Please set your exam date
Medication Reconciliation and Patient Education
Study Questions
Introduction
A nurse is preparing to teach a client about medication reconciliation. Which of the following statements should the nurse include in the teaching? (Select all that apply.)
Explanation
A) Correct. Medication reconciliation is a process that helps prevent medication errors by ensuring that the client receives the correct medications at the correct doses and times.
B) Correct. Medication reconciliation involves comparing the client's current medications with their previous ones to identify any discrepancies or changes.
C) Correct. Medication reconciliation should be done at every transition of care, such as admission, transfer, or discharge, to ensure continuity and safety of medication therapy.
D) Correct. Medication reconciliation requires the client to keep an updated list of all their medications, including prescription, over-the-counter, herbal, and dietary supplements, and to share it with their health care providers.
E) Incorrect. Medication reconciliation does not allow the client to adjust their medication doses as needed. The client should always follow the prescribed instructions and consult their health care provider before making any changes.
A nurse is reviewing a client's medication list during a home visit. The nurse notices that the client has been taking ibuprofen and naproxen together for arthritis pain. Which of the following actions should the nurse take first?
Explanation
A) Incorrect. The nurse should not instruct the client to stop taking both medications immediately without consulting the client's primary care provider. Abruptly discontinuing some medications can cause adverse effects or withdrawal symptoms.
B) Correct. The nurse should assess the client for signs of gastrointestinal bleeding, such as abdominal pain, black or tarry stools, or coffee-ground emesis. Ibuprofen and naproxen are both nonsteroidal anti-inflammatory drugs (NSAIDs) that can increase the risk of gastrointestinal bleeding when taken together or for a long time.
C) Incorrect. The nurse should document the finding in the client's medical record after assessing the client and notifying the primary care provider. Documentation is an important but not a priority action in this situation.
D) Incorrect. The nurse should notify the client's primary care provider after assessing the client for signs of gastrointestinal bleeding. The primary care provider may need to adjust or change the client's medication regimen to prevent further complications.
A nurse is providing discharge teaching to a client who has a new prescription for warfarin. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
A) Correct. The client should use an electric razor when shaving to reduce the risk of bleeding from minor cuts or nicks. Warfarin is an anticoagulant that inhibits blood clotting and increases the bleeding time.
B) Incorrect. The client should not eat more green leafy vegetables to prevent bleeding. Green leafy vegetables are high in vitamin K, which antagonizes the effect of warfarin and reduces its anticoagulant activity.
C) Incorrect. The client should not take an extra dose if they miss one. Taking an extra dose can cause excessive anticoagulation and increase the risk of bleeding or hemorrhage.
D) Incorrect. The client should not check their blood pressure every day unless instructed by their health care provider. Checking blood pressure every day is not related to warfarin therapy and may cause unnecessary anxiety or confusion.
A nurse is caring for a client who is receiving intravenous (IV) antibiotics for a severe infection. The nurse observes that the IV site is red, swollen, and painful. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
A) Correct. The nurse should discontinue the IV line and start a new one in another site. The IV site is showing signs of phlebitis, which is inflammation of the vein caused by mechanical, chemical, or bacterial irritation. Phlebitis can lead to complications such as thrombophlebitis, infection, or extravasation.
B) Correct. The nurse should apply a warm compress to the IV site to promote vasodilation and blood flow, which can help reduce inflammation and pain.
C) Correct. The nurse should elevate the affected extremity on a pillow to facilitate venous return and decrease edema.
D) Incorrect. The nurse should not administer an antihistamine to the client unless prescribed by the health care provider. Antihistamines are used to treat allergic reactions, not phlebitis.
E) Incorrect. The nurse should not flush the IV line with normal saline. Flushing the IV line can worsen the inflammation and increase the risk of infection or thrombus formation.
A nurse is teaching a client who has diabetes mellitus about self-administration of insulin. Which of the following instructions should the nurse include in the teaching?
Explanation
A) Incorrect. The nurse should instruct the client to store unopened insulin vials in the refrigerator, not in the freezer. Freezing can damage the insulin and make it ineffective.
B) Correct. The nurse should instruct the client to rotate injection sites within the same anatomical region, such as the abdomen, thighs, arms, or buttocks. Rotating injection sites can prevent lipodystrophy, which is a disorder of fat metabolism that causes hypertrophy or atrophy of subcutaneous tissue.
C) Incorrect. The nurse should instruct the client not to mix short-acting and long-acting insulins in the same syringe. Mixing different types of insulins can alter their onset, peak, and duration of action and affect blood glucose control.
D) Correct. The nurse should instruct the client to draw up regular insulin before NPH insulin when mixing them in the same syringe. This can prevent contamination of the regular insulin vial with NPH insulin, which can affect its potency and clarity.
A nurse is evaluating a client's understanding of their new prescription for albuterol inhaler. Which of the following actions by the client demonstrates correct use of the inhaler?
Explanation
A) Correct. The client should shake the inhaler well before use to mix the medication and propellant evenly and ensure proper dosage delivery.
B) Incorrect. The client should hold their breath for 10 seconds after inhaling to allow the medication to reach the lower airways and improve bronchodilation.
C) Incorrect. The client should exhale fully after placing the mouthpiece in their mouth and closing their lips around it. This can prevent wasting of medication and ensure optimal inhalation.
D) Incorrect. The client should repeat the puff after 1 minute if needed or prescribed. Waiting for 1 minute between puffs can allow enough time for the first puff to take effect and reduce adverse effects such as tachycardia or tremors.
A nurse is planning to teach a client who has hypertension about lifestyle modifications to lower their blood pressure. Which of the following topics should the nurse include in the teaching? (Select all that apply.)
Explanation
A) Correct. The nurse should include reducing sodium intake to less than 2 g per day in the teaching. Sodium can increase fluid retention and blood volume, which can raise blood pressure.
B) Correct. The nurse should include increasing physical activity to at least 30 minutes per day in the teaching. Physical activity can lower blood pressure by strengthening the heart, improving blood circulation, and reducing body weight.
C) Correct. Limiting alcohol consumption to no more than two drinks per day for men and one drink per day for women. Excessive alcohol consumption can raise blood pressure, so moderation is important.
D) Correct. Quitting smoking and avoiding exposure to secondhand smoke. Smoking and exposure to secondhand smoke are significant risk factors for hypertension and other cardiovascular diseases.
E) Incorrect. Taking a nap for 20 minutes every afternoon. While rest and relaxation are important for overall well-being, taking a nap specifically for 20 minutes every afternoon may not be directly related to lowering blood pressure. It's better to focus on the other lifestyle modifications mentioned above.
Obtaining Accurate Medication History
A nurse is reviewing a client's medication history before admission to a hospital unit. Which of the following sources of information is most reliable for obtaining an accurate medication history?
Explanation
C) Correct. The client's medication bottles brought from home are the most reliable source of information for obtaining an accurate medication history, as they contain the name, dose, frequency, and expiration date of each medication. The bottles can also be used to verify the client's verbal report and other sources of information.
A) Incorrect. The client's verbal report of their medications and doses may not be accurate, as the client may forget, omit, or confuse some medications or doses. The verbal report should be confirmed with other sources of information, such as medication bottles or lists.
B) Incorrect. The client's medication list from their primary care provider may not be up to date, as the client may have changed, discontinued, or added some medications since their last visit. The medication list should be compared with other sources of information, such as medication bottles or verbal report.
D) Incorrect. The client's electronic health record from another facility may not reflect the current medications that the client is taking, as the facility may have different policies, protocols, or formularies than the admitting hospital. The electronic health record should be supplemented with other sources of information, such as medication bottles or lists.
A nurse is reviewing a client's medication list during a routine clinic visit. The nurse notices that the client is taking warfarin and aspirin daily. Which of the following actions should the nurse take?
Explanation
A) Incorrect. Asking the client about signs of bleeding is important, but not sufficient. The nurse should also address the potential drug-drug interaction between warfarin and aspirin, which can increase the risk of bleeding complications.
B) Incorrect. Instructing the client to stop taking aspirin without consulting the prescriber is inappropriate and potentially harmful. The client may have a valid reason for taking both medications, such as atrial fibrillation and coronary artery disease.
C) Incorrect. Documenting the medication list without further investigation is negligent and unsafe. The nurse has a responsibility to ensure that the medications are appropriate and reconciled with the prescriber.
D) Correct. Contacting the prescriber to clarify the indication and dosage of both medications is the best action. The nurse should verify that the prescriber is aware of the combination and that the benefits outweigh the risks. The nurse should also confirm that the client is receiving regular monitoring of their international normalized ratio (INR).
A nurse is obtaining a medication history from a client who is admitted for pneumonia. Which of the following sources should the nurse use to verify the client's home medications? (Select all that apply.)
Explanation
A) Correct. The client's primary care provider can provide accurate information about the client's current prescriptions and any changes made recently.
B) Correct. The client's pharmacy records can show what medications the client has filled and when, which can help identify adherence issues or discrepancies.
C) Correct. The client's medication bottles can provide information about the name, dose, frequency, and expiration date of the medications, as well as any special instructions or warnings.
D) Correct. The client's spouse or caregiver can provide additional information about the client's medication use, especially if the client has cognitive impairment or difficulty managing their own medications.
E) Incorrect. The client's previous admission records may not reflect the current medication regimen, as changes may have occurred since then.
A nurse is preparing to discharge a client who has a new prescription for insulin glargine and insulin lispro. Which of the following information should the nurse include in the medication reconciliation process?
Explanation
D) Correct. All of the information listed are essential for the safe and effective use of insulin therapy. The nurse should educate the client on how to administer each insulin type, how to store and dispose of each insulin vial, how to select and rotate injection sites, and how to monitor their blood glucose levels and adjust their doses accordingly.
A nurse is reconciling a client's medications during a home health visit. The nurse observes that the client has several over-the-counter (OTC) products in their medicine cabinet, such as acetaminophen, ibuprofen, antacids, and herbal supplements. Which of the following actions should the nurse take?
Explanation
A) Correct. Asking the client how often and why they use each OTC product can help identify any potential drug-drug interactions, adverse effects, or self-treatment issues. The nurse should also educate the client on how to use OTC products safely and appropriately.
B) Incorrect. Advising the client to avoid using any OTC products without consulting their prescriber is unrealistic and unnecessary. Some OTC products are effective and safe for minor ailments, as long as they are used as directed and do not interfere with the client's prescription medications.
C) Incorrect. Recording only the prescription medications on the medication list is incomplete and inaccurate. The nurse should include all medications that the client is taking, including OTC products, vitamins, minerals, and herbal supplements.
D) Incorrect. Discarding any OTC products that are expired or unsealed without the client's consent is disrespectful and wasteful. The nurse should inform the client of the risks of using expired or contaminated products and offer to dispose of them properly.
A nurse is conducting a medication history for a client who is scheduled for elective surgery. The client reports taking ginkgo biloba, garlic, and fish oil supplements daily. Which of the following actions should the nurse take?
Explanation
A) Incorrect. Informing the client that these supplements are not effective and should be discontinued is disrespectful and inaccurate. These supplements may have some benefits for certain conditions, such as cognitive function, cardiovascular health, and inflammation. The nurse should respect the client's preferences and beliefs, as long as they do not pose a significant risk to their health.
B) Correct. Documenting the supplements on the medication list and notifying the surgical team is the best action. These supplements may have antiplatelet or anticoagulant effects, which can increase the risk of bleeding during or after surgery. The surgical team may advise the client to stop taking these supplements before the surgery, depending on their individual risk factors and type of surgery.
C) Incorrect. Instructing the client to stop taking these supplements at least 2 weeks before the surgery is premature and outside the scope of practice of the nurse. The nurse should consult with the surgical team before making any recommendations about discontinuing any medications or supplements.
D) Incorrect. Ignoring the supplements as they are not relevant to the surgical procedure is irresponsible and unsafe. The nurse should consider all medications and supplements that the client is taking, as they may have an impact on their perioperative care and outcomes.
A nurse is comparing a client's medication list with their discharge orders after a hospital stay for heart failure exacerbation. The nurse notices that the discharge orders include a new prescription for spironolactone, but do not include the client's usual dose of potassium chloride. Which of the following actions should the nurse take?
Explanation
A) Incorrect. Assuming that the prescriber intentionally omitted potassium chloride because spironolactone can increase potassium levels is risky and unprofessional. The nurse should not make assumptions about the prescriber's intentions or clinical judgment, but rather seek clarification and verification.
B) Correct. Contacting the prescriber to confirm that potassium chloride was intentionally omitted and documenting the rationale is the best action. The nurse should communicate any discrepancies or concerns about the discharge orders with the prescriber and ensure that they are resolved before discharging the client.
C) Incorrect. Administering potassium chloride as previously ordered until the prescriber responds is inappropriate and potentially harmful. The nurse should not administer any medications that are not included in the current orders, especially if they may interact with other medications or affect the client's condition.
D) Incorrect. Adding potassium chloride to the discharge orders without contacting the prescriber is illegal and unethical. The nurse does not have the authority or competence to prescribe or modify medications without consulting with an authorized prescriber.
Approach to obtaining Accurate Medication History
A nurse is obtaining a medication history from a client who has chronic obstructive pulmonary disease (COPD). Which of the following medications should the nurse include in the history? (Select all that apply.)
Explanation
A) Correct. Montelukast is a leukotriene receptor antagonist that can reduce inflammation and bronchoconstriction in clients with COPD.
B) Correct. Fluticasone is an inhaled corticosteroid that can decrease airway inflammation and improve lung function in clients with COPD.
C) Incorrect. Alprazolam is a benzodiazepine that can cause respiratory depression and worsen hypoxemia in clients with COPD.
D) Incorrect. Omeprazole is a proton pump inhibitor that can treat gastroesophageal reflux disease (GERD), which may be a comorbidity of COPD, but it is not directly related to COPD management.
E) Incorrect. Acetaminophen is an analgesic and antipyretic that can relieve pain and fever, but it has no effect on COPD.
A nurse is obtaining a medication history from a client who has hypertension. Which of the following questions should the nurse ask to assess for adherence to the prescribed therapy?
Explanation
B) Correct. The nurse should ask about any over-the-counter medications or supplements that the client is taking, as they may interact with the prescribed antihypertensive medications or affect blood pressure control.
A) Incorrect. This question is relevant for monitoring blood pressure, but not for assessing adherence to the prescribed therapy.
C) Incorrect. This question is relevant for evaluating the client's knowledge of their medications, but not for assessing adherence to the prescribed therapy.
D) Incorrect. This question is relevant for ensuring proper medication safety, but not for assessing adherence to the prescribed therapy.
A nurse is reviewing a client's medication list during a home visit. The client reports that they have been taking ibuprofen for arthritis pain. Which of the following actions should the nurse take?
Explanation
B) Correct. The nurse should instruct the client to take ibuprofen with food or milk to prevent gastric irritation, as ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can cause gastrointestinal bleeding or ulcers.
A) Incorrect. Although this is a good advice, it is not the priority action for the nurse to take, as alcohol does not directly interact with ibuprofen.
C) Incorrect. The nurse should not suggest the client to switch to another medication without consulting their provider, as acetaminophen has its own risks and contraindications, such as liver toxicity.
D) Incorrect. The nurse should not tell the client to stop taking ibuprofen abruptly without consulting their provider, as this may worsen their pain and inflammation.
A nurse is teaching a client who has a new prescription for warfarin about potential drug interactions. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
B) Correct. The client should check with their doctor before taking any herbal supplements or remedies, as some of them may interact with warfarin and increase the risk of bleeding or clotting.
A) Incorrect. The client should not avoid eating foods that are high in vitamin K, but rather maintain a consistent intake of them, as vitamin K is an antidote for warfarin and can affect its therapeutic effect.
C) Incorrect. This statement is relevant for preventing bleeding complications while taking warfarin, but it does not indicate an understanding of potential drug interactions.
D) Incorrect. This statement is relevant for monitoring the effects of warfarin on cardiovascular function, but it does not indicate an understanding of potential drug interactions.
A nurse is preparing to administer an intramuscular injection of penicillin G benzathine to a client who has syphilis. Which of the following actions should the nurse take?
Explanation
D) Correct. The nurse should use a 20-gauge needle and inject the medication into the dorsogluteal muscle, as penicillin G benzathine is a thick and viscous suspension that requires a large-bore needle and a large muscle mass for injection.
A) Incorrect. The nurse should not use a 25-gauge needle and inject the medication into the deltoid muscle, as this needle is too small and this muscle is too small for penicillin G benzathine injection.
B) Incorrect. The nurse should not use a tuberculin syringe and inject the medication into the ventrogluteal muscle, as this syringe is too small and this muscle is not recommended for penicillin G benzathine injection.
C) Incorrect. The nurse should not use an insulin syringe and inject the medication into the vastus lateralis muscle, as this syringe is too small and this muscle is not recommended for penicillin G benzathine injection.
A nurse is caring for a client who has a history of chronic kidney disease and is prescribed furosemide. Which of the following laboratory values should the nurse monitor closely while the client is taking this medication?
Explanation
B) Correct. The nurse should monitor serum potassium closely while the client is taking furosemide, as this medication is a loop diuretic that can cause hypokalemia or low potassium levels, which can lead to cardiac arrhythmias or muscle weakness.
A) Incorrect. Although serum creatinine is an indicator of kidney function, it is not directly affected by furosemide, as this medication does not cause nephrotoxicity or damage to the kidneys.
C) Incorrect. Although serum calcium is an electrolyte that can affect neuromuscular function, it is not directly affected by furosemide, as this medication does not cause hypocalcemia or low calcium levels.
D) Incorrect. Although serum albumin is a protein that can affect fluid balance, it is not directly affected by furosemide, as this medication does not cause hypoalbuminemia or low albumin levels.
A nurse is educating a client who has a new prescription for metformin about how to take this medication. Which of the following instructions should the nurse include in the teaching?
Explanation
A) Correct. The nurse should instruct the client to take metformin with meals to reduce gastrointestinal upset, such as nausea, vomiting, diarrhea, or abdominal pain, which are common adverse effects of this medication.
B) Incorrect. The nurse should not instruct the client to take metformin at bedtime, as this may increase the risk of lactic acidosis, a rare but serious complication of this medication that can cause muscle pain, weakness, fatigue, or hyperventilation.
C) Incorrect. The nurse should not instruct the client to take metformin with grapefruit juice, as this may interfere with its metabolism and increase its blood levels, which can lead to hypoglycemia or low blood sugar levels.
D) Incorrect. The nurse should not instruct the client to take metformin with an antacid, as this may decrease its absorption and effectiveness in lowering blood sugar levels.
Patient education on medication purpose, dosage, and side effects
A nurse is teaching a client who has been prescribed warfarin for atrial fibrillation. Which of the following statements by the client indicates a need for further education?
Explanation
A) Incorrect. The client should not avoid eating foods that are high in vitamin K, such as leafy green vegetables, because they can interfere with the anticoagulant effect of warfarin. The client should maintain a consistent intake of vitamin K and follow a balanced diet.
B) Correct. The client should use a soft-bristled toothbrush to prevent bleeding from the gums, which can occur due to the increased risk of bleeding caused by warfarin. The client should also avoid using dental floss and electric razors.
C) Correct. The client should monitor their blood pressure regularly at home, as warfarin can affect blood pressure and increase the risk of stroke or bleeding complications. The client should report any abnormal readings to their provider.
D) Correct. The client should report any signs of bruising or bleeding to their provider, as they may indicate an adverse reaction to warfarin or an overdose. The client should also report any signs of infection, such as fever, sore throat, or pus, as they may increase the risk of bleeding.
A nurse is teaching a client who has a new prescription for warfarin. Which of the following statements by the client indicates a need for further teaching?
Explanation
A) Incorrect. The client should eat a consistent amount of foods that are high in vitamin K, such as leafy greens, broccoli, and cabbage. Vitamin K can interfere with the anticoagulant effect of warfarin and increase the risk of clotting.
B) Correct. The client should use an electric razor for shaving to prevent cuts and bleeding.
C) Correct. The client should check their blood pressure regularly to monitor for hypertension, which can increase the risk of bleeding complications.
D) Correct. The client should report any signs of bleeding or bruising to their provider, as they may indicate a high INR level or a bleeding disorder.
A client is prescribed metformin for type 2 diabetes mellitus. The nurse instructs the client to take the medication with meals. What is the rationale for this instruction?
Explanation
A) Incorrect. Metformin does not cause hypoglycemia, as it does not stimulate insulin secretion. It lowers blood glucose levels by decreasing hepatic glucose production and increasing insulin sensitivity.
B) Incorrect. Metformin absorption is not affected by food intake. The medication can be taken with or without food, but taking it with meals can help reduce gastrointestinal side effects.
C) Correct. Metformin can cause gastrointestinal upset, such as nausea, diarrhea, and abdominal pain. Taking it with meals can help minimize these effects by slowing down the transit of the medication through the digestive tract.
D) Incorrect. Metformin effectiveness is not influenced by food intake. The medication works by improving glucose metabolism and insulin action.
A nurse is reviewing the medication list of a client who has bipolar disorder. The client is taking lithium carbonate, haloperidol, and lorazepam. The nurse should monitor the client for which of the following adverse effects?
Explanation
A) Incorrect. Extrapyramidal symptoms (EPS), such as dystonia, akathisia, and tardive dyskinesia, are caused by dopamine antagonists, such as haloperidol. However, these symptoms are not related to the combination of medications that the client is taking.
B) Incorrect. Serotonin syndrome is a potentially life-threatening condition that results from excessive serotonin activity in the central nervous system. It is caused by serotonin-enhancing medications, such as antidepressants, opioids, and triptans. None of the medications that the client is taking have this effect.
C) Correct. Neuroleptic malignant syndrome (NMS) is a rare but serious condition that occurs due to dopamine blockade in the brain and peripheral tissues. It is caused by antipsychotic medications, such as haloperidol. The risk of NMS is increased when lithium carbonate is added to antipsychotic therapy, as lithium can potentiate the dopamine-blocking effect of antipsychotics.
D) Incorrect. Lithium toxicity is a condition that occurs when lithium levels exceed the therapeutic range of 0.6 to 1.2 mEq/L. It is caused by factors that affect lithium excretion, such as dehydration, renal impairment, drug interactions, and overdose. None of the other medications that the client is taking interact with lithium or affect its excretion.
A nurse is administering morphine sulfate intravenously to a client who has acute pain due to a kidney stone. Which of the following actions should the nurse take?
Explanation
A) Incorrect. Morphine sulfate does not need to be diluted in normal saline before administration. Diluting the medication can reduce its potency and effectiveness.
B) Correct. Morphine sulfate should be injected slowly over 1 to 2 minutes to prevent adverse effects, such as hypotension, respiratory depression, and nausea.
C) Incorrect. Heparin is not indicated for flushing the IV line before and after administration of morphine sulfate. Heparin is an anticoagulant that can increase the risk of bleeding. The IV line should be flushed with normal saline or sterile water to prevent medication incompatibility and ensure complete delivery of the medication.
D) Incorrect. The nurse should monitor the client's respiratory rate more frequently than every 15 minutes, as morphine sulfate can cause respiratory depression. The nurse should monitor the client's respiratory rate before, during, and after administration of the medication, and at least every 5 minutes until the client's pain is relieved.
A client is receiving phenytoin for seizure prevention. The nurse should instruct the client to avoid which of the following over-the-counter medications while taking phenytoin?
Explanation
A) Incorrect. Acetaminophen is a non-opioid analgesic that can be used safely with phenytoin. However, the nurse should advise the client to limit their intake of acetaminophen to no more than 4 g per day, as higher doses can cause liver toxicity.
B) Incorrect. Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can be used safely with phenytoin. However, the nurse should advise the client to monitor for signs of bleeding, such as bruising, petechiae, and hematuria, as NSAIDs can inhibit platelet aggregation and increase the risk of bleeding.
C) Incorrect. Diphenhydramine is an antihistamine that can be used safely with phenytoin. However, the nurse should advise the client to avoid driving or operating machinery while taking diphenhydramine, as it can cause drowsiness and impair mental alertness.
D) Correct. Ginkgo biloba is an herbal supplement that can interact with phenytoin and reduce its effectiveness. Ginkgo biloba can induce hepatic enzymes that increase the metabolism and clearance of phenytoin, leading to subtherapeutic levels and increased risk of seizures.
A client is prescribed amoxicillin for a bacterial infection. The nurse should teach the client to report which of the following signs of an allergic reaction to the medication?
Explanation
A) Incorrect. Diarrhea is a common side effect of amoxicillin, but it is not a sign of an allergic reaction. The nurse should advise the client to drink plenty of fluids and eat foods that are high in fiber to prevent dehydration and constipation. The nurse should also instruct the client to report severe or bloody diarrhea, as it may indicate a serious condition called pseudomembranous colitis.
B) Correct. Rash is a sign of an allergic reaction to amoxicillin, and it may indicate a hypersensitivity or anaphylactic reaction. The nurse should instruct the client to report any rash, itching, hives, or swelling to their provider immediately and stop taking the medication.
C) Incorrect. Headache is a common side effect of amoxicillin, but it is not a sign of an allergic reaction. The nurse should advise the client to take over-the-counter analgesics, such as acetaminophen or ibuprofen, to relieve headache pain.
D) Incorrect. Nausea is a common side effect of amoxicillin, but it is not a sign of an allergic reaction. The nurse should advise the client to take the medication with food or milk to reduce nausea and vomiting.
Key points to consider when educating patients on medication
A nurse is teaching a client who has been prescribed warfarin for atrial fibrillation. Which of the following statements by the client indicates a need for further education?
Explanation
A) Incorrect. The client should not avoid eating foods that are high in vitamin K, such as leafy greens, broccoli, and soybeans. These foods can interfere with the anticoagulant effect of warfarin and increase the risk of clotting. The client should eat a consistent amount of vitamin K-rich foods and avoid sudden changes in their intake.
B) Correct. The client should use a soft-bristled toothbrush to prevent bleeding from the gums. Warfarin can impair the blood's ability to clot and increase the risk of bleeding from minor injuries.
C) Correct. The client should monitor their blood pressure regularly at home and report any abnormal readings to their provider. Warfarin can affect blood pressure and increase the risk of stroke or bleeding.
D) Correct. The client should report any signs of bruising or bleeding to their provider, such as nosebleeds, blood in urine or stool, heavy menstrual bleeding, or prolonged bleeding from cuts. These signs may indicate that the warfarin dose is too high and needs adjustment.
A nurse is teaching a client who has hypertension about the importance of adhering to their prescribed medication regimen. Which of the following statements by the client indicates a need for further teaching?
Explanation
C) Incorrect. The client should avoid taking their medication with grapefruit juice as it can interfere with the metabolism of some antihypertensive drugs and increase the risk of adverse effects.
A) Correct. The client should not stop taking their medication even if they feel better as this can cause a rebound increase in blood pressure and worsen their condition.
B) Correct. The client should check their blood pressure regularly and record the readings to monitor their response to treatment and identify any changes that may require adjustment of their medication dose.
D) Correct. The client should inform their doctor if they experience any side effects from their medication such as dizziness, headache, fatigue, or cough, as these may indicate a need for a different drug or a lower dose.
A nurse is reviewing the medication list of a client who has diabetes mellitus and is scheduled for surgery. The client takes metformin orally twice a day. Which of the following actions should the nurse take?
Explanation
B) Correct. The nurse should instruct the client to hold their metformin for 48 hours before and after surgery as this drug can increase the risk of lactic acidosis in clients who are undergoing procedures that involve contrast media or who have impaired renal function due to dehydration or hypotension.
A) Incorrect. The nurse should not instruct the client to take their morning dose of metformin with a sip of water on the day of surgery as this can cause hypoglycemia during anesthesia or interfere with contrast media if used during surgery.
C) Incorrect. The nurse should not instruct the client to resume their metformin as soon as they can tolerate oral intake after surgery as this can cause lactic acidosis if the client's renal function is not fully restored or if they receive contrast media during surgery or postoperatively.
D) Incorrect. The nurse should not instruct the client to switch to insulin injections until they recover from surgery as this can cause hyperglycemia or hypoglycemia depending on the type and dose of insulin used and the client's nutritional status and blood glucose levels.
A nurse is preparing to administer a new prescription for digoxin 0.125 mg orally once daily to a client who has heart failure. Which of the following actions should the nurse take before giving the medication?
Explanation
A) Correct. The nurse should check the client's apical pulse for one full minute before giving digoxin as this drug can cause bradycardia and heart block. The nurse should withhold the medication and notify the provider if the pulse is less than 60 beats/min or irregular.
B) Incorrect. The nurse should check the client's serum potassium level periodically while taking digoxin as this drug can cause hypokalemia or hyperkalemia, which can affect its therapeutic effect and toxicity. However, this is not a priority action before giving each dose of digoxin.
C) Incorrect. The nurse should check the client's blood pressure in both arms periodically while taking digoxin as this drug can cause hypotension or hypertension, which can affect its efficacy and safety. However, this is not a priority action before giving each dose of digoxin.
D) Incorrect. The nurse should check the client's serum digoxin level periodically while taking digoxin as this drug has a narrow therapeutic range and can cause toxicity if the level is above 2 ng/mL. However, this is not a priority action before giving each dose of digoxin.
A nurse is providing discharge instructions to a client who has a new prescription for warfarin. Which of the following foods should the nurse advise the client to limit in their diet?
Explanation
A) Correct. The nurse should advise the client to limit spinach in their diet as this food is high in vitamin K, which can antagonize the anticoagulant effect of warfarin and increase the risk of thrombosis.
B) Incorrect. The nurse should not advise the client to limit bananas in their diet as this food is high in potassium, which can help prevent hypokalemia that can occur with some anticoagulants such as heparin. Bananas do not affect the action of warfarin.
C) Incorrect. The nurse should not advise the client to limit cheese in their diet as this food is high in calcium, which can help prevent osteoporosis that can occur with long-term use of warfarin. Cheese does not affect the action of warfarin.
D) Incorrect. The nurse should not advise the client to limit eggs in their diet as this food is high in protein, which can help maintain muscle mass and wound healing that can be impaired by warfarin. Eggs do not affect the action of warfarin.
A nurse is caring for a client who has schizophrenia and is taking clozapine. The nurse notices that the client has a fever, sore throat, and malaise. Which of the following actions should the nurse take?
Explanation
B) Correct. The nurse should obtain a blood sample from the client for a complete blood count as these symptoms can indicate agranulocytosis, a potentially fatal adverse effect of clozapine that causes a severe decrease in white blood cells and increases the risk of infection.
A) Incorrect. The nurse should not administer acetaminophen to the client as this drug can mask the signs of infection and delay diagnosis and treatment of agranulocytosis.
C) Incorrect. The nurse should encourage the client to drink plenty of fluids and rest, but this action alone would not address the potential serious adverse effect of agranulocytosis associated with clozapine. Obtaining a blood sample for a complete blood count is necessary to assess the client's white blood cell count and determine if agranulocytosis is present.
D) Incorrect. Discontinuing clozapine and notifying the provider is important, but it should be done after obtaining a blood sample for a complete blood count to confirm the presence of agranulocytosis. This allows for appropriate medical management and alternative treatment options to be initiated.
A nurse is preparing to administer insulin to a client who has type 1 diabetes mellitus. Which of the following actions by the nurse demonstrates proper technique for mixing regular and NPH insulin in the same syringe?
Explanation
A) Incorrect. The nurse should inject air into the regular vial first, then into the NPH vial. This can prevent contamination of the regular insulin with NPH insulin and ensure accurate dosing.
B) Correct. The nurse should draw up regular insulin first, then NPH insulin. This can prevent contamination of the regular insulin with NPH insulin and ensure accurate dosing. Regular insulin is clear and NPH insulin is cloudy.
C) Correct. The nurse should roll the NPH vial between their palms before drawing up insulin. This can resuspend the insulin particles that may have settled at the bottom of the vial and ensure uniform concentration.
D) Correct. The nurse should wipe the rubber stoppers of both vials with alcohol swabs before inserting needles. This can reduce the risk of infection and contamination.
Importance of patient education on medication purpose, dosage, and side effects
A nurse is teaching a client who has hypertension about the purpose of taking a beta blocker. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Beta blockers work by blocking the effects of adrenaline on the heart and blood vessels, which results in a lower heart rate and blood pressure.
A) is incorrect because beta blockers do not dilate blood vessels.
C) is incorrect because beta blockers do not increase urine output.
D) is incorrect because beta blockers do not reduce the fluid in the lungs.
A nurse is assessing a client who has been taking digoxin for heart failure. Which of the following findings should alert the nurse to a possible digoxin toxicity?
Explanation
D) Correct. All of the above are signs of digoxin toxicity, which can be life-threatening if not treated promptly. The nurse should monitor the client's vital signs, serum digoxin level, serum potassium level, and electrocardiogram, and notify the provider immediately.
A) Incorrect. Nausea and vomiting are signs of digoxin toxicity, but not the only ones.
B) Incorrect. Bradycardia and dysrhythmias are signs of digoxin toxicity, but not the only ones.
C) Incorrect. Yellow-green halos around lights are signs of digoxin toxicity, but not the only ones.
A nurse is providing discharge instructions to a client who has a new prescription for nitroglycerin patches for angina pectoris. Which of the following information should the nurse include in the teaching?
Explanation
D) Correct. All of the above are correct information that the nurse should include in the teaching. The nurse should also instruct the client to rotate the patch sites, store the patches in a cool and dry place, and report any headaches, dizziness, or flushing to their provider.
A) Incorrect. Applying a new patch every 12 hours is correct information, but not the only one.
B) Incorrect. Removing the old patch before applying a new one is correct information, but not the only one.
C) Incorrect. Placing the patch on a hairless area of the chest or upper arm is correct information, but not the only one.
A nurse is preparing to administer insulin to a client who has type 1 diabetes mellitus. The nurse should follow which of the following guidelines when drawing up insulin from a vial?
Explanation
D) Correct. All of the above are correct guidelines that the nurse should follow when drawing up insulin from a vial. The nurse should also use an insulin syringe with units that match the insulin concentration, use aseptic technique, and verify the dosage with another nurse before administering it.
A) Incorrect. Injecting air into the vial equal to the amount of insulin needed is a correct guideline, but not the only one.
B) Incorrect. Holding the syringe with the needle pointing up and tapping it gently to remove air bubbles is a correct guideline, but not the only one.
C) Incorrect. Checking the expiration date and clarity of the insulin before drawing it up is a correct guideline, but not the only one.
A client is prescribed an antibiotic for a urinary tract infection. The nurse instructs the client to take the medication as directed until it is finished. Which of the following statements by the client indicates a need for further teaching?
Explanation
Antibiotics should be taken as prescribed until they are finished, even if the symptoms improve or disappear. This is to ensure that the infection is completely eradicated and to prevent the development of antibiotic resistance.
A) is correct because drinking fluids can help flush out the bacteria and prevent dehydration.
B) is correct because a rash or hives can indicate an allergic reaction to the antibiotic, which requires immediate medical attention.
C) is correct because some antibiotics can cause stomach irritation, which can be minimized by taking them with food or milk.
Exams on Medication Reconciliation and Patient Education
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction
- Obtaining Accurate Medication History
- Approach to obtaining Accurate Medication History
- Patient education on medication purpose, dosage, and side effects
- Key points to consider when educating patients on medication
- Importance of patient education on medication purpose, dosage, and side effects
- Conclusion
- Summary
Notes Highlighting is available once you sign in. Login Here.
Objectives
- To understand the importance of obtaining accurate medication history from patients.
- To identify the sources and methods of obtaining medication history.
- To recognize the common errors and challenges in obtaining medication history.
- To apply strategies to improve the accuracy and completeness of medication history.
- Explain the importance of patient education on medication
- Describe the key components of medication education: purpose, dosage, and side effects
- Apply the principles of effective communication and teaching strategies to educate patients on medication
Introduction
- Medication history is a record of all the medications a patient is currently taking or has taken in the past.
- Medication reconciliation is the process of comparing a patient's medication orders to all of the medications that the patient has been taking. This reconciliation is done to avoid medication errors such as omissions, duplications, dosing errors, or drug interactions.
- Obtaining an accurate medication history is essential for safe and effective patient care.
- Medication errors can cause adverse drug events, drug interactions, allergic reactions, and other complications.
- Nurses play a key role in obtaining and verifying medication history from patients and other sources.
- Medication education involves informing patients about the purpose, dosage, and side effects of their prescribed drugs, as well as how to take them safely and correctly.
- Medication education also empowers patients to make informed decisions about their health and to report any problems or concerns to their healthcare providers.

Obtaining Accurate Medication History
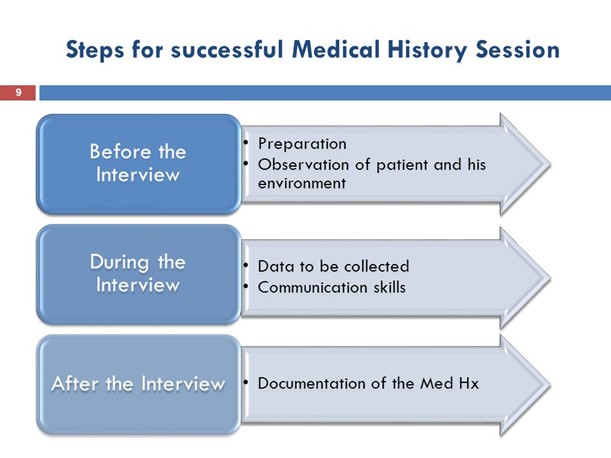
Steps for Obtaining Medication History
- Prepare for the interview: gather relevant information, equipment, and documents; establish rapport with the patient; explain the purpose and importance of the interview; obtain consent if needed.
- Ask open-ended questions: use clear and simple language; avoid leading or suggestive questions; encourage the patient to provide as much detail as possible; use prompts and cues to elicit more information.
- Use multiple sources of information: ask the patient to show their medication containers, labels, prescriptions, or lists; contact the patient's pharmacy, primary care provider, or other health care providers; review the patient's medical records, medication reconciliation forms, or discharge summaries.
- Verify and document the information: compare the information from different sources and identify any discrepancies; clarify any unclear or incomplete information with the patient or other sources; document the medication history using a standardized format and include the date, time, source, and method of verification.
Approach to obtaining Accurate Medication History
- Be respectful and nonjudgmental: acknowledge the patient's feelings and concerns; avoid blaming or criticizing the patient for their medication use; express empathy and support.
- Be thorough and systematic: cover all categories of medications, including prescription, over-the-counter, herbal, dietary, recreational, and illicit drugs; ask about the dose, frequency, route, duration, indication, and adherence of each medication; ask about any changes, additions, or discontinuations of medications; ask about any allergies, intolerances, side effects, or problems with medications.
- Be aware of potential barriers and challenges: consider the patient's age, cognitive status, literacy level, language preference, cultural background, and health beliefs; use appropriate communication strategies and tools to overcome these barriers; seek assistance from interpreters, family members, caregivers, or other health care professionals if needed.
Patient education on medication purpose, dosage, and side effects
- Patient education on medication is an essential part of nursing care that aims to improve patient outcomes and adherence to treatment.
- It involves providing accurate, clear, and individualized information to patients about their medications, including the purpose, dosage, and side effects of each drug.
- Patient education on medication can also help prevent medication errors, adverse reactions, and interactions.

Key points to consider when educating patients on medication
- Purpose: Explain to the patient why they need to take the medication, what it does, and how it works.
- Dosage: Instruct the patient on how much, how often, and when to take the medication. Also, inform them about the route of administration (e.g., oral, intravenous, etc.) and any special instructions (e.g., with or without food, shake well before use, etc.).
- Side effects: Warn the patient about the possible side effects of the medication and what to do if they occur. Also, advise them about any signs of allergic reaction or overdose and when to seek medical attention.

Importance of patient education on medication purpose, dosage, and side effects
It can help patients to:
- Understand the rationale and benefits of their prescribed medication regimen
- Adhere to the recommended dosage and frequency of administration
- Recognize and report any potential or actual adverse reactions or interactions
- Prevent medication errors and misuse
- Enhance their self-care and quality of life
Conclusion
- Obtaining accurate medication history is an essential nursing skill that can improve patient safety and quality of care.
- Nurses should obtain medication history from multiple sources and methods, communicate effectively with patients and other health care providers, recognize and overcome common errors and challenges, and implement strategies to ensure accuracy and completeness of medication history.
- Patient education on medication is an essential component of nursing practice that can improve patient satisfaction, compliance, and safety.
- Nurses should use effective communication and teaching strategies to educate patients on the purpose, dosage, and side effects of their medication.
- Nurses should also assess the patient's learning needs, preferences, and barriers, and tailor the education accordingly.
- By providing patient education on medication, nurses can enhance the quality of care and promote patient autonomy and self-care.
Summary
- To obtain accurate medication history, nurses need to use multiple sources of information, such as the patient, family members, caregivers, pharmacy records, medication labels, and electronic health records.
- Nurses also need to use effective communication skills, such as openended questions, active listening, and empathy, to elicit accurate and complete information from the patient.
- Nurses should be aware of the common errors and challenges in obtaining medication history
- The purpose of medication education is to help patients understand why they need to take their drugs, how much and how often to take them, and what to expect from them.
- The dosage of medication is determined by factors such as the patient's weight, age, condition, and other medications.
- The side effects of medication are the unwanted or harmful effects that may occur when taking the drugs.
- Some side effects are common and mild, such as nausea or headache, while others are rare and serious, such as allergic reactions or liver damage.
- Patients should be informed about the possible side effects of their medication and how to manage or prevent them.
- Patients should also be taught how to recognize and report any signs of medication errors, interactions, or adverse reactions.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Medication Reconciliation and Patient Education
This filled cannot be empty

