Please set your exam date
Cultural Competence and Diversity in Healthcare
Study Questions
Introduction to Cultural Competence and Diversity in Healthcare
A nurse is caring for a client who identifies as transgender and is undergoing hormone therapy. What is the most appropriate way for the nurse to address the client?
Explanation
Rationale: The nurse should respect the client's identity and preferences and address them by their preferred name and pronouns, regardless of their legal name or biological sex. This demonstrates cultural competence and sensitivity and promotes a trusting relationship.
Incorrect options:
B) By their legal name and biological sex - This is an inappropriate way to address the client, as it disregards their identity and preferences and may cause distress or harm.
C) By a gender-neutral term such as "they" or "them" - This may be acceptable if the client has indicated that they prefer a gender-neutral term, but it should not be assumed without asking the client first.
D) By avoiding any direct reference to the client - This is an inappropriate way to address the client, as it implies that the nurse is uncomfortable or unwilling to acknowledge the client's identity and may create a barrier to communication and care.
A nurse is conducting a health assessment of a client who belongs to a Native American tribe. The nurse notices that the client avoids eye contact during the interview. How should the nurse interpret this behavior?
Explanation
Rationale: The nurse should be aware that different cultures have different norms and expectations regarding eye contact. In some cultures, such as Native American, avoiding eye contact is a sign of respect or deference, especially when interacting with someone of higher status or authority.
Incorrect options:
A) The client is being disrespectful or dishonest - This is a misinterpretation of the client's behavior based on the nurse's own cultural bias. In some cultures, such as Western, maintaining eye contact is expected and valued as a sign of respect or honesty.
B) The client is experiencing anxiety or fear - This may be true in some cases, but it should not be assumed without further assessment or evidence. The nurse should not project their own feelings or assumptions onto the client.
D) The client is not interested or engaged - This is another misinterpretation of the client's behavior based on the nurse's own cultural bias. In some cultures, such as Western, eye contact is seen as a sign of interest or engagement, but in other cultures, it may be considered rude or intrusive.
A nurse is planning to teach a diabetic diet to a client who follows a kosher diet. Which of the following foods should the nurse include in the teaching plan?
Explanation
Rationale: The nurse should include foods that are compatible with both the diabetic and kosher diets. A kosher diet prohibits the consumption of pork, shellfish, and meat and dairy products together. A diabetic diet emphasizes complex carbohydrates, lean protein, and fiber-rich foods.
Incorrect options:
A) Cheeseburger with whole wheat bun - This food violates both the diabetic and kosher diets. It contains simple carbohydrates, saturated fat, and meat and dairy products together.
C) Ham and cheese sandwich with fruit salad - This food violates both the diabetic and kosher diets. It contains pork, simple carbohydrates, saturated fat, and meat and dairy products together.
D) Spaghetti with meatballs and tomato sauce - This food violates both the diabetic and kosher diets. It contains simple carbohydrates, saturated fat, and meat and dairy products together.
A nurse is providing care to a client who practices Islam and is observing Ramadan. The nurse notes that the client has not eaten or drank anything since sunrise. What action should the nurse take?
Explanation
Rationale: The nurse should respect the client's religious practice of fasting during Ramadan, which involves abstaining from food, fluids, medications, smoking, and sexual activity from dawn to dusk. However, the nurse should also consult with the health care provider about adjusting the medication schedule, as some medications may need to be taken with food or fluids or at specific times of the day.
Incorrect options:
A) Respect the client's religious practice and do not offer food or fluids - This is partially correct, as the nurse should respect the client's religious practice, but it is not enough. The nurse should also consult with the health care provider about adjusting the medication schedule, as some medications may need to be taken with food or fluids or at specific times of the day.
B) Educate the client about the importance of nutrition and hydration for health - This is inappropriate, as it may be perceived as disrespectful or insensitive to the client's religious practice. The nurse should not try to persuade the client to break their fast, unless there is a medical emergency or a serious risk to their health.
D) Report the client's behavior to the social worker or chaplain - This is unnecessary, as the client's behavior is not a problem or a concern, but a normal part of their religious practice. The nurse should not involve other professionals without the client's consent or request.
A nurse is working with a client who has limited English proficiency and uses an interpreter. Which of the following strategies should the nurse use to facilitate effective communication?
Explanation
Rationale: The nurse should speak directly to the client and use simple words, as this shows respect and helps to establish rapport. The nurse should also maintain eye contact with the client, not the interpreter, and avoid using jargon, slang, or idioms that may be confusing or culturally inappropriate.
Incorrect options:
A) Speak directly to the interpreter and use short sentences - This is incorrect, as the nurse should speak directly to the client, not the interpreter. The nurse should also use complete sentences, not short sentences, as this may affect the accuracy or clarity of the interpretation.
C) Speak loudly and slowly to the client and use gestures - This is incorrect, as speaking loudly and slowly may be perceived as patronizing or insulting by the client. Gestures may also be misinterpreted or culturally inappropriate.
D) Speak in a normal tone and pace to the interpreter and use medical terms - This is incorrect, as speaking in a normal tone and pace may be too fast or too quiet for the interpreter to catch every word. Medical terms may also be unfamiliar or difficult to translate for the interpreter.
A nurse is caring for a client who has a terminal illness and requests palliative care. The client's family disagrees with this decision and wants aggressive treatment. How should the nurse handle this situation?
Explanation
Rationale: The nurse should support the client's decision and explain it to the family, as this respects the client's autonomy and dignity. The nurse should also provide emotional support and education to both the client and the family about palliative care, which focuses on relieving pain and suffering and improving quality of life.
Incorrect options:
B) Support the family's decision and persuade the client to change their mind - This is inappropriate, as it violates the client's autonomy and dignity. The nurse should not coerce or pressure the client to accept a treatment that they do not want.
C) Respect both the client's and the family's decisions and refer them to an ethics committee - This is unnecessary, as there is no ethical dilemma or conflict in this situation. The client has a right to refuse treatment and choose palliative care.
D) Respect neither the client's nor the family's decisions and follow the health care provider's orders - This is unethical, as it disregards both the client's and the family's wishes and preferences. The nurse should not follow orders that are contrary to what the client wants.
Cultural Awareness and Self-Reflection
A nurse is caring for a client who has recently immigrated from China and is experiencing culture shock. Which intervention should the nurse implement to help the client cope with the stress of acculturation?
Explanation
Rationale: The nurse should provide the client with information about local support groups and resources for immigrants, as this can help the client to connect with others who share similar experiences and challenges, and to access services that can facilitate their adjustment and integration into the new culture.
Incorrect options:
A) Encourage the client to adopt the dominant culture as soon as possible. - This is an incorrect intervention, as it may cause the client to feel pressured to abandon their own cultural identity and values, which can increase their stress and alienation.
C) Discourage the client from expressing negative emotions or frustrations about the new culture. - This is an incorrect intervention, as it may invalidate the client's feelings and prevent them from coping effectively with their culture shock. The nurse should acknowledge and empathize with the client's emotions and help them to find positive ways to deal with them.
D) Avoid asking the client about their cultural beliefs and practices to prevent stereotyping. - This is an incorrect intervention, as it may create a barrier to communication and rapport between the nurse and the client, and prevent the nurse from providing culturally competent care. The nurse should ask open-ended questions and show respect and curiosity for the client's cultural background and preferences.
A nurse is conducting a health assessment of a client who belongs to an indigenous community. The nurse notices that the client avoids eye contact and speaks in a low voice. How should the nurse interpret these behaviors?
Explanation
Rationale: The nurse should interpret these behaviors as expressions of deference and respect, as some indigenous cultures consider direct eye contact and loud speech to be rude or aggressive, especially when interacting with authority figures or strangers.
Incorrect options:
A) The client is being disrespectful and uncooperative. - This is an incorrect interpretation, as it reflects a bias or ethnocentrism on the part of the nurse, who may be imposing their own cultural norms and expectations on the client.
C) The client is feeling anxious and fearful. - This is an incorrect interpretation, as it may be based on a stereotype or assumption that indigenous people are timid or submissive. The nurse should not attribute emotions or feelings to the client without further assessment or evidence.
D) The client is hiding something or lying. - This is an incorrect interpretation, as it may indicate a lack of trust or rapport between the nurse and the client, which can hinder the quality of care. The nurse should not judge or accuse the client based on their nonverbal cues alone.
A nurse is planning to teach a group of clients about diabetes management. The clients are from diverse cultural backgrounds and have different levels of health literacy. Which strategy should the nurse use to ensure effective communication and education?
Explanation
Rationale: The nurse should use visual aids, demonstrations, and examples to supplement verbal information, as this can help to enhance comprehension, retention, and application of health education among clients who may have language barriers, low literacy skills, or different learning styles.
Incorrect options:
A) Use medical jargon and technical terms to demonstrate expertise and credibility. - This is an incorrect strategy, as it may confuse or intimidate clients who are not familiar with medical terminology or concepts, and create a power imbalance between the nurse and the clients.
C) Use a standardized curriculum and teaching materials for all clients regardless of their culture or literacy level. - This is an incorrect strategy, as it may not address the specific needs, preferences, or values of each client, and fail to account for cultural variations in health beliefs, practices, or behaviors.
D) Use humor, sarcasm, and idioms to make the teaching more engaging and memorable. - This is an incorrect strategy, as it may offend or mislead clients who do not share the same cultural or linguistic context as the nurse, and cause misunderstanding or miscommunication.
A nurse is working with a client who has a terminal illness and is considering hospice care. The client's family is opposed to this option and wants the client to continue aggressive treatment. The nurse learns that the client and the family are from a collectivistic culture that values family harmony and decision-making. What should the nurse do to facilitate ethical and culturally sensitive care?
Explanation
A nurse is working with a client who has a terminal illness and is considering hospice care. The client's family is opposed to this option and wants the client to continue aggressive treatment. The nurse learns that the client and the family are from a collectivistic culture that values family harmony and decision-making. What should the nurse do to facilitate ethical and culturally sensitive care?
A) Respect the family's wishes and persuade the client to follow their advice.
B) Respect the client's wishes and inform the family that they have no say in the matter.
C) Respect the client's autonomy and support their right to make their own choices.
D) Respect the family's involvement and encourage open dialogue and negotiation among all parties.
A nurse is conducting a cultural assessment of a client who identifies as Hispanic/Latino. Which question should the nurse ask to elicit information about the client's cultural identity?
Explanation
Rationale: The nurse should ask all of these questions to elicit information about the client's cultural identity, as they can help to capture the diversity and complexity of Hispanic/Latino culture, which encompasses various ethnicities, nationalities, languages, religions, and traditions.
Incorrect options:
A) What country or region of origin do you or your ancestors come from? - This is a partial question, as it may not reflect the full extent of the client's cultural identity, which may be influenced by other factors such as language, religion, or acculturation.
B) What language or languages do you speak at home or with your family? - This is a partial question, as it may not capture the nuances of the client's cultural identity, which may vary depending on their country or region of origin, generation, or education level.
C) What religion or spiritual beliefs do you practice or follow? - This is a partial question, as it may not account for the diversity of religious or spiritual expressions among Hispanic/Latino clients, who may belong to different denominations, sects, or movements within or outside of Christianity.
A nurse is providing care to a client who has a different cultural background than their own. The nurse notices that they have some negative feelings and thoughts about the client's culture. What should the nurse do to address their own cultural bias?
Explanation
Rationale: The nurse should explore their feelings and thoughts critically and reflectively to identify their sources and effects, as this can help them to recognize and acknowledge their own cultural bias, understand how it may influence their perception and behavior toward the client, and take steps to minimize its impact on their care delivery.
Incorrect options:
A) Ignore their feelings and thoughts and focus on providing objective and standardized care. - This is an incorrect action, as it may prevent the nurse from addressing their own cultural bias, which may affect their ability to provide objective and individualized care that meets the client's needs and preferences.
B) Express their feelings and thoughts openly and honestly to the client and ask for feedback. - While open and honest communication is important in nursing, expressing negative feelings and thoughts about a client's culture directly to the client can be potentially harmful and disrespectful. It is essential for nurses to maintain professionalism and provide culturally sensitive care.
D) Change their feelings and thoughts by adopting a positive attitude and mindset toward the client's culture. - While it is important for nurses to approach their care with an open and respectful attitude, simply adopting a positive mindset may not address the underlying cultural bias. It is crucial for nurses to engage in self-reflection and critical thinking to understand and challenge their own biases effectively.
Key Elements of Cultural Competence
A nurse is caring for a client who has recently immigrated from China and does not speak English. Which action by the nurse demonstrates cultural competence?
Explanation
Rationale: The nurse demonstrates cultural competence by using an interpreter to communicate with the client and family, ensuring that the information is conveyed accurately and respectfully, and that the client's preferences and needs are understood.
Incorrect options:
B) Asking the client to teach the nurse some words in Mandarin. - This is not a culturally competent action, as it may make the client feel uncomfortable or pressured to teach the nurse, and it does not address the communication barrier effectively.
C) Assuming that the client follows traditional Chinese beliefs and practices. - This is not a culturally competent action, as it may lead to stereotyping and ignoring the individuality and diversity of the client. The nurse should not make assumptions based on the client's ethnicity, but rather ask open-ended questions to assess the client's cultural background, values, and beliefs.
D) Telling the client that the nurse has visited China before and liked it. - This is not a culturally competent action, as it may come across as superficial or patronizing, and it does not show genuine interest or respect for the client's culture.
A client from Mexico is admitted to the hospital with abdominal pain and fever. The nurse notices that the client has a red string tied around his wrist. What should the nurse do?
Explanation
Rationale: The nurse should ask the client about the meaning and purpose of the string, as it may be a cultural or religious symbol or practice that is important to the client. The nurse should respect and support the client's cultural beliefs and practices, as long as they do not interfere with the medical treatment or pose a risk to safety.
Incorrect options:
A) Cut off the string and dispose of it. - This is not a culturally competent action, as it may offend or distress the client, who may view the string as a protective or healing object. The nurse should not remove or discard any cultural or religious items without the client's consent.
C) Ignore the string and focus on the physical assessment. - This is not a culturally competent action, as it may indicate a lack of interest or respect for the client's culture. The nurse should acknowledge and inquire about any cultural or religious items or practices that are relevant to the client's care.
D) Report the string to the infection control team. - This is not a culturally competent action, as it may imply that the string is a source of infection or contamination, which may not be true. The nurse should not report any cultural or religious items or practices without first assessing their significance and impact on health.
A nurse is conducting a health education session for a group of Somali women who wear hijabs (headscarves). Which statement by the nurse reflects cultural sensitivity?
Explanation
Rationale: The nurse reflects cultural sensitivity by providing health information that is relevant and respectful to the women's cultural practice of wearing hijabs. The nurse does not criticize or discourage the women from wearing hijabs, but rather offers advice on how to prevent potential health problems associated with sun exposure.
Incorrect options:
A) "You should remove your hijabs when you are indoors to prevent overheating." - This is not a culturally sensitive statement, as it may imply that wearing hijabs is unhealthy or unnecessary. The nurse should not suggest that the women change their cultural practice without understanding its meaning and importance to them.
C) "You should wash your hijabs regularly to avoid scalp infections." - This is not a culturally sensitive statement, as it may imply that the women are unhygienic or unaware of basic hygiene practices. The nurse should not assume that
the women do not wash their hijabs regularly, but rather ask them about their hygiene habits and provide education if needed.
D) "You should consider alternative ways of covering your hair that are more fashionable." - This is not a culturally sensitive statement, as it may imply that wearing hijabs is outdated or unattractive. The nurse should not judge or comment on the women's appearance or style, but rather respect their cultural expression and identity.
A client from India is diagnosed with type 2 diabetes mellitus and is prescribed a low-carbohydrate diet. The nurse reviews the client's food preferences and notes that the client eats rice, chapati (flatbread), and dal (lentil soup) daily. Which response by the nurse is most appropriate?
Explanation
Rationale: The nurse provides an appropriate response by acknowledging the client's food preferences and offering guidance on how to adjust them to meet the dietary requirements for diabetes management. The nurse does not impose or eliminate the client's cultural foods, but rather suggests ways to incorporate them into a balanced and healthy diet.
Incorrect options:
A) "You need to stop eating rice, chapati, and dal, as they are high in carbohydrates and will raise your blood sugar levels." - This is not an appropriate response, as it may be perceived as insensitive or disrespectful to the client's culture and preferences. The nurse should not prohibit or restrict the client's cultural foods without considering their significance and alternatives.
B) "You can continue eating rice, chapati, and dal, as they are part of your culture and tradition, and you should not change them." - This is not an appropriate response, as it may be misleading or harmful to the client's health. The nurse should not endorse or encourage the client's cultural foods without assessing their nutritional value and impact on blood sugar levels.
D) "You can substitute rice, chapati, and dal with other foods that are similar in taste and texture, but lower in carbohydrates, such as quinoa, cauliflower rice, and zucchini noodles." - This is not an appropriate response, as it may be unrealistic or impractical for the client to adopt. The nurse should not suggest or recommend unfamiliar or inaccessible foods without consulting the client's availability and willingness to try them.
A nurse is planning to conduct a physical examination for a client who is Muslim. Which action by the nurse demonstrates respect for the client's culture?
Explanation
Rationale: The nurse demonstrates respect for the client's culture by asking the client if he or she prefers a male or female nurse to perform
the examination. Some Muslim clients may have religious or cultural restrictions on being touched by members of the opposite sex who are not their spouses or relatives. The nurse should honor the client's preference and arrange for a same-sex nurse if possible.
Incorrect options:
B) Telling the client that he or she must remove all clothing and jewelry for the examination. - This is not a respectful action, as it may violate the client's modesty or privacy. Some Muslim clients may wear clothing or jewelry that have religious
or cultural significance, such as hijabs (headscarves), turbans, or amulets. The nurse should not force
the client to remove any items that are not necessary for the examination.
C) Explaining the purpose and procedure of each part of the examination before doing it. - This is a respectful action,but it is not specific to the client's culture. The nurse should explain the purpose and procedure of each part of
the examination before doing it for any client, regardless of their cultural background.
D) Allowing the client to have a family member or friend present during the examination. - This is a respectful action, but it is not specific to the client's culture.
Providing Culturally Competent Care
A nurse is caring for a client who has a cultural preference for using herbal remedies. Which action should the nurse take?
Explanation
Rationale: The nurse should respect the client's cultural preference for using herbal remedies and ask about the types and effects of the herbal remedies they use, as this can help to identify any potential interactions or contraindications with the prescribed medications. The nurse should also provide information about the prescribed medications and their expected outcomes, and collaborate with the client and the health care provider to develop a mutually acceptable treatment plan that incorporates both conventional and alternative therapies.
Incorrect options:
A) Discourage the client from using any herbal remedies, as they may interfere with the prescribed medications. - This is an incorrect option, as it shows a lack of respect for the client's cultural preference and may cause the client to feel defensive or distrustful of the nurse and the health care system.
C) Report the client to the health care provider for noncompliance with the prescribed treatment plan. - This is an incorrect option, as it implies that the client is violating a rule or regulation by using herbal remedies, which may not be the case. The nurse should not assume that the client is noncompliant with the prescribed treatment plan without first assessing their understanding and adherence to it.
D) Educate the client about the evidence-based benefits of conventional medicine over herbal remedies. - This is an incorrect option, as it shows a lack of cultural sensitivity and may create a power imbalance between the nurse and the client. The nurse should not impose their own beliefs or values on the client, but rather acknowledge and respect their differences and preferences.
A nurse is conducting a health history interview with a client who belongs to a different cultural group than the nurse. Which communication strategy should the nurse use to facilitate culturally competent care?
Explanation
Rationale: The nurse should use an interpreter who is familiar with both cultures and languages, if needed, to ensure accurate and effective communication with the client. The interpreter should be a trained professional who can maintain confidentiality, avoid bias, and respect cultural nuances. The nurse should also speak directly to the client, not to the interpreter, and use simple and clear language.
Incorrect options:
B) Use closed-ended questions to obtain specific and factual information from the client. - This is an incorrect option, as it may limit the amount and quality of information that the nurse can obtain from the client. The nurse should use open-ended questions to elicit more comprehensive and descriptive responses from the client, and allow them to express their concerns, beliefs, and preferences in their own words.
C) Use gestures and body language to convey meaning and emotions to the client. - This is an incorrect option, as gestures and body language may have different meanings and interpretations across different cultures. The nurse should be aware of their own nonverbal communication and avoid using gestures or expressions that may be offensive or confusing to the client. The nurse should also observe and respect the client's nonverbal cues, such as eye contact, personal space, and touch.
D) Use humor and jokes to establish rapport and trust with
the client. - This is an incorrect option, as humor and jokes may not be appropriate or appreciated in some cultures or situations. The nurse should avoid using humor or jokes that may be insensitive, disrespectful, or stereotypical of the client's culture or background. The nurse should also be mindful of their tone of voice, volume, and pace when communicating with the client.
A nurse is planning care for a client who follows a vegan diet for religious reasons. Which intervention should the nurse include in the plan of care?
Explanation
Rationale: The nurse should assess the client's nutritional status and dietary intake, as this can help to identify any nutritional deficiencies or imbalances that may affect the client's health and recovery. The nurse should also respect the client's dietary preferences and provide them with appropriate food choices that meet their nutritional needs and religious beliefs.
Incorrect options:
B) Encourage the client to consume animal products in moderation. - This is an incorrect option, as it shows a lack of respect for the client's religious beliefs and may cause the client to feel offended or pressured. The nurse should not attempt to change the client's dietary preferences, but rather support them in maintaining their dietary practices.
C) Provide education on how to prevent vitamin B12 deficiency. - This is an incorrect option, as it assumes that the client is at risk of vitamin B12 deficiency, which may not be the case. The nurse should not provide education on a specific topic without first assessing the client's knowledge and needs. The nurse should also avoid generalizing or stereotyping the client's dietary habits based on their culture or religion.
D) Refer the client to a dietician for further counseling. - This is an incorrect option, as it implies that the client needs professional guidance or intervention for their dietary choices, which may not be true. The nurse should not refer the client to a dietician without first assessing their nutritional status and dietary intake, and discussing their goals and expectations with them.
A nurse is caring for a client who has a terminal illness and requests to have a spiritual leader visit them at the hospital. Which action should the nurse take?
Explanation
Rationale: The nurse should arrange for the spiritual leader to visit the client as soon as possible, as this can help to meet the client's spiritual needs and provide them with comfort and support during a difficult time. The nurse should respect the client's request and facilitate their access to spiritual resources and services that are consistent with their beliefs and preferences.
Incorrect options:
B) Ask the client why they want to see a spiritual leader at this time. - This is an incorrect option, as it may imply that the nurse is questioning or judging the client's decision or motivation to see a spiritual leader, which may make the client feel uncomfortable or defensive. The nurse should not probe or interrogate the client about their spiritual beliefs or practices, but rather accept and acknowledge them without bias or criticism.
C) Inform the client that spiritual leaders are not allowed in the hospital due to infection control measures. - This is an incorrect option, as it may be untrue or inaccurate, depending on the hospital policies and procedures regarding visitors and infection control measures. The nurse should not deny or restrict the client's access to spiritual resources and services without a valid reason or justification, and should consult with the health care team and administration if there are any concerns or issues regarding this matter.
D) Suggest that the client can pray or meditate on their own instead of seeing a spiritual leader. - This is an incorrect option, as it may show a lack of understanding or empathy for the client's spiritual needs and desires, which may make the client feel dismissed or ignored. The nurse should not suggest alternative or substitute ways of meeting the client's spiritual needs without first assessing their preferences and expectations, and respecting their choices.
A nurse is providing discharge instructions to a client who has limited health literacy. Which strategy should the nurse use to enhance culturally competent care?
Explanation
Rationale: The nurse should provide written materials that are at an appropriate reading level and use simple language, as this can help to improve the client's comprehension and retention of information, and reduce confusion and anxiety. The written materials should also be culturally relevant and sensitive, and include pictures, diagrams, or charts if possible.
Incorrect options:
A) Use medical jargon and technical terms to explain the diagnosis and treatment plan. - This is an incorrect option, as it may overwhelm or intimidate the client, and hinder their understanding and adherence to the diagnosis and treatment plan. The nurse should avoid using medical jargon and technical terms, and instead use plain language that is clear and concise.
C) Give verbal instructions only and ask the client to repeat them back verbatim. - This is an incorrect option, as it may not be sufficient or effective. Verbal instructions alone may not adequately address the client's limited health literacy. Additionally, asking the client to repeat the instructions verbatim may not accurately gauge their understanding, as they may feel embarrassed or hesitant to ask for clarification.
D) Assume that the client understands everything and does not have any questions. - This is an incorrect option, as it overlooks the client's limited health literacy and assumes their understanding without proper assessment. It is important for the nurse to actively assess the client's understanding, encourage questions, and provide additional explanations or clarifications as needed.
Diversity and Inclusion in Healthcare Settings
A nurse is caring for a client who identifies as transgender and is scheduled for gender-affirming surgery. What is the most appropriate way for the nurse to address the client?
Explanation
Rationale: The nurse should respect the client's autonomy and dignity by addressing them by their preferred name and gender identity, regardless of their legal status or surgical status. This demonstrates cultural competence and sensitivity, and fosters a trusting relationship between the nurse and the client.
Incorrect options:
A) By their legal name and assigned sex at birth - This is an inappropriate way to address the client, as it disregards their gender identity and expression, and may cause them distress or harm.
C) By a neutral term, such as "patient" or "client" - This is an impersonal way to address the client, and may imply that the nurse is uncomfortable or unfamiliar with the client's gender identity. It may also make the client feel dehumanized or invalidated.
D) By asking the client's family or friends how they refer to the client - This is an unreliable way to address the client, as the client's family or friends may not be supportive or knowledgeable of the client's gender identity. It may also violate the client's privacy or confidentiality.
A nurse is working with a client who has recently immigrated from Somalia and practices Islam. The client is fasting during Ramadan, which coincides with their hospitalization. What should the nurse do to support the client's cultural and religious needs?
Explanation
Rationale: The nurse should respect the client's right to practice their religion and honor their cultural beliefs, as long as they do not pose a serious threat to their health or safety. The nurse should also monitor the client for any adverse effects of fasting, such as dehydration, hypoglycemia, electrolyte imbalance, or infection, and intervene as needed.
Incorrect options:
A) Encourage the client to eat small amounts of food throughout the day to maintain their nutritional status - This is a disrespectful way to approach the client, as it shows a lack of understanding and appreciation of their religious practice. It may also offend or alienate the client.
B) Arrange for the client to have halal meals delivered to their room after sunset and before dawn - This is a thoughtful gesture, but it does not address the issue of fasting during daylight hours, which is a requirement of Ramadan. The nurse should also consult with the client before making any arrangements for their meals, as they may have other preferences or restrictions.
C) Explain to the client that fasting is not advisable for their health condition and offer them alternative options - This is a paternalistic way to approach the client, as it implies that the nurse knows better than the client what is best for them. It may also undermine the client's faith or autonomy.
A nurse is conducting a health assessment on a new client who belongs to an Indigenous community. The nurse notices that the client avoids eye contact and speaks in a low voice. How should the nurse interpret these behaviors?
Explanation
Rationale: The nurse should be aware that different cultures have different norms and expectations regarding eye contact and communication styles. In some Indigenous cultures, avoiding eye contact and speaking in a low voice are considered respectful or humble behaviors, especially when interacting with someone in a position of authority or expertise.
Incorrect options:
A) As signs of anxiety or fear - This is a misinterpretation of the client's behaviors, as they may not reflect their emotional state. The nurse should not assume that the client is anxious or fearful without further assessment or evidence.
C) As signs of dishonesty or evasion - This is a biased interpretation of the client's behaviors, as it reflects a negative stereotype or prejudice. The nurse should not judge the client's honesty or credibility based on their eye contact or voice tone.
D) As signs of depression or sadness - This is an inaccurate interpretation of the client's behaviors, as they may not indicate their mood or mental health. The nurse should not diagnose the client with depression or sadness without a comprehensive evaluation or criteria.
A nurse is providing discharge instructions to a client who has limited English proficiency. The client is accompanied by their adult son, who speaks both English and the client's native language. What is the best way for the nurse to ensure effective communication and education with the client?
Explanation
Rationale: The nurse should use a professional interpreter, preferably one who is trained and certified in health care, to ensure accurate, clear, and culturally appropriate communication and education with the client. A professional interpreter can also help to maintain the client's privacy, confidentiality, and dignity.
Incorrect options:
A) Use simple words and gestures to communicate with the client directly - This is an ineffective way to communicate with the client, as it may lead to misunderstanding, confusion, or frustration. It may also convey a lack of respect or professionalism from the nurse.
B) Ask the client's son to translate the instructions for the client verbally - This is an inappropriate way to communicate with the client, as it may compromise the quality and accuracy of the information. The client's son may not be familiar with medical terminology, may omit or alter some details, or may have a personal bias or agenda.
C) Provide written instructions in both English and the client's native language - This is an insufficient way to communicate with the client, as it may not address the client's literacy level, comprehension level, or learning style. It may also not allow for feedback or clarification from the client.
A nurse is working in a long-term care facility that serves a diverse population of older adults. The nurse notices that some residents prefer to eat foods from their own cultural backgrounds, while others enjoy trying new cuisines. What term best describes this phenomenon?
Explanation
Rationale: Acculturation is the process of adopting or adapting to some aspects of another culture, while retaining one's own cultural identity. It can occur at different levels and rates, depending on various factors, such as age, education, motivation, and exposure.
Incorrect options:
B) Assimilation - Assimilation is the process of losing one's original cultural identity and becoming fully integrated into another culture. It usually involves a complete abandonment of one's native language, values, beliefs, and customs.
C) Ethnocentrism - Ethnocentrism is the tendency to view one's own culture as superior or more desirable than other cultures. It usually involves a negative or prejudiced attitude towards other cultures, and a resistance to change or diversity.
D) Multiculturalism - Multiculturalism is the recognition and appreciation of different cultures within a society. It usually involves a respect for diversity and pluralism, and a promotion of cultural exchange and dialogue.
A nurse is planning a health promotion program for a group of clients who are refugees from Syria. The nurse wants to incorporate some culturally relevant strategies to enhance the clients' participation and engagement. What should the nurse do?
Explanation
The nurse should use a variety of culturally relevant strategies to enhance the clients' participation and engagement in the health promotion program. These strategies may include:
- Inviting a religious leader from the local mosque to deliver a prayer before each session - This may show respect for the clients' faith and spirituality, which may be an important source of strength and resilience for them.
- Including some traditional Syrian dishes and beverages as part of the refreshments - This may show appreciation for the clients' culinary heritage and preferences, which may be an important aspect of their identity and culture.
- Using some Arabic words and phrases when greeting and thanking the clients - This may show interest in learning about the clients' language and communication style, which may be an important factor in building rapport and trust with them.
Incorrect options:
None
Cultural Competence in Specific Patient Populations
A nurse is caring for a client who has sickle cell anemia and is experiencing a vaso-occlusive crisis. The client belongs to the Jehovah's Witness faith and refuses blood transfusions. What is the best action for the nurse to take?
Explanation
Rationale: The nurse should respect the client's right to autonomy and self-determination, and honor their religious beliefs and preferences regarding blood transfusions. The nurse should provide supportive care, such as hydration, oxygenation, pain management, and infection prevention, to help the client cope with the vaso-occlusive crisis.
Incorrect options:
B) Inform the client of the risks and benefits of blood transfusions. - This option may imply that the nurse is trying to persuade or coerce the client to accept blood transfusions, which would violate the client's right to informed consent and refusal. The nurse should provide information only if the client requests it or expresses doubt about their decision.
C) Contact the hospital ethics committee to override the client's refusal. - This option is unethical and unnecessary, as the client has the capacity to make their own decisions and has clearly stated their refusal of blood transfusions. The hospital ethics committee should only be involved if there is a conflict or uncertainty about the client's wishes or best interests.
D) Ask the client to sign a consent form for blood transfusions in case of emergency. - This option is disrespectful and inappropriate, as it disregards the client's religious beliefs and values, and implies that the nurse does not trust or support the client's decision.
A nurse is conducting a health assessment for a new client who immigrated from China. The client speaks limited English and has a translator present. Which of the following actions should the nurse take to facilitate effective communication?
Explanation
Rationale: The nurse should use simple words and short sentences when speaking to a client who has limited English proficiency, as this can help to avoid confusion and misunderstanding. The nurse should also speak slowly and clearly, repeat or rephrase information as needed, and ask for feedback to ensure comprehension.
Incorrect options:
B) Direct questions and statements to the translator rather than the client. - This option is incorrect, as it can make the client feel ignored or excluded from the conversation. The nurse should direct questions and statements to the client, using the translator as a facilitator rather than an intermediary. The nurse should also acknowledge and thank the translator for their assistance.
C) Avoid using gestures or nonverbal cues that may have different meanings in different cultures. - This option is partially correct, as some gestures or nonverbal cues may have different meanings or interpretations in different cultures, and may cause offense or misunderstanding. However, avoiding all gestures or nonverbal cues may also hinder communication, as they can convey emotions, attitudes, or emphasis that words alone cannot. The nurse should be aware of potential cultural differences in nonverbal communication, and use gestures or nonverbal cues that are appropriate and respectful for the client's culture.
D) Maintain eye contact with the client throughout the assessment to show interest and respect. - This option is incorrect, as eye contact may have different meanings in different cultures. In some cultures, such as China, eye contact may be considered rude, aggressive, or disrespectful, especially when interacting with someone of higher status or authority. The nurse should be sensitive to the client's cultural norms and preferences regarding eye contact, and adjust accordingly.
A nurse is planning care for a client who practices Islam and is admitted for surgery. Which of the following interventions should the nurse include in the plan of care?
Explanation
Rationale: The nurse should allow the client to practice their religious rituals, such as praying five times a day facing Mecca, as this can help them cope with stress, anxiety, and pain, and promote healing and recovery. The nurse should also respect the client's privacy and dignity during their prayer times, and avoid interrupting or disturbing them unless necessary.
Incorrect options:
A) Provide pork-free meals for the client. - This option is correct, as pork is forbidden in Islam, and the nurse should provide meals that are consistent with the client's dietary restrictions and preferences. However, this option is not the best, as it is not specific to the client's surgical care, and it is a standard practice for all clients who follow Islam.
C) Encourage family members to visit during visiting hours only. - This option is incorrect, as family members play an important role in providing emotional and spiritual support to the client, and may also assist with personal care or decision making. The nurse should accommodate the client's wishes regarding family visitation, and collaborate with the health care team and the facility policies to ensure safety and infection control.
D) Assign a same-sex nurse to perform personal care for the client. - This option is incorrect, as it may not be feasible or realistic to assign a same-sex nurse to every client who practices Islam, and it may also limit the client's access to quality care. The nurse should respect the client's modesty and preferences regarding personal care, and provide privacy, draping, and chaperones as needed. The nurse should also explain the rationale and benefits of any invasive or intimate procedures, and obtain the client's consent before performing them.
A nurse is providing discharge teaching to a client who has type 2 diabetes mellitus and follows a vegetarian diet. Which of the following food choices should the nurse recommend as a good source of protein for the client?
Explanation
Rationale: Tofu is a good source of protein for clients who follow a vegetarian diet, as it is made from soybeans, which are high in protein and low in saturated fat and cholesterol. Tofu can also help lower blood glucose levels, as it has a low glycemic index and can improve insulin sensitivity.
Incorrect options:
B) Rice - Rice is a source of carbohydrates, not protein, and it can raise blood glucose levels, as it has a high glycemic index and can cause spikes in insulin secretion.
C) Cheese - Cheese is a source of protein, but it is also high in saturated fat and cholesterol, which can increase the risk of cardiovascular complications for clients who have diabetes mellitus. Cheese can also raise blood glucose levels, as it contains lactose, which is a type of sugar.
D) Banana - Banana is a source of carbohydrates, not protein, and it can raise blood glucose levels, as it contains fructose, which is a type of sugar. Banana also has a high glycemic index and can cause rapid changes in insulin secretion.
A nurse is caring for a client who has terminal cancer and requests to receive hospice care at home. The client's family members express concern about the client's decision and ask the nurse to convince the client to stay in the hospital. Which of the following responses should the nurse make?
Explanation
Rationale: The nurse should acknowledge the family members' concern, but also respect the client's right to autonomy and self-determination regarding end-of-life care. The nurse should explain that the client has the right to choose where they want to receive hospice care, whether it is at home or in another setting.
Incorrect options:
B) "I think you should respect your loved one's decision, as hospice care can provide comfort and quality of life at home." - This option is partially correct, as hospice care can provide comfort and quality of life at home for clients who have terminal illnesses. However, this option may imply that the nurse is taking sides with the client or judging the family members for their concern. The nurse should avoid making personal opinions or assumptions about the best option for end-of-life care, as this may vary depending on the client's preferences and values.
C) "I'm sorry, but your loved one has made up their mind, and there is nothing you or I can do to change it." - This option is dismissive and insensitive, as it does not acknowledge or address the family members' concern or attempt to provide support or information. The nurse should engage in open and empathetic communication with the family members to address their concerns and provide education and resources about hospice care.
D) "I agree with your loved one's decision, as hospice care at home is more cost-effective and convenient than hospital care." - This option is inappropriate, as it focuses on cost-effectiveness and convenience rather than the client's autonomy and right to choose their preferred care setting. The nurse should prioritize the client's wishes and values when discussing end-of-life care decisions.
Promoting Cultural Competence in Healthcare Organizations
A nurse is caring for a client who has recently immigrated from China and does not speak English. Which action by the nurse demonstrates cultural competence?
Explanation
Rationale: The nurse demonstrates cultural competence by using an interpreter to communicate with the client and family, ensuring that the information is conveyed accurately and respectfully, and that the client's preferences and needs are understood.
Incorrect options:
B) Asking the client to teach the nurse some words in Mandarin. - This is not a culturally competent action, as it may put undue pressure on the client to educate the nurse, and it may not be relevant to the client's health care needs.
C) Assuming that the client follows traditional Chinese beliefs and practices. - This is not a culturally competent action, as it may lead to stereotyping and ignoring the individuality and diversity of the client.
D) Giving the client a pamphlet about American health care system. - This is not a culturally competent action, as it may imply that the American health care system is superior or more desirable than the client's own culture and values.
A nurse is conducting a health assessment for a client who identifies as Native American. The nurse notices that the client avoids eye contact during the interview. How should the nurse interpret this behavior?
Explanation
Rationale: The nurse should interpret the client's behavior as showing respect and deference, as this is a common cultural norm among some Native American groups. Eye contact may be considered intrusive or aggressive in some cultures, and avoiding eye contact may indicate respect for authority or elders.
Incorrect options:
A) The client is shy and nervous. - This is not a correct interpretation, as it may reflect the nurse's own cultural bias or assumption, rather than the client's actual feelings or intentions.
B) The client is disrespectful and rude. - This is not a correct interpretation, as it may reflect the nurse's own cultural bias or assumption, rather than the client's actual feelings or intentions.
D) The client is hiding something or lying. - This is not a correct interpretation, as it may reflect the nurse's own cultural bias or assumption, rather than the client's actual feelings or intentions.
A nurse is planning to provide education to a group of clients who have diabetes mellitus. The group consists of clients from various cultural backgrounds, including Hispanic, African American, Asian, and Middle Eastern. Which strategy should the nurse use to promote cultural competence in health education?
Explanation
Rationale: The nurse should use this strategy to promote cultural competence in health education, as it shows respect for the clients' culture and diversity, acknowledges their unique needs and preferences, and enhances their understanding and engagement.
Incorrect options:
A) Using standardized materials that are written in English and have pictures of people from different races and ethnicities. - This is not a culturally competent strategy, as it may not address the specific needs or concerns of each client group, and it may not be accessible or appropriate for clients who have limited English proficiency or literacy skills.
C) Avoiding any mention of culture or diversity, and focusing on the scientific facts and evidence-based guidelines for diabetes management. - This is not a culturally competent strategy, as it may ignore or dismiss the influence of culture on health behaviors, beliefs, and outcomes, and it may not be relevant or acceptable for clients who have different worldviews or values regarding health and illness.
D) Asking each client group to share their own experiences and challenges with diabetes, and facilitating a discussion among them. - This is not a culturally competent strategy, as it may put undue burden on the clients to educate each other or expose their personal information, and it may create conflict or misunderstanding among clients who have different perspectives or opinions.
A nurse is working in a community health center that serves a diverse population of clients. The nurse notices that some clients from certain cultural groups tend to seek health care only when they have an acute problem or an emergency, rather than for preventive or routine care. What is the most likely reason for this behavior?
Explanation
Rationale: The most likely reason for this behavior is that the clients have a low socioeconomic status and face barriers to accessing health care, such as lack of insurance, transportation, or time. These factors may limit the clients' ability or willingness to seek preventive or routine care, and may increase their risk of developing or worsening chronic conditions.
Incorrect options:
A) The clients have a fatalistic view of health and illness, and believe that they have no control over their health outcomes. - This is not the most likely reason for this behavior, as it may not apply to all clients from certain cultural groups, and it may not account for other factors that influence health-seeking behaviors, such as access, availability, or affordability of health care services.
B) The clients have a holistic view of health and illness, and prefer to use alternative or complementary therapies rather than conventional medicine. - This is not the most likely reason for this behavior, as it may not apply to all clients from certain cultural groups, and it may not account for other factors that influence health-seeking behaviors, such as access, availability, or affordability of health care services.
D) The clients have a high level of trust and satisfaction with their health care providers, and do not feel the need to seek health care unless they have a serious problem. - This is not the most likely reason for this behavior, as it may not apply to all clients from certain cultural groups, and it may not account for other factors that influence health-seeking behaviors, such as access, availability, or affordability of health care services.
A nurse is caring for a client who is Muslim and observes Ramadan. The client is scheduled to undergo a surgical procedure in the morning. Which action by the nurse demonstrates cultural sensitivity?
Explanation
The nurse demonstrates cultural sensitivity by informing the client that they can break their fast for medical reasons, as this is an exception that is allowed in Islam. The nurse should respect the client's religious beliefs and practices, but also provide accurate and relevant information that may affect their health and safety.
Incorrect options:
A) Asking the client if they would like to pray before the surgery. - This is not a culturally sensitive action, as it may imply that the nurse is questioning or challenging the client's faith or devotion.
C) Offering the client a light breakfast before the surgery. - This is not a culturally sensitive action, as it may disregard the client's religious obligation to fast during Ramadan.
D) Respecting the client's decision to fast until sunset. - This is not a culturally sensitive action, as it may compromise the client's health and safety before undergoing surgery.
A nurse is providing discharge instructions to a client who has hypertension. The client is from Haiti and speaks Creole. The nurse uses an interpreter to communicate with the client. Which statement by the nurse indicates effective use of an interpreter?
Explanation
Rationale: The nurse indicates effective use of an interpreter by using this statement, as it follows the best practices for working with an interpreter, such as speaking directly to the client in short sentences, using clear and simple language, and avoiding jargon or slang.
Incorrect options:
B) "Can you ask the client if they have any questions about their medications?" - This is not an effective use of an interpreter , as it creates a barrier between the nurse and the client by asking the interpreter to ask the client directly. The nurse should directly address the client and ask if they have any questions about their medications.
C) "How do you say 'blood pressure' in Creole?" - While it may be helpful for the nurse to learn some basic Creole terminology, this statement does not indicate effective use of an interpreter. The nurse should focus on communicating the necessary information to the client and rely on the interpreter for accurate translation.
D) "Do you think the client understands what I am saying?" - This statement does not indicate effective use of an interpreter. Instead, the nurse should directly ask the client if they understand the instructions and information provided, and seek clarification or additional explanation if needed.
Exams on Cultural Competence and Diversity in Healthcare
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction to Cultural Competence and Diversity in Healthcare
- Cultural Awareness and Self-Reflection
- Key Elements of Cultural Competence
- Providing Culturally Competent Care
- Diversity and Inclusion in Healthcare Settings
- Cultural Competence in Specific Patient Populations
- Promoting Cultural Competence in Healthcare Organizations
- Conclusion
- Summary
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Define cultural competence and diversity in healthcare
-
Explain the importance of cultural awareness and self-reflection for healthcare providers
-
Identify the key elements of cultural competence and how to apply them in practice
-
Describe strategies for providing culturally competent care to diverse patient populations
-
Discuss the benefits of diversity and inclusion in healthcare settings
-
Recognize the specific needs and challenges of different cultural groups in healthcare
-
Explore ways to promote cultural competence in healthcare organizations
-
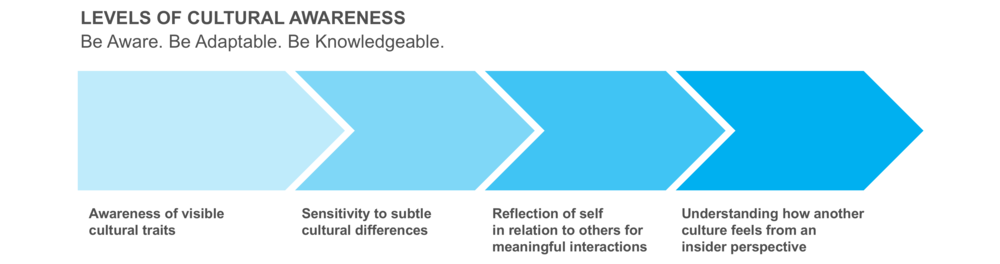
Cultural awareness is the recognition and appreciation of one's own culture and the cultures of others
-
Self-reflection is the process of examining one's own beliefs, values, assumptions, biases, stereotypes, and prejudices that may affect one's interactions with others
-
Healthcare providers need to be culturally aware and self-reflective to understand how their own culture influences their perceptions, attitudes, behaviors, and communication styles
-
Cultural awareness and self-reflection can help healthcare providers avoid cultural misunderstandings, conflicts, or errors that may compromise patient safety or quality of care
Introduction to Cultural Competence and Diversity in Healthcare
-
Cultural competence is the ability to provide effective and respectful care to patients from different cultural backgrounds, beliefs, values, and preferences
-
Diversity is the presence of differences among people, such as race, ethnicity, gender, age, religion, sexual orientation, disability, language, socioeconomic status, etc.
-
Healthcare providers encounter diverse patients every day and need to be culturally competent to meet their needs and expectations
-
Cultural competence and diversity are essential for improving health outcomes, reducing health disparities, enhancing patient satisfaction, and fostering a positive work environment
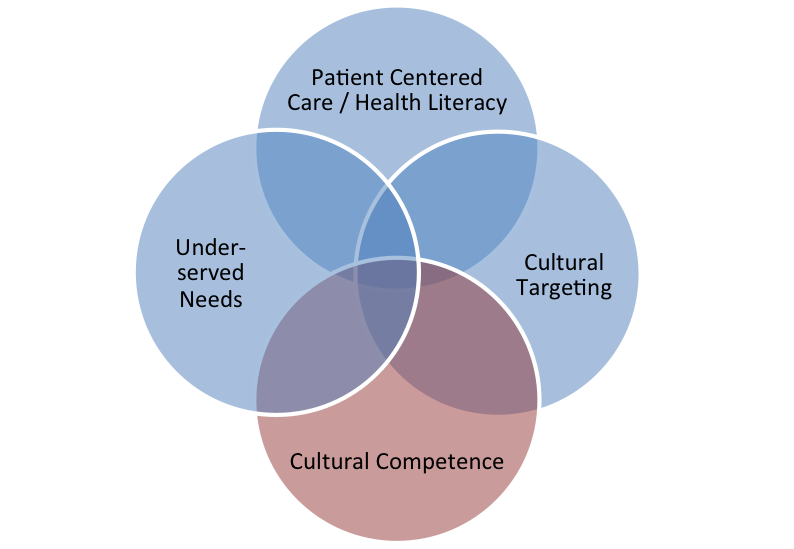
Key Elements of Cultural Competence
-
Cultural competence involves four interrelated components: cultural knowledge, cultural skills, cultural sensitivity, and cultural humility
-
Cultural knowledge is the acquisition of factual information about the history, traditions, beliefs, values, norms, practices, and health behaviors of different cultural groups
-
Cultural skills are the abilities to collect relevant cultural data, conduct culturally appropriate assessments, interventions, and evaluations, and use culturally competent communication techniques
-
Cultural sensitivity is the respect and appreciation for the diversity and uniqueness of each individual patient and their culture
-
Cultural humility is the recognition of one's own limitations and biases and the willingness to learn from others and seek feedback

Providing Culturally Competent Care
Culturally competent care is patient-centered care that takes into account the patient's cultural background, preferences, needs, values, and goals
-
Healthcare providers can provide culturally competent care by using the following strategies:
-
Ask open-ended questions to elicit the patient's perspective on their health condition, expectations, concerns, preferences, beliefs, values, etc.
-
Use active listening skills to show interest, empathy, respect, and understanding
-
Use plain language and avoid jargon or slang that may confuse or offend the patient
-
Use interpreters or translation services when needed to ensure clear and accurate communication
-
Validate the patient's feelings and experiences without judging or dismissing them
-
Negotiate a mutually agreeable plan of care that incorporates the patient's input and preferences as much as possible
-
Educate the patient about their health condition and treatment options in a culturally appropriate way
-
Advocate for the patient's rights and interests when necessar
Diversity and Inclusion in Healthcare Settings
-
Diversity and inclusion are organizational values that promote respect for differences among people and foster a culture of belonging and collaboration
-
Healthcare settings can benefit from diversity and inclusion by:
-
Attracting and retaining a diverse workforce that reflects the diversity of the patient population and brings diverse perspectives, skills, experiences, and ideas
-
Enhancing teamwork and communication among staff members from different backgrounds and disciplines
-
Improving patient satisfaction and loyalty by providing culturally competent care that meets their needs and expectations
-
Increasing innovation and creativity by encouraging diverse input and feedback
-
Reducing errors and risks by addressing potential cultural barriers or gaps in care delivery

Cultural Competence in Specific Patient Populations
-
Healthcare providers need to be aware of the specific needs and challenges of different patient populations that may require special attention or accommodation in healthcare settings. Some examples are:
-
Patients with limited English proficiency (LEP) who may face language barriers that affect their access to information, services, or resources. They may also have low health literacy or different health beliefs that influence their health behaviors or decisions.
-
Patients with disabilities who may have physical, sensory, cognitive, mental, or emotional impairments that affect their ability to communicate or perform daily activities. They may also face discrimination or stigma that affects their self-esteem or quality of life.
-
Patients from LGBTQ+ communities who may have diverse sexual orientations, gender identities, or expressions that affect their health needs or preferences. They may also face harassment, violence, or rejection that affects their mental health or social support.
-
Patients from racial or ethnic minority groups who may have different genetic, biological, environmental, or social factors that affect their health status or outcomes. They may also face racism, discrimination, or oppression that affects their access to care or trust in the healthcare system.
-
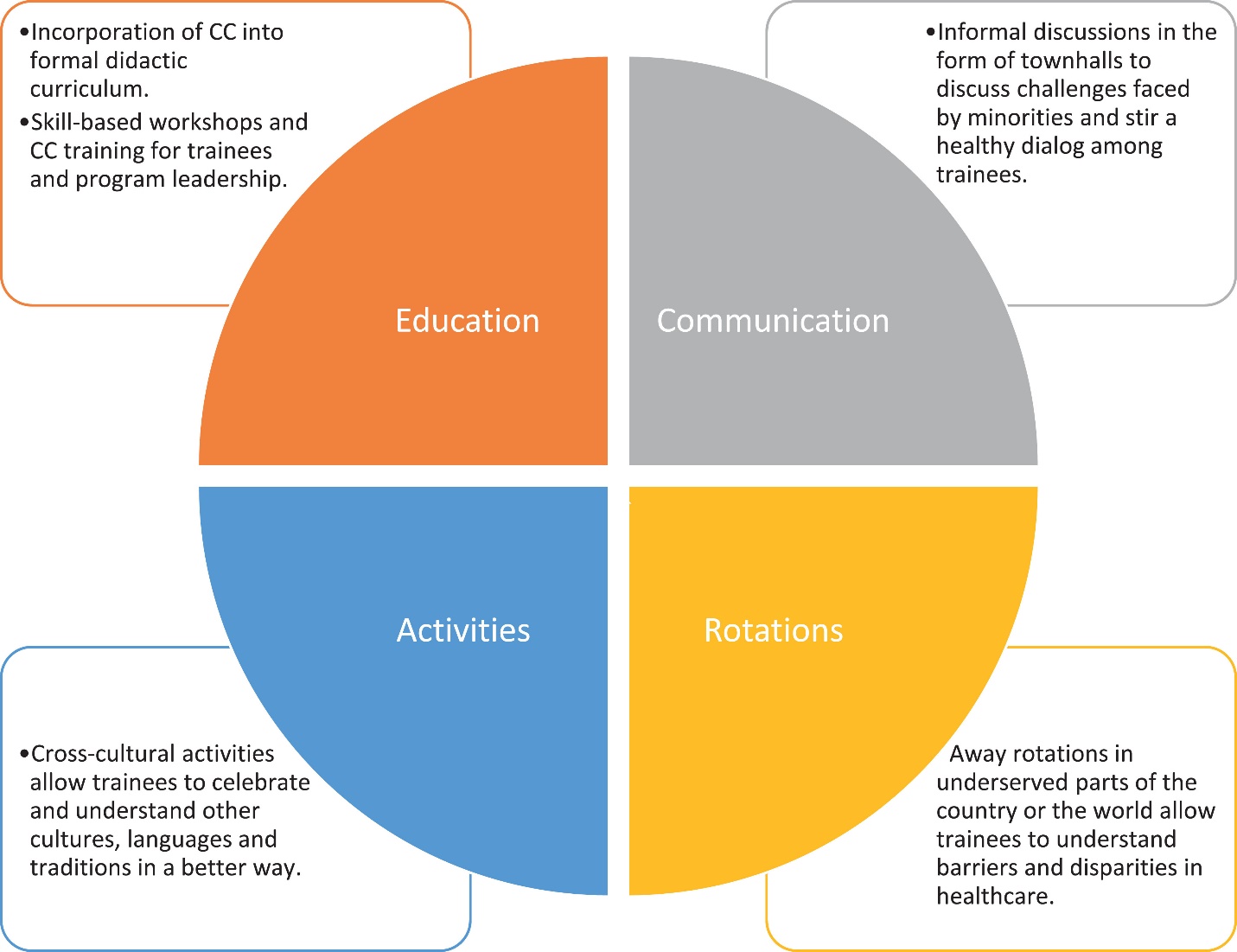
Promoting Cultural Competence in Healthcare Organizations
-
Healthcare organizations can promote cultural competence by implementing the following actions:
-
Establish a clear vision and mission statement that reflects the commitment to cultural competence and diversity
-
Develop and enforce policies and procedures that support cultural competence and diversity in all aspects of the organization
-
Provide ongoing education and training for staff members on cultural competence and diversity topics and skills
-
Conduct regular assessments and evaluations of the organization's cultural competence and diversity performance and outcomes
-
Create a supportive and inclusive work environment that values diversity and encourages feedback and collaboration
-
Engage with the community and stakeholders to build trust and partnerships

Conclusion
-
Cultural competence and diversity are vital for providing quality healthcare to diverse patient populations
-
Healthcare providers need to be culturally aware, self-reflective, knowledgeable, skilled, sensitive, and humble to provide culturally competent care
-
Healthcare settings need to embrace diversity and inclusion to create a positive work environment and improve patient satisfaction and outcomes
-
Healthcare organizations need to promote cultural competence and diversity by implementing policies, procedures, education, training, assessment, evaluation, and engagement strategies
Summary
-
Cultural competence is the ability to provide effective and respectful care to patients from different cultural backgrounds, beliefs, values, and preferences
-
Diversity is the presence of differences among people, such as race, ethnicity, gender, age, religion, sexual orientation, disability, language, socioeconomic status, etc.
-
Cultural competence and diversity are essential for improving health outcomes, reducing health disparities, enhancing patient satisfaction, and fostering a positive work environment
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Cultural Competence and Diversity in Healthcare
This filled cannot be empty

