Please set your exam date
Medication Safety and Error Prevention
Study Questions
Introduction
A nurse is preparing to administer medication to a client. Which of the following actions should the nurse take first?
Explanation
The nurse should follow the six rights of medication administration, which include the right client, right medication, right dose, right route, right time, and right documentation. The first action the nurse should take is to compare the medication label with the MAR to ensure that they match and that the medication has been prescribed for the client.
A) This is an important action, but not the first one. The nurse should check the client's identification band after comparing the medication label with the MAR and before administering the medication.
B) This is an important action, but not the first one. The nurse should explain the purpose and side effects of the medication after comparing the medication label with the MAR and before administering the medication.
C) Correct. This is the first action the nurse should take to ensure that the right medication is being given to the right client.
D) This is an important action, but not the first one. The nurse should assess the client for contraindications and allergies after comparing the medication label with the MAR and before administering the medication.
A nurse is reviewing a client's medication list and notices that the client is taking two medications that have a potential interaction. Which of the following actions should the nurse take?
Explanation
The nurse should notify the provider and document the interaction in the client's chart when a potential medication interaction is identified. The provider may need to adjust or change one or both of the medications to prevent if from harming the client.
A) Correct. This is the appropriate action for the nurse to take when a potential medication interaction is identified.
B) This is not an appropriate action. The nurse should not hold or alter any prescribed medications without consulting with the provider first.
C) This is not an appropriate action. The nurse should not administer both medications as prescribed without notifying the provider of the potential interaction. This could put the client at risk for adverse effects or reduced efficacy of one or both of the medications.
D) This is not an appropriate action. The nurse should not rely on the client's self-report of problems with taking both medications. The client may not be aware of or recognize all of the possible signs and symptoms of a medication interaction.
A nurse is teaching a client who has a new prescription for warfarin about safe medication practices. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Warfarin is an anticoagulant that inhibits vitamin K-dependent clotting factors and increases the risk of bleeding. The client should use a soft-bristled toothbrush and an electric razor to prevent trauma and bleeding from minor cuts or abrasions.
A) Correct. This statement indicates that the client understands how to prevent bleeding while taking warfarin.
B) This statement indicates a lack of understanding of the teaching. The client should avoid sudden changes in vitamin K intake, as this can affect the therapeutic level of warfarin and increase the risk of clotting or bleeding. Green leafy vegetables are high in vitamin K and should be consumed in consistent amounts.
C) This statement indicates a lack of understanding of the teaching. The client should avoid nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen while taking warfarin, as they can increase the risk of bleeding. The client should consult with the provider before taking any over-the-counter medications for pain relief.
D) This statement indicates a lack of understanding of the teaching. Warfarin does not affect blood pressure directly but rather affects blood clotting. The client should monitor their international normalized ratio (INR), which measures the effectiveness of warfarin, regularly while taking this medication.
A nurse is administering an intramuscular injection to a client. Which of the following actions should the nurse take to prevent medication errors?
Explanation
The nurse should rotate the injection sites among different muscle groups to prevent tissue damage, irritation, and absorption problems. The nurse should follow the recommended sites for intramuscular injections, such as the deltoid, ventrolateral, vastus lateralis, and dorsogluteal muscles.
A) This is not an action to prevent medication errors, but rather an action to prevent leakage of the medication from the injection site and reduce pain and irritation. The Z-track method involves pulling the skin to one side before inserting the needle and releasing it after withdrawing the needle.
B) This is not an action to prevent medication errors, but rather an action to prevent injecting the medication into a blood vessel. Aspiration involves pulling back on the plunger of the syringe before injecting the medication and checking for blood return in the syringe.
C) This is not an action to prevent medication errors, but rather an action to enhance absorption and reduce pain and irritation. Massage involves applying gentle pressure to the injection site after administering the medication.
D) Correct. This is an action to prevent medication errors by avoiding repeated injections in the same muscle group.
A client is receiving a continuous intravenous infusion of heparin for deep vein thrombosis. The nurse notes that the client's activated partial thromboplastin time (aPTT) is above the therapeutic range. Which of the following actions should the nurse take?
Explanation
Heparin is an anticoagulant that inhibits clotting factors and prevents thrombus formation. The aPTT is a laboratory test that measures the effectiveness of heparin therapy. The therapeutic range for aPTT is usually 1.5 to 2 times the normal value, which is about 25 to 35 seconds. If the aPTT is above the therapeutic range, this indicates that the client is at risk for bleeding and that the heparin dose is too high.
A) This is not an appropriate action. Stopping the infusion abruptly could put the client is at risk for clotting and complications such as pulmonary embolism or stroke The nurse should only stop the infusion if instructed by the provider or if the client has signs of severe bleeding or haemorrhage.
B) Correct. This is an appropriate action. Decreasing the infusion rate will lower the heparin dose and bring the aPTT back to the therapeutic range. The nurse should notify the provider of the aPTT result and obtain further orders for heparin therapy.
C) This is not an appropriate action. Increasing the infusion rate will raise the heparin dose and increase the aPTT further above the therapeutic range. This could worsen the risk of bleeding for the client.
D) This is not an appropriate action. Continuing the infusion without adjusting the rate or notifying the provider could result in harm to the client due to excessive anticoagulation and bleeding.
A client is receiving an intravenous (IV) infusion of potassium chloride. The nurse notices that the infusion site is red, swollen, and painful. The nurse suspects that the client has developed phlebitis. Which of the following actions should the nurse take first?
Explanation
The nurse should stop the infusion and remove the IV catheter as soon as possible if phlebitis is suspected. Phlebitis is inflammation of a vein that can be caused by mechanical, chemical, or infectious factors. Potassium chloride is a vesicant medication that can cause severe tissue damage if it extravasates into the surrounding tissues.
The nurse should apply a warm compress to the infusion site after removing the IV catheter to reduce inflammation and discomfort. The nurse should notify the provider and obtain an order for a different IV site to continue the infusion of potassium chloride at a different location. The nurse should not slow down the infusion rate and monitor the client because this could worsen the condition and increase the risk of complications.
b) Incorrect. This is an appropriate action after removing the IV catheter, but not before.
c) Incorrect. This is an appropriate action after removing the IV catheter and applying a warm compress, but not before.
d) Incorrect. This is not an appropriate action because it could worsen the condition and increase the risk of complications.
A nurse is preparing to administer medication to a client. Which of the following actions should the nurse take to ensure medication safety? (Select all that apply.)
Explanation
The nurse should check the medication label against the MAR three times: before removing the medication from the storage area, before preparing or measuring the medication, and before administering the medication to the client.
The nurse should also ask the client to state their name and date of birth and use a barcode scanner to verify the client's identification band and the medication. These are methods of ensuring that the right medication is given to the right client.
The nurse should follow the six rights of medication administration: right client, right medication, right dose, right route, right time, and right documentation.
The nurse should document the medication administration as soon as possible after giving the medication, not after completing other tasks.
a) Correct. This is one of the methods of ensuring medication safety.
b) Correct. This is another method of ensuring medication safety.
c) Correct. This is a third method of ensuring medication safety.
d) Incorrect. The nurse should document the medication administration as soon as possible after giving the medication, not after completing other tasks.
e) Correct. This is a general principle of medication safety.
Causes and risk factors
A nurse is preparing to administer medication to a client who has a history of medication errors. Which of the following actions should the nurse take to prevent medication errors? (Select all that apply.)
Explanation
A) This is correct as checking the medication label against the MAR three times is one of the six rights of medication administration and helps to ensure accuracy and safety.
B) This is correct as using two client identifiers is another one of the six rights of medication administration and helps to verify the identity of the client.
C) This is correct as asking the client to state their name and date of birth is another way of verifying the identity of the client and can also help to engage them in their care.
D) This is incorrect as documenting the medication administration should be done as soon as possible after giving the medication to avoid errors and omissions.
E) This is correct as following the six rights of medication administration (right client, right medication, right dose, right route, right time, right documentation) is a standard practice that helps to prevent medication errors.
A nurse is reviewing a client's medication list and notices that the client is taking warfarin, a blood thinner. Which of the following factors should the nurse assess as potential risk factors for bleeding? (Select all that apply.)
Explanation
A) This is correct as the INR level measures how long it takes for blood to clot and is used to monitor the effectiveness and safety of warfarin therapy. A high INR level indicates a higher risk of bleeding.
B) This is correct as some herbal supplements, such as garlic, ginger, ginkgo, and ginseng, can interact with warfarin and increase the risk of bleeding.
C) This is incorrect as vitamin K-rich foods, such as green leafy vegetables, can interfere with warfarin and decrease its effectiveness, leading to a lower risk of bleeding. However, clients taking warfarin should maintain a consistent intake of vitamin K-rich foods and avoid sudden changes in their diet.
D) This is correct as peptic ulcer disease is a condition that causes erosion and inflammation of the lining of the stomach or duodenum and can lead to bleeding complications, especially when taking warfarin.
E) This is incorrect as blood pressure does not directly affect the risk of bleeding from warfarin therapy. However, clients taking warfarin should monitor their blood pressure regularly and report any signs of hypertension or hypotension to their provider.
A nurse is administering medication to a client who has dysphagia, or difficulty swallowing. Which of the following strategies should the nurse use to prevent medication errors and ensure safety? (Select all that apply.)
Explanation
B) This is correct as mixing medications with food or liquids that are easy to swallow can help to prevent choking and aspiration and improve compliance. However, some medications may interact with certain foods or liquids, so the nurse should check with the pharmacist before mixing them.
C) This is correct as giving one medication at a time and allowing time for swallowing can help to prevent choking and aspiration and ensure that each medication is taken correctly. The nurse should also monitor the client for signs of difficulty swallowing, such as coughing, gagging, drooling, or regurgitation.
E) This is correct as assessing the client's mouth for pocketing of medications can help to prevent medication errors and ensure that each medication is taken correctly. Pocketing of medications occurs when the client holds medications in their cheeks or under their tongue instead of swallowing them. This can lead to ineffective therapy, toxicity, or adverse effects.
A) This is incorrect as crushing or dissolving tablets and capsules before giving them to the client can alter their effectiveness, absorption, or bioavailability and cause medication errors or adverse effects. Some tablets and capsules are designed to be swallowed whole, such as enteric-coated, extended-release, or sublingual formulations. The nurse should check with the pharmacist before crushing or dissolving any tablets or capsules.
D) This is incorrect as encouraging the client to drink water before and after taking medications can help to prevent choking and aspiration and ensure adequate hydration, but it may not be appropriate for some clients who have dysphagia or who are on fluid restrictions. The nurse should assess the client's ability to drink water safely and follow their individualized plan of care.
A nurse is administering an intramuscular injection to a client who has a latex allergy. Which of the following precautions should the nurse take to prevent an allergic reaction? (Select all that apply.)
Explanation
Checking the medication label for any latex components and asking the client about any previous reactions to latex products are important precautions that can help prevent an allergic reaction. Some medications may contain latex in their packaging or formulation, and some clients may have more severe reactions than others.
A, B, and C are incorrect. Using a latex-free syringe and needle, wearing non-latex gloves, and applying a non-latex bandage are not precautions, but rather standard practices for administering an intramuscular injection to any client.
A nurse is teaching a client who has diabetes mellitus about how to prevent hypoglycemia when taking insulin. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
A) This is correct as eating a snack before exercising can help to prevent hypoglycemia by providing glucose for energy and preventing a sudden drop in blood sugar levels.
B) This is incorrect as skipping a meal can cause hypoglycemia by depriving the body of glucose and creating an imbalance between insulin and glucose levels. Clients taking insulin should eat regular meals and snacks and monitor their blood sugar levels frequently.
C) This is incorrect as increasing the insulin dose without consulting with the provider can cause hypoglycemia by lowering the blood sugar levels too much. Stress can affect blood sugar levels in different ways depending on the type and duration of stress and the individual's response. Clients taking insulin should consult with their provider about how to adjust their insulin dose according to their stress level and blood sugar readings.
D) This is incorrect as drinking alcohol can cause hypoglycemia by inhibiting the liver's production of glucose and increasing the risk of insulin overdose. Clients taking insulin should avoid or limit alcohol intake and never drink alcohol on an empty stomach.
A nurse is caring for a client who is receiving intravenous (IV) fluids. The nurse notices that the IV site is red, swollen, and painful. Which of the following actions should the nurse take first?
Explanation
B) This is correct as discontinuing the IV infusion and removing the catheter is the first action that the nurse should take when suspecting an IV site infection or phlebitis. This helps to prevent further complications and damage to the vein.
A) This is incorrect as applying a warm compress to the IV site can help to reduce inflammation and discomfort, but it is not the first action that the nurse should take. The nurse should apply a warm compress after discontinuing the IV infusion and removing the catheter.
C) This is incorrect as elevating the affected arm above the level of the heart can help to reduce swelling and improve blood flow, but it is not the first action that the nurse should take. The nurse should elevate the affected arm after discontinuing the IV infusion and removing the catheter.
D) This is incorrect as notifying the provider and documenting the findings are important steps in managing an IV site infection or phlebitis, but they are not the first actions that the nurse should take. The nurse should notify the provider and document the findings after discontinuing the IV infusion and removing the catheter.
A nurse is reviewing the medication administration record of a client who is receiving digoxin, a cardiac glycoside. The nurse notes that the client's apical pulse is 58 beats per minute. Which of the following actions should the nurse take?
Explanation
Checking the client's blood pressure and oxygen saturation is an appropriate action for the nurse to take when the client's apical pulse is below 60 beats per minute, which is the lower limit of normal. This is because a low pulse rate can indicate bradycardia, which can affect the client's hemodynamic status and tissue perfusion.
A and B are incorrect. Administering the medication as prescribed or holding the medication and notifying the provider are not appropriate actions for the nurse to take without further assessment of the client's condition. Digoxin can lower the heart rate, but it can also improve cardiac output and contractility in clients with heart failure. Therefore, the nurse should not withhold the medication based on one vital sign measurement alone.
D is incorrect. Repeating the apical pulse measurement after 5 minutes is not an appropriate action for the nurse to take when the client's apical pulse is below 60 beats per minute, as it delays further assessment and intervention.
Signs and symptoms
A nurse is reviewing the medication administration record of a client who has a history of medication errors. Which of the following actions should the nurse take to prevent medication errors? (Select all that apply.)
Explanation
A) This is correct because using two client identifiers, such as name and date of birth, is a standard safety measure to ensure that the right medication is given to the right client.
B) This is correct because checking the expiration date of the medication before administering it is another safety measure to prevent giving expired or ineffective medications to clients.
C) This is correct because comparing the medication label with the prescription three times (before, during, and after preparing the medication) is a recommended practice to prevent errors such as wrong dose, wrong route, or wrong time.
D) This is incorrect because administering the medication as soon as possible after receiving it from the pharmacy may increase the risk of errors due to haste or distraction. The nurse should follow the prescribed schedule and administer the medication within a reasonable time frame.
E) This is incorrect because documenting the medication administration after completing other tasks may lead to forgetting or omitting important information. The nurse should document the medication administration as soon as possible after giving it to the client.
A client who is receiving intravenous vancomycin reports feeling dizzy and flushed. The nurse observes that the client has a macular rash on the face and neck. Which of the following actions should the nurse take first?
Explanation
A) This is correct because stopping the infusion and notifying the provider are the priority actions for a client who is experiencing signs and symptoms of anaphylaxis, which is a life-threatening allergic reaction to a medication. The nurse should also prepare to administer epinephrine as prescribed.
B) This is incorrect because administering diphenhydramine as prescribed is not the first action for a client who is experiencing anaphylaxis. Diphenhydramine is an antihistamine that can help relieve some symptoms of an allergic reaction, but it is not effective for reversing bronchoconstriction or hypotension that may occur in anaphylaxis.
C) This is incorrect because monitoring the client's vital signs and oxygen saturation is not the first action for a client who is experiencing anaphylaxis. Although these are important assessments, they are not as urgent as stopping the infusion and notifying the provider.
D) This is incorrect because slowing down the infusion rate and observing for improvement are not appropriate actions for a client who is experiencing anaphylaxis. Slowing down or continuing the infusion may worsen the client's condition and delay treatment.
A nurse is preparing to administer insulin to a client who has diabetes mellitus. The nurse notices that the insulin vial has a small amount of white precipitate at the bottom. Which of the following actions should the nurse take?
Explanation
A) This is incorrect because discarding the vial and obtaining a new one is not necessary actions for a vial of insulin that has a small amount of white precipitate at the bottom. This precipitate indicates that the insulin has crystallized due to cold storage or temperature changes, but it can be resuspended by gently rolling or rotating the vial.
B) This is incorrect because shaking the vial vigorously until the precipitate dissolves is not an appropriate action for a vial of insulin that has a small amount of white precipitate at the bottom. Shaking the vial may cause air bubbles or froth to form, which can affect the accuracy of the dose measurement and administration.
C) This is incorrect because warming the vial in a microwave oven for a few seconds is not a safe action for a vial of insulin that has a small amount of white precipitate at the bottom. Warming the vial in a microwave oven may cause uneven heating or damage to the insulin molecules, which can alter the potency and effectiveness of the medication.
D) This is correct because rolling the vial gently between the palms of both hands is the recommended action for a vial of insulin that has a small amount of white precipitate at the bottom. Rolling the vial gently helps to resuspend the insulin crystals and restore the uniform appearance of the solution.
A nurse is teaching a client who is prescribed warfarin about the signs and symptoms of bleeding that should be reported to the provider. Which of the following statements by the client indicates an understanding of the teaching? (Select all that apply.)
Explanation
A) This is correct because blood in the urine (hematuria) is a sign of bleeding that should be reported to the provider. Warfarin is an anticoagulant that can increase the risk of bleeding from any site in the body.
B) This is correct because a headache that lasts for more than an hour is a sign of bleeding that should be reported to the provider. Warfarin can increase the risk of bleeding in the brain (intracranial hemorrhage), which can manifest as a severe or persistent headache, confusion, or neurological deficits.
C) This is correct because black, tarry stools (melena) are a sign of bleeding that should be reported to the provider. Warfarin can increase the risk of bleeding in the gastrointestinal tract (GI bleed), which can manifest as dark or bloody stools, abdominal pain, or vomiting blood.
D) This is correct because a sore throat and a fever are signs of bleeding that should be reported to the provider. Warfarin can increase the risk of bleeding in the mucous membranes (mucosal bleeding), which can manifest as sore throat, mouth ulcers, nosebleeds, or gum bleeding. A fever may indicate an infection that can worsen the bleeding tendency.
E) This is incorrect because bruising on the arms and legs (ecchymosis) is not a sign of bleeding that should be reported to the provider. Warfarin can cause minor bruising due to subcutaneous bleeding, which is usually harmless and does not require treatment. However, if the bruising is extensive, painful, or accompanied by other signs of bleeding, then it should be reported to the provider.
A nurse is assessing a client for signs and symptoms of a medication error. Which of the following manifestations should the nurse be most concerned about?
Explanation
Rapid heart rate and palpitations are potential signs of a medication error, particularly if the client is receiving medication that can affect cardiac function. These symptoms can indicate an adverse reaction or an overdose of certain medications, such as those that affect the cardiovascular system. Monitoring the client's cardiac status is crucial in detecting and managing potential medication errors.
Incorrect choices:
a) Mild headache and dizziness: While these symptoms may be bothersome, they are generally not indicative of a medication error unless they persist or worsen.
b) Temporary nausea and vomiting: Nausea and vomiting can occur as side effects of medications, and they may not necessarily indicate a medication error.
d) Transient muscle weakness and fatigue: Although muscle weakness and fatigue can be associated with medication errors, they are less specific and may be caused by various other factors. Rapid heart rate and palpitations are more concerning in this context.
A nurse suspects a medication error in a client who recently started a new medication. Which of the following assessments would support this suspicion?
Explanation
An allergic reaction to a newly administered medication can be a strong indicator of a medication error. It suggests that the client may have received a medication to which they are allergic or that they were given an incorrect dose or formulation of the medication. Allergic reactions require immediate intervention to prevent further harm.
Incorrect choices:
a) The client reports mild constipation: Mild constipation is a non-specific symptom that may or may not be related to a medication error. It can occur for various reasons, including dietary changes or side effects of the medication.
b) The client's blood pressure remains within normal limits: Blood pressure within normal limits does not necessarily indicate or rule out a medication error. It is important to assess for other specific signs and symptoms related to the medication.
d) The client exhibits improved mood and increased energy: Improved mood and increased energy are positive outcomes that may occur with the appropriate use of medication. They do not suggest a medication error unless accompanied by other concerning signs or symptoms.
Diagnosis and treatment
A nurse is caring for a client who has been prescribed warfarin for atrial fibrillation. Which of the following laboratory tests should the nurse monitor to assess the effectiveness of the medication?
Explanation
Prothrombin time (PT) is a measure of how long it takes for blood to clot. Warfarin is an anticoagulant that prolongs the PT and prevents blood clots from forming. The nurse should monitor the PT and adjust the warfarin dose accordingly to maintain a therapeutic range.
Incorrect choices:
b) Activated partial thromboplastin time (aPTT): aPTT is another measure of blood clotting time, but it is used to monitor heparin therapy, not warfarin therapy.
c) Platelet count: Platelet count is a measure of how many platelets are in the blood. Platelets are involved in blood clotting, but they are not affected by warfarin therapy.
d) Hemoglobin level: Hemoglobin level is a measure of how much oxygen-carrying protein is in the blood. Haemoglobin level can be affected by bleeding or anaemia, but it is not directly related to warfarin therapy.
A nurse is teaching a client who has diabetes mellitus about self-monitoring of blood glucose (SMBG). Which of the following statements by the client indicates a need for further teaching?
Explanation
Using the same finger for each blood glucose test can cause pain, infection, and callus formation. The client should rotate the fingers and use different sites for each test.
Incorrect choices:
a) "I should check my blood glucose before meals and at bedtime.": This is correct as it follows the recommended frequency of SMBG for most clients with diabetes mellitus.
c) "I should wash my hands with soap and water before each test.": This is correct as it prevents contamination and ensures the accuracy of the test results.
d) "I should record my blood glucose results in a log book.": This is correct as it helps the client and the health care team to evaluate the effectiveness of the diabetes management plan.
A nurse is reviewing the medication administration record (MAR) of a client who has hypertension. The nurse notices that the client has been prescribed both lisinopril and spironolactone. Which of the following actions should the nurse take?
Explanation
Lisinopril is an angiotensin-converting enzyme (ACE) inhibitor that lowers blood pressure by blocking the conversion of angiotensin I to angiotensin II, which causes vasoconstriction. Spironolactone is a potassium-sparing diuretic that lowers blood pressure by increasing urine output and preventing sodium and water reabsorption.
However, both medications can also increase potassium levels in the blood, which can lead to hyperkalemia, a potentially life-threatening condition. The nurse should hold both medications and notify the provider of this potential drug interaction.
Incorrect choices:
a) Administer both medications as ordered: This is incorrect as it exposes the client to the risk of hyperkalemia.
c) Hold lisinopril and administer spironolactone: This is incorrect as it does not eliminate the risk of hyperkalemia from spironolactone alone.
d) Hold spironolactone and administer lisinopril: This is incorrect as it does not eliminate the risk of hyperkalemia from lisinopril alone.
A nurse is preparing to administer an intramuscular injection to a client who has a latex allergy. Which of the following actions should the nurse take?
Explanation
Using a latex-free syringe and needle is the appropriate action to prevent an allergic reaction in a client who has a latex allergy. The nurse should also check the medication label and vial for any latex content.
Incorrect choices:
b) Apply a latex bandage over the injection site: This is incorrect as it can cause skin irritation and allergic reaction in a client who has a latex allergy.
c) Wear latex gloves during the procedure: This is incorrect as it can expose the client and the nurse to latex particles and cause an allergic reaction.
d) Dilute the medication with normal saline: This is incorrect as it can alter the concentration and effectiveness of the medication.
A nurse is conducting a health history interview with a client who has a family history of breast cancer. Which of the following questions should the nurse ask to assess the client's risk factors for developing breast cancer?
Explanation
Consuming alcohol on a regular basis is a modifiable risk factor for developing breast cancer. The nurse should ask this question to assess the client's current lifestyle habits and provide education on reducing alcohol intake.
Incorrect choices:
a) "Have you ever had a mammogram?": This is incorrect as it does not assess a risk factor for developing breast cancer, but rather a screening method for detecting breast cancer.
b) "Do you perform monthly breast self-examinations?": This is incorrect as it does not assess a risk factor for developing breast cancer, but rather a preventive measure for early detection of breast cancer.
c) "Have you ever used oral contraceptives?": This is incorrect as it does not assess a current risk factor for developing breast cancer, but rather a past exposure that may or may not have an effect on the client's risk.
A nurse is caring for a client who has chronic obstructive pulmonary disease (COPD) and is receiving oxygen therapy via nasal cannula at 2 L/min. The nurse observes that the client's oxygen saturation level is 88%. Which of the following actions should the nurse take?
Explanation
Maintaining the current oxygen flow rate is the appropriate action for the nurse to take. Clients who have COPD have chronically low oxygen saturation levels and high carbon dioxide levels due to impaired gas exchange. Increasing the oxygen flow rate can cause oxygen toxicity and suppress the respiratory drive, leading to respiratory failure. The nurse should aim to keep the oxygen saturation level between 88% and 92% for clients who have COPD.
Incorrect choices:
a) Increase the oxygen flow rate to 4 L/min: This is incorrect as it can cause oxygen toxicity and suppress the respiratory drive, leading to respiratory failure.
b) Encourage the client to cough and deep breathe: This is incorrect as it can increase the work of breathing and cause fatigue and dyspnea in clients who have COPD.
c) Administer bronchodilator medication as prescribed: This is incorrect as it does not address the immediate issue of low oxygen saturation level. Bronchodilator medication can help improve airflow and reduce airway inflammation, but it does not directly increase oxygen delivery.
Nursing interventions and care
A nurse is caring for a client who has been prescribed warfarin for atrial fibrillation. The nurse notices that the client's INR is 6.5. What should the nurse do first?
Explanation
A high INR indicates that the client is at risk of bleeding due to excessive anticoagulation. The nurse should first assess for signs of bleeding, such as bruising, petechiae, hematuria, or melena.
Then, the nurse should notify the provider and follow orders to reverse the anticoagulation effect, such as administering vitamin K or fresh frozen plasma.
Holding the next dose of warfarin may be appropriate, but it is not the priority action.
Incorrect choices:
a) Administer vitamin K: Vitamin K is an antidote for warfarin overdose, but it should not be given without a provider's order. It may also take several hours to reverse the anticoagulation effect.
b) Notify the provider: Notifying the provider is an important step, but it is not the first action. The nurse should assess the client's condition before calling the provider.
c) Hold the next dose of warfarin: Holding the next dose of warfarin may prevent further anticoagulation, but it does not address the current risk of bleeding. The nurse should assess and intervene for bleeding before holding the medication.
A nurse is preparing to administer insulin to a client with diabetes mellitus. The nurse draws up 10 units of regular insulin and 20 units of NPH insulin in the same syringe. Which of the following actions should the nurse take next?
Explanation
When mixing two types of insulin in one syringe, the nurse should follow the mnemonic RN or "regular before NPH". This means that the nurse should first inject air into the NPH vial, then inject air into the regular vial, then withdraw regular insulin from the vial, and finally withdraw NPH insulin from the vial. This order prevents contamination of the regular insulin with NPH insulin and ensures accurate dosing.
Incorrect choices:
a) Inject air into the NPH vial: This is correct, but it is not the next action. The nurse should inject air into the NPH vial before drawing up any insulin.
c) Withdraw NPH insulin from the vial: This is incorrect and can lead to a medication error. The nurse should withdraw NPH insulin after withdrawing regular insulin.
d) Withdraw regular insulin from the vial: This is correct, but it is not the next action. The nurse should inject air into the regular vial before withdrawing regular insulin.
A nurse is reviewing a client's medication administration record (MAR). The nurse notices that a medication that was due at 0900 has not been given. It is now 1030. What should the nurse do first?
Explanation
The first step in managing a missed or delayed medication is to check if another nurse has given or withheld the medication for some reason. This can prevent duplicate or omitted doses and ensure continuity of care. The nurse should also check if there are any contraindications or changes in orders for giving the medication.
Incorrect choices:
b) Give the medication as soon as possible: Giving the medication as soon as possible may be appropriate, but it is not the first action. The nurse should verify if another nurse has given or withheld the medication before administering it.
c) Document why the medication was delayed: Documenting why the medication was delayed is important, but it is not the first action. The nurse should verify if another nurse has given or withheld the medication and give it if indicated before documenting.
d) Report the incident to the charge nurse: Reporting the incident to the charge nurse may be necessary, but it is not the first action. The nurse should verify if another nurse has given or withheld the medication and give it if indicated before reporting.
A nurse is administering medication to a client via a nasogastric (NG) tube. The nurse crushes the medication and mixes it with water. Which of the following actions should the nurse take next?
Explanation
The nurse should check the placement of the tube before administering any medication or fluid via an NG tube. This can prevent aspiration, infection, or injury to the client. The nurse can check the placement by aspirating gastric contents and measuring the pH, or by using a carbon dioxide detector.
Incorrect choices:
a) Flush the tube with 30 mL of water: Flushing the tube with water is correct, but it is not the next action. The nurse should flush the tube before and after administering the medication to prevent clogging and ensure delivery.
c) Clamp the tube for 30 minutes: Clamping the tube for 30 minutes is incorrect and can cause complications. The nurse should not clamp the tube unless ordered by the provider. Clamping the tube can increase the risk of reflux, aspiration, or tube displacement.
d) Elevate the head of the bed: Elevating the head of the bed is correct, but it is not the next action. The nurse should elevate the head of the bed at least 30 degrees before and during the administration of the medication to prevent aspiration and promote gastric emptying.
A nurse is teaching a client who has a new prescription for digoxin. Which of the following instructions should the nurse include in the teaching?
Explanation
All of the instructions are correct and important for a client who is taking digoxin. Digoxin is a cardiac glycoside that can improve the contractility and rhythm of the heart. However, it can also cause serious side effects, such as bradycardia, arrhythmias, or toxicity.
A nurse is caring for a client who has received an overdose of morphine. The nurse has an order to administer naloxone, an opioid antagonist. Which of the following effects should the nurse expect after giving naloxone?
Explanation
Naloxone is a medication that can reverse the effects of opioids, such as morphine. One of the main effects of opioids is respiratory depression, which can be life-threatening. Naloxone can increase the respiratory rate by blocking opioid receptors in the brain and restoring normal breathing.
Incorrect choices:
b) Decreased pain level: Naloxone can decrease pain level by reversing opioid analgesia, but this is not the expected effect. The nurse should monitor for increased pain levels and administer non-opioid analgesics as ordered.
c) Increased sedation: Naloxone can decrease sedation by reversing opioid-induced central nervous system depression, but this is not the expected effect. The nurse should monitor for agitation or withdrawal symptoms and provide comfort measures as needed.
d) Decreased blood pressure: Naloxone can increase blood pressure by reversing opioid-induced hypotension, but this is not the expected effect. The nurse should monitor for hypertension or tachycardia and administer antihypertensives as ordered.
A nurse is reviewing a client's laboratory results and notices that the potassium level is 6.2 mEq/L. The nurse knows that this value indicates hyperkalemia. Which of the following medications should the nurse anticipate to administer?
Explanation
All of the medications are used to treat hyperkalemia, which is a high level of potassium in the blood. Hyperkalemia can cause cardiac arrhythmias, muscle weakness, or paralysis.
Prevention and Education
A nurse is educating a client about the importance of reporting any medication errors that may occur during their hospital stay. Which of the following statements by the client indicates a need for further teaching?
Explanation
This statement shows that the client does not understand the potential consequences of medication errors, even if they seem minor. Minor errors can lead to serious adverse events, such as allergic reactions, drug interactions, or overdoses. The client should be informed that all medication errors should be reported and documented to prevent further harm and improve patient safety.
Incorrect choices:
a) I should tell you if I notice any unusual symptoms after taking my medication: This statement shows that the client understands the importance of monitoring for adverse reactions and communicating with the nurse.
b) I should check the label of the medication before I take it: This statement shows that the client is aware of their role in preventing medication errors by verifying the name, dose, and route of the medication.
d) I should ask questions if I am not sure about the purpose or side effects of the medication: This statement shows that the client is willing to seek clarification and education about their medication regimen.
A nurse is conducting a root cause analysis of a medication error that occurred in their unit. Which of the following steps should the nurse take first?
Explanation
The first step in a root cause analysis is to collect data and facts about what happened, when, where, how, and why. This includes interviewing the staff involved, reviewing medical records, policies, procedures, and protocols, and examining equipment and environmental factors. Gathering information and evidence helps to establish a timeline and a causal chain of events that led to the error.
Incorrect choices:
a) Identify all the factors that contributed to the error: This is a later step in a root cause analysis, after gathering information and evidence. Identifying contributing factors helps to determine the underlying causes and system failures that allowed the error to occur.
b) Implement corrective actions to prevent recurrence of the error: This is another later step in a root cause analysis, after identifying contributing factors. Implementing corrective actions involves developing and testing solutions that address the root causes and improve patient safety.
c) Communicate the findings and recommendations to the staff and stakeholders: This is the final step in a root cause analysis, after implementing corrective actions. Communicating the findings and recommendations involves sharing lessons learned, best practices, and feedback with those who are affected by or involved in preventing similar errors.
A nurse is reviewing a client's medication list during a home visit. The nurse notices that some of the medications have expired dates or are no longer prescribed for the client. Which of the following actions should the nurse take?
Explanation
This is the safest and most environmentally friendly way to dispose of expired or unused medications. It prevents accidental ingestion, misuse, abuse, or diversion of medications by others. It also reduces the risk of contamination of water sources or soil by pharmaceuticals.
Incorrect choices:
a) Dispose of the expired or unused medications in a trash can: This is not a safe way to dispose of expired or unused medications. It can expose others, such as children, pets, or scavengers, to potentially harmful substances. It can also allow medications to leach into landfills or groundwater.
c) Advise the client to keep the expired or unused medications for future use: This is not a safe way to manage expired or unused medications. It can lead to medication errors, such as taking the wrong medication, the wrong dose, or an ineffective or harmful medication. It can also encourage self medication or sharing of medications with others without medical supervision.
d) Flush the expired or unused medications down a toilet or a sink: This is not an environmentally friendly way to dispose of expired or unused medications. It can contaminate water sources or aquatic life with pharmaceuticals. It can also damage plumbing or sewage systems.
A nurse is preparing to administer medication to a client. The nurse scans the barcode on the medication and the client's wristband. The nurse notices that the medication name on the computer screen does not match the medication name on the label. Which of the following actions should the nurse take?
Explanation
This is the safest action to take when there is a discrepancy between the barcode and the label of a medication. It prevents administering the wrong medication to a client, which could cause harm or adverse effects. It also alerts the pharmacy of a possible error in dispensing or labelling the medication.
Incorrect choices:
a) Administer the medication as prescribed and document the discrepancy: This is not a safe action to take when there is a discrepancy between the barcode and the label of a medication. It could result in administering the wrong medication to a client, which could cause harm or adverse effects. It also does not address the source of the error or prevent its recurrence.
b) Check the medication label and the prescription order again: This is not a sufficient action to take when there is a discrepancy between the barcode and the label of a medication. It could lead to confirmation bias, where the nurse overlooks or ignores the discrepancy and assumes that the medication is correct. It also does not address the source of the error or prevent its recurrence.
c) Contact the pharmacist and verify the medication: This is not an appropriate action to take when there is a discrepancy between the barcode and the label of a medication. It could delay the administration of the medication or create confusion about which medication is correct. It also does not address the source of the error or prevent its recurrence.
A nurse is teaching a group of nursing students about strategies to prevent medical errors. Which of the following statements by a nursing student indicates an understanding of the teaching?
Explanation
This statement shows that the nursing student understands the importance of reporting errors or near misses, which are events that could have resulted in harm but did not. Reporting errors or near misses helps to identify system failures, root causes, and contributing factors that can be addressed to prevent similar errors in the future. Reporting errors or near misses also fosters a culture of safety, transparency, and learning in healthcare organizations.
Incorrect choices:
a) I should follow my intuition when making clinical decisions: This statement shows that the nursing student does not understand how intuition can lead to cognitive biases, heuristics, or shortcuts that can impair clinical reasoning and judgment. Intuition can be influenced by emotions, assumptions, stereotypes, or previous experiences that may not be relevant or applicable to the current situation. Nursing students should use evidence-based practice, critical thinking, and clinical guidelines when making clinical decisions.
b) I should use abbreviations and acronyms to save time when documenting: This statement shows that the nursing student does not understand how abbreviations and acronyms can cause communication errors, confusion, or misinterpretation among health care providers. Abbreviations and acronyms can have multiple meanings, vary by context or setting, or be easily mistaken for other words or symbols. Nursing students should use clear, concise, and standardized terminology when documenting.
d) I should work longer shifts to reduce handoffs and transitions of care: This statement shows that the nursing student does not understand how working longer shifts can increase fatigue, stress, burnout, or distraction among health care providers. Working longer shifts can impair physical, mental, and emotional well-being, as well as performance, attention, memory, and decision-making skills. Nursing students should work reasonable hours, take breaks, and ensure adequate rest and sleep. They should also use effective handoff techniques, such as SBAR (Situation-Background-Assessment-Recommendation).
A nurse is teaching a client about the importance of reporting any medication errors that may occur during hospitalization. Which of the following statements by the client indicates a need for further education?
Explanation
This statement reflects a lack of understanding of the potential consequences of medication errors. Even minor errors can lead to adverse events, complications, or increased length of stay. The client should be aware of the risks and benefits of their medication and report any errors or concerns to the nurse.
Incorrect choices:
a) "I should tell the nurse if I notice any unusual symptoms after taking my medication.": This statement shows that the client understands the importance of monitoring for adverse reactions and communicating with the nurse.
b) "I should check the label of the medication before I take it to make sure it is mine.": This statement shows that the client is taking an active role in preventing medication errors by verifying their identity and medication.
d) "I should ask questions if I am not sure about the purpose or side effects of a medication.": This statement shows that the client is seeking information and clarification about their medication, which can enhance their safety and adherence.
Exams on Medication Safety and Error Prevention
Custom Exams
Login to Create a Quiz
Click here to loginMedication Safety and Error Prevention
Lessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Login to View Medication Safety and Error Prevention Study Video
Notes Highlighting is available once you sign in. Login Here.
Objectives
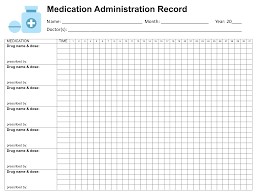
- Define medication reconciliation and medication administration record (MAR)
- Explain the importance of medication reconciliation and MAR in ensuring patient safety and quality of care
- Identify the causes and risk factors of medication errors
- Recognize the signs and symptoms of medication errors
- Describe the diagnosis and treatment of medication errors
- Discuss the nursing interventions and care for patients who experience medication errors
- Apply the prevention and education strategies to reduce medication errors
- Evaluate the reporting systems for medication errors
Introduction
- Medication reconciliation is the process of comparing a patient's medication orders with all of the medications that the patient has been taking.
- A medication administration record (MAR) is a document that records all of the medications that are administered to a patient.
- Medication reconciliation and MAR are essential tools to ensure that patients receive the correct medications at the correct doses, times, routes, and frequencies.
- Medication errors are any preventable events that may cause or lead to inappropriate medication use or patient harm.
- Medication errors are one of the most common types of medical errors and can have serious consequences for patients' health and well-being.
- Medication error prevention strategies and reporting systems are measures that aim to reduce the occurrence and impact of medication errors.
Causes and risk factors
- The causes and risk factors of medication errors can be classified into three categories:
- Human factors
- System factors
- Environmental factors
- Human factors include:
- Lack of knowledge skills or experience
- Poor communication
- Fatigue
- Stress
- Distraction
- Confirmation bias
- Memory lapses
- Calculation errors
- System factors include:
- Inadequate policies, procedures, or protocols
- lack of standardization
- Insufficient resources
- Poor documentation
- Lack of feedback
- Environmental factors include:
- Noise
- Lighting
- Temperature
- Humidity
- Clutter
- Interruptions
Signs and symptoms
- The signs and symptoms of medication errors depend on the type, severity, and duration of the error.
- Some common signs and symptoms include:
- Allergic reactions
- Adverse drug reactions
- Drug interactions
- Overdose
- Under-dose
- Therapeutic failure.
- Some specific signs and symptoms include:
- Changes in vital signs
- Changes in laboratory values
- Changes in mental status
- Changes in physical appearance or function
- Pain
- Nausea
- Vomiting
- Diarrhoea
- Constipation
- Rash
- Itching
- Swelling
- Bleeding
- Bruising

Diagnosis and treatment
- The diagnosis of medication errors involves identifying the source, type, and extent of the error.
- The diagnosis may require:
- Reviewing the patient's medical history
- Medication history
- Allergy history
- Current medications
- Interviewing the patient, family members, or caregivers
- Examining the patient
- Performing laboratory tests or imaging studies
- Consulting with other healthcare professionals
- The treatment of medication errors depends on the nature and severity of the error
- The treatment may involve:
- Discontinuing or adjusting the medication
- Administering an antidote or a reversal agent
- Providing supportive care
- Monitoring the patient's condition

Nursing interventions and care
- The nursing interventions and care for patients who experience medication errors are based on the principles of safety, quality, and accountability.
- The nursing interventions and care may include:
- Reporting the error to the appropriate authority
- Documenting the error and its consequences
- Informing the patient, family members, or caregivers about the error and its implications
- Apologizing for the error
- Providing emotional support

- Educating the patient, family members, or caregivers about the medication and its proper use
- Following up with the patient
- Evaluating the outcomes
Prevention and Education
- The prevention and education strategies to reduce medication errors are based on the principles of evidence-based practice, teamwork, and patient-centred care.
- The prevention and education strategies may include:
- Using standardized abbreviations, symbols, units, and terminology;
- Using computerized provider order entry (CPOE) systems;
- Using bar-code technology;
- Using smart pumps;
- Using automated dispensing cabinets;
- Using double-check systems;
- Using checklists;
- Using clinical decision support systems
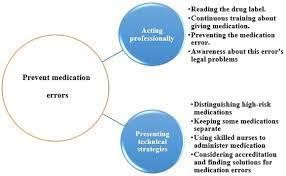
-The prevention and education strategies also involve: enhancing knowledge and skills through:
- Improving communication through verbal confirmation, read-back, or hand-off techniques
- Reducing fatigue, stress, distraction, or interruption through scheduling, staffing, or workload management
- Creating a culture of safety that encourages reporting, learning, feedback, and improvement
- Training, simulation, or continuing education

Conclusion
- Medication reconciliation and medication administration record (MAR) are important tools to ensure that patients receive the correct medications at the correct doses, times, routes, and frequencies.
- Medication errors are any preventable events that may cause or lead to inappropriate medication use or patient harm.
- Medication errors can be caused by human factors, system factors, or environmental factors.
- Medication errors can have various signs and symptoms depending on the type, severity, and duration of the error.
- Medication errors can be diagnosed and treated by identifying the source, type, and extent of the error and providing appropriate interventions and care.
- Medication errors can be prevented and reduced by applying evidence-based practice, teamwork, and patient-centred care strategies.
Summary
This study guide has covered the following topics: medication reconciliation and medication administration record (MAR), medication error prevention strategies and reporting systems, causes and risk factors of medication errors, signs and symptoms of medication errors, diagnosis and treatment of medication errors, nursing interventions and care for patients who experience medication errors, prevention and education strategies to reduce medication errors.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Medication Safety and Error Prevention
This filled cannot be empty

