Please set your exam date
Prolonged and Obstructed Labor and Ruptured Uterus
Study Questions
Introduction
A nurse is caring for a client who has been in labor for 14 hours and has not progressed beyond 4 cm dilation.
The nurse suspects that the client has prolonged labor due to a large baby.
Which of the following actions should the nurse take first?
Explanation
This is the first action the nurse should take to determine the well-being of the baby and the possible cause of the prolonged labor.Prolonged labor may happen if the baby is very big and cannot move through the birth canal, or if the baby is in an abnormal position.
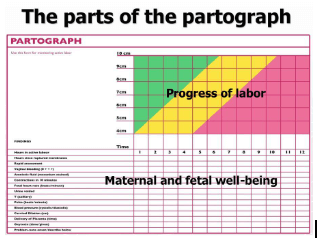
A nurse is reviewing the partograph of a client who is in labor.
The nurse notes that the cervical dilation curve is above the alert line and the fetal heart rate is 160/min.
The nurse should recognize that these findings indicate which of the following complications?
Explanation
This is because the cervical dilation curve is above the alert line, which means that the dilation is slower than 1 cm per hour and indicates a possible obstruction in the birth canal.Obstructed labor can lead to serious complications such as fetal distress, infection, uterine rupture, and maternal death.
The question does not provide any evidence of infection in this case.
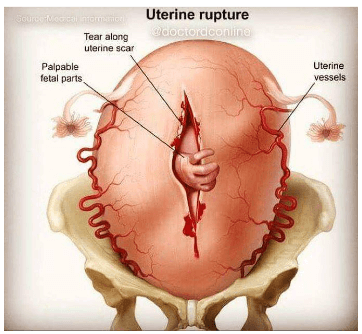
A nurse is caring for a client who had a previous cesarean delivery and is now in labor with her second child.
The client reports a sudden sharp pain in her lower abdomen and vaginal bleeding.
The nurse should suspect which of the following conditions?
Explanation
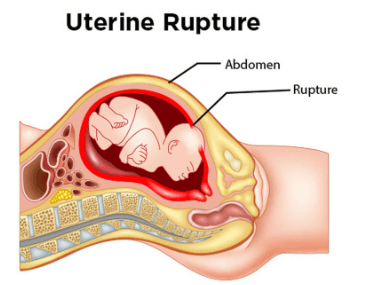
This is a rare but life-threatening complication that can occur in women who have had a previous cesarean delivery and are now in labor with their second child.Uterine rupture happens when the scar from the previous surgery tears open during contractions, causing severe pain, bleeding, and fetal distress.
A nurse is teaching a group of pregnant women about the prevention and management of prolonged and obstructed labor.
Which of the following statements by one of the participants indicates an understanding of the teaching?
Explanation
This statement indicates an understanding of the teaching because cesarean delivery is a risk factor for prolonged and obstructed labor.Avoiding unnecessary cesarean delivery can help prevent foeto-pelvic disproportion and reduce the risk of uterine rupture.
Causes and risk factors
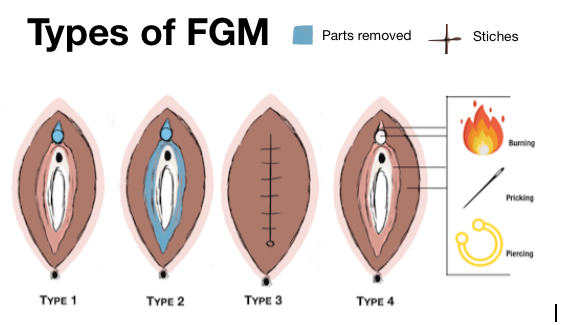
A nurse is caring for a client who is in labor and has a history of female genital mutilation (FGM).
The nurse should be aware that FGM can increase the risk of which of the following complications?
Explanation
All of the above.FGM can increase the risk of hemorrhage, infection, and obstructed labor due to the damage and scarring of the female genital organs.
Normal ranges for some relevant indicators are:
• Blood loss during vaginal delivery: less than 500 ml
• Blood loss during cesarean section: less than 1000 ml
• Duration of first stage of labor: 12 to 19 hours for nulliparous women; 10 to 14 hours for multiparous women
• Duration of second stage of labor: up to 3 hours for nulliparous women; up to 2 hours for multiparous women
A nurse is reviewing the partograph of a client who is in labor.
The nurse notes that the fetal head descent is below the alert line but above the action line.
What does this indicate?
Explanation
This is because the fetal head descent is below the alert line but above the action line on the partograph.The alert line indicates the average rate of cervical dilation of 1 cm per hour, and the action line is 4 hours to the right of the alert line.If the labor curve crosses to the right of the alert line, it means that the labor is slow and needs closer monitoring or referral.If the labor curve crosses to the right of the action line, it means that the labor is obstructed or prolonged and needs intervention such as oxytocin augmentation or cesarean delivery.
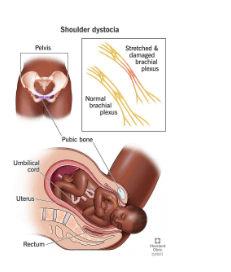
A nurse is assessing a client who is in labor and has a large baby with a cephalopelvic disproportion (CPD).
The nurse should monitor the client for signs of which of the following fetal complications?
Explanation
This is a complication that can occur when the baby’s head is delivered but one or both shoulders becomes “stuck” behind the pelvic bone.This can happen when the baby is too large or out of position when entering the pelvis, which are possible causes of cephalopelvic disproportion (CPD).
Normal ranges for fetal head circumference are 32 to 38 cm at term.
Normal ranges for maternal pelvic inlet diameter are 11 to 13 cm for anteroposterior diameter and 13 to 14 cm for transverse diameter.
A nurse is teaching a group of pregnant women about the risk factors for prolonged and obstructed labor.
Which of the following statements by one of the women indicates a need for further teaching?
Explanation
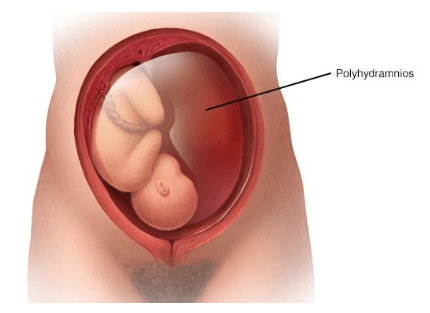
This statement indicates a need for further teaching because drinking fluids does not prevent polyhydramnios, which is a condition of having too much amniotic fluid around the baby.In fact, drinking too much fluid may worsen the condition by increasing the blood volume and urine output of the mother.
A nurse is preparing to perform a vacuum extraction for a client who has an obstructed labor due to a face presentation.
Which of the following actions should the nurse take? (Select all that apply.).
Explanation
The nurse should obtain informed consent from the client before performing a vacuum extraction, as it is an operative vaginal delivery that carries some risks for the mother and the baby.The nurse should also monitor the fetal heart rate continuously during the procedure, as vacuum extraction can cause fetal distress or scalp injuries.
A nurse is caring for a client who is in active labor and has a history of two previous cesarean deliveries.
The nurse notes that the client’s fetal heart rate is dropping and the client reports severe abdominal pain.
The nurse suspects that the client has a ruptured uterus.
What is the priority action for the nurse to take?
Explanation
Notify the provider and prepare for an emergency cesarean delivery.This is because a ruptured uterus is a life-threatening complication that requires immediate surgical intervention to save the mother and the fetus.
The nurse should also monitor the vital signs and fetal heart rate of the client and administer oxygen and IV fluids as needed.
A nurse is teaching a prenatal class about the complications of labor and delivery.
The nurse explains that a ruptured uterus is a rare but life-threatening condition that can occur during labor.
Which of the following statements by a class participant indicates a need for further teaching?
Explanation
A ruptured uterus can be prevented by avoiding induction or augmentation of labor.This is because induction or augmentation of labor can increase the pressure and stress on the uterine wall, especially if there is a previous C-section scar, and cause it to tear open.
The normal range for uterine rupture is less than 1 percent of pregnant women.It affects about 1 in 300 deliveries for women who have had one C-section delivery, and up to 9 in 300 deliveries for women who have had more than one C-section delivery.
A nurse is assessing a client who is in labor and has a history of uterine surgery.
The nurse observes that the client’s contractions are becoming more frequent and intense, but her cervix is not dilating.
The nurse suspects that the client has uterine tachysystole, which can lead to uterine rupture.
What is an appropriate nursing intervention for this client?
Explanation
Uterine tachysystole is a condition where the uterus contracts too frequently and intensely, which can reduce blood flow and oxygen to the fetus and increase the risk of uterine rupture, especially in women who have had previous uterine surgery.Oxytocin is a hormone that stimulates uterine contractions and can cause or worsen uterine tachysystole.Therefore, if oxytocin is being used to augment labor, it should be discontinued immediately to prevent further complications.
A nurse is evaluating the outcomes of care for a client who had a ruptured uterus during labor and underwent an emergency hysterectomy.
Which of the following outcomes indicates that the nursing care was effective?
Explanation
This outcome indicates that the nursing care was effective in preventing complications such as hemorrhage and sepsis after a ruptured uterus and an emergency hysterectomy.
Signs and symptoms
A nurse is caring for a client who is in the active phase of labor and has a slow cervical dilation.
The nurse should monitor the client for which of the following complications?
Explanation
This is a rare but serious complication that occurs when the uterus tears during labor.
It can cause severe bleeding, fetal distress, and maternal shock.
It can also lead to hysterectomy or death.Uterine rupture is more likely to occur in women who have had previous cesarean sections or other uterine surgeries.
A nurse is assessing a client who has been in labor for 14 hours and has a fever of 38.2°C (100.8°F).
The nurse notes that the amniotic fluid is foul-smelling.
Which of the following actions should the nurse take first?
Explanation
The nurse should report the findings of a fever and foul-smelling amniotic fluid to the provider as soon as possible, as they may indicate an infection of the amniotic sac and fluid (chorioamnionitis).Chorioamnionitis can cause serious complications for both the mother and the baby, such as sepsis, preterm birth, and neonatal pneumonia.
Therefore, notifying the provider is the priority action.
A nurse is reviewing the electronic fetal monitor (EFM) tracing of a client who is in labor and has a prolonged deceleration of the fetal heart rate to 90/min.
The nurse should recognize that this finding indicates which of the following?
Explanation
A prolonged deceleration of the fetal heart rate to 90/min indicates acute fetal hypoxia/acidosis, which is a decrease in the blood flow to the placenta that reduces the amount of oxygen and nutrients transferred to the fetus.Fetal pH drops at a rate of 0.01/min during the deceleration.Causes of acute hypoxia include low maternal blood pressure, dehydration, anemia, rapid uterine contractions, placental abruption, and fetal hypoxia.
A nurse is preparing to assist with an emergency cesarean delivery for a client who has obstructed labor and excessive vaginal bleeding.
The nurse should anticipate administering which of the following medications to prevent hemorrhage?
Explanation
This medication is a uterotonic agent that stimulates the contraction of the uterus and helps prevent hemorrhage after cesarean delivery.It is especially indicated for clients who have obstructed labor and excessive vaginal bleeding, as they are at high risk of postpartum hemorrhage.
Normal ranges for uterine tone are less than 10 mm Hg at rest and less than 25 mm Hg during contractions.
Normal ranges for blood pressure are 110-140 mm Hg systolic and 60-90 mm Hg diastolic.
Normal ranges for heart rate are 60-100 beats per minute.
A nurse is evaluating the outcomes of care for a client who had prolonged labor and delivered a newborn with Apgar scores of 6 and 8 at 1 and 5 minutes, respectively.
Which of the following findings indicates a positive outcome?
Explanation
This indicates a positive outcome because meconium aspiration can cause respiratory distress and infection in newborns.Apgar scores are used to assess the health of newborns at 1 and 5 minutes after birth based on five criteria: activity, pulse, grimace, appearance, and respiration.A score of 7 to 10 is considered normal.
A nurse is caring for a client who has a history of previous cesarean delivery with a low transverse incision.
The client is in labor and wants to have a vaginal birth after cesarean (VBAC).
The nurse should monitor the client closely for signs of which complication?
Explanation
The client with any prior history of uterine surgery is at increased risk for a uterine rupture.A falling blood pressure and increasing pulse is a sign of hemorrhage, and in this client a uterine rupture needs to be a first consideration.
A nurse is reviewing the electronic fetal monitor (EFM) tracing of a client who has a ruptured uterus.
Which of the following findings would the nurse expect to see on the EFM?
Explanation
A sinusoidal pattern is a type of fetal heart rate (FHR) tracing that shows a smooth, undulating wave-like pattern with a fixed period of 3 to 5 cycles per minute and an amplitude range of 5 to 15 beats per minute.A sinusoidal pattern is associated with severe fetal anemia, hypoxia, or acidosis and indicates a poor prognosis for the fetus.
A nurse is assisting with an artificial rupture of membranes (AROM) for a client who is in active labor.
The nurse should report which of the following findings to the provider immediately?
Explanation
This is a sign of umbilical cord prolapse, which is a medical emergency that requires immediate delivery of the baby.The umbilical cord can become compressed and cut off oxygen and blood supply to the baby.
A nurse is preparing to administer oxytocin to a client who has a previous cesarean delivery with a vertical uterine incision.
The nurse should be aware that this client has an increased risk for which of the following adverse effects?
Explanation
Oxytocin is a hormone that stimulates uterine contractions and can be used to induce or augment labor.However, it also increases the risk of uterine rupture, especially in women who have a scarred uterus from a previous cesarean delivery with a vertical uterine incision.A vertical uterine incision is made in the contractile part of the uterus and is more likely to tear under stress than a low transverse incision, which is made in the lower segment of the uterus.
Normal ranges for oxytocin infusion during labor are 0.5 to 20 milliunits per minute, depending on the indication and maternal and fetal status.The infusion rate should be adjusted according to the frequency and strength of uterine contractions and the progress of cervical dilation.
A nurse is assessing a client who has a ruptured uterus.
Which of the following findings should the nurse expect? (Select all that apply.).
Explanation
A ruptured uterus is a serious complication that can cause severe bleeding, fetal distress and shock in the mother.
The symptoms of a ruptured uterus may include:
• Sudden onset of severe abdominal paindue to the tear in the uterine wall.
• Loss of uterine contractions or tonedue to the disruption of the uterine muscle.
• Vaginal bleeding (may be minimal)due to the blood loss from the uterine vessels.
• Shock (hypotension, tachycardia, pallor)due to the hemorrhage and reduced blood flow to vital organs.
Normal ranges for blood pressure are 90/60 mmHg to 120/80 mmHg, for heart rate are 60 to 100 beats per minute, and for fetal heart rate are 110 to 160 beats per minute.
Diagnosis and treatment
A nurse is using a partograph to monitor a client in labor.
What is the main purpose of using a partograph?
Explanation
To record the maternal and fetal data during labor on a single sheet of paper.This is the main purpose of using a partograph, which is a tool for monitoring maternal and fetal wellbeing during the active phase of labor, and a decision-making aid when abnormalities are detected.
A nurse is assessing a client who has prolonged and obstructed labor.
Which of the following findings is a sign of obstructed labor?
Explanation
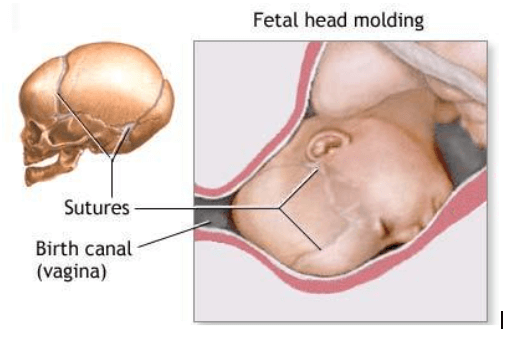
is a sign of obstructed labour, which occurs when the baby cannot pass through the birth canal due to a mismatch between the size or position of the baby and the pelvis.
Moulding is the process of overlapping of the skull bones to reduce the diameter of the head and facilitate its passage.However, excessive moulding can indicate that the head is too large or the pelvis is too small for a normal delivery.
A nurse is preparing to perform a vacuum extraction for a client who has prolonged and obstructed labor.
Which of the following criteria must be met before performing this procedure? (Select all that apply).
Explanation
1. The cervix must be fully dilated and effaced.
2. The fetal head must be engaged and well-flexed.
3. The maternal pelvis must be adequate for vaginal delivery.
These are the criteria that must be met before performing a vacuum extraction for a client who has prolonged and obstructed labor.
A nurse is caring for a client who has prolonged and obstructed labor.
The client develops signs of infection, such as fever, tachycardia, and foul-smelling lochia.
Which of the following interventions should the nurse implement?
Explanation
This is because the client has signs of infection, such as fever, tachycardia, and foul-smelling lochia, which can indicate endometritis or sepsis.Antibiotics can help treat the infection and prevent complications.
A nurse is educating a group of pregnant women about the risk factors for prolonged and obstructed labor.
Which of the following factors should the nurse include? (Select all that apply).
Explanation
Fetal presentation other than vertex, such as breech or transverse, and fetal size larger than average, such as macrosomia or hydrocephalus, are risk factors for prolonged and obstructed labor.
These factors can prevent the fetal head from descending into the pelvis or passing through the birth canal.
A nurse is caring for a client who has a history of risk factors for ruptured uterus.
What are some of the risk factors that the nurse should assess? (Select all that apply.).
Explanation
Previous cesarean section.
Uterine fibroids.
Multiparity.
Induced labor.
These are some of the risk factors that can weaken the uterine wall and increase the risk of rupture during labor or delivery.
A nurse is performing a physical examination of a mother and the fetus who are suspected to have a ruptured uterus.
What are some of the signs and symptoms that the nurse should look for? (Select all that apply.).
Explanation
A ruptured uterus is a serious complication where the uterus tears or breaks open, usually along the scar line of a previous cesarean delivery.
It can cause severe bleeding and fetal distress.Some of the signs and symptoms of a ruptured uterus are:
• Abdominal pain, tenderness, and rigidity: This is caused by the internal bleeding and the loss of uterine muscle tone.
• Vaginal bleeding and signs of shock: This is due to the hemorrhage from the rupture site and the hypovolemia (low blood volume) in the mother.
• Absent or decreased fetal movements: This is because the fetus may slip into the mother’s abdomen or lose oxygen due to the rupture.
A nurse is reviewing the laboratory tests of a client who has a ruptured uterus.
What are some of the tests that the nurse should expect to be ordered for this client?
Explanation
A client who has a ruptured uterus is at risk of severe hemorrhage and shock, so the following tests are necessary to assess the blood loss and prepare for possible transfusion:
• A complete blood count (CBC) can show the level of hemoglobin, hematocrit, red blood cells, white blood cells, and platelets.
A low hemoglobin and hematocrit indicates anemia due to blood loss.
A high white blood cell count indicates infection or inflammation.
A low platelet count indicates impaired clotting ability.
• A blood type and cross-match can determine the client’s blood group and Rh factor, and identify compatible blood units for transfusion if needed.
• A coagulation profile can measure the time it takes for the blood to clot and the activity of clotting factors.
A prolonged prothrombin time (PT), activated partial thromboplastin time (aPTT), or international normalized ratio (INR) indicates a bleeding disorder or anticoagulant use.
A low fibrinogen level indicates excessive bleeding or consumption of clotting factors.
A nurse is preparing a client who has a ruptured uterus for an emergency cesarean section.
What are some of the indications for this procedure?
Explanation
All of the above are indications for an emergency cesarean section in case of a ruptured uterus.A ruptured uterus is a serious complication where the uterus tears or breaks open, usually along the scar line of a previous C-section delivery.It can cause severe maternal hemorrhage or shock, fetal distress or demise, and complete uterine rupture or large uterine tear.
Therefore, an emergency cesarean section is needed to deliver the baby and repair the uterus as soon as possible.
A nurse is assisting a client who has an incomplete uterine rupture or small uterine tear with a vacuum extraction delivery.
What are some of the criteria for this procedure?
Explanation
All of the above are criteria for vacuum extraction delivery.Vacuum extraction is a method of assisted vaginal delivery that can help get the baby out when labor is stalled in the second stage.It involves applying a suction cup to the baby’s head and pulling while the mother pushes.
Nursing interventions and care
A nurse is caring for a client who had a prolonged and obstructed labor and is at risk for developing a ruptured uterus.
Which of the following signs should alert the nurse to this complication?
Explanation
A ruptured uterus can cause the baby to slip into the mother’s abdomen, which can stop or slow down labor.A ruptured uterus can also cause severe bleeding, shock, and fetal distress.
A nurse is preparing a client for an emergency cesarean section due to prolonged and obstructed labor.
Which of the following actions should the nurse take first?
Explanation
Informed consent is a legal and ethical requirement for any surgical procedure, including emergency cesarean section.It implies that the patient accepts the intervention willingly after comprehending adequate information about the associated risks and benefits.Informed consent also respects the patient’s autonomy and right to self-determination.
Therefore, obtaining informed consent from the client or her partner should be the first action that the nurse takes before an emergency cesarean section.
A nurse is monitoring a client who had a prolonged and obstructed labor and delivered a healthy newborn by vacuum extraction.
Which of the following interventions should the nurse implement to prevent infection in the client?
Explanation
This intervention can help prevent infection in the client by improving blood circulation, reducing edema, and promoting wound healing.Early ambulation and hydration can also prevent other complications such as thromboembolism, constipation, and urinary retention.
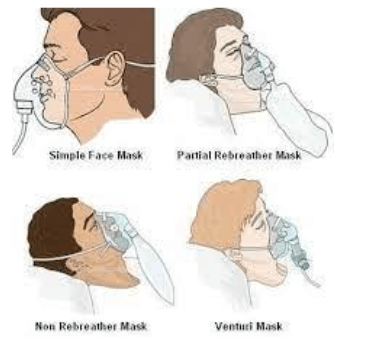
A nurse is providing oxygen therapy to a client who had a prolonged and obstructed labor and is experiencing respiratory distress.
Which of the following oxygen delivery devices should the nurse use to provide the highest concentration of oxygen?
Explanation
This is because a non-rebreather mask can deliver high concentrations of oxygen (approximately 70% O2) to a client who is experiencing respiratory distress.A non-rebreather mask has a reservoir bag that fills with oxygen and a valve that prevents the exhaled air from mixing with the oxygen in the bag.
A nurse is educating a client who had a prolonged and obstructed labor and a cesarean section about maternal-fetal bonding after delivery.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
This statement indicates that the client understands the importance of maternal-fetal bonding after delivery, which is the emotional, cognitive, and behavioral connection that mothers develop toward their babies.Skin-to-skin contact is one of the ways to promote bonding and attachment between the mother and the baby.
Summary
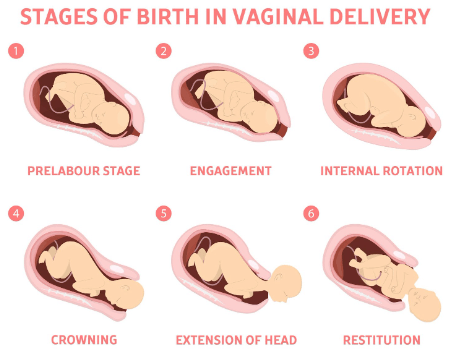
A nurse is assessing a client who is in labor and notes that the fetal head is visible at the vaginal opening but does not advance with pushing.
The nurse should identify this finding as which of the following?
Explanation
Crowning is when the fetal head is visible at the vaginal opening and does not slip back in with each contraction.This indicates that the baby is ready to be born and the mother should stop pushing to avoid tearing or the need for an episiotomy.
A nurse is caring for a client who has prolonged labor and is at risk for infection.
Which of the following actions should the nurse take to reduce this risk? (Select all that apply.)
Explanation
These actions can help reduce the risk of infection for the client who has prolonged labor.
• ChoiceBis correct because changing perineal pads every 2 hours can prevent bacterial growth and contamination of the genital tract.
• ChoiceCis correct because encouraging oral fluid intake can help maintain hydration and blood volume, which can improve uterine perfusion and prevent maternal and fetal acidosis.
• ChoiceDis correct because administering IV antibiotics as prescribed can prevent or treat maternal peripartum infections, which are among the leading causes of maternal mortality worldwide.
• ChoiceEis correct because using sterile gloves when providing perineal care can prevent introducing pathogens into the genital tract.
A nurse is preparing to assist with an emergency cesarean delivery for a client who has a ruptured uterus.
Which of the following equipment should the nurse have readily available? (Select all that apply.)
Explanation
Oxygen mask and tubing and blood products and IV fluids should be readily available for a client who has a ruptured uterus.This is because a ruptured uterus can cause severe hemorrhage, hypovolemia, and fetal distress.The client and the fetus may need oxygen therapy and blood transfusion to prevent hypoxia and shock.
A nurse is evaluating a client who has prolonged labor and suspects uterine rupture.
Which of the following findings should alert the nurse to this complication?
Explanation
Uterine rupture can cause fetal distress and hypoxia, which can slow down the fetal heart rate.
Fetal bradycardia is a sign of a serious complication that requires immediate intervention.
A nurse is caring for a client who has prolonged and obstructed labor and develops a vesicovaginal fistula.
Which of the following interventions should the nurse include in the plan of care?
Explanation
a vesicovaginal fistula is an abnormal opening that forms between the bladder and the wall of the vagina, causing urine to leak out of the vagina.Zinc oxide cream can help protect the skin from irritation and infection.
Normal ranges for fluid intake are about 2 to 3 liters per day for healthy adults, depending on age, activity level, and climate.Normal ranges for pelvic floor muscle strength are 10 to 12 contractions of 6 to 8 seconds each, with a rest period of 4 to 6 seconds between each contraction.
A nurse is counseling a client who has a small pelvis and wants to have a vaginal delivery.
Which of the following factors should the nurse consider when discussing the possibility of vaginal birth after cesarean (VBAC)?
Explanation
All of the above factors should be considered when discussing the possibility of vaginal birth after cesarean (VBAC).
Here’s why:
• The type of uterine incision used in the previous cesarean delivery affects the risk of uterine rupture during VBAC.A low transverse incision is associated with the lowest risk, while a high vertical incision is associated with the highest risk.
• The gestational age of the current pregnancy affects the success rate of VBAC.The optimal time for VBAC is between 39 and 40 weeks of gestation.Attempting VBAC before 37 weeks or after 41 weeks may increase the risk of complications.
• The presentation and position of the fetus affects the feasibility and safety of VBAC.A breech presentation, a transverse lie, or a posterior position may make vaginal delivery difficult or impossible.A cephalic presentation and an anterior position are more favorable for VBAC.
A nurse is providing discharge teaching to a client who had a ruptured uterus and a hysterectomy during labor.
Which of the following instructions should the nurse include in the teaching? (Select all that apply.)
Explanation
The nurse should include these instructions in the teaching because:
• Choice B: Using sanitary pads rather than tampons for vaginal bleeding can prevent infection and irritation of the surgical site.
• Choice D: Drinking plenty of fluids and eating foods high in fiber can help prevent constipation, which can strain the abdominal muscles and cause pain.
• Choice E: Reporting any foul-smelling vaginal discharge or fever to the provider can help detect signs of infection, which can be a complication of hysterectomy.
A nurse is reviewing the risk factors for uterine rupture with a group of nursing students.
Which of the following risk factors should the nurse include? (Select all that apply.)
Explanation
Intrauterine infection is a risk factor for uterine rupture because it can weaken the uterine wall and make it more prone to tearing.
The most common risk factor for uterine rupture is having a previous cesarean delivery or other uterine surgery that leaves a scar on the uterus.Other risk factors include uterine trauma, congenital uterine anomalies, having multiples or too much amniotic fluid, having a breech baby that requires manual turning, and prolonged labor.
A nurse is monitoring a client who had a vaginal birth after cesarean (VBAC) delivery.
The nurse notes that the client has a boggy uterus, heavy vaginal bleeding, and signs of hypovolemic shock.
The nurse suspects that the client has a concealed uterine rupture.
What is an appropriate nursing action for this client?
Explanation
This is because the client has signs of concealed uterine rupture, which is a rare but serious complication of VBAC delivery.Concealed uterine rupture occurs when the uterus tears through the endometrium and myometrium, but the peritoneum remains intact.This can cause heavy vaginal bleeding, hypovolemic shock, and fetal distress.The priority nursing action is to restore the client’s blood volume and prepare for emergency surgery to deliver the fetus and repair the uterus.
A nurse is caring for a client who is in active labor and experiencing shoulder dystocia.
Which of the following actions should the nurse take? (Select all that apply.).
Explanation
Applying suprapubic pressure and assisting the provider with McRoberts maneuver are two nursing interventions that can help dislodge the impacted shoulder and facilitate the delivery of the baby.
Normal ranges for fetal heart rate are 110 to 160 beats per minute, and for maternal blood pressure are 110/70 to 140/90 mm Hg.
A nurse is assessing a client who is in labor and has been pushing for 3 hours with no progress.
The nurse should identify that this client is at risk for which of the following complications? (Select all that apply.).
Explanation
A client who is in labor and has been pushing for 3 hours with no progress is at risk for postpartum hemorrhage and maternal exhaustion.This is because a prolonged second stage of labor can cause uterine atony, which is a failure of the uterus to contract and stop bleeding after delivery.It can also cause fatigue, dehydration, and electrolyte imbalance in the mother.
A nurse is reviewing the medical record of a client who is in labor and has cephalopelvic disproportion (CPD).
Which of the following findings should the nurse expect to see in the record?
Explanation
A macrosomic fetus is a fetus that is larger than average, usually weighing more than 4 kg or 8.8 lb at birth.A large fetus can cause cephalopelvic disproportion (CPD), which is a condition where the baby’s head does not fit through the mother’s pelvis during labor.CPD can lead to prolonged or obstructed labor, which can endanger both the mother and the baby.
A gush of blood is noted with the rupture of membranes.
On palpation, the uterus is soft (i.e., relaxed) and the patient is not reporting any pain.
An FHR deceleration down to 90 bpm is noted.
What does the nurse suspect has happened?
Explanation
This is a condition where fetal blood vessels that run through the membranes rupture and bleed.
The bleeding is from the fetus, not the mother, and can cause fetal hypoxia and death.
The FHR deceleration indicates fetal distress.
The uterus is soft because there is no uterine bleeding or contraction.
Normal ranges for FHR are 110 to 160 beats per minute.
Normal ranges for uterine contraction frequency are 2 to 5 contractions in 10 minutes.
Normal ranges for uterine contraction duration are 45 to 80 seconds.
Normal ranges for uterine contraction intensity are mild to moderate to palpation
Women with previous uterine scars are prone to uterine rupture, especially if oxytocin or forceps are used.
If a woman complains of a sharp pain accompanied by the abrupt cessation of contractions, suspect uterine rupture, a medical emergency.
Immediate surgical delivery is indicated to save the fetus and mother.
Based on this information, which of the following nursing actions is most appropriate?
Explanation
This is because uterine rupture is a life-threatening complication that requires immediate surgical intervention to save the mother and the fetus.
Delaying the delivery can result in hemorrhage, shock, infection, and fetal death.
A nurse is reviewing the partograph of a client in labor.
The nurse notes that the cervical dilation curve is above the alert line and below the action line.
What does this indicate?
Explanation
This is because the cervical dilation curve is above the alert line and below the action line, which means that the dilation is less than 1 cm per hour.This indicates a possible delay in labor progress and a risk of complications such as fetal distress, infection, or postpartum hemorrhage.
A nurse is assisting a client who has prolonged and obstructed labor to deliver by vacuum extraction.
Which of the following complications should the nurse monitor for in the newborn?
Explanation
Caput succedaneum is a swelling of the scalp that can occur after vacuum extraction delivery.It is caused by the pressure of the suction cup on the baby’s head and usually resolves within a few days.
A nurse is evaluating a client who has prolonged and obstructed labor for signs of postpartum hemorrhage.
Which of the following findings is an early indicator of postpartum hemorrhage?
Explanation
A boggy uterus that does not respond to massage is an early indicator of postpartum hemorrhage.
A boggy uterus means that the uterus is not contracting properly after delivery, which can lead to excessive bleeding from the site where the placenta was attached.This condition is called uterine atony and it is the most common cause of postpartum hemorrhage.
Massage can help stimulate the uterus to contract and stop the bleeding, but if it does not work, other interventions are needed.
A nurse is assessing a client who had a prolonged labor and is at risk for uterine atony.
Which of the following findings should indicate to the nurse that the client has this condition? Select all that apply.
Explanation
A boggy uterus is a sign of uterine atony, which is the failure of the uterus to contract sufficiently after childbirth.
This can lead to excessive bleeding and postpartum hemorrhage.
A firm fundus at the umbilicus is a normal finding after delivery and indicates that the uterus is contracting well.
Excessive lochia rubra is also a sign of uterine atony and postpartum hemorrhage.Lochia rubra is the vaginal discharge composed of blood, mucus, and tissue from the placenta and the uterus lining that occurs after childbirth.
It is normal for the first 3 to 4 days, but it should gradually decrease in amount and change in color.
Clots larger than a quarter are abnormal and indicate excessive bleeding.
A pulse rate of 110/min is a sign of tachycardia, which can be caused by blood loss, infection, or pain.
A normal pulse rate for an adult is between 60 and 100 beats per minute.
A nurse is caring for a client who had a vacuum-assisted delivery due to prolonged labor and is at risk for developing a hematoma in the perineal area.
Which of the following manifestations should alert the nurse to this complication?
Explanation
Severe perineal pain is a manifestation of a hematoma in the perineal area, which can result from vacuum-assisted delivery.A hematoma is a collection of blood under the skin or in the tissues that can cause pressure and pain.
Normal ranges for hemoglobin are 12 to 16 g/dL for women and 14 to 18 g/dL for men.Normal ranges for white blood cell count are 4,000 to 11,000 cells per microliter of blood.
A nurse is providing emotional support to a client who had a prolonged labor and delivered a stillborn baby by cesarean section.
Which of the following actions should the nurse take?
Explanation
Grief is a normal and natural response to the loss of a baby, and the nurse should provide emotional support and acknowledge the client’s pain.The nurse should also respect the client’s personal, cultural, or religious needs and preferences regarding the care of the baby.
Exams on Prolonged and Obstructed Labor and Ruptured Uterus
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Define prolonged and obstructed labor and ruptured uterus.
-
Identify the causes and risk factors of these complications.
-
Recognize the signs and symptoms of these complications.
-
Describe the diagnosis and treatment of these complications.
-
Explain the nursing interventions and care for these complications.
-
Discuss the prevention and education strategies for these complications.
-
Define prolonged and obstructed labor and ruptured uterus.
-
Identify the causes and risk factors of these complications.
-
Recognize the signs and symptoms of these complications.
-
Describe the diagnosis and treatment of these complications.
-
Explain the nursing interventions and care for these complications.
-
Discuss the prevention and education strategies for these complications.
Introduction
- Prolonged labor is when the active phase of labor lasts longer than 12 hours

-
Obstructed labor is when the baby cannot exit the pelvis because it is physically blocked by a large or abnormally positioned baby, a small pelvis, or problems with the birth canal
-
Ruptured uterus is when the uterine wall tears open, usually along the scar line of a previous cesarean delivery or other uterine surgery
-
These complications can have serious consequences for both the mother and the baby, such as hemorrhage, infection, fistula, stillbirth, asphyxia, brain damage, or death
-
These complications require prompt diagnosis and treatment, usually by cesarean section or vacuum extraction
-
Nursing interventions include monitoring vital signs, fetal heart rate, contractions, blood loss, fluid balance, pain relief, infection prevention, emotional support, and documentation
-
Prevention and education strategies include screening for risk factors, using a partograph to track labor progress, avoiding unnecessary cesarean deliveries or uterine surgeries, promoting maternal nutrition and health, and informing women about the signs and symptoms of these complications
Causes and risk factors
The main causes of prolonged and obstructed labor are:
|
Cause |
Description |
|
Large or abnormally positioned baby |
The baby’s head or shoulders may be too big to fit through the pelvis (cephalopelvic disproportion) or the baby may be in a breech (bottom-first), transverse (sideways), or face presentation. |
|
Small pelvis |
The pelvis may be too narrow or deformed due to malnutrition, vitamin D deficiency, rickets, pelvic fracture, or congenital anomalies. |
|
Problems with the birth canal |
The vagina or perineum may be too tight or scarred due to female genital mutilation (FGM), tumors, infections, or previous injuries. |
The risk factors for prolonged and obstructed labor include:
-
Previous cesarean delivery or uterine surgery
-
Multiparity (having given birth more than once)
-
Post-term pregnancy (more than 42 weeks)
-
Maternal age less than 18 years or more than 35 years
-
Maternal height less than 150 cm
-
Maternal weight less than 50 kg or more than 80 kg
-
Gestational diabetes
-
Polyhydramnios (excess amniotic fluid)
-
Fetal macrosomia (birth weight more than 4 kg)
-
Fetal anomalies (such as hydrocephalus)
The main cause of ruptured uterus is a previous cesarean delivery or uterine surgery that weakens the uterine wall and makes it prone to tearing under the pressure of labor contractions
The risk factors for ruptured uterus include:
-
Previous cesarean delivery or uterine surgery
-
Multiple previous cesarean deliveries or uterine surgeries
-
Classical (vertical) incision on the uterus
-
Short interval between pregnancies (less than 18 months)
-
Induction or augmentation of labor with oxytocin or prostaglandins
-
Excessive use of forceps or vacuum extraction
-
Trauma to the uterus (such as from an accident or violence)
Signs and symptoms
The signs and symptoms of prolonged and obstructed labor include:
-
Active phase of labor lasting longer than 12 hours
-
Slow cervical dilation (less than 1 cm per hour) or arrest of dilation
-
Failure of descent of the fetal head
-
Severe pain between contractions
-
Excessive vaginal bleeding
-
Foul-smelling amniotic fluid
-
Fever and tachycardia in the mother
-
Abnormal fetal heart rate (bradycardia or tachycardia)
The signs and symptoms of ruptured uterus include:
-
Sudden onset of severe abdominal pain or tenderness
-
Loss of uterine contractions or tone
-
Vaginal bleeding (may be minimal)
-
Shock (hypotension, tachycardia, pallor) in the mother
-
Fetal distress (bradycardia, decelerations) or demise
-
Recession of the fetal head into the abdomen
-
Bulging under the pubic bone due to protrusion of fetal parts
-
Palpation of fetal parts through the abdominal wall
Diagnosis and treatment
The diagnosis of prolonged and obstructed labor is based on:
-
History of risk factors
-
Physical examination of the mother and the fetus
-
Assessment of pelvic size and shape
-
Determination of fetal presentation, position, size, and descent
-
Measurement of cervical dilation and effacement
-
Evaluation of uterine contractions
-
Estimation of blood loss and signs of infection
-
Auscultation of fetal heart rate
-
-
Use of a partograph to track labor progress and identify deviations from normal
-
A partograph is a graphical record of key data (maternal and fetal) during labor entered against time on a single sheet of paper
-
It includes measurements such as cervical dilation, fetal heart rate, duration of labor, vital signs, blood loss, and uterine contractions
-
It helps to provide an accurate record of the progress in labor, so that any delay or obstruction can be detected quickly and treated accordingly
-
It also helps to prevent unnecessary interventions or prolonged labor that may increase the risk of complications
-
The diagnosis of ruptured uterus is based on:
-
History of risk factors
-
Physical examination of the mother and the fetus
-
Assessment of abdominal pain, tenderness, and rigidity
-
Palpation of fetal parts through the abdominal wall or under the pubic bone
-
Evaluation of vaginal bleeding and signs of shock
-
Auscultation of fetal heart rate
-
-
Laboratory tests
-
Complete blood count to check for anemia and infection
-
Blood type and cross-match for possible transfusion
-
Coagulation profile to check for disseminated intravascular coagulation (DIC)
-
-
Imaging tests
-
Ultrasound to confirm the diagnosis and locate the site and extent of the rupture
-
X-ray to rule out other causes of abdominal pain
-
The treatment of prolonged and obstructed labor and ruptured uterus is usually by cesarean section or vacuum extraction
-
Cesarean section is the surgical delivery of the baby through an incision in the abdomen and uterus. It is indicated when:
-
There is evidence of fetal distress or demise
-
There is severe maternal hemorrhage or shock
-
There is complete uterine rupture or large uterine tear
-
There is no progress in labor despite adequate contractions
-
There is cephalopelvic disproportion or malpresentation that cannot be corrected
-
-
Vacuum extraction is the use of a suction cup attached to the fetal head to assist in delivery. It is indicated when:
-
There is incomplete uterine rupture or small uterine tear
-
There is adequate cervical dilation and descent of the fetal head
-
There is no evidence of fetal distress or demise
-
There is no contraindication such as prematurity, bleeding disorder, or hydrocephalus
-
Nursing interventions and care
The nursing interventions and care for prolonged and obstructed labor and ruptured uterus include:
-
Monitoring vital signs, fetal heart rate, contractions, blood loss, fluid balance, pain relief, infection prevention, emotional support, and documentation
-
Preparing for emergency cesarean section or vacuum extraction as indicated
-
Administering intravenous fluids, antibiotics, oxytocin, analgesics, blood products, or other medications as prescribed
-
Providing oxygen therapy as needed
-
Assisting with urinary catheterization as needed
-
Supporting maternal-fetal bonding after delivery if possible
-
Educating the woman and her family about the complications and their management
Prevention and education
The prevention and education strategies for prolonged and obstructed labor and ruptured uterus include:
-
Screening for risk factors during antenatal care and referring high-risk women to appropriate facilities for delivery
-
Using a partograph to track labor progress and identify deviations from normal
-
Avoiding unnecessary cesarean deliveries or uterine surgeries that may increase the risk of uterine rupture
-
Promoting maternal nutrition and health to prevent malnutrition, vitamin D deficiency, rickets, anemia, or infection that may affect pelvic size or shape
-
Informing women about the signs and symptoms of these complications and the need for prompt medical attention
Conclusion
Prolonged and obstructed labor and ruptured uterus are serious complications that can affect both the mother and the baby. They require prompt diagnosis and treatment, usually by cesarean section or vacuum extraction. Nursing interventions include monitoring maternal and fetal well-being, preparing for emergency procedures, administering medications, providing oxygen therapy, supporting maternal-fetal bonding, educating the woman and her family. Prevention and education strategies include screening for risk factors, using a partograph to track labor progress, avoiding unnecessary interventions or surgeries, promoting maternal nutrition and health.
Summary
-
Prolonged labor is when the active phase of labor lasts longer than 12 hours.
-
Obstructed labor is when the baby cannot exit the pelvis because it is physically blocked by a large or abnormally positioned baby, a small pelvis, or problems with the birth canal.
-
Ruptured uterus is when the uterine wall tears open, usually along the scar line of a previous cesarean delivery or other uterine surgery.
-
These complications can have serious consequences for both the mother and the baby, such as hemorrhage, infection, fistula, stillbirth, asphyxia, brain damage, or death.
-
These complications require prompt diagnosis and treatment, usually by cesarean section or vacuum extraction.
-
Nursing interventions include monitoring vital signs, fetal heart rate, contractions, blood loss, fluid balance, pain relief, infection prevention, emotional support, and documentation.
-
Prevention and education strategies include screening for risk factors, using a partograph to track labor progress, avoiding unnecessary cesarean deliveries or uterine surgeries, promoting maternal nutrition and health, and informing women about the signs and symptoms of these complications.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Prolonged and Obstructed Labor and Ruptured Uterus
This filled cannot be empty

