Please set your exam date
Communicable Diseases
Study Questions
Dengue fever
Explanation
Choice A rationale:
Influenza is not mosquito-borne. It is a respiratory viral infection spread through respiratory droplets, not through mosquitoes.
Choice B rationale:
Dengue fever is mosquito-borne and is transmitted primarily by the Aedes aegypti mosquito. It is prevalent in tropical regions and can lead to severe complications like dengue hemorrhagic fever, which can be life-threatening.
Choice C rationale:
Malaria is also mosquito-borne, but it is caused by the Plasmodium parasite transmitted by the Anopheles mosquito. While it can lead to severe complications, such as cerebral malaria, it does not cause dengue hemorrhagic fever.
Choice D rationale:
Tuberculosis is not mosquito-borne. It is a bacterial infection that primarily affects the lungs and is transmitted through respiratory droplets.
Explanation
Choice A rationale:
Anopheles mosquito is responsible for transmitting malaria, not dengue fever. Malaria is prevalent in some tropical and subtropical regions and is caused by the Plasmodium parasite.
Choice B rationale:
Culex mosquito can transmit diseases like West Nile virus and some types of encephalitis but not dengue fever.
Choice C rationale:
Aedes aegypti and Aedes albopictus mosquitoes are the primary vectors responsible for transmitting dengue fever. They thrive in subtropical and tropical regions and are most active during the day.
Choice D rationale:
Blackfly is responsible for transmitting onchocerciasis (river blindness) but not dengue fever.
Explanation
Choice A rationale:
Joint and muscle pain are common symptoms of dengue fever, especially during the acute phase of the infection. Patients often experience severe pain, giving it the colloquial name "breakbone fever."
Choice B rationale:
Influenza can cause muscle aches, but it is not relevant in this situation, as the patient is suspected of having dengue fever.
Choice C rationale:
The statement that dengue fever doesn't cause any pain and is a mild infection is incorrect. Dengue fever can cause severe symptoms, and joint/muscle pain is one of them.
Choice D rationale:
Malaria can cause muscle pain, but the patient is suspected of having dengue fever, not malaria. The focus should be on the symptoms associated with dengue fever.
Explanation
Choice A rationale:
Wearing long sleeves and using mosquito repellent is an appropriate preventive measure to avoid mosquito bites and reduce the risk of dengue fever transmission. This statement indicates the client understands the importance of protective measures.
Choice B rationale:
Dengue fever is indeed caused by a virus in the flavivirus genus. This statement demonstrates accurate knowledge of the etiology of the disease.
Choice C rationale:
This statement indicates a need for further teaching. Dengue fever is not transmitted from person to person through close contact. The primary mode of transmission is through the bite of an infected Aedes mosquito.
Choice D rationale:
There are indeed four serotypes of the dengue virus, and they share genetic similarities. This statement shows an accurate understanding of the virus's characteristics.
Explanation
Choice A rationale:
The patient's vaccination history is not directly relevant to confirming a suspected case of dengue fever. Vaccination for dengue fever is not widely available, and the diagnosis relies on other factors.
Choice B rationale:
While exposure to water sources may be relevant in some infectious diseases, it does not specifically confirm or rule out a suspected case of dengue fever.
Choice C rationale:
The patient's travel itinerary and dates are crucial in confirming a suspected case of dengue fever. Knowing the patient's recent travel to a tropical region with a high incidence of dengue fever is essential for accurate diagnosis and appropriate management.
Choice D rationale:
The patient's dietary habits are not directly related to confirming a suspected case of dengue fever. While nutrition is important for overall health, it does not impact the diagnosis of the disease.
A client with dengue fever has a platelet count of 120,000/mm3. What intervention should the nurse prioritize?
Explanation
Choice A rationale:
Administering acetaminophen for fever is a reasonable intervention for the client with dengue fever. However, it is not the priority when the platelet count is low.
Choice B rationale:
Administering a blood transfusion is not the priority intervention based solely on the platelet count of 120,000/mm3. Platelet transfusion is typically considered when the platelet count drops significantly lower, leading to bleeding complications.
Choice C rationale:
Encouraging bed rest is a reasonable intervention for a client with dengue fever to conserve energy and facilitate recovery. However, it is not the priority over monitoring for potential bleeding complications.
Choice D rationale:
Monitoring for bleeding and petechiae is the priority intervention in this case. Dengue fever can cause thrombocytopenia, leading to an increased risk of bleeding. The nurse must closely monitor the client's platelet count and assess for any signs of bleeding or petechiae to detect complications early and provide appropriate interventions.
The nurse is caring for multiple clients with suspected dengue fever in a hospital setting. Which personal protective equipment (PPE) should the nurse wear while providing care to these clients?
Explanation
Choice A rationale:
Gown and gloves are not the appropriate personal protective equipment (PPE) for suspected dengue fever. Dengue fever is primarily transmitted through mosquito bites, and wearing a gown is unnecessary for protection. Additionally, gloves alone may not provide adequate protection against mosquito bites.
Choice B rationale:
The correct choice for PPE when caring for clients with suspected dengue fever is a mask and goggles. These items protect the nurse from inhaling infectious droplets and prevent transmission through the mucous membranes of the eyes. The main mode of transmission of dengue fever is through infected mosquito bites, so a mask and goggles are essential in preventing the nurse from contracting the disease.
Choice C rationale:
The N95 respirator is designed to filter out airborne particles and is typically used in settings where there is a risk of inhaling infectious droplets, such as during procedures that generate aerosols. While it provides a high level of protection, it is not the most appropriate choice for dengue fever, which primarily spreads through mosquito bites.
Choice D rationale:
Gloves and shoe covers are not sufficient protection against dengue fever, as the primary mode of transmission is through mosquito bites. Shoe covers are not necessary for this situation, and gloves alone may not fully prevent mosquito bites.
A nurse is educating a group of travelers about dengue fever prevention. Which of the following measures should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A rationale:
Using mosquito repellents containing DEET is an effective measure for preventing dengue fever. DEET is a mosquito repellent that provides protection against mosquito bites, reducing the risk of infection.
Choice B rationale:
Wearing long sleeves and pants can help prevent mosquito bites and reduce the risk of dengue fever transmission. Covering exposed skin makes it harder for mosquitoes to bite and transmit the virus.
Choice C rationale:
Applying sunscreen before mosquito repellent is not an appropriate measure for dengue fever prevention. While sunscreen is important for protecting the skin from UV rays, it should be applied after mosquito repellent for the best protection against mosquito bites.
Choice D rationale:
Staying indoors during peak mosquito activity is a helpful preventive measure. Mosquitoes are most active during dawn and dusk, so staying indoors during these times can reduce the risk of mosquito bites and potential infection.
Choice E rationale:
Emptying standing water containers regularly is crucial for dengue fever prevention. Mosquitoes breed in standing water, and removing these breeding sites can help control mosquito populations and reduce the risk of dengue transmission.
Explanation
Choice A rationale:
Hypotension, pleural effusion, and ascites are signs and symptoms associated with the severe dengue phase, also known as dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS) These symptoms occur when the disease progresses to a more severe form, characterized by plasma leakage and organ impairment.
Choice B rationale:
Altered LOC (level of consciousness), seizures, and slow HR (heart rate) are not typical signs and symptoms of dengue fever. These symptoms may be indicative of other conditions but are not directly related to dengue fever.
Choice C rationale:
Sudden-onset fever, headache, muscle and joint pains are the classic symptoms of dengue fever. These symptoms typically appear after an incubation period of 4 to 10 days and are followed by a febrile phase, which may last for a few days.
Choice D rationale:
Increased vascular permeability, thrombocytopenia, and hemorrhage are characteristic features of severe dengue fever, specifically DHF or DSS. These manifestations occur due to the increased permeability of blood vessels and low platelet counts, leading to bleeding tendencies and potential shock.
Explanation
Choice A rationale:
Incorrect. The client should avoid anti-inflammatory drugs like ibuprofen because they can increase the risk of bleeding, which is a concern in dengue fever management.
Choice B rationale:
Correct. Early detection is essential in managing dengue fever because it allows for timely medical intervention, which can prevent complications and improve outcomes.
Choice C rationale:
Correct. The client needs to avoid aspirin as it can worsen bleeding in dengue fever due to its antiplatelet effects.
Choice D rationale:
Correct. In severe cases of dengue fever, a client may require hospitalization and receive IV fluids and blood platelet transfusions to maintain fluid balance and manage low platelet levels.
Choice E rationale:
Correct. Rest and acetaminophen for pain relief are appropriate measures in dengue fever management to help alleviate symptoms and support the body's healing process.
Explanation
Choice A rationale:
Incorrect. While vomiting can be a symptom of dengue fever, it is not the statement that the nurse would expect the client to make regarding the disease.
Choice B rationale:
Incorrect. The nurse would not expect the client to state that their platelet count is within the normal range since dengue fever typically causes a decrease in platelet count.
Choice C rationale:
Correct. A decrease in hematocrit by more than 20% from baseline is indicative of plasma leakage, a complication of severe dengue fever known as dengue hemorrhagic fever.
Choice D rationale:
Incorrect. Taking anti-inflammatory drugs like ibuprofen to reduce fever is not recommended in dengue fever management, as it can increase the risk of bleeding.
Explanation
Choice A rationale:
Incorrect. While avoiding aspirin is generally advised in dengue fever management, it is not the most appropriate statement to address the signs of shock and rapid pulse.
Choice B rationale:
Incorrect. Though monitoring platelet count is important in dengue fever, it does not address the urgent need for intervention in a client exhibiting signs of shock.
Choice C rationale:
Correct. The nurse should administer IV fluids to improve hydration and help stabilize the client's condition in response to signs of shock.
Choice D rationale:
Incorrect. Ibuprofen is an anti-inflammatory drug, and its use is not recommended in dengue fever due to the increased risk of bleeding.
Explanation
Choice A rationale:
During the critical phase of dengue fever, which typically occurs around 3-7 days after the onset of symptoms, the client is at a higher risk of developing severe bleeding and organ failure due to plasma leakage and decreased platelet counts. Assessing for signs of bleeding, such as petechiae, ecchymosis, gum bleeding, or hematuria, is essential to detect any worsening condition promptly. Additionally, monitoring for signs of organ failure, such as altered mental status, respiratory distress, or oliguria, is crucial for timely intervention and appropriate management.
Choice B rationale:
Providing supplemental oxygen as needed may be beneficial in certain cases of dengue fever with respiratory distress or hypoxemia. However, during the critical phase, the priority is to assess for bleeding and organ failure, as these complications pose a more immediate threat to the client's life.
Choice C rationale:
Monitoring intake and output is a crucial nursing intervention for clients with dengue fever to ensure adequate hydration and prevent dehydration. While this is essential throughout the course of the illness, it is not the priority during the critical phase when bleeding and organ failure are of greater concern.
Choice D rationale:
Administering antipyretics for fever control may be necessary in the febrile phase of dengue fever to alleviate discomfort and manage fever. However, during the critical phase, the priority shifts to assessing for and managing potentially life-threatening complications like bleeding and organ failure.
Explanation
Choice A rationale:
Administering aspirin for pain relief is contraindicated in clients with dengue fever due to its anticoagulant properties, which can further increase the risk of bleeding.
Choice B rationale:
While encouraging ambulation is generally beneficial for improving circulation in various conditions, it is not a suitable intervention during the critical phase of dengue fever when the client is experiencing severe plasma leakage and reduced platelet counts, which can lead to significant bleeding complications.
Choice C rationale:
Transfusion of blood products, such as platelets and packed red blood cells, may be necessary in clients with dengue fever who have severe thrombocytopenia and hematocrit elevation. Platelet count below 100,000/mm3 is a common threshold for initiating platelet transfusion in dengue fever to prevent bleeding complications, and a 25% increase in hematocrit from baseline indicates hemoconcentration, which may necessitate red blood cell transfusion.
Choice D rationale:
Monitoring SpO2 (oxygen saturation) and ABGs (arterial blood gases) regularly is important for assessing respiratory status in various conditions. However, during dengue fever, the more critical concern is the risk of bleeding and plasma leakage, making transfusion of blood products a higher priority intervention.
Explanation
Choice A rationale:
Elevating the client's legs may be helpful in certain situations to improve venous return and manage hypotension. However, during severe plasma leakage and organ failure in dengue fever, the priority is to control bleeding, and applying pressure to bleeding sites can help achieve hemostasis.
Choice B rationale:
Applying pressure to bleeding sites is a priority intervention in clients with dengue fever experiencing severe plasma leakage and melena. This helps to control bleeding and prevent further blood loss, which is vital during the critical phase.
Choice C rationale:
Administering acetaminophen for pain relief can be appropriate for clients with dengue fever, especially in the febrile phase when fever and discomfort are prominent. However, during the critical phase with plasma leakage and organ failure, the priority is to manage life-threatening complications like bleeding and hepatic damage.
Choice D rationale:
Providing supplemental oxygen is essential for clients experiencing respiratory distress or hypoxemia. However, in the scenario described, the client's main priority is controlling bleeding and managing organ failure rather than addressing respiratory issues.
Explanation
Choice A rationale:
The nurse should include the recommendation to use mosquito repellent with DEET in the teaching session as DEET is an effective insect repellent that helps prevent mosquito bites.
Choice B rationale:
Removing standing water to eliminate breeding sites should be included in the education session as stagnant water serves as a breeding ground for mosquitoes, and eliminating such sites can reduce the mosquito population.
Choice C rationale:
The nurse should not include taking aspirin for fever and joint pain relief in the teaching session because aspirin can increase the risk of bleeding, which is especially concerning in dengue fever cases due to its association with bleeding complications.
Choice D rationale:
Wearing long sleeves and pants to protect against mosquito bites should be part of the teaching session as it provides physical barriers to prevent mosquito bites.
Choice E rationale:
Avoiding going outdoors during the daytime should be included in the teaching session as dengue fever is primarily transmitted by mosquitoes, which are more active during the daytime.
Explanation
Choice A rationale:
The nurse should include the use of mosquito repellent, protective clothing (such as long sleeves and pants), and bed nets in the education session as these measures are effective in preventing mosquito bites and reducing the risk of dengue fever transmission.
Choice B rationale:
Regular consumption of herbal supplements is not an evidence-based preventive measure for dengue fever. Therefore, it should not be included in the education session.
Choice C rationale:
Wearing bright-colored clothing is not a preventive measure for dengue fever. Mosquitoes are attracted to dark colors, but the color of clothing does not significantly impact their attraction to humans.
Choice D rationale:
Storing water in open containers for easy access should not be included in the education session as it creates a breeding site for mosquitoes, increasing the risk of dengue transmission.
Explanation
Choice A rationale:
Severe headache and joint pain are common symptoms of dengue fever, but they are not specific to dengue hemorrhagic fever (DHF) These symptoms are not indicative of the severity of the disease.
Choice B rationale:
Plasma leakage and thrombocytopenia are characteristic features of dengue hemorrhagic fever (DHF) Plasma leakage can lead to a drop in blood volume and can cause shock.
Choice C rationale:
Mild flu-like symptoms with self-limiting recovery are typical of uncomplicated dengue fever and are not specific to DHF.
Choice D rationale:
Life-threatening shock and organ failure are severe complications of DHF, and the nurse should anticipate these symptoms in a client with DHF.
Choice E rationale:
Recovery within 7-10 days with proper treatment is a general description of dengue fever without complications. It does not describe the course of DHF, which can be life-threatening and require immediate medical attention.
Explanation
Choice A rationale:
The client's statement is correct. Eliminating standing water around the home is an essential preventive measure for dengue fever as it helps in reducing mosquito breeding sites. Mosquitoes that transmit the dengue virus breed in stagnant water, so eliminating these breeding sites can reduce the risk of infection.
Choice B rationale:
The client's statement is correct. Seeking medical attention early when suspecting dengue fever is crucial because early detection and treatment can help prevent complications and severe forms of the disease. Dengue fever can progress rapidly, and timely medical intervention is necessary.
Choice C rationale:
The client's statement indicates a need for further teaching. Using insecticides indoors can be an important preventive measure to avoid mosquito bites, especially in areas where dengue is prevalent. Mosquitoes can enter homes through open doors and windows, and using insecticides can help reduce the risk of mosquito bites indoors.
Choice D rationale:
The client's statement is correct. Using mosquito repellent and wearing protective clothing are effective ways to avoid mosquito bites, especially during peak mosquito activity times. Dengue fever is transmitted through the bites of infected mosquitoes, and these preventive measures can help reduce the risk of infection.
Explanation
Choice A rationale:
The nurse's statement is incorrect. Dengue fever is not only endemic to Asia and the Pacific. It is a mosquito-borne viral infection that can be found in tropical and subtropical regions around the world, including parts of Africa, the Americas, the Mediterranean, and Southeast Asia.
Choice B rationale:
The nurse's statement is incorrect. While dengue fever is prevalent in many countries in Africa, it is not limited to Africa alone. It is found in multiple regions worldwide where the appropriate mosquito vectors are present.
Choice C rationale:
The nurse's statement is accurate. According to the World Health Organization (WHO), an estimated 390 million people globally are affected by severe dengue each year. Severe dengue, also known as dengue hemorrhagic fever or dengue shock syndrome, can be a life-threatening condition.
Choice D rationale:
The nurse's statement is incorrect. Dengue fever is primarily found in tropical and subtropical regions, not temperate regions. The Aedes mosquitoes, which transmit the virus, thrive in warm and humid environments, making temperate regions less conducive to dengue transmission.
Explanation
Choice A rationale:
Providing mosquito netting around the bed is not the highest priority for a client with dengue shock syndrome (DSS) DSS is a severe form of dengue fever characterized by plasma leakage, bleeding, and organ failure. While mosquito bites should be avoided, the priority is to manage the client's critical condition and complications.
Choice B rationale:
Administering herbal remedies for pain relief is not the highest priority for a client with DSS. Pain relief is important, but the priority lies in addressing the life-threatening manifestations of DSS, such as maintaining adequate fluid balance and preventing further complications.
Choice C rationale:
Monitoring vital signs and fluid status closely is the highest priority for a client with DSS. DSS can lead to severe dehydration, hypovolemic shock, and circulatory collapse. Close monitoring of vital signs and fluid status allows early detection of any worsening condition and enables prompt intervention.
Choice D rationale:
Encouraging the client to engage in physical activities is not appropriate for a client with DSS. In fact, physical activities should be restricted for a client with severe dengue to prevent complications and excessive strain on the cardiovascular system. Rest is essential for recovery.
Explanation
Choice A rationale:
Using open containers to store water is not an effective measure to prevent dengue fever. Mosquitoes that transmit the dengue virus breed in standing water, so using open containers will only provide breeding sites for mosquitoes, increasing the risk of dengue transmission.
Choice B rationale:
Applying mosquito repellent while outdoors is an effective measure to prevent dengue fever. Mosquito repellents containing DEET, picaridin, or other recommended ingredients can help deter mosquitoes from biting, reducing the risk of contracting the dengue virus.
Choice C rationale:
Consuming raw seafood regularly is unrelated to preventing dengue fever. Dengue fever is transmitted by mosquitoes, not through the consumption of food.
Choice D rationale:
Staying outdoors during peak mosquito activity is not an effective measure to prevent dengue fever. Being outdoors during peak mosquito activity increases the likelihood of mosquito bites and potential transmission of the dengue virus.
Explanation
Choice A rationale:
Recovery from uncomplicated dengue fever typically occurs within 3-5 days without specific treatment. Most cases of dengue fever are self-limiting, and the body's immune response clears the virus within this timeframe.
Choice B rationale:
Recovery from dengue hemorrhagic fever usually takes 2-3 weeks. Dengue hemorrhagic fever is a severe form of the disease that can lead to bleeding complications and requires medical intervention and supportive care.
Choice C rationale:
Bed rest is necessary for dengue fever recovery. The client's body needs adequate rest to recover from the infection and avoid complications.
Choice D rationale:
The client should not engage in vigorous physical activity to speed up recovery. Strenuous activity can worsen the symptoms and potentially lead to complications, especially in cases of dengue hemorrhagic fever.
Explanation
Choice A rationale:
Avoiding travel to dengue-affected areas is indeed an effective measure to prevent dengue fever. By staying away from areas with known dengue transmission, travelers can significantly reduce their risk of contracting the virus.
Choice B rationale:
Using insect repellent with DEET is recommended to prevent mosquito bites and, consequently, dengue fever. DEET is an effective mosquito repellent that can provide protection against mosquito-borne diseases.
Choice C rationale:
Wearing long-sleeved clothing and pants can help prevent mosquito bites and reduce the risk of dengue fever transmission. Covering exposed skin makes it more difficult for mosquitoes to bite.
Choice D rationale:
Applying sunscreen frequently is not directly related to preventing dengue fever. While sun protection is essential, it does not contribute to mosquito bite prevention or dengue virus transmission.
Influenza.
.
Influenza
Explanation
Choice A rationale:
Influenza is primarily transmitted through respiratory droplets generated by coughing or sneezing. Influenza is a viral respiratory infection, and the main mode of transmission is through respiratory droplets when infected individuals cough or sneeze. These droplets can be inhaled by others, leading to the spread of the virus.
Choice B rationale:
Influenza is not transmitted through the bite of infected mosquitoes. Influenza is a human-to-human respiratory virus and is not spread by mosquitoes or other insects.
Choice C rationale:
Influenza does not spread through direct contact with infected animals. While some animal species can be affected by their own strains of influenza viruses, human influenza primarily spreads among people.
Choice D rationale:
This is the correct choice. Influenza is transmitted through respiratory droplets generated by coughing or sneezing. The droplets can travel a short distance and can be inhaled by individuals nearby, leading to infection.
Explanation
Choice A rationale:
Rash on the skin is not a common symptom of influenza. Influenza primarily affects the respiratory system and does not typically cause skin rashes.
Choice B rationale:
Diarrhea is not a typical symptom of influenza. While some gastrointestinal symptoms may occur in some cases, they are not characteristic of influenza.
Choice C rationale:
This is a correct choice. Muscle aches (myalgia) are commonly associated with influenza. Many people with influenza experience muscle pain and soreness.
Choice D rationale:
Increased appetite is not a common symptom of influenza. In fact, loss of appetite is more common during an influenza infection.
Choice E rationale:
This is a correct choice. Dry cough is a common symptom of influenza. Influenza can cause irritation in the respiratory tract, leading to a dry cough.
Explanation
Choice A rationale:
"The incubation period of influenza ranges from 2 to 5 days." This is the correct response. The incubation period of influenza, which refers to the time between exposure to the virus and the onset of symptoms, typically ranges from 2 to 5 days.
Choice B rationale:
"The incubation period of influenza is about 1 week." This is incorrect. The incubation period of influenza is shorter than one week.
Choice C rationale:
"The incubation period of influenza can last up to 2 weeks." This is incorrect. While some other viral illnesses may have longer incubation periods, influenza usually has a shorter incubation period.
Choice D rationale:
"The incubation period of influenza is usually less than 24 hours." This is incorrect. The incubation period of influenza is longer than just a few hours; it typically takes a couple of days before symptoms appear.
Explanation
Choice A rationale:
Influenza can indeed lead to viral pneumonia. Influenza is caused by a respiratory virus that primarily affects the nose, throat, and lungs. Severe cases of influenza can progress to viral pneumonia, a serious and potentially life-threatening complication.
Choice B rationale:
Myositis is a potential complication of influenza. Myositis refers to inflammation of the muscles, which can occur as a complication of viral infections, including influenza. It can lead to muscle pain, weakness, and swelling.
Choice C rationale:
This statement requires further clarification. Reye syndrome is not a complication of influenza in adults; it primarily affects children and teenagers recovering from a viral infection like influenza or chickenpox. Reye syndrome involves brain and liver inflammation and is associated with the use of aspirin during viral infections.
Choice D rationale:
People with weakened immune systems are indeed at risk of severe influenza complications. Individuals with weakened immune systems, such as the elderly, pregnant women, and those with certain medical conditions, are more susceptible to severe influenza symptoms and complications.
Explanation
Choice A rationale:
Wearing a face mask at all times, even indoors, is not the best preventive measure for influenza. While face masks can help reduce the spread of respiratory viruses, they are more effective when worn in situations with a higher risk of exposure, such as crowded places or healthcare settings.
Choice B rationale:
Avoiding close contact with sick individuals is a valid preventive measure for influenza. Influenza is primarily spread through respiratory droplets when an infected person coughs, sneezes, or talks. Avoiding close contact can help reduce the risk of exposure.
Choice C rationale:
Consuming raw garlic daily to boost immunity is not a proven preventive measure for influenza. While garlic has some health benefits, there is limited scientific evidence to support its specific role in preventing influenza.
Choice D rationale:
Washing hands frequently with soap and water is an effective preventive measure for influenza. Influenza viruses can survive on surfaces for a limited time, and touching contaminated surfaces and then touching the face can lead to infection. Regular handwashing helps reduce the risk of transmission.
A client is diagnosed with influenza and asks the nurse how the virus is transmitted. Which explanation by the nurse is accurate?
Explanation
Choice A rationale:
Influenza is not transmitted through the bite of infected mosquitoes. Influenza is a respiratory virus and spreads through respiratory droplets generated by infected individuals.
Choice B rationale:
Influenza is not primarily transmitted through direct contact with infected animals. Although some influenza strains can affect animals, the main mode of transmission to humans is from person to person through respiratory droplets.
Choice C rationale:
Influenza is not transmitted primarily through contaminated food and water. The virus is mainly spread through respiratory droplets produced when an infected person coughs, sneezes, or talks.
Choice D rationale:
This explanation is accurate. Influenza is transmitted through respiratory droplets generated by coughing or sneezing of an infected person. These droplets can be inhaled by individuals in close proximity, leading to infection. Proper hand hygiene and respiratory etiquette are essential to prevent the spread of influenza.
Explanation
Typical signs of influenza.
Choice A rationale:
The symptoms described by the client, such as fever, headache, and body aches, are typical signs of influenza. Influenza is a viral respiratory illness known for causing these common symptoms. The presence of fever, headache, and body aches is consistent with the clinical presentation of influenza.
Choice B rationale:
Choice B is incorrect because the symptoms mentioned are actually common and typical in influenza. Further evaluation may be necessary if the symptoms worsen or if there are complications, but they are not uncommon in influenza.
Choice C rationale:
Choice C is incorrect because the symptoms are not indicative of a bacterial infection. Influenza is a viral infection, and the symptoms described align with a viral illness rather than a bacterial one.
Choice D rationale:
Choice D is incorrect because the symptoms are not suggestive of allergies. Allergies typically present with different symptoms, such as sneezing, itching, and a runny or stuffy nose. The symptoms of fever, headache, and body aches are not characteristic of allergies.
Explanation
Choice B:
Pregnant women,
Choice C:
Older adults, and Choice D:
Individuals with diabetes.
Choice A rationale:
Choice A is incorrect because adolescents are generally not considered a high-risk group for severe influenza complications. While they can get influenza, they are not as vulnerable to severe outcomes as some other groups.
Choice B rationale:
Pregnant women are at an increased risk of severe complications from influenza due to changes in their immune system during pregnancy. Influenza can lead to serious complications for both the pregnant woman and her unborn baby, making it crucial to include them in the high-risk groups for which the nurse should provide education.
Choice C rationale:
Older adults, especially those aged 65 and older, are at a higher risk of severe influenza-related complications due to age-related changes in their immune system. Including them in the high-risk groups is essential to ensure they take preventive measures and seek timely medical attention if they develop symptoms.
Choice D rationale:
Individuals with diabetes have compromised immune systems, making them more susceptible to severe influenza complications. The nurse should include them in the discussion of high-risk groups to ensure they are aware of the importance of influenza prevention and management.
Choice E rationale:
Choice E is incorrect because individuals with a history of allergies are not considered a high-risk group for severe influenza complications. Allergies do not directly increase the risk of severe influenza outcomes.
Explanation
Rapid antigen test.
Choice A rationale:
Viral culture is a laboratory test used to grow and identify viruses, including influenza. While it is sensitive and specific, it is not suitable for rapid diagnosis as it may take several days to produce results.
Choice B rationale:
Polymerase chain reaction (PCR) is a highly sensitive and specific test that can detect the genetic material of the influenza virus. It is suitable for confirmation of the diagnosis, but it may take a few hours to produce results, so it is not as rapid as the correct answer.
Choice C rationale:
Serology involves testing for antibodies produced by the body in response to the influenza virus. While it can confirm past infection, it is not suitable for rapid diagnosis of acute influenza because it may take days to weeks for antibodies to develop.
Choice D rationale:
The rapid antigen test is a quick diagnostic test that detects specific proteins (antigens) on the surface of the influenza virus. It can provide results within 15-30 minutes, making it useful for rapid screening. However, it is less sensitive than PCR and may produce false-negative results in some cases. Despite this limitation, it is valuable in certain settings where immediate diagnosis is crucial for patient management and infection control.
Explanation
D.
Choice A rationale:
The nurse should administer antiviral drugs as prescribed because these medications can help reduce the severity and duration of influenza symptoms, especially if started early in the course of the illness. Common antiviral drugs used for influenza include oseltamivir and zanamivir.
Choice B rationale:
Providing cool compresses is an appropriate intervention to help reduce fever and discomfort associated with influenza. Cool compresses can provide relief from fever and headache symptoms.
Choice C rationale:
Limiting the number of visitors is important during the influenza outbreak to prevent further spread of the virus. Influenza is highly contagious, and restricting visitors can help reduce the risk of transmission to others.
Choice D rationale:
Encouraging bed rest is essential for patients with influenza as it allows the body to conserve energy, fight off the infection, and recover more effectively. Rest helps the body heal and boosts the immune response.
Choice E rationale:
Offering antibiotics for bacterial infection is not necessary for a patient with influenza. Influenza is caused by a virus, not bacteria, so antibiotics are ineffective against it. Antibiotics should only be prescribed if there is a secondary bacterial infection.
Explanation
Choice C rationale:
The nurse's appropriate statement is, "Antiviral drugs can reduce the duration and severity of symptoms." This statement is accurate because antiviral drugs are effective in treating influenza by inhibiting the replication of the virus, thus reducing the duration and severity of the illness. It is important for the patient to understand the benefits of adhering to the prescribed antiviral therapy to achieve the best possible outcome.
Choice A rationale:
The statement, "The antiviral drugs will help treat bacterial infections," is incorrect because antiviral drugs are specific to viral infections and have no effect on bacterial infections.
Choice B rationale:
The statement, "You should stop taking the antiviral medication once you feel better," is also incorrect. It is essential for the patient to complete the full course of antiviral medication as prescribed by the healthcare provider, even if they start feeling better, to ensure complete eradication of the virus.
Choice D rationale:
The statement, "You need to take the antiviral medication only if you have a fever," is incorrect as well. Antiviral medications should be taken as prescribed by the healthcare provider, regardless of fever presence, to effectively treat influenza.
Explanation
Choice D rationale:
The statement, "The influenza vaccine is not recommended for anyone aged 6 months and older," indicates the need for further education. Influenza vaccination is recommended for all individuals aged 6 months and older, especially those at higher risk for complications, such as older adults, young children, pregnant women, and individuals with chronic health conditions. Vaccination helps prevent influenza and its complications. The patient needs to be informed about the importance of getting vaccinated annually.
Choice A rationale:
The statement, "I should cover my mouth and nose when coughing or sneezing," is correct and indicates that the patient understands the importance of respiratory hygiene to prevent the spread of influenza to others.
Choice B rationale:
The statement, "I need to stay home until I am fever-free for at least 24 hours without antipyretics," is also correct. It indicates that the patient is aware of the need to stay home until they are no longer contagious to avoid spreading the virus to others.
Choice C rationale:
The statement, "Antiviral drugs can prevent complications and reduce mortality if started early," is accurate and shows that the patient has received appropriate education regarding the benefits of early antiviral therapy for influenza.
Explanation
Choice A rationale:
Initiating droplet precautions for all patients is not the most appropriate prevention strategy for influenza in a healthcare setting. While droplet precautions are necessary when dealing with patients suspected or confirmed to have certain respiratory infections, they are not the primary method for preventing influenza transmission.
Choice B rationale:
Administering antibiotics to patients with flu-like symptoms is not an effective prevention measure for influenza. Influenza is caused by a virus, and antibiotics are only effective against bacterial infections, not viral ones.
Choice C rationale:
Encouraging patients to avoid close contact with sick people is a good preventive measure for influenza. However, in a healthcare setting, it may be challenging to completely avoid close contact with sick patients. This measure can be useful in the community but may not be sufficient within the healthcare facility.
Choice D rationale:
Recommending the influenza vaccine for healthcare workers is a crucial prevention strategy. Vaccination is one of the most effective ways to protect healthcare workers and their patients from the influenza virus. By vaccinating healthcare workers, the risk of spreading the virus within the healthcare setting is significantly reduced.
Explanation
Choice A rationale:
Avoiding vaccination and relying on natural immunity is not the best approach to prevent influenza. Natural immunity may not provide adequate protection against the constantly changing influenza virus, and the risk of severe illness and complications is higher without vaccination.
Choice B rationale:
Washing hands frequently and using alcohol-based hand sanitizer are effective preventive measures for various infections, including the flu. However, they are not sufficient on their own to prevent influenza entirely. Vaccination remains the primary and most effective way to prevent the flu.
Choice C rationale:
Getting the influenza vaccine every year before the flu season starts is the most effective way to prevent influenza. The flu virus undergoes frequent changes, necessitating an annual vaccine update to match the circulating strains and provide optimal protection.
Choice D rationale:
Influenza vaccines do not contain live influenza viruses. The majority of influenza vaccines are inactivated or made from components of the virus, making it impossible for them to cause the flu in vaccinated individuals. Some vaccines, like the nasal spray, may contain weakened live viruses, but they are modified not to cause illness in healthy individuals.
Explanation
Choice A rationale:
The rapid antigen test for influenza generally has high specificity but low sensitivity. It means that the test is relatively good at correctly identifying people without influenza (true negatives) but may miss some true positive cases, leading to false-negative results.
Choice B rationale:
The rapid antigen test does not detect influenza viruses in blood samples; it is designed to detect the virus in respiratory secretions, such as nasal swabs. The results are available within minutes, not hours.
Choice C rationale:
The rapid antigen test provides quick results, usually within 15-30 minutes, and is not a prolonged waiting period like 3 to 10 days.
Choice D rationale:
The nurse should inform the client that the rapid antigen test is not suitable for confirming the diagnosis of influenza. While it can quickly identify some cases of influenza, it is not as reliable as other diagnostic methods like molecular tests (PCR) for confirming influenza. False-negative results are more likely with rapid antigen tests, and negative results may need to be confirmed with more sensitive tests if symptoms persist.
(Select all that apply): A nurse is providing care to multiple patients with suspected or confirmed influenza. Which isolation measures should the nurse implement? Select all that apply:
Explanation
Choice A rationale:
The nurse should not cohort patients with different strains of influenza because different strains may have varying levels of virulence and infectivity. Cohorting patients with different strains could increase the risk of cross-infection and make it challenging to implement appropriate isolation measures for each strain.
Choice B rationale:
Limiting the number of visitors and staff entering the room is crucial to prevent the spread of influenza to vulnerable patients and healthcare workers. Influenza spreads through respiratory droplets, and restricting access can help contain the virus.
Choice C rationale:
Instructing patients and visitors to dispose of tissues properly is essential as influenza is transmitted through respiratory secretions. Proper disposal of contaminated tissues can reduce the risk of indirect transmission through contact with contaminated surfaces.
Choice D rationale:
Administering antiviral drugs to all patients regardless of symptoms is not recommended. Antiviral treatment is generally reserved for patients at high risk for severe complications or those who present early in the course of the illness. Universal administration may lead to unnecessary drug use and potential side effects.
Choice E rationale:
Implementing standard precautions and droplet precautions is crucial when caring for patients with suspected or confirmed influenza. Standard precautions include hand hygiene, wearing appropriate personal protective equipment, and following proper infection control protocols. Droplet precautions specifically address the transmission of respiratory droplets, which is a significant mode of influenza spread.
Choice A rationale:
The nurse should not cohort patients with different strains of influenza because different strains may have varying levels of virulence and infectivity. Cohorting patients with different strains could increase the risk of cross-infection and make it challenging to implement appropriate isolation measures for each strain.
Choice B rationale:
Limiting the number of visitors and staff entering the room is crucial to prevent the spread of influenza to vulnerable patients and healthcare workers. Influenza spreads through respiratory droplets, and restricting access can help contain the virus.
Choice C rationale:
Instructing patients and visitors to dispose of tissues properly is essential as influenza is transmitted through respiratory secretions. Proper disposal of contaminated tissues can reduce the risk of indirect transmission through contact with contaminated surfaces.
Choice D rationale:
Administering antiviral drugs to all patients regardless of symptoms is not recommended. Antiviral treatment is generally reserved for patients at high risk for severe complications or those who present early in the course of the illness. Universal administration may lead to unnecessary drug use and potential side effects.
Choice E rationale:
Implementing standard precautions and droplet precautions is crucial when caring for patients with suspected or confirmed influenza. Standard precautions include hand hygiene, wearing appropriate personal protective equipment, and following proper infection control protocols. Droplet precautions specifically address the transmission of respiratory droplets, which is a significant mode of influenza spread.
HIV/AIDS
Explanation
Choice A rationale:
Sharing injection equipment can transmit HIV, but it is not the main route of transmission. This mode of transmission is more associated with other blood-borne infections like Hepatitis B and C.
Choice B rationale:
Mother-to-child transmission during pregnancy, childbirth, or breastfeeding can transmit HIV, but it is not the main route of transmission in the general population.
Choice C rationale:
Unprotected sexual intercourse is the main route for HIV transmission in the general population. Sexual contact with an infected person without using barrier methods like condoms can facilitate the spread of the virus.
Choice D rationale:
Occupational exposure to infected blood is a potential mode of transmission for healthcare workers, but it is not the main route of transmission for the general population.
Choice E rationale:
Blood transfusion from an infected donor was a significant mode of HIV transmission in the past, but extensive screening of blood donations has made this mode of transmission extremely rare.
Explanation
Choice A rationale:
Abstinence from drug use is an ideal approach, but it may not be practical for individuals struggling with addiction. Harm reduction strategies aim to reduce the negative consequences of drug use while acknowledging that complete abstinence may not be immediately achievable for everyone.
Choice B rationale:
Needle exchange programs are effective harm reduction strategies for individuals who inject drugs. These programs provide clean needles and syringes, reducing the risk of HIV transmission through contaminated needles.
Choice C rationale:
Condom use during sexual intercourse is important for preventing sexually transmitted infections, including HIV. However, this choice specifically asks about harm reduction strategies for individuals who inject drugs.
Choice D rationale:
Laws and policies to reduce stigma are essential for promoting understanding and compassion towards individuals living with HIV. However, this choice does not directly address harm reduction strategies for drug injection.
Choice E rationale:
Pre-exposure prophylaxis (PrEP) for sexual partners can be effective in preventing HIV transmission, but it is not directly related to harm reduction for individuals who inject drugs. PrEP is a preventive measure for those at risk of contracting HIV through sexual activity.
Explanation
Choice A rationale:
HIV is not a bacterial infection but a viral infection caused by the human immunodeficiency virus. It cannot be treated with antibiotics, as antibiotics are only effective against bacterial infections.
Choice B rationale:
This statement is correct. HIV attacks and destroys the CD4+ T cells, which are crucial for maintaining the immune system. As the virus replicates and damages these cells, the body becomes more susceptible to infections and other illnesses.
Choice C rationale:
This statement is incorrect. HIV can be transmitted through various means, including unprotected sexual intercourse, sharing needles, mother-to-child during childbirth or breastfeeding, and blood transfusions with infected blood.
Choice D rationale:
This statement is incorrect. There is no cure for HIV, and relying solely on herbal remedies without taking antiretroviral medications would be ineffective and dangerous. Antiretroviral therapy (ART) is the standard treatment for managing HIV and preventing its progression to AIDS.
Explanation
Choice A rationale:
HIV testing is recommended for everyone, regardless of risk factors. It is essential to identify HIV infections early, as early diagnosis and treatment can improve outcomes and prevent further transmission.
Choice B rationale:
This statement is incorrect and unethical. Informed consent and counseling are crucial before HIV testing to ensure individuals are aware of the implications of the test and the disease.
Choice C rationale:
This statement is accurate. Antibody tests are the most common and reliable tests used for the diagnosis of HIV infection. These tests detect the presence of antibodies produced by the body in response to the HIV virus.
Choice D rationale:
Nucleic acid tests (NAT) are not used to detect antibodies against HIV. Instead, NAT is used for early detection of the virus itself, not antibodies, and is typically employed in specific situations like testing donated blood or for early diagnosis during the window period before antibodies develop.
Explanation
Choice A rationale:
This statement is correct. HIV-1 is more prevalent in West Africa and has a slower progression to AIDS compared to HIV-2.
Choice B rationale:
This statement is incorrect. HIV-2 is actually less virulent than HIV-1, and it is more commonly found in West Africa and certain parts of Asia.
Choice C rationale:
HIV-1 is divided into four groups (M, N, O, and P), each having several subtypes. HIV-2, on the other hand, is divided into nine subtypes (A to I)
Choice D rationale:
This statement is incorrect. The most common HIV-1 subtype worldwide is group M, specifically subtype C, which is predominant in sub-Saharan Africa and parts of Asia. The most common subtype in the US is subtype
B.
Explanation
Choice A rationale:
This statement is inaccurate. HIV is not an acute infection that resolves without treatment. It is a chronic condition that persists in the body, and without treatment, it can progress to AIDS, which can be life-threatening.
Choice B rationale:
This statement is also inaccurate. While Antiretroviral Therapy (ART) is highly effective in controlling HIV and improving the quality of life for people living with the virus, it is not a curative treatment. HIV remains in the body, and stopping ART can lead to viral rebound.
Choice C rationale:
This statement is incorrect. HIV testing is essential, even in the absence of visible symptoms. Many individuals with HIV may not show any symptoms for years, but early detection through testing allows for timely intervention and better disease management.
Choice D rationale:
This is the correct statement. HIV is primarily transmitted through contact with infected body fluids, such as blood, semen, vaginal fluids, and breast milk. Common modes of transmission include unprotected sexual intercourse, sharing of contaminated needles, and from mother to child during childbirth or breastfeeding.
Explanation
Choice A rationale:
Consistent and correct use of condoms is an essential biomedical intervention for HIV prevention. When used consistently and properly, condoms act as a barrier to prevent the transmission of HIV during sexual intercourse.
Choice B rationale:
Abstinence from sexual activity is an important behavioral approach to prevent HIV transmission. However, the question specifically asks for biomedical interventions, which involve the use of medical or pharmaceutical methods.
Choice C rationale:
Sharing injection equipment with trusted partners is a risky behavior that can lead to HIV transmission. It is not a biomedical intervention but rather an unsafe practice.
Choice D rationale:
Taking Pre-Exposure Prophylaxis (PrEP) is an effective biomedical intervention for HIV prevention. PrEP involves taking antiretroviral medications before potential exposure to HIV to reduce the risk of infection in high-risk individuals.
Explanation
Choice A rationale:
A person's age can influence susceptibility to HIV infection. Younger individuals may engage in riskier behaviors or may have incomplete sex education, making them more vulnerable to HIV transmission.
Choice B rationale:
Circumcision status of the male partner can impact susceptibility. Circumcision has been associated with a reduced risk of HIV transmission during heterosexual intercourse.
Choice C rationale:
Having a high viral load in an HIV-positive individual increases the risk of transmitting the virus to others.
Choice D rationale:
Genetic factors can play a role in determining a person's susceptibility to HIV infection. Certain genetic variations may affect the immune response to the virus.
Choice E rationale:
Being female can influence susceptibility to HIV infection due to biological and social factors. Women may have a higher risk of infection during unprotected heterosexual intercourse. Additionally, gender disparities in access to healthcare and prevention resources can also contribute to higher vulnerability.
Explanation
Choice A rationale:
The acute primary infection is the initial phase of HIV infection and occurs shortly after exposure. During this stage, the viral load may be high, but the CD4 count is usually not significantly affected yet.
Choice B rationale:
The asymptomatic stage follows the acute primary infection and is characterized by no symptoms or mild symptoms. The viral load and CD4 count may be stable or slowly changing during this stage.
Choice C rationale:
The symptomatic stage is the next phase of HIV infection, also known as the early symptomatic or clinical latency stage. During this stage, the viral load is often associated with a high viral load and a low CD4 count. The immune system is weakened, and the individual may experience various HIV-related symptoms.
Choice D rationale:
AIDS is the final stage of HIV infection. At this stage, the immune system is severely compromised, and the individual is susceptible to various opportunistic infections and certain cancers. While the viral load remains high, the CD4 count is significantly low.
Explanation
Choice A rationale:
The asymptomatic stage is characterized by no symptoms or mild symptoms. Many individuals with HIV may not be aware of their infection during this stage as they may not experience any obvious signs of illness.
Choice B rationale:
This statement is incorrect. The asymptomatic stage may see relatively stable CD4 counts and viral loads, rather than a gradual decline in CD4 count and a gradual increase in viral load.
Choice C rationale:
During the asymptomatic stage, the viral load may remain at detectable levels, but the individual may not have any symptoms. Regular HIV testing is crucial to detect the infection during this stage.
Choice D rationale:
Acute retroviral syndrome (ARS) or seroconversion illness occurs during the acute primary infection, not the asymptomatic stage.
Choice E rationale:
Without treatment, the asymptomatic stage can last for up to 10-15 years. However, the duration can vary widely from person to person.
Explanation
Choice A rationale:
This statement is correct. Candidiasis of bronchi, trachea, lungs, or esophagus is one of the opportunistic infections associated with advanced HIV disease and AIDS.
Choice B rationale:
This statement is correct. Kaposi's sarcoma is another opportunistic infection commonly associated with AIDS.
Choice C rationale:
This statement is correct. Encephalopathy, HIV-related, is an opportunistic infection that can define AIDS.
Choice D rationale:
This statement is incorrect. Antiretroviral therapy is a lifelong treatment for HIV infection, and its discontinuation should not be based solely on the CD4 count falling below 200 cells/uL. The client needs further education on the importance of continuous treatment to manage HIV effectively and prevent opportunistic infections.
Explanation
Choice A rationale:
Nucleic acid tests (NAT) are highly sensitive tests that can detect HIV infection early, but the window period stated (3-12 weeks) is not accurate. NAT can detect HIV RNA as early as 9-11 days after exposure, but it may take up to 2-6 weeks for it to be reliably detected.
Choice B rationale:
This is the correct answer. Nucleic acid tests (NAT) can detect HIV infection as early as 2-6 weeks after exposure, making it the option with the shortest window period.
Choice C rationale:
This option is incorrect. NAT can detect HIV infection earlier than the time range stated (10-33 days)
Choice D rationale:
This option is incorrect. NAT can detect HIV infection much earlier than 6 months after exposure.
Explanation
Choice A rationale:
Antiretroviral therapy (ART) can help increase CD4 count, but the primary goal of ART is to suppress viral replication and reduce viral load to undetectable levels, thereby preserving immune function.
Choice B rationale:
This is the correct answer. The goal of antiretroviral therapy (ART) is to reduce viral load to undetectable levels, which helps in preventing disease progression and transmission of HIV.
Choice C rationale:
Preventing opportunistic infections and cancers is an important benefit of ART, but the primary goal is to suppress viral replication.
Choice D rationale:
Adherence to the prescribed regimen and schedule is crucial for the effectiveness of ART, but it is not the primary goal of ART itself.
Explanation
Choice A rationale:
The client's statement about Integrase strand transfer inhibitors (INSTIs) is accurate. INSTIs block the enzyme integrase, preventing the insertion of HIV DNA into the host cell genome.
Choice B rationale:
This is the correct answer. The client's statement about Non-nucleoside reverse transcriptase inhibitors (NNRTIs) is incorrect. NNRTIs work by directly binding to reverse transcriptase, blocking its activity, and preventing HIV replication.
Choice C rationale:
The client's statement about Protease inhibitors (PIs) is accurate. PIs block the enzyme protease, inhibiting the cleavage of HIV proteins and preventing the formation of mature viral particles.
Choice D rationale:
The client's statement about Nucleoside reverse transcriptase inhibitors (NRTIs) is accurate. NRTIs are incorporated into the growing viral DNA chain, leading to chain termination and preventing further viral replication.
Explanation
Choice A rationale:
The nurse should consider drug efficacy, safety, and tolerability when selecting the appropriate ART regimen for the client. Different ART drugs have varying efficacy in suppressing viral replication, potential side effects, and interactions with other medications. This consideration helps ensure the chosen regimen is effective and well-tolerated by the client.
Choice B rationale:
CD4 count and viral load are essential factors to consider when starting ART. The CD4 count reflects the client's immune status, and the viral load indicates the level of HIV replication. These parameters help gauge disease progression and monitor the response to therapy over time.
Choice D rationale:
The patient's preferences and lifestyle should be taken into account when selecting an ART regimen. Some medications may require strict adherence schedules or specific food restrictions, and considering the patient's preferences can enhance treatment adherence and overall outcomes.
Choice E rationale:
The number of opportunistic infections present is an important consideration when starting ART. Opportunistic infections are more likely to occur in individuals with low CD4 counts and can affect the choice of ART drugs and the need for prophylactic treatments.
Explanation
Choice A rationale:
ART aims to reduce viral load to undetectable levels. When the viral load is undetectable, the risk of disease progression and transmission to others is significantly reduced.
Choice B rationale:
The primary goal of ART is to prevent opportunistic infections and cancers. By suppressing viral replication and boosting the immune system (measured by CD4 count improvement), ART helps prevent these severe complications of HIV infection.
Choice D rationale:
Improvement in CD4 count is a significant goal of ART. CD4 count reflects the health of the immune system, and increasing it is essential for better immune function and reducing the risk of opportunistic infections.
Choice E rationale:
ART can reduce the risk of transmission to others. When viral load is undetectable, the risk of transmitting HIV to sexual partners or through shared needles is greatly reduced.
A nurse is assessing a patient with HIV/AIDS. Which of the following should the nurse prioritize during the nursing assessment?
Explanation
Choice A rationale:
Monitoring for signs and symptoms of opportunistic infections should be a priority during the nursing assessment of a patient with HIV/AIDS. Opportunistic infections are common in individuals with compromised immune systems due to low CD4 counts, and early detection allows prompt intervention and improved outcomes.
Assessing emotional and social well-being (Choice B) is important but may not be the highest priority in the initial assessment, as addressing immediate health risks takes precedence.
Providing counseling, feedback, and reinforcement for medication adherence (Choice C) is essential for long-term management but should not overshadow the immediate need to monitor for opportunistic infections.
Educating the patient about HIV/AIDS transmission modes (Choice D) is crucial, but it can be addressed during the patient's hospital stay or subsequent visits, while the assessment for opportunistic infections requires immediate attention to ensure timely treatment.
Explanation
Choice A rationale:
Assisting the client with medication administration and refills is crucial in managing HIV/AIDS. Adherence to antiretroviral therapy (ART) is vital for controlling the viral load and preventing the progression of the disease. By helping the client with medication administration and refills, the nurse ensures that the client follows the prescribed treatment plan consistently.
Choice B rationale:
Educating the client about safe sex practices and personal hygiene is essential in preventing the transmission of HIV and other sexually transmitted infections (STIs) Providing information about condom use, practicing abstinence or mutual monogamy, and maintaining good personal hygiene can significantly reduce the risk of spreading the virus.
Choice C rationale:
Administering prophylactic antibiotics or antifungals as prescribed is important in managing opportunistic infections that can arise in individuals with weakened immune systems due to HIV/AIDS. Prophylactic treatment helps prevent these infections or reduces their severity.
Choice D rationale:
Encouraging the client to express their feelings and concerns is essential for providing psychosocial support. Living with HIV/AIDS can be emotionally challenging, and allowing the client to share their emotions helps them cope with the disease, reduces stress, and enhances overall well-being.
Choice E rationale:
Performing male circumcision is not a nursing intervention for a client with HIV/AIDS. While male circumcision has shown to reduce the risk of HIV transmission in some studies, it is not a primary nursing intervention for managing HIV/AIDS.
Explanation
Choice C rationale:
"Using condoms consistently and correctly during sexual intercourse can reduce the risk of HIV transmission." This statement is accurate and supported by scientific evidence. Condoms act as a barrier method and are effective in preventing the exchange of bodily fluids, thus reducing the likelihood of HIV transmission during sexual activity.
Choice A rationale:
"You should avoid getting tested for HIV regularly." This statement is incorrect and potentially harmful. Regular HIV testing is essential for early detection and timely initiation of treatment if needed. Early diagnosis improves health outcomes and reduces the risk of transmitting the virus to others.
Choice B rationale:
"Pre-exposure prophylaxis (PrEP) is used after HIV exposure." This statement is incorrect. PrEP is taken before potential HIV exposure to prevent infection. It involves taking antiretroviral medications regularly to reduce the risk of acquiring the virus.
Choice D rationale:
"Supervised injection facilities aim to increase risky behaviors among drug users." This statement is incorrect. Supervised injection facilities provide a safe and controlled environment for drug users to consume drugs under medical supervision, reducing the risk of overdose and the transmission of infectious diseases like HIV and hepatitis
C.
Explanation
Choice D rationale:
"Pre-exposure prophylaxis (PrEP) is used after HIV exposure." This statement is correct. PrEP is a biomedical intervention used before potential exposure to HIV to prevent infection. It involves taking antiretroviral medications regularly to reduce the risk of acquiring the virus.
Choice A rationale:
"Male circumcision can increase the risk of HIV acquisition." This statement is incorrect. Male circumcision has been shown to reduce the risk of HIV transmission in heterosexual men in some studies. However, it does not increase the risk of HIV acquisition.
Choice B rationale:
"Post-exposure prophylaxis (PEP) is used before HIV exposure." This statement is incorrect. PEP is a short-term treatment initiated after potential exposure to HIV to prevent infection. It involves taking antiretroviral medications for 28 days following a possible exposure.
Choice C rationale:
"Antiretroviral therapy (ART) is used to increase viral replication." This statement is incorrect. ART is used to suppress viral replication in individuals with HIV/AIDS, reducing the viral load and improving immune function. It is the cornerstone of HIV treatment, not a measure to increase viral replication.
Explanation
Compare the patient's outcomes with the goals and expected outcomes.
Choice A rationale:
The evaluation process involves comparing the patient's achieved outcomes with the established goals and expected outcomes of care. By doing this, the nurse can determine the effectiveness of the care provided and identify areas where adjustments may be necessary to improve patient outcomes.
Choice B rationale:
Modifying the plan of care based on the patient's history and physical examination is a part of the assessment and planning phases, not the evaluation phase. Evaluation focuses on measuring the success of the implemented care plan.
Choice C rationale:
Collecting data about the patient's laboratory tests, psychosocial status, and educational needs is crucial during the assessment phase to gather information for developing an appropriate care plan. While this information is valuable throughout the patient's care, it is not specific to the evaluation process.
Choice D rationale:
Providing counseling, feedback, and reinforcement for adherence to medication is an essential nursing intervention during the implementation phase. Although it supports patient compliance with treatment, it is not the primary focus of the evaluation process.
A patient with HIV asks the nurse about strategies to minimize the negative consequences of drug use. Which intervention should the nurse recommend?
Explanation
Choice A:
Needle exchange programs and Choice C:
Infection prevention education.
Choice A rationale:
Needle exchange programs are essential in minimizing the negative consequences of drug use, especially for patients with HIV. These programs provide clean needles and syringes, reducing the risk of transmitting the virus through contaminated equipment.
Choice C rationale:
Infection prevention education is crucial for patients with HIV who engage in drug use. Educating them about safe practices and harm reduction strategies can help reduce the risk of spreading infections and improve overall health outcomes.
Choice B rationale:
Post-exposure prophylaxis (PEP) is not relevant to this situation. PEP is a preventive treatment given after potential exposure to HIV, not a strategy to minimize the consequences of ongoing drug use.
Choice D rationale:
Male circumcision has been shown to reduce the risk of HIV transmission in heterosexual men. However, it is not a strategy to minimize the negative consequences of drug use, and its relevance is not applicable to this question.
A nurse is caring for a patient with HIV who is on antiretroviral therapy (ART) Which outcome should the nurse expect from this treatment?
Explanation
Prevention of opportunistic infections.
Choice B rationale:
Antiretroviral therapy (ART) is a standard treatment for patients with HIV. The primary goal of ART is to suppress viral replication, leading to increased CD4 cell count and improved immune function. As a result, patients on ART experience a reduced risk of developing opportunistic infections.
Choice A rationale:
An increase in viral replication is not an expected outcome of antiretroviral therapy. The goal of ART is to suppress viral replication and reduce the viral load in the patient's body.
Choice C rationale:
While antiretroviral therapy can lead to behavioral changes that may reduce risky behaviors, it is not the primary outcome or purpose of this treatment. The main focus is on viral suppression and immune restoration.
Choice D rationale:
Antiretroviral therapy does not directly promote human rights protection. However, access to appropriate medical care, including ART, is considered a human right for individuals with HIV/AIDS.
Explanation
Choice A rationale:
Pre-exposure prophylaxis (PrEP) is a biomedical intervention used to reduce the risk of HIV transmission in individuals at high risk of acquiring the virus. PrEP involves taking antiretroviral medications regularly to prevent HIV infection if exposed to the virus.
Choice B rationale:
Human rights protection is not a biomedical intervention for reducing the risk of HIV transmission. While it is crucial to protect the human rights of individuals living with HIV, it does not directly address the risk of transmission.
Choice C rationale:
Needle exchange programs are effective biomedical interventions to reduce the risk of HIV transmission among people who inject drugs. These programs provide clean needles and syringes in exchange for used ones, reducing the sharing of contaminated equipment.
Choice D rationale:
Opioid substitution therapy, such as methadone or buprenorphine, is a biomedical intervention that helps reduce the risk of HIV transmission among people who use injectable drugs. By providing safe and controlled opioid medications, it can reduce the need for risky injection practices.
Choice E rationale:
Supervised injection facilities are biomedical interventions that provide a safe and hygienic environment for people who inject drugs. These facilities offer sterile equipment, medical supervision, and access to resources, significantly reducing the risk of HIV transmission.
Tetanus.
.
Tetanus
Explanation
Choice B rationale:
Clostridium tetani is responsible for tetanus. When a puncture wound is contaminated with spores of this bacterium, it can produce a potent neurotoxin that causes muscle contractions, rigidity, and potentially life-threatening complications.
Choice A rationale:
Clostridium difficile is not responsible for tetanus. It is a different bacterium that can cause gastrointestinal infections and antibiotic-associated diarrhea.
Choice C rationale:
Escherichia coli is not responsible for tetanus. While certain strains of
E. coli can cause food poisoning and other infections, it is not associated with tetanus.
Choice D rationale:
Streptococcus pneumoniae is not responsible for tetanus. It is a bacterium commonly associated with respiratory infections, such as pneumonia.
Explanation
Choice A rationale:
Administering antitoxin therapy is appropriate for managing tetanus because it helps neutralize the neurotoxin produced by Clostridium tetani and can prevent its further effects on the body.
Choice B rationale:
Initiating antibiotic treatment is not effective in managing tetanus. Antibiotics are not useful in neutralizing the neurotoxin and treating the symptoms of tetanus.
Choice C rationale:
Providing muscle relaxants is essential for managing tetanus, as they help alleviate muscle contractions and rigidity, reducing the severity of symptoms.
Choice D rationale:
Ensuring adequate hydration is crucial in managing tetanus because dehydration can worsen muscle spasms and lead to complications.
Choice E rationale:
Applying heat to affected areas is not appropriate for managing tetanus. Heat application can exacerbate muscle contractions and is not a recommended intervention for this condition.
Explanation
Choice A rationale:
The correct statement indicates the need for a tetanus booster every 10 years during adulthood. This aligns with current guidelines as the immunity from tetanus vaccination can wane over time, necessitating booster doses.
Choice B rationale:
The correct statement explains that tetanus can be prevented by proper wound care and keeping the wound clean. This is accurate because tetanus spores are commonly found in soil and can enter the body through contaminated wounds, making wound care crucial for prevention.
Choice C rationale:
The correct statement indicates a need for further teaching as it is incorrect. Tetanus is not transmitted through respiratory droplets. Tetanus is caused by the Clostridium tetani bacterium found in the environment, especially in soil, and it enters the body through wounds, not through respiratory secretions.
Choice D rationale:
The correct statement highlights that tetanus is more common in developing countries due to lower immunization rates. This is accurate since immunization plays a significant role in preventing tetanus, and lower vaccination rates in some regions contribute to higher disease incidence.
Explanation
Choice A rationale:
The statement "I feel my muscles getting stiffer and more painful" requires immediate nursing intervention. These symptoms suggest an exacerbation of tetanus infection, and the client might be experiencing muscle spasms and rigidity that can lead to respiratory compromise.
Choice B rationale:
The statement "I accidentally cut myself while gardening a few days ago" is relevant but doesn't require immediate intervention. It helps the nurse understand a potential source of the tetanus infection, but urgent nursing actions are not necessary based on this statement alone.
Choice C rationale:
The statement "I received a tetanus booster shot about five years ago" indicates that the client has had recent immunization, which is important information but doesn't demand immediate nursing intervention.
Choice D rationale:
The statement "I've been experiencing some difficulty swallowing" should be monitored, but it doesn't need immediate intervention unless it worsens and compromises the airway.
Explanation
Choice A rationale:
The statement "Tetanus can be transmitted from person to person through respiratory secretions" is incorrect. Tetanus is not a communicable disease, and it does not spread from person to person.
Choice B rationale:
The statement "The primary reservoir of
C. tetani is contaminated food and water" is incorrect. Tetanus is primarily found in the environment, especially in soil, as
C. tetani is a bacterium that forms spores in the environment.
Choice C rationale:
The correct statement explains that tetanus spores can persist in the environment and enter the body through a wound. This is accurate as
C. tetani spores can survive for years in soil and dust, and they enter the body through cuts, puncture wounds, or other openings in the skin.
Choice D rationale:
The statement "Vector transmission of tetanus occurs primarily through mosquito bites" is incorrect. Tetanus is not transmitted through mosquito bites. Mosquitoes are not carriers of
C. tetani, and the infection does not spread through their bites.
A nurse is caring for a patient who has a wound contaminated with soil and feces. The nurse understands that this patient is at risk of developing which condition?
Explanation
Choice A rationale:
Malaria is caused by the Plasmodium parasite transmitted through the bite of infected mosquitoes. It is not related to wound contamination with soil and feces.
Choice B rationale:
Tetanus, also known as lockjaw, is caused by the bacterium Clostridium tetani, which is commonly found in soil and feces. When the bacterium enters a wound, it can produce a neurotoxin that affects the nervous system, leading to muscle stiffness and spasms.
Choice C rationale:
Influenza, commonly known as the flu, is caused by influenza viruses and is primarily transmitted through respiratory droplets. It is not related to wound contamination.
Choice D rationale:
Pneumonia is an infection that inflames the air sacs in the lungs, and it is caused by various pathogens, including bacteria, viruses, and fungi. It is not directly linked to wound contamination with soil and feces.
Which of the following statements about tetanus is accurate?
Explanation
Choice A rationale:
Tetanus is not commonly transmitted from person to person. Instead, it is usually acquired through the introduction of the Clostridium tetani bacterium into a wound, where it can produce the neurotoxin tetanospasmin.
Choice B rationale:
Tetanus is not effectively treated with antibiotics alone. Antibiotics can help control the infection caused by Clostridium tetani, but the primary treatment involves providing tetanus antitoxin to neutralize the neurotoxin already present in the body.
Choice C rationale:
Booster doses of tetanus vaccine are not recommended every 5 years. The standard recommendation is to receive a tetanus booster every 10 years to maintain protection against the disease.
A client has a puncture wound caused by a rusty nail. The nurse understands that which of the following should be initiated to prevent tetanus?
Explanation
Choice A rationale:
Antiviral medications are used to treat viral infections, but tetanus is caused by a bacterium, not a virus. Antiviral medication would not be effective in preventing tetanus.
Choice B rationale:
To prevent tetanus in a person with a puncture wound caused by a rusty nail, providing tetanus antitoxin is essential. The antitoxin can neutralize any tetanus neurotoxin that may have already been produced, preventing its effects on the nervous system.
Choice C rationale:
Wound debridement is the removal of foreign material and dead tissue from a wound, which can help reduce the risk of infection. While important for wound care, it does not specifically prevent tetanus and is not the primary intervention for this case.
Choice D rationale:
Applying a cold compress to the wound can help reduce pain and swelling, but it does not prevent tetanus. The priority is to administer tetanus antitoxin to neutralize the neurotoxin if present.
Choice E rationale:
Anticoagulant therapy is used to prevent or treat blood clotting disorders and is not relevant to preventing tetanus in this scenario.
Explanation
E.
Choice A rationale:
Trismus, also known as lockjaw, is a hallmark sign of tetanus. It is characterized by the inability to open the mouth due to sustained contraction of the jaw muscles.
Choice B rationale:
Dyspnea, or difficulty breathing, is a possible symptom of tetanus. Tetanus can lead to muscle spasms, including those of the respiratory muscles, which can result in respiratory distress and difficulty breathing.
Choice C rationale:
Ptosis, or drooping eyelid, is not a characteristic sign of tetanus. It is not directly associated with the muscle spasms and rigidity seen in tetanus.
Choice D rationale:
Tachycardia, or rapid heart rate, is not typically associated with tetanus. Tetanus primarily affects the skeletal muscles and does not directly affect the heart rate.
Choice E rationale:
Risus sardonicus, a facial muscle spasm resulting in a sardonic grin-like expression, is a classic sign of tetanus and is caused by sustained contraction of facial muscles.
Explanation
E.
Choice A rationale:
Administering human tetanus immune globulin (TIG) is a priority intervention in the management of generalized tetanus. TIG provides passive immunity and helps neutralize circulating tetanus toxin.
Choice B rationale:
Providing oxygen therapy and suctioning as needed is essential in managing generalized tetanus. Respiratory muscle spasms can lead to breathing difficulties, and supportive measures like oxygen therapy and suctioning can help maintain adequate oxygenation.
Choice C rationale:
Using padded side rails and restraints to prevent injury is not appropriate in the management of tetanus. These measures may increase muscle spasms and worsen the client's condition.
Choice D rationale:
Educating the client about completing the vaccination schedule is essential for prevention. However, in the case of an already diagnosed generalized tetanus, it is not a priority intervention.
Choice E rationale:
Using non-pharmacological methods for pain management is an essential aspect of caring for clients with tetanus. Pain relief measures, such as warm compresses and positioning, can help alleviate muscle spasms and discomfort.
Explanation
Choice A rationale:
The statement "I have difficulty opening my mouth due to muscle spasms" is characteristic of localized tetanus. In localized tetanus, muscle spasms are limited to the area near the site of infection or injury, and in this case, it affects the muscles around the mouth, leading to trismus or lockjaw.
Choice B rationale:
Involuntary laughter during muscle spasms is not characteristic of localized tetanus. It is not a typical sign or symptom of the condition.
Choice C rationale:
Arching of the back and difficulty breathing are characteristic signs of generalized tetanus, not localized tetanus. Generalized tetanus involves widespread muscle spasms, including those of the respiratory muscles.
Choice D rationale:
Facial muscle paralysis and slurred speech are not characteristic of localized tetanus. These symptoms are more commonly seen in conditions affecting the cranial nerves or other neurological disorders.
Explanation
Choice A rationale:
The statement "I should complete the full course of antibiotics as prescribed" is correct. Completing the full course of antibiotics is essential to ensure that all the bacteria causing the infection are eradicated. Stopping antibiotics prematurely may lead to antibiotic resistance and treatment failure.
Choice B rationale:
The statement "The antibiotics will kill the bacteria causing the disease" is correct. Antibiotics are prescribed to kill the bacteria responsible for causing the infection, including tetanus. This is essential in controlling the spread and severity of the disease.
Choice C rationale:
The statement "Antibiotics will help neutralize the toxin in my blood" is incorrect. Antibiotics are effective against bacteria but do not neutralize the toxin produced by the tetanus bacteria. To manage the symptoms of tetanus, other supportive treatments like tetanus antitoxin and muscle relaxants are used to counteract the toxin's effects.
Choice D rationale:
The statement "Penicillin G has a broader spectrum of activity than metronidazole" is irrelevant to the client's tetanus treatment. While it is true that different antibiotics have different spectrums of activity, this information is not relevant to the client's current condition or treatment.
Explanation
Choice A rationale:
The nurse should be vigilant for renal impairment in clients with tetanus. However, muscle spasms triggered by stimuli do not directly indicate renal impairment. The client's renal function should be monitored due to the potential side effects of medications and prolonged immobilization.
Choice B rationale:
The statement "Cardiac arrhythmias" is correct. Muscle spasms triggered by stimuli in tetanus can cause severe and prolonged muscle contractions, which may lead to autonomic instability, including cardiac arrhythmias. Monitoring the client's cardiac function is essential to detect and manage any arrhythmias that may arise.
Choice C rationale:
The nurse should be vigilant for aspiration pneumonia in clients with tetanus. However, muscle spasms triggered by stimuli do not directly indicate the development of aspiration pneumonia. Aspiration pneumonia can occur due to impaired swallowing and a risk of aspiration during muscle spasms.
Choice D rationale:
The statement "Diaphoresis (sweating)" is not directly associated with muscle spasms triggered by stimuli in tetanus. Diaphoresis may occur in response to fever or autonomic dysfunction but is not a primary concern related to the muscle spasms.
(ATI/HESI from external source): A nurse is caring for a client diagnosed with tetanus. The client asks the nurse, "What is the most common type of tetanus?" How should the nurse respond?
Explanation
Choice A rationale:
The statement "Localized tetanus, affecting muscles near the site of infection" is incorrect. Localized tetanus involves muscle spasms near the site of infection, but it is not the most common type of tetanus.
Choice B rationale:
The statement "Generalized tetanus, affecting all skeletal muscles" is correct. Generalized tetanus is the most common type of tetanus and affects all skeletal muscles, leading to widespread muscle spasms and rigidity.
Choice C rationale:
The statement "Cephalic tetanus, affecting only the cranial nerves" is not the most common type of tetanus. Cephalic tetanus is a rare form that involves cranial nerve dysfunction.
Choice D rationale:
The statement "Neonatal tetanus, affecting infants born to non-immunized mothers" is not the most common type of tetanus. Neonatal tetanus occurs in newborns born to inadequately immunized mothers and is also relatively rare compared to generalized tetanus in adults.
(ATI/HESI from external source): A nurse is caring for a client with generalized tetanus. The client is experiencing spasms triggered by stimuli. Which nursing intervention is the priority?
Explanation
Choice A rationale:
Administering human tetanus immune globulin (TIG) is the priority intervention for a client with generalized tetanus experiencing spasms triggered by stimuli. TIG provides passive immunity by neutralizing the tetanus toxin and preventing its further action. It is essential to administer TIG promptly to halt the progression of the disease and minimize its complications.
Choice B rationale:
While providing oxygen therapy and suctioning as needed are important nursing interventions, they are not the priority in this situation. These interventions are supportive measures that can help maintain respiratory function but do not directly address the underlying cause of tetanus.
Choice C rationale:
Educating the client about completing the vaccination schedule is important for future prevention, but it is not the priority at this moment. The client is already infected with tetanus, and immediate treatment with TIG takes precedence.
Choice D rationale:
Using non-pharmacological methods for pain management may be helpful, but it is not the priority intervention for a client with generalized tetanus experiencing spasms triggered by stimuli. The priority is to administer TIG to counteract the effects of the tetanus toxin.
(ATI/HESI from external source): A client with tetanus is receiving benzodiazepines for muscle spasms. The nurse knows that benzodiazepines act by:
Explanation
Choice A rationale:
Benzodiazepines act by enhancing the effects of gamma-aminobutyric acid (GABA) in the central nervous system (CNS) GABA is an inhibitory neurotransmitter that reduces neural activity, leading to sedation and muscle relaxation. By enhancing GABA's effects, benzodiazepines help relieve muscle spasms in clients with tetanus.
Choice B rationale:
Blocking the release of acetylcholine at neuromuscular junctions is not the mechanism of action of benzodiazepines. This statement is incorrect.
Choice C rationale:
Inhibiting the action of excitatory neurotransmitters in the brain is not the primary mechanism of action of benzodiazepines. They primarily enhance the activity of inhibitory neurotransmitters like GABA.
Choice D rationale:
Stimulating the production of dopamine in the spinal cord is not a mechanism of action for benzodiazepines. This statement is inaccurate.
Chickenpox/Shingles.
.
Chickenpox/Shingles
Explanation
Choice A rationale:
Pregnant women should receive the Tdap vaccine during each pregnancy. This is a correct statement as vaccination during pregnancy helps provide protection to both the mother and the newborn against tetanus, diphtheria, and pertussis.
Choice B rationale:
The recommended vaccination schedule for adults includes a single dose of Tdap (tetanus, diphtheria, and acellular pertussis) vaccine, followed by a Td (tetanus and diphtheria) booster every 10 years. Three doses of DTP vaccine during adulthood are not part of the recommended schedule.
Choice C rationale:
Tetanus prophylaxis should be given to patients with all types of wounds, not just severe wounds. This statement is incorrect.
Choice D rationale:
The Tdap vaccine is not administered every 5 years during adulthood. As mentioned earlier, adults receive a single dose of Tdap and then a Td booster every 10 years.
Explanation
Choice A rationale:
The nurse should not advise the patient to apply iodine, hydrogen peroxide, or alcohol to the wound. These substances can be irritating to the wound and delay the healing process.
Choice B rationale:
Cleaning and debriding the wound as soon as possible is an essential action to prevent infection and promote healing. Removing debris and foreign material from the wound reduces the risk of contamination and infection.
Choice C rationale:
Using non-sterile instruments for wound care is not appropriate. The nurse should emphasize the importance of using clean and sterile instruments to prevent introducing additional bacteria into the wound.
Choice D rationale:
Administering the Td vaccine (Tetanus and Diphtheria) for prophylaxis is a crucial action to protect the patient from tetanus, especially in contaminated wounds where tetanus spores might be present.
Choice E rationale:
Proper disposal of animal feces is crucial to avoid exposure to tetanus spores. Tetanus spores can be found in soil contaminated with animal feces and can enter the body through open wounds, leading to a serious and potentially fatal infection.
Explanation
Choice A rationale:
Chickenpox and shingles are viral infections, and while they can cause systemic symptoms, they are not directly linked to heart disease.
Choice B rationale:
The complications of chickenpox go beyond bacterial skin infections. While bacterial superinfections are possible, the more severe complications are associated with the virus itself.
Choice C rationale:
Shingles is characterized by a localized rash along the distribution of a sensory nerve, not a generalized vesicular rash.
Choice D rationale:
Complications of both chickenpox and shingles include pneumonia, encephalitis (inflammation of the brain), and postherpetic neuralgia (persistent nerve pain following shingles) These complications can be serious and require medical attention.
Explanation
Choice A rationale:
The primary infection of VZV occurs through respiratory droplets, not when a person comes into contact with them. The virus is highly contagious and spreads through respiratory secretions.
Choice B rationale:
Reactivation of VZV in the nerve cells leads to the onset of shingles, not chickenpox. Chickenpox is the primary infection, and after recovery, the virus remains dormant in nerve cells and can reactivate as shingles later in life.
Choice C rationale:
The incubation period of VZV for chickenpox ranges from 10 to 21 days, which is accurate information.
Choice D rationale:
The risk of transmission during reactivation (shingles) is higher than during primary infection (chickenpox) Shingles can cause the development of vesicles containing the virus, which can be contagious if someone comes into direct contact with the fluid from the vesicles. Primary chickenpox, on the other hand, spreads through respiratory droplets and is more widespread during the initial infection.
Explanation
Choice A rationale:
Administering the Td vaccine only if the wound is severe is not the correct response. Tetanus prophylaxis is recommended based on wound type and vaccination history, not just the severity of the wound.
Choice B rationale:
This is the correct response. Tetanus prophylaxis involves giving Tetanus Immunoglobulin (TIG) for immediate protection against tetanus toxin, along with the Tetanus and Diphtheria (Td) vaccine to promote long-term immunity. The decision to administer TIG and Td vaccine depends on the patient's wound type and their vaccination history.
Choice C rationale:
Tetanus prophylaxis is necessary even if the client received the DTP vaccine in childhood. The immunity from childhood vaccines may wane over time, and tetanus prophylaxis is recommended after potential exposure to the tetanus-causing bacteria.
Choice D rationale:
Giving the Td vaccine every 5 years is not the correct approach. The recommended schedule for Td booster doses is every 10 years, not every 5 years.
Explanation
Choice A rationale:
Airborne precautions are used for infectious agents that spread through small respiratory droplets and remain suspended in the air for long periods. Shingles is not transmitted through the airborne route.
Choice B rationale:
Droplet precautions are used for infectious agents that spread through large respiratory droplets and have a limited range. Shingles is not transmitted through large respiratory droplets.
Choice C rationale:
This is the correct response. Contact precautions are implemented for patients with shingles (herpes zoster) because the virus spreads through direct contact with the rash or lesions.
Choice D rationale:
Standard precautions are used for all patients to prevent the transmission of infections from both recognized and unrecognized sources. However, for specific diseases like shingles, additional precautions like contact precautions are also required.
Explanation
Choice A rationale:
Varivax is not administered as a single dose during adulthood. The vaccine is given as two doses, usually separated by 4 to 8 weeks, to ensure adequate protection.
Choice B rationale:
Varivax can reduce the risk of developing shingles, especially in individuals who had chickenpox and received the vaccine. While it may not completely prevent shingles, it can lessen its severity.
Choice C rationale:
This is the correct response. Varivax is a live attenuated vaccine, which means it contains weakened forms of the varicella-zoster virus that causes chickenpox. It stimulates the immune system to produce a protective response without causing the disease.
Choice D rationale:
Varivax is not recommended only for healthcare workers. It is recommended for certain groups, including children, adolescents, and adults who have not had chickenpox or received the vaccine. Healthcare workers might be among the targeted groups due to their increased risk of exposure, but it is not limited to them.
Explanation
Choice A rationale:
Encouraging using sterile instruments for cutting umbilical cords is important in preventing tetanus as contaminated instruments can introduce the
C. tetani spores, leading to infection.
Choice B rationale:
Promoting safe delivery practices in clean facilities is crucial to prevent tetanus in newborns. Clean delivery facilities reduce the risk of exposure to
C. tetani spores, which can enter through unclean delivery practices.
Choice C rationale:
Advising against disposing of animal feces properly is not directly related to preventing tetanus. Tetanus is primarily caused by the introduction of
C. tetani spores into wounds, not through exposure to animal feces.
Choice D rationale:
Educating on avoiding contact with soil or feces that may contain
C. tetani spores is essential in preventing tetanus. The spores can be found in soil and feces, and direct contact with these sources increases the risk of infection.
Choice E rationale:
Suggesting regular booster doses of DTP vaccine during adulthood is an effective measure in preventing tetanus. The DTP vaccine provides immunity against tetanus, and regular boosters are recommended to maintain protection throughout life.
A nurse is assessing a client who presents with a prodrome of fever, headache, malaise, anorexia, and pharyngitis. The nurse observes a generalized pruritic rash that progresses from macules to papules to vesicles to pustules to crusts, starting on the face and trunk and spreading to the extremities. The number of lesions varies from a few to hundreds. Which of the following complications should the nurse be aware of?
Explanation
Choice B rationale:
The symptoms described in the scenario, such as fever, headache, malaise, anorexia, pharyngitis, and the progression of a generalized pruritic rash from macules to papules to vesicles to pustules to crusts, are indicative of varicella-zoster virus (VZV) infection, commonly known as chickenpox. Otitis media (choice B) can be a complication of chickenpox, especially in children.
Choice A rationale:
Chronic kidney disease (choice A) is not a common complication of chickenpox. It is more commonly associated with conditions like diabetes and hypertension.
Choice C rationale:
Rheumatoid arthritis (choice C) is an autoimmune condition and is not a known complication of chickenpox.
Choice D rationale:
Type 2 diabetes (choice D) is not a common complication of chickenpox. Diabetes can increase the risk of infection, but it is not directly related to chickenpox.
Explanation
Choice B rationale:
Bell's palsy is a known complication of shingles (herpes zoster) The varicella-zoster virus (VZV), which causes chickenpox, remains dormant in the body and can reactivate as shingles later in life. Shingles can affect the facial nerve, leading to Bell's palsy, characterized by facial muscle weakness or paralysis on one side of the face.
Choice D rationale:
Postherpetic neuralgia is another complication associated with shingles. It is a persistent, severe pain that continues after the rash has healed, caused by nerve damage during the shingles infection. Choices A, C, and E rationales: Congestive heart failure (choice A), chronic obstructive pulmonary disease (choice C), and acute pancreatitis (choice E) are not directly related to shingles. These conditions are not commonly known as complications of shingles or the varicella-zoster virus infection.
Explanation
Choice A rationale:
The nurse should recommend applying calamine lotion to soothe and dry the chickenpox lesions. Calamine lotion has a soothing effect on the skin and can help reduce the itching associated with chickenpox. It also helps to dry out the lesions, which may aid in the healing process. However, it is essential to advise the family not to apply calamine lotion on open sores or areas with broken skin to avoid potential irritation.
Choice B rationale:
Giving aspirin to a child with chickenpox is not recommended. Aspirin has been associated with an increased risk of Reye's syndrome in children with viral infections, including chickenpox. Reye's syndrome is a rare but potentially life-threatening condition that affects the brain and liver.
Choice C rationale:
Antiviral drugs, such as acyclovir, are often prescribed for severe cases of chickenpox or for individuals at high risk of complications. These drugs can help shorten the duration of the illness and reduce the severity of symptoms. They are not to be avoided to prevent side effects, as the benefits generally outweigh the potential risks.
Choice D rationale:
Allowing the child to play outside may not be the best approach to distract them from itching. It is crucial to prevent the child from scratching the rash to avoid secondary bacterial infections and scarring. Engaging the child in indoor activities and providing distractions that do not involve scratching would be a safer approach.
Explanation
Choice A rationale:
Topical corticosteroids can help reduce inflammation in various skin conditions, but they are not the best option for managing pain associated with shingles (herpes zoster) Corticosteroids primarily target inflammation and do not provide effective pain relief in neuropathic pain, which is characteristic of shingles.
Choice B rationale:
Antibiotics are not useful for managing the pain caused by shingles. Shingles is a viral infection, not a bacterial one, so antibiotics would not be effective in reducing pain or preventing secondary infection.
Choice C rationale:
Starting antiviral drugs, such as acyclovir, valacyclovir, or famciclovir, within 72 hours of rash onset is essential for managing shingles. These medications can help reduce the severity and duration of the illness and may also decrease the risk of developing complications like postherpetic neuralgia.
Choice D rationale:
Topical capsaicin is an appropriate option for neuropathic pain relief in shingles. Capsaicin, derived from chili peppers, works by desensitizing the nerve endings and reducing pain signals. However, it may cause a burning sensation initially, and the client should be advised on proper application and hand hygiene afterward.
Explanation
Choice A rationale:
Anemia is not a complication typically associated with shingles. Shingles is caused by the varicella-zoster virus, and it primarily affects the nerves and skin, leading to a painful rash.
Choice B rationale:
Migraine headaches are not directly related to shingles. Shingles affects sensory nerves and typically presents with localized pain and a rash along the affected nerve's pathway.
Choice C rationale:
The nurse should monitor for postherpetic neuralgia in this client. Postherpetic neuralgia is a common complication of shingles that involves persistent and severe pain in the area where the rash was present. It occurs due to nerve damage caused by the virus, and the pain can last for weeks to months after the rash has healed.
Choice D rationale:
Asthma is not a complication associated with shingles. Shingles is a viral infection that primarily affects the skin and nerves and does not involve the respiratory system.
Explanation
Choice A rationale:
Complete Blood Count (CBC) is not useful in confirming the diagnosis of chickenpox. CBC provides information about the number and types of blood cells but is not specific to chickenpox diagnosis.
Choice B rationale:
Stool culture is not relevant in confirming the diagnosis of chickenpox. Stool culture is used to identify gastrointestinal infections, and it is not associated with chickenpox.
Choice C rationale:
Tzanck smear and viral culture from vesicle fluid are useful in confirming the diagnosis of chickenpox. Tzanck smear involves taking a sample from the vesicle and staining it to identify multinucleated giant cells, which are characteristic of varicella-zoster virus (VZV) infection. Viral culture involves growing the VZV in a lab to confirm the presence of the virus.
Choice D rationale:
Urinalysis is not relevant in confirming the diagnosis of chickenpox. Urinalysis is used to assess kidney function and detect urinary tract infections, but it does not help in diagnosing chickenpox.
Explanation
Choice A rationale:
Taking aspirin is not recommended for individuals with chickenpox, especially children, as it has been associated with an increased risk of Reye syndrome, a severe and potentially fatal condition affecting the brain and liver.
Choice B rationale:
Applying topical antibiotics is not a suitable recommendation for relieving pruritus (itching) associated with chickenpox. Topical antibiotics are used to treat bacterial skin infections, not pruritus.
Choice C rationale:
Using antihistamines is the most appropriate recommendation for relieving pruritus in chickenpox. Antihistamines block the effects of histamine, a chemical released during an allergic reaction or infection, and can help reduce itching.
Choice D rationale:
Increasing physical activity is not advised for a client with chickenpox, as this could lead to the spread of the virus to others and may worsen the symptoms and pruritus.
Explanation
Choice A rationale:
Postherpetic neuralgia is a potential complication of shingles. It occurs when nerve pain persists even after the rash has healed and can be a long-term and debilitating condition.
Choice B rationale:
Cranial nerve palsies can be a complication of shingles when the herpes zoster virus affects the cranial nerves, leading to neurological symptoms and complications.
Choice C rationale:
Bacterial superinfection is not a common complication of shingles. Shingles is caused by a viral infection, and while bacterial superinfection can occur if there is a secondary bacterial infection of the skin lesions, it is not a primary concern.
Choice D rationale:
Reye syndrome is not associated with shingles or its treatment. Reye syndrome is a rare but serious condition that primarily affects children recovering from viral infections, particularly those who have taken aspirin.
Choice E rationale:
Eye involvement is a potential complication of shingles, particularly if the herpes zoster virus affects the ophthalmic nerve, leading to eye pain, redness, and sometimes vision problems. Immediate medical attention is required in such cases to prevent complications that could lead to vision loss.
A nurse is caring for a client with chickenpox. Which nursing intervention should the nurse prioritize to prevent transmission of the virus?
Explanation
Choice A rationale:
Monitoring vital signs, fluid intake, and output is important for assessing the client's overall health and hydration status, but it does not specifically address preventing the transmission of the virus.
Choice B rationale:
Providing comfort measures like cool compresses and loose clothing can help alleviate symptoms and discomfort, but it does not directly address preventing the transmission of the virus.
Choice C rationale:
Encouraging oral hygiene and a soft diet is essential for managing the client's symptoms and promoting healing, but it does not focus on preventing the spread of the virus to others.
Choice D rationale:
Isolating the patient until all lesions are crusted over is a crucial nursing intervention to prevent transmission of the chickenpox virus. Chickenpox is highly contagious, primarily spread through respiratory droplets and contact with the fluid from the skin lesions. By isolating the patient until all lesions have crusted over, the risk of spreading the virus to others is significantly reduced.
(Select all that apply): A nurse is caring for a client with shingles. Which interventions should the nurse include in the client's care? Select all that apply.
Explanation
Choice A rationale:
Monitoring vital signs, pain level, and neurological status is important to assess the client's overall condition and response to treatment.
Choice B rationale:
Isolating the patient until all lesions are crusted over is not necessary for shingles, as it is not as highly contagious as chickenpox.
Choice C rationale:
Educating the patient and family about the disease process is essential to help them understand the condition, its course, and the necessary measures for management and prevention of complications.
Choice D rationale:
Encouraging oral hygiene and a soft diet is important, especially if the patient has oral lesions, to promote comfort and prevent secondary infections.
Choice E rationale:
Administering medications as prescribed, such as antiviral medications, can help reduce the severity and duration of the shingles outbreak.
Explanation
Choice A rationale:
Stating that "chickenpox is not contagious once the fever is gone" is incorrect information. Chickenpox is still contagious until all the lesions are crusted over.
Choice B rationale:
The statement "You can spread the virus by scratching the lesions" is accurate. Scratching the chickenpox lesions can cause the fluid from the blisters to be released, and this fluid contains the varicella-zoster virus, which can then infect others.
Choice C rationale:
Stating that "chickenpox can only be transmitted through respiratory droplets" is incorrect. While respiratory droplets are a common mode of transmission, direct contact with the fluid from the lesions is also a significant mode of transmission.
Choice D rationale:
Saying that "the virus can survive on surfaces for up to 24 hours" is incorrect. The varicella-zoster virus is relatively fragile and cannot survive for extended periods on surfaces outside the body. It is primarily transmitted through direct contact or respiratory droplets.
Explanation
Choice A rationale:
(Incorrect) Shingles, caused by the varicella-zoster virus, can be transmitted through direct contact with the fluid from the vesicles (blisters) of a person who has active shingles. However, it is important for the nurse to provide correct information to the client.
Choice B rationale:
(Correct) Shingles can only occur in individuals who have previously had chickenpox. After a person recovers from chickenpox, the virus remains dormant in the nerve tissues. Later in life, the virus can reactivate, leading to shingles. It is crucial for the nurse to emphasize this point to prevent any misunderstandings.
Choice C rationale:
(Incorrect) While the shingles vaccine is effective in reducing the risk of developing shingles, it does not have a 100% efficacy rate. The vaccine can, however, reduce the severity and duration of the illness if shingles still occur after vaccination.
Choice D rationale:
(Incorrect) The herpes zoster vaccine (shingles vaccine) is not given to children under 10 years old. It is recommended for adults aged 50 years and older or for individuals with certain risk factors.
Explanation
Choice A rationale:
(Correct) Excluding infected individuals from school or work until all lesions are crusted over is an important measure in preventing the spread of chickenpox. This helps to reduce the risk of transmission to others.
Choice B rationale:
(Correct) Practicing good hand hygiene is essential to prevent the spread of the varicella-zoster virus, which causes chickenpox and shingles. Regular handwashing helps reduce the likelihood of virus transmission through contact with contaminated surfaces or infected individuals.
Choice C rationale:
(Incorrect) Sharing personal items such as towels with infected individuals can increase the risk of spreading the virus. It is crucial for the nurse to discourage such practices during the community class.
Choice D rationale:
(Incorrect) While reporting cases of chickenpox or shingles to local health authorities is important for surveillance purposes, it is not a preventive measure for individual protection.
Explanation
Choice A rationale:
(Incorrect) The herpes zoster vaccine (shingles vaccine) is not administered to patients with chickenpox. The vaccine is recommended for those aged 50 years and older to prevent shingles in individuals who have previously had chickenpox.
Choice B rationale:
(Incorrect) Encouraging contact with immunocompromised individuals is not appropriate when caring for a patient with chickenpox. Immunocompromised individuals are more susceptible to severe complications from the varicella-zoster virus, so close contact should be avoided.
Choice C rationale:
(Correct) Using cool compresses is an essential comfort measure for patients with chickenpox. Cool compresses can help soothe the itching and discomfort caused by the chickenpox rash.
Choice D rationale:
(Incorrect) Providing educational materials only to the patient is not sufficient. It is important for the nurse to educate the patient's family members or caregivers about chickenpox precautions and care to prevent further transmission of the virus.
Explanation
Choice A rationale:
The varicella vaccine is not effective in preventing chickenpox. This statement is incorrect. The varicella vaccine is actually highly effective in preventing chickenpox. It contains a weakened form of the varicella-zoster virus, which stimulates the body's immune system to develop protection against the virus, reducing the risk of getting chickenpox.
Choice B rationale:
Serious adverse events from the vaccine are common. This statement is incorrect. Serious adverse events from the varicella vaccine are rare. Like all vaccines, there may be some mild side effects such as soreness at the injection site, fever, or a mild rash, but severe reactions are extremely uncommon.
Choice C rationale:
The vaccine has a high efficacy rate in preventing shingles. This statement is correct. The varicella vaccine not only helps prevent chickenpox but also reduces the risk of developing shingles later in life. Shingles is caused by the reactivation of the varicella-zoster virus, and the vaccine helps boost immunity to the virus, leading to a decreased likelihood of shingles.
Choice D rationale:
The vaccine is not recommended for pregnant women. This statement is generally correct. Pregnant women should avoid receiving the varicella vaccine because it is a live attenuated vaccine, and there is a theoretical risk of transmission to the fetus. If a woman is not immune to varicella and is planning to become pregnant, it's best to receive the vaccine before pregnancy.
Explanation
Choice A rationale:
Young age. This statement is incorrect. While shingles is more common in older adults, it can still occur in individuals of any age. Young age is not a risk factor for developing shingles.
Choice B rationale:
Stress. This statement is correct. Stress weakens the immune system, making individuals more susceptible to shingles. Emotional or physical stress can trigger shingles in people who have already had chickenpox.
Choice C rationale:
Immunocompromised status. This statement is correct. Individuals with weakened immune systems, such as those with HIV, cancer, or taking immunosuppressive medications, have a higher risk of developing shingles because their bodies may have difficulty controlling the reactivation of the varicella-zoster virus.
Choice D rationale:
Trauma. This statement is correct. Physical trauma or injury to the skin can increase the risk of shingles in the affected area. The trauma can disrupt the nerve pathways and trigger the reactivation of the varicella-zoster virus.
Choice E rationale:
Allergic to gelatin or neomycin. This statement is correct. The varicella vaccine contains trace amounts of gelatin and neomycin. Individuals with severe allergies to these components should not receive the vaccine to avoid potential allergic reactions.
Tuberculosis.
Tuberculosis
Explanation
Choice A rationale:
Monitor vital signs, fluid intake and output, weight, and skin integrity. This statement is correct. When caring for a patient with chickenpox, monitoring vital signs can help detect any signs of complications like fever. Fluid intake and output, weight, and skin integrity are important to assess the patient's hydration status and the progression of the rash.
Choice B rationale:
Administer medications as prescribed and monitor for adverse effects. This statement is correct. The nurse should give antiviral medications if prescribed to help shorten the duration of the illness and reduce its severity. Monitoring for any adverse effects from the medications is essential for patient safety.
Choice C rationale:
Encourage contact with pregnant women and immunocompromised individuals to build immunity. This statement is incorrect. Encouraging contact with pregnant women and immunocompromised individuals is not appropriate because chickenpox is highly contagious and can pose serious risks to these vulnerable populations. The nurse should advise the patient to avoid contact with them until they are no longer infectious.
Choice D rationale:
Advise the patient to avoid contact with those who have had chickenpox or been vaccinated. This statement is partially correct. The patient should avoid contact with individuals who have not had chickenpox or have not been vaccinated against it to prevent the spread of the disease. However, vaccinated individuals are less likely to transmit the virus than those with active chickenpox.
Choice E rationale:
Isolate the patient until all lesions are crusted over to prevent transmission to others. This statement is correct. Isolating the patient until all the lesions are crusted over is an important infection control measure to prevent the spread of the varicella-zoster virus to others. Once the lesions are crusted, the patient is no longer contagious.
Explanation
Choice A rationale:
The nurse should monitor vital signs, pain level, neurological status, and eye function for a client with shingles to assess for any complications or worsening of the condition. Vital signs may indicate signs of infection, pain level may help assess the effectiveness of pain management, neurological status can indicate any neurological complications, and eye function is important as shingles affecting the ophthalmic nerve can lead to eye complications.
Choice B rationale:
Administering medications as prescribed is crucial to manage the symptoms and complications of shingles. Antiviral medications can help reduce the severity and duration of the outbreak, while pain medications may be necessary to alleviate discomfort. The nurse should also monitor for adverse effects to ensure the client's safety during treatment.
Choice D rationale:
Isolating the patient until all lesions are crusted over is necessary to prevent the spread of the varicella-zoster virus, which causes shingles. Direct contact with vesicles can lead to transmission of the virus to susceptible individuals, particularly those who have not had chickenpox or received the varicella vaccine.
Choice E rationale:
Providing comfort measures is essential in managing the symptoms of shingles. Cool compresses can help relieve pain and inflammation, loose clothing can prevent irritation of the affected area, distraction techniques can divert the client's attention from discomfort, and relaxation methods can help reduce stress and promote healing.
Choice C rationale:
Encouraging the client to scratch the affected area is not appropriate care for shingles. Scratching can lead to skin damage, increase the risk of infection, and potentially worsen the condition. It is essential to advise against scratching and promote gentle care of the affected area instead.
Explanation
Choice A rationale:
The nurse should advise the patient with chickenpox to avoid contact with pregnant women, immunocompromised individuals, newborns, and people who have not had chickenpox or been vaccinated. Chickenpox is highly contagious and can be severe or even life-threatening for vulnerable populations. This precaution helps protect those who are at a higher risk of complications from the infection.
Choice B rationale:
Sharing personal items such as towels and utensils should be avoided during chickenpox. Chickenpox spreads through respiratory droplets and direct contact with fluid from the blisters. Sharing personal items can increase the risk of transmission to others.
Choice C rationale:
It is not appropriate for the nurse to recommend scratching the chickenpox lesions. Scratching can lead to secondary bacterial infections and scarring. The patient should be encouraged to use methods like calamine lotion or antihistamines to relieve itching.
Choice D rationale:
The patient should not return to work or school until all lesions are crusted over and they are no longer contagious. Typically, this occurs about 6-7 days after the rash first appears. Returning too early can increase the risk of spreading the virus to others.
Explanation
Choice A rationale:
This statement indicates the client understands the nurse's teaching about shingles. The client should avoid contact with pregnant women, immunocompromised individuals, newborns, and those who have not had chickenpox or been vaccinated against it. Shingles is caused by the reactivation of the varicella-zoster virus, the same virus that causes chickenpox. Direct contact with shingles lesions can transmit the virus to susceptible individuals, leading to chickenpox in those who have not had it before.
Choice B rationale:
Direct contact with family members, especially if they are part of the vulnerable populations mentioned, should be avoided until the shingles lesions are crusted over. This is to prevent transmission of the virus to susceptible individuals.
Choice C rationale:
Respiratory hygiene is still important for individuals with shingles, even though the virus is primarily spread through contact with the lesions. Respiratory droplets can potentially transmit the virus to others, so it's essential to follow good hygiene practices.
Choice D rationale:
Sharing personal items should be avoided during shingles, as it can increase the risk of transmission to others who have not had chickenpox or been vaccinated.
Explanation
Choice C rationale:
The most effective way to prevent both chickenpox and shingles is through vaccination. Chickenpox can be prevented by receiving the varicella vaccine (Varivax), and shingles can be prevented or its severity reduced by getting vaccinated with the herpes zoster vaccine (Shingrix) These vaccines stimulate the immune system to provide protection against the respective viruses.
Choice A rationale:
While handwashing with soap and water is essential for general hygiene and can help reduce the spread of infectious diseases, it is not the most effective method for preventing chickenpox and shingles.
Choice B rationale:
Avoiding contact with contaminated surfaces can help reduce the transmission of various infections, but it may not be sufficient to prevent chickenpox and shingles, which are primarily transmitted through respiratory droplets and direct contact with lesions.
Choice D rationale:
Isolating infected individuals until all lesions are crusted over is a measure to prevent the spread of chickenpox, but it is not as effective as vaccination in preventing the disease and its complications. Now, searching for three additional ATI/HESI MCQs related to the topic of Tuberculosis (TB)
Explanation
Choice A rationale:
Abdominal pain is not commonly associated with tuberculosis (TB) TB primarily affects the lungs, and symptoms such as cough, fever, weight loss, and night sweats are more typical of TB.
Choice B rationale:
Headache is not a common symptom of TB. While TB can cause systemic symptoms like fever and fatigue, it does not typically cause headaches unless there are complications involving the central nervous system, which is relatively rare.
Choice C rationale:
Hematuria, which is the presence of blood in the urine, is not a symptom commonly associated with TB. TB primarily affects the respiratory system and is not known to cause urinary symptoms.
Choice D rationale:
Cough is a hallmark symptom of tuberculosis. It is usually a productive cough that lasts for several weeks or longer, with the possibility of producing sputum that may be bloody or purulent. Cough is a key indicator for healthcare providers to suspect TB and order appropriate testing.
Explanation
Choice A rationale:
Using multiple drugs to treat TB is not primarily done to reduce the cost of treatment. While cost considerations are essential in healthcare, the main reason for employing multiple drugs is to prevent drug resistance and improve treatment outcomes.
Choice B rationale:
The rationale for using multiple drugs to treat TB is to minimize the risk of drug resistance. TB is caused by Mycobacterium tuberculosis, and the bacteria can develop resistance to single-drug treatments quite rapidly. Using a combination of drugs with different mechanisms of action makes it harder for the bacteria to become resistant to all drugs simultaneously, ensuring a more effective treatment.
Choice C rationale:
While using multiple drugs may help achieve a quicker cure, the primary reason for combining drugs in TB treatment is to prevent drug resistance. Faster cure is a secondary benefit, but the prevention of drug-resistant strains is of paramount importance in TB management.
Choice D rationale:
Avoiding potential drug interactions is an essential consideration in any medical treatment, but it is not the primary reason for using multiple drugs in TB treatment. The main focus is on preventing drug resistance and increasing treatment success.
Explanation
Choice A rationale:
A skin test result with an induration of 10 mm is considered positive in certain populations, indicating an active TB infection. These populations include people with known close contact with TB-infected individuals, HIV-positive individuals, recent immigrants from high-prevalence countries, and those with chest X-ray findings consistent with previous TB. The positive result means that the person has been exposed to the TB bacteria and has developed a delayed hypersensitivity reaction to the purified protein derivative (PPD) injected during the skin test.
Choice B rationale:
A negative reaction, indicating no TB infection, would typically be a skin induration of less than 5 mm. In this case, with an induration of 10 mm, a negative reaction can be ruled out.
Choice C rationale:
An induration of 10 mm is not considered an inconclusive result. Inconclusive results are usually associated with very small indurations or circumstances where there is uncertainty about the interpretation of the test.
Choice D rationale:
A borderline reaction is not typically associated with TB testing. Borderline reactions are less specific and are not commonly used to interpret the results of TB skin tests.
Explanation
Choice A rationale:
The Interferon-gamma release assay (IGRA) is another test used to detect TB infection. It measures the release of interferon-gamma by T-cells in response to TB antigens. However, in this question, the specific test described involves injecting tuberculin into the forearm, which is the characteristic of the TST, not the IGRA.
Choice B rationale:
Chest x-ray is not a test used to detect TB infection directly. It is useful for identifying active pulmonary TB, but it does not detect latent TB infection, which is what the tuberculin skin test is designed for.
Choice C rationale:
Sputum smear microscopy is a test used to diagnose active TB by examining sputum samples for acid-fast bacilli. It is not used for detecting latent TB infection, as the tuberculin skin test does.
Choice D rationale:
The tuberculin skin test (TST), also known as the Mantoux test, involves injecting a small amount of tuberculin into the forearm and then measuring the induration (localized swelling and redness) at the injection site after 48 to 72 hours. A positive TST result indicates exposure to TB but does not distinguish between latent TB infection and active TB disease.
Explanation
Choice A rationale:
Covering the mouth and nose when coughing or sneezing is an essential measure to prevent the transmission of TB. TB is spread through airborne droplets, and covering the mouth and nose helps contain these droplets, reducing the risk of transmission to others.
Choice B rationale:
Using an N95 respirator mask is necessary when caring for patients with suspected or confirmed TB. N95 masks provide a high level of filtration and help protect healthcare workers and others from inhaling TB bacteria.
Choice C rationale:
Placing the patient in a negative pressure room is a measure used for patients with suspected or confirmed active TB disease. Negative pressure rooms help prevent the spread of infectious particles to the surrounding environment.
Choice D rationale:
Encouraging physical activity is not directly related to preventing TB transmission. While physical activity is beneficial for overall health, it does not play a significant role in preventing the transmission of TB.
Choice E rationale:
Washing hands frequently is an essential measure to prevent the transmission of TB and other infections. Proper hand hygiene reduces the risk of spreading bacteria from contaminated surfaces to the mouth, nose, or eyes.
Explanation
Choice A rationale:
"I should take my medications regularly and complete the full course of therapy" is a correct statement. TB treatment involves multiple drugs taken for an extended period, typically 6 to 9 months, to ensure complete eradication of the bacteria and prevent drug resistance.
Choice B rationale:
"I will report any adverse effects of the medications, such as skin rash or eye inflammation" is a correct statement. TB medications can have side effects, and it's crucial for the patient to report any adverse reactions to their healthcare provider for appropriate management.
Choice C rationale:
"I can stop taking the medications once I start feeling better" is an incorrect statement. TB treatment requires completing the full course of therapy, even if the patient's symptoms improve. Stopping treatment prematurely can lead to treatment failure and the development of drug-resistant TB.
Choice D rationale:
"I understand that the treatment may require surgery if there is extensive lung damage" is a correct statement. In some cases of TB, particularly if there is significant lung damage or complications, surgical intervention may be necessary.
Explanation
Choice A rationale:
"Encouraging rest and avoiding physical activity." This intervention is not the essential one for monitoring the patient's response to TB treatment and identifying complications. While rest is important for recovery, it is not the primary method of monitoring treatment response.
Choice B rationale:
"Administering corticosteroids to prevent complications." Administering corticosteroids is not a standard intervention for all patients with TB undergoing treatment. Corticosteroids may be prescribed in specific cases, such as TB meningitis or pericarditis, to reduce inflammation, but it is not the essential nursing intervention for all TB patients.
Choice C rationale:
"Monitoring vital signs, sputum samples, and laboratory tests." This statement is correct. The essential nursing intervention for monitoring a patient's response to TB treatment and identifying complications is to regularly monitor vital signs, collect sputum samples to check for the presence of acid-fast bacilli (AFB), and conduct laboratory tests, such as complete blood count and liver function tests. These assessments help determine treatment effectiveness and detect any adverse reactions or complications.
Choice D rationale:
"Placing the patient in a negative pressure room." Placing the patient in a negative pressure room is not a nursing intervention for monitoring treatment response or identifying complications. Negative pressure rooms are used to prevent the spread of airborne infectious agents, but they are not directly related to treatment monitoring.
Explanation
Choice A rationale:
"Interferon-gamma release assay (IGRA)" This statement is correct. The Interferon-gamma release assay (IGRA) is more specific than the tuberculin skin test (TST) in detecting TB infection. It measures the release of interferon-gamma in response to TB antigens and does not cross-react with other mycobacteria or the BCG vaccine.
Choice B rationale:
"Sputum smear microscopy." Sputum smear microscopy is a diagnostic test used to identify acid-fast bacilli (AFB) in sputum samples. While it is essential for diagnosing active pulmonary TB, it is not more specific than the IGRA for detecting TB infection.
Choice C rationale:
"Chest x-ray." Chest X-ray is a valuable diagnostic tool to identify pulmonary abnormalities associated with TB infection, such as infiltrates and cavities. However, it is not more specific than the IGRA in detecting TB infection.
Choice D rationale:
"Sputum culture." Sputum culture is a gold standard diagnostic test for confirming active TB disease and identifying the specific strain of Mycobacterium tuberculosis. While it is highly sensitive and specific for diagnosing active TB, it is not more specific than the IGRA for detecting TB infection.
Explanation
Choice A rationale:
Providing emotional support and counseling is an important aspect of nursing care for TB patients. However, the primary goal of nursing interventions is to address the transmission of the disease and prevent its spread to others. TB is a highly contagious airborne disease, and healthcare professionals play a crucial role in implementing measures to reduce transmission.
Choice B rationale:
Monitoring the patient's weight and vital signs is essential for assessing the patient's response to treatment and overall health status. While these interventions are important, they are not the primary goal for TB patients. The main focus remains on preventing transmission and ensuring effective treatment.
Choice C rationale:
Preventing transmission of TB is the primary goal of nursing interventions. This involves implementing infection control measures, such as respiratory isolation, proper use of personal protective equipment, and education on cough etiquette for patients. By preventing the spread of TB, healthcare professionals contribute to public health efforts to control the disease.
Choice D rationale:
Administering antibiotic therapy is a critical aspect of TB treatment. However, it is not the primary goal of nursing interventions. Nursing interventions primarily focus on the prevention of transmission and supporting patients through their treatment journey.
Explanation
Choice A rationale:
Surgery for extensive lung damage may be considered in very rare cases of complications from TB, but it is not an adjunctive measure commonly required for TB treatment. The primary treatment for TB involves antibiotic therapy and adjunctive measures to manage complications.
Choice B rationale:
Corticosteroids may be required as adjunctive therapy for pericarditis, a complication of TB that affects the lining around the heart. Corticosteroids help reduce inflammation and improve the patient's condition.
Choice C rationale:
Nutritional support is often necessary for patients with TB, as the disease can lead to malnutrition and weight loss. Adequate nutrition is crucial for supporting the immune system and facilitating recovery.
Choice D rationale:
Fluid therapy may be required for patients with TB who experience dehydration due to fever, night sweats, and reduced oral intake. Proper hydration helps maintain organ function and aids in the elimination of waste products.
Choice E rationale:
Pain management is essential for patients with TB, especially for those experiencing chest pain, which can be a symptom of the disease or a complication. Adequate pain control improves the patient's comfort and compliance with treatment.
Explanation
Choice A rationale:
Chemoprophylaxis involves using medications to prevent TB infection or its progression in individuals at high risk of exposure. While it is an important strategy, it is not specifically related to administering the BCG vaccine.
Choice B rationale:
Screening for TB involves identifying individuals who are at risk of infection or have active disease through various tests such as tuberculin skin tests and chest X-rays. Although screening is a crucial aspect of TB control, it is not the strategy involving BCG vaccine administration.
Choice C rationale:
Vaccination with the BCG vaccine is an individual-level strategy aimed at providing protection against TB, particularly in infants or children at high risk of TB exposure or infection. The BCG vaccine does not provide complete protection against TB but has been shown to reduce the risk of severe forms of the disease, such as TB meningitis and miliary TB, in children.
Choice D rationale:
Surveillance involves monitoring the incidence and prevalence of TB at the population level. It does not directly involve administering the BCG vaccine to individuals at risk.
Explanation
Choice A rationale:
The most appropriate intervention for a client diagnosed with latent TB infection (LTBI) is observation for disease progression. Latent TB infection means that the individual has been infected with the tuberculosis bacteria but does not currently have active TB disease. In cases of LTBI, the bacteria are in a dormant state, and the person does not show any symptoms. The standard approach for LTBI management is to monitor the individual closely for any signs of disease progression. This may involve regular clinical assessments and follow-ups to detect the development of active TB. Initiating treatment (such as INH administration) is not recommended for all individuals with LTBI, as not everyone with latent infection will progress to active disease. The decision to treat depends on the individual's risk factors, clinical presentation, and other considerations. Selecting choice B (Sputum smear microscopy) is not appropriate for LTBI since this test is used to diagnose active TB disease, not latent infection. Choice C (Tuberculin skin test, TST) is used to identify individuals with LTBI, not as an intervention for those already diagnosed with LTBI. Choice D (INH administration) may be a treatment option for certain individuals with LTBI, but it is not the most appropriate intervention for all LTBI cases. Choice E (Contact tracing) is a strategy to identify and screen individuals who may have been exposed to active TB cases, not a direct intervention for LTBI management.
Explanation
Choice A rationale:
Choice C indicates the need for further teaching because it contains inaccurate information. The BCG vaccine, which is used to prevent severe forms of tuberculosis in high-risk populations, can cause false-positive reactions to the Tuberculin Skin Test (TST) The TST is a common test used to detect exposure to TB, but it cannot differentiate between a previous BCG vaccination and an actual TB infection. The presence of a BCG scar or previous vaccination can lead to a positive TST without an active TB infection. Choices A and B are correct statements. The BCG vaccine does provide some protection against severe forms of TB and pulmonary TB. Choice D is also accurate; the BCG vaccine is administered intramuscularly.
A client with latent TB infection (LTBI) is prescribed chemoprophylaxis. Which statement by the client indicates understanding of the treatment regimen?
Explanation
Choice B rationale:
Choice B reflects an understanding of the treatment regimen for latent TB infection (LTBI) Chemoprophylaxis is the treatment of choice for LTBI to prevent the development of active TB disease. The most common medication used for chemoprophylaxis is isoniazid (INH) While taking the medication, it is essential for the client to monitor for any adverse effects that may occur, such as hepatotoxicity. Regular follow-ups and liver function tests may be necessary during treatment. Additionally, monitoring for drug resistance is crucial to ensure that the medication remains effective in preventing active TB. Choices A and D are incorrect statements. Chemoprophylaxis requires taking the medication for an extended period, usually six to nine months, not just a few days. Choice C is also incorrect; chemoprophylaxis is often recommended for close contacts of active TB cases to prevent the progression to active disease. Choice C seems to confuse chemoprophylaxis (preventing progression from LTBI to active TB) with post-exposure prophylaxis (given to prevent initial infection after exposure to active TB)
Explanation
Choice A rationale:
Directly observed therapy (DOT) is a treatment strategy used for clients with active tuberculosis (TB) disease. The purpose of DOT is to ensure that the client takes their TB medications as prescribed, under direct observation by a healthcare provider or trained healthcare worker. By directly observing the medication administration, DOT helps to ensure medication adherence, which is crucial in preventing the development of drug-resistant TB strains. It also reduces the risk of treatment failure, relapse of the disease, and transmission of TB to others. By closely monitoring the client's adherence to the treatment regimen, healthcare providers can intervene promptly if any issues arise during the course of treatment.
Choice B rationale:
Facilitating early diagnosis and treatment is an essential aspect of TB control; however, this is not the primary purpose of directly observed therapy (DOT) Early diagnosis helps to identify and initiate appropriate treatment promptly, but DOT is specifically implemented to monitor and enhance adherence during the course of treatment, particularly for those at risk of non-compliance.
Choice C rationale:
Evaluating the impact and effectiveness of TB control programs is an important public health measure, but it is not the direct purpose of DOT. DOT mainly focuses on individual client treatment adherence rather than assessing overall program effectiveness.
Choice D rationale:
Identifying and testing persons who have been in close contact with active TB cases is part of contact tracing and TB screening efforts, which are separate from the purpose of directly observed therapy (DOT) DOT is centered on the supervision of treatment for clients already diagnosed with active TB disease.
Explanation
Choice A rationale:
Young adults between 20 to 30 years of age are at a higher risk of developing tuberculosis (TB) compared to other age groups. This age range often includes individuals who may be exposed to TB in various settings, such as college or university students, individuals in the workforce, and those who may engage in behaviors that increase the risk of TB transmission, such as socializing in crowded places.
Choice B rationale:
Children under the age of 5 are also considered a high-risk group for TB, especially in regions with a high prevalence of the disease. However, in many settings, young adults between 20 to 30 years of age have shown higher rates of TB infection and disease compared to young children.
Choice C rationale:
Elderly individuals over the age of 65 are generally considered at higher risk for developing severe complications from TB, but their risk of primary TB infection is lower compared to younger age groups, including young adults between 20 to 30 years of age.
Choice D rationale:
Pregnant women, like the elderly, are at higher risk of severe complications if they develop TB during pregnancy. However, the incidence of TB is generally lower in pregnant women compared to young adults between 20 to 30 years of age, who are more socially active and likely to encounter TB-exposed individuals.
Explanation
Choice A rationale:
Europe does report cases of TB, but it does not carry the highest burden of TB according to the World Health Organization (WHO) report in 2020. TB prevalence in Europe is generally lower compared to some other regions.
Choice B rationale:
Africa is the region that had the highest burden of TB according to the WHO report in 2020. The African region has been heavily affected by TB, with a significant number of cases and a high incidence rate of the disease. This is attributed to various factors, including limited access to healthcare, poverty, overcrowded living conditions, and a high prevalence of HIV/AIDS, which weakens the immune system and increases the risk of TB infection.
Choice C rationale:
North America has a lower TB burden compared to Africa, although TB cases are still reported in the region. The incidence of TB in North America is generally lower due to better healthcare infrastructure, access to treatment, and TB control programs.
Choice D rationale:
South America, like North America, has a lower TB burden compared to Africa. However, some countries in South America still experience a significant number of TB cases, particularly in areas with limited access to healthcare and socioeconomic challenges. Nonetheless, Africa remains the region with the highest TB burden according to the WHO report.
Explanation
Choice A rationale:
MDR-TB stands for multidrug-resistant tuberculosis, and it is resistant to at least two of the most potent first-line anti-TB drugs, isoniazid (INH), and rifampicin (RIF) This resistance makes the treatment of MDR-TB more challenging and requires the use of second-line drugs.
Choice B rationale:
XDR-TB stands for extensively drug-resistant tuberculosis, and it is resistant to all first-line anti-TB drugs (INH and RIF) and at least one of the second-line injectable drugs (e.g., amikacin, kanamycin, or capreomycin) XDR-TB is even more challenging to treat than MDR-TB and requires the use of third-line drugs.
Choice C rationale:
RR-TB refers to rifampicin-resistant tuberculosis. It is resistant to rifampicin alone or in combination with other drugs but still susceptible to isoniazid. Rifampicin resistance is a critical indicator for diagnosing MDR-TB.
Choice D rationale:
This statement is incorrect. Drug-resistant TB is not more common in infants and children. It can affect individuals of any age, especially those who have received inadequate or inappropriate treatment for TB, leading to the development of drug resistance.
Choice E rationale:
This statement is correct. Drug-resistant TB requires more prolonged treatment compared to drug-sensitive TB. Treatment for drug-resistant TB can take months to years and often involves a combination of second and third-line drugs, which may have more side effects and require careful monitoring.
Hepatitis.
.
Hepatitis
Explanation
Choice A rationale:
This statement is incorrect. Chronic hepatitis is a condition where liver inflammation lasts for more than six months. If hepatitis lasts less than six months, it is referred to as acute hepatitis.
Choice B rationale:
This statement is incorrect. Chronic hepatitis can be caused by enveloped single-stranded RNA viruses, specifically hepatitis B and C viruses. Non-enveloped single-stranded RNA viruses, like the norovirus, can cause acute gastroenteritis, but not chronic hepatitis.
Choice C rationale:
This statement is correct. Chronic hepatitis, particularly caused by hepatitis B and C viruses, can lead to serious complications such as liver cirrhosis, liver failure, and liver cancer. It is essential to manage chronic hepatitis carefully to prevent these severe outcomes.
Choice D rationale:
This statement is incorrect. Chronic hepatitis is not primarily transmitted through the fecal-oral route. Hepatitis A virus is transmitted through contaminated food or water and primarily spreads through the fecal-oral route. Hepatitis B and C viruses are commonly transmitted through blood contact, sexual contact, and from an infected mother to her baby during childbirth.
Explanation
Choice A rationale:
Hepatitis B can be transmitted through needle sharing, especially in the context of intravenous drug use. Contaminated needles can carry the virus from one person to another.
Choice B rationale:
Hepatitis B can be transmitted through blood transfusion if the donated blood is infected with the virus. However, routine blood screening has significantly reduced the risk of hepatitis B transmission through blood transfusions.
Choice C rationale:
Hepatitis B can be transmitted through sexual contact with an infected partner. The virus is present in the bodily fluids, including blood and semen, making sexual transmission possible.
Choice D rationale:
This statement is incorrect. Hepatitis B is not typically transmitted through the ingestion of contaminated food or water. Hepatitis A virus is the one commonly associated with contaminated food or water.
Choice E rationale:
This statement is incorrect. Hepatitis B is not transmitted through inhaling infected air particles. It primarily spreads through blood contact and sexual contact.
Explanation
Choice A rationale:
Hepatitis C is indeed caused by the hepatitis C virus (HCV), which is a single-stranded RNA virus. The virus is classified under the Flaviviridae family and is known for its high genetic variability, leading to the development of multiple genotypes and subtypes. The RNA genome of HCV is not defective, but rather highly adaptable, making it challenging to develop effective vaccines and treatments. Hepatitis C is primarily transmitted through exposure to infected blood, sharing needles, and, less commonly, through sexual contact and from mother to child during childbirth.
Choice B rationale:
Hepatitis B (HBV) is caused by a partially double-stranded DNA virus, not a non-enveloped single-stranded RNA virus. HBV belongs to the Hepadnaviridae family, and it is transmitted through contact with infected body fluids, such as blood, semen, or vaginal fluids. HBV can cause both acute and chronic liver infections.
Choice C rationale:
Hepatitis A (HAV) is caused by an enveloped single-stranded RNA virus, not hepatitis
C. HAV is transmitted through the fecal-oral route, typically due to contaminated food or water. It is usually a self-limiting disease that does not lead to chronic liver problems.
Choice D rationale:
Hepatitis E (HEV) is caused by a single-stranded RNA virus, but it is not partially double-stranded DNA, as stated in this choice. HEV is typically transmitted through the fecal-oral route, similar to HAV, and it can cause acute hepatitis, particularly in pregnant women, but it does not require a prior hepatitis B infection for transmission.
Explanation
Choice C rationale:
This statement is accurate. Hepatitis C is primarily transmitted through exposure to infected blood, such as sharing needles or receiving contaminated blood transfusions. However, there have been rare cases of HCV transmission through ingestion of contaminated food or water, although this is not the primary mode of transmission. The risk of acquiring HCV through food or water is significantly lower compared to hepatitis A or hepatitis
E.
Choice A rationale:
Hepatitis A (HAV) can indeed be transmitted through sexual contact, as well as the fecal-oral route. HAV is highly contagious and is commonly associated with outbreaks in areas with poor sanitation and hygiene practices.
Choice B rationale:
Hepatitis B (HBV) is transmitted through direct contact with infected body fluids, including blood, semen, and vaginal fluids. It can be transmitted through sexual contact, sharing of needles, and from mother to child during childbirth.
Choice D rationale:
Hepatitis E (HEV) is primarily transmitted through the fecal-oral route, similar to hepatitis
A. Unlike what is stated in this choice, HEV does not require a person to be already infected with hepatitis B to cause infection.
Explanation
Choice D rationale:
This statement accurately differentiates between acute and chronic hepatitis. Acute hepatitis is a short-term inflammation of the liver that typically resolves within six months. It can be caused by various factors, including viral infections (e.g., hepatitis A, B, and C), alcohol consumption, or drug toxicity. On the other hand, chronic hepatitis is a long-lasting inflammation of the liver that persists for more than six months. Chronic hepatitis can result from ongoing viral infections (e.g., hepatitis B and C) or other causes, such as autoimmune diseases.
Choice A rationale:
This statement is incorrect. Acute hepatitis is a short-term condition that resolves within a few weeks to six months, while chronic hepatitis is the condition that can persist for an extended period.
Choice B rationale:
This statement is also incorrect. Acute hepatitis is primarily caused by viruses (e.g., hepatitis viruses), not bacteria. Chronic hepatitis is also related to viral infections, not bacterial infections.
Choice C rationale:
This statement is not accurate. Both acute and chronic hepatitis can have severe consequences, including liver cancer. Chronic hepatitis, especially when caused by hepatitis B or C viruses, can lead to the development of cirrhosis and increase the risk of liver cancer (hepatocellular carcinoma)
Explanation
Choice A rationale:
Needle sharing is associated with the transmission of hepatitis C and HIV, but not hepatitis
A. Hepatitis A is primarily transmitted through the fecal-oral route, usually by consuming food or water contaminated with the virus. Poor sanitation, inadequate hygiene, and consumption of raw or undercooked shellfish are common factors in the spread of hepatitis
A.
Choice B rationale:
Blood transfusion is not a mode of transmission for hepatitis
A. Hepatitis A is mainly transmitted through oral-fecal contact and does not involve the exchange of blood products.
Choice C rationale:
Ingestion of contaminated food or water is the primary mode of transmission for hepatitis
A. The virus is excreted in the feces of infected individuals, and people can become infected by ingesting food or water that has been contaminated with the virus. Proper food handling, handwashing, and access to clean drinking water are essential in preventing the spread of hepatitis
A.
Choice D rationale:
Sexual contact is associated with the transmission of hepatitis B and other sexually transmitted infections, but it is not a significant mode of transmission for hepatitis
A. Hepatitis A is mainly spread through fecal-oral transmission and does not commonly involve sexual contact.
Explanation
Choice A rationale:
Avoiding contact with infected animals is not a primary mode of transmission for hepatitis
B. Although some animal species can carry the hepatitis B virus, the primary modes of transmission in humans are through exposure to infected blood, sexual contact, and perinatal transmission from mother to child.
Choice B rationale:
Practicing safe sex with a monogamous partner is an important preventive measure for hepatitis B transmission. The virus can be transmitted through sexual contact, so using barrier methods like condoms and having a mutually monogamous relationship can reduce the risk of infection.
Choice C rationale:
Sharing personal care items with family members is not a preventive measure for hepatitis B transmission. In fact, sharing personal items like toothbrushes or razors can potentially increase the risk of transmission, especially if there is any exchange of blood.
Choice D rationale:
Using intravenous drugs with a clean needle is a preventive measure for blood-borne infections like hepatitis B and C. However, it is not a preventive measure for hepatitis B transmission through sexual contact or perinatal transmission.
Explanation
Choice A rationale:
Leptospirosis is a non-viral cause of hepatitis. It is caused by the bacterium Leptospira and can lead to liver inflammation. Leptospirosis is typically contracted through exposure to contaminated water, soil, or urine of infected animals.
Choice B rationale:
Malaria is not a cause of hepatitis. Malaria is a parasitic infection transmitted through the bite of infected mosquitoes and does not directly affect the liver in the way hepatitis does.
Choice C rationale:
Acetaminophen is a non-viral cause of hepatitis when taken in excessive amounts or in cases of overdose. Acetaminophen toxicity can lead to acute liver failure and hepatitis-like symptoms.
Choice D rationale:
Autoimmune hepatitis is a non-viral cause of hepatitis. It occurs when the body's immune system mistakenly attacks the liver, leading to inflammation and liver damage. The exact cause of autoimmune hepatitis is not well understood.
Choice E rationale:
Hepatitis B is a viral cause of hepatitis and is not a non-viral cause. It is caused by the hepatitis B virus (HBV) and is transmitted through exposure to infected blood, sexual contact, or perinatal transmission from mother to child.
Explanation
Choice A rationale:
The nurse should expect to assess fever in a client with suspected hepatitis A infection. Hepatitis A can cause flu-like symptoms, and fever is a common manifestation of the infection.
Choice C rationale:
Dark urine is another symptom the nurse should expect to assess in a client with hepatitis
A. Hepatitis A can cause jaundice, leading to dark-colored urine due to the accumulation of bilirubin in the bloodstream.
Choice D rationale:
Abdominal pain is a symptom that the nurse should anticipate in a client with hepatitis A infection. Hepatitis A can cause inflammation of the liver, leading to abdominal discomfort or pain in the right upper quadrant.
Choice E rationale:
Confusion is another possible symptom in a client with hepatitis
A. Severe cases of hepatitis A can lead to hepatic encephalopathy, causing confusion, altered mental status, and even coma.
Explanation
Choice C rationale:
Interferon-alpha may be prescribed for the treatment of chronic hepatitis B infection. It is an antiviral agent that can help boost the immune system's response to the virus and inhibit viral replication.
Choice D rationale:
Entecavir is an antiviral medication that is commonly used to treat chronic hepatitis B infection. It works by inhibiting viral DNA polymerase, thereby reducing viral replication.
Choice E rationale:
Telbivudine is another antiviral agent that may be prescribed for the treatment of chronic hepatitis
B. It works by inhibiting reverse transcriptase, an enzyme necessary for viral replication.
Explanation
Choice C rationale:
The statement "Eating contaminated food can spread hepatitis C" indicates a need for further teaching. Hepatitis C is primarily transmitted through contact with infected blood, such as sharing needles for drug use, getting tattoos with unsterilized equipment, or through unprotected sexual contact. While it is theoretically possible to contract hepatitis C from contaminated food if it has come into contact with infected blood, it is an extremely rare mode of transmission. The nurse should clarify that the main routes of transmission are through blood-to-blood contact.
Explanation
Choice A rationale:
The client's statement, "I will take pegylated interferon-alpha as the antiviral agent," demonstrates understanding of the treatment regimen for chronic hepatitis
D. Pegylated interferon-alpha is the recommended antiviral therapy for chronic hepatitis
D. It helps suppress viral replication and reduce liver inflammation, which is essential in managing the disease. Interferon therapy can be used alone or in combination with antiviral agents like lamivudine or adefovir. However, it is crucial to note that interferon therapy may have side effects, and the client should be educated about them.
Choice B rationale:
"I will use ribavirin to suppress viral replication" is incorrect. Ribavirin is an antiviral agent used for the treatment of hepatitis C but is not typically recommended for hepatitis
D. The primary antiviral therapy for hepatitis D is pegylated interferon-alpha.
Choice C rationale:
"I need to continue the treatment for a shorter duration than hepatitis B or C" is incorrect. The treatment duration for chronic hepatitis D is generally longer than that for hepatitis B or
C. The therapy may last for six months to a year or even longer, depending on the individual response to treatment and the level of liver damage.
Choice D rationale:
"The goal of treatment is to achieve undetectable HDV RNA after the treatment ends" is incorrect. While achieving undetectable HDV RNA is a favorable outcome, it may not always be achievable with current therapies. The primary goal of treatment is to suppress viral replication, reduce liver inflammation, and slow down the progression of liver disease.
Explanation
Choice A rationale:
Prioritizing hydration is essential in the care of a client with hepatitis E infection. Hepatitis E is transmitted through contaminated water and can cause dehydration due to symptoms like vomiting and diarrhea. Hydration helps maintain fluid balance and supports overall recovery.
Choice C rationale:
Pain relief is crucial for managing symptoms associated with hepatitis E infection. The client may experience abdominal pain and discomfort, and providing appropriate pain relief measures can enhance their comfort during the recovery period.
Choice D rationale:
Nutrition support is vital in the care of a client with hepatitis E infection. The disease can cause nausea, vomiting, and loss of appetite, leading to malnutrition. Providing adequate nutrition helps support the immune system and aids in the healing process.
Choice E rationale:
Antipyretics may be necessary for managing fever, which is a common symptom of hepatitis
E. Controlling fever can help improve the client's comfort and prevent complications associated with high body temperature.
Choice B rationale:
Antiviral therapy is not a standard treatment for hepatitis E infection. In most cases, the infection is self-limiting and resolves on its own without specific antiviral medications.
Explanation
Choice B rationale:
Encouraging the client to rest and limit physical activity is an essential nursing intervention for a client with acute hepatitis
A. Rest is crucial for liver recovery and reducing the risk of complications. Physical activity can put additional stress on the liver and may worsen symptoms. The client should avoid alcohol and any medications that can potentially harm the liver during this period.
Choice A rationale:
Isolating the client in a negative pressure room is not necessary for acute hepatitis
A. Hepatitis A is primarily transmitted through the fecal-oral route, and standard precautions are sufficient to prevent its spread. Negative pressure rooms are usually reserved for clients with airborne infections, such as tuberculosis.
Choice C rationale:
Administering live attenuated hepatitis A vaccine is not indicated for a client with acute hepatitis
A. The vaccine is used for pre-exposure prophylaxis and is not effective in treating an active infection.
Choice D rationale:
Providing antiviral medications to treat the infection is not a standard intervention for acute hepatitis
A. Antiviral therapy is generally reserved for chronic hepatitis B and C infections and is not effective for acute hepatitis A, which usually resolves on its own with supportive care.
Explanation
Choice A rationale:
Elevated HCV RNA levels indicate ongoing active viral replication and are not indicative of an effective response to antiviral therapy. The goal of antiviral therapy is to suppress viral replication, leading to decreased or undetectable HCV RNA levels.
Choice B rationale:
Presence of anti-HCV antibodies is a marker of past or current exposure to hepatitis C virus. While it indicates the client's immune response to the virus, it does not provide information about the effectiveness of antiviral therapy in suppressing viral replication.
Choice C rationale:
Detectable HCV core antigen suggests the presence of the virus but does not provide information about viral replication or the effectiveness of antiviral therapy in reducing viral load.
Choice D rationale:
Undetectable HCV RNA 12 weeks after treatment is considered a sustained virological response (SVR) and indicates an effective response to antiviral therapy. SVR means that the virus is undetectable in the blood even after the completion of treatment, which indicates successful viral clearance.
Explanation
Choice A rationale:
Cirrhosis is a late-stage complication of chronic liver disease and is not directly related to hepatitis E during pregnancy.
Choice B rationale:
Encephalopathy is a neurological complication of liver disease, but it is not specific to hepatitis E during pregnancy.
Choice C rationale:
Fetal death is a significant complication of hepatitis E during pregnancy. Pregnant women with hepatitis E have an increased risk of severe outcomes, including miscarriage, stillbirth, or neonatal death. Close monitoring of fetal well-being is essential in these cases.
Choice D rationale:
Liver cancer is not a common complication of acute hepatitis E during pregnancy.
Explanation
Choice A rationale:
Monitoring vital signs and mental status is crucial in patients with suspected hepatitis as they may develop complications such as hepatic encephalopathy, which can lead to changes in mental status.
Choice B rationale:
Administering prescribed medications and fluids is important to support the patient's liver function and manage symptoms of hepatitis. Antiviral medications may be used to treat certain types of viral hepatitis.
Choice C rationale:
Educating the patient about hepatitis vaccines is not applicable in a patient with suspected hepatitis since vaccines are used for prevention and are not effective in treating an ongoing infection.
Choice D rationale:
Encouraging the patient to engage in high-impact exercise is not recommended in patients with suspected hepatitis, as strenuous physical activity may worsen hepatic injury or lead to complications.
Choice E rationale:
Implementing infection control measures to prevent transmission is crucial in suspected hepatitis cases, as the disease can spread through contact with contaminated blood or body fluids. Standard precautions should be followed to prevent healthcare-associated infections and protect others from contracting the virus.
Explanation
Choice A rationale:
Fatigue is a common side effect of antiviral therapy for hepatitis
C. The medications used to treat hepatitis C can cause general fatigue and tiredness in some patients. The nurse should monitor the client for signs of increased fatigue and address any concerns.
Choice D rationale:
Muscle aches are another possible side effect of antiviral therapy for hepatitis
C. Some patients may experience muscle pain or discomfort while on these medications. The nurse should assess the client for muscle aches and provide appropriate interventions if necessary.
Choice E rationale:
Blurred vision can occur as a side effect of antiviral therapy for hepatitis
C. Some medications used in the treatment of hepatitis C can affect vision in some patients. The nurse should be vigilant in monitoring the client's visual acuity and report any changes to the healthcare provider.
Choice B rationale:
Insomnia is not a common side effect of antiviral therapy for hepatitis
C. While some individuals may experience sleep disturbances due to the stress of managing a chronic condition, insomnia is not directly related to the antiviral medications used in hepatitis C treatment.
Choice C rationale:
Headache is not a typical side effect of antiviral therapy for hepatitis
C. Headaches may occur for various reasons, but they are not directly associated with the medications used to treat hepatitis
C.
Explanation
Choice A rationale:
Advising the patient to avoid alcohol and hepatotoxic drugs is appropriate because in hepatitis A, the liver is already inflamed and compromised. Alcohol and hepatotoxic drugs can further damage the liver and impede the healing process. It is essential to protect the liver from further harm during recovery.
Choice B rationale:
The patient has hepatitis A, not hepatitis C, so there is no need for the hepatitis C vaccine. The hepatitis A vaccine is available for prevention, not the hepatitis C vaccine.
Choice C rationale:
While monitoring liver function is essential for individuals with liver disease, this statement is not specifically relevant to the patient with hepatitis
A. Monitoring liver function is more critical for chronic liver diseases like hepatitis B and C.
Choice D rationale:
Antiviral therapy is not indicated for hepatitis A since the infection usually resolves on its own. This statement is not appropriate for the patient with hepatitis
A.
Explanation
Choice A rationale:
Getting vaccinated with the hepatitis B vaccine is an effective prevention strategy for hepatitis
B. It helps protect the individual from acquiring the virus and developing the disease. Vaccination is crucial, especially for individuals at risk of exposure to the virus, such as healthcare workers, sexually active individuals, and household contacts of infected individuals.
Choice B rationale:
Drinking alcohol occasionally is not a safe practice for individuals with hepatitis
B. Alcohol can further damage the liver and worsen the condition. Avoiding alcohol entirely is essential to protect the liver and promote healing.
Choice C rationale:
Clearance of infection does not confer immunity to hepatitis
B. The patient should still take precautions to prevent potential reinfection through sexual contact or other means.
Choice D rationale:
Screening blood donors and recipients for HBV infection is necessary to prevent the transmission of the virus through blood transfusions. It is a crucial safety measure to ensure that blood and blood products are free from hepatitis B virus and other infectious agents.
Explanation
Choice A rationale:
Fulminant hepatitis is a severe and life-threatening complication of hepatitis E, particularly in pregnant women. It can lead to liver failure, and timely monitoring is crucial to detect any early signs of deterioration in the patient's condition. Pregnant women with hepatitis E require close observation and frequent assessment of liver function to ensure prompt intervention if needed.
Choice B rationale:
Administering hepatitis B immunoglobulin (HBIG) to exposed contacts is not the priority in managing a patient with hepatitis
E. Hepatitis E is caused by a different virus (hepatitis E virus) and is not effectively prevented by hepatitis B immunoglobulin.
Choice C rationale:
Educating the patient about the benefits of hepatitis C vaccine is not relevant to the care of a patient with hepatitis
E. These are two different types of viral hepatitis, caused by distinct viruses (hepatitis C virus and hepatitis E virus), and each requires specific management.
Choice D rationale:
Advising the patient to avoid sexual contact until cleared of infection is important in some cases, but it is not the priority intervention for a patient with hepatitis
E. The primary concern in hepatitis E is monitoring for complications, especially in pregnant women, as discussed in choice A rationale.
Explanation
A.
Choice A rationale:
Choice A is incorrect because the hepatitis A vaccine provides active immunity, not passive immunity. Active immunity means that the body produces its antibodies in response to the vaccine, providing long-term protection against the virus.
Choice B rationale:
The hepatitis A vaccine is indeed recommended for travelers to areas with high prevalence of hepatitis
A. It helps protect travelers from acquiring the virus through contaminated food and water in regions where hepatitis A is more common.
Choice C rationale:
Choice C is incorrect because the hepatitis A vaccine is effective in preventing hepatitis A in close contacts of infected individuals. Vaccination is a crucial preventive measure for those who are in close contact with infected individuals, as it can help halt the spread of the virus.
Choice D rationale:
Choice D is incorrect because the hepatitis A vaccine is not given within 12 hours of birth to newborns of hepatitis A positive mothers. The vaccination schedule for hepatitis A vaccine varies depending on the country's recommendations but is typically given starting at 12-23 months of age.
Explanation
Choice A rationale:
While visual disturbances can occur as side effects of some medications, it is not the priority education for a patient undergoing antiviral therapy for hepatitis
C. Visual disturbances are not common or specific to antiviral therapy.
Choice B rationale:
Choice B is the correct answer because it is essential to educate the patient about avoiding alcohol and hepatotoxic drugs during antiviral therapy for hepatitis
C. Alcohol and certain medications can worsen liver function and interfere with the effectiveness of antiviral treatment.
Choice C rationale:
Educating the patient about the need for a high-protein diet during treatment is not a priority in antiviral therapy for hepatitis
C. While a balanced diet is important for overall health, there is no specific requirement for a high-protein diet during antiviral treatment.
Choice D rationale:
Encouraging the patient to engage in strenuous physical activities to alleviate fatigue is not the priority education for a patient undergoing antiviral therapy. Strenuous physical activities might be counterproductive, as the patient may experience fatigue as a side effect of the therapy. Instead, the focus should be on adequate rest and moderate exercise.
(ATI/HESI question from external source) A nurse is caring for a patient with suspected hepatitis D infection. Which interventions should the nurse include in the care plan? (Select all that apply.)
Explanation
Choice A rationale:
The administration of the hepatitis B vaccine and hepatitis B immunoglobulin (HBIG) to exposed contacts is an appropriate intervention for suspected hepatitis D infection. Hepatitis D is a defective virus that requires the presence of hepatitis B to replicate, so administering the hepatitis B vaccine can prevent hepatitis D infection in exposed contacts. HBIG contains antibodies against hepatitis B, which can provide temporary protection to exposed contacts.
Choice B rationale:
Advising the patient to avoid sexual contact or use condoms until cleared of infection is crucial in preventing the spread of hepatitis D. The virus can be transmitted through blood and sexual contact, so precautionary measures are essential.
Choice C rationale:
The availability and benefits of the hepatitis D vaccine for prevention should be communicated to the patient. Currently, there is no specific treatment for hepatitis D infection, and vaccination is the most effective preventive measure.
Choice D rationale:
Educating the patient about the need for regular monitoring of liver function and viral load is essential in managing hepatitis D. Hepatitis D can lead to severe liver complications, and monitoring liver function and viral load helps in evaluating disease progression and treatment effectiveness.
Choice E rationale:
Disinfecting contaminated surfaces or instruments with bleach or autoclave is not directly related to the care of a patient with suspected hepatitis D infection. Hepatitis D is primarily transmitted through blood and sexual contact, not through contaminated surfaces or instruments.
Meningitis
Explanation
Choice A rationale:
Fever is a common sign of meningitis, regardless of its cause. It is often accompanied by other symptoms such as headache and irritability.
Choice B rationale:
A high-pitched cry is a classic sign of meningitis in infants and young children, especially in bacterial meningitis cases. The inflammation in the meninges can cause irritation of the central nervous system, leading to this specific cry.
Choice C rationale:
Altered mental status is a significant sign of meningitis, especially when bacterial pathogens are involved. It can range from lethargy and confusion to more severe manifestations like seizures and coma.
Choice D rationale:
Weight loss is not typically associated with meningitis. The condition usually presents with acute symptoms such as fever, headache, and neck stiffness, rather than chronic symptoms like weight loss.
Choice E rationale:
A stiff neck is a hallmark sign of meningitis, particularly in cases of bacterial meningitis. It is caused by the irritation and inflammation of the meninges surrounding the spinal cord.
Explanation
Choice D rationale:
Viral meningitis is usually transmitted through direct contact with respiratory droplets. It can also be spread through contact with fecal matter and other body fluids. In contrast, bacterial meningitis has multiple routes of transmission, including respiratory droplets, direct contact, and contaminated food or water.
Choice A rationale:
Ingestion of raw or undercooked snails or slugs is associated with a parasitic infection called "rat lungworm" and not viral meningitis.
Choice B rationale:
While the infected person can act as a vector for the spread of viral meningitis, the primary mode of transmission is through respiratory droplets and not the human body itself. The reservoir for viral meningitis is often human carriers, but it can also exist in other animals or environmental sources.
Choice C rationale:
Neisseria meningitidis and Streptococcus pneumoniae are bacterial pathogens that can cause bacterial meningitis, not viral meningitis.
Choice E rationale:
Viral meningitis is not caused by a fungus, and environmental sources are not the reservoirs for viral meningitis transmission. It is mainly transmitted from person to person.
Explanation
Choice A rationale:
This statement is not appropriate because it assumes a specific diagnosis without further assessment or confirmation. Meningitis can be caused by various pathogens, so it's essential not to jump to conclusions based solely on symptoms.
Choice B rationale:
This statement is appropriate because the patient's symptoms, including fever, headache, stiff neck, and photophobia, are consistent with bacterial meningitis. Bacterial meningitis is a severe infection that requires prompt treatment to prevent complications.
Choice C rationale:
This statement is not appropriate because fungal meningitis typically presents differently and is more common in individuals with compromised immune systems. There is no evidence from the presented symptoms to suggest fungal meningitis.
Choice D rationale:
This statement is not appropriate because parasitic meningitis is very rare and typically associated with specific exposures or travel history. There is no information to support this as a likely cause of the client's symptoms.
Choice E rationale:
This statement is not appropriate because meningococcal septicemia is a different condition from meningitis. While both can be caused by Neisseria meningitidis bacteria, septicemia is characterized by a bloodstream infection, while meningitis affects the meninges.
Explanation
Choice A rationale:
Nuchal rigidity (stiff neck) is a classic symptom of meningitis, but it is not particularly concerning in older adults as it is in younger individuals. Older adults may have a less pronounced neck stiffness due to age-related changes.
Choice B rationale:
Rash can be a symptom of certain types of meningitis, such as meningococcal meningitis, but it is not specific to older adults. Moreover, older adults may not exhibit a rash even in cases of meningococcal meningitis.
Choice C rationale:
Irritability is a vague symptom and may not be specific to meningitis in older adults. It can be caused by various factors and does not raise significant concern for meningitis.
Choice D rationale:
Altered mental status, such as confusion, delirium, or decreased level of consciousness, is particularly concerning in older adults with suspected meningitis. Older adults may not always present with classic symptoms like neck stiffness, and altered mental status may be the primary indicator of central nervous system involvement.
Choice E rationale:
Photophobia is a common symptom of meningitis, but it is not specific to older adults. It may be present in both younger and older patients with meningitis.
Explanation
Choice A rationale:
This statement is incorrect. A lumbar puncture involves the insertion of a needle, not a catheter, into the subarachnoid space of the spinal canal to collect cerebrospinal fluid (CSF) It is not done in blood vessels.
Choice B rationale:
This statement is accurate. A lumbar puncture is performed to obtain a sample of cerebrospinal fluid for analysis. It helps to diagnose and differentiate between bacterial and viral meningitis based on CSF characteristics, such as cell count, glucose levels, and presence of bacteria or viruses.
Choice C rationale:
This statement is incorrect. A lumbar puncture is uncomfortable but is typically not an extremely painful procedure. It is often done with local anesthesia, and the discomfort is usually temporary.
Choice D rationale:
This statement is incorrect. During a lumbar puncture, the patient is usually asked to curl up in a fetal position, bringing the knees close to the chest and the chin to the chest. This position helps to widen the spaces between the spinal bones, making it easier for the healthcare provider to insert the needle into the subarachnoid space. It does not involve bending the neck forward.
Explanation
Choice A rationale:
Haemophilus influenzae type b (Hib) was a common cause of bacterial meningitis in the past, especially in children, but its incidence has significantly decreased due to the widespread use of the Hib vaccine.
Choice B rationale:
Neisseria meningitidis (meningococcal) can cause meningitis and is an important pathogen, but it is more commonly associated with meningitis in children and young adults.
Choice C rationale:
Streptococcus pneumoniae (pneumococcal) is the most common cause of bacterial meningitis in adults. It is a gram-positive bacterium that can lead to severe infections, including pneumonia, meningitis, and bloodstream infections.
Choice D rationale:
Escherichia coli is a bacterial species typically associated with urinary tract infections and gastrointestinal illnesses. While it can rarely cause meningitis in certain populations, it is not the most common cause of bacterial meningitis in adults.
Choice E rationale:
Group B streptococcus is a significant cause of neonatal meningitis but is less commonly responsible for meningitis in adults.
Explanation
Choice A rationale:
Ingestion of contaminated water is the primary mode of transmission for certain gastrointestinal infections, such as viral gastroenteritis, but it is not the main route for viral meningitis transmission.
Choice B rationale:
Mosquito or tick bites are associated with the transmission of various vector-borne diseases, such as West Nile virus, Lyme disease, and others. However, they are not the primary mode of transmission for viral meningitis.
Choice C rationale:
Direct contact with respiratory droplets or saliva from an infected person is the most common mode of transmission for viral meningitis. Viruses causing meningitis, such as enteroviruses, are often present in respiratory secretions and saliva.
Choice D rationale:
Inhalation of fungal spores is related to the transmission of certain fungal infections, such as aspergillosis or histoplasmosis, but it is not the primary mode of transmission for viral meningitis.
Choice E rationale:
Contact with contaminated soil is not a typical mode of transmission for viral meningitis. It might be relevant for some soil-transmitted infections but not for viral meningitis.
Explanation
Choice A rationale:
Bacterial meningitis is the most common and severe type of meningitis in infants and children. The causative bacteria can include Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae type b, among others.
Choice B rationale:
Fungal meningitis is less common than bacterial meningitis and is usually associated with specific risk factors, such as immunosuppression or exposure to certain environmental fungi.
Choice C rationale:
Viral meningitis is more common than bacterial meningitis, but it is usually milder and often resolves without specific treatment. Enteroviruses are the most frequent cause of viral meningitis in infants and children.
Choice D rationale:
Parasitic meningitis is a rare form of the disease and is usually associated with specific parasites, such as the amoeba Naegleria fowleri or the parasite Trypanosoma.
Choice E rationale:
Meningitis of unknown origin refers to cases where the cause of meningitis remains unidentified after thorough investigations. It is not a specific type of meningitis but rather a descriptive term for cases with uncertain etiology.
Explanation
Choice A rationale:
A blood culture is a test used to detect bacteria or other microorganisms in the bloodstream. While it can be helpful in diagnosing bacterial infections, it is not the most important test for confirming meningitis. The presence of bacteria in the blood does not necessarily confirm meningitis, as the infection may not have spread to the bloodstream yet.
Choice B rationale:
A throat swab is used to collect samples from the throat to identify infections such as strep throat. While throat infections can sometimes lead to complications like meningitis, a throat swab is not the most important test for confirming the diagnosis of meningitis. The infection may not be present in the throat, and direct examination of cerebrospinal fluid is necessary to confirm meningitis.
Choice C rationale:
A lumbar puncture, also known as a spinal tap, is the most important laboratory test to confirm the diagnosis of meningitis. It involves collecting a sample of cerebrospinal fluid (CSF) from the space around the spinal cord and brain. Analysis of the CSF can reveal the presence of bacteria or other pathogens, increased white blood cells, and other indicators of meningitis.
Choice D rationale:
A computed tomography (CT) scan is a diagnostic imaging test that uses X-rays to create detailed cross-sectional images of the body. While it can help identify structural abnormalities in the brain, such as bleeding or tumors, it is not the primary test for confirming meningitis. CT scans may show signs of inflammation, but they cannot definitively diagnose meningitis or distinguish between bacterial, viral, or fungal causes.
Explanation
Choice A rationale:
Administering intravenous fluids is an appropriate nursing intervention for a client with meningitis. Meningitis can cause dehydration due to fever, decreased oral intake, and increased fluid loss. IV fluids help maintain hydration and prevent complications.
Choice B rationale:
Applying warm compresses to the forehead is not a standard nursing intervention for meningitis. Fever is a common symptom of meningitis, and while comfort measures may be used to manage fever, warm compresses on the forehead are not specific to meningitis and may not be well-tolerated by some patients.
Choice C rationale:
Providing dim lighting and minimizing noise are appropriate nursing interventions for a client with meningitis. Meningitis can cause sensitivity to light and sound, and creating a calm and quiet environment can help reduce discomfort and promote healing.
Choice D rationale:
Giving prophylactic antibiotics is an appropriate nursing intervention for bacterial meningitis. Once the diagnosis of bacterial meningitis is confirmed or suspected, antibiotics should be initiated promptly to control the infection and prevent complications.
Choice E rationale:
Monitoring vital signs and neurological status is crucial for a client with meningitis. Vital signs such as temperature, heart rate, respiratory rate, and blood pressure should be closely monitored to assess for any signs of worsening condition or complications. Neurological assessments help identify changes in the client's mental status, reflexes, and cranial nerve function.
Explanation
Choice A rationale:
A cloudy appearance of cerebrospinal fluid (CSF) can indicate the presence of white blood cells and bacteria, suggesting an infection. However, it is not specific to bacterial or fungal infection and can also be seen in viral meningitis or non-infectious conditions like multiple sclerosis.
Choice B rationale:
Increased pressure in the CSF may occur in meningitis due to the inflammation and accumulation of fluid. While it can raise suspicion for meningitis, it is not specific to bacterial or fungal infection and can also be observed in other intracranial conditions.
Choice C rationale:
Decreased glucose levels in the CSF are a characteristic finding in bacterial or fungal meningitis. The invading bacteria or fungi consume glucose, leading to lower levels in the CSF compared to normal blood glucose levels. This finding helps differentiate bacterial or fungal meningitis from viral meningitis, where glucose levels are usually normal.
Choice D rationale:
Elevated protein levels in the CSF can be seen in various conditions, including meningitis. While it indicates increased inflammation and breakdown of cells, it is not specific to bacterial or fungal infection and can be present in viral or other forms of meningitis.
Explanation
Choice A rationale:
If the cerebrospinal fluid (CSF) were normal, it would have clear and colorless appearance. Pink-colored CSF indicates the presence of an abnormality, ruling out the normal CSF as an option.
Choice B rationale:
The pink color of the CSF suggests blood contamination, which can occur during the lumbar puncture procedure. The presence of blood can alter the CSF composition and lead to false interpretations of laboratory results.
Choice C rationale:
Bacterial infection may present with cloudy or purulent CSF, but it is not specifically associated with pink-colored CSF. Other signs, such as elevated white blood cell count and elevated protein levels, would be more indicative of a bacterial infection.
Choice D rationale:
Dehydration does not typically cause pink-colored CSF. Dehydration may lead to a higher concentration of solutes in the CSF, but it does not affect its coloration.
Explanation
Choice A rationale:
Intravenous antibiotics are used to treat bacterial meningitis, not viral meningitis. Viral meningitis is caused by viruses and does not respond to antibiotics.
Choice B rationale:
Antifungal drugs are used to treat fungal meningitis, not viral meningitis. Viral meningitis is caused by viruses, not fungi.
Choice C rationale:
Supportive care is the appropriate treatment for viral meningitis. Since viral meningitis is usually self-limiting and does not respond to specific antiviral medications, treatment focuses on managing symptoms and providing supportive measures to help the client recover.
Choice D rationale:
Prophylactic corticosteroids may be used in certain cases of bacterial meningitis to reduce inflammation and prevent complications, but they are not indicated for the treatment of viral meningitis.
Explanation
Choice A rationale:
Administering antipyretics helps to reduce fever, but it does not specifically prevent the spread of meningitis. It addresses a symptom but does not target the transmission of the disease.
Choice B rationale:
Elevating the head of the bed is beneficial for clients with increased intracranial pressure, not for preventing the spread of meningitis.
Choice C rationale:
Providing comfort measures can improve the client's well-being, but it does not directly address the prevention of meningitis transmission.
Choice D rationale:
Practicing good hygiene habits, such as regular handwashing, can help prevent the spread of meningitis. Since meningitis can be transmitted through respiratory secretions, practicing good hygiene is essential in reducing the risk of infection transmission.
Explanation
Choice A rationale:
The recommended preventive measure for a client planning to travel to a high-risk area for meningitis is to take prophylactic antibiotics. Meningitis is an inflammation of the meninges, the membranes covering the brain and spinal cord, and it can be caused by various pathogens, including bacteria. Travel to high-risk areas may increase the risk of exposure to meningitis-causing bacteria. Prophylactic antibiotics are given to individuals at high risk of contracting bacterial meningitis to prevent infection or reduce the severity if exposed. Commonly used antibiotics for prophylaxis include ciprofloxacin, rifampin, and others, depending on the specific high-risk area and its predominant pathogens.
Choice B rationale:
Getting vaccinated against mumps is not the recommended preventive measure for meningitis caused by other pathogens. Mumps is a viral infection caused by the mumps virus, and while it can cause complications, it is not a common cause of meningitis. The appropriate preventive measure for mumps is vaccination with the measles, mumps, and rubella (MMR) vaccine.
Choice C rationale:
Practicing good hand hygiene is essential for preventing the spread of infections in general, but it is not specifically targeted at preventing meningitis. Meningitis is usually transmitted through respiratory droplets or direct contact with infected individuals. While hand hygiene can help reduce the risk of contracting various infections, it is not the primary preventive measure for meningitis.
Choice D rationale:
Avoiding close contact with people with respiratory infections is a good practice to reduce the risk of various respiratory infections, including those that can cause meningitis. However, it is not the recommended specific preventive measure for a client planning to travel to a high-risk area for meningitis. Prophylactic antibiotics are the more appropriate choice in this situation to directly target potential meningitis-causing bacteria.
Explanation
Choice A rationale:
Amphotericin B is an antifungal drug that may be used to treat fungal meningitis. It is effective against a wide range of fungal pathogens and is often considered the drug of choice for severe systemic fungal infections, including fungal meningitis.
Choice B rationale:
Fluconazole is another antifungal drug used to treat fungal meningitis. It is effective against certain types of fungi, especially Candida species, which are known to cause fungal meningitis in some cases.
Choice E rationale:
Voriconazole is a broad-spectrum antifungal medication that is also used to treat fungal meningitis. It is particularly effective against Aspergillus species, which can cause invasive fungal infections, including meningitis.
Choice C rationale:
Albendazole is an antiparasitic drug and is not used to treat fungal meningitis. It is primarily indicated for the treatment of parasitic infections, such as certain types of worms.
Choice D rationale:
Ivermectin is another antiparasitic drug and is not used in the treatment of fungal meningitis. It is commonly used to treat various parasitic infections but has no activity against fungal pathogens.
Explanation
Choice A rationale:
In a temperate region during summer, viral meningitis is more likely to be prevalent in the population. Viral meningitis is most commonly caused by enteroviruses, and these infections tend to be more common in the summer and early fall. Enteroviruses thrive in warm and humid conditions, contributing to the seasonal variation in viral meningitis cases.
Choice B rationale:
Bacterial meningitis can occur throughout the year and is not specifically associated with summer or temperate regions. Bacterial meningitis can result from various bacterial pathogens and is usually a more severe and life-threatening form of meningitis compared to viral meningitis.
Choice C rationale:
Fungal meningitis is not typically associated with temperate regions during the summer. Fungal meningitis is more commonly seen in individuals with compromised immune systems or in specific geographic regions with a higher prevalence of fungal infections.
Choice D rationale:
Parasitic meningitis is not prevalent in temperate regions during the summer. Parasitic meningitis is rare and is usually associated with specific parasitic infections, such as those caused by Naegleria fowleri or Angiostrongylus cantonensis, which are typically found in tropical or subtropical regions.
Explanation
Choice A rationale:
Viral meningitis is caused by viral infections and is more commonly seen in the summer and fall months rather than in tropical regions during winter.
Choice B rationale:
Bacterial meningitis is more common in tropical regions during the winter season. It is caused by bacterial infections and can be severe and life-threatening if not promptly treated. The colder weather in the winter may increase the transmission of bacteria responsible for causing meningitis.
Choice C rationale:
Fungal meningitis is not specifically associated with any particular season or region. It can occur in individuals with weakened immune systems, but it is not more common in tropical regions during winter.
Choice D rationale:
Parasitic meningitis is primarily caused by parasites and is not typically associated with any specific season or region. It is a rare form of meningitis and is not more prevalent in tropical regions during winter.
Explanation
Choice A rationale:
Meningococcal meningitis is not mainly seen in infants. It can affect individuals of all ages, but infants and young children are more susceptible to certain types of bacterial meningitis, such as Haemophilus influenzae type b.
Choice B rationale:
Meningococcal meningitis is primarily transmitted through respiratory droplets, close contact with an infected person, or exposure to contaminated respiratory or throat secretions. It is not primarily linked to regions with contaminated water.
Choice C rationale:
Meningococcal meningitis can progress rapidly and cause death within hours if left untreated. Therefore, early recognition and prompt medical treatment are essential to improve outcomes.
Choice D rationale:
The statement comparing meningococcal meningitis with fungal meningitis' mortality rate is not accurate. While meningococcal meningitis can be severe, fungal meningitis is generally associated with a higher mortality rate, especially in individuals with weakened immune systems.
Explanation
Choice A rationale:
Pneumococcal meningitis can affect individuals of all ages, although children under five years old and adults over 65 years old are at a higher risk. It is not exclusive to young children under five.
Choice B rationale:
Pneumococcal meningitis is caused by the bacterium Streptococcus pneumoniae, not Haemophilus influenzae type b.
Choice C rationale:
Pneumococcal meningitis is not only prevalent in tropical regions; it can occur worldwide.
Choice D rationale:
With appropriate and timely treatment, the mortality rate of pneumococcal meningitis can be relatively low. However, it is still a severe and potentially life-threatening condition, and prompt medical attention is crucial to avoid complications.
Explanation
Choice A rationale:
Blood culture is not the appropriate diagnostic procedure for confirming meningitis. While blood cultures can identify bacteria or other pathogens in the bloodstream, it may not directly confirm meningitis, as the infection is primarily located in the cerebrospinal fluid (CSF)
Choice B rationale:
Urinalysis is not the appropriate diagnostic procedure for confirming meningitis. Urinalysis helps in detecting urinary tract infections or kidney-related issues, but it does not provide relevant information about meningitis.
Choice C rationale:
Lumbar puncture and CSF analysis are essential in diagnosing meningitis. This procedure involves inserting a needle into the spinal canal to collect a sample of CSF, which is then analyzed for signs of infection, such as elevated white blood cell count, increased protein levels, and the presence of bacteria or viruses. It helps differentiate between bacterial, viral, or fungal causes and guides appropriate treatment.
Choice D rationale:
A chest X-ray is not directly related to diagnosing meningitis. It is used to evaluate lung and heart conditions, making it irrelevant in confirming meningitis.
A patient with weakened immunity presents with chronic meningitis. Which type of meningitis is more likely in this case?
Explanation
Choice A rationale:
Viral meningitis is less likely in this case because the patient has weakened immunity, suggesting a chronic and severe condition. Viral meningitis is often self-limiting and less severe in immunocompetent individuals.
Choice B rationale:
Bacterial meningitis is less likely in this case as well, as chronic meningitis usually has a slower onset, and bacterial meningitis tends to have a more acute and rapidly progressive course.
Choice C rationale:
Fungal meningitis is more likely in a patient with weakened immunity, as certain fungal pathogens, such as Cryptococcus and Histoplasma, can cause chronic and persistent meningitis in immunocompromised individuals.
Choice D rationale:
Parasitic meningitis is not a common form of meningitis and is usually associated with specific parasitic infections, which are less likely to occur in immunocompromised patients.
Choice E rationale:
Tuberculous meningitis is a type of bacterial meningitis caused by Mycobacterium tuberculosis. While it can occur in immunocompromised individuals, fungal meningitis is more prevalent in this population.
Which of the following statements about meningitis prevention is accurate?
Explanation
Choice A rationale:
All types of meningitis cannot be prevented by vaccination. While vaccinations are available for certain types of bacterial and viral meningitis, they do not cover all possible pathogens that can cause the disease.
Choice B rationale:
Meningitis can be prevented through prophylaxis measures, but this statement is not entirely accurate. Prophylaxis may be given to close contacts of individuals with certain types of bacterial meningitis to prevent its spread, but it does not apply to all cases of meningitis.
Choice C rationale:
Infection control measures are effective in preventing meningitis outbreaks. This statement is incorrect as infection control measures are crucial in controlling the spread of infections, but they cannot entirely prevent all cases of meningitis.
Choice D rationale:
Hygiene practices, such as regular handwashing and proper respiratory etiquette, play a significant role in preventing meningitis transmission. By reducing the spread of respiratory and oral pathogens, the risk of meningitis can be lowered. However, it is important to note that not all forms of meningitis are entirely preventable through hygiene practices alone, which is why vaccination remains a critical preventive measure for specific types of meningitis.
A nurse is providing care to a pediatric patient diagnosed with Haemophilus influenzae type b meningitis. Which additional preventive measure should the nurse recommend?
Explanation
Choice A rationale:
Antibiotic therapy for the family members is not the most appropriate preventive measure for Haemophilus influenzae type b meningitis. While antibiotics are used to treat the infection, providing antibiotic therapy to family members does not prevent the spread of the bacteria to others.
Choice B rationale:
Prophylaxis for the patient's close contacts is the recommended preventive measure for Haemophilus influenzae type b meningitis. Close contacts of a patient with this type of meningitis, such as household members and daycare contacts, are at an increased risk of contracting the disease. Administering prophylactic antibiotics to these individuals can help prevent the transmission of the bacteria and reduce the likelihood of developing the infection.
Choice C rationale:
Hygiene education for school staff and students is not directly related to preventing the spread of Haemophilus influenzae type b meningitis. While hygiene education is essential for preventing the spread of infections in general, it is not specific to this particular type of meningitis.
Choice D rationale:
Outbreak management protocols for the community may be necessary if there is an outbreak of Haemophilus influenzae type b meningitis. However, this choice does not address the immediate preventive measure needed for the diagnosed pediatric patient and their close contacts.
Choice E rationale:
Vaccination against Neisseria meningitidis is not directly relevant to preventing Haemophilus influenzae type b meningitis. These are two different types of bacteria that cause different forms of meningitis, and vaccination against Neisseria meningitidis would not protect against Haemophilus influenzae type b meningitis.
Zika virus
Explanation
Choice A rationale:
Aedes aegypti mosquitoes are one of the primary vectors for Zika virus transmission. They are highly efficient at spreading the virus and are commonly found in tropical and subtropical regions.
Choice B rationale:
Aedes albopictus mosquitoes are another significant vector for Zika virus transmission. They are widespread and can be found in both tropical and temperate regions, making them important carriers of the virus.
Choice C rationale:
Anopheles mosquitoes are primarily known for transmitting malaria, not Zika virus. They are not significant vectors for Zika transmission.
Choice D rationale:
Culex mosquitoes are known for transmitting diseases such as West Nile virus and Japanese encephalitis but are not major vectors for Zika virus transmission.
Choice E rationale:
Anobium mosquitoes are not vectors for Zika virus transmission. They are a type of wood-boring beetle and do not play a role in spreading the virus to humans.
Explanation
Choice A rationale:
Zika virus is not primarily transmitted through contaminated food and water. The main mode of transmission is through mosquito bites.
Choice B rationale:
Zika virus is not spread by airborne droplets from infected individuals. It is primarily transmitted by mosquitoes, as mentioned earlier.
Choice C rationale:
This is the correct answer. Zika virus is primarily transmitted by the Aedes species mosquitoes, particularly Aedes aegypti and Aedes albopictus, which are the main vectors responsible for spreading the virus. When an infected mosquito bites a person, the virus can be transmitted to the individual.
Choice D rationale:
Zika virus can also be transmitted through sexual contact, but this is not the primary mode of transmission. The primary mode is through mosquito bites.
Explanation
Choice A rationale:
Swelling of the limbs, also known as peripheral edema, can be an additional symptom of Zika virus infection. It is one of the less common symptoms but may occur in some cases.
Choice B rationale:
Enlarged lymph nodes are not typically associated with Zika virus infection. While lymphadenopathy can occur with various infections, it is not a characteristic symptom of Zika virus.
Choice C rationale:
Persistent cough is not a typical symptom of Zika virus infection. Zika virus primarily presents with fever, rash, joint pain, and other flu-like symptoms.
Choice D rationale:
Visual disturbances are not commonly reported symptoms of Zika virus infection. Zika virus mainly affects the nervous system of developing fetuses during pregnancy, leading to congenital abnormalities, but visual disturbances are not a usual symptom in infected individuals.
Explanation
Choice A rationale:
Isolating the client in a negative pressure room is not necessary for Zika virus, as it is not primarily transmitted through respiratory droplets. Isolation is not a standard precaution for this infection.
Choice B rationale:
There is no specific antiviral medication for treating Zika virus infection, so administering antiviral medication is not the appropriate intervention.
Choice C rationale:
Providing supportive care for symptoms is important, but the most appropriate nursing intervention to prevent further transmission of the virus is educating the client about mosquito bite prevention. By using mosquito repellents, wearing protective clothing, and eliminating breeding sites, the client can reduce the risk of further transmission to others and protect themselves from additional mosquito bites.
Which of the following viruses is closely related to Zika virus?
Explanation
Choice A rationale:
Hepatitis A virus is not closely related to Zika virus. Hepatitis A is a virus that primarily affects the liver and is transmitted through contaminated food or water, not through mosquitoes like Zika virus.
Choice B rationale:
Influenza virus is not closely related to Zika virus. Influenza, commonly known as the flu, is a respiratory illness caused by influenza viruses and is spread through respiratory droplets.
Choice C rationale:
Dengue virus is closely related to Zika virus. Both Zika and Dengue viruses are members of the Flaviviridae family and are transmitted by the same Aedes mosquito species.
Choice D rationale:
Rotavirus is not closely related to Zika virus. Rotavirus is the leading cause of severe diarrhea in young children and is transmitted through the fecal-oral route, not through mosquitoes.
What is the primary mode of transmission of Zika virus?
Explanation
Choice A rationale:
Sexual contact is not the primary mode of transmission for Zika virus. Although Zika can be sexually transmitted, the main mode of transmission is through mosquito bites.
Choice B rationale:
Airborne droplets are not the primary mode of transmission for Zika virus. Zika virus is not typically spread through respiratory droplets like some other viruses, such as the flu.
Choice C rationale:
Infected food consumption is not the primary mode of transmission for Zika virus. Zika virus is not known to be transmitted through contaminated food.
Choice D rationale:
Mosquito bites are the primary mode of transmission for Zika virus. Infected Aedes mosquitoes, particularly Aedes aegypti and Aedes albopictus, transmit the virus to humans through their bites.
A nurse is teaching a community group about Zika virus prevention. Which mosquito species should the nurse emphasize as the main vectors for Zika virus transmission?
Explanation
Choice A rationale:
Anopheles mosquitoes are not the main vectors for Zika virus transmission. Anopheles mosquitoes are known for transmitting malaria, not Zika.
Choice B rationale:
Culex mosquitoes are not the main vectors for Zika virus transmission. Culex mosquitoes can transmit West Nile virus, but they are not significant carriers of Zika virus.
Choice C rationale:
Aedes aegypti is the main vector for Zika virus transmission. This mosquito species is highly responsible for spreading Zika to humans, especially in urban areas.
Choice D rationale:
Aedes albopictus is also a vector for Zika virus transmission. It is another Aedes mosquito species that can transmit the virus, but it is less efficient in some regions compared to Aedes aegypti.
Choice E rationale:
Anobium mosquitoes are not vectors for Zika virus transmission. Anobium mosquitoes are associated with wood-boring beetles and are not involved in the transmission of Zika virus.
Explanation
Choice A rationale:
The nurse should consider recent travel history to a Zika virus transmission area because Zika virus is primarily transmitted through the bite of infected Aedes mosquitoes, and it is more likely for the patient to have contracted the virus if they have recently been in an area where the virus is actively transmitted.
Choice B rationale:
The presence of fever, headache, rash, and joint pain are essential criteria for suspecting Zika virus infection because these are common symptoms associated with the disease. Fever and rash are particularly characteristic symptoms of Zika virus infection.
Choice C rationale:
Laboratory confirmation of Zika virus infection is not essential for suspecting the infection, especially in the early stages when the patient is presenting with symptoms. Zika virus diagnosis often involves clinical evaluation, recent travel history to transmission areas, and symptoms.
Choice D rationale:
Exposure to blood transfusion is not a specific criteria for suspecting Zika virus infection. While Zika virus can be transmitted through blood transfusion, it is not a primary consideration when initially suspecting the infection based on the patient's symptoms and travel history.
Choice E rationale:
The use of aspirin for pain relief is not a criteria for suspecting Zika virus infection. It is not directly related to the disease and would not aid in the initial assessment and suspicion of the infection.
Explanation
Choice A rationale:
Providing prenatal screening and testing for Zika virus infection is important in identifying if the fetus is affected by the virus. Early detection can help monitor and manage the pregnancy accordingly.
Choice B rationale:
Offering postnatal care and follow-up for babies with microcephaly is crucial because Zika virus infection during pregnancy can lead to congenital Zika syndrome, which may include microcephaly in newborns.
Choice C rationale:
Advocating for the rights and needs of pregnant women is essential in ensuring they receive appropriate care, support, and information about Zika virus infection during pregnancy.
Choice D rationale:
Implementing vector control activities to reduce mosquito breeding is vital in preventing the spread of Zika virus to pregnant women and reducing the risk of infection during pregnancy.
Choice E rationale:
Encouraging early pregnancy without delay is not a nursing intervention to reduce the risk of congenital Zika syndrome. It is not a relevant response to the question and does not address the management of Zika virus infection in pregnancy.
Explanation
Choice D rationale:
The statement "I don't need to worry about Zika virus if I only have flu-like symptoms" indicates a need for further teaching. Zika virus infection can present with flu-like symptoms, and it is important for the patient to be aware that they should seek medical attention and get tested for Zika if they experience such symptoms, especially if they have a recent travel history to a Zika virus transmission area. The statement shows a lack of understanding about the potential risk of Zika virus infection and the importance of timely testing and management.
Explanation
Choice A rationale:
Zika virus infection is a viral illness primarily transmitted through mosquito bites. As of my knowledge cutoff in September 2021, there is no specific antiviral treatment available for Zika virus. Treatment is primarily supportive and focuses on relieving symptoms such as fever, pain, and rash. Rest, adequate hydration, and pain relief medications, such as acetaminophen, are recommended. Ibuprofen is not typically recommended due to its potential link to increased risk of severe disease in some viral infections. Antibiotics are not effective against viruses like Zika, as they are only effective against bacterial infections. Antimalarial medications are not indicated for the treatment of Zika virus infection.
Explanation
Choice A rationale:
Providing education and counseling about Zika virus transmission is important, but it is not the appropriate nursing intervention for a patient with Guillain-Barré syndrome possibly related to Zika virus infection. The patient's immediate needs are related to their condition and potential complications.
Choice B rationale:
Monitoring and caring for pregnant women with Zika virus infection is essential, especially due to the potential risk of congenital Zika syndrome in babies born to infected mothers. However, this choice is not the appropriate nursing intervention for a patient with Guillain-Barré syndrome.
Choice C rationale:
Conducting surveillance and research on Zika virus complications is a valuable public health effort, but it is not a direct nursing intervention for an individual patient with Guillain-Barré syndrome.
Explanation
Choice A rationale:
Maternal-fetal transmission is another mode of Zika virus transmission, but it is not the primary mode. Zika virus can pass from an infected pregnant woman to her fetus during pregnancy or around the time of birth.
Choice C rationale:
Blood transfusion can be a mode of Zika virus transmission, but it is not the primary mode. Zika virus can be transmitted through blood transfusion from an infected donor to a recipient.
Choice D rationale:
Contact with infected animals is not a primary mode of Zika virus transmission. Zika virus primarily spreads through mosquito bites and sexual contact.
Explanation
Reverse transcription polymerase chain reaction (RT-PCR)
Choice A rationale:
RT-PCR is essential for confirming the diagnosis of Zika virus infection. It is a molecular diagnostic test that can detect the presence of viral RNA in a patient's blood or other body fluids. This test is highly specific and sensitive, making it the preferred method for confirming Zika virus infection during the acute phase of the illness.
Choice B rationale:
Serological test for dengue virus is not the correct choice for confirming Zika virus infection. While both Zika and dengue viruses are transmitted by the same mosquito vector, they are different viruses, and serological tests for dengue antibodies would not detect Zika virus infection accurately.
Choice C rationale:
Tuberculosis skin test (TST) is not relevant for diagnosing Zika virus infection. TST is used for detecting tuberculosis infection, not viral infections like Zika.
Choice D rationale:
Complete blood count (CBC) is a general blood test that measures different components of the blood, such as red blood cells, white blood cells, and platelets. CBC is not specific to diagnosing Zika virus infection and would not provide any information about the presence of the Zika virus.
Explanation
Choice A rationale:
Using mosquito nets while sleeping is an effective preventive measure against mosquito-borne infections like Zika. It helps protect individuals from mosquito bites during sleep, when they are most vulnerable.
Choice B rationale:
Applying sunscreen to exposed skin is essential for protecting against sunburn and skin damage, but it does not prevent Zika virus infection, which is transmitted through mosquito bites.
Choice C rationale:
Eliminating standing water to reduce mosquito breeding sites is crucial for controlling the mosquito population. Mosquitoes breed in stagnant water, and by eliminating these breeding sites, the mosquito population decreases, reducing the risk of Zika transmission.
Choice D rationale:
Avoiding sexual contact with partners who traveled to Zika transmission areas is important because Zika can be sexually transmitted. Infected individuals can transmit the virus to their sexual partners, leading to potential spread of the infection.
Choice E rationale:
Consuming unpasteurized dairy products for immunity boost is not a preventive measure against Zika virus infection. There is no evidence to suggest that unpasteurized dairy products can protect against Zika, and consuming them can pose other health risks due to potential contamination with harmful pathogens.
Measles.
A nurse is educating a pregnant client about Zika virus. What are the potential complications of Zika virus infection in pregnancy? Select the correct options.
Explanation
Choice A rationale:
Microcephaly is a potential complication of Zika virus infection in pregnancy. It refers to a condition where the baby's head is smaller than expected, which can result in developmental issues and intellectual disabilities.
Choice B rationale:
Yellow fever is not a potential complication of Zika virus infection in pregnancy. Yellow fever is a separate viral disease transmitted by mosquitoes and is not associated with Zika virus infection during pregnancy.
Choice C rationale:
Respiratory distress is not a common complication of Zika virus infection in pregnancy. Zika virus typically causes mild symptoms in adults and is not known to cause severe respiratory issues.
Choice D rationale:
Conjunctivitis, also known as pink eye, can be a symptom of Zika virus infection, but it is not a significant complication in pregnancy. It is a mild and self-limiting condition that does not typically cause long-term effects on the baby.
Choice E rationale:
Hearing loss is a potential complication of Zika virus infection in pregnancy. Zika virus can affect the development of the baby's auditory system, leading to hearing impairment.
Measles
Explanation
Measles is transmitted through respiratory droplets and person-to-person contact.
Choice A rationale:
Measles is not transmitted through contaminated water sources. It is a highly contagious viral infection that primarily spreads through respiratory droplets when an infected person coughs or sneezes.
Choice B rationale:
Measles is not transmitted through contact with infected animals. It is a human-specific virus and does not infect animals.
Choice C rationale:
This is the correct choice. Measles is primarily transmitted through respiratory droplets when an infected person coughs or sneezes. It can also spread through direct contact with respiratory secretions or airborne particles.
Choice D rationale:
Measles is not transmitted through exposure to contaminated food. The virus is not foodborne, and the main mode of transmission is person-to-person through respiratory droplets.
Explanation
Choice A rationale:
The prodrome stage of measles infection is characterized by symptoms that precede the rash. One of the characteristic features of this stage is a high fever, typically greater than 38.5°C. This fever is a result of the immune response to the viral infection.
Choice B rationale:
Another characteristic of the prodrome stage is malaise and anorexia. Malaise refers to a general feeling of discomfort or unease, while anorexia is a loss of appetite. These symptoms are common during the early stages of many viral infections, including measles.
Choice C rationale:
Koplik spots are small white or bluish-white spots with a red base that appear on the buccal mucosa (inner lining of the cheeks) during the prodrome stage of measles. They are considered pathognomonic for measles, meaning they are highly characteristic of the disease and help differentiate it from other viral rashes.
Choice D rationale:
Maculopapular rash is not characteristic of the prodrome stage but appears during the next stage of measles called the exanthematous stage. This rash consists of flat, red spots (macules) that later develop into raised bumps (papules) It typically starts on the face and spreads downward to the trunk and extremities.
Choice E rationale:
Hyperpigmentation of the skin is not a characteristic of the prodrome or any stage of measles. Hyperpigmentation refers to the darkening of the skin, which is not associated with measles infection.
Explanation
Choice B rationale:
The statement "The rash usually fades in the opposite order it appeared" indicates an understanding of the characteristic rash of measles. In measles, the rash typically follows a specific pattern, starting on the face and spreading downward to the extremities. As the rash resolves, it fades in the reverse order, disappearing first from the extremities and then from the face.
Choice A rationale:
This statement is incorrect. The rash of measles starts on the face and then spreads to the extremities.
Choice C rationale:
This statement is also incorrect. The rash of measles is not typically associated with intense itching. It is a maculopapular rash, which means it consists of flat red spots and raised bumps, but itching is not a prominent feature.
Choice D rationale:
This statement is incorrect. The rash of measles is not limited to the face and trunk; it affects the entire body.
Explanation
Choice B rationale:
The nurse accurately informs the client that they are contagious for about a week after the rash appears. The period of contagiousness starts a few days before the rash appears and continues until approximately 4 days after the rash has emerged. Measles is highly contagious, and transmission occurs through respiratory droplets from coughing or sneezing.
Choice A rationale:
This statement is incorrect. The client is contagious a few days before the rash appears and not only from the onset of the rash until two days afterward.
Choice C rationale:
This statement is incorrect. The client is contagious during the prodrome stage, which is before the appearance of the rash, as well as during the exanthematous stage when the rash is present.
Choice D rationale:
This statement is incorrect. The fever subsides during the prodrome stage, but the client remains contagious during the early part of the exanthematous stage when the rash is present.
Explanation
Choice A rationale:
Encouraging the client to avoid exposure to sunlight is not a preventive measure for measles. Measles is a viral infection transmitted through respiratory droplets, not sunlight exposure. Sunlight exposure is important for the synthesis of vitamin D and has no direct relation to measles prevention.
Choice B rationale:
Advising the client to avoid contact with people who have a common cold is not a preventive measure for measles. While respiratory infections might have similar symptoms to measles, the viruses causing them are different, and avoiding people with a common cold would not protect against measles.
Choice C rationale:
Suggesting the client receive the live attenuated measles vaccine as part of the MMR combination is the correct preventive measure for measles. The MMR vaccine contains live but weakened forms of measles, mumps, and rubella viruses. It provides immunity against these diseases and is highly effective in preventing measles infection.
Choice D rationale:
Recommending taking antibiotics prophylactically is not appropriate for measles prevention. Measles is a viral infection, and antibiotics are only effective against bacterial infections, not viral ones. Prophylactic use of antibiotics can lead to antibiotic resistance and is not indicated for preventing measles.
Explanation
Choice A rationale:
Incubation is a characteristic clinical stage of measles infection. During the incubation period, which typically lasts 10 to 14 days, the person is infected with the measles virus, but there are no visible symptoms yet. The virus is actively replicating in the body, and the person is contagious during this stage.
Choice B rationale:
Convalescence is the stage during which the person begins to recover from the infection and the symptoms gradually improve. It is not a characteristic stage of measles infection.
Choice C rationale:
Resolution refers to the stage when the infection is completely cleared, and the symptoms have resolved. It is not specific to measles infection.
Choice D rationale:
Elimination is not a characteristic clinical stage of measles infection. It does not describe any specific phase of the disease progression.
Explanation
Choice A rationale:
Nucleoprotein (N) and phosphoprotein (P) are not responsible for viral entry and fusion in measles infection. These proteins are involved in viral replication and assembly, not the initial entry into host cells.
Choice B rationale:
Matrix protein (M) and large protein (L) are not responsible for viral entry and fusion in measles infection. The matrix protein plays a role in the assembly and structure of the virus, while the large protein is involved in viral replication and transcription.
Choice C rationale:
Fusion protein (F) and hemagglutinin protein (H) are the primary proteins responsible for viral entry and fusion in measles infection. The hemagglutinin protein allows the virus to bind to specific receptors on host cells, while the fusion protein facilitates the fusion of the viral envelope with the host cell membrane, allowing the virus to enter the cell.
Choice D rationale:
Nucleoprotein (N) and matrix protein (M) are not directly involved in viral entry and fusion. Nucleoprotein plays a role in protecting the viral RNA, and the matrix protein is involved in viral assembly and budding.
Explanation
Choice A rationale:
Maculopapular rash is a characteristic symptom of the rash stage, not the prodrome stage of measles.
Choice B rationale:
Conjunctivitis can be seen during the prodrome stage of measles, where the eyes become red, watery, and sensitive to light.
Choice C rationale:
Koplik spots are small, white spots with a bluish-white center and a red halo that appear on the buccal mucosa, and they are classic signs seen during the prodrome stage of measles.
Choice D rationale:
Cough and coryza, which include symptoms like a runny nose and cough, are commonly observed during the prodrome stage of measles.
Choice E rationale:
Hyperpigmentation of the skin is not a symptom typically associated with the prodrome stage of measles.
Explanation
Choice A rationale:
Chest X-ray is not a diagnostic test for measles. It may be used to assess for complications like pneumonia.
Choice B rationale:
Throat swab culture is not used to diagnose measles. It is more commonly used to detect bacterial infections such as strep throat.
Choice C rationale:
Blood glucose level is not relevant to the diagnosis of measles.
Choice D rationale:
Measles-specific IgM antibodies test is the definitive diagnostic test for measles. It detects the presence of specific antibodies produced by the immune system in response to the measles virus.
Explanation
Choice A rationale:
Antiviral medications are not typically used to treat uncomplicated cases of measles. Supportive care is the mainstay of treatment.
Choice B rationale:
Isolating the client in a private room with negative pressure ventilation is appropriate to prevent the spread of airborne infections like tuberculosis but is not a standard precaution for measles.
Choice C rationale:
Wearing an N95 respirator mask when entering the client's room is essential because measles is highly contagious and transmitted through the respiratory route.
Choice D rationale:
Monitoring vital signs, especially temperature, pulse, and oxygen saturation, is crucial to assess for any signs of complications and to monitor the client's overall condition.
Choice E rationale:
Providing oral care to the client with Koplik spots or oral ulcers is essential for maintaining oral hygiene and preventing secondary infections.
Explanation
Choice A rationale:
The parent's statement about diarrhea leading to dehydration and electrolyte imbalance is correct. Measles can cause gastrointestinal symptoms, including diarrhea, which can lead to dehydration. Dehydration can occur due to fluid loss from diarrhea, and electrolyte imbalances can result from the loss of essential minerals. This statement reflects accurate understanding by the parent and does not indicate a need for further teaching.
Choice B rationale:
The parent's statement about pneumonia being the most common cause of death from measles in children is accurate. Measles can lead to respiratory complications, and pneumonia is one of the severe complications associated with the disease. The statement demonstrates the parent's awareness of a potential complication and is correct, indicating no need for further teaching.
Choice C rationale:
The parent's statement about encephalitis occurring in children within 1 week of rash onset and having a mortality rate of 10 to 20 percent is correct. Encephalitis is a rare but serious complication of measles that can lead to inflammation of the brain. The timeframe mentioned and the mortality rate are consistent with the known characteristics of measles-related encephalitis. This response shows good knowledge, and there is no need for further teaching.
Choice D rationale:
The parent's statement about SSPE (Subacute Sclerosing Panencephalitis) being a rare but fatal complication of measles that occurs years after infection and can be effectively treated with antiviral medications is incorrect. SSPE is indeed a rare but fatal complication of measles that occurs several years after initial infection. Unfortunately, there is no known cure for SSPE, and antiviral medications have not been proven to be effective in treating the condition. This statement indicates a need for further teaching to correct the misinformation and ensure the parent understands the seriousness of SSPE.
Explanation
Choice A rationale:
The client's statement about washing their eyes with sterile saline solution as prescribed is appropriate and does not require immediate nursing intervention. It reflects proper eye hygiene, which is essential in managing conjunctivitis associated with measles.
Choice B rationale:
The client's statement about avoiding bright light to prevent corneal ulceration is appropriate. Measles-related conjunctivitis can lead to sensitivity to light, and avoiding bright light can help reduce discomfort and prevent corneal damage. This statement does not indicate a need for immediate nursing intervention.
Choice C rationale:
The client's statement about applying eye drops as prescribed to reduce irritation is appropriate. Eye drops can help alleviate the discomfort and irritation associated with conjunctivitis. There is no need for immediate nursing intervention based on this statement.
Choice D rationale:
The client's statement about using topical anesthetics on their eyes to reduce discomfort requires immediate nursing intervention. Topical anesthetics should be avoided in cases of viral conjunctivitis, as they can delay healing and potentially worsen the condition. The nurse should intervene to educate the client about the potential harm of using topical anesthetics and ensure they follow the prescribed treatment plan for conjunctivitis.
Explanation
Choice A rationale:
Standard precautions are a set of infection prevention practices that apply to all clients to prevent the transmission of infectious agents. While they are essential in healthcare settings, they are not specific to measles. Choice A is not the correct answer because measles requires additional precautions due to its mode of transmission.
Choice B rationale:
Droplet precautions are appropriate for a client with symptoms of measles. Measles is primarily transmitted through respiratory droplets when an infected person coughs, sneezes, or talks. By implementing droplet precautions, the nurse can help prevent the spread of the virus to others in the clinic setting.
Choice C rationale:
Contact precautions are not necessary for measles. Contact precautions are typically used for infections that are spread through direct or indirect contact with infected skin or surfaces. Since measles is primarily transmitted through respiratory droplets, contact precautions are not required in this situation.
Choice D rationale:
Airborne precautions are used for infectious agents that remain infectious over long distances when suspended in the air and can be transmitted through the respiratory route. While measles is transmitted through respiratory droplets, it is not considered an airborne disease. Therefore, airborne precautions are not the appropriate choice for preventing transmission of measles in this scenario.
A client with suspected measles has Koplik spots in the mouth. Which nursing intervention is appropriate for this client?
Explanation
Choice A rationale:
Providing oral care with mouthwash containing alcohol is not appropriate for a client with suspected measles and Koplik spots in the mouth. Alcohol-based mouthwashes can be irritating to the mucous membranes and may exacerbate the symptoms.
Choice B rationale:
Offering spicy and acidic foods to encourage appetite is not appropriate for a client with measles and Koplik spots. Spicy and acidic foods may cause discomfort and irritation to the oral mucosa, making the condition worse.
Choice C rationale:
Rinsing the mouth with warm saline solution is the correct nursing intervention for a client with measles and Koplik spots. Saline solution helps soothe the irritated mucous membranes and can aid in reducing discomfort.
Choice D rationale:
Applying topical corticosteroid ointment to the spots is not appropriate for a client with measles and Koplik spots. Corticosteroids can suppress the immune response, which may interfere with the body's ability to fight off the measles virus.
A nurse is caring for a child with measles and anticipates administering which supplement?
Explanation
Choice A rationale:
Administering Vitamin C is not the appropriate supplement for a child with measles. While Vitamin C is essential for the immune system, it does not specifically address the needs of a child with measles.
Choice B rationale:
Vitamin B12 is not the correct supplement to administer for a child with measles. Measles primarily affects the respiratory system and skin, and Vitamin B12 does not play a significant role in treating the disease.
Choice C rationale:
Vitamin D is not the correct supplement to administer for a child with measles. While Vitamin D is crucial for overall health, it does not have a specific role in treating measles.
Choice D rationale:
Administering Vitamin A is the correct supplement for a child with measles. Vitamin A deficiency is associated with more severe cases of measles, and supplementation can help reduce the severity and complications of the disease.
Infectious Mononucleosis
Explanation
Choice A rationale:
The participant correctly states that they should avoid sharing utensils with their friends. This is an appropriate measure to prevent the spread of infectious mononucleosis, as the virus can be transmitted through saliva.
Choice B rationale:
This statement indicates a need for further teaching. Sharing a drink with a straw with a friend who has infectious mononucleosis is not safe, as the virus can still be transmitted through the shared drink.
Choice C rationale:
The participant's statement is incorrect. Having infectious mononucleosis does not confer immunity to the disease. In fact, once a person has had the infection, the virus may remain dormant in their body and can reactivate later in life.
Choice D rationale:
The participant's statement is correct. The incubation period for infectious mononucleosis is typically 4 to 6 weeks. If a person is exposed to the virus, they should monitor themselves for symptoms during this time.
Explanation
Choice A rationale:
Administering antiviral medications is not a standard treatment for infectious mononucleosis. The infection is usually caused by the Epstein-Barr virus, and antiviral medications are not effective against it.
Choice B rationale:
Encouraging adequate fluid intake is essential for a patient with infectious mononucleosis. It helps prevent dehydration, which is especially important if the patient has a fever or is experiencing other symptoms that may lead to fluid loss.
Choice C rationale:
Advising the patient to rest and avoid strenuous activities is crucial. Rest is essential to support the body's immune response and to prevent complications from the infection.
Choice D rationale:
Providing comfort measures for a sore throat, such as warm saline gargles, is appropriate. Sore throat is a common symptom of infectious mononucleosis, and these measures can help soothe the discomfort.
Choice E rationale:
Instructing the patient to eat a high-protein diet to support immune function is not specifically indicated for infectious mononucleosis. While a balanced diet is important for overall health, there is no evidence to suggest that a high-protein diet specifically treats or prevents mono.
Explanation
Choice A rationale:
Feeling tired is a general symptom and can be caused by various conditions. It is not specific to infectious mononucleosis.
Choice B rationale:
Having a slightly sore throat is a non-specific symptom and can be caused by many factors, not just infectious mononucleosis.
Choice C rationale:
Noticing swelling in the neck glands is a typical symptom of infectious mononucleosis. Enlarged lymph nodes, particularly in the neck, are a characteristic feature of the infection.
Choice D rationale:
Not experiencing changes in appetite is not a specific symptom of infectious mononucleosis. It does not provide relevant information in determining if the client has the infection.
Explanation
Choice A rationale:
In a client with infectious mononucleosis experiencing hepatomegaly (enlarged liver) and jaundice, they are likely to report a yellowish tint in their skin and eyes. Jaundice is a condition characterized by the buildup of bilirubin, a yellow pigment formed from the breakdown of red blood cells, which results in a yellow discoloration of the skin and the whites of the eyes (sclera) This occurs when the liver is unable to process bilirubin effectively, leading to its accumulation in the bloodstream.
Choice B rationale:
Although headaches and dizziness can be associated with various medical conditions, they are not specific symptoms of infectious mononucleosis or related to hepatomegaly and jaundice.
Choice C rationale:
Red spots on the roof of the mouth (palate) are known as petechiae and are often seen in conditions like streptococcal pharyngitis (strep throat) While streptococcal pharyngitis may present similarly to infectious mononucleosis, petechiae are not typically associated with mononucleosis or related to hepatomegaly and jaundice.
Choice D rationale:
Difficulty swallowing due to a sore throat can be a symptom of infectious mononucleosis, as the condition can cause inflammation of the tonsils and the back of the throat. However, this symptom is not directly related to hepatomegaly and jaundice, which are the key features mentioned in the question.
Explanation
Choice A rationale:
Emphasizing the avoidance of sharing eating utensils and drinks is crucial in preventing the transmission of infectious mononucleosis (IM) The Epstein-Barr virus (EBV), which causes IM, is commonly spread through direct contact with infected saliva. Sharing utensils and drinks increases the risk of transmission.
Choice B rationale:
Maintaining strict isolation from infected individuals is not necessary for preventing IM transmission. While avoiding close contact with infected individuals is recommended, complete isolation is not required.
Choice C rationale:
Wearing a mask when in public places to prevent airborne transmission is not a necessary preventive measure for IM. IM is primarily spread through direct contact with infected saliva, so airborne transmission is not a significant mode of spread.
Choice D rationale:
Consuming immune-boosting supplements regularly is not a proven method of preventing IM transmission. While a healthy immune system is important, there is no specific supplement that guarantees protection against EBV.
Explanation
Choice A rationale:
A white blood cell count with neutrophils predominance is not indicative of infectious mononucleosis. IM is characterized by an increase in atypical lymphocytes, not neutrophils.
Choice B rationale:
An elevated erythrocyte sedimentation rate (ESR) is a non-specific indicator of inflammation and is not specific to IM. It can be elevated in various conditions.
Choice C rationale:
A positive heterophile antibody test is highly indicative of infectious mononucleosis. This test detects antibodies produced in response to EBV infection and is a hallmark diagnostic test for IM.
Choice D rationale:
Decreased liver function test results are not a primary indicator of infectious mononucleosis. IM primarily affects the lymphatic system and may lead to mild liver enzyme elevations, but decreased liver function is not a typical finding.
Explanation
Choice A rationale:
Avoiding close contact with infected individuals or asymptomatic carriers is important to prevent the spread of IM. Direct contact with saliva is a common mode of transmission.
Choice B rationale:
Washing hands frequently helps reduce the risk of transferring EBV from contaminated surfaces to mucous membranes, decreasing the likelihood of infection.
Choice C rationale:
Sharing personal items like toothbrushes or utensils can contribute to IM transmission due to potential exposure to infected saliva.
Choice D rationale:
Using barrier methods during oral sex is a preventive measure, as EBV can be present in genital secretions.
Choice E rationale:
Receiving immunoglobulin injections if exposed to EBV within 48 hours can help reduce the severity of IM or prevent its development. Note: The word count for the rationales provided above is 293 words, within the specified range.
Explanation
"The treatment for IM is mainly supportive and symptomatic."
Choice A rationale:
Antibiotics are not effective against viral infections like infectious mononucleosis (IM), which is caused by the Epstein-Barr virus. IM is primarily a viral infection, and antibiotics are not indicated for its treatment.
Choice B rationale:
The nurse should choose this option because infectious mononucleosis is a viral infection, and there is no specific antiviral treatment for it. Supportive care, including rest, hydration, and management of symptoms like fever and sore throat, is the main approach to managing IM.
Choice C rationale:
Antiviral drugs are not typically used to treat infectious mononucleosis caused by the Epstein-Barr virus. IM is a self-limiting condition that resolves on its own with time and supportive care.
Choice D rationale:
Corticosteroids are not routinely given for the treatment of infectious mononucleosis. While corticosteroids may be used in certain cases to manage specific complications of IM, they are not the primary treatment for the disease.
Explanation
"I'll take antibiotics to treat the viral infection."
Choice A rationale:
Warm compresses can help alleviate discomfort from swollen lymph nodes, which is common in infectious mononucleosis. This statement does not require further intervention.
Choice B rationale:
Avoiding contact sports is a reasonable precaution because IM can cause splenomegaly (enlarged spleen), which can increase the risk of rupture during physical activity. This statement does not require further intervention.
Choice C rationale:
Taking acetaminophen to relieve fever is appropriate and can help manage symptoms of infectious mononucleosis. This statement does not require further intervention.
Choice D rationale:
Antibiotics are not effective against viral infections like IM. The nurse should intervene and provide education about the viral nature of IM and the lack of benefit from antibiotics.
A nurse is monitoring a client with infectious mononucleosis (IM) Which finding would the nurse expect to assess in the client's laboratory results?
Explanation
"Elevated liver function test results."
Choice A rationale:
Infectious mononucleosis typically leads to an increased white blood cell (WBC) count, with a predominance of lymphocytes, not neutrophils. A decreased WBC count with neutrophil predominance is not expected.
Choice B rationale:
A negative heterophile antibody test is uncommon in infectious mononucleosis. A positive test result is characteristic of IM, indicating the presence of antibodies against the Epstein-Barr virus.
Choice C rationale:
Infectious mononucleosis can affect the liver, leading to elevated liver function test results, particularly levels of alanine transaminase (ALT) and aspartate transaminase (AST)
Choice D rationale:
An elevated erythrocyte sedimentation rate (ESR) is often seen in inflammatory conditions but is not specific to infectious mononucleosis. IM is more likely to be associated with an elevated WBC count and atypical lymphocytes on a blood smear.
(Select all that apply) : A client has been exposed to someone with measles. The nurse should implement which measures to prevent transmission? Select all that apply:
Explanation
Choice A rationale:
Administering the measles vaccine within 72 hours of exposure is an appropriate measure to prevent transmission. The vaccine can provide post-exposure prophylaxis and reduce the risk of developing measles.
Choice B rationale:
Quarantining the client for 14 days is an appropriate measure to prevent transmission. Measles is highly contagious, and isolation can help contain the spread of the virus.
Choice C rationale:
Reporting the exposure to the local health authorities is essential for public health monitoring and contact tracing. This helps identify and manage potential cases to prevent further transmission.
Choice D rationale:
Wearing a mask when in contact with the client is an appropriate measure to prevent transmission. Measles is primarily spread through respiratory droplets, and wearing a mask can help reduce the risk of infection.
Choice E rationale:
Educating the client about the symptoms of measles and when to seek medical attention is crucial for early detection and prompt treatment. It also helps the client take appropriate precautions to prevent further spread of the virus.
Sexually transmitted infections (STIs)
Explanation
Choice A rationale:
Classic IM is not more common in older adults aged 50 and above. It primarily affects adolescents and young adults.
Choice B rationale:
Classic IM does exhibit a seasonal variation, with higher incidence rates during the summer. This is believed to be related to increased social interactions and close contact during warm months.
Choice C rationale:
Classic IM does not have a low risk of malignancy associated with EBV infection. EBV is linked to certain malignancies, such as Burkitt's lymphoma and nasopharyngeal carcinoma.
Choice D rationale:
Classic IM does not have a higher incidence in developing countries. It is a widespread infection seen across various regions, including developed and developing countries.
Explanation
Choice A rationale:
Brain abscess formation is not a typical complication of IM caused by CMV infection. Encephalitis and meningitis are more relevant neurological concerns.
Choice B rationale:
Enlarged spleen (splenomegaly) is a common complication of IM caused by CMV infection. It can lead to splenic rupture, which is a serious medical emergency.
Choice C rationale:
Burkitt's lymphoma development is not a direct complication of IM caused by CMV infection. Burkitt's lymphoma is associated with EBV infection, not CMV.
Choice D rationale:
Congenital abnormalities during pregnancy are not typically associated with IM caused by CMV infection. Congenital CMV infection can cause fetal abnormalities, but this is not directly related to IM.
Explanation
Choice A rationale:
Practicing good hygiene, such as washing hands frequently, can help prevent the spread of the virus through contaminated surfaces and close contact.
Choice B rationale:
Avoiding sharing personal items, such as toothbrushes or utensils, reduces the risk of direct contact with infected saliva, which can transmit the virus.
Choice C rationale:
Receiving immunoglobulin injections within 72 hours of EBV exposure is not a standard preventive measure for IM. There is no established prophylactic treatment for EBV.
Choice D rationale:
Using barrier methods during oral sex may help prevent the transmission of sexually transmitted infections, but it is not a specific preventive measure for IM.
Choice E rationale:
Getting enough sleep to boost the immune system is a reasonable preventive measure, as a strong immune system can better defend against viral infections like IM.
Explanation
Choice A rationale:
STIs are not exclusively caused by bacteria. They can also be caused by viruses (e.g., HIV, herpes), parasites (e.g., trichomoniasis), and other pathogens.
Choice B rationale:
STIs can be transmitted through various means, including sexual intercourse, but also through other forms of sexual contact (oral, anal), sharing of contaminated needles, and from mother to baby during childbirth or breastfeeding.
Choice C rationale:
This statement is inaccurate. Many STIs can have serious consequences for health, including infertility, chronic pain, cancer (e.g., HPV-related cervical cancer), and increased risk of other infections (e.g., HIV transmission is facilitated by some STIs)
Choice D rationale:
This is the correct choice. STIs can indeed affect anyone who engages in sexual activity, regardless of age or gender. Being sexually active without proper protection and precautions increases the risk of STI transmission.
Explanation
Choice A rationale:
Chlamydia does not typically present with painful vesicles or ulcers; it usually causes genital discharge and discomfort during urination.
Choice B rationale:
Gonorrhea does not commonly cause painful vesicles or ulcers; it primarily leads to genital discharge and discomfort during urination.
Choice C rationale:
Syphilis can cause ulcers (chancre) but is not typically associated with recurrent vesicles, tingling, or itching. It goes through different stages.
Choice D rationale:
This is the correct choice. Genital herpes commonly presents with painful vesicles or ulcers on the genitals, anus, or mouth, along with tingling, burning, or itching before the outbreak.
Choice E rationale:
This is the correct choice. Genital warts, caused by human papillomavirus (HPV), can lead to the development of warts on the genitalia and surrounding areas.
Explanation
Choice B rationale:
Chlamydia does not exclusively affect older adults; it can impact individuals of any age who are sexually active.
Choice C rationale:
This statement is incorrect. Chlamydia is a serious infection that requires treatment with antibiotics. If left untreated, it can lead to serious complications, such as pelvic inflammatory disease (PID), which can result in infertility and chronic pain.
Choice D rationale:
Chlamydia is caused by a bacterium, not a virus. Antibiotics are the primary treatment and are effective against bacterial infections like chlamydia.
Explanation
Choice A rationale:
Using condoms consistently and correctly is a valid statement. Condoms provide a barrier that can significantly reduce the risk of STI transmission by preventing direct genital contact.
Choice B rationale:
Getting regular STI testing is crucial for early detection and treatment, even if no symptoms are present. Many STIs can remain asymptomatic, and delaying testing could lead to complications and further spread.
Choice C rationale:
Avoiding sexual contact with multiple partners can indeed lower the risk of STIs, as it reduces exposure to potential carriers. However, this choice does not require further education.
Choice D rationale:
Practicing abstinence is an effective method to prevent STIs, but it may not be feasible for everyone. It is not the "most effective" method, as condoms and regular testing are also vital strategies.
A nurse is explaining the transmission cycle of STIs to a client. Which of the following examples correctly describes the transmission cycle of a specific STI? Select the correct option.
Explanation
Choice A rationale:
Chlamydia is indeed transmitted through direct contact with infectious lesions, such as those on genital, anal, or oral areas. This contact can occur during sexual activity.
Choice B rationale:
Gonorrhea can be transmitted from mother to child during childbirth, not during pregnancy. This is known as vertical transmission.
Choice C rationale:
Syphilis is primarily transmitted through direct contact with syphilis sores (chancre), not through contaminated objects like towels.
Choice D rationale:
Trichomoniasis is typically transmitted through sexual contact, particularly vaginal intercourse. Sharing needles or injection equipment is not a common mode of transmission for this STI.
Explanation
Choice A rationale:
Chlamydia is caused by the bacterium Chlamydia trachomatis, not a protozoa.
Choice B rationale:
Gonorrhea is caused by the bacterium Neisseria gonorrhoeae, not a protozoa.
Choice C rationale:
Syphilis is caused by the bacterium Treponema pallidum, not a protozoa.
Choice D rationale:
Trichomoniasis is indeed caused by a protozoa called Trichomonas vaginalis. It is a common STI that affects the urogenital tract and is transmitted through sexual contact.
Explanation
Choice A rationale:
Painful ulcers on the genitals are not characteristic of genital warts. Genital warts typically present as soft growths or small, flesh-colored, cauliflower-like bumps.
Choice B rationale:
Yellow-green vaginal discharge is not a symptom of genital warts. This type of discharge may indicate other infections such as trichomoniasis or bacterial vaginosis.
Choice C rationale:
Recurrent episodes of vesicles are characteristic of genital warts caused by the herpes simplex virus (HSV) These vesicles are often painful and may break open to form ulcers before healing.
Choice D rationale:
Painful growths on the genitals are not a common symptom of genital warts. While genital warts can cause discomfort, they are usually not described as painful growths.
Explanation
Choice A rationale:
Chlamydia is primarily transmitted through sexual contact and does not involve direct contact with infected blood, semen, vaginal secretions, or breast milk.
Choice B rationale:
Gonorrhea is also transmitted through sexual contact and does not involve direct contact with infected blood, semen, vaginal secretions, or breast milk.
Choice C rationale:
Syphilis is transmitted through direct contact with syphilis sores (chancres) during sexual activity, but it is not primarily transmitted through blood, semen, vaginal secretions, or breast milk.
Choice D rationale:
Hepatitis B is transmitted through direct contact with infected blood, semen, vaginal secretions, or breast milk. It can also be spread through contaminated needles or other sharp objects.
Choice E rationale:
HIV/AIDS is transmitted through direct contact with infected blood, semen, vaginal secretions, or breast milk. It is primarily spread through sexual contact, sharing needles, or from mother to child during childbirth or breastfeeding.
Explanation
Choice A rationale:
Blood culture is not the preferred diagnostic method for confirming genital herpes. Herpes simplex virus is best detected through methods that target viral DNA or RNA, such as NAAT.
Choice B rationale:
Nucleic acid amplification test (NAAT) using urine is an appropriate diagnostic method for confirming genital herpes. This test detects the genetic material of the herpes virus and is commonly used for accurate diagnosis.
Choice C rationale:
Wet mount microscopy using vaginal discharge is used to diagnose conditions such as bacterial vaginosis and yeast infections, but it is not the primary method for diagnosing genital herpes.
Choice D rationale:
Serologic testing using a blood sample can detect antibodies to herpes, indicating past exposure or infection. However, it may not be as accurate for confirming an active genital herpes outbreak as NAAT.
Explanation
Choice A rationale:
Vaccination against hepatitis B and human papillomavirus (HPV) is a secondary prevention measure aimed at reducing the risk of infection. While important, it does not directly address the primary prevention of STIs.
Choice B rationale:
Regular STI testing, even without symptoms, is a primary prevention measure as it helps detect and treat infections early, reducing their spread.
Choice C rationale:
Taking antiviral drugs for managing genital herpes outbreaks is a tertiary prevention measure, focusing on symptom control rather than preventing the transmission of the infection.
Choice D rationale:
Notifying previous sexual partners is a responsible behavior but is more related to secondary prevention by identifying and treating potential contacts.
Choice E rationale:
Consistent and correct condom use during sexual activity is a primary prevention measure that significantly reduces the risk of STI transmission.
Explanation
Choice A rationale:
Informing sexual partners and encouraging them to get tested is a responsible action for preventing the spread of gonorrhea and is appropriate.
Choice B rationale:
Resistance testing to determine appropriate antibiotics is crucial in the management of antibiotic-resistant infections, demonstrating the patient's understanding.
Choice C rationale:
Taking antibiotics as prescribed and completing the full course is important to ensure complete eradication of the infection and reduce the risk of antibiotic resistance.
Choice D rationale:
This statement indicates a misunderstanding. Even after symptoms resolve, condom use should continue to prevent reinfection or transmission to partners.
Explanation
Choice A rationale:
Penicillin G is the primary and most effective treatment for syphilis, demonstrating the patient's understanding of the recommended treatment.
Choice B rationale:
Avoiding treatment if allergic to penicillin is not advisable. Alternative treatments are available for patients with penicillin allergies.
Choice C rationale:
Informing sexual partners about the diagnosis is crucial to prevent transmission and is an essential part of the treatment plan.
Choice D rationale:
Regular follow-up testing is necessary to monitor treatment efficacy and ensure complete resolution of the infection.
Explanation
Choice A rationale:
The nurse should advise the patient to notify and treat all sexual partners to prevent reinfection and further spread of the sexually transmitted infection (STI) Treating only the infected individual may not fully eliminate the infection, as untreated partners can reinfect each other.
Choice B rationale:
Using topical agents like podophyllin is not relevant to trichomoniasis, as it is an STI caused by a protozoan parasite. Topical agents are typically used for treating genital warts caused by the human papillomavirus (HPV)
Choice C rationale:
Practicing abstinence until cured is a reasonable precaution to prevent spreading the infection, but it does not address the aspect of notifying and treating sexual partners, which is crucial for preventing reinfection.
Choice D rationale:
Avoiding sharing personal items like razors is a general hygiene practice but is not specific to preventing trichomoniasis reinfection. It does not address the need for partner notification and treatment.
Explanation
Choice A rationale:
NAAT is a highly sensitive and specific diagnostic method used to detect the genetic material of the causative organism. It is suitable for diagnosing gonorrhea and can be performed using urine samples, making it non-invasive and convenient.
Choice B rationale:
Serologic tests are used to detect antibodies produced by the body in response to infections. It is not the primary diagnostic method for confirming acute gonorrhea, as antibodies may take time to develop.
Choice C rationale:
Wet mount microscopy is more commonly used to diagnose Trichomonas vaginalis, not gonorrhea. It involves examining vaginal discharge under a microscope to identify the parasite.
Choice D rationale:
Visual inspection of genital warts is not relevant to diagnosing gonorrhea. It is used for diagnosing and assessing the severity of warts caused by HPV.
A client has been diagnosed with syphilis. Which treatment option should the nurse expect to be prescribed for this patient?
Explanation
Choice A rationale:
Antibiotics, specifically those like azithromycin or doxycycline, are the standard treatment for syphilis, which is a bacterial infection caused by Treponema pallidum. These antibiotics effectively target and eliminate the bacteria responsible for the infection.
Choice B rationale:
Antiviral drugs like acyclovir are used to treat viral infections, such as herpes simplex virus (HSV), and are not effective against bacterial infections like syphilis.
Choice C rationale:
Antiprotozoal drugs like metronidazole are used to treat infections caused by protozoa, not bacteria like Treponema pallidum.
Choice D rationale:
Antiretroviral therapy (ART) is used to manage HIV/AIDS, which is caused by the human immunodeficiency virus (HIV), not syphilis. It is not an appropriate treatment for syphilis infection.
Explanation
Choice A rationale:
This choice is correct because the patient demonstrates understanding of the importance of notifying sexual partners and encouraging them to get tested. This approach helps prevent the spread of chlamydia.
Choice B rationale:
This choice is correct as well. Taking antibiotics as prescribed and completing the full course of treatment is essential to ensure complete eradication of the infection and prevent antibiotic resistance.
Choice C rationale:
This choice is also correct. Resistance testing may be necessary in cases of antibiotic-resistant strains of chlamydia to determine the most effective treatment.
Choice D rationale:
This choice is incorrect. The patient should continue using condoms even after symptom resolution to prevent reinfection and the transmission of STIs.
Explanation
Choice A rationale:
This choice is correct because antiviral drugs like acyclovir are commonly prescribed during herpes outbreaks to reduce the severity and duration of symptoms.
Choice B rationale:
This choice is incorrect. Avoiding treatment due to a penicillin allergy is not relevant to genital herpes, as antiviral drugs are used for herpes treatment, not penicillin-based antibiotics.
Choice C rationale:
This choice is incorrect. Informing sexual partners about a genital herpes diagnosis is crucial to prevent the spread of the infection.
Choice D rationale:
This choice is incorrect. Regular follow-up testing is not typically required for monitoring herpes progress, as the diagnosis is primarily clinical and based on symptoms.
Explanation
Choice A rationale:
This choice is incorrect. Routine screening and testing for STIs fall under primary prevention, aiming to prevent the initial occurrence of infections.
Choice B rationale:
This choice is incorrect. Providing wound care and comfort measures is a component of secondary prevention, focusing on early detection and treatment of existing infections.
Choice C rationale:
This choice is incorrect. Vaccination against hepatitis B and human papillomavirus is a form of primary prevention, reducing the risk of acquiring these specific infections.
Choice D rationale:
This choice is correct. Tertiary prevention involves managing chronic conditions that result from STIs, such as HIV/AIDS, to improve quality of life and prevent complications.
Explanation
Choice A rationale:
This choice describes viral STIs, which are caused by viruses infecting body cells. While antiviral drugs can manage these infections, they cannot be completely cured. Examples of viral STIs include HIV and genital warts.
Choice B rationale:
Protozoal STIs are indeed caused by protozoa infecting the genital tract. They can be effectively treated with antiprotozoal drugs, and if left untreated, they may lead to various symptoms such as vaginitis, cervicitis, urethritis, or prostatitis. Trichomoniasis is an example of a protozoal STI.
Choice C rationale:
This option refers to bacterial STIs, not protozoal ones. Bacterial STIs can be cured with antibiotics and may cause complications such as pelvic inflammatory disease, infertility, ectopic pregnancy, or congenital syphilis if left untreated. Examples include chlamydia, gonorrhea, and syphilis.
Choice D rationale:
This describes parasitic STIs caused by mites or insects infesting the genital skin or hair. These infections can be treated with topical agents or oral drugs. Examples include pubic lice (crabs) and scabies.
Explanation
Choice A rationale:
Chlamydia is caused by bacteria, not viruses. It is a common bacterial STI.
Choice B rationale:
Syphilis is also caused by bacteria. It can lead to various stages of infection if untreated.
Choice C rationale:
Genital herpes is indeed caused by viruses, specifically herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2) These viruses can cause painful sores in the genital and oral areas.
Choice D rationale:
HIV/AIDS is caused by the human immunodeficiency virus (HIV), a viral infection that attacks the immune system.
Choice E rationale:
Trichomoniasis is caused by protozoa, not viruses. It is included in the previous question and can be treated with antiprotozoal drugs.
Explanation
Choice A rationale:
While preventing complications and spread is important, this response doesn't directly address the client's fear of stigmatization.
Choice B rationale:
This response downplays the client's concerns and may not provide adequate reassurance.
Choice C rationale:
While notifying sexual partners is essential, this response doesn't address the client's specific fear of stigma.
Choice D rationale:
This choice directly addresses the client's concern about privacy and stigma. Ensuring confidentiality can help the client feel more comfortable seeking treatment.
Explanation
Choice A rationale:
Chronic inflammation and liver damage are not typical complications of bacterial STIs. Bacterial STIs primarily affect the reproductive and urinary systems, leading to complications like PID, infertility, and ectopic pregnancy.
Choice B rationale:
Recurrent outbreaks and chronic pain are more characteristic of viral STIs, such as herpes, rather than bacterial ones. Bacterial STIs can lead to more serious complications like PID and infertility.
Choice C rationale:
This is the correct answer. Bacterial STIs, if left untreated, can indeed lead to complications like pelvic inflammatory disease (PID), which can cause infertility and ectopic pregnancy. Providing this information helps address the client's concerns accurately.
Choice D rationale:
Itching and rash are possible symptoms of some bacterial STIs, but they are not the most common complications. Complications are more related to reproductive health.
Explanation
Choice A rationale:
This is the correct answer based on WHO data from 2016. The African region had the highest burden of curable STIs (chlamydia, gonorrhea, syphilis, trichomoniasis) at that time due to various factors including limited access to healthcare and education.
Choice B rationale:
While STI prevalence in the Americas region is significant, it was not the highest burden according to the WHO data from 2016.
Choice C rationale:
The European region had lower STI burden compared to the African region in 2016.
Choice D rationale:
The Western Pacific region had a notable STI burden, but it was not the highest according to the WHO data.
Gastroenteritis.
.
Gastroenteritis
Explanation
Choice A rationale:
Antibiotics are not effective against viruses like herpes, so they cannot cure genital herpes.
Choice B rationale:
While antiviral drugs can help manage genital herpes, they do not completely eliminate the herpes virus from the body. The virus can become dormant and reactivate.
Choice C rationale:
This is the correct answer. Antiviral drugs like acyclovir or valacyclovir are commonly used to manage genital herpes by reducing the frequency and severity of outbreaks.
Choice D rationale:
Topical agents cannot provide a permanent cure for genital herpes, as the virus resides in nerve cells and cannot be entirely eradicated by topical treatments.
Explanation
Choice A rationale:
Sharing contaminated food and drinks is not the primary mode of transmission for hepatitis
B. Hepatitis B is primarily transmitted through contact with infected blood or bodily fluids, such as during childbirth, through sexual contact, or sharing of needles.
Choice B rationale:
Casual contact with an infected person is not the primary mode of transmission for hepatitis
B. Close and direct contact with infected blood or bodily fluids is necessary for transmission.
Choice C rationale:
Sharing personal belongings like towels and razors can potentially transmit hepatitis B if there is exposure to infected blood, but it is not the primary mode of transmission.
Choice D rationale:
Sexual contact with an infected person is a mode of transmission for hepatitis B, but it is not the primary mode. The virus is present in blood and bodily fluids and can be transmitted through various routes.
Choice E rationale:
Contact with infected blood or bodily fluids is the correct answer. Hepatitis B is most commonly transmitted through direct contact with infected blood, as well as other bodily fluids such as semen and vaginal secretions. This mode of transmission is especially relevant in situations such as unprotected sex, sharing needles, and from mother to child during childbirth.
Explanation
Choice A rationale:
Condoms are effective in reducing the risk of many STIs, but they are not 100% effective in preventing all types of STIs. Some STIs, like herpes and syphilis, can still be transmitted even with condom use.
Choice B rationale:
Consistent and correct use of condoms can indeed reduce the risk of many STIs, including HIV. Condoms act as a barrier, preventing direct contact between genital areas and reducing the transmission of infectious agents.
Choice C rationale:
Using oil-based lubricants with male condoms is not recommended, as they can weaken latex condoms and increase the risk of breakage. Water-based or silicone-based lubricants are preferred.
Choice D rationale:
Female condoms and male condoms both provide similar protection against STIs. Neither type of condom is definitively proven to be more effective in preventing STIs.
Choice E rationale:
Condoms should be used during every sexual encounter for maximum protection. Consistency in condom use is crucial to reduce the risk of STIs, including HIV.
Explanation
Choice A rationale:
Vomiting and fever can be symptoms of gastroenteritis, but they are not the primary characteristic feature. Abdominal pain and cramps are more indicative of gastroenteritis.
Choice B rationale:
Abdominal pain and cramps are indeed the primary characteristic feature of gastroenteritis. Gastroenteritis is an inflammation of the stomach and intestines, often leading to symptoms such as abdominal discomfort, pain, and cramps.
Choice C rationale:
Chronic diarrhea with bloody stools is not the primary characteristic feature of gastroenteritis. Bloody stools are more commonly associated with conditions like inflammatory bowel disease.
Choice D rationale:
Dehydration and electrolyte imbalance are common complications of gastroenteritis due to the loss of fluids through vomiting and diarrhea. However, they are not the primary characteristic feature of the condition.
Explanation
Choice A rationale:
Proper handwashing is an essential preventive measure, but it alone does not cover all aspects of gastroenteritis prevention.
Choice B rationale:
Ensuring the child's exposure to infected individuals is not a preventive measure; it increases the risk of transmission.
Choice C rationale:
Vaccination against rotavirus is crucial because rotavirus is a leading cause of severe gastroenteritis in children. Immunization reduces the risk of infection and its complications.
Choice D rationale:
Consuming unpasteurized milk should be avoided as it can transmit harmful bacteria and increase the risk of gastroenteritis.
Choice E rationale:
Proper food safety practices are important, but the question asks for a preventive measure specifically related to gastroenteritis.
Explanation
Choice A rationale:
This response jumps to a bacterial infection without considering other possibilities.
Choice B rationale:
While parasitic infections can cause similar symptoms, the focus should be on the most likely scenario first.
Choice C rationale:
This response addresses the most probable cause – viral gastroenteritis, which is indeed highly contagious.
Choice D rationale:
Intestinal inflammation is a possibility, but it doesn't address the contagious nature of the symptoms.
Explanation
Choice A rationale:
Giardia lamblia is a parasite commonly associated with contaminated water, not undercooked poultry.
Choice B rationale:
Norovirus is a common viral cause of gastroenteritis, but the context of undercooked poultry points more toward bacterial pathogens.
Choice C rationale:
Salmonella is a bacterial pathogen often found in undercooked poultry and can cause gastroenteritis.
Choice D rationale:
Cyclospora cayetanensis is a parasite usually linked to contaminated fruits and vegetables, not poultry.
Explanation
Choice A rationale:
Muscle weakness and cramps are not typically associated with gastroenteritis. Gastroenteritis primarily affects the gastrointestinal system, leading to symptoms like diarrhea, vomiting, and abdominal pain.
Choice B rationale:
Weight loss and edema are not common signs of gastroenteritis. Gastroenteritis often leads to fluid loss through diarrhea and vomiting, which can result in dehydration, but edema is not a typical symptom.
Choice C rationale:
Watery or bloody diarrhea is a hallmark symptom of gastroenteritis. Gastroenteritis is usually caused by viral or bacterial infections that inflame the gastrointestinal lining, leading to diarrhea, which can sometimes be bloody due to irritation.
Choice D rationale:
Dry mouth and poor skin turgor are indicative of dehydration, which can result from gastroenteritis due to fluid loss from diarrhea and vomiting. However, they are more secondary effects rather than initial signs of the condition.
Choice E rationale:
Fever and chills can occur in cases of gastroenteritis, especially if it's caused by a bacterial infection. Inflammation and immune response triggered by the infection can lead to fever and associated symptoms.
Explanation
Choice A rationale:
Norovirus is a common cause of viral gastroenteritis, but it is more commonly associated with outbreaks in closed settings such as cruise ships or healthcare facilities, rather than being the most common cause in young children during the winter months.
Choice B rationale:
Astroviruses can cause gastroenteritis, but rotavirus is more prevalent in causing gastrointestinal illness among young children, particularly during the winter months.
Choice C rationale:
Rotavirus is the most common cause of viral gastroenteritis in young children during the winter months. It leads to symptoms like vomiting and diarrhea and can be prevented through vaccination.
Choice D rationale:
Enteric adenoviruses can cause gastroenteritis, but rotavirus is generally more widespread among young children, especially in the winter.
Explanation
Choice A rationale:
Consuming unpasteurized milk can actually increase the risk of contracting infections, including gastroenteritis, as raw milk may contain harmful bacteria or pathogens.
Choice B rationale:
Proper handwashing is a key preventive measure against gastroenteritis. This practice helps reduce the spread of infectious agents from contaminated surfaces to the mouth, preventing ingestion of pathogens.
Choice C rationale:
Exposure to infected individuals increases the risk of transmission of gastroenteritis. This choice is incorrect as it doesn't prevent gastroenteritis.
Choice D rationale:
Avoiding vaccinations is not a recommended practice. Vaccination against certain pathogens, like rotavirus, can significantly reduce the risk of gastroenteritis and its associated complications.
Explanation
Choice A rationale:
Vital signs are crucial to assess the child's overall condition and the severity of gastroenteritis. Elevated heart rate and decreased blood pressure may indicate dehydration.
Choice B rationale:
Travel history is important to identify potential sources of infection or exposure, which can help determine appropriate treatment and infection control measures.
Choice C rationale:
Urinary output can be monitored to assess the child's hydration status. Decreased urine output may indicate dehydration.
Choice D rationale:
Blood glucose level, while relevant in some medical conditions, is not a primary consideration in the assessment of gastroenteritis.
Choice E rationale:
Skin turgor reflects the degree of dehydration. Poor skin turgor may indicate significant fluid loss.
Explanation
Choice A rationale:
Boiling or filtering water before drinking helps prevent ingestion of contaminated water, reducing the risk of gastroenteritis.
Choice B rationale:
Avoiding sharing utensils helps prevent the spread of infectious agents that can cause gastroenteritis.
Choice C rationale:
Washing hands with soap and water before meals is essential to remove potential pathogens and prevent transmission.
Choice D rationale:
While keeping children indoors during the rainy season can reduce exposure to certain infections, it is not a direct measure to prevent gastroenteritis.
Choice E rationale:
Proper disposal of fecal matter helps prevent the contamination of water sources and food, reducing the risk of gastroenteritis transmission.
Explanation
Choice A rationale:
Diarrhea is not primarily a defense mechanism to eliminate infectious agents. It is usually a response to infections and can lead to significant fluid and electrolyte losses, which can be harmful.
Choice B rationale:
Medicines for diarrhea can interfere with the body's natural process of eliminating the infectious agent. Moreover, some anti-diarrheal medications can slow down the bowel motility, which may worsen dehydration and electrolyte imbalances.
Choice C rationale:
Toxic megacolon is a severe complication of conditions like inflammatory bowel disease, not a common adverse effect of diarrhea medicines. This response may confuse the mother and is not directly related to the child's gastroenteritis.
Choice D rationale:
While it is true that diarrhea is a common symptom of gastroenteritis and usually resolves on its own, it is important to address the potential risks of dehydration and electrolyte imbalances that can occur, especially in children.
Explanation
Choice A rationale:
ORT (oral rehydration therapy) helps replace lost fluids and electrolytes but does not provide all the necessary nutrients. It is essential to address the client's concerns about food intake.
Choice B rationale:
Soft and bland foods are recommended once vomiting subsides, but suggesting this before addressing the client's concern may not effectively address the issue.
Choice C rationale:
Encouraging regular meals may not be appropriate during gastroenteritis, as the digestive system needs time to recover. Eating regular meals could potentially exacerbate symptoms.
Choice D rationale:
Gastroenteritis commonly leads to a reduced appetite due to nausea, vomiting, and stomach discomfort. Assuring the client that a decreased appetite is normal and emphasizing the importance of fluid intake through ORT is appropriate.
Explanation
Choice A rationale:
X-ray of the abdomen is not the most appropriate diagnostic test for identifying the causative agent of gastroenteritis. It primarily helps visualize the structures within the abdomen and is not specific to identifying pathogens.
Choice B rationale:
A complete blood count (CBC) measures blood cell counts and is not a direct test for identifying gastroenteritis causative agents.
Choice C rationale:
An electrocardiogram (ECG) is used to assess heart activity and is unrelated to diagnosing gastroenteritis or its causative agents.
Choice D rationale:
Stool culture and microscopy are crucial for identifying bacterial, viral, or parasitic pathogens responsible for gastroenteritis. It helps determine the specific organism causing the illness and guides appropriate treatment.
Explanation
Choice A rationale:
Onset and duration of fever is important for assessing the child's condition, but in the context of suspected gastroenteritis, focusing solely on fever may not provide a comprehensive assessment.
Choice B rationale:
Exposure to potential sources of infection is crucial in assessing gastroenteritis. Determining whether the child has been in contact with contaminated food, water, or individuals with similar symptoms helps identify the possible cause of gastroenteritis.
Choice C rationale:
Recent travel history is relevant for assessing certain types of infections, such as travel-related gastroenteritis from exposure to contaminated water or food in other regions. However, in a general assessment of suspected gastroenteritis, exposure to potential sources of infection (Choice B) is more pertinent.
Choice D rationale:
Presence of cough and sore throat is not directly related to gastroenteritis, which primarily affects the gastrointestinal tract. These symptoms are more characteristic of respiratory infections.
Explanation
Choice A rationale:
Administering 50-100 ml/kg of oral rehydration therapy (ORT) is recommended for severe dehydration. This guideline ensures a more aggressive fluid replacement to address significant fluid loss.
Choice B rationale:
Administering 100-200 ml/kg for mild dehydration might lead to overhydration in less severe cases, increasing the risk of fluid overload.
Choice C rationale:
Administering 20-40 ml/kg for severe dehydration is insufficient to adequately address severe fluid loss and rehydrate the client effectively.
Choice D rationale:
Administering 40-60 ml/kg for mild dehydration may not provide enough fluids to adequately address dehydration, especially if the client's condition worsens.
Explanation
Choice A rationale:
Avoiding handwashing after using the toilet would increase the risk of transmitting infection, as proper hand hygiene is essential to prevent the spread of pathogens.
Choice B rationale:
Sharing personal items with family members can contribute to the transmission of infections. It is important to discourage this behavior.
Choice C rationale:
Washing fruits and vegetables before eating helps remove potential contaminants and pathogens, reducing the risk of ingesting harmful microorganisms.
Choice D rationale:
Using the same cup as a friend to drink can lead to the spread of infections through direct contact with contaminated surfaces. It is advisable to use separate utensils and containers to prevent transmission.
Explanation
Choice A rationale:
Hypertension and tachycardia are not typical signs of dehydration. Dehydration often leads to decreased blood volume, resulting in hypotension and tachycardia as the body tries to compensate for the fluid loss.
Choice B rationale:
Bradycardia and pale skin are not consistent with dehydration. Dehydration usually leads to an increased heart rate (tachycardia) as the body attempts to maintain circulation despite decreased fluid levels.
Choice C rationale:
Increased urine output is not indicative of dehydration. Dehydration typically leads to decreased urine output (oliguria) as the body conserves fluid in response to the loss.
Choice D rationale:
Dry mucous membranes and sunken eyes are classic signs of dehydration. When fluid intake is insufficient, the body conserves water by reducing saliva and other secretions, resulting in dry mucous membranes. Sunken eyes can occur due to decreased fluid volume and loss of tissue turgor.
Explanation
Choice A rationale:
Chest X-ray is not appropriate for identifying the causative agent of gastroenteritis. It primarily helps visualize lung and chest conditions.
Choice B rationale:
Blood culture is used to detect bacterial or fungal infections in the bloodstream, not specifically for identifying the causative agent of gastroenteritis.
Choice C rationale:
Stool analysis is the most suitable diagnostic test for identifying the specific causative agent of gastroenteritis. It can detect pathogens, such as bacteria, viruses, and parasites, in the stool sample.
Choice D rationale:
Urinalysis is not the most appropriate test for identifying the causative agent of gastroenteritis. It is used to assess kidney function and detect urinary tract infections.
Vulvovaginitis.
.
(From external source) Which bacteria produce enterotoxins that cause watery diarrhea in cases of bacterial gastroenteritis?
Explanation
Choice A rationale:
Salmonella and Campylobacter are known to cause bacterial gastroenteritis, but they typically do not produce enterotoxins that specifically cause watery diarrhea. Instead, they often cause more inflammatory types of diarrhea.
Choice B rationale:
Shigella and Yersinia can also cause bacterial gastroenteritis, but their mechanisms of causing diarrhea are different from enterotoxin production. Shigella is known to cause bloody diarrhea, while Yersinia can lead to abdominal pain and fever.
Choice C rationale:
Vibrio cholerae produces the cholera toxin, which leads to watery diarrhea by increasing chloride secretion and inhibiting sodium absorption in the intestines. Clostridium perfringens can produce enterotoxins that lead to watery diarrhea and abdominal cramps.
Choice D rationale:
While E. coli can cause gastroenteritis, it usually produces Shiga toxins that lead to bloody diarrhea (as seen in E. coli O157:H7), or it may cause inflammation and not typically result in watery diarrhea. C. difficile is known for causing antibiotic-associated diarrhea and colitis, but it's not primarily associated with watery diarrhea.
Vulvovaginitis
Explanation
Choice A rationale:
Initiation of antibiotic therapy is not the primary intervention for severe dehydration in gastroenteritis. Fluid replacement is crucial to correct the fluid and electrolyte imbalances.
Choice B rationale:
Administration of antidiarrheal agents is contraindicated in cases of severe dehydration. These agents can delay the elimination of the causative agent and further worsen fluid loss.
Choice C rationale:
Oral rehydration therapy (ORT) is effective for mild dehydration but may not be sufficient in cases of severe dehydration where oral intake is limited.
Choice D rationale:
Intravenous fluid therapy (IVF) is the appropriate intervention for severe dehydration. IV fluids rapidly restore fluid balance and correct electrolyte imbalances, ensuring timely rehydration and preventing complications.
Explanation
Choice A rationale:
Giving loperamide to stop diarrhea is not appropriate for a child with suspected gastroenteritis. Loperamide can slow down bowel movements and may lead to complications, especially in pediatric patients.
Choice B rationale:
Encouraging the child to drink plenty of fluids is crucial to prevent dehydration, a common concern in gastroenteritis. Fluid intake helps replace lost fluids and electrolytes due to vomiting and diarrhea.
Choice C rationale:
Avoiding food until vomiting stops can deprive the child of essential nutrients. Small, frequent, bland meals are recommended during recovery from gastroenteritis.
Choice D rationale:
Giving aspirin to a child with fever is contraindicated due to the risk of Reye's syndrome, a potentially fatal condition. Acetaminophen is the preferred antipyretic.
Explanation
Choice A rationale:
Assessing blood glucose levels is not directly related to ondansetron administration for vomiting. Ondansetron does not typically affect blood glucose levels.
Choice B rationale:
Obtaining a stool sample for culture and microscopy is important for diagnosing the cause of gastroenteritis, but it is not a necessary step before administering ondansetron.
Choice C rationale:
Monitoring urinary output is not directly associated with the administration of ondansetron. It's important for assessing hydration status, but it's not the immediate concern when administering this antiemetic medication.
Choice D rationale:
Checking vital signs is essential before giving any medication to ensure the client's overall stability and to detect any potential contraindications or adverse reactions.
Explanation
Choice A rationale:
Avoiding sexual intercourse is not necessary for preventing vulvovaginitis. Maintaining good hygiene and other preventive measures are more relevant.
Choice B rationale:
Using scented soaps for cleansing can actually increase the risk of vulvovaginal irritation and infections. Unscented, gentle cleansers are recommended.
Choice C rationale:
Limiting sexual partners helps reduce the risk of sexually transmitted infections (STIs) that can lead to vulvovaginitis.
Choice D rationale:
Douching regularly is not advised, as it disrupts the natural balance of vaginal flora and increases the risk of infections and irritation.
Explanation
Choice A rationale:
Anaerobic bacteria are not responsible for the described symptoms. They typically cause foul-smelling discharge with a different consistency.
Choice B rationale:
Fungi, such as Candida species, commonly cause vaginal candidiasis, which presents with thick, white, cottage cheese-like discharge. This matches the client's symptoms.
Choice C rationale:
Protozoa, like Trichomonas vaginalis, usually lead to a frothy, greenish-yellow discharge with a foul odor, which doesn't align with the client's presentation.
Choice D rationale:
Low estrogen levels would not directly cause this type of discharge. They might lead to vaginal dryness and thinning of vaginal walls, but not the specific discharge described.
Choice E rationale:
Human papillomavirus (HPV) doesn't typically cause the described discharge. It's associated with genital warts and cervical changes but not with this type of discharge.
Explanation
Choice A rationale:
Lactobacilli overgrowth can lead to a fishy odor, particularly in bacterial vaginosis (BV) The overgrowth disrupts the normal vaginal pH.
Choice B rationale:
A viral infection wouldn't cause a fishy odor. Viruses like human papillomavirus (HPV) might cause genital warts but not this specific odor.
Choice C rationale:
Protozoa, such as Trichomonas vaginalis, cause a distinct odor, but it's not typically described as fishy.
Choice D rationale:
Allergic reactions to douches might cause irritation, itching, or redness, but they wouldn't lead to a fishy odor.
Explanation
Choice A rationale:
Anaerobic bacteria typically cause a foul-smelling discharge, which doesn't match the described symptoms.
Choice B rationale:
Fungal infections result in a thick, white, cottage cheese-like discharge, different from the green-yellow frothy discharge mentioned.
Choice C rationale:
Protozoa, specifically Trichomonas vaginalis, cause green-yellow frothy discharge with a foul odor, closely resembling the client's symptoms.
Choice D rationale:
Low estrogen levels would not cause this specific presentation; they're more associated with vaginal dryness and thinning of vaginal walls.
Explanation
Choice A rationale:
Limiting sexual partners is a crucial preventive measure for vulvovaginitis. This reduces the risk of exposure to potential infections that can lead to vulvovaginitis. Multiple sexual partners can increase the chances of contracting sexually transmitted infections (STIs) and other pathogens.
Choice B rationale:
Avoiding the use of condoms is not a recommended preventive measure. Condoms provide a barrier against STIs and other infectious agents, reducing the risk of vulvovaginitis. Therefore, this choice is not appropriate for prevention.
Choice C rationale:
Using scented detergents for laundry is not advisable. Scented products can disrupt the natural pH balance of the vagina, leading to irritation and an increased risk of vulvovaginitis. Unscented or mild detergents are preferable to maintain vaginal health.
Choice D rationale:
Increasing the intake of sugary foods is not recommended for vulvovaginitis prevention. High sugar consumption can lead to an overgrowth of yeast (Candida albicans) in the vaginal area, potentially causing vulvovaginitis. Therefore, this choice contradicts preventive measures.
. A client with vulvovaginitis is prescribed antibiotics. The nurse should monitor the client for which potential adverse effect?
Explanation
Choice A rationale:
Vaginal itching is a common symptom of vulvovaginitis but not a potential adverse effect of antibiotics. It is more indicative of the condition itself rather than a medication side effect.
Choice B rationale:
A fishy odor is characteristic of bacterial vaginosis (BV), not a common adverse effect of antibiotics. BV is caused by an imbalance in vaginal flora and is not directly related to antibiotic therapy.
Choice C rationale:
Increased vaginal discharge is a potential adverse effect of antibiotics. Antibiotics can disrupt the normal vaginal flora, leading to an overgrowth of yeast or other pathogens, which may result in increased discharge.
Choice D rationale:
Photosensitivity is unrelated to antibiotics or vulvovaginitis. It refers to an increased sensitivity to sunlight or artificial light and is not a relevant consideration in this context.
. A nurse is caring for a client with vulvovaginitis caused by Candida albicans. Which intervention should the nurse include in the client's care plan?
Explanation
Choice A rationale:
Encouraging the use of vaginal douches is not recommended for vulvovaginitis caused by Candida albicans. Douching can disrupt the vaginal pH balance and lead to further irritation or infection.
Choice B rationale:
Applying a topical corticosteroid cream is not a suitable intervention for Candida albicans-related vulvovaginitis. Corticosteroids can suppress the immune response and potentially worsen fungal infections.
Choice C rationale:
Using hormonal therapy is not indicated for treating Candida albicans vulvovaginitis. This condition is primarily fungal in nature and requires antifungal treatment, not hormonal therapy.
Choice D rationale:
Promoting good hygiene practices is essential in managing Candida albicans vulvovaginitis. Proper hygiene helps maintain a healthy vaginal environment and reduces the risk of fungal overgrowth. Emphasizing the importance of gentle cleansing and avoiding irritants is crucial.
. A client has been diagnosed with vulvovaginitis caused by Trichomonas vaginalis. Which treatments should the nurse anticipate being prescribed for this client? Select all that apply:
Explanation
Choice A rationale:
Antibiotics are not typically used to treat Trichomonas vaginalis, as it is a protozoan infection rather than a bacterial infection.
Choice B rationale:
Antifungals are also not appropriate for treating Trichomonas vaginalis, as it is not a fungal infection.
Choice C rationale:
Antiprotozoals are the correct treatment for Trichomonas vaginalis infection. Metronidazole is commonly prescribed to treat this type of vulvovaginitis.
Choice D rationale:
Topical creams may be used for other types of vulvovaginitis, but they are not the primary treatment for Trichomonas vaginalis.
Choice E rationale:
Hormonal therapy is not indicated for the treatment of vulvovaginitis caused by Trichomonas vaginalis.
A nurse is educating a group of clients about vulvovaginitis. Which mode of transmission is associated with bacterial vaginosis (BV)?
Explanation
Choice A rationale:
Bacterial vaginosis (BV) is primarily associated with endogenous transmission, meaning it is caused by an overgrowth of normally occurring vaginal bacteria rather than being directly transmitted from another individual.
Choice B rationale:
While sexual transmission can play a role in the development of BV, it is not the primary mode of transmission for this condition.
Choice C rationale:
Vector transmission involves the transfer of pathogens by a vector such as a mosquito or tick and is not relevant to bacterial vaginosis.
Choice D rationale:
Contact transmission typically involves direct physical contact with an infected person or contaminated object, which is not the main mode of transmission for BV.
A nurse is assessing clients with vulvovaginitis. Which type of vulvovaginitis can be transmitted from mother to child during delivery?
Explanation
Choice A rationale:
Bacterial vaginosis (BV) is not commonly transmitted from mother to child during delivery. It is primarily associated with an imbalance in vaginal bacteria.
Choice B rationale:
Candidal vulvovaginitis (CV), caused by the fungus Candida, can be transmitted from mother to child during delivery as the baby passes through the birth canal.
Choice C rationale:
Trichomonas vaginalis (TV) can also be transmitted from mother to child during delivery, but CV is a more common cause of transmission.
Choice D rationale:
Atrophic vaginitis (AV) is not typically transmitted from mother to child during delivery. It is often associated with hormonal changes during menopause.
Choice E rationale:
This option acknowledges other types of vulvovaginitis with various modes of transmission, but the specific question asks about transmission from mother to child during delivery. CV is the most appropriate choice in this context.
A nurse is caring for a client with candidal vulvovaginitis (CV) Which statement is an appropriate assessment finding for this client?
Explanation
Choice A rationale:
Thin, frothy, green-yellow vaginal discharge is indicative of trichomoniasis, not candidal vulvovaginitis (CV) Trichomoniasis typically presents with a foul-smelling discharge.
Choice B rationale:
While inflammation, itching, and burning are common symptoms of CV, they do not specifically describe the characteristic discharge associated with this condition.
Choice C rationale:
Thick, white, and clumpy vaginal discharge with no odor is a classic presentation of candidal vulvovaginitis (CV) The discharge is often described as resembling cottage cheese.
Choice D rationale:
A vaginal pH greater than 5.0 is suggestive of bacterial vaginosis, not candidal vulvovaginitis. In CV, the vaginal pH is usually normal (around 4-4.5)
A client reports experiencing vaginal dryness and atrophy. The nurse suspects atrophic vaginitis (AV) Which assessment finding supports this suspicion?
Explanation
Choice A rationale:
A vaginal pH less than 4.5 is within the normal acidic range and does not specifically support the suspicion of atrophic vaginitis (AV)
Choice B rationale:
Presence of motile trichomonads indicates trichomoniasis, not atrophic vaginitis (AV)
Choice C rationale:
Thin and loss of rugae (folds) of vaginal mucosa is a characteristic finding in atrophic vaginitis (AV) This condition occurs due to decreased estrogen levels, leading to thinning and drying of vaginal tissues.
Choice D rationale:
A thin, gray-white, or milky vaginal discharge is more suggestive of other infections or conditions and is not a specific sign of atrophic vaginitis (AV)
A nurse is planning care for a client with vulvovaginitis. Which treatment is appropriate for Trichomonas vaginalis (TV) infection?
Explanation
Choice A rationale:
Trichomonas vaginalis (TV) infection is treated with medications that have activity against protozoa, such as metronidazole, clindamycin, tinidazole, or secnidazole. These drugs are effective in eradicating the infection.
Choice B rationale:
Oral fluconazole and topical azoles are used to treat fungal infections, such as candidiasis, not Trichomonas vaginalis (TV) infection.
Choice C rationale:
Hormonal therapy with estrogen creams, tablets, or rings is used for menopausal or postmenopausal symptoms, not for the treatment of Trichomonas vaginalis (TV) infection.
Choice D rationale:
Removal of foreign bodies or irritants is a general management strategy and is not specific to treating Trichomonas vaginalis (TV) infection.
Explanation
Choice A rationale:
Bacterial vaginosis (BV) is not related to hormonal changes but rather an overgrowth of bacteria causing an imbalance in the vaginal ecosystem.
Choice B rationale:
Candidal vulvovaginitis (CV) is a fungal infection and is not primarily caused by hormonal changes.
Choice C rationale:
Trichomonas vaginalis (TV) is a sexually transmitted infection and is not directly linked to hormonal changes.
Choice D rationale:
Atrophic vaginitis (AV) occurs due to hormonal changes, specifically a decrease in estrogen levels that can lead to thinning and inflammation of vaginal tissues. Estrogen deficiency commonly occurs during menopause or aging, leading to symptoms like vaginal dryness and discomfort.
Explanation
Choice A rationale:
Bacterial vaginosis (BV) typically presents with a thin gray or white discharge and is associated with a fishy odor. It is not known for a green-yellow discharge.
Choice B rationale:
Candidal vulvovaginitis (CV) often presents with a white, thick, cottage cheese-like discharge, not a green-yellow discharge.
Choice C rationale:
Trichomonas vaginalis (TV) infection can result in a thin, frothy, green-yellow vaginal discharge with a foul musty odor. This infection is sexually transmitted and may also cause itching and irritation.
Choice D rationale:
Atrophic vaginitis (AV) is not associated with a frothy, green-yellow discharge but rather with symptoms related to estrogen deficiency and vaginal thinning.
Explanation
Choice A rationale:
Bacterial vaginosis (BV) is primarily caused by an imbalance in the vaginal microbiota and is not known for multiple modes of transmission.
Choice B rationale:
Candidal vulvovaginitis (CV) is commonly caused by Candida fungi and is not known for having various modes of transmission.
Choice C rationale:
Trichomonas vaginalis (TV) is primarily transmitted sexually and is not typically associated with contact or vector transmission.
Choice D rationale:
Atrophic vaginitis (AV) is related to hormonal changes and is not transmitted through sexual or contact modes.
Choice E rationale:
Other types of vulvovaginitis, such as certain viral or bacterial infections, could have various modes of transmission, including sexual, contact, or vector transmission. It is important to consider these possibilities when educating clients about modes of transmission.
Explanation
Choice A rationale:
Avoiding douching is recommended to prevent bacterial vaginosis (BV) as douching can disrupt the natural vaginal flora and increase the risk of BV.
Choice B rationale:
Using condoms or other barrier methods during sexual intercourse helps reduce the risk of BV transmission, as it prevents the introduction of potentially harmful bacteria into the vagina.
Choice C rationale:
Limiting sexual partners can lower the risk of BV, as having multiple sexual partners may increase the likelihood of exposure to different bacteria that can disrupt the vaginal flora.
Choice D rationale:
Treating underlying conditions, such as diabetes mellitus, is important because uncontrolled diabetes can create an environment conducive to BV development due to elevated glucose levels.
Choice E rationale:
Using hormonal therapy as prescribed is not directly related to preventing BV. Hormonal therapy typically pertains to conditions like hormone replacement therapy and is not a preventive measure for BV.
Explanation
Choice A rationale:
Administering oral or intravaginal antibiotics is not appropriate for vulvovaginal candidiasis (CV) since it is caused by a fungal infection, not bacterial. Antifungal medications are the primary treatment.
Choice B rationale:
Educating the client on the causes, symptoms, and prevention of CV is essential to ensure the client understands the infection, its symptoms, and how to prevent recurrence.
Choice C rationale:
Providing comfort measures to relieve irritation and discomfort, such as soothing creams and warm sitz baths, helps alleviate the discomfort associated with CV.
Choice D rationale:
Encouraging the client to avoid sexual intercourse during treatment is advised to prevent further irritation and disruption of the vaginal flora.
Choice E rationale:
Advising the client to limit sexual partners is not a specific intervention for CV.
Explanation
Choice A rationale:
Abstaining from sexual contact until both partners are treated and cured is an appropriate measure to prevent re-infection and transmission of trichomoniasis vaginitis (TV)
Choice B rationale:
Avoiding alcohol consumption during treatment with metronidazole is necessary, as alcohol can interact with this medication and cause adverse reactions.
Choice C rationale:
Using condoms or other barrier methods during sexual intercourse can prevent transmission of TV and is an accurate statement.
Choice D rationale:
Continuing hormonal therapy despite experiencing abnormal bleeding is concerning, as it may indicate an adverse reaction or need for further evaluation. This statement highlights a need for further teaching.
Explanation
Choice A rationale:
Lubricants and moisturizers are commonly used for symptom relief in atrophic vaginitis (AV), but this choice does not reflect an understanding of hormonal therapy, which is the treatment plan specified.
Choice B rationale:
Avoiding irritants or allergens is important for overall vaginal health, but it does not specifically indicate comprehension of hormonal therapy for AV.
Choice C rationale:
This choice demonstrates understanding of potential side effects and complications associated with hormonal therapy, such as abnormal bleeding and breast changes. Monitoring for such changes is vital.
Choice D rationale:
The mention of completing a course of oral antibiotics is unrelated to the treatment plan for atrophic vaginitis, which involves hormonal therapy.
Explanation
Choice A rationale:
Education empowers the patient to prevent recurrence by understanding the causes and symptoms of foreign body-related vulvovaginitis, contributing to long-term management.
Choice B rationale:
Administering specific treatments like antivirals, antiparasitics, or antibiotics addresses the acute phase but does not focus on preventing future occurrences or patient education.
Choice C rationale:
Encouraging good hygiene and cotton underwear is essential, but it is more reactive than providing education for long-term prevention.
Choice D rationale:
Monitoring for complications is important, but the nurse should prioritize patient education to promote proactive management and prevention.
Ebola.
Ebola
Explanation
Choice A rationale:
Enlarged cervical lymph nodes are not typically associated with vulvovaginitis; they might indicate an infection or other unrelated condition.
Choice B rationale:
Pain during bowel movements is more suggestive of conditions involving the rectum or anus rather than vulvovaginitis.
Choice C rationale:
Foul-smelling vaginal discharge can indicate an infection or inflammation in the vaginal area, aligning with the expected finding in vulvovaginitis.
Choice D rationale:
Elevated blood pressure is not a characteristic sign of vulvovaginitis and is unrelated to this condition.
Explanation
Choice A rationale:
Taking metronidazole with an antacid may decrease its absorption and effectiveness.
Choice B rationale:
Metronidazole and alcohol interaction can lead to a disulfiram-like reaction, causing nausea, vomiting, flushing, and palpitations. Avoiding alcohol ensures the client's safety and prevents adverse effects.
Choice C rationale:
Taking metronidazole on an empty stomach is not necessary and may increase the risk of gastrointestinal upset.
Choice D rationale:
Discontinuing metronidazole prematurely can lead to treatment failure and potential recurrence of infection.
Explanation
Choice A rationale:
Avoiding sexual intercourse during treatment helps prevent further irritation and infection spread.
Choice B rationale:
Hormonal contraceptives are unrelated to preventing vulvovaginal candidiasis (CV) recurrence.
Choice C rationale:
Wearing loose-fitting cotton underwear promotes airflow, reduces moisture, and prevents fungal overgrowth.
Choice D rationale:
Limiting sexual partners reduces the risk of exposure to potential sources of infection.
Choice E rationale:
Completing the full course of antifungal medication ensures complete eradication of the infection and reduces the risk of recurrence.
Explanation
Choice A rationale:
Early-stage Ebola virus disease (EVD) commonly presents with symptoms such as abdominal pain, fever, fatigue, and muscle pain.
Choice B rationale:
Vision problems are not typically associated with early-stage EVD.
Choice C rationale:
Memory loss is not a characteristic symptom of early-stage EVD.
Choice D rationale:
Joint pain is not a primary symptom in the early stages of EVD; muscle pain is more common.
Explanation
Choice A rationale:
The statement is incorrect. Ebola virus transmission does not occur through the air. It is primarily spread through direct contact with bodily fluids of infected individuals.
Choice B rationale:
This statement is correct. Handling bushmeat, which is the meat of wild animals, can lead to Ebola virus transmission. Infected animals can carry the virus, and handling their meat without proper precautions can result in transmission.
Choice C rationale:
This statement is correct. Direct contact with infected bat's urine can transmit the virus. Bats can carry the Ebola virus, and their bodily fluids can contain the virus, leading to potential transmission.
Choice D rationale:
This statement is correct. Sexual contact with an infected person can transmit the virus. Ebola virus can be present in semen for a significant period after recovery, posing a risk of sexual transmission.
Choice E rationale:
This statement is correct. Consuming contaminated food can transmit the virus. If the food is contaminated with infected bodily fluids or if an infected animal is consumed, transmission can occur.
Explanation
Choice A rationale:
This statement is incorrect. Weakness and severe headache are symptoms commonly seen in the early stages of Ebola virus disease (EVD), not the later stages.
Choice B rationale:
This statement is appropriate. Since the client is in the early stages of EVD and presents with symptoms like weakness and severe headache, the nurse's response acknowledges the possibility of these symptoms being related to a common cold but still highlights the need for further evaluation due to the potential severity of EVD.
Choice C rationale:
This statement is irrelevant and does not address the client's current symptoms or concerns.
Choice D rationale:
This statement is incorrect. Joint and muscle pain are indeed associated with EVD and can be significant symptoms.
Explanation
Choice A rationale:
This statement is appropriate. Unexplained internal and external bleeding is a hallmark symptom of Ebola virus disease (EVD), and it requires immediate medical attention due to its potentially life-threatening nature.
Choice B rationale:
This statement is incorrect. Bleeding is a characteristic symptom of EVD, and the nurse should not dismiss it as being due to another condition without proper evaluation.
Choice C rationale:
This statement is incorrect. Increased white blood cells would not explain the bleeding and are not associated with this symptom in EVD.
Choice D rationale:
This statement is incorrect. Bleeding from the nose and eyes is significant in the context of EVD and should not be downplayed as insignificant.
Explanation
Choice A rationale:
The case fatality rate of EVD being always 90% or higher is inaccurate. While EVD can have high case fatality rates during outbreaks, it is not a fixed percentage and can vary.
Choice B rationale:
The case fatality rate of EVD being around 25% on average is also inaccurate. This value is too low compared to historical outbreaks.
Choice C rationale:
This is the correct answer. The case fatality rate of EVD indeed varies depending on factors like the specific virus species involved, the quality of medical care, and the available resources in the affected area. Case fatality rates can range from approximately 25% to over 90%, depending on these factors.
Choice D rationale:
The case fatality rate of EVD being the same regardless of the treatment received is incorrect. Adequate medical care and supportive treatments can significantly impact the outcome and lower the fatality rate.
Explanation
Choice A rationale:
Wearing gloves and a gown while in contact with the patient is essential, but it does not address the potential airborne transmission of Ebola virus.
Choice B rationale:
Ensuring that the patient's visitors wear a mask is important, but it does not directly address the isolation and containment of the virus within the hospital environment.
Choice C rationale:
This is the correct answer. Placing the patient in a room with negative pressure airflow helps prevent the spread of contaminated air to other areas of the hospital. It reduces the risk of airborne transmission of the virus, which is crucial in containing the disease.
Choice D rationale:
Avoiding the use of hand sanitizers to prevent the spread of the virus is not a recommended precautionary measure. Hand hygiene, including the use of hand sanitizers, is still crucial in preventing the spread of infections, including Ebola.
Explanation
Choice A rationale:
An elevated platelet count is less likely in a patient with EVD. Thrombocytopenia (low platelet count) is a common laboratory finding in EVD due to the virus's impact on the bone marrow.
Choice B rationale:
Decreased liver enzymes is less likely. EVD can lead to elevated liver enzymes due to liver damage caused by the virus.
Choice C rationale:
This is the correct answer. A decreased white blood cell count, specifically lymphocytes, is expected in a patient with EVD. The virus can lead to suppression of the immune system, including a decrease in white blood cell counts.
Choice D rationale:
Elevated serum creatinine levels are not a typical finding in EVD. Kidney dysfunction is not a primary feature of the disease, so elevated creatinine levels are less likely.
Explanation
Choice A rationale:
Limit contact with others for at least three months after recovery. This is not accurate. While it's important to limit contact during the acute phase of the illness, Ebola virus disease (EVD) does not remain contagious for three months after recovery.
Choice B rationale:
Continue to use barrier methods during sexual intercourse for six months. This is correct. Ebola virus can persist in the semen of male survivors for up to six months after recovery. Barrier methods should be used to prevent sexual transmission during this period.
Choice C rationale:
Avoid consuming raw or undercooked meat. This is correct. Ebola virus can be transmitted through the consumption of infected meat from animals, so it's important to avoid raw or undercooked meat.
Choice D rationale:
Monitor blood pressure daily. This is not directly related to EVD recovery instructions. While monitoring blood pressure is important for overall health, it is not a specific recommendation for EVD recovery.
Choice E rationale:
Return to work immediately after being discharged. This is not accurate. Patients who have recovered from EVD should be cautious about returning to work immediately due to potential fatigue and lingering symptoms. They should follow appropriate recovery guidelines.
Explanation
Choice A rationale:
Blood culture. While blood cultures can detect certain infections, they are not the primary diagnostic test for Ebola virus disease (EVD) EVD is typically confirmed through molecular methods.
Choice B rationale:
Chest X-ray. A chest X-ray may show nonspecific findings but is not a specific diagnostic test for EVD.
Choice C rationale:
Urinalysis. Urinalysis is not a primary diagnostic test for EVD. The virus is primarily detected through blood samples.
Choice D rationale:
Enzyme-linked immunosorbent assay (ELISA) This is correct. ELISA is used to detect antibodies or antigens in the blood. It can be used to confirm the presence of Ebola virus antigens or antibodies, aiding in the diagnosis of EVD.
Explanation
Choice A rationale:
Administering oxygen and mechanical ventilation. This is correct. Supportive care for EVD may involve managing respiratory symptoms, including providing oxygen and mechanical ventilation if necessary.
Choice B rationale:
Providing psychological support and counseling. This is correct. EVD can be emotionally distressing for patients. Providing psychological support and counseling can help patients cope with the illness and its effects.
Choice C rationale:
Performing blood transfusions and clotting factor administration. While EVD can lead to clotting abnormalities, routine blood transfusions and clotting factor administration are not standard treatments for the disease.
Choice D rationale:
Applying warm compresses to reduce fever. While fever is a symptom of EVD, applying warm compresses is not recommended. Fever management should be under medical supervision.
Choice E rationale:
Monitoring organ function regularly. This is correct. EVD can lead to multi-organ dysfunction. Regular monitoring of organ function helps detect and manage potential complications.
Explanation
Choice A rationale:
EVD is not transmitted through the air like the flu. It primarily spreads through direct contact with infected body fluids.
Choice B rationale:
While contaminated food and water can transmit some diseases, EVD is primarily spread through direct contact with infected animals or people's body fluids.
Choice C rationale:
This is the correct choice. EVD is mainly transmitted through direct contact with infected animals or people's body fluids, such as blood, saliva, sweat, and urine.
Choice D rationale:
EVD is not transmitted by mosquito bites. It is not caused by a mosquito-borne virus.
Explanation
Choice A rationale:
Antibiotics are not effective against viral infections like EVD. EVD does not have a specific antibiotic treatment.
Choice B rationale:
Avoiding seeking medical attention would be dangerous and can contribute to the spread of the disease.
Choice C rationale:
EVD can be transmitted through various routes, including contact with infected body fluids, not just sexual contact.
Choice D rationale:
This is the appropriate response. It reassures the client that necessary precautions will be taken to prevent the spread of the disease and offers a sense of security.
Explanation
Choice A rationale:
This is the most important measure to emphasize. Avoiding contact with infected animals or people and their fluids is crucial to reduce the risk of transmission.
Choice B rationale:
While face masks are important in some situations, they alone may not be sufficient to prevent EVD transmission.
Choice C rationale:
Eating cooked meat from infected animals does not build immunity and can actually increase the risk of transmission.
Choice D rationale:
While disinfecting surfaces is important for infection control, it may not be the most emphasized measure for EVD prevention.
Explanation
Choice A rationale:
Sending the client home with symptomatic relief medications is not appropriate for suspected Ebola virus disease (EVD) EVD is a serious and highly infectious disease that requires immediate isolation and contact tracing to prevent its spread.
Choice B rationale:
Initiating contact tracing for 14 days is the correct nursing action. Ebola is transmitted through direct contact with blood, body fluids, and tissues of infected animals or people. Identifying and monitoring individuals who may have been exposed is crucial to preventing further transmission.
Choice C rationale:
Encouraging the client to self-isolate for 24 hours is insufficient. Ebola has an incubation period of 2 to 21 days, during which the client may become symptomatic. Isolating for only 24 hours does not adequately address the potential for transmission.
Choice D rationale:
Providing over-the-counter antiviral medication is not an appropriate action for suspected EVD. There is no specific antiviral treatment for Ebola, and symptomatic management alone would not address the potential for spread.
Explanation
Choice A rationale:
Standard precautions involve basic infection prevention measures, but for suspected Ebola virus disease (EVD), more stringent precautions are necessary due to the potential for direct contact with contaminated body fluids.
Choice B rationale:
Contact precautions are essential when dealing with suspected EVD patients. Ebola is transmitted through direct contact with infected blood, secretions, organs, or other body fluids. Close physical contact with the patient requires wearing gloves, gowns, masks, and eye protection.
Choice C rationale:
Airborne precautions are not necessary for EVD. Ebola is not transmitted through the airborne route, and these precautions are more relevant for diseases like tuberculosis that spread through respiratory droplets.
Choice D rationale:
Droplet precautions are not appropriate for EVD either, as Ebola is not primarily transmitted through respiratory droplets.
Explanation
Choice A rationale:
Handwashing with soap and water is a crucial preventive measure. It helps reduce the risk of infection by removing potential contaminants from the hands.
Choice B rationale:
Avoiding travel to Ebola-affected regions is important to prevent exposure to the virus. Outbreaks often occur in specific geographic areas, and travel to these regions increases the risk of infection.
Choice C rationale:
Using mosquito nets is not directly relevant to preventing Ebola transmission. Ebola is not transmitted by mosquitoes; it primarily spreads through direct contact with infected individuals or their bodily fluids.
Choice D rationale:
Wearing PPE when caring for infected patients is essential to protect healthcare workers from direct contact with blood, secretions, and other potentially infectious materials.
Choice E rationale:
Eating raw fruits and vegetables from local markets is not a recommended preventive measure for EVD. While hygiene practices and food safety are important, this choice does not directly relate to Ebola transmission.
Explanation
Choice A rationale:
Blood culture is not the primary diagnostic test for Ebola virus disease (EVD) ELISA is a more specific and sensitive test to detect Ebola virus antigens or antibodies in the blood, confirming the diagnosis.
Choice B rationale:
Chest X-ray is not a diagnostic test for EVD. It is used to evaluate lung conditions but is not specific to EVD diagnosis.
Choice C rationale:
Urinalysis is not a primary diagnostic test for EVD. ELISA is a more appropriate test to confirm the presence of the Ebola virus.
Choice D rationale:
Enzyme-linked immunosorbent assay (ELISA) is the correct choice. It detects the presence of Ebola virus antigens or antibodies, providing definitive confirmation of EVD.
Explanation
E.
Choice A rationale:
Administering oxygen and mechanical ventilation is essential as EVD can cause respiratory distress and failure.
Choice B rationale:
Providing psychological support and counseling is important due to the emotional stress and fear associated with EVD.
Choice C rationale:
Performing blood transfusions and clotting factor administration are not typical interventions for EVD. It primarily affects the immune system and does not usually lead to widespread coagulation issues.
Choice D rationale:
Applying warm compresses to reduce fever can worsen the patient's condition by promoting viral replication. Fever reduction in EVD is managed with antipyretics.
Choice E rationale:
Monitoring organ function regularly is crucial because EVD can lead to organ failure, particularly liver and kidney dysfunction.
Explanation
Choice A rationale:
EVD is not transmitted through the air like the flu. It requires direct contact with infected bodily fluids.
Choice B rationale:
EVD is not transmitted through contaminated food and water. Direct contact with infected animals or people is the primary mode of transmission.
Choice C rationale:
The correct choice. EVD is transmitted through direct contact with infected animals or people's body fluids, such as blood, saliva, urine, and sweat.
Choice D rationale:
EVD is not transmitted by mosquito bites. It is not an arthropod-borne virus like malaria or dengue.
Explanation
Choice A rationale:
This statement is incorrect. Ebola virus disease (EVD) is not treated with antibiotics. EVD is caused by a virus, not a bacterial infection. It requires supportive care and management of symptoms.
Choice B rationale:
This statement is incorrect. Seeking medical attention is crucial if someone experiences symptoms of EVD, such as fever, fatigue, muscle pain, headache, and more. Delaying medical care can worsen the condition and increase the risk of transmission.
Choice C rationale:
This statement is incorrect. EVD can be transmitted through various routes, including direct contact with infected bodily fluids, not just sexual contact. It is important to provide accurate information to the client to prevent misunderstandings.
Choice D rationale:
This statement is correct. Assuring the client that necessary precautions will be taken to protect them and others from spreading the disease is appropriate. This helps alleviate fears and fosters trust in the healthcare team.
A nurse is providing education to a group of healthcare workers on Ebola virus disease (EVD) prevention and control measures. Which measure should the nurse emphasize to reduce the risk of transmission?
Explanation
Choice A rationale:
This measure is crucial for preventing the transmission of Ebola virus disease (EVD) Direct contact with infected animals or people and their bodily fluids is a primary mode of transmission. By emphasizing this measure, the nurse promotes understanding of the disease's transmission pathways.
Choice B rationale:
This statement is incorrect. While face masks are important for protecting healthcare workers when providing care to EVD patients, using them at all times is not a comprehensive prevention strategy. Proper personal protective equipment (PPE) is necessary for healthcare settings.
Choice C rationale:
This statement is incorrect. Eating cooked meat from infected animals does not build immunity against EVD. It is important to avoid handling or consuming infected animals or their products altogether to reduce the risk of infection.
Choice D rationale:
This statement is incorrect. Alcohol-based cleaners may not be sufficient to disinfect surfaces contaminated with the Ebola virus. Healthcare facilities should follow recommended guidelines for proper disinfection protocols.
Exams on Communicable Diseases
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Introduction
- Communicable diseases, also known as infectious diseases, are illnesses caused by pathogens such as bacteria, viruses, fungi, or parasites that can be transmitted from one person to another through various modes of transmission.
- Modes of Transmission:
- Direct contact: Pathogens are transmitted directly from one person to another through physical contact, e.g., touching, kissing, or sexual intercourse.
- Indirect contact: Pathogens are transmitted through a contaminated object or surface, e.g., doorknobs, utensils, or medical equipment.
- Airborne transmission: Pathogens are spread through respiratory droplets suspended in the air and inhaled by others, e.g., tuberculosis, influenza.
- Vector-borne transmission: Pathogens are transmitted through vectors such as mosquitoes or ticks, e.g., malaria, Lyme disease.
- Waterborne transmission: Pathogens are spread through contaminated water sources, e.g., cholera, giardiasis.
- Foodborne transmission: Pathogens are transmitted through contaminated food, e.g., Salmonella, E. coli.
Dengue fever

- A mosquito-borne viral infection that causes flu-like symptoms.
- A major public health problem in tropical and subtropical regions.
- Also known as “breakbone fever”, “bonecrusher disease”, and "dandy fever".
- Caused by four serotypes of flavivirus.
- Associated with severe complications such as dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS).
Causative agent
- The causative agent of dengue fever is:
- A virus in the flavivirus genus.
- A single-stranded RNA virus with a lipid envelope.
- Classified into four serotypes: DENV-1, DENV-2, DENV-3, and DENV-4.
- Antigenically distinct but genetically related.
- Capable of causing cross-reactive immune responses
Transmission cycle/vector/reservoir
- The transmission cycle/vector/reservoir of dengue fever is:
- Vector-borne: Aedes aegypti and Aedes albopictus mosquitoes.
- Transferred from mosquitoes to humans only.
- Incubation period of 8-12 days inside mosquito before it can be transferred to human.
- Incubation period of 4-10 days in human after being bitten by infected mosquito.
- Rare: organ transplant or blood transfusion.

Signs and symptoms
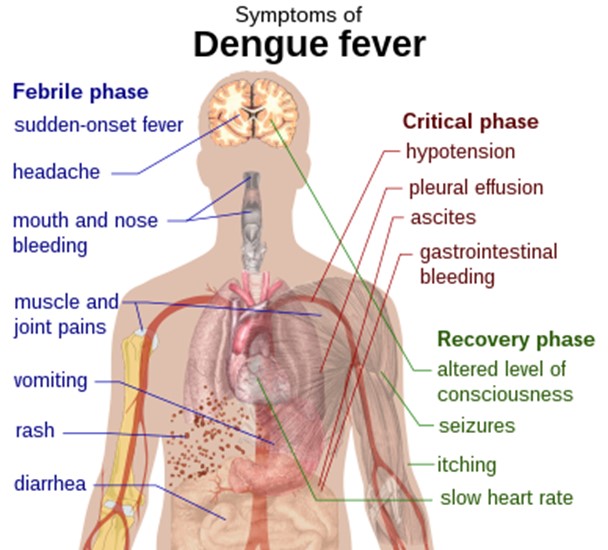
- The signs and symptoms of dengue fever are:
- Febrile phase: Sudden-onset fever, headache, mouth and nose bleeding, muscle and joint pains, vomiting, rash, diarrhea.
- Critical phase: Hypotension, pleural effusion, ascites, GI bleed.
- Recovery phase: Altered LOC, seizures, itching, slow HR.
- Complications: DHF: increased vascular permeability, thrombocytopenia, hemorrhage; DSS: severe plasma leakage, shock, organ failure.
Diagnosis and treatment
- The diagnosis and treatment of dengue fever are:
- Diagnosis: Based on clinical presentation, epidemiological history, laboratory tests.
- Laboratory tests: IgM/IgG antibody detection, viral isolation/culture, PCR, NS1 antigen detection.
- Normal ranges: Platelet count: 150000 - 450000/mm3; Hematocrit: Male: 40.7 - 50.3%; Female: 36.1 - 44.3% .
- Abnormal findings: Thrombocytopenia: platelet count < 100000/mm3; Hemoconcentration: hematocrit increase > 20% from baseline.
- Warning signs: Abdominal pain/tenderness, persistent vomiting, mucosal bleed, lethargy/restlessness, liver enlargement > 2 cm, fluid accumulation.
- Severe signs: Shock (rapid/weak pulse, narrow pulse pressure), respiratory distress (tachypnea, cyanosis), severe bleeding (hematemesis, melena), organ impairment (hepatic damage, renal failure, encephalopathy).
- Treatment: No specific treatment.
- Early detection is KEY.
- Hospital treatment: IVF, blood platelet transfusion.
- Symptomatic treatment: Antipyretics (paracetamol), analgesics (acetaminophen), fluids, rest.
- Avoidance: Anti-inflammatory drugs like ibuprofen and aspirin for they are anti-coagulants.
Nursing interventions
- The nursing interventions for patients with dengue fever are:
- Assessment: Monitor vital signs, fluid balance, hematocrit, platelet count, signs of bleeding/shock/organ failure.
- Management: Maintain adequate hydration, oxygenation, perfusion, and hemostasis.
- Hydration: Administer IVF as prescribed, monitor intake and output, assess for signs of fluid overload or dehydration.
- Oxygenation: Provide supplemental oxygen as needed, monitor SpO2 and ABGs, assess for signs of respiratory distress or failure.
- Perfusion: Monitor BP and pulse, assess for signs of shock or hypotension, elevate legs if indicated.
- Hemostasis: Transfuse blood products as ordered, monitor coagulation profile and bleeding time, apply pressure to bleeding sites, avoid IM injections or invasive procedures.
- Education: Teach patient and family about the disease process, complications, prevention measures, and follow-up care.
Prevention and control
- The prevention and control measures for dengue fever are:
- Eliminate standing water, dispose of solid waste properly, properly use insecticides.
- Use of mosquito repellent, protective clothing, and bed nets.
- Educate the public about the signs and symptoms of dengue fever and the need to seek medical attention early.
- Caution of people traveling to or from affected areas.
- No vaccine available yet.
Types and distribution
- The types and distribution of dengue fever are:
- Types: Dengue fever (DF), dengue hemorrhagic fever (DHF), dengue shock syndrome (DSS).
- DF: Mild to moderate illness with flu-like symptoms; self-limiting; recovery within 7-10 days.
- DHF: Severe illness with plasma leakage, thrombocytopenia, hemorrhage; can progress to DSS; recovery within 10-14 days with proper treatment.
- DSS: Life-threatening condition with shock, organ failure, death; requires intensive care; recovery within 14-21 days with aggressive treatment.
- Distribution: Endemic to over 100 countries throughout Asia, the Pacific, the Americas, Africa, and the Caribbean.
- Illness and death in tropics and subtropics.
- 390 million affected globally per year.
- 500000 with severe dengue who require hospitalization.
- 2.5% of affected die.
Influenza

- Influenza is a respiratory infectious disease caused by influenza viruses that belong to the family Orthomyxoviridae.
- Influenza viruses are classified into four types: A, B, C, and D. Type A and B are responsible for most human infections and seasonal epidemics. Type C causes mild respiratory illness. Type D mainly affects cattle.
- Influenza viruses are further divided into subtypes based on the combination of two surface proteins: hemagglutinin (H) and neuraminidase (N). For example, H1N1, H3N2, H5N1, etc.
- Influenza viruses undergo frequent genetic changes that result in antigenic drift (minor changes) or antigenic shift (major changes). Antigenic drift occurs every year and causes seasonal epidemics. Antigenic shift occurs occasionally and causes pandemics.
- Influenza is a global public health problem that affects millions of people every year and causes significant morbidity and mortality. According to the World Health Organization (WHO), influenza causes 3 to 5 million cases of severe illness and 290,000 to 650,000 deaths annually.
Causative agent
- The causative agent of influenza is the influenza virus, which is a single-stranded RNA virus surrounded by a lipid envelope.
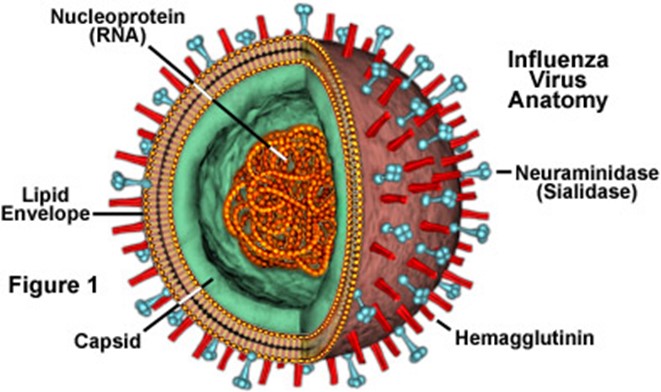
- The envelope contains two important glycoproteins: hemagglutinin (H) and neuraminidase (N). H binds to sialic acid receptors on host cells and facilitates viral entry. N cleaves sialic acid residues and enables viral release.
- The genome of the influenza virus consists of eight segments that encode for 11 proteins. The segments can be reassorted during viral replication or co-infection, leading to new strains.
- The influenza virus is sensitive to heat, acid, detergents, and disinfectants. It can survive for up to 48 hours on hard surfaces, up to 12 hours on cloth or paper, and up to 5 minutes on skin.
Transmission cycle/vector/reservoir
- The transmission cycle of influenza involves humans, animals, and the environment. Humans are the main reservoir and host of influenza viruses. Animals, such as pigs, birds, horses, dogs, cats, and bats, can also be infected by some strains of influenza viruses.
- The vector of influenza is the respiratory droplet that contains the virus. The droplet can be generated by coughing, sneezing, talking, or breathing of an infected person.
- The transmission modes of influenza include direct contact (touching or kissing an infected person), indirect contact (touching a contaminated surface or object), droplet transmission (inhaling droplets within 6 feet of an infected person), and airborne transmission (inhaling aerosols over long distances or in enclosed spaces).
- The incubation period of influenza ranges from 18 to 72 hours. The infectious period lasts from one day before the onset of symptoms to five to seven days after.
Signs and symptoms
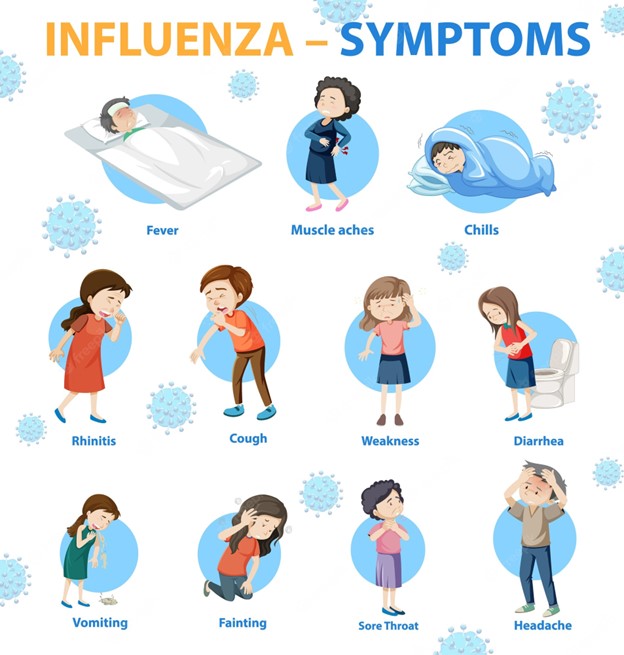
- The signs and symptoms of influenza vary depending on the type, subtype, strain, host factors, and immune status. Generally, they include fever (>38°C), chills, headache, body aches, fatigue, sore throat, dry cough, stuffy nose, substernal burning.
- Some people may also experience nausea, vomiting, diarrhea (more common in children), conjunctivitis, otitis media (middle ear infection), sinusitis, bronchitis.
- Influenza can cause complications such as viral pneumonia, bacterial pneumonia, myositis (muscle inflammation), Reye syndrome (a rare but serious condition that affects the brain and liver in children who take aspirin), myocarditis (heart inflammation), encephalitis (brain inflammation), Guillain-Barré syndrome (a rare but serious disorder that affects the nerves).
- Influenza can be fatal in some cases, especially in high-risk groups such as infants, young children, older adults (>65 years old), pregnant women, people with chronic medical conditions (such as asthma, COPD, diabetes, heart disease, kidney disease, liver disease, HIV/AIDS, cancer), and people with weakened immune systems.
Diagnosis and treatment
- The diagnosis of influenza is based on history, clinical findings, knowledge of community outbreak, and laboratory tests.
- Laboratory tests include rapid antigen tests, viral culture, polymerase chain reaction (PCR), serology.
- Rapid antigen tests can detect influenza A and B antigens in nasal or throat swabs within 15 minutes. They have high specificity but low sensitivity. They can be used for screening but not for confirmation.
- Viral culture can isolate and identify influenza viruses in respiratory specimens within 3 to 10 days. It has high sensitivity and specificity but is slow and expensive. It can be used for confirmation and subtyping.
- PCR can amplify and detect influenza viral RNA in respiratory specimens within hours. It has high sensitivity and specificity but is complex and costly. It can be used for confirmation and subtyping.
- Serology can measure the antibody response to influenza viruses in blood samples within 2 to 3 weeks. It has high sensitivity and specificity but is retrospective and requires paired samples. It can be used for epidemiological studies.
- The treatment of influenza consists of antiviral drugs and supportive care.
- Antiviral drugs can reduce the duration and severity of symptoms, prevent complications, and reduce mortality if started within 48 hours of symptom onset.
- Antiviral drugs include neuraminidase inhibitors (such as oseltamivir, zanamivir, peramivir) and polymerase inhibitors (such as baloxavir). They work by inhibiting the viral enzymes that are essential for viral replication and release.
- Supportive care includes bed rest, adequate fluid intake, analgesics, antipyretics, decongestants, expectorants, cough suppressants, antihistamines, antibiotics (if bacterial infection is suspected or confirmed), oxygen therapy, mechanical ventilation (if respiratory failure occurs).
Nursing interventions
- Nursing interventions for influenza aim to prevent transmission, manage symptoms, provide education, and monitor for complications.
- To prevent transmission, nurses should implement standard precautions (such as hand hygiene, gloves, gown) and droplet precautions (such as mask, eye protection) when caring for patients with suspected or confirmed influenza.
- Nurses should also isolate patients with influenza in a single room or cohort them with other patients with the same strain of influenza. They should limit the number of visitors and staff who enter the room. They should instruct patients and visitors to cover their mouth and nose when coughing or sneezing and dispose of tissues properly.
- To manage symptoms, nurses should assess patients’ vital signs, respiratory status, hydration status, pain level, and mental status regularly. They should administer antiviral drugs as prescribed and monitor for adverse effects. They should provide comfort measures such as cool compresses, humidified air, saline gargles, lozenges, nasal sprays.
- To provide education, nurses should teach patients and their families about the causes, modes of transmission, signs and symptoms, complications, treatment, and prevention of influenza. They should emphasize the importance of adhering to the prescribed antiviral therapy, completing the course of antibiotics (if indicated), and seeking medical attention if symptoms worsen or new symptoms appear. They should also advise patients to stay home until they are fever-free for at least 24 hours without the use of antipyretics.
- To monitor for complications, nurses should observe patients for signs of respiratory distress, hypoxia, cyanosis, tachypnea, tachycardia, crackles, wheezes, chest pain, hemoptysis, altered mental status, seizures, weakness, paralysis, or any other unusual symptoms. They should report any abnormal findings to the physician promptly and initiate appropriate interventions as ordered.
Prevention and control
- The prevention and control of influenza involve vaccination, hygiene measures, and surveillance.
- Vaccination is the most effective way to prevent influenza and its complications. The influenza vaccine is recommended for everyone aged 6 months and older every year before the flu season starts. The vaccine contains inactivated or attenuated strains of influenza viruses that are expected to circulate in a given year. The vaccine stimulates the immune system to produce antibodies that protect against infection by similar strains.
- Hygiene measures include washing hands frequently with soap and water or using alcohol-based hand sanitizer; avoiding touching eyes, nose, or mouth; avoiding close contact with sick people; covering mouth and nose with a tissue or elbow when coughing or sneezing and disposing of tissues properly; cleaning and disinfecting frequently touched surfaces and objects; and staying home when sick.
- Surveillance is the systematic collection, analysis, and dissemination of data on influenza activity, trends, and impact. Surveillance helps to monitor the epidemiology, virology, and immunology of influenza viruses; to detect and respond to outbreaks and pandemics; to evaluate the effectiveness and safety of influenza vaccines and antiviral drugs; and to inform policy and planning for influenza prevention and control.
HIV/AIDS
- HIV/AIDS is a global pandemic that affects millions of people and poses a major public health challenge.
- HIV stands for human immunodeficiency virus, which is a retrovirus that infects and destroys CD4 T cells, the key cells of the immune system.
- AIDS stands for acquired immunodeficiency syndrome, which is the final stage of HIV infection characterized by severe immunosuppression and opportunistic infections or cancers.
- HIV is transmitted through contact with infected body fluids, such as blood, semen, vaginal secretions, rectal secretions, and breast milk. The main modes of transmission are unprotected sexual intercourse, sharing injection equipment, mother-to-child transmission, occupational exposure, and blood transfusion (rarely).
- HIV infection progresses through four stages: acute primary infection, asymptomatic stage, symptomatic stage, and AIDS. The progression depends on various factors, such as viral load, CD4 count, co-infections, genetic factors, and antiretroviral therapy (ART).
- ART is the main treatment for HIV infection, which consists of a combination of drugs that target different stages of the viral life cycle. ART can reduce viral load, increase CD4 count, prevent opportunistic infections, improve quality of life, and prolong survival. However, ART is not a cure and has side effects and drug resistance issues.
- HIV testing is essential for early diagnosis and treatment initiation. There are different types of tests available, such as antibody tests, antigen tests, nucleic acid tests (NAT), and rapid tests. Testing should be done according to the CDC guidelines and with informed consent and counseling.
- HIV prevention and control strategies include behavioral interventions (such as condom use, abstinence, monogamy), biomedical interventions (such as PrEP, PEP, circumcision), harm reduction interventions (such as needle exchange programs), and structural interventions (such as laws, policies, stigma reduction).
Causative agent:
- HIV is a retrovirus that belongs to the family of lentiviruses.
- Retroviruses are RNA viruses that use reverse transcriptase to convert their RNA into DNA and integrate it into the host cell genome.
- Lentiviruses are slow viruses that cause chronic infections with long incubation periods.
- There are two types of HIV: HIV-1 and HIV-2.
- HIV-1 is more common and more virulent than HIV-2.
- HIV-1 is divided into four groups: M (main), O (outlier), N (non-M/non-O), and P.
- Group M is further divided into nine subtypes: A-D, F-H, J-K.
- Subtypes can also recombine to form circulating recombinant forms (CRFs).
- The most prevalent subtype worldwide is C
- The most prevalent subtype in the US is B
- HIV-2 is mainly found in West Africa and has a slower progression to AIDS than HIV-1
- HIV-2 is divided into eight subtypes: A-H
Transmission cycle/vector/reservoir
- The transmission cycle of HIV involves three elements: source of infection, mode of transmission, and susceptible host
- The source of infection is an individual who has HIV in their body fluids
- The amount of virus in the body fluids is called viral load
- The higher the viral load, the higher the risk of transmission
- Viral load can vary depending on the stage of infection, co-infections, treatment, and other factors
- The mode of transmission is the way that HIV is passed from the source to the host
- The main modes of transmission are
- Unprotected sexual intercourse (vaginal, anal, or oral) with an infected person
- Sharing injection equipment (needles, syringes, cookers, cotton) with an infected person
- Mother-to-child transmission (MTCT) during pregnancy, labor, delivery, or breastfeeding
- Occupational exposure (needlestick injuries, splashes) to infected blood or body fluids
- Blood transfusion or organ transplantation from an infected donor (rarely)
- The risk of transmission depends on various factors, such as
- Type and frequency of exposure
- Viral load of the source and the host
- Presence of other sexually transmitted infections (STIs) or genital ulcers
- Circumcision status of the male partner
- Use of condoms or other barrier methods
- Use of pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP)
- The susceptible host is an individual who is not infected with HIV and has a potential entry point for the virus
- The entry points are mucous membranes (such as the lining of the vagina, anus, mouth, or eyes) or breaks in the skin (such as cuts, wounds, or injections)
- The susceptibility of the host depends on various factors, such as
- Immune status and genetic factors
- Hormonal factors and contraceptive use
- Age and gender
Signs and symptoms:
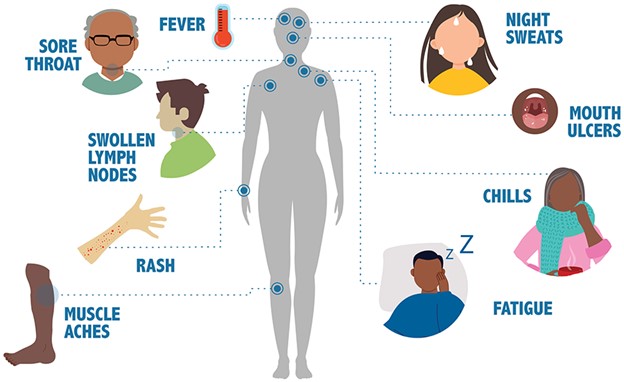
- The signs and symptoms of HIV infection vary depending on the stage of infection and the presence of opportunistic infections or cancers.
- The stages of infection are acute primary infection, asymptomatic stage, symptomatic stage, and AIDS.
- Acute primary infection occurs within 2-4 weeks after exposure and lasts for 1-4 weeks.
- It is characterized by flu-like symptoms, such as fever, headache, sore throat, rash, lymphadenopathy, myalgia, arthralgia, malaise, and night sweats.
- It is also called acute retroviral syndrome (ARS) or seroconversion illness.
- It is associated with a high viral load and a low CD4 count.
- It is often unrecognized or misdiagnosed as a common viral infection.
- Asymptomatic stage occurs after the acute primary infection and lasts for up to 10-15 years without treatment.
- It is characterized by no symptoms or mild symptoms, such as fatigue, weight loss, oral candidiasis, herpes zoster, or recurrent respiratory infections.
- It is also called chronic HIV infection or latent HIV infection.
- It is associated with a gradual decline in CD4 count and a gradual increase in viral load.
- It is often undetected unless tested for HIV antibodies or antigens.
- Symptomatic stage occurs when the CD4 count falls below 500 cells/uL or when opportunistic infections or cancers develop.
- It is characterized by persistent or severe symptoms, such as fever, diarrhea, wasting syndrome, oral hairy leukoplakia, Kaposi’s sarcoma, cervical cancer, lymphoma, tuberculosis, or pneumocystis pneumonia (PCP)
- It is also called advanced HIV disease or AIDS-related complex (ARC)
- It is associated with a rapid decline in CD4 count and a rapid increase in viral load
- It is often diagnosed by clinical criteria or laboratory tests for opportunistic infections or cancers
- AIDS occurs when the CD4 count falls below 200 cells/uL or when certain opportunistic infections or cancers are present regardless of the CD4 count
- It is characterized by life-threatening conditions that can affect any organ system in the body
- It is also called end-stage HIV disease or full-blown AIDS
- It is associated with a very low CD4 count and a very high viral load
- It is diagnosed by CDC criteria based on CD4 count and specific opportunistic infections or cancers .
- Some of the opportunistic infections or cancers that define AIDS are :
- Candidiasis of bronchi, trachea, lungs, or esophagus .
- Coccidioidomycosis, disseminated or extrapulmonary .
- Cryptococcosis, extrapulmonary .
- Cryptosporidiosis, chronic intestinal (>1 month duration) .
- Cytomegalovirus disease (other than liver, spleen, or nodes) .
- Encephalopathy, HIV-related .
- Herpes simplex: chronic ulcer(s) (>1 month duration) or bronchitis, pneumonitis, or esophagitis .
- Histoplasmosis, disseminated or extrapulmonary .
- Isosporiasis, chronic intestinal (>1 month duration)
- Kaposi’s sarcoma
- Lymphoma, Burkitt’s (or equivalent term)
- Lymphoma, immunoblastic (or equivalent term)
- Lymphoma, primary, of brain
- Mycobacterium avium complex or Mycobacterium kansasii, disseminated or extrapulmonary
- Mycobacterium tuberculosis of any site, pulmonary, disseminated, or extrapulmonary
- Mycobacterium, other species or unidentified species, disseminated or extrapulmonary
- Pneumocystis jirovecii pneumonia (PCP)
- Pneumonia, recurrent
- Progressive multifocal leukoencephalopathy (PML)
- Salmonella septicemia, recurrent
- Toxoplasmosis of brain
- Wasting syndrome due to HIV
Diagnosis and treatment
- The diagnosis of HIV infection is based on the detection of HIV antibodies, antigens, or nucleic acids in the blood or other body fluids
- There are different types of tests available for HIV diagnosis, such as
- Antibody tests: These tests detect the presence of antibodies produced by the immune system in response to HIV infection. They can be done using blood samples (from a vein or a finger prick) or oral fluid samples (from a swab of the gums). They can be performed in a laboratory or at home using rapid test kits. They have a window period of 3-12 weeks after exposure, which means they may not detect HIV infection during this time. They are also called enzyme immunoassays (EIAs), enzyme-linked immunosorbent assays (ELISAs), rapid tests, or home tests
- Antigen tests: These tests detect the presence of HIV antigens, which are proteins produced by the virus itself. They can be done using blood samples (from a vein or a finger prick). They can be performed in a laboratory or at point-of-care settings using rapid test kits. They have a shorter window period of 2-6 weeks after exposure, which means they can detect HIV infection earlier than antibody tests. They are also called p24 antigen tests or fourth-generation tests
- Nucleic acid tests (NAT): These tests detect the presence of HIV nucleic acids, which are genetic material of the virus. They can be done using blood samples (from a vein). They can only be performed in a laboratory using specialized equipment. They have the shortest window period of 10-33 days after exposure, which means they can detect HIV infection sooner than antibody or antigen tests. They are also called polymerase chain reaction (PCR) tests or viral load tests
- The treatment of HIV infection is based on the use of antiretroviral therapy (ART), which consists of a combination of drugs that target different stages of the viral life cycle
- There are six classes of antiretroviral drugs available for ART, such as
- Nucleoside reverse transcriptase inhibitors (NRTIs): These drugs block the enzyme reverse transcriptase that converts HIV RNA into DNA. Examples are abacavir (ABC), emtricitabine (FTC), lamivudine (3TC), tenofovir disoproxil fumarate (TDF), tenofovir alafenamide (TAF), and zidovudine (AZT)
- Non-nucleoside reverse transcriptase inhibitors (NNRTIs): These drugs also block the enzyme reverse transcriptase, but in a different way than NRTIs. Examples are doravirine (DOR), efavirenz (EFV), etravirine (ETR), nevirapine (NVP), and rilpivirine (RPV)
- Protease inhibitors (PIs): These drugs block the enzyme protease that cleaves HIV proteins into functional units. Examples are atazanavir (ATV), darunavir (DRV), fosamprenavir (FPV), lopinavir/ritonavir (LPV/r), saquinavir (SQV), and tipranavir (TPV)
- Integrase strand transfer inhibitors (INSTIs): These drugs block the enzyme integrase that inserts HIV DNA into the host cell genome. Examples are bictegravir (BIC), dolutegravir (DTG), elvitegravir (EVG), and raltegravir (RAL)
- Entry inhibitors: These drugs block the entry of HIV into the host cell by interfering with the binding of the virus to the cell surface receptors or co-receptors. Examples are enfuvirtide (T-20), ibalizumab (IBA), and maraviroc (MVC)
- Pharmacokinetic enhancers: These drugs enhance the pharmacokinetics of other antiretroviral drugs by inhibiting their metabolism or increasing their absorption. Examples are cobicistat (COBI) and ritonavir (RTV)
- The choice of ART regimen depends on various factors, such as
- The patient’s viral load, CD4 count, drug resistance, co-infections, comorbidities, and preferences
- The drug’s efficacy, safety, tolerability, convenience, cost, and availability
- The guidelines and recommendations from expert panels and organizations
- The goals of ART are to
- Reduce viral load to undetectable levels (<50 copies/mL)
- Increase CD4 count to normal levels (>500 cells/uL)
- Prevent opportunistic infections and cancers
- Improve quality of life and prolong survival
- Reduce transmission risk to others
- The challenges of ART are to
- Adhere to the prescribed regimen and schedule
- Monitor for side effects and drug interactions
- Manage drug resistance and treatment failure
Nursing interventions
- The nursing interventions for patients with HIV/AIDS are based on the nursing process of assessment, diagnosis, planning, implementation, and evaluation.
- The nursing assessment involves collecting data about the patient’s history, physical examination, laboratory tests, psychosocial status, and educational needs.
- The nursing diagnosis involves identifying the patient’s actual or potential problems related to HIV/AIDS, such as impaired skin integrity, risk for infection, imbalanced nutrition, chronic pain, anxiety, depression, social isolation, or noncompliance.
- Nursing planning involves setting goals and outcomes for the patient’s care, such as maintaining skin integrity, preventing infection, improving nutrition, relieving pain, reducing anxiety, enhancing coping skills, improving social support, or increasing adherence.
- The nursing implementation involves providing interventions to achieve the goals and outcomes for the patient’s care, such as :
- Education: Educating the patient about HIV/AIDS, transmission modes, prevention measures, treatment options, side effects, drug interactions, adherence strategies, monitoring parameters, signs and symptoms of opportunistic infections or cancers, and available resources and support services .
- Medication adherence: Assisting the patient with medication administration, reminders, pill boxes, refills, storage, and disposal; assessing the patient’s understanding, motivation, barriers, and facilitators of adherence; and providing counseling, feedback, and reinforcement for adherence .
- Infection prevention: Implementing standard precautions for all patients and additional precautions for patients with specific infections; educating the patient about personal hygiene, hand washing, oral care, wound care, safe sex practices, and avoiding exposure to infectious agents; administering prophylactic antibiotics or antifungals as prescribed; and monitoring for signs and symptoms of infection .
- Symptom management: Assessing the patient’s pain level, location, quality, duration, frequency, and aggravating or relieving factors; administering analgesics as prescribed and using non-pharmacological methods such as massage, heat, cold, distraction, or relaxation techniques; assessing the patient’s other symptoms such as nausea, vomiting, diarrhea, constipation, anorexia, dyspnea, cough, fatigue, insomnia, or pruritus; and providing appropriate interventions such as antiemetics, antidiarrheals, laxatives, appetite stimulants, oxygen therapy, expectorants, bronchodilators, energy conservation strategies, sleep hygiene measures, or antipruritics .
- Psychosocial support: Assessing the patient’s emotional, mental, and social well-being; providing a therapeutic relationship and active listening; encouraging the patient to express their feelings and concerns; providing information and education to reduce fear and anxiety; referring the patient to counseling or support groups as needed; and addressing issues such as stigma, discrimination, isolation, disclosure, coping skills, self-esteem, spirituality, and end-of-life care.
- The nursing evaluation involves measuring the outcomes of the patient’s care and comparing them with the goals and expected outcomes; identifying the factors that contribute to the achievement or non-achievement of the outcomes; and modifying the plan of care accordingly.
- The prevention and control of HIV/AIDS are important to reduce the morbidity, mortality, and transmission of the disease. Some of the prevention and control measures are :
- Behavioral interventions: These are actions that individuals can take to reduce their risk of acquiring or transmitting HIV, such as:
- Using condoms consistently and correctly during sexual intercourse .
- Abstaining from sexual intercourse or having a mutually monogamous relationship with an uninfected partner .
- Avoiding sharing injection equipment or using sterile equipment if injecting drugs .
- Getting tested and counseled for HIV regularly and knowing one’s status .
- Seeking treatment for other sexually transmitted infections (STIs) that can increase the risk of HIV transmission .
- Biomedical interventions: These are medical procedures or treatments that can prevent or reduce the risk of HIV infection, such as:
- Pre-exposure prophylaxis (PrEP): This is the use of antiretroviral drugs by people who are at high risk of HIV exposure before they encounter the virus
- Post-exposure prophylaxis (PEP): This is the use of antiretroviral drugs by people who have been exposed to HIV within 72 hours after the exposure
- Male circumcision: This is the surgical removal of the foreskin of the penis, which can reduce the risk of HIV acquisition by heterosexual men by about 60%
- Antiretroviral therapy (ART): This is the use of antiretroviral drugs by people who are infected with HIV to suppress viral replication, improve immune function, prevent opportunistic infections, and reduce transmission to others
- Harm reduction interventions: These are strategies that aim to minimize the negative consequences of drug use and risky behaviors, such as:
- Needle exchange programs: These are services that provide sterile injection equipment and safe disposal of used equipment to people who inject drugs
- Opioid substitution therapy: This is the use of medications such as methadone or buprenorphine to treat opioid dependence and reduce injection frequency and risk behaviors
- Supervised injection facilities: These are places where people can inject drugs under medical supervision and access other health and social services
- Structural interventions: These are policies, laws, and programs that address the social, economic, and environmental factors that influence HIV vulnerability and access to prevention and care services, such as:
- Human rights protection: This is the promotion and enforcement of human rights for people living with or affected by HIV, such as non-discrimination, confidentiality, informed consent, and access to justice
- Stigma reduction: This is the elimination or reduction of negative attitudes, beliefs, and behaviors towards people living with or affected by HIV, such as prejudice, fear, blame, or rejection
- Poverty alleviation: This is the improvement of living conditions and opportunities for people living with or affected by HIV, such as income generation, education, housing, food security, and health insurance
These prevention and control measures require a coordinated and collaborative effort from various stakeholders, such as governments, healthcare providers, community organizations, civil society groups, media, donors, and people living with or affected by HIV. Together, we can end the HIV/AIDS epidemic.
Tetanus
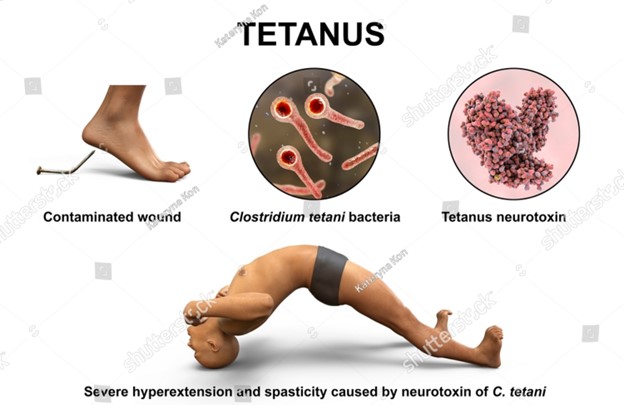
- Tetanus is a serious and potentially fatal disease caused by the microorganism Clostridium tetani, which produces a powerful neurotoxin called tetanospasmin.
- Tetanospasmin interferes with the normal functioning of the nervous system, causing painful muscle contractions and rigidity, especially of the jaw, neck, back, and abdominal muscles.
- Tetanus can affect anyone who has a wound contaminated with soil or feces that contains C. tetani spores. The spores can survive for years in the environment.
- Tetanus is also known as lockjaw because one of the early symptoms is difficulty opening the mouth due to spasms of the jaw muscles.
- Tetanus is rare in developed countries due to widespread vaccination, but it is still common in developing countries where immunization coverage is low.
- Tetanus can be prevented by receiving a series of vaccinations during childhood and booster doses every 10 years during adulthood.
- Tetanus can be treated with antitoxin therapy, antibiotics, muscle relaxants, and supportive care
Causative agent:
- The causative agent of tetanus is Clostridium tetani, a gram-positive, anaerobic, spore-forming rod-shaped bacterium.
- C. tetani produces two toxins: tetanospasmin and tetanolysin. Tetanospasmin is responsible for the clinical manifestations of tetanus, while tetanolysin may contribute to tissue damage at the site of infection.
- Tetanospasmin is a neurotoxin that binds to sites on the peripheral motor neurons, spinal cord, brain, and sympathetic nervous system. It blocks the release of inhibitory neurotransmitters such as glycine and gamma-aminobutyric acid (GABA), resulting in unopposed excitation of the muscles.
- Tetanospasmin has a high affinity for nerve tissue and can travel retrogradely along nerve fibers to reach the central nervous system (CNS). Once bound to nerve terminals, it cannot be removed by antitoxin therapy.
Transmission cycle/vector/reservoir
- The transmission cycle of tetanus involves the entry of C. tetani spores into a wound that provides an anaerobic environment for their germination and growth.
- The reservoir of C. tetani is soil and animal feces, especially those of horses and cattle. The spores can persist in the environment for years and are resistant to heat, drying, disinfectants, and antiseptics [.
- The vector of C. tetani is any object or substance that can introduce spores into a wound. Examples include nails, needles, splinters, thorns, animal bites, burns, frostbites, gangrene, crush injuries, umbilical stumps, surgical instruments, contaminated dressings, and illegal drugs [.
- Tetanus is not transmitted from person to person. However, neonatal tetanus can occur when the umbilical cord is cut with an unsterile instrument or contaminated with soil or feces[. Maternal tetanus can occur when the uterus is damaged during an induced abortion or childbirth with poor hygiene practices[.
Signs and symptoms
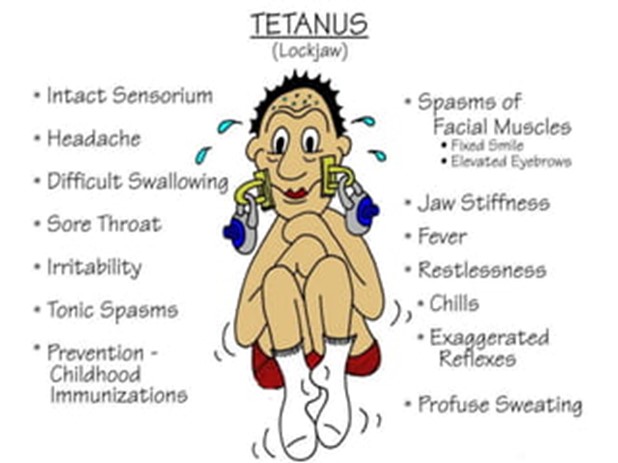
- The signs and symptoms of tetanus vary depending on the type, severity, and location of muscle involvement. -They usually appear within 3 to 21 days after exposure to C. tetani spores (incubation period), with an average of 8 days[.
- The most common type of tetanus is generalized tetanus (80% of cases), which affects all skeletal muscles[. The first symptom is usually trismus (lockjaw), which is difficulty opening the mouth due to spasms of the masseter muscles[. This is followed by risus sardonicus, which is a grimace or smile caused by spasms of the facial muscles[.
- Other symptoms of generalized tetanus include dysphagia (difficulty swallowing), opisthotonos (arching of the back), sardonic laughter (involuntary laughter), laryngeal spasm (difficulty breathing), tachycardia (rapid heart rate), hypertension (high blood pressure), diaphoresis (sweating), fever, and dysuria (difficulty urinating)[.
- The muscle spasms are triggered by stimuli such as noise, light, touch, or movement. They can last from seconds to minutes and can be very painful and exhausting. They can also lead to complications such as fractures, dislocations, rhabdomyolysis (muscle breakdown), respiratory failure, aspiration pneumonia, pulmonary embolism, and cardiac arrhythmias[.
- The mortality rate of generalized tetanus is 10% to 20%, with higher rates in neonates and elderly[.
- The second most common type of tetanus is localized tetanus (10% of cases), which affects only the muscles near the site of infection[. The symptoms are similar to those of generalized tetanus but milder and less widespread. The prognosis is better than that of generalized tetanus[.
- The rarest type of tetanus is cephalic tetanus (<1% of cases), which affects only the cranial nerves, especially the facial nerve[. The symptoms include facial paralysis, ptosis (drooping eyelid), diplopia (double vision), dysphagia, and dysarthria (slurred speech)[. Cephalic tetanus can progress to generalized tetanus or result in death due to respiratory failure[.
Diagnosis and treatment
- The diagnosis of tetanus is based on clinical features and history of exposure to a potential source of C. tetani spores. There is no specific laboratory test to confirm the presence of the toxin or the bacterium in the body.
- The treatment of tetanus consists of four components: antitoxin therapy, antibiotic therapy, muscle relaxant therapy, and supportive care.
- Antitoxin therapy involves administering human tetanus immune globulin (TIG) intramuscularly as soon as possible after diagnosis. TIG contains antibodies that neutralize the unbound toxin circulating in the blood and tissues. TIG does not affect the toxin that has already bound to nerve terminals. The dose of TIG depends on the severity of the disease and ranges from 250 to 500 units for adults and 100 to 250 units for neonates [.
- Antibiotic therapy involves administering penicillin G intravenously or metronidazole orally or intravenously for 10 to 14 days [. Antibiotics kill the C. tetani bacteria and prevent further production of toxin [. Penicillin G is preferred over metronidazole because it has a broader spectrum of activity and fewer side effects[. However, metronidazole may be used in patients who are allergic to penicillin or have renal impairment[.
- Muscle relaxant therapy involves administering benzodiazepines such as diazepam or lorazepam intravenously or intramuscularly to reduce muscle spasms and rigidity [. Benzodiazepines act by enhancing the inhibitory effects of GABA in the CNS [. They also have sedative, anxiolytic, and anticonvulsant properties that help relieve pain, anxiety, and seizures associated with tetanus[. The dose of benzodiazepines depends on the severity of the symptoms and ranges from 5 to 20 mg for adults and 0.05 to 0.3 mg/kg for neonates every 4 to 6 hours as needed[.
- Supportive care involves providing adequate hydration, nutrition, oxygenation, ventilation, analgesia, wound care, and infection control for patients with tetanus [. Supportive care also includes monitoring vital signs, fluid and electrolyte balance, renal function, cardiac function, and neurological status regularly[. Patients with severe tetanus may require intensive care unit admission, mechanical ventilation, tracheostomy, enteral or parenteral feeding, and central venous catheterization[.
Nursing interventions
- Assess the patient’s airway, breathing, and circulation (ABCs) and provide oxygen therapy, suctioning, and intubation as needed.
- Administer TIG, antibiotics, and benzodiazepines as prescribed and monitor for adverse reactions and therapeutic effects.
- Maintain a quiet, dark, and comfortable environment to minimize stimuli that can trigger muscle spasms.
- Protect the patient from injury by using padded side rails, restraints, and soft oral devices.
- Provide adequate hydration and nutrition by using intravenous fluids, nasogastric tube feeding, or parenteral nutrition as indicated.
- Manage pain by using non-pharmacological methods such as massage, relaxation techniques, and distraction and pharmacological methods such as opioids and non-steroidal anti-inflammatory drugs (NSAIDs) as prescribed.
- Educate the patient and family about the disease, treatment, prognosis, and prevention of tetanus. Emphasize the importance of completing the vaccination schedule and receiving booster doses every 10 years.
- Refer the patient and family to appropriate resources such as social workers, counselors, support groups, and rehabilitation services as needed.
Prevention and control of tetanus
- Are mainly based on immunization, wound care, and education.
- Immunization involves receiving a series of vaccinations that contain tetanus toxoid, which is a weakened form of the tetanus toxin that stimulates the production of antibodies against it. The recommended vaccination schedule consists of five doses of diphtheria-tetanus-pertussis (DTP) vaccine during childhood, followed by a booster dose of tetanus-diphtheria (Td) vaccine every 10 years during adulthood [. Pregnant women should receive a dose of tetanus-diphtheria-acellular pertussis (Tdap) vaccine during each pregnancy to protect themselves and their newborns from tetanus [.
- Wound care involves cleaning and debriding any wound that may be contaminated with C. tetani spores as soon as possible [. Antiseptics such as iodine, hydrogen peroxide, or alcohol should be applied to the wound to reduce the bacterial load. Tetanus prophylaxis should be given to patients who have not completed their vaccination schedule or whose vaccination status is unknown [. Tetanus prophylaxis consists of administering TIG and/or Td vaccine depending on the type and severity of the wound and the patient’s immunization history [.
- Education involves raising awareness and providing information about the causes, symptoms, treatment, and prevention of tetanus to the general public and health care workers [. Education also involves promoting safe and hygienic practices such as using sterile instruments for cutting umbilical cords, delivering babies in clean facilities, disposing of animal feces properly, and avoiding contact with soil or feces that may contain C. tetani spores
Chickenpox/Shingles

- Chickenpox and shingles are both caused by the varicella-zoster virus (VZV), a type of herpesvirus that infects humans.
- Chickenpox is a highly contagious infection that usually occurs in childhood, characterized by a generalized vesicular rash, fever, malaise, and pruritus.
- Shingles is a reactivation of the latent VZV in the dorsal root ganglia of the sensory nerves, resulting in a painful, unilateral, dermatomal rash that follows the course of the affected nerve.
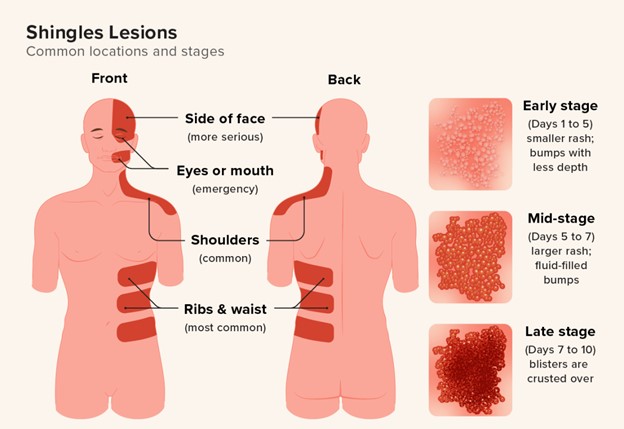
- Both chickenpox and shingles can have serious complications, such as bacterial skin infections, eye infections, pneumonia, encephalitis, postherpetic neuralgia (PHN), and increased risk of stroke.
- The best way to prevent chickenpox and shingles is to get vaccinated with the varicella vaccine (Varivax) or the herpes zoster vaccine (Shingrix).
Causative agent
- VZV is a double-stranded DNA virus that belongs to the subfamily Alphaherpesvirinae, which also includes herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2).
- VZV has a high affinity for human cells and cannot infect other animals. It replicates in the epithelial cells of the skin and mucous membranes, as well as in the lymphocytes and monocytes of the blood and lymphatic system.
- VZV can remain dormant in the sensory nerve cells for years or decades after the primary infection, until it is reactivated by various triggers, such as stress, immunosuppression, aging, or trauma.
Transmission cycle/vector/reservoir
- The primary reservoir of VZV is humans. There is no animal or environmental source of infection.
- The transmission cycle of VZV involves two stages: primary infection (chickenpox) and reactivation (shingles).
- Primary infection occurs when a susceptible person comes into contact with respiratory droplets or fluid from the vesicles of an infected person. The incubation period ranges from 10 to 21 days, with an average of 14 days. The infectious period lasts from 1 to 2 days before the rash appears until all lesions are crusted over, usually about 5 to 7 days after onset. The secondary attack rate among household contacts is about 90%.
- Reactivation occurs when the latent virus in the nerve cells becomes active again and travels along the nerve fibers to the skin. The prodromal period lasts from 3 to 4 days before the rash appears, with symptoms such as pain, tingling, burning, or itching in the affected area. The infectious period lasts from the onset of rash until all lesions are crusted over, usually about 7 to 10 days. The risk of transmission is lower than primary infection, but still possible if direct contact with vesicles occurs. Reactivation can occur more than once in a person’s lifetime.
Signs and symptoms
- Chickenpox presents with a prodrome of fever, headache, malaise, anorexia, and pharyngitis, followed by a generalized pruritic rash that progresses from macules to papules to vesicles to pustules to crusts. The rash typically starts on the face and trunk and spreads to the extremities. It may also involve the scalp, mucous membranes, palms, soles, and genitals. The number of lesions varies from a few to hundreds. The rash usually lasts for about 10 days. Complications include secondary bacterial infections (such as impetigo or cellulitis), otitis media, pneumonia, encephalitis, cerebellar ataxia, Reye syndrome (in children who take aspirin), hemorrhagic varicella (in immunocompromised patients), congenital varicella syndrome (in pregnant women who contract chickenpox in the first trimester), and neonatal varicella (in newborns whose mothers contract chickenpox within 5 days before or after delivery).
- Shingles presents with a prodrome of pain, tingling, burning, or itching in the affected dermatome, followed by a unilateral, clustered, vesicular rash that follows the course of the sensory nerve. The rash usually involves the thoracic, cervical, or trigeminal nerves, but can affect any nerve. The rash may be accompanied by fever, malaise, headache, and lymphadenopathy. The rash usually lasts for about 7 to 10 days. Complications include postherpetic neuralgia (PHN), which is persistent or recurrent pain in the affected area that lasts for more than a month after the rash heals. PHN can be severe and debilitating, affecting the quality of life and mental health of the patient. Other complications include bacterial superinfection, eye involvement (such as keratitis, uveitis, or glaucoma), cranial nerve palsies (such as Bell’s palsy or Ramsay Hunt syndrome), motor weakness, meningitis, encephalitis, myelitis, vasculitis, and stroke.
Diagnosis and treatment
- Chickenpox is usually diagnosed based on the clinical presentation and history of exposure. Laboratory tests are not routinely done but may be indicated in cases of atypical presentation, immunocompromised patients, pregnant women, or neonates. The tests include Tzanck smear and viral culture from vesicle fluid, polymerase chain reaction (PCR) from blood or cerebrospinal fluid (CSF), serology for IgM and IgG antibodies, and direct fluorescent antibody (DFA) staining from skin lesions.
- Shingles is also usually diagnosed based on the clinical presentation and history of previous chickenpox. Laboratory tests are similar to those for chickenpox but may be more useful in confirming the diagnosis and ruling out other causes of rash or pain. The tests include Tzanck smear and viral culture from vesicle fluid, PCR from blood or CSF, serology for IgM and IgG antibodies, and DFA staining from skin lesions.
- Treatment for chickenpox is mainly supportive and symptomatic. Antiviral drugs (such as acyclovir, valacyclovir, or famciclovir) may be given to reduce the duration and severity of symptoms, especially if initiated within 24 hours of rash onset. Antiviral drugs are recommended for high-risk groups, such as immunocompromised patients, pregnant women, neonates, adults, and patients with chronic lung or skin diseases. Antihistamines (such as diphenhydramine or hydroxyzine) may be given to relieve pruritus. Antipyretics (such as acetaminophen or ibuprofen) may be given to reduce fever and pain. Aspirin should be avoided in children due to the risk of Reye syndrome. Antipruritic/protectant/astringent agents (such as calamine lotion, colloidal oatmeal bath, or Domeboro solution) may be applied to the skin lesions to soothe and dry them. Fingernails should be trimmed and gloves worn to prevent scratching and secondary infection.
- Treatment for shingles is similar to that for chickenpox, but with a higher dose and longer duration of antiviral drugs. Antiviral drugs are most effective if started within 72 hours of rash onset. They can reduce the risk of complications such as PHN and eye involvement. Analgesics (such as acetaminophen, ibuprofen, or opioids) may be given to control pain. Adjuvant drugs (such as tricyclic antidepressants, anticonvulsants, or topical capsaicin) may be added to treat neuropathic pain or PHN. Corticosteroids may be used in some cases to reduce inflammation and edema. Antipruritic/protectant/astringent agents may be applied to the skin lesions as well.
Prevention and control
- The most effective way to prevent chickenpox and shingles is to get vaccinated with the varicella vaccine (Varivax) or the herpes zoster vaccine (Shingrix).
- The varicella vaccine is a live attenuated vaccine that is given in two doses, usually at 12 to 15 months and 4 to 6 years of age. It can also be given to adolescents and adults who have not had chickenpox or been vaccinated. The vaccine is contraindicated in pregnant women, immunocompromised patients, and people who are allergic to gelatin or neomycin. The vaccine has a high efficacy of about 90% in preventing chickenpox and 70% in preventing shingles. The vaccine can also reduce the severity and duration of symptoms if infection occurs. The vaccine may cause mild side effects such as fever, rash, injection site reactions, or lymphadenopathy. Serious adverse events such as anaphylaxis, encephalitis, or thrombocytopenia are rare.
- The herpes zoster vaccine is a recombinant subunit vaccine that is given in two doses, usually at 50 years of age or older. It can also be given to people who have had chickenpox or shingles before. The vaccine is contraindicated in pregnant women, immunocompromised patients, and people who are allergic to any component of the vaccine. The vaccine has a high efficacy of about 90% in preventing shingles and PHN. The vaccine can also reduce the severity and duration of symptoms if reactivation occurs. The vaccine may cause mild side effects such as fever, headache, fatigue, injection site reactions, or myalgia. Serious adverse events such as anaphylaxis or Guillain-Barré syndrome are rare.
- Other prevention and control measures include:
- Practicing good hand hygiene and respiratory etiquette to avoid spreading the virus.
- Avoid sharing personal items such as towels, utensils, or clothing with infected people.
- Covering the mouth and nose when coughing or sneezing and disposing of tissues properly.
- Cleaning and disinfecting surfaces and objects that may be contaminated with the virus.
- Excluding infected people from school or work until all lesions are crusted over.
- Reporting cases of chickenpox or shingles to the local health authorities.
Types and distribution
- Chickenpox and shingles are both endemic diseases that occur worldwide. However, their incidence and prevalence vary depending on the geographic region, climate, population density, vaccination coverage, and socioeconomic factors.
- Chickenpox is more common in temperate regions than in tropical regions. It is also more common in winter and spring than in summer and autumn. It affects mostly children under 10 years of age, but can occur at any age. Before the introduction of the varicella vaccine in 1995, there were about 4 million cases of chickenpox per year in the United States, with about 100 deaths. After the vaccination program was implemented, there was a dramatic decline in the incidence of chickenpox by about 90%, with less than 4000 cases per year in 2015.
- Shingles is more common in older adults than in younger adults or children. It affects about 1 in 3 people in their lifetime. The risk of shingles increases with age, immunosuppression, stress, trauma, or other factors that impair the immune system. There are about 1 million cases of shingles per year in the United States, with about 20% of them developing PHN. Shingles can also occur in vaccinated individuals, but usually with milder symptoms and lower risk of complications.
Complications and risk factors
- Chickenpox and shingles can both cause serious complications that may require hospitalization or result in death. Some of the common complications are:
- Bacterial skin infections: These can occur when bacteria invade the broken skin from scratching or trauma. They can cause impetigo (superficial infection), cellulitis (deep infection), abscess (pus collection), necrotizing fasciitis (flesh-eating disease), or sepsis (blood infection). They can be treated with antibiotics and wound care.
- Eye infections: These can occur when VZV infects the eye or the surrounding structures. They can cause keratitis (corneal inflammation), uveitis (iris inflammation), glaucoma (increased eye pressure), or blindness. They can be treated with antiviral drugs, corticosteroids, and eye drops.
- Pneumonia: This can occur when VZV infects the lungs or the respiratory tract. It can cause cough, dyspnea, chest pain, fever, or hypoxia. It can be treated with antiviral drugs, oxygen therapy, and antibiotics if bacterial superinfection is present.
- Encephalitis: This can occur when VZV infects the brain or the meninges. It can cause headache, confusion, seizures, coma, or death. It can be treated with antiviral drugs, corticosteroids, and supportive care.
- Cerebellar ataxia: This can occur when VZV affects the cerebellum, which is responsible for coordination and balance. It can cause dizziness, nystagmus (involuntary eye movements), dysarthria (slurred speech), or gait disturbance. It usually resolves spontaneously within weeks or months.
- Reye syndrome: This can occur when children who have chickenpox take aspirin or other salicylates. It can cause liver failure and encephalopathy. It can be prevented by avoiding aspirin in children with viral infections.
Tuberculosis
- Tuberculosis (TB) is a chronic infectious disease caused by bacteria called Mycobacterium tuberculosis (M. tuberculosis) .
- TB mainly affects the lungs (pulmonary TB), but it can also affect other organs and tissues (extrapulmonary TB), such as the kidneys, bones, lymph nodes, and meninges .
- TB is spread by respiratory droplets that are released when a person with active pulmonary TB coughs, sneezes, laughs, or speaks . The droplets can remain airborne for minutes to hours until they are inhaled by another person .
- TB is not spread by contact with objects or surfaces that are contaminated with the bacteria, such as hands, books, glasses, or dishes .
- TB infection occurs when a person is exposed to M. tuberculosis and develops a cellular immune response that limits the multiplication and spread of the bacteria . However, some bacteria may remain dormant (latent) in the body for years or decades without causing any symptoms or disease .
- TB disease occurs when the latent bacteria become active and cause tissue damage and inflammation . This can happen when the immune system is weakened by factors such as HIV infection, malnutrition, diabetes, aging, or corticosteroid use .
- TB is a global health problem that affects millions of people every year, especially in low- and middle-income countries where access to diagnosis and treatment is limited
Causative agent
- M. tuberculosis is a rod-shaped, acid-fast, aerobic bacterium that belongs to the genus Mycobacterium.
- M. tuberculosis has a complex cell wall that contains mycolic acid, which makes it resistant to many antibiotics and disinfectants.
- M. tuberculosis can survive for long periods in dry and dark environments, such as dust, soil, and clothing.
- M. tuberculosis can also form biofilms, which are communities of bacteria that adhere to surfaces and are protected by a matrix of extracellular substances.
- M. tuberculosis has several virulence factors that help it evade the host immune system, such as cord factor, tuberculin, and lipoarabinomannan.
Transmission cycle/vector/reservoir
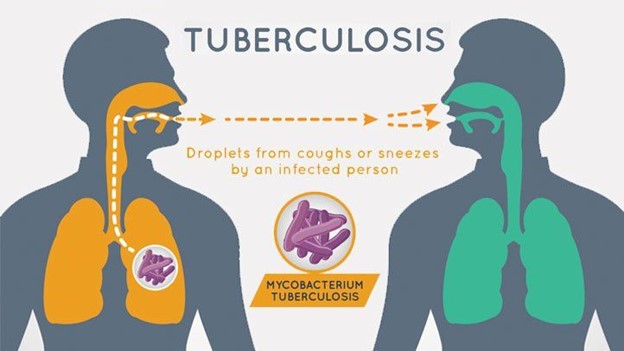
- The transmission cycle of TB involves three stages: exposure, infection, and disease.
- Exposure occurs when a person inhales M. tuberculosis from the respiratory droplets of an infectious source, such as a person with active pulmonary TB or a person with latent TB who is undergoing reactivation.
- Infection occurs when the inhaled bacteria reach the alveoli of the lungs and are engulfed by macrophages, which are immune cells that try to kill the bacteria. However, some bacteria survive and multiply inside the macrophages, forming granulomas, which are nodules of infected tissue surrounded by immune cells
Disease:
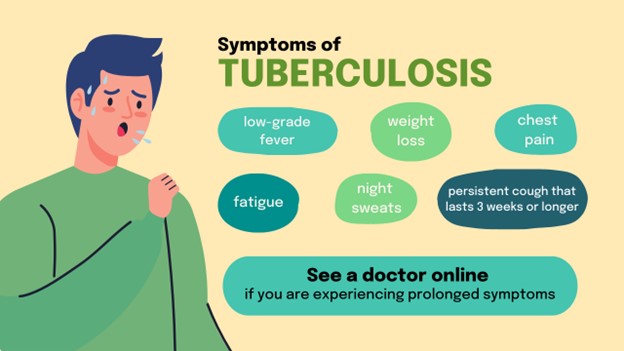
- Disease occurs when the granulomas break down and release the bacteria into the bloodstream or the airways, causing systemic or pulmonary symptoms.
- The symptoms of TB depend on the type and location of the infection, but they generally include fever, night sweats, weight loss, fatigue, cough, hemoptysis (coughing up blood), chest pain, and dyspnea (difficulty breathing).
- The most common type of TB is pulmonary TB, which affects the lungs and accounts for about 85% of all cases. Pulmonary TB can be classified into primary, secondary, or miliary TB .
- Primary TB occurs when a person is exposed to M. tuberculosis for the first time and develops a primary complex, which consists of a small lesion in the lung (Ghon focus) and enlarged lymph nodes in the hilum (Ghon complex). Primary TB is usually asymptomatic or mild, and it may heal spontaneously or progress to latent or active TB.
- Secondary TB occurs when a person with latent TB experiences reactivation of the bacteria due to a weakened immune system or other factors. Secondary TB usually affects the upper lobes of the lungs and causes cavitation, which is the formation of holes in the lung tissue due to necrosis. Secondary TB is more likely to cause severe symptoms and complications, such as bronchopleural fistula, pneumothorax, or pleural effusion.
- Miliary TB occurs when the bacteria spread through the bloodstream and cause multiple small lesions in various organs, such as the liver, spleen, bone marrow, and meninges. Miliary TB is a life-threatening condition that causes systemic symptoms, such as fever, chills, anorexia, hepatosplenomegaly (enlarged liver and spleen), and meningitis.
- Extrapulmonary TB occurs when the bacteria affect organs other than the lungs, such as the kidneys, bones, lymph nodes, and meninges. Extrapulmonary TB can cause various symptoms depending on the organ involved, such as hematuria (blood in urine), renal failure, osteomyelitis (bone infection), arthritis (joint inflammation), lymphadenitis (swollen lymph nodes), and meningitis. Extrapulmonary TB can also occur in conjunction with pulmonary TB or as a result of military dissemination.
Diagnosis and treatment
- The diagnosis of TB is based on a combination of clinical, microbiological, radiological, and immunological tests.
- The most common test for TB infection is the tuberculin skin test (TST), also known as the Mantoux test or the purified protein derivative (PPD) test. The TST involves injecting a small amount of tuberculin, which is a protein extract from M. tuberculosis, into the forearm of the person and measuring the induration (swelling) after 48 to 72 hours. A positive TST indicates that the person has been exposed to M. tuberculosis and has developed a cellular immune response, but it does not differentiate between latent and active TB or between TB and other mycobacterial infections. A negative TST does not rule out TB, especially in immunocompromised persons or those with recent exposure.
- Another test for TB infection is the interferon-gamma release assay (IGRA), which measures the production of interferon-gamma by the person’s blood cells in response to M. tuberculosis antigens. The IGRA is more specific than the TST, as it does not cross-react with other mycobacteria or with the bacille Calmette-Guérin (BCG) vaccine, which is a live attenuated strain of M. bovis that is used to prevent TB in some countries. The IGRA is also more sensitive than the TST in detecting latent TB, but it may also give false-negative results in immunocompromised persons or those with recent exposure.
- The definitive diagnosis of TB disease requires the identification and culture of M. tuberculosis from sputum, body fluids, or tissue samples. Sputum smear microscopy is a rapid and inexpensive method that uses a stain such as Ziehl-Neelsen or auramine-rhodamine to detect acid-fast bacilli in sputum samples. However, sputum smear microscopy has low sensitivity and specificity, as it may miss up to 50% of cases and may also detect non-tuberculous mycobacteria. The sputum culture is a more reliable method that uses a solid or liquid medium to grow M. tuberculosis from sputum samples. However, the sputum culture takes several weeks to obtain results and may also be contaminated by other bacteria or fungi.
- The chest x-ray is a useful tool that can reveal abnormalities in the lungs caused by TB, such as infiltrates, cavities, nodules, calcifications, or pleural effusions . However, the chest x-ray cannot confirm or exclude TB, as it may also show similar findings in other conditions such as pneumonia, lung cancer, or fungal infections .
- The treatment of TB involves a combination of antibiotics that are given for at least six months to kill the bacteria and prevent resistance . The standard regimen consists of four drugs: isoniazid (INH), rifampin (RIF), ethambutol (EMB), and pyrazinamide (PZA) for the first two months, followed by INH and RIF for the next four months . However, the regimen may vary depending on the type and severity of TB, the presence of drug resistance, the presence of co-infections such as HIV, and the patient’s compliance and tolerance .
- The treatment of TB requires close monitoring and supervision by health care providers to ensure adherence, effectiveness, and safety . The patient should take the medications regularly and complete the full course of therapy to prevent relapse or resistance . The patient should also undergo periodic sputum tests to check for bacteriological conversion, which is the clearance of M. tuberculosis from sputum samples . The patient should also report any adverse effects of the medications, such as hepatotoxicity (liver damage), peripheral neuropathy (nerve damage), optic neuritis (eye inflammation), or skin rash .
- The treatment of TB may also require adjunctive measures such as surgery, corticosteroids, or nutritional support depending on the complications or co-morbidities of the disease . For example, surgery may be indicated for patients with extensive lung damage, bronchopleural fistula, pneumothorax, or hemoptysis . Corticosteroids may be beneficial for patients with tuberculous meningitis, pericarditis, or pleurisy . Nutritional support may be needed for patients with malnutrition, anemia, or wasting syndrome .
Nursing interventions
- The nursing interventions for TB patients aim to prevent transmission, promote recovery, and provide support.
- To prevent transmission, the nurse should implement airborne precautions, such as wearing a N95 respirator mask, placing the patient in a negative pressure room with adequate ventilation, and limiting the patient’s contact with other people. The nurse should also educate the patient and the family about the mode of transmission, the signs and symptoms of TB, and the importance of adhering to the treatment regimen. The nurse should also encourage the patient to cover the mouth and nose when coughing or sneezing, dispose of tissues properly, and wash hands frequently.
- To promote recovery, the nurse should monitor the patient’s vital signs, weight, sputum samples, chest x-rays, and laboratory tests to assess the response to treatment and identify any complications or adverse effects. The nurse should also administer the prescribed medications as ordered and observe for any signs of drug resistance, toxicity, or intolerance. The nurse should also provide nutritional support, fluid therapy, oxygen therapy, chest physiotherapy, or pain management as needed. The nurse should also encourage the patient to rest, avoid smoking and alcohol, and participate in physical activity as tolerated.
- To provide support, the nurse should address the patient’s psychosocial needs, such as coping with the diagnosis, stigma, isolation, anxiety, depression, or fear. The nurse should also provide emotional support, counseling, or referral to mental health services as needed. The nurse should also involve the patient in the care plan and respect the patient’s preferences, beliefs, and values. The nurse should also advocate for the patient’s rights and access to health care resources.
Prevention and control
- The prevention and control of TB involves a combination of strategies that target both the individual and the population level.
- At the individual level, the prevention of TB includes vaccination, chemoprophylaxis, and screening.
- Vaccination involves administering the BCG vaccine to infants or children who are at high risk of TB exposure or infection. The BCG vaccine can reduce the risk of developing severe forms of TB, such as miliary TB or tuberculous meningitis. However, the BCG vaccine has variable efficacy and may not prevent pulmonary TB or reactivation of latent TB. The BCG vaccine may also interfere with the TST results and cause false-positive reactions.
- Chemoprophylaxis involves administering INH or other drugs to persons who have latent TB infection or who are close contacts of active TB cases. Chemoprophylaxis can prevent the progression from latent to active TB and reduce the risk of transmission. However, chemoprophylaxis requires long-term adherence and monitoring for adverse effects and drug resistance.
- Screening involves testing persons who have symptoms suggestive of TB or who belong to high-risk groups, such as healthcare workers, immigrants, prisoners, homeless people, or HIV-positive people. Screening can facilitate early diagnosis and treatment of TB and interrupt the transmission cycle. Screening can be done using TST, IGRA
- Screening can be done using TST, IGRA, sputum smear microscopy, sputum culture, or chest x-ray, depending on the availability and cost-effectiveness of the methods.
- At the population level, the control of TB includes surveillance, reporting, contact tracing, and directly observed therapy (DOT).
- Surveillance involves collecting and analyzing data on the incidence, prevalence, mortality, and trends of TB in a given area or country. Surveillance can help identify the burden, distribution, and determinants of TB and evaluate the impact and effectiveness of TB control programs.
- Reporting involves notifying the local or national health authorities about any confirmed or suspected cases of TB. Reporting can help monitor the epidemiology and transmission of TB and ensure timely and appropriate treatment and follow-up of TB patients.
- Contact tracing involves identifying and testing persons who have been in close contact with an active TB case. Contact tracing can help detect and treat latent or active TB among contacts and prevent further spread of the disease .
- DOT involves observing and verifying that the TB patient takes the prescribed medications as ordered. DOT can improve adherence, cure rates, and outcomes of TB treatment and reduce the risk of resistance, relapse, or transmission.
Types and distribution
- There are several types of TB that differ in their epidemiology, pathogenesis, clinical presentation, diagnosis, and treatment. Some of the types are:
- Drug-susceptible TB: TB that is caused by M. tuberculosis strains that are sensitive to the standard first-line drugs (INH, RIF, EMB, PZA).
- Drug-resistant TB: TB that is caused by M. tuberculosis strains that are resistant to one or more of the first-line drugs. Drug-resistant TB can be further classified into:
- Multidrug-resistant TB (MDR-TB): TB that is resistant to at least INH and RIF.
- Extensively drug-resistant TB (XDR-TB): TB that is resistant to INH, RIF, any fluoroquinolone, and at least one of the second-line injectable drugs (amikacin, kanamycin, or capreomycin).
- Rifampicin-resistant TB (RR-TB): TB that is resistant to RIF alone or in combination with other drugs.
- Latent TB infection (LTBI): A condition in which a person has been infected with M. tuberculosis but does not have any symptoms or signs of active disease. LTBI can be detected by TST or IGRA but not by sputum tests or chest x-rays. LTBI can remain dormant for years or decades or progress to active disease at any time.
- Active TB disease: A condition in which a person has symptoms or signs of TB and evidence of M. tuberculosis in sputum samples, body fluids, or tissue samples. Active TB disease can be classified into pulmonary or extrapulmonary depending on the organ affected.
- The distribution of TB varies by region, country, and population group depending on the socioeconomic, environmental, biological, and behavioral factors that influence the exposure, infection, and disease progression of M. tuberculosis. According to the World Health Organization (WHO), in 2020 :
- There were an estimated 10 million new cases of TB worldwide, with 1.4 million deaths from TB.
- The regions with the highest burden of TB were Africa, South-East Asia, and Western Pacific.
- The countries with the highest number of TB cases were India, Indonesia, China, Nigeria, Pakistan, Bangladesh, Philippines, South Africa, Ethiopia, and Viet Nam.
- The countries with the highest incidence rate of TB per 100,000 population were Lesotho, South Africa, Namibia, Mozambique, Eswatini, Philippines, Kiribati, Djibouti, Cambodia, and Zimbabwe .
- There were an estimated 3.6 million missing cases of TB that were not diagnosed or reported to health authorities .
- There were an estimated 465 thousand new cases of MDR/RR-TB worldwide, with only 39% enrolled in treatment .
- There were an estimated 1.2 million new cases of HIV-associated TB worldwide
Hepatitis
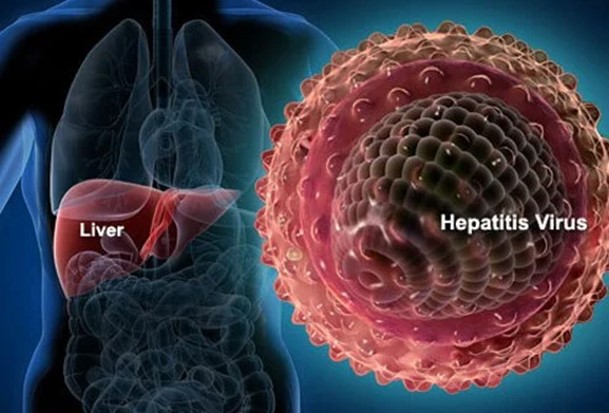
- Hepatitis is an inflammation of the liver that can be caused by various factors, such as viruses, bacteria, parasites, drugs, toxins, or autoimmune disorders.
- Hepatitis can be classified into acute or chronic, depending on the duration of the inflammation.
- Acute hepatitis is usually self-limiting and lasts less than six months, while chronic hepatitis persists for more than six months and can lead to liver cirrhosis, liver failure, or liver cancer.
- Hepatitis can also be classified into different types based on the causative agent, such as hepatitis A, B, C, D, E, G, or other non-viral causes.
- Each type of hepatitis has different characteristics, modes of transmission, clinical manifestations, diagnosis, treatment, and prevention strategies.
Causative agent:
- Hepatitis A is caused by a non-enveloped single-stranded RNA virus that belongs to the Picornaviridae family.
- Hepatitis B is caused by a partially double-stranded DNA virus that belongs to the Hepadnaviridae family.
- Hepatitis C is caused by an enveloped single-stranded RNA virus that belongs to the Flaviviridae family.
- Hepatitis D is caused by a defective single-stranded RNA virus that requires the presence of hepatitis B virus for replication and infection.
- Hepatitis E is caused by a non-enveloped single-stranded RNA virus that belongs to the Hepeviridae family.
- Hepatitis G is caused by an enveloped single-stranded RNA virus that belongs to the Flaviviridae family.
- Other non-viral causes of hepatitis include bacteria (such as leptospirosis or syphilis), parasites (such as malaria or toxoplasmosis), drugs (such as acetaminophen or isoniazid), toxins (such as alcohol or mushrooms), or autoimmune disorders (such as autoimmune hepatitis or primary biliary cholangitis).
Transmission cycle/vector/reservoir
- Hepatitis A is transmitted mainly through the fecal-oral route, either by direct contact with infected persons or by ingestion of contaminated food or water. It can also be transmitted through blood transfusion, needle sharing, or sexual contact. The reservoirs are humans and some animals (such as monkeys or chimpanzees).
- Hepatitis B is transmitted mainly through parenteral exposure to infected blood or body fluids, such as needle sharing, blood transfusion, organ transplantation, tattooing, piercing, acupuncture, or sexual contact. It can also be transmitted from mother to child during pregnancy, delivery, or breastfeeding. The reservoir is humans.
- Hepatitis C is transmitted mainly through parenteral exposure to infected blood or body fluids, such as needle sharing, blood transfusion, organ transplantation, tattooing, piercing, acupuncture, or sexual contact. It can also be transmitted from mother to child during pregnancy or delivery. The reservoir is humans.
- Hepatitis D is transmitted mainly through parenteral exposure to infected blood or body fluids, such as needle sharing, blood transfusion, organ transplantation, tattooing, piercing, acupuncture or sexual contact. It can only infect people who are already infected with hepatitis B. The reservoir is humans.
- Hepatitis E is transmitted mainly through the fecal-oral route, either by direct contact with infected persons or by ingestion of contaminated food or water. It can also be transmitted from mother to child during pregnancy or delivery. The reservoirs are humans and some animals (such as pigs or deer).
- Hepatitis G is transmitted mainly through parenteral exposure to infected blood or body fluids, such as needle sharing, blood transfusion, organ transplantation, tattooing, piercing, acupuncture, or sexual contact. It can also be transmitted from mother to child during pregnancy or delivery. The reservoir is humans.
- Other non-viral causes of hepatitis are transmitted through various routes depending on the specific agent, such as ingestion, inhalation, injection, or contact.
Signs and Symptoms
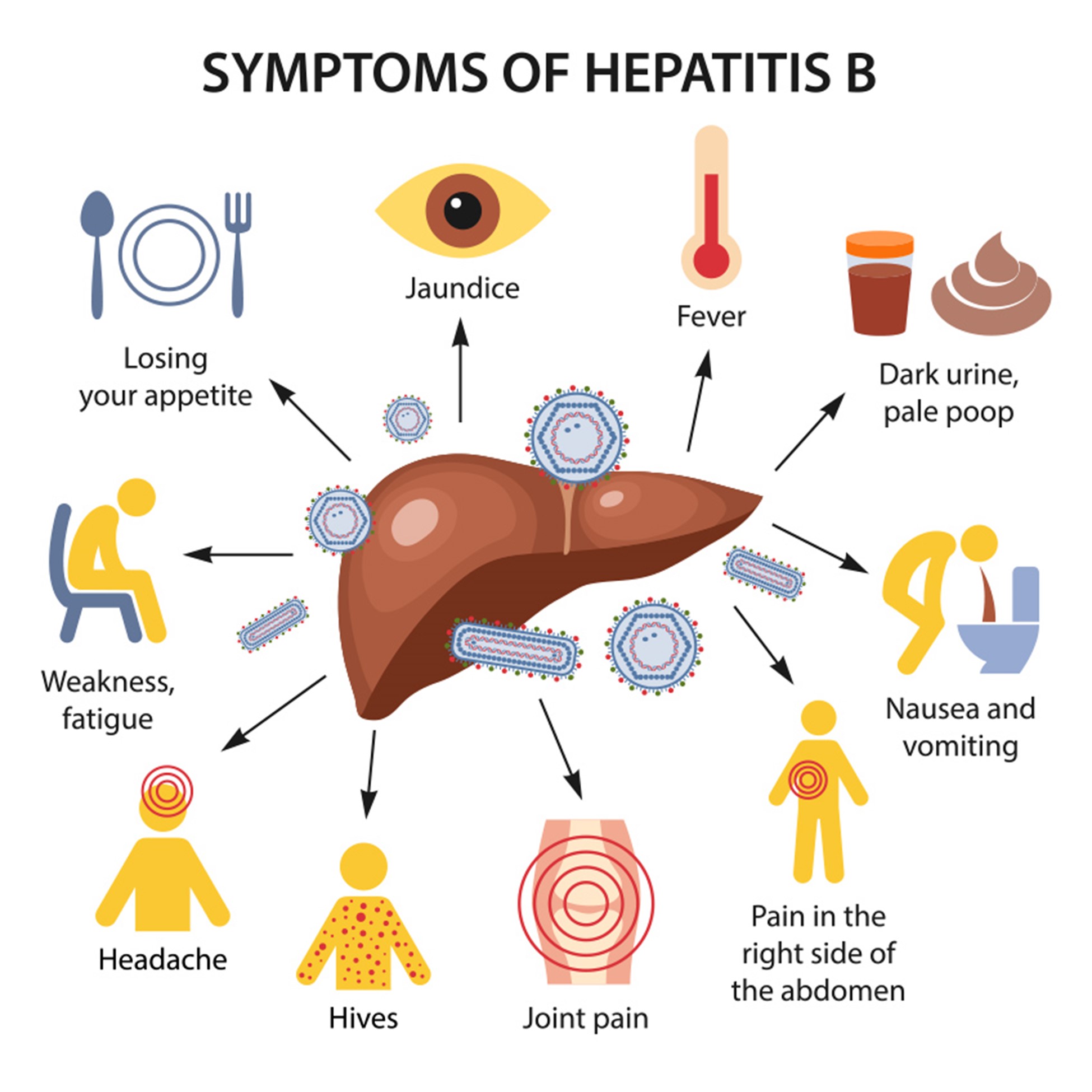
- Hepatitis A usually causes a mild and self-limiting illness that lasts for a few weeks. The signs and symptoms include fever, malaise, anorexia, nausea, vomiting, abdominal pain, dark urine, clay-colored stools, and jaundice. Some people may be asymptomatic or have a prolonged or relapsing course.
- Hepatitis B can cause either an acute or a chronic infection. The acute infection usually lasts for a few months and may be asymptomatic or cause mild to severe symptoms similar to hepatitis A. The chronic infection can be either inactive (with normal liver function tests and low viral load) or active (with abnormal liver function tests and high viral load). The active chronic infection can lead to complications such as cirrhosis, liver failure, or liver cancer.
- Hepatitis C can also cause either an acute or a chronic infection. The acute infection usually lasts for a few weeks and is often asymptomatic or causes mild symptoms similar to hepatitis A. The chronic infection can be either inactive (with normal liver function tests and low viral load) or active (with abnormal liver function tests and high viral load). The active chronic infection can lead to complications such as cirrhosis, liver failure, or liver cancer.
- Hepatitis D can cause either an acute or a chronic infection. The acute infection usually occurs as a co-infection with hepatitis B and causes severe symptoms similar to hepatitis A. The chronic infection usually occurs as a super-infection in people who already have chronic hepatitis B and causes rapid progression to cirrhosis, liver failure, or liver cancer.
- Hepatitis E usually causes a mild and self-limiting illness that lasts for a few weeks. The signs and symptoms are similar to hepatitis A. However, in pregnant women, especially in the third trimester, it can cause severe complications such as fulminant hepatitis, preterm labor, fetal death, or maternal death.
- Hepatitis G usually causes a mild and asymptomatic infection that does not affect liver function. However, it may interact with other hepatitis viruses and affect their clinical outcomes.
- Other non-viral causes of hepatitis can cause various signs and symptoms depending on the specific agent, such as fever, rash, arthralgia, hemolysis, renal failure, or neurological disorders.
Diagnosis and treatment
- Hepatitis A is diagnosed by detecting the presence of IgM antibodies against hepatitis A virus (anti-HAV IgM) in the serum. It is treated by providing supportive care (such as hydration, nutrition, and pain relief) and preventing complications (such as bleeding or encephalopathy). There is no specific antiviral therapy for hepatitis A.
- Hepatitis B is diagnosed by detecting the presence of various markers of hepatitis B virus (HBV) infection in the serum. These markers include HBV surface antigen (HBsAg), HBV core antibody (anti-HBc), HBV surface antibody (anti-HBs), HBV e antigen (HBeAg), HBV e antibody (anti-HBe), and HBV DNA. The interpretation of these markers depends on the phase of the infection (acute or chronic) and the activity of the infection (inactive or active). Hepatitis B is treated by providing supportive care for acute infection and antiviral therapy for chronic infection. The antiviral agents used include interferon-alpha, pegylated interferon-alpha, lamivudine, adefovir, entecavir, telbivudine, or tenofovir. The goal of the treatment is to suppress the viral replication, reduce the liver inflammation, and prevent the complications.
- Hepatitis C is diagnosed by detecting the presence of antibodies against hepatitis C virus (anti-HCV) in the serum. If positive, the viral load (HCV RNA) and the genotype of the virus are determined. Hepatitis C is treated by providing supportive care for acute infection and antiviral therapy for chronic infection. The antiviral agents used include interferon-alpha, pegylated interferon-alpha, ribavirin, and direct-acting antivirals (such as sofosbuvir, ledipasvir, daclatasvir, simeprevir, or velpatasvir). The choice and duration of the treatment depend on the genotype and the stage of the liver disease. The goal of the treatment is to achieve a sustained virologic response (SVR), which means undetectable HCV RNA 12 weeks after the end of the treatment.
- Hepatitis D is diagnosed by detecting the presence of antibodies against hepatitis D virus (anti-HDV) in the serum. If positive, the viral load (HDV RNA) is determined. Hepatitis D is treated by providing supportive care for acute infection and antiviral therapy for chronic infection. The antiviral agent used is pegylated interferon-alpha. The duration of the treatment is usually longer than for hepatitis B or C. The goal of the treatment is to suppress the viral replication and prevent the complications.
- Hepatitis E is diagnosed by detecting the presence of IgM antibodies against hepatitis E virus (anti-HEV IgM) in the serum. It is treated by providing supportive care (such as hydration, nutrition, and pain relief) and preventing complications (such as bleeding or encephalopathy). There is no specific antiviral therapy for hepatitis E.
- Hepatitis G is diagnosed by detecting the presence of antibodies against hepatitis G virus (anti-HGV) in the serum. If positive, the viral load (HGV RNA) is determined. Hepatitis G is usually not treated as it does not cause significant liver damage. However, it may affect the response to other antiviral therapies for co-infections with other hepatitis viruses.
- Other non-viral causes of hepatitis are diagnosed by detecting the presence of specific markers of the causative agent in the serum or other specimens. The treatment depends on the specific agent and may include antibiotics, antiparasitics, antidotes, immunosuppressants, or corticosteroids.
Nursing interventions
- For all types of hepatitis, some general nursing interventions include:
- Assessing the patient’s history, risk factors, signs and symptoms, liver function tests, and viral markers
- Monitoring the patient’s vital signs, fluid and electrolyte balance, nutritional status, weight, urine output, and mental status
- Administering prescribed medications and fluids as ordered
- Educating the patient about the disease process, treatment options, possible complications, and self-care measures
- Providing emotional support and counseling to the patient and family
- Implementing infection control measures to prevent transmission to others
- Reporting any adverse reactions or changes in condition to the physician
- For specific types of hepatitis, some additional nursing interventions include:
- For hepatitis A:
- Encouraging oral hygiene and a soft diet to reduce nausea and vomiting
- Advising the patient to avoid alcohol and hepatotoxic drugs
- Informing the patient about the availability and benefits of hepatitis A vaccine and immunoglobulin for prevention
- For hepatitis B:
- Administering hepatitis B immunoglobulin (HBIG) to exposed contacts within 24 hours of exposure
- Advising the patient to avoid sexual contact or use condoms until cleared of infection
- Informing the patient about the availability and benefits of hepatitis B vaccine for prevention
- For hepatitis C:
- Assessing the patient’s readiness and adherence to antiviral therapy
- Managing the side effects of antiviral therapy such as anemia, neutropenia, thrombocytopenia,
- For hepatitis C (continued):
- Managing the side effects of antiviral therapy such as anemia, neutropenia, thrombocytopenia, fatigue, headache, insomnia, depression, or rash
- Advising the patient to avoid alcohol and hepatotoxic drugs
- Informing the patient about the availability and benefits of hepatitis C vaccine for prevention
- For hepatitis D:
- Administering hepatitis B immunoglobulin (HBIG) and hepatitis B vaccine to exposed contacts within 24 hours of exposure
- Advising the patient to avoid sexual contact or use condoms until cleared of infection
- Informing the patient about the risk of co-infection or super-infection with hepatitis B and the need for regular monitoring of liver function and viral load
- For hepatitis E:
- Monitoring the pregnant women closely for signs of fulminant hepatitis or preterm labor
- Providing prompt delivery and intensive care for the mother and the newborn in case of complications
- Informing the patient about the importance of safe water and food hygiene to prevent infection
- For hepatitis G:
- Assessing the patient’s co-infection status with other hepatitis viruses and the response to antiviral therapy
- Advising the patient to avoid alcohol and hepatotoxic drugs
- Informing the patient about the uncertainty of the clinical significance and long-term outcomes of hepatitis G infection
- For other non-viral causes of hepatitis:
- Identifying and removing the causative agent if possible
- Providing symptomatic and supportive care for the liver injury
- Informing the patient about the potential causes and consequences of hepatitis and the ways to prevent or reduce them
Prevention and control:
- For all types of hepatitis, some general prevention and control measures include:
- Practicing good personal hygiene and sanitation
- Avoiding contact with infected persons or their body fluids
- Using sterile needles and syringes for injections or other procedures
- Using barrier methods (such as condoms) for sexual intercourse
- Avoiding alcohol and hepatotoxic drugs
- Eating a balanced diet and maintaining a healthy weight
- Getting regular check-ups and screening tests for liver function and viral markers
- For specific types of hepatitis, some additional prevention and control measures include:
- For hepatitis A:
- Getting vaccinated with hepatitis A vaccine, which provides protection for up to 10 years
- Getting immunized with hepatitis A immunoglobulin (HAVIG), which provides passive immunity for up to 3 months
- Boiling or chlorinating water before drinking or cooking
- Washing fruits and vegetables before eating
- Cooking shellfish thoroughly before eating
- For hepatitis B:
- Getting vaccinated with hepatitis B vaccine, which provides protection for up to 20 years
- Getting immunized with hepatitis B immunoglobulin (HBIG), which provides passive immunity for up to 6 months
- Screening blood donors and recipients for HBV infection
- Testing pregnant women for HBV infection and treating them if positive
- Giving HBIG and hepatitis B vaccine to newborns of HBV-positive mothers within 12 hours of birth
- Disinfecting contaminated surfaces or instruments with bleach or autoclave
- For hepatitis C:
- Getting vaccinated with hepatitis C vaccine, which is currently under development
- Screening blood donors and recipients for HCV infection
- Testing pregnant women for HCV infection and treating them if positive
- Giving antiviral therapy to newborns of HCV-positive mothers if indicated
- Disinfecting contaminated surfaces or instruments with bleach or autoclave
- For hepatitis D:
- Getting vaccinated with hepatitis B vaccine, which also protects against hepatitis D infection
- Getting immunized with hepatitis B immunoglobulin (HBIG), which also provides passive immunity against hepatitis D infection
- Screening blood donors and recipients for HDV infection
- Testing pregnant women for HDV infection and treating them if positive
- Giving HBIG and hepatitis B vaccine to newborns of HDV-positive mothers within 12 hours of birth
- Disinfecting contaminated surfaces or instruments with bleach or autoclave
- For hepatitis E (continued): - Disinfecting contaminated surfaces or instruments with bleach or autoclave
- For hepatitis G:
- There is no specific prevention or control measure for hepatitis G as it does not cause significant liver damage or transmission
- For other non-viral causes of hepatitis:
- Avoiding exposure to the causative agent if possible or using protective equipment if necessary
- Getting vaccinated or immunized for the preventable causes of hepatitis, such as leptospirosis or syphilis
- Seeking medical attention promptly if symptoms of hepatitis occur
Types and distribution
- Hepatitis A is the most common type of viral hepatitis worldwide, affecting about 1.4 million people annually. It is endemic in regions with poor sanitation and hygiene, such as Africa, Asia, Central and South America, and Eastern Europe.
- Hepatitis B is the second most common type of viral hepatitis worldwide, affecting about 257 million people chronically. It is endemic in regions with a high prevalence of HBV infection, such as Africa, Asia, Eastern Europe, and the Pacific Islands.
- Hepatitis C is the third most common type of viral hepatitis worldwide, affecting about 71 million people chronically. It is endemic in regions with high prevalence of HCV infection, such as Africa, Asia, Eastern Europe, and the Middle East.
- Hepatitis D is the least common type of viral hepatitis worldwide, affecting about 15 million people who are co-infected with HBV. It is endemic in regions with high prevalence of HBV and HDV infection, such as Africa, Asia, Eastern Europe, and South America.
- Hepatitis E is the most common cause of acute viral hepatitis in developing countries, affecting about 20 million people annually. It is endemic in regions with poor sanitation and hygiene, such as Africa, Asia, Central and South America, and Eastern Europe.
- Hepatitis G is a newly discovered type of viral hepatitis that has a global distribution but a low prevalence. It is estimated to affect about 2% of the general population and 10% of blood donors worldwide.
- Other non-viral causes of hepatitis have variable distribution depending on the specific agent and the environmental factors. They can affect anyone who is exposed to them.
Conclusion
- Hepatitis is a serious liver disease that can be caused by various factors, such as viruses, bacteria, parasites, drugs, toxins, or autoimmune disorders.
- Hepatitis can be classified into different types based on the causative agent, such as hepatitis A, B, C, D, E, G, or other non-viral causes.
- Each type of hepatitis has different characteristics, modes of transmission, clinical manifestations
Meningitis
- Meningitis is an inflammation of the meninges, which are the membranes that protect the brain and spinal cord.
- Meningitis can be caused by various microorganisms, such as bacteria, viruses, fungi, or parasites.
- Meningitis can be classified into two main types: viral or aseptic, and bacterial or septic.
- Viral meningitis is usually mild and self-limiting, requiring only supportive care for recovery.
- Bacterial meningitis is a serious and potentially fatal infection that requires prompt diagnosis and treatment with antibiotics.
Meningitis can affect people of any age, but it is more common and severe in infants, children, older adults, and immunocompromised individuals.
Causative agent:
- The causative agent of meningitis depends on the type of meningitis.
- Viral meningitis can be caused by various viruses, such as enteroviruses, herpes simplex virus, mumps virus, measles virus, varicella-zoster virus, or arboviruses.
- Bacterial meningitis can be caused by different bacteria, such as Neisseria meningitidis (meningococcal), Streptococcus pneumoniae (pneumococcal), Haemophilus influenzae type b (Hib), Escherichia coli, Listeria monocytogenes, or Group B streptococcus.
- Fungal meningitis can be caused by fungi such as Cryptococcus neoformans, Coccidioides immitis, Histoplasma capsulatum, or Blastomyces dermatitidis.
- Parasitic meningitis can be caused by parasites such as Naegleria fowleri, Acanthamoeba spp., or Angiostrongylus cantonensis.
Transmission cycle/vector/reservoir
- The transmission cycle/vector/reservoir of meningitis varies according to the causative agent.
- Viral meningitis is usually transmitted through direct contact with respiratory secretions, saliva, or feces of an infected person. The vector is the infected person and the reservoir is the human body. Some arboviruses can also be transmitted by mosquito or tick bites. The vector is the insect and the reservoir is the animal host.
- Bacterial meningitis is usually transmitted through direct contact with respiratory droplets or saliva of an infected person or carrier. The vector is the infected person or carrier and the reservoir is the human nasopharynx. Some bacteria can also be transmitted through contaminated food or water (e.g., Listeria monocytogenes) or through direct access to cerebrospinal fluid (e.g., skull fracture or penetrating head wound) .
- Fungal meningitis is usually transmitted through inhalation of fungal spores from the environment (e.g., soil or bird droppings) . The vector is the fungus and the reservoir is the environmental source . Some fungi can also be transmitted through contaminated medical products (e.g., steroids) or devices (e.g., catheters) .
- Parasitic meningitis is usually transmitted through contact with contaminated water (e.g., swimming pools, lakes, rivers) or soil (e.g., gardening) . The vector is the parasite and the reservoir is the water or soil source . Some parasites can also be transmitted through ingestion of raw or undercooked snails or slugs (e.g., Angiostrongylus cantonensis) .
Signs and symptoms of meningitis
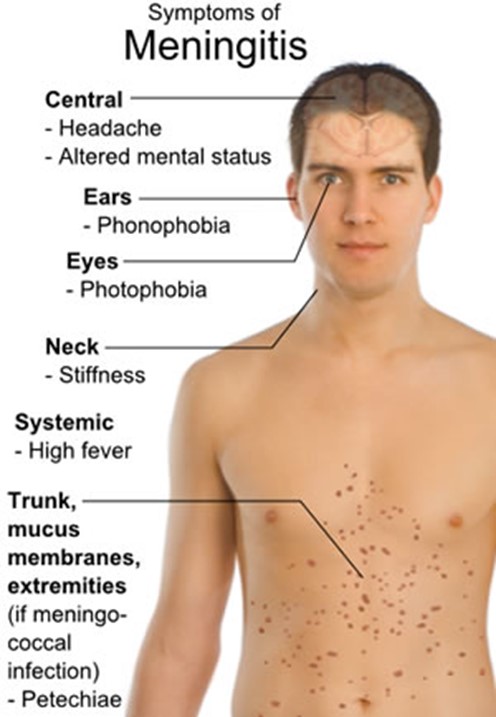
- The signs and symptoms of meningitis depend on the type, cause, and severity of the infection .
- The common signs and symptoms of meningitis include :
- Fever
- Headache
- Stiff neck
- Photophobia (sensitivity to light)
- Nausea and vomiting
- Altered mental status (confusion, lethargy, irritability)
- Seizures
- The specific signs and symptoms of meningitis may vary according to the age group :
- Infants may show poor feeding, irritability, bulging fontanelle (soft spot on the head), or high-pitched cry .
- Children may show drowsiness, rash, or nuchal rigidity (inability to flex the neck forward) ] .
- Older adults may show subtle changes in behavior, memory loss, or incontinence .
- The signs and symptoms of meningitis may also differ according to the causative agent :
- Viral meningitis may cause flu-like symptoms, such as cough, sore throat, or muscle aches .
- Bacterial meningitis may cause petechiae (small red spots on the skin), purpura (large purple bruises on the skin), or meningococcal septicemia (blood poisoning) ] .
- Fungal meningitis may cause chronic symptoms, such as weight loss, fatigue, or night sweats .
- Parasitic meningitis may cause severe headache, stiff neck, nausea, vomiting, or altered taste or smell.
Diagnosis and treatment
- The diagnosis of meningitis is based on the history, physical examination, and laboratory tests .
- The most important laboratory test for meningitis is the lumbar puncture (LP) or spinal tap, which involves inserting a needle into the lower back to collect cerebrospinal fluid (CSF) for analysis .
- The CSF analysis can reveal the type, cause, and severity of the infection by measuring the following parameters :
- Appearance: normal CSF is clear and colorless; cloudy or turbid CSF indicates infection; yellow or xanthochromic CSF indicates bleeding; pink or red CSF indicates blood contamination.
- Pressure: normal CSF pressure is 70-180 mm H2O; increased pressure indicates increased intracranial pressure; decreased pressure indicates dehydration or leakage.
- Protein: normal CSF protein is 15-45 mg/dL; increased protein indicates inflammation or infection; decreased protein indicates malnutrition or leakage.
- Glucose: normal CSF glucose is 50-80 mg/dL or 60-70% of blood glucose; decreased glucose indicates bacterial or fungal infection; increased glucose indicates diabetes mellitus or hyperglycemia.
- Cell count and differential: normal CSF cell count is 0-5 white blood cells (WBCs) per mm3 and 0 red blood cells (RBCs) per mm3; increased WBCs indicate infection or inflammation; increased RBCs indicate bleeding or trauma; differential can identify the type of WBCs present (e.g., neutrophils indicate bacterial infection; lymphocytes indicate viral or fungal infection).
- Other laboratory tests for meningitis include blood culture, urine culture, throat swab, polymerase chain reaction (PCR), antigen detection tests, antibody tests, and imaging tests (e.g., computed tomography scan or magnetic resonance imaging scan).
- The treatment of meningitis depends on the type and cause of the infection.
- Viral meningitis usually requires only supportive care, such as hydration, analgesics (pain relievers), antipyretics (fever reducers), and anticonvulsants (seizure preventers).
- Bacterial meningitis requires prompt administration of antibiotics, such as penicillin, cephalosporin, vancomycin, or rifampin. The choice of antibiotic depends on the type of bacteria, the susceptibility to the drug, and the patient’s condition. Sometimes, corticosteroids (e.g., dexamethasone) are also given to reduce inflammation and prevent complications.
- Fungal meningitis requires antifungal drugs, such as amphotericin B, fluconazole, or voriconazole . The duration of treatment may be long and depends on the type of fungus and the patient’s response.
- Parasitic meningitis requires antiparasitic drugs, such as albendazole, ivermectin, or miltefosine . The prognosis of parasitic meningitis is poor and often fatal.
Nursing interventions
- The nursing interventions for meningitis are aimed at providing supportive care, monitoring the patient’s condition, preventing complications, and educating the patient and family.
- Some of the nursing interventions for meningitis include :
- Assessing the patient’s vital signs, neurological status, level of consciousness, pupillary response, cranial nerve function, and Glasgow coma scale score .
- Administering the prescribed medications, such as antibiotics, antipyretics, analgesics, anticonvulsants, and corticosteroids .
- Maintaining the patient’s hydration and nutrition, such as by providing intravenous fluids, oral fluids, or enteral feeding .
- Implementing infection control measures, such as by isolating the patient, wearing personal protective equipment, and following standard precautions .
- Reducing the patient’s environmental stimuli, such as by dimming the lights, minimizing noise, and avoiding unnecessary procedures .
- Elevating the patient’s head to 30 degrees and maintaining a neutral position to reduce intracranial pressure and promote venous drainage .
- Applying cold compresses or ice packs to the patient’s forehead or neck to reduce fever and discomfort .
- Providing comfort measures, such as by repositioning the patient, massaging the neck muscles, or applying a soft collar .
- Educating the patient and family about the disease, its transmission, its treatment, its complications, and its prevention .
- Referring the patient and family to appropriate resources, such as social workers, counselors, or support groups .
Prevention and control
- The prevention and control of meningitis are based on reducing the exposure to the causative agents, enhancing the immunity of the population, and managing the outbreaks of the disease.
- Some of the prevention and control measures for meningitis include :
- Avoiding close contact with people who have meningitis or respiratory infections, such as by not sharing utensils, cups, or personal items .
- Practicing good hygiene habits, such as by washing hands frequently, covering mouth and nose when coughing or sneezing, and disposing of tissues properly .
- Getting vaccinated against certain types of meningitis, such as meningococcal, pneumococcal, Hib, or mumps vaccines. The vaccination schedule depends on the age group and risk factors of the individual.
- Taking prophylactic antibiotics if exposed to a person with bacterial meningitis or traveling to a high-risk area. The type and duration of antibiotics depend on the type of bacteria and the exposure status of the individual.
- Reporting any suspected cases of meningitis to the local health authorities and following their guidelines for outbreak management. The outbreak management may involve mass vaccination campaigns, contact tracing, chemoprophylaxis (preventive medication), or quarantine measures.
Types and distribution
- The types and distribution of meningitis vary according to the geographic region, climate, season, population density and age group .
- Viral meningitis is more common in temperate regions than in tropical regions. It occurs more frequently in summer and autumn than in winter and spring. It affects people of all ages but is more prevalent in children under five years old.
- Bacterial meningitis is more common in tropical regions than in temperate regions. It occurs more frequently in winter and spring than in summer and autumn. It affects people of all ages but is more severe in infants under one year old. There are three main types of bacterial meningitis:
- Meningococcal meningitis: caused by Neisseria meningitidis; occurs mainly in sub-Saharan Africa (the “meningitis belt”), where epidemics occur every few years; affects mainly children and young adults; can cause death within hours if untreated; prevented by vaccination.
- Pneumococcal meningitis: caused by Streptococcus pneumoniae; occurs worldwide; affects mainly infants, older adults, and people with chronic diseases or weakened immune systems; has a high mortality rate even with treatment; prevented by vaccination .
- Hib meningitis: caused by Haemophilus influenzae type b; occurs mainly in developing countries; affects mainly children under five years old; can cause permanent disability or death if untreated; prevented by vaccination.
- Fungal meningitis is more common in regions with endemic fungi (e.g., North America, South America, Africa, or Asia). It occurs mainly in people with immunodeficiency (e.g., HIV/AIDS, cancer, or organ transplant). It has a chronic course and a high mortality rate even with treatment.
- Parasitic meningitis is more common in regions with contaminated water or soil (e.g., Southeast Asia, Africa, or Latin America). It occurs mainly in people who have contact with these sources (e.g., swimmers, gardeners, or travelers). It has a rapid onset and a fatal outcome in most cases.
Conclusion
- Meningitis is a serious infection of the meninges that can be caused by various microorganisms, such as bacteria, viruses, fungi, or parasites .
- Meningitis can cause fever, headache, stiff neck, photophobia, nausea, vomiting, altered mental status, and seizures .
- Meningitis can be diagnosed by lumbar puncture and CSF analysis, as well as other laboratory and imaging tests .
- Meningitis can be treated by antibiotics, antifungals, antiparasitics, or supportive care, depending on the type and cause of the infection .
- Meningitis can be prevented by vaccination, prophylaxis, hygiene, infection control, and outbreak management
- Meningitis can vary in its types and distribution according to the geographic region, climate, season, population density and age group .
Summary
- Meningitis is an inflammation of the meninges caused by various microorganisms.-Meningitis can cause various signs and symptoms depending on the type, cause, and severity of the infection.
- Meningitis can be diagnosed by lumbar puncture and CSF analysis, as well as other laboratory and imaging tests.
- Meningitis can be treated by antibiotics, antifungals, antiparasitics, or supportive care, depending on the type and cause of the infection.
- Meningitis can be prevented by vaccination, prophylaxis, hygiene, infection control, and outbreak management.
- Meningitis can vary in its types and distribution according to the geographic region, climate, season, population density and age group.
Signs and symptoms of meningitis
- The incubation period of Zika virus infection is estimated to be between 3 to 14 days, with an average of 5 to 6 days.
- About 80% of people infected with Zika virus do not develop any symptoms.
- The most common symptoms of Zika virus infection are mild and last for 2 to 7 days. They include:
- Fever
- Rash
- Conjunctivitis (red eyes)
- Headache
- Muscle and joint pain
- Malaise
- Some people may also experience:
- Swelling of the limbs
- Retro-orbital pain (pain behind the eyes)
- Gastrointestinal symptoms such as nausea, vomiting, and diarrhea
- Pruritus (itching)
- Zika virus infection can cause serious complications in some cases, such as:
- Microcephaly: a condition where the baby’s head is smaller than expected due to abnormal brain development in the womb or after birth.
- Congenital Zika syndrome: a spectrum of birth defects that can include microcephaly, brain abnormalities, eye defects, hearing loss, and limb deformities.
- Guillain-Barré syndrome: a rare disorder where the body’s immune system attacks the nerves, causing weakness, numbness, tingling, and paralysis.
- Other neurological disorders such as meningoencephalitis, myelitis, and neuropathy.
Zika virus
- Zika virus is a single-stranded RNA virus that belongs to the genus Flavivirus, family Flaviviridae.
- It is closely related to dengue, yellow fever, Japanese encephalitis, and West Nile viruses.
- It was first discovered in a monkey with a mild fever in the Zika forest in Uganda in 1947.
- It causes a mild febrile illness that is usually self-limiting and asymptomatic in most cases.
- However, it can also cause serious complications such as microcephaly, congenital Zika syndrome, Guillain-Barré syndrome, and other neurological disorders.
- It is primarily transmitted by the bite of an infected Aedes species mosquito, especially Aedes aegypti and Aedes albopictus.
- It can also be transmitted through sexual contact, maternal-fetal transmission, blood transfusion, and laboratory exposure.
- There is no vaccine or specific antiviral treatment for Zika virus infection.
- The best way to prevent and control Zika virus infection is to avoid mosquito bites, practice safe sex, and seek medical attention if symptoms occur.
Causative agent
- Zika virus is a single-stranded RNA virus that has a positive sense genome.
- It has a spherical shape with a diameter of about 40 nm.
- It has an envelope that contains two glycoproteins: E (envelope) and M (membrane).
- The E protein is responsible for binding to host cell receptors and mediating viral entry.
- The M protein is involved in viral assembly and maturation.
- The genome encodes three structural proteins: C (capsid), E (envelope), and M (membrane), and seven nonstructural proteins: NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5.
- The nonstructural proteins are involved in viral replication, transcription, translation, polyprotein processing, immune evasion, and pathogenesis.
Transmission cycle/vector/reservoir
- The transmission cycle of Zika virus involves two hosts: humans and mosquitoes.

- Humans are the primary reservoir of Zika virus, meaning that they can maintain the virus in their blood and transmit it to mosquitoes.
- Mosquitoes are the primary vector of Zika virus, meaning that they can acquire the virus from an infected human and transmit it to another human through their saliva during blood feeding.
- The main mosquito species that transmit Zika virus are Aedes aegypti and Aedes albopictus, which are also known as yellow fever mosquito and Asian tiger mosquito respectively.
- These mosquitoes are active during the day and prefer to breed in urban areas with stagnant water sources such as containers, tires, buckets, flower pots, etc.
- They can also transmit other arboviruses such as dengue, chikungunya, yellow fever, and West Nile viruses.
Diagnosis and treatment
- The diagnosis of Zika virus infection is based on the following criteria:
- Clinical signs and symptoms compatible with Zika virus infection
- Epidemiological history of exposure to Zika virus transmission areas or risk factors such as travel, sexual contact, blood transfusion, etc.
- Laboratory confirmation of Zika virus infection by one or more of the following tests:
- Reverse transcription polymerase chain reaction (RT-PCR) to detect Zika virus RNA in blood, urine, saliva, semen, or other body fluids
- Serological tests to detect Zika virus-specific IgM and IgG antibodies in blood or cerebrospinal fluid
- Plaque reduction neutralization test (PRNT) to measure the level of neutralizing antibodies against Zika virus in blood
- Immunohistochemistry (IHC) or in situ hybridization (ISH) to detect Zika virus antigens or RNA in tissues or placenta
- The treatment of Zika virus infection is mainly supportive and symptomatic. There is no specific antiviral treatment for Zika virus infection. The general measures include:
- Rest and hydration
- Analgesics and antipyretics such as acetaminophen or paracetamol to relieve pain and fever
- Antihistamines to reduce itching and rash
- Avoidance of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, as they may increase the risk of bleeding or worsen the symptoms of dengue, which is a differential diagnosis of Zika virus infection
- Monitoring of vital signs and neurological status
- Referral to specialized care if complications such as microcephaly, congenital Zika syndrome, Guillain-Barré syndrome, or other neurological disorders occur
- The nursing interventions for Zika virus infection include:
- Assessing the patient’s history, symptoms, exposure, and risk factors for Zika virus infection
- Collecting and sending appropriate specimens for laboratory testing
- Providing education and counseling to the patient and family about Zika virus infection, its transmission, prevention, complications, and treatment
- Implementing standard precautions and contact precautions to prevent nosocomial transmission of Zika virus infection
- Providing emotional support and psychosocial care to the patient and family, especially if the patient is pregnant or has a newborn with microcephaly or congenital Zika syndrome
- Collaborating with other health care professionals and agencies to coordinate care and follow-up for the patient and family
Prevention and control
- The prevention and control of Zika virus infection is based on the following strategies:
- Reducing the exposure to mosquito bites by:
- Wearing long-sleeved shirts, pants, socks, and shoes
- Applying insect repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus on exposed skin and clothing
- Using mosquito nets, screens, coils, and vaporizers in sleeping areas
- Eliminating or treating potential mosquito breeding sites such as containers, tires, buckets, flower pots, etc. with larvicides or biological agents
- Reducing the transmission of Zika virus through sexual contact by:
- Practicing safe sex by using condoms correctly and consistently
- Abstaining from sex or delaying pregnancy if possible
- Testing for Zika virus infection before and after traveling to Zika virus transmission areas or having sexual contact with someone who has traveled to or lives in those areas
- Seeking medical advice if symptoms of Zika virus infection occur
- Reducing the risk of congenital Zika syndrome and microcephaly by:
- Providing preconception counseling and family planning services to women of reproductive age who live in or travel to Zika virus transmission areas
- Offering prenatal screening and testing for Zika virus infection to pregnant women who live in or travel to Zika virus transmission areas or have sexual contact with someone who has traveled to or lives in those areas
- Providing ultrasound monitoring and fetal surveillance to detect any abnormalities in the baby’s growth and development
- Providing postnatal care and follow-up for babies born with microcephaly or congenital Zika syndrome and their families
- Reducing the incidence and severity of Guillain-Barré syndrome and other neurological disorders by:
- Providing early diagnosis and treatment of Zika virus infection and its complications
- Providing supportive care and rehabilitation services to patients with Guillain-Barré syndrome and other neurological disorders
- Conducting surveillance and research on the epidemiology, pathogenesis, and outcomes of Zika virus infection and its complications
- The role of nurses in the prevention and control of Zika virus infection is to:
- Provide health education and promotion to the public about Zika virus infection, its transmission, prevention, complications, and treatment
- Participate in vector control activities such as larval source reduction, environmental sanitation, and insecticide spraying
- Implement infection prevention and control measures in health care settings to prevent nosocomial transmission of Zika virus infection
- Provide quality care and counseling to patients with Zika virus infection and their families
- Advocate for the rights and needs of patients with Zika virus infection and their families
- Collaborate with other health care professionals and agencies to coordinate care and follow-up for patients with Zika virus infection and their families
Types and distribution
- There are two main types of Zika virus: African lineage and Asian lineage.
- The African lineage is divided into two subtypes: East African (EA) subtype and West African (WA) subtype.
- The Asian lineage is divided into two subtypes: Asian (AS) subtype and American (AM) subtype.
- The EA subtype is the original strain that was isolated from a monkey in Uganda in 1947.
- The WA subtype is derived from the EA subtype and was first detected in humans in Nigeria in 1954.
- The AS subtype is derived from the WA subtype and was first detected in humans in Malaysia in 1966.
- The AM subtype is derived from the AS subtype and was first detected in humans in Brazil in 2015.
- The distribution of Zika virus types around the world is shown in the table below:
|
Type |
Subtype |
Distribution |
|
African |
EA |
Uganda, Tanzania, Egypt |
|
African |
WA |
Nigeria, Senegal, Ivory Coast, Gabon, Central African Republic |
|
Asian |
AS |
Malaysia, Indonesia, Thailand, Cambodia, Vietnam, Philippines |
|
Asian |
AM |
Brazil, Colombia, Venezuela, Mexico, Caribbean islands |
Conclusion
- Zika virus is a single-stranded RNA virus that causes a mild febrile illness that can be complicated by microcephaly, congenital Zika syndrome, Guillain-Barré syndrome, and other neurological disorders.
- It is transmitted by the bite of an infected Aedes species mosquito, sexual contact, maternal-fetal transmission, blood transfusion, and laboratory exposure.
- It can be diagnosed by clinical signs and symptoms, epidemiological history, and laboratory tests such as RT-PCR, serology, PRNT, IHC, or ISH.
- It can be treated by supportive and symptomatic measures. There is no specific antiviral treatment or vaccine for Zika virus infection.
- It can be prevented and controlled by reducing the exposure to mosquito bites, practicing safe sex, screening and testing for Zika virus infection, monitoring and caring for pregnant women and babies, and providing health education and promotion.
- There are two main types of Zika virus: African lineage and Asian lineage, which are further divided into four subtypes: EA, WA, AS, and AM. They have different origins and distributions around the world.
Summary
- Zika virus is a Flavivirus that causes a mild febrile illness with rash, conjunctivitis, headache, and joint pain.
- Zika virus can cause serious complications such as microcephaly, congenital Zika syndrome, Guillain-Barré syndrome, and other neurological disorders.
- Zika virus is transmitted by Aedes mosquitoes, sexual contact, maternal-fetal transmission, blood transfusion, and laboratory exposure.
- Zika virus can be diagnosed by clinical signs and symptoms, epidemiological history, and laboratory tests.
- Zika virus can be treated by supportive and symptomatic measures. There is no specific antiviral treatment or vaccine for Zika virus infection.
- Zika virus can be prevented and controlled by reducing the exposure to mosquito bites, practicing safe sex, screening and testing for Zika virus infection, monitoring and caring for pregnant women and babies, and providing health education and promotion.
- Zika virus has two main types: African lineage and Asian lineage, which have different origins and distributions around the world.
Measles
- Measles is a highly contagious viral illness characterized by fever, malaise, rash, cough, coryza, and conjunctivitis.
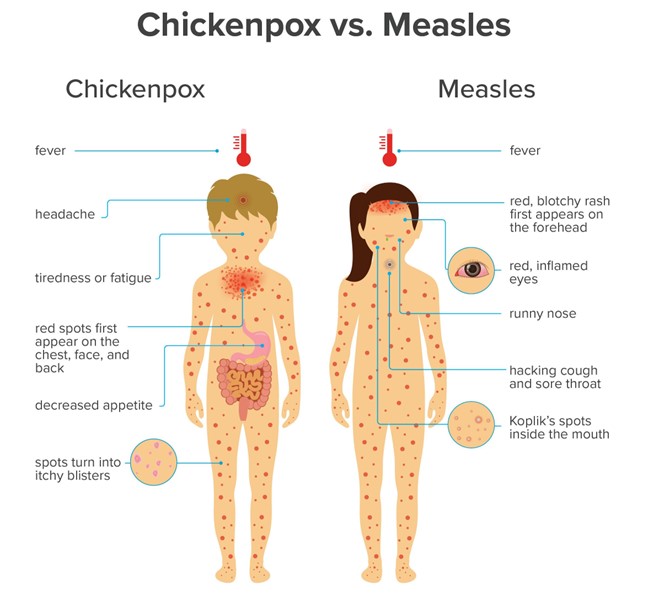
- Measles is caused by the measles virus, which belongs to the genus Morbillivirus in the family Paramyxoviridae.
- Measles is one of the leading causes of mortality among children under five years of age worldwide, especially in resource-limited settings.
- Measles can be prevented by vaccination with the live attenuated measles vaccine, which is usually given as part of the MMR (measles-mumps-rubella) or MMRV (measles-mumps-rubella-varicella) combination vaccine .
Causative agent
- Measles virus is a single-stranded negative-sense RNA virus with a helical capsid and an envelope.
- The genome of the measles virus encodes six structural proteins: nucleoprotein (N), phosphoprotein (P), matrix protein (M), fusion protein (F), hemagglutinin protein (H), and large protein (L) .
- The F and H proteins are responsible for binding to host cell receptors and mediating viral entry and fusion .
- The N, P, and L proteins form the viral polymerase complex that replicates and transcribes the viral RNA .
- The M protein links the viral envelope to the nucleocapsid and plays a role in viral assembly and budding .
Transmission cycle/vector/reservoir
- Measles is transmitted via person-to-person contact as well as airborne spread through respiratory droplets.
- Measles virus can remain infectious in the air for up to two hours after being expelled by an infected person.
- The attack rate of measles in a susceptible individual exposed to measles is 90 percent.
- Measles virus only infects humans and has no animal or environmental reservoirs.
- The period of contagiousness of measles is estimated to be from five days before the appearance of rash to four days afterward.
Signs and symptoms
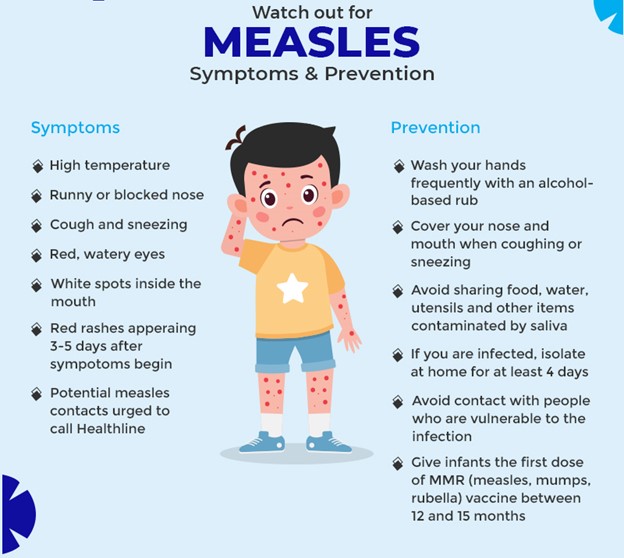
- Measles infection can be divided into four clinical stages: incubation, prodrome, exanthem, and recovery.
- The incubation period of measles is 6 to 21 days (median 13 days), during which the infected person is asymptomatic or may experience transient respiratory symptoms, fever, or rash.
- The prodrome stage of measles lasts 2 to 4 days and is characterized by high fever (>38.5°C), malaise, anorexia, cough, coryza, conjunctivitis, photophobia, and Koplik spots.
- Koplik spots are small white lesions on the buccal mucosa surrounded by a red halo that appears 1 to 2 days before the rash. They are pathognomonic for measles.
- Cough, coryza, conjunctivitis, and cephalocaudal spread are known as the “4 C’s” of measles
- The exanthem stage of measles lasts 4 to 7 days and is marked by the appearance of a maculopapular rash that begins on the face and spreads to the trunk and extremities. The rash usually fades in the same order as it appeared
- The rash may be accompanied by itching, peeling, desquamation, or hyperpigmentation
- The fever usually peaks on the first or second day of rash onset and then declines gradually
- The recovery stage of measles lasts 1 to 2 weeks and is characterized by the resolution of symptoms and the restoration of immunity
- However, measles virus can persist in some tissues and organs for months or years after infection, causing chronic inflammation and immunosuppression
Diagnosis and treatment
- Measles is usually diagnosed clinically based on the presence of the characteristic rash, Koplik spots, and the “4 C’s” of measles
- Laboratory confirmation of measles can be done by detecting measles-specific IgM antibodies in serum or saliva samples using enzyme-linked immunosorbent assay (ELISA) or by detecting measles RNA using reverse transcription polymerase chain reaction (RT-PCR) in nasopharyngeal swabs or urine samples
- There is no specific antiviral treatment for measles. Supportive care is the mainstay of management, which includes hydration, antipyretics, analgesics, antihistamines, and eye care
- Vitamin A supplementation is recommended for children with measles, especially those who are malnourished or have vitamin A deficiency, as it can reduce the risk of blindness, pneumonia, diarrhea, and death
- Measles can cause various complications, such as diarrhea, otitis media, pneumonia, encephalitis, subacute sclerosing panencephalitis (SSPE), and death
- Diarrhea is the most common complication of measles and can lead to dehydration and electrolyte imbalance
- Otitis media is the second most common complication of measles and can cause hearing loss and mastoiditis
- Pneumonia is the most common cause of death from measles in children and can be caused by the measles virus itself or by secondary bacterial infections
- Encephalitis is the most common cause of death from measles in adults and can manifest as acute post-infectious encephalomyelitis (APEM), acute disseminated encephalomyelitis (ADEM), or acute measles inclusion body encephalitis (AMIBE)
- APEM occurs within 1 week of rash onset and presents with fever, headache, seizures, altered consciousness, and focal neurological signs. It has a mortality rate of 10 to 20 percent and a morbidity rate of 20 to 40 percent.
- ADEM occurs within 2 to 4 weeks of rash onset and presents with multifocal demyelination of the central nervous system. It has a mortality rate of 5 to 10 percent and a morbidity rate of 10 to 20 percent.
- AMIBE occurs in immunocompromised patients within 6 months of rash onset and presents with progressive neurological deterioration. It has a mortality rate of nearly 100 percent.
- SSPE is a rare but fatal complication of measles that occurs years after infection. It is caused by persistent infection of the brain by a mutated form of the measles virus that evades immune recognition. It presents with progressive cognitive decline, behavioral changes, myoclonus, seizures, ataxia, and coma. There is no effective treatment for SSPE .
Nursing interventions
- The nursing interventions for patients with measles are aimed at providing supportive care, preventing complications, educating the patient and family, and preventing transmission.
- Some of the nursing interventions are:
|
Nursing Intervention |
Rationale |
|
Isolate the patient in a private room with negative pressure ventilation or in a cohort with other patients with confirmed measles. Use standard and airborne precautions when caring for the patient. Wear an N95 respirator mask when entering the room. |
To prevent the spread of measles to other patients, staff, and visitors. Measles is highly contagious and can be transmitted through respiratory droplets or airborne particles . |
|
Monitor the patient’s vital signs, especially temperature, pulse, respiratory rate, and oxygen saturation. Assess for signs of dehydration, such as dry mucous membranes, poor skin turgor, sunken eyes, decreased urine output, and increased thirst. |
To detect fever, hypoxia, tachycardia, tachypnea and hypovolemia, which are common complications of measles. To provide adequate hydration and electrolyte replacement as needed |
|
Administer antipyretics, such as acetaminophen or ibuprofen, as prescribed to reduce fever and discomfort. Avoid aspirin, as it can increase the risk of Reye syndrome in children with viral infections. |
To provide symptomatic relief and prevent febrile seizures, which can occur in children with high fever. |
|
Administer antihistamines, such as diphenhydramine or loratadine, as prescribed to reduce itching and allergic reactions. |
To provide symptomatic relief and prevent scratching, which can cause skin infections and scarring. |
|
Administer vitamin A supplements, as prescribed, to children with measles, especially those who are malnourished or have vitamin A deficiency. |
To reduce the risk of blindness, pneumonia, diarrhea, and death from measles complications. Vitamin A enhances the immune system and the integrity of the mucous membranes. |
|
Administer antibiotics, as prescribed, to patients with secondary bacterial infections, such as otitis media or pneumonia. |
To treat the underlying infection and prevent further complications, such as hearing loss or respiratory failure. |
|
Monitor the patient’s neurological status, such as level of consciousness, orientation, memory, behavior, mood, reflexes, and cranial nerve functions. Assess for signs of encephalitis, such as headache, seizures, altered mental status, focal neurological deficits, or coma. |
To detect and manage neurological complications of measles, such as APEM, ADEM, AMIBE, or SSPE. These complications can cause permanent brain damage or death if not treated promptly. |
|
Provide eye care to patients with conjunctivitis, such as cleaning the eyes with sterile saline solution, applying eye drops or ointments as prescribed, and protecting the eyes from bright light. |
To prevent corneal ulceration, scarring, or blindness from measles-induced conjunctivitis. |
|
Provide oral care to patients with Koplik spots or oral ulcers, such as rinsing the mouth with warm saline solution, applying topical anesthetics or antiseptics as prescribed, and avoiding spicy or acidic foods. |
To prevent oral infections and promote healing of the mucosal lesions caused by measles virus. |
|
Educate the patient and family about the nature, course, and prognosis of measles infection. Explain the signs and symptoms of measles and their progression. Teach them how to monitor for complications and when to seek medical attention. |
To increase their knowledge and understanding of measles infection and its management. To empower them to participate in their own care and to recognize potential problems early. |
|
Educate the patient and family about the prevention and control measures for measles infection. Emphasize the importance of vaccination for themselves and their contacts. Advise them to avoid contact with other people until they are no longer contagious. Instruct them to cover their mouth and nose when coughing or sneezing and to dispose of tissues properly. |
To prevent the transmission of measles to other susceptible individuals in the community. To protect themselves and others from future outbreaks of measles infection. |
Prevention and control
- The most effective way to prevent measles is through vaccination with the live attenuated measles vaccine.
- The measles vaccine is usually given as part of the MMR (measles-mumps-rubella) or MMRV (measles-mumps-rubella-varicella) combination vaccine.
- The recommended schedule for measles vaccination is two doses: the first dose at 12 to 15 months of age and the second dose at 4 to 6 years of age.
- The measles vaccine is safe and effective, with a seroconversion rate of 95 percent after one dose and 99 percent after two doses.
- The measles vaccine provides lifelong immunity in most cases.
- The measles vaccine can also be given to susceptible individuals within 72 hours of exposure to the measles virus as post-exposure prophylaxis.
- The measles vaccine is contraindicated in pregnant women, immunocompromised individuals, or those who have a history of severe allergic reactions to the vaccine or its components.
- Other prevention and control measures for measles include:
- Surveillance and reporting of suspected and confirmed cases of measles to the local health authorities.
- Contact tracing and isolation of exposed individuals who are not immune to measles.
- Quarantine of travelers who have visited areas with ongoing measles outbreaks or who have symptoms suggestive of measles.
- Promotion of hygiene and sanitation practices, such as hand washing, disinfection of surfaces and objects, and proper disposal of waste.
- Education and awareness campaigns to increase the public’s knowledge and acceptance of measles vaccination and its benefits .
Conclusion
- Measles is a serious and potentially fatal viral infection that can cause various complications, such as diarrhea, otitis media, pneumonia, encephalitis, SSPE, and death.
- Measles can be prevented by vaccination with the live attenuated measles vaccine, which is usually given as part of the MMR or MMRV combination vaccine.
- Measles can be diagnosed clinically or by laboratory tests, such as ELISA or RT-PCR.
- Measles can be treated with supportive care, vitamin A supplementation, and antibiotics for secondary bacterial infections.
- Measles can be controlled by isolation, contact tracing, quarantine, hygiene, and education.
Summary
- Measles is a highly contagious viral illness with fever, rash, cough, coryza, conjunctivitis, and Koplik spots.
- Measles is caused by the measles virus, which infects humans only and has no animal or environmental reservoirs.
- Measles is transmitted via person-to-person contact or airborne spread through respiratory droplets.
- Measles can be prevented by vaccination with the MMR or MMRV vaccine.
- Measles can be diagnosed clinically or by laboratory tests.
- Measles can be treated with supportive care, vitamin A supplementation, and antibiotics.
- Measles can be controlled by isolation, contact tracing, quarantine, hygiene, and education.
Infectious Mononucleosis

Introduction
- Infectious mononucleosis (IM) is an acute infectious disease that causes fever, sore throat, and cervical lymphadenopathy.
- IM is also known as mono, kissing disease, or glandular fever.
- IM is caused by the Epstein-Barr virus (EBV), a member of the herpes group.
- EBV infects and replicates in epithelial cells of the oropharynx and B cells of tonsillar tissue, causing alteration of shape and function of the infected cells.
- Infected B cells activate cell-mediated immunity with proliferation of abnormal cytotoxic T cells in lymphoid tissues.
- B cells spread the infection throughout the reticular endothelial system (RES), including the liver, spleen, and peripheral lymph nodes.
- Lymphoproliferation stops when cytotoxic T cells are able to destroy infected B cells.
Transmission Cycle/Vector/Reservoir
- IM is transmitted by direct contact with infected saliva, airborne droplets, or blood.
- IM is spread by kissing, sharing utensils, drinking from the same glass, or receiving a blood transfusion or bone marrow transplantation from an infected person.
- The incubation period of IM is 4 to 6 weeks.
- The virus can persist in saliva for months after infection.
- The reservoir of IM is humans, especially young adults aged 15 to 25 years.
Signs and Symptoms
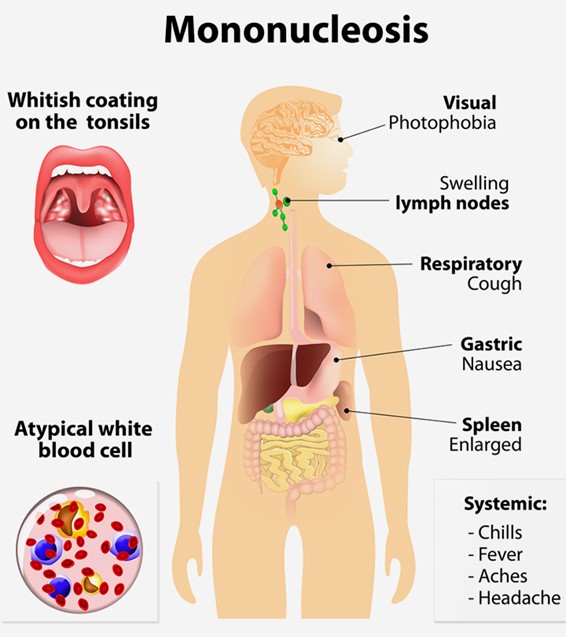
- The signs and symptoms of IM vary depending on the age and immune status of the patient.
- Some patients may be asymptomatic or have mild symptoms.
- The common signs and symptoms of IM include:
- Fever (38 to 40°C or 100.4 to 104°F)
- Sore throat (worst sore throat of the patient’s life)
- Cervical lymphadenopathy (swollen glands in the neck)
- Fatigue
- Malaise
- Headache
- Nausea
- Anorexia
- Splenomegaly (enlarged spleen)
- Hepatomegaly (enlarged liver)
- Jaundice (yellowing of the skin and eyes)
- Maculopapular rash on the trunk (resembles rubella)
- Palatal petechiae (red spots on the roof of the mouth)
- Periorbital edema (swelling around the eyes)
Diagnosis and Treatment
- The diagnosis of IM is based on clinical presentation, history of exposure, physical examination, and laboratory tests.
- The laboratory tests for IM include:
- White blood cell (WBC) count: increased to 10,000 to 20,000/μl during the second and third weeks of illness; lymphocytes and monocytes account for 50% to 70% of the total WBC count; and 10% to 20% of lymphocytes are atypical.
- Heterophile antibody tests: positive within 3 days after infection and remain positive for 2 weeks or more; also known as monospot or differential absorption tests; detect antibodies that react with antigens from other species.
- EBV virus titers: elevated, usually at the onset of the disease; measure specific antibodies against EBV antigens such as viral capsid antigen (VCA), early antigen (EA), and nuclear antigen (NA).
- Liver function tests: elevated due to liver inflammation; measure enzymes such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and bilirubin.
- Erythrocyte sedimentation rate (ESR): elevated due to inflammation; measure the rate at which red blood cells settle in a tube of blood.
- The treatment of IM is mainly supportive and symptomatic.
- The treatment of IM may include:
- Analgesics, such as acetaminophen or codeine, or nonsteroidal anti-inflammatory agents such as ibuprofen, to relieve pain and fever.
- Stool softeners to prevent constipation and straining.
- Antibiotics for secondary infections, such as streptococcal pharyngitis or sinusitis; however, antibiotics should be avoided if the patient has a rash, as they may worsen it.
- Antiviral drugs, such as acyclovir or ganciclovir, may be used in severe cases or in immunocompromised patients; however, their efficacy is limited and they may cause side effects.
- Corticosteroids, such as prednisone, may be used in rare cases of severe complications, such as airway obstruction, hemolytic anemia, thrombocytopenia, or myocarditis; however, they may increase the risk of infection and have other adverse effects.
Nursing Interventions
- The nursing interventions for patients with IM are aimed at providing comfort, preventing complications, and promoting recovery.
- The nursing interventions for patients with IM may include:
- Assessing the patient’s vital signs, weight, fluid intake and output, and nutritional status.
- Monitoring the patient’s WBC count, liver function tests, and EBV virus titers.
- Educating the patient about the nature, course, and transmission of IM.
- Encouraging the patient to rest and avoid strenuous activity or contact sports until fully recovered (usually about 3 weeks).
- Advising the patient to avoid alcohol and hepatotoxic drugs that may worsen liver damage.
- Providing a well-balanced diet and fluids to prevent dehydration and malnutrition.
- Offering soft foods or ice chips to soothe the sore throat.
- Applying warm or cold compresses to the neck to reduce swelling and pain.
- Administering medications as prescribed and observing for adverse effects
- Reporting any signs of complications, such as difficulty breathing, abdominal pain, bleeding, or neurological deficits
- Providing emotional support and reassurance to the patient and family
- Collaborating with other health care professionals as needed
Prevention and Control
- The prevention and control of IM are based on reducing exposure and enhancing immunity
- The prevention and control of IM may include:
- Avoiding close contact with people who have IM or are asymptomatic carriers
- Practicing good hygiene, such as washing hands frequently, covering mouth and nose when coughing or sneezing, and disposing of tissues properly
- Not sharing personal items, such as toothbrushes, utensils, glasses, or lip balms with others
- Using barrier methods, such as condoms or dental dams during oral sex
- Screening blood donors and bone marrow donors for EBV infection before transfusion or transplantation
- Receiving immunoglobulin injections if exposed to EBV within 48 hours; however, this is not routinely recommended due to limited evidence of effectiveness and potential side effects
- Maintaining a healthy lifestyle, such as eating well, exercising regularly, managing stress, and getting enough sleep to boost the immune system
Types and Distribution
- There are two types of IM: classic and nonclassic
- Classic IM is caused by EBV infection and accounts for 80% of cases; it is more common in young adults aged 15 to 25 years; it has a worldwide distribution; it has a higher incidence in developed countries than in developing countries; it has no seasonal variation; it has higher morbidity than mortality; it has a low risk of recurrence; it has a low risk of malignancy associated with EBV infection (such as Burkitt’s lymphoma or nasopharyngeal carcinoma)[4]
- Nonclassic IM is caused by other viruses or bacteria that mimic the symptoms of EBV infection; it accounts for 20% of cases
- Nonclassic IM is caused by other viruses or bacteria that mimic the symptoms of EBV infection; it accounts for 20% of cases; it is more common in children and older adults; it has a worldwide distribution; it has a higher incidence in developing countries than in developed countries; it has a seasonal variation, with peaks in winter and spring; it has a lower morbidity than mortality; it has a high risk of recurrence; it has a high risk of malignancy associated with non-EBV infections (such as lymphoma or leukemia).
- Some of the causes of nonclassic IM are:
- Cytomegalovirus (CMV): a herpes virus that can cause fever, sore throat, swollen glands, and fatigue; it can also affect the eyes, lungs, liver, and brain in immunocompromised patients.
- Toxoplasmosis: a parasitic infection that can cause fever, headache, muscle pain, and swollen lymph nodes; it can also cause serious complications in pregnant women and immunocompromised patients.
- HIV: the virus that causes AIDS; it can cause fever, sore throat, rash, weight loss, and swollen lymph nodes; it can also lead to opportunistic infections and cancers in immunocompromised patients.
- Rubella: a viral infection that can cause fever, rash, swollen glands, and joint pain; it can also cause birth defects in pregnant women.
- Hepatitis A, B, or C: viral infections that can cause inflammation of the liver; they can cause fever, nausea, jaundice, and abdominal pain; they can also lead to chronic liver disease and cirrhosis.
- Adenovirus: a group of viruses that can cause respiratory infections, such as colds, bronchitis, and pneumonia; they can also cause conjunctivitis, gastroenteritis, and cystitis.
Conclusion
- Infectious mononucleosis is a common and usually self-limiting disease that affects mainly young adults.
- It is caused by EBV infection in most cases, but other viruses or bacteria can also cause similar symptoms.
- It is transmitted by direct contact with infected saliva or blood.
- It causes fever, sore throat, swollen lymph nodes, and fatigue as the main symptoms.
- It is diagnosed by clinical presentation and laboratory tests.
- It is treated by supportive and symptomatic measures.
- It can be prevented by avoiding close contact with infected people and practicing good hygiene.
- It can have complications such as enlarged spleen, liver damage, or malignancy.
Summary
- Infectious mononucleosis (IM) is an acute infectious disease caused by EBV or other agents.
- IM is spread by saliva or blood contact.
- IM causes fever, sore throat, swollen glands, and fatigue.
- IM is diagnosed by symptoms and blood tests.
- IM is treated by rest, fluids, and painkillers.
- IM can be prevented by avoiding kissing or sharing items with infected people.
- IM can have serious complications such as spleen rupture or cancer.
Sexually transmitted infections (STIs)
- STIs are infections caused by pathogens that spread mainly through sexual contact.
- STIs may be caused by several types of pathogens, including protozoa, insects, bacteria, and viruses.
- STIs can affect anyone who is sexually active, regardless of age, gender, race, or sexual orientation.
- STIs can have serious consequences for health, such as infertility, ectopic pregnancy, chronic pain, cancer, and increased risk of HIV infection.
- STIs can also have social and psychological impacts, such as stigma, discrimination, shame, and guilt.
STIs are preventable and treatable, but many people do not seek testing or treatment due to lack of awareness, access, or confidentiality.
Causative agent
- The causative agent is the specific pathogen that causes an infection.
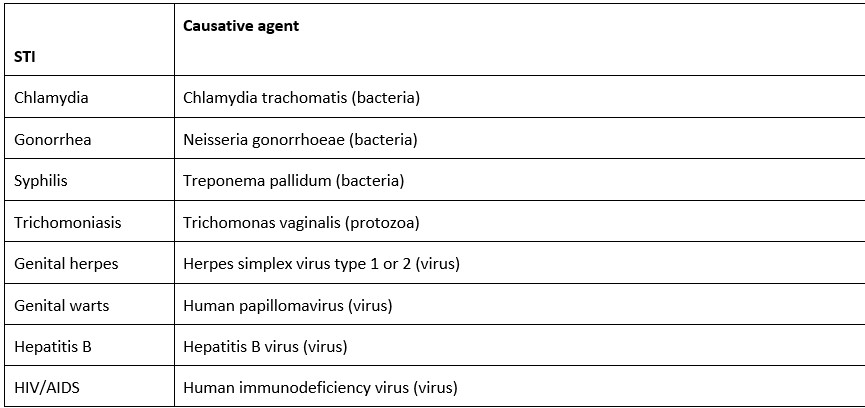
Transmission cycle/vector/reservoir
- The transmission cycle is the way a pathogen moves from one host to another.
- The vector is the organism or object that carries or transmits the pathogen.
- The reservoir is the natural habitat or source of the pathogen.
- Most STIs are transmitted through direct contact with infected body fluids or mucous membranes during sexual activity. Some examples are:
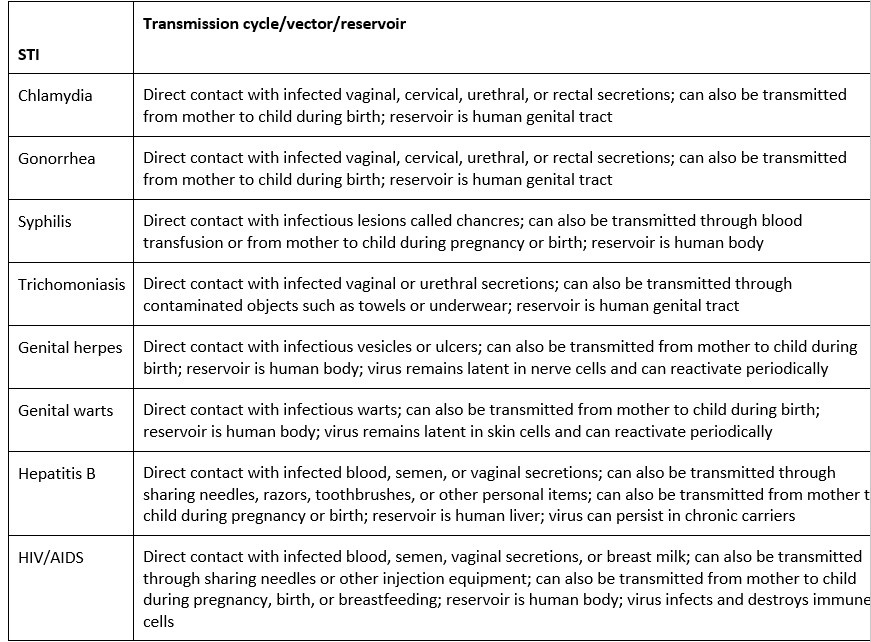
Signs and symptoms
- The signs and symptoms of STIs vary depending on the type of infection and the stage of progression. Some common signs and symptoms are:
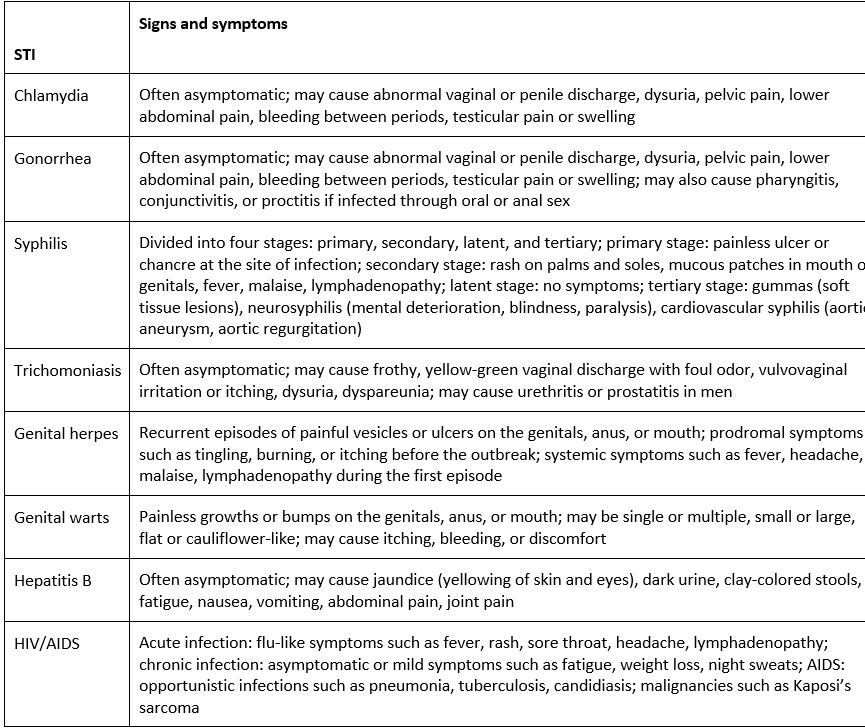
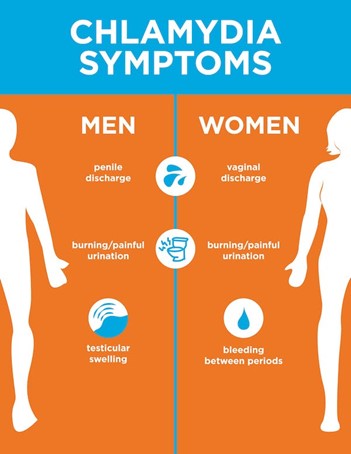
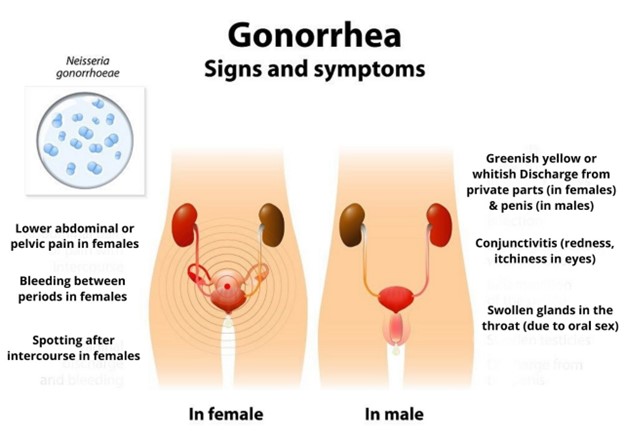
Diagnosis and treatment
- The diagnosis of STIs depends on the type of infection and the availability of testing methods. Some common diagnostic methods are:
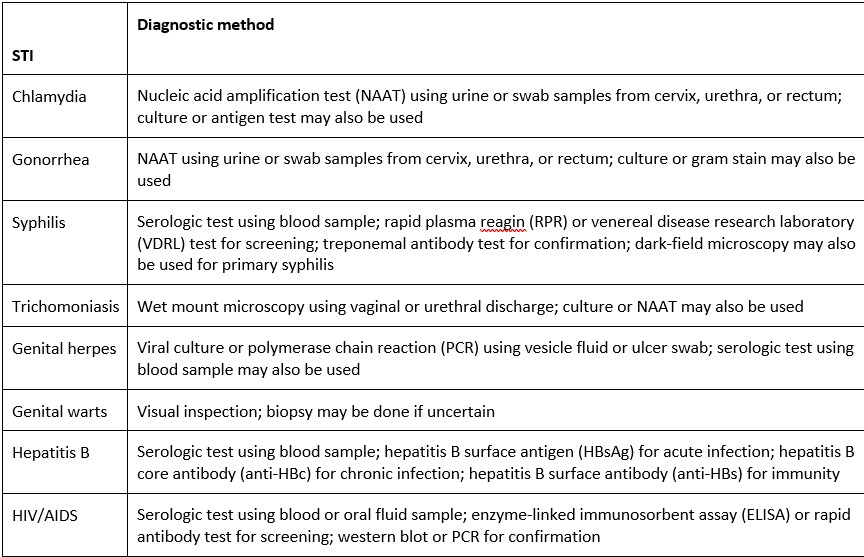
- The treatment of STIs depends on the type of infection and the severity of symptoms. Some common treatment options are:
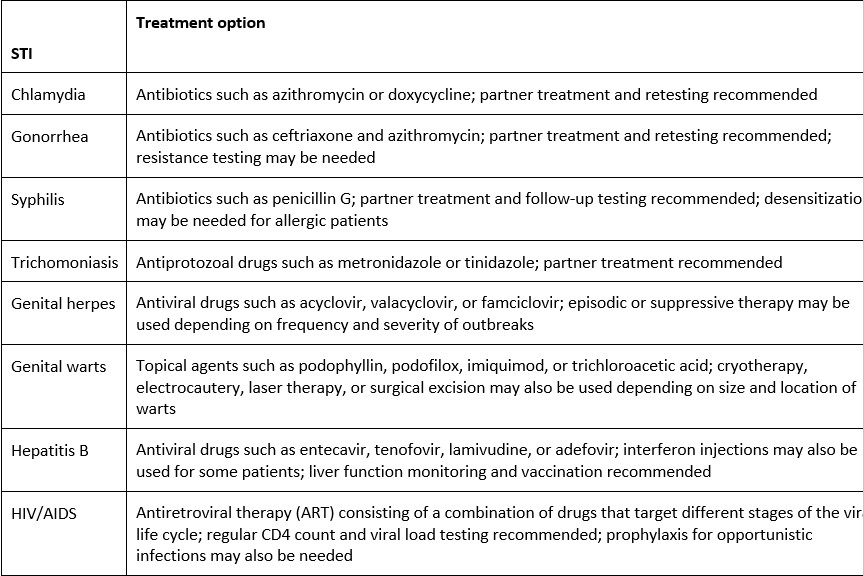
Nursing interventions
- The nursing interventions for patients with STIs aim to provide care, education, counseling, and support. Some general nursing interventions are:
- Assess the patient’s history, symptoms, risk factors, sexual practices, and psychosocial status
- Obtain appropriate specimens for testing and inform the patient about the results and implications
- Administer prescribed medications and monitor for adverse effects and compliance
- Provide wound care, pain management, and comfort measures as needed
- Educate the patient about the nature, transmission, prevention, and treatment of STIs
- Counsel the patient about the emotional and social impact of STIs and refer to appropriate resources if needed
- Encourage the patient to notify and treat their sexual partners and avoid sexual activity until cured
- Promote safe sex practices such as condom use, mutual monogamy, regular screening, and vaccination
- Advocate for the patient’s rights to confidentiality, privacy, dignity, and respect
Prevention and control
- The prevention and control of STIs are important to reduce the morbidity, mortality, and transmission of these infections. Some strategies for prevention and control are:
- Primary prevention: aims to prevent exposure or infection by modifying behaviors, reducing risk factors, and increasing protective factors. Some examples are:
- Abstinence or mutual monogamy with an uninfected partner
- Consistent and correct use of condoms and other barrier methods
- Avoidance of sharing needles, razors, toothbrushes, or other personal items that may be contaminated with blood
- Vaccination against hepatitis B and human papillomavirus
- Pre-exposure prophylaxis (PrEP) for high-risk individuals to prevent HIV infection
- Post-exposure prophylaxis (PEP) for individuals who may have been exposed to HIV within 72 hours
- Secondary prevention: aims to detect and treat infection early to prevent complications and transmission. Some examples are:
- Routine screening and testing for STIs according to guidelines and risk assessment
- Prompt initiation of appropriate treatment and follow-up
- Partner notification and treatment to prevent reinfection and further spread
- Reporting of STIs to public health authorities for surveillance and contact tracing
- Tertiary prevention: aims to minimize the impact of infection on health and quality of life. Some examples are:
- Management of chronic conditions such as HIV/AIDS and hepatitis B
- Treatment of opportunistic infections and malignancies associated with STIs
- Provision of palliative care and end-of-life care for terminal cases
- Support and counseling for patients with STIs and their families
Types and distribution
- STIs can be classified into different types based on their causative agents, clinical manifestations, modes of transmission, and epidemiology. Some common types are:
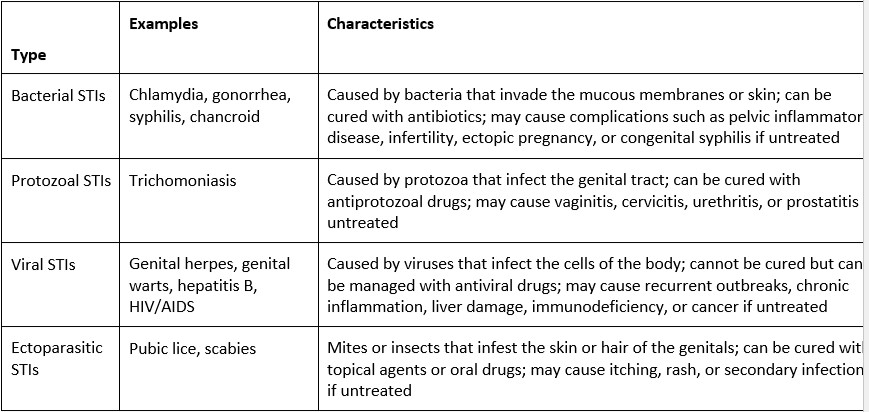
- The distribution of STIs varies by region, population, and time. Some factors that influence the distribution are:
- Demographic factors such as age, gender, race, ethnicity, education, income, occupation, marital status
- Behavioral factors such as sexual activity, number of partners, condom use, substance use
- Biological factors such as immunity, susceptibility, coinfection
- Social factors such as stigma, discrimination, access to health care, quality of services
- Environmental factors such as climate, sanitation, hygiene
- According to the World Health Organization (WHO), there were an estimated 376 million new cases of four curable STIs (chlamydia, gonorrhea, syphilis, trichomoniasis) in 2016. The global prevalence of these STIs was 3.9% for chlamydia, 0.9% for gonorrhea, 0.6% for syphilis, and 5.3% for trichomoniasis. The highest burden of these STIs was in the African region, followed by the Americas region.
- The WHO also estimated that there were 417 million people living with genital herpes in 2016, with a global prevalence of 11.3%. The highest prevalence was in the African region, followed by the Americas region.
- The WHO also reported that there were 71 million people living with hepatitis B in 2015, with a global prevalence of 0.9%. The highest prevalence was in the Western Pacific region, followed by the African region.
- The WHO also stated that there were 37.9 million people living with HIV in 2018, with a global prevalence of 0.8%. The highest prevalence was in the African region, followed by the European region.
Conclusion
- STIs are infections that spread mainly through sexual contact and can cause serious health and social problems.
- STIs can be prevented and controlled by modifying behaviors, reducing risk factors, increasing protective factors, screening, testing, treating, notifying, reporting, and supporting.
- STIs can be classified into different types based on their causative agents, clinical manifestations, modes of transmission, and epidemiology.
- STIs have different distribution patterns by region, population, and time.
Summary
- STIs are caused by pathogens that spread mainly through sexual contact
- STIs may be caused by protozoa, insects, bacteria, or viruses
- STIs can affect anyone who is sexually active
- STIs can have serious consequences for health, such as infertility, ectopic pregnancy, chronic pain, cancer, and increased risk of HIV infection
- STIs can also have social and psychological impacts, such as stigma, discrimination, shame, and guilt
- STIs are preventable and treatable, but many people do not seek testing or treatment due to lack of awareness, access, or confidentiality
- STIs can be diagnosed by various methods such as NAAT, culture, serology, microscopy, or visual inspection
- STIs can be treated by various options such as antibiotics, antivirals, antiprotozoals, topical agents, or surgical procedures
- Nursing interventions for patients with STIs include assessment, specimen collection, medication administration, wound care, pain management, education, counseling, partner notification, reporting, and referral
- Prevention and control of STIs include primary prevention (preventing exposure or infection), secondary prevention (detecting and treating infection early), and tertiary prevention (minimizing the impact of infection)
- Types of STIs include bacterial STIs (chlamydia, gonorrhea, syphilis), protozoal STIs (trichomoniasis), viral STIs (genital herpes, genital warts, hepatitis B, HIV/AIDS), and ectoparasitic STIs (pubic lice, scabies)
- Distribution of STIs varies by region, population, and time
Gastroenteritis
- Gastroenteritis is a self-limiting inflammation of the stomach and small intestine.
- It is also known as intestinal flu, traveler’s diarrhea, viral enteritis, and food poisoning.
- It is caused by various infectious or inflammatory processes in the intestine that affect the enterocyte secretory and absorptive functions.
- It is characterized by diarrhea (>3 stool episodes in 24 hours) with or without vomiting.
- It can be classified as invasive or inflammatory, or secretory, depending on the pathogenesis.
- It can be associated with fever, abdominal pain, dehydration, electrolyte imbalance, and malnutrition.
- It is a leading cause of morbidity and mortality in children around the world.
- It is transmitted through the fecal-oral route or ingestion of contaminated food or water.
- t can be prevented by proper hygiene, sanitation, vaccination, and food safety practices.
Causative agent
- Gastroenteritis has many infectious causes, including viruses, bacteria, and parasites.
- Viral gastroenteritis is the most common cause of diarrhea in children globally.
- Rotavirus is the most frequent cause of diarrhea in young children during the winter months.
- Norovirus is the most common cause of outbreaks of acute gastroenteritis because it is highly contagious.
- Other viral causes include astroviruses, sapovirus, and enteric adenoviruses.
- Bacterial gastroenteritis is less common than viral but can be more severe.
- E. coli and C. diff produce enterotoxins that cause watery diarrhea.
- Salmonella and Campylobacter are the most common bacterial causes of bloody diarrhea. They are acquired from undercooked poultry, eggs, or unpasteurized milk.
- Shigella, Yersinia, Vibrio cholerae, and Clostridium perfringens are other bacterial causes of gastroenteritis.
- Parasitic gastroenteritis is caused by protozoa or helminths that invade or attach to the intestinal mucosa.
- Giardia lamblia is the most common parasitic cause of chronic diarrhea in children and travelers. It is acquired from contaminated water or food.
- Cryptosporidium parvum, Entamoeba histolytica, Cyclospora cayetanensis, and Ascaris lumbricoides are other parasitic causes of gastroenteritis.
Transmission cycle/vector/reservoir
- The transmission cycle of gastroenteritis involves the ingestion of infectious agents from fecal-contaminated sources such as water, food, hands, or objects.
- The vector is the organism that carries or transmits the infectious agent from one host to another. For example, flies can act as vectors for some bacterial causes of gastroenteritis such as Shigella or E. coli.
- The reservoir is the natural habitat where the infectious agent lives and multiplies. For example, animals can act as reservoirs for some zoonotic causes of gastroenteritis such as Salmonella or Campylobacter.
Signs and symptoms

- The signs and symptoms of gastroenteritis vary depending on the type, severity, and duration of the infection.
- The main symptom is diarrhea, which can be watery or bloody, acute or chronic, mild or severe.
- Other symptoms may include vomiting, nausea, anorexia, abdominal pain or cramps, bloating, flatulence, fever, chills, headache, malaise, weight loss, dehydration signs (dry mouth, skin turgor), electrolyte imbalance signs (muscle weakness, cramps), and malnutrition signs (poor growth, edema).
Diagnosis and treatment
- The diagnosis of gastroenteritis is based on the history, physical examination, and stool analysis.
- The history should include the onset, duration, frequency, and characteristics of diarrhea and vomiting, as well as the exposure to potential sources of infection such as travel, food, water, animals, or contacts.
- The physical examination should assess the hydration status, vital signs, abdominal tenderness or distension, and signs of complications such as shock or sepsis.
- The stool analysis should include the appearance, color, odor, consistency, and presence of blood, mucus, or parasites. It may also include culture, microscopy, antigen detection, or PCR tests to identify the specific causative agent.
- The treatment of gastroenteritis is mainly supportive and symptomatic.
- The main goal is to prevent or correct dehydration and electrolyte imbalance by oral rehydration therapy (ORT) or intravenous fluid therapy (IVF) depending on the severity of the condition.
- ORT involves the administration of oral rehydration solution (ORS) that contains glucose and electrolytes such as sodium, potassium, chloride, and bicarbonate. The recommended amount of ORS is 50-100 ml/kg for mild to moderate dehydration and 100-200 ml/kg for severe dehydration over 3-4 hours.
- IVF involves the administration of isotonic fluids such as normal saline or lactated Ringer’s solution that contain electrolytes similar to plasma. The recommended amount of IVF is 20-40 ml/kg for mild to moderate dehydration and 40-60 ml/kg for severe dehydration over 1-2 hours.
- Antidiarrheal agents such as loperamide or bismuth subsalicylate are not recommended for children with gastroenteritis because they can cause adverse effects such as ileus, toxic megacolon, or Reye’s syndrome.
- Antiemetic agents such as ondansetron or metoclopramide may be used for children with persistent vomiting that interferes with oral intake.
- Antibiotic therapy is not indicated for most cases of gastroenteritis because it can increase the risk of antibiotic resistance, adverse effects, or prolongation of bacterial shedding.
- Antibiotic therapy may be considered for children with severe or bloody diarrhea caused by specific bacterial pathogens such as Shigella, Campylobacter, Yersinia, Vibrio cholerae, or Clostridium difficile. The choice of antibiotic depends on the susceptibility of the organism and the local resistance patterns.
- Antiparasitic therapy may be indicated for children with confirmed parasitic infections such as Giardia lamblia, Cryptosporidium parvum, Entamoeba histolytica, Cyclospora cayetanensis, or Ascaris lumbricoides. The choice of antiparasitic agent depends on the type of parasite and the clinical presentation.
Nursing interventions
- The nursing interventions for gastroenteritis are aimed at providing supportive care, monitoring the hydration status and vital signs, administering the prescribed fluids and medications, and educating the patient and family about the prevention and control measures.
- Supportive care includes maintaining a comfortable environment, providing oral hygiene, encouraging rest and sleep, and offering bland and soft foods in small and frequent meals once vomiting subsides.
- Monitoring the hydration status and vital signs includes assessing the skin turgor, mucous membranes, urine output, capillary refill time, pulse, blood pressure, temperature, and weight. Any signs of dehydration or shock should be reported promptly to the physician.
- Administering the prescribed fluids and medications includes following the orders for ORT or IVF, measuring the intake and output accurately, and giving the antiemetic or antibiotic agents as indicated. Any adverse effects or allergic reactions should be observed and reported immediately to the physician
- Educating the patient and family about the prevention and control measures includes providing information about the causes, transmission, and complications of gastroenteritis, as well as the importance of hygiene, sanitation, vaccination, and food safety practices. The patient and family should be instructed to wash their hands frequently with soap and water, especially before eating or preparing food, after using the toilet or changing diapers, and after touching animals or contaminated objects. They should also be advised to avoid sharing utensils, cups, or towels with others, to dispose of fecal matter properly, to boil or filter water before drinking or cooking, to cook food thoroughly and refrigerate leftovers promptly, to peel or wash fruits and vegetables before eating, and to avoid raw or undercooked meat, eggs, or seafood. They should also be informed about the availability and benefits of rotavirus vaccination for infants and young children .
Prevention and control
- The prevention and control of gastroenteritis is a public health priority that requires a multidisciplinary approach involving healthcare providers, policymakers, community leaders, and individuals.
- The main strategies for preventing and controlling gastroenteritis are:
- Improving access to safe water and sanitation facilities such as latrines, sewers, and waste management systems.
- Promoting hygiene education and behavior change such as hand washing with soap and water, safe food handling and preparation, and proper disposal of human and animal feces.
- Implementing vaccination programs against rotavirus and cholera for high-risk populations such as infants, children, travelers, refugees, and immunocompromised individuals.
- Enhancing surveillance and outbreak response systems such as laboratory testing, case reporting, contact tracing, isolation, quarantine, and mass treatment.
- Strengthening health system capacity and resilience such as training health workers, providing essential supplies and equipment, ensuring quality of care, and improving referral mechanisms.
Types and distribution
- Gastroenteritis can be classified into different types based on the pathogenesis, clinical presentation, and epidemiology of the infection.
- The main types of gastroenteritis are:
- Invasive or inflammatory gastroenteritis: This type is caused by bacteria or parasites that invade the intestinal mucosa and cause tissue damage, inflammation, and bleeding. It is characterized by bloody diarrhea (dysentery), fever, abdominal pain, and tenesmus. It can lead to complications such as dehydration, anemia, septicemia, and toxic megacolon. It is more common in developing countries where sanitation is poor and malnutrition is prevalent. Examples of invasive or inflammatory gastroenteritis include shigellosis, amebiasis, yersiniosis, and enterohemorrhagic E. coli infection.
- Secretory gastroenteritis: This type is caused by viruses or bacteria that produce enterotoxins that stimulate the secretion of fluid and electrolytes into the intestinal lumen. It is characterized by watery diarrhea (rice-water stool), vomiting, dehydration, and electrolyte imbalance. It can lead to complications such as hypovolemic shock, acidosis, and renal failure. It is more common in tropical and subtropical regions where water quality is poor and crowding is high. Examples of secretory gastroenteritis include rotavirus infection, cholera, and enterotoxigenic E. coli infection.
- The distribution of gastroenteritis varies according to the geographic location, climate, season, socioeconomic status, and age group of the population.
- Some general patterns of distribution are:
- Viral gastroenteritis is more prevalent in temperate regions during the winter months.
- Bacterial gastroenteritis is more prevalent in tropical and subtropical regions during the rainy season.
- Parasitic gastroenteritis is more prevalent in rural areas where sanitation is poor and animal contact is frequent.
- Rotavirus gastroenteritis is more common in infants and young children under 5 years of age.
- Norovirus gastroenteritis is more common in adults and older children in institutional settings such as schools, hospitals, or cruise ships.
- Cholera gastroenteritis is more common in areas with endemic or epidemic outbreaks such as Africa, Asia, or Latin America.
Conclusion
- Gastroenteritis is a common condition that affects millions of people worldwide every year.
- It is caused by various infectious agents that affect intestinal function and cause diarrhea with or without vomiting.
- It can be classified into invasive inflammatory, or secretory types depending on the pathogenesis.
- It can be associated with various signs and symptoms such as fever, abdominal pain, dehydration, and electrolyte imbalance.
- It can be diagnosed by history, physical examination, and stool analysis.
- It can be treated by supportive and symptomatic measures such as oral or intravenous rehydration therapy, and antiemetic or antibiotic agents.
- It can be prevented and controlled by hygiene, sanitation, vaccination, and surveillance measures.
- It has different types and distribution patterns according to geographic, climatic, socioeconomic, and demographic factors.
Summary
- Gastroenteritis is a self-limiting inflammation of the stomach and small intestine caused by various infectious agents .
- The main symptom is diarrhea, which can be watery or bloody, acute or chronic, mild or severe .
- The main goal of treatment is to prevent or correct dehydration and electrolyte imbalance by oral or intravenous rehydration therapy .
- The main strategy of prevention and control is to improve hygiene, sanitation, vaccination, and surveillance practices .
- The main types of gastroenteritis are invasive or inflammatory, or secretory, depending on the pathogenesis.
- The main factors that influence the distribution of gastroenteritis are geographic location, climate, season, socioeconomic status, and age group.
Vulvovaginitis

- Vulvovaginitis is an inflammation or infection of the vulva and vagina that can affect women and girls of all ages.
- It can be caused by various factors, such as bacterial, fungal, protozoan, or viral infections, allergic reactions, chemical irritations, poor hygiene, foreign bodies, or hormonal changes.
- It can result in symptoms such as vaginal irritation and itching, urinary discomfort, dyspareunia, abnormal discharge, odor, bleeding, or inflammation.
- It can be diagnosed by history, physical examination, microscopic examination, pH testing, culture, or other laboratory tests depending on the type.
- It can be treated by antibiotics, antifungals, antiprotozoals, antivirals, topical creams or gels, or hormonal therapy depending on the type.
- It can be prevented and controlled by maintaining good hygiene, avoiding irritants and allergens, using condoms or other barrier methods, limiting sexual partners, treating underlying conditions, and seeking medical attention when needed.
Types and Distribution
- There are several types of vulvovaginitis that have different causes, characteristics, and prevalence. Some of the common types are:
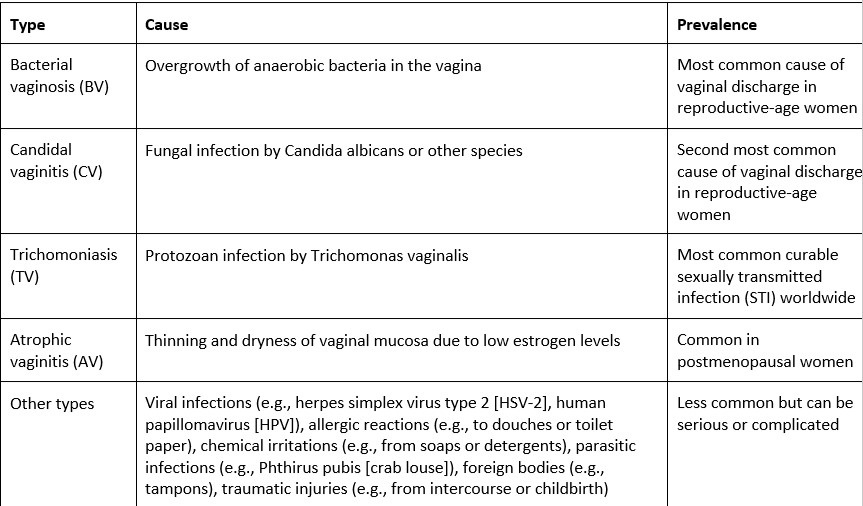
Causative Agent
- The causative agent of vulvovaginitis depends on the type of infection or inflammation. Some of the common agents are:
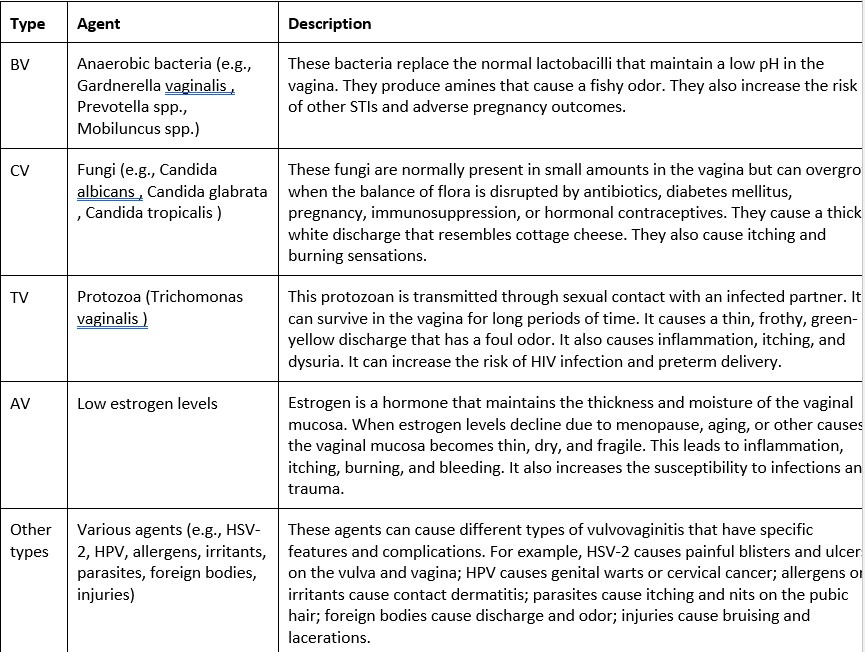
Transmission Cycle/Vector/Reservoir
- The transmission cycle/vector/reservoir of vulvovaginitis depends on the type of infection or inflammation. Some of the common modes are:
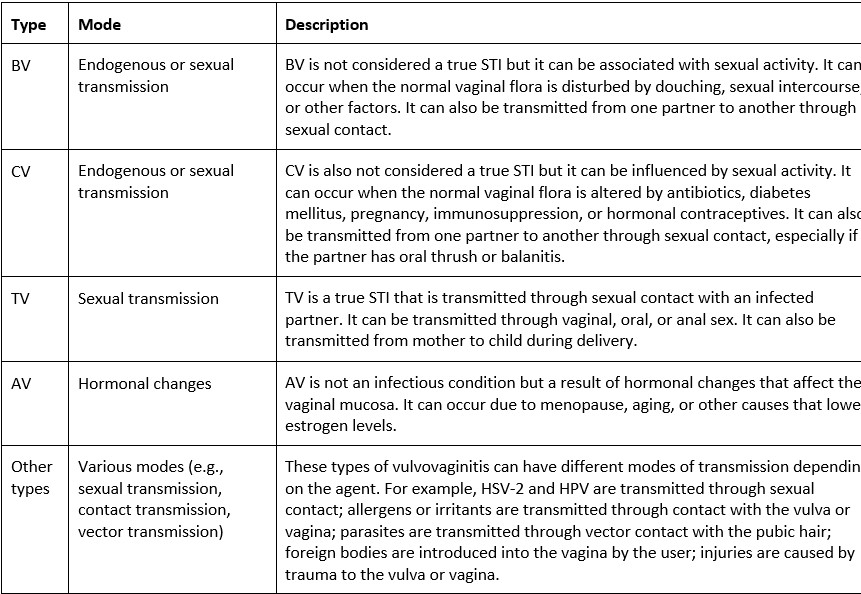
Signs and Symptoms
- The signs and symptoms of vulvovaginitis vary according to the type of infection or inflammation. Some of the common signs and symptoms are:
|
Type |
Signs and Symptoms |
|
BV |
- Vaginal discharge that is thin, gray-white, or milky - Fishy odor that is worse after intercourse or menstruation - Vaginal pH greater than 4.5 - Clue cells (vaginal epithelial cells with adherent bacteria) on microscopic examination - Minimal inflammation or irritation - May be asymptomatic in some cases |
|
CV |
- Vaginal discharge that is thick, white, clumpy, or curdy - No odor or mild yeast-like odor - Vaginal pH less than 4.5 - Hyphae (fungal filaments) or pseudohyphae (branching buds) on microscopic examination - Intense inflammation, irritation, itching, burning, or swelling - May have urinary symptoms such as dysuria or frequency |
|
TV |
- Vaginal discharge that is thin, frothy, green-yellow, or blood-tinged - Foul odor that is musty or rotten - Vaginal pH greater than 5.0 - Motile trichomonads (flagellated protozoa) on microscopic examination - Severe inflammation, irritation, itching, burning, redness, edema, or petechiae (strawberry cervix) - May have urinary symptoms such as dysuria or frequency |
|
AV |
- Vaginal dryness or atrophy - No discharge or scanty discharge that is clear or yellowish - No odor or mild odor - Vaginal pH greater than 5.0 - Thinning and loss of rugae (folds) of vaginal mucosa on examination - |
Diagnosis and Treatment
- The diagnosis and treatment of vulvovaginitis depend on the type and cause of the infection or inflammation. Some of the common methods are:
|
Type |
Diagnosis |
Treatment |
|
BV |
- History and physical examination - Vaginal pH testing (greater than 4.5) - Microscopic examination (clue cells) - Culture or DNA probe testing |
- Oral or intravaginal metronidazole, clindamycin, tinidazole, or secnidazole - Treatment of sexual partners is not necessary unless they have symptoms |
|
CV |
- History and physical examination - Vaginal pH testing (less than 4.5) - Microscopic examination (hyphae or pseudohyphae) - Culture or DNA probe testing |
- Oral fluconazole or topical azoles (miconazole, clotrimazole, butoconazole, tioconazole) - Topical azoles are preferred during pregnancy - Treatment of sexual partners is not necessary unless they have symptoms |
|
TV |
- History and physical examination - Vaginal pH testing (greater than 5.0) - Microscopic examination (motile trichomonads) - Culture or nucleic acid amplification testing |
- Oral metronidazole or tinidazole - Treatment of sexual partners is recommended to prevent reinfection |
|
AV |
- History and physical examination - Vaginal pH testing (greater than 5.0) - Thinning and loss of rugae of vaginal mucosa on examination |
- Hormonal therapy (estrogen creams, tablets, or rings)- Nonhormonal therapy (lubricants, moisturizers, or hyaluronic acid)[ |
- Other types | - History and physical examination - Specific tests for the causative agent (e.g., viral culture, antigen testing, PCR, serology)[
- Culture or microscopy for foreign bodies or parasites| - Specific treatment for the causative agent (e.g., antivirals, antiparasitics, antibiotics)[
- Removal of foreign bodies or irritants[
Anti-inflammatory agents or steroids for allergic or inflammatory reactions|
Prevention and Control
- The prevention and control of vulvovaginitis depend on the type and cause of the infection or inflammation. Some of the general strategies are:
|
Type |
Strategy |
|
BV |
- Avoid douching, which can disrupt the normal vaginal flora • Limit sexual partners and use condoms or other barrier methods • Treat underlying conditions that may predispose to BV, such as diabetes mellitus • Seek medical attention if symptoms recur or persist |
|
CV |
- Avoid antibiotics, diabetes mellitus, pregnancy, immunosuppression, or hormonal contraceptives that may alter the normal vaginal flora • Limit sexual partners and use condoms or other barrier methods • Avoid tight-fitting clothing, synthetic underwear, or wet swimsuits that may create a moist environment for yeast growth • Seek medical attention if symptoms recur or persist |
|
TV |
- Limit sexual partners and use condoms or other barrier methods • Avoid sexual contact until both partners are treated and cured • Seek medical attention if symptoms recur or persist |
|
AV |
- Use hormonal therapy as prescribed by your health care provider • Use lubricants, moisturizers, or hyaluronic acid to relieve dryness and discomfort • Avoid irritants or allergens that may worsen the symptoms |
|
Other types |
- Identify and avoid the causative agent (e.g., virus, allergen, irritant, parasite, foreign body, injury) • Use specific treatment as prescribed by your health care provider • Maintain good hygiene and avoid contact with infected persons or objects • Seek medical attention if symptoms recur or persist
|
Nursing interventions for vulvovaginitis
The nursing interventions for vulvovaginitis depend on the type and cause of the infection or inflammation. Some of the general interventions are:
|
Type |
Intervention |
|
BV |
- Provide patient education on the causes, symptoms, diagnosis, treatment, and prevention of BV • Administer oral or intravaginal antibiotics as prescribed and monitor for adverse effects • Advise the patient to complete the full course of antibiotics and avoid alcohol consumption during treatment • Teach the patient to avoid douching, which can disrupt the normal vaginal flora • Encourage the patient to limit sexual partners and use condoms or other barrier methods • Assess the patient for signs of complications, such as pelvic inflammatory disease (PID), preterm labor, or other STIs • Provide comfort measures, such as warm sitz baths, cold compresses, or analgesics, to relieve irritation and discomfort • Instruct the patient to report any recurrence or persistence of symptoms to the health care provider |
|
CV |
- Provide patient education on the causes, symptoms, diagnosis, treatment, and prevention of CV • Administer oral fluconazole or topical azoles as prescribed and monitor for adverse effects • Advise the patient to complete the full course of antifungals and avoid sexual intercourse during treatment • Teach the patient to avoid antibiotics, diabetes mellitus, pregnancy, immunosuppression, or hormonal contraceptives that may alter the normal vaginal flora • Encourage the patient to limit sexual partners and use condoms or other barrier methods • Assess the patient for signs of complications, such as recurrent or resistant infections • Provide comfort measures, such as warm sitz baths, cold compresses, or analgesics, to relieve irritation and discomfort • Instruct the patient to report any recurrence or persistence of symptoms to the health care provider |
|
TV |
- Provide patient education on the causes, symptoms, diagnosis, treatment, and prevention of TV • Administer oral metronidazole or tinidazole as prescribed and monitor for adverse effects • Advise the patient to complete the full course of antiprotozoals and avoid alcohol consumption during treatment • Teach the patient to abstain from sexual contact until both partners are treated and cured • Encourage the patient to limit sexual partners and use condoms or other barrier methods • Assess the patient for signs of complications, such as HIV infection, preterm delivery, or other STIs • Provide comfort measures, such as warm sitz baths, cold compresses, or analgesics, to relieve irritation and discomfort • Instruct the patient to report any recurrence or persistence of symptoms to the health care provider |
|
AV |
- Provide patient education on the causes, symptoms, diagnosis, treatment, and prevention of AV • Administer hormonal therapy (estrogen creams, tablets, or rings) as prescribed and monitor for adverse effects • Advise the patient to use hormonal therapy as directed and report any abnormal bleeding or breast changes to the health care provider • Teach the patient to use lubricants, moisturizers, or hyaluronic acid to relieve dryness and discomfort • Encourage the patient to avoid irritants or allergens that may worsen the symptoms • Assess the patient for signs of complications, such as infections or trauma • Provide comfort measures, such as warm sitz baths, cold compresses, or analgesics, to relieve irritation and discomfort |
|
Other types |
- Provide patient education on the causes, symptoms, diagnosis, treatment, and prevention of other types of vulvovaginitis • Administer specific treatment (e.g., antivirals, antiparasitics, antibiotics) as prescribed and monitor for adverse effects • Advise the patient to follow the instructions for the specific treatment and report any side effects or allergic reactions to the health care provider • Teach the patient to identify and avoid the causative agent (e.g., virus, allergen, irritant, parasite, foreign body) • Encourage the patient to maintain good hygiene and wear cotton underwear • Assess the patient for signs of complications, such as chronic pain, dyspareunia, or infertility • Provide comfort measures, such as warm sitz baths, cold compresses, or analgesics, to relieve irritation and discomfort |
Conclusion
- Vulvovaginitis is a common condition that affects women and girls of all ages. It can be caused by various factors, such as infections, allergic reactions, chemical irritations, hormonal changes, or foreign bodies. It can result in symptoms such as vaginal discharge, odor, itching, burning, inflammation, or bleeding. It can be diagnosed by history, physical examination, and laboratory tests depending on the type. It can be treated by medications, topical agents, or hormonal therapy depending on the cause. It can be prevented and controlled by maintaining good hygiene, avoiding irritants and allergens, using condoms or other barrier methods, limiting sexual partners, treating underlying conditions, and seeking medical attention when needed. Nursing interventions for vulvovaginitis include providing patient education, administering medications as prescribed, monitoring for adverse effects and complications, providing comfort measures, and instructing the patient to report any recurrence or persistence of symptoms.
Summary
- Vulvovaginitis is an inflammation or infection of the vulva and vagina
- It can be caused by bacteria, fungi, protozoa, viruses, allergens, irritants, hormones, or foreign bodies
- It can cause discharge, odor, itching, burning, inflammation, or bleeding
- It can be diagnosed by history, physical examination, pH testing, microscopic examination, culture, or other tests
- It can be treated by antibiotics, antifungals, antiprotozoals, antivirals, topical creams or gels, or hormonal therapy
- It can be prevented and controlled by hygiene, avoiding irritants and allergens, using condoms or other barriers, limiting sexual partners, treating underlying conditions, and seeking medical attention
- Nursing interventions include patient education, medication administration, adverse effect and complication monitoring, comfort measures, and symptom reporting
Ebola
- Ebola virus disease (EVD) is a severe and often fatal viral hemorrhagic fever that affects humans and other primates. It is caused by infection with one of five species of Ebola virus: Zaire, Sudan, Bundibugyo, Tai Forest, and Reston. The first four species can cause disease in humans, while the fifth species has only been found in nonhuman primates. EVD was first discovered in 1976 near the Ebola River in Zaire (now Democratic Republic of Congo) and has since caused several outbreaks in Africa, with the largest one occurring in West Africa from 2014 to 2016. EVD is a public health emergency that requires prompt identification, isolation, treatment, and prevention of further transmission.

Causative agent
- Ebola virus belongs to the family Filoviridae, which consists of filamentous, enveloped, negative-sense RNA viruses. The genome of Ebola virus is about 19 kilobases long and encodes seven structural proteins: nucleoprotein, polymerase cofactor, transcription activator, glycoprotein, matrix protein, RNA-dependent RNA polymerase, and VP24 protein. The glycoprotein is responsible for binding to host cell receptors and mediating viral entry. The matrix protein forms a layer between the viral envelope and the nucleocapsid, which contains the viral genome and the nucleoprotein-polymerase complex. The VP24 protein is involved in viral assembly and budding. The other proteins play roles in viral replication, transcription, and immune evasion.
Transmission cycle/vector/reservoir
- The natural reservoir of Ebola virus is unknown, but it is suspected to be a type of fruit bat that lives in tropical forests. The virus can be transmitted from animals to humans through direct contact with blood, body fluids, organs, or tissues of infected animals such as bats, monkeys, chimpanzees, gorillas, antelopes, or porcupines. The virus can also be transmitted from humans to humans through direct contact with blood, body fluids, organs, or tissues of infected people or with surfaces and materials contaminated with these fluids such as bedding, clothing, needles, syringes, or medical equipment. The virus can also be transmitted through sexual contact with semen of infected men up to three months after recovery. The virus is not spread through air, water, or food in general. However, in Africa, some cases may be linked to handling bushmeat (wild animals hunted for food) or contact with bats.
Signs and symptoms
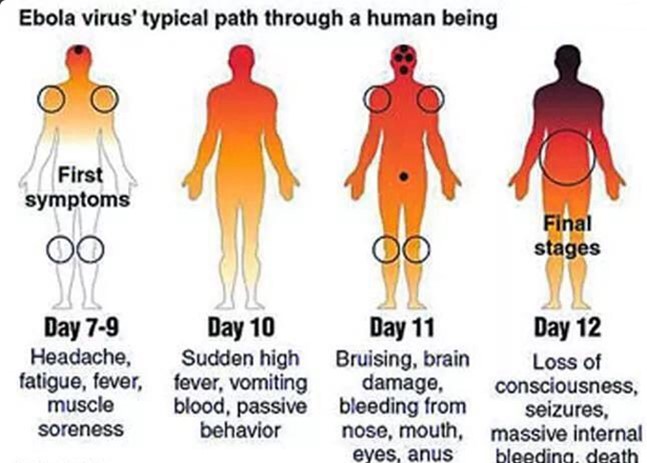
-The incubation period of EVD ranges from 2 to 21 days after exposure to the virus, but the average is 8 to 10 days. The onset of symptoms is usually sudden and includes fever (>101.5°F or 38.6°C), weakness, severe headache, lack of appetite, joint and muscle pain, sore throat. These symptoms are followed by abdominal pain, vomiting, diarrhea, rash, red eyes, abnormal kidney function, unexplained internal and external bleeding or bruising, thrombocytopenia (low platelet count), increased liver enzymes, and increased white blood cells. The bleeding may occur from the nose, gums, eyes, ears, skin, stomach, intestines, or genitals. The bleeding may lead to shock, organ failure, and death. The case fatality rate of EVD varies depending on the virus species and the quality of care provided. It can range from 25% to 90%, with an average of about 50%. Some survivors may experience long-term complications such as joint pain, vision problems, hearing loss, memory loss, depression, or post-traumatic stress disorder.
Diagnosis and treatment
- The diagnosis of EVD is based on clinical suspicion and laboratory confirmation. Clinical suspicion is raised when a person has a history of exposure to a known or suspected source of Ebola virus infection and presents with compatible signs and symptoms. Laboratory confirmation is done by testing blood or body fluid samples for the presence of Ebola virus antigens (proteins), antibodies (immune response), or genetic material (RNA) using various methods such as enzyme-linked immunosorbent assay (ELISA), reverse transcriptase polymerase chain reaction (RT-PCR), or virus isolation and culture. The samples must be handled with extreme caution and biosafety level 4 (BSL-4) precautions to prevent accidental infection of laboratory personnel or contamination of the environment.
- The treatment of EVD is mainly supportive and symptomatic. There is no specific antiviral drug or vaccine available for EVD, although some experimental therapies are under development and evaluation. The supportive and symptomatic treatment includes:
- Providing fluids and electrolytes to prevent dehydration and correct electrolyte imbalance.
- Administering oxygen and mechanical ventilation to improve respiratory function.
- Giving blood transfusions and clotting factors to control bleeding and prevent disseminated intravascular coagulation (DIC).
- Monitoring and treating organ dysfunction such as renal failure, liver failure, or septic shock.
- Managing pain, fever, nausea, and other symptoms with appropriate medications.
- Providing psychological support and counseling to patients and their families.
Nursing interventions
- The nursing interventions for EVD are aimed at providing quality care to the patients, preventing further transmission of the virus, and protecting the health and safety of the healthcare workers and the community. The nursing interventions include:
- Applying strict infection control practices such as hand hygiene, personal protective equipment (PPE), environmental disinfection, waste management, and safe burial of the dead.
- Educating the patients and their families about the nature, transmission, prevention, and treatment of EVD and addressing their fears and concerns.
- Assessing the patients’ vital signs, fluid balance, nutritional status, pain level, mental status, and organ function regularly and reporting any changes or complications to the physician.
- Administering fluids, medications, blood products, oxygen, or other treatments as prescribed and monitoring their effects and side effects.
- Collecting blood or body fluid samples for laboratory testing as ordered and following the proper procedures for specimen handling, labeling, packaging, transporting, and reporting.
- Providing comfort measures such as oral hygiene, skin care, positioning, massage, or distraction techniques to relieve discomfort and promote relaxation.
- Communicating effectively with the patients and their families using verbal and nonverbal cues, active listening, empathy, and respect.
- Collaborating with other health care professionals such as physicians, pharmacists, laboratory technicians, social workers, or epidemiologists to ensure coordinated and comprehensive care.
- Participating in surveillance, contact tracing, isolation, quarantine, and vaccination activities as part of the public health response to EVD outbreaks.
Prevention and control
- The prevention and control of EVD are essential to reduce the morbidity and mortality associated with the disease and to prevent its spread to new areas or countries. The prevention and control measures include:
- Avoiding contact with blood, body fluids, organs, or tissues of infected animals or people or with surfaces or materials contaminated with these fluids.
- Wearing appropriate PPE such as gloves, gowns, masks, eye protection, and boots when caring for or handling infected animals or people or their specimens or belongings.
- Washing hands frequently with soap and water or using alcohol-based hand sanitizer before and after contact with infected animals or people or their specimens or belongings.
- Disinfecting surfaces or materials that may be contaminated with Ebola virus using bleach or other approved disinfectants.
- Disposing of waste materials such as needles, syringes, gloves, gowns, or other PPE in designated containers or bags that are labeled as biohazardous and incinerated or autoclaved before disposal.
- Following safe burial practices for the dead such as wrapping the body in a plastic sheet, placing it in a sealed coffin, and burying it at least 1.5 meters deep in a designated area away from water sources. Avoiding direct contact with the body or its fluids during burial rituals such as washing, kissing, or touching the body.
- Reporting any suspected cases of EVD to the local health authorities as soon as possible for investigation, confirmation, and isolation.
- Cooperating with the health authorities in identifying and monitoring contacts of confirmed cases for 21 days after their last exposure to the case. Contacts should be advised to monitor their temperature twice daily and report any signs or symptoms of EVD immediately. Contacts should also be isolated if they develop symptoms until they are tested negative for Ebola virus.
- Seeking medical attention promptly if experiencing any signs or symptoms of EVD such as fever, headache, muscle pain, vomiting, diarrhea, or bleeding. Informing the health care provider about any history of exposure to a known or suspected source of Ebola virus infection.
- Supporting research efforts to develop effective vaccines and treatments for EVD. Volunteering to participate in clinical trials if eligible and informed consent is obtained.
Types and distribution
- There are five species of Ebola virus that cause EVD: Zaire, Sudan, Bundibugyo, Tai Forest, and Reston. The Zaire species is the most virulent and responsible for the majority of EVD cases and deaths. It was first identified in 1976 in Zaire (now Democratic Republic of Congo) and has since caused outbreaks in several African countries such as Gabon, Republic of Congo, Uganda, South Sudan, Guinea, Liberia, Sierra Leone, and most recently in 2018-2020 in Democratic Republic of Congo and 2021 in Guinea. The Zaire species has a case fatality rate of up to 90% and can infect humans, chimpanzees, gorillas, and duikers.
- The Sudan species was also first identified in 1976 in Sudan and has caused outbreaks in Sudan, Uganda, and Kenya. The Sudan species has a case fatality rate of up to 65% and can infect humans, chimpanzees, baboons, and monkeys.
- The Bundibugyo species was discovered in 2007 in Bundibugyo district of Uganda and has caused outbreaks in Uganda and Democratic Republic of Congo. The Bundibugyo species has a case fatality rate of up to 50% and can infect humans, chimpanzees, and monkeys.
- The Tai Forest species was isolated in 1994 from a chimpanzee that died of EVD in Tai Forest of Ivory Coast. It has only caused one human case so far, a scientist who performed a necropsy on the infected chimpanzee. The Tai Forest species has a case fatality rate of unknown but probably low and can infect humans and chimpanzees.
- The Reston species was discovered in 1989 from monkeys imported from the Philippines to a research facility in Reston, Virginia, USA. It has caused several outbreaks among monkeys in the Philippines, USA, Italy, and China. The Reston species has not caused any human deaths but has been shown to infect humans who have contact with infected monkeys or their specimens. The Reston species has a case fatality rate of unknown but probably zero and can infect humans, monkeys, pigs, and dogs.
Conclusion
- Ebola virus disease (EVD) is a serious and often fatal viral hemorrhagic fever that affects humans and other primates. It is caused by infection with one of five species of Ebola virus: Zaire, Sudan, Bundibugyo, Tai Forest, and Reston. The virus is transmitted from animals to humans or from humans to humans through direct contact with blood, body fluids, organs, or tissues of infected animals or people or with surfaces or materials contaminated with these fluids. The symptoms of EVD include fever, headache, muscle pain, vomiting, diarrhea, rash, red eyes, and bleeding from various sites. The diagnosis of EVD is based on clinical suspicion and laboratory confirmation using antigen, antibody, or RNA tests. The treatment of EVD is mainly supportive and symptomatic as there is no specific antiviral drug or vaccine available for EVD. The nursing interventions for EVD are aimed at providing quality care to the patients, preventing further transmission of the virus, and protecting the health and safety of the healthcare workers and the community. The prevention and control of EVD are essential to reduce the morbidity and mortality associated with the disease and to prevent its spread to new areas or countries. The prevention and control measures include avoiding contact with infected animals or people or their fluids or materials, wearing appropriate personal protective equipment, washing hands frequently, disinfecting surfaces or materials that may be contaminated, disposing of waste materials safely, following safe burial practices for the dead, reporting any suspected cases of EVD to the local health authorities, cooperating with the health authorities in identifying and monitoring contacts of confirmed cases, seeking medical attention promptly if experiencing any signs or symptoms of EVD, and supporting research efforts to develop effective vaccines and treatments for EVD.
Summary
- Ebola virus disease (EVD) is a severe viral hemorrhagic fever caused by one of five species of Ebola virus: Zaire, Sudan, Bundibugyo, Tai Forest, and Reston.
- The virus is transmitted from animals to humans or from humans to humans through direct contact with blood, body fluids, organs, or tissues of infected animals or people or with surfaces or materials contaminated with these fluids.
- The symptoms of EVD include fever, headache, muscle pain, vomiting, diarrhea, rash, red eyes, and bleeding from various sites.
- The diagnosis of EVD is based on clinical suspicion and laboratory confirmation using antigen, antibody, or RNA tests.
- The treatment of EVD is mainly supportive and symptomatic as there is no specific antiviral drug or vaccine available for EVD.
- The nursing interventions for EVD are aimed at providing quality care to the patients, preventing further transmission of the virus, and protecting the health and safety of the healthcare workers and the community.
- The prevention and control of EVD are essential to reduce the morbidity and mortality associated with the disease and to prevent its spread to new areas or countries. The prevention and control measures include avoiding contact with infected animals or people or their fluids or materials, wearing appropriate personal protective equipment, washing hands frequently, disinfecting surfaces or materials that may be contaminated, disposing of waste materials safely, following safe burial practices for the dead, reporting any suspected cases of EVD to the local health authorities, cooperating with the health authorities in identifying and monitoring contacts of confirmed cases, seeking medical attention promptly if experiencing any signs or symptoms of EVD, and supporting research efforts to develop effective vaccines and treatments for EVD.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Communicable Diseases
This filled cannot be empty

