Please set your exam date
Newborn Assessment
Study Questions
APGAR Score (0-10)
A nurse is assessing a newborn at 1 minute after birth.
The newborn has a heart rate of 150 bpm, a strong cry, well-flexed muscle tone, pink body with blue hands and feet, and grimaces when suctioned.
What is the newborn’s APGAR score?
Explanation
The newborn’s APGAR score is 8.The APGAR score is a test given to newborns soon after birth to assess their health based on five categories: appearance, pulse, grimace, activity, and respiration.Each category is scored from 0 to 2 points, with a total score of 10 being the best.A score of 7 to 10 is normal and indicates that the newborn is in good health.
Choice A is wrong because a score of 7 would mean that the newborn has one less point in one of the categories.For example, if the newborn had a heart rate of less than 100 beats per minute, that would be 1 point instead of 2 points for pulse.
Choice C is wrong because a score of 9 would mean that the newborn has perfect scores in all categories except appearance.Most babies have blue hands or feet immediately after birth, which gives them 1 point instead of 2 points for appearance.
Choice D is wrong because a score of 10 is very rare and would mean that the newborn has perfect scores in all categories.This is unlikely because most babies have blue hands or feet immediately after birth, which gives them 1 point instead of 2 points for appearance.
A nurse is teaching a group of expectant parents about the APGAR score.
Which of the following statements by one of the parents indicates an understanding of the teaching?
Explanation
“The APGAR score helps to identify any problems that require immediate attention.” The APGAR score is a test given to newborns soon after birth to assess their health and well-being.
It is based on five categories: appearance, pulse, grimace, activity, and respiration.
Each category is scored from 0 to 2 points, with a total score of 10 being the best.The test is usually done at one and five minutes after birth, and sometimes again at 10 minutes if the score is low.
Choice A is wrong because the APGAR score does not measure blood pressure, temperature, or pulse oximetry.These are separate tests that may be done on newborns if needed.
Choice B is wrong because the APGAR score is done before and after the delivery of the baby, not the placenta.The placenta is delivered after the baby and does not affect the baby’s health.
Choice D is wrong because the APGAR score is based on a scale of 0 to 10, not 0 to 5.A score of 7 or above is considered normal and reassuring, while a score of 4 to 6 is moderately abnormal and a score of 0 to 3 is concerning.
A nurse is reviewing the chart of a newborn who has an APGAR score of 2 at 1 minute after birth and an APGAR score of 6 at 5 minutes after birth.
Which of the following factors could have contributed to these scores? (Select all that apply.)
Explanation
The factors that could have contributed to these scores are A, D, and E. These are:
A. The mother received magnesium sulfate during labor.This statement is correct because magnesium sulfate can cause neonatal depression and lower the APGAR score.
D. The newborn had meconium-stained amniotic fluid.This statement is correct because meconium aspiration can cause respiratory distress and lower the APGAR score.
E. The mother had preeclampsia.This statement is correct because preeclampsia can cause placental insufficiency and fetal hypoxia, which can lower the APGAR score.
B. The newborn was delivered by cesarean section.This statement is wrong because cesarean delivery does not affect the APGAR score unless there are complications.
C. The mother had gestational diabetes mellitus.This statement is wrong because gestational diabetes mellitus does not affect the APGAR score unless it causes macrosomia or hypoglycemia in the newborn.
A nurse is preparing to assess the APGAR score of a newborn at 1 minute after birth.
Which of the following actions should the nurse take?
Explanation
The correct answer is choice B. Observe the respiratory effort by looking at the chest movements.This is one of the five categories that the Apgar score uses to assess the newborn’s condition at one and five minutes after birth.The other categories are activity/muscle tone, pulse/heart rate, grimace/response to stimulation, and appearance/color.Each category receives a score of 0 to 2 points, with a maximum total score of 10.
Choice A is wrong because counting the heart rate for a full minute using a stethoscope is not necessary.The pulse can be assessed by feeling the umbilical cord or placing a hand over the chest.
Choice C is wrong because assessing the muscle tone by placing the newborn in a prone position is not recommended.The muscle tone can be evaluated by observing how much the baby is moving around and how flexed their limbs are.
Choice D is wrong because evaluating the reflex irritability by flicking the sole of the foot is not the best way to stimulate the baby.The reflex irritability can be tested by suctioning the baby’s nose or rubbing their back.
The normal ranges for each category are as follows:
• Activity/muscle tone: 0 points for limp or floppy, 1 point for limbs flexed, 2 points for active movement
• Pulse/heart rate: 0 points for absent, 1 point for less than 100 beats per minute, 2 points for greater than 100 beats per minute
• Grimace/response to stimulation: 0 points for
New Ballard Scale
A nurse is using the New Ballard Scale to assess the gestational age of a newborn.
What does a higher score on the scale indicate?
Explanation
Maturity.A higher score on the New Ballard Scale indicates that the newborn is more mature based on physical and neuromuscular characteristics.The scale can be used to estimate the gestational age of a newborn infant when there is no reliable obstetrical information or a major discrepancy between the estimated date of delivery and the infant’s appearance.The scale is accurate only within plus or minus 2 weeks and can be used up to 4 days after birth, but usually within the first 24 hours.
Choice A is wrong because prematurity means that the newborn is born before the normal term of pregnancy, which is usually less than 37 weeks of gestation.Premature infants have lower scores on the New Ballard Scale because they have less developed physical and neuromuscular features.
Choice B is wrong because developmental delays mean that the newborn has not reached certain milestones of growth and development that are expected for their age.
Developmental delays are not directly related to the gestational age of a newborn and cannot be assessed by the New Ballard Scale.
Choice C is wrong because neurological immaturity means that the newborn has not developed sufficient brain function and nervous system activity that are necessary for survival and adaptation.
Neurological immaturity is not the same as neuromuscular maturity, which is one of the components of the New Ballard Scale.Neuromuscular maturity refers to the posture, tone, reflexes, and movements of the newborn’s muscles and joints.
A client asks the nurse about the purpose of the New Ballard Scale.
How should the nurse respond?
Explanation
It determines the gestational age and identifies developmental risks.TheNew Ballard Scaleis a scale that estimates the gestational age of a newborn infant based on physical and neuromuscular characteristics.The scale can be used when there is no reliable obstetrical information or a major discrepancy between the estimated date of delivery and the infant’s appearance.The scale is accurate only within plus or minus 2 weeks and can be used up to 4 days after birth, but usually within the first 24 hours.The scale has been refined and expanded to include extremely premature neonates.
Choice A is wrong because it assesses the newborn’s cognitive development.The New Ballard Scale does not measure cognitive development, but rather physical and neuromuscular maturity.
Choice B is wrong because it evaluates the baby’s physical strength and coordination.The New Ballard Scale does not measure strength and coordination, but rather physical characteristics such as skin, lanugo, plantar surface, breast, eye/ear, and genitals, and neuromuscular characteristics such as posture, square window, arm recoil, popliteal angle, scarf sign, and heel to ear.
Choice C is wrong because it measures the newborn’s respiratory maturity.The New Ballard Scale does not measure respiratory maturity, but rather gestational age based on physical and neuromuscular criteria.
A nurse is performing the neuromuscular maturity test on a newborn using the New Ballard Scale.
What does this test evaluate?
Explanation
The neuromuscular maturity test on a newborn using the New Ballard Scale evaluates the flexion in different positions.The test is a scale that estimates the gestational age of a newborn infant based on physical and neuromuscular characteristics.The test can be used when there is no reliable obstetrical information or a major discrepancy between the estimated date of delivery and the infant’s appearance.
Choice A is wrong because skin thickness and appearance are part of the physical maturity score, not the neuromuscular maturity score.
Choice B is wrong because presence of lanugo and breast buds are also part of the physical maturity score, not the neuromuscular maturity score.
Choice D is wrong because creases on the bottom of feet are another part of the physical maturity score, not the neuromuscular maturity score.
A client is concerned about the physical characteristics of their late pre-term newborn.
What might the nurse explain about their appearance?
Explanation
Thicker skin and absence of lanugo.Late preterm infants are born at a gestational age between 34 and 36 completed weeks of pregnancy.They have higher morbidity and mortality rates than term infants, but they also have some physical characteristics that distinguish them from very preterm or extremely preterm infants.
Choice B is wrong because leathery and cracked skin is a sign of postmaturity, not prematurity.
Choice C is wrong because underdeveloped breast buds and flat scrotum are signs of very preterm or extremely preterm infants, not late preterm infants.
Choice D is wrong because wrinkled and transparent skin are also signs of very preterm or extremely preterm infants, not late preterm infants.
Normal ranges for gestational age, weight, length and head circumference can be found in the table below:
|
Gestational age |
Weight |
Length |
Head circumference |
|
40 weeks |
3.4-3.6 kg |
51 cm |
35 cm |
|
35 weeks |
2.4-2.5 kg |
45-46 cm |
31.5-32 cm |
|
32 weeks |
1.7-1.8 kg |
42 cm |
29-29.5 cm |
|
28 weeks |
1.0-1.1 kg |
36-36.5 cm |
25-26 cm |
|
24 weeks |
0.6-0.65 kg |
31-32 cm |
21-22 cm |
A nurse is using the New Ballard Scale to assess a newborn and observes well-developed breast buds, creases on the bottom of feet, and no lanugo.
How would the nurse categorize the gestational age of this baby?
Explanation
According to the New Ballard Score, a newborn with well-developed breast buds, creases on the bottom of feet, and no lanugo has a total physical maturity score of 40, which corresponds to a gestational age of 40 weeks.
This is within the normal range of 37 to 42 weeks for a full-term baby.
Choice B. Pre-term is wrong because a pre-term baby has a gestational age of less than 37 weeks and would have immature physical characteristics such as sticky or transparent skin, no creases on the feet, and abundant lanugo.
Choice C. Late pre-term is wrong because a late pre-term baby has a gestational age of 34 to 36 weeks and would have less developed physical characteristics such as smooth pink skin, faint red marks on the feet, and thinning lanugo.
Choice D. Post-term is wrong because a post-term baby has a gestational age of more than 42 weeks and would have more advanced physical characteristics such as cracking or leathery skin, no lanugo, and pendulous testes or large labia majora.
Fontanelles
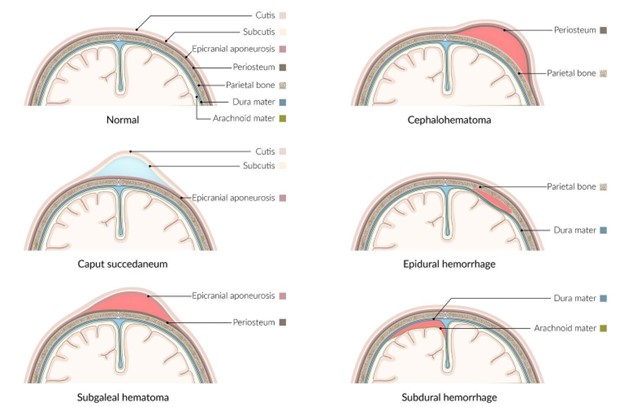
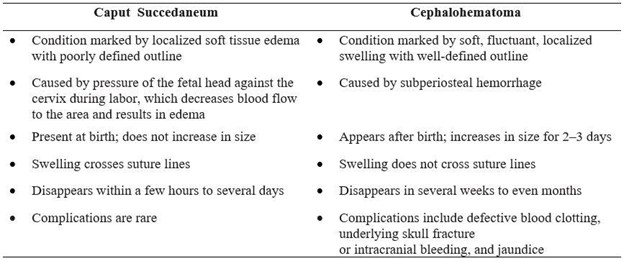
A nurse is assessing a newborn’s head and notices a swelling on the right parietal area.
The nurse suspects that this is a cephalohematoma.
What is the most likely cause of this condition?
Explanation
Birth trauma.A cephalohematoma is a collection of blood under the scalp of a newborn that forms a bulge.It is caused by rupture of blood vessels crossing the periosteum due to pressure or trauma on the fetal head during birth.This pressure or trauma may result from a prolonged second stage of labor, instrumental delivery, particularly forceps delivery, ventouse application, or the baby’s head squeezing through the birth canal.
Choice B is wrong because infection is not a cause of cephalohematoma, but a potential complication that may occur in some cases.
Choice C is wrong because dehydration is not a cause of cephalohematoma, but a possible consequence of anemia, which may result from blood loss.
Choice D is wrong because hemorrhage is not a cause of cephalohematoma, but a synonym for bleeding, which is what happens when the blood vessels rupture.
Normal ranges for newborn cephalohematoma are not applicable, as it is an abnormal condition that varies in size and severity.However, most cephalohematomas resolve on their own without intervention within weeks or months.
A nurse is teaching a new mother how to care for her infant’s fontanelles.
Which of the following statements by the mother indicates a need for further teaching?
Explanation
The mother should avoid touching the fontanelles because they are very sensitive.
This statement indicates a need for further teaching because it is a misconception.The fontanelles are not sensitive and can be gently touched and washed without causing any harm to the infant.
Choice A is correct because the fontanelles should be gently washed and dried when bathing the baby to prevent infection.
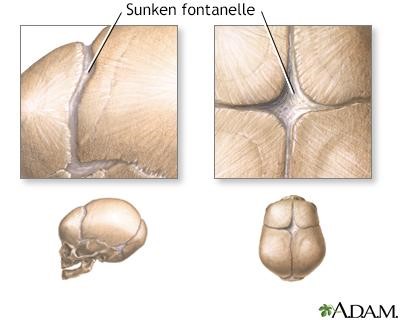
Choice B is correct because signs of bulging or sunken fontanelles can indicate increased or decreased intracranial pressure, which requires medical attention.
Choice D is correct because the fontanelles usually close by 18 months of age, but some variation is normal.
A nurse is measuring the head circumference of a 6-month-old infant.
The nurse notes that the anterior fontanel is 4 cm in size and the posterior fontanel is closed.
How should the nurse interpret these findings?
Explanation
The anterior fontanel is normal and the posterior fontanel is normal.
According to, the average size of the anterior fontanel is2.1 cm, and the median time of closure is13.8 months.The posterior fontanel generally closes2 to 3 monthsafter birth.
Therefore, a 6-month-old infant with an anterior fontanel of 4 cm and a closed posterior fontanel is within the normal range.
Choice A is wrong because the posterior fontanel is not delayed in closing.It usually closes by 3 months of age.
Choice C is wrong because the anterior fontanel is not enlarged.It can range from 0.6 cm to 3.6 cm with a mean of 2.1 cm.
Choice D is wrong because both the anterior and posterior fontanels are normal, not enlarged or delayed in closing.
Normal ranges for head circumference of a 6-month-old infant are39.59 to 44.34 cmfor girlsand40.89 to 45.34 cmfor boys, according to the CDC.
A nurse is examining a newborn’s head and observes a diffuse edema over the scalp that crosses the suture lines.
The nurse recognizes this as a caput succedaneum.
What should the nurse do next?
Explanation
Document the finding and monitor for resolution.Caput succedaneum is a harmless condition that causes swelling of the scalp due to pressure during delivery.It does not indicate any damage to the brain or the skull and usually resolves on its own within a few days.
Therefore, the nurse should document the finding and monitor for resolution.
Choice A is wrong because there is no need to notify the physician immediately.Caput succedaneum is not a medical emergency and does not require any intervention.
Choice C is wrong because applying ice packs to reduce swelling is not recommended.Ice packs can cause skin irritation, infection, or hypothermia in newborns.
Choice D is wrong because performing a neurological assessment is not necessary.Caput succedaneum does not affect the brain or the nervous system and does not cause any neurological symptoms.
A nurse is educating a group of parents about the functions of the fontanelles.
Which of the following statements by the nurse are correct? (Select all that apply.
Explanation
The fontanelles are soft spots on a baby’s head that have two main functions:
• They allow forrapid growth of the brainduring infancy
• They allow forpassage of the head through the birth canalby enabling the bony plates of the skull to flex
Choice A is wrong because the fontanelles do not allow for passage of blood from the scalp to the brain.The blood supply to the brain is provided by the internal carotid and vertebral arteries, which enter the skull through different openings
The fontanelles also allow forassessment of hydration statusandintracranial pressurein infants by palpating their size and shape.A sunken fontanelle may indicate dehydration, while a bulging fontanelle may indicate increased pressure within the skull
Eyes, Ears, and Oral Cavity
A nurse is assessing a newborn’s eyes.
The nurse should identify that which of the following is an expected finding?
Explanation
The newborn has a red reflex in both eyes.This is an expected finding that indicates the absence of cataracts or other eye abnormalities.The red reflex test is performed by using an ophthalmoscope to shine a light into the baby’s eyes and observing the reflection.
The newborn has blue or gray eyes at birth: This statement is wrong because eye color can vary at birth and may change over time.Eye color is determined by the amount and distribution of melanin in the iris.
The newborn has a nystagmus when looking to the side.This statement is wrong because nystagmus is an abnormal eye movement that can indicate a neurological problem or a visual impairment.
The newborn has a strabismus when focusing on an object.This statement is wrong because strabismus is a misalignment of the eyes that can cause amblyopia (lazy eye) or double vision.Strabismus may be present at birth or develop later in life.
A nurse is examining a newborn’s ears.
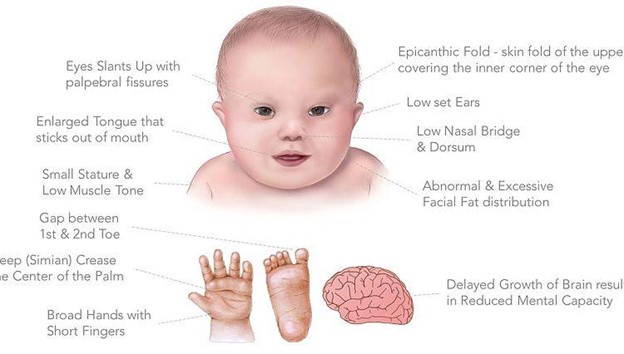
The nurse should identify that which of the following findings may indicate a chromosomal disorder?
Explanation
The newborn has low-set ears.
Low-set ears are ears that are positioned below the normal horizontal line drawn across both inner canthi of the eyes.Low-set ears may indicate a chromosomal disorder, such asDiGeorge syndromeorNoonan syndrome, or other congenital anomalies.
Choice B is wrong because small ear canals are not a sign of a chromosomal disorder, but rather a variation of normal anatomy.
Choice C is wrong because dry cerumen in the ears is not a sign of a chromosomal disorder, but rather a result of dehydration or lack of humidity.
Choice D is wrong because prominent antihelices are not a sign of a chromosomal disorder, but rather a normal feature of the external ear.
The antihelix is the curved prominence of cartilage parallel with and inside the helix (the rim) of the ear.
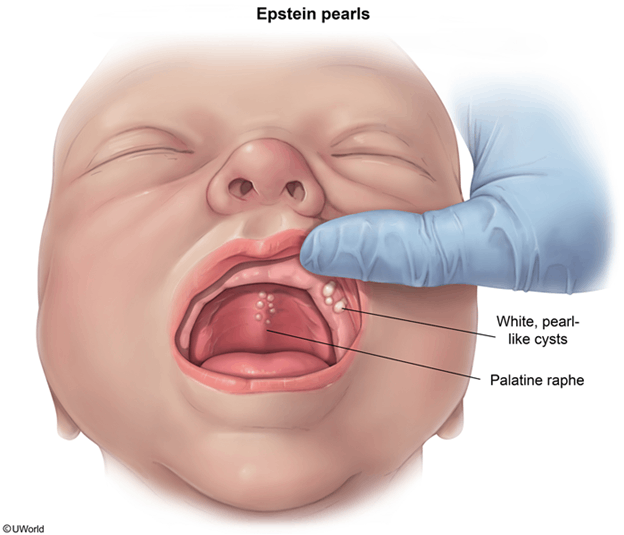
A nurse is inspecting a newborn’s oral cavity.
The nurse should identify that which of the following findings is a normal variation?
Explanation
Epstein’s pearls on the gums or palate are small, white cysts that are common and harmless in newborns.
They usually disappear within a few weeks without treatment.
Choice B is wrong because thrush on the tongue or gums is a fungal infection that causes white patches and soreness in the oral cavity.
It is not a normal variation and may require antifungal medication.
Choice C is wrong because petechiae on the hard palate are tiny red spots that indicate bleeding under the skin.
They are not a normal variation and may be caused by trauma, infection, or clotting disorders.
Choice D is wrong because yellowing of the hard palate is a sign of jaundice, which is a condition where the skin and mucous membranes turn yellow due to high levels of bilirubin in the blood.
It is not a normal variation and may indicate liver problems or hemolytic disease.
Normal ranges for oral cavity findings in newborns are:
• Gums: pink and moist, no inflammation or bleeding
• Teeth: none or natal teeth (present at birth), which may need to be removed if loose or interfering with feeding
• Tongue: pink and moist, no lesions or coating
A nurse is caring for a newborn who has thrush, an oral fungal infection.
Which of the following medications should the nurse expect to administer to treat this condition?
Explanation
Nystatin.Nystatin is an antifungal medicine that can be given as drops to treat oral thrush, a fungal infection in the mouth, in newborns.
Some possible explanations for the other choices are:
Acyclovir is an antiviral medicine that is used to treat infections caused by herpes viruses, such as cold sores or genital herpes.
It is not effective against fungal infections like thrush.
•Amoxicillin is an antibiotic medicine that is used to treat bacterial infections, such as ear infections or pneumonia.
It can actually increase the risk of developing thrush by killing the normal bacteria in the mouth that help prevent fungal overgrowth.
• Fluconazole is another antifungal medicine that can be used to treat thrush in some cases, especially in immunocompromised infants or when nystatin is not effective.
A nurse is teaching a new mother about how to care for her newborn’s eyes, ears, and oral cavity.
Which of the following instructions should the nurse include? (Select all that apply).
Explanation
The correct answer is choice A, D, and E.The nurse should instruct the mother to clean the newborn’s eyes with warm water and cotton balls from the inner to the outer canthus to prevent infection and remove any discharge.The nurse should also advise the mother to avoid using cotton-tipped applicators to clean the newborn’s ears because they can damage the eardrum or push cerumen deeper into the ear canal.Additionally, the nurse should tell the mother to report any signs of eye infection, such as redness, swelling, or discharge, to the provider as soon as possible.
Choice B is wrong because using a bulb syringe to suction any drainage from the newborn’s ears can cause trauma or infection
Normal Variations and Abnormal Findings
A nurse is assessing a newborn’s fontanelles.
Which of the following findings should the nurse report to the provider?
Explanation
The anterior fontanelle is bulging and tense when the newborn cries.This is an abnormal finding that should be reported to the provider as it may indicate increased intracranial pressure or intracranial and extracranial tumors.
Choice A is wrong because the anterior fontanelle is normally diamond-shaped and 2 cm wide.
Choice B is wrong because the posterior fontanelle is normally triangular and 0.5 cm wide.
Choice D is wrong because the posterior fontanelle normally closes by 8 weeksand may not be palpable at six weeks.
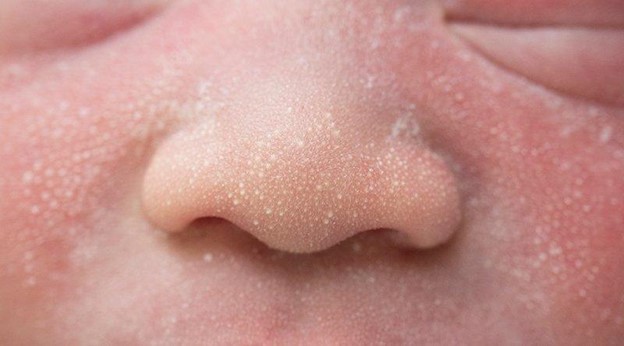
A nurse is teaching a new mother about normal variations in newborns.
Which of the following statements by the mother indicates an understanding of the teaching?
Explanation
Milia are caused by blocked sebaceous glands and will go away on their own.They are tiny, white bumps on a newborn’s nose, cheeks, chin and forehead.
Choice B is wrong because Mongolian spots are not a sign of bruising and should not be reported to the provider.They are blue or purple-colored splotches on the baby’s lower back and buttocks that are caused by a concentration of pigmented cells.They are more common in dark-skinned babies of all races and usually fade by age 5.
Choice C is wrong because head circumference should be about 2 cm larger than the chest circumference, not smaller.
A smaller head circumference may indicate a problem with brain development.
Choice D is wrong because fontanelles should be flat and soft to indicate adequate hydration.Sunken and firm fontanelles may indicate dehydration or increased intracranial pressure.Fontanelles are the soft spots on a baby’s head where the skull bones have not yet fused together.
A nurse is caring for a newborn who has a temperature of 36.1°C (97°F), heart rate of 140/min, respiratory rate of 50/min, muscle tone of 1, and reflex irritability of 1.
What is the newborn’s APGAR score at 1 minute?
Explanation
5. The APGAR score is a method of assessing the health of a newborn based on five criteria: appearance (skin color), pulse (heart rate), grimace (reflex irritability), activity (muscle tone), and respiration (breathing rate and effort).
Each criterion is scored from 0 to 2, with a total score ranging from 0 to 10.
A higher score indicates a better condition of the newborn.
The newborn in the question has a score of 1 for appearance (pale or blue extremities), 1 for pulse (heart rate below 160/min), 1 for grimace (minimal response to stimulation), 1 for activity (some flexion of extremities), and 1 for respiration (slow or irregular breathing).
The sum of these scores is 5.
Choice A is wrong because a score of 4 would mean that the newborn has a score of 0 for one of the criteria, which is not the case.
Choice C is wrong because a score of 6 would mean that the newborn has a score of 2 for one of the criteria, which is not the case.
Choice D is wrong because a score of 7 would mean that the newborn has a score of 2 for two of the criteria, which is not the case.
The normal ranges for each criterion are:
• Appearance: 0 (blue or pale all over), 1 (pink body but blue extremities), or 2 (pink all over).
• Pulse: 0 (absent), 1 (below 100/min), or 2 (above 100/min).
• Grimace: 0 (no response to stimulation), 1 (grimace or weak cry), or 2 (vigorous cry).
• Activity: 0 (limp or flaccid), 1 (some flexion of extremities), or 2 (active movement).
• Respiration: 0 (absent), 1 (slow or irregular), or 2 (good and regular).
A nurse is using the New Ballard Scale to assess the gestational age of a newborn.
Which of the following physical characteristics should the nurse evaluate? (Select all that apply.)
Explanation
The correct answer is choice A, B, C and E.The New Ballard Scale is a scale that estimates the gestational age of a newborn infant based on physical and neuromuscular characteristics.The physical characteristics include skin texture, lanugo, plantar surface, breast tissue, eye/ear and genitals.The neuromuscular characteristics include posture, square window, arm recoil, popliteal angle, scarf sign and heel to ear.
The nurse should evaluate all these characteristics and assign a score for each one.The total score determines the gestational maturity in weeks.
Choice D is wrong because hair pattern is not one of the physical characteristics used in the New Ballard Scale.
Hair pattern may vary depending on genetic factors and is not a reliable indicator of gestational age.
The normal ranges for each characteristic are given in the table below:
|
Characteristic |
Score |
-1 |
0 |
1 |
2 |
3 |
4 |
5 |
|
Posture |
Extended |
Flexed |
Full flexion |
|||||
|
Square window |
>90° |
90° |
60° |
45° |
||||
|
Arm recoil |
Extended |
Slight flex |
A nurse is examining the eyes of a newborn who was born at 38 weeks of gestation.
Which of the following findings should the nurse expect?
Explanation
Presence of subconjunctival haemorrhages.
Subconjunctival haemorrhages are small blood spots on the white part of the eye that is caused by pressure during delivery.They are harmless and usually disappear within a few weeks.
Choice A is wrong because the absence of a red reflex is a sign of a serious eye problem, such as a cataract or retinoblastoma.
The red reflex test is done by shining a light into the baby’s eyes and looking for a red reflection from the retina.It is part of the newborn physical screening examination.
Choice C is wrong because the inability to track objects is not expected in a newborn.Babies can usually follow objects with their eyes by 2 to 3 months of age.
Choice D is wrong because unequal pupil sizes can indicate a neurological problem or an eye injury.Pupil sizes should be checked and measured during the newborn physical examination.
Nursing Interventions in Newborn Assessment
A nurse is preparing to perform a newborn assessment.
What is the first step that the nurse should take?
Explanation
C. Perform hand hygiene or use an alcohol-based hand sanitizer.
This is the first step that the nurse should take before performing a newborn assessment to prevent the transmission of infection.According to the CDC, hand hygiene is the most important measure to prevent healthcare-associated infections.
Choice A is wrong because informed consent from the parents or guardians is not required for a routine newborn assessment.Consent is implied when the parents bring the newborn to the health care facility.
Choice B is wrong because positioning the newborn in a supine position on a flat surface is not the first step, but rather the second step after performing hand hygiene.The supine position allows for a complete head-to-toe examination of the newborn.
Choice D is wrong because administering prophylactic medications to the newborn is not part of the newborn assessment, but rather a separate intervention that requires a physician’s order and informed consent from the parents or guardians.
Prophylactic medications may include vitamin K injection, eye ointment, and hepatitis B vaccine.
A nurse is assessing a newborn’s vital signs.
What is the normal range for a newborn’s heart rate?
Explanation
The normal range for a newborn’s heart rate is 120 to 160 beats per minute.
This reflects the high metabolic rate and oxygen consumption of the newborn.
Choice A is wrong because 60 to 80 beats per minute is too low for a newborn and may indicate bradycardia, which can be caused by hypoxia, hypothermia, or heart block.
Choice B is wrong because 80 to 100 beats per minute is also below the normal range for a newborn and may indicate poor perfusion or cardiac dysfunction.
Choice C is wrong because 100 to 120 beats per minute is at the lower end of the normal range for a newborn and may indicate hypothermia, dehydration, or sepsis.
A nurse is auscultating a newborn’s lung sounds.
What type of breath sounds should the nurse expect to hear in a healthy newborn?
Explanation
Vesicular breath sounds are soft and low-pitched and are heard over most of the lung fields.
They indicate normal air movement in and out of the alveoli.
Bronchial breath sounds are loud and high-pitched and are heard over the trachea and larynx.
They indicate increased airway resistance or consolidation.
Bronchovesicular breath sounds are medium-pitched and are heard over the main bronchi.
They indicate partial obstruction of the airways or atelectasis.
Adventitious breath sounds are abnormal sounds such as crackles, wheezes, rhonchi, or stridor.
They indicate various lung disorders such as pneumonia, asthma, bronchitis, or foreign body aspiration.
Choice B is wrong because bronchial breath sounds are not normal in a healthy newborn and indicate a lung problem.
Choice C is wrong because bronchovesicular breath sounds are not normal in a healthy newborn and indicate a lung problem.
Choice D is wrong because adventitious breath sounds are not normal in a healthy newborn and indicate a lung problem.
A nurse is evaluating a newborn’s feeding and elimination patterns.
How many wet diapers should a newborn have per day by the fourth day of life?
Explanation
A newborn should have at least six wet diapers per day by the fourth day of life. This indicates that the baby is well hydrated and getting enough milk.
Choice A is wrong because one wet diaper per day is too low and could mean that the baby is dehydrated or not feeding well.
Choice B is wrong because three wet diapers per day is also too low and could indicate insufficient milk intake or dehydration.
Choice D is wrong because nine wet diapers per day is more than the average range and could indicate that the baby is overfed or has a urinary tract infection.
More questions
A nurse is assessing a newborn at birth using Apgar scoring system and notes that he has no respiratory effort, no heart rate, no muscle tone, no reflex irritability, and is blue all over his body.
What Apgar score would you give this patient?
Explanation
The Apgar score is a scoring system that assesses the condition of the newborn at one and five minutes after birth based on five parameters: activity, pulse, grimace, appearance, and respiration.Each parameter is given a score of 0, 1, or 2, with a maximum total score of 10.A score of 7 to 10 is considered normal, a score of 4 to 6 is moderately abnormal, and a score of 0 to 3 is severely abnormal.
In this case, the newborn has no respiratory effort, no heart rate, no muscle tone, no reflex irritability, and is blue all over his body.
Therefore, he would receive a score of 0 for each parameter, resulting in a total Apgar score of 0.
Choice B is wrong because a score of 1 means that the newborn has at least one parameter with a score of 1.For example, if the newborn has a heart rate of less than 100 beats per minute but no other signs of life, he would receive a score of 1 for pulse and 0 for the rest, resulting in a total Apgar score of 1.
Choice C is wrong because a score of 2 means that the newborn has at least one parameter with a score of 2 or two parameters with a score of 1.
For example, if the newborn has a heart rate of more than 100 beats per minute and some
A nurse is caring for a newborn who has an Apgar score of 8 at one minute after birth and an Apgar score of 10 at five minutes after birth.
Which statement best describes this newborn’s condition?
Explanation
The newborn had some problems at birth but is now in excellent condition.
The Apgar score is a method of assessing the health of a newborn on a scale of 0 to 10 based on five criteria: appearance, pulse, grimace, activity, and respiration.
A score of 7 to 10 indicates that the newborn is in good condition and does not need any special care.
A score of 4 to 6 indicates that the newborn has some problems and may need some assistance.
A score of 0 to 3 indicates that the newborn is in serious trouble and needs immediate medical attention.
Choice A is wrong because a score of 8 at one minute after birth does not indicate a difficult transition.
It means that the newborn had only minor problems and was in good condition.
Choice B is wrong because a score of 10 at five minutes after birth does not indicate an improvement from a score of 8.
It means that the newborn had no problems and was in excellent condition.
Choice D is wrong because a score of 10 at five minutes after birth does not indicate a deterioration from a score of 8.
It means that the newborn had no problems and was in excellent condition.
Normal ranges for the Apgar score are:
• At one minute after birth: 7 to 10
• At five minutes after birth: 8 to 10
A nurse is teaching a class on Apgar scoring to nursing students. Which statement by a student indicates a need for further teaching
Explanation
This is wrong because acrocyanosis means that the body is pink but the extremities are blue, which indicates poor circulation.A normal Apgar score for color is two points, which means that the baby is pink all over.
Choice A is correct because a heart rate below 100 beats per minute is considered moderately abnormal and receives one point.
Choice C is correct because active motion of extremities indicates good muscle tone and receives two points.
Choice D is correct because a vigorous cry when stimulated indicates good reflex irritability and receives two points.
A nurse is assessing a newborn's gestational age using the New Ballard Scale.
Which of the following signs would indicate prematurity?
Explanation
Thin and transparent skin is a sign of prematurity in newborns.The New Ballard Scale is a scale that estimates the gestational age of a newborn infant based on physical and neuromuscular characteristics.
The other choices are signs of maturity or postmaturity in newborns:
• Choice B: Well-developed breastbuds indicate a gestational age of 38 to 44 weeks.
• Choice C: Creases on the bottom of feet indicate a gestational age of 32 to 44 weeks.
• Choice D: Developed labia indicate a gestational age of 40 to 44 weeks.
The normal range for gestational age is 37 to 42 weeks.Premature infants are those born before 37 weeks, and postmature infants are those born after 42 weeks.
A client asks the nurse about the purpose of the New Ballard Scale.
How should the nurse respond?
Explanation
It helps identify potential developmental delays.The New Ballard Scale is a scale that estimates the gestational age of a newborn infant based on physical and neuromuscular characteristics.The scale can be used when there is no reliable obstetrical information or a major discrepancy between the estimated date of delivery and the infant’s appearance.The scale is accurate only within plus or minus 2 weeks and can be used up to 4 days after birth, but usually within the first 24 hours.The scale has been refined and expanded to include extremely premature neonates.
Choice A is wrong because the New Ballard Scale does not determine the newborn’s nutritional needs.It only assesses the gestational maturity of the newborn based on physical and neuromuscular signs.
Choice B is wrong because the New Ballard Scale does not assess the baby’s cognitive development.It only estimates the gestational age of the newborn, which is the primary determinant of organ maturity.
Choice D is wrong because the New Ballard Scale does not measure the newborn’s respiratory function.It only evaluates the physical and neuromuscular characteristics of the newborn, such as skin texture, lanugo, plantar surface, breast tissue, eye/ear development and genitalia.
A nurse is performing the physical maturity test on a newborn using the New Ballard Scale.
What characteristic would the nurse assess?
Explanation
Flexion in different positions.The New Ballard Scale is a scale that estimates the gestational age of a newborn infant based on physical and neuromuscular characteristics.Flexion in different positions is one of the six neuromuscular signs that are assessed using the scale.The other neuromuscular signs are square window, arm recoil, popliteal angle, scarf sign, and heel to ear.
The other statements are wrong because:
Skin thickness and presence of lanugo are physical signs, not neuromuscular signs.They are also assessed using the New Ballard Scale, along with plantar surface, breast, eye/ear, and genitals.
Creases on the bottom of feet are part of the plantar surface assessment, which is a physical sign, not a neuromuscular sign.
Scrotum development is part of the genital assessment, which is a physical sign, not a neuromuscular sign.
The New Ballard Scale can be used up to 4 days after birth, but usually within the first 24 hours.The scale is accurate only within plus or minus 2 weeks.The total score determines the gestational maturity in weeks.
A nurse palpates an infant’s anterior fontanelle and notes that it feels soft and flat when lying down, but slightly elevated when sitting up or crying.
What should be included in documentation?
Explanation
Normal finding.
The anterior fontanelle is the soft spot on the top of an infant’s head that allows for brain growth and skull expansion.
It normally feels soft and flat when the infant is lying down, and may bulge slightly when the infant is sitting up or crying due to increased blood flow and pressure.
This is not a sign of any problem and should be documented as a normal finding.
Dehydration is wrong because dehydration would cause the fontanelle to feel sunken or depressed, not elevated. Dehydration can also cause other signs such as dry mouth, decreased urine output, and lethargy.
Increased intracranial pressure is wrong because increased intracranial pressure would cause the fontanelle to feel tense or bulging at all times, not only when sitting up or crying. Increased intracranial pressure can also cause other signs such as vomiting, irritability, seizures, and altered level of consciousness.
Infection is wrong because infection would cause the fontanelle to feel warm or tender, not elevated. Infection can also cause other signs such as fever, rash, poor feeding, and fussiness.
A nurse observes that an infant has an elongated head shape due to molding during delivery.
The nurse explains to the parents that this condition is called:
Explanation
Plagiocephaly.
This condition is also known as flat head syndrome and it occurs when an infant’s head shape becomes flattened due to external pressure.It can be caused by molding during delivery or by sleeping in the same position for a long time.
Choice A is wrong because caput succedaneum is a swelling of the scalp that results from pressure on the baby’s head during childbirth.It does not affect the shape of the head, but only causes temporary puffiness and bruising.
Choice B is wrong because cephalohematoma is bleeding under the scalp that occurs when blood vessels are damaged during delivery.It causes a firm lump on one side of the head that does not cross the suture lines.
Choice C is wrong because craniosynostosis is a condition where one or more of the sutures (joints) between the skull bones close prematurely, preventing normal growth of the head.It can cause an abnormal head shape, but it is not related to molding during delivery.
A nurse is caring for an infant who has a cephalohematoma on the left side of his skull.
Which of the following interventions should the nurse implement?
Explanation
Monitor for signs of jaundice.A cephalohematoma is a collection of blood under the scalp that occurs due to trauma or pressure during delivery.It may increase the risk of jaundice in the newborn due to the breakdown of red blood cells and the release of bilirubin.Jaundice is a condition that causes yellowing of the skin and eyes due to high levels of bilirubin in the blood.Monitoring for signs of jaundice is important to prevent complications such as brain damage or kernicterus.
Apply pressure dressing over the area.This is wrong because applying pressure may increase the bleeding and cause more damage to the scalp and skull.A cephalohematoma does not require any treatment and usually resolves on its own within weeks or months.
Administer antibiotics as prescribed.This is wrong because antibiotics are not indicated for a cephalohematoma unless there is evidence of infection.Infection is a rare complication that may lead to osteomyelitis or meningitis.Antibiotics should be used only if prescribed by a doctor based on clinical signs and laboratory tests.
Elevate the head of the bed.This is wrong because elevating the head of the bed may not have any effect on a cephalohematoma.It may also cause discomfort or compromise the airway of the newborn.The position of the baby should be adjusted according to their comfort and safety.
A nurse is assessing an older adult client’s mouth.
The nurse should identify that which of the following is an expected variation for this client?
Explanation
Darkening of the mucosa.This is an expected variation for an older adult client because the melanin production increases with age.
Some possible explanations for the other choices are:
• Choice A.White patches on the tongue could indicate candidiasis, an oral fungal infection.
• Choice B.Bleeding of the gums could indicate gingivitis, periodontitis, or vitamin C deficiency.
• Choice C.Red spots on the hard palate could indicate petechiae, which are small hemorrhages caused by trauma, infection, or bleeding disorders.
Normal ranges for oral mucosa color vary depending on the skin tone and ethnicity of the client.Generally, the oral mucosa should be pink and moist without lesions or discolorations.
A nurse is preparing to assess a client’s conjunctiva.
Identify the sequence the nurse should follow when taking the following actions.
1) Apply examination gloves.
2) Instruct the client to look up.
3) Place the thumbs below each of the client’s lower eyelids.
4) Gently pull the client’s skin down to the top edge of the bony orbital rim.
5) Inspect the color and condition of the conductive and sclera, noting any color change, swelling, drainage, or lesions.
Explanation
The nurse should follow the sequence of 1, 2, 3, 4, 5 when assessing the client’s conjunctiva.This is because the nurse should first apply examination gloves to prevent contamination and infection.Then, the nurse should instruct the client to look up to expose the lower eyelid and conjunctiva.Next, the nurse should place the thumbs below each of the client’s lower eyelids and gently pull the skin down to the top edge of the bony orbital rim.This allows the nurse to inspect the color and condition of the conjunctiva and sclera, noting any color change, swelling, drainage, or lesions.The sclera should be white and the conjunctiva should be pink.
Choice B is wrong because the nurse should not pull down the skin before instructing the client to look up.
This could cause discomfort and injury to the eye.
Choice C is wrong because the nurse should not instruct the client to look up after pulling down the skin.
This could also cause discomfort and injury to the eye.
Choice D is wrong because the nurse should not place the thumbs below each of the client’s lower eyelids before applying examination gloves.
This could introduce infection and irritants to the eye.
A nurse is caring for a client who reports that he has a headache and vertigo after turning on his furnace for the first time this season.
The nurse suspect which of the following?
Explanation
Carbon monoxide poisoning.
This is because the client reports having a headache and vertigo after turning on his furnace for the first time this season.These are common symptoms of carbon monoxide poisoning, which can occur when carbon monoxide, a colorless and odorless gas, builds up in the blood due to exposure to combustion fumes.
The furnace may have been a source of carbon monoxide if it was not well vented or maintained.
The other statements are wrong because:
Meniere’s disease is a disorder of the inner ear that causes vertigo, hearing loss, tinnitus and ear fullness. It is not related to carbon monoxide exposure or furnace use.
Migraine is a type of headache that causes throbbing pain, nausea, sensitivity to light and sound, and sometimes visual disturbances. It is not caused by carbon monoxide exposure or furnace use, but by genetic and environmental factors.
Benign paroxysmal positional vertigo (BPPV) is a condition that causes brief episodes of vertigo triggered by changes in head position. It is caused by tiny crystals in the inner ear that become dislodged and stimulate the balance sensors. It is not related to carbon monoxide exposure or furnace use.
A nurse is preparing to administer erythromycin ointment to a newborn’s eyes as prophylaxis for gonorrhea and chlamydia infections.
Which of the following actions should the nurse take?
Explanation
Apply a thin ribbon of ointment along the inner canthus of each eye.This is the recommended method for administering erythromycin ointment to a newborn’s eyes as prophylaxis for gonorrhea and chlamydia infections.The ointment should be applied into the conjunctival sac to avoid accidental injury to the eye.
ChoiceBis wrong because the eyes should not be wiped off after applying the ointment.The ointment will gradually dissolve and disperse over the eye surface.
ChoiceCis wrong because the medication is an ointment, not a drop.
A drop would not provide adequate coverage of the eye and would be more likely to cause irritation
A nurse is caring for a newborn who has hyperbilirubinemia and is receiving phototherapy.
Which of the following interventions should the nurse implement?
Explanation
Cover the newborn’s eyes with eye shields or patches.This is because phototherapy can cause eye damage and irritation to the newborn, so the eyes should be protected while the lights are on.
Some possible explanations for the other choices are:
• Choice A is wrong because applying sunscreen to the newborn’s skin before placing under the lights can interfere with the effectiveness of phototherapy and increase the risk of skin irritation and infection.
• Choice C is wrong because turning off the phototherapy lights during feedings can reduce the exposure time and delay the clearance of bilirubin from the newborn’s blood.
• Choice D is wrong because keeping the newborn fully clothed to prevent heat loss can also interfere with the effectiveness of phototherapy and increase the risk of overheating and dehydration.
Normal ranges for bilirubin levels in newborns vary depending on the age, gestational age, and risk factors of the newborn.Generally, a total serum bilirubin level of less than 12 mg/dL (205 micromol/L) is considered normal for term newborns in the first week of life.Phototherapy is usually indicated when the total serum bilirubin level exceeds 15 mg/dL (257 micromol/L) for term newborns or 10 mg/dL (171 micromol/L) for preterm newborns.
A nurse is reviewing laboratory results for a newborn who was born to a mother who has type O positive blood and tested negative for hepatitis B surface antigen (HBsAg).
The newborn has type A positive blood and tested positive for Coombs antibody (anti-A).
Which of the following actions should the nurse take?
Explanation
Monitor the newborn for signs of jaundice and anemia.
This is because the newborn has a positive Coombs test, which means that there are antibodies against the newborn’s red blood cells (RBCs) in the blood.
These antibodies can cause hemolysis (destruction) of the RBCs, leading to jaundice (yellowing of the skin and eyes due to high bilirubin levels) and anemia (low RBC count and hemoglobin levels).The most likely cause of the positive Coombs test in this case is ABO incompatibility, which occurs when the mother has type O blood and the newborn has type A or B blood.
Choice A is wrong because administering hepatitis B immune globulin (HBIG) to the newborn within 12 hours of birth is indicated for newborns whose mothers are positive for hepatitis B surface antigen (HBsAg), which is not the case here.
Choice C is wrong because obtaining a blood sample from the newborn for blood typing and crossmatching is not necessary, as the newborn’s blood type is already known to be A positive.
Choice D is wrong because preparing the newborn for exchange transfusion with type O negative blood is a treatment option for severe cases of hemolytic disease of the newborn (HDN), which is not evident in this scenario.Exchange transfusion involves replacing the newborn’s blood with donor blood to remove antibodies and bilirubin.
A nurse is performing a head-to-toe assessment of a newborn.
What finding should alert the nurse to a potential problem with the newborn’s fontanelles?
Explanation
Bulging fontanelles.Bulging fontanelles can be a sign of increased intracranial pressure or intracranial and extracranial tumors.This is a potential problem for the newborn’s brain and health and should be evaluated by imaging studies.
Choice A is wrong because sunken fontanelles are usually a sign of dehydration, which is not a problem with the fontanelles themselves, but with the fluid balance of the newborn.
Choice C is wrong because a diamond-shaped anterior fontanelle is normal for a newborn.The anterior fontanelle is the largest and most important for clinical evaluation.It has an average size of 2.1 cm and a median time of closure of 13.8 months.
Choice D is wrong because a triangular posterior fontanelle is also normal for a newborn.The posterior fontanelle is smaller than the anterior one and normally closes by 8 weeks.
A nurse is supporting bonding and attachment between parents and their newborn.
What intervention should the nurse implement to promote skin-to-skin contact?
Explanation
Place the newborn on the mother’s chest after delivery.This is because skin-to-skin contact between mother and baby promotes bonding and attachment, which are essential for the baby’s emotional and psychological development.Skin-to-skin contact also helps regulate the baby’s body temperature, heart rate, breathing and blood sugar levels.
Choice B is wrong because wrapping the newborn in a blanket reduces the skin-to-skin contact and may interfere with the bonding process.The father can also bond with the baby by holding him or her against his own skin.
Choice C is wrong because placing the newborn in an isolette separates the baby from the mother and prevents close interaction and communication.The baby may feel insecure and isolated in an isolette.
Choice D is wrong because dressing the newborn in a gown and hat also reduces the skin-to-skin contact and may delay the initiation of breastfeeding.The baby may also lose more heat through clothing than through direct contact with the mother’s body.
Select all that apply.
A nurse is providing comfort measures to a newborn during an assessment.
What non-pharmacological interventions can the nurse use to soothe the newborn?
Explanation
Swaddling, pacifiers, gentle touch and music therapy are all non-pharmacological interventions that can help soothe a newborn during an assessment.
These methods can provide comfort, security, distraction and stimulation for the newborn.
Choice D is wrong because glucose water is a pharmacological intervention that can be used to reduce pain during procedures such as heel sticks or circumcision.Glucose water should not be given routinely to newborns as it can interfere with breastfeeding and cause electrolyte imbalances.
: PN maternal newborn practice B Flashcards | Quizlet: Maternal Newborn Alternate Item Format Quiz Flashcards | Quizlet: NCLEX-maternity and newborn Flashcards | Quizlet
Exams on Newborn Assessment
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Conclusion
A thorough newborn assessment encompasses various aspects, including the APGAR score, the New Ballard Scale, fontanelles, eyes, ears, and oral cavity findings. Understanding normal variations and distinguishing them from abnormal findings is crucial for identifying potential health issues in newborns. By following a systematic approach and paying attention to detail, healthcare professionals can provide appropriate interventions and ensure the well-being of newborns.
Objectives
-
Understand the significance of the APGAR score in assessing a newborn's immediate condition.
-
Familiarize with the New Ballard Scale and its use in evaluating neuromuscular and physical maturity.
-
Recognize normal variations in newborn appearance and distinguish them from abnormal findings.
-
Identify and interpret fontanelle abnormalities.
-
Describe normal findings and potential abnormalities in the eyes, ears, and oral cavity of a newborn.
-
Understand the importance of recognizing and addressing abnormal findings during a newborn assessment.
Introduction
A comprehensive newborn assessment is essential to evaluate the baby's overall health and identify any potential issues that require immediate attention. This set of nursing notes will cover key aspects of a newborn assessment, including the APGAR score, the New Ballard Scale, normal variations in appearance, fontanelle abnormalities, eye and ear assessment, and oral cavity findings.
APGAR Score (0-10)
- The APGAR score is a quick assessment tool performed at 1 and 5 minutes after birth to evaluate the newborn's transition to extrauterine life.
- Scores range from 0 to 10, with higher scores indicating better overall condition.
- Components of the APGAR score include heart rate (HR), respiratory rate (RR), muscle tone, reflex irritability, and color.
- HR > 100 bpm receives 2 points, HR < 100 bpm receives 1 point.
- RR with a good cry receives 2 points, no cry receives 0 points.
- Well-flexed muscle tone receives 2 points, flaccid tone receives 0 points.
- Crying indicates 2 points for reflex irritability, silence receives 0 points, and grimacing receives 1 point.
Pink color receives 2 points, pink body with cyanotic hands/feet (acrocyanosis) receives 1 point, and overall blue/pale color receives 0 points.
|
Category |
Description |
Score |
|
Color |
Skin color |
0 = blue, pale; 1 = pink body, blue hands and feet; 2 = completely pink |
|
Heart rate |
Heart rate |
0 = <100 beats per minute; 1 = 100-140 beats per minute; 2 = >140 beats per minute |
|
Respiration |
Respiratory effort |
0 = no respirations; 1 = gasping respirations; 2 = crying lustily |
|
Muscle tone |
Muscle tone |
0 = limp; 1 = some flexion of extremities; 2 = active motion of extremities |
|
Reflex irritability |
Response to stimulation |
0 = no response; 1 = grimace; 2 = vigorous cry |
- A score of 7-10 indicates good condition, 4-6 indicates moderate distress, and less than 4 indicates severe distress.
New Ballard Scale
-
The New Ballard Scale is a tool used to assess the gestational age of a newborn. It is based on physical and neurological signs of maturity. The scale ranges from 0 to 50, with a higher score indicating a more mature baby. The New Ballard Scale is used to help determine the need for medical intervention and to identify babies who may be at risk for developmental delays.
-
The New Ballard Scale is used to assess neuromuscular and physical maturity in newborns.
-
The neuromuscular maturity test evaluates the baby's level of flexion in different positions, including square window, arm recoil, scarf sign, popliteal angle, and heel-to-ear test.
-
The physical maturity test assesses various characteristics such as skin thickness, presence of lanugo (fine hair), creases on the bottom of feet, breast buds, scrotum development, and labia appearance.
-
Pre-term newborns exhibit thinner, more transparent skin, lanugo present, absence of creases on the bottom of feet, underdeveloped breast buds, flat scrotum, and prominent clitoris.
-
Full-term newborns have thicker skin, no lanugo, well-developed breast buds (5-10mm width), pendulum scrotum, developed labia, and creases on the bottom of feet.
-
Late pre-term newborns may have a wrinkled, cracked, leathery appearance.
-
Abnormal findings may indicate gestational age discrepancies or potential issues requiring further assessment.
Fontanelles
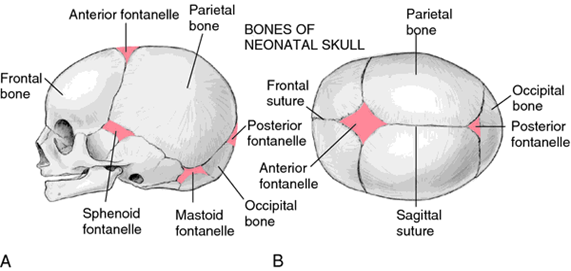
- The anterior fontanel is diamond-shaped and approximately 5cm in size.
- The posterior fontanel is triangular-shaped and smaller than the anterior fontanel.
- Bulging fontanelles may indicate hemorrhage or infection and require immediate medical attention.

- Sunken fontanelles suggest dehydration and necessitate appropriate intervention.
- Caput succedaneum refers to an elongated head shape due to passage through the birth canal and typically resolves within 3-4 days.
- Cephalohematoma refers to swelling or collection of blood in a specific area of the skull and should resolve within 2-3 weeks.
Eyes, Ears, and Oral Cavity
- Newborns typically have blue or gray eyes at birth, with the true eye color established within 3-12 months.
- Ears that are set lower than usual may indicate chromosomal disorders such as Down syndrome.
- Epstein's pearls are small, white cysts found on the gums or at the junction of the soft and hard palate, which are normal findings.
- Grey or white patches on the tongue or gums may indicate thrush, a fungal infection that requires treatment.
Normal Variations and Abnormal Findings
- Milia are small, raised white spots commonly found on the nose and chin of newborns, which typically resolve without treatment.
- Mongolian spots are bluish or purple spots that may appear on the back or bottom of newborns, representing normal variations.

- Head circumference should be approximately 2-3 cm larger than the chest circumference in a healthy newborn.
- It is important to recognize what is considered normal in a newborn to differentiate it from abnormal findings.
Nursing Interventions in Newborn Assessment
- Prepare the environment: Ensure a warm, quiet, and dimly lit room to promote a calm and comfortable environment for the newborn. Maintain a safe and sterile area for the assessment.
- Obtain informed consent: Explain the purpose and process of the newborn assessment to the parents or guardians. Obtain their consent before initiating any procedures.
- Perform hand hygiene: Wash hands thoroughly or use an alcohol-based hand sanitizer to prevent the transmission of pathogens.
- Positioning: Place the newborn in a supine position on a flat, padded surface, ensuring proper support for the head and neck.
- Maintain thermal regulation: Ensure a warm environment by using a radiant warmer or placing the newborn under a pre-warmed radiant heat source during the assessment. Use blankets or warmers to prevent heat loss.
- Assess vital signs: Measure the newborn's temperature, heart rate, respiratory rate, and blood pressure according to the facility's protocol. Document the findings and report any abnormalities promptly.
- Assess color and oxygenation: Observe the newborn's skin color, noting any signs of cyanosis, pallor, or jaundice. Assess oxygen saturation levels using a pulse oximeter if indicated.
- Auscultate lung sounds: Use a stethoscope to listen to the newborn's breath sounds in all lung fields. Report any abnormal findings, such as crackles or diminished breath sounds, to the healthcare provider.
- Evaluate feeding and elimination: Assess the newborn's ability to latch onto the breast or bottle and swallow effectively. Monitor the frequency and characteristics of urine and stool output, ensuring adequate hydration and nutrition.
- Perform a thorough head-to-toe assessment: Systematically assess the newborn's head, fontanelles, face, eyes, ears, nose, mouth, neck, chest, abdomen, genitalia, extremities, and skin. Document any abnormal findings and communicate them to the healthcare team.
- Support bonding and attachment: Encourage parents to participate in the assessment, promoting skin-to-skin contact and initiating breastfeeding if desired. Provide emotional support and education to facilitate parent-infant bonding.
- Provide comfort measures: Use non-pharmacological interventions such as swaddling, pacifiers, or gentle touch to soothe the newborn during the assessment.
- Administer prophylactic medications: Follow institutional protocols for administering vitamin K and erythromycin eye ointment to prevent hemorrhagic disorders and eye infections, respectively.
- Educate parents: Explain the purpose and significance of the newborn assessment findings. Provide guidance on normal newborn behaviors, feeding cues, safe sleep practices, and newborn care at home.
- Document findings: Record all assessment findings accurately and comprehensively, including measurements, observations, and any deviations from the normal range. Use standardized documentation tools and follow institutional policies.
Summary
- The APGAR score assesses the newborn's condition based on HR, RR, muscle tone, reflex irritability, and color.
- The New Ballard Scale evaluates neuromuscular and physical maturity.
- Fontanelles include the anterior and posterior fontanelles, with bulging indicating potential issues.
- Normal variations include caput succedaneum, cephalohematoma, eye color development, ear placement, Epstein's pearls, milia, and Mongolian spots.
- Abnormal findings may indicate abnormalities or potential health issues.
- Recognition of normal and abnormal findings is essential in a newborn assessment.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Newborn Assessment
This filled cannot be empty

