Please set your exam date
Skin integrity and Basic wound care and dressing changes
Study Questions
Introduction to Skin Integrity and Basic Wound Care
A nurse is assessing a client with a pressure ulcer on the sacrum. Which of the following factors would increase the risk of infection in the wound?
Explanation
Answer: A.
The presence of necrotic tissue increases the risk of infection by providing a medium for bacterial growth and impairing wound healing. Necrotic tissue should be debrided to promote wound healing.
B. The use of hydrocolloid dressing is not a risk factor for infection. Hydrocolloid dressings are occlusive and adhesive, which create a moist environment that facilitates wound healing and prevents bacterial contamination.
C. The frequency of wound irrigation is not a risk factor for infection. Wound irrigation is done to cleanse the wound and remove debris and exudate. It should be done gently and with sterile solution to avoid trauma and contamination.
D. The application of topical antibiotics is not a risk factor for infection. Topical antibiotics are used to treat or prevent infection in some wounds. They should be used with caution and as prescribed, as overuse may lead to resistance or allergic reactions.
A client is admitted with a burn injury that involves the epidermis and part of the dermis. The nurse knows that this type of burn is classified as:
Explanation
Answer: B
Partial-thickness burn is a burn that involves the epidermis and part of the dermis. It causes blisters, pain, and redness. It may heal spontaneously or require skin grafting depending on the depth and extent of the injury.
A. Superficial burn is a burn that involves only the epidermis. It causes erythema, mild pain, and no blisters. It heals within a few days without scarring.
C. Full-thickness burn is a burn that involves the epidermis, dermis, and underlying tissues such as fat, muscle, or bone. It causes charred, white, or black skin, no pain, and loss of sensation. It requires skin grafting and may result in scarring and contractures.
D. Deep partial-thickness burn is a burn that involves the epidermis and most of the dermis. It causes white or red skin, severe pain, and decreased sensation. It may heal slowly or require skin grafting.
A nurse is caring for a client who has a surgical incision with sutures. The nurse observes that the edges of the wound are well approximated and there is minimal drainage from the site. The nurse documents this type of wound healing as:
Explanation
Answer: A
Primary intention is a type of wound healing that occurs when the edges of the wound are well approximated and there is minimal tissue loss or infection. It results in minimal scarring and fast healing.
B. Secondary intention is a type of wound healing that occurs when the edges of the wound are not approximated or there is extensive tissue loss or infection. It results in granulation tissue formation, contraction, and epithelialization. It takes longer to heal and may result in scarring and infection.
C. Tertiary intention is a type of wound healing that occurs when there is a delay in closing the wound or when the wound is intentionally left open for drainage or debridement. It results in less scarring than secondary intention but more than primary intention.
D. Quaternary intention is not a valid term for wound healing.
A client has a wound on the lower leg that is covered with dry, yellow crusts. The nurse recognizes this as an indication of:
Explanation
Answer: A.
Slough is dead tissue that is shed from the surface of the wound. It may be white, yellow, green, or brown in color and may have a soft, moist, or dry texture. It should be removed to promote wound healing.
B. Eschar is dead tissue that adheres to the surface of the wound. It may be black, brown, or tan in color and may have a hard, dry, or leathery texture. It may act as a natural barrier to infection in some cases, but it may also impair wound healing and circulation in others.
C. Granulation tissue is new tissue that forms in the base of the wound during healing. It is red or pink in color and has a shiny, moist, granular appearance. It indicates healthy wound healing and should be protected from trauma or infection.
D. Epithelial tissue is new tissue that forms over the granulation tissue during healing. It is pink or pale in color and has a thin, smooth, translucent appearance. It indicates the final stage of wound healing and should be moisturized and protected from sun exposure.
A nurse is applying a dressing to a wound that has moderate to heavy exudate. Which of the following types of dressing would be most appropriate for this wound?
Explanation
Answer: D
Alginate dressing is a type of dressing that is made from seaweed fibers and is highly absorbent. It is suitable for wounds that have moderate to heavy exudate, as it can absorb up to 20 times its weight in fluid. It also forms a gel-like substance when in contact with wound fluid, which creates a moist environment that facilitates wound healing and autolytic debridement.
C. Foam dressing is a type of dressing that is made from polyurethane or silicone and is moderately absorbent. It is suitable for wounds that have light to moderate exudate, as it can absorb up to four times its weight in fluid. It also provides cushioning and insulation for the wound, and prevents bacterial contamination.
B. Hydrogel dressing is a type of dressing that is made from water or glycerin and is minimally absorbent. It is suitable for wounds that have minimal exudate, as it can only absorb up to 10% of its weight in fluid. It also provides hydration and cooling for the wound, and promotes autolytic debridement and granulation tissue formation.
A. Transparent film dressing is a type of dressing that is made from polyurethane and is non-absorbent. It is suitable for wounds that have no exudate, as it does not absorb any fluid. It also provides protection and visualization for the wound, and allows gas exchange and moisture vapor transmission.
A nurse is evaluating the effectiveness of negative pressure wound therapy (NPWT) on a client with a chronic wound. Which of the following outcomes would indicate that the therapy is successful?
Explanation
Answer: B
The wound has decreased in drainage is an outcome that would indicate that NPWT is successful. NPWT is a type of therapy that uses a vacuum device to apply negative pressure to the wound, which removes excess fluid, debris, and infectious material from the wound bed. This reduces edema, inflammation, and bacterial load, and promotes blood flow, oxygenation, and granulation tissue formation.
A. The wound has increased in size is an outcome that would indicate that NPWT is unsuccessful or harmful. NPWT should not cause wound enlargement, as this may indicate tissue damage, infection, or poor healing.
C. The wound has increased in pain is an outcome that would indicate that NPWT is unsuccessful or harmful. NPWT should not cause excessive pain, as this may indicate tissue damage, infection, or poor healing.
D. The wound has decreased in granulation tissue is an outcome that would indicate that NPWT is unsuccessful or harmful. NPWT should promote granulation tissue formation, as this indicates healthy wound healing.
A client has a venous ulcer on the lower leg that is treated with compression therapy. The nurse instructs the client to elevate the leg above the level of the heart whenever possible. What is the rationale for this instruction?
Explanation
Answer: A
To reduce edema and venous pressure is the rationale for elevating the leg above the level of the heart whenever possible. Venous ulcers are caused by chronic venous insufficiency, which impairs venous return and causes blood pooling, increased venous pressure, and edema in the lower extremities. Elevation helps to facilitate venous return and reduce edema and venous pressure, which improves wound healing.
B. To increase arterial blood flow and oxygenation is not the rationale for elevating the leg above the level of the heart whenever possible. Arterial ulcers are caused by arterial insufficiency, which impairs arterial blood flow and oxygenation to the lower extremities. Elevation may worsen arterial blood flow and oxygenation, as it reduces the effect of gravity on arterial perfusion.
C. To prevent infection and inflammation is not the rationale for elevating the leg above the level of the heart whenever possible. Infection and inflammation are complications of venous ulcers, but they are not directly affected by elevation. Infection and inflammation are prevented by proper wound care, such as cleansing, dressing, debridement, and antibiotic therapy.
D. To stimulate nerve regeneration and sensation doesn’t help with venous ulcers.
client with a burn wound on the chest has a silver sulfadiazine (Silvadene) cream applied to the wound. Which adverse reaction should the nurse monitor for in this client?
Explanation
Correct answer: D) A and B.
Rationale: Silver sulfadiazine (Silvadene) is a topical antimicrobial agent used to prevent or treat infection in burn wounds. The nurse should monitor for hypersensitivity or allergic reaction, such as rash, itching, swelling, or difficulty breathing; and leukopenia or decreased white blood cell count, which can increase the risk of infection. The nurse should obtain a baseline complete blood count (CBC) before applying the cream and repeat it every few days during treatment.
Incorrect option:
C) Hyperglycemia or increased blood glucose level. - This is not a common adverse reaction of silver sulfadiazine (Silvadene). However, the client with a burn wound may have hyperglycemia due to stress, inflammation, or infection. The nurse should monitor the blood glucose level regularly and administer insulin as prescribed.
A client with a surgical wound on the abdomen has a negative pressure wound therapy (NPWT) device attached to the wound. Which action should the nurse take when caring for this client?
Explanation
Correct answer: C) Ensure that the dressing is sealed and airtight around the wound.
Rationale: Negative pressure wound therapy (NPWT) is a device that applies
subatmospheric pressure to the wound bed, which promotes granulation tissue formation, removes excess fluid and debris, and reduces edema and bacterial colonization. The nurse should ensure that the dressing is sealed and airtight around the wound to maintain negative pressure and prevent air leaks.
Incorrect options:
A) Change the dressing every 12 hours or as needed. - This is not recommended for NPWT, as frequent dressing changes can disrupt wound healing and increase the risk of infection. The nurse should change the dressing every 48 to 72 hours or as prescribed by the provider.
B) Irrigate the wound with normal saline before applying the dressing. - This is not recommended for NPWT, as irrigation can introduce bacteria into the wound and interfere with negative pressure. The nurse should clean the wound with normal saline or sterile water and pat it dry gently before applying the dressing.
D) Clamp the tubing when ambulating or repositioning the client. - This is not recommended for NPWT, as clamping can interrupt negative pressure and cause tissue damage. The nurse should secure the tubing to prevent kinking or dislodgment and keep the device below the level of the wound when ambulating or repositioning the client.
Assessment of Skin Integrity and Wound Characteristics
A nurse is assessing a client with a pressure ulcer on the sacrum. Which finding indicates a potential complication of the wound?
Explanation
Correct answer: C) Foul odor from the wound
Rationale: Foul odor from the wound may indicate an infection or necrotic tissue, which can impair wound healing and increase the risk of sepsis. The nurse should notify the provider and obtain a wound culture if indicated.
Incorrect options:
A) Serous drainage from the wound - This is a normal finding, as serous drainage is clear and watery and indicates fluid leakage from damaged capillaries.
B) Erythema around the wound edges - This is a normal finding, as erythema (redness) around the wound edges indicates inflammation and increased blood flow to the area, which are part of the normal healing process.
D) Granulation tissue in the wound bed - This is a normal finding, as granulation tissue is pink or red and indicates new tissue growth and blood vessel formation in the wound.
A client is admitted to the hospital with a burn injury covering 30% of the body surface area. The nurse anticipates that the client will require which type of dressing for wound care?
Explanation
Correct answer: D) Silver dressing
Rationale: Silver dressing is a type of antimicrobial dressing that contains silver ions, which have bactericidal properties and can prevent or treat wound infections. Silver dressing can also reduce pain, inflammation, and odor from the wound. Silver dressing is often used for burn injuries, as they are at high risk of infection due to loss of skin integrity and exposure to pathogens.
Incorrect options:
A) Hydrocolloid dressing - This is a type of occlusive dressing that forms a gel-like substance when in contact with wound exudate. Hydrocolloid dressing can promote moist wound healing, reduce pain, and protect the wound from contamination. However, it is not suitable for infected wounds or wounds with heavy drainage, as it can trap bacteria and fluid in the wound and cause maceration of the surrounding skin.
B) Hydrogel dressing - This is a type of dressing that contains water or glycerin and provides moisture to dry wounds. Hydrogel dressing can hydrate necrotic tissue, reduce pain, and facilitate autolytic debridement. However, it is not suitable for wounds with heavy drainage, as it can increase fluid loss and cause maceration of the surrounding skin.
C) Alginate dressing - This is a type of dressing that contains seaweed fibers and forms a gel-like substance when in contact with wound exudate. Alginate dressing can absorb large amounts of fluid, fill dead space in the wound, and facilitate hemostasis. However, it is not suitable for dry wounds or wounds with minimal drainage, as it can dehydrate the wound and cause trauma to granulation tissue when removed.
A nurse is evaluating a client's response to negative pressure wound therapy (NPWT). Which outcome indicates that the therapy is effective?
Explanation
Correct answer: A) Decreased edema in the wound area
Rationale: Decreased edema in the wound area indicates that NPWT is effective, as NPWT applies negative pressure (suction) to the wound, which removes excess fluid, reduces swelling, and improves blood circulation to the area.
Incorrect options:
B) Increased drainage from the wound - This indicates that NPWT is ineffective, as NPWT should reduce drainage from the wound by removing excess fluid and promoting wound closure.
C) Decreased granulation tissue in the wound bed - This indicates that NPWT is ineffective, as NPWT should increase granulation tissue in the wound bed by stimulating cell proliferation and angiogenesis.
D) Increased eschar formation on the wound surface - This indicates that NPWT is ineffective, as NPWT should decrease eschar formation on the wound surface by facilitating debridement and removing necrotic tissue.
Principles of Basic Wound Care
A nurse is assessing a client with a pressure ulcer on the sacrum. Which finding indicates a potential complication of the wound?
Explanation
Correct answer: C) Foul-smelling greenish discharge from the wound
Rationale: Foul-smelling greenish discharge from the wound indicates a possible infection, which can delay wound healing and increase the risk of sepsis. The nurse should notify the provider and obtain a wound culture to identify the causative organism and guide antibiotic therapy.
Incorrect options:
A) Serous drainage from the wound - This is a normal finding, as serous drainage is clear and watery and indicates a healthy inflammatory response.
B) Redness and warmth around the wound - This is a normal finding, as redness and warmth indicate increased blood flow to the wound site, which facilitates healing.
D) Granulation tissue forming in the wound bed - This is a positive finding, as granulation tissue is new connective tissue that fills the wound and supports epithelialization.
A client with diabetes mellitus has a diabetic foot ulcer on the left heel. The nurse is preparing to apply a hydrocolloid dressing to the wound. What is an advantage of using this type of dressing?
Explanation
Correct answer: D) It stimulates autolytic debridement of necrotic tissue in the wound.
Rationale: Hydrocolloid dressings are occlusive or semi-occlusive dressings that adhere to the skin and form a gel-like substance over the wound. This creates a moist environment that stimulates autolytic debridement, which is the natural breakdown of necrotic tissue by enzymes in the wound fluid.
Incorrect options:
A) It provides a moist environment for wound healing. - This is true, but not specific to hydrocolloid dressings, as other types of dressings, such as hydrogels and alginates, also provide a moist environment for wound healing.
B) It absorbs large amounts of exudate from the wound. - This is false, as hydrocolloid dressings are not suitable for wounds with heavy exudate, as they can become saturated and leak. Alginates or foams are more appropriate for wounds with large amounts of drainage.
C) It allows frequent inspection of the wound without removal. - This is false, as hydrocolloid dressings are opaque and do not allow visualization of the wound. They should be left in place for several days, unless there are signs of infection or leakage.
A nurse is caring for a client who has undergone a skin graft to cover a burn injury on the right arm. Which intervention should the nurse include in the plan of care to promote graft adherence?
Explanation
Correct answer: C) Immobilize the right arm with a splint or sling
Rationale: Immobilizing the right arm with a splint or sling helps to prevent movement and shear forces that can dislodge or damage the graft. The nurse should also avoid applying pressure or friction to the graft site.
Incorrect options:
A) Elevate the right arm above the level of the heart - This is not necessary for graft adherence, but it may help to reduce edema and pain in the affected arm.
B) Apply negative pressure wound therapy to the graft site - This is contraindicated for skin grafts, as it can cause bleeding, infection, or graft loss. Negative pressure wound therapy is used for wounds that are difficult to heal by primary intention, such as chronic ulcers or open abdominal wounds.
D) Irrigate the graft site with normal saline twice daily - This is not recommended for skin grafts, as it can interfere with graft adherence and increase the risk of infection. The nurse should follow the provider's orders for dressing changes and use sterile technique.
A client has an arterial ulcer on the left lower leg. The nurse observes that the ulcer has a pale pink base, minimal drainage, and no signs of infection. What is an appropriate dressing for this ulcer?
Explanation
Correct answer: D) Hydrogel dressing
Rationale: Hydrogel dressings are water-based or glycerin-based gels that hydrate the wound and provide a moist environment for healing. They are suitable for dry wounds, such as arterial ulcers, as they help to rehydrate the wound bed and facilitate autolytic debridement.
Incorrect options:
A) Transparent film dressing - This is not an appropriate dressing for arterial ulcers, as it does not provide moisture or cushioning to the wound. Transparent film dressings are used for superficial wounds, such as abrasions or stage I pressure ulcers, or as a secondary dressing to cover other dressings.
B) Calcium alginate dressing - This is not an appropriate dressing for arterial ulcers, as it is designed for wounds with moderate to heavy exudate, such as venous ulcers or infected wounds. Calcium alginate dressings are highly absorbent and form a gel-like substance when in contact with wound fluid.
C) Silver-impregnated dressing - This is not an appropriate dressing for arterial ulcers, unless there is evidence of infection. Silver-impregnated dressings have antimicrobial properties and are used for wounds that are infected or at high risk of infection, such as diabetic foot ulcers or surgical wounds.
Wound Care Techniques and Interventions
A nurse is caring for a client who has a pressure ulcer on the sacrum. Which intervention should the nurse perform first?
Explanation
Correct answer: D) Reposition the client to relieve pressure on the wound.
Rationale: The nurse should follow the ABCDE priority-setting framework when caring for a client with a pressure ulcer. The first priority is to address airway, breathing, and circulation (ABC) issues, which include relieving pressure on the wound to prevent further tissue damage and promote blood flow to the area. The other interventions are also important, but they are not the first priority.
Incorrect options:
A) Apply a hydrocolloid dressing to the wound. - This is an appropriate intervention, as hydrocolloid dressings provide a moist environment that promotes wound healing and prevents bacterial contamination. However, this is not the first priority, as it does not address ABC issues.
B) Assess the wound for signs of infection. - This is an appropriate intervention, as assessing the wound for signs of infection, such as redness, swelling, warmth, drainage, odor, or increased pain, is essential to monitor the wound healing process and identify any complications. However, this is not the first priority, as it does not address ABC issues.
C) Cleanse the wound with normal saline solution. - This is an appropriate intervention, as cleansing the wound with normal saline solution helps to remove debris and bacteria from the wound and prevent infection. However, this is not the first priority, as it does not address ABC issues.
A client is admitted to the hospital with a diabetic foot ulcer. The nurse notes that the wound has a black, dry, and hard eschar covering most of its surface. Which action should the nurse take?
Explanation
Correct answer: D) Consult with the provider about surgical debridement.
Rationale: The nurse should consult with the provider about surgical debridement for a wound that has a black, dry, and hard eschar covering most of its surface. This type of eschar indicates necrotic tissue that impairs wound healing and increases the risk of infection. Surgical debridement is the most effective method of removing large amounts of necrotic tissue from a wound.
Incorrect options:
A) Debride the wound using wet-to-dry dressings. - This is not an appropriate intervention, as wet-to-dry dressings are not recommended for wounds with dry eschar, as they can cause trauma and bleeding to healthy tissue. Wet-to-dry dressings are used for wounds with moist necrotic tissue or slough that needs to be removed.
B) Cover the wound with a transparent film dressing. - This is not an appropriate intervention, as transparent film dressings are not indicated for wounds with necrotic tissue or infection. Transparent film dressings are used for wounds with minimal drainage that need protection from external contamination and moisture loss.
C) Leave the wound open to air without any dressing. - This is not an appropriate intervention, as leaving the wound open to air without any dressing can expose it to further trauma and infection. Wounds need to be covered with an appropriate dressing that maintains a moist environment and supports wound healing.
A nurse is preparing to change a dressing on a client's surgical incision. Which type of dressing should the nurse use to promote autolytic debridement of the wound?
Explanation
Correct answer: D) Hydrogel dressing
Rationale: The nurse should use a hydrogel dressing to promote autolytic debridement of the wound. Autolytic debridement is a natural process that uses the body's own enzymes and moisture to liquefy and remove necrotic tissue from a wound. Hydrogel dressings provide hydration and moisture to dry wounds and facilitate autolytic debridement.
Incorrect options:
A) Alginate dressing - This is not an appropriate dressing for autolytic debridement, as alginate dressings are used for wounds with moderate to heavy exudate that need absorption and hemostasis. Alginate dressings form a gel-like substance when in contact with wound fluid and help to maintain a moist environment for wound healing.
B) Foam dressing - This is not an appropriate dressing for autolytic debridement, as foam dressings are used for wounds with moderate to heavy exudate that need insulation and protection. Foam dressings have a soft and absorbent layer that cushions the wound and prevents maceration of the surrounding skin.
C) Gauze dressing - This is not an appropriate dressing for autolytic debridement, as gauze dressings are used for wounds with minimal to moderate exudate that need cleansing and packing. Gauze dressings can adhere to the wound surface and cause trauma and bleeding when removed.
A client is receiving negative pressure wound therapy (NPWT) for a chronic wound on the lower leg. The nurse observes that the wound edges are approximated and granulation tissue is filling the wound bed. Which action should the nurse take?
Explanation
Correct answer: C) Discontinue the NPWT and apply a moist dressing.
Rationale: The nurse should discontinue the NPWT and apply a moist dressing when the wound edges are approximated and granulation tissue is filling the wound bed. This indicates that the wound is healing well and does not need further NPWT. NPWT is a type of advanced wound therapy that uses a vacuum device to apply negative pressure to a wound, which helps to remove excess fluid, reduce edema, increase blood flow, and stimulate granulation tissue formation. NPWT should be discontinued when the wound has achieved sufficient granulation tissue or epithelialization, or when there are signs of infection or bleeding.
Incorrect options:
A) Increase the frequency of dressing changes. - This is not an appropriate action, as increasing the frequency of dressing changes can disrupt the wound healing process and cause trauma and pain to the client. Dressing changes for NPWT are usually done every 48 to 72 hours, depending on the type of dressing and the amount of drainage.
B) Decrease the amount of negative pressure applied. - This is not an appropriate action, as decreasing the amount of negative pressure applied can reduce the effectiveness of NPWT and delay wound healing. The amount of negative pressure applied should be determined by the provider based on the type and location of the wound, the amount of drainage, and the client's tolerance.
D) Continue the NPWT until the wound is completely closed. - This is not an appropriate action, as continuing the NPWT until the wound is completely closed can cause overgranulation or maceration of the wound and surrounding skin. NPWT should be discontinued when the wound has achieved sufficient granulation tissue or epithelialization, or when there are signs of infection or bleeding.
Documentation and Evaluation of Wound Care
A nurse is assessing a client who has a pressure ulcer on the sacrum. Which finding should the nurse report to the wound care specialist?
Explanation
Correct answer: B) The wound has a yellowish-green drainage.
Rationale: The wound has a yellowish-green drainage, which indicates infection and possible necrosis of the wound tissue. This finding should be reported to the wound care specialist for further evaluation and treatment.
Incorrect options:
A) The wound has a foul odor. - This is not a reportable finding, as foul odor may be present in some wounds without infection, especially if the wound is colonized by anaerobic bacteria. However, the nurse should monitor the wound for other signs of infection, such as increased pain, redness, swelling, or fever.
C) The wound has a granulation tissue in the base. - This is not a reportable finding, as granulation tissue is a sign of healing and indicates that new blood vessels and connective tissue are forming in the wound bed.
D) The wound has a partial-thickness skin loss. - This is not a reportable finding, as partial-thickness skin loss is consistent with the definition of a pressure ulcer, which is a localized injury to the skin and/or underlying tissue due to pressure or shear.
A client is receiving negative pressure wound therapy (NPWT) for a diabetic foot ulcer. Which action should the nurse take when changing the dressing?
Explanation
Correct answer: A) Apply sterile saline to moisten the foam dressing before removal.
Rationale: The nurse should apply sterile saline to moisten the foam dressing before removal, as this helps to prevent trauma and bleeding from adherent dressing. The nurse should also wear sterile gloves and use aseptic technique when changing the dressing.
Incorrect options:
B) Cut the foam dressing to fit loosely into the wound cavity. - This is an incorrect action, as the foam dressing should be cut to fit snugly into the wound cavity, leaving no gaps or spaces between the foam and the wound edges. This ensures optimal contact and negative pressure distribution within the wound.
C) Secure the transparent film dressing with tape around the edges. - This is an incorrect action, as the transparent film dressing should be secured with an adhesive drape that covers at least 3 cm beyond the edges of the film. This prevents air leaks and maintains negative pressure within the wound.
D) Disconnect the suction tubing from the foam dressing before turning off the device. - This is an incorrect action, as the suction tubing should be disconnected from the device before removing the foam dressing from the wound. This prevents accidental suction of air or fluid into the tubing or device.
A nurse is evaluating a client's progress after receiving hyperbaric oxygen therapy (HBOT) for a chronic venous ulcer. Which outcome indicates that HBOT has been effective?
Explanation
Correct answer: D) The client has increased granulation tissue in the ulcer.
Rationale: The client has increased granulation tissue in
the ulcer, which indicates that HBOT has been effective in enhancing wound healing. HBOT delivers 100% oxygen at high pressure to increase oxygen delivery and diffusion to hypoxic tissues, stimulating angiogenesis, collagen synthesis, and fibroblast proliferation.
Incorrect options:
A) The client reports reduced pain in the affected leg. - This is not an outcome that indicates HBOT effectiveness, as pain reduction may be due to other factors, such as analgesics, compression therapy, or elevation of the leg. Pain is also not a reliable indicator of wound healing, as some wounds may heal without pain or have persistent pain despite healing.
B) The client has increased oxygen saturation in the blood. - This is not an outcome that indicates HBOT effectiveness, as oxygen saturation in the blood reflects systemic oxygenation and does not necessarily correlate with tissue oxygenation. Oxygen saturation may also vary depending on factors such as hemoglobin level, cardiac output, or ventilation-perfusion mismatch.
C) The client has decreased edema in the affected leg. - This is not an outcome that indicates HBOT effectiveness, as edema reduction may be due to other factors, such as compression therapy, diuretics, or elevation of
the leg. Edema is also not a reliable indicator of wound healing, as some wounds may heal with edema or have persistent edema despite healing.
Special Considerations in Wound Care
A nurse is assessing a client with a pressure ulcer on the sacrum. Which finding should the nurse report to the provider immediately?
Explanation
Correct answer: A) The wound has a foul odor and purulent drainage.
Rationale: The wound with a foul odor and purulent drainage indicates an infection, which can delay healing and cause systemic complications, such as sepsis. The nurse should report this finding to the provider immediately and obtain a wound culture and sensitivity test.
Incorrect options:
B) The wound has a black, necrotic tissue in the center. - This indicates eschar, which is dead tissue that needs to be debrided to promote healing. However, this is not an urgent finding and can be addressed by the wound care team.
C) The wound has a red, granulating tissue at the edges. - This indicates healthy tissue formation and healing. This is a positive finding and does not need to be reported.
D) The wound has a yellow, sloughing tissue on the surface. - This indicates fibrin, which is a protein that forms during inflammation and can impede healing. The nurse should remove this tissue by irrigation or debridement, but this is not an urgent finding.
A client with venous insufficiency has a venous stasis ulcer on the lower leg. Which instruction should the nurse give to the client to promote wound healing?
Explanation
Rationale: The client with venous insufficiency has impaired venous return from the lower extremities, which causes edema, inflammation, and skin breakdown. The nurse should instruct the client to apply compression stockings or bandages to improve blood flow and reduce swelling; avoid crossing the legs or wearing tight-fitting clothing that can constrict blood vessels; and keep the leg elevated when sitting or lying down to facilitate venous return.
A client with arterial insufficiency has an arterial ulcer on the dorsum of the foot. Which assessment finding should alert the nurse to a potential complication?
Explanation
Correct answer: D) Gangrene or necrosis of the toes.
Rationale: The client with arterial insufficiency has reduced arterial blood supply to
the lower extremities, which causes ischemia, pain, and tissue damage. Gangrene or necrosis of
the toes indicates severe tissue death that can lead to amputation if not treated promptly. The nurse should report this finding to the provider immediately and monitor for signs of infection or sepsis.
Incorrect options:
A) Absent or diminished pedal pulses. - This is an expected finding in clients with arterial insufficiency, as the blood flow to the lower extremities is compromised. The nurse should document this finding and compare it with the baseline and previous assessments.
B) Cold, pale, or cyanotic skin color. - This is an expected finding in clients with arterial insufficiency, as the skin does not receive adequate oxygen and nutrients from the blood. The nurse should document this finding and monitor for changes in skin temperature and color.
C) Loss of hair growth on the lower leg. - This is an expected finding in clients with arterial insufficiency, as the hair follicles do not receive adequate oxygen and nutrients from the blood. The nurse should document this finding and educate the client about proper foot care.
More Questions on This Topic
A nurse is assessing a client who has a pressure ulcer on the sacrum. Which finding indicates a possible infection of the wound?
Explanation
Correct answer: C) Increased pain and tenderness
Rationale: Increased pain and tenderness of the wound site may indicate an infection, as the inflammatory response is triggered by the presence of microorganisms. The nurse should obtain a wound culture and notify the provider of the suspected infection.
Incorrect options:
A) Serous drainage - This is a normal finding for a healing wound, as serous fluid is clear and watery and contains plasma and white blood cells. It does not indicate an infection unless it is cloudy, foul-smelling, or purulent.
B) Reddened periwound skin - This is a normal finding for a healing wound, as the increased blood flow to the area promotes oxygen and nutrient delivery to the wound site. It does not indicate an infection unless the redness is spreading, warm, or accompanied by other signs of inflammation.
D) Granulation tissue formation - This is a normal finding for a healing wound, as granulation tissue is new connective tissue that fills the wound bed and supports epithelialization. It does not indicate an infection unless it is pale, friable, or necrotic.
A client is admitted to the hospital with a diabetic foot ulcer. The nurse notes that the wound has black, dry, and hard tissue covering most of the wound bed. How should the nurse document this finding?
Explanation
Correct answer: A) Eschar
Rationale: Eschar is dead tissue that is black, dry, and hard and adheres firmly to the wound bed or ulcer edges. It may be stable (dry, adherent, intact without erythema or fluctuance) or unstable (loose, moist, boggy, edematous). Stable eschar on the heels serves as the body's natural cover and should not be removed. Unstable eschar in infected wounds should be debrided to expose viable tissue.
Incorrect options:
B) Slough - This is dead tissue that is yellow, tan, gray, green, or brown and has a moist, stringy, or mucinous appearance. It may be loosely attached or firmly adherent to the wound bed. It should be removed to promote wound healing.
C) Fibrin - This is a protein involved in blood clotting that forms a mesh-like structure to seal the wound and stop bleeding. It may appear as a yellowish-white film on the wound surface. It should not be confused with slough or pus.
D) Exudate - This is fluid that leaks out of blood vessels into the surrounding tissues due to inflammation or injury. It may have different characteristics depending on the type and stage of the wound. It should be managed to maintain a moist but not wet wound environment.
A nurse is planning care for a client who has a surgical incision with staples. Which intervention should the nurse include in the plan to prevent wound dehiscence?
Explanation
Correct answer: B) Instruct the client to splint the incision when coughing
Rationale: Splinting the incision when coughing or sneezing helps to reduce tension and stress on the wound edges and prevent wound dehiscence, which is the partial or total separation of the wound layers. The nurse should also instruct the client to avoid lifting heavy objects or straining during bowel movements.
Incorrect options:
A) Apply steri-strips along the incision line - Steri-strips are thin adhesive strips that are used to approximate wound edges and enhance healing by primary intention. They are not used to prevent wound dehiscence, as they do not provide enough support for the wound closure.
C) Change the dressing every 8 hours using sterile technique - Changing the dressing frequently using sterile technique helps to prevent wound infection but not wound dehiscence. The frequency of dressing changes depends on the type and amount of drainage, the condition of the wound, and the type of dressing used.
D) Irrigate the wound with normal saline twice daily - Irrigating the wound with normal saline helps to cleanse the wound and remove debris but not prevent wound dehiscence. Irrigation should be done gently and carefully to avoid disrupting granulation tissue or causing trauma to the wound.
A client has a stage 3 pressure ulcer on the left trochanter with moderate serosanguineous drainage. The wound is 4 cm in length, 3 cm in width, and 2 cm in depth. The wound bed is 80% granulation tissue and 20% slough. Which type of dressing should the nurse use for this wound?
Explanation
Correct answer: C) Alginate
Rationale: Alginate is a type of dressing that is derived from seaweed and forms a gel-like substance when in contact with wound exudate. It is highly absorbent and can handle moderate to large amounts of drainage. It also provides a moist wound environment and supports autolytic debridement of slough and eschar. It is suitable for wounds with depth, such as stage 3 or 4 pressure ulcers.
Incorrect options:
A) Hydrocolloid - This is a type of dressing that has an adhesive outer layer and an inner layer that forms a gel when in contact with wound fluid. It is occlusive and waterproof and provides a moist wound environment. It is suitable for wounds with minimal to moderate drainage, such as stage 2 pressure ulcers or partial-thickness burns. It is not recommended for wounds with depth, as it may cause maceration of the surrounding skin.
B) Hydrogel - This is a type of dressing that consists of water or glycerin-based gels that are available in sheets, gauze, or impregnated into other types of dressings. It provides moisture to dry wounds and facilitates autolytic debridement. It is suitable for wounds with minimal drainage, such as stage 2 pressure ulcers or partial-thickness burns. It is not recommended for wounds with moderate to large amounts of drainage, as it may cause maceration or leakage.
D) Transparent film - This is a type of dressing that consists of a thin sheet of polyurethane with an adhesive coating that allows the exchange of oxygen and moisture vapor but not bacteria or water. It provides a moist wound environment and facilitates autolytic debridement. It is suitable for wounds with minimal drainage, such as stage 1 pressure ulcers or superficial abrasions. It is not recommended for wounds with depth or moderate to large amounts of drainage, as it may cause maceration or leakage.
A nurse is caring for a client who has a venous leg ulcer on the lower left calf. The nurse notes that the wound has copious amounts of yellow-green purulent drainage with a foul odor. The periwound skin is erythematous, warm, and edematous. The client reports increased pain and fever. What should the nurse do first?
Explanation
Correct answer: B) Obtain a wound culture and sensitivity
Rationale: The nurse should first obtain a wound culture and sensitivity to identify the causative organism and the appropriate antibiotic therapy for the client's wound infection. The nurse should use sterile technique and collect the specimen from the wound bed after cleansing the wound with normal saline.
Incorrect options:
A) Apply compression bandages to the affected leg - Compression therapy is indicated for clients with venous leg ulcers to improve venous return and reduce edema, but it is not the first priority in this case. The nurse should first address the infection before applying compression bandages.
C) Administer prescribed analgesics and antipyretics - Administering analgesics and antipyretics may help to relieve the client's pain and fever, but it does not treat the underlying cause of the infection. The nurse should first obtain a wound culture and sensitivity before administering medications.
D) Elevate the affected leg above the level of the heart - Elevating the affected leg may help to reduce edema and improve blood flow, but it does not address the infection. The nurse should first obtain a wound culture and sensitivity before elevating the leg.
A nurse is caring for a client who has a stage 3 pressure ulcer on the sacrum. Which type of dressing should the nurse use to promote moist wound healing?
Explanation
Correct answer: A) Hydrocolloid
Rationale: Hydrocolloid dressings are occlusive and adhesive, forming a gel-like substance over the wound bed that maintains a moist environment and facilitates autolytic debridement. They are suitable for stage 3 pressure ulcers, as they protect the wound from contamination and reduce pain and trauma during dressing changes.
Incorrect options:
B) Transparent film - This type of dressing is semi-permeable and allows oxygen exchange, but does not absorb exudate or provide cushioning. It is suitable for stage 1 pressure ulcers, as it protects the skin from friction and moisture.
C) Calcium alginate - This type of dressing is highly absorbent and forms a gel-like substance when in contact with wound exudate. It is suitable for stage 4 pressure ulcers with heavy drainage, as it fills the dead space and promotes hemostasis.
D) Gauze - This type of dressing is inexpensive and readily available, but it can adhere to the wound bed and cause pain and bleeding during removal. It is suitable for stage 4 pressure ulcers with minimal drainage, as it provides mechanical debridement.
A client is admitted to the hospital with a burn injury that covers 30% of the total body surface area (TBSA). The client's weight is 70 kg. Using the Parkland formula, how much fluid should the client receive in the first 24 hours after the injury?
Explanation
Correct answer: D) 16,800 mL
Rationale: The Parkland formula is used to calculate the fluid resuscitation for burn clients. It states that the client should receive 4 mL of lactated Ringer's solution per kg of body weight per percentage of TBSA burned in the first 24 hours after the injury. Half of this amount should be given in the first 8 hours, and the remaining half should be given in the next 16 hours. Therefore, for this client, the calculation is as follows:
4 mL x 70 kg x 30% = 8,400 mL in the first 24 hours
8,400 mL / 2 = 4,200 mL in the first 8 hours
8,400 mL - 4,200 mL = 4,200 mL in the next 16 hours
Incorrect options:
A) 2,100 mL - This is half of the amount that should be given in the first 8 hours.
B) 4,200 mL - This is the amount that should be given in the first 8 hours or in the next 16 hours.
C) 8,400 mL - This is half of the amount that should be given in the first 24 hours.
A nurse is preparing to change a wet-to-dry dressing for a client who has a chronic wound on the lower leg. Which action by the nurse demonstrates proper technique?
Explanation
Correct answer: C) Moistening the new dressing with sterile water before wringing it out and applying it to the wound
Rationale: Wet-to-dry dressings are used for mechanical debridement of necrotic tissue from chronic wounds. The new dressing should be moistened with sterile water (not saline, as saline can cause sodium crystals to form on the wound bed and impair healing), wrung out to remove excess moisture (to prevent maceration of surrounding skin), and loosely packed into the wound (to allow contact with necrotic tissue). The old dressing should be removed dry (not soaked, as soaking can rehydrate necrotic tissue and reduce debridement).
Incorrect options:
A) Soaking the old dressing with sterile saline before removing it - This can rehydrate necrotic tissue and reduce debridement.
B) Applying antibiotic ointment to the new dressing before placing it on the wound - This can interfere with debridement and increase the risk of infection and resistance.
D) Covering the new dressing with an occlusive secondary dressing to prevent evaporation - This can create a moist environment that promotes bacterial growth and infection.
A client is scheduled for a skin graft surgery to treat a large wound on the arm. The nurse explains to the client that the graft will be taken from the thigh. What term should the nurse use to describe this type of graft?
Explanation
Correct answer: A) Autograft
Rationale: An autograft is a type of skin graft that uses the client's own skin as the donor site. This is the preferred type of graft, as it has the lowest risk of rejection and infection, and provides the best cosmetic and functional results.
Incorrect options:
B) Allograft - This is a type of skin graft that uses human skin from a cadaver or a living donor as the donor site. This type of graft is used as a temporary measure to cover large wounds until an autograft is available.
C) Xenograft - This is a type of skin graft that uses animal skin, usually from pigs, as the donor site. This type of graft is also used as a temporary measure to protect wounds from infection and fluid loss until an autograft is available.
D) Mesh graft - This is a type of skin graft that involves making small slits in the donor skin to create a mesh-like pattern. This allows the graft to cover a larger area and conform to irregular surfaces. This type of graft can be either an autograft or an allograft.
A nurse is assessing a client who has a wound on the abdomen. The nurse observes that the wound edges are approximated, there is minimal drainage, and granulation tissue is visible. How should the nurse document this wound?
Explanation
Correct answer: C) Primary intention wound
Rationale: A primary intention wound is one that heals by epithelialization, with minimal tissue loss and scarring. The wound edges are approximated (closed), either naturally or by surgical means, and there is minimal drainage and inflammation. Granulation tissue is the new connective tissue that forms on the wound bed, indicating healing.
Incorrect options:
A) Partial-thickness wound - This is a wound that involves damage to the epidermis and part of the dermis, such as an abrasion or a blister. It heals by regeneration, with minimal scarring.
B) Full-thickness wound - This is a wound that involves damage to the epidermis, dermis, and underlying structures, such as a pressure ulcer or a surgical incision. It heals by granulation, contraction, and epithelialization, with significant scarring.
D) Secondary intention wound - This is a wound that heals by granulation, contraction, and epithelialization, with significant tissue loss and scarring. The wound edges are not approximated (open), either due to infection, trauma, or chronicity, and there is copious drainage and inflammation.
Exams on Skin integrity and Basic wound care and dressing changes
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction to Skin Integrity and Basic Wound Care
- Assessment of Skin Integrity and Wound Characteristics
- Principles of Basic Wound Care
- Wound Care Techniques and Interventions
- Documentation and Evaluation of Wound Care
- Special Considerations in Wound Care
- Conclusion
- Summary
- More Questions on This Topic
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define skin integrity and basic wound care
- Identify the types and causes of common wounds
- Describe the assessment and documentation of skin integrity and wound characteristics
- Explain the principles and techniques of basic wound care and dressing changes
- Discuss the special considerations in wound care for different populations and settings
Introduction to Skin Integrity and Basic Wound Care
- Skin integrity is the state of intact and healthy skin that provides a protective barrier against infection and injury
- Basic wound care is the management of acute or chronic wounds that are not complicated by infection, necrosis, or other factors that require advanced interventions
- Basic wound care aims to promote wound healing, prevent infection, reduce pain, and maintain function
Assessment of Skin Integrity and Wound Characteristics
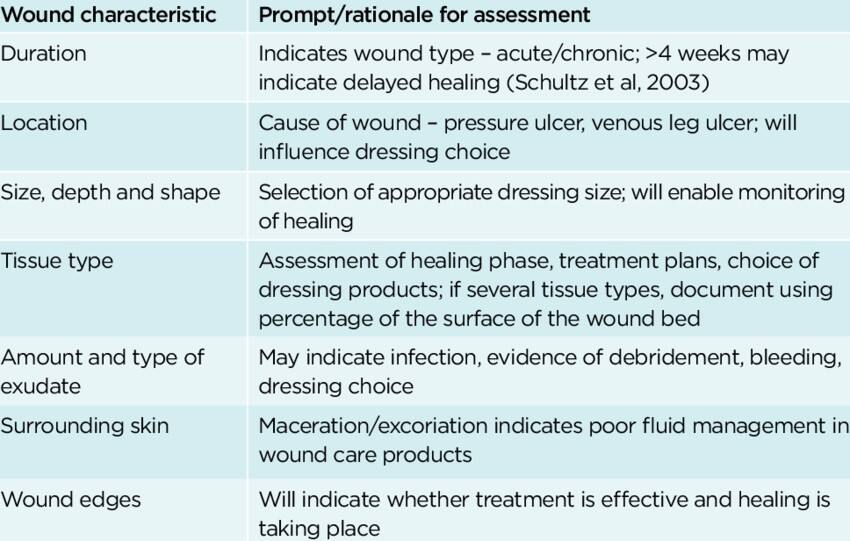
- Assessment of skin integrity and wound characteristics is essential for planning and evaluating wound care interventions
- Assessment of skin integrity includes inspecting the skin for color, temperature, moisture, turgor, texture, lesions, and signs of infection or inflammation
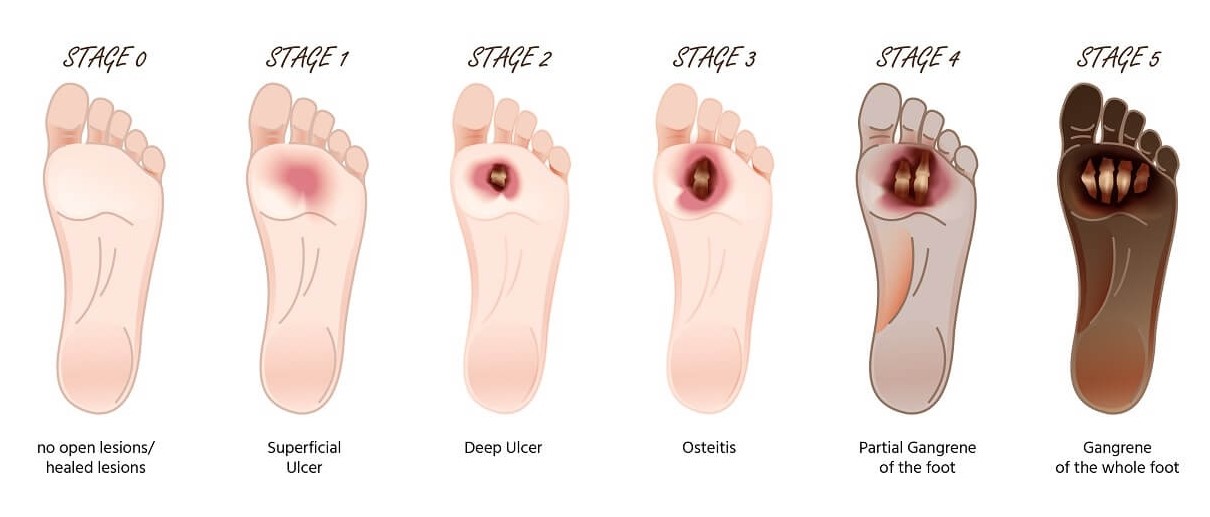
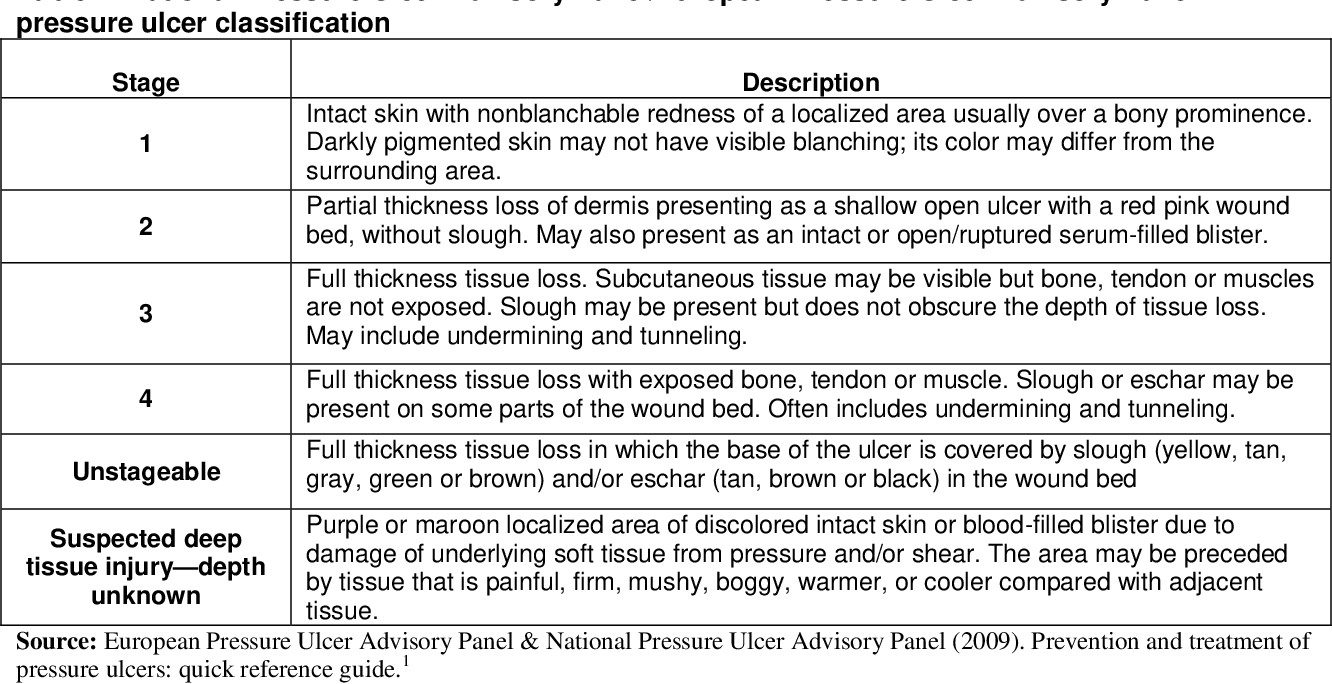
- Assessment of wound characteristics includes measuring the size, depth, shape, location, and stage of the wound; identifying the type and amount of exudate, odor, and necrotic tissue; and evaluating the condition of the wound edges, margins, and surrounding skin.
Principles of Basic Wound Care
- Principles of basic wound care include cleaning, debriding, dressing, and protecting the wound
- Cleaning the wound involves removing debris, bacteria, and dead tissue from the wound bed using sterile saline or water, antiseptic solutions, or wound cleansers
- Debriding the wound involves removing necrotic tissue that may impair healing or increase infection risk using mechanical, enzymatic, autolytic, or surgical methods
- Dressing the wound involves applying an appropriate dressing that maintains a moist wound environment, absorbs excess exudate, prevents infection, protects the wound from trauma, and facilitates healing
- Protecting the wound involves covering the dressing with a secondary dressing or bandage that secures the dressing in place, prevents contamination or leakage, and provides comfort and insulation
Wound Care Techniques and Interventions
- Wound care techniques and interventions vary depending on the type, stage, location, and condition of the wound
- Some common wound care techniques and interventions include irrigation, packing, negative pressure wound therapy (NPWT), hydrotherapy, electrical stimulation, ultrasound therapy, hyperbaric oxygen therapy (HBOT), growth factors, skin substitutes, and biological dressings
- Wound care techniques and interventions should be based on evidencebased practice guidelines and individualized to the patient's needs and preferences
Documentation and Evaluation of Wound Care
- Documentation and evaluation of wound care are vital for monitoring the progress of wound healing, identifying complications or delays in healing, adjusting the plan of care as needed, communicating with other health care providers, and ensuring quality of care
- Documentation of wound care should include the date and time of assessment and intervention; the type, size, shape, location, stage, exudate, odor,
- necrosis, edges/margins/surrounding skin of the wound; the type,
- size/amount/frequency/change/application/removal of dressing; the patient's response to intervention; any problems or complications; any teaching or referrals; and any other relevant information
- Evaluation of wound care should include comparing the current status of the wound with previous assessments; determining if the goals and outcomes are met; identifying any factors that may affect healing; modifying the plan of care as indicated; and documenting the evaluation findings
Special Considerations in Wound Care
- Special considerations in wound care may arise from different factors such as age,comorbidities, medications, nutrition, immunocompetence, lifestyle, psychosocial issues, culture, religion, and health care setting
- Special considerations in wound care may require modifying the assessment, intervention, education, or referral strategies to meet the specific needs and challenges of each patient
- Special considerations in wound care should be addressed in a holistic,
patient-centered, and culturally sensitive manner
Conclusion
- Skin integrity and basic wound care are important aspects of nursing practice that require knowledge, skills, and judgment to provide safe, effective, and quality care to patients with wounds
- Skin integrity and basic wound care involve assessing, planning, implementing, documenting, evaluating, and modifying the plan of care based on evidence-based practice guidelines and individualized patient factors
- Skin integrity and basic wound care also involve considering special populations and settings that may pose unique challenges or opportunities for wound healing
Summary
- In this paper, we discussed the assessment, principles, techniques/interventions, documentation/evaluation, and special considerations in skin integrity and basic wound care.
- Nurses have a crucial role in the management of chronic conditions, maintaining skin integrity and ensuring that clients have access to the best possible services.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Skin integrity and Basic wound care and dressing changes
This filled cannot be empty

