Please set your exam date
Endocrine Systems
Study Questions
Diabetes Mellitus
The nurse is providing education to a client newly diagnosed with diabetes mellitus. Which statement by the client indicates a need for further clarification?
Explanation
This statement is incorrect because not all individuals with diabetes can control their condition through diet and exercise alone. Insulin or other medications may be necessary to achieve and maintain target blood sugar levels.
Incorrect choices:
a. This statement is correct. Diabetes mellitus is a chronic condition that affects how the body uses glucose for energy.
b. This statement is correct. Regular blood sugar monitoring is important to manage and maintain blood sugar levels within a target range.
d. This statement is correct. If left uncontrolled, diabetes can lead to various complications, including kidney damage and nerve problems.
Which of the following best describes type 1 diabetes mellitus?
Explanation
Type 1 diabetes mellitus is characterized by an autoimmune destruction of pancreatic beta cells, leading to an absolute insulin deficiency. It is not primarily characterized by insulin resistance (choice a) and is not typically diagnosed in adulthood (choice b). Oral hypoglycemic agents (choice d) are not the mainstay of treatment for type 1 diabetes.
The nurse is explaining the role of insulin in diabetes mellitus. Which statement by the client indicates a need for further clarification?
Explanation
This statement is incorrect because it inaccurately suggests that insulin administration is only necessary for type 1 diabetes. While it is essential for type 1 diabetes, it can also be used in some cases of type 2 diabetes when other treatments are ineffective.
Incorrect choices:
a. This statement is correct. Insulin facilitates the entry of glucose into cells for energy.
b. This statement is correct. Insulin is produced by the pancreas and released in response to elevated blood sugar levels.
d. This statement is correct. In type 2 diabetes, insulin resistance occurs, meaning the body's cells become less responsive to the effects of insulin.
Which of the following is a classic symptom of hyperglycemia in diabetes mellitus?
Explanation
Excessive thirst and frequent urination are classic symptoms of hyperglycemia in diabetes mellitus. These symptoms result from the body's attempt to eliminate excess glucose through urine.
Incorrect choices:
b. This choice is incorrect. Bradycardia and low blood pressure are not classic symptoms of hyperglycemia; they may be associated with other conditions.
c. This choice is incorrect. Weight gain and increased appetite are not typical symptoms of hyperglycemia; they may be observed in certain situations, but they are not characteristic of uncontrolled diabetes.
d. This choice is incorrect. Hypoglycemic episodes with confusion are symptoms of low blood sugar, not hyperglycemia.
Which of the following is a modifiable risk factor for the development of type 2 diabetes mellitus?
Explanation
Sedentary lifestyle and obesity are modifiable risk factors for the development of type 2 diabetes mellitus. Lifestyle changes, such as increasing physical activity and achieving a healthy weight, can help reduce the risk.
Incorrect choices:
a. This choice is incorrect. Family history of type 2 diabetes is a non-modifiable risk factor.
b. This choice is incorrect. Age over 65 years is a non-modifiable risk factor.
d. This choice is incorrect. Autoimmune destruction of pancreatic cells is associated with type 1 diabetes, not type 2.
The nurse is teaching a client with diabetes about the importance of blood sugar monitoring. Which statement by the client indicates a need for further clarification?
Explanation
This statement is incorrect because blood sugar monitoring is an essential part of diabetes management, even when the client is feeling well. It provides valuable information about blood sugar levels and helps prevent both high and low blood sugar episodes.
Incorrect choices:
a. This statement is correct. Regular blood sugar monitoring provides insights into how the body responds to food and medication.
b. This statement is correct. Blood sugar monitoring is important for preventing both hyperglycemic and hypoglycemic episodes.
d. This statement is correct. Monitoring blood sugar levels empowers the client to make informed decisions about their diabetes management.
Which of the following is a long-term complication associated with uncontrolled diabetes mellitus?
Explanation
Uncontrolled diabetes can lead to nerve damage, a condition known as neuropathy. This can result in symptoms such as numbness, tingling, and pain in the extremities.
Incorrect choices:
a. This choice is incorrect. Temporary vision changes may occur due to high blood sugar levels, but it is not a long-term complication.
b. This choice is incorrect. Frequent hypoglycemic episodes may occur with medication use, but it is not a typical long-term complication of uncontrolled diabetes.
c. This choice is incorrect. Diarrhea and stomach cramps are not commonly associated with long-term complications of diabetes.
Which of the following is an appropriate dietary recommendation for a client with diabetes mellitus?
Explanation
Including a variety of whole grains, lean proteins, and vegetables in meals is an appropriate dietary recommendation for a client with diabetes. Carbohydrates should not be completely avoided (choice a), and sugary snacks should be limited (choice b). Adequate fluid intake is important, and there is no need to restrict fluids (choice d).
Incorrect choices:
a. This choice is incorrect. Carbohydrates are an important source of energy and should not be completely avoided. The focus should be on managing portion sizes and making healthy carbohydrate choices.
b. This choice is incorrect. Consuming high amounts of sugary snacks can lead to blood sugar spikes and is not recommended for individuals with diabetes.
d. This choice is incorrect. Adequate fluid intake is important for overall health and is not typically restricted in diabetes management.
A client with diabetes is experiencing symptoms of hypoglycemia. The nurse should instruct the client to consume:
Explanation
Consuming a piece of fruit is an appropriate choice for treating hypoglycemia, as it provides a source of natural sugars that can help raise blood sugar levels.
Incorrect choices:
a. This choice is incorrect. A large serving of pasta contains complex carbohydrates that may take longer to raise blood sugar levels.
c. This choice is incorrect. A candy bar may provide a quick source of sugar, but it is often high in added sugars and unhealthy fats.
d. This choice is incorrect. Alcohol can further lower blood sugar levels and is not recommended for treating hypoglycemia.
The nurse is teaching a client about foot care for diabetes management. Which statement by the client indicates a need for further clarification?
Explanation
Soaking feet in hot water can lead to burns and is not recommended for individuals with diabetes, as they may have reduced sensation. Warm water and gentle cleaning are more appropriate for foot care.
Incorrect choices:
a. This statement is correct. Daily inspection of the feet is important to detect any cuts, sores, or blisters early and prevent complications.
c. This statement is correct. Wearing comfortable shoes and avoiding high heels helps protect the feet and prevent injuries.
d. This statement is correct. Moisturizing the feet regularly can help prevent dry skin, which can lead to cracks and potential infections.
Which of the following statements accurately describes the pathophysiology of type 1 diabetes mellitus?
Explanation
Type 1 diabetes is characterized by the autoimmune destruction of pancreatic beta cells, leading to a lack of insulin production. This results in an absolute insulin deficiency and requires external insulin administration.
Incorrect choices:
a. This choice is incorrect. Insulin resistance is a characteristic of type 2 diabetes, not type 1.
b. This choice is incorrect. Type 1 diabetes is not primarily caused by lifestyle factors; it has an autoimmune etiology.
d. This choice is incorrect. Type 1 diabetes typically develops in childhood or adolescence, not adulthood, and is not associated with insulin resistance.
Which of the following pathophysiological mechanisms contributes to hyperglycemia in type 2 diabetes mellitus?
Explanation
In type 2 diabetes, insulin resistance occurs, meaning that the body's cells do not respond effectively to the action of insulin. This leads to decreased glucose uptake by cells and elevated blood sugar levels.
Incorrect choices:
a. This choice is incorrect. Autoimmune destruction of pancreatic beta cells is characteristic of type 1 diabetes, not type 2.
b. This choice is incorrect. Increased sensitivity of cells to insulin would result in improved glucose uptake and reduced hyperglycemia.
d. This choice is incorrect. Excess insulin production by the pancreas is not a typical mechanism in type 2 diabetes.
Which of the following accurately describes the role of insulin in glucose metabolism?
Explanation
Insulin plays a key role in glucose metabolism by facilitating the uptake of glucose into cells, reducing blood sugar levels. It also promotes glycogen synthesis in the liver and muscle cells.
Incorrect choices:
a. This choice is incorrect. Insulin promotes glucose uptake into cells, leading to decreased blood sugar levels.
b. This choice is incorrect. Insulin promotes glycogen synthesis, which stores glucose and reduces blood sugar levels.
d. This choice is incorrect. Insulin promotes glycogen synthesis, contributing to the storage of glucose and lowering blood sugar levels.
Which of the following is a potential consequence of prolonged hyperglycemia in diabetes mellitus?
Explanation
Prolonged hyperglycemia in diabetes can lead to the formation of advanced glycation end products (AGEs), which contribute to tissue damage, inflammation, and complications such as neuropathy and nephropathy.
Incorrect choices:
a. This choice is incorrect. Hypoglycemic episodes are associated with low blood sugar, not prolonged hyperglycemia.
b. This choice is incorrect. Increased cellular glucose uptake and energy production would not be consequences of prolonged hyperglycemia; rather, hyperglycemia impairs cellular glucose uptake.
d. This choice is incorrect. Prolonged hyperglycemia leads to insulin resistance, not enhanced insulin sensitivity.
Which classification of diabetes mellitus is characterized by an autoimmune destruction of pancreatic beta cells, resulting in an absolute insulin deficiency?
Explanation
Type 1 diabetes mellitus is characterized by an autoimmune response that targets and destroys pancreatic beta cells, leading to an absolute deficiency of insulin production.
Incorrect choices:
b. This choice is incorrect. Type 2 diabetes mellitus involves insulin resistance and relative insulin deficiency, but not the autoimmune destruction of beta cells.
c. This choice is incorrect. Gestational diabetes mellitus occurs during pregnancy and is not characterized by autoimmune destruction of beta cells.
d. This choice is incorrect. Secondary diabetes mellitus is caused by other underlying medical conditions or factors and is not primarily characterized by autoimmune destruction of beta cells.
Which classification of diabetes mellitus is primarily characterized by insulin resistance and relative insulin deficiency?
Explanation
Type 2 diabetes mellitus is characterized by insulin resistance, where cells do not effectively respond to insulin, and relative insulin deficiency due to impaired beta cell function.
Incorrect choices:
a. This choice is incorrect. Type 1 diabetes mellitus involves autoimmune destruction of beta cells and an absolute insulin deficiency.
c. This choice is incorrect. Gestational diabetes mellitus occurs during pregnancy and may involve a combination of insulin resistance and impaired insulin secretion.
d. This choice is incorrect. Secondary diabetes mellitus is caused by other medical conditions or factors, not primarily by insulin resistance and relative insulin deficiency.
Which classification of diabetes mellitus occurs during pregnancy and typically resolves after childbirth?
Explanation
Gestational diabetes mellitus (GDM) occurs during pregnancy due to hormonal changes that increase insulin resistance. It usually resolves after childbirth, but women with GDM have an increased risk of developing type 2 diabetes later in life.
Incorrect choices:
a. This choice is incorrect. Type 1 diabetes mellitus involves autoimmune destruction of beta cells and is not related to pregnancy.
b. This choice is incorrect. Type 2 diabetes mellitus involves insulin resistance and relative insulin deficiency and is not specific to pregnancy.
d. This choice is incorrect. Secondary diabetes mellitus is caused by other underlying medical conditions or factors and is not specific to pregnancy.
Which classification of diabetes mellitus is caused by other medical conditions or factors, such as certain medications or hormonal imbalances?
Explanation
Secondary diabetes mellitus is caused by other medical conditions or factors that affect insulin secretion or action, such as medications, hormonal disorders, or specific medical conditions.
Incorrect choices:
a. This choice is incorrect. Type 1 diabetes mellitus is primarily caused by autoimmune destruction of beta cells.
b. This choice is incorrect. Type 2 diabetes mellitus involves insulin resistance and relative insulin deficiency, often influenced by lifestyle factors.
c. This choice is incorrect. Gestational diabetes mellitus occurs during pregnancy due to hormonal changes and is not primarily caused by other medical conditions or factors.
Which classification of diabetes mellitus is not related to insulin deficiency or resistance, but rather results from genetic mutations affecting the function of specific genes involved in beta cell function?
Explanation
MODY is a rare form of diabetes caused by genetic mutations affecting beta cell function. It is not primarily related to insulin deficiency or resistance.
Incorrect choices:
a. This choice is incorrect. Type 1 diabetes mellitus involves autoimmune destruction of beta cells and insulin deficiency.
b. This choice is incorrect. Type 2 diabetes mellitus involves insulin resistance and relative insulin deficiency.
d. This choice is incorrect. Gestational diabetes mellitus occurs during pregnancy due to hormonal changes and is not primarily caused by genetic mutations.
Which clinical manifestation is often referred to as the "three P's" of diabetes mellitus?
Explanation
The "three P's" of diabetes mellitus refer to polyuria (excessive urination), polydipsia (excessive thirst), and polyphagia (excessive hunger) due to the body's inability to effectively use glucose for energy.
Incorrect choices:
a. This choice is incorrect. Increased appetite, weight gain, and bloating are not characteristic of diabetes mellitus; rather, diabetes is associated with weight loss despite increased appetite (polyphagia).
c. This choice is incorrect. Pallor, palpitations, and pain are not specific manifestations of diabetes mellitus.
d. This choice is incorrect. Panic attacks, paranoia, and paresthesia are not typical clinical manifestations of diabetes mellitus.
Which clinical manifestation of diabetes mellitus is related to long-standing hyperglycemia and may result in slow wound healing and frequent infections?
Explanation
Long-standing hyperglycemia in diabetes mellitus can lead to impaired wound healing, as high blood sugar levels affect blood flow and immune function, increasing the risk of infections.
Incorrect choices:
a. This choice is incorrect. Polyuria, polydipsia, and polyphagia are the "three P's" associated with diabetes-related hyperglycemia.
b. This choice is incorrect. Nausea, vomiting, and abdominal pain are not typically related to long-standing hyperglycemia in diabetes.
c. This choice is incorrect. Blurred vision and vision loss are manifestations of diabetic retinopathy, a microvascular complication, rather than impaired wound healing.
Which clinical manifestation of diabetes mellitus results from chronic hyperglycemia damaging small blood vessels and nerves?
Explanation
Chronic hyperglycemia in diabetes mellitus can lead to damage of small blood vessels and nerves, resulting in neuropathy characterized by numbness, tingling, and pain in the extremities.
Incorrect choices:
a. This choice is incorrect. Nausea, vomiting, and abdominal pain are not typically manifestations of neuropathy in diabetes mellitus.
b. This choice is incorrect. Blurred vision and vision loss are associated with diabetic retinopathy, a microvascular complication, not nerve damage.
c. This choice is incorrect. Impaired wound healing and increased susceptibility to infections are related to the effects of hyperglycemia on blood flow and immune function, rather than nerve damage.
Which clinical manifestation of diabetes mellitus is characterized by blurred or distorted vision?
Explanation
Diabetic retinopathy, a microvascular complication of diabetes mellitus, can lead to blurred or distorted vision due to damage to the blood vessels in the retina.
Incorrect choices:
a. This choice is incorrect. Polyuria, polydipsia, and polyphagia are the "three P's" associated with hyperglycemia in diabetes mellitus.
b. This choice is incorrect. Nausea, vomiting, and abdominal pain are not typically associated with blurred or distorted vision.
c. This choice is incorrect. Impaired wound healing and increased susceptibility to infections are related to the effects of hyperglycemia on blood flow and immune function, rather than visual disturbances.
Which clinical manifestation of diabetes mellitus is commonly associated with weight loss despite increased appetite?
Explanation
Weight loss despite increased appetite (polyphagia) is a clinical manifestation of diabetes mellitus due to the body's inability to effectively use glucose for energy, leading to breakdown of muscle and fat tissue.
Incorrect choices:
b. This choice is incorrect. Nausea, vomiting, and abdominal pain are not directly related to weight loss despite increased appetite.
c. This choice is incorrect. Impaired wound healing and increased susceptibility to infections are consequences of chronic hyperglycemia, but they are not directly related to weight loss.
d. This choice is incorrect. Rapid weight gain and bloating are not characteristic manifestations of diabetes mellitus; weight loss is more common.
Which diagnostic test is commonly used to assess long-term glucose control in individuals with diabetes mellitus?
Explanation
The HbA1c test measures the average blood glucose level over the past 2-3 months and provides information about long-term glucose control. It is commonly used to monitor diabetes management and assess the effectiveness of treatment.
Incorrect choices:
a. This choice is incorrect. The fasting blood glucose test measures blood glucose levels after an overnight fast and provides information about current glucose levels, not long-term control.
b. This choice is incorrect. The OGTT measures the body's ability to clear glucose from the blood and is used to diagnose diabetes and impaired glucose tolerance, but it is not typically used for assessing long-term glucose control.
d. This choice is incorrect. The C-peptide test is used to assess insulin production by the pancreas and is not typically used to assess long-term glucose control.
Which diagnostic criterion is indicative of diabetes mellitus on a fasting blood glucose test?
Explanation
A fasting blood glucose level of 126 mg/dL or higher on two separate occasions is indicative of diabetes mellitus. A level of 110 mg/dL is within the normal range, and levels of 90 mg/dL and 100 mg/dL are also normal.
Incorrect choices:
a. This choice is incorrect. A fasting blood glucose level of 110 mg/dL is within the normal range.
c. This choice is incorrect. A fasting blood glucose level of 90 mg/dL is within the normal range.
d. This choice is incorrect. A fasting blood glucose level of 100 mg/dL is within the normal range.
Which diagnostic test is used to assess glucose tolerance and diagnose gestational diabetes mellitus during pregnancy?
Explanation
The OGTT involves drinking a glucose solution and measuring blood glucose levels at specific intervals. It is used to assess glucose tolerance and diagnose gestational diabetes mellitus during pregnancy.
Incorrect choices:
a. This choice is incorrect. The fasting blood glucose test measures blood glucose levels after an overnight fast and is not specifically used for diagnosing gestational diabetes.
b. This choice is incorrect. The HbA1c test measures average blood glucose levels over the past 2-3 months and is not typically used for diagnosing gestational diabetes.
d. This choice is incorrect. The random blood glucose test measures blood glucose levels at any time and is not specific for diagnosing gestational diabetes.
Which diagnostic test is used to assess the body's ability to clear glucose from the blood and is commonly used to diagnose diabetes mellitus?
Explanation
The OGTT measures the body's ability to clear glucose from the blood by drinking a glucose solution and measuring blood glucose levels at specific intervals. It is commonly used to diagnose diabetes mellitus.
Incorrect choices:
a. This choice is incorrect. The fasting blood glucose test measures blood glucose levels after an overnight fast and is not specifically used to assess glucose clearance.
b. This choice is incorrect. The HbA1c test measures average blood glucose levels over the past 2-3 months and is not specifically used to assess glucose clearance.
c. This choice is incorrect. The C-peptide test assesses insulin production by the pancreas and is not specifically used to assess glucose clearance.
Which diagnostic criterion is indicative of diabetes mellitus on a random blood glucose test?
Explanation
A random blood glucose level of 140 mg/dL or higher, along with symptoms of hyperglycemia, is indicative of diabetes mellitus. Symptoms may include excessive thirst, frequent urination, and unexplained weight loss.
Incorrect choices:
a. This choice is incorrect. A random blood glucose level of 90 mg/dL is within the normal range.
c. This choice is incorrect. A random blood glucose level of 110 mg/dL is within the normal range.
d. This choice is incorrect. A random blood glucose level of 120 mg/dL is within the normal range
Which medication works by increasing insulin sensitivity in peripheral tissues, facilitating glucose uptake by cells, and is commonly used in the treatment of type 2 diabetes mellitus?
Explanation
Metformin is a commonly used oral antidiabetic medication that improves insulin sensitivity in peripheral tissues, reduces hepatic glucose production, and enhances glucose uptake by cells.
Incorrect choices:
b. This choice is incorrect. Glipizide is a sulfonylurea medication that stimulates insulin secretion from the pancreas, rather than increasing insulin sensitivity.
c. This choice is incorrect. Insulin lispro is a rapid-acting insulin analog used for mealtime coverage in insulin therapy.
d. This choice is incorrect. Exenatide is a glucagon-like peptide-1 (GLP-1) receptor agonist that stimulates insulin secretion and suppresses glucagon release, but it does not primarily target insulin sensitivity.
Which medication enhances insulin secretion from pancreatic beta cells and is commonly used to manage type 2 diabetes mellitus?
Explanation
Glipizide is a sulfonylurea medication that stimulates insulin secretion from pancreatic beta cells, helping to lower blood glucose levels in individuals with type 2 diabetes mellitus.
Incorrect choices:
a. This choice is incorrect. Metformin is an oral antidiabetic medication that primarily improves insulin sensitivity and reduces hepatic glucose production.
c. This choice is incorrect. Insulin glargine is a long-acting basal insulin used in insulin therapy to provide consistent background insulin coverage.
d. This choice is incorrect. Acarbose is an alpha-glucosidase inhibitor that delays carbohydrate absorption in the intestines and is used to manage postprandial hyperglycemia.
Which medication works by inhibiting the sodium-glucose cotransporter 2 (SGLT2) in the kidneys, leading to increased glucose excretion in the urine, and is used in the treatment of type 2 diabetes mellitus?
Explanation
Empagliflozin is an SGLT2 inhibitor that reduces renal glucose reabsorption, leading to increased urinary glucose excretion and improved glycemic control in type 2 diabetes mellitus.
Incorrect choices:
a. This choice is incorrect. Metformin primarily improves insulin sensitivity and reduces hepatic glucose production.
b. This choice is incorrect. Glipizide stimulates insulin secretion from pancreatic beta cells.
d. This choice is incorrect. Insulin detemir is a long-acting basal insulin used in insulin therapy.
Which treatment approach involves delivering a continuous subcutaneous insulin infusion using an insulin pump and providing bolus doses before meals to mimic physiologic insulin secretion?
Explanation
Basal-bolus insulin therapy involves administering a continuous basal insulin infusion to provide background insulin coverage and delivering bolus doses of insulin before meals to cover postprandial glucose elevations.
Incorrect choices:
a. This choice is incorrect. Oral antidiabetic medications are not used in basal-bolus insulin therapy.
c. This choice is incorrect. Sliding-scale insulin therapy involves adjusting insulin doses based on current blood glucose levels, rather than providing consistent basal and mealtime coverage.
d. This choice is incorrect. Insulin glargine therapy provides long-acting basal insulin coverage but does not involve bolus doses before meals.
Which treatment modality involves monitoring blood glucose levels and adjusting insulin doses based on carbohydrate intake, activity level, and current blood glucose levels to achieve tight glycemic control?
Explanation
Intensive insulin therapy involves close monitoring of blood glucose levels and making frequent adjustments to insulin doses to achieve tight glycemic control and prevent complications in individuals with diabetes mellitus.
Incorrect choices:
a. This choice is incorrect. Sliding-scale insulin therapy involves adjusting insulin doses based on current blood glucose levels, without considering other factors such as carbohydrate intake and activity.
c. This choice is incorrect. Insulin detemir therapy is a form of basal insulin coverage and does not necessarily involve frequent adjustments.
d. This choice is incorrect. Oral antidiabetic medications are not part of intensive insulin therapy.
Which chronic complication of diabetes mellitus is characterized by the thickening and narrowing of small blood vessels, leading to impaired blood flow to the lower extremities?
Explanation
Peripheral arterial disease (PAD) is a chronic complication of diabetes mellitus that results from the thickening and narrowing of small blood vessels, leading to reduced blood flow to the lower extremities. This can cause symptoms such as leg pain, numbness, and poor wound healing.
Incorrect choices:
a. This choice is incorrect. Diabetic ketoacidosis (DKA) is an acute complication characterized by high blood glucose levels, ketosis, and metabolic acidosis.
b. This choice is incorrect. Diabetic nephropathy is a chronic complication that affects the kidneys and can lead to impaired kidney function.
c. This choice is incorrect. Diabetic neuropathy refers to nerve damage due to diabetes and can cause symptoms such as tingling, pain, and loss of sensation in the extremities.
Which complication of diabetes mellitus is characterized by the accumulation of glucose within the lens of the eye, leading to changes in vision and the development of cataracts?
Explanation
Diabetic cataracts result from the accumulation of glucose within the lens of the eye, leading to changes in vision and the development of cataracts. This can cause blurred vision and visual disturbances.
Incorrect choices:
a. This choice is incorrect. Diabetic retinopathy is a complication that affects the blood vessels of the retina and can lead to vision loss.
b. This choice is incorrect. Diabetic neuropathy refers to nerve damage due to diabetes and can cause symptoms such as tingling, pain, and loss of sensation in the extremities.
c. This choice is incorrect. Diabetic ketoacidosis (DKA) is an acute complication characterized by high blood glucose levels, ketosis, and metabolic acidosis.
Which complication of diabetes mellitus is characterized by high blood glucose levels and the presence of ketones in the urine, leading to metabolic acidosis and potentially life-threatening complications?
Explanation
Diabetic ketoacidosis (DKA) is an acute complication of diabetes mellitus characterized by high blood glucose levels, the presence of ketones in the urine, metabolic acidosis, dehydration, and electrolyte imbalances. It can lead to life-threatening complications if not treated promptly.
Incorrect choices:
b. This choice is incorrect. Diabetic nephropathy is a chronic complication that affects the kidneys and can lead to impaired kidney function.
c. This choice is incorrect. Diabetic neuropathy refers to nerve damage due to diabetes and can cause symptoms such as tingling, pain, and loss of sensation in the extremities.
d. This choice is incorrect. Diabetic retinopathy is a complication that affects the blood vessels of the retina and can lead to vision loss.
Which complication of diabetes mellitus is characterized by damage to the blood vessels of the retina, leading to vision impairment and potential blindness?
Explanation
Diabetic retinopathy is a complication of diabetes mellitus that affects the blood vessels of the retina, leading to vision impairment and potential blindness. It is a result of prolonged high blood glucose levels damaging the small blood vessels in the eye.
Incorrect choices:
a. This choice is incorrect. Diabetic ketoacidosis (DKA) is an acute complication characterized by high blood glucose levels, ketosis, and metabolic acidosis.
b. This choice is incorrect. Diabetic nephropathy is a chronic complication that affects the kidneys and can lead to impaired kidney function.
c. This choice is incorrect. Diabetic neuropathy refers to nerve damage due to diabetes and can cause symptoms such as tingling, pain, and loss of sensation in the extremities.
Which complication of diabetes mellitus is characterized by kidney damage due to prolonged high blood glucose levels, leading to impaired kidney function and potential kidney failure?
Explanation
Diabetic nephropathy is a chronic complication of diabetes mellitus that affects the kidneys and can lead to impaired kidney function and potential kidney failure. Prolonged high blood glucose levels damage the small blood vessels in the kidneys, leading to kidney damage.
Incorrect choices:
a. This choice is incorrect. Diabetic ketoacidosis (DKA) is an acute complication characterized by high blood glucose levels, ketosis, and metabolic acidosis.
c. This choice is incorrect. Diabetic neuropathy refers to nerve damage due to diabetes and can cause symptoms such as tingling, pain, and loss of sensation in the extremities.
d. This choice is incorrect. Diabetic retinopathy is a complication that affects the blood vessels of the retina and can lead to vision loss.
Which type of diabetes mellitus is characterized by an autoimmune destruction of pancreatic beta cells, leading to an absolute deficiency of insulin production?
Explanation
Type 1 diabetes mellitus is characterized by an autoimmune process in which the body's immune system destroys the pancreatic beta cells responsible for producing insulin. This results in an absolute deficiency of insulin, requiring exogenous insulin administration for glycemic control.
Incorrect choices:
b. This choice is incorrect. Type 2 diabetes mellitus is characterized by insulin resistance and impaired insulin secretion, rather than autoimmune destruction of beta cells.
c. This choice is incorrect. Gestational diabetes mellitus occurs during pregnancy and is not characterized by autoimmune destruction of beta cells.
d. This choice is incorrect. Prediabetes is a precursor to type 2 diabetes and involves impaired glucose tolerance, but it does not result from autoimmune destruction of beta cells.
Which hormone, produced by the pancreas, plays a key role in regulating blood glucose levels by facilitating glucose uptake into cells and promoting its storage as glycogen in the liver and muscles?
Explanation
Insulin is a hormone produced by the pancreas that plays a crucial role in regulating blood glucose levels. It facilitates glucose uptake into cells, promotes glycogen synthesis in the liver and muscles, and inhibits hepatic glucose production.
Incorrect choices:
a. This choice is incorrect. Glucagon is another pancreatic hormone that increases blood glucose levels by promoting glycogen breakdown and glucose release from the liver.
c. This choice is incorrect. Epinephrine is a hormone produced by the adrenal glands that can raise blood glucose levels during times of stress.
d. This choice is incorrect. Cortisol, also produced by the adrenal glands, can increase blood glucose levels in response to stress and inflammation.
Which laboratory test is commonly used to monitor long-term glycemic control in individuals with diabetes mellitus by measuring average blood glucose levels over the past 2 to 3 months?
Explanation
The Hemoglobin A1c (HbA1c) test measures the percentage of hemoglobin that is glycated, reflecting average blood glucose levels over the past 2 to 3 months. It is a valuable tool for assessing long-term glycemic control.
Incorrect choices:
a. This choice is incorrect. The fasting blood glucose test measures blood glucose levels after an overnight fast and provides a snapshot of current glucose levels, rather than long-term control.
b. This choice is incorrect. The oral glucose tolerance test (OGTT) measures how the body responds to a glucose load and is used to diagnose diabetes and impaired glucose tolerance, rather than monitor long-term control.
d. This choice is incorrect. The C-peptide test is used to assess insulin production by measuring the level of C-peptide, a byproduct of insulin production.
Which dietary component is particularly important for individuals with diabetes mellitus to monitor and control due to its direct impact on blood glucose levels?
Explanation
Carbohydrates have the most significant impact on blood glucose levels as they are broken down into glucose during digestion. Monitoring and controlling carbohydrate intake is crucial for managing blood glucose levels in individuals with diabetes mellitus.
Incorrect choices:
a. This choice is incorrect. Fiber intake is important for digestive health and can help stabilize blood glucose levels, but it does not have as direct an impact as carbohydrates.
b. This choice is incorrect. Protein intake can influence insulin secretion, but it has a more modest effect on blood glucose compared to carbohydrates.
c. This choice is incorrect. Fat intake affects overall health, but it has a minimal direct impact on blood glucose levels.
Carbohydrates have the most significant impact on blood glucose levels as they are broken down into glucose during digestion. Monitoring and controlling carbohydrate intake is crucial for managing blood glucose levels in individuals with diabetes mellitus.
Explanation
Diabetic ketoacidosis (DKA) is an acute complication of diabetes mellitus characterized by severe hyperglycemia, metabolic acidosis, and ketone production. It requires prompt medical intervention, including insulin therapy and fluid replacement.
Incorrect choices:
a. This choice is incorrect. Diabetic nephropathy is a chronic complication that affects the kidneys and can lead to impaired kidney function.
b. This choice is incorrect. Diabetic retinopathy is a complication that affects the blood vessels of the retina and can lead to vision loss.
d. This choice is incorrect. Diabetic neuropathy refers to nerve damage due to diabetes and can cause symptoms such as tingling, pain, and loss of sensation in the extremities.
Which type of diabetes mellitus is characterized by an autoimmune destruction of pancreatic beta cells, leading to an absolute deficiency of insulin secretion?
Explanation
Type 1 diabetes mellitus is an autoimmune condition in which the body's immune system attacks and destroys pancreatic beta cells, resulting in a lack of insulin production.
Incorrect choices:
b. This choice is incorrect. Type 2 diabetes mellitus is characterized by insulin resistance and impaired insulin secretion, but pancreatic beta cells are not completely destroyed.
c. This choice is incorrect. Gestational diabetes mellitus occurs during pregnancy and is not caused by autoimmune destruction of pancreatic beta cells.
d. This choice is incorrect. Prediabetes is a condition in which blood glucose levels are higher than normal but not high enough to be classified as diabetes. It is not characterized by autoimmune destruction of beta cells.
Which statement about type 2 diabetes mellitus is accurate?
Explanation
Type 2 diabetes mellitus is characterized by insulin resistance, in which cells do not respond effectively to insulin, and impaired insulin secretion by pancreatic beta cells.
Incorrect choices:
a. This choice is incorrect. Type 2 diabetes mellitus is not characterized by an absolute deficiency of insulin secretion as seen in type 1 diabetes.
b. This choice is incorrect. Type 2 diabetes mellitus primarily affects adults, especially those who are older and have risk factors such as obesity and sedentary lifestyle.
d. This choice is incorrect. Type 2 diabetes mellitus is not caused by autoimmune destruction of pancreatic beta cells as seen in type 1 diabetes.
Which blood glucose level range is considered indicative of prediabetes?
Explanation
A fasting blood glucose level of 100 to 125 mg/dL is considered indicative of prediabetes, which is a condition where blood glucose levels are higher than normal but not high enough to be classified as diabetes.
Incorrect choices:
a. This choice is incorrect. A fasting blood glucose level of 70 mg/dL is within the normal range.
c. This choice is incorrect. A random blood glucose level of 150 mg/dL indicates hyperglycemia, but it is not indicative of prediabetes.
d. This choice is incorrect. An hemoglobin A1c level of 6.5% or higher is diagnostic of diabetes mellitus, not prediabetes.
Which statement accurately describes gestational diabetes mellitus (GDM)?
Explanation
Gestational diabetes mellitus (GDM) is a type of diabetes that develops during pregnancy and is characterized by high blood glucose levels. It usually resolves after childbirth but increases the risk of developing type 2 diabetes in the future.
Incorrect choices:
a. This choice is incorrect. GDM typically resolves after childbirth, not after.
b. This choice is incorrect. GDM is not a rare condition; it affects a significant percentage of pregnant women.
c. This choice is incorrect. Women with GDM have an increased risk of developing type 2 diabetes, not type 1 diabetes, later in life.
Which organ plays a central role in regulating blood glucose levels by secreting insulin and glucagon?
Explanation
The liver plays a central role in blood glucose regulation by releasing glucose into the bloodstream through glycogenolysis and gluconeogenesis when blood glucose levels are low. It also stores glucose as glycogen and responds to insulin and glucagon signals.
Incorrect choices:
b. This choice is incorrect. While the kidneys play a role in filtering blood and excreting waste products, they are not primarily responsible for regulating blood glucose levels.
c. This choice is incorrect. The lungs are involved in oxygen and carbon dioxide exchange and are not directly involved in blood glucose regulation.
d. This choice is incorrect. The spleen is involved in immune function and blood filtration, but it does not play a central role in blood glucose regulation.
Diabetes Insipidus
What is the primary cause of diabetes insipidus (DI)?
Explanation
Diabetes insipidus is primarily caused by the hyposecretion or inadequate release of antidiuretic hormone (ADH), also known as vasopressin. ADH is responsible for regulating water balance by promoting water reabsorption in the kidneys.
Incorrect choices:
a. This choice is incorrect. Overproduction of ADH would lead to excessive water reabsorption and concentrated urine, which is not characteristic of diabetes insipidus.
c. This choice is incorrect. Hypersecretion of aldosterone would lead to sodium retention and increased fluid volume, which is not characteristic of diabetes insipidus.
d. This choice is incorrect. Impaired function of the thyroid gland would lead to thyroid-related disorders, not diabetes insipidus.
What is the main target organ affected by the hyposecretion of antidiuretic hormone (ADH) in diabetes insipidus?
Explanation
The kidneys are the main target organ affected by the hyposecretion of antidiuretic hormone (ADH) in diabetes insipidus. ADH normally acts on the kidneys to promote water reabsorption and concentrate urine. In diabetes insipidus, the lack of ADH results in excessive urine production and dilute urine.
Incorrect choices:
a. This choice is incorrect. The liver is not the primary target organ affected by ADH in diabetes insipidus.
c. This choice is incorrect. The pancreas is not the primary target organ affected by ADH in diabetes insipidus.
d. This choice is incorrect. The heart is not the primary target organ affected by ADH in diabetes insipidus.
Which part of the brain is responsible for producing and releasing antidiuretic hormone (ADH)?
Explanation
The posterior lobe of the pituitary gland, also known as the neurohypophysis, is responsible for producing and releasing antidiuretic hormone (ADH) in response to signals from the hypothalamus.
Incorrect choices:
a. This choice is incorrect. The hypothalamus produces ADH and releases it into the posterior pituitary for storage and release.
c. This choice is incorrect. The anterior lobe of the pituitary gland is responsible for producing and releasing other hormones, such as growth hormone and thyroid-stimulating hormone.
d. This choice is incorrect. The pineal gland is responsible for producing melatonin, a hormone that regulates sleep-wake cycles, and is not involved in ADH production.
Which of the following statements best describes the effect of hyposecretion of antidiuretic hormone (ADH) on urine output?
Explanation
In diabetes insipidus, the hyposecretion of antidiuretic hormone (ADH) leads to decreased water reabsorption in the kidneys, resulting in increased urine output. The urine produced is dilute and lacks the normal concentration of solutes.
Incorrect choices:
a. This choice is incorrect. Urine output increases, but it becomes dilute, not concentrated.
c. This choice is incorrect. Urine output increases, and the urine becomes dilute, not concentrated.
d. This choice is incorrect. Urine output increases, but it becomes dilute, not concentrated.
Which of the following is a potential cause of central diabetes insipidus (CDI)?
Explanation
Central diabetes insipidus (CDI) can be caused by trauma or injury to the hypothalamus or pituitary gland, which disrupts the production or release of antidiuretic hormone (ADH). Other causes of CDI include tumors, infections, and certain medications.
Incorrect choices:
a. This choice is incorrect. Excessive fluid intake can lead to increased urine output, but it is not a cause of CDI.
b. This choice is incorrect. Kidney dysfunction is not a common cause of central diabetes insipidus.
d. This choice is incorrect. Hypersecretion of aldosterone would lead to sodium retention and increased fluid volume, which is not characteristic of central diabetes insipidus.
Which type of diabetes insipidus is characterized by a lack of response to antidiuretic hormone (ADH) by the kidneys, leading to excessive urine output and dehydration?
Explanation
Nephrogenic diabetes insipidus is characterized by a lack of response to ADH by the kidneys, resulting in decreased water reabsorption and increased urine output.
Incorrect choices:
a. This choice is incorrect. Central diabetes insipidus is characterized by inadequate production or release of ADH from the hypothalamus or pituitary gland.
c. This choice is incorrect. Gestational diabetes insipidus occurs during pregnancy and is rare.
d. This choice is incorrect. Type 1 diabetes insipidus is not a recognized classification of diabetes insipidus.
Which type of diabetes insipidus is caused by trauma, surgery, or other factors that disrupt the production or release of antidiuretic hormone (ADH)?
Explanation
Central diabetes insipidus is caused by trauma, surgery, or other factors that affect the production or release of ADH from the hypothalamus or pituitary gland.
Incorrect choices:
b. This choice is incorrect. Nephrogenic diabetes insipidus is characterized by a lack of response to ADH by the kidneys.
c. This choice is incorrect. Neurogenic diabetes insipidus is not a recognized classification of diabetes insipidus.
d. This choice is incorrect. Type 2 diabetes insipidus is not a recognized classification of diabetes insipidus.
Which type of diabetes insipidus occurs during pregnancy and is characterized by increased thirst and excessive urine production?
Explanation
Gestational diabetes insipidus is a rare condition that occurs during pregnancy and is characterized by increased thirst and excessive urine production. It is caused by placental production of an enzyme that breaks down ADH.
Incorrect choices:
a. This choice is incorrect. Central diabetes insipidus is not specifically associated with pregnancy and is not caused by placental factors.
b. This choice is incorrect. Nephrogenic diabetes insipidus is not specifically associated with pregnancy and is not caused by placental factors.
d. This choice is incorrect. Type 3 diabetes insipidus is not a recognized classification of diabetes insipidus.
Which type of diabetes insipidus is more commonly acquired as a result of kidney disease, medications, or electrolyte imbalances?
Explanation
Nephrogenic diabetes insipidus is more commonly acquired as a result of kidney disease, medications, electrolyte imbalances, or other factors that affect the kidney's response to ADH.
Incorrect choices:
a. This choice is incorrect. Central diabetes insipidus is not commonly acquired due to kidney disease or medications.
c. This choice is incorrect. Congenital diabetes insipidus refers to cases present from birth and is not typically acquired.
d. This choice is incorrect. Gestational diabetes insipidus is a rare condition that occurs during pregnancy and is not commonly acquired due to kidney disease or medications.
Which type of diabetes insipidus is characterized by inadequate production or release of antidiuretic hormone (ADH) from the hypothalamus or pituitary gland?
Explanation
Central diabetes insipidus is characterized by inadequate production or release of ADH from the hypothalamus or pituitary gland.
Incorrect choices:
b. This choice is incorrect. Nephrogenic diabetes insipidus is characterized by a lack of response to ADH by the kidneys.
c. This choice is incorrect. Neurogenic diabetes insipidus is not a recognized classification of diabetes insipidus.
d. This choice is incorrect. Secondary diabetes insipidus refers to cases where another condition or factor, such as head trauma or tumor, affects ADH production or release.
Which clinical manifestation is commonly observed in a client with diabetes insipidus (DI)?
Explanation
Polyuria, which refers to excessive urine output, is a hallmark clinical manifestation of diabetes insipidus (DI). In DI, the kidneys are unable to concentrate urine properly, leading to the excretion of large volumes of dilute urine.
Incorrect choices:
a. This choice is incorrect. Hypertension is not a typical clinical manifestation of diabetes insipidus.
b. This choice is incorrect. Bradycardia is not a typical clinical manifestation of diabetes insipidus.
d. This choice is incorrect. Hypoglycemia is not a typical clinical manifestation of diabetes insipidus.
Which symptom is commonly reported by clients with diabetes insipidus (DI) due to excessive fluid loss?
Explanation
Excessive fluid loss in diabetes insipidus (DI) can lead to dehydration, resulting in dry skin and mucous membranes.
Incorrect choices:
a. This choice is incorrect. Constipation is not a typical symptom of diabetes insipidus.
c. This choice is incorrect. Bradycardia is not commonly associated with diabetes insipidus.
d. This choice is incorrect. Hypoglycemia is not a typical symptom of diabetes insipidus.
Which clinical manifestation is consistent with diabetes insipidus (DI)?
Explanation
Increased thirst, or polydipsia, is a common clinical manifestation of diabetes insipidus (DI) due to the body's attempt to compensate for fluid loss.
Incorrect choices:
a. This choice is incorrect. Weight gain is not a typical clinical manifestation of diabetes insipidus, which is characterized by excessive urine output.
c. This choice is incorrect. Slow wound healing is not typically associated with diabetes insipidus.
d. This choice is incorrect. Elevated blood glucose levels are characteristic of diabetes mellitus, not diabetes insipidus.
Which symptom is a potential consequence of electrolyte imbalances resulting from excessive urine output in diabetes insipidus (DI)?
Explanation
Excessive urine output in diabetes insipidus can lead to dehydration and electrolyte imbalances, particularly hypernatremia (elevated sodium levels).
Incorrect choices:
a. This choice is incorrect. Hypokalemia (low potassium levels) is not a typical consequence of diabetes insipidus.
c. This choice is incorrect. Hypocalcemia (low calcium levels) is not a typical consequence of diabetes insipidus.
d. This choice is incorrect. Hypoglycemia is not a typical consequence of diabetes insipidus.
Which clinical manifestation is commonly observed in a client with diabetes insipidus (DI) due to excessive fluid intake to compensate for fluid loss?
Explanation
Excessive fluid intake to compensate for fluid loss in diabetes insipidus (DI) can lead to weight loss as the body attempts to excrete excess water.
Incorrect choices:
a. This choice is incorrect. Bradycardia is not typically associated with excessive fluid intake or diabetes insipidus.
b. This choice is incorrect. Hypotension is not typically associated with excessive fluid intake or diabetes insipidus.
c. This choice is incorrect. Edema is not typically associated with excessive fluid intake or diabetes insipidus.
Which diagnostic test is commonly used to confirm the diagnosis of diabetes insipidus (DI) and distinguish between central and nephrogenic DI?
Explanation
The water deprivation test is commonly used to diagnose diabetes insipidus and differentiate between central and nephrogenic DI. During this test, the client is deprived of fluids while their urine output and concentration are monitored.
Incorrect choices:
a. This choice is incorrect. Blood glucose testing is used to diagnose diabetes mellitus, not diabetes insipidus.
b. This choice is incorrect. A serum electrolyte panel may provide information about electrolyte imbalances, but it is not the primary diagnostic test for diabetes insipidus.
c. This choice is incorrect. Urine osmolality may be measured as part of the diagnostic evaluation for diabetes insipidus, but it is not the primary diagnostic test.
Which laboratory finding is indicative of diabetes insipidus (DI)?
Explanation
In diabetes insipidus, the inability to concentrate urine leads to diluted urine with low osmolality. An elevated urine osmolality is indicative of the inability to properly conserve water.
Incorrect choices:
a. This choice is incorrect. Low blood glucose levels are not characteristic of diabetes insipidus.
c. This choice is incorrect. Hypernatremia, or elevated sodium levels, can result from excessive fluid loss in diabetes insipidus, but it is not a direct diagnostic indicator.
d. This choice is incorrect. High urine glucose levels are indicative of diabetes mellitus, not diabetes insipidus.
Which diagnostic test measures the concentration of antidiuretic hormone (ADH) in the blood and is used to differentiate between central and nephrogenic diabetes insipidus?
Explanation
The desmopressin stimulation test measures the response of the kidneys to synthetic ADH (desmopressin) and is used to differentiate between central and nephrogenic diabetes insipidus.
Incorrect choices:
a. This choice is incorrect. The glucose tolerance test is used to diagnose diabetes mellitus, not diabetes insipidus.
b. This choice is incorrect. A serum electrolyte panel provides information about electrolyte levels but is not specific to diabetes insipidus diagnosis.
c. This choice is incorrect. The water deprivation test, not the desmopressin stimulation test, is used to diagnose diabetes insipidus and assess the ability of the kidneys to concentrate urine.
Which diagnostic test involves administering a synthetic form of antidiuretic hormone (ADH) to assess the response of the kidneys and differentiate between central and nephrogenic diabetes insipidus?
Explanation
The desmopressin stimulation test involves administering synthetic ADH (desmopressin) to assess the response of the kidneys and differentiate between central and nephrogenic diabetes insipidus.
Incorrect choices:
a. This choice is incorrect. The glucose tolerance test is used to diagnose diabetes mellitus, not diabetes insipidus.
b. This choice is incorrect. A serum electrolyte panel provides information about electrolyte levels but is not specific to diabetes insipidus diagnosis.
c. This choice is incorrect. The water deprivation test, not the desmopressin stimulation test, is used to diagnose diabetes insipidus and assess the ability of the kidneys to concentrate urine.
Which diagnostic test measures the concentration of electrolytes, such as sodium and potassium, in the blood and may reveal abnormalities related to fluid and electrolyte balance in diabetes insipidus?
Explanation
A serum electrolyte panel measures the concentration of various electrolytes in the blood and can reveal abnormalities related to fluid and electrolyte balance, which may be present in diabetes insipidus.
Incorrect choices:
a. This choice is incorrect. The glucose tolerance test is used to diagnose diabetes mellitus, not diabetes insipidus.
c. This choice is incorrect. The water deprivation test is used to diagnose diabetes insipidus and assess the ability of the kidneys to concentrate urine.
d. This choice is incorrect. The desmopressin stimulation test involves administering synthetic ADH to differentiate between central and nephrogenic diabetes insipidus.
Which intervention is a key component of the management plan for a client with diabetes insipidus (DI)?
Explanation
Desmopressin (DDAVP) is a synthetic form of antidiuretic hormone (ADH) that is commonly used to manage diabetes insipidus by increasing water reabsorption in the kidneys and reducing urine output.
Incorrect choices:
a. This choice is incorrect. Limiting fluid intake to 500 mL per day is not a typical management approach for diabetes insipidus. Adequate fluid intake is necessary to prevent dehydration.
b. This choice is incorrect. Administering hypertonic saline solution is not a standard treatment for diabetes insipidus and may worsen fluid and electrolyte imbalances.
c. This choice is incorrect. Encouraging excessive fluid consumption is not a suitable approach for managing diabetes insipidus, as it can exacerbate fluid loss.
What is the primary goal of pharmacological therapy for diabetes insipidus (DI)?
Explanation
The primary goal of pharmacological therapy for diabetes insipidus is to prevent fluid overload and dehydration by restoring the balance of water and electrolytes through the administration of medications such as desmopressin.
Incorrect choices:
a. This choice is incorrect. The goal of pharmacological therapy for diabetes insipidus is to reduce excessive urine output, not increase it.
c. This choice is incorrect. Stimulating thirst sensation is not the primary goal of pharmacological therapy for diabetes insipidus.
d. This choice is incorrect. While maintaining electrolyte balance is important, preventing fluid overload and dehydration is the primary goal of treatment.
What dietary recommendation should the nurse provide to a client with diabetes insipidus (DI)?
Explanation
Clients with diabetes insipidus should maintain a balanced and adequate diet to ensure proper nutrition and hydration. While fluid intake may need to be monitored, severe fluid restriction is not typically necessary.
Incorrect choices:
a. This choice is incorrect. Avoiding all sources of dietary sodium is not a standard dietary recommendation for diabetes insipidus. Sodium balance is important for overall health.
b. This choice is incorrect. There is no specific indication for a high-protein diet in the management of diabetes insipidus.
c. This choice is incorrect. Limiting fluid intake to 1 liter per day may not be appropriate for all clients and should be based on individual needs and medical guidance.
Which instruction should the nurse include when educating a client with diabetes insipidus (DI) about the administration of desmopressin (DDAVP)?
Explanation
Desmopressin (DDAVP) is typically taken orally with a full glass of water to ensure proper absorption and effectiveness. It is important to maintain adequate hydration.
Incorrect choices:
b. This choice is incorrect. Desmopressin is commonly administered orally, intranasally, or subcutaneously, but not via intramuscular injection.
c. This choice is incorrect. Monitoring blood glucose levels is important for clients with diabetes mellitus, not diabetes insipidus.
d. This choice is incorrect. There is no specific indication to limit dietary fiber intake for clients with diabetes insipidus.
What is a potential adverse effect of desmopressin (DDAVP) therapy in the treatment of diabetes insipidus (DI)?
Explanation
Desmopressin (DDAVP) can lead to excessive water retention, which may dilute the blood and potentially cause hypoglycemia, especially in clients with diabetes mellitus.
Incorrect choices:
a. This choice is incorrect. Desmopressin therapy is not typically associated with hypertension.
c. This choice is incorrect. Hyperkalemia is not a common adverse effect of desmopressin therapy.
d. This choice is incorrect. While fluid retention is a potential effect of desmopressin therapy, it is not typically associated with adverse outcomes.
The nurse is assessing a client with suspected diabetes insipidus. Which clinical manifestation is consistent with this condition?
Explanation
Polyuria, or excessive urine output, is a hallmark clinical manifestation of diabetes insipidus. Clients with diabetes insipidus produce large volumes of dilute urine.
Incorrect choices:
a. This choice is incorrect. Polyphagia refers to excessive hunger and is not a characteristic symptom of diabetes insipidus.
c. This choice is incorrect. Polydipsia refers to excessive thirst and is often present in diabetes mellitus, not diabetes insipidus.
d. This choice is incorrect. Polydyspnea refers to difficulty breathing and is not associated with diabetes insipidus.
The nurse is caring for a client with diabetes insipidus. Which laboratory finding is consistent with this condition?
Explanation
Hypernatremia, or elevated sodium levels, is a common laboratory finding in clients with diabetes insipidus due to the excessive loss of water in urine.
Incorrect choices:
a. This choice is incorrect. Elevated urine specific gravity is not typically seen in diabetes insipidus; instead, urine specific gravity is often diluted.
c. This choice is incorrect. Low serum osmolality is not characteristic of diabetes insipidus, which is associated with concentrated serum.
d. This choice is incorrect. Hypouricemia refers to low levels of uric acid and is not directly related to diabetes insipidus.
Which diagnostic test is commonly used to differentiate between central and nephrogenic diabetes insipidus?
Explanation
The water deprivation test is commonly used to differentiate between central and nephrogenic diabetes insipidus. It involves withholding fluids and monitoring urine output and concentration.
Incorrect choices:
b. This choice is incorrect. A blood glucose test is used to diagnose and monitor diabetes mellitus, not diabetes insipidus.
c. This choice is incorrect. A thyroid function test is not directly related to the diagnosis of diabetes insipidus.
d. This choice is incorrect. A serum creatinine test assesses kidney function but is not specific to diabetes insipidus diagnosis.
The nurse is providing education to a client with diabetes insipidus. Which instruction should the nurse include?
Explanation
Desmopressin is a common medication used to manage diabetes insipidus by promoting water reabsorption in the kidneys. It is important for the client to take the medication as prescribed.
Incorrect choices:
a. This choice is incorrect. While fluid intake may need to be monitored, severe fluid restriction is not typically necessary for clients with diabetes insipidus.
b. This choice is incorrect. While reducing sodium intake may be beneficial for overall health, it is not a specific instruction for managing diabetes insipidus.
c. This choice is incorrect. Monitoring blood glucose levels is important for clients with diabetes mellitus, not diabetes insipidus.
The nurse is assessing a client with diabetes insipidus. Which intervention is appropriate for preventing complications in this client?
Explanation
Clients with diabetes insipidus may experience electrolyte imbalances, including hypernatremia and hyperkalemia. Monitoring serum potassium levels is important to prevent complications.
Incorrect choices:
a. This choice is incorrect. Administering diuretics is not appropriate for a client with diabetes insipidus, as they are already experiencing excessive fluid loss.
b. This choice is incorrect. While encouraging fluid intake is important, excessive fluid intake may exacerbate fluid loss in clients with diabetes insipidus.
d. This choice is incorrect. Antidiabetic medications are used to manage diabetes mellitus, not diabetes insipidus.
Diabetic Foot care
The nurse is providing education to a client with diabetes about foot care. Which statement by the client indicates a need for further teaching?
Explanation
The client's statement that wearing tight-fitting shoes is important for preventing friction is incorrect. Tight-fitting shoes can actually increase the risk of friction and pressure, leading to foot problems in individuals with diabetes. Properly fitting shoes with cushioning and support are recommended to prevent foot complications.
Incorrect choices:
a. This choice is incorrect. Daily foot inspection is a crucial aspect of diabetic foot care to detect any cuts, blisters, or changes in the skin.
c. This choice is incorrect. Washing the feet daily with mild soap and warm water is an important hygiene practice to prevent infection.
d. This choice is incorrect. Moisturizing the feet with lotion, while avoiding between the toes, helps prevent dry skin and cracking, which can lead to foot problems.
The nurse is educating a client with diabetes about the importance of proper footwear. Which type of footwear is most suitable for this client?
Explanation
Closed-toe shoes with cushioning and support are the most suitable footwear for a client with diabetes. These shoes provide protection, reduce friction, and help prevent foot complications.
Incorrect choices:
a. This choice is incorrect. High-heeled shoes can increase pressure on certain areas of the feet and may lead to discomfort and foot problems for individuals with diabetes.
b. This choice is incorrect. Tight-fitting shoes can lead to friction, pressure, and potential foot injuries in individuals with diabetes.
c. This choice is incorrect. Open-toed sandals do not provide adequate protection and support for the feet, which is essential for preventing foot complications.
The nurse is teaching a client with diabetes about how to trim their toenails. Which instruction should the nurse provide?
Explanation
Clients with diabetes should be instructed to trim their toenails straight across to prevent ingrown toenails and potential foot infections.
Incorrect choices:
b. This choice is incorrect. Trimming toenails in a curved shape can increase the risk of ingrown toenails and should be avoided.
c. This choice is incorrect. Trimming toenails too short can lead to cuts, infections, and other foot problems.
d. This choice is incorrect. Trimming toenails at a 90-degree angle is not recommended and may lead to ingrown toenails.
The nurse is discussing foot care with a client with diabetes. Which statement by the client indicates a good understanding of proper foot care?
Explanation
Wearing clean, dry socks and changing them daily helps prevent moisture buildup, which can lead to fungal infections and foot complications in clients with diabetes.
Incorrect choices:
a. This choice is incorrect. Soaking the feet in hot water can lead to dry skin and increased risk of injury. Warm water should be used for foot soaking.
b. This choice is incorrect. Over-the-counter callus removers can cause skin irritation and should be avoided. Clients with diabetes should not attempt to remove calluses at home.
c. This choice is incorrect. Using a mirror to inspect the soles of the feet is a recommended practice for clients who may have difficulty visualizing the bottoms of their feet.
The nurse is teaching a client with diabetes about the importance of blood flow to the feet. Which instruction should the nurse provide to promote adequate circulation?
Explanation
Wiggling toes and moving ankles regularly can help promote blood flow and prevent blood pooling in the feet, which is important for maintaining circulation in clients with diabetes.
Incorrect choices:
a. This choice is incorrect. Crossing legs when sitting can impede blood flow and should be avoided to prevent circulatory issues.
b. This choice is incorrect. Elevating the legs above heart level can reduce blood flow and is not recommended for individuals with diabetes.
c. This choice is incorrect. Vigorous foot massage may cause friction and potential harm to the feet, especially for individuals with diabetes who are at risk of developing foot ulcers.
The nurse is educating a client with diabetes about the importance of diabetic foot care. Which statement by the client indicates a good understanding of the importance of foot care?
Explanation
Diabetic foot care is essential to prevent serious complications such as foot ulcers and amputations, which can result from poor circulation and nerve damage in individuals with diabetes.
Incorrect choices:
a. This choice is incorrect. While wanting to have nice-looking feet is a valid concern, the primary focus of diabetic foot care is to prevent complications and ensure overall foot health.
c. This choice is incorrect. Foot care is necessary on a regular basis, not just when pain or discomfort is present, to prevent complications.
d. This choice is incorrect. Changes in skin color are only one aspect of diabetic foot care. Other factors, such as inspecting for cuts, blisters, and sores, are equally important.
The nurse is discussing diabetic foot care with a client. Which statement accurately reflects the importance of regular foot inspections?
Explanation
Regular foot inspections, done on a daily basis, help individuals with diabetes identify early signs of problems such as cuts, blisters, or changes in skin integrity. This enables timely intervention to prevent further complications.
Incorrect choices:
a. This choice is incorrect. While choosing comfortable footwear is important, the primary purpose of daily foot inspections is to identify and prevent complications, not fashion.
c. This choice is incorrect. Foot inspections should be performed routinely to prevent complications, rather than waiting for an infection or injury to develop.
d. This choice is incorrect. Weekly foot inspections may not provide timely detection of potential problems, as complications can arise rapidly in individuals with diabetes.
The nurse is teaching a client with diabetes about the significance of proper footwear. Which statement accurately describes the importance of appropriate footwear for diabetic foot care?
Explanation
Proper footwear is essential for protecting the feet from injury and pressure points that can lead to foot ulcers and complications in individuals with diabetes.
Incorrect choices:
a. This choice is incorrect. While proper fit is important, the type and quality of shoes also matter. Not all types of shoes are suitable for individuals with diabetes.
b. This choice is incorrect. While improved balance and coordination can be beneficial, the primary purpose of proper footwear in diabetes is to prevent foot injuries.
c. This choice is incorrect. Shoes with a snug fit can actually increase the risk of friction and pressure, which may lead to foot problems in individuals with diabetes.
The nurse is educating a client with diabetes about maintaining proper foot hygiene. Which statement accurately reflects the importance of this aspect of foot care?
Explanation
Proper foot hygiene, including keeping the feet clean and dry, is essential for preventing fungal infections and skin breakdown in individuals with diabetes.
Incorrect choices:
a. This choice is incorrect. While overall hygiene can contribute to a healthy immune response, foot hygiene is specifically important for preventing foot-related complications.
b. This choice is incorrect. Toenail color is not the primary focus of foot hygiene. The focus is on preventing infections and skin problems.
d. This choice is incorrect. Foot hygiene does not directly regulate blood glucose levels or prevent foot pain; its primary role is in preventing infections and complications.
The nurse is discussing the importance of regular foot care with a client with diabetes. Which statement accurately explains the rationale for daily foot care?
Explanation
Daily foot care is crucial to prevent foot complications and identify problems early, such as cuts, blisters, or changes in skin integrity, which can lead to serious complications in individuals with diabetes.
Incorrect choices:
a. This choice is incorrect. While daily foot care is important, its primary focus is on preventing foot complications, not weight loss or diabetes management.
c. This choice is incorrect. Foot care should be performed routinely, not just when numbness or tingling is experienced, to prevent complications.
d. This choice is incorrect. Waiting until a visible foot injury is noticed may lead to delayed intervention and increased risk of complications. Daily foot care is preventive in nature.
The nurse is conducting a foot assessment for a client with diabetes. Which action is a priority during the foot examination?
Explanation
Inspecting the skin for cuts, blisters, sores, and other abnormalities is a priority during a foot examination for a client with diabetes. Early detection of these issues can help prevent complications such as infections and ulcers.
Incorrect choices:
a. This choice is incorrect. While assessing toenail color is important, it is not the priority during a foot examination. Applying nail polish should be avoided due to the risk of hiding potential issues.
c. This choice is incorrect. Massaging the feet can be beneficial, but it is not the priority during a foot examination. The focus is on assessing for potential problems.
d. This choice is incorrect. While applying lotion to prevent dryness is important, lotion should not be applied between the toes, as it can create a moist environment that promotes fungal growth.
The nurse is assessing a client's foot as part of diabetic foot care. Which finding requires immediate intervention?
Explanation
An area of deep, blackened tissue indicates tissue necrosis and potential gangrene, which requires immediate intervention to prevent further complications and possible amputation.
Incorrect choices:
a. This choice is incorrect. Dry and slightly rough skin may require moisturizing but does not indicate an immediate need for intervention.
b. This choice is incorrect. Warmth and redness on the sole of the foot may indicate increased blood flow or irritation but does not necessarily require immediate intervention.
c. This choice is incorrect. A small, superficial blister can be addressed with appropriate wound care, but it does not require immediate intervention unless it shows signs of infection.
During a foot assessment, the nurse notices a red, warm, and swollen area on the client's foot. Which action should the nurse take next?
Explanation
A red, warm, and swollen area on the foot may indicate an infection or inflammation, which requires further evaluation and treatment by a healthcare provider.
Incorrect choices:
a. This choice is incorrect. Applying heat to an already warm and swollen area may exacerbate inflammation and should be avoided.
b. This choice is incorrect. While elevation and rest can be beneficial for certain foot conditions, they may not be sufficient for addressing infection or inflammation.
c. This choice is incorrect. Massaging the area may further irritate the inflamed tissues and is not recommended without proper assessment and guidance from a healthcare provider.
The nurse is performing a foot assessment for a client with diabetes. Which finding requires immediate intervention?
Explanation
An area of skin that is cracked and bleeding indicates a breakdown of the skin's integrity, which can lead to infection. Immediate intervention is needed to clean and protect the area.
Incorrect choices:
a. This choice is incorrect. A small callus may require intervention, but it does not necessarily require immediate attention unless it is causing discomfort or open sores.
b. This choice is incorrect. Slight discoloration of the toenails may be due to various factors and does not indicate an immediate need for intervention.
d. This choice is incorrect. Mild swelling of the ankle may require monitoring, but it does not necessarily indicate an immediate need for intervention unless it is accompanied by other concerning symptoms.
The nurse is assessing a client's foot for signs of poor circulation. Which finding is indicative of poor circulation?
Explanation
Absence of hair on the toes and feet is indicative of poor circulation, as reduced blood flow to the extremities can lead to decreased hair growth.
Incorrect choices:
a. This choice is incorrect. Capillary refill less than 2 seconds is a normal finding and indicates good circulation.
b. This choice is incorrect. Warm and pink skin temperature is a normal finding and indicates adequate blood flow.
d. This choice is incorrect. The presence of superficial veins does not necessarily indicate poor circulation and can vary among individuals.
The nurse is assessing a client's feet for neuropathy. Which finding is consistent with peripheral neuropathy?
Explanation
Loss of sensation to touch in the feet is consistent with peripheral neuropathy, a common complication of diabetes that affects nerve function.
Incorrect choices:
a. This choice is incorrect. Rapid capillary refill indicates good blood flow and is not directly related to neuropathy.
c. This choice is incorrect. The presence of abundant hair does not directly indicate neuropathy; rather, absence of hair may be more indicative of poor circulation.
d. This choice is incorrect. Normal skin temperature does not necessarily indicate the presence or absence of neuropathy.
The nurse is assessing a client's feet as part of diabetic foot care. Which finding requires further assessment and intervention?
Explanation
Redness and warmth on the sole of the foot may indicate inflammation or infection and require further assessment and intervention to prevent complications.
Incorrect choices:
a. This choice is incorrect. Mild dryness of the skin may require moisturizing but does not necessarily require immediate intervention.
b. This choice is incorrect. A small, superficial blister can be addressed with appropriate wound care and monitoring.
d. This choice is incorrect. Mild swelling of the ankles may require monitoring but does not necessarily indicate an immediate need for intervention.
During a foot assessment, the nurse observes an area of skin that is discolored, darkened, and slightly raised. The client reports that the area has been present for several weeks. What action should the nurse take?
Explanation
An area of discolored, darkened, and slightly raised skin that has been present for several weeks may indicate a potential skin condition or complication that requires further evaluation and treatment by a healthcare provider.
Incorrect choices:
a. This choice is incorrect. Applying an antibiotic ointment without a proper diagnosis may not address the underlying issue.
b. This choice is incorrect. The described findings are not consistent with a normal skin variation and require further assessment.
c. This choice is incorrect. While keeping the area dry and clean is important, it may not be sufficient to address the underlying issue.
The nurse is assessing a client's feet for signs of infection as part of diabetic foot care. Which finding suggests a possible infection?
Explanation
Pain and tenderness at the base of the toes may suggest an infection, and further assessment and intervention are needed to prevent complications.
Incorrect choices:
a. This choice is incorrect. Calluses are areas of thickened skin and do not necessarily indicate an infection.
b. This choice is incorrect. Dry and flaky skin may require moisturizing but does not necessarily indicate an infection.
d. This choice is incorrect. Mild swelling of the ankles may require monitoring but does not necessarily indicate an infection.
The nurse is assessing a client's feet for potential complications of diabetes. Which finding requires immediate intervention?
Explanation
A small, non-painful ulcer on the sole of the foot may indicate tissue breakdown and the potential for infection, requiring immediate intervention.
Incorrect choices:
a. This choice is incorrect. Dry skin with small cracks may require moisturizing and care, but it does not necessarily require immediate intervention.
b. This choice is incorrect. A callus on the side of the foot may require attention, but it does not necessarily require immediate intervention unless it is causing discomfort or open sores.
d. This choice is incorrect. Swelling and redness of the toes may indicate various issues and may not necessarily require immediate intervention unless accompanied by other concerning symptoms.
The nurse is providing education to a client with diabetes about nail care. Which statement by the client indicates a need for further teaching?
Explanation
Applying petroleum jelly between the toes can create a moist environment and increase the risk of fungal infections. It is important to keep the feet clean and dry to prevent complications.
Incorrect choices:
a. This choice is correct. Trimming toenails straight across and avoiding cutting the corners is the correct technique to prevent ingrown nails and potential complications.
b. This choice is correct. Using a magnifying glass can help improve visibility and accuracy while trimming nails, reducing the risk of injury.
d. This choice is correct. Wearing closed-toe shoes that fit well is important to protect the feet from potential injuries and complications.
The nurse is teaching a client with diabetes about foot care. Which statement by the client indicates a need for further education?
Explanation
Popping a blister with a sterile needle increases the risk of infection and complications. It is important to avoid popping blisters and to properly care for them to prevent infection.
Incorrect choices:
a. This choice is correct. Daily foot inspection, especially between the toes, is an important part of foot care for clients with diabetes to detect any abnormalities or issues.
c. This choice is correct. Washing the feet daily with mild soap and warm water helps maintain hygiene and prevent infections.
d. This choice is correct. Gently patting the feet dry, especially between the toes, helps prevent moisture buildup and reduces the risk of fungal infections.
The nurse is educating a client with diabetes about proper footwear. Which statement by the client indicates understanding of the teaching?
Explanation
Proper footwear for clients with diabetes includes shoes with cushioning, good arch support, and adequate room for the toes to prevent pressure points and potential complications.
Incorrect choices:
a. This choice is correct. Shoes with pointed toes can compress the toes and increase the risk of pressure points, ulcers, and other foot issues.
b. This choice is correct. Open-toe shoes and sandals do not provide adequate protection for the feet and may increase the risk of injuries.
c. This choice is correct. Tight shoes can lead to pressure points, reduced circulation, and potential foot complications. Comfort and fit are more important than appearance.
The nurse is providing education to a client with diabetes about moisturizing the feet. Which statement by the client indicates understanding of proper moisturizing techniques?
Explanation
Applying lotion between the toes can create a moist environment and increase the risk of fungal infections. It is important to keep the feet clean and dry, especially between the toes.
Incorrect choices:
b. This choice is correct. Soaking the feet in hot water can lead to excessive dryness and skin damage. Warm water is preferable for foot soaking.
c. This choice is correct. Alcohol-based products can strip the skin of natural oils and cause dryness. Mild soap and water are recommended for cleaning the feet.
d. This choice is correct. Vigorous rubbing motions during lotion application can damage the skin and lead to irritation. Gentle massaging is preferred.
The nurse is teaching a client with diabetes about the importance of avoiding tight socks or stockings. Which information should the nurse include in the teaching?
Explanation
Tight socks and stockings can constrict blood flow and lead to pressure points, reduced circulation, and potential foot complications.
Incorrect choices:
a. This choice is correct. Tight socks and stockings can actually impede circulation to the feet, increasing the risk of complications.
b. This choice is correct. While tight socks and stockings may temporarily prevent swelling, they can lead to more significant issues such as pressure ulcers and compromised circulation.
d. This choice is correct. Tight socks and stockings can force the feet into unnatural positions, increasing the risk of pressure points and deformities. Proper foot alignment is achieved through well-fitting footwear with good arch support.
The nurse is teaching a client with diabetes about preventing injuries to the feet. Which statement by the client indicates a need for further education?
Explanation
Using a heating pad to warm the feet can increase the risk of burns and damage to the skin. It is recommended to wear warm socks and appropriate footwear to keep the feet warm.
Incorrect choices:
a. This choice is correct. Inspecting shoes for foreign objects or rough areas before wearing them helps prevent injuries and irritation to the feet.
b. This choice is correct. Walking barefoot, even indoors, increases the risk of injuries, cuts, and infections. Proper footwear should be worn at all times.
c. This choice is correct. Trimming toenails straight across helps prevent ingrown nails, reducing the risk of complications.
The nurse is educating a client with diabetes about preventing injuries to the feet. Which activity should the client avoid?
Explanation
Walking barefoot on the beach exposes the feet to potential injuries from sharp objects, hot sand, and direct sunlight. Proper footwear should be worn to prevent such injuries.
Incorrect choices:
a. This choice is correct. Checking bathwater temperature with the elbow before immersing the feet helps prevent burns and injuries from hot water.
c. This choice is correct. Using adhesive tape to secure dressings on the feet can help protect wounds and prevent infections.
d. This choice is correct. Applying lotion to the feet before bedtime helps prevent dryness and maintain skin integrity.
The nurse is discussing strategies to prevent foot injuries with a client who has diabetes. Which statement by the client indicates a need for further education?
Explanation
Avoiding leg crossing does not directly relate to preventing foot injuries. It is important to focus on wearing proper footwear, maintaining foot hygiene, and checking for signs of injury.
Incorrect choices:
b. This choice is correct. Wearing clean, dry socks and changing them daily helps prevent moisture buildup and reduces the risk of infections.
c. This choice is correct. Using a pumice stone to gently remove calluses helps prevent excessive skin thickening and pressure points.
d. This choice is correct. Using a mirror to inspect the bottom of the feet helps detect any changes or abnormalities that may not be visible directly.
The nurse is teaching a client with diabetes about preventing foot injuries. Which activity should the client avoid?
Explanation
Wearing shoes with pointed toes can compress the toes and increase the risk of pressure points, ulcers, and other foot issues.
Incorrect choices:
b. This choice is correct. Keeping the feet elevated for extended periods can reduce swelling and improve circulation.
c. This choice is correct. Using a foot roller to massage the soles of the feet can promote circulation and reduce tension.
d. This choice is correct. Applying moisturizer between the toes is not recommended as it can create a moist environment and increase the risk of fungal infections.
The nurse is providing education to a client with diabetes about preventing foot injuries. Which action should the client prioritize?
Explanation
Wearing closed-toe shoes with proper arch support helps protect the feet from injuries, pressure points, and potential complications.
Incorrect choices:
a. This choice is correct. Applying a heating pad to the feet before bedtime can increase the risk of burns and skin damage.
b. This choice is correct. Loose-fitting socks and shoes can lead to friction and blisters, increasing the risk of injuries.
d. This choice is correct. Soaking the feet in hot water can lead to dryness and potential skin damage. Warm water is preferable for foot soaking.
The nurse is providing education to a client with a diabetic foot ulcer about wound care and infection prevention. Which statement by the client indicates effective understanding of wound management?
Explanation
Regular daily inspections of the feet for signs of infection are crucial in preventing complications related to diabetic foot ulcers. Increased redness, swelling, warmth, and foul odor may indicate infection and should be reported to a healthcare provider.
Incorrect choices:
a. This choice is incorrect. Using hot water can damage the delicate tissue of the ulcer and increase the risk of infection. Lukewarm water is recommended for cleansing.
b. This choice is incorrect. Keeping the ulcer uncovered can expose it to dirt, bacteria, and the risk of further injury. Proper dressing and wound coverage are essential for wound healing.
d. This choice is incorrect. Soaking the feet in Epsom salt water is not recommended for diabetic foot ulcers, as it can cause drying and may delay wound healing.
The nurse is instructing a client with a diabetic foot ulcer on the importance of controlling blood sugar levels. Which statement by the client indicates effective management of foot ulcers?
Explanation
Consistently following the healthcare provider's instructions for insulin and medication management is essential in controlling blood sugar levels and promoting wound healing in clients with diabetic foot ulcers.
Incorrect choices:
a. This choice is incorrect. Taking diabetes medication inconsistently can lead to fluctuations in blood sugar levels and hinder wound healing.
b. This choice is incorrect. Checking blood sugar levels once a week is not sufficient for effective diabetes management, especially for individuals with diabetic foot ulcers.
d. This choice is incorrect. Skipping meals can lead to unstable blood sugar levels and negatively impact wound healing and overall health.
The nurse is teaching a client with a diabetic foot ulcer about footwear. Which statement by the client indicates a need for further education?
Explanation
Tight-fitting socks can restrict blood flow and increase the risk of friction and pressure on the feet, leading to complications. Loose-fitting socks made of moisture-wicking material are recommended.
Incorrect choices:
a. This choice is correct. Choosing shoes with a wide toe box helps prevent pressure on the toes and reduces the risk of developing foot ulcers.
b. This choice is correct. Checking the inside of shoes for objects or rough spots is important to prevent injuries and friction that can lead to foot ulcers.
d. This choice is correct. Wearing sandals or open-toed shoes increases the risk of injury and exposure to debris, making closed-toe shoes a safer choice for foot protection.
The nurse is educating a client with a diabetic foot ulcer about proper wound dressing. Which statement by the client indicates understanding of wound management?
Explanation
Cleaning the ulcer with an antiseptic solution before applying the dressing helps prevent infection and promotes a healthy wound healing environment.
Incorrect choices:
a. This choice is incorrect. Applying petroleum jelly to the ulcer can trap moisture and hinder wound healing.
b. This choice is incorrect. Using adhesive tape directly on the wound can disrupt the wound bed and hinder healing.
c. This choice is incorrect. Changing the dressing every other day may be too frequent and can disrupt the wound healing process. Dressing change frequency should be determined by the healthcare provider based on the wound's condition.
The nurse is providing education to a client with a diabetic foot ulcer about the importance of staying hydrated. Which statement by the client indicates effective understanding of hydration?
Explanation
Adequate hydration is important for overall health and wound healing. Drinking plenty of water helps improve blood circulation and supports the body's healing processes.
Incorrect choices:
a. This choice is incorrect. Limiting fluid intake to prevent frequent urination can lead to dehydration and hinder wound healing.
c. This choice is incorrect. Consuming sugary beverages can negatively impact blood sugar levels and overall health, potentially hindering wound healing.
d. This choice is incorrect. Avoiding fluids before bedtime can increase the risk of dehydration and may not have a significant impact on nighttime urination. Staying hydrated is more important for wound healing.
The nurse is educating a client with diabetes about proper foot care. Which statement by the client indicates understanding of diabetic foot care?
Explanation
Daily foot inspections are crucial for detecting any cuts, blisters, sores, or changes in the skin. Early detection and prompt treatment of any foot issues can prevent complications.
Incorrect choices:
a. This choice is incorrect. Soaking feet in hot water can lead to dryness and skin damage, increasing the risk of foot complications.
c. This choice is incorrect. Trimming toenails with pointed scissors can lead to injuries and cuts. Using proper nail clippers and trimming straight across is recommended.
d. This choice is incorrect. Using adhesive tape directly on wounds can disrupt the wound healing process and increase the risk of infection.
The nurse is discussing proper footwear with a client who has diabetes. Which statement by the client indicates a need for further education?
Explanation
New shoes should be gradually broken in to prevent friction and blisters. Wearing new shoes for long periods of time can lead to discomfort and foot injuries.
Incorrect choices:
a. This choice is correct. Choosing shoes with a wide toe box helps prevent pressure on the toes and reduces the risk of developing foot ulcers.
c. This choice is correct. Shaking out shoes before putting them on helps remove any debris that could cause discomfort or injury to the feet.
d. This choice is correct. Wearing moisture-wicking socks helps keep the feet dry and reduces the risk of moisture-related skin issues.
The nurse is teaching a client with diabetes about proper toenail care. Which statement by the client indicates effective understanding of toenail care?
Explanation
Cutting toenails straight across and avoiding cutting the corners helps prevent ingrown toenails and reduces the risk of injury and infection.
Incorrect choices:
a. This choice is incorrect. Cutting toenails at an angle can lead to ingrown toenails and increase the risk of injury.
b. This choice is incorrect. Filing toenails in a rounded shape can create sharp edges and increase the risk of ingrown toenails.
d. This choice is incorrect. Soaking feet in warm water before trimming toenails can lead to excessive moisture and increase the risk of infection.
The nurse is providing education to a client with diabetes about moisturizing the feet. Which statement by the client indicates effective understanding of foot moisturizing?
Explanation
Applying moisturizer to the tops and bottoms of the feet helps prevent dryness and cracking. However, moisturizer should be avoided between the toes to prevent excess moisture buildup and the risk of fungal infections.
Incorrect choices:
a. This choice is incorrect. Applying moisturizer between the toes can lead to excess moisture and increase the risk of fungal infections.
b. This choice is incorrect. Petroleum jelly may not be the best choice for preventing calluses, and it should not be used between the toes.
c. This choice is incorrect. Moisturizers with fragrances and alcohol can dry out the skin and cause irritation, which is not recommended for individuals with diabetes.
The nurse is educating a client with diabetes about the importance of proper blood sugar control for foot health. Which statement by the client indicates understanding of the relationship between blood sugar control and foot care?
Explanation
High blood sugar levels can weaken the immune system and increase the risk of infections, including fungal infections, in the feet.
Incorrect choices:
b. This choice is incorrect. Low blood sugar levels do not directly lead to calluses and corns on the feet. Proper footwear and foot care are more relevant to preventing calluses and corns.
c. This choice is incorrect. Blood sugar control has a significant impact on foot health. Poorly controlled blood sugar levels can lead to nerve damage, poor circulation, and delayed wound healing, all of which affect foot health.
d. This choice is incorrect. Checking blood sugar levels only when experiencing foot pain may not provide timely information about blood sugar control and foot health. Regular monitoring of blood sugar levels is important for overall diabetes management.
The nurse is educating a client with diabetes about foot care. Which statement by the client indicates a need for further education?
Explanation
Tight-fitting shoes can lead to friction, pressure, and poor circulation, increasing the risk of foot ulcers and complications for individuals with diabetes. Proper-fitting shoes are essential for foot care.
Incorrect choices:
a. This choice is correct. Washing feet daily using warm water and mild soap helps maintain hygiene and prevent infections.
b. This choice is correct. Applying lotion between the toes should be avoided to prevent moisture buildup, which can lead to fungal infections.
c. This choice is correct. Trimming toenails straight across and filing sharp edges helps prevent ingrown toenails and injuries.
The nurse is instructing a client with diabetes on how to perform a self-foot assessment. Which statement by the client indicates effective understanding of the assessment technique?
Explanation
Using a mirror to inspect the soles of the feet allows for a thorough assessment of hard-to-see areas and early detection of any abnormalities.
Incorrect choices:
b. This choice is incorrect. Regular daily foot assessments are recommended to detect any issues early and prevent complications.
c. This choice is incorrect. Performing the foot assessment when feet are most swollen may make it more difficult to identify abnormalities.
d. This choice is incorrect. Pressing feet against a hard surface is not a standard technique for assessing foot health.
The nurse is teaching a client with diabetes about the importance of proper footwear. Which statement by the client indicates effective understanding of footwear choices?
Explanation
Shoes with closed-toes and a wide toe box provide protection, support, and ample space for toes, reducing the risk of pressure, friction, and ulcers for individuals with diabetes.
Incorrect choices:
a. This choice is incorrect. Tight-fitting shoes can lead to pressure and friction, increasing the risk of foot ulcers and complications.
b. This choice is incorrect. Wearing socks is recommended to prevent friction and moisture buildup, reducing the risk of fungal infections.
d. This choice is incorrect. High-heeled shoes can alter foot mechanics, increase pressure, and negatively impact blood circulation, posing risks for individuals with diabetes.
The nurse is educating a client with diabetes about nail care. Which statement by the client indicates effective understanding of nail care practices?
Explanation
Trimming toenails straight across and slightly longer at the corners helps prevent ingrown toenails and potential injuries for individuals with diabetes.
Incorrect choices:
a. This choice is incorrect. Using pointed objects to clean under toenails can lead to injury and damage to the nail bed.
c. This choice is incorrect. Soaking feet in hot water can increase the risk of skin breakdown and should be avoided.
d. This choice is incorrect. Cutting toenails in a curved shape can increase the risk of ingrown toenails and complications.
The nurse is discussing proper foot hygiene with a client who has diabetes. Which statement by the client indicates a need for further education?
Explanation
Applying lotion between the toes can lead to moisture buildup, creating an environment favorable for fungal infections. It is recommended to avoid applying lotion between the toes.
Incorrect choices:
a. This choice is correct. Walking barefoot increases the risk of injury and exposure to potential hazards, making proper footwear essential.
b. This choice is correct. Washing feet daily using mild soap and warm water helps maintain hygiene and prevent infections.
c. This choice is correct. Gently patting feet dry, especially between the toes, helps prevent moisture buildup and reduces the risk of fungal infections.
Insulin therapy
What is the primary purpose of insulin therapy?
Explanation
To regulate blood glucose levels. Insulin therapy is used to help individuals with diabetes regulate their blood glucose levels by supplementing or replacing the insulin their body is not producing or using effectively.
Incorrect choices:
a. Insulin therapy does not cure diabetes but helps manage blood glucose levels.
b. Insulin therapy can lead to weight gain in some individuals due to improved glucose utilization, but its primary purpose is to regulate blood glucose.
c. Insulin therapy aims to decrease blood glucose levels, not increase them.
Which type of diabetes typically requires insulin therapy?
Explanation
Insulin therapy is a critical component of treatment for individuals with type 1 diabetes, as their pancreas does not produce insulin.
Incorrect choices:
b. Type 2 diabetes may initially be managed with oral medications, diet, and exercise, and insulin therapy might be added later if other treatments are not effective.
c. Gestational diabetes usually involves dietary changes and monitoring blood glucose levels. Insulin therapy may be necessary in some cases, but it is not typically the first-line treatment.
d. Pre-diabetes indicates higher-than-normal blood glucose levels, but insulin therapy is not usually required at this stage.
How is insulin administered?
Explanation
Subcutaneously. Insulin is typically administered through subcutaneous injections, allowing it to be absorbed into the bloodstream from fatty tissue under the skin.
Incorrect choices:
a. Insulin is a protein and would be broken down in the digestive system if taken orally.
b. Intravenous administration is not commonly used for insulin therapy due to the rapid onset of action and risk of hypoglycemia.
d. Intramuscular administration is not common for insulin therapy because absorption may be unpredictable and could lead to variability in blood glucose control.
What is the purpose of insulin therapy in diabetes management?
Explanation
The correct answer is d. To replace or supplement insulin in the body. Insulin therapy aims to provide the body with the insulin it needs when the natural production is insufficient.
Incorrect choices:
a. Insulin therapy does not stimulate the pancreas to produce more insulin; it directly provides insulin from an external source.
b. Insulin therapy does not target insulin resistance in muscle cells but provides the missing insulin.
c. Insulin therapy does not aim to increase glucose production by the liver; instead, it helps regulate glucose utilization and storage.
Which individuals are candidates for insulin therapy?
Explanation
Those with type 1 diabetes and some with type 2 diabetes. Individuals with type 1 diabetes require insulin therapy, and some individuals with type 2 diabetes may need insulin if other treatments are not effective.
Incorrect choices:
a. Individuals with normal blood glucose levels do not require insulin therapy.
b. Allergies to insulin are extremely rare, and insulin therapy can still be considered after careful evaluation.
d. Insulin therapy may be considered for gestational diabetes if blood glucose levels are not well-controlled with diet and exercise, but it is not the first-line treatment.
Which type of insulin has the fastest onset of action?
Explanation
Rapid-acting insulin has a rapid onset of action, typically within 15 minutes, making it suitable for controlling post-meal blood glucose spikes.
Incorrect choices:
b. Short-acting insulin has a slightly slower onset than rapid-acting insulin.
c. Intermediate-acting insulin has a slower onset and a longer duration of action than rapid-acting insulin.
d. Long-acting insulin has a slow and steady onset of action over a longer period compared to rapid-acting insulin.
Which type of insulin is also known as "basal insulin"?
Explanation
Long-acting insulin provides a steady baseline level of insulin, mimicking the body's basal insulin secretion.
Incorrect choices:
a. Rapid-acting insulin is used to control post-meal glucose spikes.
b. Short-acting insulin is used to cover mealtime glucose elevations.
c. Intermediate-acting insulin provides coverage beyond mealtime but does not mimic basal insulin as closely as long-acting insulin.
Which type of insulin is commonly used in insulin pumps?
Explanation
Rapid-acting insulin is often used in insulin pumps due to its fast onset of action and short duration, allowing for precise control of basal and bolus insulin needs.
Incorrect choices:
b. Short-acting insulin can also be used in insulin pumps but may not provide as flexible dosing options as rapid-acting insulin.
c. Intermediate-acting insulin has a longer duration and may not be ideal for the dynamic dosing required in insulin pumps.
d. Long-acting insulin's slow onset and steady release make it less suitable for insulin pump therapy.
Which type of insulin is cloudy in appearance?
Explanation
Intermediate-acting insulin appears cloudy due to its composition and requires proper mixing before administration.
Incorrect choices:
a. Rapid-acting insulin is clear in appearance.
b. Short-acting insulin is clear in appearance.
d. Long-acting insulin is clear in appearance.
Which type of insulin can be used to cover meals and snacks?
Explanation
Rapid-acting insulin is used to control post-meal blood glucose elevations and can be taken to cover meals and snacks.
Incorrect choices:
b. Short-acting insulin can also cover meals and snacks, but it may not be as rapid-acting as the name suggests.
c. Intermediate-acting insulin provides coverage beyond mealtime and is not specifically designed for mealtime glucose control.
d. Long-acting insulin provides a steady baseline and is not intended for mealtime coverage.
Which insulin administration route has the slowest onset of action?
Explanation
Subcutaneous injection has a slower onset of action compared to IV infusion and is the most common route for insulin administration.
Incorrect choices:
a. IM injection is not a common route for insulin administration and has a slower onset than subcutaneous injection.
c. IV infusion provides a rapid onset of action, making it inappropriate for routine insulin administration.
d. Inhalation is not a typical route for insulin administration. It is used for specific types of medications, not insulin.
What is the recommended technique for insulin injection?
Explanation
Pinch the skin and insert the needle at a 45-degree angle. This technique helps ensure proper subcutaneous injection and absorption of insulin.
Incorrect choices:
a. Inserting the needle at a 90-degree angle may result in intramuscular injection, leading to rapid absorption and potential hypoglycemia.
c. Inserting the needle at a 30-degree angle may result in shallow injection and inadequate insulin absorption.
d. Pressing the needle against the skin and releasing quickly may result in the medication leaking out of the injection site.
Which site is commonly used for insulin injection in children?
Explanation
The abdomen is a common site for insulin injection in children due to its larger subcutaneous tissue area and ease of access.
Incorrect choices:
a. The upper arm is not typically recommended for insulin injection due to limited subcutaneous tissue and potential discomfort.
c. The thigh is also a suitable site for insulin injection, but the abdomen is often preferred in children.
d. The buttock is not commonly used for insulin injection due to difficulties in self-administration and limited visibility.
How should insulin vials be stored?
Explanation
Store insulin vials at room temperature away from direct sunlight. Refrigeration is generally not necessary for most insulin types when in use, and freezing or exposure to high temperatures can damage insulin.
Incorrect choices:
a. Freezing insulin can alter its efficacy and should be avoided.
c. Insulin stored in the refrigerator should not be warmed before injection, as this can lead to temperature-related degradation.
d. Storing insulin in a hot environment can lead to degradation and loss of effectiveness.
When drawing up insulin from two different vials (e.g., rapid-acting and intermediate-acting insulin), which type of insulin should be drawn up first?
Explanation
Drawing up rapid-acting insulin before intermediate-acting insulin prevents contamination of the rapid-acting insulin vial with the longer-acting insulin.
Incorrect choices:
b. Drawing up intermediate-acting insulin first can contaminate the vial with rapid-acting insulin, potentially altering dosing accuracy.
c. The order in which insulin is drawn up does matter to prevent contamination.
d. Regular insulin is not commonly used for injection in routine insulin therapy.
A client with type 2 diabetes is prescribed insulin therapy. Which of the following statements is correct regarding basal insulin dosing?
Explanation
Basal insulin is typically administered once or twice daily to mimic the body's basal insulin secretion and maintain stable blood glucose levels between meals and overnight.
Incorrect choices:
a. Basal insulin is not administered before meals; it is intended to regulate fasting glucose levels.
b. Basal insulin does not cover carbohydrates consumed in meals; it targets basal glucose levels.
c. Rapid-acting insulin is not synonymous with basal insulin; they serve different purposes in insulin therapy.
A client is transitioning from an insulin pump to multiple daily injections. Which of the following statements about mealtime insulin dosing is accurate?
Explanation
Mealtime insulin is rapid-acting or short-acting insulin administered before or after meals to control postprandial glucose levels.
Incorrect choices:
a. Mealtime insulin is usually administered multiple times a day, not as a single daily injection.
b. Mealtime insulin is not typically a long-acting insulin; it is rapid-acting or short-acting insulin.
d. Mealtime insulin is administered before or after each meal, not only for the evening meal.
A nurse is teaching a client about self-administering insulin. The client asks, "Where is the best site to inject insulin?" Which response is correct?
Explanation
Rotating injection sites within the same anatomical area (e.g., abdomen, thigh) helps prevent lipohypertrophy and ensures consistent insulin absorption.
Incorrect choices:
a. Injecting into the same site each time can lead to lipohypertrophy and uneven insulin absorption.
c. While the abdomen is a common injection site, rotating within the same area is essential to prevent tissue damage.
d. Insulin absorption rates are similar across different anatomical sites, so there is no "fastest" absorption site.
A client is prescribed insulin therapy and is experiencing hypoglycemia. The nurse prepares to administer glucagon. How should the nurse explain the dosing of glucagon?
Explanation
Glucagon is administered as an injection, usually subcutaneously or intramuscularly, to rapidly raise blood glucose levels during severe hypoglycemia.
Incorrect choices:
a. Glucagon is administered differently from insulin injections and is intended for emergency use during severe hypoglycemia.
b. Glucagon is not available in oral tablet form due to its protein nature, which would be broken down in the digestive system.
d. Glucagon is not typically administered intravenously but rather through subcutaneous or intramuscular injection for rapid action.
A client with type 1 diabetes is prescribed an insulin-to-carbohydrate ratio (ICR) of 1:10. How should the nurse explain this dosing to the client?
Explanation
An insulin-to-carbohydrate ratio (ICR) of 1:10 means that for every 1 unit of insulin, the client should consume 10 grams of carbohydrates to help manage postprandial glucose levels.
Incorrect choices:
b. Injecting 10 units of insulin for every 1 gram of carbohydrates would result in excessive insulin dosing and potential hypoglycemia.
c. Consuming 10 units of insulin for every 1 unit of carbohydrates would lead to excessive insulin administration and hypoglycemia.
d. Injecting 1 unit of insulin for every 10 grams of carbohydrates would result in insufficient insulin dosing and potentially high blood glucose levels.
A client with type 2 diabetes has been on insulin therapy for several months. The client reports frequent episodes of hypoglycemia. Which action by the nurse is appropriate for monitoring and adjusting insulin therapy?
Explanation
Frequent hypoglycemic episodes indicate the need for a possible adjustment in insulin therapy. The nurse should work with the healthcare provider to modify the insulin regimen to better match the client's needs.
Incorrect choices:
a. Increasing the insulin dose without healthcare provider guidance may lead to further hypoglycemia and potential harm.
b. Consuming more carbohydrates may provide temporary relief from hypoglycemia but does not address the underlying insulin dosing issue.
d. Skipping meals can lead to unstable blood glucose levels and is not a recommended approach to managing insulin therapy.
A client on insulin therapy has been consistently experiencing elevated fasting blood glucose levels. What should the nurse do to monitor and adjust the client's insulin regimen?
Explanation
Fasting hyperglycemia suggests insufficient basal insulin coverage. Adjusting the basal insulin dose can help stabilize fasting blood glucose levels.
Incorrect choices:
a. Administering rapid-acting insulin after meals targets postprandial glucose levels, not fasting hyperglycemia.
c. Skipping meals is not a recommended approach and may lead to further blood glucose imbalances.
d. Decreasing insulin doses may worsen hyperglycemia and is not appropriate without healthcare provider guidance.
A client with type 1 diabetes is experiencing variability in blood glucose levels throughout the day. What should the nurse teach the client about monitoring and adjusting insulin therapy?
Explanation
Monitoring blood glucose levels regularly and adjusting insulin doses based on patterns and carbohydrate intake helps maintain stable blood glucose levels.
Incorrect choices:
a. Administering the same insulin dose regardless of carbohydrate content can lead to inconsistent blood glucose control.
b. Monitoring blood glucose levels only once daily does not provide enough information for effective insulin dosing adjustments.
d. The described approach involves using insulin types inappropriately for their intended purposes.
A client on insulin therapy is planning to engage in increased physical activity. How should the nurse advise the client about monitoring and adjusting insulin therapy?
Explanation
Increased physical activity can affect blood glucose levels, and the client should monitor levels more frequently and adjust insulin doses to maintain glucose control.
Incorrect choices:
a. Decreasing insulin doses without proper monitoring can lead to hypoglycemia during or after physical activity.
b. Skipping insulin doses can result in elevated blood glucose levels and is not recommended.
d. Administering extra insulin doses without monitoring blood glucose levels can lead to unpredictable outcomes and potential harm.
A client with diabetes is scheduled for surgery and will be fasting before the procedure. How should the nurse instruct the client about monitoring and adjusting insulin therapy on the day of surgery?
Explanation
Continue with the regular insulin regimen as usual. It is important for the client to maintain blood glucose control even on the day of surgery. The nurse should advise the client to follow the regular insulin regimen unless otherwise instructed by the healthcare provider.
Incorrect choices:
b. Skipping insulin doses can lead to hyperglycemia and unstable blood glucose levels, especially during fasting.
c. Decreasing the insulin dose without appropriate guidance can result in poor blood glucose control.
d. Stopping insulin therapy abruptly can lead to hyperglycemia and potential complications. Insulin adjustments should be made under healthcare provider supervision.
A client with diabetes is asking about storing insulin. Which statement by the client indicates a need for further education about insulin storage and handling?
Explanation
Insulin should be protected from extreme temperatures, including direct sunlight. Freezing or exposing insulin to high temperatures can alter its effectiveness.
Incorrect choices:
a. Storing insulin in the refrigerator is the correct way to maintain its effectiveness.
b. Gently rolling the insulin vial before use helps mix the solution but does not pertain to storage.
c. Checking the expiration date before using insulin is an important step to ensure its safety and effectiveness.
A nurse is teaching a client about storing insulin pens. Which statement by the client indicates a correct understanding of insulin pen storage and handling?
Explanation
Insulin pens should be stored at room temperature and protected from direct sunlight. Extreme temperatures can affect insulin's effectiveness.
Incorrect choices:
a. Storing insulin pens in the glove compartment of a car exposes them to temperature fluctuations and extreme heat, which can impact their potency.
b. While an insulated cooler bag can help protect insulin during travel, insulin pens should not be stored in extreme cold.
d. Placing insulin pens in the freezer is not recommended as it can alter the medication's properties and affect its effectiveness.
A client with diabetes is going on a vacation and asks the nurse about storing insulin while traveling. Which response by the nurse is accurate regarding insulin storage and handling during travel?
Explanation
Insulin should be stored at room temperature and protected from extreme temperatures during travel to maintain its effectiveness.
Incorrect choices:
a. Leaving insulin vials on the car dashboard exposes them to heat and temperature fluctuations, which can impact their potency.
b. Storing insulin in the overhead compartment of an airplane may subject it to extreme cold or heat, affecting its effectiveness.
d. Freezing insulin is not recommended, as it can alter the medication's properties and impact its efficacy.
A client is concerned about traveling with insulin and asks the nurse if there are any specific storage recommendations. Which information should the nurse provide regarding insulin storage during travel?
Explanation
Storing insulin in a cool place, such as a mini-fridge in a hotel room, helps maintain its effectiveness while traveling.
Incorrect choices:
a. Storing insulin in checked baggage on an airplane can expose it to temperature fluctuations and extreme conditions that may affect its potency.
c. Storing insulin next to electronic devices may subject it to heat, which can impact its effectiveness.
d. Storing insulin in the glove compartment of a car during sightseeing can expose it to temperature fluctuations and extreme heat, affecting its potency.
. A client is worried about maintaining the effectiveness of insulin during hot summer months. What guidance should the nurse provide to the client regarding insulin storage and handling in warm weather?
Explanation
Storing insulin in a cooler bag with ice packs can help maintain its temperature and effectiveness during hot weather.
Incorrect choices:
a. Storing insulin in the freezer is not recommended, as it can alter the medication's properties and impact its efficacy.
c. Storing insulin in direct sunlight can expose it to extreme temperatures and affect its potency.
d. Leaving insulin in a parked car, even with cracked windows, exposes it to temperature fluctuations and extreme heat, which can impact its effectiveness.
A nurse is teaching a client with diabetes about hypoglycemia management. Which statement by the client indicates a need for further education?
Explanation
Treating hypoglycemia promptly is crucial to prevent more severe symptoms or complications. Waiting until blood sugar drops very low can lead to a dangerous situation.
Incorrect choices:
a. Carrying a source of fast-acting carbohydrates, like glucose tablets or juice, helps quickly raise blood sugar levels during an episode of hypoglycemia.
c. Checking blood sugar levels when experiencing symptoms of hypoglycemia helps confirm if blood sugar is low and guides appropriate treatment.
d. Notifying the healthcare provider about frequent hypoglycemia episodes is important to adjust the diabetes management plan and prevent future occurrences.
A client with diabetes is experiencing symptoms of hypoglycemia, including sweating, shakiness, and confusion. Which action by the nurse is appropriate for hypoglycemia management?
Explanation
Offering a source of fast-acting carbohydrates. Fast-acting carbohydrates, such as glucose tablets or juice, can quickly raise blood sugar levels and alleviate hypoglycemic symptoms.
Incorrect choices:
a. Administering a long-acting insulin injection would not address the immediate need to raise blood sugar levels during an episode of hypoglycemia.
b. Providing a high-fat snack would not rapidly increase blood sugar levels and alleviate symptoms of hypoglycemia.
c. Giving a rapid-acting insulin injection would further lower blood sugar levels and worsen hypoglycemia symptoms.
A client with diabetes is experiencing hypoglycemia and is conscious. Which intervention should the nurse implement for hypoglycemia management?
Explanation
Encouraging the client to consume a high-protein snack. Consuming a high-protein snack along with a source of fast-acting carbohydrates helps stabilize blood sugar levels and prevent further hypoglycemia.
Incorrect choices:
a. Administering glucagon injection is indicated for severe hypoglycemia when the client is unconscious or unable to swallow.
b. Starting an IV glucose infusion is reserved for severe hypoglycemia cases that are unresponsive to other interventions or when the client is unable to tolerate oral intake.
d. Monitoring blood sugar levels every 4 hours is a routine practice but does not address the immediate need to treat hypoglycemia.
A client with diabetes is unconscious and experiencing severe hypoglycemia. What is the appropriate nursing intervention for hypoglycemia management?
Explanation
Glucagon is administered in cases of severe hypoglycemia to rapidly raise blood sugar levels in an unconscious client.
Incorrect choices:
a. Administering an oral glucose solution is not appropriate for an unconscious client who cannot swallow.
b. Initiating an insulin infusion would further lower blood sugar levels and worsen the hypoglycemic state.
d. Encouraging the client to consume a high-protein meal is not feasible for an unconscious client.
A client with diabetes is experiencing hypoglycemia and is conscious. The nurse provides the client with a glucose gel tube. What should the nurse instruct the client to do next?
Explanation
Swallow the gel and drink a glass of water. Glucose gel is designed to be swallowed, and consuming a source of carbohydrates along with water will help rapidly raise blood sugar levels.
Incorrect choices:
b. Applying the gel topically to the skin will not effectively raise blood sugar levels and alleviate hypoglycemic symptoms.
c. Massaging the gel into the site of injection is not appropriate, as glucose gel is meant to be swallowed.
d. Rubbing the gel between the palms and inhaling deeply will not have a significant impact on blood sugar levels.
A nurse is providing education to a client newly diagnosed with type 1 diabetes who will be starting insulin therapy. Which statement by the client indicates a need for further education?
Explanation
Insulin syringes should not be reused due to the risk of contamination, infection, and inaccurate dosing.
Incorrect choices:
a. Rotating injection sites between different anatomical areas helps prevent lipohypertrophy and ensures consistent absorption.
c. Insulin vials can be kept at room temperature for up to 28 days once in use, but they should be stored away from direct sunlight and extreme temperatures.
d. Eating a meal or snack within 15 minutes of taking rapid-acting insulin helps prevent hypoglycemia and ensures that the insulin is working when glucose levels rise after eating.
A client with type 2 diabetes is learning about self-administration of insulin. Which statement by the client indicates a need for further education?
Explanation
Insulin should be injected into the subcutaneous tissue, not the muscle.
Incorrect choices:
a. Cleaning the injection site with an alcohol swab before injection is a recommended practice to prevent infection.
c. Insulin pens are a convenient and accurate way to measure and administer insulin doses.
d. Rotating injection sites helps prevent lipohypertrophy and ensures consistent absorption.
A nurse is teaching a client about insulin storage and handling. Which statement by the client indicates a need for further education?
Explanation
Insulin pens should not be exposed to extreme temperatures, including heat, as it can affect their potency.
Incorrect choices:
a. Storing insulin vials in the refrigerator helps maintain their potency, but they can be kept at room temperature for up to 28 days once in use.
c. Checking the expiration date on insulin vials is important to ensure their effectiveness and safety.
d. Gently rolling the insulin vial between palms helps mix the insulin if it appears cloudy, but it should not be done with clear insulin.
A client with diabetes is learning about managing hypoglycemia. Which statement by the client indicates a need for further education?
Explanation
While orange juice can raise blood sugar quickly, it can also cause a rapid spike and subsequent crash, leading to further hypoglycemia.
Incorrect choices:
a. Keeping glucose tablets or gel on hand is a recommended practice to rapidly raise blood sugar in case of hypoglycemia.
c. Eating a high-protein snack can help stabilize blood sugar and prevent it from dropping too low.
d. Following up with a healthcare provider about frequent episodes of hypoglycemia is important to adjust insulin therapy and prevent future episodes.
A nurse is educating a client on self-monitoring blood glucose (SMBG) levels. Which statement by the client indicates a need for further education?
Explanation
Applying alcohol before lancing can affect the accuracy of blood glucose readings.
Incorrect choices:
a. Cleaning hands with soap and water before using the glucose meter is a good practice to ensure accurate readings.
b. Applying a lancet to the side of the fingertip is a correct technique to obtain a blood sample for glucose testing.
d. Testing blood sugar regularly, regardless of symptoms, helps monitor and manage glucose levels effectively.
A client newly diagnosed with type 2 diabetes is prescribed insulin therapy. The client asks the nurse, "Why do I need insulin if I have type 2 diabetes?" Which response by the nurse is accurate?
Explanation
In type 2 diabetes, the body's cells may become resistant to the effects of insulin, and the pancreas may produce less insulin over time. This can result in the need for insulin therapy to help manage blood sugar levels effectively.
Incorrect choices:
a. This statement is incorrect. While insulin therapy is commonly associated with type 1 diabetes, it can also be used in type 2 diabetes when other treatments are not sufficient.
b. Insulin therapy does not cure diabetes. It helps manage blood sugar levels and prevents complications, but it does not eliminate the underlying condition.
d. Insulin therapy may be used temporarily, but it can also be a long-term treatment option for type 2 diabetes, especially if other treatments are not effective.
A client with type 1 diabetes is starting insulin therapy. The client asks the nurse, "How do I know what dose of insulin to take?" What is the nurse's best response?
Explanation
Insulin therapy for type 1 diabetes is individualized and based on factors such as the client's weight, activity level, blood sugar levels, and overall health. The healthcare provider will determine the appropriate insulin dose for the client.
Incorrect choices:
a. Adjusting insulin dose based on how one feels is not a safe or accurate method. Insulin dosing should be guided by healthcare provider recommendations.
c. Starting with a high dose of insulin is not advisable and can lead to hypoglycemia. Insulin dosing should be started conservatively and adjusted as needed.
d. While monitoring blood sugar levels before and after meals is important for diabetes management, it is not the sole method for determining insulin dosing. Healthcare provider guidance is essential.
A client with type 1 diabetes is starting insulin therapy. The client asks the nurse, "How do I know what dose of insulin to take?" What is the nurse's best response?
Explanation
Insulin therapy for type 1 diabetes is individualized and based on factors such as the client's weight, activity level, blood sugar levels, and overall health. The healthcare provider will determine the appropriate insulin dose for the client.
Incorrect choices:
a. Adjusting insulin dose based on how one feels is not a safe or accurate method. Insulin dosing should be guided by healthcare provider recommendations.
c. Starting with a high dose of insulin is not advisable and can lead to hypoglycemia. Insulin dosing should be started conservatively and adjusted as needed.
d. While monitoring blood sugar levels before and after meals is important for diabetes management, it is not the sole method for determining insulin dosing. Healthcare provider guidance is essential.
A client with diabetes is prescribed a basal-bolus insulin regimen. The nurse teaches the client about this regimen. Which statement by the client indicates a need for further education?
Explanation
With a basal-bolus insulin regimen, clients are often encouraged to have snacks between meals to help prevent hypoglycemia caused by rapid-acting insulin. Snacking helps maintain more stable blood sugar levels.
Incorrect choices:
a. Taking a long-acting insulin in the morning and evening is consistent with a basal-bolus regimen. This statement is correct.
b. Using rapid-acting insulin before each meal is consistent with a basal-bolus regimen. This statement is correct.
d. Rotating injection sites within the same area is a recommended practice to prevent skin changes and complications associated with repeated injections. This statement is correct.
A client is receiving insulin therapy for diabetes management. The nurse is providing education about the importance of proper injection techniques. Which statement by the client indicates a need for further education?
Explanation
Injecting insulin into the same spot every day can lead to skin changes, scar tissue formation, and poor insulin absorption. Rotating injection sites is important to prevent complications.
Incorrect choices:
b. Using a 90-degree angle when inserting the needle is a common technique for insulin injections. This statement is correct.
c. Avoiding scar tissue and areas with visible blood vessels is important to ensure proper insulin absorption. This statement is correct.
d. Pinching the skin before inserting the needle can help ensure subcutaneous injection and prevent injecting into muscle. This statement is correct.
A client with diabetes is prescribed both basal and prandial insulin. The nurse is teaching the client about the difference between these two types of insulin. Which statement by the client indicates a need for further education?
Explanation
Basal insulin is typically taken once or twice a day to provide a steady baseline level of insulin, while prandial (mealtime) insulin is taken before meals to control post-meal blood sugar spikes.
Incorrect choices:
a. Basal insulin indeed provides a steady amount of insulin to cover the body's basic metabolic needs between meals and overnight. This statement is correct.
b. Prandial insulin does help control the rise in blood sugar after meals. This statement is correct.
d. Prandial insulin is indeed a type of rapid-acting insulin used to cover meals and control post-meal blood sugar levels. This statement is correct.
A nurse is teaching a client with diabetes about insulin therapy. Which statement by the client indicates a need for further education?
Explanation
Insulin syringes should not be reused due to the risk of contamination, infection, and inaccurate dosing.
Incorrect choices:
a. Drawing up short-acting insulin before long-acting insulin is a recommended practice to prevent contamination of the long-acting insulin vial.
c. Rotating injection sites within the same anatomical area helps prevent lipohypertrophy and ensures consistent absorption.
d. Insulin vials should be kept refrigerated to maintain their potency, but they can be kept at room temperature for up to 28 days once in use to prevent discomfort from cold injections.
A client is prescribed both long-acting and short-acting insulin. Which statement by the client demonstrates an understanding of insulin administration?
Explanation
Short-acting insulin is administered before meals to cover postprandial glucose spikes, while long-acting insulin is typically administered once daily, often at bedtime.
Incorrect choices:
a. Administering short-acting insulin in the morning and long-acting insulin at bedtime does not coincide with the timing needed to control glucose levels effectively.
c. Short-acting and long-acting insulins should not be mixed in the same syringe to maintain their proper dosing and actions.
d. Administering long-acting insulin right after a meal would not match the onset and duration of action needed for glucose control.
A client with diabetes is prescribed insulin glargine (Lantus) once daily. Which statement by the client indicates a need for further education about insulin administration?
Explanation
Insulin glargine (Lantus) is a long-acting insulin that should not be mixed with other types of insulin in the same syringe.
Incorrect choices:
a. Insulin glargine (Lantus) is a U-100 insulin and should be administered using a U-100 insulin syringe.
b. Lantus can be injected into the abdomen, thigh, or upper arm to ensure consistent absorption and to prevent lipohypertrophy.
d. Injecting Lantus at the same time each day helps maintain consistent blood sugar levels and optimize its effectiveness.
A client is receiving multiple daily injections of insulin. Which technique by the client indicates a need for further education?
Explanation
Drawing up the cloudy insulin before the clear insulin. When mixing insulins, clear insulin should be drawn up first to prevent contaminating the clear insulin with the cloudy insulin.
Incorrect choices:
a. Rotating injection sites within the same area helps prevent lipohypertrophy and ensures consistent absorption.
b. Administering regular insulin before meals aligns with the timing needed to cover postprandial glucose spikes.
d. Using a 45-degree angle for subcutaneous injections is a recommended technique for insulin administration to ensure proper subcutaneous delivery.
A nurse is preparing to administer insulin lispro (Humalog) to a client. Which action by the nurse indicates the need for further education about insulin administration?
Explanation
Insulin lispro should not be stored in the refrigerator; it can be kept at room temperature for up to 28 days once in use.
Incorrect choices:
a. Administering insulin lispro within 15 minutes of a meal matches its rapid onset of action, which helps control postprandial glucose levels.
b. Using an insulin syringe to draw up insulin lispro is an appropriate technique for accurate dosing.
d. Injecting insulin lispro into the subcutaneous tissue is the correct route of administration for this rapid-acting insulin.
Goitre
The nurse is providing education to a group of clients about goiter. Which statement best describes a goiter?
Explanation
A goiter is a noncancerous enlargement of the thyroid gland in the neck. It can result from various causes, including iodine deficiency, thyroid dysfunction, and autoimmune conditions.
Incorrect choices:
a. A goiter is not a hormonal disorder that affects blood sugar levels; it specifically involves the thyroid gland.
c. A goiter is not a bacterial infection affecting the throat and tonsils but related to the thyroid gland.
d. A goiter does not cause inflammation of the adrenal glands; it is specific to the thyroid gland.
The nurse is conducting a health assessment for a client with a suspected goiter. Which area should the nurse palpate to assess for a goiter?
Explanation
The thyroid gland is located in the front of the neck, just below the Adam's apple. Palpation of this area can help assess for the presence of a goiter.
Incorrect choices:
a. Palpation over the sternum is not relevant to assessing a goiter.
b. Palpation behind the ears is not relevant to assessing a goiter.
c. Palpation over the parotid glands is not relevant to assessing a goiter.
The nurse is reviewing the medical history of a client with a goiter. Which condition is commonly associated with goiter development?
Explanation
Hypothyroidism, or an underactive thyroid, is commonly associated with goiter development. When the thyroid gland is unable to produce enough thyroid hormones, it can lead to an enlargement of the gland.
Incorrect choices:
a. Type 2 diabetes is not directly associated with goiter development.
b. Osteoporosis is not directly associated with goiter development.
d. Chronic obstructive pulmonary disease (COPD) is not directly associated with goiter development.
The nurse is assessing a client with a goiter. Which symptom is commonly associated with a goiter that is causing compression of nearby structures?
Explanation
A goiter that causes compression of nearby structures, such as the esophagus, can lead to difficulty swallowing (dysphagia).
Incorrect choices:
a. Weight gain is a symptom of hypothyroidism but not specifically related to goiter compression.
b. Constipation is a symptom of hypothyroidism but not specifically related to goiter compression.
d. Heat intolerance is a symptom of hyperthyroidism but not specifically related to goiter compression.
The nurse is providing education to a client with a goiter. Which dietary element is important for preventing goiter development?
Explanation
Iodine is an essential element for thyroid hormone production. Adequate dietary iodine intake is important for preventing goiter development.
Incorrect choices:
a. Sodium is not directly related to goiter prevention.
b. Calcium is important for bone health but not specifically related to goiter prevention.
d. Iron is important for red blood cell production but not specifically related to goiter prevention.
The nurse is educating a client about the different types of goiters. Which type of goiter is caused by an overproduction of thyroid hormones?
Explanation
A toxic goiter, also known as a toxic nodular goiter or toxic adenoma, is caused by the overproduction of thyroid hormones, leading to hyperthyroidism.
Incorrect choices:
a. A simple goiter is an enlargement of the thyroid gland without any specific hormonal dysfunction.
c. A colloid goiter is characterized by the accumulation of colloid within thyroid follicles and is not specifically related to thyroid hormone overproduction.
d. An endemic goiter is caused by iodine deficiency and is not specifically related to thyroid hormone overproduction.
The nurse is reviewing the medical records of several clients with goiters. Which type of goiter is characterized by multiple nodules within the thyroid gland?
Explanation
A multinodular goiter is characterized by the presence of multiple nodules within the thyroid gland. These nodules can be benign or malignant.
Incorrect choices:
a. A simple goiter is an enlargement of the thyroid gland without specific nodules.
b. A toxic goiter is characterized by the overproduction of thyroid hormones and may or may not be associated with nodules.
c. A colloid goiter is characterized by the accumulation of colloid within thyroid follicles and does not specifically refer to the presence of multiple nodules.
The nurse is providing education to a group of clients about the different types of goiters. Which type of goiter is associated with iodine deficiency?
Explanation
A simple goiter, also known as a nontoxic goiter, is often caused by iodine deficiency. It is characterized by the enlargement of the thyroid gland without specific nodules or hormonal dysfunction.
Incorrect choices:
b. A toxic goiter is characterized by the overproduction of thyroid hormones and may or may not be associated with iodine deficiency.
c. A colloid goiter is characterized by the accumulation of colloid within thyroid follicles and is not specifically related to iodine deficiency.
d. A multinodular goiter may or may not be associated with iodine deficiency and is characterized by the presence of multiple nodules within the thyroid gland.
The nurse is assessing a client with a large, diffuse, painless swelling in the neck. Which type of goiter is characterized by these findings?
Explanation
A simple goiter is characterized by a diffuse enlargement of the thyroid gland that is typically painless and not associated with specific nodules or hormonal dysfunction.
Incorrect choices:
b. A toxic goiter is characterized by the overproduction of thyroid hormones and may or may not present with a large, diffuse swelling.
c. A colloid goiter is characterized by the accumulation of colloid within thyroid follicles and does not specifically refer to the size or painlessness of the swelling.
d. An endemic goiter is caused by iodine deficiency and is not specifically characterized by a large, diffuse, painless swelling.
The nurse is caring for a client with a goiter and is reviewing the client's medical history. Which type of goiter is associated with Hashimoto's thyroiditis?
Explanation
Hashimoto's thyroiditis, an autoimmune condition, is commonly associated with the development of a simple goiter. The immune system attacks the thyroid gland, leading to its enlargement.
Incorrect choices:
b. A toxic goiter is characterized by the overproduction of thyroid hormones and is not specifically associated with Hashimoto's thyroiditis.
c. A colloid goiter is characterized by the accumulation of colloid within thyroid follicles and is not specifically associated with Hashimoto's thyroiditis.
d. An endemic goiter is caused by iodine deficiency and is not specifically associated with Hashimoto's thyroiditis.
The nurse is educating a group of clients about the different causes of goiter. Which cause of goiter is related to a deficiency of dietary iodine?
Explanation
Iodine deficiency is a common cause of goiter, especially in regions where there is insufficient dietary intake of iodine, leading to inadequate production of thyroid hormones.
Incorrect choices:
a. Autoimmune thyroid disease, such as Hashimoto's thyroiditis, is not specifically related to iodine deficiency and is characterized by immune system attack on the thyroid gland.
b. Excessive thyroid hormone production is associated with conditions such as toxic goiter or Graves' disease and is not directly related to iodine deficiency.
c. Radiation exposure can damage the thyroid gland and lead to goiter, but it is not directly related to iodine deficiency.
The nurse is assessing a client with a history of taking certain medications. Which class of medications is known to interfere with thyroid hormone synthesis and may contribute to the development of goiter?
Explanation
Antithyroid medications, such as propylthiouracil (PTU) and methimazole, can interfere with thyroid hormone synthesis and contribute to the development of goiter.
Incorrect choices:
a. Antihypertensives are not known to directly interfere with thyroid hormone synthesis or contribute to goiter development.
b. Antibiotics are not known to directly interfere with thyroid hormone synthesis or contribute to goiter development.
c. Anticoagulants are not known to directly interfere with thyroid hormone synthesis or contribute to goiter development.
The nurse is providing education to a client about the potential causes of goiter. Which condition is characterized by the immune system attacking the thyroid gland, leading to goiter development?
Explanation
Hashimoto's thyroiditis is an autoimmune condition in which the immune system attacks the thyroid gland, leading to inflammation and goiter development.
Incorrect choices:
a. Hypothyroidism can result from various causes, including Hashimoto's thyroiditis, but it is not the primary cause of goiter.
b. Hyperparathyroidism affects the parathyroid glands and is not the primary cause of goiter.
d. Cushing's syndrome is caused by excessive cortisol production and is not the primary cause of goiter.
The nurse is reviewing the medical history of a client with a goiter. Which condition is commonly associated with the development of a goiter?
Explanation
Hyperthyroidism, or excessive thyroid hormone production, is commonly associated with the development of a goiter.
Incorrect choices:
a. Osteoporosis is not directly related to the development of a goiter.
b. Diabetes mellitus is not directly related to the development of a goiter.
d. Chronic obstructive pulmonary disease (COPD) is not directly related to the development of a goiter.
The nurse is providing education to a client about the potential causes of goiter. Which factor may contribute to the development of a goiter in individuals with a genetic predisposition?
Explanation
A family history of thyroid disorders, especially goiter or autoimmune thyroid conditions, can contribute to the development of goiter in individuals with a genetic predisposition.
Incorrect choices:
a. Consumption of high-iodine foods can contribute to iodine-induced goiter but is not specifically related to genetic predisposition.
b. Regular physical exercise is not directly related to the development of goiter.
c. Exposure to cold temperatures is not directly related to the development of goiter.
The nurse is assessing a client with a goiter. Which clinical manifestation is commonly associated with a goiter?
Explanation
Enlargement of the thyroid gland in a goiter can lead to pressure on the esophagus and trachea, causing difficulty swallowing and sometimes difficulty breathing.
Incorrect choices:
a. Increased body temperature is not a typical clinical manifestation of a goiter.
b. Weight gain is not a typical clinical manifestation of a goiter.
d. Excessive thirst is not a typical clinical manifestation of a goiter.
The nurse is performing an assessment on a client with a goiter. Which symptom is commonly associated with a large goiter pressing on the trachea?
Explanation
A large goiter pressing on the trachea can cause wheezing or difficulty breathing due to the obstruction of airflow.
Incorrect choices:
a. Increased urination is not typically associated with a large goiter pressing on the trachea.
c. Increased appetite is not typically associated with a large goiter pressing on the trachea.
d. Swollen ankles are not typically associated with a large goiter pressing on the trachea.
The nurse is assessing a client with a goiter. Which clinical manifestation is commonly associated with an overactive thyroid gland (hyperthyroidism) that may accompany a goiter?
Explanation
Hyperthyroidism, which can be associated with a goiter, often leads to a rapid heartbeat (tachycardia) as a result of increased thyroid hormone levels.
Incorrect choices:
a. Weight gain is not typically associated with hyperthyroidism and goiter.
b. Cold intolerance is not typically associated with hyperthyroidism and goiter.
c. Fatigue may be present in hyperthyroidism, but it is not as specific as a rapid heartbeat.
The nurse is assessing a client with a goiter. Which clinical manifestation is commonly associated with an underactive thyroid gland (hypothyroidism) that may accompany a goiter?
Explanation
Hypothyroidism, which can be associated with a goiter, often leads to fatigue and lethargy due to decreased thyroid hormone levels.
Incorrect choices:
a. Heat intolerance is not typically associated with hypothyroidism and goiter.
b. Restlessness is not typically associated with hypothyroidism and goiter.
c. Weight loss is not typically associated with hypothyroidism and goiter.
The nurse is assessing a client with a goiter. Which clinical manifestation is commonly associated with a goiter that is caused by iodine deficiency?
Explanation
Iodine deficiency can lead to hypothyroidism, which may manifest as dry skin due to decreased thyroid hormone levels.
Incorrect choices:
a. Excessive sweating is not typically associated with iodine deficiency and goiter.
b. Weight gain is a common clinical manifestation of hypothyroidism but is not specific to iodine deficiency.
d. Exophthalmos (bulging eyes) is associated with hyperthyroidism (Graves' disease) and is not typically seen in iodine deficiency-related goiter.
The nurse is reviewing the diagnostic evaluation for a client suspected of having a goiter. Which laboratory test is commonly used to assess thyroid function and determine if the goiter is associated with hyperthyroidism or hypothyroidism?
Explanation
Thyroid-stimulating hormone (TSH) is a hormone produced by the pituitary gland that stimulates the thyroid gland to produce thyroid hormones. An elevated TSH level indicates hypothyroidism, while a low TSH level indicates hyperthyroidism, both of which can be associated with a goiter.
Incorrect choices:
a. Complete blood count (CBC) assesses various components of blood but is not directly related to thyroid function or goiter diagnosis.
b. Blood glucose level is used to diagnose diabetes mellitus and is not directly related to goiter diagnosis.
d. Serum creatinine level is used to assess kidney function and is not directly related to thyroid function or goiter diagnosis.
The nurse is assisting with a radioactive iodine uptake (RAIU) test for a client with a suspected goiter. What is the primary purpose of the RAIU test in the diagnosis of a goiter?
Explanation
The RAIU test involves administering a small amount of radioactive iodine and measuring its uptake by the thyroid gland. This helps assess the production and distribution of thyroid hormones and can aid in diagnosing various thyroid disorders, including goiter.
Incorrect choices:
a. Measuring blood glucose levels is not the primary purpose of the RAIU test and is not directly related to goiter diagnosis.
b. Assessing kidney function is not the primary purpose of the RAIU test and is not directly related to goiter diagnosis.
d. Detecting inflammation in the thyroid gland is not the primary purpose of the RAIU test and is not directly related to goiter diagnosis.
The nurse is reviewing the diagnostic process for a client with a suspected goiter. Which imaging technique is commonly used to visualize the size, shape, and characteristics of the thyroid gland?
Explanation
Thyroid ultrasound is a noninvasive imaging technique that uses sound waves to visualize the thyroid gland, assess its size, shape, and characteristics, and identify any abnormalities or nodules.
Incorrect choices:
a. Electrocardiogram (ECG) is used to assess the electrical activity of the heart and is not related to thyroid imaging.
b. Magnetic resonance imaging (MRI) and c. Computed tomography (CT) scan are imaging techniques that may be used for other purposes but are not typically used for routine thyroid imaging.
The nurse is assisting with a fine-needle aspiration (FNA) biopsy for a client with a thyroid nodule and suspected goiter. What is the primary purpose of an FNA biopsy in the diagnosis of a goiter?
Explanation
Fine-needle aspiration (FNA) biopsy involves using a thin needle to aspirate a tissue sample from the thyroid nodule. The tissue sample is then analyzed to determine if the nodule is benign or malignant, helping in the diagnosis of a goiter.
Incorrect choices:
a. Assessing blood clotting function is not the primary purpose of an FNA biopsy and is not directly related to goiter diagnosis.
b. Evaluating kidney function is not the primary purpose of an FNA biopsy and is not directly related to goiter diagnosis.
c. Determining blood glucose levels is not the primary purpose of an FNA biopsy and is not directly related to goiter diagnosis.
The nurse is educating a client about the diagnostic evaluation for goiter. Which diagnostic test measures the levels of thyroid hormones (T3 and T4) in the blood and can help determine if the goiter is associated with hyperthyroidism or hypothyroidism?
Explanation
A thyroid function panel measures the levels of thyroid hormones (T3 and T4) in the blood, as well as thyroid-stimulating hormone (TSH) levels. This test can help determine if the goiter is associated with hyperthyroidism or hypothyroidism.
Incorrect choices:
a. Serum albumin level is not directly related to thyroid function or goiter diagnosis.
b. Hemoglobin A1c level is used to assess long-term blood glucose control in diabetes and is not directly related to goiter diagnosis.
d. C-reactive protein (CRP) level is a marker of inflammation and is not directly related to thyroid function or goiter diagnosis.
The nurse is caring for a client with a goiter. Which dietary recommendation should the nurse provide to the client to support thyroid health and manage the goiter?
Explanation
Iodine is essential for thyroid hormone production. Increasing the consumption of iodized salt can help support thyroid health and manage goiter caused by iodine deficiency.
Incorrect choices:
b. Limiting intake of fruits and vegetables is not necessary and is not directly related to managing a goiter.
c. Consuming foods high in calcium is important for bone health but is not directly related to managing a goiter.
d. Avoiding foods rich in omega-3 fatty acids is not necessary and is not directly related to managing a goiter.
The nurse is caring for a client with a goiter. Which medication is commonly prescribed to manage hyperthyroidism and reduce the size of a goiter?
Explanation
Methimazole is an antithyroid medication commonly prescribed to manage hyperthyroidism and reduce the size of a goiter by decreasing thyroid hormone production.
Incorrect choices:
a. Levothyroxine (Synthroid) is a thyroid hormone replacement medication and is not used to manage hyperthyroidism or goiter.
c. Insulin glargine (Lantus) is used to manage diabetes and is not related to managing hyperthyroidism or goiter.
d. Metformin (Glucophage) is used to manage diabetes and is not related to managing hyperthyroidism or goiter.
The nurse is providing education to a client with a goiter. Which self-care measure should the nurse recommend to the client to alleviate discomfort and promote thyroid health?
Explanation
Applying warm compresses to the neck can help alleviate discomfort, improve circulation, and promote thyroid health.
Incorrect choices:
a. Applying ice packs to the neck is not recommended as it may worsen discomfort and is not related to promoting thyroid health.
b. Massaging the thyroid gland is not recommended as it can potentially irritate the thyroid and is not related to promoting thyroid health.
c. Performing neck stretches is not recommended as it may worsen discomfort and is not related to promoting thyroid health.
The nurse is caring for a client with a goiter. Which surgical procedure involves the removal of the entire thyroid gland and is considered a definitive treatment for goiter?
Explanation
Thyroidectomy is a surgical procedure that involves the removal of the entire thyroid gland. It is considered a definitive treatment for goiter when other management options are not effective.
Incorrect choices:
b. Parathyroidectomy involves the removal of the parathyroid glands and is not directly related to goiter treatment.
c. Adrenalectomy involves the removal of the adrenal glands and is not directly related to goiter treatment.
d. Nephrectomy involves the removal of a kidney and is not directly related to goiter treatment.
The nurse is caring for a client with a goiter. Which nursing intervention is important to include in the plan of care to prevent potential complications after thyroidectomy?
Explanation
Encouraging deep breathing and coughing exercises helps prevent respiratory complications such as pneumonia after thyroidectomy.
Incorrect choices:
b. Limiting fluid intake is not necessary and does not prevent complications after thyroidectomy.
c. Administering high doses of aspirin is not appropriate for pain management after thyroidectomy and can lead to bleeding complications.
d. Encouraging the client to flex the neck frequently is not recommended after thyroidectomy as it may strain the surgical site and potentially lead to complications.
The nurse is caring for a client with a large goiter. Which complication should the nurse monitor for that can occur due to compression of the trachea and airway obstruction?
Explanation
Compression of the trachea by a large goiter can lead to difficulty breathing (dyspnea) due to airway obstruction. This is an important complication to monitor for in clients with goiter.
Incorrect choices:
a. Hypothyroidism is not a direct complication of tracheal compression and airway obstruction caused by a goiter.
b. Hyperthyroidism is not a direct complication of tracheal compression and airway obstruction caused by a goiter.
c. Dysphagia, or difficulty swallowing, can be a complication of goiter but is not directly related to tracheal compression and airway obstruction.
The nurse is caring for a client with a goiter. Which potential complication should the nurse monitor for that can result from an untreated or inadequately managed goiter?
Explanation
An untreated or inadequately managed goiter can lead to hormonal imbalances and excessive thyroid hormone production, which can result in cardiac arrhythmias.
Incorrect choices:
a. Bradycardia is not a typical complication of an untreated or inadequately managed goiter.
b. Hypertension is not a typical complication of an untreated or inadequately managed goiter.
d. Gastrointestinal bleeding is not a direct complication of an untreated or inadequately managed goiter.
The nurse is providing education to a client with a goiter. Which potential complication should the nurse emphasize as a result of an enlarged thyroid gland pressing on the esophagus?
Explanation
An enlarged thyroid gland pressing on the esophagus can lead to difficulty swallowing (dysphagia) as a potential complication.
Incorrect choices:
a. Gastric ulcers are not directly related to an enlarged thyroid gland pressing on the esophagus.
b. Liver dysfunction is not directly related to an enlarged thyroid gland pressing on the esophagus.
c. Malabsorption is not directly related to an enlarged thyroid gland pressing on the esophagus.
The nurse is caring for a client with a goiter. Which complication should the nurse monitor for that can occur as a result of pressure on the recurrent laryngeal nerve by the enlarged thyroid gland?
Explanation
Pressure on the recurrent laryngeal nerve by an enlarged thyroid gland can lead to hoarseness or voice changes.
Incorrect choices:
a. Osteoporosis is not directly related to pressure on the recurrent laryngeal nerve by an enlarged thyroid gland.
b. Hypertension is not directly related to pressure on the recurrent laryngeal nerve by an enlarged thyroid gland.
d. Peripheral neuropathy is not directly related to pressure on the recurrent laryngeal nerve by an enlarged thyroid gland.
The nurse is assessing a client with a goiter. Which potential complication should the nurse monitor for that can occur due to the release of excess thyroid hormones into the bloodstream?
Explanation
The release of excess thyroid hormones into the bloodstream can lead to a life-threatening condition called thyroid storm, characterized by severe hyperthyroidism.
Incorrect choices:
a. Anemia is not directly related to the release of excess thyroid hormones into the bloodstream.
b. Hyperglycemia is not directly related to the release of excess thyroid hormones into the bloodstream.
c. Hypothyroidism is not directly related to the release of excess thyroid hormones into the bloodstream.
The nurse is assessing a client with a suspected goiter. Which finding would the nurse expect to observe upon physical examination?
Explanation
A goiter is characterized by an enlarged thyroid gland, which can be observed and palpated during a physical examination.
Incorrect choices:
a. Increased body temperature is not a specific finding associated with a goiter.
b. Bradycardia is not a specific finding associated with a goiter.
d. Cyanotic nail beds are not a specific finding associated with a goiter.
The nurse is educating a client about the risk factors for developing a goiter. Which statement by the client indicates a correct understanding of the risk factors?
Explanation
Exposure to excessive radiation is a known risk factor for the development of goiter.
Incorrect choices:
a. Having a family history of goiter can increase the risk of developing it.
b. Consuming a diet rich in iodine is important to prevent iodine deficiency-related goiter, but excessive iodine intake can also contribute to goiter.
d. Being physically inactive is not directly linked to the development of goiter.
The nurse is reviewing the medical history of a client with a goiter. Which condition should the nurse recognize as a potential cause of secondary goiter?
Explanation
Hypothyroidism can lead to an increase in thyroid-stimulating hormone (TSH), which can cause secondary goiter.
Incorrect choices:
b. Hyperthyroidism is more commonly associated with primary goiter.
c. Diabetes mellitus is not a direct cause of goiter.
d. Hypertension is not a direct cause of goiter.
The nurse is caring for a client with a goiter. Which assessment finding should the nurse prioritize in order to determine the client's thyroid function?
Explanation
Thyroid function blood tests, such as measuring levels of thyroid-stimulating hormone (TSH), thyroxine (T4), and triiodothyronine (T3), are the most accurate indicators of thyroid function.
Incorrect choices:
a. Blood pressure measurement is not directly related to determining thyroid function.
b. Visual acuity test is not directly related to determining thyroid function.
c. Deep tendon reflexes are not directly related to determining thyroid function.
The nurse is providing education to a client with a goiter. Which statement by the client indicates a need for further clarification regarding the management of goiter?
Explanation
While iodine deficiency can contribute to goiter, it's important for clients to have an adequate intake of iodine. Avoiding iodine-rich foods is not recommended.
Incorrect choices:
a. Taking prescribed thyroid hormone replacement medication as directed is an important part of managing goiter.
c. Regular follow-up appointments with a healthcare provider are important for monitoring the progress of the goiter and thyroid function.
d. Using over-the-counter pain relievers to manage discomfort associated with goiter is a reasonable approach.
Thyroid Storm
The nurse is providing education to a group of nursing students about thyroid storm. Which statement by a student indicates a correct understanding of thyroid storm?
Explanation
Thyroid storm is an acute, life-threatening condition that occurs as a result of uncontrolled hyperthyroidism. It is characterized by a sudden and dramatic increase in thyroid hormone levels, leading to severe symptoms and potential complications.
The nurse is reviewing the medical history of a client with thyroid storm. Which underlying condition should the nurse recognize as a potential trigger for thyroid storm?
Explanation
Thyroid storm can be triggered by various factors, including uncontrolled hyperthyroidism, infection, trauma, or certain medications. Hypothyroidism is not a trigger for thyroid storm; it is a separate condition characterized by an underactive thyroid gland.
The nurse is assessing a client suspected of experiencing thyroid storm. Which clinical manifestation is commonly associated with thyroid storm?
Explanation
Profuse sweating is a common clinical manifestation of thyroid storm. Other symptoms include tachycardia, hypertension, fever, restlessness, agitation, delirium, and gastrointestinal symptoms.
The nurse is caring for a client diagnosed with thyroid storm. Which intervention should the nurse prioritize in the management of this condition?
Explanation
Providing supplemental oxygen therapy is a priority intervention to ensure adequate oxygenation and support vital organ function in a client with thyroid storm. This condition can cause increased metabolic demand and potential respiratory distress.
The nurse is educating a client about the importance of adhering to medication therapy for thyroid storm. Which statement by the client indicates a correct understanding of the treatment?
Explanation
Adherence to medication therapy is crucial in managing thyroid storm. Medications are used to reduce thyroid hormone production and control symptoms. Stopping medications prematurely can lead to a recurrence of the condition.
Incorrect choices:
a. Stopping medications once symptoms improve is not recommended, as it can lead to a relapse of thyroid storm.
c. Medications should be taken as prescribed, regardless of symptom severity.
d. Skipping doses can disrupt the effectiveness of medication therapy and worsen the client's condition.
The nurse is explaining the pathophysiology of thyroid storm to a client. Which statement accurately describes the underlying process that contributes to thyroid storm?
Explanation
Thyroid storm is a life-threatening condition characterized by a sudden and severe increase in thyroid hormone levels in the bloodstream. This occurs due to the uncontrolled release of thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), from the thyroid gland.
The nurse is discussing the physiological effects of thyroid storm with a group of nursing students. Which manifestation is a direct result of the excessive thyroid hormone levels seen in thyroid storm?
Explanation
Excessive thyroid hormone levels in thyroid storm lead to hypermetabolism, which results in increased oxygen consumption, heat production, and energy expenditure. This hypermetabolic state is associated with symptoms such as tachycardia, hypertension, fever, and profuse sweating.
The nurse is explaining the role of the sympathetic nervous system in thyroid storm. Which statement accurately describes the interaction between the sympathetic nervous system and thyroid hormone release in this condition?
Explanation
Thyroid storm is associated with sympathetic nervous system stimulation, leading to increased release of thyroid hormones from the thyroid gland. This results in a cascade of hypermetabolic effects throughout the body.
The nurse is discussing the feedback loop that regulates thyroid hormone production with a client. Which component of the feedback loop is disrupted in thyroid storm?
Explanation
In thyroid storm, the usual negative feedback loop between the hypothalamus, pituitary gland, and thyroid gland is disrupted. The excessive release of thyroid hormones suppresses the secretion of thyroid-stimulating hormone (TSH) from the pituitary gland, leading to uncontrolled thyroid hormone production.
The nurse is educating a client about the triggers for thyroid storm. Which statement accurately describes a common trigger for thyroid storm?
Explanation
Excessive iodine intake, such as from contrast agents used in imaging studies, can trigger thyroid storm in individuals with underlying hyperthyroidism. The additional iodine can stimulate further thyroid hormone release and exacerbate the condition.
Incorrect choices:
a. Prolonged exposure to cold temperatures is not a common trigger for thyroid storm.
c. Parathyroid hormone is not directly involved in thyroid hormone regulation and does not trigger thyroid storm.
d. Bacterial infections are not a common trigger for thyroid storm.
The nurse is assessing a client suspected of experiencing thyroid storm. Which cardiovascular manifestation is commonly associated with thyroid storm?
Explanation
Hypertension is a common cardiovascular manifestation of thyroid storm. The excessive release of thyroid hormones leads to increased cardiac output, resulting in elevated blood pressure.
The nurse is caring for a client diagnosed with thyroid storm. Which ocular manifestation should the nurse closely monitor for in this client?
Explanation
Exophthalmos, or protruding eyeballs, is an ocular manifestation commonly associated with thyroid storm. It is caused by the accumulation of fluid and tissue behind the eyes, often seen in Graves' disease.
The nurse is assessing a client with suspected thyroid storm. Which gastrointestinal manifestation is frequently observed in clients experiencing thyroid storm?
Explanation
Diarrhea is a common gastrointestinal manifestation of thyroid storm. The increased metabolic rate and hyperactivity of the digestive system can lead to frequent bowel movements and loose stools.
The nurse is educating a client about the potential manifestations of thyroid storm. Which neuromuscular manifestation should the nurse include in the teaching?
Explanation
Muscle weakness is a neuromuscular manifestation commonly observed in clients experiencing thyroid storm. It is attributed to the hypermetabolic state and increased breakdown of muscle tissue.
The nurse is assessing a client with suspected thyroid storm. Which respiratory manifestation should the nurse anticipate in this client?
Explanation
Hyperventilation, or rapid and deep breathing, is a respiratory manifestation commonly observed in clients with thyroid storm. The increased metabolic rate and elevated body temperature contribute to respiratory alkalosis and hyperventilation.
Incorrect choices:
a. Bradypnea, or slow breathing, is not a characteristic respiratory manifestation of thyroid storm.
c. Wheezing is not commonly associated with thyroid storm and is more indicative of respiratory conditions such as asthma.
d. Decreased respiratory rate is not a typical manifestation of thyroid storm, as clients often experience rapid breathing due to the hypermetabolic state.
The nurse is caring for a client suspected of having thyroid storm. Which laboratory test is commonly used to assess thyroid function and diagnose thyroid storm?
Explanation
Measuring thyroid hormone levels, specifically triiodothyronine (T3) and thyroxine (T4), is an essential diagnostic evaluation for thyroid storm. Elevated levels of these hormones indicate excessive thyroid hormone production and are indicative of thyroid storm.
The nurse is reviewing diagnostic tests for a client suspected of experiencing thyroid storm. Which imaging study can provide information about the size and activity of the thyroid gland?
Explanation
A thyroid ultrasound is a diagnostic tool that can assess the size, structure, and activity of the thyroid gland. It provides information about the presence of any thyroid nodules, enlargement, or abnormalities.
The nurse is assessing a client with suspected thyroid storm. Which diagnostic test is used to evaluate the presence of thyroid autoantibodies and diagnose autoimmune thyroid conditions?
Explanation
The thyroid peroxidase antibody (TPOAb) test is used to detect the presence of antibodies against thyroid peroxidase, an enzyme involved in thyroid hormone production. Elevated TPOAb levels indicate autoimmune thyroid conditions, which can contribute to thyroid storm.
The nurse is caring for a client with suspected thyroid storm. Which diagnostic test is used to visualize the structure and function of the thyroid gland, as well as assess for the presence of thyroid nodules or tumors?
Explanation
A thyroid ultrasound is a non-invasive imaging test that provides detailed images of the thyroid gland. It can help visualize the gland's structure, identify nodules or tumors, and assess for abnormalities.
The nurse is educating a client about diagnostic evaluations for thyroid storm. Which diagnostic test involves administering a radioactive tracer and measuring its uptake by the thyroid gland?
Explanation
The radioactive iodine uptake test involves administering a small amount of radioactive iodine and measuring its uptake by the thyroid gland. This test assesses the thyroid's ability to take up iodine and produce thyroid hormones.
Incorrect choices:
a. Thyroid ultrasound is used to visualize the thyroid gland's structure and function but does not involve the use of radioactive tracers.
c. Thyroid-stimulating hormone (TSH) level is a blood test that measures the pituitary gland's response to thyroid hormone levels.
d. Thyroid peroxidase antibody (TPOAb) test detects the presence of thyroid autoantibodies and is used to diagnose autoimmune thyroid conditions.
The nurse is caring for a client diagnosed with thyroid storm. Which medication is commonly used to block the synthesis of thyroid hormones and manage thyroid storm?
Explanation
Methimazole is an antithyroid medication that inhibits the synthesis of thyroid hormones by blocking the enzyme thyroid peroxidase. It is often used as part of the medical management of thyroid storm to decrease excessive thyroid hormone production.
The nurse is administering medications to a client with thyroid storm. Which medication should the nurse administer to reduce heart rate and alleviate symptoms of hyperthyroidism?
Explanation
Propranolol is a beta-blocker that helps reduce heart rate and manage symptoms such as palpitations, tremors, and anxiety associated with thyroid storm.
The nurse is caring for a client with thyroid storm. Which medication is administered to inhibit the release of thyroid hormones and manage thyroid storm?
Explanation
Propylthiouracil (PTU) is an antithyroid medication that blocks the synthesis of thyroid hormones and inhibits the conversion of thyroxine (T4) to triiodothyronine (T3). It is used to manage thyroid storm and decrease thyroid hormone levels.
The nurse is caring for a client with thyroid storm. Which medication should the nurse administer to restore normal heart rhythm and manage cardiac manifestations?
Explanation
Potassium iodide is administered to block the release of thyroid hormones and manage thyroid storm. It helps restore normal heart rhythm and reduce cardiac manifestations.
The nurse is educating a client about medications used in the management of thyroid storm. Which medication should the nurse explain is used to temporarily reduce thyroid hormone release and manage severe hyperthyroidism?
Explanation
Sodium polystyrene sulfonate (Kayexalate) is used to bind excess thyroid hormones and temporarily reduce their release. It is part of the medical management of thyroid storm to manage severe hyperthyroidism.
Incorrect choices:
a. Levothyroxine (Synthroid) is a thyroid hormone replacement medication used to treat hypothyroidism and would exacerbate thyroid storm if given.
b. Methimazole (Tapazole) is an antithyroid medication that inhibits thyroid hormone synthesis and is used to manage thyroid storm, but it does not temporarily reduce thyroid hormone release.
c. Propranolol (Inderal) is a beta-blocker used to manage symptoms of hyperthyroidism but does not directly reduce thyroid hormone release.
The nurse is caring for a client with thyroid storm. Which medication is the most appropriate for the management of thyroid storm?
Explanation
Methimazole is an antithyroid medication that inhibits the production of thyroid hormones and is commonly used in the management of thyroid storm to reduce thyroid hormone levels.
Incorrect choices:
a. Levothyroxine (Synthroid) is a thyroid hormone replacement medication and is contraindicated in the treatment of thyroid storm, as it would worsen the hyperthyroid state.
c. Propranolol (Inderal) is a beta-blocker that can help control symptoms such as tachycardia and hypertension in thyroid storm, but it does not address the underlying thyroid hormone excess.
d. Liothyronine (Cytomel) is a thyroid hormone replacement medication and is contraindicated in the treatment of thyroid storm, as it would worsen the hyperthyroid state.
The nurse is caring for a client with thyroid storm. In addition to antithyroid medications, which medication should the nurse anticipate administering to alleviate symptoms of increased heart rate and anxiety?
Explanation
Propranolol is a beta-blocker that can help control symptoms such as tachycardia and anxiety by blocking the effects of excess thyroid hormones on the heart.
Incorrect choices:
a. Furosemide (Lasix) is a diuretic and is not indicated for the management of symptoms in thyroid storm.
b. Atropine is not typically used to manage symptoms in thyroid storm, and it may increase heart rate.
d. Digoxin (Lanoxin) is used to treat heart failure and is not typically used to manage symptoms in thyroid storm.
The nurse is caring for a client with thyroid storm. Which electrolyte imbalance is commonly associated with thyroid storm and requires monitoring and correction?
Explanation
Thyroid storm can lead to increased metabolism and utilization of electrolytes, including potassium. Hypokalemia may develop and requires monitoring and correction.
Incorrect choices:
a. Hyperkalemia is not commonly associated with thyroid storm and is less likely to occur.
c. Hypercalcemia is not a typical electrolyte imbalance in thyroid storm.
d. Hypocalcemia is not a typical electrolyte imbalance in thyroid storm.
The nurse is caring for a client with thyroid storm. Which intervention is important in maintaining a safe and quiet environment for the client?
Explanation
Minimizing external stimuli and noise helps reduce stress and anxiety for the client with thyroid storm and promotes a calm and safe environment.
Incorrect choices:
a. Administering sedatives may be necessary, but it is not the primary intervention to maintain a safe environment.
b. Providing a dark and dimly lit room is not necessary and may contribute to feelings of isolation.
c. Encouraging social interaction may not be appropriate for a client experiencing symptoms of thyroid storm, as rest and reduced stimuli are important.
The nurse is providing care for a client with thyroid storm. Which vital sign is crucial for the nurse to monitor frequently to assess the client's response to treatment?
Explanation
Body temperature is a crucial indicator of thyroid storm severity and response to treatment. Monitoring body temperature helps assess the effectiveness of interventions in reducing hyperthermia.
Incorrect choices:
a. Blood pressure is important to monitor, but body temperature provides more direct information about the client's metabolic state.
b. Respiratory rate and oxygen saturation are important indicators of respiratory status but may not directly reflect thyroid storm severity.
d. Oxygen saturation is important for assessing respiratory status but may not directly reflect thyroid storm severity or treatment response.
The nurse is caring for a client with thyroid storm. Which intervention should the nurse prioritize in the management of this condition?
Explanation
Administering antithyroid medications, such as propylthiouracil (PTU) or methimazole, is a priority in managing thyroid storm. These medications inhibit the production of thyroid hormones and help control the hyperthyroid state.
Incorrect choices:
b. Initiating high-dose thyroid hormone replacement therapy is not appropriate for thyroid storm, as the goal is to reduce thyroid hormone levels, not increase them.
c. While intravenous fluid resuscitation may be necessary to manage dehydration and electrolyte imbalances associated with thyroid storm, it is not the initial priority intervention.
d. Encouraging physical activity is contraindicated in thyroid storm, as it can exacerbate symptoms and increase the risk of complications.
The nurse is providing care for a client with thyroid storm. Which nursing intervention is essential to prevent complications in this client?
Explanation
Thyroid storm can suppress the immune system, making the client more susceptible to infections. Monitoring for signs of infection, such as fever, increased white blood cell count, and localized redness, helps prevent and promptly address complications.
Incorrect choices:
a. Administering supplemental iodine is not indicated in thyroid storm management and could worsen the condition.
c. While adequate nutrition is important, encouraging a high-calorie, high-protein diet is not a priority intervention in thyroid storm.
d. Administering intravenous potassium supplements is not a standard intervention for thyroid storm. Electrolyte imbalances may occur, but potassium replacement should be based on laboratory values.
The nurse is providing care to a client with thyroid storm. Which intervention should the nurse implement to promote a safe environment for the client?
Explanation
Thyroid storm can lead to increased metabolism and utilization of glucose, potentially causing hypoglycemia. Monitoring blood glucose levels and assessing for signs of hypoglycemia is important to prevent complications.
Incorrect choices:
a. Keeping the room warm is not necessary and may exacerbate the client's hypermetabolic state. A comfortable room temperature is sufficient.
c. Strenuous physical activity is contraindicated in thyroid storm and can worsen symptoms. Rest is recommended.
d. Administering sedatives can mask the client's true condition and may not be appropriate for a client in thyroid storm.
The nurse is caring for a client with thyroid storm. Which intervention is essential to manage hyperthermia in this client?
Explanation
Applying cold packs to the client's skin helps lower body temperature and manage hyperthermia associated with thyroid storm.
Incorrect choices:
a. Administering acetaminophen (Tylenol) alone may not effectively manage hyperthermia in thyroid storm. Cooling measures, such as cold packs, are more appropriate.
c. Administering antihistamines is not a standard intervention for managing hyperthermia in thyroid storm.
d. Encouraging warm baths is contraindicated in thyroid storm, as it can exacerbate hyperthermia. Cold measures are preferred.
The nurse is providing care for a client with thyroid storm. Which intervention is important to address fluid and electrolyte imbalances in this client?
Explanation
Monitoring intake and output is important to assess fluid balance and prevent dehydration or fluid overload, which can occur in thyroid storm.
Incorrect choices:
a. Administering diuretics is not typically indicated in thyroid storm management and may exacerbate fluid and electrolyte imbalances.
c. Restricting fluid intake is not appropriate in thyroid storm, as clients may require intravenous fluids to maintain hydration.
d. Encouraging high-sodium foods is not a priority intervention in thyroid storm and may exacerbate fluid and electrolyte imbalances.
The nurse is providing education to a client with a history of hyperthyroidism about preventing thyroid storm. Which statement by the client indicates a need for further education?
Explanation
Regular follow-up appointments are essential for monitoring thyroid function and adjusting medication doses if necessary. Skipping appointments even when feeling well can lead to inadequate management and potential risk of thyroid storm.
Incorrect choices:
a. This choice is correct. Taking antithyroid medication as prescribed helps to regulate thyroid hormone levels and prevent hyperthyroidism, reducing the risk of thyroid storm.
b. This choice is correct. Stress management and relaxation techniques can help prevent exacerbation of hyperthyroidism and decrease the risk of thyroid storm.
d. This choice is correct. Notifying the healthcare provider about palpitations or rapid heartbeat is important to address potential worsening of hyperthyroidism and prevent thyroid storm.
The nurse is discussing strategies to prevent thyroid storm with a client who recently underwent radioactive iodine therapy for hyperthyroidism. Which statement by the client indicates understanding of the teaching?
Explanation
After radioactive iodine therapy, it may take several weeks for thyroid hormone levels to normalize. Continuing antithyroid medication during this period helps prevent exacerbation of hyperthyroidism and potential thyroid storm.
Incorrect choices:
a. This choice is incorrect. While avoiding excessive iodine intake is important, avoiding all foods high in iodine is unnecessary and could lead to nutritional deficiencies.
b. This choice is incorrect. Strenuous physical activity can exacerbate hyperthyroidism and increase the risk of thyroid storm. Moderation in physical activity is recommended.
c. This choice is incorrect. Stopping antithyroid medication after radioactive iodine therapy is not recommended, as thyroid hormone levels may not immediately normalize.
The nurse is teaching a client with hyperthyroidism about measures to prevent thyroid storm. Which statement by the client indicates a need for further education?
Explanation
Consuming foods rich in iodine can exacerbate hyperthyroidism and increase the risk of thyroid storm. Iodine is a component of thyroid hormones, and excess intake can worsen thyroid hormone production.
Incorrect choices:
a. This choice is correct. Over-the-counter medications containing pseudoephedrine can stimulate the sympathetic nervous system and exacerbate hyperthyroidism, leading to thyroid storm.
b. This choice is correct. Staying cool in hot weather helps prevent excessive heat stress on the body and minimizes sympathetic nervous system activity that can exacerbate hyperthyroidism.
d. This choice is correct. Reporting signs of infection or illness is important to ensure timely medical attention and prevent potential exacerbation of hyperthyroidism or thyroid storm.
The nurse is providing discharge instructions to a client who experienced thyroid storm and has been stabilized. Which statement by the client indicates a need for further education?
Explanation
Increasing intake of iodized salt can exacerbate hyperthyroidism and increase the risk of thyroid storm. Clients with hyperthyroidism are often advised to reduce iodine intake.
Incorrect choices:
a. This choice is correct. Continuing to take beta-blocker medication helps control heart rate and sympathetic nervous system effects, reducing the risk of thyroid storm.
b. This choice is correct. Exposure to extreme cold temperatures can trigger sympathetic nervous system activity and worsen hyperthyroidism or thyroid storm.
c. This choice is correct. Regular follow-up appointments with the healthcare provider are important to monitor thyroid function and adjust treatment as needed to prevent recurrence of thyroid storm.
The nurse is caring for a client who is newly diagnosed with hyperthyroidism. Which action by the client indicates effective prevention of thyroid storm?
Explanation
Consistently taking antithyroid medications helps regulate thyroid hormone levels and prevent exacerbation of hyperthyroidism, reducing the risk of thyroid storm.
Incorrect choices:
a. This choice is correct. High-intensity interval training can exacerbate hyperthyroidism and increase the risk of thyroid storm. Moderate exercise is recommended.
c. This choice is correct. Consuming large amounts of caffeine can stimulate the sympathetic nervous system and worsen hyperthyroidism, leading to thyroid storm.
d. This choice is correct. While seafood is a source of iodine, consuming excessive amounts can exacerbate hyperthyroidism and increase the risk of thyroid storm. Moderate iodine intake is recommended.
The nurse is caring for a client who is experiencing a thyroid storm. Which assessment finding would the nurse expect to observe?
Explanation
Thyroid storm is a life-threatening condition characterized by severe hyperthyroidism. Hypertension is a common manifestation of thyroid storm, along with tachycardia, fever, and other signs of sympathetic nervous system overactivity.
Incorrect choices:
a. This choice is incorrect. Bradycardia is not a typical finding in thyroid storm. Tachycardia is more common due to increased sympathetic activity.
b. This choice is incorrect. Thyroid storm is associated with hyperthermia, not hypothermia.
d. This choice is incorrect. Weight loss, rather than weight gain, is a characteristic feature of hyperthyroidism, including thyroid storm.
The nurse is assessing a client suspected of having thyroid storm. Which finding would be of immediate concern and require prompt intervention?
Explanation
Restlessness and agitation are signs of increased sympathetic nervous system activity and can indicate the severity of thyroid storm. Prompt intervention is required to prevent further deterioration.
Incorrect choices:
a. This choice is incorrect. Diarrhea can be a symptom of thyroid storm, but it is not an immediate concern that requires urgent intervention.
c. This choice is incorrect. Increased appetite is not a characteristic feature of thyroid storm. In fact, clients with thyroid storm often have decreased appetite due to the severity of their condition.
d. This choice is incorrect. Muscle weakness is a symptom of hyperthyroidism but is not an immediate concern that requires urgent intervention.
The nurse is caring for a client with thyroid storm. Which medication would the nurse anticipate being administered as a priority?
Explanation
Propranolol is a beta-blocker that helps manage the cardiovascular symptoms of thyroid storm, such as tachycardia and hypertension. It is often administered as a priority to stabilize the client's condition.
Incorrect choices:
a. This choice is incorrect. Levothyroxine is a thyroid hormone replacement medication and would not be administered as a priority in the acute management of thyroid storm.
b. This choice is incorrect. Methimazole is an antithyroid medication used to block thyroid hormone production. It is important for long-term management but may not be administered as a priority during a thyroid storm crisis.
d. This choice is incorrect. Calcium gluconate may be administered to address the potential risk of hypocalcemia associated with thyroid storm, but it is not typically administered as a first-line priority medication.
The nurse is providing education to a client with a history of hyperthyroidism about the importance of managing stress. Which rationale should the nurse provide to the client?
Explanation
Stress is a known trigger for thyroid storm in individuals with a history of hyperthyroidism. Effective stress management can help reduce the risk of thyroid storm episodes.
Incorrect choices:
b. This choice is incorrect. Stress reduction is important to prevent exacerbation of hyperthyroidism and the risk of thyroid storm, not to increase thyroid hormone production.
c. This choice is incorrect. Stress management primarily aims to prevent thyroid storm and manage hyperthyroidism, not hypothyroidism.
d. This choice is incorrect. Stress reduction helps manage hyperthyroidism and prevent thyroid storm but does not necessarily "normalize" thyroid hormone levels.
The nurse is assessing a client with thyroid storm. Which finding would be consistent with the increased metabolic rate associated with this condition?
Explanation
Thyroid storm is characterized by an increased metabolic rate, leading to hyperglycemia. The increased metabolic demand and stress response can result in elevated blood glucose levels.
Incorrect choices:
a. This choice is incorrect. Thyroid storm is associated with hypertension, not hypotension.
b. This choice is incorrect. Thyroid storm is associated with tachycardia, not bradycardia.
c. This choice is incorrect. Thyroid storm is associated with hyperthermia, not hypothermia.
The nurse is caring for a client who is experiencing a thyroid storm. Which assessment finding would the nurse prioritize as an early sign of thyroid storm?
Explanation
Tremors, restlessness, and anxiety are early signs of thyroid storm. Thyroid storm is a life-threatening condition characterized by an excessive release of thyroid hormones, leading to hypermetabolic state.
Incorrect choices:
a. This choice is incorrect. Bradycardia is not typically associated with thyroid storm. Tachycardia is more common due to increased sympathetic activity.
b. This choice is incorrect. Thyroid storm is associated with hyperthermia, not hypothermia. Increased metabolic rate leads to elevated body temperature.
d. This choice is incorrect. Decreased appetite is not a priority assessment finding in thyroid storm. More significant symptoms such as agitation and tachycardia take precedence.
The nurse is preparing a plan of care for a client with thyroid storm. Which nursing intervention would be the highest priority?
Explanation
Administering beta-blockers is a priority intervention in thyroid storm to reduce heart rate and control sympathetic nervous system effects. Thyroid storm is characterized by severe tachycardia and increased sympathetic activity.
Incorrect choices:
a. This choice is incorrect. Administering thyroid replacement hormones is not a priority intervention in the acute management of thyroid storm.
b. This choice is incorrect. While fever may occur in thyroid storm, addressing tachycardia and sympathetic overactivity is of higher priority.
c. This choice is incorrect. Monitoring blood glucose levels is important, but addressing the severe tachycardia and other immediate symptoms takes precedence.
The nurse is educating a client with hyperthyroidism about thyroid storm. Which statement by the client indicates a need for further education?
Explanation
Diarrhea, not constipation, is a common gastrointestinal symptom associated with thyroid storm. Increased metabolic rate in thyroid storm can lead to diarrhea.
Incorrect choices:
a. This choice is correct. Taking antithyroid medications as prescribed is important to control thyroid hormone levels and prevent thyroid storm.
b. This choice is correct. Avoiding stress and practicing relaxation techniques can help manage sympathetic overactivity and prevent exacerbation of thyroid storm.
c. This choice is correct. Monitoring heart rate and reporting irregularities is essential for early detection of worsening symptoms in thyroid storm.
The nurse is assessing a client with suspected thyroid storm. Which finding would the nurse anticipate during the assessment?
Explanation
Exophthalmos (protruding eyeballs) is a characteristic finding in thyroid storm due to increased sympathetic activity and inflammation of the orbital tissues.
Incorrect choices:
a. This choice is incorrect. Thyroid storm is characterized by tachycardia, not bradycardia.
b. This choice is incorrect. Thyroid storm is associated with hyperthermia, not hypothermia.
c. This choice is incorrect. Low blood pressure is not a typical finding in thyroid storm. Hypertension and tachycardia are more common.
The nurse is caring for a client with thyroid storm. Which laboratory finding would the nurse anticipate in this condition?
Explanation
Thyroid storm is characterized by significantly elevated levels of T3 and T4, the thyroid hormones.
Incorrect choices:
a. This choice is incorrect. Elevated TSH levels are not expected in thyroid storm. TSH would be suppressed due to high thyroid hormone levels.
c. This choice is incorrect. Low T3 and T4 levels are not indicative of thyroid storm. Thyroid storm is associated with excess thyroid hormone release.
d. This choice is incorrect. Normal TSH levels would not be seen in thyroid storm, as TSH would be suppressed due to elevated thyroid hormone levels.
Exams on Endocrine Systems
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
I. Define Diabetes Mellitus:
- Differentiate between Type 1 and Type 2 diabetes in terms of pathophysiology, etiology, and clinical manifestations.
- Explain the role of insulin in glucose metabolism and its deficiency in diabetes.
II. Describe Thyroid Disorders:
-
Identify the major thyroid hormones (T3, T4) and their functions in regulating metabolism, growth, and development.
-
Explain the role of the hypothalamus-pituitary-thyroid axis in thyroid hormone regulation.
III. Understand Diagnostic Methods:
-
Differentiate between fasting plasma glucose, oral glucose tolerance test, and hemoglobin A1c as diagnostic tests for diabetes mellitus.
-
Describe the use of thyroid function tests (TSH, T3, T4) in diagnosing thyroid disorders.
IV. Explain Complications:
-
Identify acute complications of diabetes mellitus, including hypoglycemia, diabetic ketoacidosis (DKA), and hyperosmolar hyperglycemic state (HHS).
-
Discuss the chronic complications of diabetes, such as neuropathy, nephropathy, retinopathy, and cardiovascular disease.
-
Describe potential complications of thyroid disorders, including hyperthyroidism (thyrotoxicosis) and hypothyroidism.
V. Discuss Treatment Strategies:
-
Outline the principles of diabetes management, including lifestyle modifications (diet, exercise), oral medications, and insulin therapy.
-
Describe the treatment options for thyroid disorders, including anti-thyroid drugs, radioactive iodine therapy, and thyroidectomy.
VI. Identify Nursing Interventions:
-
Discuss nursing interventions to prevent and manage acute complications of diabetes, such as monitoring blood glucose levels and administering insulin.
-
Describe nursing care for patients undergoing radioactive iodine therapy or thyroidectomy, including monitoring for complications and patient education.
VII. Educate Patients:
-
Develop patient education plans to promote self-care and glycemic control in diabetes mellitus, including medication administration, blood glucose monitoring, and recognizing signs of hypo/hyperglycemia.
-
Provide patient education on thyroid disorders, emphasizing the importance of medication adherence, potential side effects, and the need for regular follow-up.
VIII. Consider Special Populations:
-
Discuss the unique considerations and challenges in managing diabetes and thyroid disorders in pregnant individuals.
-
Address the impact of thyroid disorders on pediatric and geriatric populations, including appropriate dosing adjustments and monitoring.
IX. Interpret Clinical Scenarios:
-
Analyze case studies or clinical scenarios involving diabetes and thyroid disorders to apply theoretical knowledge in real-world situations.
-
Formulate nursing care plans based on patient assessments and diagnoses related to endocrine system dysfunctions.
X. Promote Patient Safety:
-
Recognize potential medication interactions and contraindications for patients with diabetes and thyroid disorders.
-
Implement measures to ensure patient safety during insulin administration, radioactive iodine therapy, or surgical procedures.
Diabetes Mellitus
Introduction
Diabetes mellitus is a intricate and chronic metabolic disorder that profoundly impacts the body's ability to regulate glucose, the primary source of energy.
This condition arises due to disruptions in insulin production, utilization, or both, leading to elevated blood glucose levels.
Comprehensive understanding of diabetes mellitus involves delving into its pathophysiology, classification, clinical manifestations, diagnostic methods, treatment approaches, and potential complications.

Pathophysiology
Diabetes mellitus is rooted in the intricate interplay between insulin, a hormone produced by the pancreas, and glucose, the body's key energy source.
The two primary forms of diabetes, Type 1 and Type 2, have distinct pathophysiological mechanisms:
- Type 1 Diabetes (T1D):
- Autoimmune Attack: T1D is marked by an autoimmune assault on the pancreatic beta cells responsible for insulin production. This results in an absolute deficiency of insulin.
- Genetic Predisposition: Genetic factors contribute to susceptibility, while environmental triggers like viral infections may initiate the autoimmune response.
- Hyperglycemia Emergence: The lack of insulin hinders glucose uptake, leading to hyperglycemia, which is characteristic of T1D.
- Type 2 Diabetes (T2D):
- Insulin Resistance: T2D primarily stems from insulin resistance, where cells become less responsive to insulin signals, reducing glucose uptake.
- Beta Cell Dysfunction: The pancreas may struggle to produce enough insulin over time, contributing to relative insulin deficiency.
- Obesity and Lifestyle: Obesity, sedentary behavior, and genetics play pivotal roles in T2D development.

Classification
In addition to Type 1 and Type 2, diabetes mellitus includes other variants:
- Gestational Diabetes: Occurs during pregnancy and requires careful management to prevent maternal and fetal complications.
- Secondary Diabetes: Arises from other conditions, such as pancreatic disorders or certain medications.
- Monogenic Diabetes: Results from single-gene mutations affecting insulin production or action.
Clinical Manifestations
Diabetes mellitus manifests through a spectrum of symptoms:
- Polyuria: Excessive urination due to glucose-spiked urine.
- Polydipsia: Unquenchable thirst driven by fluid loss.
- Polyphagia: Intense hunger as cells starve despite high glucose levels.
- Weight Loss: Body metabolizes fat and muscle for energy.
- Fatigue: Cells' energy deprivation leads to persistent tiredness.
- Blurred Vision: High glucose affects the lens, leading to visual disturbances.
Diagnosis
Diagnosing diabetes involves assessing various parameters:
- Fasting Plasma Glucose Test: Measures glucose after an overnight fast.
- Oral Glucose Tolerance Test: Evaluates glucose response after consuming a glucose-rich beverage.
- Hemoglobin A1c (HbA1c) Test: Provides a retrospective view of blood glucose control over several months.
Treatment
Comprehensive diabetes management strategies encompass multiple facets:
- Lifestyle Modifications: Balanced diet, regular exercise, stress management, and weight control are pivotal in glycemic control.
- Oral Medications: For T2D, oral antidiabetic drugs enhance insulin sensitivity or stimulate insulin production.
- Insulin Therapy: Essential for T1D and may be required in advanced T2D cases.
Complications
Acute Complications: Acute complications of diabetes often arise suddenly and require immediate attention and intervention.
- Hypoglycemia:
- Definition: Hypoglycemia is characterized by abnormally low blood glucose levels, usually below 70 mg/dL.
- Symptoms: Shakiness, sweating, palpitations, confusion, irritability, dizziness, and hunger.
- Treatment: Rapid consumption of glucose-rich foods or drinks to raise blood sugar levels.
- Diabetic Ketoacidosis (DKA):
- Definition: DKA results from severe insulin deficiency, leading to the breakdown of fats for energy and the production of acidic ketones.
- Symptoms: Excessive thirst, frequent urination, nausea, vomiting, abdominal pain, fruity breath odor.
- Treatment: Insulin therapy, fluid replacement, and electrolyte correction under medical supervision.
- Hyperosmolar Hyperglycemic State (HHS):
- Definition: HHS occurs when blood glucose levels rise very high, causing extreme dehydration and an altered mental state.
- Symptoms: Profound dehydration, confusion, lethargy, seizures, and coma.
- Treatment: Fluid replacement, insulin therapy, and addressing underlying triggers.
Chronic Complications: Chronic complications of diabetes develop over time due to prolonged exposure to high blood glucose levels.
- Cardiovascular Complications:
- Chronic Effects: Elevated glucose levels contribute to atherosclerosis, increasing the risk of heart attacks, stroke, and peripheral artery disease.
- Long-Term Impact: Chronic cardiovascular complications are a leading cause of morbidity and mortality in diabetes.
- Neuropathy:
- Chronic Effects: Nerve damage can lead to peripheral neuropathy (numbness, tingling), autonomic neuropathy (digestive, and urinary issues), and neuropathic pain.
- Long-Term Impact: Neuropathy affects quality of life, increases susceptibility to injuries, and can lead to foot ulcers and amputations.
- Nephropathy:
- Chronic Effects: High blood glucose damages kidney vessels, leading to diabetic nephropathy and potential kidney failure (end-stage renal disease).
- Long-Term Impact: Diabetic nephropathy is a significant cause of chronic kidney disease and necessitates dialysis or transplantation.
- Retinopathy:
- Chronic Effects: Elevated glucose levels damage retinal blood vessels, causing diabetic retinopathy, and leading to vision impairment and blindness.
- Long-Term Impact: Diabetic retinopathy is a leading cause of blindness in adults.
- Foot Complications:
- Chronic Effects: Neuropathy and poor circulation contribute to diabetic foot ulcers, which may lead to infections and, in severe cases, amputations.
- Long-Term Impact: Foot complications are a major source of morbidity and disability in diabetes.
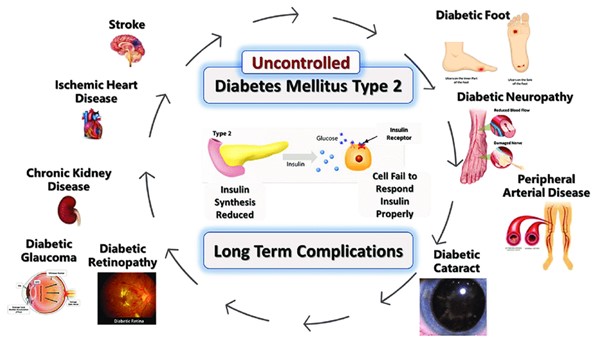
Patient Education
Empowering individuals with diabetes through education is paramount:
- Blood Glucose Monitoring: Regular self-monitoring informs management decisions.
- Medication Management: Understanding prescribed medications and administration methods is crucial.
- Carbohydrate Counting: Knowing how to adjust insulin doses based on carbohydrate intake enhances glycemic control.
- Lifestyle Adherence: Embracing a healthy lifestyle, stress reduction, and regular medical check-ups are essential.
Conclusion
In essence, diabetes mellitus represents a multifaceted metabolic disorder with widespread implications. A comprehensive grasp of its intricacies is imperative for healthcare professionals to offer tailored care, guide patients in effective self-management, and mitigate the potential complications that can arise from uncontrolled blood glucose levels.

Diabetes Insipidus
Diabetes insipidus (DI) is a rare but significant endocrine disorder that disrupts the body's ability to regulate fluid balance, leading to excessive urination and thirst.
Unlike diabetes mellitus, which involves glucose metabolism, diabetes insipidus focuses on water balance regulation.
This condition arises from insufficient production or utilization of antidiuretic hormone (ADH), also known as vasopressin. Understanding the causes, types, clinical manifestations, diagnosis, and management of diabetes insipidus provides insights into this unique disorder.
Pathophysiology
Diabetes insipidus occurs due to disruptions in the synthesis, release, or action of ADH, which plays a crucial role in regulating water reabsorption in the kidneys.
This disruption leads to reduced water reabsorption, resulting in excessive urine production and subsequent dehydration.
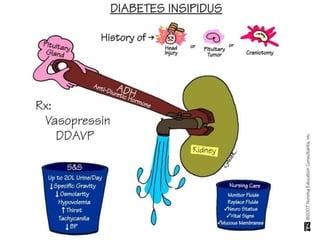
Types of Diabetes Insipidus
There are several forms of diabetes insipidus, each with distinct causes:
- Central Diabetes Insipidus (CDI):
- Cause: Results from inadequate production or release of ADH by the hypothalamus or posterior pituitary gland.
- Etiology: Can be idiopathic (unknown cause), genetic, or due to head trauma, tumors, infections, or certain medications.
- Nephrogenic Diabetes Insipidus (NDI):
- Cause: Results from kidneys' inability to respond to ADH, leading to reduced water reabsorption.
- Etiology: Often genetic, acquired due to kidney disease, medications (e.g., lithium), or electrolyte imbalances.
- Gestational Diabetes Insipidus:
- Cause: Transient form occurring during pregnancy due to increased metabolism of ADH by the placenta.
- Etiology: Typically resolves after childbirth.
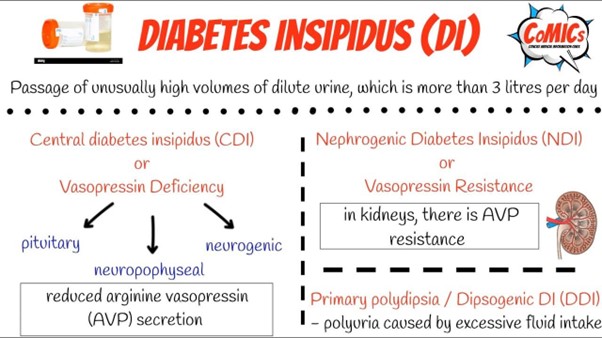
Clinical Manifestations
The hallmark symptoms of diabetes insipidus include:
- Polyuria: Excessive urine production, leading to frequent urination and large volumes of dilute urine.
- Polydipsia: Intense thirst to compensate for fluid loss.
- Nocturia: Frequent urination during the night, disrupting sleep.
- Dehydration: Due to fluid loss, individuals may experience dry mouth, dry skin, and fatigue.
Diagnosis
Diagnosing diabetes insipidus involves several steps:
- Fluid Deprivation Test: Monitoring changes in urine output and concentration after restricting fluid intake.
- Desmopressin Test: Administering synthetic ADH to differentiate between central and nephrogenic forms.
Management
Effective management of diabetes insipidus depends on the underlying cause:
Central Diabetes Insipidus (CDI):
- Desmopressin: Synthetic ADH replacement therapy via nasal spray, tablet, or injection.
- Monitoring: Regular assessment of urine output, thirst, and electrolyte levels.
Nephrogenic Diabetes Insipidus (NDI):
- Treat Underlying Cause: Addressing the root cause, such as discontinuing offending medications.
- Hydration: Ensuring adequate fluid intake to counteract excessive urine production.
Gestational Diabetes Insipidus:
- Monitoring: Regular evaluation during pregnancy, with symptoms often resolving postpartum.
Long-Term Outlook
With proper management, most individuals with diabetes insipidus can lead normal lives. Monitoring fluid intake, recognizing symptoms of dehydration, and adhering to treatment plans are crucial for preventing complications and maintaining optimal fluid balance.
Conclusion
In conclusion, diabetes insipidus is a distinct endocrine disorder characterized by disrupted water balance regulation, leading to excessive urination and thirst.
Understanding the types, causes, clinical manifestations, diagnosis, and management of diabetes insipidus empowers healthcare professionals to provide comprehensive care and improve the quality of life for individuals living with this condition.
Diabetic Foot care
Introduction
Diabetic foot care is a critical aspect of diabetes management as individuals with diabetes are at a higher risk of developing foot complications due to reduced blood flow, nerve damage (neuropathy), and impaired wound healing.
Proper foot care can help prevent diabetic foot ulcers, infections, and potential amputations.
Understanding diabetic foot care is crucial for healthcare professionals to educate patients and provide comprehensive care.

Importance of Diabetic Foot Care
A. High Risk Population: Individuals with diabetes are at an increased risk of foot complications due to peripheral neuropathy, peripheral arterial disease (PAD), and immune system impairment.
B. Preventing Foot Ulcers: Diabetic foot ulcers can lead to serious infections and potential amputations, making prevention a priority.
Foot Assessment and Examination
A. Comprehensive Foot Assessment: Healthcare professionals should perform regular foot examinations to assess skin integrity, sensation, circulation, and foot deformities.
B. Monofilament Test: The use of a monofilament is a common method to assess loss of protective sensation in the feet, indicating peripheral neuropathy.
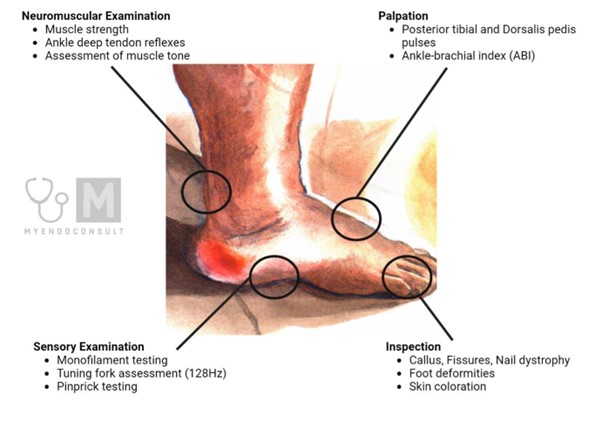
Footwear and Socks
A. Proper Footwear: Patients should wear well-fitting, supportive, and comfortable shoes that protect their feet and prevent pressure points.
B. Socks: Diabetic socks made of moisture-wicking and non-constricting materials can help prevent friction and skin breakdown.
Daily Foot Care
A. Washing and Drying: Patients should wash their feet daily with lukewarm water and mild soap, ensuring to dry them thoroughly, especially between the toes.
B. Moisturizing: Applying a thin layer of moisturizer to the feet, except between the toes, can prevent dry skin and cracking.
Nail Care
A. Trimming Nails: Patients should trim their toenails straight across and avoid cutting into the corners to prevent ingrown toenails and injuries.
B. Professional Foot Care: Patients with decreased sensation or circulation should seek professional podiatry care for nail trimming and callus removal.
Prevention of Injuries
A. Foot Protection: Patients should avoid walking barefoot and protect their feet from extreme temperatures and sharp objects.
B. Foot Elevation: Elevating the feet when sitting or resting can reduce swelling and improve circulation.
Management of Foot Ulcers
A. Early Detection: Patients should be educated about recognizing and reporting any signs of foot ulcers, such as redness, warmth, swelling, or drainage.
B. Prompt Treatment: Immediate medical attention is crucial for early intervention and management of foot ulcers to prevent complications.
Peripheral Arterial Disease (PAD) Screening
A. Ankle-Brachial Index (ABI): Healthcare professionals may perform ABI tests to assess blood flow in the lower extremities and identify PAD.
Patient Education
A. Importance of Self-Care: Patients should be educated about the significance of regular foot care and self-assessment.
B. When to Seek Medical Attention: Patients need to understand the signs of foot complications and when to seek prompt medical attention.
Individualized Care Plans
A. Collaborative Approach: Healthcare professionals should work together to develop individualized foot care plans based on patients' risk factors and needs.
B. Multidisciplinary Team: In complex cases, involving a multidisciplinary team, including podiatrists, wound care specialists, and vascular surgeons, can improve patient outcomes.
Conclusion
In conclusion, diabetic foot care is a crucial component of diabetes management, especially for individuals at higher risk of foot complications due to peripheral neuropathy and PAD.
By understanding the importance of foot assessment, proper footwear, daily foot care, prevention of injuries, and management of foot ulcers, healthcare professionals can educate patients effectively and promote optimal foot health.
Through comprehensive diabetic foot care, healthcare providers can significantly reduce the risk of foot complications and improve the quality of life for individuals living with diabetes.
Insulin therapy
Introduction
Insulin therapy is a crucial component of diabetes management for individuals with type 1 diabetes and some cases of type 2 diabetes.
Insulin is a hormone produced by the beta cells in the pancreas, and it plays a vital role in regulating blood glucose levels.
In diabetes, there is either a deficiency of insulin production or a decreased response to insulin, leading to elevated blood glucose levels.
Insulin therapy aims to supplement or replace the body's insulin to achieve optimal glucose control and prevent complications associated with diabetes.

Types of Insulin
A. Rapid-Acting Insulin:
1. Examples: Insulin lispro, insulin aspart, insulin glulisine.
2. Onset: Rapid, typically within 15 minutes.
3. Peak: Peaks around 1 to 2 hours after injection.
4. Duration: Lasts for about 3 to 5 hours.
5. Administration: Administered just before or immediately after meals to manage postprandial glucose spikes.
B. Short-Acting Insulin (Regular Insulin):
1. Onset: Starts working within 30 minutes.
2. Peak: Peaks around 2 to 3 hours after injection.
3. Duration: Lasts for about 5 to 8 hours.
4. Administration: Usually given 30 minutes before meals to manage pre-meal glucose levels.
C. Intermediate-Acting Insulin:
1. Examples: Neutral protamine Hagedorn (NPH) insulin.
2. Onset: Starts working within 1 to 2 hours.
3. Peak: Peaks around 4 to 6 hours after injection.
4. Duration: Lasts for about 12 to 18 hours.
5. Administration: Usually administered twice daily to manage fasting and between-meal glucose levels.
D. Long-Acting Insulin:
1. Examples: Insulin glargine, insulin detemir, insulin degludec.
2. Onset: Starts working within 1 to 2 hours.
3. Peak: Peakless, providing a relatively constant level of insulin over an extended duration.
4. Duration: Lasts for about 24 hours or longer.
5. Administration: Typically given once daily to provide basal insulin coverage.
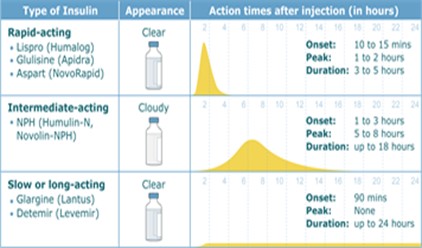
Insulin Administration
A. Subcutaneous Injection: Insulin is administered subcutaneously into the fatty tissue using insulin syringes, insulin pens, or insulin pumps.

B. Insulin Pump Therapy: Insulin pumps deliver a continuous infusion of rapid-acting insulin, mimicking the basal insulin secretion of the pancreas.
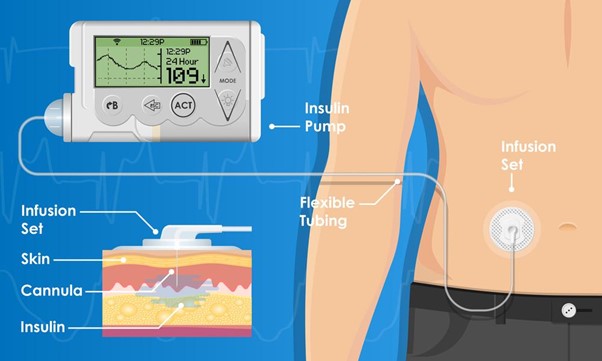
Insulin Dosing
A. Basal-Bolus Regimen: Consists of long-acting insulin for basal coverage and rapid-acting or short-acting insulin before meals for prandial coverage.

B. Sliding Scale Insulin: Used for patients with variable glucose levels; the insulin dose is adjusted based on the current blood glucose level.
Monitoring and Adjusting Insulin Therapy
- Blood Glucose Monitoring:
- Regular blood glucose monitoring is essential to assess how well insulin therapy is working and to identify trends in glucose levels.
- Monitoring before meals, after meals, before exercise, and at bedtime provides valuable information about glucose control throughout the day.
- Self-Monitoring of Blood Glucose (SMBG):
- SMBG involves using a glucometer to check blood glucose levels at home.
- It helps individuals make informed decisions about insulin doses, meal choices, and physical activity.
- Continuous Glucose Monitoring (CGM):
- CGM systems provide real-time glucose readings, offering a more comprehensive view of glucose fluctuations.
- Trends, patterns, and alarms help individuals adjust insulin doses more effectively.
- Insulin Adjustment:
- Insulin doses may need to be adjusted based on blood glucose readings, lifestyle changes, illness, or weight fluctuations.
- Dosage adjustments aim to achieve target blood glucose ranges and prevent hypo- or hyperglycemia.
- Healthcare Provider Involvement:
- A healthcare provider, such as an endocrinologist or diabetes educator, plays a crucial role in guiding insulin adjustments.
- Regular appointments are essential to review blood glucose logs, assess insulin requirements, and make necessary changes.
- Factors Affecting Insulin Needs:
- Physical activity, stress, illness, changes in diet, and hormonal fluctuations can impact insulin sensitivity and requirements.
- Monitoring helps identify these factors and adjust insulin doses accordingly.
- Carbohydrate Counting:
- Individuals who count carbohydrates can adjust insulin doses based on the amount of carbohydrates consumed.
- Accurate carbohydrate counting enables precise insulin adjustments to match meal intake.
- Basal-Bolus Insulin Regimen:
- The basal insulin provides a continuous background level, while bolus insulin is given before meals to cover carbohydrate intake.
- Adjusting basal and bolus insulin doses helps maintain stable blood glucose levels.
- Titration Protocols:
- Healthcare providers may develop titration protocols to guide insulin adjustments based on specific criteria, such as pre-meal and post-meal glucose levels.
- Patient Education:
- Education on insulin therapy, blood glucose monitoring, and insulin adjustments empowers individuals to manage their diabetes effectively.
- Understanding insulin action, timing, and individualized insulin-to-carbohydrate ratios is essential for accurate adjustments.
- Avoiding Rapid Changes:
- Gradual and cautious insulin adjustments are recommended to prevent extreme blood glucose fluctuations and minimize the risk of hypoglycemia.
Insulin Storage and Handling
A. Insulin should be stored properly to maintain its efficacy.
B. Unopened insulin vials and cartridges should be refrigerated, and opened insulin can be stored at room temperature for up to 28 days.
Hypoglycemia Management
Hypoglycemia is a condition characterized by abnormally low blood glucose levels, typically below 70 mg/dL.
It can occur in individuals with diabetes who are taking medications such as insulin or certain oral hypoglycemic agents.
Proper management of hypoglycemia is crucial to prevent complications and ensure the individual's safety and well-being.
- Recognizing Symptoms:
- Hypoglycemia symptoms vary and can include shakiness, sweating, palpitations, confusion, irritability, dizziness, and hunger.
- Immediate action is required when symptoms are observed, especially in individuals with diabetes.
- Rule of 15:
- The "rule of 15" is a common guideline for treating hypoglycemia.
- Consume 15 grams of rapidly absorbed carbohydrates, such as glucose tablets, fruit juice, or regular soda.
- Wait for about 15 minutes and recheck blood glucose levels. If still low, repeat the process.
- Complex Carbohydrates:
- After treating hypoglycemia with the rule of 15 and blood glucose levels stabilize, consume a small snack containing complex carbohydrates and protein to prevent recurrence.
- Glucagon Injection:
- Glucagon is an emergency treatment for severe hypoglycemia when the individual is unconscious or unable to consume carbohydrates.
- Family members or close contacts of individuals with diabetes should be educated on how to administer a glucagon injection.
- Prevention:
- Preventing hypoglycemia is essential. Regular monitoring of blood glucose levels, especially before meals, exercise, and bedtime, helps detect and prevent episodes.
- Adjusting insulin or medication doses under the guidance of a healthcare provider can help prevent frequent hypoglycemia.
- Meal Planning:
- Consistent and balanced meal planning is key to avoiding blood sugar fluctuations.
- Eating meals and snacks at regular intervals, avoiding skipping meals, and including a mix of carbohydrates, proteins, and healthy fats can help stabilize blood glucose levels.
- Exercise Management:
- Individuals on insulin or medications that can cause hypoglycemia should be cautious during physical activity.
- Monitoring blood glucose levels before, during, and after exercise and adjusting carbohydrate intake and insulin doses accordingly can help prevent hypoglycemia.
- Continuous Glucose Monitoring (CGM):
- CGM devices provide real-time blood glucose readings, helping individuals monitor trends and take proactive steps to avoid hypoglycemia.
- Educating Others:
- Individuals with diabetes and their close contacts should be educated about hypoglycemia symptoms, treatment, and glucagon administration.
- Medical alert identification, such as a bracelet or necklace, is important to inform others about the individual's condition in case of emergencies.
- Medical Follow-Up:
- Regular visits to a healthcare provider help monitor and adjust diabetes management, reducing the risk of hypoglycemia.
- Discussing any recurrent hypoglycemic episodes with a healthcare provider is crucial to make necessary changes.
Patient Education
A. Adherence: Patients should be educated about the importance of adhering to their insulin regimen and the potential consequences of missed doses.
B. Injection Technique: Proper injection technique, rotation of injection sites, and needle disposal should be taught.
C. Hypoglycemia Prevention: Patients need to learn strategies to prevent hypoglycemia and how to respond if it occurs.
Conclusion
In conclusion, insulin therapy is a cornerstone of diabetes management, helping individuals achieve glycemic control and prevent complications.
Understanding the types of insulin, insulin administration, dosing strategies, monitoring, and patient education is essential for healthcare professionals to support patients with diabetes in managing their condition effectively.
Through comprehensive insulin therapy, patients can improve their quality of life, reduce the risk of long-term complications, and achieve better glycemic control.
Goitre
Introduction
Goitre, a term derived from the Latin word "guttur" meaning throat, refers to the abnormal enlargement of the thyroid gland, a butterfly-shaped endocrine organ in the neck.
Goitre can develop due to various underlying causes and is a visual manifestation of thyroid dysfunction.
Understanding the types, causes, clinical manifestations, diagnosis, and management of goitre sheds light on this complex condition.

Types of Goitre
Goitre can be classified based on its size, cause, and characteristics:
- Diffuse Goitre: Uniform enlargement of the entire thyroid gland.
- Multinodular Goitre: Characterized by multiple nodules or lumps within the thyroid.
- Solitary Nodule Goitre: A single distinct nodule within the thyroid gland.
- Endemic Goitre: Widespread occurrence in areas with iodine deficiency.
- Toxic Goitre (Graves' Disease): Accompanied by hyperthyroidism due to autoimmune stimulation of the thyroid gland.
- Non-Toxic Goitre: Enlargement without significant changes in thyroid hormone levels.
Causes of Goitre
Several factors contribute to the development of goitre:
- Iodine Deficiency: A lack of dietary iodine, crucial for thyroid hormone synthesis, is a leading cause of endemic goitre.
- Thyroiditis: Inflammation of the thyroid gland can trigger goitre formation.
- Autoimmune Disorders: Conditions like Graves' disease and Hashimoto's thyroiditis can lead to goitre.
- Genetic Factors: Certain genetic mutations may increase the risk of goitre.
- Thyroid Nodules: Benign or cancerous growths within the thyroid can cause enlargement.
Clinical Manifestations
Goitre may present with various symptoms:
- Visible Swelling: Enlargement of the thyroid gland visible as a swelling in the neck.
- Neck Discomfort: Feeling of pressure or fullness in the neck.
- Difficulty Swallowing: Enlarged thyroid can compress the esophagus, causing swallowing difficulties.
- Voice Changes: Pressure on the vocal cords may lead to voice hoarseness.
- Thyroid Dysfunction: Goitre can be associated with both hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid), depending on the underlying cause.
Diagnosis
Diagnosing goitre involves various assessments:
- Physical Examination: A healthcare provider examines the neck for swelling and other signs.
- Thyroid Function Tests: Blood tests to assess thyroid hormone levels and function.
- Imaging: Ultrasound, CT scan, or MRI to visualize the thyroid gland's size and structure.
- Biopsy: Fine-needle aspiration to analyze thyroid tissue for malignancy.
Management
Goitre management depends on its cause and severity:
- Iodine Supplementation: For iodine-deficient goitre, providing iodine through diet or supplements.
- Medications: Thyroid hormone replacement for hypothyroidism, anti-thyroid drugs for hyperthyroidism.
- Surgery: Surgical removal of all or part of the thyroid gland (thyroidectomy) if necessary.
- Radioactive Iodine: Used to shrink an overactive thyroid (hyperthyroidism) causing goitre.
- Close Monitoring: Regular follow-up to assess thyroid function and size.
Complications and Long-Term Outlook
Goitre complications vary based on its underlying cause.
While most cases are benign, some may lead to thyroid dysfunction, difficulty breathing or swallowing, or malignancy.
Early detection, proper diagnosis, and appropriate management contribute to positive outcomes and improved quality of life for individuals with goitre.
Conclusion
In conclusion, goitre represents a multifaceted condition stemming from various causes and manifesting in different forms. A comprehensive understanding of its types, causes, clinical manifestations, diagnosis, and management empowers healthcare professionals to provide effective care, ensuring optimal thyroid health and overall well-being for individuals affected by goitre.
Thyroid Storm
Introduction
Thyroid storm, also known as thyrotoxic crisis, is a life-threatening and rare medical emergency caused by the excessive release of thyroid hormones in individuals with untreated or inadequately managed hyperthyroidism.
It is crucial for healthcare professionals to understand thyroid storm thoroughly, as prompt recognition and immediate interventions are essential for patient survival.
Pathophysiology
A. Thyroid Hormones: Thyroid storm occurs due to a sudden and significant increase in circulating thyroid hormones, predominantly triiodothyronine (T3) and thyroxine (T4).
B. Precipitating Factors: Thyroid storm can be triggered by stressful events, such as infection, surgery, trauma, or discontinuation of antithyroid medications.
C. Hypermetabolic State: The excessive thyroid hormones lead to a state of hypermetabolism, causing a cascade of symptoms affecting multiple body systems.
Clinical Manifestations
A. Cardiovascular Manifestations:
1. Tachycardia: Severe, persistent, and often refractory to treatment.
2. Hypertension: High blood pressure resulting from increased cardiac output and peripheral vascular resistance.
3. Arrhythmias: Atrial fibrillation and other dysrhythmias are common and may lead to cardiac decompensation.
B. Central Nervous System (CNS) Manifestations:
1. Agitation and Delirium: Patients may exhibit extreme restlessness, confusion, or altered mental status.
2. Seizures: In severe cases, seizures may occur due to the hyperexcitable state of the CNS.
3. Coma: In untreated or advanced stages, thyroid storm can progress to a coma.
C. Gastrointestinal Manifestations:
1. Nausea and Vomiting: Patients may experience severe gastrointestinal symptoms.
2. Diarrhea: Frequent and watery bowel movements due to increased gut motility.
D. Hyperthermia:
Profound fever, often exceeding 40°C (104°F), due to increased metabolic rate and impaired thermoregulation.
E. Respiratory Manifestations:
1. Dyspnea: Rapid, shallow breathing and increased respiratory rate.
2. Respiratory Failure: In severe cases, respiratory failure may occur due to increased oxygen demand and metabolic acidosis.

Diagnostic Evaluation
A. Clinical Assessment: Thyroid storm is primarily a clinical diagnosis based on the presence of characteristic signs and symptoms.
B. Laboratory Tests:
1. Thyroid Function Tests: Elevated levels of free T3 and T4 hormones confirm the hyperthyroid state.
2. Thyroid-Stimulating Hormone (TSH): TSH levels are typically suppressed in thyroid storm.
Medical Management
A. Stabilization: Immediate measures are taken to stabilize the patient's condition, including cardiac monitoring, oxygen supplementation, and intravenous fluids.
B. Antithyroid Medications: High-dose antithyroid drugs (propylthiouracil and methimazole) are administered to block thyroid hormone synthesis.
C. Beta-Blockers: Beta-adrenergic blockers (propranolol or esmolol) are used to control tachycardia and manage cardiovascular symptoms.
D. Glucocorticoids: Steroids (e.g., hydrocortisone) may be administered to inhibit the peripheral conversion of T4 to T3.

Supportive Care
A. Cooling Measures: External cooling techniques, such as cooling blankets or ice packs, are used to manage hyperthermia.
B. Fluid and Electrolyte Management: Intravenous fluids are given to correct dehydration and maintain electrolyte balance.
Nursing Intervention
A. Frequent Monitoring: Vital signs, cardiac rhythms, neurological status, and urine output should be continuously assessed.
B. ECG Monitoring: Continuous cardiac monitoring is essential to identify and manage dysrhythmias promptly.
C. Seizure Precautions: Safety measures should be implemented to prevent seizure injury.
Prevention
A. Patient Education: Patients with hyperthyroidism should be educated about the signs and symptoms of thyroid storm and instructed to seek immediate medical attention if they occur.
B. Compliance: Adherence to prescribed antithyroid medications and regular follow-up visits with healthcare providers are essential to prevent thyroid storm recurrence.
Conclusion
In conclusion, thyroid storm is a severe and life-threatening complication of hyperthyroidism. Recognizing its clinical manifestations, promptly initiating medical management, and providing supportive care are crucial for improving patient outcomes.
Through comprehensive understanding and vigilant nursing care, healthcare professionals can play a vital role in identifying and managing thyroid storm promptly, potentially saving lives and preventing further complications.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Endocrine Systems
This filled cannot be empty

