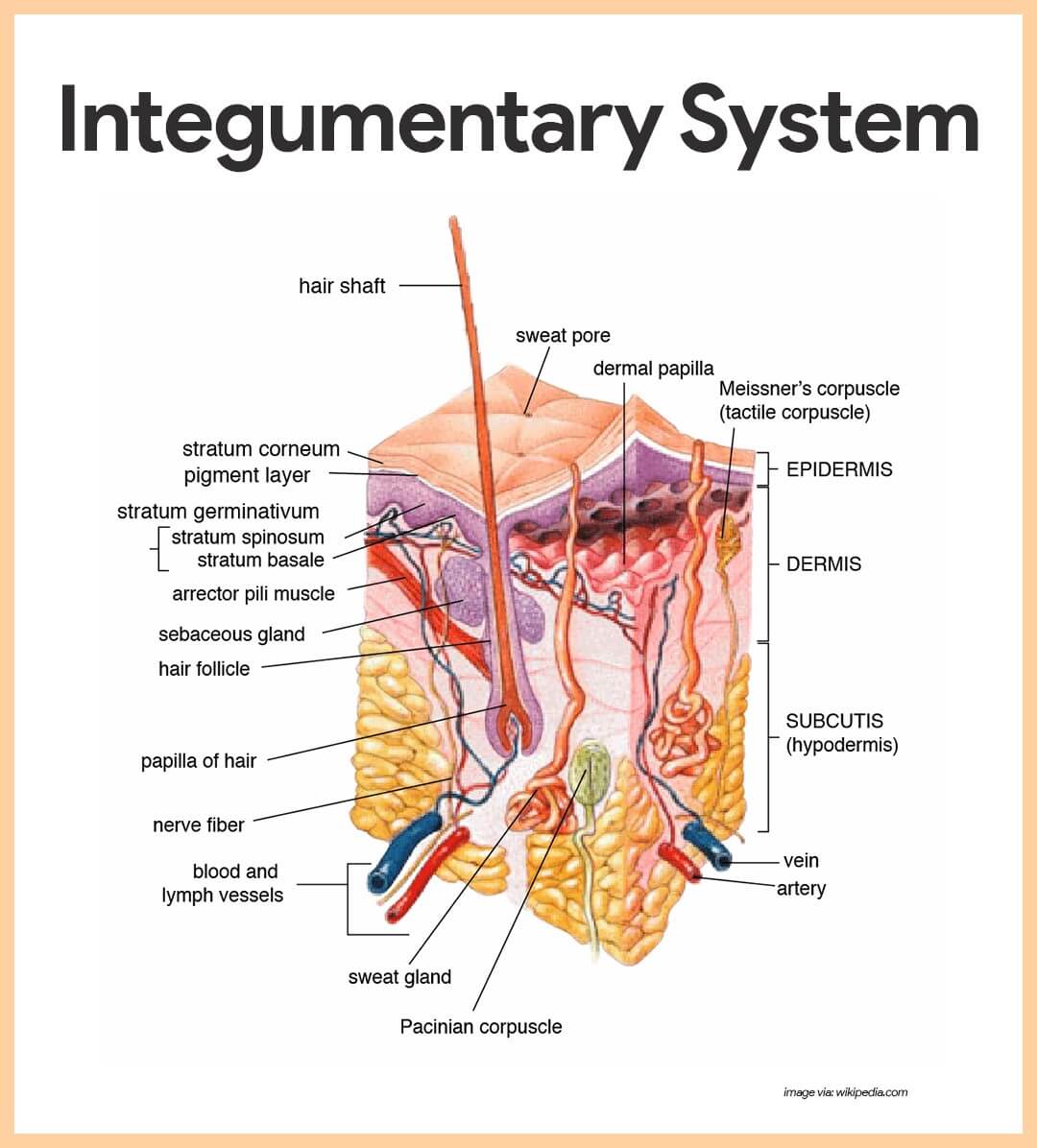
- Increased skin dryness, pallor and fragility
- Decreased vascularity of blood vessels
- Progressive wrinkling of the skin
- Decreased perspiration due to decreased sebaceous gland activity
- Thinning and graying of the scalp, pubic and axillary hair
- Slower nail growth , decreased calcium, increased thickening with ridges
- Brown age spots (lentigo senilis) on exposed body parts
Genitourinary System
Introduction to Communication and Therapeutic Relationships
-
Communication is the process of exchanging information, ideas, feelings, and meanings through verbal and nonverbal messages
-
Therapeutic communication is a purposeful form of communication that focuses on the needs, goals, and outcomes of the patient
-
Therapeutic relationships are professional, goal-directed, and patient-centered relationships that are based on trust, respect, empathy, and collaboration
-
Communication and therapeutic relationships are essential skills for nurses to provide safe, quality, and patient-centered care
Genitourinary System
- Decreased kidney size and function results in decreased glomerular filtration rate, decreased urine concentration and increased risk of dehydration
- Decreased bladder capacity and tone results in urinary frequency, urgency and nocturia
- Decreased sphincter control results in urinary incontinence
- Decreased estrogen levels in women results in vaginal dryness, atrophy and increased risk of infection
- Decreased testosterone levels in men results in erectile dysfunction, decreased libido and benign prostatic hyperplasia
Reproductive System
- Decreased ovarian function in women results in menopause, cessation of menstruation and decreased fertility
- Decreased uterine and breast size in women results in decreased support and sagging
- Decreased testicular function in men results in decreased sperm production and quality
- Decreased sexual response in both genders results in delayed arousal, orgasm and resolution
Endocrine System
Endocrine System
- Decreased thyroid function results in decreased basal metabolic rate, increased fat deposition and decreased body temperature
- Decreased adrenal function results in decreased cortisol production, increased stress response and decreased immune response
- Decreased pancreatic function results in decreased insulin production, increased blood glucose levels and increased risk of diabetes mellitus
- Decreased pituitary function results in decreased growth hormone production, decreased muscle mass and bone density
Immune System
- Decreased thymus size and function results in decreased T-cell production and activity
- Decreased bone marrow function results in decreased B-cell production and antibody response
- Decreased inflammatory response results in delayed wound healing and increased risk of infection
Functional Status
Functional Status
Functional status refers to the day-to-day activities of daily living (ADLs) involving activities within physical, psychological, cognitive and social domains. Functional status is influenced by the physiological changes with aging as well as by the presence of chronic diseases, disabilities, medications, environmental factors and psychosocial factors. Functional status can be assessed by using standardized tools such as the Katz Index of Independence in Activities of Daily Living (ADLs) or the Lawton Instrumental Activities of Daily Living (IADLs) Scale. These tools measure the ability of older adults to perform basic tasks such as bathing, dressing, toileting, transferring, feeding, grooming, using the telephone, managing finances, shopping, preparing meals, doing housework, taking medications and using transportation.
The functional status of older adults can be improved by providing interventions such as:
- Promoting physical activity and exercise to maintain muscle strength, joint mobility, balance and coordination
- Encouraging adequate nutrition and hydration to prevent malnutrition, dehydration and electrolyte imbalance
- Managing chronic diseases and medications to prevent complications, adverse effects and polypharmacy
- Providing assistive devices and adaptive equipment to enhance mobility, safety and independence
- Modifying the environment to reduce hazards, improve accessibility and facilitate self-care
- Educating older adults and caregivers about the normal aging process, health promotion strategies and available resources
Cognitive Conditions
Cognitive Conditions
Cognitive conditions refer to the mental processes that involve thinking, learning, memory, reasoning, problem-solving, decision-making and communication. Cognitive conditions can be affected by the physiological changes with aging as well as by the presence of acute or chronic illnesses that impair brain function. Some of the common cognitive conditions that affect older adults are:
Delirium
Delirium is an acute confusional state that is characterized by a sudden onset of altered mental status that fluctuates over time. It is usually caused by an underlying medical condition such as infection, dehydration, hypoxia, electrolyte imbalance or drug toxicity. It is manifested by symptoms such as:
- Impaired attention span and concentration
- Disorientation to time, place or person
- Disturbance of consciousness or level of arousal
- Hallucinations or delusions
- Agitation or lethargy
- Mood swings or emotional lability
Delirium is a medical emergency that requires prompt identification and treatment of the underlying cause. It can be prevented by providing interventions such as:
- Monitoring vital signs, blood glucose levels and oxygen saturation regularly
- Reviewing medications for potential interactions or side effects
- Maintaining adequate hydration and nutrition
- Providing a calm and familiar environment with adequate lighting and orientation cues
- Avoiding sensory overload or deprivation by limiting noise, visitors and procedures
- Encouraging family involvement and support
Dementia
Dementia
Dementia is a generalized impairment of intellectual functioning that interferes with social or occupational functioning. It is usually caused by a chronic degenerative disease of the brain such as Alzheimer’s disease, vascular dementia, Lewy body dementia or frontotemporal dementia. It is manifested by symptoms such as:
- Gradual onset and progressive decline of cognitive abilities
- Memory loss, especially for recent events
- Aphasia, apraxia, agnosia or executive dysfunction
- Personality changes, behavioral problems or mood disturbances
- Impaired judgment, insight or reasoning
- Difficulty with ADLs and IADLs
Dementia is a chronic condition that has no cure but can be managed by providing interventions such as:
- Diagnosing the type and stage of dementia and treating any reversible causes
- Prescribing medications to slow down the progression of cognitive decline or to manage behavioral symptoms
- Providing cognitive stimulation and reminiscence therapy to enhance memory and orientation
- Providing reality orientation or validation therapy to reduce confusion and agitation
- Providing structured routines and consistent caregivers to promote familiarity and security
- Providing safety measures and supervision to prevent wandering, falls or injuries
- Providing palliative care and end-of-life care when appropriate
Depression
Depression

Depression is a mood disturbance that is characterized by feelings of sadness, despair, hopelessness, guilt, worthlessness or anhedonia. It can be triggered by stressful life events such as retirement, loss of spouse, social isolation, chronic illness or disability. It is manifested by symptoms such as:
- Persistent low mood or irritability for more than two weeks
- Loss of interest or pleasure in usual activities
- Changes in appetite, weight, sleep or energy level
- Difficulty with concentration, memory or decision-making
- Suicidal thoughts or attempts
- Somatic complaints or physical pain
Depression is a treatable condition that can be improved by providing interventions such as:
- Screening for depression using standardized tools such as the Geriatric Depression Scale (GDS) or the Patient Health Questionnaire (PHQ-9)
- Prescribing antidepressant medications to correct the chemical imbalance in the brain
- Providing psychotherapy such as cognitive-behavioral therapy (CBT) or interpersonal therapy (IPT) to change negative thoughts and behaviors
- Providing social support and counseling to address the psychosocial issues and coping skills
- Encouraging physical activity and exercise to improve mood and well-being
- Referring to mental health services or crisis intervention if needed
Psychosocial Changes
Psychosocial Changes
Psychosocial changes refer to the emotional, social and spiritual aspects of aging that affect the older adult’s self-concept, identity, roles, relationships and meaning of life. Psychosocial changes are influenced by the developmental tasks of older adults as well as by the physiological changes with aging, cognitive conditions, functional status and environmental factors. Some of the psychosocial changes that occur in older adults are:
Retirement
Retirement is the cessation of work-related activities that may occur voluntarily or involuntarily. It can have positive or negative effects on the older adult’s sense of ego integrity or despair (Erikson). Retirement can lead to:
- Increased leisure time and opportunities for hobbies, travel, education or volunteering
- Decreased income and financial security
- Decreased social interaction and support from coworkers
- Decreased self-esteem and identity from work role
- Increased stress from role changes or family responsibilities
Retirement can be facilitated by providing interventions such as:
- Planning ahead for retirement goals, finances and lifestyle
- Maintaining a balanced schedule of activities that provide stimulation, satisfaction and purpose
- Seeking alternative sources of income or employment if needed
- Joining social groups or clubs that share common interests or values
- Seeking counseling or support groups if experiencing adjustment difficulties
Social Isolation
Social Isolation
 Social isolation is the lack of meaningful contact or interaction with other people. It can result from factors such as:
Social isolation is the lack of meaningful contact or interaction with other people. It can result from factors such as:
- Loss of spouse, friends or relatives due to death, divorce or relocation
- Decreased mobility or transportation due to physical limitations or lack of access
- Decreased hearing or vision due to sensory impairments
- Decreased communication skills due to cognitive impairments or language barriers
- Decreased social skills due to depression, anxiety or personality changes
Social isolation can have adverse effects on the older adult’s physical and mental health such as:
- Increased risk of cardiovascular disease, infection, dementia or mortality
- Decreased immune function, wound healing and pain tolerance
- Decreased cognitive function, memory and learning ability
- Decreased self-esteem, self-efficacy and coping skills
- Increased depression, anxiety, loneliness and suicidal ideation
Social isolation can be prevented or reduced by providing interventions such as:
- Assessing the older adult’s social network, support system and preferences
- Encouraging the older adult to maintain contact with family, friends and neighbors
- Facilitating the older adult’s participation in community activities or events that match their interests, abilities and values
- Providing assistive devices or adaptive equipment to enhance hearing, vision or mobility
- Providing transportation or escort services to enable access to social venues
- Referring the older adult to social services or agencies that offer companionship, respite or home care
Sexuality
Sexuality
Sexuality is the expression of one’s sexual identity, orientation, feelings, desires and behaviors. It is an integral part of human development that continues throughout the lifespan. Sexuality can be affected by factors such as:
- Physiological changes with aging that alter sexual response or function
- Chronic diseases or medications that impair sexual performance or satisfaction
- Psychological factors such as depression, anxiety, stress or low self-esteem
- Sociocultural factors such as myths, stereotypes, attitudes or expectations
- Environmental factors such as privacy, comfort or safety
Sexuality can be enhanced by providing interventions such as:
- Educating the older adult and their partner about the normal changes with aging and how to adapt to them
- Encouraging the older adult and their partner to communicate openly and honestly about their sexual needs and preferences
- Providing counseling or therapy to address any emotional or relational issues that affect sexuality
- Prescribing medications or devices to treat any physical conditions that impair sexuality
- Providing information or referrals to resources that support sexuality
Nursing Interventions
Nursing Interventions
Nursing interventions for promoting health and wellness in older adults are based on the principles of gerontological nursing, which are:
- Respect the individuality and diversity of older adults
- Provide holistic, person-centered care that meets their physical, psychological, social and spiritual needs
- Empower older adults to participate in decision-making and self-care
- Promote health promotion and disease prevention strategies
- Support the dignity, autonomy and quality of life of older adults
- Collaborate with interdisciplinary team members and caregivers
Some examples of nursing interventions for promoting health and wellness in older adults are:
- Assessing the older adult’s health status, functional status, cognitive condition and psychosocial changes using standardized tools and age-specific approaches
- Developing a comprehensive care plan that addresses the older adult’s strengths, needs, goals and preferences
- Implementing evidence-based interventions that are tailored to the older adult’s condition, situation and response
- Evaluating the outcomes of interventions and modifying them as needed
- Educating the older adult and their caregivers about the normal aging process, health promotion strategies and available resources
- Advocating for the rights, interests and needs of older adults
Conclusion
Care of the older adult is a complex and challenging task that requires specialized knowledge, skills and attitudes. Nurses play a vital role in providing quality care to older adults by understanding the physiological changes with aging, assessing the functional status and cognitive conditions of older adults, identifying the psychosocial changes that occur in older adults and implementing nursing interventions for promoting health and wellness in older adults.
Summary
The main points of these notes are:
- Older adults are persons age 65 and over who are diverse in their backgrounds, experiences, preferences, needs and abilities.
- Ageism is discrimination against people because of increasing age that can lead to negative attitudes, stereotypes and behaviors towards older adults.
- Physiological changes with aging involve gradual changes in the structure and function of different body systems that vary from person to person depending on various factors.
- Functional status refers to the day-to-day activities of daily living (ADLs) involving activities within physical, psychological, cognitive and social domains that are influenced by physiological changes with aging as well as other factors.
- Cognitive conditions refer to the mental processes that involve thinking, learning, memory, reasoning, problem-solving, decision-making and communication that can be affected by physiological changes with aging as well as acute or chronic illnesses that impair brain function.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Care Of The Older Adult
This filled cannot be empty

