Please set your exam date
Pathophysiology of the Nervous System
Study Questions
Introduction
Explanation
Choice A reason:
This is a correct statement. The central nervous system (CNS) is responsible for processing sensory information, generating motor commands, and regulating cognitive and emotional functions.
Choice B reason:
This is an incorrect statement. The peripheral nervous system (PNS) consists of the cranial nerves, spinal nerves, and ganglia that connect the CNS to the rest of the body.
Choice C reason:
This is a correct statement. The autonomic nervous system (ANS) regulates involuntary functions of smooth muscles, cardiac muscles, and glands. It has two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS).
Choice D reason:
This is a correct statement. The sympathetic nervous system (SNS) prepares the body for stress or emergency situations by increasing heart rate, blood pressure, respiratory rate, and blood glucose levels. It also dilates the pupils, bronchi, and blood vessels to skeletal muscles.
Explanation
Choice A reason:
This is a correct answer. A spinal cord injury at the level of T6 affects the sensory nerves that innervate the lower half of the body, resulting in loss of sensation below the waist.
Choice B reason:
This is a correct answer. A spinal cord injury at the level of T6 affects the motor nerves that innervate the lower half of the body, resulting in paralysis of the lower extremities.
Choice C reason:
This is a correct answer. A spinal cord injury at the level of T6 affects the autonomic nerves that innervate the bladder and bowel, resulting in impaired bladder and bowel control.
Choice D reason:
This is an incorrect answer. A spinal cord injury at the level of T6 does not affect the cranial nerves that innervate the pharynx and esophagus, which are responsible for swallowing.
Choice E reason:
This is a correct answer. A spinal cord injury at the level of T6 affects the autonomic nerves that innervate the sweat glands and thermoregulatory centers, resulting in decreased sweating and shivering.
Explanation
Choice A reason:
This is an incorrect answer. The nurse should not give information that might overwhelm or distress the client without assessing their readiness to learn.
Choice B reason:
This is an incorrect answer. The nurse should not give false reassurance or minimize the client's condition.
Choice C reason:
This is an incorrect answer. The nurse should not ask questions that might confuse or frustrate the client who has memory impairment.
Choice D reason:
This is a correct answer. The nurse should use therapeutic communication techniques such as exploring feelings, reflecting, and active listening to provide emotional support and establish rapport with the client.
Explanation
Choice A reason:
This is a correct answer. Glia cells are supportive cells that provide insulation, protection, nutrition, and regulation for neurons. One type of glia cells, called oligodendrocytes, produce myelin that insulates nerve fibers and increases the speed of electrical impulses.
Choice B reason:
This is an incorrect answer. Glia cells do not transmit electrical impulses along nerve fibers. This is the function of neurons, which are the primary cells of the nervous system.
Choice C reason:
This is an incorrect answer. Glia cells do not secrete neurotransmitters that communicate with other cells. This is also the function of neurons, which release neurotransmitters at the synapses to transmit signals to other neurons, muscles, or glands.
Choice D reason:
This is an incorrect answer. Glia cells do not destroy pathogens and foreign substances in the nervous system. This is the function of microglia, which are a type of immune cells that reside in the nervous system and act as macrophages.
Explanation
Choice A reason:
This is an incorrect answer. A tonic-clonic seizure (also known as a grand mal seizure) is characterized by alternating phases of muscle rigidity and jerking movements, along with loss of consciousness and postictal confusion.
Choice B reason:
This is a correct answer. An absence seizure (also known as a petit mal seizure) is characterized by brief episodes of staring, blinking, lip smacking, or other subtle movements, along with impaired awareness and no postictal confusion.
Choice C reason:
This is an incorrect answer. A myoclonic seizure is characterized by sudden, brief, and irregular muscle contractions, usually involving the arms, legs, or trunk.
Choice D reason:
This is an incorrect answer. An atonic seizure (also known as a drop attack) is characterized by sudden loss of muscle tone, resulting in falling or collapsing.
Explanation
Choice A reason:
This is a correct answer. Elevating the head of the bed to 30 degrees helps to reduce ICP by facilitating venous drainage from the brain and decreasing cerebral edema.
Choice B reason:
This is an incorrect answer. Administering morphine sulfate for pain relief can increase ICP by causing vasodilation, respiratory depression, and increased carbon dioxide levels in the blood.
Choice C reason:
This is an incorrect answer. Encouraging coughing and deep breathing exercises can increase ICP by increasing intrathoracic pressure, which impedes venous drainage from the brain.
Choice D reason:
This is an incorrect answer. Performing passive range of motion exercises can increase ICP by stimulating the sympathetic nervous system, which increases blood pressure and cerebral blood flow.
Explanation
Choice A reason:
This is an incorrect answer. Elevated CSF protein level is a common finding in clients who have GBS due to demyelination of peripheral nerves. It does not indicate infection or inflammation and does not require immediate intervention.
Choice B reason:
This is an incorrect answer. Decreased serum CK level is a normal finding in clients who have GBS because CK is released from damaged muscle tissue and GBS does not affect muscle cells directly.
Choice C reason:
This is a correct answer. Increased CSF WBC count indicates infection or inflammation in the central nervous system (CNS), which can be a complication of GBS or a sign of another condition such as meningitis or encephalitis. The nurse should report this finding to the provider for further evaluation and treatment.
Choice D reason:
This is an incorrect answer. Decreased serum sodium level can occur.
Explanation
Choice A reason:
This is a correct answer. Encouraging the client to perform ADLs independently helps to maintain their functional ability, self-esteem, and quality of life. The nurse should provide assistance and supervision as needed, but avoid doing everything for the client.
Choice B reason:
This is an incorrect answer. Providing the client with a high-protein, low-carbohydrate diet can interfere with the absorption and effectiveness of levodopa-carbidopa, which is the main medication used to treat Parkinson's disease. The nurse should provide the client with a balanced diet that includes adequate fluids and fiber.
Choice C reason:
This is a correct answer. Administering levodopa-carbidopa as prescribed helps to reduce the symptoms of Parkinson's disease such as tremors, rigidity, bradykinesia, and postural instability. Levodopa is converted to dopamine in the brain, which is deficient in clients who have Parkinson's disease. Carbidopa prevents the breakdown of levodopa in the peripheral tissues, allowing more levodopa to reach the brain.
Choice D reason:
This is a correct answer. Teaching the client to use assistive devices such as a walker or cane helps to improve their mobility, balance, and safety. The nurse should also teach the client strategies to overcome freezing episodes, such as rocking from side to side or stepping over an imaginary line.
Choice E reason:
This is a correct answer. Monitoring the client for orthostatic hypotension helps to prevent falls and injuries. Orthostatic hypotension is a common complication of Parkinson's disease and its medications, which can cause a sudden drop in blood pressure when changing positions. The nurse should instruct the client to change positions slowly and report any symptoms such as dizziness, lightheadedness, or fainting.
Traumatic Brain Injury: Concussions,
Explanation
Choice A reason:
This is a correct answer. Frequent headaches are a common symptom of CTE, which is a progressive degenerative brain disease caused by repeated head trauma. Headaches may be triggered by physical or mental exertion, stress, or noise.
Choice B reason:
This is a correct answer. Memory loss is another common symptom of CTE, which affects the areas of the brain responsible for learning and recall. Memory loss may manifest as difficulty remembering names, dates, events, or conversations.
Choice C reason:
This is a correct answer. Personality changes are also a common symptom of CTE, which affects the areas of the brain responsible for mood and behavior. Personality changes may include irritability, aggression, depression, anxiety, impulsivity, or apathy.
Choice D reason:
This is a correct answer. All of the above are possible symptoms of CTE, which can vary in severity and onset depending on the individual and the extent of brain damage. Other possible symptoms include confusion, cognitive impairment, speech problems, vision problems, balance problems, motor problems, or suicidal thoughts.
Explanation
Choice A reason:
This is a correct answer. Monitoring the client's GCS score helps to assess the level of consciousness and neurological function after a concussion. The GCS score ranges from 3 to 15, with lower scores indicating more severe brain injury.
Choice B reason:
This is a correct answer. Administering acetaminophen for pain relief helps to reduce headache and discomfort after a concussion. Acetaminophen is preferred over nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin, which can increase the risk of bleeding.
Choice C reason:
This is a correct answer. Encouraging the client to rest in a dark and quiet room helps to promote healing and recovery after a concussion. Rest includes physical and mental rest, which means avoiding strenuous activities, sports, driving, work, school, or screen time until symptoms resolve.
Choice D reason:
This is an incorrect answer. Providing stimulating activities such as puzzles and games can worsen symptoms and delay recovery after a concussion. The client should avoid cognitive tasks that require concentration, attention, or memory until cleared by a health care provider.
Choice E reason:
This is a correct answer. Educating the client about the signs of post-concussion syndrome helps to prepare them for possible complications and when to seek medical attention. Post-concussion syndrome is a condition in which symptoms persist for weeks or months after a concussion. Symptoms may include headache, dizziness, fatigue, insomnia, anxiety, depression, or cognitive impairment.
Explanation
Choice A reason:
This is an incorrect answer. The nurse should not advise the client to resume their normal activities as long as they wear a helmet. A helmet does not prevent concussions from occurring and may give a false sense of security. The client should not return to sports or other physical activities until they are asymptomatic and cleared by their doctor.
Choice B reason:
This is an incorrect answer. The nurse should not advise the client to avoid any physical activity until their symptoms are completely gone. While the client should avoid strenuous or risky activities that could cause another concussion, they may be able to engage in some light or moderate activities that do not worsen their symptoms or increase their heart rate. The client should follow a gradual return-to-play protocol under the guidance of their doctor.
Choice C reason:
This is a correct answer. The nurse should advise the client to consult their doctor first and follow their recommendations. The doctor will evaluate the client's recovery and determine when it is safe for them to return to sports or other physical activities. The doctor will also provide a gradual return-to-play protocol that involves increasing the intensity and duration of activity over several days or weeks.
Choice D reason:
This is an incorrect answer. The nurse should not advise the client to ask their coach or trainer what they think. The coach or trainer may not be qualified or knowledgeable enough to assess the client's condition and readiness to return to sports or other physical activities. The client should rely on their doctor's advice and not on their coach's or trainer's opinion.
Explanation
Choice A reason:
This is an incorrect answer. The client does not need further teaching if they say they will take acetaminophen if they have a headache. Acetaminophen is a safe and effective medication for pain relief after a concussion. It does not increase the risk of bleeding or interfere with brain function.
Choice B reason:
This is an incorrect answer. The client does not need further teaching if they say they will avoid drinking alcohol or taking sleeping pills. Alcohol and sleeping pills can worsen the symptoms and recovery of a concussion. They can also mask the signs of worsening brain injury or increase the risk of falls or accidents.
Choice C reason:
This is a correct answer. The client needs further teaching if they say they will check their pupils every hour for any changes. Checking the pupils is not a reliable or accurate way to monitor the condition of a concussion. Pupil changes may not occur until late stages of brain injury or may be caused by other factors such as light exposure or medication use.
Choice D reason:
This is an incorrect answer. The client does not need further teaching if they say they will have someone stay with them for the next 24 hours. Having someone stay with them is a recommended precaution after a concussion. The person can observe the client for any signs of worsening brain injury such as confusion, vomiting, seizures, or loss of consciousness and call for help if needed.
Explanation
Choice A reason:
This is an incorrect answer. The nurse should not instruct the client to return to work or school as soon as possible after a concussion. The client should rest and avoid cognitive tasks that require concentration, attention, or memory until their symptoms resolve and they are cleared by their provider.
Choice B reason:
This is a correct answer. The nurse should instruct the client to avoid driving or operating machinery until cleared by the provider after a concussion. Driving or operating machinery can be dangerous and impairing for the client who may have symptoms such as headache, dizziness, fatigue, blurred vision, or slowed reaction time.
Choice C reason:
This is an incorrect answer. The nurse should not instruct the client to resume sports or physical activities within a week after a concussion. The client should avoid strenuous or risky activities that could cause another concussion or worsen their symptoms until they are asymptomatic and cleared by their provider.
Choice D reason:
This is an incorrect answer. The nurse should not instruct the client to take ibuprofen or aspirin for pain relief after a concussion. Ibuprofen and aspirin are nonsteroidal anti-inflammatory drugs (NSAIDs) that can increase the risk of bleeding in the brain or interfere with blood clotting.
Explanation
Choice A reason:
This is an incorrect answer. Administering antiemetic medication as prescribed is an appropriate action for the nurse to take, but not the first one. The nurse should first assess the client's neurological status, as nausea and vomiting can be signs of increased intracranial pressure (ICP) or worsening brain injury.
Choice B reason:
This is a correct answer. Assessing the client's level of consciousness and orientation is the first action that the nurse should take when caring for a client who has a concussion and reports nausea and vomiting. The nurse should use tools such as the Glasgow Coma Scale (GCS) or the Alert, Verbal, Painful, Unresponsive (AVPU) scale to evaluate the client's neurological function and identify any changes or deterioration.
Choice C reason:
This is an incorrect answer. Providing oral fluids and crackers to the client is not an appropriate action for the nurse to take, especially not the first one. The nurse should avoid giving anything by mouth to the client who has nausea and vomiting, as this can increase the risk of aspiration or dehydration.
Choice D reason:
This is an incorrect answer. Notifying the provider of the client's condition is an important action for the nurse to take, but not the first one. The nurse should first assess the client's neurological status and gather relevant data before reporting to the provider.
Explanation
Choice A reason:
This is an incorrect answer. The client does not need immediate reporting if they have a GCS score of 15. This is the highest possible score on the GCS, which indicates that the client is fully alert and oriented.
Choice B reason:
This is a correct answer. The client needs immediate reporting if they have unequal pupils with a difference of 2 mm. This is an abnormal finding that indicates increased intracranial pressure (ICP) or cranial nerve damage, which can be life-threatening.
Choice C reason:
This is an incorrect answer. The client does not need immediate reporting if they have a positive Babinski reflex on both feet. This is a normal finding in infants and young children, but an abnormal finding in adults. However, it does not indicate an acute or urgent condition, but rather a chronic or long-term damage to the corticospinal tract.
Choice D reason:
This is an incorrect answer. The client does not need immediate reporting if they have difficulty performing finger-to-nose test. This is an abnormal finding that indicates cerebellar dysfunction, which affects coordination and balance. However, it does not indicate an acute or urgent condition, but rather a mild or moderate impairment.
Explanation
Choice A reason:
This is a correct answer. Wearing appropriate protective equipment such as helmets and mouth guards helps to reduce the risk and severity of concussion by absorbing some of the impact force and protecting the head and teeth from injury.
Choice B reason:
This is a correct answer. Reporting any symptoms of concussion to the coach or trainer immediately helps to ensure proper diagnosis and treatment of concussion by a health care provider. Symptoms may include headache, dizziness, nausea, vomiting, confusion, memory loss, blurred vision, or sensitivity to light or noise.
Choice C reason:
This is an incorrect answer. Seeking medical attention if symptoms persist for more than 24 hours is not enough for concussion management. The nurse should advise the athletes to seek medical attention as soon as possible after a suspected concussion, regardless of how long the symptoms last or how severe they are.
Choice D reason:
This is a correct answer. Taking a baseline cognitive test before the season starts helps to establish a reference point for comparison after a concussion. A cognitive test measures mental functions such as memory, attention, reaction time, and problem-solving.
Choice E reason:
This is a correct answer. Drinking plenty of fluids and eating a balanced diet after a concussion helps to promote healing and recovery by providing hydration and nutrition to the brain and body.
Stroke: Ischemic stroke, Hemorrhagic stroke, Transient ischemic attack (TIA)
Explanation
Choice A reason:
This is a correct answer. Alteplase is a thrombolytic agent that dissolves blood clots and restores blood flow to the brain in clients who have an ischemic stroke. It should be administered within 3 to 4.5 hours of symptom onset and after ruling out hemorrhagic stroke.
Choice B reason:
This is an incorrect answer. Mannitol is an osmotic diuretic that reduces intracranial pressure (ICP) by drawing fluid out of the brain tissue and into the bloodstream. It is used for clients who have increased ICP due to cerebral edema, not ischemic stroke.
Choice C reason:
This is an incorrect answer. Nimodipine is a calcium channel blocker that prevents vasospasm and improves cerebral blood flow in clients who have a subarachnoid hemorrhage, which is a type of hemorrhagic stroke, not ischemic stroke.
Choice D reason:
This is an incorrect answer. Phenytoin is an anticonvulsant that prevents or treats seizures in clients who have a brain injury or tumor, not ischemic stroke.
Explanation
Choice A reason:
This is a correct answer. Sudden severe headache is a common symptom of hemorrhagic stroke, which is caused by bleeding into the brain tissue or subarachnoid space. The headache may be described as "the worst headache of my life" or "thunderclap headache".
Choice B reason:
This is an incorrect answer. Facial drooping is a common symptom of ischemic stroke, which is caused by a blockage in a cerebral artery that reduces blood flow to the brain tissue. Facial drooping may affect one side of the face and cause asymmetry or difficulty smiling.
Choice C reason:
This is an incorrect answer. Slurred speech is another common symptom of ischemic stroke, which affects the areas of the brain responsible for language and communication. Slurred speech may also be accompanied by aphasia, which is difficulty understanding or expressing words.
Choice D reason:
This is a correct answer. Nuchal rigidity is a common symptom of subarachnoid hemorrhage, which is a type of hemorrhagic stroke that involves bleeding into the space between the brain and the meninges. Nuchal rigidity refers to stiffness or pain in the neck when flexing or extending it.
Choice E reason:
This is a correct answer. Hemiparesis is a common symptom of both ischemic and hemorrhagic stroke, which affect the motor areas of the brain and cause weakness or paralysis on one side of the body. Hemiparesis may affect the face, arm, leg, or trunk on the opposite side of the brain injury.
Explanation
Choice A reason:
This is an incorrect answer. Elevated troponin level is not a finding that indicates atrial fibrillation as the cause of ischemic stroke. Troponin is a cardiac enzyme that is released into the bloodstream when there is damage to the heart muscle, such as in myocardial infarction (MI) or heart failure. Troponin level may be elevated in some clients who have ischemic stroke due to concurrent cardiac conditions, but it does not indicate the source of embolism.
Choice B reason:
This is a correct answer. Elevated D-dimer level is a finding that indicates atrial fibrillation as the cause of ischemic stroke. D-dimer is a protein fragment that is produced when a blood clot is dissolved by fibrinolysis. D-dimer level may be elevated in clients who have ischemic stroke due to embolism from atrial fibrillation, which is an irregular and rapid heart rhythm that causes poor blood flow and clot formation in the atria.
Choice C reason:
This is an incorrect answer. Elevated C-reactive protein level is not a finding that indicates atrial fibrillation as the cause of ischemic stroke. C-reactive protein is an inflammatory marker that is produced by the liver in response to infection, inflammation, or tissue injury. C-reactive protein level may be elevated in clients who have ischemic stroke due to various causes, but it does not indicate the source of embolism.
Choice D reason:
This is an incorrect answer. Elevated INR is not a finding that indicates atrial fibrillation as the cause of ischemic stroke. INR is a measure of how long it takes for blood to clot, which reflects the effect of anticoagulant medications such as warfarin. INR may be elevated in clients who have ischemic stroke due to anticoagulant therapy, but it does not indicate the source of embolism.
Explanation
Choice A reason:
This is an incorrect answer. Elevating the head of the bed to 30 degrees is not an appropriate intervention for a client who has a hemorrhagic stroke. Elevating the head of the bed can lower blood pressure and reduce cerebral perfusion pressure, which can worsen brain ischemia and injury.
Choice B reason:
This is an incorrect answer. Administering aspirin as prescribed is not an appropriate intervention for a client who has a hemorrhagic stroke. Aspirin is an antiplatelet agent that inhibits
the clotting of blood and increases the risk of bleeding in the brain or elsewhere. Aspirin is contraindicated for clients who have a hemorrhagic stroke and may worsen their condition.
Choice C reason:
This is a correct answer. Monitoring blood pressure and keeping it within normal range is an appropriate intervention for a client who has a hemorrhagic stroke. Blood pressure is a major factor that affects the severity and outcome of hemorrhagic stroke. High blood pressure can increase the bleeding and ICP, while low blood pressure can reduce cerebral perfusion and oxygenation. The nurse should monitor blood pressure frequently and administer antihypertensive or vasopressor medications as prescribed to maintain optimal blood pressure.
Choice D reason:
This is an incorrect answer. Performing passive range of motion exercises is not an appropriate intervention for a client who has a hemorrhagic stroke. Passive range of motion exercises can increase ICP and bleeding by stimulating the sympathetic nervous system, which increases blood pressure and cerebral blood flow. The nurse should avoid any activity that can increase ICP or bleeding in the acute phase of hemorrhagic stroke.
A nurse is educating a client who has a transient ischemic attack (TIA). The client says to the nurse, "I don't understand why I need to take medication if it was just a mini-stroke." How should the nurse respond?
Explanation
Choice A reason:
This is a correct answer. The nurse should explain to the client that they need to take medication to prevent blood clots from forming in their arteries after a TIA. A TIA is caused by a temporary blockage in a cerebral artery that reduces blood flow to the brain tissue and causes stroke-like symptoms that resolve within 24 hours. However, a TIA increases the risk of having a full-blown ischemic stroke in the future, which can cause permanent brain damage or death. Therefore, antiplatelet or anticoagulant medications are prescribed to prevent clot formation and reduce stroke risk.
Choice B reason:
This is an incorrect answer. The nurse should not tell the client that they need to take medication to reduce the swelling in their brain after a stroke. This is not the purpose of medication therapy for a TIA. A TIA does not cause significant swelling or edema in the brain, unlike a hemorrhagic stroke, which involves bleeding into the brain tissue or subarachnoid space. Swelling in the brain can increase intracranial pressure (ICP) and cause further brain damage or herniation.
Choice C reason:
This is an incorrect answer. The nurse should not tell the client that they need to take medication to lower their blood pressure and cholesterol levels. This is not the immediate purpose of medication therapy for a TIA, although it may be part of the long-term management of stroke risk factors. High blood pressure and high cholesterol are common causes of atherosclerosis, which is the buildup of plaque in the arterial walls that narrows the lumen and reduces blood flow. Atherosclerosis can lead to ischemic stroke if a piece of plaque breaks off and blocks a cerebral artery.
Choice D reason:
This is an incorrect answer. The nurse should not tell the client that they need to take medication to control their blood sugar and prevent diabetes. This is not the immediate purpose of medication therapy for a TIA, although it may be part of the long-term management of stroke risk factors. High blood sugar and diabetes are common causes of endothelial dysfunction, which is the impairment of the inner lining of the blood vessels that regulates blood flow and clotting. Endothelial dysfunction can lead to ischemic stroke if a blood clot forms and blocks a cerebral artery.
Peripheral Nervous System Disorders: Peripheral neuropathy; Radiculopathy; Charcot-Marie-Tooth disease
Explanation
Choice A reason:
This is a correct answer. Inspecting the client's feet daily for any injuries or infections is an important intervention for a client who has peripheral neuropathy due to diabetes mellitus. Peripheral neuropathy is a condition that affects the nerves in the extremities, causing numbness, tingling, pain, or weakness. Diabetes mellitus is a common cause of peripheral neuropathy, as high blood sugar levels can damage the nerves and blood vessels. The client may not feel any cuts, blisters, ulcers, or infections on their feet due to reduced sensation, which can lead to complications such as gangrene or amputation. Therefore, the nurse should inspect the client's feet daily and report any abnormalities to the provider.
Choice B reason:
This is an incorrect answer. Massaging the client's legs and feet with lotion to improve circulation is not an appropriate intervention for a client who has peripheral neuropathy due to diabetes mellitus. Massaging the client's legs and feet can cause further damage to the nerves or skin, especially if there are any injuries or infections present. Lotion can also increase the risk of infection by creating a moist environment for bacteria to grow. The nurse should avoid massaging the client's legs and feet and use other methods to improve circulation, such as elevating the legs, wearing compression stockings, or exercising regularly.
Choice C reason:
This is an incorrect answer. Encouraging the client to wear tight-fitting shoes and socks to prevent friction is not an appropriate intervention for a client who has peripheral neuropathy due to diabetes mellitus. Tight-fitting shoes and socks can impair blood flow and oxygen delivery to the feet, which can worsen peripheral neuropathy and increase the risk of tissue damage or necrosis. Tight-fitting shoes and socks can also cause pressure ulcers, blisters, or corns on the feet, which can become infected or difficult to heal. The nurse should encourage the client to wear loose-fitting shoes and socks that are comfortable and breathable.
Choice D reason:
This is an incorrect answer. Teaching the client to soak their feet in warm water for 15 minutes twice a day is not an appropriate intervention for a client who has peripheral neuropathy due to diabetes mellitus. Soaking the feet in warm water can cause burns or scalds on the skin, as the client may not be able to sense the temperature of the water due to reduced sensation. Soaking the feet in warm water can also increase the risk of infection by softening the skin and making it more prone to injury or breakdown. The nurse should teach the client to wash their feet with mild soap and water daily, dry them thoroughly, and check the water temperature with their elbow or thermometer before using it.
Explanation
Choice A reason:
This is a correct answer. Low back pain that radiates down the leg is a common symptom of radiculopathy due to a herniated intervertebral disc in the lumbar spine. Radiculopathy is a condition that affects the nerve roots that exit from the spinal cord, causing pain, numbness, tingling, or weakness along their distribution. A herniated intervertebral disc is a common cause of radiculopathy, as it can compress or irritate the nerve roots in the spinal canal or intervertebral foramen. The pain may follow a dermatomal pattern depending on which nerve root is affected.
Choice B reason:
This is a correct answer. Muscle weakness or atrophy in the affected leg is another common symptom of radiculopathy due to a herniated intervertebral disc in the lumbar spine. Muscle weakness or atrophy may result from reduced nerve stimulation or innervation to the muscles in the leg, which can affect their function and appearance. The muscle weakness or atrophy may follow a myotomal pattern depending on which nerve root is affected.
Choice C reason:
This is a correct answer. Diminished or absent deep tendon reflexes in the affected leg is another common symptom of radiculopathy due to a herniated intervertebral disc in the lumbar spine. Deep tendon reflexes are involuntary responses that are elicited by tapping on specific tendons with a reflex hammer, such as the patellar or Achilles tendon. Diminished or absent deep tendon reflexes may indicate damage or dysfunction of the nerve roots that mediate the reflex arc. The diminished or absent deep tendon reflexes may follow a segmental pattern depending on which nerve root is affected.
Choice D reason:
This is a correct answer. Positive straight leg raise test on the affected side is another common symptom of radiculopathy due to a herniated intervertebral disc in the lumbar spine. The straight leg raise test is a physical examination maneuver that involves raising the client's leg while keeping it straight and flexing the foot. A positive test is indicated by pain in the low back or leg that is reproduced or worsened by the maneuver, which suggests nerve root compression or irritation by the herniated disc.
Choice E reason:
This is an incorrect answer. Loss of bladder or bowel control is not a common symptom of radiculopathy due to a herniated intervertebral disc in the lumbar spine. Loss of bladder or bowel control may indicate cauda equina syndrome, which is a rare but serious condition that involves compression of the nerve roots at the end of the spinal cord, causing severe low back pain, saddle anesthesia, sexual dysfunction, and urinary or fecal incontinence. Cauda equina syndrome requires immediate medical attention and surgical decompression to prevent permanent nerve damage or paralysis.
Explanation
Choice A reason:
This is an incorrect answer. The client does not need further teaching if they say they will wear braces or splints to support their feet and ankles. Braces or splints are helpful devices for clients who have CMT, which is a hereditary disorder that affects the peripheral nerves and causes muscle weakness, atrophy, and deformity in the feet, legs, hands, and arms. Braces or splints can improve mobility, stability, and alignment of the affected limbs.
Choice B reason:
This is an incorrect answer. The client does not need further teaching if they say they will avoid strenuous exercise and heavy lifting. These activities can worsen the symptoms and progression of CMT, as they can cause fatigue, injury, or overuse of the weakened muscles and nerves. The client should engage in moderate exercise and physical therapy that are tailored to their abilities and needs.
Choice C reason:
This is a correct answer. The client needs further teaching if they say they will take vitamin B12 supplements to prevent nerve damage. Vitamin B12 deficiency can cause peripheral neuropathy, which is a condition that affects the peripheral nerves and causes numbness, tingling, pain, or weakness in the extremities. However, vitamin B12 supplements do not prevent or treat CMT, which is a genetic disorder that affects the structure and function of the peripheral nerves.
Choice D reason:
This is an incorrect answer. The client does not need further teaching if they say they will inspect their feet daily for any injuries or infections. This is an important self-care measure for clients who have CMT, as they may have reduced sensation, circulation, or healing in their feet due to nerve damage. The client should inspect their feet daily and report any abnormalities to their provider.
Explanation
Choice A reason:
This is a correct answer. Spurling's test is a physical examination maneuver that involves extending, rotating, and laterally flexing the client's neck to the affected side and applying downward pressure on the head. A positive test is indicated by pain or paresthesia radiating from the neck to the shoulder or arm on the same side, which suggests nerve root compression or irritation by cervical spine degeneration.
Choice B reason:
This is an incorrect answer. Romberg's test is a physical examination maneuver that involves asking the client to stand with their feet together and eyes closed for 20 seconds while observing for balance and sway. A positive test is indicated by loss of balance or increased sway, which suggests cerebellar dysfunction or proprioceptive impairment.
Choice C reason:
This is an incorrect answer. Tinel's sign is a physical examination maneuver that involves tapping over the median nerve at the wrist or the ulnar nerve at the elbow. A positive sign is indicated by tingling or pain in the distribution of the nerve, which suggests nerve entrapment or injury.
Choice D reason:
This is an incorrect answer. Phalen's test is a physical examination maneuver that involves asking the client to hold their wrists in full flexion for 60 seconds while pressing the dorsal surfaces of their hands together. A positive test is indicated by numbness, tingling, or pain in the median nerve distribution of the hand, which suggests carpal tunnel syndrome.
Explanation
Choice A reason:
This is a correct answer. The nurse should inform the client that the symptoms of peripheral neuropathy may improve after stopping chemotherapy, as chemotherapy is a common cause of peripheral neuropathy. Chemotherapy can damage the peripheral nerves and cause numbness, tingling, pain, or weakness in the extremities. The symptoms may be reversible or permanent depending on the type, dose, and duration of chemotherapy and the individual's response.
Choice B reason:
This is an incorrect answer. The nurse should not tell the client that the risk of peripheral neuropathy can be reduced by taking antioxidants, as there is no evidence to support this claim. Antioxidants are substances that protect the cells from oxidative stress and free radical damage, which may contribute to various diseases and aging. However, antioxidants have not been proven to prevent or treat peripheral neuropathy, and some antioxidants may interact with chemotherapy or other medications.
Choice C reason:
This is a correct answer. The nurse should inform the client that the treatment of peripheral neuropathy may include medications such as gabapentin or duloxetine, which are commonly used to manage neuropathic pain. Gabapentin is an anticonvulsant that modulates calcium channels and reduces nerve excitability. Duloxetine is an antidepressant that inhibits the reuptake of serotonin and norepinephrine and enhances pain inhibition. The nurse should also educate the client about the possible side effects and interactions of these medications.
Choice D reason:
This is a correct answer. The nurse should inform the client that the prevention of peripheral neuropathy includes avoiding alcohol and smoking, which are common risk factors for peripheral neuropathy. Alcohol and smoking can damage the peripheral nerves and blood vessels, impairing blood flow and oxygen delivery to the extremities. The nurse should advise the client to limit or quit alcohol and smoking and seek help if needed.
Choice E reason:
This is a correct answer. The nurse should inform the client that the complications of peripheral neuropathy may include falls or injuries, which can affect their safety and quality of life. Peripheral neuropathy can impair sensation, balance, coordination, and reflexes in the extremities, increasing the risk of falls or injuries. The nurse should teach the client strategies to prevent falls or injuries, such as wearing proper footwear, using assistive devices, removing hazards from the environment, and inspecting their feet daily for any wounds or infections.
Neurodegenerative Diseases: Alzheimer's disease, Parkinson's disease
Explanation
Choice A reason:
This is a correct answer. The nurse should explain to the client's family that AD is caused by a buildup of abnormal protein deposits called amyloid plaques and twisted fibers called neurofibrillary tangles in the brain that impair nerve function and communication. These changes lead to progressive loss of memory, language, reasoning, judgment, and other cognitive abilities.
Choice B reason:
This is an incorrect answer. The nurse should not tell the client's family that AD is caused by a deficiency of dopamine in the brain that affects movement and cognition. This is not the cause of AD, but rather Parkinson's disease (PD), which is another neurodegenerative disorder that affects the basal ganglia and causes tremors, rigidity, bradykinesia, and postural instability.
Choice C reason:
This is an incorrect answer. The nurse should not tell the client's family that AD is caused by an autoimmune disorder that attacks the myelin sheath of the nerve cells in the brain and spinal cord. This is not the cause of AD, but rather multiple sclerosis (MS), which is another neurodegenerative disorder that causes demyelination and inflammation of the central nervous system (CNS) and leads to sensory, motor, and cognitive impairments.
Choice D reason:
This is an incorrect answer. The nurse should not tell the client's family that AD is caused by a viral infection that destroys the neurons in the brain and causes inflammation and swelling. This is not the cause of AD, but rather encephalitis, which is an acute inflammatory condition of the brain that can be caused by various viruses or bacteria and can result in neurological deficits or death.
Explanation
Choice A reason:
This is a correct answer. Resting tremor is a common symptom of PD, which occurs when the affected limb or body part shakes involuntarily at rest and stops with voluntary movement or sleep. Resting tremor usually affects one side of the body first and then progresses to both sides. It typically involves the hand, arm, leg, jaw, or tongue.
Choice B reason:
This is a correct answer. Muscle rigidity is another common symptom of PD, which occurs when there is increased resistance to passive movement of the joints due to sustained muscle contraction. Muscle rigidity can cause stiffness, pain, reduced range of motion, and difficulty initiating movement.
Choice C reason:
This is a correct answer. Bradykinesia is another common symptom of PD, which occurs when there is slowness or paucity of movement due to impaired initiation or execution of movement. Bradykinesia can affect various aspects of motor function, such as facial expression, speech, swallowing, gait, writing, dressing, and self-care.
Choice D reason:
This is a correct answer. Postural instability is another common symptom of PD, which occurs when there is impaired balance or coordination due to reduced postural reflexes or sensory feedback. Postural instability can cause falls, difficulty turning or changing direction, stooped posture, shuffling steps, or freezing episodes.
Choice E reason:
This is an incorrect answer. Nuchal rigidity is not a common symptom of PD, but rather a sign of meningitis or subarachnoid hemorrhage. Nuchal rigidity occurs when there is stiffness or pain in the neck when flexing or extending it due to inflammation or irritation of the meninges or subarachnoid space.
Explanation
Choice A reason:
This is a correct answer. The nurse should explain to the client that donepezil is a cholinesterase inhibitor that works by increasing the level of acetylcholine in the brain, which is a neurotransmitter that is involved in memory, learning, and cognition. Donepezil can slow down the progression of AD and improve the client's memory and thinking abilities.
Choice B reason:
This is an incorrect answer. The nurse should not tell the client that donepezil will increase the level of dopamine in the brain and reduce their tremors and rigidity. This is not the mechanism or effect of donepezil, but rather levodopa or carbidopa, which are medications used to treat Parkinson's disease (PD). PD is caused by a deficiency of dopamine in the brain, which affects movement and cognition.
Choice C reason:
This is an incorrect answer. The nurse should not tell the client that donepezil will prevent the inflammation and swelling in their brain and reduce their headaches and confusion. This is not the mechanism or effect of donepezil, but rather corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs), which are medications used to treat encephalitis or meningitis. Encephalitis or meningitis are inflammatory conditions of the brain or meninges that can be caused by various viruses or bacteria.
Choice D reason:
This is an incorrect answer. The nurse should not tell the client that donepezil will enhance the transmission of nerve impulses in their brain and improve their mood and behavior. This is not the mechanism or effect of donepezil, but rather antidepressants or mood stabilizers, which are medications used to treat depression or bipolar disorder. Depression or bipolar disorder are mood disorders that affect the levels of serotonin, norepinephrine, or dopamine in the brain.
Explanation
Choice A reason:
This is an incorrect answer. Instructing the client to lift their feet and take big steps when walking is not an effective intervention for a client who has PD and experiences freezing episodes. Freezing episodes are sudden and brief periods of inability to move or initiate movement, especially when starting to walk, turning, or crossing a threshold. Lifting the feet and taking big steps may be difficult or impossible for the client during a freezing episode and may increase the risk of falls or injuries.
Choice B reason:
This is an incorrect answer. Instructing the client to use a walker or cane for support and stability is not an effective intervention for a client who has PD and experiences freezing episodes. A walker or cane may actually trigger or worsen freezing episodes by creating a visual cue that interferes with the initiation of movement. A walker or cane may also reduce the client's confidence and independence in walking.
Choice C reason:
This is a correct answer. Instructing the client to focus on an object or a line on the floor ahead of them is an effective intervention for a client who has PD and experiences freezing episodes. Focusing on an external cue can help the client overcome the internal blockage that prevents them from moving or initiating movement. Focusing on an object or a line can also help the client maintain their balance and direction while walking.
Choice D reason:
This is an incorrect answer. Instructing the client to hum or sing a song while walking is not an effective intervention for a client who has PD and experiences freezing episodes. Humming or singing a song may distract the client from their walking and cause them to lose their rhythm or coordination. Humming or singing a song may also increase the risk of aspiration or choking if the client has dysphagia, which is difficulty swallowing due to impaired muscle control in PD.
Explanation
Choice A reason:
This is an incorrect answer. The caregiver does not need further teaching if they say that memantine will help reduce the amount of glutamate in their loved one's brain. Memantine is an N-methyl-D-aspartate (NMDA) receptor antagonist that works by blocking the excessive stimulation of glutamate, which is a neurotransmitter that is involved in learning, memory, and cognition. Glutamate can be toxic to nerve cells if it accumulates in high levels in AD.
Choice B reason:
This is an incorrect answer. The caregiver does not need further teaching if they say that memantine will help improve their loved one's memory and attention span. Memantine can improve some aspects of cognitive function in clients who have moderate to severe AD by enhancing nerve communication and preventing nerve damage.
Choice C reason:
This is a correct answer. The caregiver needs further teaching if they say that memantine will help prevent their loved one from having seizures or hallucinations. This is not the purpose or effect of memantine, but rather anticonvulsants or antipsychotics, which are medications used to treat seizures or psychosis, respectively. Seizures or hallucinations are not common symptoms of AD, but rather complications that may occur in advanced stages of the disease.
Choice D reason:
This is an incorrect answer. The caregiver does not need further teaching if they say that memantine will help slow down the decline of their loved one's cognitive function. Memantine can slow down the progression of AD and delay the need for institutionalization by preserving some cognitive abilities and daily functioning.
Explanation
Choice A reason:
This is an incorrect answer. The nurse should not instruct the client to take levodopa-carbidopa with food to prevent nausea and vomiting. This is not an effective way to prevent these side effects, as food, especially protein-rich food, can interfere with the absorption and effectiveness of levodopa-carbidopa. The nurse should advise the client to take levodopa-carbidopa on an empty stomach, at least 30 minutes before or 1 hour after meals.
Choice B reason:
This is a correct answer. The nurse should instruct the client to take levodopa-carbidopa at the same time every day to maintain a steady level. Levodopa-carbidopa is a combination medication that increases the level of dopamine in the brain, which is a neurotransmitter that is deficient in PD and affects movement and cognition. Levodopa-carbidopa should be taken at regular intervals to prevent fluctuations in dopamine levels and avoid "wearing-off" or "on-off" phenomena, which are periods of reduced or enhanced response to the medication.
Choice C reason:
This is an incorrect answer. The nurse should not instruct the client to take levodopa-carbidopa with a glass of milk to enhance absorption. This is not an effective way to enhance absorption, as milk, especially dairy products, can decrease the absorption and effectiveness of levodopa-carbidopa. The nurse should advise the client to avoid dairy products or limit their intake when taking levodopa-carbidopa.
Choice D reason:
This is an incorrect answer. The nurse should not instruct the client to take levodopa-carbidopa as needed when they have symptoms of PD. This is not an appropriate way to take levodopa-carbidopa, as it can cause erratic changes in dopamine levels and worsen the symptoms and progression of PD. The nurse should advise the client to take levodopa-carbidopa as prescribed by their provider and not to skip or adjust doses without consulting their provider.
Explanation
Choice A reason:
This is an incorrect answer. The caregiver does not need further teaching if they say that pramipexole will help reduce the symptoms of PD by stimulating dopamine receptors in the brain. Pramipexole is a dopamine agonist that works by mimicking the action of dopamine, which is a neurotransmitter that is deficient in PD and affects movement and cognition. Pramipexole can reduce tremors, rigidity, bradykinesia, and postural instability in clients who have PD.
Choice B reason:
This is an incorrect answer. The caregiver does not need further teaching if they say that pramipexole will help prevent the development of dyskinesia or involuntary movements in their loved one. Dyskinesia is a common side effect of levodopa-carbidopa, which is another medication used to treat PD. Pramipexole can delay or reduce the occurrence of dyskinesia by allowing lower doses of levodopa-carbidopa to be used.
Choice C reason:
This is an incorrect answer. The caregiver does not need further teaching if they say that pramipexole will help increase the duration and quality of sleep in their loved one. Sleep disturbances are common in clients who have PD, due to various factors such as nocturia, pain, restless legs syndrome, or anxiety. Pramipexole can improve sleep quality and quantity by reducing nighttime awakenings and increasing REM sleep.
Choice D reason:
This is a correct answer. The caregiver needs further teaching if they say that pramipexole will help improve the mood and motivation of their loved one. This is not the purpose or effect of pramipexole, but rather antidepressants or stimulants, which are medications used to treat depression or apathy, respectively. Depression or apathy are common neuropsychiatric symptoms of PD, which affect the levels of serotonin, norepinephrine, or dopamine in the brain.
Explanation
Choice A reason:
This is a correct answer. The nurse should advise the client and their caregiver to maintain a consistent daily routine and environment, as this can help reduce anxiety, agitation, or disorientation in clients who have AD. AD is a progressive neurodegenerative disorder that affects memory, language, reasoning, judgment, and other cognitive abilities. Maintaining a consistent daily routine and environment can provide structure, familiarity, and security for the client.
Choice B reason:
This is a correct answer. The nurse should advise the client and their caregiver to use memory aids such as calendars, clocks, or lists, as this can help enhance memory and orientation in clients who have AD. Memory aids can provide cues or reminders for the client about important information such as dates, events, tasks, or names.
Choice C reason:
This is a correct answer. The nurse should advise the client and their caregiver to engage in physical and mental activities that are enjoyable and stimulating, as this can help preserve cognitive function and well-being in clients who have AD. Physical and mental activities can improve blood flow and oxygen delivery to the brain, stimulate neural connections, enhance mood and self-esteem, and prevent boredom and depression.
Choice D reason:
This is an incorrect answer. The nurse should not advise the client and their caregiver to avoid social interactions that may cause stress or confusion, as this can have negative effects on cognitive function and well-being in clients who have AD. Social interactions can provide emotional support, companionship, communication skills, and cognitive stimulation for the client. The nurse should encourage the client and their caregiver to maintain social contacts and participate in activities that are appropriate for the client's level of functioning and interest.
Choice E reason:
This is an incorrect answer. The nurse should not advise the client and their caregiver to limit fluid intake and caffeine consumption, as this can have negative effects on cognitive function and well-being in clients who have AD. Fluid intake and caffeine consumption are not directly related to the cause or progression of AD, and limiting them can cause dehydration, constipation, or headaches. The nurse should advise the client and their caregiver to ensure adequate hydration and nutrition for the client and avoid substances that may interfere with sleep quality or medication effectiveness, such as alcohol or nicotine.
Neuroinflammation: Multiple sclerosis; Meningitis; Guillain-Barré syndrome
Explanation
Choice A reason:
This is an incorrect answer. Nystagmus is a condition that causes involuntary and rhythmic eye movements, which can affect vision and balance. Nystagmus can occur in some clients who have MS due to damage to the brainstem or cerebellum, but it does not cause eye pain or loss of color perception.
Choice B reason:
This is an incorrect answer. Diplopia is a condition that causes double vision, which can affect depth perception and coordination. Diplopia can occur in some clients who have MS due to damage to the cranial nerves or ocular muscles, but it does not cause eye pain or loss of color perception.
Choice C reason:
This is a correct answer. Optic neuritis is a condition that causes inflammation and demyelination of the optic nerve, which can affect visual acuity and color perception. Optic neuritis can occur in some clients who have MS due to damage to the optic nerve or chiasm, and it often causes blurred vision, eye pain, and loss of color perception.
Choice D reason:
This is an incorrect answer. Papilledema is a condition that causes swelling of the optic disc, which can affect peripheral vision and cause headaches. Papilledema can occur in some clients who have increased intracranial pressure (ICP) due to various causes, such as brain tumors, meningitis, or hydrocephalus, but it is not a common finding in MS.
Explanation
Choice A reason:
This is a correct answer. Fever is a common symptom of meningitis, which is an inflammation of the meninges or the membranes that cover the brain and spinal cord. Fever occurs due to the infection or immune response that causes meningitis, which can be bacterial, viral, fungal, or parasitic.
Choice B reason:
This is a correct answer. Photophobia is another common symptom of meningitis, which is an intolerance or sensitivity to light that causes eye pain or discomfort. Photophobia occurs due to the irritation of the optic nerve or cranial nerves that control the pupillary reflex by the inflamed meninges.
Choice C reason:
This is a correct answer. Nuchal rigidity is another common symptom of meningitis, which is stiffness or pain in the neck when flexing or extending it. Nuchal rigidity occurs due to the inflammation or spasm of the neck muscles by the inflamed meninges.
Choice D reason:
This is an incorrect answer. Positive Babinski sign is not a common symptom of meningitis, but rather a sign of upper motor neuron lesion or damage to the corticospinal tract that controls voluntary movement. Positive Babinski sign occurs when the big toe extends upward and the other toes fan out when stroking the sole of the foot with a blunt object.
Choice E reason:
This is a correct answer. Positive Brudzinski sign is another common symptom of meningitis, which is flexion of the hips and knees when flexing the neck forward. Positive Brudzinski sign occurs due to the irritation of the spinal nerve roots by the inflamed meninges.
Explanation
Choice A reason:
This is a correct answer. The nurse should explain to the client that GBS is an autoimmune disorder that causes inflammation and demyelination of the peripheral nerves, which can affect sensation, movement, and autonomic function. GBS occurs when the immune system mistakenly attacks the peripheral nerves, often after an infection or vaccination.
Choice B reason:
This is an incorrect answer. The nurse should not tell the client that they have GBS because their body produces antibodies against their myelin sheath. This is not the mechanism of GBS, but rather multiple sclerosis (MS), which is another autoimmune disorder that causes inflammation and demyelination of the central nervous system (CNS).
Choice C reason:
This is an incorrect answer. The nurse should not tell the client that they have GBS because they have a genetic mutation that affects their nerve function. This is not the cause of GBS, but rather Charcot-Marie-Tooth disease (CMT), which is a hereditary disorder that affects the structure and function of the peripheral nerves.
Choice D reason:
This is an incorrect answer. The nurse should not tell the client that they have GBS because they have been exposed to a virus that infects their nerve cells. This is not the cause of GBS, but rather encephalitis, which is an acute inflammatory condition of the brain that can be caused by various viruses or bacteria.
Explanation
Choice A reason:
This is an incorrect answer. Administering analgesics and antiemetics as prescribed is not an effective intervention to relieve the client's symptoms of headache, nausea, and vomiting due to meningitis. Analgesics and antiemetics can have adverse effects such as sedation, hypotension, or constipation, which can worsen the client's condition or mask signs of increased intracranial pressure (ICP). The nurse should use non-pharmacological methods to relieve the client's symptoms and monitor their vital signs and neurological status.
Choice B reason:
This is an incorrect answer. Elevating the head of the bed to 45 degrees is not an effective intervention to relieve the client's symptoms of headache, nausea, and vomiting due to meningitis. Elevating the head of the bed can increase ICP by reducing venous drainage from the brain, which can worsen the client's condition or cause complications such as herniation or hydrocephalus. The nurse should keep the head of the bed flat or slightly elevated and avoid neck flexion or rotation.
Choice C reason:
This is an incorrect answer. Applying a cold compress to the forehead is not an effective intervention to relieve the client's symptoms of headache, nausea, and vomiting due to meningitis. A cold compress can cause vasoconstriction and reduce blood flow and oxygen delivery to the brain, which can worsen the client's condition or cause ischemia or infarction. The nurse should avoid applying cold or heat to the head and maintain a normal body temperature for the client.
Choice D reason:
This is a correct answer. Dimming the lights and reducing noise in the room is an effective intervention to relieve the client's symptoms of headache, nausea, and vomiting due to meningitis. Dimming the lights and reducing noise can decrease sensory stimulation and irritation of the optic nerve or cranial nerves that control the pupillary reflex by the inflamed meninges. The nurse should also provide a quiet and calm environment for the client and limit visitors and activities.
Epilepsy: Status epilepticus
Explanation
Choice A reason:
This is an incorrect answer. Administering IV lorazepam as prescribed is an important action for the nurse to take for a client who has epilepsy and is experiencing status epilepticus, but it is not the first action. Lorazepam is a benzodiazepine that can stop or reduce seizure activity by enhancing the inhibitory effects of gamma-aminobutyric acid (GABA) in the brain. However, before administering any medication, the nurse should ensure that the client's airway and head are protected from injury or obstruction.
Choice B reason:
This is a correct answer. Protecting the client's airway and head is the first action that the nurse should take for a client who has epilepsy and is experiencing status epilepticus. Status epilepticus is a medical emergency that occurs when a seizure lasts longer than 5 minutes or when two or more seizures occur without recovery of consciousness in between. Status epilepticus can cause hypoxia, brain damage, or death if not treated promptly. The nurse should protect the client's airway and head by placing them in a side-lying position, removing any objects or clothing that may restrict breathing, inserting an oral airway if needed, and padding the side rails or bed to prevent injury.
Choice C reason:
This is an incorrect answer. Monitoring the client's vital signs and oxygen saturation is an important action for the nurse to take for a client who has epilepsy and is experiencing status epilepticus, but it is not the first action. Vital signs and oxygen saturation can indicate the severity and effects of seizure activity on the client's cardiovascular, respiratory, and neurological systems. The nurse should monitor these parameters closely and provide oxygen therapy if needed to maintain adequate oxygenation and perfusion of the brain. However, before monitoring any parameters, the nurse should ensure that the client's airway and head are protected from injury or obstruction.
Choice D reason:
This is an incorrect answer. Documenting the onset, duration, and characteristics of the seizure is an important action for the nurse to take for a client who has epilepsy and is experiencing status epilepticus, but it is not the first action. Documentation can provide valuable information for diagnosis, treatment, and evaluation of seizure activity and its effects on the client's condition and quality of life. The nurse should document these details accurately and objectively as soon as possible after the seizure ends. However, before documenting any details, the nurse should ensure that the client's airway and head are protected from injury or obstruction.
Explanation
Choice A reason:
This is a correct answer. The nurse should advise the client and their caregiver to avoid triggers such as stress, fatigue, or flashing lights that may provoke seizure activity by altering brain electrical activity or neurotransmitter levels. The nurse should also educate them about other potential triggers such as alcohol, caffeine, nicotine, fever, infection, hormonal changes, or certain medications.
Choice B reason:
This is a correct answer. The nurse should advise the client and their caregiver to follow a ketogenic diet that is high in fat and low in carbohydrates under medical supervision if pharmacological therapy is ineffective or intolerable. A ketogenic diet can reduce seizure frequency and severity by inducing ketosis, which is a metabolic state where ketone bodies are used as an alternative fuel source for the brain instead of glucose.
Choice C reason:
This is a correct answer. The nurse should advise the client and their caregiver to wear a medical alert bracelet or necklace that identifies epilepsy and provides emergency contact information. This can help ensure prompt and appropriate care in case of a seizure and prevent unnecessary interventions or complications.
Choice D reason:
This is an incorrect answer. The nurse should not advise the client and their caregiver to use herbal remedies such as valerian or chamomile to reduce anxiety, as this can have negative effects on seizure activity and medication effectiveness. Herbal remedies can interact with antiepileptic drugs (AEDs) and alter their absorption, metabolism, or excretion, which can increase the risk of toxicity or breakthrough seizures. The nurse should advise the client and their caregiver to consult their provider before using any herbal remedies or supplements.
Choice E reason:
This is a correct answer. The nurse should advise the client and their caregiver to perform relaxation techniques such as deep breathing or meditation, as this can help prevent seizures by reducing stress, anxiety, or tension that may trigger seizure activity. Relaxation techniques can also improve mood, sleep quality, and coping skills for the client and their caregiver.
Explanation
Choice A reason:
This is an incorrect answer. The nurse should not tell the client that phenytoin can cause drowsiness, dizziness, nausea, or rash. These are not the common or serious side effects of phenytoin, but rather other antiepileptic drugs (AEDs) such as carbamazepine or valproic acid.
Choice B reason:
This is an incorrect answer. The nurse should not tell the client that phenytoin can cause weight gain, hair loss, tremors, or mood swings. These are not the common or serious side effects of phenytoin, but rather other AEDs such as valproic acid or lamotrigine.
Choice C reason:
This is an incorrect answer. The nurse should not tell the client that phenytoin can cause blurred vision, dry mouth, constipation, or urinary retention. These are not the common or serious side effects of phenytoin, but rather other AEDs such as gabapentin or topiramate.
Choice D reason:
This is a correct answer. The nurse should tell the client that phenytoin can cause gingival hyperplasia, nystagmus, ataxia, or dysrhythmias. These are the common or serious side effects of phenytoin that can affect the oral health, vision, balance, or cardiac function of the client. The nurse should also educate the client about the signs and symptoms of these side effects and how to prevent or manage them.
Explanation
Choice A reason:
This is an incorrect answer. The nurse should not monitor for hypotension during plasmapheresis for a client who has GBS. Hypotension is not a common complication of plasmapheresis, but rather hemodialysis or peritoneal dialysis, which are procedures that remove excess fluid and waste products from the blood in clients who have kidney failure.
Choice B reason:
This is an incorrect answer. The nurse should not monitor for hyperkalemia during plasmapheresis for a client who has GBS. Hyperkalemia is not a common complication of plasmapheresis, but rather hemodialysis or peritoneal dialysis, which can cause a rapid shift of potassium from the cells to the blood in clients who have kidney failure.
Choice C reason:
This is a correct answer. The nurse should monitor for hypocalcemia during plasmapheresis for a client who has GBS. Hypocalcemia is a common complication of plasmapheresis that occurs when calcium is removed from the blood along with plasma proteins and antibodies. Hypocalcemia can cause muscle cramps, tetany, paresthesia, seizures, or cardiac arrhythmias.
Choice D reason:
This is an incorrect answer. The nurse should not monitor for hyperglycemia during plasmapheresis for a client who has GBS. Hyperglycemia is not a common complication of plasmapheresis, but rather insulin therapy or steroid therapy, which can increase blood glucose levels in clients who have diabetes mellitus or other endocrine disorders.
Brain Tumors: Gliomas, Meningiomas, Metastatic brain tumors
Explanation
Choice A reason:
Meningeal cells are not the origin of gliomas, but of meningiomas, which are benign brain tumors that develop from the meninges, the membranes that cover the brain and spinal cord.
Choice B reason:
Neuroglial cells are the origin of gliomas, as explained above.
Choice C reason:
Pituitary cells are not the origin of gliomas, but of pituitary adenomas, which are benign brain tumors that grow from the pituitary gland and may cause endocrine dysfunction.
Choice D reason:
Acoustic nerve cells are not the origin of gliomas, but of acoustic neuromas, which are benign brain tumors that arise from the acoustic cranial nerve and may cause hearing loss or ringing in the ears.
Explanation
Choice A reason:
This statement is true. Metastatic brain tumors are lesions that spread from a primary cancer site outside of the body, such as breast, kidney, lung, or gastrointestinal tract cancers.
Choice B reason:
This statement is true. Metastatic brain tumors are more common than primary brain tumors, accounting for about half of all brain tumors.
Choice C reason:
This statement is true. Metastatic brain tumors can be treated with surgery, radiation therapy, or chemotherapy, depending on the location, size, number, and type of tumor.
Choice D reason:
This statement is false. Metastatic brain tumors usually have a worse prognosis than primary brain tumors, because they indicate a systemic disease and often recur after treatment.
Choice E reason:
This statement is true. Metastatic brain tumors can cause increased intracranial pressure and neurological deficits by applying pressure to surrounding brain tissue and impairing cerebral blood flow and cerebrospinal fluid drainage.
Explanation
Choice A reason:
This statement is not indicative of a meningioma, but of a pituitary adenoma, which is a benign brain tumor that grows from the pituitary gland and may cause endocrine dysfunction such as diabetes insipidus (excessive thirst and urination).
Choice B reason:
This statement is not indicative of a meningioma, but of an acoustic neuroma, which is a benign brain tumor that arises from the acoustic cranial nerve and may cause hearing loss or ringing in the ears.
Choice C reason:
This statement is indicative of a meningioma, as explained above.
Choice D reason:
This statement is not indicative of a meningioma, but of a supratentorial tumor, which occurs in the cerebral hemispheres above the tentorium cerebelli and may cause loss of voluntary movement or hemiparesis (weakness or numbness on one side of the body).
Explanation
Choice A reason:
This statement is true, as explained above.
Choice B reason:
This statement is not specific to the surgery, but to the brain tumor itself. Brain tumors can cause seizures, memory loss, or changes in personality by affecting the function of different areas of the brain.
Choice C reason:
This statement is not specific to the surgery, but to the increased intracranial pressure caused by the brain tumor. Increased intracranial pressure can cause nausea, vomiting, or difficulty swallowing by compressing the brainstem and affecting the autonomic nervous system.
Choice D reason:
This statement is not specific to the surgery, but to the location of the brain tumor. Brain tumors that involve the cranial nerves can cause hearing loss, vision loss, or facial paralysis by impairing their function.
Explanation
Choice A reason:
This statement is true, as explained above.
Choice B reason:
This statement is not an adverse effect of chemotherapy, but of the brain tumor itself. Brain tumors can cause cerebral edema by applying pressure to surrounding brain tissue and impairing cerebral blood flow and cerebrospinal fluid drainage.
Choice C reason:
This statement is not an adverse effect of chemotherapy, but of the brain tumor itself. Brain tumors can cause increased intracranial pressure by applying pressure to surrounding brain tissue and impairing cerebral blood flow and cerebrospinal fluid drainage.
Choice D reason:
This statement is not an adverse effect of chemotherapy, but of the brain tumor itself. Brain tumors can cause seizures by affecting the function of different areas of the brain and disrupting the electrical activity of neurons.
Explanation
Choice A reason:
This statement is not correct. Gliomas are malignant brain tumors that arise from neuroglial tissue and may cause various neurological deficits depending on their location and size, but they do not typically affect vision or reading ability.
Choice B reason:
This statement is not correct. Meningiomas are benign brain tumors that develop from the meninges and may cause severe headaches that are worse in the morning, seizures, or cranial nerve dysfunction, but they do not typically affect vision or reading ability.
Choice C reason:
This statement is correct, as explained above.
Choice D reason:
This statement is not correct. Acoustic neuromas are benign brain tumors that arise from the acoustic cranial nerve and may cause hearing loss or ringing in the ears, vertigo, facial drooping, or difficulty swallowing, but they do not typically affect vision or reading ability.
Explanation
Choice A reason:
This statement is true. Ataxia is a lack of coordination of voluntary movements that can affect the gait, balance, speech, or eye movements. It is caused by damage to the cerebellum, which is responsible for coordinating muscle activity and maintaining posture and equilibrium.
Choice B reason:
This statement is true. Nystagmus is a rapid involuntary movement of the eyes that can be horizontal, vertical, or rotary. It is caused by damage to the cerebellum or the vestibular system, which regulates the sense of balance and spatial orientation.
Choice C reason:
This statement is true. Dysphagia is difficulty swallowing that can affect the oral, pharyngeal, or esophageal stages of swallowing. It is caused by damage to the cerebellum or the brainstem, which control the muscles involved in swallowing.
Choice D reason:
This statement is false. Aphasia is a loss or impairment of language function that can affect the expression, comprehension, reading, or writing of speech. It is caused by damage to the cerebral cortex, especially the left hemisphere, which is responsible for language processing.
Choice E reason:
This statement is false. Hemiparesis is weakness or paralysis of one side of the body that can affect the face, arm, or leg. It is caused by damage to the cerebral cortex or the corticospinal tract, which control voluntary movement.
Explanation
Choice A reason:
This statement is true. New onset of seizures is a sign of radiation necrosis, which is a delayed complication of radiation therapy that occurs when normal brain tissue dies due to radiation exposure. Radiation necrosis can cause neurological deficits such as seizures by affecting the function of different areas of the brain and disrupting the electrical activity of neurons.
Choice B reason:
This statement is true. Increased intracranial pressure is a sign of radiation necrosis, which is a delayed complication of radiation therapy that occurs when normal brain tissue dies due to radiation exposure. Radiation necrosis can cause increased intracranial pressure by applying pressure to surrounding brain tissue and impairing cerebral blood flow and cerebrospinal fluid drainage.
Choice C reason:
This statement is false. Hair loss at the radiation site is not a sign of radiation necrosis, but a common side effect of radiation therapy that occurs when hair follicles are damaged by radiation exposure. Hair loss at the radiation site is usually temporary and reversible.
Choice D reason:
This statement is true. Cognitive impairment is a sign of radiation necrosis, which is a delayed complication of radiation therapy that occurs when normal brain tissue dies due to radiation exposure. Radiation necrosis can cause cognitive impairment such as memory loss, confusion, or dementia by affecting the function of different areas of the brain and disrupting the cognitive processes.
Choice E reason:
This statement is false. Skin erythema at the radiation site is not a sign of radiation necrosis, but a common side effect of radiation therapy that occurs when skin cells are damaged by radiation exposure. Skin erythema at the radiation site is usually mild and self-limiting.
More Questions on Pathophysiology of the Nervous System
Explanation
Choice A reason:
This is a correct statement, as the CNS receives sensory information from various receptors in the body and interprets it.
Choice B reason:
This is a correct statement, as the CNS initiates and coordinates motor commands to control voluntary and involuntary movements.
Choice C reason:
This is a correct statement, as the CNS is involved in higher cognitive functions such as memory, learning, reasoning, and emotions.
Choice D reason:
This is an incorrect statement, as this is the function of the PNS. The PNS consists of cranial and spinal nerves that connect the CNS to the rest of the body and transmit sensory and motor signals.
Explanation
Choice A reason:
This is a correct answer, as bladder control is regulated by nerves that originate from the sacral region of the spinal cord, which is below T6.
Choice B reason:
This is an incorrect answer, as respiratory rate is regulated by nerves that originate from the cervical and thoracic regions of the spinal cord, which are above T6.
Choice C reason:
This is a correct answer, as heart rate is regulated by nerves that originate from the thoracic and lumbar regions of the spinal cord, which are below T6.
Choice D reason:
This is an incorrect answer, as arm movement is regulated by nerves that originate from the cervical region of the spinal cord, which is above T6.
Choice E reason:
This is a correct answer, as leg movement is regulated by nerves that originate from the lumbar and sacral regions of the spinal cord, which are below T6.
Explanation
Choice A reason:
This is an incorrect answer, as seizures do not occur due to too much stimulation in brain cells, but rather due to abnormal electrical activity caused by neurotransmitter imbalance.
Choice B reason:
This is a correct answer, as seizures occur due to neurotransmitter imbalance, which disrupts communication between neurons and causes abnormal electrical activity in the brain.
Choice C reason:
This is an incorrect answer, as seizures do not occur due to lack of oxygen in brain tissue, but rather due to abnormal electrical activity caused by neurotransmitter imbalance.
Choice D reason:
This is an incorrect answer, as seizures do not occur due to infection in brain tissue, but rather due to abnormal electrical activity caused by neurotransmitter imbalance.
Explanation
Choice A reason:
This is a correct answer, as the medication increases dopamine levels in the brain, which helps to improve the symptoms of Parkinson's disease, such as tremors, rigidity, and bradykinesia.
Choice B reason:
This is an incorrect answer, as the medication does not decrease acetylcholine levels in the brain, but rather increases dopamine levels. Acetylcholine is another neurotransmitter that controls muscle contraction, learning, and memory.
Choice C reason:
This is an incorrect answer, as the medication does not increase serotonin levels in the brain, but rather increases dopamine levels. Serotonin is another neurotransmitter that controls mood, sleep, and appetite.
Choice D reason:
This is an incorrect answer, as the medication does not decrease glutamate levels in the brain, but rather increases dopamine levels. Glutamate is another neurotransmitter that controls excitatory signals in the brain.
Explanation
Choice A reason:
This is a correct statement, as the PNS consists of cranial and spinal nerves that connect the CNS to the rest of the body and transmit sensory and motor signals.
Choice B reason:
This is a correct statement, as the PNS is divided into two subdivisions: the somatic nervous system (SNS) and the autonomic nervous system (ANS).
Choice C reason:
This is a correct statement, as the PNS controls voluntary movements of skeletal muscles and provides sensory feedback from the skin, joints, and muscles through the SNS.
Choice D reason:
This is an incorrect statement, as this is the function of the ANS, which is a subdivision of the PNS. The ANS regulates involuntary functions of smooth muscles, cardiac muscles, and glands through its two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS).
Explanation
Choice A reason:
This is an incorrect answer, as MS is not caused by an autoimmune attack on nerve cells, but rather on nerve coverings called myelin sheaths.
Choice B reason:
This is an incorrect answer, as MS is not caused by a degeneration of nerve fibers, but rather by an inflammation of nerve coverings called myelin sheaths.
Choice C reason:
This is a correct answer, as MS is caused by an inflammation of nerve coverings called myelin sheaths, which impair transmission of nerve impulses.
Choice D reason:
This is an incorrect answer, as MS is not caused by a compression of nerve roots, but rather by an inflammation of nerve coverings called myelin sheaths.
Explanation
Choice A reason:
This is the correct answer because peripheral neuropathy affects the sensory nerves, which can cause loss of sensation, especially in the distal parts of the body. Diabetes mellitus is a common cause of peripheral neuropathy.
Choice B reason:
This is incorrect because peripheral neuropathy does not affect the motor nerves, which control muscle tone and reflexes. Increased muscle tone and reflexes in the upper limbs are more likely to indicate a central nervous system disorder, such as a stroke or spinal cord injury.
Choice C reason:
This is incorrect because peripheral neuropathy can cause decreased pain perception in any part of the body, not just the hands and fingers. However, this is not a specific finding for peripheral neuropathy, as other conditions can also impair pain perception, such as spinal cord injury or opioid use.
Choice D reason:
This is incorrect because peripheral neuropathy does not affect the autonomic nerves, which control sweating and flushing. Increased sweating and flushing in the face and neck are more likely to indicate a sympathetic nervous system disorder, such as pheochromocytoma or carcinoid syndrome.
Explanation
Choice A reason:
This is correct because bending forward at the waist can increase the pressure on the spinal discs and nerve roots, which can worsen radiculopathy symptoms.
Choice B reason:
This is correct because lifting heavy objects can also increase the pressure on the spinal discs and nerve roots, as well as strain the back muscles and ligaments, which can worsen radiculopathy symptoms.
Choice C reason:
This is correct because sitting for prolonged periods can reduce blood flow to the spinal discs and nerve roots, which can impair healing and worsen radiculopathy symptoms.
Choice D reason:
This is incorrect because swimming or water aerobics can be beneficial for clients with radiculopathy, as they can reduce stress on the spine, improve flexibility and strength, and relieve pain.
Choice E reason:
This is incorrect because walking or jogging can also be beneficial for clients with radiculopathy, as they can improve blood flow to the spine, enhance mood and well-being, and prevent deconditioning.
Explanation
Choice A reason:
This is the correct answer because Spurling's test is used to diagnose cervical radiculopathy by reproducing radicular pain with neck extension, lateral flexion, and compression. A positive result indicates nerve root compression by a herniated disc, osteophyte, or other lesion.
Choice B reason:
This is incorrect because straight leg raise test is used to diagnose lumbar radiculopathy by reproducing radicular pain with hip flexion and knee extension. A positive result indicates nerve root compression by a herniated disc or other lesion in the lower back.
Choice C reason:
This is incorrect because Tinel's sign is used to diagnose peripheral neuropathy by reproducing tingling or paresthesia with tapping over a damaged nerve. A positive result indicates nerve regeneration or irritation by a scar, tumor, or other lesion.
Choice D reason:
This is incorrect because Phalen's test is used to diagnose carpal tunnel syndrome by reproducing numbness or tingling in the median nerve distribution with wrist flexion for 60 seconds. A positive result indicates median nerve compression by a thickened flexor retinaculum or other lesion in the wrist.
Explanation
Choice A reason:
This is the correct answer because epidural steroid injections are used to treat radiculopathy by reducing inflammation and edema of the nerve root, which can relieve radicular pain and improve neurological function.
Choice B reason:
This is incorrect because local anesthetic alone can provide temporary pain relief by blocking nerve conduction, but it does not address the underlying cause of radiculopathy, which is nerve root compression.
Choice C reason:
This is incorrect because steroid and local anesthetic do not have any effect on the size or shape of the disc or bone spur that is compressing the nerve root. They only reduce inflammation and pain.
Choice D reason:
This is incorrect because although epidural injections may have fewer systemic side effects than oral or intravenous medications, they still have some risks and complications, such as infection, bleeding, nerve damage, or spinal headache.
Explanation
Choice A reason:
This is incorrect because wearing tight-fitting shoes can cause pressure ulcers, blisters, or infections in clients with peripheral neuropathy, who have reduced sensation and blood flow in their feet. The nurse should advise the client to wear well-fitting shoes with cushioned socks and avoid walking barefoot.
Choice B reason:
This is incorrect because using a heating pad can cause burns or skin damage in clients with peripheral neuropathy, who have impaired temperature perception and pain sensation in their affected areas. The nurse should advise the client to avoid exposure to extreme heat or cold and use other methods to relieve pain, such as medications, massage, or acupuncture.
Choice C reason:
This is the correct answer because inspecting the skin daily for cuts, blisters, or ulcers can help prevent infection and complications in clients with peripheral neuropathy, who have reduced sensation and healing ability in their affected areas. The nurse should advise the client to wash their skin with mild soap and water, apply moisturizer, and report any signs of infection to their provider.
Choice D reason:
This is incorrect because taking vitamin B supplements can help prevent or treat peripheral neuropathy caused by vitamin B deficiency, which can occur in clients who receive chemotherapy. The nurse should advise the client to consult with their provider before taking any supplements and follow a balanced diet that includes foods rich in vitamin B, such as meat, eggs, dairy products, and fortified cereals.
Explanation
Choice A reason:
This is incorrect because biceps brachii is innervated by C5-C6 nerve roots, which are not affected by a herniated disc at C6-C7 level.
Choice B reason:
This is the correct answer because triceps brachii is innervated by C6-C8 nerve roots, which are affected by a herniated disc at C6-C7 level.
Choice C reason:
This is incorrect because deltoid is innervated by C5-C6 nerve roots, which are not affected by a herniated disc at C6-C7 level.
Choice D reason:
This is incorrect because trapezius is innervated by cranial nerve XI (spinal accessory nerve), which is not affected by a herniated disc at C6-C7 level.
Explanation
Choice A reason:
This is the correct answer because trimming the toenails straight across and filing the edges can prevent ingrown toenails, which can cause infection and complications in clients with peripheral neuropathy.
Choice B reason:
This is incorrect because soaking the feet in warm water for 15 minutes every day can cause maceration, which can increase the risk of skin breakdown and infection in clients with peripheral neuropathy.
Choice C reason:
This is incorrect because wearing cotton socks and changing them when they are damp can cause friction and moisture, which can also increase the risk of skin breakdown and infection in clients with peripheral neuropathy.
Choice D reason:
This is incorrect because applying lotion between the toes can cause fungal growth, which can lead to athlete's foot or other infections in clients with peripheral neuropathy.
Explanation
Choice A reason:
This is the correct answer because atherosclerosis is the main cause of ischemic stroke, as it leads to the formation of plaques that narrow the cerebral arteries and reduce blood flow to the brain.
Choice B reason:
This is incorrect because atrial fibrillation is a risk factor for ischemic stroke, but not the most common cause. Atrial fibrillation can cause embolic stroke, which occurs when a blood clot from the heart travels to the brain and blocks a cerebral artery.
Choice C reason:
This is incorrect because cerebral aneurysm is a cause of hemorrhagic stroke, not ischemic stroke. Cerebral aneurysm is a weak spot in a cerebral artery that can rupture and bleed into the brain.
Choice D reason:
This is incorrect because arteriovenous malformation is also a cause of hemorrhagic stroke, not ischemic stroke. Arteriovenous malformation is a congenital abnormality of the blood vessels in the brain that can leak or burst and cause bleeding.
A nurse is caring for a client who has ischemic stroke and is receiving thrombolytic therapy with recombinant tissue plasminogen activator (rtPA). Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A reason:
This is correct because monitoring the client's vital signs and neurological status frequently can help detect any changes in the client's condition, such as improvement or deterioration of symptoms, or complications such as bleeding or increased intracranial pressure.
Choice B reason:
This is correct because administering rtPA within 4.5 hours of symptom onset can increase the chances of restoring blood flow to the ischemic brain tissue and reducing neurological damage. The effectiveness and safety of rtPA decrease after this time window.
Choice C reason:
This is correct because maintaining the client's systolic blood pressure below 180 mm Hg can prevent further ischemia or hemorrhage in the brain. High blood pressure can increase the risk of bleeding or reperfusion injury after thrombolytic therapy.
Choice D reason:
This is incorrect because giving aspirin or other antiplatelet agents along with rtPA can increase the risk of bleeding or hemorrhagic transformation. Antiplatelet agents should be avoided for at least 24 hours after thrombolytic therapy.
Choice E reason:
This is correct because assessing the client for signs of bleeding or hemorrhagic transformation can help identify any adverse effects of thrombolytic therapy. Bleeding or hemorrhagic transformation can manifest as hematuria, hematemesis, melena, petechiae, ecchymosis, epistaxis, gingival bleeding, headache, altered mental status, or worsening neurological deficits.
A nurse is performing a neurological assessment on a client who has ischemic stroke affecting the left cerebral hemisphere. The nurse asks the client to name an object that the nurse points to, but the client does not respond verbally. The nurse interprets this as a sign of which of the following types of aphasia?
Explanation
Choice A reason:
This is incorrect because expressive aphasia is a type of aphasia that affects the ability to produce speech, but not to comprehend it. A client with expressive aphasia would be able to respond verbally, but with difficulty or errors.
Choice B reason:
This is the correct answer because receptive aphasia is a type of aphasia that affects the ability to comprehend speech, but not to produce it. A client with receptive aphasia would not be able to respond verbally, as they do not understand what is being asked.
Choice C reason:
This is incorrect because global aphasia is a type of aphasia that affects both the ability to produce and comprehend speech. A client with global aphasia would not be able to respond verbally or nonverbally, as they have no language function.
Choice D reason:
This is incorrect because anomic aphasia is a type of aphasia that affects the ability to recall specific words or names, but not the general ability to produce or comprehend speech. A client with anomic aphasia would be able to respond verbally, but with pauses or substitutions.
A nurse is planning care for a client who has ischemic stroke and is at risk for cerebral edema. Which of the following interventions should the nurse include in the plan?
Explanation
Choice A reason:
This is correct because elevating the head of the bed to 30 degrees can help reduce intracranial pressure by facilitating venous drainage and decreasing cerebral blood volume.
Choice B reason:
This is correct because administering mannitol as prescribed can help reduce intracranial pressure by creating an osmotic gradient that draws fluid out of the brain tissue and into the bloodstream.
Choice C reason:
This is correct because monitoring the client's intracranial pressure can help detect any signs of increased intracranial pressure or cerebral herniation, which can be life-threatening complications of cerebral edema.
Choice D reason:
This is correct because all of the above interventions are appropriate for a client who has ischemic stroke and is at risk for cerebral edema.
A nurse is evaluating the outcomes of a client who has ischemic stroke and has received rehabilitation. Which of the following statements by the client indicates an improvement in functional recovery?
Explanation
Choice A reason:
This is correct because improved movement of the arm and leg on the affected side indicates an improvement in motor function, which can be impaired by ischemic stroke.
Choice B reason:
This is correct because improved speech and comprehension indicate an improvement in language function, which can be impaired by ischemic stroke, especially if it affects the dominant hemisphere.
Choice C reason:
This is correct because improved swallowing indicates an improvement in cranial nerve function, which can be impaired by ischemic stroke, especially if it affects the brainstem.
Choice D reason:
This is correct because all of the above statements indicate an improvement in functional recovery, which is the goal of rehabilitation for clients who have ischemic stroke.
A nurse is educating a client who has a history of ischemic stroke about modifiable risk factors. Which of the following risk factors should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A reason:
This is correct because hypertension is a modifiable risk factor for ischemic stroke, as it increases the stress on the arterial walls and accelerates atherosclerosis, which can lead to plaque formation and reduced blood flow to the brain.
Choice B reason:
This is correct because smoking is a modifiable risk factor for ischemic stroke, as it damages the endothelial lining of the arteries and promotes thrombosis, which can lead to clot formation and blockage of blood flow to the brain.
Choice C reason:
This is correct because diabetes mellitus is a modifiable risk factor for ischemic stroke, as it causes hyperglycemia and dyslipidemia, which can damage the blood vessels and increase the risk of atherosclerosis and thrombosis.
Choice D reason:
This is incorrect because age is a non-modifiable risk factor for ischemic stroke, as it cannot be changed or controlled by the client. The risk of ischemic stroke increases with age due to physiological changes in the blood vessels and other organs.
Choice E reason:
This is incorrect because family history is also a non-modifiable risk factor for ischemic stroke, as it cannot be changed or controlled by the client. The risk of ischemic stroke may be higher in clients who have relatives who had a stroke due to genetic or environmental factors.
Exams on Pathophysiology of the Nervous System
Stroke: Ischemic stroke, Hemorrhagic stroke, Transient ischemic attack (TIA)
Review Practice Mode Take ExamPeripheral Nervous System Disorders: Peripheral neuropathy; Radiculopathy; Charcot-Marie-Tooth disease
Review Practice Mode Take ExamCustom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction
- Traumatic Brain Injury: Concussions,
- Stroke: Ischemic stroke, Hemorrhagic stroke, Transient ischemic attack (TIA)
- Peripheral Nervous System Disorders: Peripheral neuropathy; Radiculopathy; Charcot-Marie-Tooth disease
- Neurodegenerative Diseases: Alzheimer's disease, Parkinson's disease
- Neuroinflammation: Multiple sclerosis; Meningitis; Guillain-Barré syndrome
- Epilepsy: Status epilepticus
- Brain Tumors: Gliomas, Meningiomas, Metastatic brain tumors
- Summary
- More Questions on Pathophysiology of the Nervous System
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define the structure and function of the central and peripheral nervous systems
- Describe the types and causes of traumatic brain injury
- Explain the pathophysiology, manifestations, diagnosis, and treatment of concussions
- Compare and contrast ischemic stroke, hemorrhagic stroke, and transient ischemic attack
- Identify the risk factors, prevention strategies, and nursing interventions for stroke
- Discuss the common disorders of the peripheral nervous system
- Analyze the etiology, symptoms, diagnosis, and management of peripheral neuropathy, radiculopathy, and Charcot-Marie-Tooth disease
- Define and describe the structure and function of the nervous system
- Identify and explain the causes, risk factors, signs and symptoms, diagnosis, treatment, and prevention of neurodegenerative diseases: Alzheimer’s disease and Parkinson’s disease
- Identify and explain the causes, risk factors, signs and symptoms, diagnosis, treatment, and prevention of neuroinflammation: Multiple sclerosis, Meningitis, and Guillain-Barré syndrome
- Identify and explain the causes, risk factors, signs and symptoms, diagnosis, treatment, and prevention of epilepsy and seizure disorders: Epileptic seizures and Status epilepticus
- Compare and contrast the different types of neurodegenerative diseases, neuroinflammation, and epilepsy and seizure disorders
- Apply the nursing process to provide holistic care for patients with neurological disorders
- Define status epilepticus and its types
- Identify the causes and risk factors of status epilepticus
- Explain the pathophysiology and clinical manifestations of status epilepticus
- Describe the diagnosis and treatment of status epilepticus
- Discuss the nursing care and management of patients with status epilepticus
- Recognize the complications and outcomes of status epilepticus
- Define glioma and its types, causes, risk factors, symptoms, diagnosis, and treatment.
- Explain the role of glial cells and their abnormal growth in glioma formation.
- Compare and contrast the different types of gliomas based on their origin, grade, location, and prognosis.
- Identify the common complications and challenges of managing gliomas, such as seizures, cognitive impairment, and recurrence.
- Apply the nursing process to plan and provide holistic care for patients with gliomas and their families.
- Evaluate the effectiveness of various interventions and therapies for gliomas, such as surgery, radiation, chemotherapy, and targeted drugs.
- Define the term meningioma and describe its characteristics and subtypes.
- Explain the possible causes and risk factors for developing meningiomas.
- Identify the signs and symptoms of meningiomas based on their location and grade.
- Discuss the diagnostic tests and procedures used to confirm and classify meningiomas.
- Compare the treatment options and nursing interventions for meningiomas, including surgery, radiation therapy, and pharmacological management.
- Evaluate the potential complications and outcomes of meningiomas, such as recurrence, neurological deficits, and quality of life issues.
- Define brain tumors and metastatic brain tumors
- Identify the common types and causes of brain tumors and metastatic brain tumors
- Describe the signs and symptoms of brain tumors and metastatic brain tumors
- Explain the diagnostic tests and procedures for brain tumors and metastatic brain tumors
- Discuss the treatment options and nursing interventions for brain tumors and metastatic brain tumors
- Evaluate the complications and prognosis of brain tumors and metastatic brain tumors
- The nervous system is composed of two main divisions: the central nervous system (CNS) and the peripheral nervous system (PNS)
- The CNS consists of the brain and spinal cord, which are responsible for processing sensory information, generating motor commands, and regulating cognitive and emotional functions
- The PNS consists of the cranial and spinal nerves, which connect the CNS to the rest of the body and transmit sensory and motor signals
- The PNS is further divided into two subdivisions: the somatic nervous system (SNS) and the autonomic nervous system (ANS)
- The SNS controls voluntary movements of skeletal muscles and provides sensory feedback from the skin, joints, and muscles
- The ANS regulates involuntary functions of smooth muscles, cardiac muscles, and glands. It has two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS)
- The SNS prepares the body for stress or emergency situations by increasing heart rate, blood pressure, respiratory rate, and blood glucose levels. It also dilates the pupils, bronchi, and blood vessels to skeletal muscles
- The PNS restores the body to a state of rest and relaxation by decreasing heart rate, blood pressure, respiratory rate, and blood glucose levels. It also constricts the pupils, bronchi, and blood vessels to skeletal muscles
- The nervous system is composed of two main divisions: the central nervous system (CNS) and the peripheral nervous system (PNS)
- The CNS consists of the brain and spinal cord, which are responsible for processing sensory information, generating motor commands, regulating autonomic functions, and performing higher cognitive functions
- The PNS consists of the cranial nerves, spinal nerves, and peripheral nerves, which connect the CNS to the rest of the body and transmit sensory and motor signals
- The nervous system is composed of two types of cells: neurons and glial cells
- Neurons are specialized cells that generate and conduct electrical impulses along their axons
- Glial cells are supportive cells that provide insulation, nutrition, protection, and repair for neurons
- The nervous system is vulnerable to various diseases and disorders that can affect its structure or function
- Neurological disorders can be classified into four main categories: neurodegenerative diseases, neuroinflammation, epilepsy and seizure disorders, and others (such as trauma, stroke, tumors, infections, etc.)
- Neurological disorders can have significant impacts on the physical, mental, emotional, social, and occupational aspects of a patient’s life
- Nursing care for patients with neurological disorders requires a comprehensive assessment, diagnosis, planning, implementation, and evaluation of interventions that address the patient’s needs and goals
- The nervous system is composed of two types of cells: neurons and glia
- Neurons are specialized cells that transmit electrical impulses and chemical signals
- Glia are supportive cells that provide insulation, protection, nutrition, and regulation for neurons
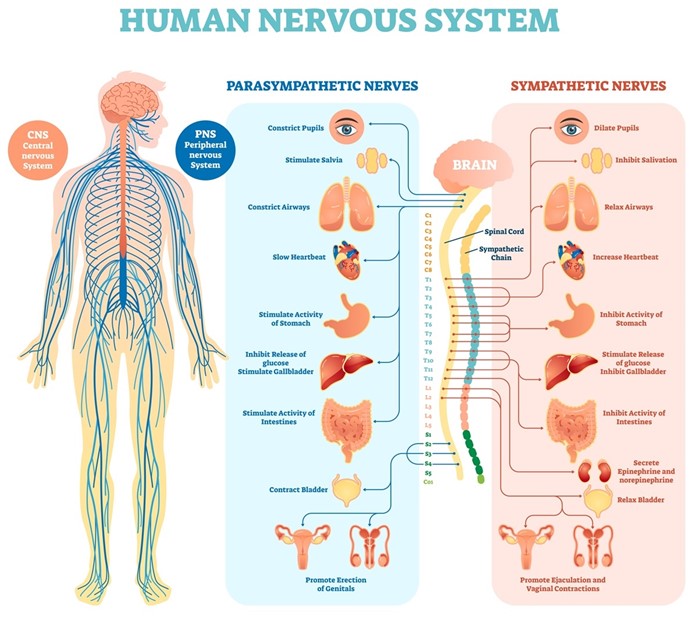
Introduction
- The nervous system is composed of two main divisions: the central nervous system (CNS) and the peripheral nervous system (PNS)
- The CNS consists of the brain and spinal cord, which are responsible for processing sensory information, generating motor commands, and regulating cognitive and emotional functions
- The PNS consists of the cranial and spinal nerves, which connect the CNS to the rest of the body and transmit sensory and motor signals
- The PNS is further divided into two subdivisions: the somatic nervous system (SNS) and the autonomic nervous system (ANS)
- The SNS controls voluntary movements of skeletal muscles and provides sensory feedback from the skin, joints, and muscles
- The ANS regulates involuntary functions of smooth muscles, cardiac muscles, and glands. It has two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS)
- The SNS prepares the body for stress or emergency situations by increasing heart rate, blood pressure, respiratory rate, and blood glucose levels. It also dilates the pupils, bronchi, and blood vessels to skeletal muscles
- The PNS restores the body to a state of rest and relaxation by decreasing heart rate, blood pressure, respiratory rate, and blood glucose levels. It also constricts the pupils, bronchi, and blood vessels to skeletal muscles
- The nervous system is composed of two main divisions: the central nervous system (CNS) and the peripheral nervous system (PNS)
- The CNS consists of the brain and spinal cord, which are responsible for processing sensory information, generating motor commands, regulating autonomic functions, and performing higher cognitive functions
- The PNS consists of the cranial nerves, spinal nerves, and peripheral nerves, which connect the CNS to the rest of the body and transmit sensory and motor signals
- The nervous system is composed of two types of cells: neurons and glial cells
- Neurons are specialized cells that generate and conduct electrical impulses along their axons
- Glial cells are supportive cells that provide insulation, nutrition, protection, and repair for neurons
- The nervous system is vulnerable to various diseases and disorders that can affect its structure or function
- Neurological disorders can be classified into four main categories: neurodegenerative diseases, neuroinflammation, epilepsy and seizure disorders, and others (such as trauma, stroke, tumors, infections, etc.)
- Neurological disorders can have significant impacts on the physical, mental, emotional, social, and occupational aspects of a patient’s life
- Nursing care for patients with neurological disorders requires a comprehensive assessment, diagnosis, planning, implementation, and evaluation of interventions that address the patient’s needs and goals
- The nervous system is composed of two types of cells: neurons and glia
- Neurons are specialized cells that transmit electrical impulses and chemical signals
- Glia are supportive cells that provide insulation, protection, nutrition, and regulation for neurons
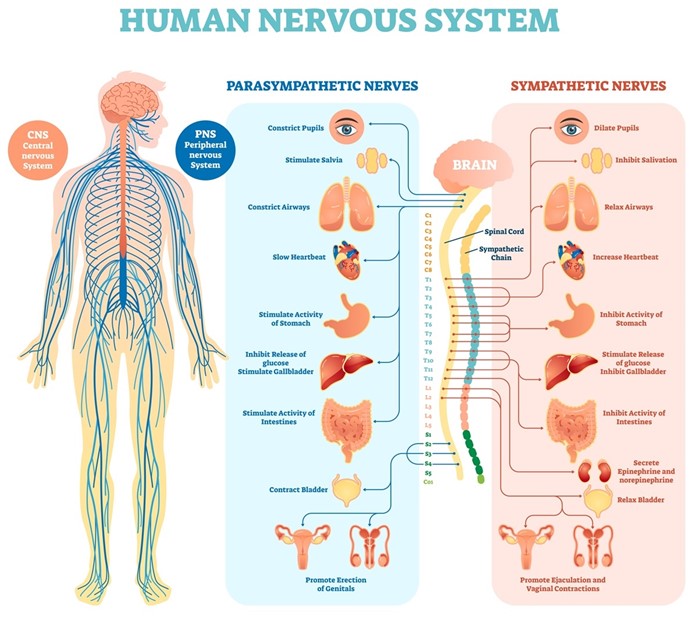
Traumatic Brain Injury: Concussions,
- Traumatic brain injury (TBI) is defined as an alteration in brain function or other evidence of brain pathology caused by an external force3. TBI can result from a direct impact to the head (such as a fall, assault, motor vehicle accident, sports injury, etc.), a penetrating injury (such as a gunshot wound or stab wound), or an indirect injury (such as a blast wave or acceleration-deceleration force)3.
- TBI can be classified according to its severity into mild, moderate, or severe based on the Glasgow Coma Scale (GCS), which measures the level of consciousness by assessing eye opening, verbal response, and motor response4. The GCS ranges from 3 to 15, with lower scores indicating worse outcomes. A mild TBI has a GCS score of 13 to 15; a moderate TBI has a GCS score of 9 to 12; a severe TBI has a GCS score of 8 or less4.
- A concussion is a type of mild TBI that occurs when the brain is rapidly shaken or twisted within the skull due to an external force. This causes stretching or tearing of axons (the long extensions of neurons that transmit signals), disruption of synaptic transmission (the communication between neurons), release of inflammatory mediators (substances that trigger inflammation), alteration of blood flow (the delivery of oxygen and nutrients to the brain), and activation of cell death pathways (the mechanisms that lead to cell death)5.
- A concussion can cause various signs and symptoms that may appear immediately or later after the injury. These include headache, dizziness, nausea, vomiting, fatigue, blurred vision, ringing in the ears, confusion, amnesia (loss of memory), disorientation (loss of sense of direction), difficulty concentrating or remembering information, slurred speech, delayed reaction time, irritability, mood changes, anxiety, depression, insomnia, sensitivity to light or noise, and balance problems5.
- Most concussions resolve within days to weeks with rest and gradual return to normal activities. However, some concussions may have persistent or delayed symptoms that last for months or years. This is known as post-concussion syndrome (PCS)6. PCS can affect physical, cognitive, emotional, and behavioral functioning, and impair quality of life6.
- Some concussions may also increase the risk of developing chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease that affects people who have had repeated head trauma over time. CTE is characterized by accumulation of abnormal tau protein in the brain, which leads to neuronal loss, brain atrophy, and cognitive impairment7. CTE can cause symptoms such as memory loss, confusion, dementia, personality changes, aggression, depression, suicidal ideation, and parkinsonism.
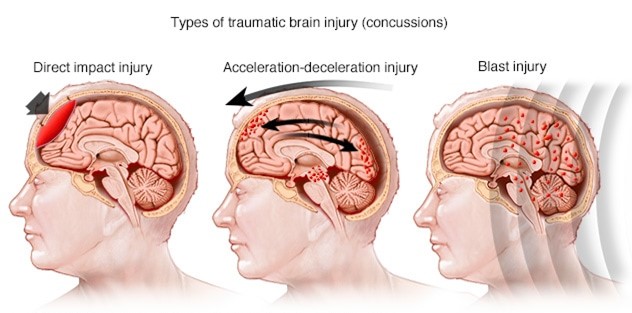
Risk Factors and Prevention of concussion
- The risk factors for TBI and concussion include age, gender, occupation, lifestyle, and medical history.
- TBI and concussion are more common in young children, adolescents, young adults, and older adults, due to their increased exposure to falls, sports injuries, motor vehicle accidents, and violence8.
- Males are more likely than females to sustain TBI and concussion, due to their higher involvement in risky behaviors, physical activities, and occupations8.
- People who work in construction, mining, transportation, military, or law enforcement are also at higher risk of TBI and concussion, due to their exposure to hazards and trauma8.
- People who have a history of substance abuse, mental illness, epilepsy, or previous TBI or concussion are also more prone to TBI and concussion, due to their impaired judgment, coordination, or brain function8.
- The prevention of TBI and concussion involves reducing the exposure to potential causes and increasing the protection of the head.
- Some of the prevention strategies include wearing helmets or seat belts when engaging in activities such as cycling, skiing, riding motorcycles, or driving cars;
- avoiding alcohol or drugs that can impair cognition or motor skills; following safety rules and regulations in sports or workplaces;
- avoiding fights or violence; and seeking medical attention for any neurological symptoms or conditions9.
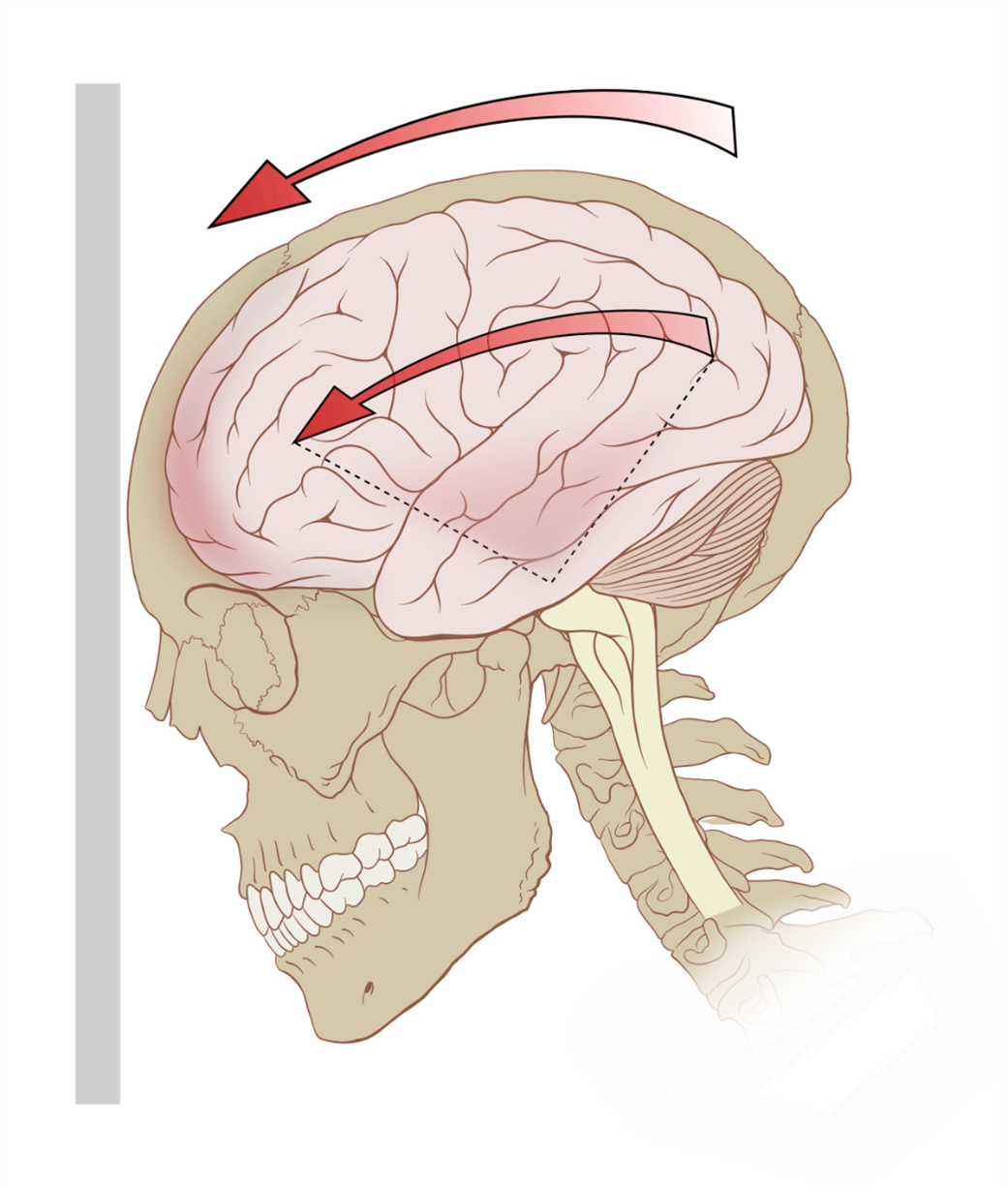
Role of Nurses
- The role of nurses in TBI and concussion is to provide screening, assessment, management, education, and support for patients and their families. Nurses can screen patients for TBI and concussion by asking about their history of head trauma, symptoms, and risk factors; performing a physical examination; and using tools such as the GCS or the Sport Concussion Assessment Tool (SCAT)10. Nurses can assess patients for TBI and concussion by monitoring their vital signs (such as blood pressure, pulse, respiration, temperature), neurological status (such as level of consciousness, pupil size and reaction, cranial nerve function), cognitive function (such as orientation, memory, attention, language), emotional state (such as mood, affect, behavior), and functional ability (such as mobility, balance, coordination)10.
- Nurses can manage patients with TBI and concussion by providing interventions such as administering medications (such as analgesics for pain relief, antiemetics for nausea control, anticonvulsants for seizure prevention), maintaining airway patency (such as suctioning secretions, positioning the head midline), ensuring adequate oxygenation (such as administering supplemental oxygen, monitoring oxygen saturation), preventing increased intracranial pressure (ICP) (such as elevating the head of the bed 30 degrees, avoiding coughing or straining), preventing infection (such as using sterile technique for wound care, administering antibiotics), promoting rest and recovery (such as limiting noise and stimulation, encouraging sleep hygiene), and facilitating rehabilitation (such as providing physical, occupational, or speech therapy)10.
- Nurses can educate patients and their families about TBI and concussion by providing information about the causes, mechanisms, signs, symptoms, complications, and outcomes of TBI and concussion; the diagnostic tests and imaging techniques used to evaluate TBI and concussion; the pharmacological and non-pharmacological interventions for TBI and concussion; the prevention strategies for TBI and concussion; the expected course of recovery from TBI and concussion; the possible long-term effects of TBI and concussion; and the available resources and support services for TBI and concussion10.
- Nurses can support patients and their families by providing emotional support (such as listening to their concerns, validating their feelings, offering reassurance), psychosocial support (such as facilitating coping skills, referring to counseling or support groups), and practical support (such as assisting with discharge planning, coordinating care transitions)10.
Pathophysiological Changes
- The pathophysiological changes that occur in the brain after TBI and concussion involve primary injury and secondary injury.
- Primary injury refers to the immediate damage caused by the external force that disrupts the integrity of the brain tissue.
- Secondary injury refers to the delayed damage caused by the cascade of molecular and cellular events that are triggered by the primary injury11.
- Primary injury can cause various types of brain lesions depending on the nature and magnitude of the external force.
- These include contusions (bruises on the brain surface), lacerations (tears in the brain tissue), hematomas (blood clots within or around the brain), diffuse axonal injury (widespread damage to axons), and penetrating injury (entry of foreign objects into the brain)11.
- Secondary injury can cause various types of brain dysfunction depending on the extent and duration of the molecular and cellular events.
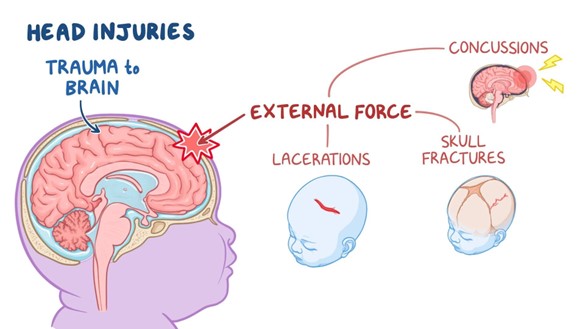
- Molecular and cellular events that contribute to secondary injury are:
- Ischemia (reduced blood flow to the brain), which leads to hypoxia (low oxygen level in the brain), and energy failure (depletion of ATP, the main energy source for cells).
- Excitotoxicity (excessive stimulation of neurons by glutamate, the main excitatory neurotransmitter in the brain), which leads to calcium overload (increased intracellular calcium level in neurons), and oxidative stress (production of reactive oxygen species that damage cell components).
- Inflammation (activation of immune cells and release of inflammatory mediators in the brain), which leads to edema (swelling of the brain tissue), and cytokine storm (overproduction of pro-inflammatory cytokines that worsen inflammation).
- Apoptosis (programmed cell death) and necrosis (uncontrolled cell death) of neurons and glia, which leads to neuronal loss, gliosis (scarring of the brain tissue), and atrophy (shrinking of the brain volume).
- These pathophysiological changes can affect the function of various components of the nervous system, such as:
- Neurons, which are the basic units of the nervous system that generate and transmit electrical signals. TBI and concussion can impair the structure and function of neurons by damaging their axons, dendrites, soma, or synapses; altering their membrane potential, action potential, or resting potential; disrupting their neurotransmitter synthesis, release, reuptake, or degradation; and affecting their gene expression, protein synthesis, or metabolism.
- Glia, which are the supporting cells of the nervous system that provide various functions such as insulation, nutrition, protection, and modulation for neurons. TBI and concussion can impair the structure and function of glia by damaging their processes, membranes, or nuclei; altering their proliferation, differentiation, or activation; disrupting their communication with neurons or other glia; and affecting their gene expression, protein synthesis, or metabolism.
- Synapses, which are the junctions between neurons where neurotransmitters are released and received. TBI and concussion can impair the structure and function of synapses by damaging their pre-synaptic terminals, post-synaptic receptors, or synaptic clefts; altering their synaptic strength, plasticity, or pruning; disrupting their neurotransmitter availability, affinity, or efficacy; and affecting their gene expression, protein synthesis, or metabolism.
- Neurotransmitters, which are the chemical messengers that mediate communication between neurons. TBI and concussion can impair the function of neurotransmitters by altering their synthesis, release, reuptake, degradation, or receptor binding; disrupting their balance between excitatory and inhibitory neurotransmitters; and affecting their modulation by other neurotransmitters or neuromodulators.
- Brain regions, which are the specialized areas of the brain that perform specific functions such as sensory processing, motor control, cognitive processing, emotional regulation, memory formation, learning consolidation, behavioral adaptation, autonomic regulation, endocrine regulation, and immune regulation. TBI and concussion can impair the function of brain regions by damaging their anatomical connections, functional networks, or hemispheric dominance; altering their activation, inhibition, or integration; disrupting their coordination, synchronization, or modulation; and affecting their plasticity, adaptability, or resilience.
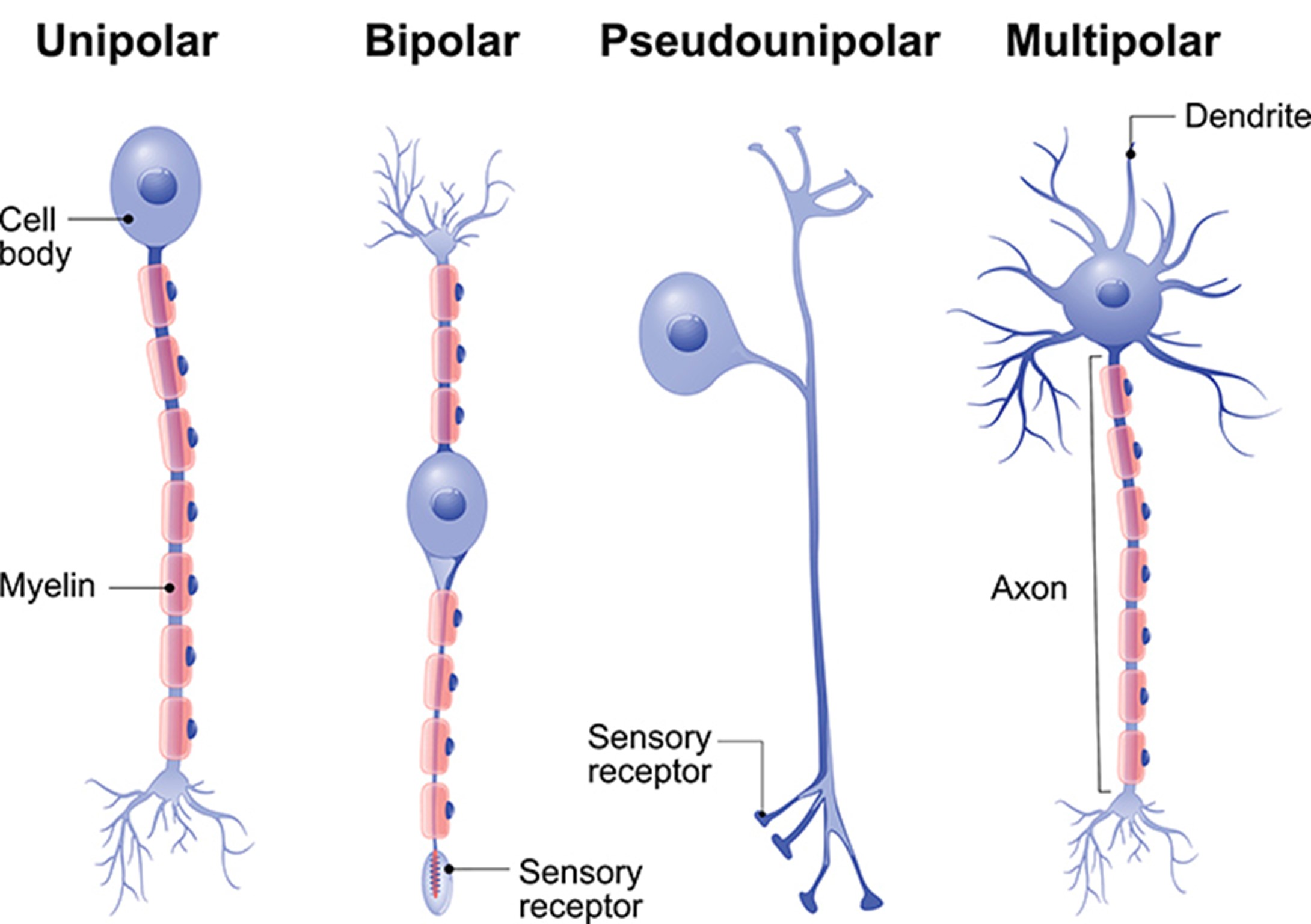
Diagnostic Tests and Imaging Techniques
- The diagnostic tests and imaging techniques used to evaluate TBI and concussion include:
- Neurological examination: A clinical assessment of the patient’s level of consciousness, mental status, cranial nerve function, motor function, sensory function, reflexes, coordination, and balance. This can help determine the severity and location of brain injury and monitor any changes over time.
- Glasgow Coma Scale (GCS): A numerical scale that measures the level of consciousness by assessing eye opening, verbal response, and motor response. This can help classify TBI into mild, moderate, or severe and predict outcomes.
- Sport Concussion Assessment Tool (SCAT): A standardized tool that assesses concussion symptoms, cognitive function, balance performance, and neck examination. This can help diagnose concussion and guide return-to-play decisions.
- Neuropsychological tests: A series of tests that measure cognitive functions such as attention, memory, language, executive function, visuospatial function, and processing speed. This can help identify cognitive impairments and monitor recovery.
- Blood tests: A collection of blood samples that measure biomarkers such as proteins or enzymes that are released from damaged brain cells. This can help detect brain injury and estimate its severity.
- Electroencephalogram (EEG): A recording of electrical activity in the brain using electrodes attached to the scalp. This can help detect abnormal brain waves or seizures that may occur after TBI or concussion.
- Evoked potentials (EPs): A recording of electrical responses in the brain to specific stimuli such as sounds or flashes. This can help assess the integrity of sensory pathways or cortical function that may be affected by TBI or concussion.
- Computed tomography (CT) scan: An imaging technique that uses x-rays to produce cross-sectional images of the brain. This can help visualize brain structures and detect brain lesions such as contusions, hematomas, or fractures that may occur after TBI or concussion.
- Magnetic resonance imaging (MRI) scan: An imaging technique that uses magnetic fields and radio waves to produce detailed images of the brain. This can help visualize brain structures and detect brain lesions such as diffuse axonal injury, edema, or atrophy that may occur after TBI or concussion.
- Diffusion tensor imaging (DTI) scan: A type of MRI scan that measures the diffusion of water molecules in the brain. This can help visualize brain connections and detect axonal damage that may occur after TBI or concussion.
- Functional MRI (fMRI) scan: A type of MRI scan that measures blood flow in the brain. This can help visualize brain activity and detect functional changes that may occur after TBI or concussion.
- Positron emission tomography (PET) scan: An imaging technique that uses radioactive tracers to measure metabolic activity in the brain. This can help visualize brain activity and detect metabolic changes that may occur after TBI or concussion.
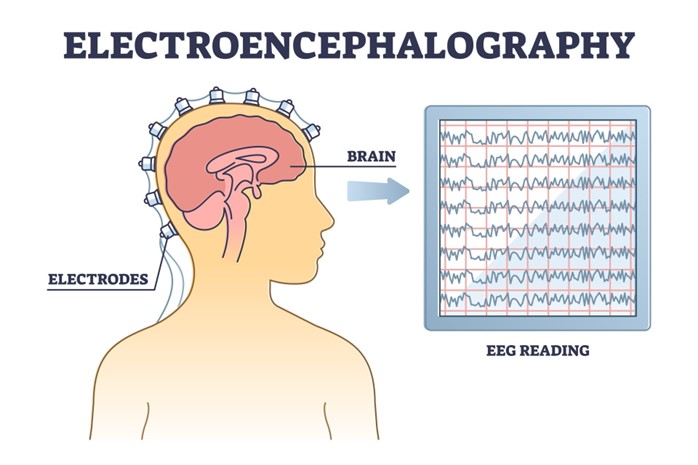
The advantages and limitations of these diagnostic tests and imaging techniques are:
- Neurological examination: It is simple, quick, and inexpensive, but it is subjective, variable, and insensitive to subtle changes.
- Glasgow Coma Scale (GCS): It is simple, quick, and widely used, but it is subjective, variable, and insensitive to mild TBI or concussion.
- Sport Concussion Assessment Tool (SCAT): It is standardized, comprehensive, and sensitive to concussion, but it is time-consuming, variable, and dependent on baseline data.
- Neuropsychological tests: They are objective, reliable, and sensitive to cognitive impairments, but they are time-consuming, expensive, and dependent on baseline data.
- Blood tests: They are objective, reliable, and sensitive to brain injury, but they are invasive, expensive, and dependent on timing and cutoff values.
- Electroencephalogram (EEG): It is non-invasive, inexpensive, and sensitive to abnormal brain activity or seizures, but it is noisy, variable, and dependent on expertise and interpretation.
- Evoked potentials (EPs): They are non-invasive, inexpensive, and sensitive to sensory or cortical dysfunction, but they are noisy, variable, and dependent on expertise and interpretation.
- Computed tomography (CT) scan: It is fast, widely available, and sensitive to structural lesions such as contusions, hematomas, or fractures, but it is invasive, expensive, and exposes the patient to radiation.
- Magnetic resonance imaging (MRI) scan: It is non-invasive, high-resolution, and sensitive to structural lesions such as diffuse axonal injury, edema, or atrophy, but it is slow, expensive, and contraindicated for patients with metal implants or claustrophobia.
- Diffusion tensor imaging (DTI) scan: It is non-invasive, high-resolution, and sensitive to axonal damage, but it is slow, expensive, and dependent on expertise and interpretation.
- Functional MRI (fMRI) scan: It is non-invasive, high-resolution, and sensitive to functional changes, but it is slow, expensive, and dependent on task design and performance.
- Positron emission tomography (PET) scan: It is non-invasive, high-resolution, and sensitive to metabolic changes, but it is slow, expensive, and exposes the patient to radiation.
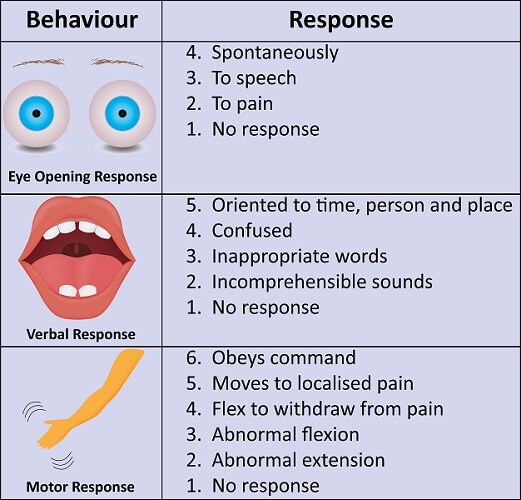
Pharmacological and Non-pharmacological Interventions
The pharmacological and non-pharmacological interventions for TBI and concussion include:
- Pharmacological interventions: These are medications that are used to treat or prevent various symptoms or complications of TBI and concussion, such as pain, nausea, vomiting, seizures, intracranial hypertension, cerebral edema, infection, inflammation, depression, anxiety, insomnia, or cognitive impairment. Some of the pharmacological interventions for TBI and concussion are:
- Analgesics: These are medications that relieve pain by blocking pain signals or reducing inflammation. Examples of analgesics include acetaminophen, ibuprofen, naproxen, aspirin, tramadol, morphine, fentanyl, and ketamine.
- Antiemetics: These are medications that prevent or reduce nausea and vomiting by blocking receptors in the brain or gastrointestinal tract that trigger these symptoms. Examples of antiemetics include ondansetron, metoclopramide, promethazine, and scopolamine.
- Anticonvulsants: These are medications that prevent or stop seizures by stabilizing the electrical activity of neurons or enhancing the inhibitory effects of gamma-aminobutyric acid (GABA), the main inhibitory neurotransmitter in the brain. Examples of anticonvulsants include phenytoin, carbamazepine, valproic acid, levetiracetam, and lorazepam.
- Osmotic agents: These are medications that reduce intracranial pressure (ICP) and cerebral edema by drawing water out of the brain tissue into the blood vessels. Examples of osmotic agents include mannitol and hypertonic saline.
- Antibiotics: These are medications that prevent or treat infection by killing or inhibiting the growth of bacteria. Examples of antibiotics include ceftriaxone, vancomycin, metronidazole, and meropenem.
- Corticosteroids: These are medications that reduce inflammation by suppressing the immune system and inhibiting the production of inflammatory mediators. Examples of corticosteroids include dexamethasone and methylprednisolone.
- Antidepressants: These are medications that treat depression by increasing the availability or efficacy of serotonin, norepinephrine, or dopamine, the main mood-regulating neurotransmitters in the brain. Examples of antidepressants include selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine, sertraline, and citalopram; serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine, duloxetine, and desvenlafaxine; and dopamine-norepinephrine reuptake inhibitors (DNRIs) such as bupropion.
- Anxiolytics: These are medications that treat anxiety by enhancing the inhibitory effects of GABA or reducing the activity of noradrenaline, a neurotransmitter that mediates stress responses. Examples of anxiolytics include benzodiazepines such as diazepam, alprazolam, and clonazepam; and beta-blockers such as propranolol, atenolol, and metoprolol.
- Hypnotics: These are medications that induce or maintain sleep by enhancing the inhibitory effects of GABA or melatonin, a hormone that regulates circadian rhythms. Examples of hypnotics include zolpidem, zaleplon, eszopiclone, and melatonin.
- Cognitive enhancers: These are medications that improve cognitive function by modulating the activity of acetylcholine, glutamate, or dopamine, neurotransmitters that are involved in learning, memory, attention, and executive function. Examples of cognitive enhancers include cholinesterase inhibitors such as donepezil, rivastigmine, and galantamine; N-methyl-D-aspartate (NMDA) receptor antagonists such as memantine; and dopamine agonists such as methylphenidate and modafinil.
- The indications, contraindications, side effects, and nursing implications of these pharmacological interventions depend on various factors such as the type, severity, and duration of TBI or concussion; the patient’s age, weight, medical history, allergies, and current medications; the drug’s dose, route, frequency, and duration; and the drug’s pharmacokinetics (how it is absorbed, distributed, metabolized, and excreted) and pharmacodynamics (how it interacts with its target receptors).
- Therefore, nurses should consult with physicians or pharmacists before administering any medication to patients with TBI or concussion; monitor patients for any adverse reactions or interactions; educate patients about the purpose, benefits, risks, and precautions of the medication; and document the medication administration and patient response.
- Non-pharmacological interventions: These are interventions that do not involve medications but use other methods such as physical, occupational, or speech therapy; cognitive behavioral therapy (CBT); biofeedback; neurofeedback; transcranial magnetic stimulation (TMS); transcranial direct current stimulation (tDCS); or acupuncture to treat or prevent various symptoms or complications of TBI or concussion, such as pain, nausea, vomiting, seizures, intracranial hypertension, cerebral edema, infection, inflammation, depression, anxiety, insomnia, or cognitive impairment. Some of the non-pharmacological interventions for TBI and concussion are:
- Physical therapy: This is a type of therapy that uses exercises, stretches, massages, heat, cold, electrical stimulation, or ultrasound to improve the patient’s physical function, mobility, strength, endurance, balance, and coordination. Physical therapy can help patients with TBI or concussion recover from motor impairments, spasticity, contractures, pain, or fatigue.
- Occupational therapy: This is a type of therapy that uses activities of daily living (ADLs), instrumental activities of daily living (IADLs), leisure activities, or work-related tasks to improve the patient’s functional ability, independence, self-care, and quality of life. Occupational therapy can help patients with TBI or concussion recover from sensory impairments, visual impairments, perceptual impairments, cognitive impairments, or behavioral impairments.
- Speech therapy: This is a type of therapy that uses exercises, games, drills, strategies, or devices to improve the patient’s speech, language, communication, swallowing, or cognition. Speech therapy can help patients with TBI or concussion recover from aphasia (language impairment), dysarthria (speech impairment), apraxia (motor speech impairment), dysphagia (swallowing impairment), or cognitive-communication impairment.
- Cognitive behavioral therapy (CBT): This is a type of psychotherapy that uses cognitive techniques (such as identifying and challenging negative thoughts), behavioral techniques (such as exposure and response prevention), and emotional techniques (such as relaxation and mindfulness) to help the patient cope with psychological symptoms such as depression, anxiety, insomnia, or post-traumatic stress disorder (PTSD). CBT can help patients with TBI or concussion modify their maladaptive beliefs, behaviors, and emotions that result from their brain injury.
- Biofeedback: This is a type of therapy that uses sensors and monitors to measure the patient’s physiological responses such as heart rate, blood pressure, muscle tension, skin temperature, or brain waves. The patient then receives feedback on these responses through visual, auditory, or tactile cues, and learns to control them through relaxation or cognitive techniques. Biofeedback can help patients with TBI or concussion reduce stress, pain, anxiety, or insomnia, and improve autonomic regulation, mood, or cognition.
-
- Neurofeedback: This is a type of biofeedback that uses electroencephalogram (EEG) to measure the patient’s brain waves and provide feedback on their frequency, amplitude, or coherence. The patient then learns to modify their brain waves through operant conditioning or neurostimulation techniques. Neurofeedback can help patients with TBI or concussion enhance brain function, neuroplasticity, or recovery by increasing or decreasing specific brain wave patterns that are associated with different cognitive or emotional states.
- Transcranial magnetic stimulation (TMS): This is a type of therapy that uses a coil to generate a magnetic field that induces an electric current in the brain. The current then stimulates or inhibits specific brain regions or networks that are involved in various functions such as motor control, language, memory, attention, emotion, or mood. TMS can help patients with TBI or concussion improve neurological function, cognitive function, or psychiatric symptoms by modulating the activity of the targeted brain regions or networks.
- Transcranial direct current stimulation (tDCS): This is a type of therapy that uses electrodes to deliver a low-intensity direct current to the scalp. The current then alters the excitability of the underlying brain tissue by depolarizing or hyperpolarizing the neurons. tDCS can help patients with TBI or concussion improve neurological function, cognitive function, or psychiatric symptoms by enhancing or suppressing the activity of the affected brain regions.
- Acupuncture: This is a type of therapy that uses needles to stimulate specific points on the body that are connected to different organs or systems. Acupuncture can help patients with TBI or concussion reduce pain, inflammation, nausea, vomiting, anxiety, depression, insomnia, or cognitive impairment by regulating the flow of qi (vital energy) and blood in the body.
- The indications, contraindications, side effects, and nursing implications of these non-pharmacological interventions depend on various factors such as the type, severity, and duration of TBI or concussion; the patient’s age, weight, medical history, allergies, and current medications; the intervention’s dose, frequency, and duration; and the intervention’s mechanism of action and evidence base. Therefore, nurses should consult with physicians or therapists before recommending or administering any non-pharmacological intervention to patients with TBI or concussion; monitor patients for any adverse reactions or interactions; educate patients about the purpose, benefits, risks, and precautions of the intervention; and document the intervention administration and patient response.
Stroke: Ischemic stroke, Hemorrhagic stroke, Transient ischemic attack (TIA)
- The nervous system relies on a constant supply of oxygen and glucose from the blood to maintain its function and viability
- Ischemic stroke is a condition that occurs when the blood flow to a part of the brain is interrupted, resulting in tissue hypoxia, ischemia, and infarction
- The nervous system is highly sensitive to changes in blood flow, oxygen, glucose, and electrolytes, which can affect its function and structure.
- A stroke is a sudden interruption of blood flow to a part of the brain, resulting in tissue damage and neurological deficits.
- A stroke can be classified as ischemic or hemorrhagic, depending on the underlying mechanism.
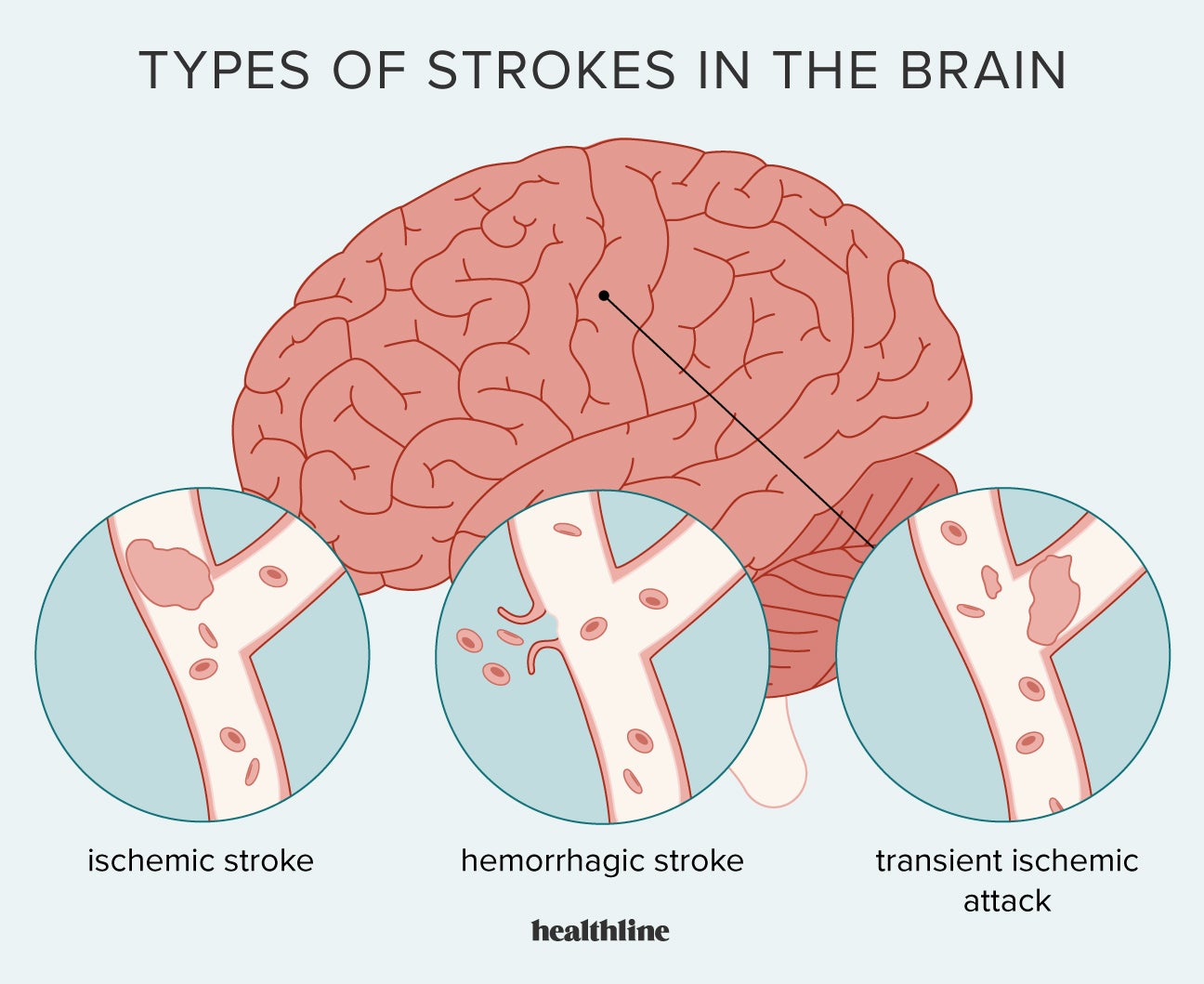
Ischemic Stroke:
- Ischemic stroke is the most common type of stroke, accounting for about 80% of all strokes1
- Ischemic stroke can be classified into two main types: thrombotic and embolic2
- Thrombotic stroke occurs when a blood clot forms on an atherosclerotic plaque in a cerebral artery, blocking the blood flow to the downstream brain tissue
- Embolic stroke occurs when a blood clot or other debris travels from another part of the body (such as the heart or carotid artery) and lodges in a cerebral artery, cutting off the blood supply to the distal brain tissue
- Ischemic stroke can also be classified according to the location and size of the affected brain region3
- Large artery thrombotic stroke affects the major cerebral arteries, such as the internal carotid, middle cerebral, or anterior cerebral arteries
- Small penetrating artery thrombotic stroke affects the smaller branches of the cerebral arteries, such as the lenticulostriate arteries
- Cardiogenic embolic stroke affects any cerebral artery, depending on the source and size of the embolus
- Cryptogenic stroke is a term used when the cause of ischemic stroke is unknown or undetermined
- Other causes of ischemic stroke include vasculitis, dissection, hypercoagulable states, sickle cell disease, and cocaine abuse
Risk Factors and Causes of Ischemic Stroke:
- Ischemic stroke is associated with several modifiable and non-modifiable risk factors4
- Modifiable risk factors include hypertension, diabetes mellitus, dyslipidemia, smoking, obesity, physical inactivity, atrial fibrillation, coronary artery disease, carotid artery stenosis, oral contraceptive use, alcohol abuse, and illicit drug use
- Non-modifiable risk factors include age (increased risk after 55 years), sex (higher risk in men than women), race (higher risk in African Americans than Caucasians), family history, genetic factors, and low birth weight
- The main cause of ischemic stroke is atherosclerosis, which is a chronic inflammatory process that leads to plaque formation and narrowing of the arterial lumen5
- Atherosclerosis can affect any artery in the body, but it is especially prevalent in the carotid and cerebral arteries
- Atherosclerosis can cause thrombotic stroke by inducing platelet aggregation and thrombus formation on the plaque surface
- Atherosclerosis can also cause embolic stroke by causing plaque rupture or ulceration, which can release fragments of plaque material or thrombus into the bloodstream
- Atherosclerosis can also reduce the collateral blood flow to the brain, making it more vulnerable to ischemia
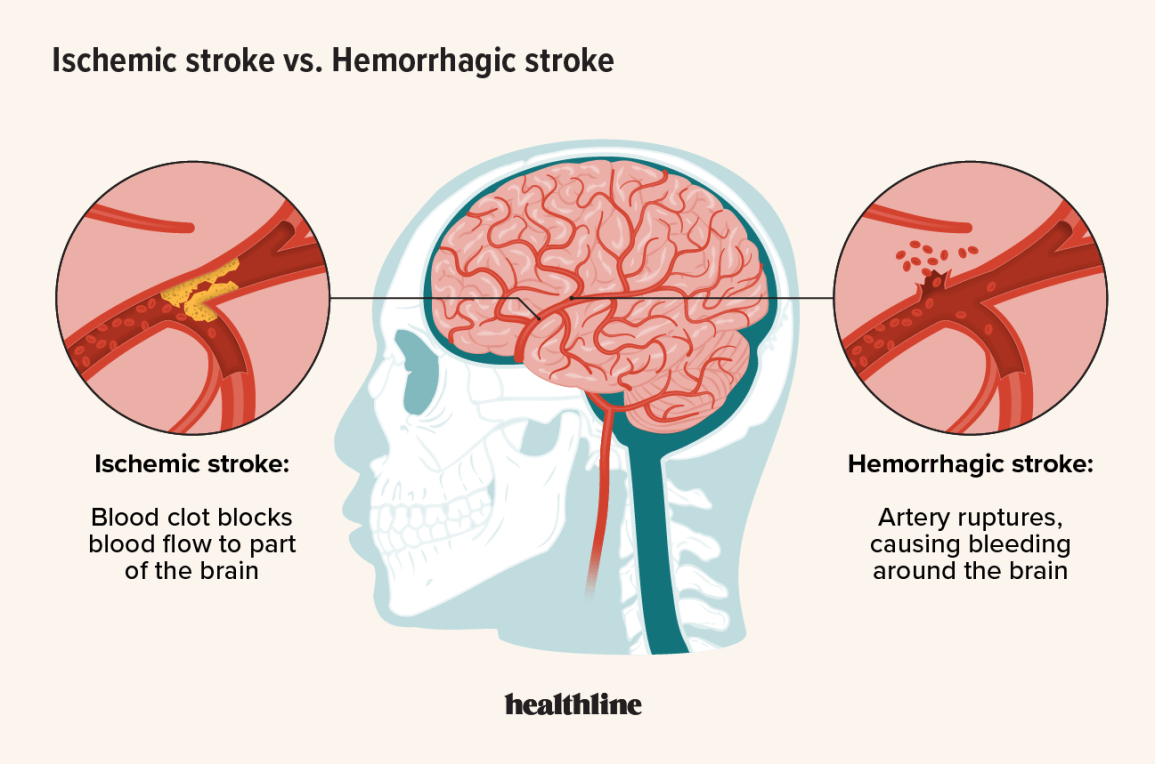
Pathophysiology and Clinical Manifestations of Ischemic Stroke:
- The pathophysiology of ischemic stroke involves a complex cascade of cellular and molecular events that lead to neuronal injury and death6
- When blood flow to a part of the brain is reduced below a critical threshold (about 25 ml/100 g/min), neurons switch from aerobic to anaerobic metabolism to produce ATP7
- Anaerobic metabolism is less efficient and produces lactic acid, which lowers the pH and causes acidosis
- Acidosis impairs the function of membrane pumps that maintain ionic gradients across neuronal membranes
- As a result, sodium and calcium ions accumulate inside neurons, while potassium ions leak out
- This leads to membrane depolarization, which triggers the release of excitatory neurotransmitters such as glutamate
- Glutamate binds to NMDA receptors on postsynaptic neurons, causing further influx of calcium and sodium ions
- Excess calcium activates various enzymes that degrade proteins, lipids, and DNA, leading to cell death by necrosis or apoptosis
- Excess glutamate also causes excitotoxicity, which damages neighboring neurons and glial cells
- The area of irreversible ischemic damage is called the infarct core, which is surrounded by a zone of potentially salvageable tissue called the ischemic penumbra
- The ischemic penumbra can be rescued by restoring blood flow within a narrow time window (about 3 to 4.5 hours), using thrombolytic therapy or mechanical thrombectomy
- The clinical manifestations of ischemic stroke depend on the location and extent of the brain injury8
- The most common symptoms of ischemic stroke are sudden onset of focal neurological deficits, such as weakness, numbness, visual loss, aphasia, dysarthria, dysphagia, ataxia, and vertigo
- The neurological deficits are usually contralateral to the side of the brain lesion, except for some cranial nerve deficits that are ipsilateral
- The neurological deficits can be assessed using the National Institutes of Health Stroke Scale (NIHSS), which is a standardized tool that evaluates 11 items related to level of consciousness, eye movements, visual fields, facial palsy, motor strength, limb ataxia, sensory loss, language, speech, and extinction9
- The NIHSS score ranges from 0 to 42, with higher scores indicating more severe stroke
- The neurological deficits can also be recognized using the FAST mnemonic, which stands for Face (ask the person to smile and check for facial droop), Arms (ask the person to raise both arms and check for arm drift), Speech (ask the person to repeat a simple sentence and check for slurred or inappropriate speech), and Time (note the time when symptoms started and call 911 immediately)10
- Some patients may also experience headache, nausea, vomiting, seizures, or altered mental status
Diagnostic Tests and Procedures for Ischemic Stroke:
- The diagnosis of ischemic stroke is based on clinical history, physical examination, and neuroimaging studies11
- Clinical history should include the onset, duration, and progression of symptoms, as well as the presence of risk factors and comorbidities
- Physical examination should include a comprehensive neurological assessment using the NIHSS or other validated scales
- Neuroimaging studies are essential to confirm the diagnosis of ischemic stroke, exclude hemorrhagic stroke or other causes of neurological deficits, identify the location and size of the brain lesion, and evaluate the vascular anatomy and perfusion status
- The most commonly used neuroimaging modality for ischemic stroke is noncontrast computed tomography (CT) scan12
- CT scan is widely available, fast, and reliable in detecting intracranial hemorrhage
- CT scan can also show early signs of ischemic stroke in some cases, such as loss of gray-white matter differentiation, hypodensity in the affected brain region, or hyperdense artery sign
- CT scan can also be combined with CT angiography (CTA) or CT perfusion (CTP) to provide more information about the cerebral blood vessels and blood flow
- Another neuroimaging modality for ischemic stroke is magnetic resonance imaging (MRI)13
- MRI is more sensitive and specific than CT scan in detecting acute ischemic stroke, especially in the posterior fossa and subcortical regions
- MRI can also show different stages of ischemic stroke evolution using different sequences, such as diffusion-weighted imaging (DWI), perfusion-weighted imaging (PWI), fluid-attenuated inversion recovery (FLAIR), gradient-recalled echo (GRE), or susceptibility-weighted imaging (SWI)
- MRI can also be combined with magnetic resonance angiography (MRA) or magnetic resonance venography (MRV) to visualize the cerebral arteries and veins
- Other diagnostic tests and procedures for ischemic stroke include14
- Blood tests to measure glucose level, electrolytes, renal function, liver function, complete blood count, coagulation profile, lipid profile, cardiac enzymes, and inflammatory markers
- Electrocardiogram (ECG) to detect cardiac arrhythmias, ischemia, or infarction
- Echocardiogram to evaluate cardiac structure and function, and to detect potential sources of emboli, such as valvular disease, cardiac thrombi, or patent foramen ovale
- Carotid ultrasound to assess carotid artery stenosis or plaque morphology
- Transcranial Doppler to measure cerebral blood flow velocity and detect intracranial stenosis or emboli
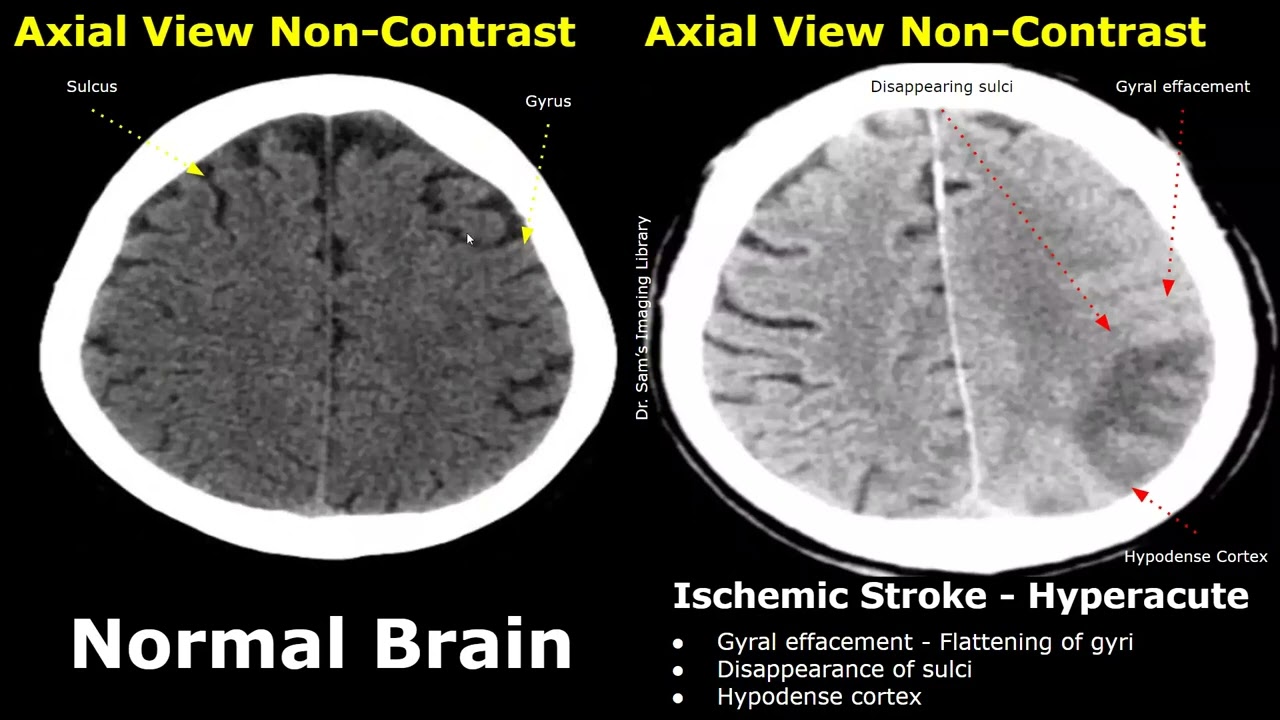
Complications and Therapeutic Interventions for Ischemic Stroke:
- Ischemic stroke can lead to several complications that can worsen the prognosis and quality of life of patients
- Hemorrhagic transformation is a condition that occurs when blood leaks into the ischemic brain tissue, causing secondary hemorrhage and edema
- Cerebral edema is a condition that occurs when fluid accumulates in the brain tissue, causing increased intracranial pressure and compression of vital structures
- Vasospasm is a condition that occurs when cerebral arteries constrict, reducing blood flow and causing delayed ischemia
- Seizures are abnormal electrical discharges in the brain that can cause convulsions, loss of consciousness, or other neurological symptoms
- Hydrocephalus is a condition that occurs when cerebrospinal fluid accumulates in the ventricles, causing increased intracranial pressure and impaired brain function
- Infections are conditions that occur when microorganisms invade the body, causing fever, inflammation, and systemic or local complications
- Dysphagia is a condition that occurs when swallowing muscles are impaired, causing difficulty or inability to swallow food, liquids, or saliva
- Aspiration pneumonia is a condition that occurs when food, liquids, or saliva enter the lungs, causing inflammation and infection
- Malnutrition is a condition that occurs when nutritional intake is inadequate, causing weight loss, muscle wasting, and impaired immunity
- Pressure ulcers are conditions that occur when skin and underlying tissues are damaged by prolonged pressure, friction, or shear forces
- Deep vein thrombosis (DVT) is a condition that occurs when blood clots form in the deep veins of the legs or pelvis, causing pain, swelling, and inflammation
- Pulmonary embolism (PE) is a condition that occurs when a blood clot from a DVT breaks off and travels to the lungs, causing chest pain, shortness of breath, and hypoxia
- Depression is a condition that occurs when mood is persistently low, causing sadness, hopelessness, loss of interest, and suicidal thoughts
- The therapeutic interventions for ischemic stroke aim to restore blood flow to the ischemic brain tissue, prevent further ischemia or hemorrhage, reduce complications, and improve functional recovery
- Thrombolytic therapy is a treatment that involves administering an intravenous drug (such as alteplase) that dissolves the blood clot and restores blood flow to the affected brain region
- Thrombolytic therapy can reduce the disability and mortality from ischemic stroke if given within 4.5 hours of symptom onset
- Thrombolytic therapy has several contraindications and risks, such as hemorrhagic stroke, intracranial hemorrhage, or systemic bleeding
- Thrombolytic therapy requires careful monitoring of vital signs, neurological status, and coagulation parameters
- Mechanical thrombectomy is a treatment that involves inserting a catheter through a groin artery and advancing it to the occluded cerebral artery, where a device (such as a stent retriever or an aspiration catheter) is used to remove the clot and restore blood flow
- Mechanical thrombectomy can improve the outcomes of ischemic stroke if performed within 6 hours of symptom onset, or up to 24 hours in selected cases
- Mechanical thrombectomy has some limitations and complications, such as difficulty in accessing the clot, vessel perforation, or distal embolization
- Mechanical thrombectomy requires specialized equipment and personnel, and close collaboration between neurologists, radiologists, and neurosurgeons
- Anticoagulant therapy is a treatment that involves administering drugs (such as heparin or warfarin) that prevent the formation or extension of blood clots
- Anticoagulant therapy can prevent recurrent ischemic stroke in patients with atrial fibrillation or other cardiac sources of emboli
- Anticoagulant therapy has several contraindications and risks, such as hemorrhagic stroke, intracranial hemorrhage, or systemic bleeding
- Anticoagulant therapy requires regular monitoring of coagulation parameters (such as INR) and adjustment of drug dosage
- Antiplatelet therapy is a treatment that involves administering drugs (such as aspirin or clopidogrel) that inhibit platelet aggregation and adhesion
- Antiplatelet therapy can prevent recurrent ischemic stroke in patients with noncardioembolic stroke or transient ischemic attack (TIA)
- Antiplatelet therapy has some contraindications and risks, such as hemorrhagic stroke, intracranial hemorrhage, or gastrointestinal bleeding
- Antiplatelet therapy does not require routine monitoring of coagulation parameters, but may interact with other drugs or foods
- Neuroprotective therapy is a treatment that involves administering drugs (such as magnesium or nimodipine) that protect the brain cells from ischemic injury by modulating calcium influx, glutamate release, or oxidative stress
- Neuroprotective therapy has shown promising results in animal models of ischemic stroke, but has failed to demonstrate efficacy in human trials
- Neuroprotective therapy has some adverse effects, such as hypotension, bradycardia, or headache
- Neuroprotective therapy is still under investigation and not widely used in clinical practice
- Surgical intervention is a treatment that involves performing a procedure (such as carotid endarterectomy, carotid stenting, or decompressive craniectomy) that removes the source of ischemia or reduces the intracranial pressure
- Surgical intervention can prevent recurrent ischemic stroke in patients with severe carotid artery stenosis or symptomatic intracranial stenosis
- Surgical intervention can also improve the survival and outcome of patients with malignant cerebral edema or large hemispheric infarction
- Surgical intervention has some indications and risks, such as perioperative stroke, infection, or bleeding
- Surgical intervention requires careful selection of candidates and timing of surgery, and multidisciplinary collaboration between neurologists, vascular surgeons, and neurosurgeons
- Rehabilitation is a treatment that involves providing physical, occupational, speech, and psychological therapies that aim to restore function, independence, and quality of life of patients with ischemic stroke
- Rehabilitation can improve the motor, sensory, cognitive, linguistic, and emotional recovery of patients with ischemic stroke
- Rehabilitation can also prevent complications such as contractures, spasticity, falls, infections, depression, or social isolation
- Rehabilitation requires a comprehensive assessment of the patient’s needs and goals, and a tailored plan of interventions that involve the patient, family, and caregivers
- Rehabilitation should start as soon as possible after ischemic stroke and continue for as long as needed
- Thrombolytic therapy is a treatment that involves administering an intravenous drug (such as alteplase) that dissolves the blood clot and restores blood flow to the affected brain region
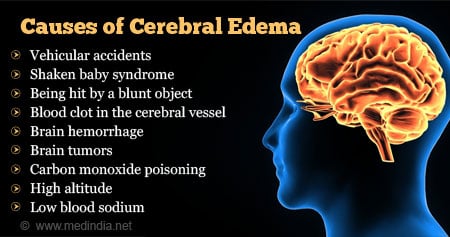
Nursing Care and Education for Patients with Ischemic Stroke:
- Nursing care for patients with ischemic stroke involves providing holistic and evidence-based care that addresses the physical, psychological, and social needs of the patient and family
- Nursing care should follow the nursing process of assessment, diagnosis, planning, implementation, and evaluation
- Nursing care should be based on the best available research and guidelines, such as the American Stroke Association (ASA) guidelines or the Stroke Best Practice Recommendations (SBPR)
- Nursing care should be delivered by a competent and compassionate nurse who works as part of an interdisciplinary stroke team
- Nursing assessment for patients with ischemic stroke involves collecting subjective and objective data that are relevant to the patient’s condition and response to treatment
- Subjective data include the patient’s history of present illness, past medical history, family history, medication history, allergy history, social history, and review of systems
- Objective data include the patient’s vital signs, neurological examination using the NIHSS or other scales, cardiovascular examination using the ECG or echocardiogram, vascular examination using the carotid ultrasound or transcranial Doppler, laboratory tests such as blood glucose level or coagulation profile, and neuroimaging studies such as CT scan or MRI
- Nursing diagnosis for patients with ischemic stroke involves identifying the actual or potential problems that affect the patient’s health and well-being
- Some examples of nursing diagnoses for patients with ischemic stroke are:
- Ineffective tissue perfusion related to reduced cerebral blood flow
- Impaired physical mobility related to hemiparesis or hemiplegia
- Impaired verbal communication related to aphasia or dysarthria
- Impaired swallowing related to dysphagia or cranial nerve deficits
- Risk for aspiration related to impaired swallowing or decreased level of consciousness
- Risk for infection related to impaired immunity or invasive procedures
- Risk for injury related to seizures or falls
- Risk for impaired skin integrity related to immobility or pressure ulcers
- Risk for venous thromboembolism related to immobility or hypercoagulability
- Acute pain related to headache or muscle spasms
- Anxiety related to fear of death or disability
- Depression related to loss of function or social support
- Some examples of nursing diagnoses for patients with ischemic stroke are:
- Nursing planning for patients with ischemic stroke involves setting realistic and measurable goals and outcomes that are based on the patient’s needs, preferences, and potential
- Some examples of nursing goals and outcomes for patients with ischemic stroke are:
- The patient will maintain adequate tissue perfusion as evidenced by normal vital signs, neurological status, and neuroimaging findings
- The patient will improve physical mobility as evidenced by increased range of motion, strength, and coordination of the affected limbs
- The patient will improve verbal communication as evidenced by increased comprehension, expression, and articulation of speech
- The patient will improve swallowing as evidenced by decreased risk of aspiration, improved oral intake, and normal weight
- The patient will prevent infection as evidenced by absence of fever, inflammation, or positive cultures
- The patient will prevent injury as evidenced by absence of seizures, falls, or trauma
- The patient will prevent impaired skin integrity as evidenced by absence of pressure ulcers, erythema, or breakdown
- The patient will prevent venous thromboembolism as evidenced by absence of pain, swelling, or inflammation in the lower extremities or chest
- The patient will manage pain as evidenced by decreased pain intensity, frequency, and duration
- The patient will reduce anxiety as evidenced by decreased heart rate, blood pressure, and respiratory rate
- The patient will cope with depression as evidenced by increased mood, interest, and social interaction
- Some examples of nursing goals and outcomes for patients with ischemic stroke are:
- Nursing implementation for patients with ischemic stroke involves performing interventions that are consistent with the nursing diagnoses, goals, and outcomes
- Some examples of nursing interventions for patients with ischemic stroke are:
- Monitor vital signs, neurological status, and coagulation parameters frequently and report any changes or abnormalities to the physician
- Administer thrombolytic therapy, anticoagulant therapy, antiplatelet therapy, or neuroprotective therapy as prescribed and monitor for any adverse effects or complications
- Assist with mechanical thrombectomy or surgical intervention as needed and monitor for any perioperative or postoperative complications
- Maintain a patent airway and oxygen saturation above 95% by providing supplemental oxygen, suctioning, or intubation as needed
- Elevate the head of the bed to 30 degrees and position the patient on the unaffected side to reduce intracranial pressure and facilitate drainage
- Assess swallowing function using a bedside swallow test or a videofluoroscopic swallow study and provide appropriate oral care and hydration
- Initiate enteral or parenteral nutrition as prescribed and monitor for any signs of intolerance or malabsorption
- Prevent aspiration pneumonia by elevating the head of the bed to 45 degrees during feeding, thickening liquids, using chin tuck or swallow maneuvers, and administering prophylactic antibiotics as prescribed
- Encourage early mobilization and exercise of the affected limbs using passive, active, or resistive movements, and provide assistive devices such as braces, splints, or walkers as needed
- Some examples of nursing interventions for patients with ischemic stroke are:
- Prevent contractures and spasticity by applying range of motion exercises, heat, cold, or massage therapy, and administering muscle relaxants or botulinum toxin injections as prescribed
- Prevent pressure ulcers by repositioning the patient every 2 hours, using pressure-relieving mattresses or cushions, and inspecting the skin for any signs of breakdown or infection
- Prevent venous thromboembolism by applying compression stockings or pneumatic devices, elevating the lower extremities, and administering anticoagulants or thrombolytics as prescribed
- Manage pain by assessing its location, intensity, and quality using a valid scale (such as the numeric rating scale or the faces pain scale), and administering analgesics or nonpharmacological methods (such as relaxation techniques or distraction) as prescribed
- Reduce anxiety by providing reassurance, information, and emotional support to the patient and family, and administering anxiolytics or sedatives as prescribed
- Cope with depression by assessing its severity using a valid tool (such as the Hamilton depression rating scale or the Beck depression inventory), and administering antidepressants or psychotherapy as prescribed
- Improve verbal communication by assessing the type and severity of aphasia using a valid tool (such as the Boston diagnostic aphasia examination or the Western aphasia battery), and providing speech therapy or augmentative communication devices (such as picture boards or computer programs) as needed
- Promote cognitive function by assessing the presence and extent of cognitive impairment using a valid tool (such as the mini-mental state examination or the Montreal cognitive assessment), and providing cognitive stimulation or rehabilitation activities (such as memory games or puzzles) as needed
- Facilitate social interaction by encouraging family and friends to visit and participate in care, and providing opportunities for group activities or support groups as available
- Nursing evaluation for patients with ischemic stroke involves measuring the effectiveness of the interventions and comparing them with the expected outcomes
- Nursing evaluation should be done continuously and systematically throughout the care process
- Nursing evaluation should involve the patient, family, and other members of the stroke team
- Nursing evaluation should use the same tools and scales that were used for the assessment and planning phases
- Nursing evaluation should document the results and findings in a clear and concise manner
- Nursing evaluation should identify any gaps or discrepancies between the actual and expected outcomes
- Nursing evaluation should modify or revise the nursing diagnoses, goals, outcomes, or interventions as needed
Hemorrhagic stroke
- A hemorrhagic stroke occurs when a blood vessel in the brain ruptures and bleeds into the surrounding brain tissue or into the subarachnoid space (the space between the brain and the meninges).
- The bleeding causes increased intracranial pressure (ICP), which compresses and damages the brain tissue, as well as reduces cerebral perfusion pressure (CPP), which impairs blood flow to the brain.
- A hemorrhagic stroke can be further classified as intracerebral or subarachnoid, depending on the location of the bleeding.
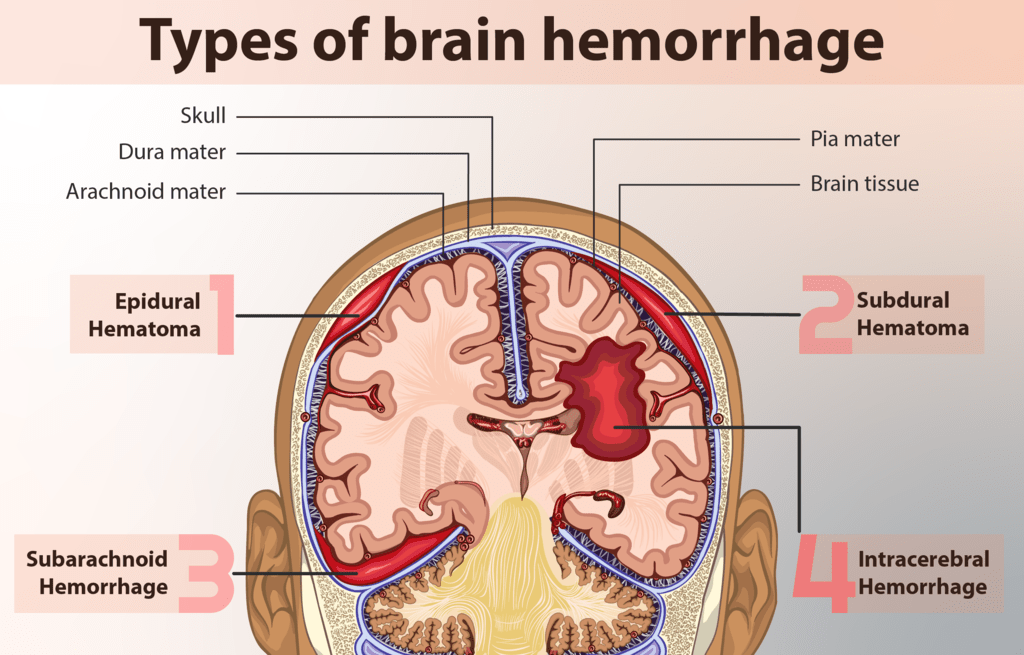
Intracerebral Hemorrhage
- An intracerebral hemorrhage (ICH) is a type of hemorrhagic stroke that occurs when a blood vessel within the brain parenchyma (the functional tissue) ruptures and bleeds into the brain tissue.
- The most common cause of ICH is hypertension, which weakens the walls of small arteries in the brain over time. Other causes include trauma, vascular malformations, tumors, coagulopathy, amyloid angiopathy, and illicit drug use.
- The signs and symptoms of ICH depend on the location and extent of bleeding, but may include headache, nausea, vomiting, altered level of consciousness, hemiparesis (weakness on one side of the body), hemiplegia (paralysis on one side of the body), aphasia (language impairment), dysarthria (speech impairment), dysphagia (swallowing impairment), ataxia (coordination impairment), visual disturbances, seizures, and coma.
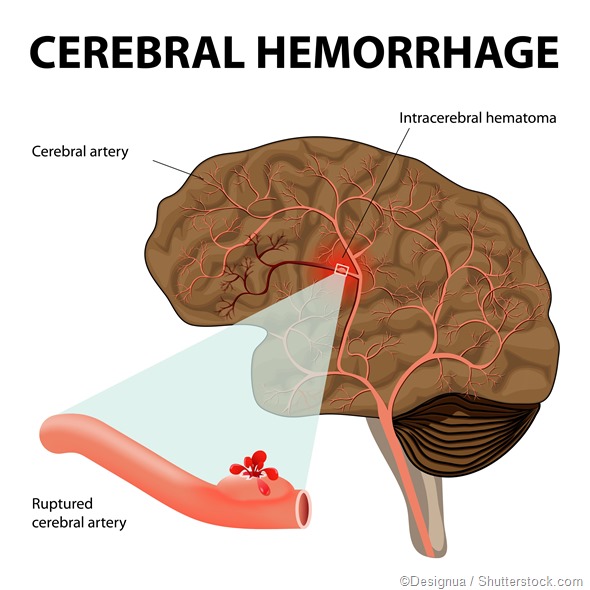
Subarachnoid Hemorrhage
- A subarachnoid hemorrhage (SAH) is a type of hemorrhagic stroke that occurs when a blood vessel between the brain and the meninges ruptures and bleeds into the subarachnoid space.
- The most common cause of SAH is a ruptured cerebral aneurysm, which is a bulging or ballooning of a weakened area in an artery wall. Other causes include trauma, vascular malformations, tumors, coagulopathy, and illicit drug use.
- The signs and symptoms of SAH include sudden severe headache ("thunderclap headache"), nausea, vomiting, neck stiffness ("nuchal rigidity"), photophobia (sensitivity to light), altered level of consciousness, focal neurological deficits (such as hemiparesis or aphasia), cranial nerve palsies (such as ptosis or diplopia), seizures, and coma.
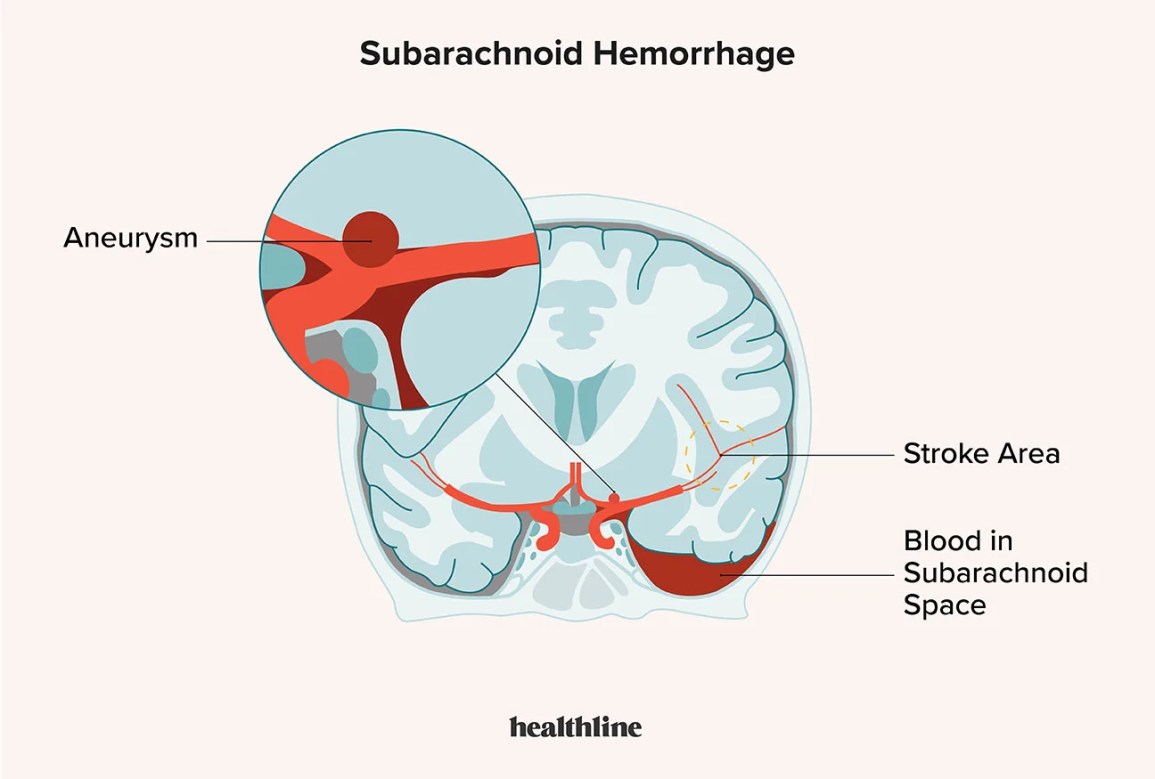
Diagnosis of hemorrhagic stroke
- The diagnosis of hemorrhagic stroke is based on clinical presentation, medical history, physical examination, neurological assessment, and imaging studies.
- The imaging studies that are used to confirm hemorrhagic stroke are computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of the head. These tests can show the location and extent of bleeding in the brain. They can also help differentiate between ischemic and hemorrhagic stroke.
- Other tests that may be performed to identify the cause or complications of hemorrhagic stroke include lumbar puncture (to obtain cerebrospinal fluid for analysis), angiography (to visualize blood vessels in the brain), electroencephalography (to monitor brain activity), blood tests (to check for coagulation disorders or infection), chest X-ray (to rule out cardiac or pulmonary sources of emboli), electrocardiogram (to assess cardiac function), echocardiogram (to evaluate cardiac structure and function), carotid ultrasound (to assess carotid artery stenosis or plaque).
Treatment of hemorrhagic stroke
- The treatment of hemorrhagic stroke aims to stop bleeding, reduce ICP, prevent complications, and restore neurological function.
- The treatment options depend on the type, location, and severity of bleeding, as well as the patient's condition and preferences.
- The treatment options may include medical management, surgical intervention, or endovascular therapy.
-
- Medical Management
- Medical management of hemorrhagic stroke involves supportive care and pharmacological therapy.
- Supportive care includes monitoring vital signs, neurological status, ICP, CPP, fluid and electrolyte balance, oxygenation, and glucose levels. It also includes maintaining a patent airway, providing adequate ventilation, ensuring proper positioning and alignment, preventing aspiration and infection, managing pain and fever, and providing nutritional support.
- Pharmacological therapy includes administering medications to control blood pressure, reduce ICP, prevent seizures, prevent vasospasm (narrowing of blood vessels), prevent or treat coagulopathy or infection, and provide sedation or analgesia.
- Surgical Intervention
- Surgical intervention of hemorrhagic stroke involves removing the source of bleeding or decompressing the brain tissue.
- The surgical procedures that may be performed include craniotomy (opening the skull to access the brain), hematoma evacuation (removing the blood clot from the brain), aneurysm clipping (placing a metal clip on the neck of the aneurysm to stop blood flow), ventriculostomy (inserting a catheter into a ventricle to drain excess cerebrospinal fluid and reduce ICP), or craniectomy (removing a part of the skull to allow brain swelling).
- Endovascular Therapy
- Endovascular therapy of hemorrhagic stroke involves using catheters and devices to treat the blood vessel abnormalities that cause bleeding.
- The endovascular procedures that may be performed include aneurysm coiling (placing coils into the aneurysm to block blood flow and induce clotting), aneurysm stenting (placing a stent into the artery to support the vessel wall and prevent rebleeding), or embolization (injecting glue or particles into the vessel to occlude it).
- Medical Management
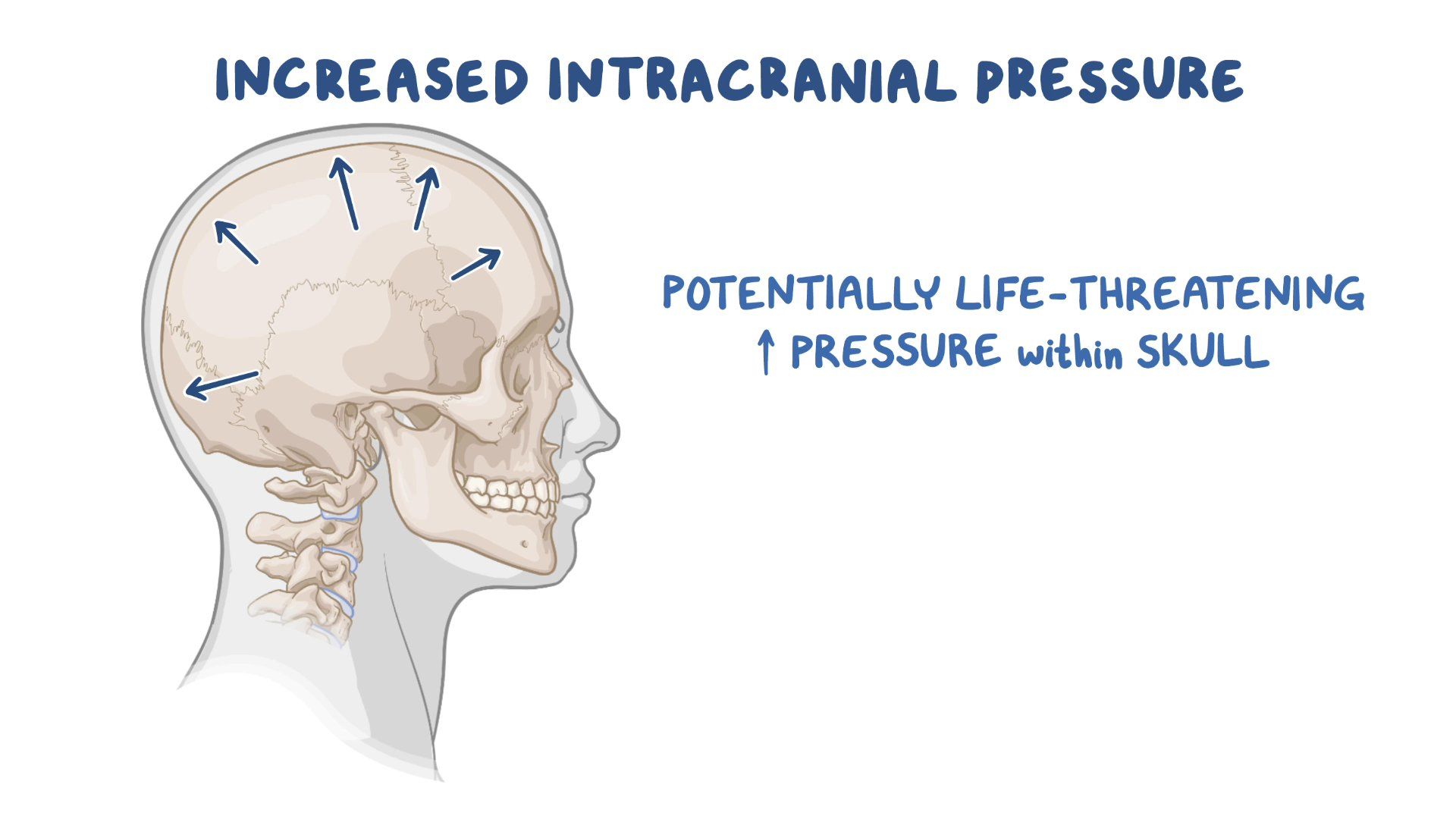
Prevention of hemorrhagic stroke
- The prevention of hemorrhagic stroke involves identifying and modifying risk factors, screening for vascular abnormalities, and taking prophylactic medications.
- The risk factors for hemorrhagic stroke include hypertension, smoking, alcohol abuse, obesity, diabetes mellitus, hyperlipidemia, atrial fibrillation, oral contraceptive use, anticoagulant use, illicit drug use, family history of stroke or aneurysm, and age.
- The screening for vascular abnormalities includes performing imaging studies such as CT scan, MRI scan, or angiography to detect aneurysms or malformations in asymptomatic patients who have a high risk of bleeding.
- The prophylactic medications include taking antihypertensive drugs to control blood pressure, antiplatelet drugs to prevent thrombosis in patients with ischemic stroke or transient ischemic attack (TIA), statins to lower cholesterol levels, and anticonvulsants to prevent seizures in patients with SAH.
Nursing Interventions of hemorrhagic stroke
- The nursing interventions for hemorrhagic stroke are based on the nursing process: assessment, diagnosis, planning, implementation, and evaluation.
- Assessment: The nurse should assess the patient's vital signs, neurological status (using tools such as Glasgow Coma Scale or NIH Stroke Scale), ICP and CPP (if monitored), oxygenation and ventilation (using pulse oximetry or arterial blood gas analysis), fluid and electrolyte balance (using intake and output measurement or laboratory tests), pain level (using scales such as Numeric Rating Scale or Wong-Baker Faces Scale), skin integrity (using tools such as Braden Scale or Norton Scale), nutritional status (using tools such as Body Mass Index or Albumin Level), bowel and bladder function (using tools such as Bristol Stool Chart or Urine Color Chart), psychosocial status (using tools such as Beck Depression Inventory or Hamilton Anxiety Rating Scale), and family support and coping skills.
- Diagnosis: The nurse should identify the patient's actual or potential problems related to hemorrhagic stroke.
- Some examples of nursing diagnoses are: Ineffective tissue perfusion related to bleeding in the brain;
- Increased intracranial pressure related to hematoma formation; Impaired physical mobility related to hemiparesis or hemiplegia;
- Impaired verbal communication related to aphasia or dysarthria; Impaired swallowing related to dysphagia; Risk for aspiration related to impaired cough reflex;
- Risk for infection related to invasive procedures or immunosuppression; Acute pain related to increased ICP or surgical incision; Anxiety related to fear of death or disability;
- Powerlessness related to loss of control or independence; Deficient knowledge related to disease process or treatment regimen.
- Planning: The nurse should establish goals and expected outcomes for the patient based on the nursing diagnoses.
- Some examples of goals are: The patient will maintain adequate tissue perfusion as evidenced by normal vital signs, neurological status, ICP, CPP, oxygenation, and glucose levels;
- The patient will demonstrate improved physical mobility as evidenced by increased range of motion, strength, and coordination;
- The patient will express understanding of verbal and nonverbal messages as evidenced by appropriate responses and feedback; The patient will swallow safely and effectively as evidenced by absence of coughing, choking, or aspiration;
- The patient will remain free from infection as evidenced by normal temperature, white blood cell count, and wound healing;
- The patient will report pain relief as evidenced by decreased pain score and increased comfort level; The patient will exhibit reduced anxiety as evidenced by relaxed demeanor, positive coping strategies, and verbalization of feelings;
- The patient will demonstrate knowledge of disease process and treatment regimen as evidenced by verbalization, return demonstration, or written materials.
- Implementation: The nurse should perform the interventions that are appropriate for the patient's condition and goals.
- Some examples of interventions are:
- Administer medications as prescribed to control blood pressure,
- reduce ICP,
- prevent seizures,
- prevent vasospasm,
- prevent or treat coagulopathy or infection,
- and provide sedation or analgesia;
- Monitor vital signs, neurological status, ICP, CPP, oxygenation, ventilation, fluid and electrolyte balance, glucose levels, pain level, skin integrity, nutritional status, bowel and bladder function, psychosocial status, and family support and coping skills;
- Maintain a patent airway, provide adequate ventilation, suction secretions as needed, and administer oxygen therapy as ordered;
- Ensure proper positioning and alignment of the patient, elevate the head of the bed to 30 degrees or as ordered, avoid extreme flexion or rotation of the neck, and prevent valsalva maneuver;
- Prevent aspiration and infection by performing oral hygiene, providing thickened liquids or pureed foods as indicated, using a nasogastric tube or a percutaneous endoscopic gastrostomy (PEG) tube for enteral feeding if necessary, and using sterile technique for invasive procedures;
- Promote physical mobility by performing passive or active range of motion exercises, applying splints or braces as needed, assisting with transfers and ambulation as tolerated, and providing assistive devices such as a cane or a walker if indicated;
- Enhance verbal communication by using simple and clear language, speaking slowly and loudly, allowing time for the patient to respond, using gestures or pictures to supplement verbal messages, and providing alternative methods of communication such as a pen and paper or an electronic device if needed;
- Improve swallowing by assessing the patient's gag reflex and swallow function before each feeding, placing the patient in an upright position during and after feeding, offering small bites and sips of food and liquid at a time, instructing the patient to tuck the chin down when swallowing, and observing for signs of aspiration such as coughing, choking, or wheezing; Educate the patient and family about the disease process and treatment regimen,
Transient Ischemic Attack (TIA)
- A TIA occurs when a blood clot or a piece of plaque blocks or narrows an artery that supplies blood to a part of the brain. The blockage is usually temporary and resolves within 24 hours, often within minutes or hours.
- The nervous system has three main functions: sensory, integrative, and motor
- Ischemia is reduced or interrupted blood flow to a part of the brain
- Hypoxia and anoxia are low or no oxygen levels in the affected brain tissue
- TIA is a temporary episode of neurological dysfunction caused by focal ischemia without infarction
- TIA is also known as a mini-stroke or a warning stroke
- TIA can indicate a high risk of a future stroke
- Stroke is a more severe form of ischemia that results in infarction and irreversible damage to the brain tissue
- There are two main types of stroke: ischemic stroke and hemorrhagic stroke
- The risk factors for TIA and ischemic stroke are similar
- The diagnosis of TIA is based on clinical observation, assessment of risk factors, and neuroimaging tests
- The management of TIA aims to prevent a future stroke by restoring blood flow, reducing modifiable risk factors, and using antiplatelet or anticoagulant medications
- The main arteries that supply blood to the brain are the internal carotid arteries and the vertebral arteries
- The internal carotid arteries branch into the anterior cerebral arteries and the middle cerebral arteries
- The vertebral arteries join to form the basilar artery, which branches into the posterior cerebral arteries
- The anterior, middle, and posterior cerebral arteries supply blood to different regions of the brain with different functions
- The ABCD2 score is a tool designed to predict the risk of stroke in the 3-90 days after a TIA
- The ABCD2 score is based on five factors: age, blood pressure, clinical features, duration of symptoms, and diabetes
- The ABCD2 score can help clinicians decide whether to admit a patient with TIA to the hospital or to manage them as an outpatient
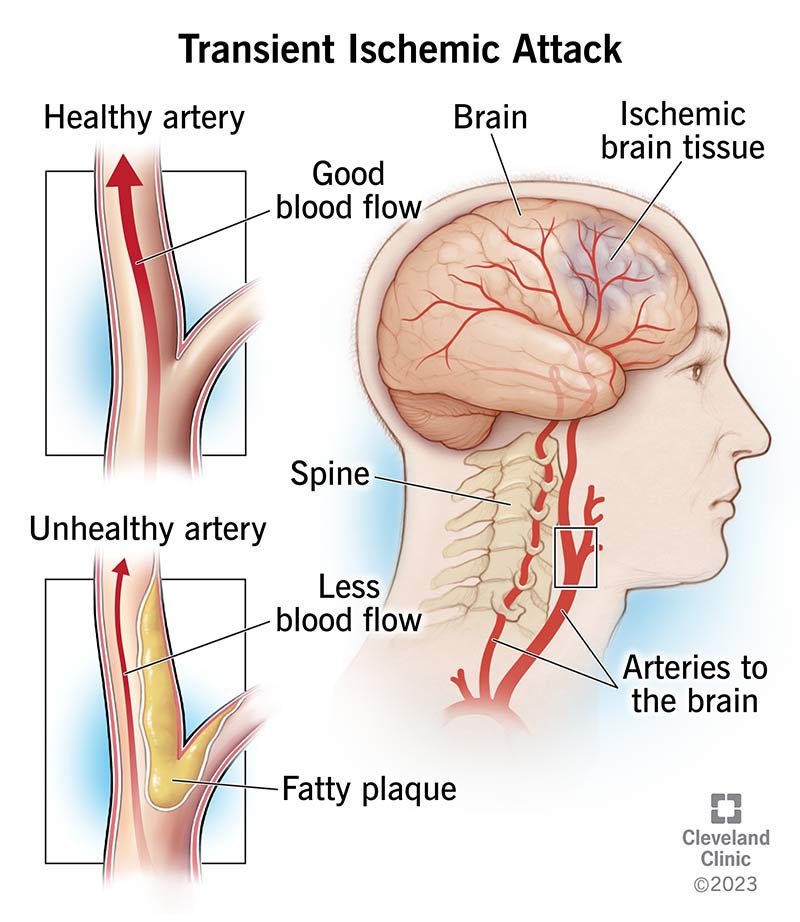
Symptoms of a Transient Ischemic Attack
- The symptoms of a TIA depend on which artery is affected and which region of the brain is deprived of blood. The symptoms may include:
- Weakness or numbness in one side of the face, arm, or leg
- Difficulty speaking or understanding speech
- Loss or blurring of vision in one or both eyes
- Dizziness, vertigo, or loss of balance
- Severe headache with no known cause
- The symptoms of a TIA are similar to those of an ischemic stroke, but they are reversible and do not cause permanent damage to the brain. However, a TIA is a serious medical emergency that requires immediate attention, because it can be a sign of an impending stroke.
- A stroke is a more severe form of ischemia that results in infarction and irreversible damage to the brain tissue.
- A stroke can cause lasting disability or death.
- There are two main types of stroke: ischemic stroke and hemorrhagic stroke.
- An ischemic stroke occurs when a blood clot or a piece of plaque blocks an artery that supplies blood to a part of the brain, causing infarction.
- A hemorrhagic stroke occurs when an artery in or around the brain ruptures, causing bleeding into the brain tissue or the surrounding space.
Risk factors for TIA
The risk factors for TIA and ischemic stroke are similar. They include:
- Age (older than 60 years)
- Hypertension (high blood pressure)
- Diabetes mellitus
- Hyperlipidemia (high cholesterol)
- Atrial fibrillation (irregular heartbeat)
- Smoking
- Obesity
- Physical inactivity
- Family history of stroke
- Previous history of TIA or stroke
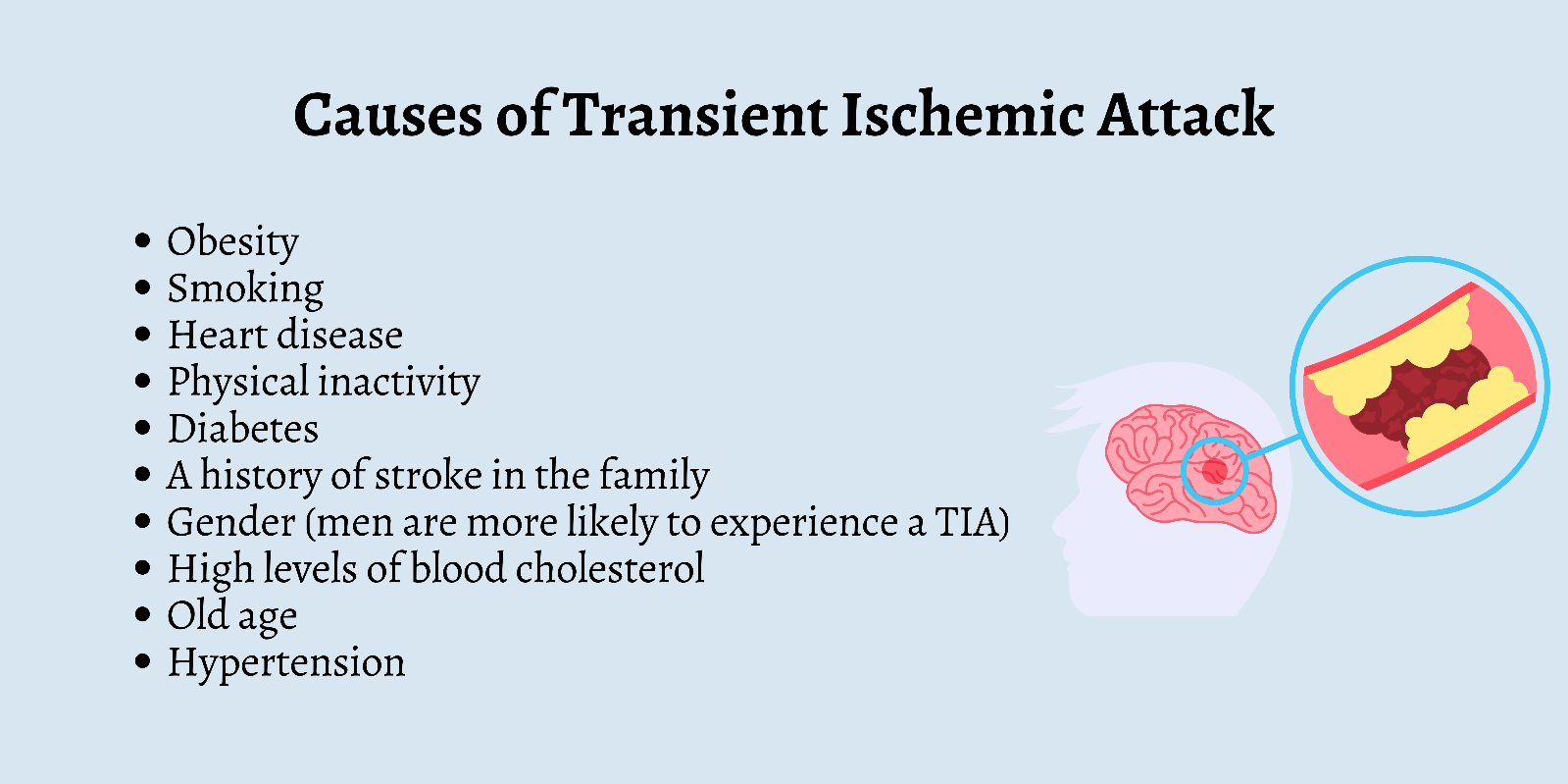
Diagnosis of TIA
- The diagnosis of TIA is based on clinical observation of signs and symptoms, assessment of risk factors, and neuroimaging tests.
- The neuroimaging tests include computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of the brain to rule out hemorrhage or infarction.
- Other tests may include carotid ultrasound, echocardiogram, electrocardiogram (EKG), blood tests, and angiography.

Management of TIA
- The management of TIA aims to prevent a future stroke by restoring blood flow to the affected area, reducing modifiable risk factors, and using antiplatelet or anticoagulant medications.
- Antiplatelet medications such as aspirin prevent platelets from sticking together and forming clots.
- Anticoagulant medications such as warfarin prevent blood from clotting.
- Some patients may also benefit from surgical procedures such as carotid endarterectomy or stenting to remove or widen a narrowed artery.
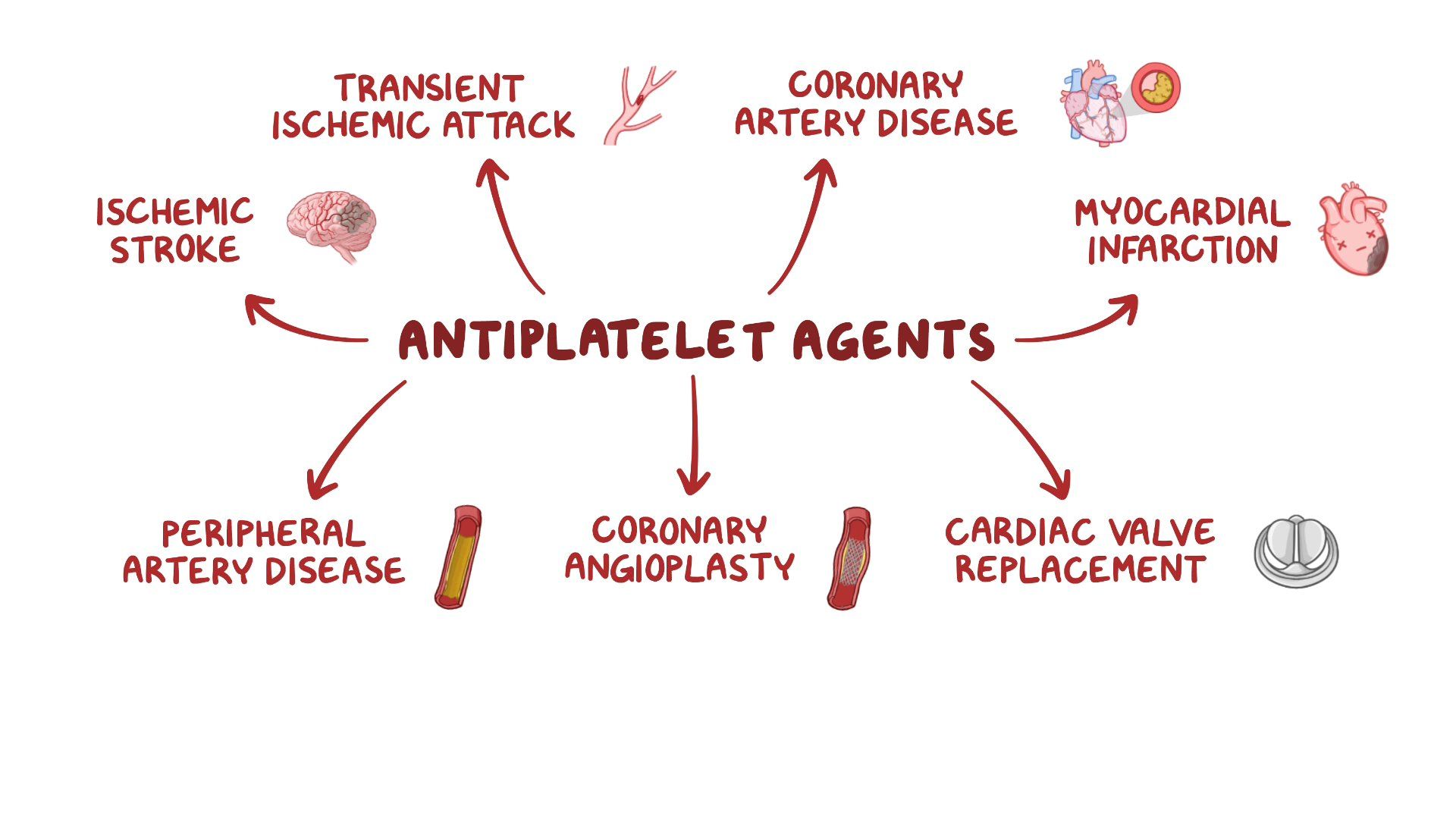
Main Arteries of the Brain
- The brain receives blood from two pairs of arteries: the internal carotid arteries and the vertebral arteries.
- The internal carotid arteries branch into the anterior cerebral arteries and the middle cerebral arteries.
- The vertebral arteries join to form the basilar artery, which branches into the posterior cerebral arteries.
- The anterior, middle, and posterior cerebral arteries supply blood to different regions of the brain.
- The regions and their functions are summarized in the table below.
|
Artery |
Region |
Function |
|
Anterior cerebral artery |
Frontal lobe |
Personality, judgment, planning, motor control |
|
Middle cerebral artery |
Temporal lobe, parietal lobe, part of frontal lobe |
Language, speech, hearing, sensation, spatial awareness |
|
Posterior cerebral artery |
Occipital lobe, part of temporal lobe |
Vision, memory |
- The anterior, middle, and posterior cerebral arteries are connected by smaller arteries called the circle of Willis. The circle of Willis provides collateral circulation in case of a blockage in one of the main arteries.
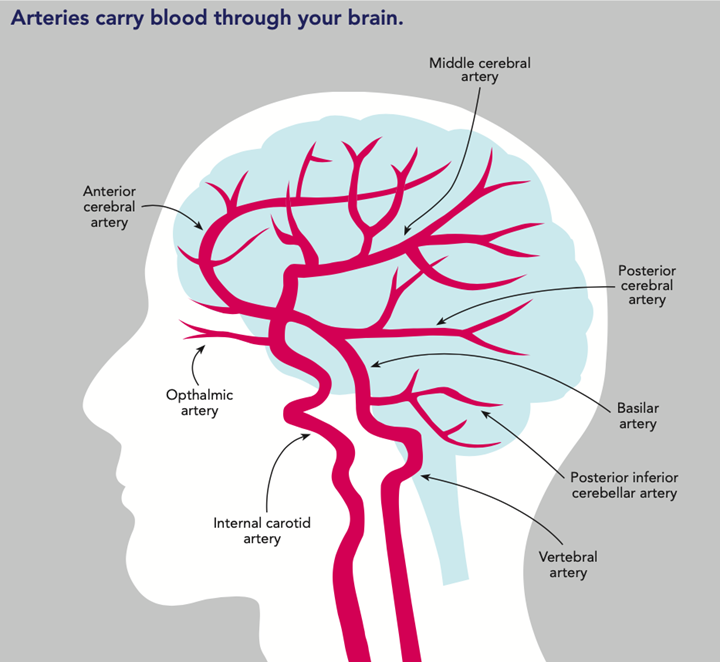
ABCD2 Score
- The ABCD2 score is a tool designed to predict the risk of stroke in the 3-90 days after a TIA.
- It is based on five factors: age, blood pressure, clinical features, duration of symptoms, and diabetes.
- Each factor is assigned a score from 0 to 2. The total score ranges from 0 to 7.
- The higher the score, the higher the risk of stroke.
- The score and the corresponding risk are shown in the table below.
|
Score |
Risk of stroke at 2 days (%) |
Risk of stroke at 90 days (%) |
|
0-3 |
1.0 |
3.1 |
|
4-5 |
4.1 |
9.8 |
|
6-7 |
8.1 |
17.8 |
- The ABCD2 score can help clinicians decide whether to admit a patient with TIA to the hospital or to manage them as an outpatient.
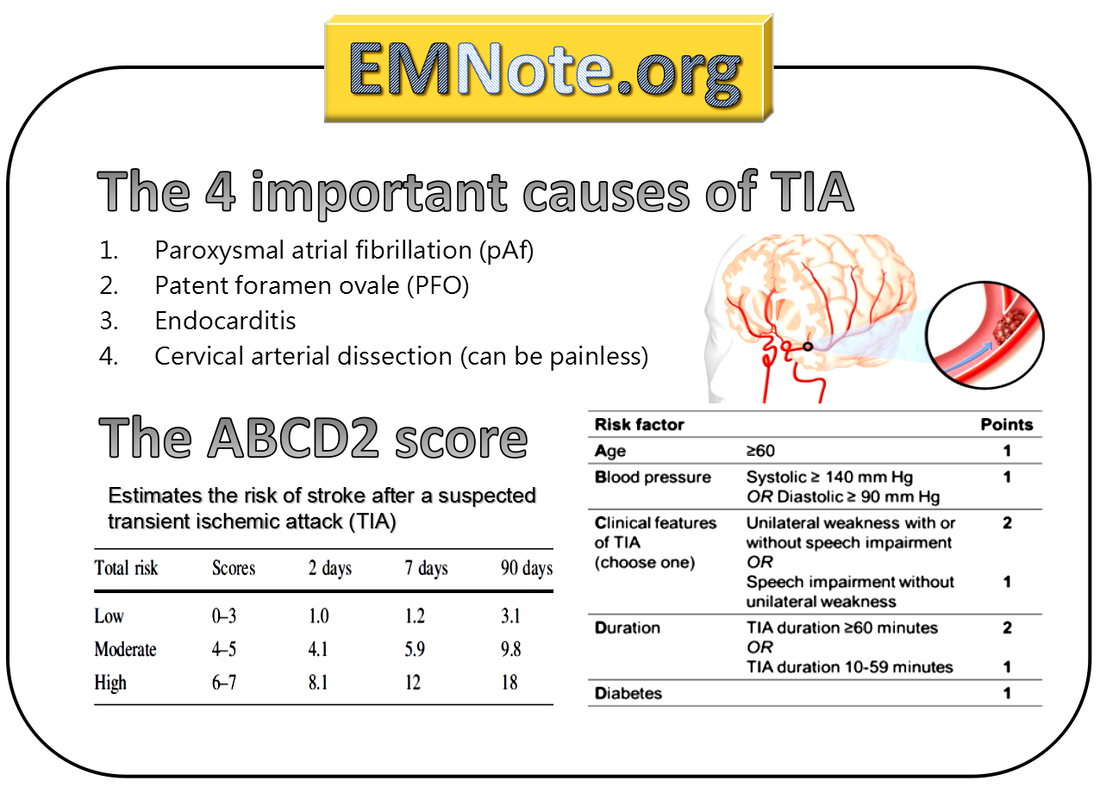
Peripheral Nervous System Disorders: Peripheral neuropathy; Radiculopathy; Charcot-Marie-Tooth disease
- Peripheral nervous system disorders are conditions that affect the nerves outside the brain and spinal cord. They can cause sensory, motor, or autonomic dysfunction depending on the type and location of nerve damage
- Peripheral nervous system disorders can be classified as mononeuropathy or polyneuropathy based on the number of nerves involved
- Mononeuropathy is a disorder that affects a single nerve or nerve branch. It can be caused by trauma, compression, entrapment, infection, inflammation, ischemia, or toxins. Examples of mononeuropathy include carpal tunnel syndrome, radial nerve palsy, ulnar nerve palsy, peroneal nerve palsy, and Bell’s palsy
- Polyneuropathy is a disorder that affects multiple nerves in a symmetrical pattern. It can be caused by systemic diseases, metabolic disorders, immune-mediated disorders, or inherited disorders. Examples of polyneuropathy include diabetic neuropathy, alcoholic neuropathy, Guillain-Barré syndrome, and Charcot-Marie-Tooth disease
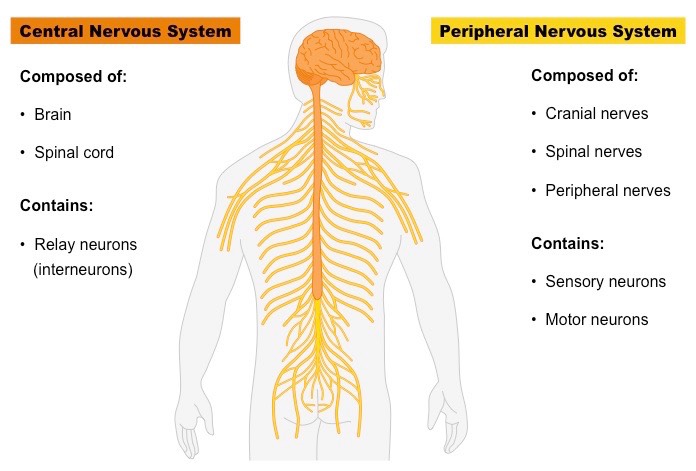
- Peripheral neuropathy is a term that encompasses any disorder that causes damage to the peripheral nerves. It can affect sensory, motor, or autonomic functions depending on the type and location of nerve damage
- Peripheral neuropathy can be classified as axonal or demyelinating based on the mechanism of nerve damage
- Axonal neuropathy is caused by injury to the axon (the long projection of the neuron that carries nerve impulses). It can result from metabolic disturbances, toxic exposures, ischemia, or inflammation. Axonal neuropathy can cause symptoms such as numbness, tingling, burning, or pain in the affected nerves. It can also cause muscle weakness, atrophy, or fasciculations in the affected muscles
- Demyelinating neuropathy is caused by injury to the myelin sheath (the fatty layer that surrounds and insulates the axon). It can result from immune-mediated disorders, inherited disorders, or infections. Demyelinating neuropathy can cause symptoms such as impaired sensation, reduced reflexes, or slowed nerve conduction in the affected nerves. It can also cause muscle weakness, spasticity, or paralysis in the affected muscles
- Peripheral neuropathy can be diagnosed by a detailed history taking, physical examination, neurological assessment (including sensory testing, motor testing, reflex testing, and autonomic testing), and electrodiagnostic studies (such as nerve conduction studies [NCS] or electromyography [EMG]). Laboratory tests (such as blood glucose, electrolytes, vitamin levels, liver function tests, kidney function tests, thyroid function tests, inflammatory markers, immunological markers, and genetic tests) are also performed to identify the underlying cause of peripheral neuropathy
- Peripheral neuropathy can be treated by addressing the underlying cause (such as controlling blood glucose levels in diabetic neuropathy or avoiding alcohol intake in alcoholic neuropathy), managing the symptoms (such as using analgesics, anticonvulsants, antidepressants, or topical agents for neuropathic pain or using orthotic devices, physical therapy, or occupational therapy for muscle weakness or atrophy), and preventing complications (such as avoiding injuries, infections, or ulcers in the affected areas or maintaining good nutrition and hydration)
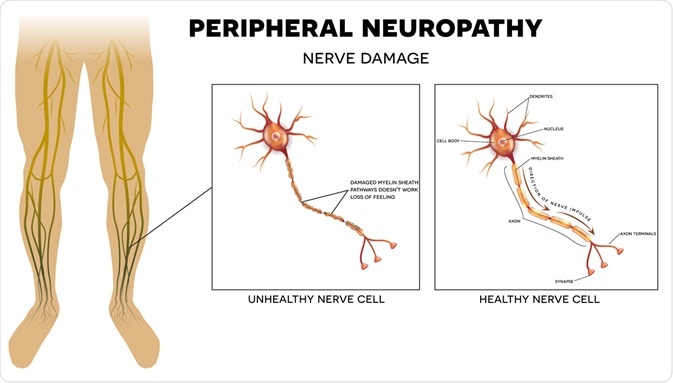
Types and Classifications of Peripheral Neuropathy:
Peripheral neuropathy can be classified according to the type of nerve affected, the pattern of nerve involvement, or the underlying cause. According to the type of nerve affected, peripheral neuropathy can be:
- Sensory neuropathy: affects the sensory nerves that carry information about sensations such as pain, temperature, touch, vibration, and position from the skin and muscles to the brain. Sensory neuropathy can cause numbness, tingling, burning, or loss of sensation in the affected areas.
- Motor neuropathy: affects the motor nerves that control the movement of muscles. Motor neuropathy can cause weakness, cramps, spasms, or paralysis of the affected muscles.
- Autonomic neuropathy: affects the autonomic nerves that regulate involuntary functions such as heart rate, blood pressure, digestion, sweating, and bladder control. Autonomic neuropathy can cause symptoms such as orthostatic hypotension, tachycardia, constipation, diarrhea, urinary retention or incontinence, erectile dysfunction, or abnormal sweating.
According to the pattern of nerve involvement, peripheral neuropathy can be:
- Mononeuropathy: affects a single nerve or a nerve group. Mononeuropathy is usually caused by trauma, compression, or entrapment of the nerve. Examples of mononeuropathy include carpal tunnel syndrome (median nerve), ulnar nerve palsy (ulnar nerve), radial nerve palsy (radial nerve), peroneal nerve palsy (peroneal nerve), or Bell’s palsy (facial nerve).
- Multiple mononeuropathy: affects two or more nerves in different areas. Multiple mononeuropathy is usually caused by an inflammatory or ischemic process that affects several nerves. Examples of multiple mononeuropathy include vasculitis (inflammation of blood vessels), diabetic amyotrophy (diabetic nerve damage), or mononeuritis multiplex (multiple nerve inflammation).
- Polyneuropathy: affects many nerves in a symmetrical and diffuse pattern. Polyneuropathy is usually caused by a systemic or metabolic disorder that affects the entire nervous system. Examples of polyneuropathy include diabetic peripheral neuropathy (diabetic nerve damage), alcoholic neuropathy (alcohol-induced nerve damage), Guillain-Barré syndrome (acute inflammatory demyelinating polyneuropathy), or Charcot-Marie-Tooth disease (inherited demyelinating polyneuropathy).
According to the underlying cause, peripheral neuropathy can be:
- Acquired: develops after birth due to various factors such as diabetes, trauma, infection, autoimmune diseases, toxins, metabolic disorders, nutritional deficiencies, or cancer.
- Hereditary: inherited from one or both parents due to genetic mutations that affect the structure or function of the nerves. Examples of hereditary peripheral neuropathies include Charcot-Marie-Tooth disease (inherited demyelinating polyneuropathy), familial amyloid polyneuropathy (inherited amyloid deposition in nerves), or Fabry disease (inherited lysosomal storage disorder).
- Idiopathic: has no known cause.
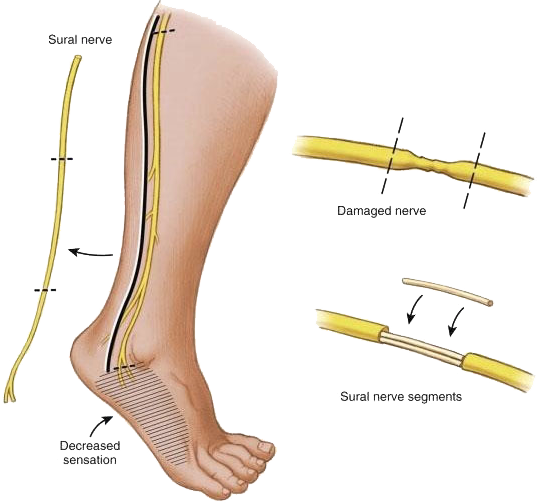
Pathophysiology of Peripheral Neuropathy:
The pathophysiology of peripheral neuropathy depends on the type and cause of nerve damage. In general, peripheral neuropathies can result from:
- Axonal degeneration: damage to the axon (the long projection of a nerve cell that carries electrical impulses) due to ischemia (lack of blood supply), toxins (such as alcohol or chemotherapy drugs), metabolic disorders (such as diabetes or uremia), or inflammation (such as in Guillain-Barré syndrome). Axonal degeneration leads to reduced nerve conduction velocity (NCV) and reduced amplitude of action potentials.
- Demyelination: damage to the myelin sheath (the fatty layer that surrounds and insulates some axons) due to autoimmune diseases (such as Guillain-Barré syndrome or multiple sclerosis), inherited disorders (such as Charcot-Marie-Tooth disease or metachromatic leukodystrophy), or toxins (such as lead or arsenic). Demyelination leads to slowed NCV and increased latency of action potentials.
- Wallerian degeneration: damage to the distal part of the axon and the myelin sheath following a nerve injury (such as a cut or a crush). Wallerian degeneration leads to loss of nerve function and regeneration of the nerve over time.
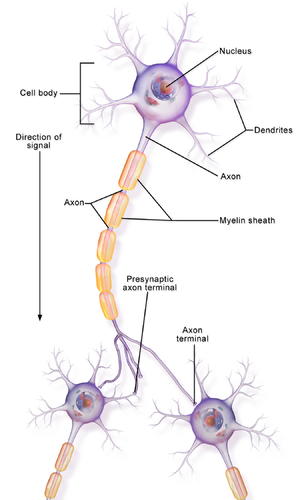
Clinical Manifestations and Diagnostic Tests for Peripheral Neuropathy:
The clinical manifestations of peripheral neuropathy depend on the type, location, and severity of nerve damage. The common signs and symptoms of peripheral neuropathy include:
- Sensory symptoms: numbness, tingling, burning, pain, or loss of sensation in the affected areas. Sensory symptoms usually start in the distal parts of the limbs (such as the toes or fingers) and progress proximally (towards the trunk). Sensory symptoms can affect the quality of life and increase the risk of injuries, infections, or ulcers in the affected areas.
- Motor symptoms: weakness, cramps, spasms, or paralysis of the affected muscles. Motor symptoms usually affect the proximal parts of the limbs (such as the thighs or arms) and progress distally. Motor symptoms can impair mobility and function and increase the risk of falls, fractures, or contractures in the affected areas.
- Autonomic symptoms: orthostatic hypotension (drop in blood pressure upon standing), tachycardia (fast heart rate), constipation, diarrhea, urinary retention or incontinence, erectile dysfunction, or abnormal sweating. Autonomic symptoms can affect various organ systems and cause complications such as fainting, cardiac arrhythmias, malnutrition, dehydration, or infections.
The diagnostic tests for peripheral neuropathy include:
- History and physical examination: to identify the possible causes, risk factors, and characteristics of the neuropathy.
- The history should include questions about medical conditions, medications, family history, alcohol intake, nutritional status, exposure to toxins, trauma, or infections.
- The physical examination should include a neurological examination to assess the sensory, motor, and autonomic functions of the nerves.
- The physical examination should also include a skin examination to look for signs of injuries, infections, or ulcers in the affected areas.
- Nerve conduction studies (NCS): to measure the NCV and amplitude of action potentials in the peripheral nerves.
- NCS can help determine the type (axonal or demyelinating), location (mononeuropathy or polyneuropathy), and severity (mild or severe) of nerve damage.
- NCS can also help differentiate between peripheral neuropathy and other neurological disorders that affect nerve function (such as myopathy or radiculopathy).
- Electromyography (EMG): to measure the electrical activity of muscles at rest and during contraction.
- EMG can help detect muscle denervation (loss of nerve supply) or reinnervation (regeneration of nerve supply) due to peripheral neuropathy.
- EMG can also help differentiate between peripheral neuropathy and other muscular disorders that affect muscle function (such as myopathy or myasthenia gravis).
- Blood tests: to identify the possible causes or complications of peripheral neuropathy.
- Blood tests may include glucose level (to diagnose diabetes), hemoglobin A1c level (to monitor diabetes control), vitamin B12 level (to diagnose vitamin B12 deficiency), thyroid function tests (to diagnose thyroid disorders), serum protein electrophoresis (to diagnose monoclonal gammopathy), erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level (to detect inflammation), antinuclear antibody (ANA) test (to diagnose autoimmune diseases), liver function tests (to diagnose liver disorders), kidney function tests (to diagnose kidney disorders), or urine screening (to detect toxins).
- Nerve biopsy: to obtain a sample of nerve tissue for microscopic examination.
- Nerve biopsy can help confirm the diagnosis of certain types of peripheral neuropathies that have characteristic histological features (such as vasculitis, amyloidosis, leprosy, or sarcoidosis).
- Nerve biopsy is usually reserved for cases where other diagnostic tests are inconclusive or contradictory.
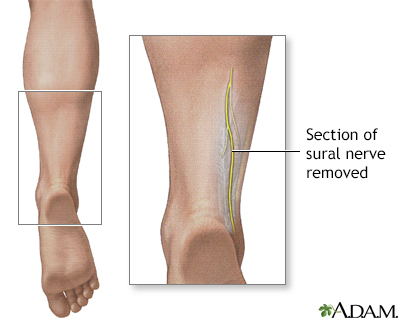
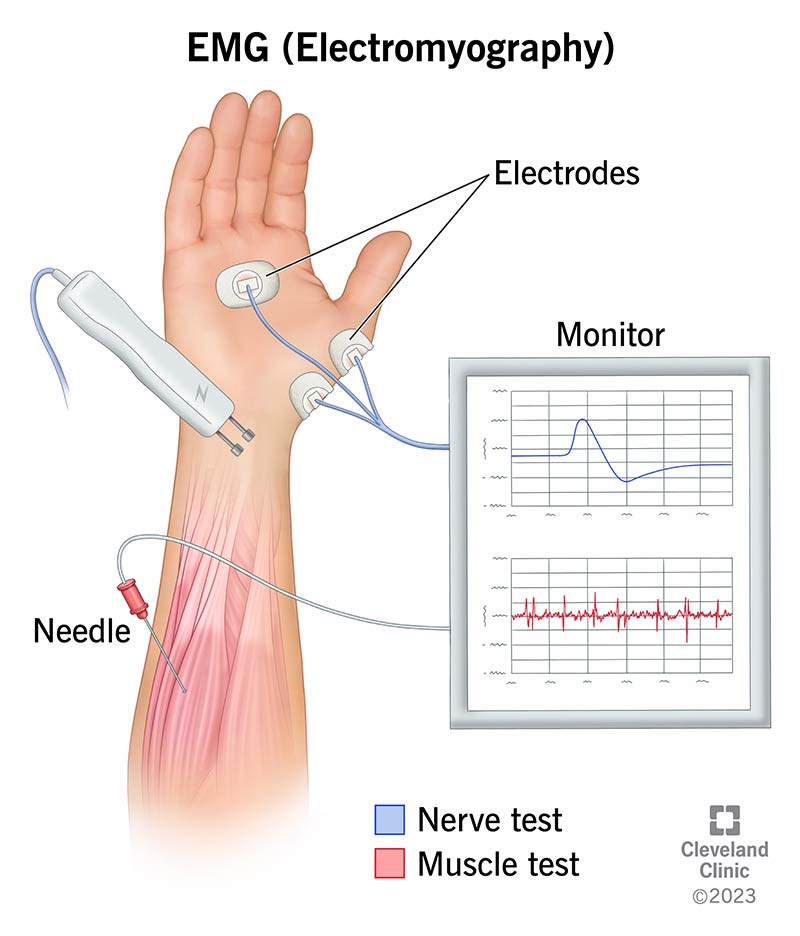
Treatment and Nursing Care for Peripheral Neuropathy:
- The treatment and nursing care for peripheral neuropathy depend on the cause, type, and severity of nerve damage. The general goals of treatment and nursing care are to:
- Treat the underlying cause: if possible, identify and treat the cause of peripheral neuropathy to prevent further nerve damage or complications. For example, control blood glucose level in diabetic neuropathy, avoid alcohol intake in alcoholic neuropathy, correct vitamin B12 deficiency in pernicious anemia neuropathy, use immunosuppressive drugs in autoimmune neuropathy, remove toxins in toxic neuropathy, or treat infections in infectious neuropathy.
- Manage pain: use pharmacological and non-pharmacological methods to relieve pain caused by peripheral neuropathy. Pharmacological methods
Pharmacological methods include:
- Analgesics: drugs that reduce pain by blocking pain signals or receptors. Examples of analgesics include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, acetaminophen, opioids such as morphine or oxycodone, or topical agents such as lidocaine or capsaicin.
- Anticonvulsants: drugs that reduce pain by stabilizing nerve membranes and inhibiting the transmission of abnormal nerve impulses. Examples of anticonvulsants include gabapentin, pregabalin, carbamazepine, or phenytoin.
- Antidepressants: drugs that reduce pain by enhancing the activity of neurotransmitters such as serotonin and norepinephrine that modulate pain perception. Examples of antidepressants include tricyclic antidepressants such as amitriptyline or nortriptyline, selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine or paroxetine, or serotonin-norepinephrine reuptake inhibitors (SNRIs) such as duloxetine or venlafaxine.
Non-pharmacological methods include:
- Physical therapy: exercises that improve muscle strength, flexibility, and coordination and prevent muscle atrophy, contractures, or deformities. Physical therapy can also include modalities such as massage, heat, cold, ultrasound, electrical stimulation, or transcutaneous electrical nerve stimulation (TENS) that improve blood circulation, reduce inflammation, or stimulate nerve regeneration.
- Occupational therapy: activities that enhance functional ability and independence in daily living tasks such as dressing, bathing, eating, or working. Occupational therapy can also include adaptive devices such as braces, splints, orthotics, or prosthetics that support or replace the function of the affected limbs.
- Cognitive-behavioral therapy (CBT): techniques that help cope with pain and improve emotional well-being by changing negative thoughts and behaviors that worsen pain. CBT can also include relaxation methods such as deep breathing, progressive muscle relaxation, guided imagery, or meditation that reduce stress and anxiety associated with pain.
- Alternative therapies: approaches that may provide relief from pain or improve quality of life by using natural or holistic methods. Examples of alternative therapies include acupuncture, acupressure, biofeedback, hypnosis, aromatherapy, herbal remedies, or dietary supplements.
- Prevent complications: monitor and manage the potential complications of peripheral neuropathy such as injuries, infections, ulcers, falls, fractures, cardiac arrhythmias, malnutrition, dehydration, or urinary tract infections. Preventive measures include:
- Educating the patient and family about the causes, symptoms, and treatment of peripheral neuropathy and the importance of regular follow-up and self-care.
- Inspecting the skin and feet daily for signs of injuries, infections, or ulcers and applying moisturizer to prevent dryness and cracking. Wearing comfortable shoes and socks and avoiding tight-fitting clothing or footwear that may cause pressure or friction. Seeking medical attention for any wounds or infections promptly.
- Using assistive devices such as a cane, walker, wheelchair, or handrails to maintain balance and prevent falls. Removing any hazards or obstacles in the home environment that may cause tripping or slipping. Wearing protective gear such as a helmet or pads when engaging in physical activities.
- Monitoring vital signs such as blood pressure, heart rate, temperature, and oxygen saturation regularly and reporting any abnormal findings to the health care provider. Taking medications as prescribed and avoiding substances that may affect the autonomic nervous system such as caffeine, alcohol, nicotine, or illicit drugs.
- Eating a balanced diet that provides adequate calories, protein, vitamins, minerals, and fluids to support nerve function and healing. Avoiding foods that may worsen neuropathy symptoms such as spicy foods, artificial sweeteners
- artificial sweeteners, or alcohol. Taking supplements that may improve nerve health such as vitamin B complex, alpha-lipoic acid, or omega-3 fatty acids as recommended by the health care provider.
- Drinking enough fluids to prevent dehydration and maintain blood volume and pressure. Avoiding sudden changes in posture that may cause orthostatic hypotension. Using compression stockings or medications that may increase blood pressure as prescribed by the health care provider.
- Emptying the bladder regularly and completely to prevent urinary retention or infection. Using catheters or medications that may improve bladder function as prescribed by the health care provider. Practicing good hygiene and avoiding irritants or allergens that may cause urinary tract infections.
- Seeking help for sexual dysfunction that may result from peripheral neuropathy. Using lubricants, devices, or medications that may enhance sexual performance or satisfaction as recommended by the health care provider. Communicating with the partner and exploring alternative ways of intimacy and pleasure.
Radiculopathy
- The nervous system is a complex network of cells that communicate with each other and coordinate the functions of the body.
- It consists of two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS).
- The CNS includes the brain and the spinal cord, which are protected by the skull and the vertebral column.
- The PNS includes the cranial nerves, which emerge from the brain, and the spinal nerves, which emerge from the spinal cord.
- The spinal nerves branch into smaller nerves that innervate different parts of the body.
- The nervous system can be affected by various diseases and disorders that impair its normal function and cause neurological symptoms.
- One of these conditions is radiculopathy, which is a clinical term for a pinched or compressed nerve root in the spine.
- The nerve root is where the nerve exits the spinal cord and joins the peripheral nerve. When a nerve root is pinched, it becomes inflamed and irritated, resulting in pain, weakness, numbness, tingling, or difficulty controlling specific muscles.
- Radiculopathy can occur at any level of the spine, but it is more common in the cervical (neck) and lumbar (lower back) regions.
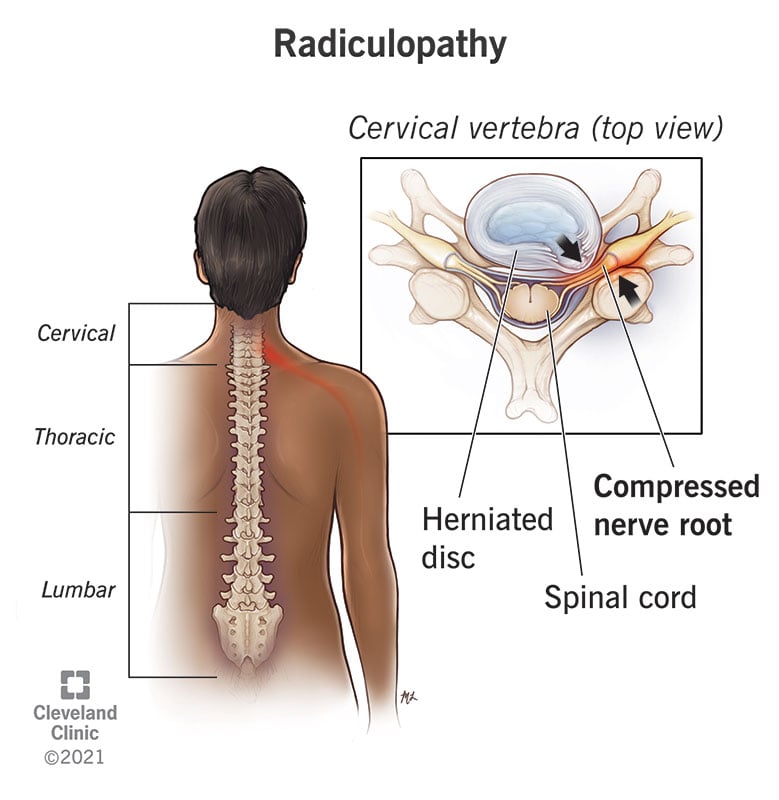
Causes and Mechanisms of Nerve Injury and Dysfunction
- Nerve injury and dysfunction can be caused by various factors, such as trauma, inflammation, infection, degeneration, compression, ischemia, toxins, or metabolic disorders.
- These factors can damage the nerve cells (neurons) or their supporting cells (glia), as well as their axons (nerve fibers) or myelin sheath (protective covering).
- Depending on the type, severity, location, and duration of the injury, nerve damage can be classified into three categories:
- Neuropraxia: This is a mild form of nerve injury that involves a temporary loss of function due to compression or ischemia of the nerve. The nerve structure remains intact, but its conduction is impaired. This type of injury usually recovers within days to weeks without permanent damage.
- Axonotmesis: This is a moderate form of nerve injury that involves a disruption of the axon and its myelin sheath due to stretching or crushing of the nerve. The nerve cell body and connective tissue remain intact, but the axon degenerates distal to the site of injury. This type of injury may recover within months to years with partial or complete regeneration of the axon.
- Neurotmesis: This is a severe form of nerve injury that involves a complete transection or rupture of the nerve due to laceration or avulsion. The nerve cell body, axon, myelin sheath, and connective tissue are all damaged beyond repair. This type of injury results in permanent loss of function and sensation.
- Radiculopathy is usually caused by compression or irritation of the nerve root due to narrowing of the space where it exits the spine.
- This can be due to various conditions that affect the spinal column, such as:
- Herniated disc: This is when a part of an intervertebral disc (a cushion between two vertebrae) protrudes out of its normal position and presses on a nearby nerve root.
- Spinal stenosis: This is when the spinal canal (the space that contains the spinal cord) or the intervertebral foramen (the opening where a nerve root exits) becomes narrowed due to bone spurs, thickened ligaments, or arthritis.
- Spondylolisthesis: This is when one vertebra slips forward over another vertebra due to a fracture or weakness in the spine.
- Spondylosis: This is a general term for degenerative changes in the spine due to aging or wear and tear.
- Spinal tumor: This is an abnormal growth of cells in or near the spine that can compress or invade a nerve root.
- Spinal infection: This is an inflammation or infection of the spine that can cause swelling or abscess formation around a nerve root.
- Spinal trauma: This is an injury to the spine due to an accident or violence that can cause fracture, dislocation, or hematoma around a nerve root.
- When a nerve root is compressed or irritated, it triggers an inflammatory response that releases chemical mediators such as prostaglandins, cytokines, histamine, bradykinin, substance P, and glutamate.
- These mediators activate nociceptors (pain receptors) on the nerve fibers and cause the transmission of pain signals to the spinal cord and the brain.
- The mediators also increase the sensitivity of the nerve fibers to mechanical, thermal, or chemical stimuli, resulting in hyperalgesia (increased pain response) and allodynia (pain response to normally non-painful stimuli).
- In addition, the compression or irritation of the nerve root can impair the conduction of motor and sensory signals along the nerve fibers, resulting in weakness, numbness, tingling, or difficulty controlling specific muscles.
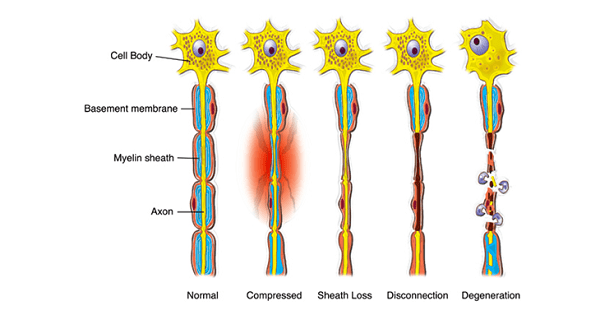
Signs and Symptoms of Radiculopathy and How It Is Diagnosed
- The signs and symptoms of radiculopathy depend on the level and location of the affected nerve root, as well as the type and severity of the compression or irritation.
- The most common symptom is radicular pain, which is a sharp, shooting, or burning pain that radiates along the course of the nerve from the spine to the extremity.
- The pain may be worsened by certain movements or positions of the spine, such as coughing, sneezing, bending, or twisting.
- The pain may also be accompanied by paresthesia (abnormal sensations such as tingling, pins and needles, or numbness) or dysesthesia (unpleasant sensations such as burning, itching, or electric shock).
- Other symptoms may include weakness, atrophy (wasting), or fasciculations (twitching) of the muscles innervated by the affected nerve root.
- The diagnosis of radiculopathy is based on a combination of history, physical examination, and diagnostic tests.
- The history should include information about the onset, duration, frequency, intensity, quality, location, distribution, and aggravating or relieving factors of the symptoms.
- The physical examination should include a neurological assessment that evaluates the motor function, sensory function, reflexes, and coordination of the affected area.
- The examination should also include a spinal assessment that evaluates the posture, alignment, range of motion, tenderness, deformity, and stability of the spine.
- The diagnostic tests may include:
- Imaging studies: These are used to visualize the structure and anatomy of the spine and identify any abnormalities that may cause radiculopathy. The most common imaging studies are X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, and myelography (an X-ray with contrast dye injected into the spinal canal).
- Electromyography (EMG) and nerve conduction studies (NCS): These are used to measure the electrical activity and conduction of the nerves and muscles and identify any damage or dysfunction. EMG involves inserting fine needles into the muscles and recording their electrical signals. NCS involves applying electrical stimuli to the skin over the nerves and recording their responses.
- Selective nerve root blocks (SNRB): These are used to confirm the diagnosis and provide temporary relief of radicular pain. SNRB involves injecting a local anesthetic and a steroid into a specific nerve root under fluoroscopic (X-ray) guidance. If the injection reduces or eliminates the pain, it indicates that the injected nerve root is responsible for the symptoms.

Common Types and Locations of Radiculopathy and Their Associated Nerve Roots
- Radiculopathy can occur at any level of the spine, but it is more common in the cervical (neck) and lumbar (lower back) regions.
- This is because these regions have more mobility and flexibility than other parts of the spine, making them more prone to injury and degeneration.
- The thoracic (upper middle back) region is less commonly affected by radiculopathy because it has less mobility and is more stabilized by the rib cage.
- The common types and locations of radiculopathy and their associated nerve roots are:
- Cervical radiculopathy: This affects the nerve roots in the cervical spine (C1-C8), which innervate the neck, shoulders, arms, hands, and fingers. The most common levels are C5-C7. The symptoms may include:
- C5 radiculopathy: Pain in the shoulder blade and outer arm; weakness in shoulder abduction (raising arm sideways) and elbow flexion (bending arm); diminished biceps reflex; numbness or tingling in thumb side of hand.
- C6 radiculopathy: Pain in the neck, shoulder blade, outer arm, thumb, index finger; weakness in elbow flexion and wrist extension (bending hand backward); diminished brachioradialis reflex; numbness or tingling in thumb index finger.
- C7 radiculopathy: Pain in the neck, shoulder blade, middle arm, middle finger; weakness in elbow extension (straightening arm) and wrist flexion (bending hand forward); diminished triceps reflex; numbness or tingling in middle finger.
- C8 radiculopathy: Pain in neck, shoulder blade, inner arm, ring and little finger; weakness in finger flexion (bending fingers) and extension (straightening fingers); diminished finger flexor reflex; numbness or tingling in ring and little finger.
- Lumbar radiculopathy: This affects the nerve roots in the lumbar spine (L1-L5), which innervate the lower back, buttocks, legs, feet, and toes. The most common levels are L4-L5 and L5-S1. The symptoms may include:
- L4 radiculopathy: Pain in the lower back, buttock, outer thigh, inner calf, and big toe; weakness in knee extension (straightening leg) and ankle dorsiflexion (lifting foot upward); diminished patellar reflex; numbness or tingling in big toe.
- L5 radiculopathy: Pain in the lower back, buttock, outer thigh, outer calf, and top of foot; weakness in hip abduction (moving leg sideways) and ankle dorsiflexion; diminished medial hamstring reflex; numbness or tingling in top of foot and toes.
- S1 radiculopathy: Pain in the lower back, buttock, back of thigh, back of calf, and outer edge of foot; weakness in hip extension (moving leg backward) and ankle plantarflexion (pushing foot downward); diminished Achilles reflex; numbness or tingling in outer edge of foot and little toe.
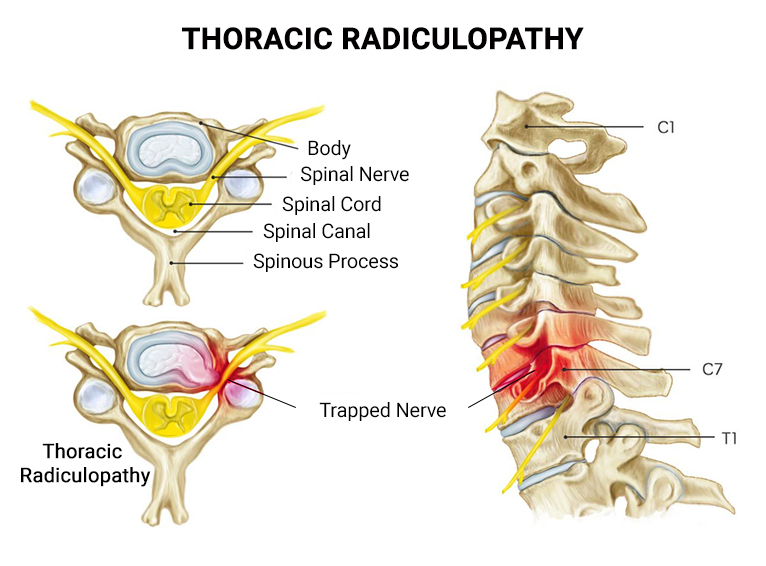
Treatment Options and Nursing Interventions for Radiculopathy
- The treatment options for radiculopathy depend on the cause, severity, duration, and location of the nerve root compression or irritation.
- The main goals of treatment are to relieve pain, reduce inflammation, restore function, and prevent complications. The treatment options may include:
- Conservative management: This involves non-surgical methods such as medication, physical therapy, exercise, massage, heat or cold therapy, acupuncture, traction, or spinal manipulation. These methods aim to reduce pain and inflammation, improve blood flow and nerve conduction, relax muscles and spasms, increase range of motion and flexibility, and strengthen muscles and posture. Conservative management is usually the first line of treatment for mild to moderate cases of radiculopathy that are not associated with severe neurological deficits or progressive symptoms.
- Interventional procedures: These involve minimally invasive methods such as injections or radiofrequency ablation. These methods aim to block or reduce pain signals from the affected nerve root by delivering a local anesthetic, a steroid, or a heat lesion. Interventional procedures are usually reserved for cases of radiculopathy that do not respond to conservative management or have severe pain that interferes with daily activities.
- Surgery: This involves invasive methods such as decompression or fusion. These methods aim to remove or stabilize the source of nerve root compression or irritation by removing a herniated disc, a bone spur, a tumor, or an infection; or by fusing two or more vertebrae together with screws, rods, plates, or cages. Surgery is usually considered as a last resort for cases of radiculopathy that have significant neurological deficits or progressive symptoms that do not improve with other treatments.
- The nursing interventions for radiculopathy are based on the assessment of the patient’s condition and the implementation of the prescribed treatment plan.
- The nursing interventions may include:
- Pain management: This involves administering analgesics (painkillers) as prescribed; monitoring pain level and response to treatment; educating the patient about pain relief options and their side effects; providing comfort measures such as positioning, massage, heat cold therapy; and encouraging relaxation techniques such as breathing exercises, meditation, or distraction.
- Neurological assessment: This involves monitoring motor function, sensory function, reflexes, and coordination of the affected area; reporting any changes or abnormalities; and documenting any neurological deficits or improvements.
- Functional assessment: This involves monitoring mobility, range of motion, strength, balance, and coordination of the affected area; assisting with activities of daily living (ADLs) such as dressing, bathing, feeding, or toileting; and providing assistive devices such as braces, splints, or crutches if needed.
- Physical therapy: This involves collaborating with the physical therapist to provide exercises, stretching, massage, traction, or spinal manipulation to the affected area; encouraging the patient to participate in the therapy sessions; and reinforcing the home exercise program.
- Patient education: This involves educating the patient about the cause, mechanism, signs symptoms of radiculopathy; the treatment options their benefits risks; the expected outcomes potential complications; the prevention strategies such as maintaining good posture, avoiding heavy lifting twisting bending of the spine; and the follow-up care such as regular check-ups imaging studies or EMG/NCS.
- Emotional support: This involves providing psychological support to the patient who may experience anxiety, depression, fear, or frustration due to radiculopathy; listening to the patient’s concerns feelings; and providing coping strategies such as counseling, support groups, or referral to a mental health professional if needed.
Outcomes and Potential Complications of Radiculopathy
The outcomes and potential complications of radiculopathy depend on the cause, severity, duration, and location of the nerve root compression or irritation, as well as the type and effectiveness of the treatment. The possible outcomes and complications are:
- Complete recovery: This is when the nerve root compression or irritation is resolved and the patient regains normal function and sensation of the affected area. This outcome is more likely for mild to moderate cases of radiculopathy that are treated early and conservatively.
- Partial recovery: This is when the nerve root compression or irritation is improved but not completely resolved and the patient has some residual symptoms or deficits of the affected area. This outcome is more common for moderate to severe cases of radiculopathy that are treated late or invasively.
- No recovery: This is when the nerve root compression or irritation is persistent or progressive and the patient has no improvement or worsening of the symptoms or deficits of the affected area. This outcome is rare but possible for severe cases of radiculopathy that are associated with irreversible nerve damage or complications.
- Complications: These are adverse events that may occur during or after the treatment of radiculopathy. They may include infection, bleeding, hematoma, nerve injury, spinal cord injury, spinal instability, failed back surgery syndrome, chronic pain, disability, or death.
Charcot-Marie-Tooth disease
- The nervous system is a complex network of cells that communicate with each other and coordinate the body’s functions1.
- The nervous system consists of two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS)1.
- The CNS includes the brain and the spinal cord, which process and integrate sensory and motor information1.
- The PNS includes all the nerves that connect the CNS to the rest of the body, such as the cranial nerves, spinal nerves, and autonomic nerves1.
- The PNS can be divided into two functional categories: the somatic nervous system (SNS) and the autonomic nervous system (ANS)1.
- The SNS controls voluntary movements and sensations, such as walking, talking, seeing, hearing, etc.1
- The ANS controls involuntary functions, such as heart rate, blood pressure, digestion, etc.1
- Charcot-Marie-Tooth disease (CMT) is a group of inherited disorders that cause damage to the peripheral nerves3.
- CMT is also known as hereditary motor and sensory neuropathy (HMSN), because it affects both motor and sensory nerve fibers3.
- CMT is one of the most common inherited neurological disorders, affecting about 1 in 2500 people worldwide3.
- CMT is caused by mutations in different genes that affect either the structure or function of peripheral nerve fibers or their myelin sheath3.
- CMT can be inherited in different patterns: autosomal dominant (AD), autosomal recessive (AR), or X-linked (XL)3.
- AD means that one copy of the mutated gene from either parent is enough to cause the disease3.
- AR means that two copies of the mutated gene from both parents are needed to cause the disease3.
- XL means that the mutated gene is located on the X chromosome, which determines sex3. Males have one X chromosome and one Y chromosome, while females have two X chromosomes. Therefore, males are more likely to develop XL-CMT than females3.
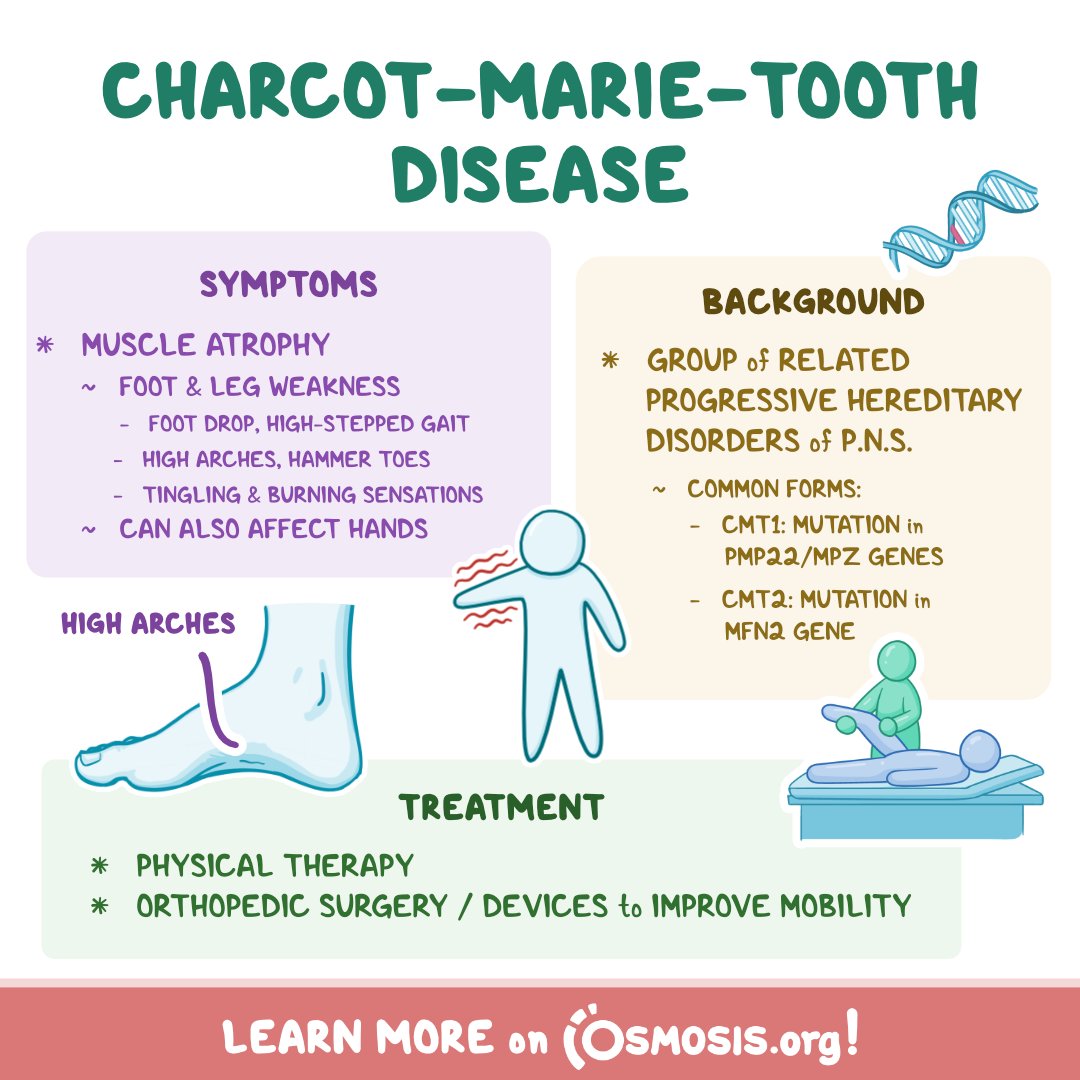
Peripheral nerves
- Peripheral nerves are bundles of nerve fibers that transmit signals between the CNS and the body2.
- Peripheral nerves are composed of two types of nerve fibers: motor fibers and sensory fibers2.
- Motor fibers carry impulses from the CNS to the muscles, causing them to contract2.
- Sensory fibers carry impulses from the receptors in the skin, muscles, joints, and organs to the CNS, providing information about touch, pain, temperature, position, etc.2
- Peripheral nerves are also surrounded by a protective layer called the myelin sheath2.
- Myelin is a fatty substance that insulates and speeds up the conduction of nerve impulses2.
- Myelin is produced by specialized cells called Schwann cells in the PNS and oligodendrocytes in the CNS2.
Classification of Charcot-Marie-Tooth disease (CMT)
CMT can be classified into different types based on the genetic mutation, inheritance pattern, clinical features, and nerve conduction studies4.
-
- CMT type 1 (CMT1) is caused by mutations in genes that affect the myelin sheath of peripheral nerves. It is usually inherited in an AD manner. It causes slow nerve conduction velocity (NCV), which measures how fast nerve impulses travel. The symptoms usually begin in childhood or adolescence. It affects both motor and sensory nerves, causing muscle weakness and atrophy, sensory loss, foot deformities, balance problems, etc.4
- CMT type 2 (CMT2) is caused by mutations in genes that affect the axons of peripheral nerves. It is usually inherited in an AD manner. It causes normal or slightly reduced NCV. The symptoms usually begin in late adolescence or adulthood. It affects mainly motor nerves, causing muscle weakness and atrophy in distal limbs. Sensory loss may be mild or absent4.
- CMT type 3 (CMT3) is also known as Dejerine-Sottas disease. It is caused by severe mutations in genes that affect the myelin sheath of peripheral nerves. It can be inherited in an AD or AR manner. It causes very slow NCV. The symptoms usually begin in infancy or early childhood. It affects both motor and sensory nerves, causing severe muscle weakness and atrophy, sensory loss, foot deformities, scoliosis, etc.4
- CMT type 4 (CMT4) is caused by mutations in genes that affect either the myelin sheath or the axons of peripheral nerves. It is inherited in an AR manner. It causes variable NCV. The symptoms usually begin in childhood or adolescence. It affects both motor and sensory nerves, causing muscle weakness and atrophy, sensory loss, foot deformities, scoliosis, etc. Some subtypes of CMT4 may also cause optic atrophy, deafness, or respiratory failure4.
- CMT type X (CMTX) is caused by mutations in genes that are located on the X chromosome. It is inherited in an XL manner. It causes variable NCV. The symptoms usually begin in childhood or adolescence. It affects both motor and sensory nerves, causing muscle weakness and atrophy, sensory loss, foot deformities, etc. Males are more severely affected than females4.
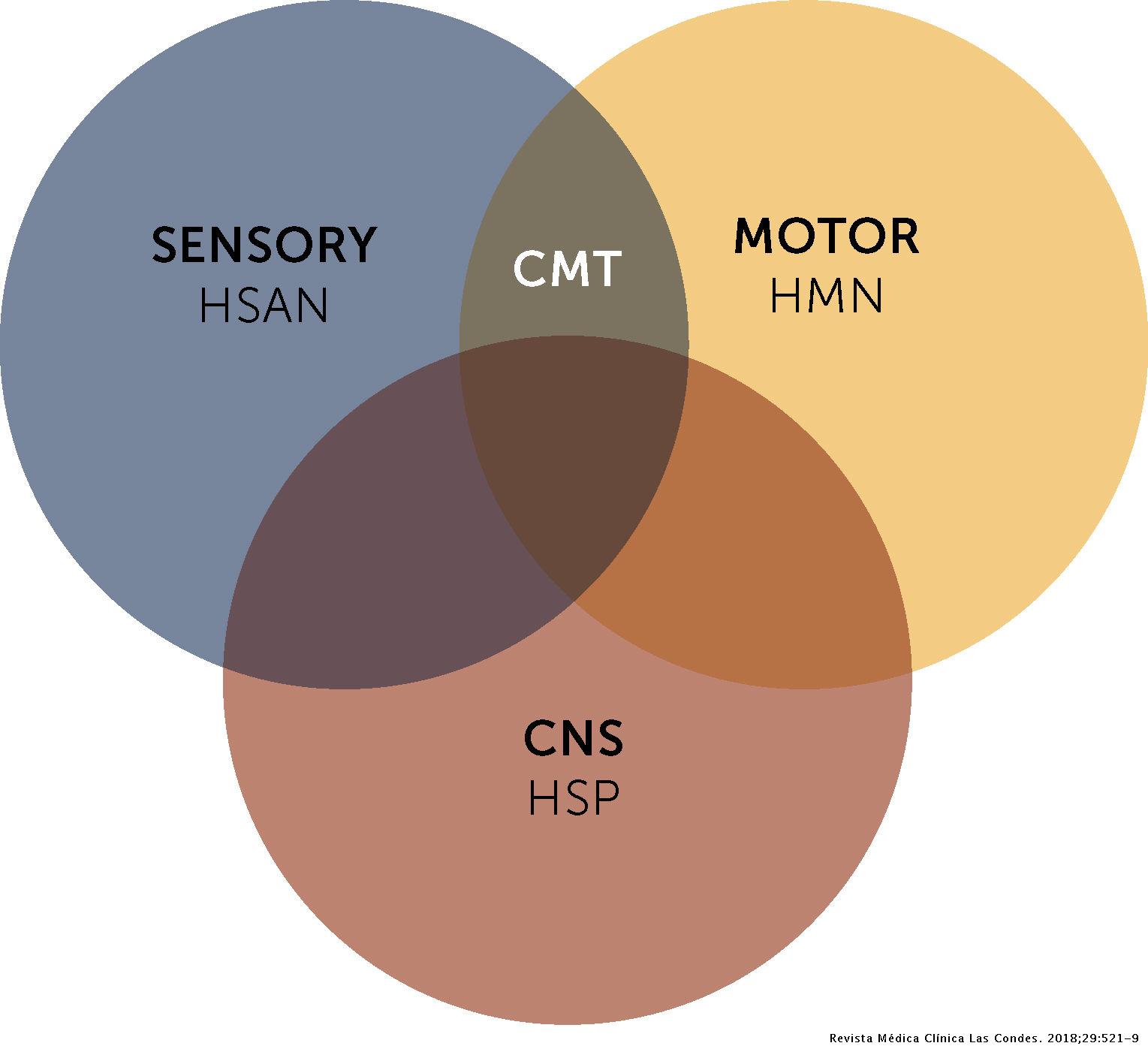
Signs and symptoms of CMT
- The signs and symptoms of CMT vary depending on the type, subtype, and severity of the disease5.
- The most common signs and symptoms of CMT include5:
- Weakness or paralysis of the foot and lower leg muscles, which can cause difficulty lifting the foot (foot drop)
- A high-stepped gait with frequent tripping or falling
- Balance problems
- Foot deformities, such as high arches and curled toes (hammertoes)
- Lower legs may take on an "inverted champagne bottle" shape due to the loss of muscle bulk
- Reduced ability to feel heat, cold, and touch
- Weakness and atrophy may occur in the hands, causing difficulty with fine motor skills
- Decreased sense of vibration and position (proprioception)
- Curvature of the spine (scoliosis)
- Hip displacement
- Contractures (chronic shortening of muscles or tendons around joints)
- Muscle cramping
- Nerve pain
- Some individuals may need to rely on foot or leg braces or other orthopedic devices to maintain mobility5.
- Some people living with CMT experience tremor, and vision and hearing can also be affected5.
- In rare cases, breathing difficulties may occur if the nerves that control the muscles of the diaphragm are affected5.
- The severity of symptoms can vary greatly among individuals and even among family members with the disease and gene mutation5.
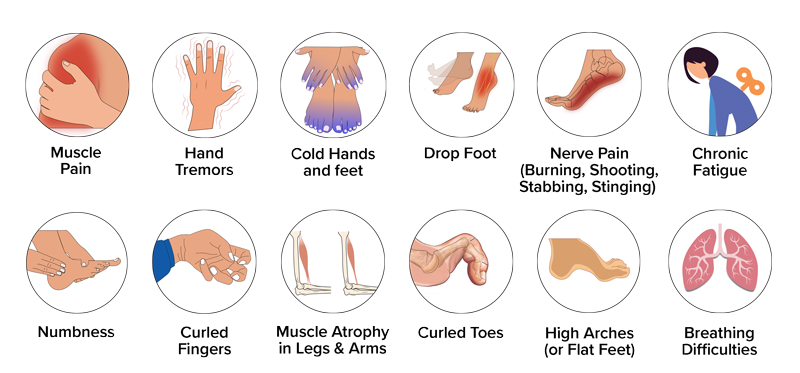
Diagnosis of CMT
- The diagnosis of CMT is based on a combination of clinical examination, family history, nerve conduction studies, electromyography (EMG), nerve biopsy, and genetic testing6.
- Clinical examination involves assessing the muscle strength, reflexes, sensation, and deformities of the limbs6.
- Family history can provide clues about the inheritance pattern and type of CMT6.
- Nerve conduction studies measure the speed and amplitude of nerve impulses in different nerves6. They can help differentiate between demyelinating (CMT1) and axonal (CMT2) forms of CMT6.
- EMG measures the electrical activity of muscles at rest and during contraction6. It can help detect muscle denervation and reinnervation due to nerve damage6.
- Nerve biopsy involves taking a small sample of nerve tissue for microscopic examination6. It can show abnormalities in the myelin sheath or axons of peripheral nerves6.
- Genetic testing involves analyzing the DNA for mutations in specific genes that cause CMT6. It can confirm the diagnosis and identify the exact type and subtype of CMT6.
Treatment of CMT
- There is no cure for CMT, but treatments can help manage the symptoms and improve the quality of life for patients with CMT7.
- The treatments for CMT include7:
- Physical therapy: exercises to maintain muscle strength and flexibility, prevent contractures, improve balance, etc.
- Occupational therapy: activities to improve fine motor skills, self-care abilities, etc.
- Orthotic devices: braces, splints, orthopedic shoes, etc. to support weak muscles, correct foot deformities, prevent injuries, etc.
- Surgery: procedures to correct severe foot deformities, such as high arches or hammertoes
- Medications: drugs to relieve nerve pain or muscle cramps
- Assistive devices: canes, walkers, wheelchairs, etc. to enhance mobility
- Genetic counseling: information and guidance for patients and families about the inheritance, risks, and implications of CMT
- Research: participation in clinical trials or studies to test new therapies or interventions for CMT
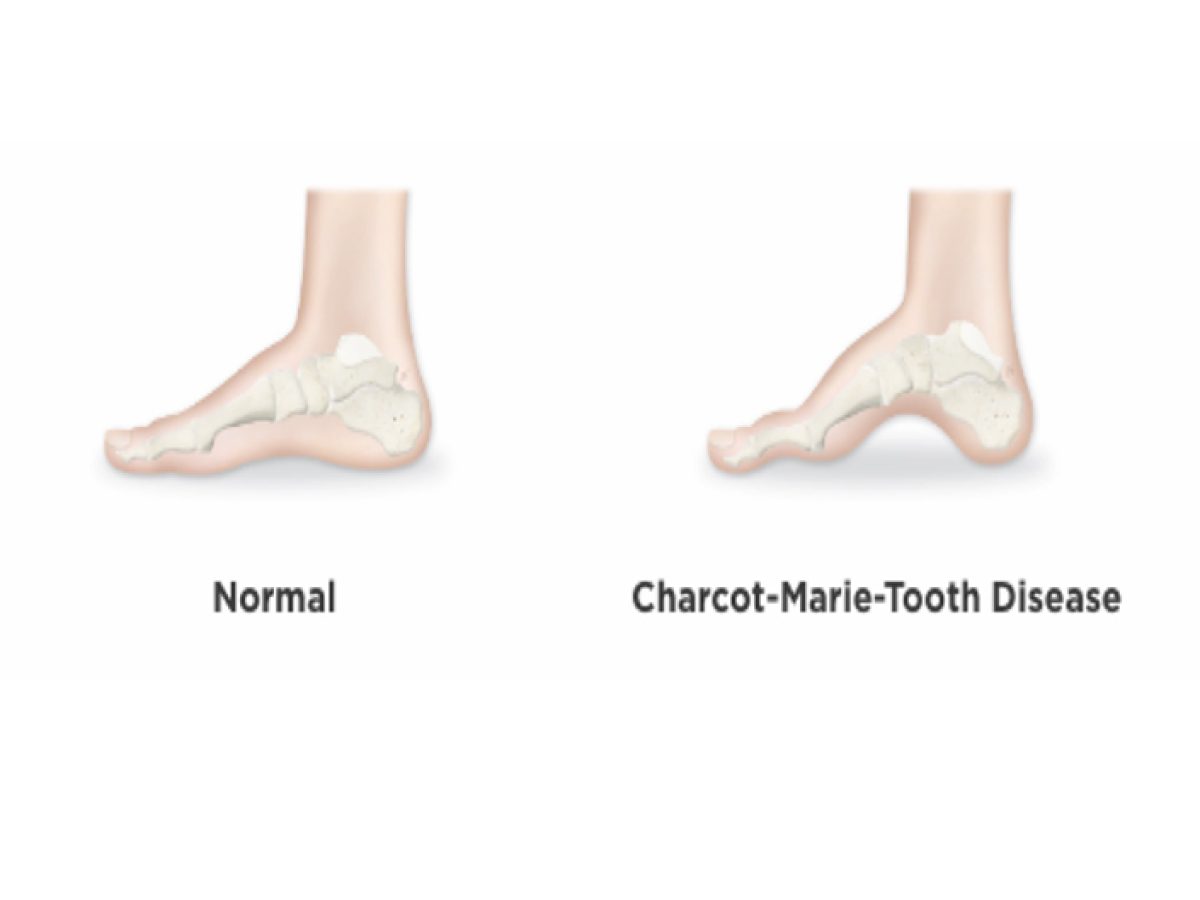
Nursing care and education for patients with CMT
- The nursing care and education for patients with CMT aim to provide holistic and individualized support, promote independence and self-management, prevent complications, and enhance quality of life.
- The nursing care and education for patients with CMT include:
- Assessing the patient’s physical, psychological, social, and spiritual needs
- Monitoring the patient’s vital signs, neurological status, muscle strength, sensation, mobility, etc.
- Providing pain relief, comfort measures, wound care, infection prevention, etc.
- Assisting the patient with activities of daily living (ADLs), such as bathing, dressing, feeding, etc.
- Educating the patient and family about the nature, progression, and prognosis of CMT
- Teaching the patient and family about the available treatments and resources for CMT
- Encouraging the patient and family to adhere to the prescribed therapy regimen and follow-up appointments
- Referring the patient and family to appropriate specialists and services, such as physical therapists, occupational therapists, orthotists, surgeons, genetic counselors, social workers, etc.
- Empowering the patient and family to participate in decision-making and self-care
- Providing emotional support and counseling to the patient and family
- Advocating for the patient’s rights and preferences
- Collaborating with the interdisciplinary team to coordinate care and ensure continuity
Neurodegenerative Diseases: Alzheimer's disease, Parkinson's disease
- Neurodegenerative diseases are a group of chronic progressive disorders that result from the loss or dysfunction of neurons in specific regions of the brain
- Alzheimer’s disease (AD) is the most common cause of dementia in older adults. It is characterized by the accumulation of amyloid plaques and neurofibrillary tangles in the cerebral cortex, leading to cognitive impairment, memory loss, behavioral changes, and functional decline
- Parkinson’s disease (PD) is a movement disorder that affects the basal ganglia. It is characterized by the degeneration of dopaminergic neurons in the substantia nigra pars compacta (SNpc), leading to motor symptoms such as tremor, rigidity, bradykinesia (slowness of movement), postural instability (balance problems), and non-motor symptoms such as depression, anxiety, sleep disorders, autonomic dysfunction (e.g., constipation), etc.
- The exact causes of AD and PD are unknown. However, some possible risk factors include:
- Age: The risk of developing AD or PD increases with advancing age
- Genetics: Some forms of AD or PD are inherited or associated with specific gene mutations or variants
- Environmental factors: Exposure to toxins (e.g., pesticides), head trauma, infections (e.g., viral encephalitis), oxidative stress (e.g., free radicals), inflammation (e.g., chronic systemic diseases), etc. may contribute to neuronal damage or dysfunction
- Lifestyle factors: Smoking, alcohol consumption, poor diet, physical inactivity, cognitive inactivity, etc. may increase the risk or worsen the progression of AD or PD
- The signs and symptoms of AD or PD vary depending on the stage and severity of the disease. Some common manifestations include:
- Alzheimer’s disease (AD:
- Mild cognitive impairment (MCI): The earliest stage of AD that involves subtle changes in memory or thinking that do not interfere with daily activities
- Mild AD: The stage of AD that involves noticeable memory loss (especially short-term memory), difficulty with language (e.g., word-finding problems), visuospatial skills (e.g., getting lost), executive functions (e.g., planning), judgment, reasoning, etc. that affect daily functioning
- Moderate AD: The stage of AD that involves more severe cognitive impairment that affects long-term memory, orientation, recognition, calculation, etc. as well as behavioral changes such as agitation, irritability, mood swings, delusions, hallucinations, etc.
- Severe AD: The stage of AD that involves profound cognitive impairment that affects all aspects of mental functioning as well as functional decline that requires total dependence on others for basic activities of daily living (ADLs) such as eating, dressing, bathing, toileting, etc.
- Alzheimer’s disease (AD:
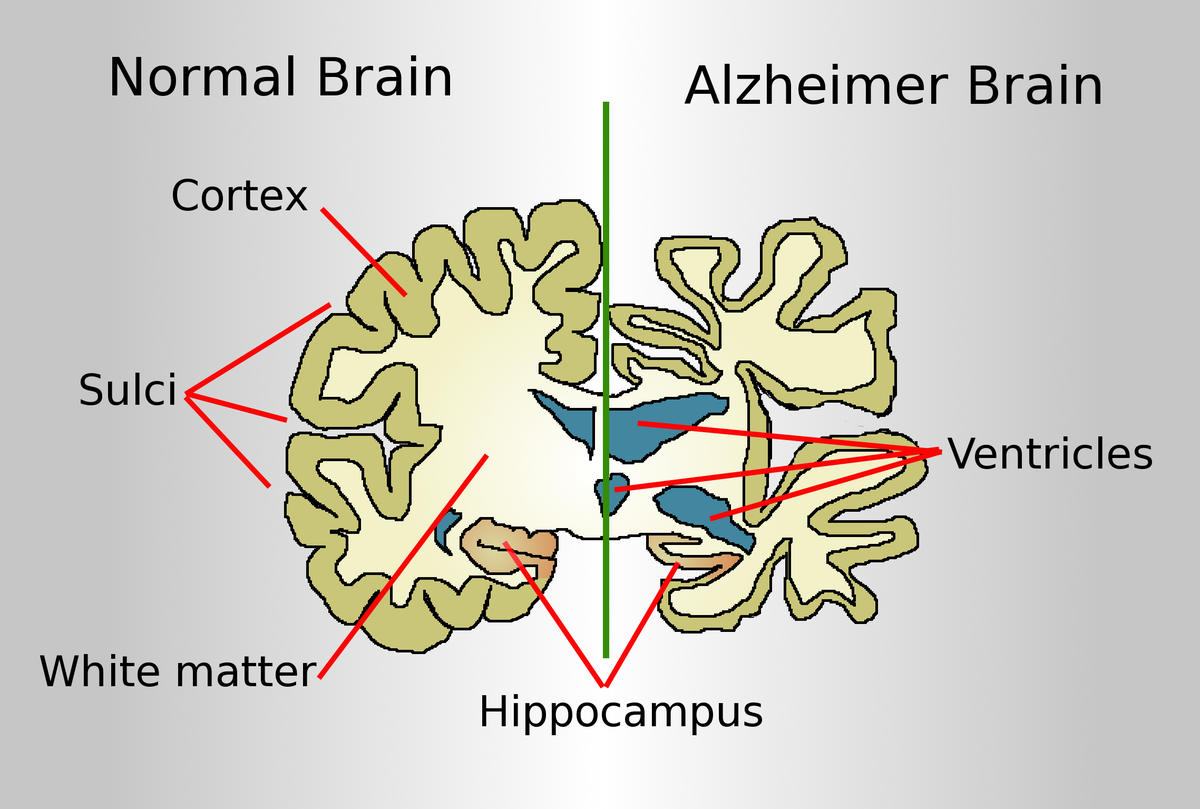
- Parkinson’s disease (PD):
- Advanced PD: The stage of PD that involves severe motor complications such as dyskinesia (involuntary movements), dystonia (abnormal muscle tone), freezing (sudden inability to move), wearing-off (reduced duration of medication effect), on-off (fluctuations between mobility and immobility), etc. as well as non-motor complications such as cognitive impairment, dementia, psychosis, etc.
- Clinical PD: The stage of PD that involves the presence of motor symptoms that are typically asymmetric and respond to dopaminergic therapy. The motor symptoms are classified into four cardinal features: tremor, rigidity, bradykinesia, and postural instability. The severity of the motor symptoms is assessed by the Hoehn and Yahr scale, which ranges from stage 1 (unilateral involvement) to stage 5 (wheelchair-bound or bedridden)
- Prodromal PD: The stage of PD that occurs when the motor symptoms are not yet clinically detectable but can be identified by specialized tests such as neuroimaging or biomarkers
- Preclinical PD: The stage of PD that occurs before the onset of motor symptoms and involves non-motor symptoms such as loss of smell (anosmia), constipation, depression, anxiety, REM sleep behavior disorder (RBD), etc.
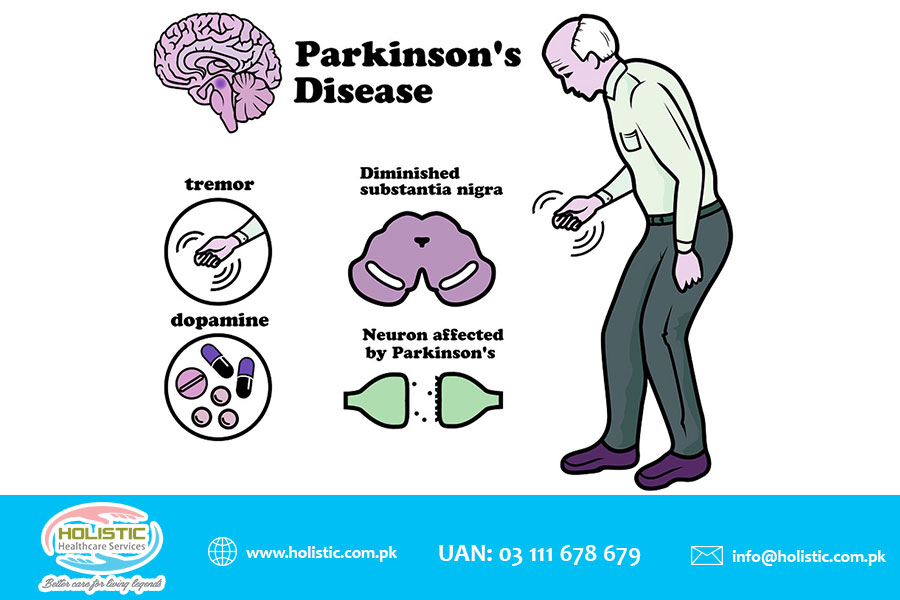
Diagnosis of AD or Parkinson’s disease (PD)
- The diagnosis of AD or Parkinson’s disease (PD) is based on clinical criteria that include medical history, physical examination, neurological examination, cognitive assessment, and exclusion of other possible causes. Some diagnostic tests that may be used to support the diagnosis or rule out other conditions include:
- Alzheimer’s disease (AD:
- Blood tests: To check for vitamin B12 deficiency, thyroid dysfunction, infection, etc.
- Urinalysis: To check for urinary tract infection, dehydration, etc.
- Lumbar puncture: To measure the levels of amyloid beta and tau proteins in the cerebrospinal fluid (CSF) that may indicate AD
- Neuroimaging: To visualize the structure and function of the brain using techniques such as computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), single-photon emission computed tomography (SPECT), etc. that may show atrophy (shrinkage) or hypometabolism (reduced activity) of specific brain regions affected by AD
- Neuropsychological testing: To assess the cognitive domains such as memory, language, visuospatial skills, executive functions, etc. using standardized tools such as the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog), etc.
- Parkinson’s disease (PD):
- Blood tests: To check for infection, electrolyte imbalance, liver or kidney function, etc.
- Urinalysis: To check for infection, dehydration, etc.
- Lumbar puncture: To measure the levels of alpha-synuclein protein in the CSF that may indicate PD
- Neuroimaging: To visualize the structure and function of the brain using techniques such as CT, MRI, PET, SPECT, etc. that may show loss or dysfunction of dopaminergic neurons in the SNpc or other brain regions affected by PD
- Neuropsychological testing: To assess the cognitive domains such as attention, memory, language, visuospatial skills, executive functions, etc. using standardized tools such as the MMSE, MoCA, Parkinson’s Disease Cognitive Rating Scale (PD-CRS), etc.
- DaTscan: A specific type of SPECT scan that uses a radioactive tracer that binds to dopamine transporters in the brain and can detect reduced dopamine uptake in the striatum (a part of the basal ganglia) that is characteristic of PD
- Alzheimer’s disease (AD:
Treatment of AD or Parkinson’s disease (PD)
- The treatment of AD or PD is aimed at slowing down the progression of the disease, managing the symptoms, improving the quality of life, and providing support and education for the patient and caregivers. Some treatment options include:
- Alzheimer’s disease (AD:
- Pharmacological therapy: To enhance or modulate neurotransmitter activity in the brain using drugs such as cholinesterase inhibitors (e.g., donepezil, rivastigmine, galantamine) that increase acetylcholine levels or N-methyl-D-aspartate (NMDA) receptor antagonists (e.g., memantine) that block glutamate excitotoxicity. These drugs may improve cognition, behavior, and function in mild to moderate AD but have limited efficacy and side effects such as nausea, vomiting, diarrhea, headache, dizziness, etc.
- Non-pharmacological therapy: To stimulate or maintain cognitive abilities and social interactions using interventions such as cognitive stimulation therapy (CST), reminiscence therapy, music therapy, art therapy, etc. that involve engaging in meaningful activities, recalling past experiences, expressing emotions, etc. These interventions may enhance mood, self-esteem, communication, and well-being in AD patients and caregivers - Behavioral therapy: To manage or modify behavioral symptoms such as agitation, irritability, aggression, wandering, etc. using interventions such as validation therapy, reality orientation, redirection, distraction, environmental modification, etc. that involve acknowledging the patient’s feelings, providing orientation cues, diverting attention to other activities, creating a safe and comfortable environment, etc. These interventions may reduce stress, anxiety, and frustration in AD patients and caregivers - Physical therapy: To improve or maintain physical function and mobility using interventions such as exercise, stretching, balance training, gait training, etc. that involve performing physical activities that are appropriate for the patient’s condition and preferences. These interventions may prevent or delay complications such as falls, fractures, pressure ulcers, contractures, etc. and improve cardiovascular health, muscle strength, flexibility, and endurance in AD patients - Occupational therapy: To improve or maintain daily living skills and independence using interventions such as task analysis, task simplification, assistive devices, environmental adaptation, etc. that involve breaking down complex tasks into simpler steps, reducing the cognitive demands of tasks, providing aids or tools to facilitate tasks, modifying the environment to suit the patient’s needs and abilities, etc. These interventions may enhance self-care, productivity, leisure, and safety in AD patients - Speech therapy: To improve or maintain communication and swallowing skills using interventions such as language stimulation, cueing, prompting, alternative or augmentative communication (AAC) devices, swallowing exercises, diet modification, etc. that involve providing verbal or non-verbal cues to elicit responses, repeating or rephrasing words or sentences, using pictures or symbols to convey messages, performing oral motor exercises to strengthen the muscles involved in swallowing, changing the texture or consistency of food or liquids to facilitate swallowing, etc. These interventions may prevent or reduce communication difficulties, social isolation, aspiration pneumonia, malnutrition, dehydration, etc. in AD patients
- Alzheimer’s disease (AD:
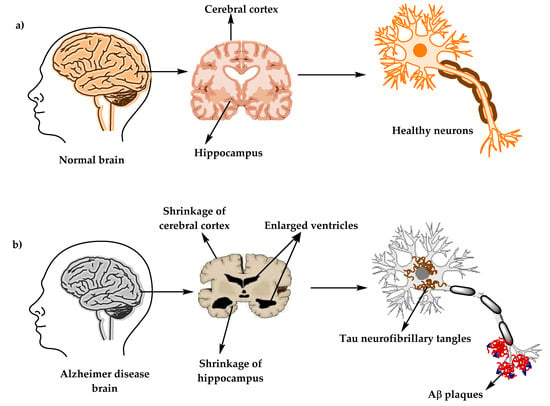
- Parkinson’s disease (PD):
- Non-pharmacological therapy: To manage or reduce non-motor symptoms and complications using interventions such as deep brain stimulation (DBS), transcranial magnetic stimulation (TMS), physical therapy, occupational therapy, speech therapy, cognitive behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), etc. that involve stimulating specific brain regions with electrical currents or magnetic fields to modulate neuronal activity, improving physical function and mobility, enhancing daily living skills and independence, improving communication and swallowing skills, addressing psychological issues such as depression, anxiety, etc., reducing stress and improving coping skills, etc. These interventions may improve quality of life and well-being in PD patients and caregivers
- Pharmacological therapy: To restore or modulate dopamine activity in the brain using drugs such as levodopa (L-dopa), carbidopa, dopamine agonists (e.g., pramipexole, ropinirole), monoamine oxidase B (MAO-B) inhibitors (e.g., selegiline, rasagiline), catechol-O-methyltransferase (COMT) inhibitors (e.g., entacapone), anticholinergics (e.g., trihexyphenidyl), etc. These drugs may improve motor symptoms and function in PD patients but have side effects such as nausea, vomiting, orthostatic hypotension (low blood pressure when standing up), dyskinesia, psychosis, etc.
- The prevention of Alzheimer’s disease (AD) or Parkinson’s disease (PD) is not fully established. However, some possible preventive measures include:
- Maintaining a healthy lifestyle: Eating a balanced diet rich in antioxidants (e.g., fruits, vegetables), omega-3 fatty acids (e.g., fish), and vitamins (e.g., B12), avoiding smoking and excessive alcohol consumption, exercising regularly (at least 150 minutes per week of moderate-intensity aerobic activity), managing chronic conditions such as hypertension, diabetes, hyperlipidemia (high cholesterol), etc., getting enough sleep (7-9 hours per night), and avoiding head injuries
- Engaging in cognitive and social activities: Reading books, playing games, learning new skills, taking courses, volunteering for a cause, joining a club or group, maintaining social contacts with family and friends, etc.
- Seeking medical attention: Consulting a doctor if experiencing any signs or symptoms of AD or PD or having a family history of these diseases
Neuroinflammation: Multiple sclerosis; Meningitis; Guillain-Barré syndrome
- Neuroinflammation is a pathological process that involves the activation of the immune system in response to injury or infection in the nervous system
- Neuroinflammation can be beneficial or harmful depending on the type, duration, and intensity of the immune response
- Beneficial neuroinflammation can promote tissue repair and regeneration by removing debris, releasing growth factors, and stimulating neurogenesis (the formation of new neurons)
- Harmful neuroinflammation can cause tissue damage and dysfunction by releasing pro-inflammatory cytokines (chemical messengers), reactive oxygen species (free radicals), and excitatory neurotransmitters (e.g., glutamate) that can induce neuronal death, demyelination (the loss of the myelin sheath that insulates axons), and synaptic dysfunction (the impairment of communication between neurons)
- Neuroinflammation can be triggered by various factors such as trauma, stroke, tumors, infections, autoimmune diseases, etc.
- Neuroinflammation can result in various neurological disorders such as:
- multiple sclerosis (MS),
- meningitis,
- Guillain-Barré syndrome (GBS)
- MS is a chronic autoimmune disease that affects the CNS. It is characterized by the formation of inflammatory lesions or plaques in the white matter of the brain and spinal cord, leading to demyelination and axonal damage
- Meningitis is an acute infection that affects the meninges (the membranes that cover the brain and spinal cord). It is caused by various microorganisms such as bacteria, viruses, fungi, parasites, etc. that enter the CNS through the bloodstream or direct contact. It is characterized by inflammation of the meninges, leading to headache, fever, neck stiffness, photophobia (sensitivity to light), altered mental status, etc.
- GBS is an acute inflammatory polyneuropathy (a disorder that affects multiple peripheral nerves). It is caused by an abnormal immune response to a preceding infection or vaccination that targets the myelin or axons of the peripheral nerves. It is characterized by ascending weakness or paralysis of the limbs, face, and respiratory muscles, leading to difficulty in walking, speaking, swallowing, breathing, etc.
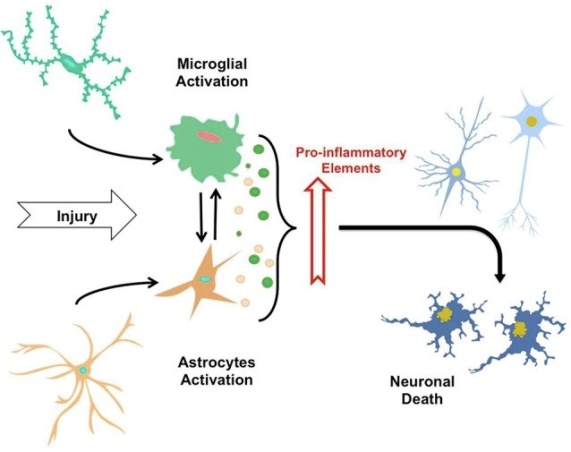
multiple sclerosis (MS)
- MS is a chronic and unpredictable disease of the central nervous system (CNS), which consists of the brain, spinal cord, and optic nerves 12
- In MS, the immune system mistakenly attacks the protective covering (myelin) of nerve fibers, causing inflammation, damage, and scar tissue (sclerosis or lesions) 123
- The damage to the nerve fibers disrupts the communication between the brain and the rest of the body, resulting in various symptoms that depend on the location and extent of the lesions 123
- The cause of MS is unknown, but it is likely influenced by a combination of genetic and environmental factors, such as infections, vitamin D deficiency, smoking, or exposure to toxins 123
- MS affects people differently and can have a wide range of symptoms, such as numbness, tingling, weakness, fatigue, vision problems, balance problems, coordination problems, bladder problems, bowel problems, cognitive problems, mood problems, pain, and spasticity 123
- MS is diagnosed based on the signs and symptoms, medical history, physical examination, blood tests, and imaging tests such as magnetic resonance imaging (MRI) or optical coherence tomography (OCT) 123
- There are four main types of MS based on the pattern of symptoms over time: relapsing-remitting MS (RRMS), secondary-progressive MS (SPMS), primary-progressive MS (PPMS), and progressive-relapsing MS (PRMS) 123
- There is no cure for MS, but there are treatments that can help reduce the frequency and severity of relapses, slow down the progression of the disease, manage the symptoms, and improve the quality of life. These treatments include disease-modifying therapies (DMTs), corticosteroids, symptom management medications, rehabilitation therapies, complementary and alternative therapies, and lifestyle modifications 123
- MS is more common in women than in men and usually affects people between the ages of 20 and 50. It is estimated that about 2.8 million people worldwide have MS. The prevalence of MS varies by geographic region, with higher rates in temperate zones than in tropical zones 12
Causes and Risk factors of multiple sclerosis (MS)
- Causes: The exact cause of multiple sclerosis (MS) is unknown. However, some possible factors that may trigger or contribute to the development of MS include
- genetic susceptibility,
- environmental exposure (e.g., vitamin D deficiency, smoking, infection),
- immune dysregulation (e.g., molecular mimicry, epitope spreading, bystander activation) that lead to the activation of autoreactive T cells and B cells that cross the blood-brain barrier (BBB) and attack the myelin and axons of the CNS
Risk factors of multiple sclerosis (MS)
- Risk factors:
- age (20-50 years),
- sex (female),
- race (white),
- family history,
- geography (higher prevalence in temperate regions),
- certain infections (e.g., Epstein-Barr virus, human herpesvirus 6, etc.)
Signs and symptoms of multiple sclerosis (MS)
- Signs and symptoms: The signs and symptoms of MS vary depending on the location and extent of the lesions or plaques in the CNS.
- Some common manifestations include:
- sensory disturbances (e.g., numbness, tingling, pain)
- motor weakness or spasticity
- visual impairment or optic neuritis (inflammation of the optic nerve)
- fatigue
- cognitive impairment or dementia
- emotional changes or depression
- bladder or bowel dysfunction
- sexual dysfunction
Diagnosis of multiple sclerosis (MS)
- Diagnosis: The diagnosis of MS is based on clinical criteria that include evidence of dissemination in space (DIS) and dissemination in time (DIT) of CNS lesions that are consistent with MS and not better explained by other conditions. Some diagnostic tests that may be used to support the diagnosis or rule out other causes include:
- Neuroimaging: To visualize the structure and function of the brain and spinal cord using techniques such as MRI, PET, SPECT, etc. that may show multiple lesions or plaques in different regions and stages of MS
- Lumbar puncture: To measure the levels of immunoglobulin G (IgG) and oligoclonal bands (OCBs) in the CSF that may indicate an immune response in the CNS
- Evoked potentials: To measure the electrical activity of the brain in response to sensory stimuli such as visual, auditory, or somatosensory stimuli that may show delayed or reduced responses due to demyelination
- Blood tests: To check for infection, inflammation, autoantibodies, etc. that may cause or mimic MS
Treatment of multiple sclerosis (MS)
- Treatment: The treatment of MS is aimed at modifying the course of the disease, managing the symptoms, preventing relapses, and improving the quality of life. Some treatment options include:
- Disease-modifying therapies (DMTs): To reduce the frequency and severity of relapses and delay the progression of disability using drugs such as interferons (e.g., interferon beta-1a, interferon beta-1b), glatiramer acetate, natalizumab, fingolimod, alemtuzumab, ocrelizumab, etc. that modulate the immune system by inhibiting T cell activation, migration, or proliferation; reducing inflammation; or depleting B cells. These drugs may have side effects such as injection site reactions, flu-like symptoms, liver toxicity, infection risk, etc.
- Symptomatic therapies: To manage or reduce specific symptoms such as spasticity, pain, fatigue, depression, bladder dysfunction, etc. using drugs such as baclofen, tizanidine, gabapentin, amitriptyline, modafinil, fluoxetine, oxybutynin, etc. that act on various neurotransmitter systems or receptors to relax muscles, relieve pain, enhance energy, improve mood, control urination, etc.
- Rehabilitation therapies: To improve or maintain physical function and mobility using interventions such as exercise, stretching, balance training, gait training, etc. that involve performing physical activities that are appropriate for the patient’s condition and preferences. These interventions may prevent or delay complications such as falls, fractures, pressure ulcers, contractures, etc. and improve cardiovascular health, muscle strength, flexibility, and endurance in MS patients
- Occupational therapy: To improve or maintain daily living skills and independence using interventions such as task analysis, task simplification, assistive devices, environmental adaptation, etc. that involve breaking down complex tasks into simpler steps, reducing the cognitive demands of tasks, providing aids or tools to facilitate tasks, modifying the environment to suit the patient’s needs and abilities, etc. These interventions may enhance self-care,productivity,leisure,and safety in MS patients - Speech therapy: To improve or maintain communication and swallowing skills using interventions such as language stimulation,cueing,prompting,AAC devices,swallowing exercises,diet modification,etc. that involve providing verbal or non-verbal cues to elicit responses,repeating or rephrasing words or sentences,using pictures or symbols to convey messages,performing oral motor exercises to strengthen the muscles involved in swallowing,changing the texture or consistency of food or liquids to facilitate swallowing,etc. These interventions may prevent or reduce communication difficulties,social isolation,aspiration pneumonia,malnutrition,dehydration,etc. in MS patients
- Cognitive therapy: To improve or maintain cognitive abilities and function using interventions such as cognitive stimulation therapy (CST), cognitive rehabilitation, cognitive behavioral therapy (CBT), etc. that involve engaging in meaningful activities, training specific cognitive domains, addressing psychological issues, etc. These interventions may enhance memory, attention, language, executive functions, etc. and improve mood, self-esteem, coping skills, etc. in MS patients - Prevention: The prevention of MS is not fully established. However, some possible preventive measures include avoiding smoking, maintaining adequate vitamin D levels, avoiding infections, and following a healthy lifestyle
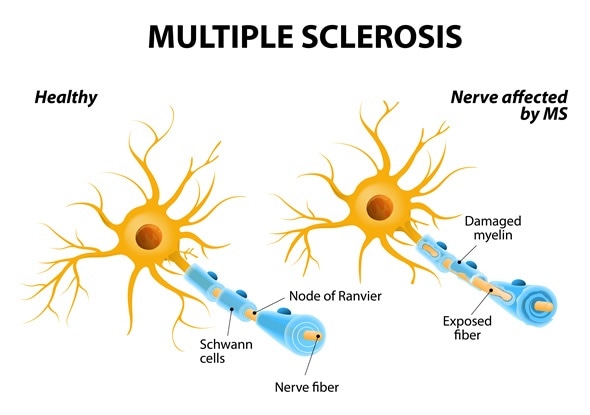
Meningitis
- Meningitis is an inflammation of the meninges, which are the protective layers surrounding the brain and spinal cord 12
- Meningitis can be life-threatening and requires immediate medical attention, especially if it is caused by bacteria, which can lead to serious complications, such as brain damage, hearing loss, or death 124
- The symptoms of meningitis may vary depending on the cause and age of the person, but they often include fever, headache, stiff neck, nausea, vomiting, confusion, sensitivity to light, and skin rash 124
Causes and Risk factors of Menengitis
- Meningitis can be caused by various types of infections, such as bacteria, viruses, fungi, and parasites, as well as non-infectious conditions, such as cancer, drugs, or autoimmune disorders 123
- Causes: The causes of meningitis vary depending on the type of microorganism that infects the meninges. Some common causes include:
- Bacterial meningitis: Caused by bacteria such as Streptococcus pneumoniae (pneumococcus), Neisseria meningitidis (meningococcus), Haemophilus influenzae type b (Hib), Listeria monocytogenes, etc. that enter the CNS through the bloodstream or direct contact (e.g., respiratory droplets, contaminated food, etc.)
- Viral meningitis: Caused by viruses such as enteroviruses (e.g., coxsackievirus, echovirus), herpes simplex virus (HSV), varicella-zoster virus (VZV), mumps virus, etc. that enter the CNS through the bloodstream or direct contact (e.g., saliva, blisters, etc.)
- Fungal meningitis: Caused by fungi such as Cryptococcus neoformans, Candida albicans, Histoplasma capsulatum, etc. that enter the CNS through the bloodstream or direct contact (e.g., inhalation of spores, skin contact with infected animals, etc.)
- Parasitic meningitis: Caused by parasites such as Naegleria fowleri, Acanthamoeba spp., Angiostrongylus cantonensis, etc. that enter the CNS through the bloodstream or direct contact (e.g., nasal irrigation with contaminated water, ingestion of raw or undercooked snails or slugs, etc.)
- Risk factors: Some factors that may increase the risk of developing meningitis include age (infants and young children), immunocompromised status (e.g., HIV/AIDS, cancer, transplantation, etc.), close contact with infected individuals or animals, travel to endemic areas, lack of vaccination, etc.
Signs and symptoms of Meningitis
- Signs and symptoms: The signs and symptoms of meningitis vary depending on the type and severity of the infection.
- headache
- fever
- neck stiffness
- photophobia
- altered mental status
- nausea
- vomiting
- rash
- seizures
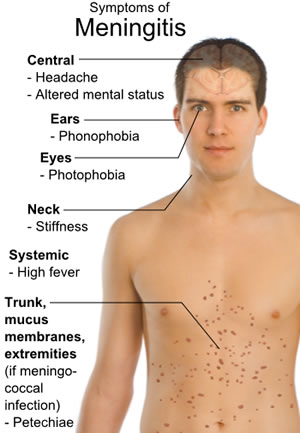
Diagnosis of Meningitis
- Diagnosis: The diagnosis of meningitis is based on clinical criteria that include medical history, physical examination, neurological examination, and exclusion of other possible causes. Some diagnostic tests that may be used to confirm the diagnosis or identify the causative agent include:
- Lumbar puncture: To obtain a sample of CSF for analysis and culture that may show increased pressure, increased white blood cell count (WBC), decreased glucose level, increased protein level, and presence of bacteria, viruses, fungi, or parasites
- Blood tests: To check for infection, inflammation, blood culture, etc. that may show increased WBC, increased erythrocyte sedimentation rate (ESR), increased C-reactive protein (CRP), and presence of bacteria, viruses, fungi, or parasites
- Urine tests: To check for infection and culture that may show presence of bacteria, viruses, fungi, or parasites
- Neuroimaging: To visualize the structure and function of the brain and spinal cord using techniques such as CT, MRI, PET, SPECT, etc. that may show inflammation of the meninges or other complications such as abscesses, hydrocephalus (excess fluid in the brain), cerebral edema (swelling of the brain), etc.
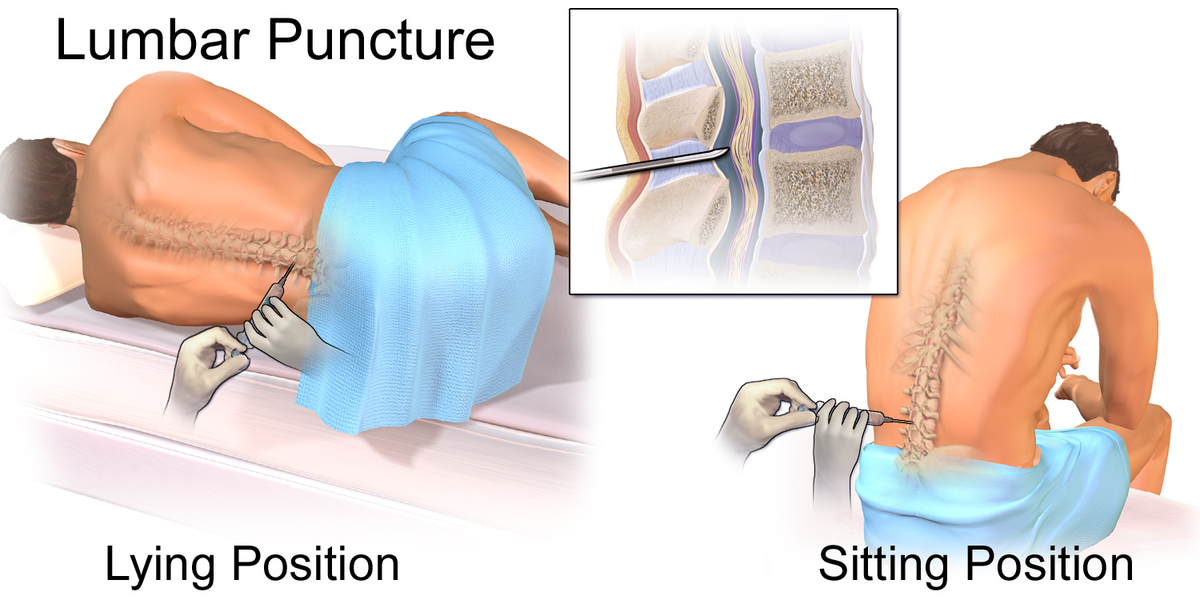
Treatment of Meningitis
- Treatment: The treatment of meningitis is aimed at eradicating the infection, reducing the inflammation, managing the symptoms, preventing complications, and improving the outcome. Some treatment options include:
- Antibiotics: To treat bacterial meningitis using drugs such as penicillin, ceftriaxone, vancomycin, etc. that target the specific type of bacteria causing the infection. These drugs may have side effects such as allergic reactions, diarrhea, kidney toxicity, etc.
- Antivirals: To treat viral meningitis using drugs such as acyclovir, ganciclovir, etc. that inhibit the replication of the virus causing the infection. These drugs may have side effects such as nausea, vomiting, headache, etc.
- Antifungals: To treat fungal meningitis using drugs such as amphotericin B, fluconazole, etc. that interfere with the cell membrane or synthesis of the fungus causing the infection. These drugs may have side effects such as fever, chills, kidney toxicity, liver toxicity, etc.
- Antiparasitics: To treat parasitic meningitis using drugs such as albendazole, ivermectin, etc. that kill or paralyze the parasite causing the infection. These drugs may have side effects such as abdominal pain, dizziness, rash, etc.
- Corticosteroids: To reduce the inflammation and swelling of the meninges and brain using drugs such as dexamethasone, prednisone, etc. that suppress the immune system and inhibit the production of pro-inflammatory cytokines. These drugs may have side effects such as increased blood pressure, increased blood sugar, increased risk of infection, etc.
- Analgesics: To relieve pain and fever using drugs such as acetaminophen, ibuprofen, etc. that block the production of prostaglandins (chemical messengers) that mediate pain and inflammation. These drugs may have side effects such as stomach irritation, bleeding, liver toxicity, kidney toxicity, etc.
- Anticonvulsants: To prevent or control seizures using drugs such as phenytoin, carbamazepine, valproic acid, etc. that stabilize the electrical activity of the brain by modulating sodium, calcium, or potassium channels or enhancing gamma-aminobutyric acid (GABA) activity. These drugs may have side effects such as drowsiness, dizziness, rash, liver toxicity, etc.
- Fluids and electrolytes: To maintain hydration and electrolyte balance using intravenous fluids that contain water, sodium, potassium, chloride, bicarbonate, etc. that regulate the osmolarity, pH, and volume of body fluids
- Oxygen therapy: To provide adequate oxygenation and ventilation using devices such as nasal cannula, face mask, ventilator, etc. that deliver oxygen to the lungs and remove carbon dioxide from the body
Prevention of Meningitis
- Prevention: The prevention of meningitis depends on the type and source of infection.
- Some preventive measures include
- vaccination against common causes of bacterial or viral meningitis (e.g., pneumococcal vaccine, meningococcal vaccine, Hib vaccine, MMR vaccine, etc.),
- avoiding close contact with infected individuals or animals,
- practicing good hygiene (e.g., washing hands, covering mouth and nose when coughing or sneezing, etc.),
- avoiding contaminated food or water (e.g., cooking food thoroughly, boiling or filtering water, etc.)
- seeking medical attention if experiencing any signs or symptoms of meningitis
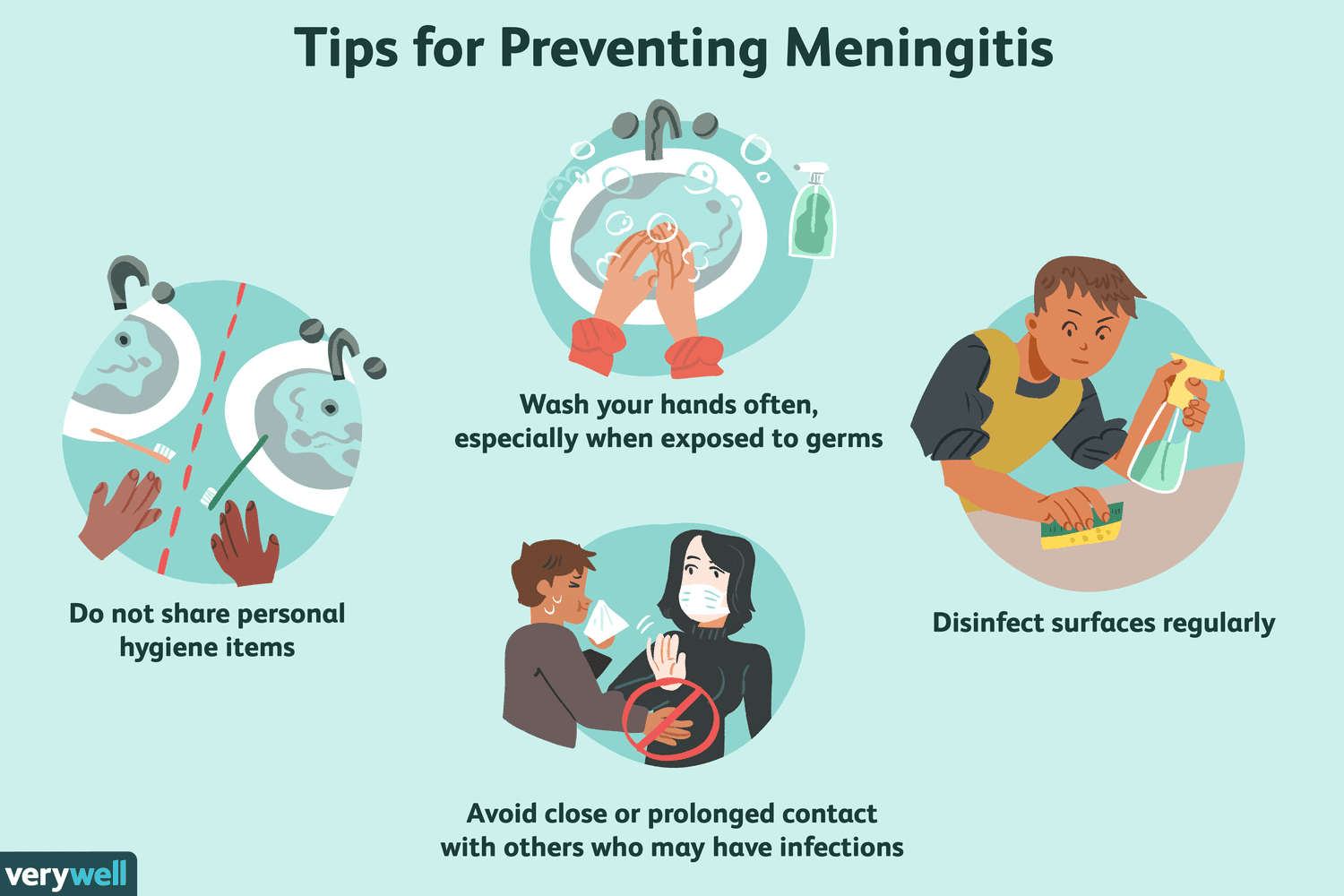
Guillain-Barré syndrome (GBS)
- GBS is a rare but serious autoimmune disorder in which the immune system mistakenly attacks healthy nerve cells in the peripheral nervous system (PNS) 12
- The PNS is the network of nerves located outside of the brain and spinal cord that control sensory, motor, and autonomic functions 13
- The immune attack causes inflammation and damage to the myelin sheaths that protect and insulate the nerve fibers, resulting in impaired transmission of nerve impulses 24
- The exact cause of GBS is unknown, but it is often triggered by an infection, such as COVID-19, respiratory or gastrointestinal infection, or Zika virus, or less commonly by surgery or vaccination 24
- GBS can be life-threatening if it affects the breathing muscles or the autonomic nervous system, which can cause dangerous abnormalities in heart rate and blood pressure 12
- The diagnosis of GBS is based on the signs and symptoms, nerve conduction studies that measure the speed and strength of nerve signals, and lumbar puncture that examines the cerebrospinal fluid for elevated protein levels 24
- There are several subtypes of GBS based on the areas of weakness, results of nerve conduction studies, and the presence of certain antibodies. The most common subtype in North America and Europe is acute inflammatory demyelinating polyradiculoneuropathy (AIDP), while other subtypes include Miller Fisher syndrome (MFS), acute motor axonal neuropathy (AMAN), and acute motor-sensory axonal neuropathy (AMSAN) 25
- There is no cure for GBS, but treatments can ease symptoms and reduce the duration of the illness. The main treatments are intravenous immunoglobulins (IVIG) or plasmapheresis (plasma exchange), which both aim to remove harmful antibodies from the blood. Supportive care may include mechanical ventilation, pain management, physical therapy, and psychological support 24
- Most people with GBS recover completely or have only mild residual weakness. Recovery may take weeks to years, with about a third having some permanent weakness. About 15% of people have a relapse of muscle weakness or sensory symptoms. The mortality rate of GBS is about 7.5%, mainly due to complications such as infections, blood clots, or cardiac arrest 124
- GBS is rare, affecting about 1 or 2 people per 100,000 every year. It can affect anyone at any age and any gender. It was first described by French neurologists Georges Guillain and Jean Alexandre Barré in 1916 2
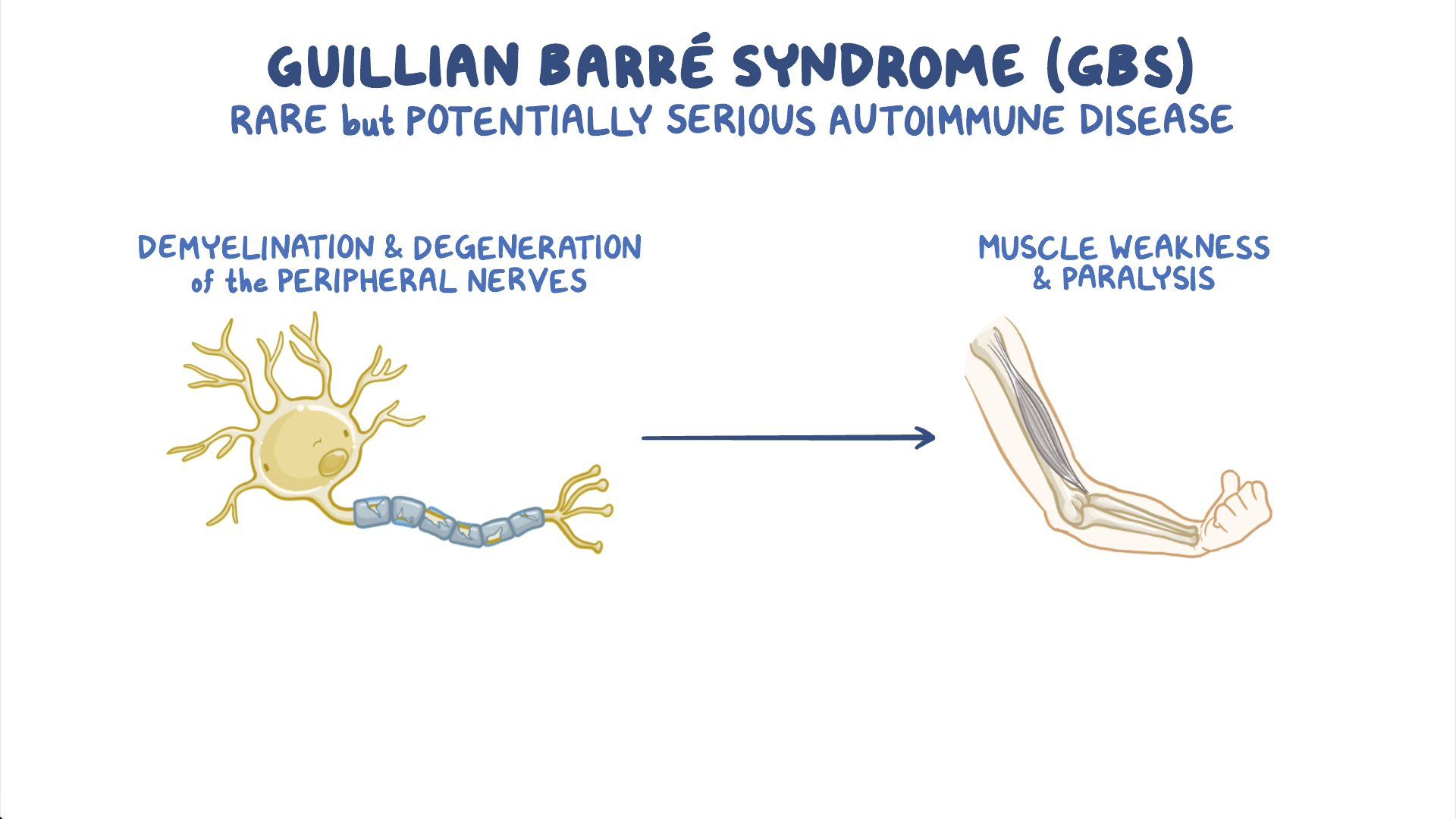
Causes and risk factors of GBS
- Causes: The exact cause of GBS is unknown.
- However, some possible factors that may trigger or contribute to the development of GBS include
- preceding infection (e.g., Campylobacter jejuni, cytomegalovirus (CMV), Epstein-Barr virus (EBV), Zika virus, etc.), vaccination (e.g., influenza vaccine), surgery, trauma, etc. that induce an abnormal immune response that cross-reacts with the myelin or axons of the peripheral nerves
- Risk factors: Some factors that may increase the risk of developing GBS include age (older adults), sex (male), genetics (e.g., HLA alleles), immunocompromised status (e.g., HIV/AIDS), etc.
Signs and symptoms of GBS
- Signs and symptoms: The signs and symptoms of GBS vary depending on the type and severity of the nerve damage.
- Some common manifestations include ascending weakness or paralysis of the limbs, face, and respiratory muscles; sensory disturbances (e.g., numbness, tingling, pain);
- autonomic dysfunction (e.g., blood pressure fluctuations, heart rate abnormalities, sweating abnormalities);
- cranial nerve involvement (e.g., facial palsy, ophthalmoplegia (eye movement paralysis), dysphagia (difficulty swallowing), dysarthria (difficulty speaking)); etc.
Diagnosis and symptoms of GBS
- Diagnosis: The diagnosis of GBS is based on clinical criteria that include medical history, physical examination, neurological examination, and exclusion of other possible causes. Some diagnostic tests that may be used to support the diagnosis or rule out other conditions include:
- Lumbar puncture: To obtain a sample of CSF for analysis that may show increased protein level and normal WBC count (albuminocytologic dissociation) that indicate nerve damage
- Nerve conduction studies (NCS) and electromyography (EMG): To measure the electrical activity and function of the peripheral nerves and muscles that may show reduced nerve conduction velocity, prolonged distal latency, reduced amplitude, and abnormal spontaneous activity that indicate demyelination or axonal degeneration
- Blood tests: To check for infection, inflammation, autoantibodies, etc. that may cause or mimic GBS
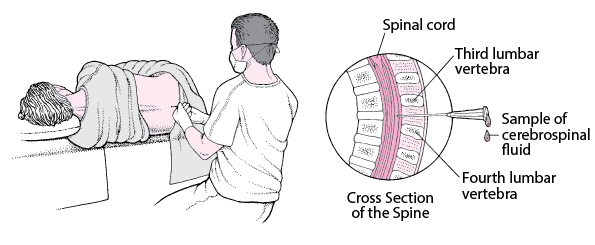
Treatment and prevention of GBS
- Treatment: The treatment of GBS is aimed at stopping the immune attack, supporting the vital functions, managing the symptoms, preventing complications, and promoting recovery. Some treatment options include:
- Immunotherapy: To reduce the immune response and remove the harmful antibodies using methods such as plasma exchange (PE) or intravenous immunoglobulin (IVIG) that involve removing or diluting the patient’s plasma (the liquid part of blood that contains antibodies) and replacing it with fresh plasma or immunoglobulin (a solution of antibodies) that can neutralize or block the harmful antibodies. These methods may have side effects such as allergic reactions, infection risk, fluid overload, etc.
- Supportive therapy: To provide adequate oxygenation and ventilation using devices such as nasal cannula, face mask, ventilator, etc. that deliver oxygen to the lungs and remove carbon dioxide from the body; to maintain hydration and electrolyte balance using intravenous fluids that contain water, sodium, potassium, chloride, bicarbonate, etc. that regulate the osmolarity, pH, and volume of body fluids; to prevent or treat infections using antibiotics or antivirals that target the specific type of microorganism causing the infection; to prevent or treat thromboembolism (blood clot formation) using anticoagulants (e.g., heparin, warfarin, etc.) that inhibit the coagulation cascade or thrombolytics (e.g., streptokinase, tissue plasminogen activator (tPA), etc.) that dissolve existing clots
- Symptomatic therapy: To manage or reduce specific symptoms such as pain, spasticity, autonomic dysfunction, etc. using drugs such as gabapentin, baclofen, midodrine, etc. that act on various neurotransmitter systems or receptors to relieve pain, relax muscles, increase blood pressure, etc.
- Rehabilitation therapy: To improve or maintain physical function and mobility using interventions such as exercise, stretching, balance training, gait training, etc. that involve performing physical activities that are appropriate for the patient’s condition and preferences. These interventions may prevent or delay complications such as contractures, muscle atrophy, pressure ulcers, etc. and improve muscle strength, flexibility, and endurance in GBS patients
- Occupational therapy: To improve or maintain daily living skills and independence using interventions such as task analysis, task simplification, assistive devices, environmental adaptation, etc. that involve breaking down complex tasks into simpler steps, reducing the cognitive demands of tasks, providing aids or tools to facilitate tasks, modifying the environment to suit the patient’s needs and abilities, etc. These interventions may enhance self-care, productivity, leisure, and safety in GBS patients
- Speech therapy: To improve or maintain communication and swallowing skills using interventions such as language stimulation, cueing, prompting, AAC devices, swallowing exercises, diet modification, etc. that involve providing verbal or noverbal cues to elicit responses, repeating or rephrasing words or sentences, using pictures or symbols to convey messages, performing oral motor exercises to strengthen the muscles involved in swallowing, changing the texture or consistency of food or liquids to facilitate swallowing, etc. These interventions may prevent or reduce communication difficulties, social isolation, aspiration pneumonia, malnutrition, dehydration, etc. in GBS patients
- Prevention: The prevention of GBS is not fully established. However, some possible preventive measures include avoiding infections or vaccinations that may trigger GBS, practicing good hygiene (e.g., washing hands), and seeking medical attention if experiencing any signs or symptoms of GBS
Epilepsy: Status epilepticus
- Epilepsy is a chronic neurological disorder that affects the brain. It is characterized by recurrent unprovoked seizures that result from abnormal synchronous electrical activity of a group of neurons in the brain
Epileptic seizures
- Seizures are transient episodes of altered consciousness, behavior, sensation, motor activity, or autonomic function that result from abnormal electrical activity of a group of neurons in the brain
- Seizures can be classified into two main types: focal (partial) seizures and generalized seizures
- Focal seizures: Seizures that originate from a specific region of the brain and affect only one hemisphere. They can be further divided into:
- Focal aware seizures: Seizures that do not impair consciousness or awareness. They may cause motor symptoms (e.g., twitching, jerking, stiffening), sensory symptoms (e.g., tingling, numbness, flashing lights), autonomic symptoms (e.g., sweating, flushing, palpitations), or psychic symptoms (e.g., deja vu, fear, joy)
- Focal impaired awareness seizures: Seizures that impair consciousness or awareness. They may cause automatisms (e.g., lip smacking, fumbling, wandering), confusion, amnesia, or postictal (after seizure) symptoms (e.g., headache, fatigue, weakness)
- Generalized seizures: Seizures that involve both hemispheres of the brain and affect the whole body. They can be further divided into:
- Absence seizures: Seizures that cause brief lapses of consciousness or awareness. They may cause staring, blinking, or subtle movements
- Myoclonic seizures: Seizures that cause sudden brief muscle contractions or jerks. They may affect one or more limbs or the whole body
- Atonic seizures: Seizures that cause sudden loss of muscle tone or strength. They may cause falls or head drops
- Tonic seizures: Seizures that cause sudden increase of muscle tone or stiffness. They may cause rigid posture or extension of limbs
- Clonic seizures: Seizures that cause rhythmic muscle contractions or spasms. They may affect one or more limbs or the whole body
- Tonic-clonic seizures: Seizures that cause a combination of tonic and clonic phases. They may cause loss of consciousness, convulsions, biting of tongue, incontinence, etc.
- Focal seizures: Seizures that originate from a specific region of the brain and affect only one hemisphere. They can be further divided into:
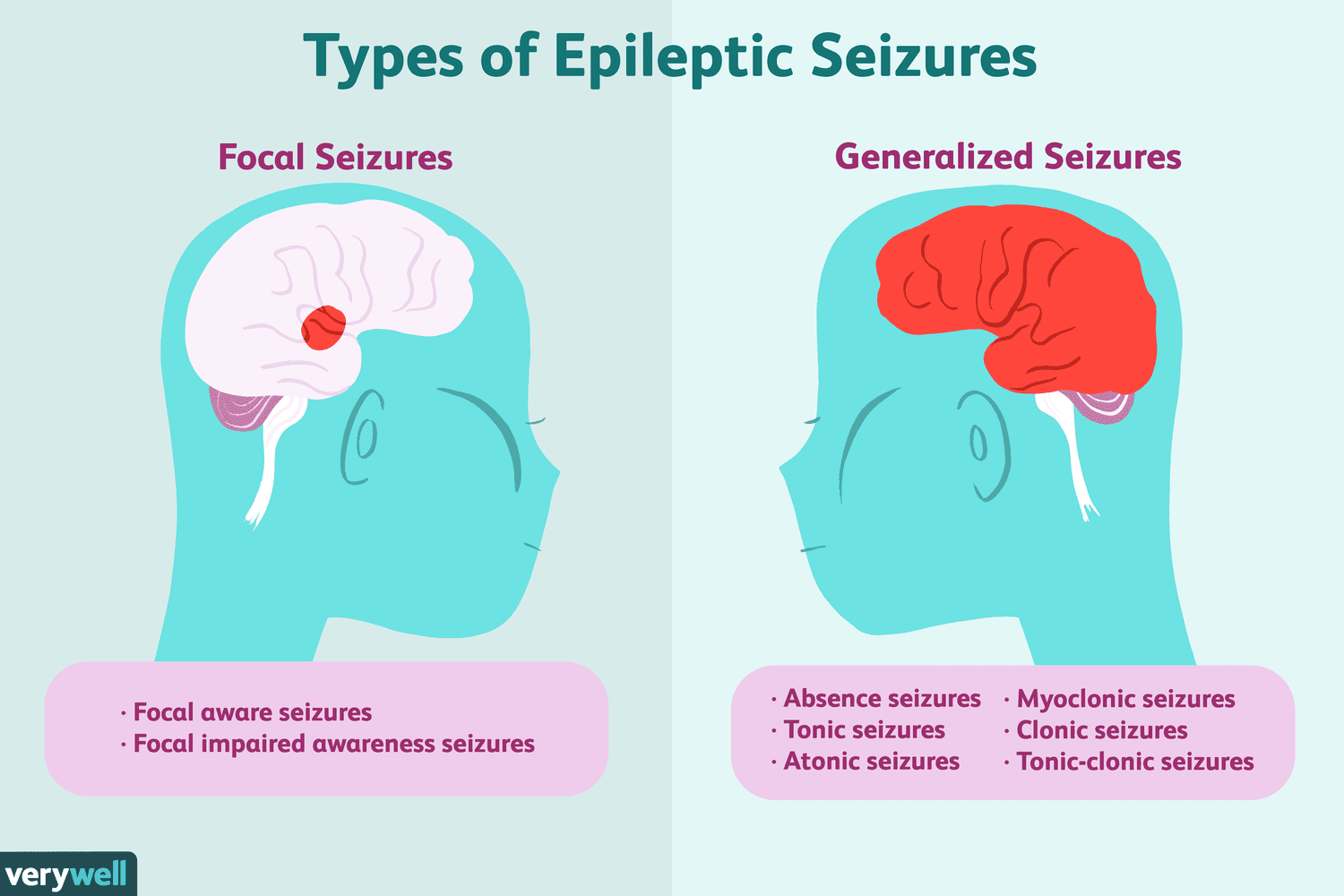
Causes of epilepsy and seizure disorders
- The causes of epilepsy and seizure disorders vary depending on the type and origin of the seizures.
- some common causes include
- genetic factors (e.g., mutations or syndromes),
- structural factors (e.g., trauma, stroke, tumor, infection),
- metabolic factors (e.g., electrolyte imbalance, hypoglycemia, hypoxia),
- immune factors (e.g., autoimmune diseases, inflammation),
- pharmacological factors (e.g., drug withdrawal, drug toxicity),
- idiopathic factors (e.g., unknown causes)
Risk factors of epilepsy and seizure disorders
- Some factors that may increase the risk of developing epilepsy and seizure disorders include
- age (infants and older adults),
- sex (male),
- family history,
- head injury,
- brain infection (e.g., meningitis, encephalitis),
- brain tumor,
- stroke,
- dementia, etc.
Signs and symptoms of epilepsy and seizure disorders
- The signs and symptoms of epilepsy and seizure disorders vary depending on the type and severity of the seizures.
- Some common manifestations include
- altered consciousness, behavior, sensation, motor activity, or autonomic function as described above;
- aura (a warning sign before a seizure such as a smell, sound, or feeling);
- prodrome (a mood or physical change before a seizure such as irritability, anxiety, or headache);
- postictal state (a recovery period after a seizure such as confusion, drowsiness, or weakness);
- status epilepticus (a prolonged or recurrent seizure that lasts more than 5 minutes or does not stop without treatment)
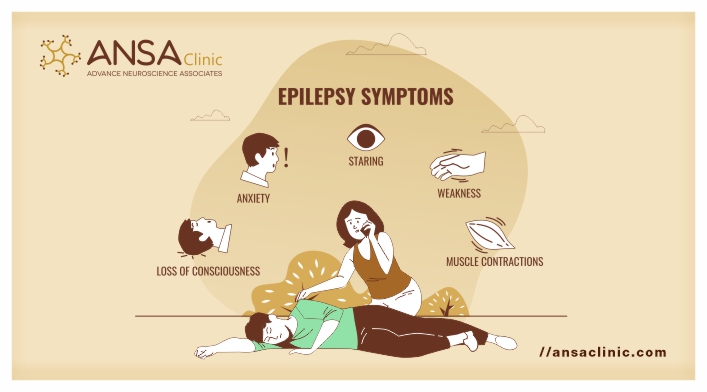
Diagnosis of epilepsy and seizure disorders
- The diagnosis of epilepsy and seizure disorders is based on clinical criteria that include medical history, physical examination, neurological examination, and exclusion of other possible causes.
- Some diagnostic tests that may be used to confirm the diagnosis or identify the type and origin of the seizures include:
- Electroencephalography (EEG): To measure the electrical activity of the brain using electrodes attached to the scalp that may show abnormal patterns or spikes that indicate seizure activity
- Neuroimaging: To visualize the structure and function of the brain using techniques such as CT, MRI, PET, SPECT, etc. that may show structural abnormalities or lesions that cause seizures
- Blood tests: To check for metabolic disorders, infection, inflammation, drug levels, etc. that may cause or mimic seizures
- Lumbar puncture: To obtain a sample of CSF for analysis and culture that may show infection, inflammation, or bleeding that cause seizures
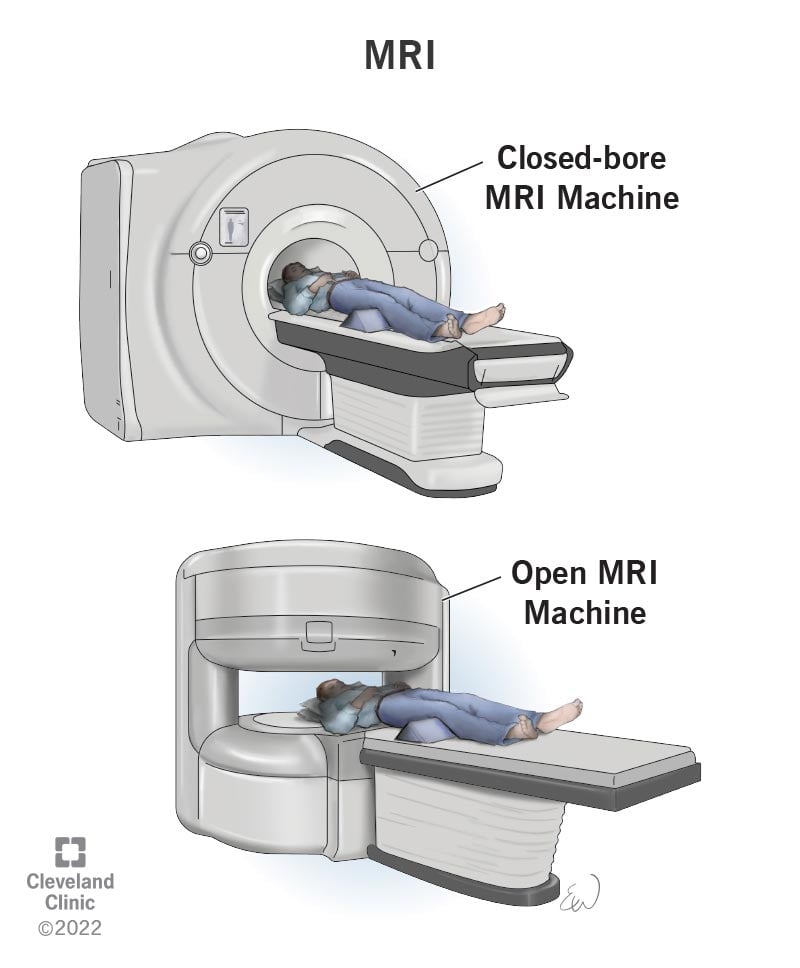
Treatment of epilepsy and seizure disorders
- The treatment of epilepsy and seizure disorders is aimed at controlling the seizures, reducing the side effects, improving the quality of life, and providing support and education for the patient and caregivers.
- Some treatment options include:
- Antiepileptic drugs (AEDs): To prevent or reduce the frequency and severity of seizures using drugs such as phenytoin, carbamazepine, valproic acid, lamotrigine, levetiracetam, etc. that act on various neurotransmitter systems or receptors to stabilize the electrical activity of the brain. These drugs may have side effects such as drowsiness, dizziness, rash, liver toxicity, etc.
- Surgery: To remove or disconnect the brain tissue that causes seizures using procedures such as lobectomy (removal of a lobe of the brain), hemispherectomy (removal of a hemisphere of the brain), corpus callosotomy (cutting of the corpus callosum that connects the two hemispheres of the brain), etc. These procedures may have risks such as infection, bleeding, stroke, cognitive impairment, etc.
- Neuromodulation: To stimulate or inhibit specific brain regions or nerves using devices such as vagus nerve stimulator (VNS), responsive neurostimulation (RNS), deep brain stimulation (DBS), transcranial magnetic stimulation (TMS), etc. that deliver electrical currents or magnetic fields to modulate neuronal activity. These devices may have side effects such as infection, bleeding, headache, voice changes, etc.
- Dietary therapy: To modify the intake of carbohydrates, fats, and proteins using diets such as ketogenic diet, modified Atkins diet, low glycemic index treatment, etc. that induce ketosis (a metabolic state that uses fat as the main source of energy) that may reduce seizure activity. These diets may have side effects such as weight loss, constipation, kidney stones, etc.
- Lifestyle therapy: To avoid or reduce triggers or factors that may provoke seizures using interventions such as stress management, sleep hygiene, exercise, etc. that involve coping with stress, getting enough sleep, performing physical activities, etc. These interventions may improve mood, energy, and well-being in epilepsy and seizure disorder patients
Treatment of epilepsy and seizure disorders
- The prevention of epilepsy and seizure disorders depends on the type and cause of the seizures.
- Some preventive measures include:
-
- avoiding head injury, infection, stroke, tumor, etc. that may damage the brain
- avoiding drugs, alcohol, caffeine, etc. that may alter the brain chemistry
- avoiding flashing lights, loud noises, etc. that may stimulate the brain
- taking AEDs as prescribed
- following a healthy lifestyle
- seeking medical attention if experiencing any signs or symptoms of seizures
Status epilepticus.
- The nervous system consists of the central nervous system (CNS) and the peripheral nervous system (PNS)
- The CNS includes the brain and the spinal cord, which are responsible for processing and integrating sensory and motor information
- The PNS includes the cranial and spinal nerves, which connect the CNS to the rest of the body
- The nervous system communicates through electrical impulses and chemical signals called neurotransmitters
- A seizure is a sudden, abnormal, and excessive discharge of neurons in the brain that causes a change in behavior, sensation, or consciousness
- Status epilepticus (SE) is a neurologic emergency that occurs when a seizure lasts longer than 5 minutes or when seizures occur very close together without recovery between them
- SE can be classified into two main types: generalized convulsive SE (GCSE) and nonconvulsive SE (NCSE)
- GCSE is characterized by repeated tonic-clonic seizures that involve both hemispheres of the brain and cause loss of consciousness, muscle contractions, and rhythmic jerking of the extremities
- NCSE is characterized by continuous or fluctuating altered mental status or behavior without overt motor manifestations
- SE can cause permanent brain damage or death if not treated promptly and effectively
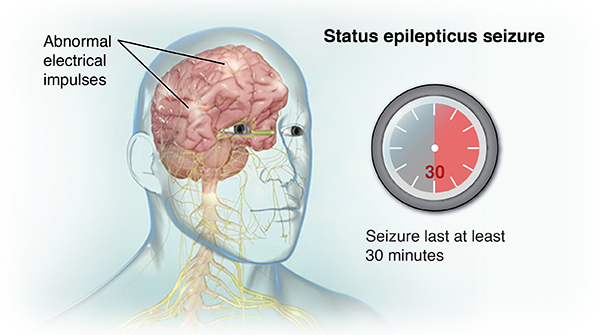
Causes and risk factors of Status epilepticus.
- SE can be caused by various factors that trigger or exacerbate seizures, such as:
- Acute or chronic CNS disorders, such as stroke, trauma, infection, tumor, malformation, degeneration, or inflammation
- Metabolic disturbances, such as hypoglycemia, hyponatremia, hypocalcemia, hypomagnesemia, uremia, hepatic encephalopathy, or acidosis
- Drug toxicity or withdrawal, such as from alcohol, benzodiazepines, barbiturates, opioids, anticonvulsants, or illicit substances
- Acute or chronic systemic illnesses, such as sepsis, fever, hypoxia, hypotension, anemia, or electrolyte imbalance
- Genetic or idiopathic epilepsy syndromes, such as Dravet syndrome, Lennox-Gastaut syndrome, or febrile seizures
- The risk factors for SE vary depending on the age group and the underlying etiology of seizures
- In general, some risk factors include:
- History of epilepsy or previous seizures
- Nonadherence or subtherapeutic levels of anticonvulsant therapy
- African American race
- Male gender
- Low socioeconomic status
- Comorbidities that affect the CNS or metabolism
Pathophysiology of Status epilepticus.
- SE occurs when the normal mechanisms that terminate a seizure fail to function properly
- This results in a mismatch of excitatory and inhibitory neurotransmitters in the brain, such as glutamate and gamma-aminobutyric acid (GABA)
- Glutamate is the main excitatory neurotransmitter that stimulates neuronal activity and increases calcium influx into neurons
- GABA is the main inhibitory neurotransmitter that reduces neuronal activity and increases chloride influx into neurons
- In SE, there is an excessive release of glutamate and a reduced release of GABA, leading to neuronal hyperexcitability and hypersynchronization
- SE can be divided into two phases: phase I and phase II
- Phase I occurs in the first 30 minutes of seizure activity and is characterized by increased autonomic activity and cerebral blood flow
- Each seizure causes a sharp increase in epinephrine, norepinephrine, and steroid concentrations that cause hypertension, tachycardia, cardiac arrhythmias, hyperglycemia, hyperthermia, sweating, and salivation
- Cerebral blood flow is increased to meet the increased metabolic demand of the brain during seizures
- Increased sympathetic and parasympathetic stimulation with muscle hypoxia can lead to ventricular arrhythmias, severe acidosis, and rhabdomyolysis (breakdown of muscle tissue)
- Shock, hypotension, hyperkalemia, and acute tubular necrosis may occur as a result of prolonged muscle contractions and tissue damage
- Phase II occurs after 30 minutes of seizure activity and is characterized by loss of cerebral autoregulation, decreased cerebral blood flow, increased intracranial pressure, and systemic hypotension
- The body is no longer able to compensate for the increased metabolic demand of the brain and the seizures become self-sustaining
- Hypoglycemia, hyperthermia, respiratory failure, hypoxia, respiratory and metabolic acidosis, hyperkalemia, hyponatremia, and uremia may develop as a result of impaired organ function and homeostasis
- The prolonged and recurrent seizures can cause neuronal injury and death through various mechanisms, such as:
- Excitotoxicity, which is the excessive stimulation of neurons by glutamate that leads to calcium overload and oxidative stress
- Apoptosis, which is the programmed cell death that is triggered by mitochondrial dysfunction and DNA damage
- Necrosis, which is the uncontrolled cell death that is caused by energy depletion and membrane disruption
- Inflammation, which is the activation of immune cells and cytokines that cause further neuronal damage and edema
- The neuronal injury and death can result in permanent brain damage or death, depending on the extent and location of the affected brain regions
Clinical manifestation of Status epilepticus.
- The clinical manifestations of SE depend on the type, duration, and severity of seizures, as well as the underlying etiology and comorbidities of the patient
- In general, some common signs and symptoms include:
- Altered level of consciousness, ranging from confusion to coma
- Motor manifestations, such as tonic-clonic movements, myoclonus, focal seizures, or subtle twitching
- Autonomic manifestations, such as hypertension, tachycardia, cardiac arrhythmias, hyperthermia, sweating, salivation, or incontinence
- Neurologic manifestations, such as headache, visual disturbances, aphasia, hemiparesis, or focal deficits
- Metabolic manifestations, such as hypoglycemia, hyponatremia, hyperkalemia, acidosis, or uremia
- Respiratory manifestations, such as hypoxia, hypercapnia, respiratory failure, or pulmonary edema
- Musculoskeletal manifestations, such as rhabdomyolysis, muscle breakdown, or compartment syndrome
Diagnosis of Status epilepticus.
- The diagnosis of SE is based on the clinical history and presentation of the patient, as well as the results of laboratory and imaging tests
- The diagnosis requires a high index of suspicion and prompt recognition of seizure activity and its duration
- The diagnosis can be confirmed by electroencephalography (EEG), which is the gold standard for detecting seizure activity in the brain
- EEG can also help to differentiate between GCSE and NCSE, as well as to identify the seizure focus and etiology
- EEG should be performed as soon as possible after the onset of SE or after the administration of initial anticonvulsant therapy
- Other diagnostic tests that may be performed include:
- Blood tests to measure glucose, electrolytes, calcium, magnesium, liver function tests, renal function tests, blood cultures, arterial blood gas, and serum anticonvulsant levels
- Urine tests to screen for drugs or toxins that may cause or worsen seizures
- Lumbar puncture to obtain cerebrospinal fluid (CSF) for analysis and culture to rule out CNS infection or inflammation
- Computed tomography (CT) scan or magnetic resonance imaging (MRI) of the brain to detect structural lesions or abnormalities that may cause or result from seizures
Treatment of Status epilepticus.
- The treatment of SE aims to stop the seizures as quickly and safely as possible, to identify and treat the underlying cause, and to prevent complications and recurrence
- The treatment involves a stepwise approach that consists of three stages: initial stabilization, initial therapy, and refractory therapy
- Initial stabilization involves securing the airway, breathing, and circulation (ABCs) of the patient, as well as monitoring vital signs, oxygen saturation, and glucose levels
- Initial therapy involves administering intravenous benzodiazepines, such as lorazepam or diazepam, as first-line anticonvulsants to terminate the seizures within 5 minutes of administration
- Refractory therapy involves administering intravenous non-benzodiazepine anticonvulsants, such as phenytoin, fosphenytoin, valproate, levetiracetam, or lacosamide, as second-line anticonvulsants to prevent seizure recurrence within 60 minutes of administration
- If seizures persist despite initial and refractory therapy, the patient is considered to have super-refractory SE and may require more aggressive treatment options, such as continuous infusion of anesthetic agents (e.g. propofol), ketamine, or barbiturates (e.g. pentobarbital), or other interventions such as hypothermia or surgery
Nursing care and management of Status epilepticus.
- The nursing care and management of patients with SE involves:
- Providing a safe and supportive environment for the patient, such as padding the bed rails, removing any potential hazards, maintaining a patent airway, administering oxygen, and suctioning secretions as needed
- Administering anticonvulsant medications as prescribed and monitoring their effectiveness and adverse effects, such as respiratory depression, hypotension, sedation, or allergic reactions
- Monitoring the patient’s vital signs, neurologic status, seizure activity, and EEG findings, and reporting any changes or abnormalities to the health care provider
- Performing frequent blood tests to assess glucose, electrolytes, calcium, magnesium, liver function, renal function, blood cultures, arterial blood gas, and serum anticonvulsant levels, and correcting any imbalances or abnormalities as ordered
- Providing adequate hydration and nutrition to the patient, either orally or parenterally, and preventing aspiration or dehydration
- Preventing complications such as infection, pressure ulcers, contractures, or venous thromboembolism by implementing appropriate measures such as hygiene, skin care, passive range of motion exercises, and prophylactic anticoagulation
- Educating the patient and family about the causes, signs and symptoms, treatment, and prevention of SE and seizures in general, as well as the importance of adherence to anticonvulsant therapy and regular follow-up visits
- Providing emotional support and reassurance to the patient and family and addressing any concerns or fears they may have
Complications and outcomes of Status epilepticus.
- SE is a life-threatening condition that can cause serious complications and poor outcomes if not treated promptly and effectively
- Some of the possible complications include:
- Permanent brain damage or death due to neuronal injury or death, cerebral edema, increased intracranial pressure, or cerebral ischemia
- Respiratory failure or pulmonary edema due to hypoxia, hypercapnia, or aspiration
- Cardiac arrest or arrhythmias due to autonomic instability, hypotension, or electrolyte imbalance
- Shock or multiorgan failure due to hypoperfusion, acidosis, or rhabdomyolysis
- Infection or sepsis due to impaired immunity, invasive procedures, or catheter-associated complications
- The outcomes of SE depend on various factors such as the type, duration, and severity of seizures, the underlying etiology and comorbidities of the patient, and the timeliness and effectiveness of treatment
- Some of the possible outcomes include:
- Complete recovery without any residual neurologic deficits or recurrence of seizures
- Partial recovery with some degree of neurologic impairment or increased frequency or severity of seizures
- Persistent vegetative state or coma due to extensive brain damage or anoxic injury
- Death due to refractory seizures or complications
Brain Tumors: Gliomas, Meningiomas, Metastatic brain tumors
- Brain tumors are abnormal growths of cells in the brain or surrounding tissues
- Brain tumors can be classified as primary or secondary, benign or malignant, and according to their location and cell type
- Primary brain tumors originate in the brain or its coverings (meninges), such as gliomas, meningiomas, pituitary adenomas, acoustic neuromas, etc.
- Secondary brain tumors (also called metastatic brain tumors) result from cancer cells that spread from another part of the body to the brain, such as lung cancer, breast cancer, melanoma, etc.
- Benign brain tumors are noncancerous and do not invade nearby tissues or spread to other parts of the body. However, they can still cause symptoms by compressing or displacing normal brain structures
- Malignant brain tumors are cancerous and can invade nearby tissues or spread to other parts of the body. They are more aggressive and have a poorer prognosis than benign brain tumors
- The location of a brain tumor determines its effects on the brain functions. For example, a tumor in the frontal lobe can affect personality, judgment, memory, etc., while a tumor in the temporal lobe can affect language, hearing, emotion, etc.
- The cell type of a brain tumor determines its characteristics and behavior. For example, gliomas are derived from glial cells and are graded from I to IV based on their degree of malignancy. Grade I gliomas are slow-growing and benign, while grade IV gliomas (glioblastoma multiforme) are fast-growing and highly malignant
- The nervous system consists of the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS includes the brain and the spinal cord, while the PNS includes the nerves that connect the CNS to the rest of the body.
- The brain is composed of billions of neurons (nerve cells) that communicate with each other through electrical and chemical signals. The neurons are supported by glial cells, which provide structural and functional support, such as nutrition, metabolism, immunity, myelin formation, and synaptic modulation.
- A brain tumor is an abnormal mass of tissue that grows in or around the brain. Brain tumors can be primary (originating in the brain) or secondary (spreading from another part of the body). Primary brain tumors can be benign (non-cancerous) or malignant (cancerous).
- The nervous system is composed of the central nervous system (CNS), which includes the brain and spinal cord, and the peripheral nervous system (PNS), which includes the cranial and spinal nerves.
- The CNS is protected by three layers of membranes called meninges: the dura mater, the arachnoid mater, and the pia mater. The meninges also contain blood vessels and cerebrospinal fluid (CSF) that nourish and cushion the CNS.
Gliomas
- A glioma is a tumor that originates from the glial cells in the brain or spinal cord. It is the most common type of primary brain tumor, accounting for about 30% of all brain tumors. Gliomas can affect children or adults, but are more common in older adults (over 65) and white people.
- Gliomas are classified into different types based on the type of glial cell they arise from: astrocytomas (from astrocytes), ependymomas (from ependymal cells), oligodendrogliomas (from oligodendrocytes), or mixed gliomas (from more than one type of glial cell).
- Gliomas are also graded according to their degree of malignancy (cancerousness), aggressiveness, and invasiveness. The World Health Organization (WHO) uses a four-tier grading system: grade I (low-grade or benign), grade II (low-grade or slow-growing), grade III (high-grade or anaplastic), and grade IV (high-grade or glioblastoma).
- Gliomas can cause various symptoms depending on their location, size, and growth rate. Some common symptoms include headache, nausea, vomiting, confusion, memory loss, personality changes, vision problems, speech difficulties, seizures, muscle weakness, and balance problems.
- Gliomas are diagnosed by a neurological examination, imaging tests (such as CT scan, MRI scan, PET scan), and biopsy (taking a sample of the tumor tissue for microscopic analysis).
- Gliomas are treated by a multidisciplinary team of specialists, such as neurologists, neurosurgeons, radiation oncologists, medical oncologists, nurses, and other allied health professionals. The treatment options include surgery (to remove as much of the tumor as possible), radiation therapy (to destroy the remaining tumor cells with high-energy beams), chemotherapy (to kill the tumor cells with drugs), targeted drug therapy (to block specific molecules or pathways that drive tumor growth), and supportive care (to manage symptoms and complications).
- Astrocytoma is the most common type of glioma. It arises from astrocytes, which are star-shaped cells that regulate the blood-brain barrier, the extracellular fluid, and neurotransmitter uptake. Astrocytomas can be low-grade (grade I or II) or high-grade (grade III or IV). Low-grade astrocytomas grow slowly and may not cause symptoms for years. High-grade astrocytomas grow rapidly and invade nearby tissues. The most aggressive form of astrocytoma is glioblastoma (grade IV), which has a poor prognosis (median survival of 15 months). A rare but very malignant form of astrocytoma that affects children is diffuse intrinsic pontine glioma (DIPG), which grows in the brain stem and causes cranial nerve dysfunction.
- Oligodendroglioma is a rare type of glioma that arises from oligodendrocytes, which are cells that produce myelin (a fatty substance that insulates the nerve fibers). Oligodendrogliomas tend to grow slowly and have a better prognosis than astrocytomas. They are usually low-grade (grade II) or anaplastic (grade III). Oligodendrogliomas often have genetic mutations that make them more sensitive to chemotherapy and radiation therapy. They are more common in adults than children and usually occur in the frontal or temporal lobes of the brain.
- Ependymoma is another rare type of glioma that arises from ependymal cells, which are cells that line the ventricles (fluid-filled spaces) of the brain and the central canal of the spinal cord. Ependymomas can be low-grade (grade I or II) or anaplastic (grade III). They can block the flow of cerebrospinal fluid (CSF), causing increased intracranial pressure (ICP) and hydrocephalus (water on the brain). Ependymomas can also spread through the CSF to other parts of the brain or spinal cord. They are more common in children than adults and usually occur in the posterior fossa (the back part of the skull) or the spinal cord.
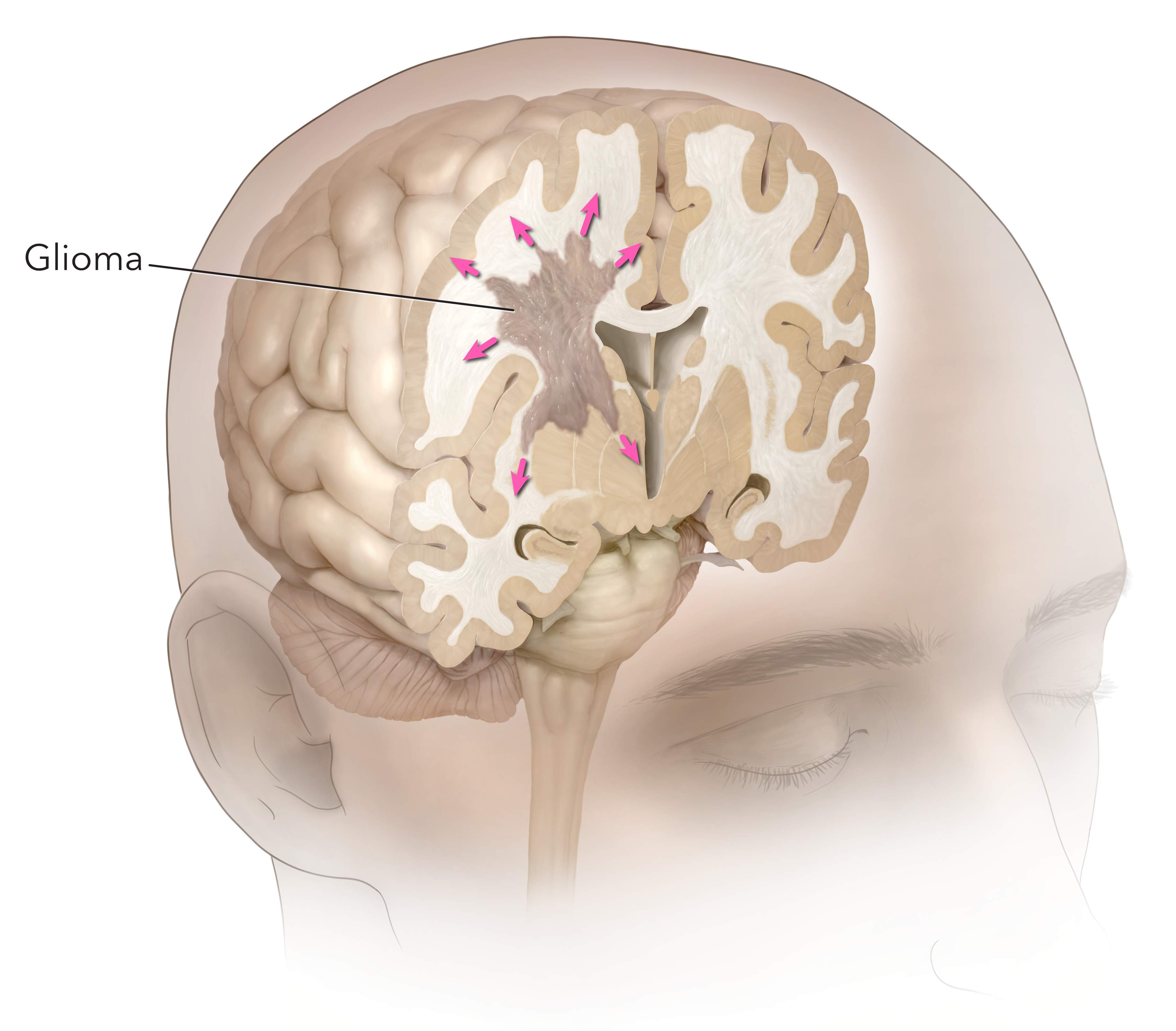
Complications and Challenges
- Gliomas can cause various complications and challenges for patients and their families. Some of these include:
- Seizures: Gliomas can irritate or damage the brain cells that control electrical activity, causing abnormal bursts of signals that result in seizures. Seizures can affect different parts of the body, such as the muscles, sensations, emotions, or consciousness. Seizures can be treated with anticonvulsant drugs, such as gabapentin or lamotrigine, but may have side effects such as drowsiness, dizziness, or rash.
- Cognitive impairment: Gliomas can affect the brain functions that are responsible for thinking, learning, memory, language, and behavior. Cognitive impairment can manifest as confusion, forgetfulness, difficulty concentrating, aphasia (loss of speech), dysarthria (slurred speech), or personality changes. Cognitive impairment can be assessed by neuropsychological tests and managed by cognitive rehabilitation, speech therapy, occupational therapy, or supportive devices.
- Recurrence: Gliomas can recur after treatment, either in the same location or in a different part of the brain or spinal cord. Recurrence can be detected by regular follow-up imaging tests and monitored by tumor markers, such as MGMT (a gene that predicts response to chemotherapy) or IDH1/2 (genes that indicate tumor grade and prognosis). Recurrence can be treated by repeat surgery, radiation therapy, chemotherapy, targeted drug therapy, or clinical trials.
- Quality of life: Gliomas can affect the physical, emotional, social, and spiritual aspects of a patient’s life. Quality of life can be measured by standardized questionnaires and improved by palliative care, which aims to relieve symptoms and enhance comfort. Quality of life can also be enhanced by psychosocial support, such as counseling, support groups, education, or complementary therapies.
Nursing Care
- Nursing care for patients with gliomas involves applying the nursing process to plan and provide holistic care that meets the individual needs and preferences of each patient and their family. The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation.
- Assessment: The nurse collects data about the patient’s health history, physical examination, diagnostic tests, symptoms, complications, medications, treatments, coping strategies, support systems, and goals. The nurse uses various tools and techniques to gather data, such as observation, interview, inspection, palpation, percussion, auscultation, or standardized scales.
- Diagnosis: The nurse analyzes the data and identifies the patient’s actual or potential health problems or needs. The nurse uses standardized terminology to formulate nursing diagnoses, which are statements that describe the patient’s response to their health condition. For example, a nursing diagnosis for a patient with glioma could be “Risk for ineffective cerebral tissue perfusion related to increased intracranial pressure”.
- Planning: The nurse prioritizes the patient’s nursing diagnoses and sets measurable and realistic goals and outcomes for each one. The nurse also selects appropriate nursing interventions that are evidence-based and consistent with the patient’s preferences and values. For example, a goal for a patient with glioma could be “The patient will maintain normal intracranial pressure within 24 hours” and an intervention could be “Monitor vital signs, neurological status, and ICP hourly”.
- Implementation: The nurse performs the planned interventions and documents their actions and outcomes. The nurse also coordinates care with other members of the healthcare team and involves the patient and family in decision making and education. An example of implementation could be “Administer anticonvulsant drugs as prescribed and observe for adverse effects”.
- Evaluation: The nurse evaluates the patient’s progress and outcomes and compares them with the expected goals and outcomes. The nurse also modifies the plan of care as needed based on the evaluation results and feedback from the patient and family. For example, an evaluation for a patient with glioma could be “The patient’s intracranial pressure was within normal range (10-15 mmHg) for 24 hours and the patient reported no headache, nausea, or vision problems”.
Meningiomas
- A meningioma is a tumor that arises from the meningeal cells, usually in the dura mater. It is not technically a brain tumor, but it can compress or invade the adjacent brain tissue, nerves, or vessels, causing various neurological symptoms.
- Meningiomas are the most common type of primary CNS tumor, accounting for about one-third of all cases. They occur more frequently in middle-aged women, but they can affect anyone at any age.
- Meningiomas are classified into three grades based on their histological features and biological behavior: grade I (benign), grade II (atypical), and grade III (malignant). Each grade includes different subtypes that have different molecular markers and prognoses.

- The exact cause of meningiomas is unknown, but some possible factors include:
- Exposure to ionizing radiation, especially in childhood or during radiation therapy for other conditions.
- Genetic mutations or disorders, such as neurofibromatosis type 2 (NF2), which is associated with bilateral vestibular schwannomas and multiple meningiomas.
- Hormonal influences, such as estrogen receptors found in some meningiomas, which may explain the higher incidence in women. Some studies suggest that oral contraceptives or hormone replacement therapy may increase the risk of meningioma growth.
- Other factors, such as obesity, head trauma, infection, or inflammation, which may contribute to meningioma development or progression.
- The signs and symptoms of meningiomas depend on their location, size, grade, and rate of growth. Some common manifestations include:
- Headache, which is often worse in the morning or with changes in position. It may be caused by increased intracranial pressure (ICP), mass effect, or irritation of pain-sensitive structures.
- Seizures, which may be focal or generalized. They may result from compression or invasion of cortical areas or epileptogenic foci.
- Visual disturbances, such as blurred vision, diplopia (double vision), hemianopia (loss of half of the visual field), or papilledema (swelling of the optic disc). They may occur due to compression or invasion of the optic nerve, chiasm, tract, or radiation.
- Hearing loss or tinnitus (ringing in the ears), which may be caused by compression or invasion of the acoustic nerve or vestibulocochlear nerve.
- Cranial nerve palsies, which may affect any of the 12 cranial nerves and cause various sensory or motor deficits. For example, facial weakness or numbness may result from compression or invasion of the facial nerve or trigeminal nerve.
- Cognitive impairment or personality changes, which may be due to compression or invasion of frontal lobes, temporal lobes, or other areas involved in memory, language, judgment, or behavior.
- Motor weakness or sensory loss, which may affect one or more limbs depending on the location of the tumor. It may be caused by compression or invasion of motor cortex, corticospinal tract, or spinal cord.
- The diagnosis of meningiomas is based on a combination of clinical history, physical examination, neurological assessment, and imaging studies. Some common tests and procedures include:
- Magnetic resonance imaging (MRI), which is the preferred modality for detecting and characterizing meningiomas. It can provide detailed information about the tumor size, shape, location, enhancement pattern, edema, mass effect, and invasion. It can also help differentiate between different subtypes of meningiomas based on their signal intensity and contrast uptake.
- Computed tomography (CT) scan, which can also show the presence and features of meningiomas, but with less resolution and contrast than MRI. It can be useful for detecting calcifications, bone erosion, or hyperostosis (thickening of the skull) associated with some meningiomas.
- Angiography, which can show the blood supply and vascularization of meningiomas. It can help plan for surgical resection or embolization of the tumor.
- Lumbar puncture, which can measure the CSF pressure and analyze the CSF composition. It can help rule out other causes of increased ICP, such as infection or hemorrhage. It can also detect tumor cells or markers in the CSF in some cases of malignant meningiomas.
- Biopsy, which is the definitive method for confirming and grading meningiomas. It involves taking a small sample of tumor tissue and examining it under a microscope. It can also help identify the molecular markers and genetic alterations of the tumor, which can guide the treatment and prognosis.
- The treatment of meningiomas depends on several factors, such as the tumor grade, size, location, symptoms, and patient preferences. Some common options include:
- Surgery, which is the mainstay of treatment for most meningiomas. The goal is to achieve a gross total resection (GTR), which means removing the entire tumor and its attachments to the dura mater. This can improve the symptoms, reduce the recurrence rate, and prolong the survival. However, surgery may not be possible or advisable in some cases, such as when the tumor is located in an inaccessible or eloquent area (such as the brainstem or optic nerve), or when the patient has significant comorbidities or risks. In these cases, a subtotal resection (STR) or a biopsy may be performed instead.
- Radiation therapy, which involves delivering high-energy rays to the tumor site to destroy the tumor cells or prevent their growth. It can be used as an adjuvant therapy after surgery to reduce the recurrence rate, especially for grade II or III meningiomas or for residual tumors after STR. It can also be used as a primary therapy for inoperable or recurrent meningiomas, or as a palliative therapy for symptomatic relief. There are different types of radiation therapy, such as external beam radiation therapy (EBRT), stereotactic radiosurgery (SRS), or brachytherapy.
- Pharmacological management, which involves using medications to treat the symptoms or slow down the growth of meningiomas. There are no specific drugs approved for meningiomas, but some agents that have been used in clinical trials or off-label include corticosteroids (to reduce edema and ICP), anticonvulsants (to prevent seizures), analgesics (to relieve pain), antiangiogenic drugs (to inhibit blood vessel formation), hormonal drugs (to block estrogen receptors), and chemotherapeutic drugs (to kill tumor cells).
Nursing Interventions
- The nursing interventions for meningiomas are aimed at providing holistic care to the patient and family throughout the course of the disease. Some common interventions include:
- Assessing and monitoring the patient’s neurological status, vital signs, ICP, pain level, and response to treatment. Reporting any changes or abnormalities to the health care provider promptly.
- Administering medications as prescribed and monitoring their effects and side effects. Educating the patient and family about the purpose, dosage, route, frequency, and potential interactions of each drug.
- Preparing the patient for surgery or radiation therapy and providing postoperative or post-treatment care. Following the standard precautions and protocols for infection control, wound care, fluid and electrolyte balance, nutrition support, mobility assistance, and complication prevention.
- Providing emotional support and counseling to the patient and family. Addressing their fears, concerns, expectations, and coping strategies. Referring them to appropriate resources or services if needed.
- Educating the patient and family about the disease process, treatment options, prognosis, and follow-up care. Encouraging them to participate in decision making and self-care activities. Providing them with written instructions and contact information.
Complications and Outcomes
- The complications and outcomes of meningiomas vary depending on several factors, such as the tumor grade, size, location, treatment modality, and patient characteristics. Some possible complications include:
- Recurrence or progression of the tumor, which may require repeated surgery or radiation therapy. The recurrence rate is higher for grade II or III meningiomas, or for tumors that are incompletely resected.
- Neurological deficits, which may result from compression or invasion of brain tissue, nerves, or vessels by the tumor or its treatment. They may affect vision, hearing, speech, cognition, motor function, sensory function, or cranial nerve function. Some deficits may be temporary or reversible, while others may be permanent or progressive.
- Increased ICP, which may cause headache, nausea, vomiting, drowsiness, confusion, or coma. It may result from tumor growth, edema, hemorrhage, hydrocephalus, or infection. It may require urgent intervention to prevent brain herniation or death.
- Infection, which may occur at the surgical site, in the CSF, or in the bloodstream. It may cause fever, chills, malaise, wound drainage, meningitis, or sepsis. It may require antibiotic therapy and wound care.
- Hemorrhage, which may occur during or after surgery or radiation therapy. It may cause bleeding in the brain tissue, subdural space, epidural space, or subarachnoid space. It may cause increased ICP, stroke-like symptoms, or death.
- Radiation-induced injury, which may occur after radiation therapy. It may cause delayed effects such as radiation necrosis (tissue death), vasculopathy (blood vessel damage), leukoencephalopathy (white matter damage), or secondary tumors. It may cause neurological deterioration or cognitive decline.
- The outcomes of meningiomas depend on the tumor grade and the extent of resection. The survival rates are generally high for grade I meningiomas (>90% at 10 years), intermediate for grade II meningiomas (50-80% at 10 years), and low for grade III meningiomas (10-30% at 10 years). The quality of life is also affected by the presence and severity of neurological deficits and complications.
Metastatic Brain Tumors
- Metastatic brain tumors are more common than primary brain tumors. They account for about 40% of all intracranial neoplasms1
- Metastatic brain tumors usually occur in multiple sites within the brain. The most common locations are the cerebral hemispheres (80%), cerebellum (15%), and brainstem (5%)2
- Metastatic brain tumors usually arise from cancers that have a high propensity to spread to the brain via hematogenous or lymphatic routes. The most common primary cancers that cause metastatic brain tumors are lung cancer (50%), breast cancer (15%), melanoma (10%), renal cell carcinoma (5%), and colorectal cancer (5%)3
- Metastatic brain tumors can cause symptoms by increasing intracranial pressure (ICP), causing cerebral edema (swelling), hemorrhage (bleeding), or hydrocephalus (accumulation of cerebrospinal fluid), or by affecting specific functions of the affected regions of the brain
- The symptoms of metastatic brain tumors depend on their size, number, location, rate of growth, and response to treatment. The most common symptoms are headache (50%), seizures (30%), focal neurological deficits (25%), cognitive impairment (20%), nausea/vomiting (15%), papilledema (10%), and personality changes (10%)4
Diagnostic Tests and Procedures
- The diagnosis of brain tumors and metastatic brain tumors is based on a combination of clinical history, physical examination, neurological examination, imaging studies, laboratory tests, and biopsy
- Clinical history: The patient’s medical history, family history, risk factors, symptoms, duration, frequency, severity, and triggers are obtained to assess the possibility of a brain tumor
- Physical examination: The patient’s vital signs, general appearance, skin condition, head/neck examination, eye examination, ear/nose/throat examination, cardiovascular examination, respiratory examination, abdominal examination, musculoskeletal examination, and neurological examination are performed to evaluate the patient’s overall health status and detect any signs of increased ICP, focal neurological deficits, or systemic diseases
- Neurological examination: The patient’s mental status, cranial nerve functions, motor functions, sensory functions, coordination, reflexes, and gait are assessed to determine the location and extent of the brain tumor
- Imaging studies: The most commonly used imaging modalities for brain tumors and metastatic brain tumors are computed tomography (CT) scan and magnetic resonance imaging (MRI) scan. These tests can provide detailed information about the size, shape, location, number, and characteristics of the brain tumor and its effects on the surrounding structures. Other imaging tests that may be used are positron emission tomography (PET) scan, single-photon emission computed tomography (SPECT) scan, magnetic resonance spectroscopy (MRS), and magnetic resonance angiography (MRA)
- Laboratory tests: The patient’s blood, urine, cerebrospinal fluid (CSF), and tumor tissue samples may be analyzed to detect any abnormalities in the levels of glucose, electrolytes, blood cells, hormones, tumor markers, genetic mutations, etc. that may indicate the presence or type of brain tumor
- Biopsy: The definitive diagnosis of a brain tumor or a metastatic brain tumor requires a biopsy, which is the removal of a small sample of the tumor tissue for microscopic examination. A biopsy can confirm the type and grade of the tumor and guide the treatment plan. A biopsy can be performed by surgery (open or stereotactic) or by needle aspiration (fine-needle or core-needle)
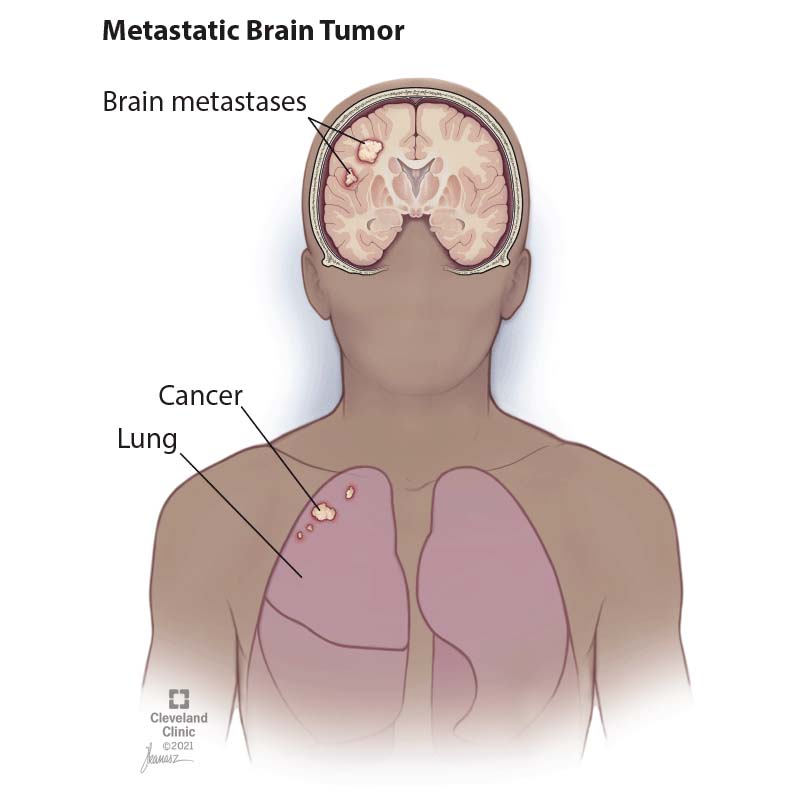
Treatment Options and Nursing Interventions
- The treatment of brain tumors and metastatic brain tumors depends on several factors, such as the type, grade, size, location, number, and symptoms of the tumor; the patient’s age, general health, preferences, and goals; and the availability and effectiveness of the treatment modalities
- The main treatment options for brain tumors and metastatic brain tumors are surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapy, and palliative care
- Surgery: Surgery is the preferred treatment for most brain tumors and some metastatic brain tumors that are accessible and resectable. Surgery aims to remove as much of the tumor as possible while preserving the normal brain function. Surgery can also reduce the mass effect of the tumor and relieve the symptoms of increased ICP. Surgery can be performed by craniotomy (opening of the skull) or by minimally invasive techniques (endoscopy or laser ablation). Surgery may be combined with other treatments such as radiation therapy or chemotherapy
- Radiation therapy: Radiation therapy uses high-energy rays or particles to kill cancer cells or stop their growth. Radiation therapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that are inoperable or incompletely resected. Radiation therapy can also be used as an adjuvant treatment after surgery to prevent recurrence or as a palliative treatment to relieve symptoms. Radiation therapy can be delivered by external beam radiation therapy (EBRT), stereotactic radiosurgery (SRS), brachytherapy (implantation of radioactive seeds), or radioisotope therapy (injection of radioactive substances)
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop their growth. Chemotherapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that are sensitive to drugs. Chemotherapy can also be used as an adjuvant treatment after surgery or radiation therapy to prevent recurrence or as a palliative treatment to relieve symptoms. Chemotherapy can be administered by oral route, intravenous route, intrathecal route (injection into the CSF), or intra-arterial route (injection into the blood vessel supplying the tumor). Chemotherapy may be combined with other treatments such as radiation therapy or targeted therapy
- Immunotherapy: Immunotherapy uses substances that stimulate or modify the immune system to fight cancer cells. Immunotherapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that express specific antigens or receptors. Immunotherapy can also be used as an adjuvant treatment after surgery or radiation therapy to prevent recurrence or as a palliative treatment to relieve symptoms. Immunotherapy can be administered by intravenous route, subcutaneous route, intratumoral route (injection into the tumor), or intraventricular route (injection into the ventricles of the brain). Immunotherapy may include monoclonal antibodies, cytokines, vaccines, or adoptive cell transfer
- Targeted therapy: Targeted therapy uses drugs that target specific molecules or pathways involved in the growth and survival of cancer cells. Targeted therapy can be used as a primary treatment for some brain tumors and metastatic brain tumors that have specific genetic mutations or alterations. Targeted therapy can also be used as an adjuvant treatment after surgery or radiation therapy to prevent recurrence or as a palliative treatment to relieve symptoms. Targeted therapy can be administered by oral route, intravenous route, or intra-arterial route (injection into the blood vessel supplying the tumor). Targeted therapy may include tyrosine kinase inhibitors, angiogenesis inhibitors, or proteasome inhibitors
Palliative Care
- Palliative care is a holistic approach that aims to improve the quality of life of patients and their families who are facing life-threatening illnesses such as brain tumors and metastatic brain tumors
- Palliative care focuses on relieving the physical, emotional, social, and spiritual suffering of patients and their families
- Palliative care can be provided at any stage of the disease, along with other treatments or as the main treatment when no cure is possible
- Palliative care can be delivered by a multidisciplinary team of health professionals, such as physicians, nurses, social workers, psychologists, chaplains, etc.
- Palliative care can involve various interventions, such as pain management, symptom control, psychosocial support, spiritual care, advance care planning, hospice care, and bereavement care
Complications and Prognosis
- Brain tumors and metastatic brain tumors can cause various complications that can affect the patient’s survival and quality of life
- The most common complications are increased ICP, cerebral herniation, brainstem compression, hydrocephalus, seizures, hemorrhage, infection, neurological deficits, cognitive impairment, behavioral changes, endocrine disorders, and systemic effects
- The prognosis of brain tumors and metastatic brain tumors depends on several factors, such as the type, grade, size, location, number, and symptoms of the tumor; the patient’s age, general health, preferences, and goals; and the availability and effectiveness of the treatment modalities
- The prognosis of brain tumors and metastatic brain tumors is usually poor. The median survival time for primary brain tumors ranges from 1 to 15 years, depending on the type and grade of the tumor. The median survival time for metastatic brain tumors is about 6 months
Summary
- The nervous system consists of two main divisions: the CNS and the PNS
- The CNS consists of the brain and spinal cord, which process sensory information, generate motor commands, and regulate cognitive and emotional functions
- The PNS consists of the cranial and spinal nerves, which connect the CNS to the rest of the body and transmit sensory and motor signals
- The PNS is further divided into two subdivisions: the SNS and the ANS
- The SNS controls voluntary movements of skeletal muscles and provides sensory feedback from the skin, joints, and muscles
- The ANS regulates involuntary functions of smooth muscles, cardiac muscles, and glands. It has two branches: the SNS and the PNS
- TBI is any damage to the brain caused by an external force or impact. It can be classified as mild, moderate, or severe based on the GCS, or as focal or diffuse based on the location and extent of brain damage
- A concussion is a type of mild TBI that results from a sudden acceleration or deceleration of the head that causes the brain to move within the skull. It can cause temporary alteration or loss of consciousness, memory loss, confusion, headache, dizziness, nausea, vomiting, blurred vision, sensitivity to light or noise, mood changes, or sleep disturbances. It can also cause PCS, which is a persistent or delayed onset of symptoms that last for weeks or months after the injury. PCS can include cognitive impairment, emotional problems, physical complaints, or behavioral changes
- A concussion can be diagnosed by a thorough history taking, physical examination, neurological assessment (including GCS), and symptom checklist. Imaging tests are usually not indicated unless there is suspicion of intracranial bleeding or skull fracture
- A concussion can be treated by rest (both physical and mental), symptom management (such as analgesics for headache or antiemetics for nausea), education (about expected recovery course and possible complications), and gradual return to normal activities (following a stepwise protocol that monitors symptom exacerbation). Repeated concussions can increase the risk of CTE, which is a progressive neurodegenerative disorder characterized by cognitive decline, behavioral disturbances, mood disorders, motor impairment, and dementia
- A stroke is any interruption of blood flow to a part of the brain that causes ischemia and necrosis of brain tissue. It can be classified as ischemic or hemorrhagic based on the underlying cause
- Ischemic stroke is caused by a blockage of a blood vessel that supplies the brain, usually due to a thrombus or an embolus
- Hemorrhagic stroke is caused by a rupture of a blood vessel that bleeds into the brain, usually due to an aneurysm or an arteriovenous malformation
- A TIA is a temporary interruption of blood flow to a part of the brain that causes reversible neurological symptoms that last for less than 24 hours. A TIA is often a warning sign of an impending stroke and requires urgent evaluation and treatment
- A stroke can cause various neurological deficits depending on the location and size of the affected area. The most common symptoms include weakness or paralysis of one side of the body (hemiparesis or hemiplegia), numbness or tingling of one side of the body (hemisensory loss), difficulty with speech or language (aphasia), difficulty with vision (hemianopia), difficulty with coordination or balance (ataxia), difficulty with swallowing (dysphagia), or altered level of consciousness
- SE is a neurologic emergency that occurs when a seizure lasts longer than 5 minutes or when seizures occur very close together without recovery between them
- SE can be classified into two main types: GCSE and NCSE, which have different clinical manifestations and require different diagnostic approaches
- SE can be caused by various factors that trigger or exacerbate seizures, such as CNS disorders, metabolic disturbances, drug toxicity or withdrawal, systemic illnesses, or genetic or idiopathic epilepsy syndromes
- SE occurs when the normal mechanisms that terminate a seizure fail to function properly, resulting in a mismatch of excitatory and inhibitory neurotransmitters in the brain, such as glutamate and GABA
- SE can be divided into two phases: phase I and phase II, which have different effects on the cerebral blood flow, metabolism, and neuronal injury
- The treatment of SE aims to stop the seizures as quickly and safely as possible, to identify and treat the underlying cause, and to prevent complications and recurrence
- The treatment involves a stepwise approach that consists of three stages: initial stabilization, initial therapy, and refractory therapy
- The nursing care and management of patients with SE involves providing a safe and supportive environment for the patient, administering anticonvulsant medications and monitoring their effectiveness and adverse effects, monitoring the patient’s vital signs, neurologic status, seizure activity, and EEG findings, performing frequent blood tests to assess glucose, electrolytes, calcium, magnesium, liver function, renal function, blood cultures, arterial blood gas, and serum anticonvulsant levels, providing adequate hydration and nutrition to the patient, preventing complications such as infection, pressure ulcers, contractures, or venous thromboembolism by implementing appropriate measures such as hygiene, skin care, passive range of motion exercises, and prophylactic anticoagulation educating the patient and family about the causes, signs and symptoms, treatment, and prevention of SE and seizures in general, as well as the importance of adherence to anticonvulsant therapy and regular follow-up visits, and providing emotional support and reassurance to the patient and family
- SE is a life-threatening condition that can cause serious complications and poor outcomes if not treated promptly and effectively
- The possible complications include permanent brain damage or death, respiratory failure or pulmonary edema, cardiac arrest or arrhythmias, shock or multiorgan failure, or infection or sepsis
- The possible outcomes include complete recovery without any residual neurologic deficits or recurrence of seizures, partial recovery with some degree of neurologic impairment or increased frequency or severity of seizures, persistent vegetative state or coma due to extensive brain damage or anoxic injury, or death due to refractory seizures or complications
- Gliomas are primary brain tumors that originate from glial cells in the brain or spinal cord. They are classified into different types based on the type of glial cell they arise from, their grade, and their location.
- Gliomas can cause various symptoms and complications depending on their size, growth rate, and location. Some common ones include seizures, cognitive impairment, recurrence, and reduced quality of life.
- Gliomas are diagnosed by neurological examination, imaging tests, and biopsy. They are treated by surgery, radiation therapy, chemotherapy, targeted drug therapy, and supportive care.
- Nursing care for patients with gliomas involves applying the nursing process to plan and provide holistic care that meets the individual needs and preferences of each patient and their family. The nursing process consists of assessment, diagnosis, planning, implementation, and evaluation.
- Meningiomas are tumors that arise from the meningeal cells in the dura mater. They are classified into three grades based on their histological features and biological behavior: grade I (benign), grade II (atypical), and grade III (malignant).
- Meningiomas are caused by unknown factors, but some possible risk factors include radiation exposure, genetic mutations, hormonal influences, and other factors.
- Meningiomas cause various signs and symptoms depending on their location, size, grade, and rate of growth. Some common manifestations include headache, seizures, visual disturbances, hearing loss, cranial nerve palsies, cognitive impairment, and motor weakness.
- Meningiomas are diagnosed by clinical history, physical examination, neurological assessment, and imaging studies. Some common tests and procedures include MRI, CT scan, angiography, lumbar puncture, and biopsy.
- Meningiomas are treated by surgery, radiation therapy, or pharmacological management. The goal is to achieve a gross total resection of the tumor and to prevent recurrence or progression.
- Meningiomas can cause complications such as recurrence, neurological deficits, increased ICP, infection, hemorrhage, or radiation-induced injury. The outcomes depend on the tumor grade and the extent of resection. The survival rates are high for grade I meningiomas, intermediate for grade II meningiomas, and low for grade III meningiomas. The quality of life is affected by the presence and severity of neurological deficits and complications.
- Brain tumors are abnormal growths of cells in the brain or surrounding tissues. Metastatic brain tumors are brain tumors that result from cancer cells that spread from another part of the body to the brain
- Brain tumors and metastatic brain tumors can cause symptoms by increasing ICP, causing cerebral edema, hemorrhage, or hydrocephalus, or by affecting specific functions of the affected regions of the brain
- The diagnosis of brain tumors and metastatic brain tumors is based on a combination of clinical history, physical examination, neurological examination, imaging studies, laboratory tests, and biopsy
- The treatment of brain tumors and metastatic brain tumors depends on several factors, such as the type, grade, size, location, number, and symptoms of the tumor; the patient’s age, general health, preferences, and goals; and the availability and effectiveness of the treatment modalities. The main treatment options are surgery, radiation therapy, chemotherapy, immunotherapy, targeted therapy, and palliative care
- Brain tumors and metastatic brain tumors can cause various complications that can affect the patient’s survival and quality of life. The prognosis of brain tumors and metastatic brain tumors is usually poor
- TBI and concussion are caused by an external force that damages the brain tissue and triggers molecular and cellular events that impair neuronal and glial function and synaptic and neurotransmitter function and affect different brain regions and networks.
- TBI and concussion can be classified into mild, moderate, or severe based on the GCS score and can cause various signs and symptoms such as headache, dizziness, nausea, vomiting, fatigue, blurred vision, ringing in the ears, confusion, amnesia, disorientation, difficulty concentrating or remembering information, slurred speech, delayed reaction time, irritability, mood changes, anxiety, depression, insomnia, sensitivity to light or noise, and balance problems.
- TBI and concussion can have persistent or delayed symptoms such as PCS or CTE that affect physical, cognitive, emotional, and behavioral functioning and impair quality of life.
- TBI and concussion can be diagnosed and evaluated by using neurological examination, GCS, SCAT, neuropsychological tests, blood tests, EEG, EPs, CT scan, MRI scan, DTI scan, fMRI scan, or PET scan that have different advantages and limitations.
- TBI and concussion can be treated and prevented by using pharmacological interventions such as analgesics, antiemetics, anticonvulsants, osmotic agents, antibiotics, corticosteroids, antidepressants, anxiolytics, hypnotics, or cognitive enhancers or non-pharmacological interventions such as physical therapy, occupational therapy, speech therapy, CBT, biofeedback, neurofeedback, TMS, tDCS, or acupuncture that have different indications, contraindications, side effects, and nursing implications.
- Nurses provide screening, assessment, management, education, and support for patients with TBI or concussion and their families.
- Ischemic stroke is a condition that occurs when the blood flow to a part of the brain is interrupted, resulting in tissue hypoxia, ischemia, and infarction
- Ischemic stroke can be classified into thrombotic or embolic types, depending on the origin of the clot
- Ischemic stroke can also be classified according to the location and size of the affected brain region
- Ischemic stroke is associated with several modifiable and non-modifiable risk factors, with atherosclerosis being the main cause
- Ischemic stroke involves a complex cascade of cellular and molecular events that lead to neuronal injury and death
- Ischemic stroke causes sudden onset of focal neurological deficits, such as weakness, numbness, visual loss, aphasia, dysarthria, dysphagia, ataxia, and vertigo
- Ischemic stroke is diagnosed by clinical history, physical examination, and neuroimaging studies, such as CT scan or MRI
- Ischemic stroke can lead to several complications, such as hemorrhagic transformation, cerebral edema, vasospasm, seizures, hydrocephalus, infections, dysphagia, aspiration pneumonia, malnutrition, pressure ulcers, DVT, PE, depression, or anxiety
- Ischemic stroke is treated by restoring blood flow to the ischemic brain tissue using thrombolytic therapy or mechanical thrombectomy, preventing further ischemia or hemorrhage using anticoagulant therapy or antiplatelet therapy, reducing complications using neuroprotective therapy or surgical intervention, and improving functional recovery using rehabilitation
- Nursing care for patients with ischemic stroke involves providing holistic and evidence-based care that follows the nursing process of assessment, diagnosis, planning, implementation, and evaluation
- Peripheral neuropathy is any disorder, disease, or damage that affects the peripheral nervous system.
- Peripheral neuropathy can affect sensory, motor, or autonomic nerves in a single, multiple, or diffuse pattern.
- Peripheral neuropathy can be caused by diabetes, trauma, infection, autoimmune diseases, toxins, metabolic disorders, nutritional deficiencies, inherited conditions, or unknown factors.
- Peripheral neuropathy can cause numbness, tingling, burning, pain, weakness, cramps, spasms, paralysis, orthostatic hypotension, tachycardia, constipation, diarrhea, urinary retention or incontinence, erectile dysfunction, or abnormal sweating.
- Peripheral neuropathy can be diagnosed by history and physical examination, nerve conduction studies, electromyography, blood tests, or nerve biopsy.
- Peripheral neuropathy can be treated by pharmacological and non-pharmacological methods to relieve pain, physical and occupational therapy to improve function and mobility, cognitive-behavioral therapy to cope with pain and stress, alternative therapies to enhance well-being and healing, and preventive measures to avoid complications and injuries.
- Radiculopathy is a clinical term for a pinched or compressed nerve root in the spine that causes pain, weakness, numbness, tingling, or difficulty controlling specific muscles along the course of the nerve.
- Radiculopathy can be caused by various conditions that affect the spinal column, such as herniated disc, spinal stenosis, spondylolisthesis, spondylosis, spinal tumor, spinal infection, or spinal trauma.
- Radiculopathy can occur at any level of the spine, but it is more common in the cervical (neck) and lumbar (lower back) regions. The symptoms depend on the level and location of the affected nerve root.
- Radiculopathy can be diagnosed by a combination of history, physical examination, and diagnostic tests such as imaging studies, EMG/NCS, or SNRB.
- Radiculopathy can be treated by conservative management, interventional procedures, or surgery. The treatment options depend on the cause, severity, duration, and location of the nerve root compression or irritation.
- Radiculopathy can have various outcomes and potential complications depending on the type and effectiveness of the treatment. The outcomes may range from complete recovery to no recovery. The complications may include infection, bleeding, hematoma, nerve injury, spinal cord injury, spinal instability, failed back surgery syndrome, chronic pain, disability, or death.
- Radiculopathy requires nursing interventions such as pain management, neurological assessment, functional assessment, physical therapy, patient education, and emotional support.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Pathophysiology of the Nervous System
This filled cannot be empty

