Please set your exam date
Anti-inflammatory and Immunosuppressive Drugs
Study Questions
Introduction
A nurse is caring for a client who has rheumatoid arthritis and is prescribed prednisone, a glucocorticoid. What is the primary mechanism of action of prednisone in this condition?
Explanation
A. It inhibits the synthesis of inflammatory mediators and suppresses the activation and proliferation of immune cells.
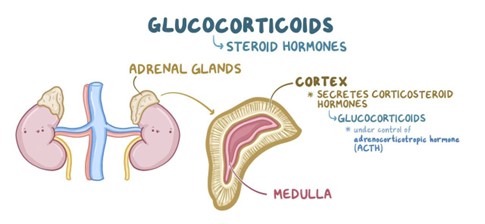
Prednisone is a synthetic glucocorticoid that mimics the natural hormone cortisol, which is produced by the adrenal cortex. Cortisol has potent anti-inflammatory and immunosuppressive effects by inhibiting the synthesis of inflammatory mediators such as prostaglandins, leukotrienes, histamine, cytokines, and adhesion molecules, and by suppressing the activation and proliferation of lymphocytes, macrophages, eosinophils, and mast cells. These effects reduce the immune-mediated damage to the self-tissues in autoimmune diseases such as rheumatoid arthritis.
The other options are wrong because:
B. It blocks the activation of T cells by inhibiting the enzyme calcineurin, which is required for the transcription of interleukin-2.
This option is wrong because it describes the mechanism of action of calcineurin inhibitors, not glucocorticoids. Calcineurin inhibitors are a type of immunosuppressant that target T cells specifically, while glucocorticoids have a broader effect on various immune cells and inflammatory mediators.
C. It interferes with the synthesis of nucleic acids, which are essential for the replication and function of immune cells.
This option is wrong because it describes the mechanism of action of antimetabolites, not glucocorticoids. Antimetabolites are a type of immunosuppressant that interfere with the synthesis of nucleic acids, which are the building blocks of DNA and RNA. This affects the replication and function of immune cells, as well as other rapidly dividing cells such as cancer cells.
D. It binds to specific antigens or receptors on the surface of immune cells and either neutralizes them or induces their destruction.
This option is wrong because it describes the mechanism of action of monoclonal antibodies, not glucocorticoids. Monoclonal antibodies are a type of immunosuppressant that bind to specific antigens or receptors on the surface of immune cells and either neutralize them or induce their destruction. This can prevent the activation or function of immune cells that are involved in transplant rejection or autoimmune diseases.
A nurse is administering ibuprofen, a nonselective COX inhibitor, to a client who has osteoarthritis. What are the expected pharmacologic effects of ibuprofen in this condition?
Explanation
This is because ibuprofen is a nonselective COX inhibitor, which means it blocks both COX-1 and COX-2 enzymes². COX-1 is responsible for producing prostaglandins that protect the gastric mucosa, regulate platelet aggregation, and maintain renal function². COX-2 is responsible for producing prostaglandins that mediate inflammation, pain, and fever². Therefore, by inhibiting both COX-1 and COX-2, ibuprofen reduces inflammation, pain, fever, and gastric mucosal protection by blocking the production of prostaglandins.
The other options are incorrect because:
A. It reduces inflammation, pain, fever, and platelet aggregation by blocking the production of prostaglandins.
This is incorrect because ibuprofen also blocks the production of prostaglandins that regulate platelet aggregation. Therefore, ibuprofen can increase the risk of bleeding by inhibiting platelet function².
C. It reduces inflammation, pain, fever, and sodium retention by blocking the production of prostaglandins.
This is incorrect because ibuprofen also blocks the production of prostaglandins that maintain renal function. Therefore, ibuprofen can cause sodium and water retention by impairing renal perfusion and glomerular filtration².
D. It reduces inflammation, pain, fever, and bronchoconstriction by blocking the production of prostaglandins.
This is incorrect because ibuprofen also blocks the production of prostaglandins that mediate bronchodilation. Therefore, ibuprofen can cause bronchoconstriction by shifting the balance between prostanoids and leukotrienes in favor of leukotrienes².
A nurse is teaching a client who has Crohn's disease and is prescribed azathioprine, an antimetabolite. What should the nurse include in the teaching?
Explanation
This is because azathioprine can affect the production of blood cells in your bone marrow, which are essential for fighting infections and clotting blood². Therefore, you may have a higher chance of getting infections or bleeding more easily while taking this drug. You should monitor your blood counts regularly and report any signs of infection (such as fever, sore throat, cough) or bleeding (such as bruising, nosebleeds, blood in urine or stool) to your doctor².
The other options are incorrect because:
B. The drug may cause nephrotoxicity and increase the risk of renal impairment and electrolyte imbalances.
This is incorrect because azathioprine is not known to cause nephrotoxicity or damage to the kidneys². However, some other drugs that are used to treat IBD, such as mesalazine or sulfasalazine, may have this effect³. Therefore, you should have your kidney function checked before starting these drugs and periodically during treatment³.
C. The drug may cause neurotoxicity and increase the risk of tremor, headache, and seizures.
This is incorrect because azathioprine is not known to cause neurotoxicity or damage to the nervous system². However, some other drugs that are used to treat IBD, such as metronidazole or ciprofloxacin, may have this effect³. Therefore, you should report any signs of neurological problems (such as numbness, tingling, weakness, vision changes, confusion) to your doctor³.
D. The drug may cause hepatotoxicity and increase the risk of liver impairment and jaundice.
This is incorrect because azathioprine is not known to cause hepatotoxicity or damage to the liver². However, some other drugs that are used to treat IBD, such as methotrexate or 6-mercaptopurine, may have this effect³. Therefore, you should have your liver function checked before starting these drugs and periodically during treatment³.
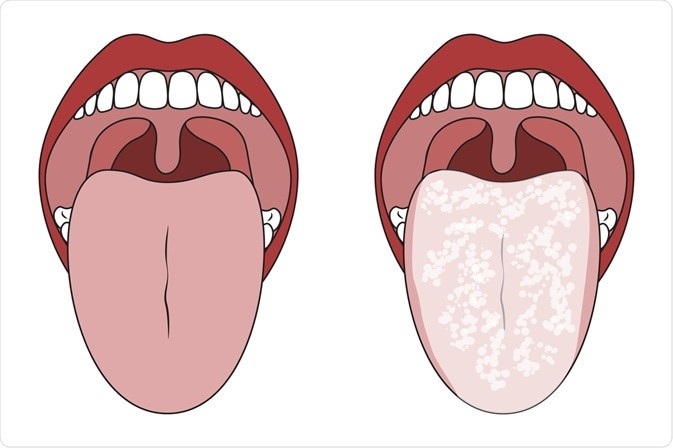
A nurse is monitoring a client who has asthma and is receiving fluticasone, a corticosteroid, by inhalation. What are some of the adverse effects that the nurse should watch for?
Explanation
This is because fluticasone inhalation can cause local side effects in the mouth and throat, such as oral candidiasis (thrush), hoarseness, cough, and dysphonia (voice changes)²³. These side effects are more likely to occur if the dose is high, the duration of treatment is long, or the inhaler technique is poor². To prevent or reduce these side effects, the nurse should instruct the client to rinse the mouth with water after each use of the inhaler, use a spacer device if possible, and check the inhaler technique regularly². Fluticasone is a corticosteroid that is used to treat asthma and other respiratory conditions by reducing inflammation and swelling in the airways¹. It can be administered by inhalation using an aerosol or a powder device.
The other options are incorrect because:
A. Hyperglycemia, osteoporosis, glaucoma, and cataracts
This is incorrect because these are systemic side effects of corticosteroids that are more likely to occur with oral or injectable forms of the drug². Fluticasone inhalation has a low systemic absorption and a high first-pass metabolism, which means that only a small amount of the drug reaches the bloodstream and most of it is broken down in the liver before it can cause systemic effects¹. Therefore, these side effects are rare with fluticasone inhalation².
B. Hypoglycemia, osteomalacia, myopia, and dry eyes
This is incorrect because these are not known side effects of fluticasone inhalation or corticosteroids in general². Hypoglycemia (low blood sugar) is more likely to occur with drugs that lower blood glucose levels, such as insulin or oral antidiabetic agents⁴. Osteomalacia (softening of the bones) is more likely to occur with drugs that affect vitamin D metabolism, such as anticonvulsants or antiretrovirals⁵. Myopia (nearsightedness) and dry eyes are more likely to occur with drugs that affect the eye muscles or tear production, such as antihistamines or anticholinergics⁶.
D. Oral ulcers, dysphagia, wheeze, and dyspnea
This is incorrect because these are not common side effects of fluticasone inhalation or corticosteroids in general². Oral ulcers (sores in the mouth) are more likely to occur with drugs that irritate the mucous membranes, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or chemotherapy agents. Dysphagia (difficulty swallowing) is more likely to occur with drugs that affect the esophageal motility or sphincter function, such as calcium channel blockers or antipsychotics. Wheeze (a high-pitched sound when breathing) and dyspnea (shortness of breath) are more likely to occur with drugs that cause bronchoconstriction or respiratory depression, such as beta blockers or opioids.
A nurse is evaluating a client who has ulcerative colitis and is receiving infliximab, a monoclonal antibody. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
Infliximab is a monoclonal antibody that is used to treat ulcerative colitis and other inflammatory conditions by blocking the action of tumor necrosis factor-alpha (TNF-α), a cytokine that causes inflammation and tissue damage in the gut¹. It can be given intravenously every 8 weeks as a maintenance therapy for moderate to severe ulcerative colitis¹. However, it can also have some potential benefits and risks that the nurse should monitor.
The correct answer to your question is:
D. All of the above
This is because infliximab can improve the clinical outcomes of ulcerative colitis in several ways, such as:
A. Decreased frequency and severity of diarrhea, abdominal pain, and rectal bleeding:
These are the main symptoms of ulcerative colitis that affect the quality of life of patients. Infliximab can reduce these symptoms by healing the inflammation and ulcers in the colon and rectum. Several studies have shown that infliximab can induce and maintain clinical remission, response, and mucosal healing in patients with moderate to severe ulcerative colitis who are refractory to conventional therapies²³⁴.
B. Increased appetite, weight gain, energy level, and quality of life:
These are the secondary outcomes of ulcerative colitis that reflect the nutritional status and well-being of patients. Infliximab can improve these outcomes by reducing the systemic effects of inflammation, such as malabsorption, anemia, fatigue, and fever. Several studies have shown that infliximab can improve the health-related quality of life, nutritional status, and functional status of patients with moderate to severe ulcerative colitis²³⁴.
C. Normalized stool culture, blood count, electrolytes, and liver function tests:
These are the laboratory tests that indicate the severity and complications of ulcerative colitis. Infliximab can normalize these tests by reducing the bacterial translocation, blood loss, dehydration, and liver involvement that may occur in ulcerative colitis. Several studies have shown that infliximab can improve the stool culture, hemoglobin, albumin, C-reactive protein, and liver enzymes of patients with moderate to severe ulcerative colitis²³⁴.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
A nurse is teaching a client who has osteoarthritis and is prescribed celecoxib (Celebrex), a selective COX-2 inhibitor. What should the nurse include in the teaching?
Explanation
Celecoxib is a selective COX-2 inhibitor that blocks the production of prostaglandins that are involved in pain and inflammation, but spares the COX-1 enzyme that is responsible for protecting the stomach lining and platelet function¹²³⁴⁵. Therefore, celecoxib has less gastrointestinal toxicity than nonselective COX inhibitors, such as ibuprofen and naproxen, that inhibit both COX-1 and COX-2 enzymes¹²³⁴⁵. However, celecoxib still carries some risk of gastrointestinal bleeding and ulceration, especially in patients with a history of peptic ulcer disease, concomitant use of anticoagulants or corticosteroids, or high doses or long-term use of celecoxib¹²³⁴⁵. Therefore, the lowest effective dose and the shortest duration of treatment should be used, and patients should be monitored for signs and symptoms of gastrointestinal adverse events¹²³⁴⁵.
The other options are incorrect because:
B. The drug has more anti-inflammatory and analgesic effects than nonselective COX inhibitors because it blocks both COX-1 and COX-2 enzymes.
This option is wrong because celecoxib is a selective COX-2 inhibitor that does not block COX-1, which is involved in the production of prostaglandins that have anti-inflammatory and analgesic effects . Therefore, celecoxib has less anti-inflammatory and analgesic effects than nonselective COX inhibitors that block both COX-1 and COX-2 enzymes .
C. The drug has less cardiovascular risk than nonselective COX inhibitors because it inhibits vasodilatory and antiplatelet prostaglandins produced by COX-2 in the endothelium.
This option is wrong because celecoxib has more cardiovascular risk than nonselective COX inhibitors because it inhibits the production of prostacyclin, a prostaglandin that has vasodilatory and antiplatelet effects, while leaving the synthesis of thromboxane A2, a prostaglandin that promotes platelet aggregation, vasoconstriction, and smooth-muscle proliferation, unchanged or increased . This imbalance may favor thrombosis and vasoconstriction in the blood vessels and increase the risk of cardiovascular events, such as heart attacks and strokes . Therefore, celecoxib should be used with caution in patients with a history or risk factors for cardiovascular disease, and the lowest effective dose and the shortest duration of treatment should be used .
D. The drug has more antipyretic and antiplatelet effects than nonselective COX inhibitors because it blocks the production of prostaglandins involved in fever and platelet aggregation.
This option is wrong because celecoxib has less antipyretic and antiplatelet effects than nonselective COX inhibitors because it does not block the production of prostaglandins involved in fever and platelet aggregation . Celecoxib is a selective COX-2 inhibitor that spares the COX-1 enzyme that is responsible for protecting the stomach lining and platelet function
A nurse is administering aspirin (ASA), a nonselective COX inhibitor, to a client who has rheumatoid arthritis. What are some of the specific indications of aspirin in this condition?
Explanation
According to various sources, aspirin is a nonselective COX inhibitor that blocks the production of prostaglandins that are involved in inflammation, pain, fever, and platelet aggregation¹²³⁴. Aspirin is used to relieve the symptoms of rheumatoid arthritis (RA), such as joint swelling, stiffness, and pain¹²³⁴. Aspirin also has antiplatelet effects that can prevent cardiovascular events, such as myocardial infarction and stroke, in patients with RA who have an increased risk of atherosclerosis²³. However, aspirin does not modify the course or progression of RA, and it may cause gastrointestinal bleeding, ulceration, and perforation, as well as hypersensitivity reactions, renal impairment, and Reye's syndrome¹²³⁴. Therefore, aspirin should be used with caution and under medical supervision in patients with RA.
The other options are incorrect because:
B. It prevents cardiovascular events such as myocardial infarction and stroke by inhibiting platelet aggregation and thromboxane synthesis.
This option is wrong because it is not a specific indication of aspirin in rheumatoid arthritis, but a general indication of aspirin in patients with or at risk of cardiovascular disease . Aspirin can prevent cardiovascular events by inhibiting platelet aggregation and thromboxane synthesis, but this effect is not related to the treatment of rheumatoid arthritis symptoms, such as inflammation, pain, and fever . However, aspirin may have a secondary benefit of reducing the cardiovascular risk in patients with rheumatoid arthritis who have an increased risk of atherosclerosis .
C. It treats gouty arthritis by inhibiting the enzyme xanthine oxidase and reducing the production of uric acid.
This option is wrong because it describes the mechanism of action and indication of allopurinol, not aspirin . Allopurinol is a drug that treats gouty arthritis by inhibiting the enzyme xanthine oxidase and reducing the production of uric acid, which causes inflammation and pain in the joints . Aspirin does not inhibit xanthine oxidase or reduce uric acid levels, and it is not used to treat gouty arthritis . In fact, aspirin may worsen gouty arthritis by interfering with the renal excretion of uric acid and increasing its concentration in the blood .
D. It induces labor by stimulating uterine contractions and cervical ripening by blocking the production of prostaglandins.
This option is wrong because it describes the mechanism of action and indication of misoprostol, not aspirin . Misoprostol is a synthetic prostaglandin that induces labor by stimulating uterine contractions and cervical ripening . Aspirin does not induce labor, but rather blocks the production of prostaglandins that are involved in inflammation, pain, fever, and platelet aggregation
A nurse is evaluating a client who has fever and is receiving acetaminophen (Tylenol), a nonsalicylate NSAID. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
Acetaminophen (Tylenol) is commonly used to reduce fever. Fever is an elevated body temperature, and one of the main goals of using acetaminophen is to lower the body temperature back to the normal range. Therefore, a decreased temperature within the normal range would indicate the effectiveness of the therapy in reducing fever.
Options B, C, and D, are not directly related to the use of acetaminophen.
B.
Option B refers to the effects of NSAIDs (nonsteroidal anti-inflammatory drugs) in general, which include reducing inflammation, pain, and swelling. Acetaminophen is not primarily an anti-inflammatory drug, so it may not have significant effects on inflammation, pain, or swelling.
C.
Option C refers to the gastrointestinal side effects associated with NSAIDs, such as bleeding and ulceration. Acetaminophen is generally considered safer for the gastrointestinal system compared to NSAIDs, but it does not specifically decrease the risk of gastrointestinal bleeding and ulceration.
D.
Option D refers to the potential adverse effects of acetaminophen on the liver, such as hepatotoxicity and liver impairment. While these are possible risks associated with acetaminophen, decreased risk is not an outcome that directly indicates the effectiveness of the therapy. Monitoring liver function is important when using acetaminophen, especially at higher doses or with prolonged use, but it does not serve as an indicator of the therapy's effectiveness in reducing fever.

A nurse is preparing to administer ketorolac (Toradol), a nonselective COX inhibitor, to a client who has moderate to severe pain after surgery. What are some of the nursing considerations for this drug?
Explanation
This is because ketorolac can cause gastrointestinal, renal, and cardiovascular effects as a result of its nonselective inhibition of cyclooxygenase (COX) enzymes². COX enzymes are responsible for producing prostaglandins that have different functions in different tissues. By blocking both COX-1 and COX-2 enzymes, ketorolac can interfere with the protective, regulatory, and homeostatic roles of prostaglandins in various organs². Therefore, the nurse should consider the following points when administering this drug:
A. ssas
It should be given orally with food or milk to minimize gastrointestinal irritation: This is because ketorolac can cause gastrointestinal effects such as nausea, vomiting, ulceration, bleeding, and perforation by blocking the production of prostaglandins that protect the gastric mucosa from acid and pepsin²³. The nurse should advise the client to take ketorolac with food or milk, avoid alcohol and tobacco, report any signs of gastrointestinal bleeding (such as black or tarry stools, abdominal pain, vomiting blood), and use the lowest effective dose for the shortest duration possible²³.
B. asdasd
It should be given intravenously slowly over 15 to 30 minutes to prevent hypotension or thrombophlebitis: This is because ketorolac can cause hypotension by blocking the production of prostaglandins that regulate blood pressure and vascular tone² . It can also cause thrombophlebitis by irritating the vein wall and causing inflammation and clot formation² . The nurse should monitor the client's blood pressure and infusion site during and after the administration of ketorolac and report any signs of hypotension (such as dizziness, fainting, blurred vision) or thrombophlebitis (such as redness, swelling, pain, warmth) to the doctor² .
C. asfdeaf
It should be given for short-term use only (up to 5 days) to avoid renal impairment or gastrointestinal bleeding: This is because ketorolac can cause renal impairment by blocking the production of prostaglandins that maintain renal blood flow, glomerular filtration rate, sodium excretion, and water balance² . It can also cause gastrointestinal bleeding by blocking the production of prostaglandins that inhibit platelet aggregation and promote hemostasis²³. The risk of these effects is higher in those with preexisting renal impairment, heart failure, liver cirrhosis, dehydration, or hypovolemia, and those who use diuretics or anticoagulants²³ . The nurse should monitor the client's fluid intake and output, body weight, electrolytes, and renal function tests, and report any signs of renal dysfunction (such as oliguria, anuria, edema) or gastrointestinal bleeding (such as black or tarry stools, abdominal pain, vomiting blood) to the doctor²³ .
Contraindications of NSAIDs
A nurse is teaching a client who has osteoarthritis and is prescribed celecoxib (Celebrex), a selective COX-2 inhibitor. What should the nurse include in the teaching?
Explanation
A. The drug has less gastrointestinal toxicity than nonselective COX inhibitors because it does not interfere with gastric mucosal protection by prostaglandins.
This is because celecoxib (Celebrex), a selective COX-2 inhibitor, selectively inhibits the cyclooxygenase-2 (COX-2) enzyme, which is responsible for prostaglandin synthesis in inflammation, pain, and fever¹. Prostaglandins produced by the cyclooxygenase-1 (COX-1) enzyme, which is not affected by celecoxib, have protective effects on the gastrointestinal mucosa and platelet function¹. Therefore, celecoxib has less risk of causing gastrointestinal ulceration and bleeding than nonselective COX inhibitors, which block both COX-1 and COX-2 enzymes²³.
The other options are wrong because they are either false or contradictory to the facts about celecoxib (Celebrex), a selective COX-2 inhibitor.
- Option B is wrong because celecoxib does not block both COX-1 and COX-2 enzymes, but only COX-2 enzyme. Therefore, it does not have more anti-inflammatory and analgesic effects than nonselective COX inhibitors, but similar effects .
- Option C is wrong because celecoxib does not inhibit vasodilatory and antiplatelet prostaglandins produced by COX-2 in the endothelium, but rather it inhibits the production of these prostaglandins by COX-2 in the inflammatory sites. Therefore, it does not have less cardiovascular risk than nonselective COX inhibitors, but more risk .
- Option D is wrong because celecoxib does not block the production of prostaglandins involved in fever and platelet aggregation, but rather it spares the production of these prostaglandins by COX-1. Therefore, it does not have more antipyretic and antiplatelet effects than nonselective COX inhibitors, but none or minimal effects .
A nurse is administering aspirin (ASA), a nonselective COX inhibitor, to a client who has rheumatoid arthritis. What are some of the specific indications of aspirin in this condition?
Explanation
A. It reduces inflammation, pain, fever, and platelet aggregation by blocking the production of prostaglandins.
This is because aspirin (ASA), a nonselective COX inhibitor, inhibits both cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) enzymes, which are responsible for prostaglandin synthesis in various tissues¹. Prostaglandins are involved in inflammation, pain, fever, and platelet aggregation. Therefore, aspirin has anti-inflammatory, analgesic, antipyretic, and antiplatelet effects¹².
- Aspirin is used to relieve the symptoms of rheumatoid arthritis (arthritis caused by swelling of the lining of the joints), osteoarthritis (arthritis caused by breakdown of the lining of the joints), systemic lupus erythematosus (condition in which the immune system attacks the joints and organs and causes pain and swelling) and certain other rheumatologic conditions (conditions in which the immune system attacks parts of the body)¹.
- Aspirin is also used to prevent cardiovascular events such as myocardial infarction and stroke by inhibiting platelet aggregation and thromboxane synthesis¹². However, this effect requires low doses of aspirin (typically 75 to 81 mg/day) that are insufficient to inhibit COX-2 and have anti-inflammatory effects².
- Aspirin does not treat gouty arthritis by inhibiting the enzyme xanthine oxidase and reducing the production of uric acid. This is the mechanism of action of allopurinol, a drug used for gout³. In fact, aspirin can worsen gout by increasing uric acid levels in the blood and decreasing its excretion in the urine⁴.
- Aspirin does not induce labor by stimulating uterine contractions and cervical ripening by blocking the production of prostaglandins. This is the mechanism of action of misoprostol, a synthetic prostaglandin E1 analog used for labor induction. In fact, aspirin is contraindicated in pregnancy because it can cause bleeding complications, premature closure of the ductus arteriosus, and delayed onset of labor¹ .
The other options are wrong because they are either false or irrelevant to the specific indications of aspirin (ASA), a nonselective COX inhibitor, in rheumatoid arthritis.
- Option B is wrong because it is not a specific indication of aspirin in rheumatoid arthritis, but a general indication of aspirin in cardiovascular prevention. Aspirin can prevent cardiovascular events such as myocardial infarction and stroke by inhibiting platelet aggregation and thromboxane synthesis, but this effect requires low doses of aspirin that are not effective for rheumatoid arthritis .
- Option C is wrong because it is not the mechanism of action of aspirin, but of allopurinol, a drug used for gout. Aspirin does not inhibit the enzyme xanthine oxidase and reduce the production of uric acid, but rather it inhibits both COX-1 and COX-2 enzymes and blocks the production of prostaglandins. Aspirin is not used to treat gouty arthritis, but rather it can worsen it by increasing uric acid levels in the blood and decreasing its excretion in the urine.
- Option D is wrong because it is not the mechanism of action of aspirin, but of misoprostol, a drug used for labor induction. Aspirin does not stimulate uterine contractions and cervical ripening by blocking the production of prostaglandins, but rather it inhibits both COX-1 and COX-2 enzymes and blocks the production of prostaglandins. Aspirin is not used to induce labor, but rather it is contraindicated in pregnancy because it can cause bleeding complications, premature closure of the ductus arteriosus, and delayed onset of labor.
A nurse is monitoring a client who has gout and is receiving indomethacin (Indocin), a nonselective COX inhibitor. What are some of the adverse effects that the nurse should watch for?
Explanation
This is because indomethacin can cause gastrointestinal, renal, and cardiovascular effects as a result of its nonselective inhibition of cyclooxygenase (COX) enzymes. COX enzymes are responsible for producing prostaglandins that have different functions in different tissues. By blocking both COX-1 and COX-2 enzymes, indomethacin can interfere with the protective, regulatory, and homeostatic roles of prostaglandins in various organs. Therefore, the nurse should monitor the client for the following adverse effects:
A. Gastrointestinal effects such as nausea, vomiting, ulceration, bleeding, and perforation:
These are the most common and serious side effects of indomethacin and other NSAIDs . They occur because indomethacin blocks the production of prostaglandins that protect the gastric mucosa from acid and pepsin, maintain the mucosal blood flow, and promote healing of ulcers. The risk of these effects is higher in older adults, those with a history of peptic ulcer disease or gastrointestinal bleeding, those who use alcohol or tobacco, and those who take other drugs that irritate the stomach, such as corticosteroids or anticoagulants . The nurse should advise the client to take indomethacin with food or milk, avoid alcohol and tobacco, report any signs of gastrointestinal bleeding (such as black or tarry stools, abdominal pain, vomiting blood), and use the lowest effective dose for the shortest duration possible .
B. Renal effects such as reduced glomerular filtration rate, sodium and water retention, edema, hypertension, and acute renal failure:
These are less common but potentially serious side effects of indomethacin and other NSAIDs . They occur because indomethacin blocks the production of prostaglandins that regulate renal blood flow, glomerular filtration rate, sodium excretion, and water balance. The risk of these effects is higher in those with preexisting renal impairment, heart failure, liver cirrhosis, dehydration, or hypovolemia, and those who use diuretics or angiotensin-converting enzyme inhibitors . The nurse should monitor the client's fluid intake and output, body weight, blood pressure, electrolytes, and renal function tests, and report any signs of renal dysfunction (such as oliguria, anuria, edema) or worsening heart failure (such as dyspnea, fatigue) to the doctor .
C. Cardiovascular effects such as increased risk of myocardial infarction and stroke due to platelet aggregation and vasoconstriction:
These are rare but potentially fatal side effects of indomethacin and other NSAIDs . They occur because indomethacin blocks the production of prostaglandins that inhibit platelet aggregation and vasodilation. The risk of these effects is higher in those with a history of cardiovascular disease or risk factors such as hypertension, diabetes mellitus, hyperlipidemia, smoking, or obesity . The nurse should assess the client's cardiovascular status and history before starting indomethacin therapy and advise the client to seek immediate medical attention if they experience any signs of a heart attack (such as chest pain or pressure) or a stroke (such as sudden weakness or numbness on one side of the body) while taking this drug.

A nurse is evaluating a client who has fever and is receiving acetaminophen (Tylenol), a nonsalicylate NSAID. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
This is because acetaminophen (Tylenol), a nonsalicylate NSAID, reduces fever by inhibiting the synthesis of prostaglandins in the hypothalamus, the part of the brain that regulates body temperature¹. Prostaglandins are involved in inflammation, pain, fever, and platelet aggregation. Therefore, acetaminophen has antipyretic and analgesic effects, but not anti-inflammatory or antiplatelet effects¹².
The other options are wrong because they are either false or unrelated to the outcomes that indicate the effectiveness of acetaminophen (Tylenol), a nonsalicylate NSAID, in fever.
- Option B is wrong because acetaminophen does not reduce inflammation, pain, and swelling, but only pain and fever. Acetaminophen does not inhibit the synthesis of prostaglandins in the peripheral tissues, where they mediate inflammation and pain, but only in the central nervous system and the hypothalamus, where they modulate pain perception and body temperature.
- Option C is wrong because acetaminophen does not reduce the risk of gastrointestinal bleeding and ulceration, but rather it has no effect on it. Acetaminophen does not inhibit the synthesis of prostaglandins in the gastrointestinal mucosa, where they protect the lining from acid and enzymes, but only in the central nervous system and the hypothalamus. Therefore, acetaminophen is safer than nonselective COX inhibitors for patients with peptic ulcer disease or bleeding disorders.
- Option D is wrong because acetaminophen does not reduce the risk of hepatotoxicity and liver impairment, but rather it can cause it if taken in high doses or with alcohol or other drugs that affect the liver. Acetaminophen is metabolized by the liver into a toxic intermediate that can deplete glutathione, a substance that protects the liver cells from damage. If the amount of this intermediate exceeds the amount of glutathione, liver injury can occur.
A nurse is preparing to administer ketorolac (Toradol), a nonselective COX inhibitor, to a client who has moderate to severe pain after surgery. What are some of the nursing considerations for this drug?
Explanation
This is because ketorolac (Toradol), a nonselective COX inhibitor, inhibits both cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) enzymes, which are responsible for prostaglandin synthesis in various tissues. Prostaglandins are involved in inflammation, pain, fever, and platelet aggregation. Therefore, ketorolac has anti-inflammatory, analgesic, antipyretic, and antiplatelet effects.
Some of the nursing considerations for ketorolac are:
- It should be given orally with food or milk to minimize gastrointestinal irritation .
Ketorolac can cause gastrointestinal effects such as nausea, vomiting, ulceration, bleeding, and perforation because it inhibits the synthesis of prostaglandins that protect the gastric mucosa .
- It should be given intravenously slowly over 15 seconds to prevent hypotension or thrombophlebitis.
Ketorolac can cause hypotension by inhibiting the synthesis of prostaglandins that regulate blood pressure and renal blood flow . It can also cause thrombophlebitis by irritating the vein wall and activating platelets.
- It should be given for short-term use only (up to 5 days) to avoid renal impairment or gastrointestinal bleeding .
Ketorolac can cause renal impairment by reducing the glomerular filtration rate and causing sodium and water retention, edema, hypertension, and acute renal failure . It can also cause gastrointestinal bleeding by inhibiting the synthesis of prostaglandins that maintain mucosal blood flow and integrity .
Adverse effects of NSAIDs
A nurse is teaching a client who has peptic ulcer disease and is prescribed misoprostol (Cytotec), a synthetic prostaglandin. What should the nurse include in the teaching?
Explanation
Misoprostol is a synthetic prostaglandin that works by "replacing" prostaglandins whose production is blocked by aspirin or NSAIDs¹. Prostaglandins are hormone-like substances that help protect the stomach lining from damage caused by acid and pepsin². Misoprostol produces a dose-related inhibition of gastric acid and pepsin secretion and enhances mucosal resistance to injury¹.
The other options are incorrect because:
- A. The drug does not have anti-inflammatory and analgesic effects by blocking the production of prostaglandins. On the contrary, it stimulates the production of prostaglandins to protect the stomach lining. Blocking the production of prostaglandins would increase the risk of ulcers.
- B. The drug does not have antipyretic and antiplatelet effects by blocking the production of prostaglandins. Antipyretic means reducing fever, and antiplatelet means preventing blood clots. Misoprostol does not have these effects, and blocking the production of prostaglandins would not cause them either.
- D. The drug does not have renal protective effects by stimulating the production of prostaglandins. Renal means related to the kidneys, and misoprostol does not affect the kidneys. Stimulating the production of prostaglandins would not protect the kidneys either.
A nurse is administering naproxen (Naprosyn), a nonselective COX inhibitor, to a client who has bursitis. What are some of the contraindications for this drug?
Explanation
Naproxen is a nonselective COX inhibitor, which means it blocks the production of prostaglandins, which are involved in inflammation, pain, fever, and blood clotting. Naproxen can cause serious side effects such as cardiovascular thrombotic events, gastrointestinal bleeding and ulceration, renal toxicity, and hypersensitivity reactions¹²³.
The other options are incorrect because:
- B. Asthma, hypertension, heart failure, diabetes, dehydration, alcoholism, smoking, advanced age, and concurrent use of anticoagulants, glucocorticoids, or other NSAIDs are not contraindications for naproxen, but they are cautions or risk factors that may increase the likelihood of adverse effects or require dose adjustment or monitoring¹²³.
- C. History of cardiovascular thrombotic events, such as myocardial infarction or stroke, severe allergic reactions to NSAIDs or aspirin, such as anaphylaxis or angioedema, and coronary artery bypass graft surgery are not specific contraindications for naproxen, but they are warnings that apply to all NSAIDs due to their potential to increase the risk of these serious events¹²³.
- D. None of the above is incorrect because option A contains some valid contraindications for naproxen.

A nurse is evaluating a client who has fever and is receiving ibuprofen (Motrin), a nonselective COX inhibitor. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
Ibuprofen is a nonselective COX inhibitor, which means it blocks the production of prostaglandins, which are involved in inflammation, pain, fever, and blood clotting. Ibuprofen has antipyretic (fever-reducing) effects by inhibiting the synthesis of prostaglandins in the hypothalamus, the part of the brain that regulates body temperature . Ibuprofen can lower fever by 1 to 2°C within 2 to 4 hours of administration . The normal body temperature range is 36.5 to 37.5°C (97.7 to 99.5°F).
The other options are incorrect because:
B. Decreased inflammation, pain, and swelling are not outcomes that indicate the effectiveness of ibuprofen therapy for fever. These are outcomes that indicate the effectiveness of ibuprofen therapy for inflammation and pain, which are other indications for ibuprofen. Ibuprofen has anti-inflammatory and analgesic effects by blocking the production of prostaglandins that mediate inflammation and pain . However, these effects are not relevant for fever management.
C. Decreased risk of gastrointestinal bleeding and ulceration are not outcomes that indicate the effectiveness of ibuprofen therapy for fever. These are outcomes that indicate the prevention or reduction of adverse effects of ibuprofen therapy. Ibuprofen has gastrointestinal effects such as nausea, vomiting, ulceration, bleeding, and perforation by blocking the production of prostaglandins that protect the stomach lining from acid and pepsin . These effects are more likely to occur in patients with a history of peptic ulcer disease or gastrointestinal bleeding or in patients who take high doses or long-term use of ibuprofen. The nurse should monitor the client for signs and symptoms of gastrointestinal bleeding and ulceration such as abdominal pain, black or bloody stools, hematemesis (vomiting blood), melena (dark tarry stools), anemia (low red blood cell count), or hypotension (low blood pressure). The nurse should also advise the client to take ibuprofen with food or milk to reduce gastric irritation and to avoid alcohol or other NSAIDs that may increase the risk of gastrointestinal bleeding and ulceration.
D. Decreased risk of hepatotoxicity and liver impairment are not outcomes that indicate the effectiveness of ibuprofen therapy for fever. These are outcomes that indicate the prevention or reduction of adverse effects of ibuprofen therapy. Ibuprofen has hepatic effects such as elevated liver enzymes, jaundice (yellowing of skin or eyes), hepatitis (inflammation of liver), and liver failure by affecting hepatic function and metabolism . These effects are rare but serious and may occur in patients with hepatic impairment or risk factors for hepatic toxicity such as alcoholism or concurrent use of other hepatotoxic drugs. The nurse should monitor the client's liver function tests and report any abnormal results or signs and symptoms of liver injury such as nausea, vomiting, anorexia (loss of appetite), fatigue
Nursing considerations for NSAIDs
A nurse is caring for a client who has systemic lupus erythematosus and is prescribed prednisone, a glucocorticoid. What is the primary mechanism of action of prednisone in this condition?
Explanation
Prednisone, a glucocorticoid, exerts its primary mechanism of action in systemic lupus erythematosus (SLE) by inhibiting the synthesis of inflammatory mediators and suppressing the activation and proliferation of immune cells.
The other options are incorrect because:
A. It inhibits the synthesis of inflammatory mediators and suppresses the activation and proliferation of immune cells: Glucocorticoids like prednisone have potent anti-inflammatory and immunosuppressive effects. They work by suppressing the production of various pro-inflammatory mediators, such as cytokines and prostaglandins. Additionally, glucocorticoids can inhibit the activation and proliferation of immune cells, including T cells and B cells, which play a role in the pathogenesis of SLE.
B. It blocks the activation of T cells by inhibiting the enzyme calcineurin, which is required for the transcription of interleukin-2: This mechanism of action describes the action of calcineurin inhibitors like cyclosporine, not prednisone. Prednisone does not directly inhibit calcineurin or interfere with the transcription of interleukin-2.
C. It interferes with the synthesis of nucleic acids, which are essential for the replication and function of immune cells: This statement is not accurate. Prednisone primarily acts by modulating immune cell function and reducing inflammation rather than interfering with nucleic acid synthesis.
D. It binds to specific antigens or receptors on the surface of immune cells and either neutralizes them or induces their destruction: This statement does not accurately describe the mechanism of action of prednisone. Prednisone acts through intracellular receptors rather than binding to antigens or surface receptors on immune cells.
A nurse is administering fludrocortisone (Florinef), a mineralocorticoid, to a client who has Addison's disease. What are some of the expected pharmacologic effects of fludrocortisone in this condition?
Explanation
Fludrocortisone, a mineralocorticoid, is used in the treatment of Addison's disease, a condition characterized by adrenal insufficiency. The primary pharmacologic effects of fludrocortisone in this condition are related to its mineralocorticoid activity. It promotes sodium reabsorption and potassium excretion in the kidney, increasing blood volume and blood pressure: Fludrocortisone acts on the kidneys to enhance the reabsorption of sodium and increase the excretion of potassium. This action helps to regulate electrolyte balance and fluid volume, which can contribute to an increase in blood volume and blood pressure.
The other options are incorrect because:
B. It reduces inflammation, pain, fever, and allergic reactions by inhibiting the synthesis of prostaglandins and leukotrienes: This statement describes the pharmacologic effects of glucocorticoids, not mineralocorticoids like fludrocortisone. While fludrocortisone may have some mild anti-inflammatory effects, its primary role is related to electrolyte and fluid balance rather than inflammation modulation.
C. It regulates the secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary gland, maintaining the feedback loop of cortisol production: This statement describes the role of cortisol, not fludrocortisone. Fludrocortisone primarily acts as a synthetic mineralocorticoid and does not directly regulate ACTH secretion or cortisol production.
D. It influences the carbohydrate, protein, and fat metabolism in various tissues, increasing blood glucose and suppressing immune response: This statement describes the pharmacologic effects of glucocorticoids like cortisol, not mineralocorticoids. Fludrocortisone has minimal impact on carbohydrate, protein, and fat metabolism and does not exert significant immunosuppressive effects.
A nurse is monitoring a client who has asthma and is receiving fluticasone (Flovent), a corticosteroid, by inhalation. What are some of the adverse effects that the nurse should watch for?
Explanation
These adverse effects are more commonly observed with inhaled corticosteroids like fluticasone. Inhaled corticosteroids can cause local side effects in the mouth and throat, such as oral candidiasis (thrush), a fungal infection. Hoarseness, cough, and dysphonia (voice changes) may also occur due to local irritation of the throat.
The other options are incorrect because:
A. Hyperglycemia, osteoporosis, glaucoma, and cataracts: These adverse effects are associated with systemic corticosteroid use, particularly when administered orally or by injection. When using inhaled corticosteroids like fluticasone, the systemic absorption is minimal, and the risk of these adverse effects is significantly lower compared to systemic administration.
B. Hypoglycemia, osteomalacia, myopia, and dry eyes: Hypoglycemia is not a commonly observed adverse effect of inhaled corticosteroids like fluticasone. Osteomalacia (softening of bones) is more commonly associated with long-term systemic corticosteroid use. Myopia (nearsightedness) and dry eyes are not typically seen as adverse effects of inhaled corticosteroids.
D. Oral ulcers, dysphagia, wheeze, and dyspnea: Oral ulcers, dysphagia (difficulty swallowing), wheeze, and dyspnea (difficulty breathing) are not commonly associated with inhaled corticosteroids and are not typical adverse effects of fluticasone.

A nurse is evaluating a client who has ulcerative colitis and is receiving infliximab (Remicade), a monoclonal antibody. What are some of the outcomes that indicate the effectiveness of the therapy? (Select all that apply)
Explanation
Decreased frequency and severity of diarrhea, abdominal pain, and rectal bleeding . These are the main symptoms of ulcerative colitis, a chronic inflammatory condition of the colon and rectum that causes ulcers, bleeding, and mucus production in the lining of the bowel. Infliximab is a monoclonal antibody that works by blocking the action of tumor necrosis factor-alpha (TNF-alpha), a cytokine that mediates inflammation and tissue damage in ulcerative colitis. Infliximab can reduce the inflammation and ulceration of the bowel and improve the clinical symptoms of ulcerative colitis .
- Improved endoscopic findings and mucosal healing . Endoscopy is a procedure that uses a flexible tube with a camera and light to examine the inside of the digestive tract. Mucosal healing is the restoration of the normal structure and function of the bowel lining. Infliximab can improve the endoscopic appearance and mucosal healing of the colon and rectum in patients with ulcerative colitis . This may reduce the risk of complications such as strictures, fistulas, abscesses, or cancer .
- Decreased levels of inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) . CRP and ESR are blood tests that measure the level of inflammation in the body. CRP is a protein produced by the liver in response to inflammation, and ESR is a measure of how fast red blood cells settle in a tube of blood. Both tests are elevated in patients with ulcerative colitis due to the chronic inflammation of the bowel. Infliximab can lower the levels of CRP and ESR by reducing the inflammation and tissue damage in ulcerative colitis . This may reflect the improvement in disease activity and prognosis .
- Resolution of extraintestinal manifestations associated with ulcerative colitis (e.g., joint pain, skin lesions) . Extraintestinal manifestations are symptoms or conditions that affect other organs or systems outside the digestive tract. They occur in about 25% of patients with ulcerative colitis and may include arthritis (joint inflammation), uveitis (eye inflammation), erythema nodosum (skin nodules), pyoderma gangrenosum (skin ulcers), primary sclerosing cholangitis (liver inflammation), or ankylosing spondylitis (spine inflammation) . Infliximab can resolve or improve some of these extraintestinal manifestations by blocking TNF-alpha, which is involved in their pathogenesis .
Indications of corticosteroids and immunosuppressants
A nurse is caring for a client who has rheumatoid arthritis and is prescribed prednisone, a glucocorticoid. What is the primary mechanism of action of prednisone in this condition?
Explanation
Prednisone, a glucocorticoid, is commonly used in the treatment of rheumatoid arthritis. Its primary mechanism of action in this condition is related to its anti-inflammatory and immunosuppressive effects.
A. It inhibits the synthesis of inflammatory mediators and suppresses the activation and proliferation of immune cells: Prednisone acts by suppressing the synthesis of various inflammatory mediators, including prostaglandins, leukotrienes, and cytokines. It also inhibits the activation and proliferation of immune cells such as lymphocytes and macrophages. By reducing inflammation and immune response, it helps manage the symptoms of rheumatoid arthritis.
B. It blocks the activation of T cells by inhibiting the enzyme calcineurin, which is required for the transcription of interleukin-2: This mechanism of action is associated with a different class of immunosuppressive medications called calcineurin inhibitors, such as cyclosporine. Prednisone does not directly block T-cell activation by inhibiting calcineurin.
C. It interferes with the synthesis of nucleic acids, which are essential for the replication and function of immune cells: While prednisone may have some impact on nucleic acid synthesis, it is not the primary mechanism of action for its therapeutic effects in rheumatoid arthritis. The anti-inflammatory and immunosuppressive effects of prednisone primarily result from the inhibition of inflammatory mediators and immune cell activity.
D. It binds to specific antigens or receptors on the surface of immune cells and either neutralizes them or induces their destruction: This mechanism of action is associated with targeted therapies such as monoclonal antibodies. Prednisone, as a glucocorticoid, exerts its effects through genomic mechanisms by binding to cytoplasmic receptors and modulating gene expression, rather than direct binding to specific antigens or receptors on immune cells.
A nurse is administering fludrocortisone (Florinef), a mineralocorticoid, to a client who has Addison's disease. What are some of the expected pharmacologic effects of fludrocortisone in this condition?
Explanation
Fludrocortisone is a synthetic mineralocorticoid that is used in the treatment of Addison's disease, a condition characterized by deficient production of adrenal hormones, including cortisol and aldosterone. Fludrocortisone primarily acts as a replacement for aldosterone, which is responsible for regulating electrolyte balance and fluid volume in the body.
A. It promotes sodium reabsorption and potassium excretion in the kidney, increasing blood volume and blood pressure: Fludrocortisone mimics the action of aldosterone by promoting the reabsorption of sodium and the excretion of potassium in the kidneys. This leads to an increase in blood volume and blood pressure, helping to manage the hypotension that is often associated with Addison's disease.
B. It reduces inflammation, pain, fever, and allergic reactions by inhibiting the synthesis of prostaglandins and leukotrienes: This description corresponds to the pharmacologic effects of glucocorticoids rather than mineralocorticoids like fludrocortisone. While glucocorticoids can have anti-inflammatory effects, fludrocortisone primarily focuses on the mineralocorticoid actions related to electrolyte balance.
C. It regulates the secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary gland, maintaining the feedback loop of cortisol production: Fludrocortisone does not directly regulate the secretion of ACTH. It primarily acts at the level of the kidneys to promote sodium reabsorption and potassium excretion.
D. It influences the carbohydrate, protein, and fat metabolism in various tissues, increasing blood glucose and suppressing immune response: These effects are associated with glucocorticoids rather than mineralocorticoids. Fludrocortisone primarily focuses on the mineralocorticoid effects related to electrolyte balance rather than the metabolic and immunosuppressive actions of glucocorticoids.
A nurse is teaching a client who has Crohn's disease and is prescribed azathioprine (Imuran), an antimetabolite. What should the nurse include in the teaching?
Explanation
Azathioprine (Imuran) is an antimetabolite medication that is commonly used in the treatment of Crohn's disease. It works by suppressing the immune system and reducing inflammation. When teaching a client about azathioprine, the nurse should include important information about potential side effects and adverse reactions.
A. The drug may cause bone marrow suppression and increase the risk of infection and bleeding: Azathioprine can suppress the bone marrow, leading to decreased production of blood cells, including white blood cells, red blood cells, and platelets. This can increase the risk of infections, as well as bleeding tendencies.
B. The drug may cause nephrotoxicity and increase the risk of renal impairment and electrolyte imbalances: While azathioprine can have adverse effects on the kidneys in some cases, nephrotoxicity is not a commonly reported side effect. It is not a primary concern when using azathioprine in the treatment of Crohn's disease.
C. The drug may cause neurotoxicity and increase the risk of tremor, headache, and seizures: Neurotoxicity is not a commonly reported side effect of azathioprine. The potential for neurotoxicity is relatively low compared to other adverse effects associated with the medication.
D. The drug may cause hepatotoxicity and increase the risk of liver impairment and jaundice: Azathioprine has the potential to cause hepatotoxicity in some individuals, but it is not a commonly observed side effect. Liver impairment and jaundice are rare adverse effects associated with azathioprine use.
A nurse is evaluating a client who has ulcerative colitis and is receiving infliximab (Remicade), a monoclonal antibody. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
A. Decreased frequency and severity of diarrhea, abdominal pain, and rectal bleeding . These are the main symptoms of ulcerative colitis, a chronic inflammatory condition of the colon and rectum that causes ulcers, bleeding, and mucus production in the lining of the bowel. Infliximab is a monoclonal antibody that works by blocking the action of tumor necrosis factor-alpha (TNF-alpha), a cytokine that mediates inflammation and tissue damage in ulcerative colitis. Infliximab can reduce the inflammation and ulceration of the bowel and improve the clinical symptoms of ulcerative colitis .
B. Improved endoscopic findings and mucosal healing . Endoscopy is a procedure that uses a flexible tube with a camera and light to examine the inside of the digestive tract. Mucosal healing is the restoration of the normal structure and function of the bowel lining. Infliximab can improve the endoscopic appearance and mucosal healing of the colon and rectum in patients with ulcerative colitis . This may reduce the risk of complications such as strictures, fistulas, abscesses, or cancer .
C. Decreased levels of inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) . CRP and ESR are blood tests that measure the level of inflammation in the body. CRP is a protein produced by the liver in response to inflammation, and ESR is a measure of how fast red blood cells settle in a tube of blood. Both tests are elevated in patients with ulcerative colitis due to the chronic inflammation of the bowel. Infliximab can lower the levels of CRP and ESR by reducing the inflammation and tissue damage in ulcerative colitis . This may reflect the improvement in disease activity and prognosis .
D. Resolution of extraintestinal manifestations associated with ulcerative colitis (e.g., joint pain, skin lesions) . Extraintestinal manifestations are symptoms or conditions that affect other organs or systems outside the digestive tract. They occur in about 25% of patients with ulcerative colitis and may include arthritis (joint inflammation), uveitis (eye inflammation), erythema nodosum (skin nodules), pyoderma gangrenosum (skin ulcers), primary sclerosing cholangitis (liver inflammation), or ankylosing spondylitis (spine inflammation) . Infliximab can resolve or improve some of these extraintestinal manifestations by blocking TNF-alpha, which is involved in their pathogenesis .
Adverse effects of corticosteroids and immunosuppressants
A nurse is caring for a client who has systemic lupus erythematosus and is prescribed prednisone, a glucocorticoid. What are some of the indications of prednisone in this condition? (Select all that apply)
Explanation
- It reduces the immune-mediated damage to the self-tissues by inhibiting the synthesis of inflammatory mediators and suppressing the activation and proliferation of immune cells . Systemic lupus erythematosus is an autoimmune disease that affects multiple organ systems. It is characterized by autoantibody production that targets the self-tissues and causes inflammation and tissue damage. Prednisone is a glucocorticoid that works by inhibiting the synthesis of cytokines, chemokines, and other inflammatory mediators that mediate the immune response. Prednisone also suppresses the activation and proliferation of T cells, B cells, macrophages, and other immune cells that are involved in the pathogenesis of systemic lupus erythematosus .
- It reduces the inflammation and allergic reactions by inhibiting the synthesis of prostaglandins and leukotrienes . Prostaglandins and leukotrienes are lipid-derived inflammatory mediators that are involved in pain, fever, vasodilation, edema, and bronchoconstriction. Prednisone inhibits the enzyme cyclooxygenase (COX), which is responsible for converting arachidonic acid into prostaglandins. Prednisone also inhibits the enzyme 5-lipoxygenase, which is responsible for converting arachidonic acid into leukotrienes. By inhibiting these enzymes, prednisone reduces the production of prostaglandins and leukotrienes and their associated inflammatory and allergic effects .
The other options are incorrect because:
- A. It prevents or treats transplant rejection by suppressing the immune response to the foreign antigens on the donor organ is not an indication of prednisone in systemic lupus erythematosus. This is an indication of prednisone in organ transplantation, which is a different condition. Organ transplantation involves replacing a diseased or damaged organ with a healthy one from a donor. The immune system may recognize the donor organ as foreign and attack it, causing transplant rejection. Prednisone can prevent or treat transplant rejection by suppressing the immune response to the foreign antigens on the donor organ .
- D. It kills or inhibits the growth of malignant cells by interfering with the synthesis of nucleic acids is not an indication of prednisone in systemic lupus erythematosus. This is an indication of prednisone in cancer, which is a different condition. Cancer involves abnormal or uncontrolled growth of cells that invade and destroy normal tissues. Prednisone can kill or inhibit the growth of malignant cells by interfering with the synthesis of nucleic acids, which are essential for cell division and replication .
A nurse is administering fludrocortisone (Florinef), a mineralocorticoid, to a client who has Addison's disease. What are some of the contraindications for this drug? (Select all that apply)
Explanation
Known hypersensitivity to fludrocortisone or any component of the drug . Hypersensitivity is an exaggerated or inappropriate immune reaction to a substance that can cause allergic reactions such as rash, itching, hives, swelling, or difficulty breathing. The nurse should instruct the client to stop taking fludrocortisone and seek immediate medical attention if they experience any of these symptoms.
Pregnancy . Pregnancy is a condition in which a woman carries a developing fetus in her uterus. Fludrocortisone is a mineralocorticoid that can cross the placenta and affect the fetus. Fludrocortisone can cause fetal growth retardation, low birth weight, cleft palate, and adrenal insufficiency in the newborn. The nurse should instruct the client to use effective contraception while taking fludrocortisone and to inform their doctor if they become pregnant or plan to become pregnant.
Lactation . Lactation is the production and secretion of breast milk by a woman who has given birth. Fludrocortisone is a mineralocorticoid that can pass into breast milk and affect the nursing infant. Fludrocortisone can cause electrolyte imbalance, growth suppression, and adrenal suppression in the infant. The nurse should instruct the client not to breastfeed while taking fludrocortisone and to consult their doctor about alternative feeding methods.
The other options are incorrect because:
B. Diabetes mellitus, hypertension, heart failure, osteoporosis, glaucoma, cataracts, renal or hepatic impairment, bleeding disorders, and concurrent use of other immunosuppressive agents or live vaccines are not contraindications for fludrocortisone, but they are cautions or risk factors that may increase the likelihood of adverse effects or require dose adjustment or monitoring . These are conditions or factors that may affect the metabolism, excretion, efficacy, or safety of fludrocortisone. The nurse should assess the client's medical history and current medications before administering fludrocortisone and monitor their vital signs, blood glucose, electrolytes, bone density, intraocular pressure, liver function tests, coagulation tests, and immune status during treatment. The nurse should also educate the client about the potential adverse effects of fludrocortisone and how to prevent or manage them.
C. Hypertension, heart failure, renal or hepatic impairment, and concurrent use of other immunosuppressive agents or live vaccines are not specific contraindications for fludrocortisone, but they are cautions or risk factors that may increase the likelihood of adverse effects or require dose adjustment or monitoring . These are conditions or factors that may affect the metabolism, excretion, efficacy, or safety of fludrocortisone. The nurse should assess the client's medical history and current medications before administering fludrocortisone and monitor their vital signs, blood glucose, electrolytes, bone density, intraocular pressure, liver function tests, coagulation tests. The nurse should assess the client's medical history and current medications before administering fludrocortisone and monitor their vital signs, blood glucose, electrolytes, bone density, intraocular pressure, liver function tests, coagulation tests, and immune status during treatment. The nurse should also educate the client about the potential adverse effects of fludrocortisone and how to prevent or manage them.
D. Active infection, malignancy, pregnancy, lactation, peptic ulcer disease, and bleeding disorders are not specific contraindications for fludrocortisone, but they are contraindications for glucocorticoids in general . Glucocorticoids are a class of drugs that include fludrocortisone and prednisone. They have anti-inflammatory, immunosuppressive, and metabolic effects by binding to glucocorticoid receptors and modulating gene expression. Glucocorticoids can cause serious side effects such as infection, malignancy, teratogenicity, gastrointestinal bleeding and ulceration, and bleeding disorders by suppressing the immune system, increasing the risk of opportunistic infections and cancers, crossing the placenta and breast milk, inhibiting gastric mucosal protection and healing, and reducing platelet aggregation and clotting factors . The nurse should use glucocorticoids with caution in patients with these conditions or risk factors and monitor them closely for signs and symptoms of complications.
A nurse is teaching a client who has Crohn's disease and is prescribed azathioprine (Imuran), an antimetabolite. What are some of the adverse effects that the nurse should watch for?
Explanation
A. Infection due to suppression of the immune system and increased susceptibility to opportunistic pathogens such as fungi, viruses, bacteria, and parasites . Azathioprine is an antimetabolite that works by suppressing the immune system and reducing inflammation. It is used to treat Crohn's disease, a chronic inflammatory condition of the digestive tract that causes symptoms such as abdominal pain, diarrhea, weight loss, and fever. Azathioprine can reduce the ability of the immune system to fight off infections and increase the risk of serious or fatal infections. The nurse should instruct the client to monitor their temperature and white blood cell count regularly and report any signs of infection (such as fever, chills, sore throat, cough, or wound drainage) to their doctor. The nurse should also advise the client to avoid contact with people who have infections and to receive prophylactic antibiotics or antifungals as prescribed.
B. Gastrointestinal effects such as nausea, vomiting, diarrhea, ulceration, and bleeding due to irritation or erosion of the gastric mucosa, and hepatotoxicity due to metabolic stress on the liver . Azathioprine is an antimetabolite that works by interfering with the synthesis of nucleic acids, which are essential for cell division and replication. Azathioprine can affect the rapidly dividing cells of the gastrointestinal tract and cause gastrointestinal effects such as nausea, vomiting, diarrhea, ulceration, and bleeding. Azathioprine can also affect the liver and cause hepatotoxicity such as elevated liver enzymes, jaundice (yellowing of skin or eyes), hepatitis (inflammation of liver), or liver failure. The nurse should instruct the client to take azathioprine with food or milk to reduce stomach irritation and to drink plenty of fluids to prevent dehydration. The nurse should also instruct the client to monitor their liver function tests regularly and report any signs of liver injury (such as nausea, vomiting, anorexia (loss of appetite), fatigue, dark urine, or clay-colored stools) to their doctor.
C. Bone marrow suppression such as anemia (low red blood cell count), leukopenia (low white blood cell count), thrombocytopenia (low platelet count) due to interference with the synthesis of nucleic acids . Azathioprine is an antimetabolite that works by interfering with the synthesis of nucleic acids, which are essential for cell division and replication. Azathioprine can affect the rapidly dividing cells of the bone marrow and cause bone marrow suppression such as anemia, leukopenia, thrombocytopenia. These conditions can cause symptoms such as fatigue, weakness, pallor (pale skin), shortness of breath, increased susceptibility to infection, bruising, bleeding, or petechiae (small red spots on skin). The nurse should instruct the client to monitor their blood counts regularly and report any abnormal results or signs of bone marrow suppression to their doctor. The nurse should also advise the client to avoid activities that may cause injury or bleeding and to use caution when using sharp objects or dental floss.
D. Skin reactions such as rash, pruritus (itching), alopecia (hair loss), and photosensitivity (increased sensitivity to sunlight) due to hypersensitivity or allergic response to the drug . Azathioprine is an antimetabolite that can cause skin reactions such as rash, pruritus, alopecia. Azathioprine is an antimetabolite that can cause skin reactions such as rash, pruritus, alopecia, and photosensitivity due to hypersensitivity or allergic response to the drug . The nurse should instruct the client to stop taking azathioprine and seek immediate medical attention if they experience any severe or persistent skin reactions. The nurse should also inform the client that they may develop a delayed hypersensitivity reaction after several weeks or months of treatment that may manifest as fever, rash, joint pain, or lymph node enlargement. The nurse should instruct the client to report any of these symptoms to their doctor as well . The nurse should also advise the client to protect their skin from sun exposure by wearing sunscreen, hats, sunglasses, and clothing and to avoid tanning beds or lamps.
The nurse should monitor the client for signs and symptoms of these adverse effects and intervene as appropriate. The nurse should also educate the client about the importance of adhering to the prescribed dosage and schedule of azathioprine and not to stop or change the dose without consulting their doctor. The nurse should also remind the client to follow up with their doctor regularly and to have periodic blood tests to check their blood counts, liver function, and immune status.
A nurse is monitoring a client who has asthma and is receiving fluticasone (Flovent), a corticosteroid, by inhalation. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
Decreased frequency and severity of asthma attacks, wheezing, coughing, and dyspnea . These are the main symptoms of asthma, a chronic respiratory condition that causes inflammation and narrowing of the airways, resulting in difficulty breathing. Fluticasone is a corticosteroid that works by reducing inflammation and mucus production in the airways. Fluticasone can prevent or reduce the occurrence and intensity of asthma attacks and improve the airflow and lung function in patients with asthma .
The other options are incorrect because:
B. Increased appetite, weight gain, energy level, and quality of life are not outcomes that indicate the effectiveness of fluticasone therapy for asthma. These are outcomes that indicate the effectiveness of systemic corticosteroids such as prednisone or hydrocortisone, which are used to treat severe or life-threatening asthma exacerbations or other inflammatory conditions. Systemic corticosteroids have anti-inflammatory, immunosuppressive, and metabolic effects by binding to glucocorticoid receptors and modulating gene expression. Systemic corticosteroids can increase appetite, weight gain, energy level, and quality of life by reducing inflammation, pain, fatigue, and stress. However, systemic corticosteroids also have many adverse effects such as infection, osteoporosis, diabetes, hypertension, cataracts, glaucoma, mood changes, insomnia, acne. - Continue with the answer above. Systemic corticosteroids also have many adverse effects such as infection, osteoporosis, diabetes, hypertension, cataracts, glaucoma, mood changes, insomnia, acne, hirsutism, and adrenal suppression. Therefore, systemic corticosteroids should be used at the lowest effective dose and for the shortest possible duration to achieve the desired outcomes . Fluticasone is an inhaled corticosteroid that works locally in the lungs and has minimal systemic effects. Fluticasone does not have the same benefits or risks as systemic corticosteroids .
C. Normalized blood glucose, electrolytes, blood count, and liver function tests are not outcomes that indicate the effectiveness of fluticasone therapy for asthma. These are outcomes that indicate the prevention or reduction of adverse effects of systemic corticosteroids such as prednisone or hydrocortisone, which are used to treat severe or life-threatening asthma exacerbations or other inflammatory conditions. Systemic corticosteroids have anti-inflammatory, immunosuppressive, and metabolic effects by binding to glucocorticoid receptors and modulating gene expression. Systemic corticosteroids can affect blood glucose, electrolytes, blood count, and liver function tests by altering carbohydrate, protein, fat, water, and mineral metabolism. The nurse should monitor these parameters regularly and report any abnormal results or changes to the doctor. The nurse should also educate the client about the potential adverse effects of systemic corticosteroids and how to prevent or manage them. Fluticasone is an inhaled corticosteroid that works locally in the lungs and has minimal systemic effects. Fluticasone does not have the same effects or risks as systemic corticosteroids .
D. Reduced inflammation and mucus production in the airways is not an outcome that indicates the effectiveness of fluticasone therapy for asthma. This is a mechanism of action of fluticasone therapy for asthma. Fluticasone is a corticosteroid that works by reducing inflammation and mucus production in the airways. Fluticasone can prevent or reduce the occurrence and intensity of asthma attacks and improve the airflow and lung function in patients with asthma . However, this mechanism of action is not directly observable or measurable by the client or the nurse. The nurse should evaluate the outcomes that reflect the clinical improvement of asthma symptoms and signs such as decreased frequency and severity of asthma attacks, wheezing, coughing, and dyspnea; improved peak expiratory flow and forced expiratory volume in one second; and reduced need for rescue medication such as short-acting beta2 agonists.
A nurse is evaluating a client who has ulcerative colitis and is receiving infliximab (Remicade), a monoclonal antibody. What are some of the nursing considerations for this drug?
Explanation
A. It should be given intravenously slowly over 2 hours to prevent infusion reactions such as fever, chills, rash, pruritus, and dyspnea . Infliximab is a monoclonal antibody that works by blocking the action of tumor necrosis factor-alpha (TNF-alpha), a cytokine that mediates inflammation and tissue damage in ulcerative colitis. Infliximab can cause infusion reactions such as fever, chills, rash, pruritus, and dyspnea during or shortly after the infusion. These reactions are usually mild to moderate and can be prevented or managed by slowing down the infusion rate, premedicating with antihistamines, acetaminophen, or corticosteroids, and monitoring the vital signs and symptoms of the client. The nurse should instruct the client to report any signs of infusion reaction to the health care provider immediately.
B. It should be given with concomitant immunosuppressive agents such as azathioprine or methotrexate to enhance its efficacy and reduce antibody formation . Infliximab is a monoclonal antibody that works by blocking the action of TNF-alpha, a cytokine that mediates inflammation and tissue damage in ulcerative colitis. Infliximab can lose its efficacy over time due to the formation of antibodies against it. These antibodies can also increase the risk of adverse effects such as infusion reactions, infection, or malignancy. To prevent or reduce antibody formation, infliximab should be given with concomitant immunosuppressive agents such as azathioprine or methotrexate. These agents can also enhance the efficacy of infliximab by suppressing the immune system and reducing inflammation. The nurse should instruct the client to take these agents as prescribed by their doctor and to monitor their blood counts and liver function tests regularly.
C. It should be given with prophylactic antibiotics or antifungals to prevent infection due to suppression of the immune system . Infliximab is a monoclonal antibody that works by blocking the action of TNF-alpha, a cytokine that mediates inflammation and tissue damage in ulcerative colitis. Infliximab can suppress the immune system and increase the risk of serious or fatal infections such as tuberculosis, fungal infections, bacterial infections, viral infections, or parasitic infections. To prevent or treat these infections, infliximab should be given with prophylactic antibiotics or antifungals as prescribed by their doctor. The nurse should instruct the client to undergo screening tests for latent tuberculosis and hepatitis B before starting infliximab therapy and to report any signs of infection (such as fever, chills, sore throat, cough, or wound drainage) to their doctor. The nurse should also advise the client to avoid contact with people who have infections and to receive inactivated vaccines as recommended by their doctor.
D. It should be monitored for signs of hypersensitivity, infection, malignancy, and hepatotoxicity during and after the infusion . Infliximab is a monoclonal antibody that works by blocking the action of TNF-alpha, a cytokine that mediates inflammation and tissue damage in ulcerative colitis. Infliximab can cause serious adverse effects such as hypersensitivity reactions (such as anaphylaxis or serum sickness), infection (such as tuberculosis or fungal infections), malignancy (such as lymphoma or skin cancer), and hepatotoxicity (such as elevated liver enzymes or liver failure). The nurse should monitor the client for signs and symptoms of these adverse effects during and after the infusion and intervene as appropriate. The nurse should also educate the client about the potential adverse effects of infliximab and how to prevent or manage them.
Nursing considerations for corticosteroids and immunosuppressants
A nurse is caring for a client who has a kidney transplant and is receiving cyclosporine (Sandimmune), a calcineurin inhibitor. What is the primary mechanism of action of cyclosporine in this condition?
Explanation
Cyclosporine blocks the activation of T cells by inhibiting the enzyme calcineurin, which is required for the transcription of interleukin-2¹². Interleukin-2 is a cytokine that stimulates the proliferation and differentiation of T cells, which are responsible for recognizing and attacking foreign antigens on the donor organ. By blocking interleukin-2 production, cyclosporine prevents the activation and expansion of T cells, and thus reduces the immune response to the transplanted organ¹³.
The other options are incorrect because:
- Option A is incorrect because cyclosporine does not inhibit the synthesis of inflammatory mediators or suppress the activation and proliferation of immune cells in general. Cyclosporine is a selective inhibitor of calcineurin, which is mainly involved in T cell activation. Cyclosporine does not affect other inflammatory mediators such as prostaglandins, leukotrienes, or histamine, or other immune cells such as B cells, macrophages, or natural killer cells¹².
C. Option C is incorrect because cyclosporine does not interfere with the synthesis of nucleic acids, which are essential for the replication and function of immune cells. Cyclosporine does not directly affect DNA or RNA synthesis or function, but rather modulates gene expression through its interaction with cyclophilin and calcineurin. Cyclosporine may have some anti-cancer effects by inducing apoptosis or inhibiting angiogenesis in some malignant cells, but this is not its primary mechanism of action¹².
D. Option D is incorrect because cyclosporine does not bind to specific antigens or receptors on the surface of immune cells and either neutralize them or induce their destruction. Cyclosporine acts intracellularly by binding to cyclophilin and inhibiting calcineurin, which are both involved in signal transduction pathways that regulate T cell activation. Cyclosporine does not directly bind to or affect the antigen recognition or receptor-mediated signaling of immune cells¹².
A nurse is administering methylprednisolone (Medrol), a glucocorticoid, to a client who has multiple sclerosis. What are some of the expected pharmacologic effects of methylprednisolone in this condition? (Select all that apply)
Explanation
Methylprednisolone is a synthetic glucocorticoid that reduces inflammation, pain, fever, and allergic reactions by inhibiting the synthesis of prostaglandins and leukotrienes¹². Prostaglandins and leukotrienes are lipid-derived inflammatory mediators that are involved in various inflammatory and allergic conditions such as asthma, rheumatoid arthritis, and anaphylaxis. Methylprednisolone inhibits their synthesis by blocking the enzyme cyclooxygenase (COX) and lipoxygenase (LOX), respectively. Methylprednisolone also influences the carbohydrate, protein, and fat metabolism in various tissues, increasing blood glucose and suppressing immune response¹². Methylprednisolone modulates the expression of genes involved in immune regulation, apoptosis, and cell differentiation by interacting with glucocorticoid receptors.
Multiple sclerosis is a chronic autoimmune disease that affects the central nervous system, causing inflammation, demyelination, and axonal damage³. Methylprednisolone is used to treat acute relapses of multiple sclerosis by reducing the inflammation and edema in the brain and spinal cord³. Methylprednisolone may also have some neuroprotective effects by inhibiting the production of reactive oxygen species and nitric oxide, which can cause oxidative stress and neuronal injury³.
The other options are incorrect because:
Option A is incorrect because methylprednisolone does not promote sodium reabsorption and potassium excretion in the kidney, increasing blood volume and blood pressure. This is the effect of mineralocorticoids such as aldosterone, which regulate the fluid and electrolyte balance in the body. Methylprednisolone has a low affinity for mineralocorticoid receptors and does not have significant mineralocorticoid activity¹².
Option C is incorrect because methylprednisolone does not regulate the secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary gland, maintaining the feedback loop of cortisol production. This is the effect of endogenous glucocorticoids such as cortisol, which are produced by the adrenal cortex in response to ACTH stimulation. Methylprednisolone suppresses the secretion of ACTH from the pituitary gland by negative feedback inhibition, which can lead to adrenal insufficiency if methylprednisolone is discontinued abruptly¹².
A nurse is evaluating a client who has leukemia and is receiving daclizumab (Zenapax), a monoclonal antibody. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
Daclizumab is a humanized monoclonal antibody that blocks IL-2 binding by recognizing the interleukin-2 receptor α chain (CD25)¹². CD25 is overexpressed in some leukemias, especially human T-cell leukemia virus 1 associated adult T-cell leukemia/lymphoma (ATL)²³. Daclizumab may have an antileukemic effect by reducing the proliferation and survival of leukemic cells that depend on IL-2 for growth¹³. Daclizumab may also induce antibody-dependent cellular cytotoxicity (ADCC) or complement-dependent cytotoxicity (CDC) against leukemic cells that express CD25¹⁴. Daclizumab may reduce the number and size of malignant cells in the blood and bone marrow, which are the main sites of leukemia¹³.
The other options are incorrect because:
Option A is incorrect because daclizumab does not decrease the frequency and severity of diarrhea, abdominal pain, and rectal bleeding. These are symptoms of ulcerative colitis, a chronic inflammatory bowel disease that affects the colon and rectum. Daclizumab may be used to treat ulcerative colitis by reducing the inflammation and immune-mediated damage to the intestinal mucosa , but this is not its effect in leukemia.
Option B is incorrect because daclizumab does not increase appetite, weight gain, energy level, and quality of life. These are general indicators of health and well-being that may be affected by various factors such as nutrition, physical activity, mental health, social support, and environmental conditions. Daclizumab may improve some aspects of quality of life for patients with leukemia by reducing symptoms and complications of the disease¹³, but this is not a specific outcome of its therapy.
Option C is incorrect because daclizumab does not normalize stool culture, blood count, electrolytes, and liver function tests. These are laboratory tests that measure different aspects of the body's function and health status. Daclizumab may affect some of these tests by causing side effects such as infection, bone marrow suppression, hepatotoxicity, or electrolyte imbalances¹², but this is not an indication of its effectiveness.
More Questions
A nurse is preparing to administer cyclosporine (Sandimmune), a calcineurin inhibitor, to a client who had a kidney transplant. Which of the following actions should the nurse take? (Select all that apply.)¹
Explanation
A. Shake the oral solution vigorously before administration. This is to ensure that the drug is well mixed and evenly distributed in the solution¹². Cyclosporine is a lipophilic drug that forms a microemulsion in the oral solution, which enhances its absorption and bioavailability¹². Shaking the oral solution helps to maintain the stability and consistency of the microemulsion¹².
B. Dilute the oral solution in a glass container with milk or orange juice. This is to improve the taste and palatability of the drug, which may otherwise be bitter or unpleasant¹². Cyclosporine can be diluted with milk, chocolate milk, or orange juice, but not with grapefruit juice, which can increase its blood levels and toxicity¹². The diluted solution should be consumed immediately or refrigerated and used within 24 hours¹². A glass container should be used instead of a plastic one, which may absorb some of the drug and reduce its dose¹².
C. Administer the medication at the same time every day. This is to maintain a consistent blood level of the drug and avoid fluctuations that may affect its efficacy and safety¹². Cyclosporine has a narrow therapeutic window and requires careful monitoring and dosing adjustment to prevent organ rejection or toxicity¹². Administering the medication at regular intervals helps to achieve optimal blood concentrations and avoid peaks and troughs that may increase the risk of adverse effects or suboptimal response¹².
D. Monitor blood pressure and report hypertension to the provider. This is to detect and manage one of the most common and serious side effects of cyclosporine, which is hypertension¹². Cyclosporine can cause vasoconstriction and sodium retention, which can increase blood pressure and lead to cardiovascular complications such as stroke, heart failure, or kidney damage¹². The nurse should measure blood pressure regularly and report any elevation or signs of hypertensive crisis to the provider¹². The provider may prescribe antihypertensive drugs or adjust the dose of cyclosporine to control blood pressure¹².
E. Obtain serum drug levels periodically to verify therapeutic range. This is to ensure that the dose of cyclosporine is adequate and appropriate for the individual patient's needs and response¹². Cyclosporine has a high inter- and intra-patient variability in pharmacokinetics, which means that its absorption, distribution, metabolism, and excretion can differ significantly among different patients or even within the same patient over time¹². Factors such as age, weight, gender, genetics, diet, drug interactions, organ function, and disease state can affect cyclosporine blood levels and require dose adjustment¹². The nurse should obtain serum drug levels at specified times (usually 12 hours after the last dose) and report them to the provider, who may modify the dose based on the results¹².
A nurse is caring for a client who has gouty arthritis and is taking allopurinol (Zyloprim). Which laboratory value should be monitored periodically?²
Explanation
The laboratory value that should be monitored periodically when taking allopurinol is serum creatinine level. Allopurinol is a drug that lowers the level of uric acid in the blood and urine by inhibiting the enzyme xanthine oxidase, which is involved in the metabolism of purines¹². Allopurinol is used to treat gouty arthritis, a condition that causes painful inflammation of the joints due to the deposition of uric acid crystals¹².
The other options are incorrect because:
- Option A is wrong because serum uric acid level is not the laboratory value that should be monitored periodically when taking allopurinol. Serum uric acid level is the amount of uric acid in the blood, which is a waste product that is produced by the breakdown of purines. Serum uric acid level is usually high in patients with gouty arthritis, which causes inflammation and pain in the joints due to the deposition of uric acid crystals . Allopurinol lowers serum uric acid level by inhibiting xanthine oxidase, which is involved in the metabolism of purines . However, serum uric acid level is not a reliable indicator of allopurinol's effectiveness or toxicity, because it does not reflect the amount of uric acid in the tissues or urine, where it can cause damage or complications . Serum uric acid level may also fluctuate due to various factors such as diet, hydration, renal function, or drug interactions . Therefore, serum uric acid level is not the laboratory value that should be monitored periodically when taking allopurinol.
- Option B is wrong because serum potassium level is not the laboratory value that should be monitored periodically when taking allopurinol. Serum potassium level is the amount of potassium in the blood, which is an electrolyte that is essential for the function of nerves, muscles, and heart. Serum potassium level is normally regulated by the kidneys, which excrete excess potassium or retain potassium when needed . Serum potassium level can be affected by various factors such as diet, hydration, acid-base balance, renal function, or drug interactions . Allopurinol does not have a direct effect on serum potassium level, but it may interact with some drugs that can alter serum potassium level, such as diuretics, angiotensin-converting enzyme inhibitors, or potassium supplements . However, these drug interactions are not specific to allopurinol and can occur with any drug that affects renal function or electrolyte balance . Therefore, serum potassium level is not the laboratory value that should be monitored periodically when taking allopurinol.
- Option D is wrong because serum calcium level is not the laboratory value that should be monitored periodically when taking allopurinol. Serum calcium level is the amount of calcium in the blood, which is a mineral that is involved in various processes such as bone formation, muscle contraction, nerve transmission, and blood clotting. Serum calcium level is normally regulated by the parathyroid glands, which secrete parathyroid hormone (PTH) to increase calcium absorption from the gut and bone resorption from the skeleton . Serum calcium level can be affected by various factors such as diet, hydration, vitamin D status, renal function, or drug interactions . Allopurinol does not have a direct effect on serum calcium level, but it may interact with some drugs that can alter serum calcium level, such as thiazide diuretics, which can increase calcium reabsorption in the kidney and cause hypercalcemia . However, these drug interactions are not specific to allopurinol and can occur with any drug that affects renal function or calcium metabolism . Therefore, serum calcium level is not the laboratory value that should be monitored periodically when taking allopurinol.
A nurse is reviewing discharge instructions with a client who will be taking prednisone (Deltasone) for rheumatoid arthritis. Which statement by the client indicates understanding of the teaching?³
Explanation
D. "I will report any signs of infection to my provider." Prednisone is a synthetic glucocorticoid that is used to treat rheumatoid arthritis, a chronic inflammatory autoimmune disease that affects the joints and other tissues . Prednisone reduces inflammation, pain, swelling, and stiffness by inhibiting the synthesis of inflammatory mediators and suppressing the immune system .
One of the possible side effects of prednisone is infection, which can be serious or life-threatening due to the suppression of the immune system and increased susceptibility to opportunistic pathogens such as fungi, viruses, bacteria, and parasites . The client should monitor for signs of infection such as fever, sore throat, cough, wound drainage, or urinary symptoms, and report them to the provider as soon as possible . The provider may prescribe antibiotics or antifungals to treat the infection or adjust the dose of prednisone to prevent further complications .
The other options are incorrect because:
Option A is wrong because the client should not take prednisone every other day to prevent side effects. Prednisone should be taken as prescribed by the provider, usually once or twice daily with food or milk to prevent gastrointestinal irritation . Prednisone should not be taken every other day or on an irregular schedule, because this can cause fluctuations in blood levels and increase the risk of adverse effects or suboptimal response . Prednisone should also not be stopped abruptly, because this can cause withdrawal symptoms such as fatigue, weakness, nausea, vomiting, or hypotension due to adrenal insufficiency . Prednisone should be tapered gradually under the supervision of the provider to allow the adrenal glands to resume normal cortisol production .
Option B is wrong because the client should not stop taking prednisone if they develop indigestion. Indigestion is a common side effect of prednisone that can be caused by irritation or ulceration of the gastric mucosa due to increased acid secretion and decreased mucus production . The client should not stop taking prednisone without consulting with the provider, because this can cause withdrawal symptoms or worsen their condition . The client should take prednisone with food or milk to reduce gastric irritation and report any severe or persistent indigestion to the provider . The provider may prescribe antacids, histamine-2 blockers, or proton pump inhibitors to protect the stomach lining and prevent bleeding or perforation .
Option C is wrong because the client does not need to increase their intake of foods that are high in potassium. Potassium is an electrolyte that is essential for the function of nerves, muscles, and heart. Potassium levels are normally regulated by the kidneys, which excrete excess potassium or retain potassium when needed . Prednisone does not have a significant effect on potassium levels, unlike mineralocorticoids such as aldosterone, which promote sodium reabsorption and potassium excretion in the kidney . Prednisone may interact with some drugs that can alter potassium levels, such as diuretics, angiotensin-converting enzyme inhibitors, or potassium supplements . However, these drug interactions are not specific to prednisone and can occur with any drug that affects renal function or electrolyte balance . The client should have their potassium levels monitored periodically and follow a balanced diet that meets their nutritional needs . The client should not increase their intake of foods that are high in potassium without consulting with the provider, because this can cause hyperkalemia , which can lead to cardiac arrhythmias or cardiac arrest .
A nurse is reviewing discharge instructions with a client who will be taking celecoxib (Celebrex) for osteoarthritis. Which statement by the client indicates understanding of the teaching?²
Explanation
The statement by the client that indicates understanding of the teaching is B. "I will report any signs of chest pain or shortness of breath to my provider." Celecoxib is a selective COX-2 inhibitor that is used to treat osteoarthritis, a degenerative joint disease that causes pain, stiffness, and reduced mobility . Celecoxib works by inhibiting the enzyme COX-2, which is involved in the synthesis of prostaglandins, thromboxanes, and prostacyclins . These are lipid-derived inflammatory mediators that regulate various physiological processes such as pain, inflammation, blood clotting, and gastric protection .
One of the possible side effects of celecoxib is cardiovascular events, such as myocardial infarction, stroke, or heart failure . Celecoxib can cause cardiovascular events by increasing the risk of thrombosis, vasoconstriction, and hypertension . Celecoxib inhibits the synthesis of prostacyclin, which is a vasodilator and antiplatelet agent that protects the endothelium and prevents thrombus formation . Celecoxib also increases the synthesis of thromboxane A2, which is a vasoconstrictor and proplatelet agent that promotes platelet aggregation and thrombus formation . Celecoxib also reduces the renal excretion of sodium and water, which can increase blood volume and blood pressure . The risk of cardiovascular events is higher in patients who have preexisting cardiovascular disease, diabetes, hypertension, hyperlipidemia, or smoking history , or who use high doses or long-term treatment of celecoxib .
The other options are incorrect because:
Option A is wrong because the client should not take celecoxib with grapefruit juice to enhance its absorption. Grapefruit juice can interact with celecoxib and increase its blood levels and toxicity . Grapefruit juice inhibits the enzyme CYP3A4, which is involved in the metabolism of celecoxib . By inhibiting CYP3A4, grapefruit juice reduces the clearance of celecoxib and increases its bioavailability and half-life . This can lead to overdose or adverse effects such as gastrointestinal bleeding, renal impairment, or liver damage . The client should avoid grapefruit juice and other foods or drinks that can affect the metabolism of celecoxib .
Option C is wrong because the client should not take celecoxib on an empty stomach to avoid nausea. Nausea is a common side effect of celecoxib that can be caused by irritation or ulceration of the gastric mucosa due to decreased mucus production and increased acid secretion . The client should not take celecoxib on an empty stomach, because this can worsen gastric irritation and increase the risk of bleeding or perforation . The client should take celecoxib with food or milk to reduce gastric irritation and report any severe or persistent nausea to the provider . The provider may prescribe antacids, histamine-2 blockers, or proton pump inhibitors to protect the stomach lining and prevent bleeding or perforation .
Option D is wrong because the client should not stop taking celecoxib if they develop a rash or itching. Rash or itching are possible signs of hypersensitivity or allergic reaction to celecoxib , which can be serious or life-threatening. The client should not stop taking celecoxib without consulting with the provider, because this can cause withdrawal symptoms or worsen their condition . The client should monitor for signs of hypersensitivity or allergic reaction such as rash, itching, hives, swelling, difficulty breathing, or anaphylaxis , and report them to the provider as soon as possible . The provider may prescribe antihistamines or corticosteroids to treat the reaction or discontinue celecoxib and switch to another drug.
A nurse is administering aspirin (ASA) to a client who has a history of peptic ulcer disease. Which of the following actions should the nurse take?³
Explanation
Aspirin is a nonsteroidal anti-inflammatory drug (NSAID) that can irritate the stomach lining and increase the risk of ulcers. Proton pump inhibitors (PPIs) and misoprostol are medications that can help protect the stomach lining and reduce the risk of ulcers in people taking NSAIDs. PPIs work by reducing the amount of acid produced by the stomach, while misoprostol helps to replace prostaglandins, which are important for protecting the stomach lining. Giving aspirin with a PPI or misoprostol can help prevent ulcer formation in people with a history of peptic ulcer disease who need to take aspirin.³
The other options are incorrect because:
- A. Give enteric-coated or buffered aspirin to reduce gastric irritation: Enteric-coated aspirin is designed to resist dissolving and being absorbed in the stomach, so it passes into the small intestine, where it’s absorbed into the bloodstream. The goal is to prevent stomach ulcers and bleeding that can sometimes occur with aspirin use. However, research indicates that enteric-coated aspirin may not be as effective as regular aspirin at reducing blood clot risk. Also, the gastrointestinal benefit of enteric-coated aspirin is minimal to nonexistent. When it comes to rates of ulceration and bleeding, there’s no difference between enteric-coated and regular aspirin¹.
- B. Give aspirin with an antacid to neutralize gastric acid: While antacids can help reduce heartburn and upset stomach that aspirin may cause, they do not prevent the formation of ulcers. Aspirin is a nonsteroidal anti-inflammatory drug (NSAID) that can increase the risk of bleeding, including in the stomach and gastrointestinal tract (digestive tract)⁵.
- D. Give aspirin with food or milk to decrease gastric absorption: Taking aspirin with food or milk can help reduce stomach irritation caused by aspirin⁷. However, this does not prevent the formation of ulcers in people with a history of peptic ulcer disease.
A nurse is caring for a client who is taking cyclosporine (Sandimmune), a calcineurin inhibitor, to prevent kidney transplant rejection. Which assessment does the nurse perform as a priority before administering the medication? (Select all that apply.)¹
Explanation
Cyclosporine (Sandimmune) is a calcineurin inhibitor used to prevent organ rejection after a kidney transplant. It works by suppressing the immune system to prevent the body from attacking the transplanted organ. Before administering the medication, the nurse should check the client's blood pressure because cyclosporine can cause hypertension¹. The nurse should also obtain serum drug levels periodically to verify that the medication is within the therapeutic range. This is important because cyclosporine has a narrow therapeutic index, meaning that there is a small difference between an effective dose and a toxic dose. Monitoring drug levels can help ensure that the client is receiving an effective dose while avoiding toxicity¹.
The other options are not the best choices for the following reasons:
B. Checking the client's peripheral pulses: While it is important to monitor the client's peripheral pulses as part of routine care, it is not a priority assessment before administering cyclosporine.
C. Checking the most recent potassium level: Cyclosporine can affect electrolyte levels, including potassium, but it is not a priority assessment before administering the medication.
D. Checking the client's intake-and-output record for the last 24 hours: Monitoring the client's fluid balance is important, but it is not a priority assessment before administering cyclosporine.
Exams on Anti-inflammatory and Immunosuppressive Drugs
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Indications of NSAIDs
- Contraindications of NSAIDs
- Adverse effects of NSAIDs
- Nursing considerations for NSAIDs
- Corticosteroids and immunosuppressants
- Classification of corticosteroids
- Classification of immunosuppressants
- Indications of corticosteroids and immunosuppressants
- Contraindications of corticosteroids and immunosuppressants
- Adverse effects of corticosteroids and immunosuppressants
- Nursing considerations for corticosteroids and immunosuppressants
- Conclusion
- Summary
- First-generation vs second-generation NSAIDs:
- More Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define the immune system and its functions
- Explain the mechanisms of action and pharmacologic effects of NSAIDs, corticosteroids, and immunosuppressants
- Identify the indications, contraindications, adverse effects, and nursing considerations of NSAIDs, corticosteroids, and immunosuppressants
- Compare and contrast the different types and generations of NSAIDs, corticosteroids, and immunosuppressants
- Apply the nursing process to the care of patients receiving anti-inflammatory and immunosuppressive drugs
- Evaluate the outcomes and effectiveness of anti-inflammatory and immunosuppressive therapy
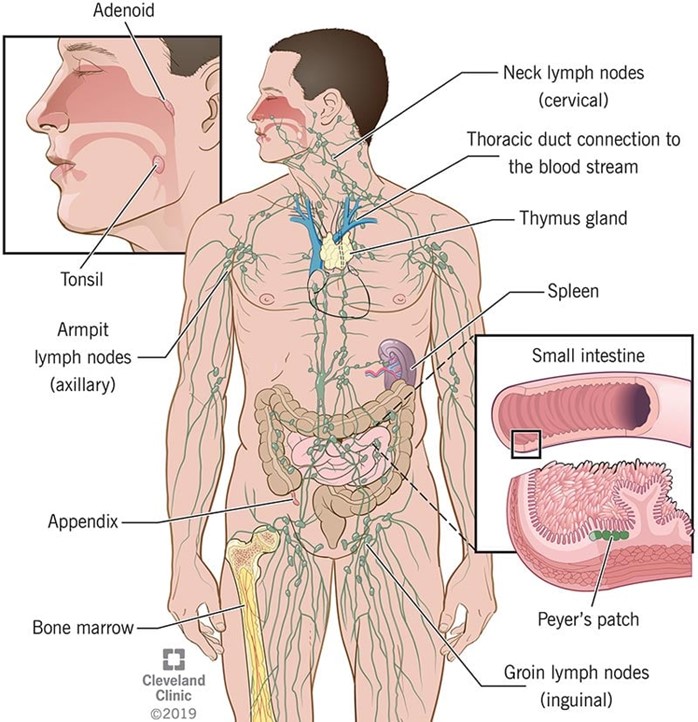
Introduction
- Anti-inflammatory and immunosuppressive drugs are medications that modulate the immune system and reduce inflammation, pain, fever, and allergic reactions
- They are used to treat various conditions such as rheumatoid arthritis, osteoarthritis, gout, asthma, allergic disorders, inflammatory bowel disease, transplant rejection, autoimmune diseases, and cancer
- They have different mechanisms of action, pharmacokinetics, pharmacodynamics, and side effects depending on their chemical structure, selectivity, and dosage
- They require careful monitoring and assessment to prevent or manage potential complications such as gastrointestinal bleeding, infection, renal impairment, cardiovascular events, osteoporosis, hyperglycemia, electrolyte imbalances, hormonal disturbances, and psychological changes

Nonsteroidal anti-inflammatory drugs (NSAIDs)
- NSAIDs are a group of drugs that inhibit the enzyme cyclooxygenase (COX), which is responsible for the synthesis of prostaglandins from arachidonic acid
- Prostaglandins are mediators of inflammation, pain, fever, platelet aggregation, gastric mucosal protection, renal blood flow, and uterine contraction
- NSAIDs block the production of prostaglandins and thus have analgesic (pain-relieving), antipyretic (fever-reducing), anti-inflammatory (inflammation-reducing), and antiplatelet (blood clot-preventing) effects
- NSAIDs can be classified into two main types: nonselective COX inhibitors and selective COX-2 inhibitors
Nonselective COX inhibitors:
- Nonselective COX inhibitors block both COX-1 and COX-2 enzymes
- COX-1 is constitutively expressed in most tissues and is involved in physiological functions such as gastric mucosal protection, platelet aggregation, and renal blood flow
- COX-2 is inducibly expressed in response to inflammatory stimuli and is involved in pathological functions such as inflammation, pain, fever, and tumorigenesis
- Nonselective COX inhibitors have more adverse effects than selective COX-2 inhibitors because they inhibit both beneficial and harmful prostaglandins
- Examples of nonselective COX inhibitors are aspirin (ASA), ibuprofen (Motrin), naproxen (Naprosyn), indomethacin (Indocin), ketorolac (Toradol), diclofenac (Voltaren), etc.
Selective COX-2 inhibitors:
- Selective COX-2 inhibitors block only COX-2 enzyme and spare COX-1 enzyme
- They have less gastrointestinal toxicity than nonselective COX inhibitors because they do not interfere with gastric mucosal protection by prostaglandins
- However, they have more cardiovascular risk than nonselective COX inhibitors because they inhibit vasodilatory and antiplatelet prostaglandins produced by COX-2 in the endothelium
- Examples of selective COX-2 inhibitors are celecoxib (Celebrex), rofecoxib (Vioxx), valdecoxib (Bextra), etc.
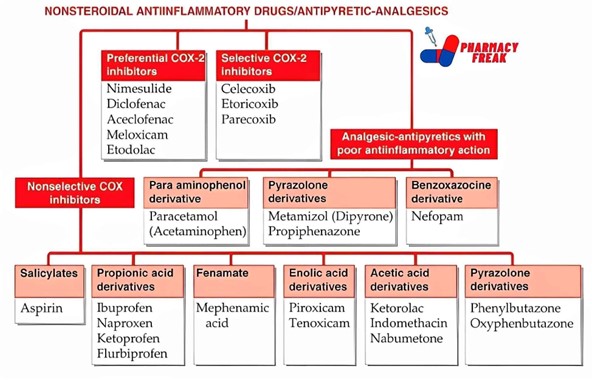
Indications of NSAIDs
- NSAIDs are indicated for the treatment of inflammatory disorders such as rheumatoid arthritis, osteoarthritis, bursitis, gout, ankylosing spondylitis, etc.
- They are also indicated for the relief of mild to moderate pain such as headache, dental pain, musculoskeletal pain, dysmenorrhea, postoperative pain, etc.
- They are also indicated for the reduction of fever in various infections or inflammatory conditions
- Some NSAIDs have specific indications such as aspirin for the prevention of cardiovascular events, ketorolac for short-term management of moderate to severe pain, and indomethacin for patent ductus arteriosus
Contraindications of NSAIDs
- NSAIDs are contraindicated in patients with hypersensitivity to any NSAID or salicylate, history of peptic ulcer disease or gastrointestinal bleeding, renal or hepatic impairment, bleeding disorders, pregnancy (especially third trimester), and lactation
- NSAIDs should be used with caution in patients with asthma, hypertension, heart failure, diabetes, dehydration, alcoholism, smoking, advanced age, and concurrent use of anticoagulants, glucocorticoids, or other NSAIDs
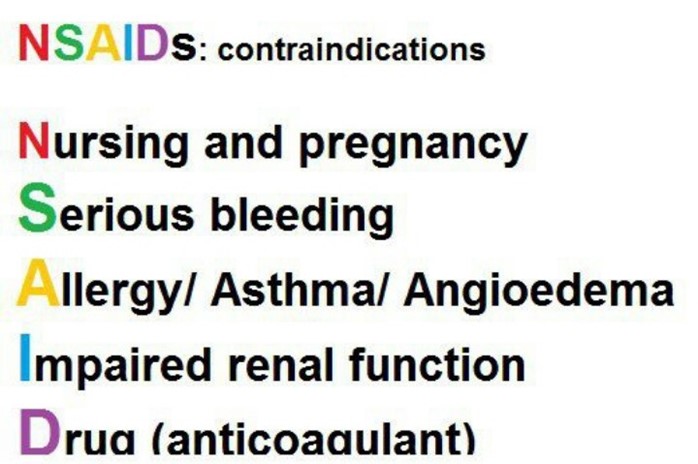
Adverse effects of NSAIDs
- The most common adverse effects of NSAIDs are gastrointestinal effects such as nausea, vomiting, dyspepsia, ulceration, bleeding, and perforation
- The risk of gastrointestinal effects can be reduced by taking NSAIDs with food or milk, using the lowest effective dose and duration, avoiding alcohol and smoking, and using a proton pump inhibitor or a misoprostol (a synthetic prostaglandin) as prophylaxis
- The most serious adverse effects of NSAIDs are renal effects such as reduced glomerular filtration rate, sodium and water retention, edema, hypertension, acute renal failure, and interstitial nephritis
- The risk of renal effects can be reduced by monitoring renal function tests, blood pressure, and fluid status, avoiding dehydration and concurrent use of nephrotoxic drugs, and discontinuing NSAIDs at the first sign of renal impairment
- Other adverse effects of NSAIDs include cardiovascular effects such as increased risk of myocardial infarction and stroke due to platelet aggregation and vasoconstriction (more with selective COX-2 inhibitors), hematologic effects such as bleeding and anemia due to inhibition of platelet function and gastric erosion (more with nonselective COX inhibitors), hypersensitivity reactions such as rash, urticaria, angioedema, bronchospasm, and anaphylaxis due to cross-sensitivity among NSAIDs and salicylates, and central nervous system effects such as headache, dizziness, confusion, and mood changes due to altered prostaglandin synthesis in the brain

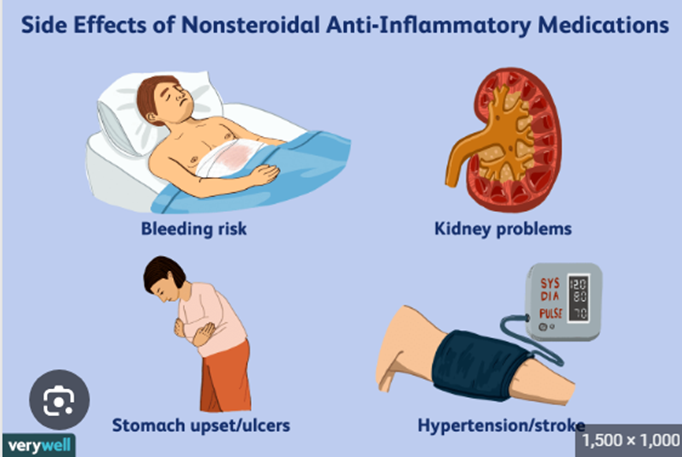
Nursing considerations for NSAIDs
- Before administering NSAIDs, obtain a thorough medical history and physical examination, assess for contraindications and drug interactions, and evaluate the baseline renal function tests, blood pressure, fluid status, and pain level
- During administration of NSAIDs, give oral forms with food or milk to minimize gastrointestinal irritation, give intravenous forms slowly over 15 to 30 minutes to prevent hypotension or thrombophlebitis, and monitor the infusion site for signs of inflammation or extravasation
- After administration of NSAIDs, monitor the patient for therapeutic effects such as reduced pain, inflammation, fever, and dysmenorrhea, and for adverse effects such as gastrointestinal bleeding, renal impairment, cardiovascular events, bleeding disorders, hypersensitivity reactions, and central nervous system changes
- Educate the patient about the proper use of NSAIDs, the potential side effects and complications, the need for regular follow-up and laboratory tests, the importance of reporting any signs of bleeding, infection, or renal impairment, and the avoidance of alcohol,
smoking, and other NSAIDs or salicylates
Corticosteroids and immunosuppressants
- Corticosteroids are synthetic derivatives of the natural hormones cortisol and aldosterone produced by the adrenal cortex
- They have potent anti-inflammatory and immunosuppressive effects by inhibiting the synthesis of inflammatory mediators such as prostaglandins, leukotrienes, histamine, cytokines, and adhesion molecules, and by suppressing the activation and proliferation of lymphocytes, macrophages, eosinophils, and mast cells
- They also have metabolic effects by influencing the carbohydrate, protein, and fat metabolism in various tissues
- They also have endocrine effects by regulating the secretion of adrenocorticotropic hormone (ACTH) from the anterior pituitary gland through a negative feedback mechanism
- Immunosuppressants are drugs that suppress or prevent the immune response by interfering with the activation or function of immune cells or molecules
- They are used to prevent or treat transplant rejection or autoimmune diseases by reducing the immune-mediated damage to the transplanted organ or the self-tissues
- They have different mechanisms of action depending on their target in the immune system
Classification of immunosuppressants
- Immunosuppressants can be classified into four main categories: calcineurin inhibitors, antimetabolites, monoclonal antibodies, and corticosteroids
- Calcineurin inhibitors block the activation of T cells by inhibiting the enzyme calcineurin, which is required for the transcription of interleukin-2 (IL-2), a cytokine that stimulates T cell proliferation and differentiation
- Examples of calcineurin inhibitors are cyclosporine (Sandimmune), tacrolimus (Prograf), and pimecrolimus (Elidel)
- Antimetabolites interfere with the synthesis of nucleic acids, which are essential for the replication and function of immune cells
- Examples of antimetabolites are azathioprine (Imuran), mycophenolate mofetil (CellCept), and methotrexate (Rheumatrex)
- Monoclonal antibodies bind to specific antigens or receptors on the surface of immune cells and either neutralize them or induce their destruction
- Examples of monoclonal antibodies are basiliximab (Simulect), daclizumab (Zenapax), muromonab-CD3 (Orthoclone OKT3), infliximab (Remicade), adalimumab (Humira), etc.
- Corticosteroids have anti-inflammatory and immunosuppressive effects by inhibiting the synthesis of inflammatory mediators and suppressing the activation and proliferation of immune cells
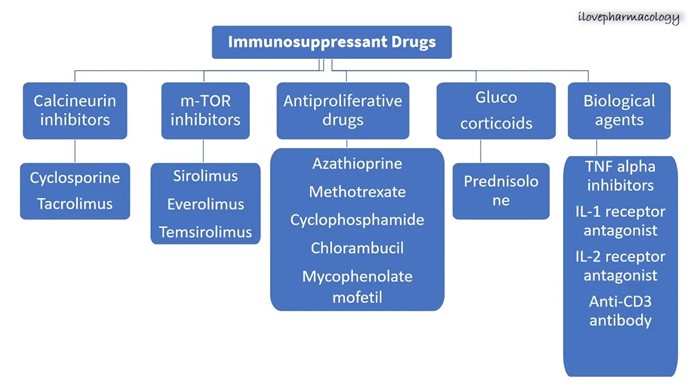
Indications of corticosteroids and immunosuppressants
- Corticosteroids and immunosuppressants are indicated for the prevention or treatment of transplant rejection by suppressing the immune response to the foreign antigens on the donor organ
- They are also indicated for the treatment of autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, myasthenia gravis, Crohn's disease, ulcerative colitis, etc. by reducing the immune-mediated damage to the self-tissues
- They are also indicated for the treatment of inflammatory disorders such as asthma, allergic rhinitis, dermatitis, etc. by reducing the inflammation and allergic reactions
- They are also indicated for the treatment of some cancers such as leukemia, lymphoma, etc. by killing or inhibiting the growth of malignant cells
Contraindications of corticosteroids and immunosuppressants
- Corticosteroids and immunosuppressants are contraindicated in patients with hypersensitivity to any component of the drug, active infection, malignancy, pregnancy, lactation, and peptic ulcer disease
- They should be used with caution in patients with diabetes mellitus, hypertension, heart failure, osteoporosis, glaucoma, cataracts, renal or hepatic impairment, bleeding disorders, and concurrent use of other immunosuppressive agents or live vaccines
Adverse effects of corticosteroids and immunosuppressants
- The most common adverse effects of corticosteroids and immunosuppressants are infection due to suppression of the immune system and increased susceptibility to opportunistic pathogens such as fungi, viruses, bacteria, and parasites
- The risk of infection can be reduced by monitoring the patient's temperature, white blood cell count,
and signs and symptoms of infection, avoiding exposure to infectious agents, and administering prophylactic antibiotics or antifungals as prescribed
- Other adverse effects of corticosteroids and immunosuppressants include gastrointestinal effects such as nausea, vomiting, diarrhea, ulceration, and bleeding due to irritation or erosion of the gastric mucosa, and hepatotoxicity due to metabolic stress on the liver
- The risk of gastrointestinal effects can be reduced by taking the drugs with food or milk, using enteric-coated or delayed-release formulations, and using a proton pump inhibitor or misoprostol as prophylaxis
- The risk of hepatotoxicity can be reduced by monitoring liver function tests, avoiding alcohol and other hepatotoxic drugs, and discontinuing the drugs at the first sign of liver impairment
Nursing considerations for corticosteroids and immunosuppressants
- Before administering corticosteroids and immunosuppressants, obtain a thorough medical history and physical examination, assess for contraindications and drug interactions, and evaluate the baseline vital signs, weight, blood glucose, electrolytes, blood count, liver and kidney function tests, and infection status
- During administration of corticosteroids and immunosuppressants, give oral forms with food or milk to minimize gastrointestinal irritation, give intravenous forms slowly over 30 to 60 minutes to prevent hypotension or thrombophlebitis, and monitor the infusion site for signs of inflammation or extravasation
- After administration of corticosteroids and immunosuppressants, monitor the patient for therapeutic effects such as reduced inflammation, pain, fever, and rejection symptoms, and for adverse effects such as infection,
gastrointestinal bleeding, hepatotoxicity, hyperglycemia, electrolyte imbalances, osteoporosis, glaucoma, cataracts, psychological changes, etc.
- Educate the patient about the proper use of corticosteroids and immunosuppressants, the potential side effects and complications, the need for regular follow-up and laboratory tests, the importance of reporting any signs of infection, bleeding, or organ impairment, and the avoidance of alcohol, grapefruit t juice, and live vaccines
Conclusion
- Anti-inflammatory and immunosuppressive drugs are medications that modulate the immune system and reduce inflammation, pain, fever, and allergic reactions
- They are used to treat various conditions such as rheumatoid arthritis, osteoarthritis, gout, asthma, allergic disorders, inflammatory bowel disease, transplant rejection, autoimmune diseases, and cancer
- They have different mechanisms of action, pharmacokinetics, pharmacodynamics, and side effects depending on their chemical structure, selectivity, and dosage
- They require careful monitoring and assessment to prevent or manage potential complications such as gastrointestinal bleeding, infection, renal impairment, cardiovascular events, osteoporosis, hyperglycemia, electrolyte imbalances, hormonal disturbances, and psychological changes
Summary
- The immune system is composed of innate and adaptive components that protect the body from foreign invaders
- NSAIDs are drugs that inhibit COX enzymes and block the production of prostaglandins
- NSAIDs have analgesic, antipyretic, anti-inflammatory, and antiplatelet effects
- NSAIDs can be classified into nonselective COX inhibitors (first-generation) and selective COX-2 inhibitors (second-generation)
- NSAIDs are indicated for inflammatory disorders, mild to moderate pain, fever, and dysmenorrhea
- NSAIDs are contraindicated in patients with hypersensitivity, peptic ulcer disease, renal or hepatic impairment, bleeding disorders, pregnancy, and lactation
- NSAIDs can cause gastrointestinal effects (ulceration, bleeding), renal effects (impairment), cardiovascular effects (increased risk of MI and stroke), hematologic effects (bleeding), hypersensitivity reactions (rash, anaphylaxis), and central nervous system effects (headache, dizziness)
- Corticosteroids are synthetic derivatives of cortisol and aldosterone that have anti-inflammatory and immunosuppressive effects
- Corticosteroids can be classified into glucocorticoids (prednisone) and mineralocorticoids (fludrocortisone)
- Corticosteroids are indicated for transplant rejection, autoimmune diseases, inflammatory disorders, and some cancers
- Corticosteroids are contraindicated in patients with hypersensitivity, active infection, malignancy, pregnancy, lactation, and peptic ulcer disease
- Corticosteroids can cause infection (suppression of immune system), gastrointestinal effects (ulceration), hepatotoxicity (metabolic stress), hyperglycemia (carbohydrate metabolism), electrolyte imbalances (sodium retention), osteoporosis (bone resorption), glaucoma (increased intraocular pressure), cataracts (lens opacity), psychological changes (mood swings)
- Immunosuppressants are drugs that suppress or prevent the immune response by interfering with the activation or function of immune cells or molecules
- Immunosuppressants can be classified into calcineurin inhibitors (cyclosporine), antimetabolites (azathioprine), monoclonal antibodies (basiliximab), and corticosteroids
- Immunosuppressants are indicated for transplant rejection and autoimmune diseases
- Immunosuppressants are contraindicated in patients with hypersensitivity, active infection, malignancy
First-generation vs second-generation NSAIDs:
- First-generation NSAIDs are nonselective COX inhibitors that have similar efficacy but different pharmacokinetics and side effects
- Second-generation NSAIDs are selective COX-2 inhibitors that have less gastrointestinal toxicity but more cardiovascular risk than first-generation NSAIDs
- The choice of NSAID depends on the patient's condition, comorbidities, drug interactions, allergies, preferences, and cost
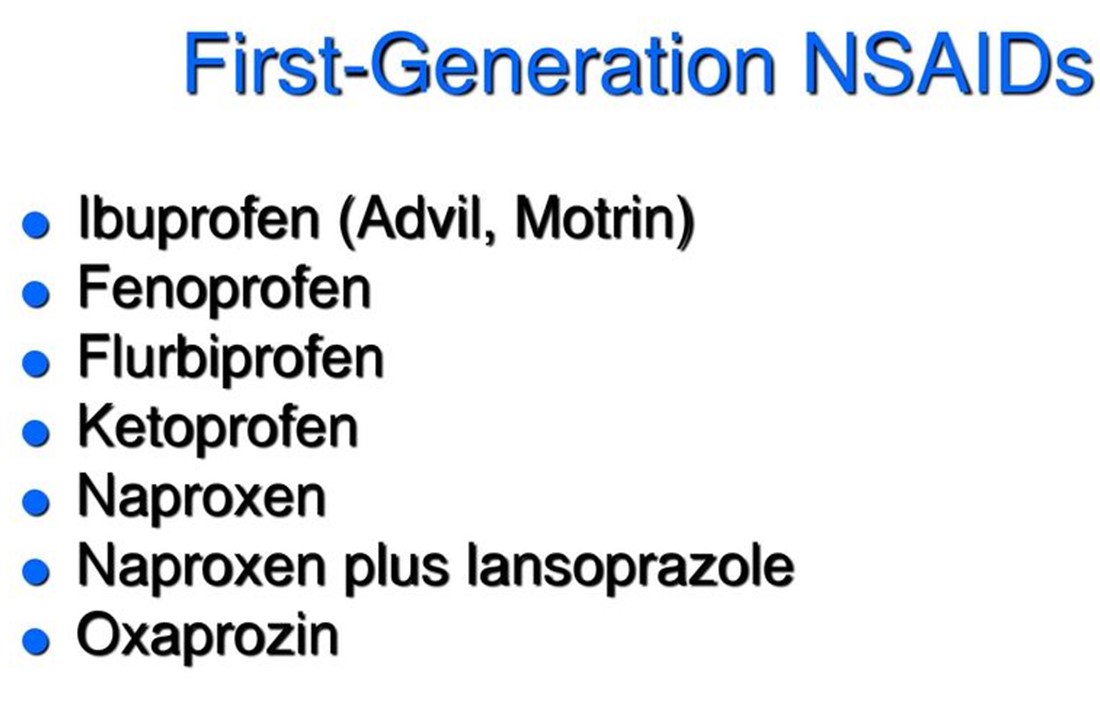
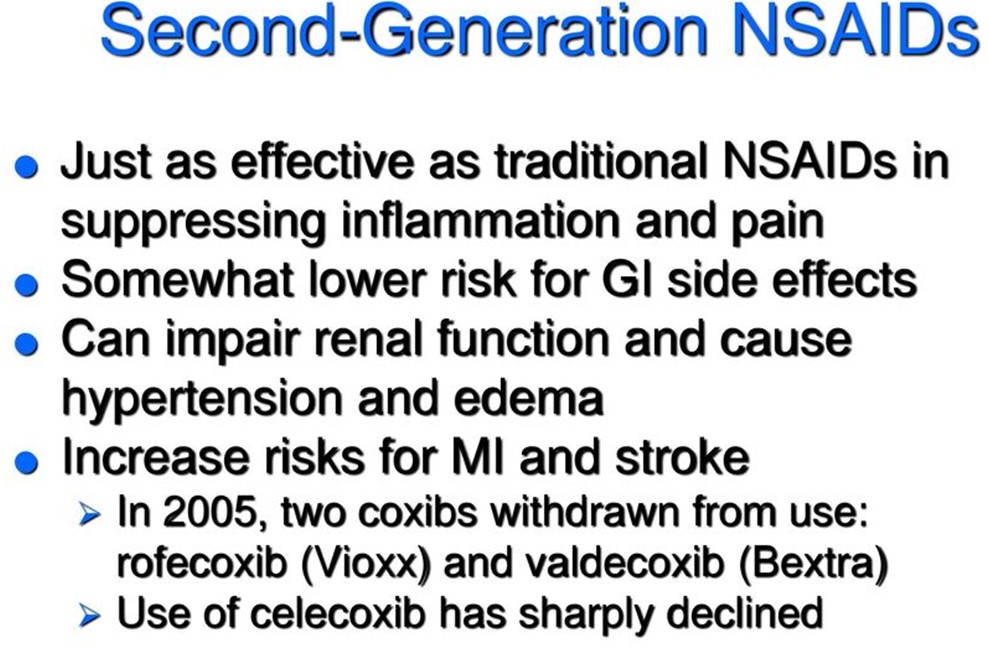
- Corticosteroids can be classified into two main types: glucocorticoids and mineralocorticoids
- Glucocorticoids have anti-inflammatory and immunosuppressive effects as well as metabolic and endocrine effects
- Mineralocorticoids have salt-retaining effects by promoting sodium reabsorption and potassium excretion in the kidney
- Some corticosteroids have different potencies, durations of action, and ratios of glucocorticoid to mineralocorticoid activity
- Examples of glucocorticoids are prednisone (Deltasone), methylprednisolone (Medrol), hydrocortisone (Cortef), dexamethasone (Decadron), etc.
- Examples of mineralocorticoids are fludrocortisone (Florinef), which has both glucocorticoid and mineralocorticoid effects, and desoxycorticosterone (Percorten), which has only mineralocorticoid effects
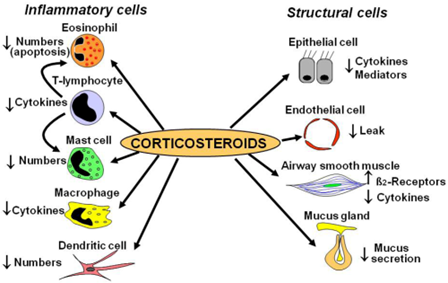
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Anti-inflammatory and Immunosuppressive Drugs
This filled cannot be empty

