Please set your exam date
Common Pediatric Conditions
Study Questions
Croup
A 2-year-old boy is brought to the emergency department with a barking cough, hoarseness, and inspiratory stridor.
His parents report that he has been sick for 2 days and that his symptoms have been getting worse.
The boy's vital signs are as follows: temperature 102°F (38.9°C), heart rate 120 beats/minute, respiratory rate 28 breaths/minute, and oxygen saturation 95% on room air.
Physical examination reveals a well-developed, well-nourished boy in moderate respiratory distress.
He is using accessory muscles of respiration and has intercostal retractions.
His lungs are clear to auscultation.
Which of the following statements by the nurse is most appropriate?
Explanation
Choice A rationale:
Croup typically presents with a barking cough, hoarseness, and inspiratory stridor, which are caused by inflammation of the larynx, trachea, and bronchi.
This choice is incorrect.
Choice B rationale:
The patient's symptoms, including inspiratory stridor, hoarseness, and rapid deterioration, are indicative of epiglottitis, a serious bacterial infection that can cause airway obstruction.
It is a medical emergency requiring urgent intervention.
This choice is correct.
Choice C rationale:
Asthma is characterized by chronic inflammation and narrowing of the airways, leading to symptoms such as wheezing and shortness of breath.
The absence of wheezing in this patient makes this choice incorrect.
Choice D rationale:
Pneumonia can cause fever, cough, and shortness of breath, but it usually presents with focal findings on lung examination, such as crackles or decreased breath sounds.
The absence of these findings in this patient makes this choice incorrect.
Which clinical manifestations should the nurse include in the teaching? Select all that apply.
Explanation
Choice A rationale:
High fever is not a typical symptom of croup.
Croup is often caused by viral infections, and high fever is more commonly associated with bacterial infections.
This choice is incorrect.
Choice B rationale:
Inspiratory stridor is a classic symptom of croup and is caused by the narrowing of the larynx and trachea, leading to a high-pitched sound during inspiration.
This choice is correct.
Choice C rationale:
A barking cough is a distinctive symptom of croup and is caused by inflammation of the larynx and trachea.
This choice is correct.
Choice D rationale:
Wheezing is not a typical symptom of croup.
Wheezing is more commonly associated with conditions like asthma, where there is narrowing of the smaller airways (bronchioles).
This choice is incorrect.
Choice E rationale:
Respiratory distress, indicated by increased work of breathing, is a common symptom of croup.
It can manifest as the use of accessory muscles, intercostal retractions, and nasal flaring.
This choice is correct.
What should the nurse assess to determine the severity of respiratory distress?
Explanation
The nurse should assess the degree of airway obstruction to determine the severity of respiratory distress.
Choice A rationale:
Assessing the child's height and weight is important for overall health assessment but does not specifically determine the severity of respiratory distress in croup.
Respiratory distress is primarily evaluated by assessing airway patency, effort of breathing, and oxygenation.
Choice B rationale:
The child's vaccination history is crucial for preventing certain infectious diseases, but it does not directly assess the severity of respiratory distress in croup.
Croup is commonly caused by viral infections such as parainfluenza viruses.
Choice C rationale:
Assessing the degree of airway obstruction is essential in determining the severity of respiratory distress in croup.
Children with croup often present with stridor, a high-pitched sound heard during inspiration, indicating partial airway obstruction.
The severity of stridor, along with signs of increased work of breathing, provides valuable information about the child's respiratory status.
Choice D rationale:
The child's social activities are not directly related to the assessment of respiratory distress in croup.
While social history is important in a comprehensive nursing assessment, it does not provide specific information about the severity of airway obstruction in croup.
What interventions are appropriate for a child with croup? Select all that apply.
Explanation
Nursing interventions for a child with croup include providing cool mist humidification, administering bronchodilators, and administering corticosteroids.
Choice A rationale:
Administering antibiotics is not a standard intervention for croup unless there is a secondary bacterial infection present.
Croup is typically caused by viral infections, so antiviral medications might be considered if the cause is identified as a specific virus.
However, antibiotics do not directly address the symptoms of croup.
Choice B rationale:
Providing cool mist humidification is appropriate for a child with croup.
Cool mist helps soothe the inflamed airways and can alleviate respiratory distress by reducing airway edema.
Moist air can make breathing easier for the child.
Choice C rationale:
Administering bronchodilators can be beneficial in the treatment of croup, especially if there is evidence of bronchoconstriction.
Bronchodilators help dilate the airways, making breathing easier for the child.
This intervention can be particularly useful if the child is experiencing wheezing in addition to stridor.
Choice D rationale:
Administering corticosteroids, such as dexamethasone, is a common and evidence-based intervention for croup.
Corticosteroids reduce airway inflammation and edema, leading to symptom improvement.
A single dose of oral corticosteroids is often sufficient to manage croup symptoms effectively.
Choice E rationale:
Encouraging the child to cough loudly is not a recommended intervention for croup.
Coughing forcefully may exacerbate airway irritation and inflammation, worsening the child's symptoms.
Instead, interventions should focus on reducing airway edema and providing respiratory support.
The child's mother states that the child has had a barking cough for 2 days, which is worse at night.
The child also has a fever and is hoarse.
Which of the following statements by the nurse is most appropriate?
Explanation
The nurse should assess the child's vital signs and listen to his lungs.
Choice A rationale:
Assessing vital signs, including heart rate, respiratory rate, oxygen saturation, and temperature, is essential in evaluating the child's overall condition and the severity of respiratory distress.
Listening to the child's lungs can help identify abnormal breath sounds, such as stridor or wheezing, which are common in croup.
This information guides further interventions and helps determine the appropriate level of care.
Choice B rationale:
While croup can cause respiratory distress, not every case requires an emergency room visit.
The severity of symptoms, including the child's ability to breathe and oxygenate, should guide the decision to seek emergency care.
In this scenario, assessing vital signs and lung sounds is the initial appropriate action.
Choice C rationale:
Croup is a treatable condition, and there are specific interventions, such as providing humidified air and corticosteroids, that can alleviate symptoms and prevent complications.
It is incorrect to tell the parent that there is nothing that can be done for croup.
Medical intervention can significantly improve the child's condition.
Choice D rationale:
Croup is primarily caused by viral infections, not bacterial infections.
Administering antibiotics without confirming a bacterial infection is inappropriate and contributes to antibiotic resistance.
The nurse explains that croup is a viral infection that causes inflammation of the upper airway.
The nurse also explains that the most common symptoms of croup are a barking cough, hoarseness, and stridor.
Which of the following statements by the client indicates that they understand the nurse's explanation?
Explanation
Choice A rationale:
This statement does not indicate a complete understanding of croup.
Croup is not just a cold that affects the throat; it specifically involves inflammation of the upper airway.
Choice B rationale:
This statement acknowledges that croup can be serious but usually resolves on its own.
While this is true, it does not encompass the key symptoms and actions the parent should take if the child's condition worsens.
Choice C rationale:
This statement addresses general cold symptoms but does not specifically mention the characteristic symptoms of croup, such as barking cough, hoarseness, and stridor.
Choice D rationale:
This is The correct answer.
It shows an understanding of the symptoms of croup, particularly the mention of having trouble breathing, which is a sign of severe croup that requires medical attention.
Parents should seek emergency medical care if their child experiences difficulty breathing due to croup.
Providing this information demonstrates a comprehensive understanding of the condition.
Which of the following are nursing interventions for a child with croup?
Explanation
Choice A rationale:
Administering oxygen therapy is essential in cases of severe croup where the child has difficulty breathing.
Oxygen therapy helps ensure adequate oxygenation, which is crucial in managing respiratory distress.
Choice B rationale:
Positioning the child upright facilitates breathing by allowing the airways to remain open and reducing airway obstruction.
This position helps alleviate symptoms like stridor and allows the child to breathe more comfortably.
Choice C rationale:
Providing humidified air helps loosen secretions and makes it easier for the child to breathe.
Humidification can reduce airway irritation and soothe the inflamed throat, providing relief from croup symptoms.
Choice D rationale:
This choice is incorrect because encouraging the child to drink plenty of fluids is generally good advice for any illness but is not specific to croup.
While it is essential to keep the child hydrated, it is not a direct nursing intervention for managing croup symptoms.
Choice E rationale:
Monitoring the child's respiratory status closely is crucial in assessing the effectiveness of the interventions and identifying any signs of respiratory distress.
Close monitoring allows nurses to make timely decisions and take appropriate actions to maintain the child's respiratory function.
The nurse explains that it is important to keep the child hydrated and to provide humidified air.
Which of the following statements by the parent indicates that they understand the nurse's instructions?
Explanation
Choice A rationale:
While giving the child plenty of water and juice is important for hydration, this statement does not address the specific management of croup symptoms.
Choice B rationale:
Running a hot shower and letting the child sit in the bathroom can create a steamy environment, but it is not the most effective way to provide humidified air.
A cool mist humidifier is a more controlled and efficient method for delivering humidified air to the child.
Choice C rationale:
This is The correct answer.
Using a cool mist humidifier in the child's bedroom is an appropriate way to provide humidified air, which can help ease breathing difficulties associated with croup.
Cool mist humidifiers add moisture to the air without heating it, making it easier for the child to breathe and reducing throat irritation.
Choice D rationale:
Giving the child a warm bath may provide some comfort but does not specifically address the need for humidified air, which is crucial in managing croup symptoms.
Providing humidified air helps soothe the inflamed airways and reduce respiratory distress associated with croup.
The child's respiratory status is worsening, and they are becoming increasingly agitated.
What action should the nurse take?
Explanation
Choice A rationale:
Continuing to monitor the child's respiratory status may not be the best action in this situation, as the child's respiratory status is worsening and they are becoming increasingly agitated.
Immediate intervention is required to alleviate the child's distress.
Choice B rationale:
Administering oxygen therapy as needed is a supportive measure in respiratory distress situations, but in the case of severe croup with worsening respiratory status and agitation, nebulized epinephrine is the treatment of choice to reduce airway inflammation and improve breathing.
Choice C rationale:
Nebulized epinephrine is the primary treatment for severe croup as it helps reduce upper airway edema, relieve stridor, and improve respiratory distress.
It acts by causing vasoconstriction, which reduces swelling in the upper airway, making breathing easier for the child.
Therefore, preparing to administer nebulized epinephrine is the most appropriate action in this situation.
Choice D rationale:
Notifying the physician immediately is essential, but immediate intervention to improve the child's respiratory distress is also necessary.
Nebulized epinephrine should be administered promptly to alleviate the child's symptoms and prevent further deterioration.
The child's oxygen saturation is 92%.
The nurse assesses the child's respiratory status and determines that the child has moderate croup.
Which of the following statements by the nurse is most appropriate?
Explanation
Choice A rationale:
Placing the child on a ventilator might be necessary in severe cases of croup, but it should not be the first action taken.
In this scenario, the child has moderate croup, so less invasive interventions should be attempted first.
Choice B rationale:
Administering medication to help the child's cough and breathing is an appropriate first step in managing moderate croup.
Nebulized epinephrine or corticosteroids are commonly used to reduce airway inflammation and relieve respiratory distress in croup.
This intervention can be effective in improving the child's symptoms and overall condition.
Choice C rationale:
Transferring the child to the ICU for closer monitoring is not immediately necessary in this case of moderate croup.
Such a step might be considered if the child's condition worsens despite initial interventions or if there are signs of severe respiratory distress.
Choice D rationale:
Discharging the child home without appropriate treatment and monitoring would be unsafe, given the child's symptoms and oxygen saturation level.
Immediate intervention and observation are required to ensure the child's respiratory status improves.
Which of the following statements should the nurse include in the teaching?
Select all that apply.
Explanation
Choice A rationale:
Croup is indeed a common viral infection of the upper respiratory tract that causes inflammation of the larynx.
This statement is accurate and important for the parent to understand the nature of the illness.
Choice B rationale:
Croup is most common in children under the age of 5, not just under the age of 3.
However, this statement is not entirely accurate, as older children can also be affected by croup.
It is essential to provide correct information to the parent.
Choice C rationale:
The symptoms of croup often worsen at night due to the natural narrowing of the airways during sleep, making breathing more difficult.
Therefore, this statement is correct and relevant to include in the teaching.
Choice D rationale:
The classic croup cough is indeed described as a barking cough, which results from the inflammation of the larynx and trachea.
This description helps the parent recognize a distinctive symptom of croup.
Including this information in the teaching is appropriate.
Choice E rationale:
Croup is primarily managed with supportive care, such as humidified air and nebulized medications.
Over-the-counter cough syrup and expectorants are not typically recommended for treating croup in children.
This statement is incorrect and should not be included in the teaching.
The child is receiving humidified air and nebulized racemic epinephrine.
The nurse monitors the child's respiratory status closely.
Which of the following findings would indicate to the nurse that the child's condition is worsening?
Explanation
Choice A rationale:
An oxygen saturation level of 95% is within the normal range (normal range is typically 95-100%).
While it is essential to monitor oxygen saturation, this value does not indicate worsening of the child's condition.
Choice B rationale:
A respiratory rate of 30 breaths per minute is above the normal range for a child and can indicate respiratory distress.
An increased respiratory rate is a concerning sign, suggesting the child is having difficulty breathing.
This finding indicates the child's condition is worsening and requires prompt attention.
Choice C rationale:
Mild retractions suggest that the child is working harder to breathe but may not necessarily indicate a severe worsening of the condition.
Retractions are a sign of increased respiratory effort but may vary in severity.
Choice D rationale:
A child with croup experiencing severe respiratory distress may not be able to speak in complete sentences due to the difficulty in breathing.
However, the ability to speak in complete sentences alone may not be a definitive indicator of worsening.
Monitoring the respiratory rate and effort is crucial in assessing the child's condition accurately.
Which of the following statements should the nurse include in the teaching?
Explanation
Choice A rationale:
There is no vaccine to prevent croup, but practicing good hand hygiene and avoiding contact with sick people can help reduce the child's risk of getting croup.
Croup is mainly caused by viral infections, so minimizing exposure to viruses is essential in prevention.
Choice B rationale:
Giving a daily dose of vitamin C is not a proven method for preventing croup.
While vitamin C is essential for overall health, it does not specifically prevent croup.
Providing accurate and evidence-based information is crucial in parental education.
Choice C rationale:
Keeping the child's bedroom cool and humid may provide comfort during the illness, but it is not a proven method for preventing croup.
This statement does not contribute significantly to preventive measures against croup.
Choice D rationale:
Using a humidifier in the home can help maintain adequate humidity levels, which may reduce the risk of croup, especially during dry seasons.
Proper humidity can prevent irritation of the upper respiratory tract and decrease the likelihood of developing croup.
Including this information in the teaching is appropriate and beneficial for the parent to know.
Tonsillitis in children.
She explains that tonsillitis is a common condition in children and can be caused by various factors.
One of the parents asks about the causes of tonsillitis.
Which of the following statements by the nurse would be most accurate?
Explanation
Choice A rationale:
Tonsillitis is not always caused by bacterial infections.
It can also be caused by viral infections.
Choice B rationale:
Tonsillitis is not only caused by viral infections.
Bacterial infections can also lead to tonsillitis.
Choice C rationale:
Tonsillitis can be caused by either viral infections such as adenovirus, rhinovirus, or Epstein-Barr virus, or bacterial infections, particularly Streptococcus pyogenes.
This is the most accurate statement.
Streptococcus pyogenes is a common bacterial cause of tonsillitis, and viral infections can also lead to this condition.
Choice D rationale:
Tonsillitis is not usually caused by allergies.
While allergies can cause throat discomfort, they are not a common cause of tonsillitis.
She asks the nurse why her child keeps getting tonsillitis.
Which of the following responses by the nurse would be most appropriate?
Explanation
Choice A rationale:
Enlarged tonsils might contribute to recurrent tonsillitis, but it is not the primary cause.
Choice B rationale:
Dust and irritants can irritate the throat, but they are not the main reason for recurring tonsillitis.
Choice C rationale:
Your child’s immune system might be deficient, making them more susceptible to infections.
This response is appropriate because a weakened immune system can make a child more prone to recurrent infections, including tonsillitis.
Choice D rationale:
Improper handwashing can lead to various infections, but it is not specifically linked to tonsillitis.
The nurse suspects tonsillitis and knows that certain signs and symptoms are indicative of this condition.
Which of the following should the nurse consider? (Select all that apply).
Explanation
Choice A rationale:
The child has been having difficulty swallowing.
Difficulty swallowing is a common symptom of tonsillitis.
Inflamed tonsils can make swallowing painful and difficult.
Choice B rationale:
The child has been experiencing ear pain.
While ear pain can be associated with throat infections, it is not a direct symptom of tonsillitis.
Choice C rationale:
The child has a rash on their arms and legs.
A rash is not a typical symptom of tonsillitis.
It could indicate other conditions such as an allergic reaction or viral illness.
Choice D rationale:
The child’s tonsils appear red and swollen.
Red and swollen tonsils are characteristic signs of tonsillitis.
Inflammation of the tonsils is a key indicator of the condition.
Choice E rationale:
The child has been experiencing frequent nosebleeds.
Nosebleeds are not typically associated with tonsillitis.
They could be due to other factors such as dry air or nasal irritation.
She mentions that in bacterial tonsillitis, certain processes occur within the body.
Which of the following statements best describes these processes?
Explanation
Choice A rationale:
Bacterial tonsillitis is caused by the colonization of bacteria on the tonsils, triggering an immune response.
When bacteria, often Streptococcus species, invade the tonsils, the body's immune system recognizes them as foreign invaders.
This recognition prompts an immune response, leading to inflammation and swelling of the tonsils.
The immune system releases white blood cells and other substances to fight the infection, causing the characteristic symptoms of tonsillitis, such as sore throat, difficulty swallowing, and fever.
This process is a localized immune response specific to the tonsils and their surrounding tissues.
Choice B rationale:
This choice is incorrect because bacteria do not invade the tonsils directly and immediately cause inflammation and swelling.
The immune response is triggered upon recognition of the bacteria, leading to the inflammation and swelling of the tonsils.
Choice C rationale:
This choice is incorrect because bacterial tonsillitis is not caused by an allergic reaction in the tonsils.
It is primarily a result of a bacterial infection, not an allergic response.
Choice D rationale:
This choice is incorrect because bacterial tonsillitis is a localized infection in the tonsils and does not cause a systemic infection that indirectly leads to tonsillitis.
The infection remains localized in the throat area, causing symptoms specific to the tonsils and nearby lymph nodes.
A nurse knows that understanding the etiology of tonsillitis is essential for providing appropriate care to these patients.
Which of the following factors should the nurse consider when assessing this client?
Explanation
Choice A rationale:
When assessing a client with suspected tonsillitis, it is essential to consider whether the client has been exposed to viral or bacterial infections recently.
Tonsillitis can be caused by both viral and bacterial infections, with streptococcal bacteria being a common culprit.
Understanding the type of infection helps healthcare providers determine the appropriate treatment, such as antibiotics for bacterial infections.
Recent exposure to infected individuals or environments increases the likelihood of a contagious infection.
Choice B rationale:
This choice is incorrect because while a balanced diet is crucial for overall health, it is not a direct factor in the etiology of tonsillitis.
Tonsillitis is primarily caused by infections, either viral or bacterial, and is not related to dietary habits.
Choice C rationale:
This choice is incorrect because exposure to cold temperatures is not a direct cause of tonsillitis.
Tonsillitis is caused by infections and is not related to environmental factors like cold weather.
However, cold weather can weaken the immune system, making individuals more susceptible to infections.
Choice D rationale:
This choice is incorrect because recent injuries to the throat area can cause throat pain and discomfort but are not a common cause of tonsillitis.
Tonsillitis is predominantly caused by infections, and injuries play a minor role in its etiology.
The child’s mother reports that the child has been having difficulty swallowing and has had a fever.
Upon examination, the nurse notes that the child’s tonsils are red and swollen, with white patches visible.
The child also has enlarged lymph nodes in the neck.
Which of the following statements by the mother indicates a need for further teaching?
Explanation
Choice A rationale:
Encouraging the child to drink plenty of fluids is a suitable response by the mother.
Staying hydrated is essential to prevent dehydration, especially when the child has difficulty swallowing due to swollen tonsils.
Adequate fluid intake can also soothe the throat and help in the recovery process.
Choice B rationale:
Providing warm soup to soothe the throat is a suitable response.
Warm, soothing liquids can help alleviate throat discomfort and make swallowing easier.
It is a common home remedy for managing sore throat symptoms.
Choice C rationale:
This choice is correct because encouraging the child to cough to clear the throat is not appropriate.
Coughing can irritate the already inflamed tonsils and worsen the sore throat.
Instead, the child should be advised to avoid coughing forcefully, which can aggravate the pain.
Choice D rationale:
Giving the child over-the-counter pain medication as directed is a suitable response.
Over-the-counter pain relievers like acetaminophen or ibuprofen can help reduce pain and fever associated with tonsillitis.
However, it's important to use these medications as directed by a healthcare professional or following the recommended dosage instructions, especially in children.
The nurse observes red and swollen tonsils with white patches, enlarged lymph nodes in the neck, and bad breath.
The client also complains of a headache and abdominal pain.
Which of the following statements by the client indicates an understanding of the care plan?
Explanation
Choice A rationale:
The client's symptoms, including sore throat, difficulty swallowing, fever, red and swollen tonsils with white patches, enlarged lymph nodes, bad breath, headache, and abdominal pain, indicate possible tonsillitis, which is often caused by a bacterial infection.
Rest and increased fluid intake are essential components of the care plan for tonsillitis.
Adequate rest helps the body fight the infection, and increased fluid intake helps prevent dehydration, especially if swallowing is painful.
This choice demonstrates the client's understanding of self-care measures to promote recovery.
Choice B rationale:
Continuing to smoke can worsen the irritation of the throat and prolong the healing process.
Smoking irritates the mucous membranes, making it difficult for the throat to heal.
It can also exacerbate the symptoms and delay recovery.
Choice C rationale:
Tonsillitis caused by bacteria often requires antibiotics to clear the infection completely.
Taking antibiotics only when in pain might lead to incomplete eradication of the bacteria, resulting in a recurrence of the infection or complications.
It is essential to take the full course of antibiotics as prescribed by the healthcare provider.
Choice D rationale:
Going to work when experiencing symptoms of tonsillitis not only jeopardizes the client's health but also puts coworkers at risk of contracting the infection.
Resting at home and avoiding contact with others can prevent the spread of the illness.
The child’s symptoms include a severe sore throat, difficulty swallowing, fever, red and swollen tonsils with white patches, enlarged lymph nodes in the neck, bad breath, headache, abdominal pain, and fatigue.
Select all that apply:.
Explanation
Choice A rationale:
Assessing for drooling is important because severe tonsillitis can cause difficulty swallowing, leading to excessive drooling, especially in children.
Drooling indicates difficulty managing oral secretions and can be a sign of airway obstruction, necessitating immediate medical attention.
Choice B rationale:
Assessing for an earache is crucial because the infection from the tonsils can spread to the nearby ear structures, causing ear pain.
Earache in conjunction with other symptoms can indicate the spread of the infection and may require additional medical evaluation and treatment.
Choice C rationale:
Assessing for neck stiffness is important because it can be a sign of meningitis, a serious complication of some bacterial infections, including streptococcal bacteria that can cause tonsillitis.
Neck stiffness, along with other symptoms, can indicate the involvement of the central nervous system and requires urgent medical attention.
Choice D rationale:
Assessing for increased energy levels is not relevant to tonsillitis.
In fact, individuals with tonsillitis often experience fatigue due to the body's immune response to the infection.
Increased energy levels would not be a typical symptom of this condition.
Choice E rationale:
Assessing for vomiting is not a common symptom of tonsillitis.
While individuals with severe throat pain might have difficulty swallowing, leading to decreased oral intake, vomiting is not a direct symptom of tonsillitis.
Vomiting could indicate other underlying issues that need further assessment but is not specifically related to tonsillitis.
The child is experiencing severe throat pain and is refusing to drink fluids.
The nurse understands the importance of hydration in promoting recovery and preventing complications.
Which of the following statements should the nurse make to encourage the child to drink fluids?
Explanation
Choice A rationale:
This statement uses fear as a tactic to encourage the child to drink fluids, which is not a supportive or therapeutic approach.
It may create anxiety and resistance in the child, making them less likely to cooperate.
Choice B rationale:
This statement provides a positive and encouraging approach by explaining the benefits of drinking fluids.
It educates the child about the importance of hydration in feeling better faster, which can motivate them to cooperate with the nurse's recommendations.
Choice C rationale:
Threatening the child with an injection may create fear and distress, potentially worsening the child's refusal to drink fluids.
This approach is not conducive to building trust and cooperation with the child.
Choice D rationale:
Using threats related to discharge or privileges may cause stress and anxiety in the child.
It is important to maintain a supportive and reassuring approach to promote cooperation and comfort in the child.
The nurse is providing discharge education to the client and their family about the importance of completing the prescribed antibiotic therapy.
Which of the following statements should the nurse make?
Explanation
Choice A rationale:
Stopping antibiotics once feeling better can lead to incomplete eradication of the infection, allowing remaining bacteria to develop resistance to the antibiotic.
It is essential to complete the full course of antibiotics to ensure complete resolution of the infection.
Choice B rationale:
Finishing all the antibiotics, even if symptoms improve, is crucial to prevent the development of antibiotic-resistant strains of bacteria.
Incomplete courses of antibiotics can lead to treatment failure and potential complications.
Choice C rationale:
While it is important to monitor for and report any side effects of antibiotics, stopping the medication immediately without consulting a healthcare provider can compromise the effectiveness of the treatment.
The nurse should instruct the client to report any adverse reactions for proper evaluation and management.
Choice D rationale:
Sharing antibiotics with others is dangerous and highly discouraged.
Each person's condition is unique, and taking antibiotics without proper diagnosis and prescription can lead to inappropriate use, antibiotic resistance, and potential harm to individuals with allergies or other medical conditions.
Which of the following interventions should be included in the plan? (Select all that apply).
Explanation
Choice A rationale:
Encouraging the child to participate in strenuous physical activities is not appropriate for a child with tonsillitis.
Strenuous physical activities can exacerbate the symptoms and discomfort associated with tonsillitis.
Choice B rationale:
Providing pain relief measures, such as acetaminophen or ibuprofen, as prescribed, is essential in managing the pain and discomfort associated with tonsillitis.
These medications can help reduce pain and fever, improving the child's overall comfort.
Choice C rationale:
Offering cool or warm liquids and soft foods is crucial in soothing the throat and making it easier for the child to swallow.
Cold or warm liquids can help alleviate the discomfort, and soft foods are less likely to irritate the inflamed tonsils.
Choice D rationale:
Educating the child and family about the importance of completing prescribed antibiotic therapy is essential.
Tonsillitis caused by bacteria requires antibiotic treatment to eliminate the infection fully.
Incomplete antibiotic therapy can lead to treatment failure and recurrent infections.
Choice E rationale:
Discouraging rest and promoting active play is not appropriate for a child with tonsillitis.
Rest is essential for the body to heal, and promoting active play can worsen the symptoms and delay the healing process.
The nurse understands that this surgical intervention is considered for which of the following reasons?
Explanation
Choice A rationale:
Having at least one episode of tonsillitis might not be a sufficient indication for a tonsillectomy.
Tonsillectomy is typically considered for recurrent tonsillitis, not just a single episode.
Choice B rationale:
Tonsillectomy is considered when the child's tonsillitis does not respond to antibiotic therapy and becomes recurrent.
Recurrent tonsillitis can significantly impact a child's quality of life and may necessitate surgical intervention to prevent frequent infections and complications.
Choice C rationale:
Mild throat discomfort alone is not a strong indication for tonsillectomy.
Tonsillectomy is usually reserved for cases of recurrent tonsillitis that do not respond to conservative treatments.
Choice D rationale:
The parents' anxiety about their child's condition is not a direct indication for tonsillectomy.
The decision for surgery should be based on the child's medical condition and the medical necessity of the procedure.
The nurse knows that this medication is used for which of the following reasons?
Explanation
Choice A rationale:
Erythromycin is an antibiotic that does not primarily target inflammation and swelling in the tonsils.
Its mechanism of action involves inhibiting protein synthesis in bacteria, thereby preventing the growth and spread of the bacterial infection causing tonsillitis.
Choice B rationale:
Erythromycin is used to treat bacterial infections by inhibiting protein synthesis in bacteria.
It is effective against a wide range of bacterial strains and can be prescribed for various infections, including tonsillitis, caused by susceptible bacteria.
Choice C rationale:
Erythromycin does not provide symptomatic relief from throat pain and discomfort directly.
While it addresses the underlying bacterial infection, it does not have analgesic properties to relieve pain.
Pain relief measures, such as acetaminophen or ibuprofen, are typically prescribed for managing throat pain associated with tonsillitis.
Choice D rationale:
Erythromycin does not prevent dehydration by encouraging fluid intake.
While staying hydrated is essential during illness, the role of erythromycin is to target the bacterial infection, not to promote fluid intake.
RSV in children
The nurse wants to emphasize the importance of prevention, especially in the winter and early spring months.
Which of the following statements would be most effective for the nurse to use?
Explanation
Choice A rationale:
This statement is incorrect.
RSV is most common in winter and early spring, not summer and fall.
Stating this misinformation would not effectively educate the parents about RSV prevention during the high-risk months.
Choice B rationale:
This is The correct answer.
RSV does occur in yearly outbreaks, especially in winter and early spring.
By emphasizing this, the nurse educates parents about the specific periods when they should take extra precautions to prevent RSV transmission.
Choice C rationale:
This statement is incorrect.
RSV is indeed seasonal, with higher incidence during the winter and early spring months.
Denying its seasonality would provide inaccurate information to the parents.
Choice D rationale:
This statement is incorrect.
RSV primarily affects infants and young children, not adults.
Providing this misinformation would not help parents understand the risks associated with RSV for their children.
The client is particularly concerned about how long the virus can survive on surfaces.
Which of the following responses from the nurse would be most accurate?
Explanation
Choice A rationale:
This is The correct answer.
RSV can survive on hard surfaces for several days and on hands for several hours.
Providing this information addresses the client's concern about the virus's survivability on surfaces.
Choice B rationale:
This statement is incorrect.
RSV can survive on hard surfaces for a longer duration than just several hours.
Providing this incorrect information could lead to misunderstandings about RSV transmission.
Choice C rationale:
This statement is incorrect.
RSV can survive on surfaces, so stating that it cannot survive outside of the body would be inaccurate and misleading.
Choice D rationale:
This statement is incorrect.
RSV can be transmitted not only through direct contact with an infected person but also through contact with contaminated surfaces and respiratory droplets.
Which of the following findings should alert the nurse that the child may have RSV? (Select all that apply).
Explanation
Choice A rationale:
This statement is incorrect.
A history of recurrent pneumonia is not a specific indicator of RSV infection.
RSV primarily affects the respiratory system, causing symptoms such as cough, wheezing, and difficulty breathing.
Choice B rationale:
This is a correct answer.
RSV symptoms typically appear 2 to 5 days after exposure.
Including this option helps identify the duration of symptoms, which is relevant to diagnosing RSV.
Choice C rationale:
This is a correct answer.
RSV commonly presents with symptoms like high fever and severe cough.
Recognizing these symptoms can help healthcare providers consider RSV as a possible diagnosis.
Choice D rationale:
This is a correct answer.
RSV can lead to bronchiolitis, which is inflammation of the small airways in the lungs.
Diagnosing a child with bronchiolitis can raise suspicion of RSV infection.
Choice E rationale:
This statement is incorrect.
A history of bacterial infections is not specific to RSV and does not provide relevant information for identifying RSV infection in this context.
The client is concerned about the risk of transmission to their young grandchildren.
Which of the following statements should the nurse make?
Explanation
Choice A rationale:
RSV (Respiratory Syncytial Virus) primarily affects young children and infants, making them more vulnerable to severe complications.
Adults can also contract the virus, but it is most common and dangerous in children under one year old.
Therefore, stating that RSV is most common in adults is incorrect.
Choice B rationale:
RSV is most common in children under one year old, so your grandchildren could be at risk.
This statement is correct.
RSV is highly contagious and spreads through respiratory droplets.
Infants and young children are more prone to severe infections due to their underdeveloped immune systems.
Hence, the nurse should educate the client that their grandchildren, especially those under one year old, are at risk of contracting RSV.
Choice C rationale:
RSV does affect individuals with compromised immune systems, but it is not limited to them.
Children, especially those under one year old, are also highly susceptible to RSV infections.
Therefore, this statement is not comprehensive and accurate.
Choice D rationale:
RSV can be transmitted from person to person through respiratory secretions.
It is highly contagious, especially in crowded places like daycare centers and hospitals.
This statement is incorrect, as RSV transmission is well-documented.
Which of the following explanations should the nurse provide?
Explanation
Choice A rationale:
RSV infects the squamous epithelial cells of your bronchioles, alveoli, and nasal passages.
This statement is accurate.
RSV primarily targets the respiratory tract, infecting the cells lining the bronchioles, alveoli, and nasal passages.
This infection can lead to symptoms ranging from mild cold-like symptoms to severe respiratory distress, particularly in young children and individuals with weakened immune systems.
Choice B rationale:
RSV does not cause the immune system to attack the body's own cells.
It primarily targets the respiratory system, leading to respiratory symptoms.
Autoimmune responses are not associated with RSV infections.
Choice C rationale:
RSV does not lead to an overproduction of red blood cells.
This statement is incorrect and not related to the pathophysiology of RSV infections.
Choice D rationale:
RSV does not cause the body to stop producing white blood cells.
White blood cells play a crucial role in the immune response, and stopping their production would severely compromise the body's ability to fight infections.
RSV primarily affects the respiratory system and does not directly impact white blood cell production.
The child’s mother reports that the child has had a runny nose, fever, and decreased appetite for the past two days.
The nurse notes that the child appears irritable and has a persistent cough.
Based on these symptoms, the nurse suspects that the child’s illness may progress to bronchiolitis or pneumonia, which could cause more severe respiratory distress.
What statement should the nurse make to educate the mother about the potential progression of RSV infection?
Explanation
Choice A rationale:
Your child may start to experience difficulty breathing.
This statement is accurate and crucial for the mother to be aware of.
RSV infections can progress to bronchiolitis or pneumonia, leading to more severe respiratory distress.
Difficulty breathing is a common symptom in these advanced stages of the infection, indicating the need for immediate medical attention.
Choice B rationale:
While a decreased appetite is a symptom mentioned in the scenario, it does not reflect the potential progression of RSV infection.
The focus should be on respiratory symptoms, which can indicate worsening conditions.
Choice C rationale:
Drowsiness is not a typical symptom of RSV progression.
Respiratory distress, such as difficulty breathing, is a more concerning sign and requires prompt medical evaluation.
Choice D rationale:
Developing a high fever is a general symptom of various infections, including RSV.
While fever is a concern, the scenario specifically mentions symptoms related to the respiratory system, making difficulty breathing a more relevant and specific warning sign for the mother to be aware of.
The client is worried about the child’s persistent cough and decreased appetite.
The nurse explains that in children younger than age 3, RSV infection can progress to bronchiolitis or pneumonia, causing more severe respiratory distress.
What statement should the nurse make to reassure the client about the management of these potential complications?
Explanation
Choice A rationale:
The nurse should reassure the client by stating, “We will monitor your child closely for any signs of respiratory distress.”.
This is the appropriate response because close monitoring is crucial in children with RSV infection, especially those younger than age 3.
Respiratory distress can rapidly progress in this age group, and early detection is essential for timely intervention.
Monitoring the child's respiratory rate, oxygen saturation, and other respiratory symptoms allows healthcare providers to assess the severity of the condition and provide appropriate interventions promptly.
Choice B rationale:
While ensuring rest and fluids is generally good advice for managing various illnesses, it does not specifically address the client’s concerns about the potential complications of RSV infection, such as bronchiolitis or pneumonia leading to respiratory distress.
Choice C rationale:
Administering medication to reduce fever is not the most pertinent information in this scenario.
The primary concern for the client is the progression of RSV infection to severe respiratory distress, not fever reduction.
Choice D rationale:
Providing a special diet to improve appetite does not address the client’s concerns about the respiratory complications associated with RSV infection.
Respiratory distress is the main worry in this situation, and dietary changes are not the appropriate focus.
The nurse notes that the child’s respiratory rate is 35 breaths per minute, oxygen saturation is 96%, pH is 7.38, and PaCO2 is 40.
Which of the following actions should the nurse take based on these results? (Select all that apply).
Explanation
Choice A rationale:
Continuing to monitor the child’s respiratory rate is essential.
The nurse should closely observe the child's respiratory status to detect any changes.
Monitoring helps in assessing the effectiveness of interventions and identifying any worsening of the condition promptly.
Choice B rationale:
Administering supplemental oxygen is appropriate in this situation because the child's oxygen saturation is 96%, which indicates that the child is not receiving adequate oxygen.
Supplemental oxygen helps maintain appropriate oxygen levels and prevents hypoxia.
Choice C rationale:
Reassessing the child’s oxygen saturation in one hour is a good nursing practice to ensure that the child's respiratory status remains stable or improves.
Regular reassessment allows for timely adjustments in the treatment plan if needed.
Choice D rationale:
While the pH value is within the normal range (7.35-7.45), it is essential to consider the entire clinical picture.
The nurse should continue to monitor the child's respiratory status and other parameters.
Notification to the healthcare provider may be necessary if there are significant changes in the child's condition, but the pH value alone does not warrant immediate notification.
Choice E rationale:
Immediate intubation based solely on the elevated PaCO2 is not indicated.
The child's PaCO2 of 40 mmHg falls within the normal range (35-45 mmHg) for a 3-year-old.
Intubation is a significant intervention and should be considered based on the overall clinical assessment, including the child's respiratory distress, oxygen saturation, and other vital signs.
The toddler’s symptoms include wheezing, retractions, nasal flaring, tachypnea, and cyanosis.
The nurse understands that these symptoms indicate severe respiratory distress, which is common in children younger than age 3 with RSV infection.
Which of the following interventions should be included in the toddler’s care plan?
Explanation
Choice A rationale:
Administering bronchodilators as prescribed is appropriate for managing severe respiratory distress and wheezing in children with RSV infection.
Bronchodilators help dilate the airways, making it easier for the child to breathe.
This intervention addresses one of the specific symptoms mentioned in the scenario.
Choice B rationale:
Encouraging fluid intake is important to prevent dehydration, especially in children with respiratory infections.
It helps maintain hydration status, which is essential for overall health.
While important, this choice alone does not address the severe respiratory distress symptoms mentioned in the scenario.
Choice C rationale:
Monitoring oxygen saturation levels is crucial in children with RSV infection, especially when they exhibit symptoms of severe respiratory distress such as wheezing, retractions, nasal flaring, tachypnea, and cyanosis.
Monitoring oxygen saturation helps assess the child's oxygenation status and guides interventions such as oxygen therapy.
Choice D rationale:
The correct answer is choice D, “All of these.”.
This is because all the interventions mentioned in choices A, B, and C are appropriate and necessary for managing severe respiratory distress in a toddler with RSV infection.
Administering bronchodilators addresses airway constriction and wheezing, encouraging fluid intake prevents dehydration, and monitoring oxygen saturation levels ensures appropriate oxygenation, allowing comprehensive care for the child’s condition.
The nurse explains to the client that these symptoms are likely due to bronchiolitis or pneumonia, which are common complications of RSV infection in children younger than age 3.
Which of the following statements by the client indicates an understanding of the infant’s condition?
Explanation
Choice A rationale:
The nurse should educate the client about the expected course of RSV infection in infants.
RSV (Respiratory Syncytial Virus) infection can lead to complications such as bronchiolitis or pneumonia, especially in children under the age of 3.
Symptoms like wheezing and tachypnea are indicative of respiratory distress.
Educating the client about the expected duration of the symptoms is crucial.
The client needs to understand that the baby's symptoms may last for about 10 days, and this is a common timeframe for the resolution of RSV infection in infants.
This information helps manage the client's expectations and reduces anxiety.
Choice B rationale:
While fever can be a sign of infection, it is not the most pertinent symptom to monitor in this case.
The primary concern is the respiratory distress caused by bronchiolitis or pneumonia.
While fever might indicate worsening infection, it is not the most relevant information in this context.
Choice C rationale:
Over-the-counter cold medicine is generally not recommended for infants and young children due to the risk of side effects.
Moreover, these medications may not be effective in managing the specific symptoms caused by RSV infection.
Advising the client to administer such medication could be harmful and is not an appropriate response.
Choice D rationale:
While it is essential to prevent the spread of RSV infection, especially among siblings, this choice does not address the client's understanding of the infant's condition.
The primary concern here is the client's grasp of the infant's symptoms and the expected course of the illness, which is best addressed by choice A.
The nurse knows that maintaining a patent airway is crucial in the management of this condition.
The child’s mother asks the nurse, “What can I do to help my child breathe better?” Which of the following responses by the nurse would be most appropriate?
Explanation
Choice A rationale:
Keeping the child calm and comfortable is generally advisable, but in the context of RSV infection, maintaining a patent airway is crucial.
While comfort measures are essential, this choice does not directly address the mother's query regarding improving the child's breathing.
Choice B rationale:
This is The correct answer because suctioning the child's nose and mouth as needed helps in removing secretions, thus maintaining a clear airway.
RSV infection often leads to increased mucus production, which can obstruct the airways, making it difficult for the child to breathe.
By suctioning secretions, the mother can help her child breathe more comfortably, which is essential in managing RSV infection.
Choice C rationale:
Over-the-counter cold medicine is generally not recommended for infants and young children due to the risk of adverse effects.
Additionally, these medications may not specifically address the underlying cause of respiratory distress in RSV infection.
Choice D rationale:
Avoiding feeding the child until their breathing improves is not appropriate advice.
Nutrition is essential, especially for infants, and withholding feeding could lead to dehydration and other complications.
It is important to maintain adequate nutrition while managing the respiratory distress caused by RSV infection.
The client is concerned about the risk of dehydration for their child.
The nurse reassures the client by saying which of the following?
Explanation
Choice A rationale:
This is The correct answer because it addresses the client's concern about dehydration.
Infants and young children with RSV infection are at risk of dehydration due to increased respiratory effort, fever, and decreased oral intake.
Encouraging oral fluids or providing intravenous fluids as prescribed helps prevent dehydration, ensuring the child remains hydrated during the illness.
Choice B rationale:
While adequate fluid intake is essential, stating a specific quantity like 8 glasses of water a day is not appropriate for infants and young children.
The fluid requirements vary based on the child's age, weight, and overall health condition.
Providing a specific quantity without proper assessment can be misleading and may not meet the child's individual needs.
Choice C rationale:
Limiting the child's fluid intake to prevent overhydration is not the primary concern in this context.
Dehydration due to increased respiratory effort and decreased oral intake is a more significant concern.
Adequate hydration is crucial in preventing complications associated with dehydration.
Choice D rationale:
Restricting the child to clear liquids only is not appropriate, especially in the context of RSV infection.
While clear liquids are essential, they may not provide adequate nutrition.
Maintaining appropriate oral intake, which includes a variety of fluids and, if possible, nutritionally balanced foods, is important for the child's overall well-being during the illness.
Which of the following instructions should the nurse include? (Select all that apply).
Explanation
Choice A rationale:
Isolating the child from other children or adults with respiratory infections is crucial in preventing the spread of Respiratory Syncytial Virus (RSV).
RSV is highly contagious and spreads through respiratory droplets.
By isolating the infected child, the nurse helps prevent the transmission of the virus to others.
Choice B rationale:
Using contact precautions such as gown and gloves when caring for the child is essential to prevent the spread of RSV.
Direct contact with respiratory secretions can easily lead to transmission.
Wearing protective gear like gowns and gloves creates a barrier, reducing the risk of contamination and spread.
Choice C rationale:
Encouraging frequent hand hygiene is a fundamental preventive measure.
RSV can survive on surfaces for several hours, so regular handwashing with soap and water for at least 20 seconds can help eliminate the virus from hands, reducing the risk of infection.
Choice E rationale:
Avoiding exposure to tobacco smoke is important because smoke irritates the respiratory tract, making individuals more susceptible to respiratory infections like RSV.
Secondhand smoke can also worsen symptoms in infected individuals and increase the severity of the illness.
Choice D rationale:
Allowing siblings to share toys and utensils with the infected child is not recommended.
RSV spreads through respiratory droplets and direct contact with contaminated surfaces.
Sharing toys and utensils can facilitate the transmission of the virus to other children, increasing the risk of infection.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice B rationale:
Offering frequent small feedings of breast milk or formula to maintain nutrition is an appropriate response.
Infants with RSV may experience decreased appetite and difficulty feeding due to respiratory distress.
Providing small, frequent feedings ensures that the infant receives adequate nutrition and hydration despite reduced intake during each feeding session.
Choice A rationale:
Giving the baby aspirin if they develop a fever is not recommended.
Aspirin use in children with viral infections like RSV has been associated with Reye's syndrome, a severe and potentially fatal condition.
Acetaminophen or ibuprofen, if appropriate for the child's age, can be used to manage fever and discomfort.
Choice C rationale:
Keeping the baby in a flat position to promote comfort is not advisable.
Elevating the head of the crib or bassinet slightly can help improve breathing and reduce nasal congestion in infants with respiratory infections, promoting better comfort and easier breathing.
Choice D rationale:
Stopping all feedings if the baby seems to be having trouble breathing is not The correct approach.
Adequate nutrition is crucial for the infant's overall health and recovery.
Instead, the caregiver should seek medical advice if the baby experiences significant difficulty breathing or feeding.
Adjustments in feeding techniques or temporary alternative feeding methods may be recommended under medical supervision.
Epiglottitis
The child presents with a muffled voice and is leaning forward with outstretched arms.
Which statement regarding epiglottitis is accurate?
Explanation
Choice A rationale:
Epiglottitis is most commonly caused by bacterial infections, specifically Haemophilus influenzae type b (Hib) bacteria.
This bacterium can cause inflammation and swelling of the epiglottis, leading to airway obstruction.
Viral infections are not the primary cause of epiglottitis in children.
Choice B rationale:
Epiglottitis primarily affects children, not adolescents and adults.
The peak incidence occurs in children between the ages of 2 and 6 years.
Choice C rationale:
The child adopting a tripod position, leaning forward with outstretched arms, is a classic sign of epiglottitis.
This position helps maximize airway patency and ease breathing.
It is a protective mechanism that children instinctively assume to maintain their airway.
Choice D rationale:
Epiglottitis does not typically result in a loud, high-pitched cry.
The child with epiglottitis is usually quiet and prefers to sit still in a tripod position to maintain airway patency.
The client is drooling saliva and has difficulty swallowing.
Which statement accurately describes the pathophysiology of epiglottitis?
Explanation
Choice A rationale:
Epiglottitis does not cause the epiglottis to shrink and recede into the throat.
Instead, it leads to inflammation and swelling of the epiglottis, causing airway obstruction.
Choice B rationale:
The inflammation in epiglottitis does not primarily affect the vocal cords.
It specifically affects the epiglottis, a flap-like structure located at the base of the tongue, which covers the trachea during swallowing to prevent food or liquid from entering the windpipe.
Choice C rationale:
Epiglottitis leads to increased airway resistance and respiratory distress due to the swelling and obstruction of the airway.
This can result in difficulty swallowing, drooling, and a muffled voice, as seen in the client's symptoms described in the question.
Choice D rationale:
The swelling in epiglottitis is not limited to the vocal cord area.
It involves the epiglottis, which can obstruct the airway and cause respiratory distress.
Which factors should the nurse include in the discussion?
Explanation
Choice A rationale:
Haemophilus influenzae type b (Hib) infection is a significant risk factor for epiglottitis in children.
Hib vaccination has significantly reduced the incidence of epiglottitis caused by this bacterium.
Choice B rationale:
Trauma to the throat or neck is not a common risk factor for epiglottitis.
The primary cause is bacterial infection, especially by Hib bacteria.
Choice C rationale:
Thermal injury from hot liquids can lead to thermal epiglottitis, a rare condition caused by the inhalation of hot steam or liquid, resulting in inflammation and swelling of the epiglottis.
Choice D rationale:
Seasonal factors are not a direct risk factor for epiglottitis.
The condition is primarily caused by bacterial infections and is not significantly influenced by seasonal changes.
Choice E rationale:
Mycoplasma pneumoniae infection is not a common cause of epiglottitis.
Bacterial infections, especially Hib, are the primary culprits in pediatric cases of epiglottitis.
The child is leaning forward and has a muffled voice.
Which statement is true regarding the demographics of epiglottitis?
Explanation
Choice A rationale:
Epiglottitis is not necessarily more common in females than in males.
It can affect both genders equally.
Choice B rationale:
While epiglottitis is more common in children, it primarily affects those between the ages of 2 and 8 years old, not just infants under 1 year old.
Choice C rationale:
There is no significant evidence to suggest that epiglottitis is more prevalent in colder months.
The occurrence of epiglottitis is not strictly related to seasonal changes.
Choice D rationale:
Children between 2 and 8 years old are at higher risk of developing epiglottitis.
This age group is more susceptible due to their smaller airways and less developed immune systems, making them prone to infections like epiglottitis.
What is the most common causative agent of epiglottitis in children?
Explanation
Choice A rationale:
Streptococcus pneumoniae is a common bacterium associated with respiratory infections, but it is not the most common causative agent of epiglottitis in children.
Choice B rationale:
Staphylococcus aureus can cause various infections, but it is not the primary causative agent of epiglottitis in children.
Choice C rationale:
Haemophilus influenzae type b (Hib) is the most common causative agent of epiglottitis in children.
Hib infection can lead to inflammation and swelling of the epiglottis, causing the characteristic symptoms of epiglottitis, including difficulty swallowing and a muffled voice.
Choice D rationale:
Neisseria meningitidis is a bacterium that can cause meningitis and septicemia, but it is not the main causative agent of epiglottitis.
Which clinical manifestation should the nurse prioritize when evaluating the severity of the condition?
Explanation
Choice A rationale:
Difficulty swallowing and throat pain are common symptoms of epiglottitis, but they do not necessarily indicate the severity of the condition.
Choice B rationale:
Feeling anxious and restless may be a sign of distress, but it does not specifically indicate the severity of epiglottitis.
Choice C rationale:
Making a high-pitched sound when breathing (called stridor) is a serious symptom indicating airway obstruction.
While this is concerning, it is not the most critical manifestation in evaluating the severity of epiglottitis.
Choice D rationale:
Cyanosis, characterized by a bluish discoloration of the skin and lips, indicates severe lack of oxygen and is a critical sign in assessing the severity of epiglottitis.
Cyanosis suggests inadequate oxygenation and is indicative of impending respiratory failure, requiring immediate medical intervention.
Which statement made by the child would be most concerning for the nurse?
Explanation
Choice A rationale:
The statement "My throat is really sore.”.
is a common symptom of throat infections, including epiglottitis.
While it is concerning, it is not the most concerning symptom in this case.
Epiglottitis can rapidly progress, leading to respiratory distress, which is a life-threatening condition.
Choice B rationale:
The statement "I can't stop drooling.”.
is a significant concern in a child suspected of having epiglottitis.
Drooling and difficulty managing secretions are hallmark signs of epiglottitis and indicate compromised airway protection.
This symptom suggests that the epiglottis is inflamed and obstructing the airway, potentially leading to respiratory distress and the need for urgent intervention.
Choice C rationale:
The statement "I feel restless and agitated.”.
is a non-specific symptom and may be seen in various illnesses, including infections.
While it indicates the child's discomfort, it does not directly point to the severity of the condition or airway compromise, making it less concerning than the inability to handle secretions.
Choice D rationale:
The statement "I'm having trouble breathing.”.
is the most concerning symptom in a child suspected of having epiglottitis.
Difficulty breathing indicates significant airway obstruction, which can rapidly progress to respiratory failure.
This symptom requires immediate medical attention and intervention to secure the airway and prevent further complications.
Select all the clinical manifestations that are characteristic of epiglottitis.
Explanation
Choice A rationale:
Drooling and inability to handle secretions are characteristic manifestations of epiglottitis.
Inflamed epiglottis impairs the child's ability to swallow and manage saliva, leading to drooling.
This symptom is a key clinical indicator of epiglottitis.
Choice B rationale:
Cough and wheezing are not typical manifestations of epiglottitis.
Epiglottitis primarily affects the upper airway, leading to symptoms such as drooling, stridor, and respiratory distress.
Cough and wheezing are more common in lower respiratory tract infections, such as bronchitis or pneumonia.
Choice C rationale:
Cyanosis and pallor are not specific to epiglottitis and can occur in various respiratory and cardiovascular conditions.
While these symptoms indicate decreased oxygenation, they are not unique to epiglottitis and are not considered characteristic manifestations of this condition.
Choice D rationale:
Muffled voice and stridor are characteristic signs of epiglottitis.
A muffled voice occurs due to the swollen epiglottis obstructing airflow, resulting in a change in the sound of the child's voice.
Stridor is a high-pitched, noisy breathing sound that occurs during inspiration and indicates partial airway obstruction.
Both symptoms are indicative of compromised upper airway in epiglottitis.
Choice E rationale:
Tachypnea (rapid breathing) and tachycardia (rapid heartbeat) are common physiological responses to respiratory distress.
In epiglottitis, the child may exhibit these symptoms due to the body's attempt to compensate for decreased oxygen levels.
These manifestations reflect the severity of the condition and the child's physiological response to airway compromise.
Explanation
Choice A rationale:
Computed tomography (CT) scan provides detailed images of internal structures but is not the preferred imaging test for visualizing a swollen epiglottis.
CT scans are more commonly used for evaluating conditions in other parts of the body, such as the brain or abdomen, and may not provide the necessary detail for assessing the upper airway.
Choice B rationale:
Magnetic resonance imaging (MRI) can produce high-resolution images of soft tissues, but it is not the first choice for visualizing a swollen epiglottis.
MRI scans are time-consuming and may not be readily available in urgent situations.
In cases of suspected epiglottitis, prompt diagnosis and intervention are crucial to prevent respiratory compromise.
Choice C rationale:
Lateral neck radiograph is the preferred imaging test for visualizing a swollen epiglottis.
This X-ray technique allows healthcare providers to assess the size of the epiglottis and its relationship with nearby structures.
A classic finding in epiglottitis on a lateral neck radiograph is a swollen epiglottis, giving a thumbprint sign appearance.
This imaging study can aid in the diagnosis and guide appropriate management.
Choice D rationale:
X-ray of the chest is not the preferred imaging test for evaluating epiglottitis.
While a chest X-ray can provide information about the lungs and surrounding structures, it does not offer the necessary detail to visualize the upper airway, including the epiglottis.
Lateral neck radiograph is specifically tailored to assess the structures in the throat region and is the imaging modality of choice in suspected cases of epiglottitis.
Explanation
Choice A rationale:
Allergies to foods are not directly related to epiglottitis.
While it's essential information for a general health assessment, it doesn't provide specific insights into the condition.
Choice B rationale:
Immunization history is crucial in the assessment of a child with suspected epiglottitis.
Haemophilus influenzae type b (Hib) vaccination is highly effective in preventing epiglottitis caused by Hib bacteria.
Knowing the child's immunization status helps the nurse assess the likelihood of Hib infection.
Choice C rationale:
Recent travel destinations are not directly relevant to epiglottitis.
This information is more pertinent when assessing the risk of diseases like malaria or dengue fever, which are region-specific.
Choice D rationale:
Current hobbies and interests are not pertinent to the assessment of epiglottitis.
This information is important in a broader context for understanding the child's lifestyle but does not provide relevant data regarding the condition.
Which nursing intervention should the nurse prioritize to maintain a patent airway?
Explanation
Choice A rationale:
Administering antibiotics intravenously is important in treating the infection, but it doesn't directly address maintaining a patent airway.
The priority in epiglottitis is to ensure an open airway to prevent respiratory distress.
Choice B rationale:
Providing humidified air or cool mist therapy helps moisten the airway, making it easier for the child to breathe.
This intervention can provide immediate relief and aid in maintaining a patent airway, which is crucial in epiglottitis.
Choice C rationale:
Administering corticosteroids intravenously can help reduce inflammation, but it might not be the primary intervention to maintain a patent airway.
Humidified air therapy directly addresses airway moisture, which is essential in epiglottitis management.
Choice D rationale:
Administering analgesics and antipyretics can address pain and fever associated with epiglottitis but does not directly contribute to maintaining a patent airway.
While these medications can improve the child's comfort, they are not the priority in this situation.
What information should the nurse include in the education?
Explanation
Choice A rationale:
The importance of oral medications to relieve symptoms is relevant, but it doesn't specifically prevent epiglottitis.
Preventive measures like vaccination are more crucial in avoiding the condition.
Choice B rationale:
Educating the child and their family about the signs and symptoms of epiglottitis is essential for early recognition and prompt medical intervention.
Understanding the symptoms can lead to quicker medical attention, which is vital in managing epiglottitis effectively.
Choice C rationale:
Avoiding complete immunization against Hib is not a recommended practice.
Hib vaccination significantly reduces the risk of epiglottitis caused by Hib bacteria.
Encouraging complete immunization is a key preventive measure against the disease.
Choice D rationale:
Using nebulized medications for treatment might be a part of the management plan if the child already has epiglottitis, but it's not a preventive measure.
Prevention focuses on vaccination and awareness of symptoms, making choice D less relevant in the context of prevention.
Select all appropriate interventions for supportive care.
Explanation
Choice A rationale:
Administering antibiotics intravenously as prescribed is a crucial intervention in the management of epiglottitis.
Epiglottitis is commonly caused by bacterial infections, and intravenous antibiotics are essential to target the underlying infection and prevent its spread.
The choice of antibiotic should be based on the specific causative organism and local antibiotic resistance patterns.
Choice B rationale:
Administering corticosteroids intravenously as prescribed is another important intervention in the supportive care of epiglottitis.
Corticosteroids help reduce airway inflammation, which is a significant concern in epiglottitis.
By decreasing inflammation, corticosteroids can alleviate respiratory distress and improve the patient's breathing.
Choice C rationale:
Providing hydration and nutrition by intravenous fluids is necessary in the management of epiglottitis, especially if the child is having difficulty swallowing or breathing.
Intravenous fluids ensure that the child receives adequate hydration and nutrition while minimizing the risk of aspiration, which can worsen the airway obstruction.
Choice E rationale:
Providing humidified air or cool mist therapy to moisten the airway is a supportive measure that can help ease breathing difficulties in children with epiglottitis.
Humidified air or cool mist therapy can soothe the inflamed airway, making it easier for the child to breathe.
It is essential to maintain a moist environment to prevent further irritation and discomfort.
Choice D rationale:
Educating the child and family about the prevention of epiglottitis is important for overall health awareness, but it is not a direct supportive intervention for a child already diagnosed with the condition.
While prevention strategies, such as timely vaccinations and good hygiene, are crucial, they do not constitute immediate supportive care for a child with active epiglottitis.
Which statement about airway management is correct?
Explanation
Choice A rationale:
Tracheostomy may be necessary in severe cases of epiglottitis where the airway obstruction is life-threatening and cannot be managed with other interventions.
In such cases, creating a surgical airway via tracheostomy can provide a more stable and secure airway, ensuring adequate oxygenation.
However, this option is typically considered when other measures, such as intubation, have failed or are not feasible due to the severity of the obstruction.
Choice B rationale:
Intubation may be required in cases where the airway obstruction is significant, and the child is unable to maintain oxygenation and ventilation adequately.
Intubation allows for mechanical ventilation, ensuring a patent airway and adequate oxygen supply.
However, it is not always the only option and may depend on the severity of the condition and the response to other interventions.
Choice C rationale:
Tracheostomy is more invasive than intubation.
While tracheostomy is a surgical procedure that involves creating an opening in the trachea, intubation involves inserting a tube through the mouth or nose into the trachea.
Tracheostomy is considered more invasive because it requires a surgical incision and the placement of a permanent or temporary tracheostomy tube.
Choice D rationale:
Intubation is not always the first choice for airway management in epiglottitis.
The choice of airway management (intubation, tracheostomy, or other interventions) depends on the severity of the airway obstruction, the child's clinical condition, and the healthcare provider's assessment.
Intubation may be chosen if the obstruction is significant and the child cannot maintain adequate oxygenation and ventilation.
What should the nurse monitor for as potential side effects of corticosteroid therapy?
Explanation
Choice A rationale:
The nurse should monitor for signs of adrenal insufficiency and hyperglycemia as potential side effects of corticosteroid therapy.
Corticosteroids can suppress the adrenal glands, leading to adrenal insufficiency, which can manifest as weakness, fatigue, low blood pressure, and abdominal pain.
Hyperglycemia (elevated blood sugar levels) is a common side effect of corticosteroids and can worsen diabetes or predispose non-diabetic individuals to high blood sugar levels.
Choice B rationale:
Decreased oxygen saturation levels are not a common side effect of corticosteroid therapy.
Corticosteroids help reduce airway inflammation, which can actually improve oxygenation in conditions like epiglottitis by reducing airway obstruction and respiratory distress.
Choice C rationale:
Allergic reactions to corticosteroids are possible, but they are relatively rare.
Symptoms of an allergic reaction can include rash, itching, swelling, severe dizziness, or difficulty breathing.
While allergic reactions are a concern with any medication, they are not the primary side effect that nurses should monitor for when administering corticosteroids.
Choice D rationale:
Increased sensitivity to antibiotics is not a known side effect of corticosteroid therapy.
Corticosteroids work by suppressing the immune response and reducing inflammation, but they do not affect the body's sensitivity to antibiotics.
Antibiotic effectiveness is determined by factors such as the specific antibiotic used, the type of bacteria causing the infection, and antibiotic resistance patterns.
Otitis media
Which of the following statements accurately describes the primary cause of otitis media as per the information provided in the text?
Explanation
Choice A rationale:
Otitis media is not mainly caused by the presence of bacteria in the middle ear.
While bacterial infections can contribute to otitis media, it is not the primary cause as per the information provided in the text.
Choice B rationale:
Eustachian tube dysfunction is indeed the primary cause of otitis media.
The Eustachian tube connects the middle ear to the back of the throat.
When this tube is not functioning correctly, it can lead to the accumulation of fluid in the middle ear, providing an ideal environment for bacterial growth and infection, which results in otitis media.
Choice C rationale:
Otitis media is not primarily caused by allergic reactions.
While allergies can lead to Eustachian tube dysfunction, it is not the main cause of otitis media.
Choice D rationale:
The statement that "The risk factors for otitis media are not well-defined" is incorrect.
The risk factors for otitis media are well-established, including factors like age (more common in children), exposure to smoke, attending daycare, and Eustachian tube abnormalities.
Which statement accurately describes one of the risk factors mentioned in the text for developing otitis media?
Explanation
Choice A rationale:
Otitis media is more common in young children, especially those between 6 months and 3 years of age.
It is not more common in children over 6 years of age.
Choice B rationale:
Seasonal changes can indeed impact the frequency of otitis media.
During cold seasons, upper respiratory infections are more common, which can lead to otitis media.
Choice C rationale:
Noncompliance with vaccinations is associated with otitis media.
Proper vaccination can prevent certain infections that may lead to otitis media.
Choice D rationale:
Passive smoking can increase the risk of otitis media.
Exposure to secondhand smoke can cause irritation and inflammation in the Eustachian tubes, making individuals, especially children, more susceptible to ear infections.
Which of the following statements regarding the pathophysiology of otitis media, as described in the text, are correct? (Choose three.).
Explanation
Choice A rationale:
Eustachian tube obstruction does lead to decreased pressure in the middle ear.
When the Eustachian tube is blocked or not functioning properly, it can create a vacuum in the middle ear, leading to negative pressure, which can pull fluid into the middle ear space.
Choice B rationale:
Effusion is indeed the fluid that fills the normally air-filled middle ear cavity in otitis media.
This fluid can accumulate due to Eustachian tube dysfunction or inflammation, leading to the characteristic symptoms of otitis media.
Choice C rationale:
Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis are indeed common pathogens causing otitis media.
These bacteria can infect the middle ear and lead to the inflammation and fluid accumulation characteristic of otitis media.
Choice D rationale:
Otitis media does not result from the inflammation of the outer ear.
Otitis media specifically refers to inflammation and infection of the middle ear.
Choice E rationale:
The statement about the eardrum becoming red, swollen, and bulging due to the absence of effusion is incorrect.
The presence of effusion behind the eardrum can cause it to appear red, swollen, and bulging, not the absence of effusion.
Which of the following complications is mentioned in the text as a potential consequence of otitis media?
Explanation
Choice A rationale:
Migraines and tension headaches are not mentioned as complications of otitis media in the text.
Otitis media primarily affects the middle ear and is associated with complications related to the ear and hearing.
Choice B rationale:
Chronic back pain and joint issues are unrelated to otitis media.
The complications of otitis media are primarily associated with the ear, hearing, and speech.
Choice C rationale:
Speech delay and hearing loss are mentioned as potential consequences of otitis media.
Otitis media can lead to hearing impairment, especially in children, which can subsequently cause speech delays.
This complication occurs due to the accumulation of fluid in the middle ear, which impairs the normal conduction of sound.
Choice D rationale:
Skin rashes and allergic reactions are not mentioned as consequences of otitis media.
Complications of otitis media primarily revolve around the auditory system and related functions.
Which of the following factors mentioned in the text as risk factors for otitis media is most closely associated with an increased exposure to infectious agents?
Explanation
Choice A rationale:
Age alone is not a risk factor for otitis media.
However, certain age groups, such as young children, are more susceptible to ear infections due to their developing immune systems and shorter Eustachian tubes.
Choice B rationale:
Season is not a direct risk factor for otitis media.
While certain respiratory infections might be more common in specific seasons, otitis media itself is not strongly influenced by seasonal changes.
Choice C rationale:
Allergies can contribute to ear infections, but they are not the most closely associated risk factor mentioned in the context.
Allergies can lead to inflammation and fluid buildup in the middle ear, making individuals more prone to infections.
However, in the given options, day care attendance is a more specific risk factor related to exposure to infectious agents.
Choice D rationale:
Day care attendance is closely associated with an increased exposure to infectious agents, including the bacteria that can cause otitis media.
Children in day care settings are in close contact with others, facilitating the spread of infections.
Which clinical manifestations are commonly associated with AOM? Select The correct statements from the following options:.
Explanation
and "Balance problems result from serous fluid in the ear canal.”.
Choice A rationale:
The statement that "The ear pain is usually mild and intermittent" is incorrect.
Ear pain associated with acute otitis media (AOM) is often severe and continuous, causing discomfort and distress to the affected individual.
Choice B rationale:
Irritability, manifested as crying or fussiness, is a common symptom of AOM.
Ear pain and pressure can cause considerable discomfort, leading to irritability and changes in behavior, especially in children.
Choice C rationale:
The statement "Hearing loss in AOM is typically severe" is incorrect.
While hearing loss can occur in AOM, it is not always severe.
The degree of hearing impairment can vary based on the severity of the infection and the presence of fluid in the middle ear.
Choice D rationale:
Balance problems resulting from serous fluid in the ear canal are correct.
Serous fluid buildup in the middle ear can affect the balance mechanisms, leading to balance issues and dizziness, especially in children.
This fluid buildup can cause pressure changes, impacting the normal functioning of the inner ear.
Choice E rationale:
Otorrhea, which refers to discharge from the ear, is not a common symptom of AOM.
Otorrhea is more commonly associated with chronic ear infections or other ear conditions but not necessarily with acute otitis media.
Which symptoms should the nurse inquire about in the child's history to assess for otitis media? Choose the appropriate options from the following:.
Explanation
Choice A rationale:
A history of frequent episodes of otitis media is important to inquire about because recurrent ear infections are a common sign of otitis media.
Children who have experienced multiple episodes of otitis media are at a higher risk for developing the condition again.
This information helps the nurse assess the child's susceptibility to ear infections and guides further evaluation and treatment decisions.
Choice B rationale:
Previous upper respiratory tract infections are relevant to the child's overall health but are not specific symptoms of otitis media.
Otitis media can be a complication of upper respiratory infections, but the presence of previous infections alone does not confirm otitis media.
Choice C rationale:
Exposure to loud noise as a daily occurrence is not a symptom of otitis media.
Otitis media is an inflammation of the middle ear, commonly caused by bacterial or viral infections, and is not related to exposure to loud noises.
Choice D rationale:
A feeling of fullness or pressure in the ear can be associated with otitis media, but it is a nonspecific symptom that can occur in various ear conditions.
While it may raise suspicion, it is not a definitive sign of otitis media.
Choice E rationale:
Immunization history of the child is important for the child's overall health, but it is not a specific symptom of otitis media.
Immunizations do not directly influence the development or presence of otitis media.
Which findings indicate acute otitis media (AOM) based on the examination of the tympanic membrane? Select all that apply:.
Explanation
Choice A rationale:
Redness of the tympanic membrane can indicate inflammation, which is a common sign of acute otitis media (AOM).
Inflammation causes increased blood flow to the area, leading to redness and often pain.
Choice B rationale:
Bulging of the tympanic membrane occurs when there is increased pressure behind the eardrum, often due to fluid accumulation.
In the context of acute otitis media, this bulging is caused by the buildup of pus or other fluids in the middle ear.
Choice C rationale:
Purulence (pus) observed in the ear canal is a definitive sign of acute otitis media.
The presence of pus indicates an active infection within the middle ear.
Choice D rationale:
Orange discoloration of the tympanic membrane is not a typical finding in acute otitis media.
The color change could be due to various factors but is not specific to this condition.
Choice E rationale:
Decreased mobility of the tympanic membrane can occur due to the accumulation of fluid in the middle ear, leading to impaired movement.
This decreased mobility is often observed in acute otitis media and contributes to the diagnosis.
Which assessment findings are more likely associated with otitis media with effusion (OME)? Select The correct statements:.
Explanation
Choice A rationale:
The child reporting severe, throbbing ear pain is more indicative of acute otitis media (AOM) rather than otitis media with effusion (OME).
Severe pain is a common symptom of an active infection in the middle ear.
Choice B rationale:
Pus observed draining from the ear canal is a sign of acute otitis media (AOM).
Drainage indicates a ruptured eardrum, allowing the infected fluid to escape, relieving pressure and pain.
Choice C rationale:
Hearing loss that is mild to moderate is characteristic of otitis media with effusion (OME).
OME occurs when fluid remains trapped in the middle ear after the infection has resolved.
The presence of fluid can affect hearing, especially at lower frequencies, leading to mild to moderate hearing loss.
Choice D rationale:
The eardrum appearing red and bulging is a typical finding in acute otitis media (AOM), not otitis media with effusion (OME).
In AOM, the eardrum becomes red due to inflammation and bulges due to increased pressure from fluid buildup.
What clinical manifestations are indicative of hearing loss in children with otitis media? Choose the appropriate options:.
Explanation
"Difficulty locating sounds or following directions.”.
Choice A rationale:
Difficulty locating sounds or following directions is a common sign of hearing loss in children with otitis media.
Hearing loss can affect a child's ability to hear and process sounds, leading to problems in locating the source of sounds or following instructions.
This manifestation is indicative of conductive hearing loss, which is commonly associated with otitis media.
Children may have trouble understanding speech, especially in noisy environments.
Choice B rationale:
Ringing or buzzing sound in the ear, also known as tinnitus, is not a typical manifestation of hearing loss in otitis media.
Tinnitus can occur due to various reasons, but it is not a specific indicator of hearing loss associated with otitis media.
Choice C rationale:
Severe, pulsating ear pain is a symptom of acute otitis media, but it is not directly indicative of hearing loss.
Ear pain is caused by the buildup of fluid and pressure in the middle ear, leading to discomfort and pain.
However, it does not necessarily mean the child has hearing loss.
Choice D rationale:
Vertigo and nystagmus are symptoms associated with inner ear disorders, such as vestibular labyrinthitis or Meniere's disease, but they are not typical manifestations of hearing loss in otitis media.
These symptoms involve problems with balance and coordination and are not directly related to hearing loss.
Choice E rationale:
Inconsolable crying due to discomfort is a general symptom that can occur in children with various illnesses, including otitis media.
While it indicates the child is in pain or discomfort, it is not a specific sign of hearing loss.
Children may cry due to ear pain, but this symptom alone does not confirm hearing loss.
Which aspect should the nurse evaluate regarding pain?
Explanation
"The pain gets worse when I lie down.”.
Choice A rationale:
"I feel a sharp pain in my ear sometimes.”.
This statement suggests intermittent ear pain, which can occur in otitis media when there is a sudden change in pressure in the middle ear.
It is a possible symptom, but it is not specific to otitis media as other ear conditions can also cause sharp ear pain.
Choice B rationale:
"My ear hurts all the time.”.
Constant ear pain is a common symptom of acute otitis media.
The pain is caused by inflammation and pressure in the middle ear.
This symptom is indicative of otitis media but does not provide specific information about the pain worsening when lying down, which is a crucial aspect to assess.
Choice C rationale:
"The pain gets worse when I lie down.”.
This statement is indicative of otitis media.
When the child lies down, the fluid in the middle ear can put additional pressure on the eardrum, causing increased pain.
This worsening of pain in specific positions helps differentiate otitis media from other ear conditions.
Choice D rationale:
"I have no pain in my ear.”.
Absence of ear pain is not consistent with otitis media.
Otitis media is characterized by ear pain, especially in acute cases when there is inflammation and pressure in the middle ear.
Lack of ear pain suggests the absence of this condition.
Explanation
"I have a high fever, and I'm shivering.”.
Choice A rationale:
"I have a high fever, and I'm shivering.”.
A high fever with chills indicates a systemic response to infection, which can be seen in severe cases of otitis media.
Fever is a common symptom and can indicate a spreading or worsening infection.
Shivering (rigors) often accompanies a high fever and suggests a significant inflammatory response in the body.
Choice B rationale:
"I feel warm, but I'm not sweating.”.
Feeling warm without sweating may indicate a low-grade fever, which can occur in various infections, including otitis media.
However, this statement does not provide information about the severity of the fever or the child's overall condition.
Choice C rationale:
"I'm sweating a lot, and I'm very tired.”.
Sweating and fatigue can be symptoms of various illnesses, including infections.
Sweating, especially if accompanied by other symptoms like fever, can indicate a fever breaking, but it does not specifically provide information about the severity of the infection or its relationship to otitis media.
Choice D rationale:
"I don't have a fever at all.”.
The absence of fever is not consistent with acute otitis media.
Fever is a common systemic response to infection and inflammation.
In the context of otitis media, the presence of fever indicates a more severe or active infection.
Select all the appropriate assessment findings the nurse should consider.
Explanation
Choice A rationale:
The nurse should consider the results of the whisper test when assessing a child with otitis media.
A whisper test helps to assess hearing acuity and can indicate if there is a hearing impairment in the child.
If the child does not respond appropriately to the whisper test, it could suggest hearing problems related to otitis media.
Choice B rationale:
Assessing the child's response to sounds is crucial in evaluating their hearing abilities.
Children with otitis media may have difficulty hearing soft sounds or may not respond appropriately to auditory stimuli.
This assessment finding can provide valuable information about the child's hearing status and potential issues related to otitis media.
Choice D rationale:
Considering the child's history of hearing problems is essential in understanding the overall context of their ear health.
A history of recurrent ear infections or hearing difficulties can indicate a chronic issue, such as otitis media, which the nurse needs to address and monitor closely.
Past hearing problems can influence the current assessment and guide appropriate interventions.
Choice C rationale:
Temperature measurement is not directly related to assessing a child with otitis media.
Otitis media primarily affects the middle ear, leading to symptoms such as ear pain, hearing loss, and sometimes drainage from the ear.
Monitoring the child's temperature is important for assessing fever, which could be a sign of infection, but it is not specific to otitis media assessment.
Choice E rationale:
Lip reading skills are not typically assessed in the context of otitis media.
Otitis media primarily affects the auditory system, leading to hearing difficulties.
While lip reading skills might be relevant for individuals with profound hearing loss, it is not a standard assessment for children with otitis media, especially during a comprehensive assessment.
Explanation
Choice A rationale:
The statement "I sometimes feel dizzy and unsteady" indicates balance problems in the child.
Balance issues can occur in individuals with otitis media due to disturbances in the inner ear, affecting the vestibular system responsible for balance and spatial orientation.
Dizziness and unsteadiness are common symptoms associated with inner ear problems, including otitis media.
Therefore, this statement should be evaluated further to assess the child's balance and related concerns.
Choice B rationale:
The statement "My ear feels heavy" is related to a sensation in the ear and does not specifically indicate balance problems.
While otitis media can cause ear discomfort and pain, the sensation of heaviness alone does not provide information about the child's balance issues.
It is important to differentiate between symptoms related to ear discomfort and those indicating problems with balance.
Choice C rationale:
The statement "I have trouble swallowing" is not directly related to balance problems associated with otitis media.
Swallowing difficulties are typically not a primary symptom of otitis media.
This statement might indicate issues with the throat or esophagus but does not provide relevant information about the child's balance concerns.
Choice D rationale:
The statement "I can balance perfectly" suggests that the child does not experience balance problems.
This statement contradicts the typical symptoms associated with otitis media, which can include dizziness, unsteadiness, and balance issues.
If the child can balance perfectly, it indicates that their vestibular system, responsible for balance, is functioning normally and is not affected by otitis media.
Explanation
Choice A rationale:
Watchful waiting is a management approach for mild cases of otitis media, especially if the infection is suspected to be viral and not bacterial.
It involves monitoring the child's symptoms without immediate antibiotic treatment.
Watchful waiting allows healthcare providers to assess the progression of symptoms before deciding on further interventions, such as prescribing antibiotics.
Therefore, this choice is a valid way to manage otitis media in children.
Choice B rationale:
Antibiotics or antivirals are commonly prescribed to manage otitis media, especially when the infection is bacterial.
Antibiotics help treat the bacterial infection and reduce inflammation in the middle ear.
Antivirals may be considered if the infection is caused by a virus.
Prescribing appropriate medications is a standard and effective way to manage otitis media in children, helping to alleviate symptoms and prevent complications.
Choice C rationale:
Myringotomy is a surgical procedure in which a small incision is made in the eardrum to drain fluid from the middle ear.
This procedure is often performed when there is persistent fluid accumulation, recurrent infections, or hearing loss due to otitis media.
Myringotomy helps relieve pressure in the middle ear, promote drainage, and improve hearing.
While it is a medical intervention, it is a valid way to manage otitis media, especially in cases where other treatments have not been effective.
Choice D rationale:
Administration of over-the-counter pain relievers, such as acetaminophen or ibuprofen, is a common approach to managing pain and discomfort associated with otitis media.
These medications can help reduce ear pain and fever, providing relief to the child while the infection resolves.
While pain relievers do not directly treat the underlying infection, they play a supportive role in managing symptoms and improving the child's comfort level during the illness.
Gastroenteritis in Children:
The nurse asks the child's parent, "Have you noticed any changes in your child's bowel movements recently?" What would be an expected statement from the parent?
Explanation
Choice A rationale:
The parent's statement, "Yes, my child has had frequent diarrhea," is expected in a child with gastroenteritis caused by a viral infection.
Viral gastroenteritis often presents with symptoms like diarrhea, vomiting, stomach pain, and sometimes fever.
Frequent, watery diarrhea is a common characteristic of viral gastroenteritis in children.
The nurse should be aware of this symptom to provide appropriate care, including rehydration and monitoring for signs of dehydration.
Choice B rationale:
The statement, "No, my child's bowel movements are normal," would not be an expected response from the parent of a child with gastroenteritis.
As mentioned earlier, viral gastroenteritis typically causes changes in bowel habits, leading to frequent diarrhea.
Choice C rationale:
The statement, "My child has been constipated," is not consistent with the symptoms of gastroenteritis.
Constipation involves infrequent and difficult bowel movements, which are not typical symptoms of viral gastroenteritis.
Choice D rationale:
The statement, "My child has been vomiting a lot," is a symptom of gastroenteritis.
However, the question specifically asks about changes in bowel movements.
While vomiting is a common symptom of gastroenteritis, the focus here is on bowel movements, making choice A The correct answer.
The client reports, "My child has been vomiting and has stomach pain.”.
What is a potential statement the nurse might hear during the assessment?
Explanation
Choice D rationale:
The statement, "My child has had diarrhea for a few days," is a potential statement the nurse might hear during the assessment of a child with gastroenteritis.
Diarrhea is a common symptom of viral gastroenteritis and can lead to dehydration if not properly managed.
The nurse should assess the duration, frequency, and characteristics of the diarrhea to determine the severity of the condition and plan appropriate interventions.
Choice A rationale:
The statement, "My child has been eating and drinking normally," does not align with the symptoms described by the client.
Children with gastroenteritis often have decreased appetite and may not tolerate normal food and fluid intake due to nausea, vomiting, and diarrhea.
Choice B rationale:
The statement, "My child's bowel movements have been regular," contradicts the reported symptoms of diarrhea and stomach pain.
Regular bowel movements are not expected in a child with gastroenteritis, which commonly causes loose or watery stools.
Choice C rationale:
The statement, "My child hasn't had any abdominal discomfort," is not consistent with the typical symptoms of gastroenteritis.
Abdominal discomfort, cramping, and pain are common complaints in individuals with gastroenteritis, especially during episodes of diarrhea.
Select all that apply to effective prevention strategies.
Explanation
Choice A rationale:
Ensuring proper handwashing before meals and after using the toilet is an effective prevention strategy for gastroenteritis.
Proper hand hygiene helps prevent the spread of viral and bacterial infections, including those causing gastroenteritis.
Choice D rationale:
Advising parents to keep their child away from sick individuals is another effective prevention strategy.
Gastroenteritis is highly contagious and can spread through close contact with infected individuals.
Avoiding contact with sick individuals reduces the risk of exposure to the viruses or bacteria causing gastroenteritis.
Choice E rationale:
Recommending vaccination against common viral causes of gastroenteritis is a preventive measure.
Vaccines are available for certain viruses, such as rotavirus, which is a common cause of gastroenteritis in children.
Immunization helps protect children from severe cases of gastroenteritis and reduces the overall prevalence of the disease in the community.
Choice B rationale:
Encouraging the sharing of utensils among children to build immunity is not a recommended strategy for preventing gastroenteritis.
Sharing utensils can increase the risk of spreading infections, including gastroenteritis.
Proper hygiene practices, such as using separate utensils and avoiding sharing drinks and food, are essential to prevent the transmission of the disease.
Choice C rationale:
Promoting the consumption of untreated stream water during outdoor activities is not a safe practice.
Untreated water sources, including streams, can contain harmful bacteria, parasites, and other pathogens that can cause gastroenteritis and other waterborne illnesses.
Encouraging children to drink clean, treated water from safe sources is important to prevent gastrointestinal infections.
Explanation
Choice A rationale:
Gastroenteritis does not cause the intestines to absorb excess fluids.
In fact, it does the opposite by decreasing absorption and increasing fluid secretion, leading to diarrhea.
Choice B rationale:
This statement is incorrect.
Gastroenteritis does not inhibit fluid secretion; instead, it damages the intestines, causing increased fluid secretion and decreased absorption, which results in diarrhea.
Choice C rationale:
The correct answer.
Gastroenteritis, especially the infectious type, damages the intestines.
The infection leads to decreased absorption of fluids and increased fluid secretion, causing diarrhea.
Choice D rationale:
This statement is inaccurate.
Gastroenteritis does impact fluid balance in the intestines.
It disrupts the normal functioning of the intestines, leading to fluid imbalances.
Explanation
Choice A rationale:
Fungal infections are not a common cause of gastroenteritis in children.
Viral, bacterial, and parasitic infections are the primary culprits.
Choice B rationale:
Exposure to cold weather is not a direct cause of gastroenteritis.
The condition is mainly caused by infections, as mentioned in choice C.
Choice C rationale:
The correct answer.
Gastroenteritis in children is commonly caused by viral, bacterial, and parasitic infections.
These microorganisms can lead to inflammation of the gastrointestinal tract, resulting in symptoms like diarrhea and vomiting.
Choice D rationale:
Gastroenteritis is generally not caused by food allergies in children.
While food allergies can cause gastrointestinal symptoms, the typical presentation of gastroenteritis involves infectious agents rather than allergic reactions.
The child presents with diarrhea, vomiting, abdominal pain, and fever.
Which diagnostic test may be performed to identify the causative organism in bacterial infections related to gastroenteritis?
Explanation
Choice A rationale:
The correct answer.
Stool culture and sensitivity testing are essential diagnostic tests for identifying the causative organism in bacterial infections related to gastroenteritis.
This test helps determine the specific bacteria causing the infection and their susceptibility to antibiotics, guiding appropriate treatment.
Choice B rationale:
Blood tests to assess kidney function are not specific to diagnosing gastroenteritis or its causative organism.
These tests are more relevant in assessing kidney-related issues.
Choice C rationale:
Imaging studies such as abdominal ultrasound are not the primary diagnostic tests for identifying the causative organism in gastroenteritis.
These studies are used for visualizing the internal structures of the abdomen and may not provide specific information about the infectious agent.
Choice D rationale:
Viral testing using polymerase chain reaction (PCR) is valuable for detecting viruses, but it is not the first-line diagnostic test for bacterial infections related to gastroenteritis.
Stool culture and sensitivity testing are more appropriate in this context.
The client asks, "What should I look for to assess my child's hydration status?" What should the nurse advise the client to monitor?
Explanation
Choice A rationale:
The child's fever is not the most reliable indicator of hydration status.
While fever can indicate an infection, it does not provide direct information about the child's hydration level.
Choice B rationale:
The frequency of stools is relevant to gastroenteritis but does not provide a comprehensive assessment of hydration status.
Dehydration can occur even if the child is having frequent stools.
Choice C rationale:
The child's abdominal pain level is important but does not directly assess hydration status.
Abdominal pain is a symptom of gastroenteritis, but it does not provide specific information about the child's hydration level.
Choice D rationale:
Skin turgor, mucous membranes, and urine output are crucial indicators of hydration status.
Skin turgor refers to the skin's elasticity and how quickly it returns to normal after being pinched.
Poor skin turgor can indicate dehydration.
Mucous membranes, such as the inside of the mouth, should be moist.
Dry mucous membranes can suggest dehydration.
Additionally, monitoring urine output is essential.
A decreased urine output or dark-colored urine can indicate dehydration.
These parameters provide a comprehensive assessment of the child's hydration status and guide appropriate interventions.
A nurse is conducting a nursing assessment of a child with suspected gastroenteritis.
What should the nurse include in the assessment? (Select all that apply).
Explanation
Choice A rationale:
The child's weight and height are essential for assessing growth and nutritional status.
Changes in weight and height can indicate malnutrition or other health issues.
Choice B rationale:
Documentation of stool characteristics is crucial in assessing gastrointestinal issues such as gastroenteritis.
Characteristics like color, consistency, and presence of blood or mucus can provide important diagnostic information.
Choice C rationale:
Assessment of skin turgor is relevant for hydration status but is not specific to gastroenteritis.
While decreased skin turgor can indicate dehydration, other factors like mucous membranes and urine output are more specific indicators for gastroenteritis-related dehydration.
Choice D rationale:
Monitoring the child's temperature is essential to identify fever, which is a common symptom of gastroenteritis and can indicate infection or inflammation.
Choice E rationale:
Evaluating the child's overall appearance and behavior is crucial.
Lethargy, irritability, or other changes in behavior can indicate dehydration or worsening illness.
Additionally, observing the child's general appearance can provide valuable information about their overall health status.
Explanation
Choice A rationale:
"In gastroenteritis, diarrhea is often bloody and mucus-filled.”.
This statement is incorrect.
While gastroenteritis can cause loose stools, they are usually watery rather than bloody or mucus-filled.
Bloody or mucus-filled stools might indicate other gastrointestinal issues that need further evaluation.
Choice B rationale:
"Diarrhea in gastroenteritis is typically chronic and persistent.”.
This statement is incorrect.
Gastroenteritis often presents with acute symptoms, including sudden onset of diarrhea, vomiting, and abdominal pain.
Chronic and persistent diarrhea might suggest other chronic gastrointestinal conditions but is not characteristic of gastroenteritis.
Choice C rationale:
"Gastroenteritis usually presents with constipation.”.
This statement is incorrect.
Gastroenteritis typically presents with diarrhea, not constipation.
Constipation is the opposite of diarrhea and is not a symptom associated with gastroenteritis.
Choice D rationale:
"The diarrhea in gastroenteritis is usually watery.”.
This statement is correct.
Watery diarrhea is a hallmark symptom of gastroenteritis.
It results from inflammation of the gastrointestinal tract, leading to increased water content in the stools.
This type of diarrhea can quickly lead to dehydration if not managed promptly.
The nurse needs to assess the child's pain level.
Which pain assessment method should the nurse use for this evaluation?
Explanation
Choice A rationale:
The Pediatric Assessment Tool is a broad term and doesn't specify a particular pain assessment method.
It's not the best choice in this context.
Choice B rationale:
The Wong-Baker FACES Pain Rating Scale is a widely used and validated tool for assessing pain in children, especially those who might have difficulty expressing their pain verbally.
It uses facial expressions as indicators of pain levels, making it particularly useful for young children.
Choice C rationale:
The Numeric Pain Rating Scale is a numerical scale from 0 to 10 where patients rate their pain intensity.
While it can be used for children, the Wong-Baker FACES Pain Rating Scale is more child-friendly and visually oriented.
Choice D rationale:
The Visual Analog Scale (VAS) is a continuous scale used for pain assessment.
It's more suitable for adults and older children, as younger children might find it challenging to understand and use effectively.
The child's parent asks, "Why is my child receiving oral rehydration therapy?" Which response by the nurse is appropriate?
Explanation
Choice A rationale:
Oral rehydration therapy (ORT) is a key treatment for gastroenteritis.
It helps to replace lost fluids and electrolytes due to vomiting and diarrhea, preventing dehydration.
The primary goal of ORT is to control these symptoms and maintain hydration.
Choice B rationale:
While ORT does treat the consequences of the infection (dehydration), it doesn't directly treat the underlying cause, which is often a viral or bacterial infection.
Choice C rationale:
ORT does prevent dehydration, which is a complication of gastroenteritis, but it doesn't specifically prevent the spread of the infection to others.
Choice D rationale:
ORT can often prevent the need for hospitalization by effectively managing dehydration on an outpatient basis.
However, its primary purpose is to prevent dehydration, not to eliminate the need for hospitalization in all cases.
The client states, "I can't keep anything down; I'm so thirsty.”.
How should the nurse respond?
Explanation
Choice A rationale:
Prescribing an antiemetic might be necessary in some cases, but the immediate concern is to manage the client's thirst and fluid intake.
Trying to control vomiting is secondary to ensuring hydration.
Choice B rationale:
Avoiding any fluid intake can lead to dehydration, especially if the client is experiencing severe vomiting.
This option is not appropriate and can worsen the client's condition.
Choice C rationale:
Starting with a clear liquid diet is a standard approach in managing gastroenteritis.
Clear liquids are easier to digest and can help assess the client's ability to tolerate oral intake.
If the client can tolerate clear liquids without vomiting, it indicates a positive step toward hydration and nutritional intake.
Choice D rationale:
Drinking as much water as possible might not be appropriate, especially if the client is vomiting severely.
Introducing clear liquids first allows for a gradual reintroduction of fluids and assesses the client's tolerance before advancing to more complex diets.
Select all the appropriate measures to prevent the spread of infection to others:.
Explanation
Choice A rationale:
Instructing the parents to teach the child to cover their mouth and nose when coughing or sneezing is crucial in preventing the spread of infections, especially in cases of gastroenteritis.
This measure helps in containing respiratory droplets that might carry the virus or bacteria causing the illness.
Choice B rationale:
Isolating the child in a separate room away from other family members is essential to prevent the transmission of the disease to others in the household.
Gastroenteritis spreads through contaminated food, water, or contact with an infected person.
By isolating the child, the risk of spreading the infection to family members is significantly reduced.
Choice C rationale:
Washing hands thoroughly with soap and water after handling the child's soiled items is a fundamental hygiene practice.
Proper handwashing removes bacteria and viruses from the hands, preventing the spread of infections.
Teaching the parents this measure ensures they do not inadvertently transfer the bacteria to surfaces or other people in the household.
Choice D rationale:
Sharing utensils and towels with the child is not an appropriate measure to prevent the spread of gastroenteritis.
This behavior increases the risk of cross-contamination and can lead to other family members becoming infected.
It is important to stress the importance of personal hygiene items to limit the spread of the disease.
Choice E rationale:
Disinfecting surfaces and toys that the child has come into contact with is crucial in preventing the spread of gastroenteritis.
The virus or bacteria causing the illness can survive on surfaces for a certain period, making it essential to regularly disinfect commonly touched items.
This measure reduces the risk of other family members coming into contact with the pathogens and getting sick.
Which intervention is appropriate for this child?
Explanation
Choice D rationale:
Administering antibiotics is appropriate for a child with bacterial gastroenteritis.
Bacterial gastroenteritis is caused by bacteria such as Salmonella or Escherichia coli, and antibiotics are prescribed to eliminate the bacteria from the body.
However, it is essential to note that not all cases of gastroenteritis require antibiotics.
Antibiotics are specifically used for bacterial infections and are not effective against viral gastroenteritis.
Choice A rationale:
Administering antiviral medication is not appropriate for bacterial gastroenteritis.
Antiviral medications are designed to treat viral infections, and bacterial gastroenteritis requires antibiotics to eliminate the bacteria causing the illness.
Choice B rationale:
Offering a clear liquid diet is a general measure used for both viral and bacterial gastroenteritis.
Clear liquids help prevent dehydration and provide essential electrolytes.
However, this intervention does not directly target the bacterial infection.
It is important to combine this with antibiotic therapy for bacterial gastroenteritis.
Choice C rationale:
Providing probiotics is generally beneficial for gut health but may not be the primary intervention for bacterial gastroenteritis.
Probiotics contain beneficial bacteria that can help restore the natural balance of the gut flora.
While probiotics can be useful in some cases, the primary treatment for bacterial gastroenteritis remains antibiotics to eliminate the harmful bacteria causing the infection.
The client asks, "What do probiotics do?" How should the nurse respond?
Explanation
Choice C rationale:
Probiotics promote the growth of beneficial bacteria in the gut.
In the context of gastroenteritis, probiotics can help restore the balance of the gut flora, especially after a course of antibiotics.
Beneficial bacteria aid in digestion and support the immune system.
By promoting the growth of these beneficial bacteria, probiotics contribute to the overall health of the gastrointestinal tract.
Choice A rationale:
"They help prevent the infection from spreading to others.”.
This statement is incorrect.
Probiotics do not prevent the spread of infections to others.
Instead, they focus on restoring the natural balance of bacteria in the gut.
Choice B rationale:
"Probiotics kill the bacteria causing gastroenteritis.”.
This statement is incorrect.
Probiotics do not have a direct bactericidal effect against the bacteria causing gastroenteritis.
They work by promoting the growth of beneficial bacteria rather than killing harmful bacteria.
Choice D rationale:
"Probiotics relieve the symptoms of gastroenteritis.”.
While probiotics can support overall gut health, saying they directly relieve symptoms might be an oversimplification.
Probiotics may help in reducing symptoms indirectly by restoring gut balance, but they might not provide immediate relief from symptoms like diarrhea or abdominal pain.
It's essential to manage symptoms with appropriate medical guidance and treatments.
Dehydration in Children
The child presents with diarrhea and vomiting.
What clinical manifestations would the nurse expect to observe in this patient?
Explanation
Choice A rationale:
Thirst and dry mouth are common signs of dehydration in adults, but in pediatric patients, especially infants, the signs are different.
Children may not be able to communicate their thirst effectively, and dry mouth might not be as noticeable as other signs.
Choice B rationale:
Rapid heart rate and low blood pressure are symptoms of shock, which can occur in severe dehydration.
However, these symptoms are not specific to dehydration and can be present in other conditions.
Sunken eyes and fontanelle in infants are more specific indicators of dehydration in pediatric patients.
Sunken eyes occur due to loss of tissue turgor, and a sunken fontanelle (the soft spot on an infant's head) is a late sign of dehydration.
Choice D rationale:
Lethargy and irritability can be signs of dehydration, but they are nonspecific and can occur in various pediatric conditions.
Sunken eyes and fontanelle, on the other hand, are more specific to dehydration, especially in infants.
The child has been experiencing decreased urine output and dark-colored urine.
What etiological factors could contribute to the child's dehydration, as discussed in the text?
Explanation
Choice A rationale:
Gastrointestinal illnesses, particularly diarrhea and vomiting, lead to fluid loss from the body.
Diarrhea can cause significant loss of water and electrolytes, leading to dehydration.
Vomiting, especially when persistent, can also result in fluid depletion.
These conditions are common causes of dehydration in both children and adults.
Choice B rationale:
Excessive sweating during physical activity or in hot weather can lead to dehydration in individuals, but this scenario does not apply to the child described in the question, who is experiencing decreased urine output and dark-colored urine.
Sweating excessively is more common in older children and adults during physical activities.
Choice C rationale:
Fever, which increases the body's fluid requirements, is a valid point.
However, the child in this scenario does not have fever mentioned as a symptom.
In the absence of fever, gastrointestinal illnesses are the more likely cause of dehydration.
Choice D rationale:
Certain medical conditions, such as diabetes or kidney disease, can lead to chronic dehydration.
However, these conditions are not mentioned in the scenario provided.
In the absence of information about underlying medical conditions, gastrointestinal illnesses remain the most likely cause of the child's dehydration.
Select all the clinical manifestations of dehydration in children mentioned in the text.
Explanation
Choice A rationale:
Thirst and dry mouth are early signs of dehydration.
When the body loses fluids, it signals the brain to increase thirst and conserve water.
Dry mouth can occur due to reduced saliva production when the body is dehydrated.
Choice B rationale:
Decreased urine output and dark-colored urine are indicators of concentrated urine, suggesting dehydration.
Reduced fluid intake or excessive fluid loss can lead to decreased urine production, and the urine becomes more concentrated, appearing darker than usual.
Choice C rationale:
Rapid heart rate and low blood pressure are signs of hypovolemic shock, a severe form of dehydration where the body cannot circulate enough blood to meet its needs.
This can happen in severe cases of dehydration when there is a significant loss of fluids and electrolytes.
Choice D rationale:
Poor skin turgor is a classic clinical sign of dehydration.
Skin turgor refers to the skin's ability to return to its normal position after being pinched.
In dehydrated individuals, the skin loses elasticity and remains tented or "pinched" after being pulled up.
This indicates a lack of fluid in the body.
Choice E rationale:
Increased energy and playfulness are not typical signs of dehydration.
Dehydrated children are more likely to be lethargic and irritable due to the physiological stress on their bodies.
The child is lethargic and irritable.
What diagnostic evaluations might the healthcare provider perform to assess the child's condition, as mentioned in the text?
Explanation
Choice A rationale:
Vital signs are essential in assessing dehydration.
An elevated heart rate may indicate compensatory mechanisms due to decreased intravascular volume.
Low blood pressure may suggest severe dehydration, and abnormal temperature may indicate an underlying infection.
These parameters provide crucial information about the child's circulatory status, helping to assess the severity of dehydration.
Choice B rationale:
Physical examination findings, such as skin turgor and mucous membrane moisture, are valuable indicators of dehydration.
Poor skin turgor, where the skin doesn't return to its normal position promptly when pinched, indicates decreased tissue turgor due to fluid loss.
Dry mucous membranes, including the mouth, suggest dehydration and help evaluate the extent of fluid deficit.
These signs offer direct visual clues about the child's hydration status.
Choice C rationale:
Laboratory tests play a significant role in diagnosing dehydration.
A complete blood count (CBC) helps identify elevated hematocrit levels, indicating hemoconcentration due to fluid loss.
Electrolyte levels, specifically sodium and potassium, provide insights into the child's electrolyte balance, which can be disrupted in dehydration.
Urine specific gravity measures the kidney's ability to concentrate urine; a high specific gravity suggests concentrated urine due to reduced fluid intake.
These tests aid in confirming the diagnosis and assessing the severity of dehydration.
Choice D rationale:
Assessing the child's history is fundamental in understanding the underlying cause of dehydration.
Recent fluid intake and urine output patterns help determine the balance between intake and output.
Symptoms such as diarrhea, vomiting, and fever indicate potential causes of fluid loss.
Additionally, evaluating the child's overall health and any recent illnesses provides context for the dehydration, guiding appropriate treatment.
What etiological factors can contribute to dehydration in children, as discussed in the text?
Explanation
Choice A rationale:
Gastrointestinal illnesses, including diarrhea and vomiting, lead to fluid loss, significantly contributing to dehydration in children.
Diarrhea increases water and electrolyte loss from the body, while vomiting leads to rapid fluid depletion.
These conditions can be severe, especially in infants and young children, making them prone to dehydration.
Choice B rationale:
Excessive sweating during physical activity or in hot weather can result in significant fluid loss.
Children, especially when engaged in vigorous activities, can sweat profusely, leading to dehydration, especially if fluid intake does not match the loss.
Monitoring fluid balance is crucial during such situations to prevent dehydration-related complications.
Choice C rationale:
Insufficient fluid intake due to poor feeding or decreased thirst perception can lead to dehydration, especially in infants and young children who rely heavily on fluid intake for their hydration needs.
Children may not recognize their thirst or may refuse to drink due to illness, leading to decreased fluid intake.
This can result in dehydration, emphasizing the importance of assessing feeding habits and fluid intake patterns.
Choice D rationale:
Sunken eyes and fontanelle in infants are physical signs of dehydration, not etiological factors.
Sunken eyes are due to decreased tissue turgor, indicating dehydration.
Fontanelle, the soft spot on an infant's head, can appear sunken in dehydration.
These signs are crucial in assessing the severity of dehydration during physical examination but do not contribute to the causes of dehydration.
Which of the following should the nurse evaluate during the physical examination?
Explanation
Choice A rationale:
"The child's favorite foods and beverages" are not relevant when assessing dehydration.
While dietary habits are essential for overall health, they do not provide information about the child's hydration status.
Choice B rationale:
"The child's school attendance and activities" are unrelated to the assessment of dehydration.
School attendance and activities are important for a child's social and educational development but do not provide any insight into the child's fluid balance or hydration status.
Choice C rationale:
"The child's skin turgor and mucous membranes" are crucial indicators of dehydration during physical examination.
Poor skin turgor, where the skin tents or remains elevated after being pinched, suggests decreased tissue elasticity due to fluid loss.
Dry mucous membranes, including the mouth, indicate dehydration.
These signs provide immediate visual clues about the child's hydration status and guide further assessment and intervention.
Choice D rationale:
"The child's vaccination history" is not relevant to the assessment of dehydration.
While vaccination history is essential for preventive healthcare, it does not provide any information about the child's current hydration status or fluid balance.
What should the nurse educate the client about?
Explanation
Choice A rationale:
Maintaining a warm room temperature is not the key to preventing dehydration.
Dehydration occurs when the body loses more fluids than it takes in, and temperature control in the room doesn't directly address this issue.
Choice B rationale:
The significance of oral rehydration solution (ORS) is a crucial factor in preventing and treating dehydration.
ORS contains a balanced mixture of salts and sugars that help the body reabsorb water and electrolytes lost due to dehydration.
It is the most effective way to rehydrate a dehydrated child.
Educating the client about the importance of ORS is essential because it provides a clear solution to the problem of dehydration.
Choice C rationale:
The need for a complete blood count (CBC) testing is unrelated to the prevention of dehydration.
CBC is a diagnostic test used to assess various blood parameters, including red and white blood cell counts.
It is not a preventive measure against dehydration.
Choice D rationale:
Suggesting the child's need for frequent, heavy meals is not an appropriate way to prevent dehydration.
In fact, heavy meals can sometimes worsen dehydration as they may be difficult to digest, leading to an increased risk of vomiting and diarrhea, which exacerbate fluid loss.
Select all appropriate nursing interventions from the following options (A-E).
Explanation
Choice A rationale:
Administering oral rehydration solution (ORS) is a crucial nursing intervention for a dehydrated child.
ORS helps replenish the lost fluids and electrolytes, making it an effective treatment for dehydration.
Choice B rationale:
Keeping the child in a cold environment is not an appropriate intervention for a dehydrated child.
Dehydration is not related to room temperature, and maintaining a comfortable environment is important, but extreme cold could cause discomfort to the child.
Choice C rationale:
Monitoring the child's vital signs is an essential nursing intervention when caring for a dehydrated child.
Vital signs, including heart rate, respiratory rate, blood pressure, and temperature, can provide important information about the child's condition and hydration status.
Regular monitoring helps in assessing the child's progress and identifying any worsening symptoms.
Choice D rationale:
Providing heavy meals at regular intervals is not an appropriate intervention for a dehydrated child.
As mentioned earlier, heavy meals can be difficult to digest and may worsen dehydration.
It is more important to focus on rehydration with fluids like ORS.
Choice E rationale:
Educating the child and caregivers about dehydration is an important nursing intervention.
Teaching them about the signs and symptoms of dehydration, the importance of ORS, and how to prevent it in the future is essential for the child's well-being and for preventing future episodes of dehydration.
Which symptoms should the nurse mention?
Explanation
Choice A rationale:
Lethargy and muscle weakness are common signs of electrolyte imbalances in a dehydrated child.
Dehydration can lead to an imbalance of electrolytes, such as sodium and potassium, which affects muscle function and overall energy levels.
Choice B rationale:
Increased appetite and hyperactivity are not typical signs of electrolyte imbalances in a dehydrated child.
Dehydration often leads to a decreased appetite and lethargy.
Choice C rationale:
Shortness of breath and coughing are not directly related to electrolyte imbalances in a dehydrated child.
These symptoms are more likely to be associated with respiratory or pulmonary issues rather than dehydration.
Choice D rationale:
Excessive thirst and urination are common signs of dehydration but are not indicative of electrolyte imbalances.
These symptoms occur as the body attempts to compensate for fluid loss by increasing thirst and increasing urine output.
Electrolyte imbalances are more likely to manifest as muscle weakness and cardiac arrhythmias.
What parameters should the nurse monitor?
Explanation
Choice A rationale:
"Height and weight.”.
Rationale: While monitoring height and weight is important for a child's growth and development, these parameters are not the primary vital signs to assess dehydration.
Dehydration assessment focuses on immediate physiological indicators, such as heart rate and blood pressure.
Choice B rationale:
"Heart rate and blood pressure.”.
Rationale: This is The correct answer.
When assessing a dehydrated child, monitoring vital signs such as heart rate and blood pressure is crucial.
Dehydration can lead to an increased heart rate and decreased blood pressure.
These parameters provide valuable information about the child's circulatory status and fluid balance.
Choice C rationale:
"Hair and eye color.”.
Rationale: Hair and eye color are not relevant parameters for assessing dehydration.
They are genetic traits and do not change in response to dehydration.
Choice D rationale:
"Shoe size and clothing size.”.
Rationale: Shoe size and clothing size are not relevant for assessing dehydration.
These measurements are related to a child's growth and body structure but do not provide information about their hydration status.
What is the appropriate fluid deficit calculation for a child who weighs 12 kg?
Explanation
Choice A rationale:
Fluid deficit (in mL) = body weight (in kg) x 0.03.
Rationale: This calculation significantly underestimates the fluid deficit for a child with moderate dehydration.
Dehydration often requires more significant fluid replacement.
Choice B rationale:
Fluid deficit (in mL) = body weight (in kg) x 0.06.
Rationale: This calculation overestimates the fluid deficit for a child with moderate dehydration.
Using this formula would result in excessive fluid replacement, which can be harmful.
Choice C rationale:
Fluid deficit (in mL) = body weight (in kg) x 0.1.
Rationale: This calculation overestimates the fluid deficit for a child with moderate dehydration.
Using this formula would result in excessive fluid replacement, which can be harmful.
Choice D rationale:
Fluid deficit (in mL) = body weight (in kg) x 0.04.
Rationale: This is The correct answer.
The appropriate fluid deficit calculation for a child who weighs 12 kg with moderate dehydration is to multiply their body weight by 0.04.
For this child, it would be 12 kg x 0.04 = 480 mL.
This formula is a commonly used guideline to estimate fluid deficit in cases of dehydration.
According to the Holliday-Segar method, what would be the total maintenance fluid requirement for this child?
Explanation
Choice A rationale:
Total maintenance fluids = 1800 mL/day.
Rationale: According to the Holliday-Segar method, the total maintenance fluid requirement for a child who weighs 18 kg would be approximately 100 mL/kg/day.
In this case, it would be 18 kg x 100 mL/kg/day = 1800 mL/day.
Choice B rationale:
Total maintenance fluids = 1200 mL/day.
Rationale: This calculation significantly underestimates the total maintenance fluid requirement.
Children generally require a higher amount of maintenance fluids to support their growth and physiological functions.
Choice C rationale:
Total maintenance fluids = 1600 mL/day.
Rationale: This calculation underestimates the total maintenance fluid requirement.
According to the Holliday-Segar method, children typically need a maintenance fluid intake of around 100 mL/kg/day.
Choice D rationale:
Total maintenance fluids = 1400 mL/day.
Rationale: This calculation underestimates the total maintenance fluid requirement.
According to the Holliday-Segar method, the recommended maintenance fluid intake is approximately 100 mL/kg/day.
For an 18 kg child, this would be 18 kg x 100 mL/kg/day = 1800 mL/day.
The nurse understands that the child’s degree of dehydration is typically classified based on the loss of body weight.
The nurse observes dry mucous membranes, decreased urine output, and decreased skin turgor in the child.
Based on these observations, the nurse should classify the child’s dehydration as:.
Explanation
“Severe dehydration, which is ≥10% loss of body weight.”.
Choice A rationale:
Mild dehydration is typically classified as a 3-5% loss of body weight.
The signs and symptoms described in the scenario, such as dry mucous membranes, decreased urine output, and decreased skin turgor, are indicative of more severe dehydration than a 3-5% loss.
Choice B rationale:
Moderate dehydration is generally considered to be a 6-9% loss of body weight.
However, the signs and symptoms presented in the scenario suggest a more severe state of dehydration.
Choice C rationale:
Severe dehydration is classified as a loss of ≥10% of body weight.
The signs and symptoms observed by the nurse, including dry mucous membranes, decreased urine output, and decreased skin turgor, are consistent with severe dehydration, making choice C The correct classification.
Choice D rationale:
No dehydration is defined as less than a 3% loss of body weight.
The clinical manifestations observed in the child, as described in the scenario, clearly indicate dehydration.
In this case, the child's signs and symptoms align with the classification of severe dehydration, which is characterized by a loss of ≥10% of body weight.
These symptoms include dry mucous membranes, decreased urine output, and decreased skin turgor.
It's crucial to recognize the severity of dehydration accurately to initiate the appropriate treatment and prevent complications.
The nurse reassures the mother and explains the steps involved in fluid replacement for a dehydrated child.
Which of the following statements by the mother indicates a correct understanding of the nurse’s explanation?
Explanation
“I understand that my child’s hydration status will be continuously assessed.”.
Choice A rationale:
While a child's age and weight may play a role in determining fluid replacement, this statement doesn't encompass the entire concept of managing dehydration.
Monitoring hydration status involves assessing clinical signs and symptoms, as well as ongoing evaluation.
Choice B rationale:
Electrolyte solutions and supplements are indeed part of the treatment for dehydration.
However, this statement doesn't reflect the comprehensive understanding of managing a dehydrated child, including continuous assessment of hydration status.
Choice C rationale:
This statement indicates a correct understanding.
Continuous assessment of a child's hydration status is essential in managing dehydration.
It allows healthcare providers to monitor the child's response to treatment and make necessary adjustments.
Choice D rationale:
Collaboration within the healthcare team is important, but this statement doesn't specifically address the understanding of fluid replacement and dehydration management.
The correct response is choice C because it highlights the critical aspect of continuous assessment, which is essential to ensure that the child's hydration status is being monitored effectively during treatment.
Which of the following steps should the nurse take? (Select all that apply).
Explanation
Choice A rationale:
Assessing the degree of dehydration based on clinical signs and symptoms is a fundamental step in managing a dehydrated child.
This assessment guides the choice of appropriate treatment and fluid replacement.
Choice B rationale:
Calculating the fluid deficit based on the degree of dehydration is crucial in determining the amount of fluid that needs to be replaced accurately.
This calculation helps prevent under or overhydration.
Choice D rationale:
Monitoring the child's response to treatment and adjusting the plan accordingly is essential.
Dehydration management is an ongoing process, and adjustments may be necessary based on how the child is progressing.
Choice E rationale:
Communication with physicians, nutritionists, and other healthcare professionals is vital for comprehensive care.
Dehydration management often involves a multidisciplinary approach to address the child's overall health and nutritional needs.
Selecting all of these options (A, B, D, and E) ensures a comprehensive approach to managing dehydration in a child.
It involves assessment, calculation, monitoring, and collaboration with healthcare professionals for the best outcome.
Which of the following actions should be taken by the nurse?
Explanation
Choice A rationale:
Administer electrolyte solutions or supplements as prescribed by the physician.
Rationale: While administering electrolyte solutions or supplements may be part of the treatment plan for a dehydrated child, it is not the initial action that the nurse should take.
The first step should be to assess the child's condition and monitor their response to treatment.
Choice B rationale:
Monitor the child’s response to treatment and adjust the plan accordingly.
Rationale: This is The correct answer.
Dehydration is a complex condition, and the nurse's initial action should be to closely monitor the child's response to treatment, which may include oral or intravenous rehydration.
By monitoring the child's vital signs, urine output, and clinical signs, the nurse can make real-time adjustments to the treatment plan.
Choice C rationale:
Collaborate with physicians, nutritionists, and other healthcare professionals to ensure comprehensive care.
Rationale: Collaboration with other healthcare professionals is important for the overall care of the child, but it is not the immediate action needed to correct electrolyte imbalances in a dehydrated child.
Monitoring and treatment adjustments come first.
Choice D rationale:
Assess the degree of dehydration based on clinical signs and symptoms.
Rationale: While assessing the degree of dehydration is important, it should not be the only action taken.
Monitoring the child's response to treatment and adjusting the plan is equally crucial.
Dehydration assessment is typically part of the initial evaluation, but ongoing monitoring is necessary to ensure the child's condition improves.
Which of the following advice should be given by the nurse?
Explanation
Choice A rationale:
Ensure appropriate fluid intake based on age and weight.
Rationale: This is an essential piece of advice to prevent dehydration in children.
Proper fluid intake based on age and weight helps maintain hydration.
However, it's not the only advice that should be given.
Choice B rationale:
Monitor for signs of dehydration such as dry mucous membranes and decreased urine output.
Rationale: Monitoring for signs of dehydration is crucial, but it's not the only preventive measure.
Detecting dehydration early is important for timely intervention, but proactive prevention is also necessary.
Choice C rationale:
Encourage consumption of electrolyte solutions during periods of illness.
Rationale: Encouraging the consumption of electrolyte solutions during illness is a valuable piece of advice, especially when children may lose fluids due to vomiting or diarrhea.
However, it's not the only preventive measure.
Choice D rationale:
All these measures are necessary to prevent dehydration in children.
Rationale: This is The correct answer.
Preventing dehydration in children involves a combination of measures, including ensuring appropriate fluid intake, monitoring for signs of dehydration, and encouraging electrolyte solutions during illness.
All these measures work together to keep a child well-hydrated and prevent dehydration.
The nurse is preparing to start an intravenous (IV) infusion.
Which of the following IV fluids is the most appropriate for this client?
Explanation
Choice A rationale:
Normal saline (0.9% NaCl).
Rationale: Normal saline is the most appropriate choice for a client with dehydration and hyponatremia.
It provides a balanced solution with sodium and chloride, which can help correct hyponatremia and rehydrate the client.
It is an isotonic solution and is commonly used for fluid resuscitation.
Choice B rationale:
Half normal saline (0.45% NaCl).
Rationale: Half normal saline is also an isotonic solution, but it contains less sodium than normal saline.
In a case of hyponatremia, it's better to use a solution with a higher sodium concentration, making choice A (normal saline) more appropriate.
Choice C rationale:
Lactated Ringer’s.
Rationale: Lactated Ringer's is another isotonic solution, but it may not be the best choice for a client with hyponatremia.
It contains lactate, which can be metabolized to bicarbonate, potentially worsening the client's hyponatremia.
Therefore, it's not the most appropriate option in this case.
Choice D rationale:
D5W (5% dextrose in water).
Rationale: D5W is a hypotonic solution and should not be used for rehydration in a client with hyponatremia.
It can exacerbate the electrolyte imbalance and is not suitable for addressing dehydration.
The nurse is preparing to start an intravenous (IV) infusion.
Which of the following IV fluids is the most appropriate for this client?
Explanation
Normal saline (0.9% NaCl).
Choice A rationale:
Normal saline (0.9% NaCl) is the most appropriate choice for a client with burns and hypovolemia.
This isotonic solution helps to restore intravascular volume and replace lost fluids.
It contains sodium chloride in a concentration similar to that of the body's extracellular fluid, making it effective for rehydration and replenishing electrolytes in hypovolemic patients.
Choice B rationale:
Half normal saline (0.45% NaCl) is a hypotonic solution with a lower sodium concentration than the body's extracellular fluid.
It is not the best choice for treating hypovolemia and burns because it may not effectively expand intravascular volume and may cause cellular swelling.
Choice C rationale:
Lactated Ringer's is an isotonic solution, but it contains additional electrolytes and lactate.
While it can be suitable for some fluid replacement needs, normal saline is preferred for burn patients because it has a simpler composition and is effective for volume resuscitation in cases of hypovolemia.
Choice D rationale:
D5W (5% dextrose in water) is a solution that primarily provides dextrose for energy, not suitable for hypovolemia and burns.
It can cause dilutional hyponatremia if used as the primary fluid in hypovolemic patients.
The client is unconscious and has a blood sugar of 30 mg/dL.
The nurse is preparing to start an intravenous (IV) infusion.
Which of the following IV fluids is the most appropriate for this client?
Explanation
Normal saline (0.9% NaCl).
Choice A rationale:
For a client with severe hypoglycemia and unconsciousness, the priority is to provide a fluid that will rapidly raise blood sugar levels.
Normal saline is the appropriate choice because it does not contain dextrose and will not lower blood glucose levels further.
It helps maintain blood pressure and intravascular volume.
Choice B rationale:
Half normal saline (0.45% NaCl) is not the best choice for this scenario as it does not provide glucose to correct hypoglycemia.
It could be used for volume resuscitation but should be combined with a glucose source for this specific client.
Choice C rationale:
Lactated Ringer's is not ideal for treating hypoglycemia because it does not contain glucose.
It is more suitable for patients with fluid deficits but not for rapidly correcting hypoglycemia.
Choice D rationale:
D50W (50% dextrose in water) is too concentrated and could lead to rapid increases in blood sugar levels, potentially causing hyperglycemia.
It is typically reserved for situations where very rapid correction of severe hypoglycemia is necessary and can be administered in a controlled manner.
Choice E rationale:
D10W (10% dextrose in water) contains a lower concentration of dextrose compared to D50W, but it is still too concentrated for this scenario and may lead to overly rapid correction of hypoglycemia.
Normal saline is the preferred choice because it does not contain dextrose and allows for more controlled glucose administration.
The nurse is preparing to start an intravenous (IV) infusion.
Which of the following IV fluids is the most appropriate for this client?
Explanation
Normal saline (0.9% NaCl).
Choice A rationale:
Normal saline (0.9% NaCl) is the most appropriate choice for a client with cerebral edema.
This isotonic solution is commonly used to maintain intravascular volume and provides a neutral effect on fluid balance in the brain.
It does not introduce additional electrolytes that could potentially worsen cerebral edema.
Choice B rationale:
Half normal saline (0.45% NaCl) is not the best choice for cerebral edema because it is hypotonic and may lead to cellular swelling, potentially exacerbating the edema.
Choice C rationale:
Lactated Ringer's, while isotonic, contains additional electrolytes and lactate.
In the case of cerebral edema, it is safer to use a solution with a simpler composition like normal saline to avoid any potential complications related to electrolyte imbalances.
Choice D rationale:
D5W (5% dextrose in water) is not recommended for cerebral edema because it contains dextrose and may not adequately address the underlying issue of increased intracranial pressure associated with cerebral edema.
The nurse is preparing to start an intravenous (IV) infusion.
Which of the following IV fluids is the most appropriate for this client?
Explanation
Choice A rationale:
Albumin (5% or 25%) Albumin is the most appropriate IV fluid for a client with hypoalbuminemia and shock.
Albumin is a colloid solution that helps to increase oncotic pressure, which can be decreased in conditions like hypoalbuminemia.
This increased oncotic pressure can help draw fluids back into the vascular space, improving intravascular volume and blood pressure.
Therefore, it is a suitable choice for a patient with shock.
The two concentrations mentioned, 5% and 25%, refer to the percentage of albumin in the solution, and the choice between them depends on the severity of the patient's condition and the desired effect.
The 5% solution is often used for volume expansion and to improve hemodynamics, while the 25% solution is used for rapid volume expansion.
Choice B rationale:
Dextrans (Dextran-40 or Dextran-70) Dextrans are another type of colloid solution, but they are not the best choice for this specific situation.
Dextrans are often used as volume expanders but are more commonly employed in conditions where there is no issue with albumin levels.
In this case, the primary concern is hypoalbuminemia, and using albumin-based solutions would be more appropriate.
Choice C rationale:
Gelatin (Gelofusine or Haemaccel) Gelatin-based solutions are also colloids and can be used for volume expansion.
However, they are not the best choice for a patient with hypoalbuminemia because they do not address the low albumin levels.
Albumin solutions are preferred in such cases to help restore oncotic pressure and improve intravascular volume.
Choice D rationale:
Plasma protein fraction (Plasmanate or Plasmasteril) Plasma protein fraction solutions, also known as human albumin, are similar to albumin solutions.
However, in this context, albumin solutions are more commonly used.
Plasma protein fraction solutions may be indicated in specific situations, but the primary choice for a patient with hypoalbuminemia and shock would be albumin-based solutions, as they are specifically designed to address albumin deficiencies.
The nurse understands that this type of intravenous fluid contains Sodium 154 mEq/L and Chloride 154 mEq/L.
It is often used in cases of hyponatremia, shock, maintenance fluids, and dehydration.
However, it should not be used in cases of hypernatremia, fluid overload, heart failure, edema, heart disease, cardiac decompensation, primary or secondary aldosteronism.
What should the nurse say to the client to explain why they are receiving this particular IV fluid?
Explanation
Choice A rationale:
“This fluid will help to increase your sodium levels which are currently too low.”.
The nurse should explain to the client that they are receiving Normal Saline (0.9% NaCl) to increase their sodium levels.
This is The correct choice because Normal Saline is a hypertonic solution containing 154 mEq/L of sodium and 154 mEq/L of chloride.
It is used in cases of hyponatremia to raise sodium levels.
Sodium is an essential electrolyte, and low levels can lead to symptoms such as weakness, confusion, and muscle cramps.
Choice B rationale:
“This fluid will help to decrease your sodium levels which are currently too high.”.
Normal Saline is a hypertonic solution that would not be used to lower sodium levels, as it would have the opposite effect and further elevate sodium levels.
Choice C rationale:
“This fluid will help to increase your potassium levels which are currently too low.”.
It is not used to increase potassium levels, and potassium replacement would require a different solution, such as potassium chloride.
Choice D rationale:
“This fluid will help to decrease your potassium levels which are currently too high.”.
Normal Saline does not address high potassium levels; it is used to address hyponatremia and dehydration by increasing sodium levels.
This intravenous fluid contains Sodium 77 mEq/L and Chloride 77 mEq/L.
It is contraindicated in cases of hypovolemia, hyponatremia, increased intracranial pressure, liver disease, trauma, and burns.
What should the client say to demonstrate understanding of the treatment plan?
Explanation
Choice A rationale:
“This fluid will help to restore my sodium levels and replace the fluids I lost from vomiting.”.
The client should understand that they are receiving Half Normal Saline (0.45% NaCl) to restore sodium levels and replace lost fluids due to vomiting.
Half Normal Saline contains 77 mEq/L of sodium and 77 mEq/L of chloride, making it a suitable choice for a patient with mild hyponatremia and fluid loss from vomiting.
It helps restore sodium levels without the risk of overcorrection seen with 0.9% NaCl.
Choice B rationale:
“This fluid will help to lower my sodium levels and replace the fluids I lost from sweating.”.
Half Normal Saline is not used to lower sodium levels; its purpose is to restore sodium levels and provide fluids for cases like vomiting or other fluid losses.
Sweating typically leads to fluid loss, not sodium loss, and Half Normal Saline is not a treatment for high sodium levels.
Choice C rationale:
“This fluid will help to restore my potassium levels and replace the fluids I lost from vomiting.”.
Half Normal Saline does not address potassium levels, and the primary reason for using it is to address sodium imbalances and fluid loss, not potassium-related issues.
Choice D rationale:
“This fluid will help to lower my potassium levels and replace the fluids I lost from sweating.”.
Half Normal Saline is not used to lower potassium levels and is not specifically indicated for treating high potassium.
Additionally, it is not typically used to address fluid loss from sweating.
The physician orders Lactated Ringer’s solution for fluid resuscitation.
The nurse knows that this solution contains Sodium 130 mEq/L, Chloride 109 mEq/L, Potassium 4 mEq/L, Calcium 3 mEq/L, and Lactate 28 mEq/L.
Which of the following statements are true regarding Lactated Ringer’s solution? (Select all that apply).
Explanation
Choice A rationale:
Lactated Ringer's solution is not contraindicated in cases of hyperkalemia.
This solution contains potassium in a relatively low concentration of 4 mEq/L, which is unlikely to significantly impact hyperkalemia.
Choice B rationale:
Lactated Ringer's solution can be contraindicated in cases of hypokalemia.
While it does contain potassium, the concentration is relatively low at 4 mEq/L.
In cases of severe hypokalemia, a more potassium-rich solution might be preferred.
Choice C rationale:
Lactated Ringer's solution can be used in cases of lower GI fluid loss.
It can help replace lost fluids and electrolytes effectively.
Choice D rationale:
Lactated Ringer's solution can be used in cases of upper GI fluid loss.
It helps restore lost fluids and electrolytes.
Choice E rationale:
Lactated Ringer's solution is not contraindicated in cases of lactic acidosis.
In fact, it contains lactate (28 mEq/L), which can be metabolized to bicarbonate and help correct acidosis.
The nurse explains that this intravenous fluid contains Dextrose 100 g/L and Water 900 mL.
Which of the following statements made by the client indicates a correct understanding of their treatment?
Explanation
Choice A rationale:
The client's statement, "This IV fluid will provide me with hydration and calories," is correct.
D10W contains 10% dextrose and is used to provide both hydration and calories to the patient.
Choice B rationale:
D10W would not help lower blood sugar levels.
In fact, it would increase blood sugar levels due to the high concentration of dextrose.
Choice C rationale:
D10W does not provide essential electrolytes, so the statement is incorrect.
It's primarily used for calorie supplementation and hydration.
Choice D rationale:
D10W would not help increase blood pressure.
While it can provide hydration, it does not contain medications or components specifically intended to increase blood pressure.
Select all the clinical signs and symptoms of dehydration that the nurse should consider.
Explanation
Sunken fontanelle (in infants).
C. Dry mucous membranes.
E. Lethargy.
Choice A rationale:
Sunken fontanelle (in infants) is a clinical sign of dehydration.
The fontanelle is the soft spot on an infant's head, and when it becomes sunken, it suggests that the child is dehydrated.
This occurs because a lack of adequate fluid causes the brain to temporarily shrink, leading to the sunken appearance.
Choice B rationale:
Increased urine output is not typically a sign of dehydration.
In fact, dehydration often leads to decreased urine output as the body attempts to conserve fluid.
Increased urine output can be a sign of other conditions, such as diabetes.
Choice C rationale:
Dry mucous membranes are a classic sign of dehydration.
When the body lacks sufficient fluids, the mucous membranes in the mouth and other areas can become dry and sticky.
This is an important clinical indicator of dehydration.
Choice D rationale:
Normal skin turgor is not a sign of dehydration.
Skin turgor refers to the skin's ability to bounce back when pinched and released.
In a hydrated individual, the skin should have good turgor.
Dehydration can lead to poor skin turgor, but normal skin turgor does not indicate dehydration.
Choice E rationale:
Lethargy is a potential sign of dehydration.
When a child is dehydrated, they may become lethargic or unusually tired because their body is not receiving the necessary fluids to function properly.
Lethargy can be an early sign of dehydration in children.
What would be the total hourly fluid replacement rate for this child?
Explanation
Approximately 100 mL/hour.
To calculate the total hourly fluid replacement rate, we can use the Holliday-Segar method, which is commonly used in pediatrics.
According to this method, a child's daily maintenance fluid requirement is calculated as follows: For the first 10 kg of body weight: 100 mL/kg/day.
For the next 10 kg of body weight: 50 mL/kg/day.
For each additional kg of body weight: 20 mL/kg/day.
In this case, the child weighs 14 kg.
So, we calculate as follows: For the first 10 kg: 10 kg x 100 mL/kg/day = 1000 mL/day.
For the next 4 kg (14 kg - 10 kg): 4 kg x 50 mL/kg/day = 200 mL/day.
Now, add these two together: 1000 mL/day + 200 mL/day = 1200 mL/day.
To find the hourly rate, we divide the daily requirement by 24 (hours in a day): 1200 mL/day ÷ 24 hours/day = 50 mL/hour.
So, the child's total hourly fluid replacement rate should be approximately 50 mL/hour.
However, this is an approximate rate.
To be more conservative in the case of severe dehydration, it's common to round this up to approximately 100 mL/hour to ensure that the child receives adequate fluids to rehydrate.
Choice A rationale:
Approximately 58 mL/hour is not The correct answer.
This calculation does not match the standard Holliday-Segar method used in pediatrics for fluid replacement.
Choice B rationale:
Approximately 140 mL/hour is not The correct answer.
This calculation significantly exceeds the recommended hourly fluid replacement rate for a child of this weight, which could potentially lead to overhydration.
Choice D rationale:
Approximately 82 mL/hour is not The correct answer.
This calculation does not align with the standard method for calculating fluid replacement in pediatric patients.
What should the nurse do to ensure comprehensive care during the treatment and management of dehydration in children?
Explanation
Communicate with the healthcare team.
To ensure comprehensive care during the treatment and management of dehydration in children, communication with the healthcare team is essential.
Here's the rationale for this choice:
Choice A rationale:
Administer electrolyte solutions only.
This is not The correct approach.
While administering electrolyte solutions is a vital part of managing dehydration, it is not the only aspect of care.
Comprehensive care also includes assessing the child's overall condition, monitoring vital signs, and addressing any underlying causes of dehydration.
Choice B rationale:
Communicate with the healthcare team.
This is The correct answer.
Dehydration management often requires a multidisciplinary approach.
Communicating with the healthcare team, which may include physicians, dietitians, and other specialists, is crucial to ensure that the child receives appropriate treatment and that any underlying medical issues are addressed.
It also allows for coordinated care and adjustment of the treatment plan as needed.
Choice C rationale:
Rely solely on clinical signs to assess hydration status.
Relying solely on clinical signs is not sufficient for comprehensive care.
While clinical signs are important indicators of hydration status, laboratory tests and monitoring are also necessary to accurately assess and manage dehydration.
Choice D rationale:
Skip monitoring the child's response to treatment.
Skipping monitoring is not advisable.
Monitoring the child's response to treatment is a critical part of dehydration management.
It helps ensure that the child is improving, and adjustments can be made to the treatment plan if necessary.
Allergies and Asthma in Children
Which of the following statements by the nurse is accurate regarding the etiology of allergies in children?
Explanation
Choice A rationale:
Allergies in children are not primarily caused by bacterial infections.
While infections can certainly exacerbate allergy symptoms, they are not the primary cause of allergies in children.
Allergies are more related to immune responses to specific substances.
Choice B rationale:
Common allergens for children do not typically include cigarette smoke and exercise.
Cigarette smoke can exacerbate respiratory issues and trigger symptoms in children with allergies or asthma, but it is not an allergen itself.
Exercise is generally a healthy activity for children and is not considered an allergen.
Choice D rationale:
Allergies in children are not solely caused by exposure to pet dander.
While pet dander can be a significant allergen for some children, allergies in children are typically triggered by a wide range of allergens, including pollen, dust mites, certain foods, and more.
Choice C rationale:
The correct answer is C.
Allergies in children can be influenced by genetic factors, environmental exposures, and immune system dysregulation.
Genetic predisposition can make a child more susceptible to allergies.
Environmental exposures to allergens can trigger allergic reactions, and immune system dysregulation can contribute to the development of allergies.
Which of the following statements by the nurse is correct regarding the pathophysiology of asthma in children?
Explanation
Choice A rationale:
Asthma is not characterized by a lack of airway sensitivity and hyperresponsiveness.
In fact, asthma is often associated with increased airway sensitivity and hyperresponsiveness.
This heightened reactivity of the airways is a hallmark of asthma.
Choice B rationale:
In asthma, airway muscles do not relax and widen during an episode.
Instead, they constrict or tighten, leading to airway obstruction and making breathing more difficult.
This bronchoconstriction is a key feature of asthma.
Choice D rationale:
Exposure to allergens or irritants in asthma does have an impact on airway constriction.
In individuals with asthma, exposure to allergens or irritants can trigger an inflammatory response in the airways, leading to increased bronchoconstriction and worsening symptoms.
Choice C rationale:
The correct answer is C.
Chronic inflammation of the airways in asthma does lead to increased airway sensitivity and hyperresponsiveness.
This chronic inflammation makes the airways more reactive to various triggers, including allergens, and contributes to the characteristic symptoms of asthma.
Select all the interventions that the nurse should include in the teaching session:.
Explanation
Choice B rationale:
While exercise is generally beneficial for children, it can trigger asthma symptoms in some individuals, especially if they have exercise-induced bronchoconstriction.
However, the primary focus should be on managing and controlling asthma symptoms during exercise rather than discouraging physical activity.
The other options are more directly related to managing allergies and asthma.
Choice E rationale:
Administering antibiotics regularly to prevent asthma exacerbations is not a recommended intervention.
Antibiotics are used to treat bacterial infections, not to prevent asthma exacerbations.
In fact, overuse of antibiotics can lead to antibiotic resistance and should be avoided unless there is a specific medical indication.
Choice A rationale:
The correct answer is A.
Providing a smoke-free environment at home is essential for managing allergies and asthma in children.
Secondhand smoke can exacerbate respiratory symptoms and increase the risk of asthma attacks.
Eliminating exposure to smoke is a crucial step in managing these conditions.
Choice C rationale:
The correct answer is C.
Identifying and avoiding allergens that trigger symptoms is a key component of managing allergies and asthma in children.
By minimizing exposure to known allergens, individuals can reduce the frequency and severity of allergic and asthmatic reactions.
Choice D rationale:
The correct answer is D.
Promoting good hand hygiene to prevent allergies is important, especially for reducing the risk of infections that could exacerbate allergy symptoms or asthma.
Proper hand hygiene can help prevent the spread of illnesses and reduce the likelihood of respiratory infections.
Which of the following triggers should the nurse include in the response?
Explanation
Choice A rationale:
Exposure to allergens and respiratory infections are common triggers for asthma symptoms in children.
Allergens, such as pollen, dust mites, and pet dander, can trigger allergic reactions in the airways, leading to asthma symptoms.
Respiratory infections, like the common cold or flu, can exacerbate asthma by causing airway inflammation and increased mucus production.
These triggers can lead to bronchoconstriction and worsen asthma symptoms in children.
Choice B rationale:
Consumption of certain foods and insect venom is not a common trigger for asthma symptoms in children.
While food allergies can lead to allergic reactions, they typically manifest as gastrointestinal or skin symptoms rather than respiratory issues.
Insect venom may cause anaphylactic reactions but is not a common cause of asthma symptoms.
Choice C rationale:
Playing outdoors and engaging in physical activities are not common triggers for asthma symptoms in children.
Physical activity can induce exercise-induced bronchoconstriction in some children with asthma, but this is different from the common triggers mentioned in choice A.
Being active is essential for overall health, and children with asthma can participate in sports with appropriate management.
Choice D rationale:
Exposure to excessive sunlight and hot weather is not a common trigger for asthma symptoms in children.
Asthma symptoms are typically worsened by cold, dry air, which can lead to airway constriction.
Hot weather and sunlight do not directly contribute to asthma exacerbations.
The child's parent is concerned about the role of IgE antibodies in allergies.
Which of the following explanations by the nurse is accurate regarding the role of IgE antibodies in allergic reactions?
Explanation
Choice A rationale:
IgE antibodies play a significant role in allergic reactions.
They are not insignificant.
IgE antibodies are specifically designed to recognize and bind to allergens, and when they do so, they trigger an immune response that includes the release of histamine and other inflammatory mediators.
These substances are responsible for the symptoms of allergies, such as itching, redness, and swelling.
Choice B rationale:
IgE antibodies do not inhibit the release of histamine in response to allergens; rather, they facilitate it.
The role of IgE antibodies is to promote the allergic response, leading to the release of histamine and other inflammatory molecules.
Choice D rationale:
IgE antibodies are not limited to respiratory infections.
While they are involved in the immune response against infections, they are primarily associated with allergic reactions.
IgE antibodies do not play a role exclusively in respiratory infections but are a key component in the allergic response.
Which of the following manifestations are common symptoms of allergic rhinitis in children?
Explanation
Choice A rationale:
A high-pitched whistling sound when breathing is not a common symptom of allergic rhinitis in children.
This sound, known as wheezing, is more characteristic of asthma and bronchoconstriction.
Choice B rationale:
Difficulty breathing and chest tightness are not typical symptoms of allergic rhinitis but are more closely associated with asthma.
Allergic rhinitis primarily involves symptoms such as sneezing, nasal congestion, and itchy or watery eyes.
Choice D rationale:
A persistent cough, especially at night, is not a classic symptom of allergic rhinitis in children.
Instead, it is more often associated with conditions like postnasal drip or nighttime asthma symptoms.
What is the likely manifestation the nurse will observe in this child?
Explanation
The child's skin shows dryness, itching, and rash.
Choice A rationale:
"The child exhibits wheezing and coughing.”.
Wheezing and coughing are typical symptoms of respiratory issues like asthma but not necessarily associated with dry, itchy skin and redness, which are dermatological symptoms.
Therefore, this choice is not the likely manifestation.
Choice B rationale:
"The child has nasal congestion and itchy eyes.”.
Nasal congestion and itchy eyes are more indicative of allergic rhinitis or hay fever, not dry, itchy skin and redness.
This choice does not align with the presenting symptoms and is not the likely manifestation.
Choice D rationale:
"The child experiences difficulty breathing and chest tightness.”.
Difficulty breathing and chest tightness are more characteristic of asthma, but these symptoms primarily relate to the respiratory system.
The primary manifestation described in the question is related to the skin.
Therefore, this choice is not the likely manifestation.
Choice C rationale:
"The child's skin shows dryness, itching, and rash.”.
This choice is The correct answer.
The symptoms of dry, itchy skin and redness are typical signs of a skin condition, such as eczema or contact dermatitis.
The nurse is likely to observe these dermatological symptoms in the child.
Dryness, itching, and rash are often associated with skin conditions, and they are distinct from respiratory symptoms like coughing and wheezing.
Which of the following assessments are appropriate for determining asthma symptoms in children?
Explanation
Choice A rationale:
"Measure specific IgE antibodies in blood.”.
Measuring specific IgE antibodies in blood is a diagnostic test to identify allergies, but it is not directly related to assessing asthma symptoms in children.
This choice does not align with the question's focus on determining asthma symptoms.
Choice B rationale:
"Evaluate lung function using spirometry.”.
Spirometry is a crucial diagnostic tool for assessing lung function and is highly relevant for determining asthma symptoms in children.
It allows for the measurement of lung volume and airflow, making it an appropriate choice for evaluating asthma.
Choice C rationale:
"Assess for recurrent cough, especially at night.”.
Recurrent cough, especially at night, is a common symptom in children with asthma.
It is related to the narrowing of the airways and increased mucus production, making this choice appropriate for assessing asthma symptoms.
Choice D rationale:
"Monitor peak flow meter measurements.”.
Peak flow meter measurements are used to monitor lung function and are essential for managing asthma.
It helps assess the severity of asthma and the effectiveness of treatment.
Therefore, it is an appropriate choice for evaluating asthma symptoms.
Choice E rationale:
"Perform skin prick tests to identify allergens.”.
Skin prick tests are used to identify specific allergens, which can be useful in diagnosing allergies, but they are not directly related to assessing asthma symptoms.
Asthma assessment focuses more on lung function and respiratory symptoms.
Which of the following diagnostic methods are used to identify specific allergens in children?
Explanation
"Perform a skin prick test.”.
Choice A rationale:
"Perform a skin prick test.”.
A skin prick test, also known as a skin allergy test, is a common method used to identify specific allergens in both children and adults.
It involves applying small amounts of allergens to the skin and observing for any allergic reactions, such as redness and swelling at the test sites.
This is a valuable diagnostic method to pinpoint the allergens triggering allergic reactions.
Choice B rationale:
"Conduct a spirometry test.”.
Spirometry is a lung function test and is not used to identify specific allergens.
It measures lung volume and airflow, making it more suitable for assessing respiratory conditions like asthma.
Choice C rationale:
"Administer a peak flow meter measurement.”.
Peak flow meter measurements are used to monitor lung function and asthma symptoms but do not identify specific allergens.
This choice is not relevant to the task of identifying allergens.
Choice D rationale:
"Measure specific IgE antibodies in blood.”.
Measuring specific IgE antibodies in the blood can help determine if a person has allergies, but it does not identify the specific allergens causing the allergies.
This test is valuable for confirming the presence of allergies but not for pinpointing allergens.
What kind of information should the nurse seek in this context?
Explanation
Choice A rationale:
The child's response to bronchodilators and other asthma medications is an important aspect of managing asthma, but in the context of assessing asthma triggers, it is not the primary concern.
This information is more relevant when evaluating the child's response to treatment and not identifying potential triggers.
Choice C rationale:
Assessing the child's lung function using spirometry measurements is essential in managing asthma, but it is not directly related to identifying asthma triggers.
Spirometry helps in diagnosing and monitoring the severity of asthma but does not provide information about what triggers the child's asthma symptoms.
Choice D rationale:
The child's skin prick test results for allergen identification are helpful in determining specific allergens that might trigger allergic reactions, but this is not the primary focus when assessing asthma triggers.
Allergen identification is more relevant for allergies other than asthma.
Now, let's move on to .
The correct
A nurse is providing education to a child and their family about managing allergies.
Which intervention should the nurse include in the teaching?
Explanation
Choice A rationale:
Avoidance of allergens is a fundamental aspect of managing allergies, and taking antihistamines regularly can help control symptoms but does not eliminate the need for allergen avoidance.
It is important to educate the child and family about avoiding allergens and using antihistamines as part of the management plan.
Choice B rationale:
Immunotherapy is not typically the first-line treatment for allergies in children.
It is considered when other treatments, including allergen avoidance and medications, are not effective.
The primary focus should be on educating the child and their family about allergen avoidance and other appropriate interventions.
Choice D rationale:
Managing allergies involves more than just using inhalers.
Inhalers are primarily used for managing asthma, not allergies.
Allergy management may include antihistamines, corticosteroids, and allergen avoidance strategies.
Educating the child and family on a comprehensive approach to allergy management is crucial.
A client is experiencing asthma symptoms and seeks advice on managing their condition.
What advice should the nurse provide regarding asthma management?
Explanation
Choice A rationale:
Asthma attacks can be relieved with quick-relief medications (not long-term control medications), but this advice focuses on symptom management rather than addressing the root causes of asthma symptoms.
Long-term control medications are used to prevent symptoms over time, not for immediate relief.
Choice B rationale:
Using inhalers and nebulizers only during asthma exacerbations is not a recommended approach to asthma management.
Asthma management often involves both long-term control medications and quick-relief medications.
Using inhalers and nebulizers during exacerbations is essential, but they can also be part of a daily management plan for some individuals.
Choice C rationale:
Regular monitoring of lung function is essential for managing asthma.
Monitoring helps assess the effectiveness of treatment and allows for adjustments to the management plan as needed.
Neglecting regular monitoring can lead to uncontrolled asthma and worsening symptoms.
Which interventions are appropriate for the nurse to include in the education? Select all that apply.
Explanation
Choice A rationale:
Administering antihistamines regularly to prevent allergic reactions is not a recommended intervention.
Antihistamines are typically used to manage allergic reactions when they occur, but they are not a preventive measure.
Using them regularly without symptoms can lead to unnecessary medication use and potential side effects.
Choice B rationale:
Educating the child and their family about allergen avoidance strategies, such as dust mite control, is a crucial part of managing allergies.
Dust mites are a common allergen, and reducing exposure to them can help prevent allergic reactions.
Teaching families how to create an allergen-free environment is an essential component of allergy management.
Choice C rationale:
Teaching the use of an epinephrine auto-injector for severe allergic reactions is a vital skill for families with children who have allergies.
Anaphylaxis can be life-threatening, and having an epinephrine auto-injector on hand and knowing how to use it can save a child's life in case of a severe allergic reaction.
Choice D rationale:
Recommending immunotherapy (allergy shots) for all children with allergies is not a standard practice.
Immunotherapy is typically reserved for individuals with severe allergies that do not respond to other treatments.
It involves a series of injections to desensitize the individual to specific allergens and is not suitable for all children with allergies.
Choice E rationale:
Providing emotional support to help the child cope with the impact of allergies is a critical aspect of care.
Allergies can have a significant impact on a child's quality of life, and emotional support can help them manage the emotional and psychological aspects of living with allergies.
What advice should the nurse provide regarding asthma trigger management?
Explanation
Choice A rationale:
Stating that regular follow-up visits are not necessary for asthma control is incorrect.
Regular follow-up visits are essential to monitor asthma control, adjust medications if needed, and provide ongoing education and support to the client.
It is important to assess and manage asthma continuously.
Choice B rationale:
Claiming that quick-relief medications are the mainstay of asthma management is not accurate.
While quick-relief medications (such as short-acting beta-agonists) are crucial for relieving acute asthma symptoms, the mainstay of asthma management involves long-term control medications to prevent exacerbations and reduce airway inflammation.
Choice C rationale:
Teaching the child and family about asthma triggers and how to avoid them is The correct advice.
Identifying and avoiding asthma triggers, such as allergens or irritants, is a key component of asthma management.
This education can help prevent asthma exacerbations and improve overall control.
Choice D rationale:
Suggesting that long-term control medications are used to reduce airway inflammation is accurate.
Long-term control medications, such as inhaled corticosteroids, are prescribed to reduce airway inflammation and prevent asthma symptoms.
These medications are an integral part of asthma management.
Which components should be included in the asthma action plan?
Explanation
Choice A rationale:
Including steps to take during asthma exacerbations in the asthma action plan is essential.
This guidance helps the child and their family know what to do in case of worsening symptoms or an asthma attack.
Knowing the appropriate steps to take can prevent complications and ensure timely intervention.
Choice B rationale:
Recommending avoidance of all physical activity to prevent asthma symptoms is not appropriate.
Physical activity is crucial for overall health, and children with asthma can and should participate in activities.
Asthma management should focus on controlling symptoms, not restricting physical activity.
Choice C rationale:
Using long-term control medications as needed during asthma attacks is not an effective strategy.
Long-term control medications are typically used on a daily basis to maintain asthma control and prevent exacerbations.
Quick-relief medications are used during attacks to provide immediate relief.
Choice D rationale:
Stating that regular monitoring of lung function is unnecessary for effective asthma management is inaccurate.
Regular lung function monitoring, such as peak flow measurements or spirometry, is a valuable tool for assessing asthma control and adjusting treatment as needed.
It is an important part of managing asthma effectively.
Diabetes Mellitus in Children
Which statement by the nurse accurately explains one of the causes of diabetes mellitus in children?
Explanation
Choice A rationale:
The statement mentions that children with a family history of diabetes have an increased risk of developing the condition.
While family history is a risk factor for diabetes, it doesn't explain the causes of diabetes mellitus in children.
It only highlights one of the risk factors.
Choice B rationale:
This statement accurately explains one of the causes of diabetes mellitus in children.
In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
This immune-mediated destruction of beta cells is a key factor in the development of type 1 diabetes in children.
Choice C rationale:
This statement mentions that certain viral infections and dietary factors may trigger the development of diabetes in susceptible individuals.
Choice D rationale:
This statement is more relevant to type 2 diabetes as it mentions a combination of insulin resistance and impaired insulin secretion.
Which statement by the nurse accurately describes the pathophysiology of diabetes mellitus in children?
Explanation
Choice A rationale:
This statement accurately describes the pathophysiology of diabetes mellitus in children.
Insufficient insulin results in elevated blood glucose levels, leading to the characteristic symptoms of diabetes.
In type 1 diabetes, there is a lack of insulin due to the destruction of insulin-producing beta cells by the immune system.
Choice B rationale:
This statement incorrectly suggests that there is a combination of insulin resistance and impaired insulin secretion in type 1 diabetes.
In reality, type 1 diabetes is characterized by a lack of insulin production due to the destruction of beta cells by the immune system.
Choice C rationale:
This statement inaccurately states that in type 2 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
This description is more aligned with type 1 diabetes, not type 2 diabetes.
Choice D rationale:
This statement falsely claims that certain viral infections and dietary factors are the sole causes of diabetes in children.
While these factors can contribute to the development of diabetes, they are not the sole causes, and this oversimplification doesn't accurately represent the pathophysiology of diabetes mellitus in children.
Select all the factors that increase the risk of diabetes in children.
Explanation
Choice A rationale:
Genetic factors play a significant role in increasing the risk of diabetes in children.
If there is a family history of diabetes, the genetic predisposition can contribute to the development of the condition.
Choice B rationale:
Autoimmune destruction of beta cells is a risk factor for type 1 diabetes in children.
In this condition, the immune system attacks and destroys the insulin-producing beta cells in the pancreas, leading to a lack of insulin.
Choice C rationale:
Insulin resistance is a risk factor for type 2 diabetes in children.
It is characterized by the body's reduced response to insulin, leading to elevated blood glucose levels.
Choice D rationale:
Lack of physical activity is a modifiable risk factor for both type 1 and type 2 diabetes.
However, it is more strongly associated with type 2 diabetes, and it's not a primary risk factor for diabetes in children.
Choice E rationale:
Environmental factors can also contribute to the risk of diabetes in children.
These factors may include dietary choices, exposure to certain toxins, and lifestyle factors, among others.
Which factor mentioned in the text contributes to an increased risk of diabetes mellitus in children with a family history of the disease?
Explanation
Choice A rationale:
Genetic factors play a significant role in the development of diabetes mellitus, especially when there is a family history of the disease.
People with a family history of diabetes are at a higher risk of developing the condition due to the inheritance of certain genes that predispose them to diabetes.
These genetic factors can influence insulin production, insulin sensitivity, and glucose regulation.
The genetic component of diabetes is well-established, and research has identified specific genes associated with both type 1 and type 2 diabetes.
It's important to educate the client about the importance of monitoring their blood sugar levels and adopting a healthy lifestyle to reduce their risk, given their family history.
Choice B rationale:
Autoimmune destruction of beta cells is more associated with type 1 diabetes rather than a family history of the disease.
Type 1 diabetes is an autoimmune condition in which the body's immune system mistakenly targets and destroys the insulin-producing beta cells in the pancreas.
While this is a critical factor in type 1 diabetes, it is not typically linked to family history as a primary risk factor.
Choice C rationale:
Insufficient insulin is a consequence of diabetes rather than a risk factor.
In diabetes, the problem is usually related to the body's inability to produce enough insulin (in type 1 diabetes) or effectively use the insulin produced (in type 2 diabetes).
Insufficient insulin is a result of the disease, not a contributing factor related to family history.
Choice D rationale:
Lack of physical activity can be a risk factor for diabetes, especially type 2 diabetes, but it is not the primary factor associated with a family history of the disease.
Lack of physical activity may contribute to the development of diabetes in individuals who are already at risk due to genetic factors or other lifestyle-related factors.
It's essential to promote physical activity and a healthy lifestyle, but this is not the primary risk factor in the context of family history.
Which statement by the nurse is accurate in explaining the role of viral infections in the development of diabetes?
Explanation
Choice A rationale:
Stating that viral infections are the primary cause of diabetes in children is inaccurate.
While viral infections can play a role in the development of diabetes, they are not the primary cause.
Diabetes has multifactorial causes, including genetic predisposition, lifestyle factors, and viral infections are only one of several potential triggers.
Choice C rationale:
Suggesting that viral infections only lead to insulin resistance in children is an oversimplification.
Viral infections can have various effects on the development of diabetes, and it's not limited to insulin resistance.
The relationship between viral infections and diabetes is complex and can involve factors like inflammation and autoimmunity.
Choice D rationale:
Diabetes is associated with viral infections, especially in certain cases.
However, stating that diabetes is not associated with viral infections in any way is incorrect.
Viral infections can sometimes trigger an autoimmune response that damages pancreatic beta cells or cause inflammation that affects insulin sensitivity.
Therefore, it's essential to acknowledge the potential link between viral infections and diabetes, particularly in susceptible individuals.
The child complains of excessive thirst and increased urination.
Which statement by the nurse is appropriate for addressing the child's concern?
Explanation
Choice A rationale:
Telling the child to drink less water to control urination is not an appropriate response.
Excessive thirst and increased urination are common symptoms of diabetes, and they occur because the body is trying to get rid of excess glucose through urine.
Dehydration is a concern in diabetes, so advising the child to drink less water is not advisable.
Choice B rationale:
Explaining to the child that these symptoms are due to their body having trouble using glucose properly is an accurate and appropriate response.
Excessive thirst and increased urination are classic symptoms of diabetes mellitus.
When the body cannot use glucose effectively, it tries to eliminate excess glucose through urine, leading to increased urination and subsequent thirst to combat dehydration.
Choice C rationale:
Suggesting that the child should eat more to satisfy their increased hunger is not an appropriate response.
Increased hunger can also be a symptom of diabetes, and advising the child to eat more without addressing the underlying issue of glucose regulation is not helpful.
Choice D rationale:
Weight loss is often an early symptom of diabetes, and it occurs because the body is unable to properly utilize glucose for energy.
A nurse is assessing a child with diabetes mellitus.
Which components should be included in the psychosocial assessment of the child?
Explanation
A. "Evaluate the child's emotional well-being.”.
D. "Obtain a detailed history, including family history of diabetes.”.
E. "Regularly monitor blood glucose levels to assess glycemic control.”.
Choice A rationale:
Evaluate the child's emotional well-being.
Assessing the emotional well-being of a child with diabetes is crucial because living with a chronic condition can have a significant impact on a child's mental health.
Children may experience stress, anxiety, and other emotional challenges related to their condition.
This assessment helps in providing comprehensive care and support to the child.
Choice B rationale:
Assess for signs of hyperglycemia, such as polyuria.
While assessing for signs of hyperglycemia, such as polyuria, is important in managing diabetes, it is primarily a physical assessment and not a psychosocial assessment.
It focuses on the physiological aspects of the condition.
Choice C rationale:
Monitor growth patterns and assess for any delays.
Monitoring growth patterns and assessing for delays in a child's development is important but is also primarily a physical assessment.
It is not a direct component of the psychosocial assessment, although it may indirectly impact a child's emotional well-being.
Choice D rationale:
Obtain a detailed history, including family history of diabetes.
Obtaining a detailed history, including a family history of diabetes, is a crucial part of the assessment.
Family history can be a significant risk factor for the development of diabetes in a child.
Understanding the family history helps in identifying potential genetic predispositions.
Choice E rationale:
Regularly monitor blood glucose levels to assess glycemic control.
Regularly monitoring blood glucose levels is essential in managing diabetes.
While it is a key aspect of diabetes care, it primarily falls under the category of physiological monitoring rather than a direct component of psychosocial assessment.
The nurse explains the oral glucose tolerance test to the client.
Which statement by the nurse is accurate?
Explanation
"A glucose level ≥200 mg/dL two hours after a glucose load confirms the diagnosis.”.
Choice A rationale:
A glucose level ≥100 mg/dL two hours after a glucose load confirms the diagnosis.
This statement is incorrect.
A glucose level of 100 mg/dL two hours after a glucose load is not sufficient to confirm the diagnosis of diabetes.
The diagnostic criteria for diabetes typically involve higher glucose levels.
Choice B rationale:
A glucose level ≥180 mg/dL one hour after a glucose load indicates diabetes.
This statement is incorrect.
While a glucose level of 180 mg/dL one hour after a glucose load may be elevated, it is not enough to confirm a diagnosis of diabetes.
The diagnostic criteria for diabetes primarily involve glucose levels at the two-hour mark.
Choice C rationale:
A glucose level ≥200 mg/dL two hours after a glucose load confirms the diagnosis.
This statement is correct.
The oral glucose tolerance test (OGTT) is a diagnostic test for diabetes, and the ADA diagnostic criteria specify that a glucose level of 200 mg/dL or higher at the two-hour mark after a glucose load confirms the diagnosis of diabetes.
This threshold is used to ensure accurate diagnosis.
Choice D rationale:
A glucose level ≥250 mg/dL one hour after a glucose load suggests uncontrolled diabetes.
This statement is not part of the diagnostic criteria for diabetes.
While a glucose level of 250 mg/dL one hour after a glucose load is elevated, it is not used to confirm the diagnosis of diabetes.
The diagnostic threshold is typically set at the two-hour mark.
The child has complained of increased hunger despite increased appetite.
How should the nurse respond to address the child's concern?
Explanation
Choice A rationale:
"This hunger is a normal part of growing up.”.
This response is not appropriate.
Increased hunger in a child with diabetes is not a normal part of growing up.
It is essential to provide accurate information and address the child's concerns.
Choice B rationale:
"Increased hunger is a result of the body's inability to utilize glucose properly.”.
This is The correct response.
Increased hunger in diabetes is often due to the body's inability to use glucose properly.
When insulin is deficient or not functioning effectively, the cells cannot take up glucose for energy, leading to increased hunger.
Providing this information helps the child understand the physiological basis of their hunger.
Choice C rationale:
"You should eat smaller, more frequent meals to control your hunger.”.
While this advice can be helpful for managing blood sugar levels in diabetes, it doesn't address the cause of increased hunger.
It is essential to explain the underlying reasons for the symptom.
Choice D rationale:
"This is a side effect of the medication you're taking.”.
This response is not accurate.
Increased hunger in diabetes is primarily related to glucose metabolism and insulin deficiency, not a medication side effect.
Which of the following statements is essential for the nurse to include in the education process?
Explanation
Choice A rationale:
"You should avoid any physical activity to keep your blood glucose levels stable.”.
This statement is incorrect.
Physical activity is essential for managing diabetes as it helps lower blood glucose levels.
Advising the child to avoid physical activity is not appropriate.
Choice B rationale:
"Insulin injections are not necessary; you can manage diabetes with diet alone.”.
This statement is misleading and potentially dangerous.
Insulin is a crucial treatment for many individuals with diabetes, and suggesting that it is not necessary can have severe consequences.
Diet alone is not sufficient to manage diabetes for most individuals.
Choice C rationale:
"Regular blood glucose monitoring is important to assess glycemic control.”.
This is The correct response.
Regular blood glucose monitoring is crucial in diabetes management.
It allows the child and their family to assess how well they are managing blood sugar levels and make necessary adjustments to their treatment plan.
Choice D rationale:
"Eating as much sugar as you want won't affect your diabetes.”.
This statement is false.
Consuming excessive sugar can significantly impact blood glucose levels, and individuals with diabetes should be mindful of their sugar intake.
Providing this information is essential for the child and their family to make informed choices.
What should the nurse explain about the primary treatment for children with diabetes mellitus?
Explanation
Choice A rationale:
"The primary treatment for children with diabetes is insulin therapy.”.
This is The correct response.
Insulin therapy is the primary treatment for type 1 diabetes in children and may also be necessary for some with type 2 diabetes.
It is crucial to explain this to the client accurately.
Choice B rationale:
"Children with diabetes can manage their condition solely through dietary modifications.”.
This statement is not accurate.
While diet plays a significant role in diabetes management, it is not the sole treatment.
Insulin or other medications may be necessary, depending on the type and severity of diabetes.
Choice C rationale:
"Regular physical activity is the primary treatment for diabetes in children.”.
While physical activity is essential for diabetes management, it is not the primary treatment.
Insulin therapy or other medications take precedence, and physical activity complements the treatment plan.
Choice D rationale:
"Blood glucose monitoring is not necessary for managing diabetes in children.”.
This statement is incorrect.
Blood glucose monitoring is a crucial part of diabetes management, allowing the child and their healthcare team to make informed decisions about treatment and lifestyle adjustments.
A nurse is educating a patient and their family about DKA.
What should the nurse emphasize regarding DKA prevention?
Explanation
Choice A rationale:
Insulin is a crucial part of managing diabetes, especially in the case of diabetic ketoacidosis (DKA).
It helps lower blood sugar levels and counteracts the effects of high blood glucose, which is characteristic of DKA.
Avoiding insulin at all costs is not an appropriate approach as it can lead to worsening of DKA.
Choice B rationale:
The nurse should emphasize the need for frequent monitoring of blood glucose levels.
This is because DKA is associated with significantly elevated blood glucose levels.
Regular monitoring allows for timely adjustments in insulin and other treatments, reducing the risk of complications.
Monitoring blood glucose levels is a fundamental aspect of diabetes management.
Choice C rationale:
Consuming a high-carbohydrate diet is not advisable in the context of DKA prevention.
High-carbohydrate diets can lead to elevated blood sugar levels, which may exacerbate the risk of DKA.
It's essential to maintain a balanced and controlled carbohydrate intake for individuals with diabetes.
Choice D rationale:
Avoiding follow-up appointments is not a suitable approach for DKA prevention.
Regular follow-up appointments with healthcare providers are essential for monitoring and adjusting the diabetes management plan.
Skipping follow-up appointments can lead to uncontrolled blood sugar levels and an increased risk of DKA.
The nurse tells the parent that the child should eat regular meals and snacks throughout the day.
Which of the following statements by the parent demonstrates that they understand the nurse's teaching?
Explanation
Choice A rationale:
Eating three large meals per day may not be the best approach for managing blood sugar levels in a child with diabetes.
Spacing meals and snacks throughout the day can help stabilize blood glucose levels and prevent large fluctuations.
It's important to maintain a balanced eating pattern.
Choice B rationale:
Providing snacks every two hours, even if the child is not hungry, may lead to overconsumption and could potentially affect blood sugar levels.
Regular, balanced snacks are essential, but they should be based on the child's hunger and in accordance with the diabetes management plan.
Choice C rationale:
This statement demonstrates a good understanding of the nurse's teaching.
Offering a variety of healthy foods and drinks throughout the day helps maintain stable blood sugar levels and provides necessary nutrients.
It aligns with the principles of diabetes management.
Choice D rationale:
Avoiding sugary foods and drinks is important for DKA prevention, but this statement doesn't directly address the need for regular meals and snacks, which is the main focus of the nurse's teaching.
While avoiding sugary items is crucial, overall dietary balance is essential.
A nurse is caring for a child with DKA.
The child's blood glucose level is 300 mg/dL (16.7 mmol/L).
The nurse has started an intravenous insulin infusion and is monitoring the child's blood glucose levels closely.
Which of the following assessment findings would indicate that the child's DKA is improving?
Select all that apply.
Explanation
Choice A rationale:
A decrease in the child's blood glucose level from 300 mg/dL to 250 mg/dL would indicate an improvement in DKA.
This is because DKA is characterized by hyperglycemia, and a decrease in blood glucose levels shows that the insulin infusion is working to correct the high blood sugar.
The normal range for blood glucose levels in children is typically 70-140 mg/dL, so 250 mg/dL is still high but represents an improvement.
Choice B rationale:
A decrease in ketones in the urine is another positive sign in the management of DKA.
Ketones in the urine are a sign of metabolic acidosis, which is a hallmark of DKA.
A reduction in ketones indicates that the body is shifting away from using fats for energy and is starting to correct the metabolic derangement.
It's important to note that ketone levels are usually assessed qualitatively as negative, trace, small, moderate, or large, and a decrease from a higher level to a lower level is a positive sign.
Choice C rationale:
An increase in the respiratory rate is not typically an indicator of DKA improvement.
In fact, during DKA, the respiratory rate may increase as the body tries to compensate for the acidosis by blowing off carbon dioxide through rapid breathing.
Therefore, a further increase in respiratory rate may not necessarily be a sign of improvement.
Monitoring the respiratory rate is essential, but it doesn't directly indicate the resolution of DKA.
Choice D rationale:
An increase in pH is a significant indicator of DKA improvement.
In DKA, the blood becomes acidic due to the accumulation of ketones and the decreased pH levels.
An increase in pH levels suggests that the acidosis is being corrected, which is a positive sign in the management of DKA.
Normal blood pH levels for children typically range from 7.35 to 7.45.
Choice E rationale:
A decrease in bicarbonate levels is not a sign of DKA improvement.
In DKA, bicarbonate levels are typically low due to the acidosis.
As treatment progresses and the acidosis resolves, bicarbonate levels may start to increase, indicating improvement.
Therefore, a decrease in bicarbonate levels would not be a positive sign in this context.
The child is lethargic and has a headache.
The nurse assesses the child's vital signs and finds that the blood pressure is elevated and the respiratory rate is slow.
Which of the following interventions should the nurse take first?
Explanation
Choice B rationale:
Elevating the head of the bed 30 degrees is the most appropriate initial intervention for a child with DKA experiencing cerebral edema.
Cerebral edema is a serious complication of DKA, and it can lead to increased intracranial pressure.
Elevating the head of the bed helps to reduce intracranial pressure by promoting venous drainage from the brain.
This intervention should be initiated promptly to help alleviate the symptoms and prevent further complications.
Administering mannitol (choice A) or oxygen (choice C) can be considered later, but elevating the head of the bed is the priority.
Monitoring vital signs (choice D) is important but not the first action in addressing elevated intracranial pressure.
The nurse meets with the child's parents to discuss the child's discharge plan and answer any questions they may have.
Which of the following topics should the nurse include in the discharge plan?
Select all that apply.
Explanation
Choice A rationale:
Teaching parents how to monitor the child's blood glucose levels at home is essential in the discharge plan for a child with DKA.
It empowers parents to manage their child's condition and ensure that blood glucose levels are within a safe range.
Home monitoring is crucial for preventing recurrence and managing diabetes effectively.
Choice B rationale:
Instructing parents on how to give the child insulin injections is another critical aspect of the discharge plan.
Children with DKA often require insulin therapy to manage their blood glucose levels.
Proper administration of insulin is essential to prevent hyperglycemia and DKA recurrence.
Choice C rationale:
Educating parents on what to do if the child develops symptoms of DKA, such as abdominal pain, nausea, and vomiting, is important.
Recognizing the early signs of DKA and seeking medical attention promptly is crucial to prevent the condition from worsening.
Teaching parents to be vigilant for these symptoms can help prevent DKA recurrence.
Choice D rationale:
Preventing the child from developing DKA again in the future is a crucial part of the discharge plan.
While this is a broad goal, it can encompass education on various aspects, such as the importance of insulin compliance, regular medical check-ups, and diabetes management strategies.
Preventing recurrence is a primary objective of DKA management.
Choice E rationale:
Providing information on how to contact the child's healthcare provider if parents have any questions or concerns is essential.
Open communication with healthcare providers is vital for ongoing support, guidance, and adjustments to the child's diabetes management plan.
A nurse is reviewing the medical history of a child suspected of having Diabetic Ketoacidosis (DKA).
The nurse notes that the child has had previous episodes of DKA, a diagnosis of diabetes, and recent changes in medication.
The nurse also notes recent illnesses and infections that may have contributed to the development of DKA.
Which of the following statements should the nurse make to the child’s parents?
Explanation
Choice A rationale:
The nurse should not tell the child's parents that their child's condition is stable and that there is no need for concern.
This is not an accurate assessment, especially when there are recent changes in medication, a diagnosis of diabetes, and a history of previous episodes of Diabetic Ketoacidosis (DKA).
It is important to address the potential issues that might have contributed to the development of DKA.
Choice B rationale:
This is The correct choice.
The nurse should inform the child's parents that the recent changes in their child's medication may have contributed to the situation.
Medication changes can affect blood glucose levels and, in some cases, lead to DKA.
It's essential to consider all possible factors contributing to the condition.
Choice C rationale:
Telling the child's parents that their child's diabetes diagnosis is incorrect is not appropriate, as there is already a confirmed diagnosis of diabetes.
DKA is a complication of diabetes, and addressing the current situation is more important than questioning the diagnosis itself.
Choice D rationale:
Accusing the child of not taking their medication correctly without proper evidence is not a good approach.
It's important to investigate the medication changes and other factors before making such an assumption.
Which statement about fluid resuscitation is correct?
Explanation
"We'll administer 0.9% saline to restore intravascular volume.”.
Choice A rationale:
The statement "We'll administer 0.9% saline to restore intravascular volume" is correct.
In the management of DKA, fluid resuscitation is a crucial initial step to restore intravascular volume.
What is an essential aspect of patient and family education in DKA care?
Explanation
Choice A rationale:
Education on insulin therapy is a fundamental aspect of DKA management.
Insulin is a crucial component in treating DKA as it helps lower elevated blood glucose levels and corrects the ketosis and acidosis.
It is essential for the patient and their family to understand how insulin works, how to administer it, and when to administer it.
Proper insulin therapy can prevent further complications and guide the management of DKA.
Choice B rationale:
Focusing solely on dietary recommendations is not appropriate in the initial management of DKA.
While dietary management is important for long-term diabetes care, it is not the primary focus during the acute phase of DKA.
The priority is to address the high blood glucose levels and ketoacidosis, which is best achieved through insulin therapy and fluid resuscitation.
Choice C rationale:
Avoiding discussions about blood glucose monitoring is not recommended.
Blood glucose monitoring is a critical aspect of DKA management.
It helps healthcare providers determine the effectiveness of insulin therapy and the patient's response to treatment.
Avoiding these discussions would be detrimental to the patient's care.
Choice D rationale:
Neglecting to mention the risk of cerebral edema is not appropriate in DKA education.
Cerebral edema is a severe complication of DKA that can be life-threatening.
It is crucial to inform the patient and their family about this risk so they can seek prompt medical attention if symptoms occur.
Neglecting to mention this risk could lead to delayed treatment and potential harm to the patient.
The client asks the nurse about the reason for frequent monitoring of blood glucose and electrolyte levels.
Which of the following responses should the nurse give?
Explanation
Choice A rationale:
Frequent monitoring is not primarily done to adjust the diet plan.
While monitoring can provide information about the patient's nutritional needs, the primary purpose of monitoring in DKA is to assess the effectiveness of insulin therapy and to guide electrolyte replacement.
Choice B rationale:
Monitoring blood glucose and electrolyte levels helps guide insulin and electrolyte replacement therapy in DKA.
It allows healthcare providers to make necessary adjustments in insulin dosing and electrolyte replacement to ensure the patient's safety and a successful recovery.
Choice C rationale:
Frequent monitoring is not primarily aimed at checking for allergic reactions to insulin.
Allergic reactions to insulin are relatively rare, and monitoring is mainly done to assess treatment effectiveness and the patient's response to therapy.
Choice D rationale:
Monitoring is not a standard procedure for all patients regardless of their condition.
It is essential in DKA management, but it is not universally applicable to all patients.
Monitoring is performed based on the patient's specific condition and treatment needs.
A nurse is preparing an education session for staff nurses about the treatment and management of DKA in children.
Which of the following points should be included in the session? (Select all that apply).
Explanation
Choice A rationale:
Fluid resuscitation with 0.9% saline is indeed a crucial part of the initial management of diabetic ketoacidosis (DKA).
DKA often results in severe dehydration due to excessive urination and can lead to a state of shock.
The administration of normal saline helps to rehydrate the patient and restore adequate blood volume.
Choice B rationale:
Electrolyte imbalances, especially hypokalemia, are common in DKA.
When a person has DKA, there is a significant loss of fluids and electrolytes through excessive urination.
This loss can lead to low potassium levels, which can be life-threatening.
Therefore, monitoring and correcting electrolyte imbalances, including potassium, is essential in the treatment of DKA.
Choice C rationale:
Insulin therapy is crucial in the treatment of DKA.
This choice is incorrect because insulin helps to reverse the metabolic processes that lead to ketone formation and hyperglycemia in DKA.
By administering insulin, the body can utilize glucose for energy, reduce blood glucose levels, and stop the production of ketones.
Choice D rationale:
Monitoring blood glucose and electrolyte levels is essential during the treatment of DKA.
Frequent monitoring allows healthcare providers to assess the effectiveness of treatment, make necessary adjustments, and ensure the patient's safety.
It helps in tracking the response to insulin therapy and The correction of electrolyte imbalances.
Choice E rationale:
Children with DKA are indeed at risk for complications.
This choice is incorrect because DKA can lead to a range of complications, including cerebral edema, which is more common in children.
Cerebral edema is a severe and potentially life-threatening complication that highlights the importance of vigilant management and monitoring in pediatric DKA cases.
A nurse is reviewing a care plan for a child with DKA.
The care plan includes interventions such as fluid resuscitation, electrolyte replacement, insulin therapy, and monitoring for complications.
The nurse understands that these interventions are aimed at:
Explanation
All of these.
Choice A rationale:
Correcting fluid and electrolyte imbalances is an essential part of the care plan for a child with DKA.
This is because DKA often leads to severe dehydration and electrolyte imbalances due to excessive urination.
Restoring fluid and electrolyte balance is crucial to stabilize the patient's condition.
Choice B rationale:
Reducing hyperglycemia is a critical goal in the care of a child with DKA.
Elevated blood glucose levels are a hallmark of DKA, and addressing hyperglycemia is achieved through insulin therapy.
Reducing hyperglycemia helps to stop the production of ketones and normalize metabolic processes.
Choice C rationale:
Preventing complications is an important aspect of managing DKA.
Complications such as cerebral edema and organ dysfunction can occur if DKA is not promptly and effectively treated.
Therefore, monitoring for and taking steps to prevent complications is a fundamental component of the care plan.
Choice D rationale:
The correct answer is "All of these" because the care plan for a child with DKA includes interventions that address fluid and electrolyte imbalances, hyperglycemia, and complications.
These interventions work together to stabilize the patient's condition and prevent further deterioration.
The nurse should explain that:.
Explanation
Potassium replacement is done to prevent hypokalemia, which is common in DKA.
Choice A rationale:
Potassium replacement is indeed necessary in DKA treatment.
This choice is incorrect because DKA often leads to hypokalemia (low potassium levels).
Potassium is an essential electrolyte for various bodily functions, including proper heart function, and low levels can be life-threatening.
Therefore, potassium replacement is a vital part of DKA treatment.
Choice B rationale:
The primary reason for potassium replacement in DKA is to prevent hypokalemia.
As mentioned earlier, DKA leads to excessive urination, which results in the loss of potassium and other electrolytes.
Hypokalemia can lead to cardiac arrhythmias and muscle weakness.
Therefore, replenishing potassium is crucial to maintaining normal physiological functions.
Choice C rationale:
Potassium replacement is not done to treat hyperkalemia in DKA.
DKA typically leads to hypokalemia, not hyperkalemia.
Hyperkalemia, or high potassium levels, is a less common complication in DKA.
Treating hyperkalemia may involve different interventions, but it is not the primary reason for potassium replacement in DKA.
Choice D rationale:
Potassium replacement is not done solely based on the client's request.
It is a medical decision made by healthcare providers based on clinical assessment and laboratory values.
Ignoring potassium replacement in DKA could lead to severe complications, so it is not a matter of personal preference.
Which dietary principles should the nurse recommend for glycemic control in children with diabetes?
Explanation
Choice A rationale:
Carbohydrate counting and portion control.
Carbohydrate counting and portion control are essential dietary principles for glycemic control in children with diabetes.
Carbohydrates have a significant impact on blood sugar levels, so teaching children and their families how to count carbohydrates and control portion sizes helps them manage their blood glucose levels more effectively.
By knowing the amount of carbohydrates in their meals, children can adjust their insulin or medication doses accordingly, promoting better glycemic control.
Choice B rationale:
Unlimited sugar intake for quick energy.
Unlimited sugar intake is not a recommended dietary principle for children with diabetes.
Consuming excessive amounts of sugar can lead to rapid spikes in blood sugar levels, making it difficult to maintain stable glycemic control.
It can also contribute to the development of long-term complications associated with diabetes.
Therefore, it is important to limit sugar intake and choose healthier carbohydrate sources.
Choice C rationale:
High-fat, low-carbohydrate diet.
A high-fat, low-carbohydrate diet is not a suitable dietary recommendation for children with diabetes.
Such a diet may lead to increased fat accumulation and negatively affect glycemic control.
It is important to focus on balanced and moderate carbohydrate intake, as well as selecting healthy fats in the diet.
A diet rich in healthy carbohydrates, lean proteins, and good fats is more appropriate for children with diabetes.
Choice D rationale:
Avoiding all carbohydrates in the diet.
Avoiding all carbohydrates in the diet is not a practical or safe approach for children with diabetes.
Carbohydrates are a primary source of energy, and completely eliminating them from the diet can lead to nutrient deficiencies and other health issues.
The goal is to manage carbohydrate intake, not eliminate it entirely.
Choice E rationale:
Random and irregular meal times.
Random and irregular meal times are not recommended for children with diabetes.
Consistency in meal timing is crucial to maintain stable blood sugar levels.
It helps synchronize food intake with insulin or medication administration, making it easier to control blood glucose.
Irregular meal times can lead to fluctuations in blood sugar levels, which are undesirable for children with diabetes.
What should the nurse emphasize regarding insulin types used in the management of diabetes in children?
Explanation
Choice A rationale:
"Children with diabetes should never use insulin pumps.”.
This statement is not accurate.
Insulin pumps can be a valuable tool in the management of diabetes in children.
Insulin pumps provide continuous subcutaneous insulin delivery, offering a more flexible and precise way to administer insulin.
They can be particularly beneficial for children who require multiple daily injections or have difficulty with insulin injections.
Choice B rationale:
"Insulin therapy is not a significant part of diabetes management in children.”.
Insulin therapy is a significant and often essential part of diabetes management in children, especially for those with type 1 diabetes.
Children with type 1 diabetes do not produce insulin and require lifelong insulin therapy to survive.
It plays a crucial role in maintaining glycemic control and preventing complications.
Choice C rationale:
"There are different types of insulin, including rapid-acting and long-acting.”.
This statement is accurate.
Children with diabetes may require different types of insulin to manage their blood sugar effectively.
Rapid-acting insulin is used to cover meals and correct high blood sugar levels, while long-acting insulin provides basal insulin to keep blood sugar stable between meals and overnight.
Understanding the different types of insulin and their respective roles is essential for proper diabetes management.
Choice D rationale:
"Children with diabetes only need short-acting insulin.”.
This statement is not accurate.
While short-acting insulin (rapid-acting) is necessary for mealtime coverage, it is not the only type of insulin children may need.
Long-acting insulin is crucial for providing a basal level of insulin throughout the day and night.
Children with diabetes often require both short-acting and long-acting insulin to achieve optimal glycemic control.
What should the nurse explain about the prevention of complications in children with diabetes mellitus?
Explanation
Choice A rationale:
"Acute complications like hypoglycemia cannot be prevented in children.”.
Hypoglycemia is an acute complication of diabetes that can be prevented and managed.
Education on recognizing and treating low blood sugar episodes, monitoring blood glucose levels, and adjusting insulin or medications appropriately can significantly reduce the risk of hypoglycemia in children with diabetes.
Choice B rationale:
"Long-term complications such as retinopathy and nephropathy are not a concern for children.”.
Long-term complications like retinopathy (eye problems) and nephropathy (kidney problems) can affect children with diabetes, especially if their blood sugar levels are poorly controlled over time.
It is essential to emphasize the importance of glycemic control and regular medical check-ups to monitor for early signs of these complications and take preventive measures.
Choice C rationale:
"Strategies can be implemented to prevent both acute and long-term complications.”.
This is The correct answer.
Strategies can be implemented to prevent both acute and long-term complications in children with diabetes.
These strategies include maintaining good glycemic control through proper insulin management, following a healthy diet, engaging in regular physical activity, and regular medical follow-ups.
Preventive measures, such as eye and kidney screenings, can also help detect potential issues early and intervene appropriately.
Choice D rationale:
"There is no need for regular follow-up visits to monitor glycemic control.”.
Regular follow-up visits to monitor glycemic control are essential for children with diabetes.
These visits allow healthcare professionals to assess the child's blood sugar management, adjust treatment plans as needed, and provide ongoing education and support.
Skipping follow-up visits can increase the risk of complications and hinder effective diabetes management.
Explanation
Dehydration.
Choice A rationale:
Hypovolemia Hypovolemia refers to a decreased blood volume and can lead to decreased urine output.
However, in the context of a patient with suspected DKA, the primary concern is dehydration due to excessive loss of fluids and electrolytes through polyuria (excessive urination) and osmotic diuresis.
This leads to dehydration rather than hypovolemia.
Choice B rationale:
Hyperglycemia Hyperglycemia is a characteristic feature of DKA, but it doesn't directly cause decreased urine output.
In fact, hyperglycemia often leads to increased urine output due to the osmotic diuresis caused by high blood glucose levels.
Choice D rationale:
Prolonged capillary refill time Prolonged capillary refill time is a sign of poor perfusion and can be associated with hypovolemia.
However, it is not the primary concern in a patient with suspected DKA who is experiencing dehydration.
The decreased urine output is primarily due to the loss of fluids and electrolytes from hyperglycemia and osmotic diuresis.
Now, let's move on to the next question.
What does this finding indicate about the patient's condition?
Explanation
Hyperglycemia.
Choice A rationale:
Hypoglycemia A blood glucose level of 250 mg/dL is not indicative of hypoglycemia.
Hypoglycemia is defined as low blood glucose levels typically below 70 mg/dL.
In DKA, the primary concern is hyperglycemia, and blood glucose levels are significantly higher than normal.
Choice C rationale:
Normoglycemia A blood glucose level of 250 mg/dL is above the normal range, which typically falls between 70 and 100 mg/dL.
Therefore, it does not indicate normoglycemia.
Hyperglycemia is the characteristic feature of DKA.
Choice D rationale:
Ketonuria While ketonuria is often present in DKA, the finding of a blood glucose level of 250 mg/dL primarily indicates hyperglycemia.
Ketonuria is assessed through urinalysis and relates to the presence of ketones in the urine, which is a common feature of DKA along with hyperglycemia.
What should the nurse do regarding potassium replacement?
Explanation
Choice A rationale:
Initiating potassium replacement once urine output is established and serum potassium levels are known is the appropriate approach in managing hypokalemia in a client with diabetic ketoacidosis (DKA).
Hypokalemia is a common complication in DKA due to excessive loss of potassium through osmotic diuresis.
The first step is to ensure adequate urine output, as potassium replacement can potentially lead to kidney damage in the absence of diuresis.
Once urine output is established, the nurse can then monitor serum potassium levels and administer potassium as necessary to correct the imbalance.
Choice B rationale:
Delaying potassium replacement until blood glucose levels stabilize is not the best approach.
Hypokalemia in DKA should be addressed promptly to prevent complications such as cardiac dysrhythmias, which can be aggravated by low potassium levels.
Correcting hypokalemia is an essential part of DKA management and should not be postponed.
Choice C rationale:
Waiting for the client to complain of muscle weakness before replacing potassium is not advisable.
Muscle weakness is a late sign of severe hypokalemia, and by the time it occurs, the client may already be at risk of life-threatening complications.
It is essential to monitor laboratory values and replace potassium proactively when necessary.
Choice D rationale:
Asserting that potassium replacement is not necessary in DKA management is incorrect.
Hypokalemia is a well-recognized complication in DKA, and addressing it is a vital part of the overall treatment plan.
Failure to replace potassium in a timely manner can lead to serious health risks, including cardiac arrhythmias.
Explanation
Blood glucose levels.
B. Electrolyte levels.
C. Respiratory rate.
E. Skin color.
Choice A rationale:
Monitoring blood glucose levels is essential in managing a child with diabetic ketoacidosis (DKA).
Hyperglycemia is a hallmark of DKA, and effective insulin therapy is necessary to lower blood glucose levels to normal or near-normal ranges.
Frequent blood glucose monitoring helps adjust insulin infusion rates, preventing both hyperglycemia and hypoglycemia.
Choice B rationale:
Electrolyte levels, including potassium, sodium, and chloride, should be closely monitored in a child with DKA.
DKA can lead to electrolyte imbalances, such as hypokalemia and hyponatremia, which can be life-threatening.
Monitoring electrolytes ensures that appropriate replacements are administered to correct these imbalances.
Choice C rationale:
Respiratory rate monitoring is vital to detect signs of impending respiratory distress in a child with DKA.
As DKA progresses, metabolic acidosis can result in Kussmaul respirations, which are deep and rapid.
Monitoring respiratory rate can help identify respiratory distress early and prompt timely intervention.
Choice E rationale:
Monitoring skin color is important to assess perfusion and oxygenation.
In severe cases of DKA, there may be impaired tissue perfusion, resulting in pallor or cyanosis.
Skin color changes can be an early indicator of circulatory compromise, and prompt action can help prevent complications associated with inadequate tissue perfusion.
Choice D rationale:
Cardiac output is not typically monitored as a routine measure in managing DKA.
While DKA can affect cardiac function indirectly by causing electrolyte imbalances, monitoring cardiac output is not a direct preventive measure for DKA complications.
Instead, the focus should be on correcting the underlying metabolic and electrolyte imbalances.
How is insulin typically administered in DKA management?
Explanation
Choice A rationale:
In DKA management, insulin is typically administered intravenously as a continuous infusion.
This approach allows for precise control of insulin delivery, making it possible to titrate the insulin dose according to the patient's response.
Intravenous insulin is preferred because it provides rapid onset and offset of action and can be adjusted as needed to address changes in the patient's condition.
Choice B rationale:
Administering insulin as a single, large dose is not the standard practice in DKA management.
Large bolus doses of insulin can lead to rapid reductions in blood glucose levels, potentially causing hypoglycemia.
Continuous intravenous infusions are favored for gradual correction of hyperglycemia while avoiding rapid fluctuations in blood glucose levels.
Choice C rationale:
Oral insulin is not preferred for the treatment of DKA.
In this acute condition, the absorption of oral medications can be unpredictable and slow, which may not provide the rapid and consistent control of blood glucose levels required in DKA management.
Choice D rationale:
Insulin injections are typically given subcutaneously for routine diabetes management, but in the case of DKA, intravenous administration is the preferred route.
Subcutaneous injections have a slower onset of action and may not be suitable for addressing the acute and severe hyperglycemia characteristic of DKA.
Cystic Fibrosis in Children: Comprehensive Nursing Notes
The parent asks, "How is CF inherited?" Which of the following statements by the nurse is correct?
Explanation
"CF is an autosomal recessive genetic disorder.”.
Choice A rationale:
CF is not inherited through an X-linked dominant pattern.
X-linked inheritance involves genes located on the X chromosome, and CF is not linked to this type of inheritance.
Choice C rationale:
CF is not solely related to inheriting a defective CFTR gene from one parent.
While inheriting a mutated CFTR gene is a factor, CF is an autosomal recessive disorder, meaning it requires mutations in both copies of the CFTR gene (one from each parent) for the disease to manifest.
Choice D rationale:
CF is not solely caused by the deletion of phenylalanine at position 508 (F508del).
While this mutation is one of the most common causes of CF, it is not the only genetic variation associated with the disease.
CF can result from various mutations in the CFTR gene.
The client asks, "Why does CF lead to the production of thick mucus in the lungs and other organs?" Which of the following responses by the nurse is accurate?
Explanation
"The CFTR gene mutation impairs chloride and water transport in cells.”.
Choice A rationale:
The CFTR gene mutation does not cause excessive water transport in the body.
In fact, CF leads to a defect in chloride and water transport in cells, which results in the production of thick mucus.
Choice B rationale:
CF does not result in an overproduction of a specific enzyme that thickens mucus.
Instead, it affects the functioning of the CFTR protein, which is responsible for maintaining the balance of chloride and water in cells.
Choice D rationale:
CF does not primarily affect the production of surfactant in the lungs.
Surfactant is a substance that helps prevent the collapse of alveoli in the lungs, and CF primarily affects the mucus and airway clearance, not surfactant production.
Which of the following interventions should the nurse include in the teaching? (Select all that apply).
Explanation
Choice A rationale:
Encouraging physical activity and exercise is important in managing CF.
It helps improve lung function and overall health in individuals with CF.
Choice B rationale:
Administering pancreatic enzyme replacement therapy is a crucial part of CF management.
CF often affects the pancreas, leading to malabsorption, and these enzymes help digest and absorb nutrients properly.
Choice C rationale:
Restricting fluid intake to reduce mucus production is not a recommended intervention for CF.
Hydration is essential to keep mucus from becoming too thick and sticky.
Dehydration can worsen mucus obstruction.
Choice D rationale:
Teaching airway clearance techniques is essential in CF management.
It helps individuals clear the thick mucus from their airways, promoting better lung function.
Choice E rationale:
Promoting a high-fat, high-calorie diet is important for individuals with CF.
CF often leads to malnutrition, and a high-calorie diet helps maintain proper nutrition and growth.
Which of the following findings should the nurse consider as a common respiratory complication of CF?
Explanation
Choice A rationale:
Increased lung compliance is not a common respiratory complication of cystic fibrosis (CF).
CF is characterized by the production of thick and sticky mucus in the airways, which leads to decreased lung compliance.
This thick mucus obstructs the airways, making it difficult for the child to breathe.
Choice B rationale:
Decreased breath sounds are a common respiratory complication of CF.
The thick and sticky mucus produced in CF can block the airways, leading to decreased breath sounds upon auscultation.
This can result in impaired air movement and reduced ventilation in affected areas of the lungs.
Choice C rationale:
Normal oxygen saturation is not typically a common respiratory complication of CF.
CF often leads to decreased oxygen saturation due to the impaired lung function caused by mucus buildup and recurrent infections.
Choice D rationale:
Clear and thin sputum production is not a common finding in CF.
CF is associated with the production of thick and sticky mucus, leading to productive cough with thick, tenacious sputum.
The parent asks, "How does CF affect the pancreas?" Which of the following statements by the nurse is accurate?
Explanation
Choice A rationale:
"CF leads to excessive production of digestive enzymes in the pancreas.”.
This statement is not accurate.
In fact, CF impairs the production of digestive enzymes in the pancreas.
The thick mucus produced in CF can block the pancreatic ducts, preventing the release of enzymes needed for proper digestion.
Choice B rationale:
"CF has no impact on the function of the pancreas.”.
This statement is incorrect.
CF significantly affects the function of the pancreas by obstructing the pancreatic ducts and impairing the production of digestive enzymes.
Choice C rationale:
"CF impairs the pancreas's ability to produce digestive enzymes.”.
This statement is accurate.
CF causes the thick and sticky mucus to accumulate in the pancreas, obstructing the release of digestive enzymes, which are essential for the digestion of fats and proteins.
Choice D rationale:
"CF causes the pancreas to produce excessive insulin.”.
This statement is not correct.
CF does not lead to excessive insulin production.
Instead, it primarily affects the production of digestive enzymes and can lead to issues related to fat malabsorption.
The child presents with chronic cough, wheezing, and recurrent respiratory infections.
What should the nurse expect to find during this assessment?
Explanation
Choice A rationale:
"I have difficulty breathing when I'm playing outside.”.
This statement may be relevant to a respiratory assessment in a child with CF but does not address the typical gastrointestinal symptoms associated with the condition, such as greasy stools.
Choice B rationale:
"My fingers and toes look round and wide.”.
This statement is not related to the typical symptoms of CF.
The characteristic physical findings in CF are often related to respiratory and gastrointestinal issues rather than finger and toe appearance.
Choice C rationale:
"My stools are greasy and float in the toilet.”.
This statement is an accurate description of one of the common gastrointestinal symptoms of CF.
CF can lead to malabsorption of fats, resulting in greasy, foul-smelling stools that float in the toilet due to their high fat content.
Choice D rationale:
"I often have trouble controlling my blood sugar.”.
This statement is not typically associated with CF.
Blood sugar control issues are more commonly linked to conditions like diabetes, not CF, which primarily affects the respiratory and gastrointestinal systems.
Which part of the nursing assessment is most relevant in this case?
Explanation
Choice A rationale:
Monitoring the child's blood sugar levels is not relevant to a child with cystic fibrosis experiencing recurrent respiratory infections.
Cystic fibrosis primarily affects the respiratory and digestive systems, and blood sugar levels are not a significant concern in this context.
Choice B rationale:
Assessing the child's dental hygiene practices is important for overall health, but it is not the most relevant assessment in the case of a child with cystic fibrosis and recurrent respiratory infections.
The primary focus should be on the respiratory system.
Choice D rationale:
Observing for signs of gastrointestinal obstructions is an essential part of caring for a child with cystic fibrosis, but in the context of recurrent respiratory infections, evaluating lung sounds and respiratory rate is the most critical assessment.
Gastrointestinal issues are important but secondary to the respiratory concerns in this case.
The nurse is responsible for providing nutritional support as part of the treatment plan.
What is an appropriate nursing intervention in this context?
Explanation
Choice A rationale:
Avoiding high-calorie foods to prevent weight gain is not an appropriate nursing intervention for a child with cystic fibrosis.
These children often have difficulty maintaining their weight due to malabsorption, and they may need a high-calorie diet to ensure proper growth and development.
Choice C rationale:
Disregarding the diet's impact on cystic fibrosis is not a valid approach.
Nutrition plays a crucial role in managing the condition, and dietary choices can significantly impact a child's health and well-being.
The statement is inaccurate and should not be followed.
Choice D rationale:
Limiting food intake to avoid digestive issues is not a suitable approach for a child with cystic fibrosis.
While digestive issues can be a concern, it is essential to provide adequate nutrition to support growth and development.
Restricting food intake can lead to malnutrition in these patients.
What should the nurse recommend for effective infection control?
Explanation
Choice B rationale:
Stating that hand hygiene is unnecessary in this case is incorrect.
Hand hygiene is crucial in infection control, especially for individuals with cystic fibrosis who may be more susceptible to infections due to compromised lung function.
Encouraging frequent handwashing is a key preventive measure.
Choice C rationale:
Having a child interact closely with friends and classmates to build immunity is not a recommended strategy for infection control in a child with cystic fibrosis.
Close contact with others can increase the risk of exposure to respiratory infections, which should be minimized.
Choice D rationale:
Avoiding vaccinations is not advisable, as vaccinations are an essential part of preventing various infectious diseases.
While certain vaccinations may need to be discussed with the healthcare provider to account for the child's individual health status, it is generally not recommended to avoid vaccinations as they can help prevent illness.
Explanation
Administer respiratory treatments, including chest physiotherapy.
C. Emphasize the importance of hand hygiene.
D. Provide psychological counseling and support.
Choice A rationale:
Administering respiratory treatments, including chest physiotherapy, is essential in managing cystic fibrosis in children.
Cystic fibrosis often results in thick, sticky mucus in the lungs, making it difficult to clear airway secretions.
Chest physiotherapy helps loosen and mobilize these secretions, improving lung function and reducing the risk of respiratory infections.
Choice B rationale:
Encouraging a low-calorie, low-protein diet is not an appropriate intervention for managing cystic fibrosis in children.
Children with cystic fibrosis typically have increased nutritional needs due to malabsorption of nutrients, and a low-calorie, low-protein diet could exacerbate their nutritional deficiencies and growth issues.
Choice C rationale:
Emphasizing the importance of hand hygiene is a crucial nursing intervention for managing cystic fibrosis in children.
Cystic fibrosis patients are more susceptible to respiratory infections, and good hand hygiene helps prevent the spread of infections, which is especially important in a healthcare setting.
Choice D rationale:
Providing psychological counseling and support is essential for children with cystic fibrosis.
The chronic nature of the disease, frequent hospitalizations, and daily treatments can take a toll on a child's mental health.
Psychological support helps them cope with the emotional challenges and stress associated with their condition.
Choice E rationale:
Avoiding exercise and physical activity is not an appropriate intervention for managing cystic fibrosis in children.
Physical activity is beneficial for maintaining lung function and overall health in individuals with cystic fibrosis.
It helps improve airway clearance and strengthen respiratory muscles.
What pharmacological interventions might be part of the treatment plan for this child?
Explanation
"You'll need to take bronchodilators as prescribed.”.
Choice A rationale:
Bronchodilators are commonly prescribed to children with cystic fibrosis to help open airways, making it easier for them to breathe.
These medications assist in relieving airway constriction and improving respiratory function.
Choice B rationale:
Stating that "antibiotics are unnecessary for cystic fibrosis" is incorrect.
Antibiotics are often required for cystic fibrosis patients to treat and prevent respiratory infections, which are common due to the thick mucus buildup in the airways.
Choice C rationale:
Mucolytics are medications that help thin and mobilize mucus in the airways.
Advising the child to "avoid mucolytics" is not appropriate, as these drugs can be beneficial in managing cystic fibrosis by facilitating mucus clearance and reducing the risk of lung infections.
Choice D rationale:
Telling the child to "skip the medications; they won't help" is incorrect and potentially dangerous advice.
Medications prescribed for cystic fibrosis are essential for managing the disease, and skipping them can lead to worsened symptoms and complications.
What is an essential aspect of this support?
Explanation
"Offer emotional support and resources for coping with the challenges.”.
Choice A rationale:
Suggesting that "isolation is the best way to manage cystic fibrosis" is not appropriate.
Isolation can lead to feelings of loneliness and depression in children with cystic fibrosis.
Social support and interaction are important for their emotional well-being.
Choice B rationale:
Advising the child to "avoid discussing the condition" is not a suitable approach.
Open and honest communication about the disease can help the child understand and cope with their condition better.
Avoiding discussions may lead to increased anxiety and uncertainty.
Choice C rationale:
"Offering emotional support and resources for coping with the challenges" is a vital aspect of psychosocial support for children with cystic fibrosis.
Providing emotional support and connecting the child and their family with resources such as support groups and counseling can help them navigate the emotional and psychological challenges that come with the disease.
Choice D rationale:
"Minimizing contact with friends and social activities" is not a recommended approach for managing cystic fibrosis.
While infection control is essential, complete isolation from social activities can lead to social and emotional isolation.
It's important to strike a balance between precautions and maintaining a healthy social life.
Congenital Heart Defects in Children
The child presents with poor feeding, fast breathing, and sweating with exertion.
Which of the following is the characteristic heart murmur associated with VSD?
Explanation
Choice A rationale:
A continuous "machinery" murmur that is loudest below the left clavicle is typically associated with a patent ductus arteriosus (PDA), not VSD.
PDA is a different congenital heart defect.
Choice B rationale:
A harsh holosystolic murmur that is best heard at the left lower sternal border is the characteristic murmur associated with Ventricular Septal Defect (VSD).
This murmur is caused by the blood flowing from the high-pressure left ventricle to the low-pressure right ventricle through the VSD hole throughout the cardiac cycle.
Choice C rationale:
A systolic ejection murmur that is best heard at the left upper sternal border is often associated with aortic stenosis, not VSD.
Choice D rationale:
A systolic ejection murmur that radiates to the back is characteristic of aortic regurgitation, which is a different cardiac condition.
The characteristic heart murmur in VSD is the result of blood flowing from the left ventricle to the right ventricle through the VSD hole during systole.
This causes a harsh holosystolic murmur, which is loudest at the left lower sternal border due to the location of the defect in the ventricular septum.
Therefore, choice B is The correct answer.
Which factors may contribute to the development of congenital heart defects in children? Select all that apply.
Explanation
Choice A rationale:
Genetic factors can contribute to the development of congenital heart defects in children.
Certain genetic mutations or abnormalities can increase the risk of congenital heart conditions.
Choice B rationale:
Maternal health is a factor that may contribute to the development of congenital heart defects in children.
Maternal conditions such as diabetes or rubella during pregnancy can increase the risk of congenital heart defects in the fetus.
Choice C rationale:
Exposure to infections during pregnancy is a known risk factor for the development of congenital heart defects.
Infections like rubella and certain medications can increase the risk of congenital heart conditions.
Choice D rationale:
Chromosomal abnormalities, such as Down syndrome (Trisomy 21), can be associated with congenital heart defects.
These genetic abnormalities can impact the development of the heart.
Choice E rationale:
While paternal health is important for overall fetal development, it is not a well-established risk factor for congenital heart defects.
The primary factors are maternal and genetic.
Congenital heart defects in children can be influenced by a combination of genetic factors, maternal health, exposure to infections during pregnancy, and chromosomal abnormalities.
These factors interact to increase the risk of congenital heart conditions.
Therefore, choices A, B, C, and D are all correct answers.
Which of the following symptoms are characteristic of TOF?
Explanation
Choice A rationale:
Cyanosis that worsens with crying or feeding is characteristic of Tetralogy of Fallot (TOF).
TOF is a congenital heart defect characterized by four specific cardiac abnormalities, one of which is a ventricular septal defect (VSD).
The VSD allows deoxygenated blood to flow from the right ventricle into the left ventricle and then into the aorta, leading to systemic cyanosis, which is exacerbated by crying or feeding due to increased right-to-left shunting.
Choice B rationale:
Severe chest pain is not a characteristic symptom of Tetralogy of Fallot (TOF).
TOF primarily presents with cyanosis and other associated symptoms related to the heart defect.
Choice C rationale:
Palpitations are not a characteristic symptom of TOF.
While some children with congenital heart defects may experience palpitations, this is not a specific hallmark of TOF.
Choice D rationale:
Frequent respiratory infections are not a characteristic symptom of TOF.
The symptoms associated with TOF are primarily related to cardiac function, such as cyanosis, and do not directly cause respiratory infections.
The nurse hears a harsh holosystolic murmur that is best heard at the left lower sternal border during auscultation.
Which of the following statements should the client make to the nurse?
Explanation
Choice A rationale:
"I have been feeling very tired lately and I am unable to eat properly.”.
This choice does not address the specific symptoms associated with a Ventricular septal defect (VSD) and is not the best response to the nurse's findings.
While tiredness and poor feeding may be related to heart failure, it does not directly reflect the symptoms associated with VSD, such as breathlessness and sweating with exertion.
Choice B rationale:
"I have been experiencing shortness of breath and rapid weight gain.”.
This is The correct answer.
The symptoms of shortness of breath and rapid weight gain align with the typical presentation of a VSD.
VSD can lead to heart failure, which results in fluid retention, manifesting as rapid weight gain, and shortness of breath due to congestion in the lungs.
Choice C rationale:
"I have been feeling dizzy and fainting frequently.”.
This choice describes symptoms that can be related to various health issues, but it doesn't directly correlate with the characteristic signs of VSD.
The primary symptoms in VSD are related to heart failure, and while dizziness and fainting can occur with severe heart issues, they are not the primary indicators in this case.
Choice D rationale:
"I have been having severe chest pain and palpitations.”.
This response does not align with the typical symptoms of VSD.
While palpitations can be associated with heart issues, chest pain is not a common symptom of VSD.
The client reports difficulty breathing (dyspnea), frequent respiratory infections, feeling the heart beat (palpitations), and shortness of breath with activity.
During auscultation, the nurse hears a systolic ejection murmur that is best heard at the left upper sternal border.
Which of the following nursing interventions are appropriate for this client? Select all that apply.
Explanation
Choice A rationale:
Monitor vital signs regularly.
This is an appropriate nursing intervention for a client with Atrial septal defect (ASD).
Regular monitoring of vital signs, including heart rate and blood pressure, helps to assess the client's cardiovascular status and response to treatment.
Choice B rationale:
Administer prescribed medications.
Administering medications as prescribed is a crucial nursing intervention.
Depending on the client's condition, medications may include diuretics, antiarrhythmics, or other medications to manage symptoms and improve heart function.
Choice C rationale:
Encourage bed rest.
Encouraging bed rest is not typically required for clients with ASD unless there are specific indications, such as severe symptoms.
It's important to promote activity within the limits of the client's condition to prevent deconditioning.
Choice D rationale:
Provide oxygen therapy as needed.
Oxygen therapy may be needed for clients with ASD if they experience significant hypoxia or respiratory distress.
It can help improve oxygen saturation and relieve dyspnea.
Choice E rationale:
Educate the client about lifestyle modifications.
Educating the client about lifestyle modifications is essential.
Clients with ASD may benefit from lifestyle changes such as a heart-healthy diet, regular exercise within their limits, and smoking cessation if applicable.
These modifications can help manage symptoms and improve overall cardiovascular health.
What should be the nurse's immediate response?
Explanation
Prepare for emergency surgery.
Choice A rationale:
Administer oxygen therapy immediately.
Administering oxygen therapy would provide temporary relief to the patient's cyanosis, but it does not address the underlying issue in Tetralogy of Fallot (TOF).
TOF is a congenital heart defect characterized by a combination of four heart abnormalities, one of which is a ventricular septal defect (VSD) that allows oxygen-poor blood to mix with oxygen-rich blood.
Administering oxygen will increase the oxygen saturation in the blood but will not fix the structural problem.
The immediate priority for a patient with TOF experiencing a hypercyanotic spell is to address the heart defect itself.
Choice B rationale:
Prepare for emergency surgery.
In Tetralogy of Fallot, hypercyanotic spells, also known as "tet spells," are a medical emergency.
These spells occur due to a sudden decrease in systemic vascular resistance, causing more blood to flow into the right ventricle, leading to increased right-to-left shunting, further decreasing oxygenation.
The most appropriate intervention is to prepare for emergency surgery to correct the underlying cardiac defects, such as closing the VSD and relieving right ventricular outflow obstruction.
Surgery is the definitive treatment for TOF and should be performed promptly during a tet spell to prevent severe hypoxia and potential long-term complications.
Choice C rationale:
Monitor vital signs closely.
While monitoring vital signs is essential in the care of a patient with TOF, it is not the most immediate response in the scenario of a hypercyanotic spell.
Monitoring alone will not address the critical need for intervention to improve oxygenation and prevent hypoxia.
Choice D rationale:
Administer prescribed medication.
Administering prescribed medication may be part of the overall management of a patient with TOF, but it is not the immediate response during a hypercyanotic spell.
Medications can help manage symptoms and stabilize the patient, but the definitive treatment for TOF is surgical correction.
The client has no other symptoms and is otherwise healthy.
The client asks the nurse, "What does this murmur mean?".
The nurse's best response is:.
Explanation
"This murmur is a sign of a heart defect called coarctation of the aorta (COA).”.
Choice A rationale:
"This murmur is a sign of a heart defect called coarctation of the aorta (COA).”.
A systolic ejection murmur heard at the left upper sternal border can be indicative of coarctation of the aorta (COA).
Coarctation of the aorta is a congenital heart defect characterized by a narrowing or constriction of the aorta, typically near the site of the ductus arteriosus.
This narrowing leads to increased pressure and turbulence in the left ventricle and aorta, resulting in the systolic ejection murmur.
Informing the client about the likely diagnosis is a good approach as it helps provide them with essential information about their condition.
Choice B rationale:
"This murmur is a sign of a heart defect called atrial septal defect (ASD).”.
An atrial septal defect (ASD) typically presents with a different type of murmur, not a systolic ejection murmur heard at the left upper sternal border.
ASD is characterized by a fixed, split second heart sound (S2) and a mid-systolic murmur at the upper left sternal border.
The description in the question does not align with the typical findings of an ASD.
Choice C rationale:
"This murmur is a sign of a heart defect called ventricular septal defect (VSD).”.
A ventricular septal defect (VSD) also presents with a different type of murmur, typically a harsh holosystolic murmur heard at the lower left sternal border.
The description of the murmur in the question, a systolic ejection murmur at the left upper sternal border, is not characteristic of a VSD.
Choice D rationale:
"This murmur is a sign of a heart defect called tetralogy of Fallot (TOF).”.
Tetralogy of Fallot (TOF) is characterized by a different set of heart defects, including a ventricular septal defect (VSD), overriding aorta, right ventricular outflow tract obstruction, and right ventricular hypertrophy.
The murmur described in the question is not specific to TOF and is more indicative of coarctation of the aorta (COA) due to its location and characteristics.
The nurse should expect which of the following symptoms in this patient?
Explanation
Choice A rationale:
The patient's statement, "My baby's skin and lips have turned bluish," is a classic symptom of cyanosis.
Cyanosis is a bluish or purple discoloration of the skin and mucous membranes, which occurs due to a lack of oxygen in the blood.
In this case, it's associated with a ventricular septal defect (VSD), which is a congenital heart defect that allows oxygen-poor blood from the right side of the heart to mix with oxygen-rich blood from the left side.
Choice B rationale:
The statement, "My baby has difficulty feeding and is not gaining weight properly," may be related to the VSD, but it is not a typical symptom of cyanosis.
This symptom can occur due to congestive heart failure in infants with VSD.
Choice C rationale:
"My baby gets tired quickly during physical activity" can also be associated with VSD and congestive heart failure, but it is not a direct symptom of cyanosis.
Choice D rationale:
"I can hear abnormal heart sounds during the check-up" is not a symptom but rather a sign of a ventricular septal defect.
Abnormal heart sounds, like a loud holosystolic murmur, may be heard on auscultation.
What is a likely symptom associated with this condition?
Explanation
Choice A rationale:
"I've noticed a bluish discoloration of my skin and lips" is not a typical symptom of an atrial septal defect (ASD).
ASD is a congenital heart defect that involves an abnormal opening between the atria of the heart, and it typically results in increased blood flow to the lungs, not cyanosis.
Choice B rationale:
"I find it hard to feed, and I'm not gaining weight as expected" can be related to ASD, but it is not a primary symptom.
The increased blood flow to the lungs in ASD may lead to congestive heart failure, which can cause poor feeding and inadequate weight gain.
Choice C rationale:
"I feel short of breath and tired during physical activities" is a likely symptom of ASD.
With ASD, there is an increased volume of blood being pumped into the lungs, which can lead to pulmonary congestion, shortness of breath, and fatigue.
Choice D rationale:
"The doctor mentioned hearing unusual heart sounds during the examination" is not a symptom but rather a sign of an atrial septal defect.
Unusual heart sounds, like a fixed split second heart sound, may be heard on auscultation.
Explanation
Choice A rationale:
Bluish discoloration of the skin, lips, or nail beds (cyanosis) is a classic symptom of cyanotic congenital heart disease (CCHD).
This occurs because of the inadequate oxygenation of the blood, which leads to oxygen-poor blood being circulated in the body.
Choice B rationale:
Poor feeding and inadequate weight gain can be associated with CCHD, especially when there is a significant reduction in cardiac output.
Infants with CCHD may have difficulty feeding due to the increased workload on their heart and may struggle to gain weight.
Choice C rationale:
Rapid breathing and shortness of breath are common symptoms in children with CCHD.
The inadequate oxygenation of the blood can lead to an increased respiratory rate and shortness of breath as the body tries to compensate for the lack of oxygen.
Choice D rationale:
Abnormal heart sounds heard during auscultation are characteristic of CCHD.
The specific type of abnormal heart sound may vary depending on the specific defect but can include murmurs, clicks, or other unusual sounds.
Choice E rationale:
Frequent respiratory infections are not typically associated with CCHD.
While children with CCHD may be more susceptible to infections due to their compromised oxygenation, it is not a direct symptom of the condition.
Which diagnostic test is most appropriate for assessing the size and shape of the heart and detecting associated abnormalities?
Explanation
Choice A rationale:
Echocardiography Echocardiography is the most appropriate diagnostic test for assessing the size and shape of the heart and detecting associated abnormalities in a child with a suspected congenital heart defect.
It uses sound waves to create images of the heart, providing detailed information about the heart's structure and function.
It is non-invasive and safe, making it an excellent choice for initial evaluation.
Choice B rationale:
Electrocardiography (ECG) Electrocardiography (ECG) is a valuable test for assessing the electrical activity of the heart, including rhythm and conduction abnormalities.
However, it does not provide detailed information about the size and shape of the heart or structural abnormalities.
ECG is often used in conjunction with other tests like echocardiography.
Choice C rationale:
Chest X-ray A chest X-ray can provide some information about the heart's size and shape but is not as detailed as echocardiography.
It is often used as an initial screening tool but is not the primary diagnostic test for assessing congenital heart defects and their associated abnormalities.
Choice D rationale:
Cardiac catheterization Cardiac catheterization is an invasive procedure that involves threading a thin tube (catheter) through blood vessels into the heart.
It is primarily used to obtain detailed hemodynamic information and to perform interventions such as closing defects or dilating narrowed blood vessels.
While it can be valuable in certain situations, it is not the initial diagnostic test of choice for assessing the size and shape of the heart in a child with a suspected congenital heart defect.
Explanation
Choice A rationale:
Measuring the level of oxygen in a child's blood does not help assess the electrical activity of the heart.
Oxygen measurement and the assessment of heart electrical activity are two separate concepts.
Choice B rationale:
Measuring oxygen levels in the blood primarily evaluates the child's oxygen saturation, not the respiratory rate and effort.
While oxygen saturation is related to respiratory function, it doesn't directly assess the rate and effort of breathing.
Choice C rationale:
Measuring the level of oxygen in a child's blood monitors oxygen saturation using pulse oximetry.
Pulse oximetry is a non-invasive method used to measure the percentage of oxygen saturation in the blood.
This is important because it provides information about the child's oxygen levels, which is crucial for assessing their respiratory and circulatory status.
Choice D rationale:
Measuring the level of oxygen in the blood does not measure the child's weight and developmental milestones.
This response is unrelated to the purpose of monitoring oxygen levels in the blood.
A nurse is performing a nursing assessment on a child with a congenital heart defect.
Which aspects should the nurse include in the assessment? Select all that apply.
Explanation
Choice A rationale:
A physical examination is an essential part of the nursing assessment for a child with a congenital heart defect.
It helps the nurse identify physical signs and symptoms that may be indicative of the heart defect.
Choice B rationale:
Assessing growth and development is crucial when caring for a child with a congenital heart defect.
This helps monitor the child's overall health and well-being and can detect any developmental delays or issues related to the heart condition.
Choice C rationale:
Oxygen saturation monitoring is important for children with congenital heart defects as it helps assess the effectiveness of their oxygen delivery and may indicate the need for interventions or adjustments in their care.
Choice D rationale:
A feeding assessment is necessary for children with congenital heart defects as they may experience difficulties with feeding due to limited energy and respiratory issues.
Ensuring adequate nutrition is essential for their growth and development.
Choice E rationale:
Genetic testing is not typically a part of the routine nursing assessment for a child with a congenital heart defect.
While some heart defects may have a genetic component, this is not a standard part of the assessment process.
What is an example of a medication that may be administered as prescribed to this child?
Explanation
Choice A rationale:
Antibiotics are not specific to congenital heart defects.
While a child with a heart defect may need antibiotics in certain situations, they are not a medication that is universally prescribed for all children with heart defects.
Choice B rationale:
Anti-seizure medication is not typically prescribed for children with congenital heart defects unless there is a specific medical indication related to seizures.
It is not a standard treatment for heart defects.
Choice C rationale:
Diuretics are an example of a medication that may be prescribed to a child with a congenital heart defect.
Diuretics can help manage fluid retention, reduce the workload on the heart, and improve the child's overall condition.
Choice D rationale:
Painkillers may be prescribed for pain relief, but they are not specific to congenital heart defects.
Their use would depend on the individual circumstances and whether the child is experiencing pain.
Explanation
Choice A rationale:
The nurse's response should include teaching proper positioning techniques as optimizing a child's respiratory function can be improved by correct positioning.
Proper positioning helps ensure that the child's airways are open and not obstructed, which is essential for effective breathing.
This is a fundamental aspect of respiratory care, especially in pediatric patients who may not be able to reposition themselves if they are uncomfortable or experiencing difficulty breathing.
Choice B rationale:
Administering vasodilators is not typically a measure to optimize a child's respiratory function.
Vasodilators are medications that dilate blood vessels and are usually used in specific cardiovascular conditions to reduce the workload on the heart.
They are not directly related to optimizing respiratory function.
Choice C rationale:
Monitoring growth patterns, while important for a child's overall health, is not a direct response to the client's question about optimizing respiratory function.
Growth patterns are assessed for general development and health, but they do not specifically address respiratory function.
Choice D rationale:
Providing information on the child's condition is essential, but it does not directly address the question about optimizing respiratory function.
While education is crucial, the primary focus should be on practical measures to improve the child's respiratory function, such as proper positioning and breathing techniques.
Which statement reflects an appropriate action during the assessment?
Explanation
Choice A rationale:
Checking the child's oxygen saturation using a pulse oximeter is an appropriate action during the assessment of a child with a congenital heart defect.
Oxygen saturation monitoring helps assess the child's oxygen levels, which is crucial in determining the adequacy of oxygen supply to the body.
Children with congenital heart defects are at risk of reduced oxygen levels, and monitoring oxygen saturation is a vital part of their care.
Choice B rationale:
Ensuring the child receives all their vaccinations is important for the child's overall health but is not directly related to the assessment of a congenital heart defect.
Vaccinations are typically administered as part of routine healthcare, but they do not address the specific concerns related to a congenital heart defect assessment.
Choice C rationale:
Assessing the child's neurological development is important but is not the primary focus of the assessment for a congenital heart defect.
While neurological assessment is important for overall child development, it does not directly relate to the cardiac assessment.
Choice D rationale:
Monitoring the child's growth based on height alone is not a comprehensive assessment for a child with a congenital heart defect.
Monitoring growth should include various parameters, such as weight, head circumference, and developmental milestones.
Relying solely on height may not provide a complete picture of the child's overall development.
What statement by the client indicates a need for further education about medication management?
Explanation
Choice A rationale:
The statement, "I need to make sure my child takes their medications on time," indicates the client's awareness of the importance of medication adherence.
This statement reflects responsible medication management and does not indicate a need for further education.
Choice B rationale:
The statement, "Are there any side effects I should watch out for with these medications?" reflects a responsible and informed approach to medication management.
It shows that the client is concerned about potential side effects and is willing to monitor for them, which is a positive sign of medication education.
Choice C rationale:
The statement, "I can give my child herbal supplements to enhance the effect of the medication," indicates a need for further education about medication management.
Herbal supplements can interact with medications and may have unpredictable effects.
Combining them without medical guidance can be dangerous and is not recommended.
Choice D rationale:
The statement, "I should keep a record of all the medications my child is taking," is a responsible and proactive approach to medication management.
Keeping a record helps ensure that the child is receiving The correct medications and doses and can be helpful in case of any emergencies.
It indicates a good understanding of the importance of medication management.
Select all appropriate nursing interventions for parents to promote their child's well-being.
Explanation
Encourage regular follow-up appointments with the cardiologist.
B. Teach parents how to administer medication to the child.
E. Provide resources for support groups and counseling for the parents.
Choice A rationale:
Encouraging regular follow-up appointments with the cardiologist is essential for a child with a congenital heart defect.
These appointments allow for the monitoring of the child's heart condition, adjustments in their treatment plan, and early detection of any potential issues or complications.
Regular follow-up ensures that the child's heart health is closely monitored, which is crucial for their well-being.
Choice B rationale:
Teaching parents how to administer medication to the child is another important nursing intervention.
Many children with congenital heart defects require medications to manage their condition.
Proper administration is critical to maintaining the child's health and preventing complications.
Education empowers parents to be actively involved in their child's care, ensuring medication compliance and safety.
Choice C rationale:
Advising parents to expose the child to secondhand smoke is not appropriate.
Secondhand smoke is harmful and can have detrimental effects on a child's health, especially a child with a congenital heart defect.
It can worsen respiratory and cardiovascular problems, which is the opposite of promoting the child's well-being.
This choice should be avoided.
Choice D rationale:
Instructing parents to limit physical activity to prevent any stress on the child's heart is not a suitable nursing intervention.
While some restrictions on physical activity may be necessary, they should be determined by the cardiologist based on the child's specific condition.
Complete physical inactivity can have negative effects on a child's overall health and development.
It's important to strike a balance between physical activity and the child's heart health.
Choice E rationale:
Providing resources for support groups and counseling for the parents is an excellent nursing intervention.
Having a child with a congenital heart defect can be emotionally challenging for parents.
Support groups and counseling can offer them emotional support, guidance, and a safe space to share their concerns and experiences.
This contributes to the parents' well-being, which in turn benefits the child's care and family dynamics.
What is a key nursing intervention during this time?
Explanation
Assessing for signs of infection or bleeding at the surgical site.
Choice A rationale:
Administering herbal supplements to aid in healing is not a key nursing intervention in post-operative care for a child who has undergone heart surgery.
The use of herbal supplements should be carefully considered and discussed with the healthcare team, as they may interact with medications or affect the child's recovery.
However, it's not a primary nursing intervention.
Choice B rationale:
Monitoring the child's growth and development is an important aspect of pediatric care, but it is not the key nursing intervention during the immediate post-operative period.
The primary focus in this phase is on assessing for immediate post-surgical complications and ensuring the child's stability and recovery.
Choice C rationale:
Ensuring the child maintains complete bed rest is not a recommended intervention in the post-operative care of a child who has undergone heart surgery.
While some restrictions on physical activity may be necessary, complete bed rest is generally not advisable.
Mobilization, as appropriate, is essential to prevent complications such as deep vein thrombosis and to promote recovery.
Choice D rationale:
Assessing for signs of infection or bleeding at the surgical site is a key nursing intervention during the post-operative period.
Infection and bleeding are immediate post-operative complications that can have serious consequences.
Early detection and prompt intervention are crucial to ensure the child's safety and well-being.
Nursing assessments focus on monitoring vital signs, wound appearance, and any signs of infection or bleeding.
What information should the nurse provide regarding follow-up care?
Explanation
"Long-term monitoring will include regular follow-up appointments with the cardiologist.”.
Choice A rationale:
Stating, "It's essential to schedule cardiac rehabilitation sessions for your child," is not accurate for the long-term management of a congenital heart defect.
Cardiac rehabilitation is typically recommended for individuals who have experienced a cardiac event, such as a heart attack, but it is not a standard part of the long-term management of congenital heart defects in children.
Choice B rationale:
Informing the client that long-term monitoring will include regular follow-up appointments with the cardiologist is The correct nursing response.
Regular follow-up appointments are essential for monitoring the child's heart condition, adjusting treatment as needed, and ensuring their overall well-being.
This choice is accurate and aligned with best practices.
Choice C rationale:
Stating, "You can discontinue all medications once your child reaches a certain age," is not accurate or safe advice.
The need for medications in the management of a congenital heart defect is determined by the child's specific condition and the recommendations of the healthcare team.
Discontinuing medications without medical guidance can be dangerous and is not a standard practice.
Choice D rationale:
Claiming, "Balloon valvuloplasty will be the primary treatment for long-term management," is not a universally applicable statement.
The choice of treatment for long-term management of a congenital heart defect depends on the specific diagnosis and clinical circumstances.
While balloon valvuloplasty may be a suitable treatment in some cases, it is not the primary treatment for all congenital heart defects.
Individualized care plans are developed based on the child's condition.
Therefore, this statement is not accurate as a general rule.
Epilepsy in Children:
Which statement by the nurse is correct regarding the etiology of epilepsy in children?
Explanation
Choice A rationale:
Epilepsy in children can have multiple etiological factors, and this statement accurately reflects this.
Genetic factors, brain injury, infections, developmental disorders, and metabolic abnormalities can all contribute to epilepsy in children.
Choice B rationale:
This statement is not correct.
While genetic factors can play a role in epilepsy, it's an oversimplification to say they are the primary cause, and other factors are minimal.
Choice C rationale:
This statement is incorrect.
Infections like meningitis can certainly lead to epilepsy in children, but they are not the most common cause.
Choice D rationale:
This statement is not accurate.
Brain injury, while a potential cause, is not the sole cause of epilepsy in children.
There are multiple contributing factors.
Which statement by the client indicates a correct understanding of the condition's pathophysiology?
Explanation
Choice A rationale:
This statement accurately describes the pathophysiology of epilepsy.
Seizures result from abnormal electrical activity in the brain, and an imbalance in neurotransmitters can contribute to this.
It's a complex neurological condition.
Choice B rationale:
This statement is not accurate.
While structural abnormalities in the brain can be a contributing factor, it's not the primary cause of epilepsy in children.
Choice C rationale:
This statement is incorrect.
Seizures can originate in different areas of the brain and may spread to other regions.
They are not always confined to specific areas.
Choice D rationale:
This statement is not correct.
Abnormalities in blood vessels are not the primary cause of epilepsy in children.
Select all that apply:.
Explanation
Choice A rationale:
Genetic factors can contribute to epilepsy in children.
Some children may have a genetic predisposition to the condition.
Choice B rationale:
Infections can indeed be a cause of epilepsy in children.
Infections like meningitis can lead to seizures.
Choice C rationale:
Metabolic disorders can also contribute to epilepsy.
An imbalance in metabolic processes can affect brain function and lead to seizures.
Choice D rationale:
Traumatic brain injury is a known cause of epilepsy in children.
Severe head injuries can result in epilepsy.
Choice E rationale:
Structural abnormalities in the brain can lead to epilepsy.
These abnormalities can disrupt normal brain function and trigger seizures.
What should the nurse explain regarding genetic factors in childhood epilepsy?
Explanation
Choice A rationale:
Epilepsy is a complex condition, and it is not solely caused by genetic factors.
While genetics can play a significant role in some cases of epilepsy, it is not the exclusive cause.
Various other factors, including brain injury, infections, and other environmental factors, can also contribute to the development of epilepsy.
Choice B rationale:
This statement is incorrect.
Epilepsy in children can be influenced by genetic predisposition in some cases, so it is not accurate to claim that genetic factors never play a role.
Choice D rationale:
This statement is also incorrect.
Genetic factors can affect individuals at any age, including infants and adolescents.
Therefore, it is not accurate to claim that genetic factors only affect adolescents and not infants.
How should the nurse respond regarding the pathophysiology of epilepsy in children?
Explanation
Choice A rationale:
Metabolic disorders can indeed lead to seizures in some cases, but they are not the primary cause of seizures in children with epilepsy.
The most common underlying mechanism for seizures in epilepsy is abnormal electrical activity in the brain.
Choice B rationale:
While structural abnormalities in the brain can be a cause of seizures, they are not the main cause of seizures in all children with epilepsy.
The primary pathophysiology of epilepsy involves abnormal electrical activity in the brain.
Choice D rationale:
Hormonal imbalances can influence seizure activity in certain cases, but they are not the primary cause of seizures in children with epilepsy.
Abnormal electrical activity in the brain is the central mechanism.
The child experiences generalized tonic-clonic seizures.
What motor symptoms might the nurse observe during these seizures?
Explanation
Choice A rationale:
Generalized tonic-clonic seizures are characterized by tonic (stiffening) and clonic (jerking) phases.
During the clonic phase, the child may exhibit jerking movements, and this is a typical motor symptom of this type of seizure.
Choice B rationale:
Visual hallucinations are not typically associated with generalized tonic-clonic seizures.
They are more commonly seen in other types of seizures or neurological conditions.
Choice C rationale:
Aggressive behavior is not a specific motor symptom of generalized tonic-clonic seizures.
Seizures can cause altered consciousness and bizarre or unusual behaviors, but aggression is not a hallmark of this seizure type.
Choice D rationale:
Difficulties in learning are not a motor symptom of generalized tonic-clonic seizures.
However, individuals with epilepsy may experience cognitive and learning difficulties as a result of their condition, but these difficulties are not direct motor symptoms of the seizures.
What information is relevant for the nurse to collect?
Explanation
Choice A rationale:
The nurse should collect information about the frequency and duration of the child's seizures as it is directly related to the child's condition and will help in planning the care and management of the child's epilepsy.
This information is essential for determining the severity and impact of the seizures on the child's daily life, and it will guide the healthcare team in making informed decisions about treatment and interventions.
The frequency and duration of seizures can vary among individuals, and it's important to have accurate data to tailor the care plan to the child's specific needs.
Choice B rationale:
The child's genetic test results are not directly relevant to the nurse's assessment of the child's seizure episodes.
While genetics can play a role in epilepsy, the immediate concern for the nurse is gathering information about the seizures' frequency and duration, as this will inform the care provided to the child.
Choice C rationale:
The child's blood pressure during seizures, although it may be monitored during a seizure, is not the primary information the nurse needs to collect as part of the assessment.
Seizures can cause changes in blood pressure, but this parameter is not the main focus when assessing the child's seizure episodes.
Choice D rationale:
While the family's support system is important, it is not the primary information the nurse should gather when assessing the child's seizure episodes.
The focus should be on the specific details of the seizures to ensure appropriate management and care for the child.
A nurse is conducting a safety assessment for a child with epilepsy.
What measures should the nurse consider implementing to prevent injury during seizures?
Explanation
Choice A rationale:
Removing sharp objects or hazards from the child's environment is essential for preventing injury during seizures.
Seizures can lead to uncontrolled movements and may cause the child to inadvertently come into contact with hazardous objects, potentially resulting in injuries.
Removing such objects from the environment is a crucial safety measure.
Choice B rationale:
Administering antiepileptic medication is not a safety measure to prevent injury during seizures; it is a part of the child's long-term management plan.
Antiepileptic medications are prescribed to help control and reduce the frequency and severity of seizures but do not address immediate safety concerns during a seizure.
Choice C rationale:
Placing the child in a prone position is not a safe practice during a seizure.
The recommended position during a seizure is the recovery position, which helps maintain an open airway and prevents aspiration.
Placing the child in a prone position can increase the risk of airway obstruction and should be avoided.
Choice D rationale:
Ensuring the child's head is protected is a crucial safety measure during seizures.
Head injuries are a common risk during seizures due to the uncontrolled movements and thrashing that may occur.
Protecting the head with padding or by placing a soft object underneath can reduce the risk of head injuries.
Choice E rationale:
Restricting the child's fluid intake is not a typical safety measure during seizures.
Dehydration can be a concern, and it's important to maintain the child's hydration status, especially if there are any concerns related to antiepileptic medications or other medical conditions.
Restricting fluids can lead to potential health risks and is not a recommended safety measure during seizures.
What aspects should the nurse assess during this examination?
Explanation
Choice A rationale:
During a neurological assessment of a child with epilepsy, the nurse should assess the child's sensory responses.
This includes evaluating the child's sensory perception, such as touch, pain, temperature, and proprioception.
Sensory responses are essential to determine if there are any sensory deficits or abnormalities that may be related to the child's epilepsy or its management.
Choice B rationale:
The child's family history of epilepsy is not directly relevant to the neurological assessment of the child.
While a family history of epilepsy can be significant in understanding the potential genetic component of the condition, it is not part of the immediate neurological assessment.
Choice C rationale:
The child's blood glucose levels are important but not typically assessed as part of a neurological assessment for epilepsy.
Blood glucose levels are more relevant in the evaluation of other conditions, such as diabetes.
However, if a child has diabetes and epilepsy, blood glucose levels may be monitored for overall health management.
Choice D rationale:
The child's cognitive abilities should be assessed during a neurological assessment of epilepsy.
Cognitive abilities, including memory, attention, language, and problem-solving skills, are important to assess as epilepsy can impact these functions.
Changes in cognitive abilities may be indicative of the effects of seizures or the side effects of antiepileptic medications, making this assessment relevant.
The child experiences absence seizures.
What should the nurse include in the documentation?
Explanation
Choice A rationale:
In documenting a child's seizures, it's important to include the type and duration of the seizures.
This information is crucial for healthcare providers to properly diagnose and manage the condition.
Absence seizures are a type of seizure characterized by brief episodes of altered consciousness, which may involve staring spells or minor movements.
Understanding the type and duration of these seizures helps in making an accurate diagnosis and determining the appropriate treatment and management strategies.
Choice B rationale:
The child's genetic test results are not typically relevant when documenting the characteristics of seizures, particularly absence seizures.
Genetic testing may be considered in certain cases, especially when there is a family history of epilepsy or a suspected genetic component, but it is not a standard part of documenting seizure characteristics.
Choice C rationale:
The child's mood swings are not directly related to documenting the characteristics of seizures.
While mood changes can sometimes be associated with epilepsy, they are not the primary focus of documentation.
The key information to include is the type and duration of seizures, as this helps healthcare providers in assessing and managing the condition.
Choice D rationale:
Visual hallucinations are not typically associated with absence seizures, and including them in the documentation may lead to confusion.
Absence seizures are characterized by a brief loss of awareness and consciousness, often without any significant movements or hallucinations.
Therefore, the presence of visual hallucinations would be more relevant to other types of seizures and should not be included in the documentation of absence seizures.
Which statement by the nurse is accurate regarding seizure precautions?
Explanation
Choice A rationale:
Keeping the child away from bright lights during a seizure is an accurate statement regarding seizure precautions.
Bright or flashing lights can trigger seizures in some individuals, a condition known as photosensitive epilepsy.
It's important to create an environment that minimizes potential seizure triggers, including avoiding bright or flashing lights, to reduce the risk of seizures in susceptible individuals.
Choice B rationale:
The statement "The child should avoid taking baths to prevent seizures" is not accurate.
Taking a bath is not a common trigger for seizures, and there is no need to advise against it as a general precaution.
Seizure precautions should focus on more common triggers, such as sleep deprivation, stress, or specific environmental factors.
Choice C rationale:
Wearing medical identification is necessary for children with epilepsy.
This helps inform healthcare providers, first responders, and others about the child's condition in case of a medical emergency.
Medical identification, such as a bracelet or necklace, can provide crucial information about the child's epilepsy and any specific medications or allergies they may have.
Choice D rationale:
"Creating a safe environment involves removing all potential triggers" is not entirely accurate.
While minimizing potential triggers is essential, it's not always possible to eliminate all triggers, and some triggers may be individual-specific.
Seizure management also involves ensuring the child's safety during a seizure by providing a safe space and support.
Removing all potential triggers may not always be feasible, but it's essential to take reasonable precautions.
Which statement by the client reflects their understanding of medication management?
Explanation
Choice B rationale:
The statement "I need to closely monitor for any side effects and report them to the doctor" reflects an understanding of medication management for children with epilepsy.
Antiepileptic medications can have side effects, and it's important for caregivers to be vigilant in monitoring the child for any adverse reactions.
Promptly reporting any side effects to the doctor allows for adjustments to the medication regimen or other interventions as needed.
Choice A rationale:
"I should stop the medication if my child has a single seizure" is not a correct understanding of medication management for epilepsy.
Discontinuing medication after a single seizure is not recommended.
Epilepsy treatment typically involves ongoing medication to reduce the frequency and severity of seizures.
Stopping medication abruptly can lead to uncontrolled seizures.
Choice C rationale:
"Medication compliance is not crucial for children with epilepsy" is an incorrect statement.
Medication compliance is essential for managing epilepsy effectively.
Missing doses or not taking medication as prescribed can lead to uncontrolled seizures and potentially serious consequences.
Caregivers should ensure that the child takes their medication as directed by the healthcare provider.
Choice D rationale:
"Antiepileptic medications are only given during a seizure" is not accurate.
Antiepileptic medications are typically prescribed to be taken regularly, even when the child is not actively experiencing a seizure.
These medications are used to prevent seizures and maintain seizure control over time.
They are not meant to be taken solely during a seizure episode.
Down Syndrome
A student asks, "What is the primary cause of Down syndrome?" Which response by the nurse is correct?
Explanation
Choice A rationale:
Down syndrome is primarily caused by the presence of an extra copy of chromosome 21, not chromosome 22.
This condition is known as Trisomy 21, where an individual has three copies of chromosome 21 instead of the usual two.
This extra genetic material disrupts normal development and results in the characteristic features of Down syndrome.
Choice B rationale:
Down syndrome is not caused by an error in cell division resulting in an extra copy of chromosome 20.
Trisomy 20 is not associated with Down syndrome.
The genetic basis of Down syndrome is the extra copy of chromosome 21.
Choice D rationale:
Down syndrome is not primarily due to a deletion of chromosome 18.
Deletion of chromosome 18 results in a different genetic disorder known as Edwards syndrome, not Down syndrome.
The primary genetic anomaly in Down syndrome is the presence of an extra chromosome 21.
The client asks, "What is the most common type of Down syndrome?" How should the nurse respond?
Explanation
Choice A rationale:
Trisomy 20 is not the most common type of Down syndrome.
The most prevalent form of Down syndrome is Trisomy 21, where there is an extra copy of chromosome 21, resulting in the typical features and characteristics associated with Down syndrome.
Choice B rationale:
Translocation Down syndrome is not the most common type.
Translocation Down syndrome occurs when a part of chromosome 21 attaches to another chromosome, but it is not the most common form.
Trisomy 21 is more common.
Choice C rationale:
Mosaic Down syndrome is not the most common type.
Mosaic Down syndrome is a rarer form in which not all cells have the extra chromosome 21.
The most common type is Trisomy 21, where all cells have the extra chromosome 21.
Which physical characteristics are commonly associated with Down syndrome?
Explanation
Choice A rationale:
Almond-shaped eyes are a common physical characteristic associated with Down syndrome.
These distinctive eye features are often seen in individuals with the condition.
Choice B rationale:
Low muscle tone is another common physical characteristic of Down syndrome.
This condition, also known as hypotonia, results in reduced muscle strength and can impact motor skills and coordination in individuals with Down syndrome.
Choice C rationale:
While an extra copy of chromosome 21 is the underlying genetic cause of Down syndrome, this is not a physical characteristic that can be observed directly.
It is a genetic abnormality that leads to the physical features associated with Down syndrome.
Choice D rationale:
A prominent nasal bridge is not a common physical characteristic of Down syndrome.
Individuals with Down syndrome may have flatter nasal bridges, which is one of the facial features associated with the condition.
Choice E rationale:
High muscle tone is not a common characteristic of Down syndrome.
In fact, low muscle tone (hypotonia) is more typical in individuals with Down syndrome and can affect their motor development and physical abilities.
A parent asks, "Why do individuals with Down syndrome experience cognitive impairment?" What should the nurse's response include?
Explanation
Choice A rationale:
The statement that "cognitive impairment is not related to genetics" is incorrect.
Down syndrome is a genetic condition caused by the presence of an extra copy of chromosome 21, which directly impacts cognitive functioning.
Choice B rationale:
The statement that "cognitive impairment is primarily due to a lack of intellectual stimulation" is also incorrect.
While early intervention and intellectual stimulation can have a positive impact on individuals with Down syndrome, the condition itself is primarily caused by genetic factors.
Choice C rationale:
The correct answer is choice C, "The impact on brain development and functioning is a key factor.”.
Down syndrome results from an extra copy of chromosome 21, which leads to abnormalities in brain development and functioning.
This genetic anomaly directly affects cognitive abilities.
Individuals with Down syndrome typically have intellectual disabilities due to these genetic factors.
Choice D rationale:
The statement that "cognitive impairment in Down syndrome is caused by a lack of social interaction" is not accurate.
Social interaction can be beneficial for individuals with Down syndrome, but the primary cause of cognitive impairment in Down syndrome is genetic, not social interaction.
The client asks, "What are some common health issues in individuals with Down syndrome?" How should the nurse respond?
Explanation
Choice A rationale:
The statement that "there are no specific health issues associated with Down syndrome" is incorrect.
Individuals with Down syndrome are at an increased risk for several health issues, including congenital heart defects, respiratory problems, and gastrointestinal issues.
Choice B rationale:
The statement that "common health issues include an extra copy of chromosome 22" is incorrect.
Down syndrome is caused by an extra copy of chromosome 21, not chromosome 22.
This extra chromosome leads to the characteristic features and health concerns associated with the condition.
Choice C rationale:
The correct answer is choice C, "Individuals with Down syndrome often experience congenital heart defects.”.
Congenital heart defects are one of the most common health issues in individuals with Down syndrome.
These heart defects can vary in severity and may require medical intervention.
Choice D rationale:
The statement that "the primary health concern is related to a lack of physical activity" is not accurate.
While physical activity is essential for overall health, it is not the primary health concern associated with Down syndrome.
Congenital heart defects and other medical issues are more significant health concerns for individuals with this condition.
Which physical characteristics should the nurse observe for in the infant?
Explanation
Choice A rationale:
The physical characteristics to observe for in a newborn with Down syndrome include upward slanting eyes, a flat nasal bridge, and a small mouth.
These features are part of the characteristic facial appearance associated with Down syndrome.
It's important to note that not all infants with Down syndrome will exhibit these features to the same degree.
Choice B rationale:
The statement that infants with Down syndrome have "high muscle tone and joint stiffness" is not accurate.
In fact, infants with Down syndrome often exhibit low muscle tone (hypotonia), which can affect their motor development.
Choice C rationale:
The statement that infants with Down syndrome have "above-average height and weight" is not typically observed.
Growth patterns can vary among individuals with Down syndrome, but there is no consistent pattern of above-average height and weight associated with the condition.
Choice D rationale:
The statement that infants with Down syndrome have "perfectly symmetrical facial features" is not accurate.
Infants with Down syndrome typically have distinct facial features, including the upward slanting eyes and a flatter nasal bridge, which are characteristic of the condition.
What additional information should the nurse gather during the assessment?
Explanation
Evaluate growth parameters, including height, weight, and head circumference.
Choice A rationale:
It is essential to evaluate growth parameters when assessing a child with Down syndrome for several reasons.
Children with Down syndrome often have growth-related concerns, including growth delays and potential issues with weight management.
By monitoring height, weight, and head circumference, the nurse can assess whether the child is following a growth curve that is appropriate for their age.
Deviations from normal growth patterns may indicate underlying health issues that need to be addressed.
Furthermore, assessing head circumference is important because changes in head size can be indicative of conditions such as hydrocephalus, which is more common in individuals with Down syndrome.
Choice B rationale:
Monitoring for speech and language delays is relevant when assessing children with Down syndrome, as they often experience communication challenges.
However, in the context of the presented case where low muscle tone and joint laxity are observed, focusing on growth parameters is more immediately relevant.
Speech and language delays can be assessed in a separate part of the assessment.
Choice C rationale:
Assessing for above-average motor skills development is not a priority in this scenario.
Children with Down syndrome typically experience low muscle tone, which can affect their motor skills development.
It is important to address the observed low muscle tone first before assessing motor skills.
Choice D rationale:
Screening for heart defects and gastrointestinal abnormalities is crucial in the overall care of a child with Down syndrome.
However, in the context of the initial assessment of low muscle tone and joint laxity, evaluating growth parameters is more directly related to the observed physical findings.
Heart defects and gastrointestinal abnormalities can be assessed as part of a comprehensive evaluation but are not the primary focus at this stage.
Select all the appropriate aspects the nurse should evaluate.
Explanation
Cognitive abilities and intellectual functioning.
B. Hearing or vision impairments.
C. Social interactions and ability to form relationships.
E. Emotional well-being of the child and their family members.
Choice A rationale:
Evaluating cognitive abilities and intellectual functioning is crucial when assessing a child with Down syndrome.
These individuals may have varying degrees of cognitive impairment, and understanding their intellectual capabilities is essential for tailoring educational and therapeutic interventions.
Choice B rationale:
Assessing hearing and vision impairments is vital because children with Down syndrome are at an increased risk of sensory deficits, including hearing and vision problems.
Identifying and addressing these issues early can significantly impact the child's development and overall well-being.
Choice C rationale:
Evaluating social interactions and the ability to form relationships is important for assessing the child's social and emotional development.
Children with Down syndrome may face challenges in socialization and communication, and the nurse should assess their progress in developing relationships with peers and caregivers.
Choice D rationale:
High muscle tone and joint stiffness are not typical characteristics of individuals with Down syndrome.
In fact, as mentioned in the question stem, low muscle tone and joint laxity are more common in this population.
Therefore, assessing for high muscle tone and joint stiffness is not relevant in this context.
Choice E rationale:
Assessing the emotional well-being of the child and their family members is important as it can have a significant impact on the overall quality of life.
However, the assessment of emotional well-being should be conducted alongside the evaluation of other developmental aspects, as it is not a direct developmental milestone like cognitive abilities, social interactions, or sensory impairments.
Explanation
Performing a physical examination to assess characteristic features.
Choice A rationale:
Monitoring for gastrointestinal abnormalities is an important aspect of caring for a child with Down syndrome but is not a component of the initial assessment for diagnosing Down syndrome.
The diagnosis of Down syndrome is typically based on clinical features and genetic testing, not on the presence of gastrointestinal abnormalities.
Choice B rationale:
Performing a physical examination to assess characteristic features is indeed an essential component of the assessment process for diagnosing Down syndrome.
There are specific physical characteristics associated with Down syndrome, including a characteristic facial appearance, low muscle tone, joint laxity, and other features.
A physical examination helps confirm the clinical signs of Down syndrome, which can then be confirmed through genetic testing.
Choice C rationale:
Administering psychological tests to assess cognitive abilities is a valuable assessment for children with Down syndrome, but it is not a primary component of the diagnostic process.
The diagnosis is typically made based on clinical features and genetic testing.
Psychological tests may be conducted after the diagnosis to assess the child's cognitive abilities and inform their educational plan.
Choice D rationale:
Conducting DNA sequencing tests is not typically the first step in diagnosing Down syndrome.
The diagnosis is often based on clinical evaluation, including the physical examination of characteristic features, and confirmed through genetic testing such as karyotyping or chromosomal microarray analysis.
Which aspects should the nurse consider during this assessment?
Explanation
Choice A rationale:
Fine and gross motor skills are important aspects to assess in a child's developmental evaluation, but these primarily pertain to physical abilities and coordination.
When assessing the cognitive abilities of a child with Down syndrome, it's essential to focus on intellectual functioning and developmental milestones, which include cognitive aspects such as problem-solving, memory, and language development.
Choice A is not the most appropriate answer in this context.
Choice B rationale:
Speech and language delays are certainly important to consider when assessing a child with Down syndrome, as many children with this condition may experience delays in their speech and language development.
However, this choice only addresses one aspect of cognitive abilities, while the question asks for what aspects the nurse should consider during the assessment.
Therefore, choice B is not comprehensive enough to address the full scope of cognitive abilities in a child with Down syndrome.
Choice C rationale:
The emotional well-being of the child and their family members is undoubtedly important, but this relates more to the psychosocial aspects of care rather than the assessment of cognitive abilities.
While addressing emotional well-being is crucial, it is not the primary focus when assessing cognitive abilities.
Therefore, choice C is not the most appropriate answer in this context.
Choice D rationale:
Intellectual functioning and developmental milestones are the key areas that the nurse should consider during the assessment of a child with Down syndrome.
Children with Down syndrome often have unique cognitive profiles, and assessing their intellectual abilities and developmental progress is essential for tailoring educational and therapeutic interventions.
This choice provides the most comprehensive and relevant answer to the question.
What nursing interventions should the nurse prioritize to promote the well-being of the individual?
Explanation
Choice A rationale:
Creating a safe environment, encouraging physical activity, and offering counseling are appropriate nursing interventions to promote the well-being of an individual with Down syndrome.
Safety is essential to prevent injuries, and physical activity can support overall health and well-being.
Additionally, counseling can address emotional and psychological needs, which are often important for individuals with Down syndrome.
This choice covers a wide range of well-being aspects.
Choice B rationale:
Administering medications, monitoring vital signs, and facilitating communication are important aspects of nursing care, but they may not be the top priorities for promoting the well-being of an individual with Down syndrome.
Medications and vital signs monitoring are specific to medical conditions, and communication is important but does not cover all aspects of well-being.
Choice C rationale:
Providing emotional support, promoting cognitive development, and offering early intervention services are indeed relevant interventions for individuals with Down syndrome.
However, choice A is more comprehensive as it not only includes these but also emphasizes creating a safe environment and counseling, which are essential aspects of overall well-being.
Choice D rationale:
Collaborating with therapists, addressing health conditions, and advocating for inclusive education are important interventions for individuals with Down syndrome, but they may not be the top priorities for promoting overall well-being.
These interventions focus more on specific domains of care, whereas choice A offers a broader perspective on well-being.
What should the nurse recommend to the caregiver?
Explanation
Choice A rationale:
Using age-appropriate educational materials and visual aids is a sound recommendation to support the development of a child with Down syndrome.
These tools can enhance learning and provide valuable resources for educational activities, which are essential for their cognitive development.
Choice B rationale:
Administering medications and monitoring vital signs regularly may be necessary for managing specific health conditions in a child with Down syndrome, but it is not a general recommendation for supporting their development.
This choice is more medically oriented and does not directly address developmental support.
Choice C rationale:
Encouraging regular exercise and creating a nurturing environment are important recommendations for supporting a child's development, including those with Down syndrome.
Physical activity is beneficial for their overall health, and a nurturing environment can provide emotional support and a conducive atmosphere for growth.
Choice D rationale:
Collaborating with healthcare providers and managing chronic health conditions is certainly important, but it is not the primary recommendation for supporting a child's development.
This choice focuses more on health management rather than developmental support, which is the main concern in this context.
A nurse is planning interventions for an individual with Down syndrome.
Which of the following actions should the nurse consider as part of the care plan? Select all that apply:.
Explanation
Choice A rationale:
Collaborating with educators and therapists for individualized education is a crucial part of caring for individuals with Down syndrome.
These individuals often have unique learning needs, and individualized education plans (IEPs) can help address their specific challenges and strengths.
By working with educators and therapists, the nurse can ensure that the individual receives appropriate educational support tailored to their needs.
Choice B rationale:
Administering medications as prescribed for comorbidities is not typically a nursing responsibility.
Medication administration is usually the role of a healthcare provider, such as a physician or nurse practitioner.
While the nurse may need to monitor and report on the individual's response to medications, they should not be responsible for prescribing or administering them.
Choice C rationale:
Encouraging regular physical activity and exercise is important for individuals with Down syndrome.
Physical activity can help improve muscle tone, cardiovascular health, and overall well-being.
It can also support weight management, which is important as obesity is a common issue in this population.
However, it's essential to tailor exercise recommendations to the individual's abilities and needs, and this should be done in collaboration with healthcare providers and therapists.
Choice D rationale:
Providing counseling and guidance to the individual and family is a crucial aspect of caring for individuals with Down syndrome.
This population may face unique social and emotional challenges, and offering support and guidance can help them navigate these issues effectively.
Counseling can address concerns related to behavior, communication, and family dynamics, promoting a higher quality of life for both the individual and their family.
Choice E rationale:
Monitoring and managing associated health conditions are essential in caring for individuals with Down syndrome.
This population is at an increased risk of various medical issues, including congenital heart defects, thyroid disorders, and gastrointestinal problems.
Regular monitoring and timely intervention are necessary to address these health conditions and prevent complications.
However, this is not solely the nurse's responsibility; it involves collaboration with healthcare providers.
What should the nurse advise the parent to do?
Explanation
Choice A rationale:
Facilitating communication and collaboration among healthcare providers is important, but it may not directly address the parent's concerns about advocating for their child's rights and inclusive educational opportunities.
While healthcare providers play a role in the overall care of a child with Down syndrome, advocating for inclusive education and rights involves a different set of actions.
Choice B rationale:
Advocating for community integration and support networks is a crucial step in ensuring that a child with Down syndrome receives the necessary support and educational opportunities.
Inclusive education and social inclusion can significantly benefit these individuals.
Advocacy efforts should focus on building connections with local organizations and support networks that can help the child access the resources and opportunities they need.
Choice C rationale:
Implementing individualized intervention plans with therapists is important for the child's development and well-being.
However, this option is more about the child's therapy and intervention, and it doesn't directly address the parent's role in advocating for their child's rights and inclusive educational opportunities.
Choice D rationale:
Educating themselves about resources and available support networks is an essential step for parents of children with Down syndrome.
Knowledge empowers parents to advocate effectively for their child's rights and educational opportunities.
By understanding available resources and support networks, parents can make informed decisions and connect with the right organizations and individuals to support their child.
What should the nurse consider in managing these health conditions?
Explanation
Choice A rationale:
Administering medications as prescribed with no concerns is an oversimplified approach to managing associated health conditions in individuals with Down syndrome.
While medication adherence is important, it is not the sole responsibility of the nurse, and it doesn't encompass the holistic approach needed for managing the complex health issues often associated with Down syndrome.
Choice B rationale:
Collaborating with healthcare providers to manage chronic health conditions is a comprehensive and appropriate approach.
Many individuals with Down syndrome have chronic health conditions such as heart defects, thyroid issues, and gastrointestinal problems.
Managing these conditions requires a multidisciplinary approach, including input from physicians, therapists, and nurses.
Collaboration ensures that the individual receives the best possible care and support for their specific health needs.
Choice C rationale:
Offering counseling and guidance to the individual and their family is valuable but may not directly address the management of associated health conditions.
Counseling and guidance can support emotional well-being, but the primary focus in managing health conditions should be on medical interventions and coordination of care.
Choice D rationale:
Facilitating communication and collaboration among healthcare providers is essential in managing associated health conditions in individuals with Down syndrome.
Effective communication among the healthcare team ensures that all aspects of the individual's care are addressed, and that interventions are coordinated to provide the best possible outcomes.
This choice complements choice B and is part of the overall strategy for managing complex health conditions.
Sickle Cell Disease
Which statement accurately describes the genetic basis of this condition?
Explanation
Choice A rationale:
"Sickle cell disease results from a dominant genetic mutation.”.
This statement is not accurate.
Sickle cell disease is not caused by a dominant genetic mutation.
It is an autosomal recessive genetic disorder, meaning that both parents must pass on the mutated gene for the disease to manifest.
In this condition, a person must inherit two copies of the mutated HBB gene (one from each parent) to have sickle cell disease.
Choice B rationale:
"Both parents must pass on the mutated gene for sickle cell disease to manifest.”.
This is The correct answer.
Sickle cell disease is inherited in an autosomal recessive manner, which means that it only manifests when a person inherits two copies of the mutated HBB gene, one from each parent.
If only one copy of the gene is inherited, the individual is a carrier (sickle cell trait) and does not have the disease.
Choice C rationale:
"The mutation in the HBB gene leads to the production of normal hemoglobin.”.
This statement is incorrect.
The mutation in the HBB gene results in the production of abnormal hemoglobin, known as hemoglobin S (HbS).
This abnormal hemoglobin is responsible for the characteristic changes in red blood cells seen in sickle cell disease.
Choice D rationale:
"Sickle cell disease is inherited in an autosomal dominant manner.”.
This statement is also incorrect.
Sickle cell disease is not inherited in an autosomal dominant manner.
It is an autosomal recessive genetic disorder, as explained in Choice B.
Which statement by the nurse accurately explains the pathophysiology of this condition?
Explanation
Choice A rationale:
"Hemoglobin S causes red blood cells to become more flexible.”.
This statement is not accurate.
Hemoglobin S (HbS) actually causes red blood cells to become less flexible and take on a characteristic sickle shape.
This change in shape is a key feature of sickle cell disease and can lead to various complications.
Choice B rationale:
"Sickle-shaped cells improve blood flow in the body.”.
This statement is incorrect.
Sickle-shaped cells do not improve blood flow.
In fact, they can impair blood flow by blocking blood vessels.
The abnormal shape of these cells makes them more likely to get stuck in small blood vessels, leading to vaso-occlusive crises and other complications.
Choice C rationale:
"Chronic hemolysis and anemia are not associated with sickle cell disease.”.
This statement is also incorrect.
Chronic hemolysis (the breakdown of red blood cells) is a hallmark of sickle cell disease.
The abnormal shape of sickle cells makes them more fragile, leading to their premature destruction, which results in anemia.
Choice D rationale:
"Sickle-shaped cells can block blood vessels and impair blood flow.”.
This is The correct answer.
Sickle-shaped red blood cells can block blood vessels, leading to vaso-occlusive crises and impaired blood flow.
This is a key part of the pathophysiology of sickle cell disease.
Select all the appropriate self-care strategies for this client:.
Explanation
Choice A rationale:
"Increasing fluid intake to stay hydrated.”.
Staying hydrated is an important self-care strategy for individuals with sickle cell disease.
Dehydration can increase the risk of vaso-occlusive crises and other complications.
Adequate fluid intake helps to prevent the excessive sickling of red blood cells, which can block blood vessels.
Choice B rationale:
"Engaging in regular strenuous physical exercise.”.
Engaging in regular strenuous physical exercise is not an appropriate self-care strategy for individuals with sickle cell disease.
Intense exercise can increase the risk of vaso-occlusive crises and should be done with caution.
Low-impact, moderate exercise may be more suitable for these individuals.
Choice C rationale:
"Avoiding extreme temperature conditions.”.
Avoiding extreme temperature conditions is a sensible self-care strategy for individuals with sickle cell disease.
Extreme cold or heat can trigger vaso-occlusive crises and other complications.
Maintaining a comfortable temperature can help prevent these issues.
Choice D rationale:
"Taking prescribed medications as directed.”.
Taking prescribed medications as directed is crucial for managing sickle cell disease.
This may include medications to manage pain, prevent infections, and reduce complications.
Adhering to the prescribed treatment plan is essential for improving the quality of life and preventing crises.
Choice E rationale:
"Smoking tobacco to alleviate pain.”.
Smoking tobacco is not an appropriate self-care strategy for individuals with sickle cell disease.
Smoking can worsen the condition and increase the risk of complications.
It is important to avoid smoking and any other activities that can harm the lungs or blood vessels in individuals with sickle cell disease.
What interventions should the nurse prioritize when providing care for this client?
Explanation
Administering pain medication as prescribed.
Choice A rationale:
Administering pain medication as prescribed is the highest priority when caring for a client experiencing a sickling crisis in sickle cell disease.
Sickle cell crises are characterized by severe pain due to vaso-occlusion, and the nurse's primary responsibility is to alleviate this pain.
Pain medication helps to relieve the suffering and improve the client's overall comfort.
It is crucial to administer medication promptly to prevent further complications and distress.
Choice B rationale:
Encouraging the client to engage in intense physical activity is not an appropriate intervention during a sickling crisis.
Physical activity can exacerbate the crisis by increasing oxygen demand, which may worsen tissue hypoxia.
It is essential to encourage rest and limit physical exertion to minimize the risk of complications.
Choice C rationale:
Keeping the room at a very low temperature is not a recommended intervention for a sickle cell crisis.
Cold temperatures can cause vasoconstriction, which may further worsen vaso-occlusion.
Maintaining a warm and comfortable environment is more suitable to help ease the client's pain and discomfort.
Choice D rationale:
Encouraging the client to smoke to relieve pain is not a safe or appropriate intervention.
Smoking can lead to vasoconstriction and worsen the client's condition.
It is essential to promote healthy behaviors and provide effective pain management rather than suggesting harmful practices like smoking.
Which clinical manifestations should the nurse be particularly attentive to during the assessment?
Explanation
Jaundice and dark urine.
Choice A rationale:
Pale skin and nail beds are not typically the primary clinical manifestations of sickle cell disease during a crisis.
Sickle cell crises are primarily characterized by vaso-occlusive events leading to severe pain.
While paleness may occur due to anemia associated with sickle cell disease, it is not the hallmark manifestation during a crisis.
Choice B rationale:
An elevation in blood pressure is not a specific clinical manifestation of sickle cell disease.
In fact, individuals with sickle cell disease may experience a drop in blood pressure during a crisis due to reduced blood flow and organ perfusion.
Elevated blood pressure is more likely to be associated with other health conditions or stressors.
Choice C rationale:
Swelling of the lower extremities is not a typical clinical manifestation of sickle cell disease during a crisis.
The hallmark features of a sickling crisis include pain, jaundice, and, in some cases, dark urine, which results from the breakdown of sickled red blood cells.
Swelling may occur in other conditions but is not specific to sickle cell disease.
Choice D rationale:
Jaundice and dark urine are crucial clinical manifestations to monitor in a client with sickle cell disease during a crisis.
Jaundice indicates the breakdown of red blood cells, which is a common occurrence during vaso-occlusive events.
Dark urine results from the excretion of bilirubin, a byproduct of red blood cell breakdown.
These manifestations provide important diagnostic information and guide treatment.
The nurse observes the patient wincing in pain and states, "I feel a sharp, stabbing pain in my abdomen and my joints ache terribly.”.
What is the most likely clinical manifestation of sickle cell disease that the nurse is assessing in this patient?
Explanation
Painful vaso-occlusive crisis.
Choice A rationale:
Impaired immune function is not the primary clinical manifestation assessed in a client with sickle cell disease experiencing severe pain in the joints and abdomen.
While sickle cell disease can affect the immune system, the immediate concern in this scenario is addressing the intense pain caused by vaso-occlusion.
Choice B rationale:
Organ damage is a potential long-term complication of sickle cell disease, but it is not the primary clinical manifestation being assessed in this patient.
The description of sharp, stabbing pain in the abdomen and joint aches is indicative of a vaso-occlusive crisis, and the focus should be on pain management and addressing the crisis itself.
Choice C rationale:
The nurse is most likely assessing a painful vaso-occlusive crisis in this patient.
The description of sharp, stabbing pain and joint discomfort is consistent with the pain experienced during a vaso-occlusive crisis.
These crises are a hallmark feature of sickle cell disease, characterized by the occlusion of blood vessels by sickled red blood cells, resulting in severe pain.
Choice D rationale:
Delayed growth and development are long-term consequences of sickle cell disease, primarily seen in pediatric patients.
In this scenario, the acute issue is the pain and discomfort the patient is currently experiencing, which is more indicative of a vaso-occlusive crisis.
The child's parent reports, "My child always looks pale and gets tired very easily.”.
Based on this information, which complication of sickle cell disease is the nurse most likely assessing in this patient?
Explanation
Choice A rationale:
Pulmonary Hypertension Sickle cell disease is primarily characterized by the presence of abnormal hemoglobin (HbS), leading to the formation of sickle-shaped red blood cells.
While pulmonary hypertension can occur in patients with sickle cell disease, it is not the most likely complication based on the presented symptoms.
The patient's paleness and easy fatigue are more indicative of anemia, which is a common complication in sickle cell disease.
Anemia results from a reduced number of functional red blood cells, leading to reduced oxygen-carrying capacity and fatigue.
Choice C rationale:
Hematuria Hematuria, the presence of blood in the urine, can occur in sickle cell disease, but it is not the most likely complication based on the child's reported symptoms of paleness and easy fatigue.
Hematuria may be associated with other complications such as kidney damage, but it is not the primary concern in this case.
Choice D rationale:
Functional Asplenia Functional asplenia refers to the impaired function of the spleen, which is a common complication in sickle cell disease.
However, the symptoms described by the child's parent, including paleness and easy fatigue, are more indicative of anemia, which is a consequence of sickle cell disease.
A nurse is performing a comprehensive assessment of a patient with sickle cell disease.
Which of the following assessments are essential for monitoring signs and symptoms related to sickle cell disease? .
Explanation
Choice B rationale:
Renal Failure Renal failure is not the most likely complication in this case.
The client's sharp chest pain, aggravated by deep breaths, is more consistent with the symptoms of Acute Chest Syndrome.
This syndrome is a common complication of sickle cell disease and is characterized by chest pain, fever, cough, and shortness of breath.
While kidney complications can occur in sickle cell disease, they are not the primary concern based on the client's presentation.
Choice C rationale:
Acute Chest Syndrome is a more pressing concern due to its potential to lead to severe respiratory distress.
Choice D rationale:
Functional Asplenia Functional asplenia may contribute to the risk of infections in individuals with sickle cell disease, but it is not the primary cause of the client's current symptoms.
The client's chest pain and difficulty breathing are more indicative of Acute Chest Syndrome, a serious and potentially life-threatening complication of sickle cell disease.
The client states, "I have sharp chest pain, and it hurts more when I take a deep breath.”.
Which complication of sickle cell disease is the client likely experiencing?
Explanation
Choice D rationale:
Evaluation of psychosocial well-being and coping mechanisms Monitoring psychosocial well-being and coping mechanisms is essential for holistic care but may not directly relate to monitoring signs and symptoms of sickle cell disease.
The primary focus should be on physical assessments and symptoms related to the disease itself.
Now, let's provide rationales for The correct answers:
Choice A rationale:
Assessment of vital signs, including temperature, heart rate, blood pressure, and respiratory rate Monitoring vital signs is crucial for assessing a patient's overall health and detecting any signs of deterioration.
Patients with sickle cell disease can experience vaso-occlusive crises, which may result in changes in vital signs, such as an elevated heart rate and respiratory rate.
Elevated temperature may indicate an infection, which is another concern in sickle cell disease.
Choice B rationale:
Evaluation of pain intensity and location Sickle cell disease is associated with recurrent painful vaso-occlusive crises, where sickled red blood cells block blood vessels, leading to pain.
Assessing the intensity and location of pain is essential to determine the severity of the crisis and to provide appropriate pain management.
Choice C rationale:
Assessment of neurologic status, including cognitive function and sensory perception Sickle cell disease can lead to complications such as strokes, which may result in neurological deficits.
Monitoring cognitive function and sensory perception is crucial to detect any neurological complications early and provide timely interventions.
Choice E rationale:
Monitoring for signs and symptoms of anemia, such as fatigue, pallor, and shortness of breath Anemia is a common complication in sickle cell disease, and monitoring for signs and symptoms of anemia is vital.
Fatigue, pallor, and shortness of breath are typical manifestations of anemia, and early detection allows for appropriate management and intervention.
These assessments help in ensuring the comprehensive care of patients with sickle cell disease, addressing both acute and chronic complications.
The patient states, "I always feel tired, and I get sick easily, especially with respiratory infections.”.
Based on this information, what aspect of sickle cell disease is the nurse likely evaluating in this patient?
Explanation
Impaired immune function.
Choice A rationale:
Chronic hypoxia.
Chronic hypoxia is not the primary concern described by the patient.
While individuals with sickle cell disease can experience episodes of hypoxia, the patient's main complaints are related to fatigue and frequent infections.
Chronic hypoxia could be a consequence of the disease, but it is not the aspect the nurse is likely evaluating in this case.
Choice B rationale:
Impaired immune function.
The patient's complaints of feeling tired and getting sick easily, especially with respiratory infections, suggest impaired immune function.
Sickle cell disease can affect the spleen, which plays a crucial role in the immune system.
Many individuals with this condition experience functional asplenia, making them more susceptible to infections, particularly encapsulated bacteria like Streptococcus pneumoniae.
This compromised immune function is a significant concern for patients with sickle cell disease, and the nurse should assess and address it.
Choice C rationale:
Delayed growth and development.
Delayed growth and development are not the primary concerns mentioned by the patient in this scenario.
While children with sickle cell disease can experience delayed growth and development due to chronic anemia and other factors, the patient's main complaints are related to fatigue and frequent infections, which are more indicative of impaired immune function.
Choice D rationale:
Vascular occlusion.
Vascular occlusion can be a significant issue in sickle cell disease, leading to pain and tissue damage, but it is not the aspect the nurse is likely evaluating in this patient based on the information provided.
The patient's chief complaints are related to fatigue and frequent infections, suggesting that impaired immune function is the primary concern.
The nurse states, "You may find relief by taking prescribed pain medications promptly and ensuring they are effective.”.
What nursing intervention is the nurse describing?
Explanation
Providing emotional support and counseling to help patients cope with the chronic nature of the disease.
Choice A rationale:
Administering antibiotics prophylaxis to prevent infections.
This option is not the intervention described by the nurse in the scenario.
The nurse is discussing pain management strategies and the importance of taking prescribed pain medications promptly.
Antibiotics prophylaxis is a different aspect of care for sickle cell disease that focuses on preventing infections, particularly those caused by encapsulated bacteria.
Choice B rationale:
Encouraging adequate hydration to prevent dehydration and promote blood flow.
While adequate hydration is essential for individuals with sickle cell disease to prevent dehydration and promote blood flow, it is not the intervention described by the nurse in this scenario.
The nurse is specifically addressing the importance of taking pain medications and ensuring their effectiveness.
Choice C rationale:
Assisting with activities of daily living and mobility to prevent complications and maintain independence.
Assisting with activities of daily living and mobility is an important aspect of care for patients with sickle cell disease, but it is not the intervention mentioned by the nurse in this scenario.
The nurse is emphasizing the need for effective pain management, which is crucial for patients experiencing vaso-occlusive crises.
Choice D rationale:
Providing emotional support and counseling to help patients cope with the chronic nature of the disease.
The nurse is describing the importance of providing emotional support and counseling to help patients cope with the chronic nature of sickle cell disease and the pain associated with it.
This intervention is critical for addressing the emotional and psychological aspects of the disease and ensuring that patients can manage their pain effectively.
It also promotes overall well-being and quality of life for individuals with this chronic condition.
The patient asks, "What activities should I avoid to prevent these painful episodes?" What education is the nurse likely to provide?
Explanation
"It's crucial to stay away from extreme temperatures and physical exertion to prevent vaso-occlusive crises.”.
Choice A rationale:
"It's crucial to stay away from extreme temperatures and physical exertion to prevent vaso-occlusive crises.”.
Extreme temperatures (both hot and cold) can trigger vaso-occlusive crises in patients with sickle cell disease.
Cold temperatures can cause blood vessels to constrict, leading to reduced blood flow and increased risk of blockages, while hot temperatures can lead to dehydration, which can also contribute to vaso-occlusive events.
Physical exertion can increase the risk of sickling, as the cells are more likely to become misshapen and block blood vessels during periods of increased activity.
Choice B rationale:
"You should engage in regular physical activities to keep your body in good shape.”.
While physical activity is generally encouraged for overall health, patients with sickle cell disease need to be cautious about the type and intensity of exercise they engage in.
Strenuous or high-impact activities can increase the risk of vaso-occlusive crises.
The nurse is likely to advise the patient to engage in regular, moderate physical activity that does not overexert the body.
Choice C rationale:
"Avoiding certain foods can significantly reduce the frequency of painful episodes.”.
While a healthy diet is important for individuals with sickle cell disease, avoiding specific foods is not the primary strategy for preventing vaso-occlusive crises.
The patient's question is more focused on activities and lifestyle factors that can trigger these painful episodes.
Diet plays a role in overall health and can indirectly affect the frequency of crises, but it is not the primary concern in this context.
Choice D rationale:
"Taking hot showers or baths can help prevent vaso-occlusive crises.”.
Taking hot showers or baths is not a recommended strategy for preventing vaso-occlusive crises.
In fact, exposure to hot water can lead to dehydration, which is a risk factor for sickle cell crises.
The nurse is likely to advise the patient to use warm, not hot, water for bathing and to stay well-hydrated but not to rely on hot showers or baths as a preventive measure for vaso-occlusive events.
A nurse is collaborating with a healthcare team to develop an individualized care plan for a patient with sickle cell disease.
Which interventions are appropriate for the nurse to include in the plan to manage the patient's condition? .
Explanation
Choice A rationale:
Administering blood transfusions to increase the number of healthy red blood cells.
This choice is not appropriate for the management of sickle cell disease because blood transfusions are typically reserved for specific situations, such as severe anemia, acute complications, or in patients with frequent vaso-occlusive crises.
It is not a routine intervention for all patients with sickle cell disease.
Choice B rationale:
Providing genetic counseling and education for individuals and families affected by sickle cell disease.
Genetic counseling and education are essential for patients and families affected by sickle cell disease.
This helps individuals understand the inheritance pattern, make informed family planning decisions, and manage the emotional and psychological aspects of living with a genetic disorder.
Education can also include information on preventive measures.
Choice C rationale:
Educating patients about the importance of regular follow-up appointments and adherence to prescribed treatment regimens.
Regular follow-up appointments and adherence to prescribed treatment regimens are crucial in managing sickle cell disease.
Patients need ongoing monitoring and support to detect complications early, manage pain, and optimize their overall health.
Non-adherence can lead to exacerbations and complications.
Choice D rationale:
Offering oxygen therapy for patients with acute chest syndrome or respiratory distress.
Oxygen therapy is vital for patients with sickle cell disease, especially when they experience acute chest syndrome or respiratory distress.
This intervention helps improve oxygenation, alleviate respiratory distress, and prevent further complications.
Adequate oxygenation is essential to minimize tissue damage and support the body during these acute events.
Choice E rationale:
Encouraging patients to engage in high-intensity physical activities to improve overall health.
Encouraging high-intensity physical activities is not appropriate for patients with sickle cell disease, as it can trigger vaso-occlusive crises and increase the risk of complications.
Patients with sickle cell disease are typically advised to engage in moderate, low-impact physical activities to maintain their health without exacerbating their condition.
The nurse decides to initiate oxygen therapy.
What is the rationale behind this intervention?
Explanation
Choice A rationale:
To increase the number of healthy red blood cells in the patient's body.
The primary goal of oxygen therapy in acute chest syndrome is not to increase the number of healthy red blood cells but to provide immediate relief by improving oxygenation.
Increasing healthy red blood cell production would take time and is not a suitable acute intervention.
Choice B rationale:
To reduce the frequency of pain crises and complications.
Oxygen therapy is not primarily aimed at reducing the frequency of pain crises.
It is used to address acute respiratory distress and improve oxygenation, which is essential in acute chest syndrome.
Choice D rationale:
To prevent infections and enhance the immune system response.
Oxygen therapy is not administered to prevent infections or enhance the immune system response.
Its main purpose is to address respiratory distress and hypoxia in patients with acute chest syndrome.
A nurse is providing psychosocial support and counseling to a patient with sickle cell disease. The patient expresses feelings of anxiety and depression related to the chronic nature of the disease.
What is the primary goal of the nurse's intervention in this situation?
Explanation
Choice A rationale:
To encourage the patient to avoid stressful situations to minimize anxiety.
Avoiding stressful situations is not a comprehensive solution for managing anxiety and depression related to a chronic disease.
While stress management is important, the primary goal should be to address the emotional and psychological impact of the disease and provide support and coping strategies.
Choice B rationale:
To promote self-care strategies, such as stress management and pain management techniques.
Promoting self-care strategies is a valuable component of addressing anxiety and depression, but the primary goal is to address the emotional and psychological impact of the disease.
This can include providing emotional support, counseling, and coping strategies beyond stress and pain management.
Choice D rationale:
To administer prescribed antidepressant medications to alleviate symptoms of depression.
While administering antidepressant medications may be a treatment option, it is not the primary goal of the nurse's intervention.
The primary goal is to address the emotional and psychological impact and provide support and coping strategies.
Medications may be part of a broader treatment plan, but they are not the primary focus of nursing care.
Cerebral Palsy
The child's parent asks, "What could have caused my child's condition?" Which response by the nurse is accurate based on the information provided in the text?
Explanation
Choice A rationale:
Cerebral palsy is not primarily caused by birth asphyxia.
While birth asphyxia can be a contributing factor in some cases, cerebral palsy can result from a variety of causes, including prenatal, perinatal, and postnatal factors.
Choice B rationale:
Cerebral palsy is not commonly caused by genetic factors.
While genetic factors can play a role in some cases, they are not the most common cause of cerebral palsy.
Choice C rationale:
Multiple births are not the leading cause of cerebral palsy.
While the risk of cerebral palsy may be slightly higher in multiple births, it is not the primary cause.
Choice D rationale:
The correct answer is D.
Cerebral palsy can result from various factors, including infections and maternal health issues.
Cerebral palsy is a complex condition, and it can be caused by a combination of factors, including prenatal infections, maternal health problems, and perinatal issues, among others.
Explanation
Choice A rationale:
Cerebral palsy is not limited to only one type, which is spastic.
There are multiple types of cerebral palsy with different characteristics.
Choice B rationale:
There are more than two main types of cerebral palsy.
The correct answer is D, as it mentions the four main types of cerebral palsy: spastic, dyskinetic, ataxic, and mixed.
Choice C rationale:
While spastic, dyskinetic, and ataxic are three common types of cerebral palsy, The correct answer is D, which includes the additional type of cerebral palsy, "mixed.”.
Choice D rationale:
The correct answer is D.
Cerebral palsy has four main types, including spastic, dyskinetic, ataxic, and mixed.
This provides a comprehensive overview of the types of cerebral palsy.
Which statements about cerebral palsy should the nurse include in the presentation? (Select all that apply).
Explanation
Choice A rationale:
Cerebral palsy is not solely caused by genetic factors.
While genetic factors can contribute, cerebral palsy is a complex condition with various causes, including prenatal, perinatal, and postnatal factors.
Choice B rationale:
Ataxic cerebral palsy primarily affects balance and coordination.
This statement is correct, but it is not one of the options you can select.
Choice C rationale:
Premature birth is a perinatal factor associated with cerebral palsy.
This is correct, as premature birth is a risk factor for cerebral palsy.
Choice D rationale:
Spastic cerebral palsy is not characterized by involuntary movements.
It is characterized by muscle stiffness and spasticity.
Choice E rationale:
Cerebral palsy can result from postnatal factors like infections and traumatic brain injury.
This statement is correct, as cerebral palsy can have both prenatal and postnatal causes.
Infections and traumatic brain injury are examples of postnatal factors that can lead to cerebral palsy.
Explanation
Choice A rationale:
"Spastic cerebral palsy involves involuntary and uncontrolled movements.”.
This statement is not accurate.
Spastic cerebral palsy is not characterized by involuntary and uncontrolled movements.
In fact, it is characterized by increased muscle tone and stiffness, which can lead to difficulties in movement.
Involuntary and uncontrolled movements are more commonly associated with other types of cerebral palsy, such as dyskinetic cerebral palsy.
Choice B rationale:
"It primarily affects balance and coordination.”.
This statement is not correct.
While spastic cerebral palsy can affect balance and coordination to some extent, its primary characteristic is increased muscle tone and stiffness.
This stiffness can make it challenging for individuals with spastic cerebral palsy to control their movements, but it's not primarily about balance and coordination.
Choice C rationale:
"Spastic cerebral palsy is characterized by increased muscle tone and stiffness.”.
This is The correct choice.
Spastic cerebral palsy is indeed characterized by increased muscle tone and stiffness, which can result in tight and rigid muscles.
This stiffness can affect the range of motion and lead to difficulties in performing coordinated movements.
Choice D rationale:
"It is a mixed type of cerebral palsy.”.
This statement is not accurate.
Spastic cerebral palsy is one of the specific subtypes of cerebral palsy, and it is not a mixed type.
There are different subtypes of cerebral palsy, each with its own distinct characteristics, and spastic cerebral palsy is characterized by increased muscle tone and stiffness.
What should the nurse inform the caregiver based on the information provided in the text?
Explanation
Choice A rationale:
"Cerebral palsy is primarily caused by genetic factors.”.
This statement is not accurate.
While genetics can play a role in the development of cerebral palsy, it is not primarily caused by genetic factors.
Cerebral palsy can result from various factors, including prenatal infections, birth complications, and exposure to toxins.
It is a complex condition with multiple potential causes.
Choice B rationale:
"Infections during pregnancy are the main cause of cerebral palsy.”.
This statement is also not entirely accurate.
While infections during pregnancy can increase the risk of cerebral palsy, they are not the main cause.
Cerebral palsy can result from various factors, and the main causes are often considered to be prenatal brain injuries, premature birth, and other perinatal factors.
Choice C rationale:
"Multiple births are the leading cause of cerebral palsy.”.
This statement is not accurate.
While multiple births, such as twins or triplets, can increase the risk of cerebral palsy, they are not the leading cause.
Multiple births are a factor that can contribute to the development of cerebral palsy, but it is not the primary cause.
Choice D rationale:
"Cerebral palsy can result from various factors, including premature birth and exposure to toxins.”.
This is The correct choice.
Cerebral palsy can indeed result from various factors, including premature birth and exposure to toxins.
Premature birth is a significant risk factor, and exposure to toxins during pregnancy can also increase the risk of cerebral palsy.
It is a multifactorial condition with multiple potential causes.
Which of the following clinical manifestations should the nurse specifically inquire about?
Explanation
Choice A rationale:
"Is the child experiencing seizures?" While seizures can be a concern in some cases of cerebral palsy, they are not the primary clinical manifestation that characterizes the condition.
The primary concern in cerebral palsy is related to motor function and coordination.
Choice B rationale:
"Can the child roll over, sit, crawl, or walk at the expected age?" This is The correct choice.
When assessing a child suspected of having cerebral palsy, the nurse should inquire about developmental milestones such as rolling over, sitting, crawling, and walking.
Delayed achievement of these milestones can be an early sign of cerebral palsy and is an essential part of the assessment.
Choice C rationale:
"Has the child had a genetic test to identify underlying causes?" While genetic testing can be a part of the diagnostic process for cerebral palsy, it is not one of the primary clinical manifestations that the nurse should inquire about.
The focus of the assessment should be on the child's physical and developmental abilities.
Choice D rationale:
"Is the child experiencing vision and hearing impairments?" Vision and hearing impairments can be associated with cerebral palsy, but they are not the primary clinical manifestations that the nurse should specifically inquire about.
The focus should be on motor and developmental milestones as they are more indicative of cerebral palsy.
Which statement by the client indicates an accurate understanding of their condition?
Explanation
Choice A rationale:
The statement, "I have no issues with coordination or balance," is incorrect because cerebral palsy often affects coordination and balance, and the client's reported symptoms indicate otherwise.
Choice B rationale:
The statement, "My muscles are floppy, which is completely normal," is incorrect because floppy or hypotonic muscles are not a normal characteristic of cerebral palsy.
The condition typically presents with abnormal muscle tone.
Choice C rationale:
The statement, "I often experience involuntary movements," is also incorrect.
While involuntary movements can be a symptom of some forms of cerebral palsy, it doesn't encompass the full spectrum of the condition, which includes issues with muscle tone and coordination.
Choice D rationale:
This is The correct answer.
The statement, "I'm aware that abnormal muscle tone is a common symptom," indicates an accurate understanding of the condition.
Cerebral palsy is characterized by abnormal muscle tone, which can manifest as stiffness, tightness, or spasticity, affecting a person's ability to maintain balance and coordinate movements.
This response demonstrates knowledge of one of the key features of cerebral palsy.
Select all the appropriate components the nurse should include in the assessment.
Explanation
Choice A rationale:
Evaluating the child's cognitive function and developmental milestones is crucial in the assessment of a child with cerebral palsy.
This condition can affect not only motor skills but also cognitive and developmental aspects.
Assessing these areas helps in developing a comprehensive understanding of the child's needs and abilities.
Choice B rationale:
Checking if the child had an MRI or CT scan to assess brain structure is essential in the assessment of cerebral palsy.
These imaging studies can provide valuable information about brain abnormalities or lesions that may have contributed to the development of cerebral palsy.
Choice C rationale:
Asking the child about any hearing difficulties is important because hearing impairments can co-occur with cerebral palsy, and it's crucial to address all potential challenges a child may face.
This information can guide appropriate interventions and support.
Choice D rationale:
Observing the child's posture, gait, and mobility is a fundamental part of assessing cerebral palsy.
These physical observations can help determine the type and severity of motor impairments associated with the condition.
They also aid in developing tailored rehabilitation and therapeutic plans.
Choice E rationale:
Inquiring about the child's preferences for recreational activities is not directly related to the assessment of cerebral palsy.
While recreational activities are important for a child's overall well-being, they are not primary components of the initial assessment process for this specific condition.
What action should the nurse take based on this observation?
Explanation
Choice A rationale:
Recommending immediate genetic testing is not the appropriate action based on the observation of speech and language difficulties in a child with cerebral palsy.
These difficulties are primarily related to motor control and neurological issues, rather than genetics.
Choice B rationale:
Initiating a referral for a hearing assessment is not The correct action for speech and language difficulties observed in a child with cerebral palsy.
Hearing assessments are more relevant when hearing impairments are suspected, but in this case, the issue is related to communication and motor control.
Choice C rationale:
This is The correct answer.
Documenting the speech and language difficulties is the appropriate action.
Documenting the observed difficulties is essential for the child's medical record and helps in developing a comprehensive care plan and tracking progress.
It also serves as a basis for appropriate interventions.
Choice D rationale:
Assessing the child's cognitive development is not the immediate action needed in response to speech and language difficulties observed in a child with cerebral palsy.
While cognitive assessments are important, addressing the speech and language challenges should take precedence in this scenario.
What nursing intervention should the nurse prioritize to promote the child's independence and well-being?
Explanation
Choice A rationale:
Assisting with bathing and dressing is a fundamental nursing intervention to promote the independence and well-being of a child with cerebral palsy.
Encouraging the child to participate in these activities to the best of their ability fosters a sense of autonomy and self-esteem.
It also helps maintain their personal hygiene and physical comfort, which are essential for overall well-being.
Choice B rationale:
Addressing communication difficulties is undoubtedly important for a child with cerebral palsy.
However, communication interventions should not be the nurse's primary focus unless it is specifically the child's most urgent need.
Communication strategies are crucial for the child to express their needs and desires effectively, but assisting with daily activities like bathing and dressing is more foundational for their overall well-being.
Choice C rationale:
Managing seizures is a critical aspect of care for a child with cerebral palsy, as seizures can be life-threatening.
However, the question is about promoting independence and well-being.
While seizure management is essential, it is more focused on the child's safety rather than directly promoting their independence.
It should be addressed but not necessarily prioritized over other daily living activities.
Choice D rationale:
Correcting skeletal deformities is an important aspect of care for children with cerebral palsy, especially when such deformities affect their mobility and quality of life.
However, like seizure management, it is not the primary intervention for promoting independence and well-being.
Correcting skeletal deformities is important for physical function but may not have the immediate impact on independence and well-being that activities like bathing and dressing can provide.
Which nursing intervention is essential for managing this symptom?
Explanation
Choice C rationale:
Spasticity is a common symptom in cerebral palsy, characterized by increased muscle tone and stiffness.
Implementing range of motion exercises and positioning techniques is essential in managing spasticity.
Range of motion exercises help prevent contractures and maintain joint flexibility, which can improve the client's comfort and mobility.
Proper positioning techniques can relieve pressure on the affected muscles and joints, reducing pain and discomfort.
These interventions are fundamental in improving the client's quality of life and functionality.
Choice A rationale:
Educating the family on proper nutrition is important for the overall health and well-being of the client with cerebral palsy, but it is not the primary intervention for managing spasticity.
While good nutrition can support the client's general health, it may not directly address the spasticity symptoms.
Choice B rationale:
Collaborating with occupational therapists is essential in the care of a client with cerebral palsy, as they can provide valuable insights and interventions.
However, this choice does not directly address the management of spasticity.
Occupational therapists can be involved in various aspects of care, including adaptive equipment and activities of daily living, but they may not be the primary intervention for spasticity management.
Choice D rationale:
Providing emotional support is crucial in caring for clients with cerebral palsy, as they often face physical and emotional challenges.
However, emotional support, while important, is not the primary intervention for managing spasticity.
Spasticity is a physical symptom that requires specific interventions to improve the client's comfort and mobility.
Select all the appropriate nursing interventions for promoting the child's well-being and independence.
Explanation
Choice A rationale:
Assisting with mobility aids and adaptive devices is essential for promoting the child's well-being and independence.
Many children with cerebral palsy have mobility impairments, and providing them with the necessary aids and devices can significantly improve their ability to move and explore their environment.
This can include wheelchairs, walkers, orthotic devices, or any other assistive technology.
By enabling the child to move more freely, you enhance their independence and quality of life.
Choice B rationale:
Providing support for activities of daily living is another crucial aspect of caring for a child with cerebral palsy.
Many children with cerebral palsy may struggle with basic self-care tasks, such as dressing, feeding, and hygiene.
By offering support and teaching them adaptive techniques, nurses can help these children become more self-reliant.
This support empowers the child and fosters their independence.
Choice C rationale:
Administering medications to manage spasticity is a potential intervention for some children with cerebral palsy.
However, this is not universally applicable to all children with the condition.
The use of medications depends on the severity of spasticity and should be determined by the child's healthcare provider.
It is not an intervention that should be applied to all cases, and it doesn't directly promote independence.
Choice D rationale:
Collaborating with speech therapists to improve communication skills is an essential intervention, but it is not a primary nursing responsibility.
Speech therapy is typically provided by a specialized therapist.
While the nurse can support the child's participation in speech therapy, it is not a direct nursing intervention for promoting well-being and independence.
Choice E rationale:
Facilitating communication and socialization opportunities is valuable for the child's overall development, but it is not a primary nursing intervention.
Creating opportunities for social interaction and communication is a part of the holistic care approach for children with cerebral palsy.
However, it is typically carried out in collaboration with other healthcare professionals and as part of the child's daily routine rather than as a specific nursing intervention.
Which treatment option should the nurse consider to address these issues?
Explanation
Choice A rationale:
Surgical procedures to correct skeletal deformities are typically considered when there are severe skeletal abnormalities that significantly impact the child's mobility or quality of life.
While this may be necessary in some cases, it is not the first-line treatment for delayed motor milestones and poor coordination in cerebral palsy.
Physical therapy is often the initial approach.
Choice B rationale:
Regular physical therapy sessions to improve muscle strength are a fundamental and effective treatment option for addressing delayed motor milestones and poor coordination in cerebral palsy.
Physical therapy aims to enhance the child's muscle strength, coordination, and overall motor skills.
It is a well-established and evidence-based intervention for children with cerebral palsy.
Choice C rationale:
Medications to manage seizures are relevant if the child with cerebral palsy also experiences seizures, but this choice doesn't directly address the motor coordination and developmental delay issues mentioned in the question.
Choice D rationale:
Occupational therapy is valuable for enhancing daily activities and fine motor skills.
However, it may not be the primary choice for addressing delayed motor milestones and poor coordination, which are more directly addressed through physical therapy.
What should the nurse prioritize in the assessment process?
Explanation
Choice A rationale:
While evaluating cognitive function is important, it may not be the initial priority in the assessment of a child with cerebral palsy.
Priority should be given to aspects that directly impact the child's physical and developmental needs, such as assessing motor function, mobility, and other physical concerns.
Cognitive function assessment may follow but should not be the primary focus.
Choice B rationale:
Assessing vision and hearing impairments should be a priority in the assessment process.
Many children with cerebral palsy may have sensory impairments that can significantly impact their overall well-being and development.
Identifying and addressing vision and hearing issues are critical to providing appropriate care and support.
Choice C rationale:
Focusing on correcting skeletal deformities is essential but may not be the initial priority in the nursing assessment.
Assessing the child's current condition and immediate needs should come before focusing on correction.
Skeletal deformities are often addressed through a multidisciplinary approach and may require consultation with orthopedic specialists.
Choice D rationale:
Performing neuroimaging studies is typically not the primary responsibility of a nurse during the initial assessment of a child with cerebral palsy.
Such studies are ordered by physicians or specialists when specific indications arise, and they are not routinely performed in all cases.
Exams on Common Pediatric Conditions
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Croup
- Tonsillitis in children.
- RSV in children
- Epiglottitis
- Otitis media
- Gastroenteritis in Children:
- Dehydration in Children
- Allergies and Asthma in Children
- Diabetes Mellitus in Children
- Cystic Fibrosis in Children: Comprehensive Nursing Notes
- Congenital Heart Defects in Children
- Epilepsy in Children:
- Down Syndrome
- Sickle Cell Disease
- Cerebral Palsy
- Diabetic Ketoacidosis (DKA) in Children
Notes Highlighting is available once you sign in. Login Here.
Croup
Introduction
- Croup is a common upper respiratory illness of childhood, which is characterized by inflammation, edema, and obstruction of the larynx, trachea, and bronchi.
- Croup is typically caused by a viral infection, most often parainfluenza virus.
- Croup can cause a barking cough, hoarseness, inspiratory stridor, and respiratory distress.
- Croup usually affects children between 6 months and 3 years of age, and is more common in boys than girls.
- Croup can be classified into four types: acute epiglottitis, acute laryngitis, acute laryngotracheobronchitis (LTB), and acute spasmodic laryngitis.
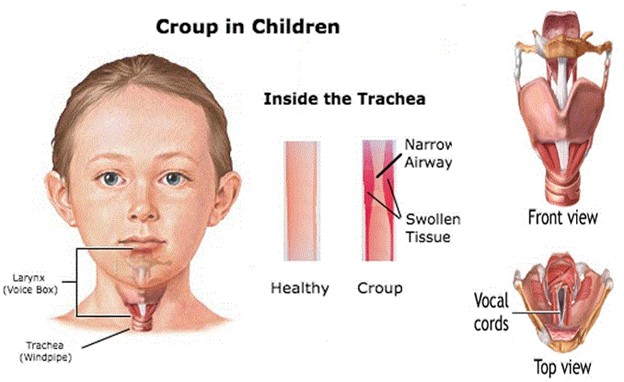
Etiology of Croup
- The most common cause of croup is a viral infection, especially parainfluenza virus type 1.
- Other viruses that can cause croup include respiratory syncytial virus (RSV), adenovirus, rhinovirus, influenza virus, and coronavirus.
- Bacterial infection can also cause croup, such as Haemophilus influenzae type b (Hib), Streptococcus pneumoniae, Staphylococcus aureus, and Moraxella catarrhalis.
- Croup can be transmitted by airborne droplets or direct contact with respiratory secretions.
Croup can occur at any time of the year, but is more prevalent in fall and winter months.
Pathophysiology of Croup
- Croup involves inflammation and edema of the mucosa lining the larynx, trachea, and bronchi.
- The inflammation and edema narrow the airway and increase the resistance to airflow.
- The narrowed airway causes turbulent airflow, which produces the characteristic barking cough and inspiratory stridor.
- The degree of airway obstruction determines the severity of respiratory distress.
- The obstruction can also impair gas exchange and lead to hypoxia and hypercarbia.
Clinical Manifestations of Croup
- The clinical manifestations of croup vary depending on the type and severity of the condition.
- The common signs and symptoms of croup include:
- Barking cough that is worse at night
- Hoarseness or loss of voice
- Inspiratory stridor that is worse when lying down
- Respiratory distress with retractions, nasal flaring, tachypnea, and cyanosis
- Fever, runny nose, sore throat, and malaise
- Anxiety, agitation, or lethargy
- Drooling or difficulty swallowing (in epiglottitis)
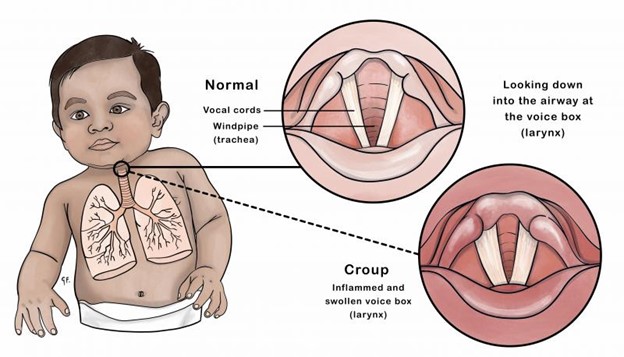
Diagnostic Evaluation of Croup
- The diagnosis of croup is mainly based on the history and physical examination of the child.
- The following tests may be performed to confirm the diagnosis or rule out other causes of respiratory distress:
- Throat culture or rapid antigen test to identify the causative organism
- Blood tests to check for infection, inflammation, and oxygen saturation
- Chest x-ray to visualize the airway narrowing (steeple sign) or other lung abnormalities
- Lateral neck x-ray to detect epiglottal swelling (thumb sign) or retropharyngeal abscess
- Pulse oximetry to monitor oxygen saturation
- Arterial blood gas (ABG) analysis to assess acid-base balance and gas exchange
Nursing Assessment of Croup
- The nursing assessment of a child with croup includes:
- Obtaining a detailed history of the onset, duration, frequency, and severity of symptoms
- Assessing the child’s respiratory status by observing for signs of distress, such as retractions, nasal flaring, tachypnea, cyanosis, stridor, and wheezes
- Auscultating the lungs for breath sounds and adventitious sounds
- Measuring vital signs, including temperature, pulse rate, respiratory rate, blood pressure, and oxygen saturation
- Evaluating the child’s level of consciousness, behavior, and comfort
- Inspecting the throat for redness, swelling, or exudate (avoid using tongue depressor in epiglottitis)
- Asking about any history of allergies, asthma, or exposure to sick contacts
Nursing Assessment of Croup
- The nursing interventions for a child with croup include:
- Maintaining a patent airway and providing oxygen therapy as ordered
- Administering medications as prescribed, such as corticosteroids, racemic epinephrine, antipyretics, and antibiotics (if bacterial infection is present)
- Providing humidified or cool mist therapy to reduce airway edema and inflammation
- Encouraging fluid intake to prevent dehydration and thin secretions
- Positioning the child in a semi-Fowler’s or upright position to facilitate breathing
- Providing comfort measures, such as distraction, relaxation, and reassurance
- Educating the parents about the signs and symptoms of croup, the treatment and management of croup, and the prevention of croup
Treatment and Management of Croup
- The treatment and management of croup depends on the type and severity of the condition.
- Most cases of croup are mild and can be treated at home with supportive care, such as rest, fluids, humidified air, and fever control.
- Moderate to severe cases of croup may require hospitalization and intensive care, such as oxygen therapy, nebulized racemic epinephrine, intravenous corticosteroids, antibiotics (if bacterial infection is present), and mechanical ventilation (if respiratory failure occurs).
- The prognosis of croup is generally good, with most children recovering within a week.
- However, some complications of croup may include hypoxia, respiratory failure, pulmonary edema, pneumonia, bacterial superinfection, and airway obstruction.
Conclusion
- Croup is a common upper respiratory illness of childhood that causes inflammation, edema, and obstruction of the larynx, trachea, and bronchi.
- Croup is typically caused by a viral infection, most often parainfluenza virus.
- Croup can cause a barking cough, hoarseness, inspiratory stridor, and respiratory distress.
- Croup can be diagnosed by history, physical examination, and some tests, such as throat culture, blood tests, chest x-ray, and lateral neck x-ray.
- Croup can be treated with supportive care at home or with oxygen therapy, medications, and mechanical ventilation in the hospital.
- Croup has a good prognosis but may have some complications.
Summary
- Croup is a viral infection that affects the upper airway
- Croup causes inflammation and edema of the larynx, trachea, and bronchi
- Croup causes a barking cough, hoarseness, stridor, and respiratory distress
- Croup is diagnosed by history, physical examination, and some tests
- Croup is treated with supportive care at home or with oxygen therapy, medications, and mechanical ventilation in the hospital
- Croup has a good prognosis but may have some complications
Tonsillitis in children.
Objectives:
- Understand the etiology of tonsillitis in children.
- Explain the pathophysiology of tonsillitis in children.
- Identify the clinical manifestations of tonsillitis in children.
- Describe the diagnostic evaluation methods for tonsillitis in children.
- Perform a comprehensive nursing assessment for a child with tonsillitis.
- Implement appropriate nursing interventions for a child with tonsillitis.
- Discuss the treatment and management options for tonsillitis in children.
Introduction
- Tonsillitis is a common condition in children characterized by inflammation of the tonsils, which are located at the back of the throat. It can be caused by various factors, including viral or bacterial infections. Understanding the etiology, pathophysiology, clinical manifestations, diagnostic evaluation, nursing assessment, nursing interventions, and treatment options for tonsillitis in children is essential for nurses providing care to these patients.
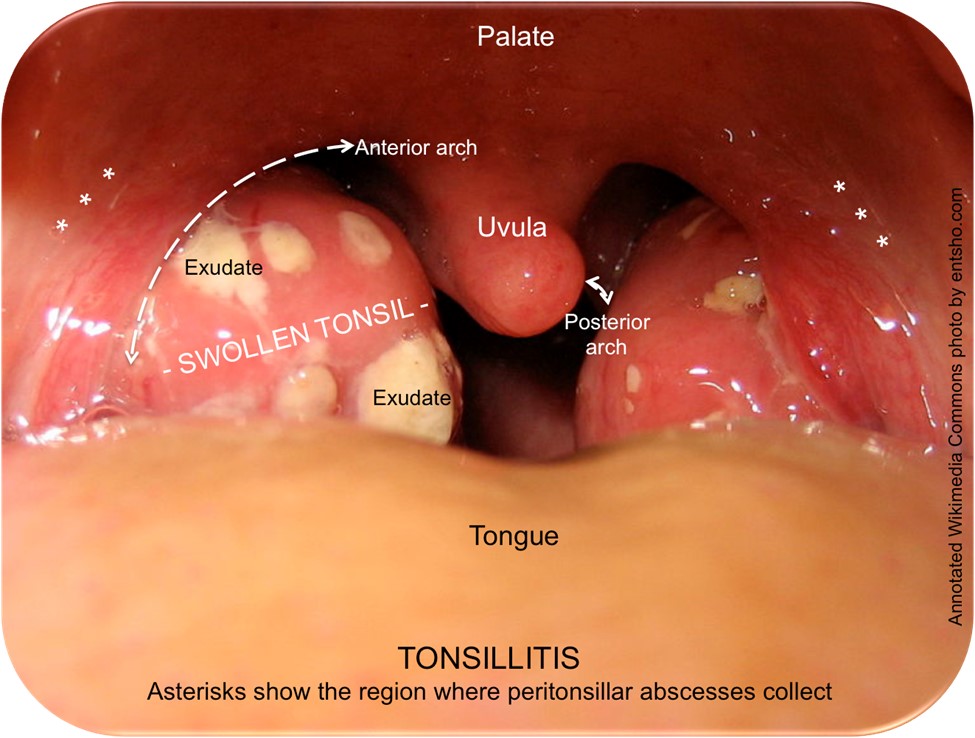
Etiology of Tonsillitis in children:
- Tonsillitis can be caused by viral infections such as adenovirus, rhinovirus, or Epstein-Barr virus.
- Bacterial infections, particularly Streptococcus pyogenes, can also lead to tonsillitis.
- Other factors that contribute to tonsillitis include allergies, irritants, and immune system deficiencies.
Pathophysiology of Tonsillitis in children:
- Tonsillitis occurs when the tonsils become infected and inflamed.
- In viral tonsillitis, the virus invades the tonsillar tissue, leading to an immune response and subsequent inflammation.
- In bacterial tonsillitis, the bacteria colonize the tonsils and trigger an immune response, causing inflammation and swelling.
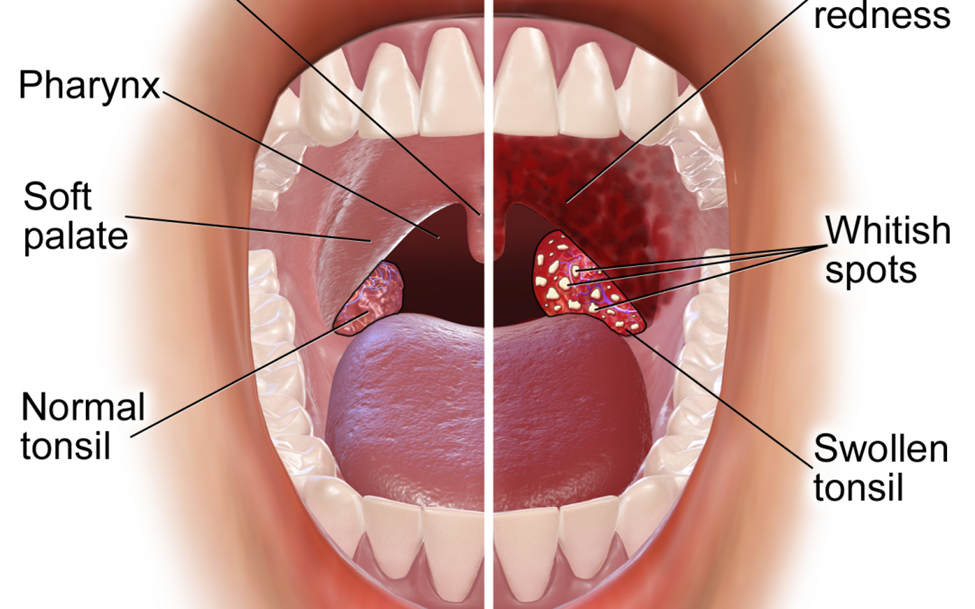
Clinical Manifestations of Tonsillitis in children:
- Sore throat, often severe
- Difficulty swallowing
- Fever
- Red and swollen tonsils, sometimes with white or yellow patches
- Enlarged lymph nodes in the neck
- Bad breath
- Headache
- Abdominal pain
- Fatigue
- In some cases, children with tonsillitis may also experience:
- Drooling
- Bad breath
- Earache
- Neck stiffness
- Abdominal pain
- Vomiting
Diagnostic Evaluation of Tonsillitis in children:
- Throat culture to identify bacterial pathogens, such as Streptococcus pyogenes.
- Rapid strep test to quickly diagnose streptococcal tonsillitis.
- Complete blood count (CBC) to assess for elevated white blood cell count.
- Testing for infectious mononucleosis in suspected cases.
Nursing Assessment of Tonsillitis in children:
- Obtain a detailed medical history, including current and past illnesses, allergies, and medications.
- Assess the child's vital signs, including temperature, heart rate, and respiratory rate.
- Perform a thorough physical examination, focusing on the throat, tonsils, lymph nodes, and overall appearance.
- Evaluate the child's ability to swallow, speak, and breathe comfortably.
Nursing Interventions for Tonsillitis in children:
- Encourage the child to drink plenty of fluids to prevent dehydration.
- Provide pain relief measures, such as acetaminophen or ibuprofen, as prescribed.
- Offer cool or warm liquids and soft foods to soothe the throat.
- Educate the child and family about the importance of completing prescribed antibiotic therapy, if applicable.
- Promote rest and comfort by providing a quiet and calm environment.
Treatment and Management of Tonsillitis in children:
- Antibiotics, such as penicillin or erythromycin, may be prescribed for bacterial tonsillitis.
- Symptomatic relief measures, including pain relievers and throat lozenges, can help alleviate discomfort.
- Surgery, such as tonsillectomy, may be considered for recurrent or severe cases of tonsillitis.
Conclusion
- Tonsillitis in children is a common condition caused by viral or bacterial infections. Nurses play a crucial role in assessing, managing, and educating children and their families about tonsillitis. By understanding the etiology, pathophysiology, clinical manifestations, diagnostic evaluation, nursing assessment, nursing interventions, and treatment options for tonsillitis, nurses can provide effective care and support to children with this condition.
Summary:
- Tonsillitis in children is caused by viral or bacterial infections.
- The pathophysiology involves invasion of the tonsils by the infecting organism, leading to an immune response and inflammation.
- Clinical manifestations include sore throat, difficulty swallowing, fever, and swollen tonsils.
- Diagnostic evaluation includes throat culture, rapid strep test, CBC, and testing for infectious mononucleosis.
- Nursing assessment involves obtaining a detailed medical history, assessing vital signs, and performing a physical examination.
- Nursing interventions include encouraging fluid intake, providing pain relief, and promoting rest and comfort.
- Treatment options include antibiotics, symptomatic relief measures, and surgery in severe cases.
- Nurses play a crucial role in managing and educating children and their families about tonsillitis.
RSV in children
Objectives
- Define RSV and its etiology
- Explain the pathophysiology of RSV infection
- Identify the clinical manifestations of RSV in children
- Describe the diagnostic evaluation of RSV in children
- Perform a nursing assessment of a child with RSV
- Implement nursing interventions for a child with RSV
- Discuss the treatment and management of RSV in children
Introduction
- RSV is a viral illness that causes respiratory tract infections, including the common cold, bronchiolitis, and pneumonia.
- RSV is the most common cause of bronchiolitis and pneumonia in children under one-year-old.
- RSV can affect a person of any age but causes the most problems for the very young and very old.
- RSV is spread by contact with fluid from an infected person’s nose or mouth.
- RSV often occurs in yearly outbreaks in communities, classrooms, and childcare centers.
- RSV is more common in winter and early spring months.
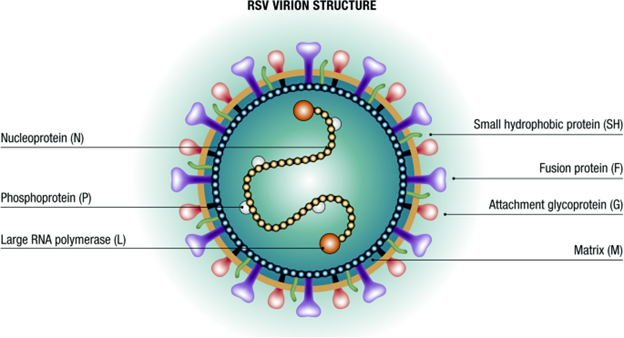
Etiology of RSV
- RSV is caused by a single-stranded RNA virus that belongs to the Paramyxoviridae family.
- There are two subtypes of RSV: A and B.
- Subtype A is more prevalent and more virulent than subtype B.
- RSV can survive on hard surfaces for several hours and on hands for 20 minutes.
- RSV is transmitted by direct or indirect contact with respiratory secretions or droplets from an infected person.
- The incubation period of RSV is 2 to 5 days.
Pathophysiology of RSV infection
- RSV infects the squamous epithelial cells of the bronchioles, alveoli, and nasal passages.
- Infected cells merge with adjacent cells, forming syncytia that burst and die.
- The resulting debris clogs the minute airways and causes inflammation, edema, and mucus production.
- The airways become partially obstructed, allowing air in but hindering air expulsion.
- This leads to wheezing, crackles, rhinorrhea, atelectasis, and hypoxemia.
- In severe cases, RSV infection may cause apnea, pulmonary edema, respiratory failure, or death.
Clinical Manifestations of RSV in children
- The early phase of RSV infection in children is often mild, like a cold.
- The symptoms may include runny nose, fever, cough, irritability, and decreased appetite.
- In children younger than age 3, the illness may progress to bronchiolitis or pneumonia, causing more severe respiratory distress.
- The symptoms may include wheezing, retractions, nasal flaring, tachypnea, cyanosis, lethargy, and apnea.
- The symptoms of RSV infection may last for up to 10 days, with the peak severity occurring around day 56.
Diagnostic Evaluation of RSV in children
- The diagnosis of RSV infection is based on the history, physical examination, and laboratory tests5.
- The laboratory tests may include a nasal swab or wash to detect the virus by antigen detection tests or polymerase chain reaction assays 5.
- Other tests may include a chest X-ray to rule out pneumonia, a blood gas analysis to assess oxygenation status, and a complete blood count to check for leukocytosis or anemia.
- The normal ranges for some parameters are:
|
Parameter |
Normal Range |
|
Respiratory rate |
20 to 40 breaths per minute for infants; 15 to 30 breaths per minute for toddlers; 12 to 25 breaths per minute for preschoolers; 10 to 20 breaths per minute for school-age children |
|
Oxygen saturation |
95% to 100% |
|
pH |
7.35 to 7.45 |
|
PaCO2 |
35 to 45 mmHg |
|
PaO2 |
80 to 100 mmHg |
|
HCO3 |
22 to 26 mEq/L |
|
White blood cell count |
5,000 to 10,000 cells/mm3 |
|
Hemoglobin |
11 to 16 g/dL for infants; 10 to 15 g/dL for children |
Nursing Assessment of a child with RSV
- The nursing assessment of a child with RSV should include the following aspects :
- History: Obtain information about the onset, duration, and severity of symptoms; exposure to other children or adults with respiratory infections; risk factors such as prematurity, chronic lung disease, congenital heart disease, or immunodeficiency; and previous history of RSV infection or asthma.
- Vital signs: Monitor the respiratory rate, heart rate, blood pressure, temperature, and oxygen saturation. Note any signs of respiratory distress such as tachypnea, tachycardia, hypotension, fever, or hypoxia.
- Respiratory system: Auscultate the lungs for wheezes, crackles, or diminished breath sounds. Observe the chest wall for retractions, flaring, or asymmetry. Assess the nasal passages for congestion, discharge, or bleeding. Evaluate the cough for frequency, quality, and productivity.
- Cardiovascular system: Assess the heart sounds for murmurs, gallops, or extra sounds. Palpate the peripheral pulses for rate, rhythm, and strength. Check the capillary refill time for adequacy of perfusion. Inspect the skin for color, temperature, and moisture.
- Gastrointestinal system: Assess the abdomen for distension, tenderness, or masses. Monitor the intake and output for hydration status. Weigh the child daily for fluid balance. Observe the stools for color, consistency, and frequency.
- Neurological system: Assess the level of consciousness, orientation, and behavior. Evaluate the cranial nerve functions for symmetry and sensation. Test the motor and sensory functions for strength and coordination. Check the reflexes for normal response.
- Psychosocial system: Assess the child’s coping skills, emotional state, and developmental level. Provide support and education to the child and family. Encourage parental involvement in care.
Nursing Interventions for a child with RSV
- The nursing interventions for a child with RSV should aim to maintain a patent airway, promote oxygenation, prevent dehydration, reduce fever, prevent complications, and provide comfort. Some examples of nursing interventions are:
- Suction the nose and mouth as needed to remove secretions and improve breathing.
- Administer humidified oxygen as prescribed to increase oxygen delivery.
- Position the child in a semi-Fowler’s or upright position to facilitate lung expansion.
- Monitor the oxygen saturation and blood gas levels to assess oxygenation status.
- Encourage oral fluids or provide intravenous fluids as prescribed to prevent dehydration.
- Offer frequent small feedings of breast milk or formula to maintain nutrition.
- Administer antipyretics as prescribed to reduce fever.
- Avoid aspirin use in children to prevent Reye syndrome.
- Isolate the child from other children or adults with respiratory infections to prevent transmission.
- Use contact precautions such as gowns and gloves when caring for the child to prevent cross-contamination.
- Educate the parents about RSV prevention measures such as hand hygiene, avoiding tobacco smoke exposure, and immunizing high-risk infants with palivizumab.
Treatment and Management of RSV in children
- The treatment and management of RSV in children is mainly supportive and symptomatic. Some examples of treatment modalities are:
- Antiviral therapy: Ribavirin is an antiviral drug that may be used in severe cases of RSV infection in high-risk infants. It is given by aerosol inhalation under strict guidelines. It may have side effects such as bronchospasm, rash, conjunctivitis, or anemia.
- Bronchodilator therapy: Albuterol is a bronchodilator that may be used to relieve bronchospasm and wheezing in children with RSV infection. It is given by nebulizer or metered-dose inhaler. It may have side effects such as tachycardia, tremors, nervousness, or nausea.
- Corticosteroid therapy: Dexamethasone is a corticosteroid that may be used to reduce inflammation and edema in children with RSV infection. It is given by injection or orally. It may have side effects such as hyperglycemia, hypertension, fluid retention, or immunosuppression.
- Antibiotic therapy: Antibiotics are not effective against RSV infection but may be used to treat secondary bacterial infections such as otitis media, sinusitis, or pneumonia. The choice of antibiotic depends on the type and sensitivity of the bacteria. Antibiotics may have side effects such as allergic reactions, diarrhea, or yeast infections.
- Immunoprophylaxis: Palivizumab is a monoclonal antibody that may be used to prevent RSV infection in high-risk infants such as those with prematurity, chronic lung disease, or congenital heart disease. It is given by intramuscular injection once a month during the RSV season. It may have side effects such as fever, rash, or injection site reactions.
Conclusion
- RSV is a common and potentially serious respiratory infection in children, especially those under one year old or with underlying conditions.
- RSV infection causes inflammation, obstruction, and mucus production in the small airways, leading to respiratory distress and hypoxemia.
- RSV infection is diagnosed by history, physical examination, and laboratory tests such as nasal swab or wash.
- RSV infection is treated and managed by supportive and symptomatic measures such as oxygen therapy, fluid therapy, antipyretics, and isolation.
- RSV infection may be prevented by immunoprophylaxis with palivizumab in high-risk infants and by infection control measures such as hand hygiene and avoiding exposure to sick people.
Summary
- RSV is a viral illness that causes bronchiolitis and pneumonia in children
- RSV infects the epithelial cells of the bronchioles and alveoli, causing cell death and debris
- RSV symptoms include runny nose, fever, cough, wheezing, retractions, cyanosis, and apnea
- RSV diagnosis includes nasal swab or wash, chest X-ray, blood gas analysis, and complete blood count
- RSV nursing assessment includes history, vital signs, respiratory system, cardiovascular system, gastrointestinal system, neurological system, and psychosocial system
- RSV nursing interventions include suctioning, humidified oxygen, semi-Fowler’s position, oral or intravenous fluids, antipyretics, isolation, contact precautions, and parent education
- RSV treatment includes antiviral therapy with ribavirin, bronchodilator therapy with albuterol, corticosteroid therapy with dexamethasone, antibiotic therapy for secondary infections, and immunoprophylaxis with palivizumab
Epiglottitis
Objectives
- Define epiglottitis and its etiology
- Explain the pathophysiology of epiglottitis and how it affects the airway
- Identify the clinical manifestations of epiglottitis and how to differentiate it from other conditions
- Describe the diagnostic evaluation of epiglottitis and the role of imaging and laboratory tests
- Perform a nursing assessment of a child with epiglottitis and recognize the signs of impending airway obstruction
- Implement nursing interventions for a child with epiglottitis and provide supportive care and education
- Discuss the treatment and management of epiglottitis and the prevention of complications
Introduction
- Epiglottitis is a potentially life-threatening condition that occurs when the epiglottis, a cartilage flap that covers the entrance to the larynx during swallowing, becomes inflamed and swollen.
- The most common cause of epiglottitis in children is infection by Haemophilus influenzae type b (Hib) bacteria, which can also cause meningitis, pneumonia, and septic arthritis. Other causes include streptococcal or staphylococcal infections, trauma, thermal or chemical injury, foreign body aspiration, or immunodeficiency.
- Epiglottitis can affect children of any age, but it is more common in children between 2 and 8 years old. It is more prevalent in males than females and in colder months than warmer months.
- Epiglottitis can rapidly progress to complete airway obstruction and respiratory failure within hours if not treated promptly. Therefore, it is essential to recognize the signs and symptoms of epiglottitis and provide immediate medical attention.
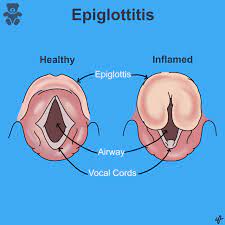
Etiology of Epiglottitis
- The etiology of epiglottitis is usually infectious, with Hib being the most common causative agent. Hib is a gram-negative coccobacillus that colonizes the nasopharynx and can invade the bloodstream and cause systemic infections.
- Hib can reach the epiglottis through hematogenous spread or direct extension from the pharynx. The bacteria can attach to the surface of the epiglottis and produce toxins that damage the tissue and trigger an inflammatory response.
- Other bacteria that can cause epiglottitis include Streptococcus pneumoniae, Streptococcus pyogenes, Staphylococcus aureus, Neisseria meningitidis, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Mycoplasma pneumoniae.
- Non-infectious causes of epiglottitis include trauma to the throat or neck, such as from intubation, foreign body aspiration, or blunt force injury; thermal injury from hot liquids or steam inhalation; chemical injury from caustic substances or drugs; or immunodeficiency from HIV infection or chemotherapy.
Pathophysiology of Epiglottitis
- The pathophysiology of epiglottitis involves the inflammation and edema of the epiglottis and surrounding structures, such as the aryepiglottic folds, arytenoids, and supraglottic larynx.
- The inflammation starts on the lingual surface of the epiglottis and spreads rapidly to involve the entire structure within hours. The edema causes the epiglottis to enlarge and protrude into the laryngeal inlet, obstructing the airflow into the trachea.
- The epithelium of the vocal cords is tightly bound to the underlying tissue, limiting the swelling progression and increasing the pressure in a small area. This leads to further narrowing of the glottic opening and increased airway resistance.
- The obstruction of the airway causes hypoxia, hypercapnia, acidosis, and respiratory distress. The child may adopt a tripod position (leaning forward with outstretched arms, neck extended, and tongue protruding) to maximize airway patency. The child may also drool saliva due to difficulty swallowing and have a muffled voice due to laryngeal edema.
- If left untreated, epiglottitis can progress to complete airway occlusion, resulting in respiratory arrest, cardiac arrest, brain damage, or death.
Clinical Manifestations of Epiglottitis
- The clinical manifestations of epiglottitis are usually sudden and severe. They include:
- High fever (>38°C or 100.4°F)
- Severe sore throat and dysphagia (difficulty swallowing)
- Drooling and inability to handle secretions
- Muffled or hoarse voice and stridor (high-pitched sound on inspiration)
- Respiratory distress and tachypnea (rapid breathing)
- Tachycardia (rapid heart rate) and hypotension (low blood pressure)
- Anxiety, agitation, and restlessness
- Cyanosis (bluish discoloration of the skin and mucous membranes) and pallor (pale appearance)
- Tripod position and use of accessory muscles to breathe
- The clinical manifestations of epiglottitis can vary depending on the age of the child, the degree of airway obstruction, and the presence of complications. Some children may have a more gradual onset of symptoms or present with atypical features, such as cough, wheezing, or abdominal pain.
- The clinical manifestations of epiglottitis can also mimic other conditions that cause upper airway obstruction, such as croup, foreign body aspiration, retropharyngeal abscess, or anaphylaxis. Therefore, it is important to differentiate epiglottitis from these conditions based on the history, physical examination, and diagnostic tests.
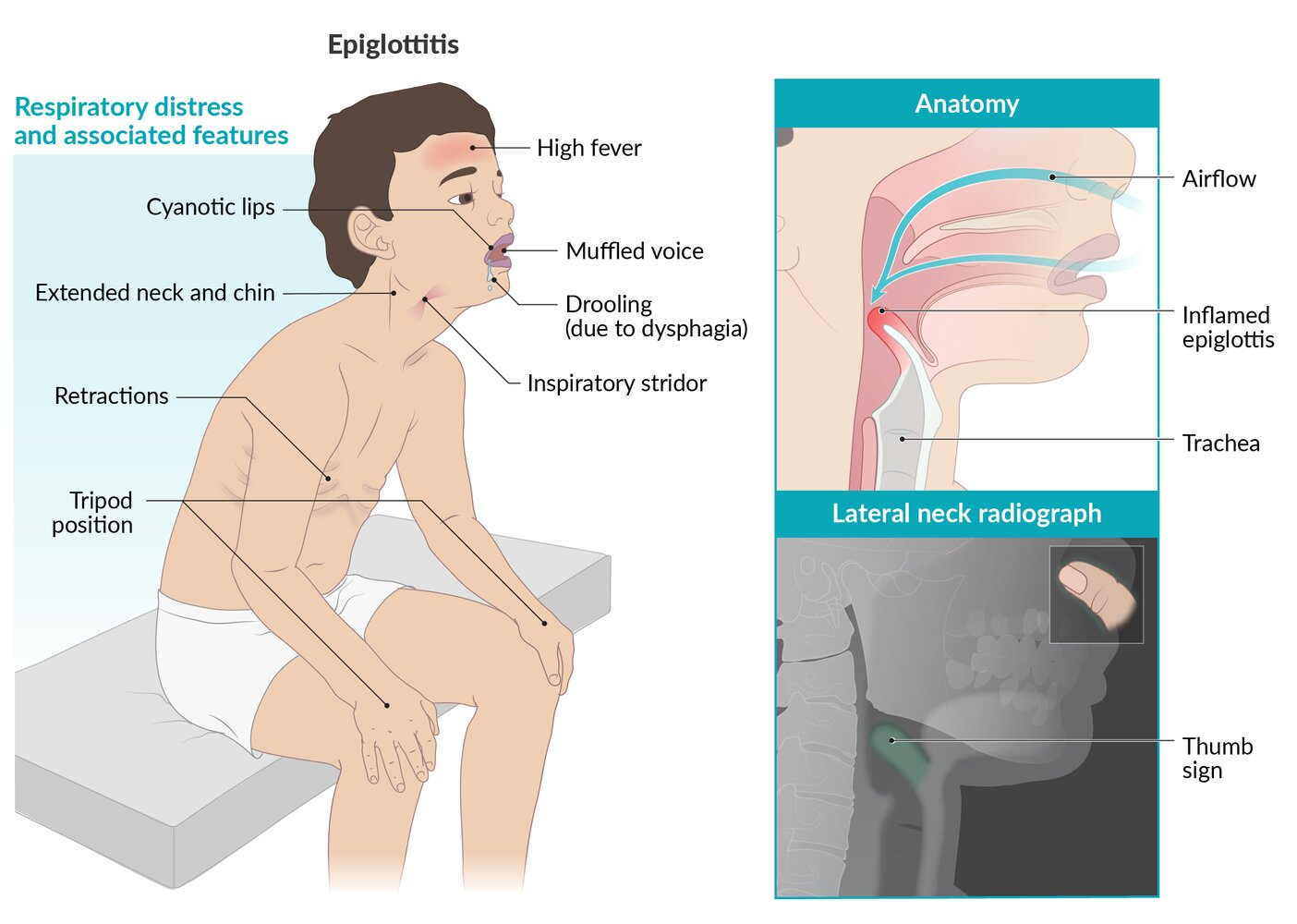
Diagnostic Evaluation of Epiglottitis
- The diagnostic evaluation of epiglottitis is based on the clinical presentation and the confirmation by imaging and laboratory tests. However, the priority is to secure the airway before performing any invasive procedures or tests that may aggravate the condition.
- The imaging test of choice for epiglottitis is a lateral neck radiograph, which can show a characteristic “thumb sign” indicating a swollen epiglottis. However, this test should only be done in a controlled setting with emergency equipment and personnel available, as it may provoke laryngospasm or complete airway obstruction.
- Other imaging tests that can be used to diagnose epiglottitis include computed tomography (CT) scan or magnetic resonance imaging (MRI) of the neck, which can provide more detailed information about the extent of the inflammation and edema. However, these tests are also risky and require sedation, which may compromise the respiratory status of the child.
- The laboratory tests that can be used to diagnose epiglottitis include blood cultures, throat cultures, or polymerase chain reaction (PCR) tests to identify the causative organism; complete blood count (CBC) to detect leukocytosis (increased white blood cells) or anemia (decreased red blood cells); arterial blood gas (ABG) analysis to assess hypoxia, hypercapnia, and acidosis; and serum electrolytes to monitor hydration status. However, these tests are also invasive and may delay the treatment of epiglottitis.
Nursing Assessment of Epiglottitis
- The nursing assessment of a child with epiglottitis involves obtaining a history, performing a physical examination, and monitoring the vital signs. However, the nurse should be careful not to disturb or upset the child, as any manipulation or stimulation may worsen the airway obstruction.
- The history should include information about the onset and duration of symptoms, exposure to infectious agents or allergens, immunization status, history of trauma or injury to the throat or neck, history of foreign body aspiration or ingestion, history of chronic diseases or immunodeficiency, and medications or treatments used.
- The physical examination should focus on the respiratory system and include inspection, auscultation, palpation, and percussion. The nurse should look for signs of respiratory distress, such as tachypnea, stridor, cyanosis, pallor, tripod position, use of accessory muscles, nasal flaring, intercostal or subcostal retractions, and chest wall movement asymmetry. The nurse should also assess the level of consciousness, mental status, orientation, and behavior of the child.
- The vital signs should include temperature, pulse rate, blood pressure, respiratory rate, oxygen saturation (SpO2), and capillary refill time. The nurse should monitor for changes in these parameters that may indicate worsening of the condition or impending respiratory failure.
Nursing Interventions for Epiglottitis
- The nursing interventions for a child with epiglottitis are aimed at maintaining a patent airway, providing supportive care, and educating the child and family. They include:
- Securing the airway by assisting with intubation or tracheostomy if indicated. The nurse should have emergency equipment ready at all times and avoid any procedures that may trigger laryngeal spasms or obstruction.
- Administering oxygen therapy by nasal cannula, mask, or hood, depending on the child’s tolerance and oxygen requirement. The nurse should monitor the SpO2 and adjust the oxygen flow accordingly.
- - Administering antibiotics intravenously as prescribed to treat the infection and prevent complications. The nurse should monitor the blood cultures and antibiotic sensitivity results to ensure the effectiveness of the therapy
- - Administering corticosteroids intravenously as prescribed to reduce the inflammation and edema of the epiglottis and larynx. The nurse should monitor the child for signs of adrenal insufficiency or hyperglycemia as side effects of the therapy.
- - Administering analgesics and antipyretics as prescribed to relieve pain and fever. The nurse should avoid oral medications that may cause gagging or vomiting and use rectal or intravenous routes instead.
- - Providing humidified air or cool mist therapy to moisten the airway and reduce irritation. The nurse should avoid nebulized medications that may cause bronchospasm or coughing.
- - Providing hydration and nutrition by intravenous fluids or nasogastric tube feeding as prescribed. The nurse should avoid oral fluids or foods that may cause aspiration or choking.
- - Providing comfort and reassurance to the child and family by explaining the condition, treatment, and prognosis. The nurse should use a calm and gentle approach and avoid any actions that may frighten or agitate the child.
- - Educating the child and family about the prevention of epiglottitis by ensuring complete immunization against Hib and other causative agents. The nurse should also teach the child and family about the signs and symptoms of epiglottitis and when to seek medical attention.
Treatment and Management of Epiglottitis
- The treatment and management of epiglottitis are aimed at relieving the airway obstruction, eradicating the infection, preventing complications, and promoting recovery. They include:
- Airway management by intubation or tracheostomy if indicated. Intubation is preferred over tracheostomy as it is less invasive and has fewer complications. However, intubation may be difficult or impossible due to the distorted anatomy of the larynx. Therefore, tracheostomy may be necessary in some cases. The child may need to stay intubated or tracheostomized for several days until the inflammation subsides.
- Antibiotic therapy by intravenous route for 7 to 10 days, depending on the causative organism and antibiotic sensitivity. The most commonly used antibiotics are cephalosporins, such as ceftriaxone or cefotaxime, which are effective against Hib and other gram-negative bacteria. Other antibiotics that can be used include ampicillin-sulbactam, clindamycin, or vancomycin.
- Corticosteroid therapy by intravenous route for 24 to 48 hours, depending on the severity of the condition. The most commonly used corticosteroid is dexamethasone, which can reduce the inflammation and edema of the epiglottis and larynx. However, corticosteroid therapy is controversial and not universally recommended, as it may have adverse effects such as immunosuppression, hyperglycemia, or gastrointestinal bleeding.
- Supportive care by oxygen therapy, humidified air or cool mist therapy, analgesics and antipyretics, hydration and nutrition, comfort and reassurance, and education. The child may also need physiotherapy to prevent atelectasis (collapse of lung tissue) or pneumonia due to prolonged bed rest or immobility.
Conclusion
- Epiglottitis is a serious condition that can cause life-threatening airway obstruction in children. It is usually caused by Hib infection, but other bacteria or non-infectious factors can also be involved. It is characterized by sudden onset of high fever, severe sore throat, drooling, stridor, respiratory distress, and tripod position.
- Epiglottitis requires prompt diagnosis and treatment to prevent respiratory failure or death. The diagnosis is based on the clinical presentation and confirmed by imaging and laboratory tests. The treatment involves securing the airway by intubation or tracheostomy, administering antibiotics and corticosteroids intravenously, and providing supportive care.
- Epiglottitis can be prevented by immunizing children against Hib and other causative agents. Children and families should also be educated about the signs and symptoms of epiglottitis and when to seek medical attention.
Summary
- Epiglottitis is a potentially life-threatening inflammation of the epiglottis that can obstruct the airway
- It is usually caused by Hib infection in children between 2 and 8 years old
- It presents with sudden onset of high fever, severe sore throat, drooling, stridor, respiratory distress, and tripod position
- It is diagnosed by clinical presentation and confirmed by lateral neck radiograph, which shows a “thumb sign”
- It is treated by securing the airway by intubation or tracheostomy, administering antibiotics and corticosteroids intravenously, and providing supportive care
- It is prevented by immunizing children against Hib and other causative agents and educating them about the signs and symptoms of epiglottitis
Otitis media
Objectives
- To define otitis media and its types
- To describe the etiology and pathophysiology of otitis media
- To identify the clinical manifestations and complications of otitis media
- To explain the diagnostic evaluation and treatment of otitis media
- To perform a nursing assessment and interventions for otitis media
- To educate the patient and family about otitis media prevention and management
Introduction
- Otitis media is an infection of the middle ear, which is the space behind the eardrum that contains the small bones of hearing.
- Otitis media can be classified into two types: acute otitis media (AOM) and otitis media with effusion (OME).
- AOM is a rapid onset of inflammation and infection of the middle ear, usually caused by bacteria or viruses.
- OME is a collection of fluid in the middle ear without signs of infection, usually due to impaired drainage of the eustachian tube.
- Otitis media is one of the most common childhood infections and a leading cause of antibiotic use in children.
- Otitis media can cause pain, fever, hearing loss, speech delay, and complications such as mastoiditis, labyrinthitis, meningitis, and cholesteatoma.
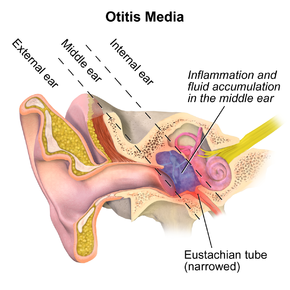
Etiology of Otitis media
- The main cause of otitis media is eustachian tube dysfunction, which prevents normal ventilation and drainage of the middle ear.
- The eustachian tube connects the middle ear to the nasopharynx and equalizes the pressure between them.
- In children, the eustachian tube is shorter, wider, and more horizontal than in adults, making it more prone to obstruction by secretions, inflammation, or swelling.
- The risk factors for otitis media include:
- Age: most common in children under 2 years old and again at 5 to 6 years old
- Season: more frequent in winter and spring
- Allergies: can cause congestion and inflammation of the eustachian tube
- Upper respiratory tract infections: can spread to the middle ear or cause eustachian tube blockage
- Day care attendance: increases exposure to infectious agents
- Bottle feeding: especially in a supine position, can cause reflux of milk into the eustachian tube
- Passive smoking: can impair mucociliary clearance and immune function
- Anatomic anomalies: such as cleft palate, Down syndrome, or craniofacial defects, can affect eustachian tube function
- Immunodeficiency: can impair host defense against pathogens
- Noncompliance with vaccinations: such as pneumococcal conjugate vaccine (PCV), Haemophilus influenzae type b (Hib) vaccine, and influenza vaccine, which can prevent some causes of otitis media
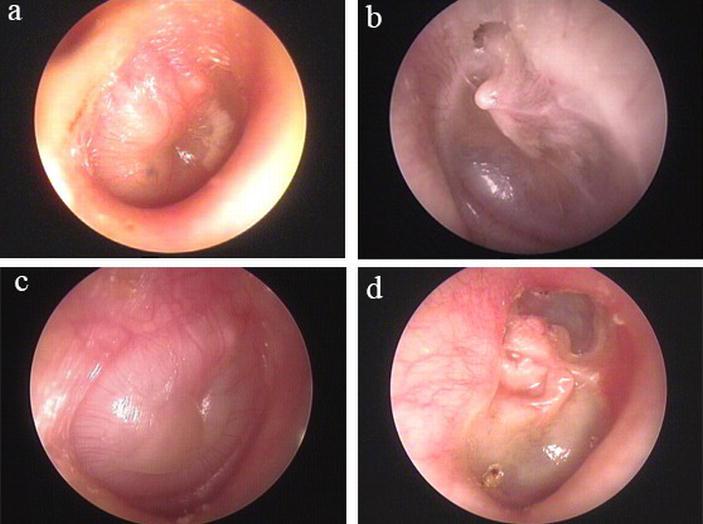
Pathophysiology of Otitis media
- The pathophysiology of otitis media involves three main steps:
- Eustachian tube obstruction: due to any of the risk factors mentioned above, the eustachian tube becomes blocked or narrowed, preventing air from entering or leaving the middle ear. This creates a negative pressure in the middle ear, which pulls fluid from the surrounding tissues into the middle ear space. This fluid is called effusion and it fills up the normally air-filled cavity.
- Bacterial or viral invasion: the effusion provides a favorable environment for bacterial or viral growth. The most common pathogens that cause AOM are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. These organisms can reach the middle ear from the nasopharynx through the eustachian tube or from the bloodstream. They multiply rapidly and trigger an inflammatory response in the middle ear.
- Inflammation and infection: as a result of the microbial invasion and immune reaction, the middle ear becomes inflamed and infected. The eardrum becomes red, swollen, and bulging. The fluid in the middle ear becomes purulent (pus-filled) and exerts pressure on the eardrum and the ossicles (the small bones of hearing). This causes pain, fever, hearing loss, and impaired balance. If left untreated, AOM can lead to perforation of the eardrum, which allows drainage of pus from the ear canal. This may relieve pain but increase hearing loss.
Clinical Manifestations Otitis media
- The clinical manifestations of otitis media vary depending on the type, severity, age of the child, and presence of complications.
- The common signs and symptoms of AOM include:
- Ear pain: may be severe, throbbing, or pulsating; may worsen when lying down; may radiate to other parts of the head or neck; may be accompanied by tugging or rubbing of the ear
- Fever: may range from low-grade to high-grade; may indicate bacterial infection or inflammation
- Irritability: may be due to pain, discomfort, or fever; may manifest as crying, fussiness, or inconsolability
- Loss of appetite: may be due to pain, nausea, or vomiting; may lead to dehydration or weight loss
- Hearing loss: may be mild to moderate; may affect speech and language development; may cause difficulty in locating sounds or following directions
- Balance problems: may be due to disruption of the vestibular system in the inner ear; may cause dizziness, vertigo, or nystagmus (involuntary eye movements)
- Otorrhea: drainage of fluid or pus from the ear canal; may indicate perforation of the eardrum; may have a foul odor or color
- The common signs and symptoms of OME include:
- Feeling of fullness or pressure in the ear: may be uncomfortable but not painful; may affect hearing and balance
- Hearing loss: may be mild to moderate; may affect speech and language development; may cause difficulty in locating sounds or following directions
- Tinnitus: ringing or buzzing sound in the ear; may be intermittent or constant; may worsen with noise exposure
- Recurrent infections: fluid in the middle ear may become infected by bacteria or viruses, leading to AOM
Diagnostic Evaluation Otitis media
- The diagnostic evaluation of otitis media is based on history, physical examination, and otoscopy.
- History: the nurse should obtain information about the onset, duration, frequency, and severity of symptoms; the presence of fever, ear pain, drainage, hearing loss, balance problems, or speech delay; the history of previous episodes of otitis media, upper respiratory tract infections, allergies, immunizations, or exposure to smoke or other irritants; the feeding method and position of infants; and the use of any medications or treatments.
- Physical examination: the nurse should assess the general appearance and behavior of the child; the vital signs, especially temperature and respiratory rate; the lymph nodes of the head and neck for enlargement or tenderness; and the oral cavity for signs of infection or inflammation.
- Otoscopy: the nurse should use a pneumatic otoscope to visualize the tympanic membrane and assess its color, contour, mobility, and transparency. The nurse should gently pull the pinna down and back for children under 3 years old and up and back for children over 3 years old. The normal tympanic membrane is pearly gray, concave, mobile, and translucent. The abnormal findings that indicate otitis media are:
|
Finding |
Description |
Type of Otitis Media |
|
Redness |
Increased blood flow due to inflammation |
AOM |
|
Bulging |
Increased pressure due to fluid accumulation |
AOM |
|
Purulence |
Presence of pus due to infection |
AOM |
|
Perforation |
Rupture of the eardrum due to increased pressure |
AOM |
|
Drainage |
Leakage of fluid or pus from the ear canal due to perforation |
AOM |
|
Orange discoloration |
Presence of serous fluid due to chronic effusion |
OME |
|
Decreased mobility |
Impaired movement due to fluid accumulation |
OME |
Nursing Assessment Otitis media
- The nursing assessment of otitis media is based on the following aspects:
- Pain: the nurse should assess the location, intensity, quality, frequency, and duration of ear pain using a developmentally appropriate pain scale (such as FLACC for infants and toddlers, Wong-Baker FACES for preschoolers and school-age children, and numeric rating scale for adolescents). The nurse should also ask about any factors that aggravate or relieve pain (such as position, pressure, heat, cold, analgesics, or distraction).
- Fever: the nurse should measure the temperature using a reliable method (such as tympanic, oral, axillary, or rectal) and compare it with the normal range for age (36.5°C to 37.5°C for infants and children). The nurse should also ask about any associated symptoms (such as chills, sweating, malaise, or dehydration) or interventions (such as antipyretics, fluids, or cooling measures).
- Hearing loss: the nurse should assess the degree and impact of hearing loss using a screening tool (such as whisper test or audiometry) and observation (such as response to sounds, speech clarity and volume, lip reading, or social interaction). The nurse should also ask about any history of hearing problems or delays in speech and language development.
- Balance problems: the nurse should assess the presence and severity of balance problems using a test (such as Romberg test or tandem watchful waiting, myringotomy, or tympanostomy tube insertion.
Summary
- Otitis media is an infection of the middle ear that can cause pain, fever, hearing loss, balance problems, and complications.
- Otitis media is caused by eustachian tube dysfunction, which leads to fluid accumulation and bacterial or viral invasion in the middle ear.
- Otitis media can be classified into two types: acute otitis media (AOM) and otitis media with effusion (OME).
- Otitis media is diagnosed by history, physical examination, and otoscopy.
- Otitis media is treated and managed by symptomatic relief, antibiotics or antivirals, watchful waiting, myringotomy, or tympanostomy tube insertion.
- Otitis media can be prevented by avoiding risk factors and vaccinating against common pathogens.
Gastroenteritis in Children:
Pathophysiology of Gastroenteritis in Children:
- Gastroenteritis occurs when the gastrointestinal tract becomes infected with a pathogen, leading to inflammation and damage to the intestinal lining.
- The infection is usually acquired through ingestion of contaminated food or water.
- Once the pathogen enters the body, it binds to the intestinal epithelial cells and replicates, causing cell damage and disruption of normal gut function.
- This leads to increased fluid secretion and decreased absorption, resulting in diarrhea and electrolyte imbalances.
Clinical Manifestations of Gastroenteritis in Children:
- The clinical presentation of gastroenteritis in children can vary depending on the causative agent and the severity of the infection.
- Common symptoms include diarrhea, vomiting, abdominal pain, fever, and dehydration.
- Diarrhea may be watery or contain blood and mucus.
- Vomiting can be frequent and may lead to fluid and electrolyte imbalances.
- Abdominal pain is often crampy and may be accompanied by bloating and discomfort.
- Dehydration can manifest as decreased urine output, dry mucous membranes, sunken eyes, and lethargy.
Diagnostic Evaluation of Gastroenteritis in Children:
- The diagnosis of gastroenteritis in children is primarily based on clinical presentation and history.
- Stool culture and sensitivity testing can be performed to identify the causative organism in bacterial infections.
- Viral testing, such as enzyme immunoassay or polymerase chain reaction, can be used to detect viral pathogens.
- Blood tests may be done to assess electrolyte levels, kidney function, and markers of inflammation.
- Imaging studies, such as abdominal ultrasound, may be indicated in severe cases to evaluate for complications.
Nursing Assessment Gastroenteritis in Children:
- Assess the child's vital signs, including temperature, pulse, respiratory rate, and blood pressure.
- Monitor the child's hydration status by assessing skin turgor, mucous membranes, and urine output.
- Document the frequency, consistency, and characteristics of the child's stools.
- Assess the child's abdominal pain level using a pain scale appropriate for their age.
- Evaluate the child's overall appearance, behavior, and level of distress.
- Perform a thorough physical examination, paying attention to the gastrointestinal system.
Nursing Interventions Gastroenteritis in Children:
- Provide oral rehydration therapy to replace fluid and electrolyte losses.
- Administer antiemetic medications as prescribed to alleviate vomiting.
- Offer small, frequent meals and encourage the child to resume their regular diet gradually.
- Monitor the child's intake and output, ensuring adequate hydration is maintained.
- Implement infection control measures to prevent the spread of the infection.
- Educate parents and caregivers on proper hand hygiene and sanitation practices.
Treatment and Management Gastroenteritis in Children:
- Supportive care, including rest and adequate fluid intake, is the primary treatment for viral gastroenteritis.
- Antibiotics may be prescribed for bacterial gastroenteritis based on the causative organism.
- Probiotics can be used to restore the gut flora and promote faster recovery.
- In severe cases, hospitalization may be required for intravenous fluid administration.
- Monitor the child's response to treatment and adjust the management plan accordingly.
Conclusion:
Gastroenteritis in children is a common condition that requires comprehensive nursing care. Through proper assessment, interventions, and management, nurses can help alleviate symptoms, prevent complications, and promote the child's recovery. It is essential to prioritize fluid and electrolyte balance, provide appropriate nutrition, and educate parents and caregivers on infection control measures.
Summary:
- Gastroenteritis in children requires thorough nursing assessment, including vital signs, hydration status, stool characteristics, abdominal pain, and overall appearance.
- Nursing interventions involve providing oral rehydration therapy, administering antiemetics, offering small, frequent meals, monitoring intake and output, and implementing infection control measures.
- Treatment options include supportive care, antibiotics for bacterial gastroenteritis, probiotics, and, in severe cases, hospitalization for intravenous fluid administration.
- Nurses should prioritize fluid and electrolyte balance, nutrition, and education on infection control practices.
- Regular monitoring and adjustment of the management plan are necessary for optimal outcomes.
Dehydration in Children
Objectives:
- Define dehydration and its significance in pediatric patients.
- Understand the etiology of dehydration in children.
- Explain the pathophysiology of dehydration in children.
- Identify the clinical manifestations of dehydration in children.
- Discuss the diagnostic evaluation methods for dehydration in children.
- Provide guidelines for managing dehydration in children.
Understand the nursing assessment of dehydration in children.
Identify appropriate nursing interventions for managing dehydration in children.
Describe the treatment and management strategies for dehydration in children.
Introduction
- Dehydration is a common condition in pediatric patients, characterized by an inadequate fluid balance. It occurs when the body loses more fluid than it takes in, leading to an imbalance that disrupts normal bodily functions. Dehydration in children can be a serious medical concern and requires prompt intervention to prevent complications.
I. Etiology of Dehydration in Children: Dehydration in children can be caused by various factors, including:
- Gastrointestinal illnesses, such as diarrhea and vomiting.
- Insufficient fluid intake due to poor feeding or decreased thirst perception.
- Excessive sweating during physical activity or in hot weather.
- Fever, which increases the body's fluid requirements.
- Certain medical conditions, such as diabetes or kidney disease.
II. Pathophysiology of Dehydration in Children: Dehydration in children occurs when there is a disruption in the balance between fluid intake and loss. This can lead to imbalances in electrolytes, such as sodium and potassium, which are essential for normal body functioning. The severity of dehydration depends on the extent of fluid loss and the child's age and overall health status.
III. Clinical Manifestations of Dehydration in Children: The clinical manifestations of dehydration in children can vary depending on the degree of fluid loss. Common signs and symptoms include:
- Thirst and dry mouth.
- Decreased urine output and dark-colored urine.
- Dry skin and mucous membranes.
- Sunken eyes and fontanelle in infants.
- Lethargy and irritability.
- Poor skin turgor.
- Rapid heart rate and low blood pressure in severe cases.
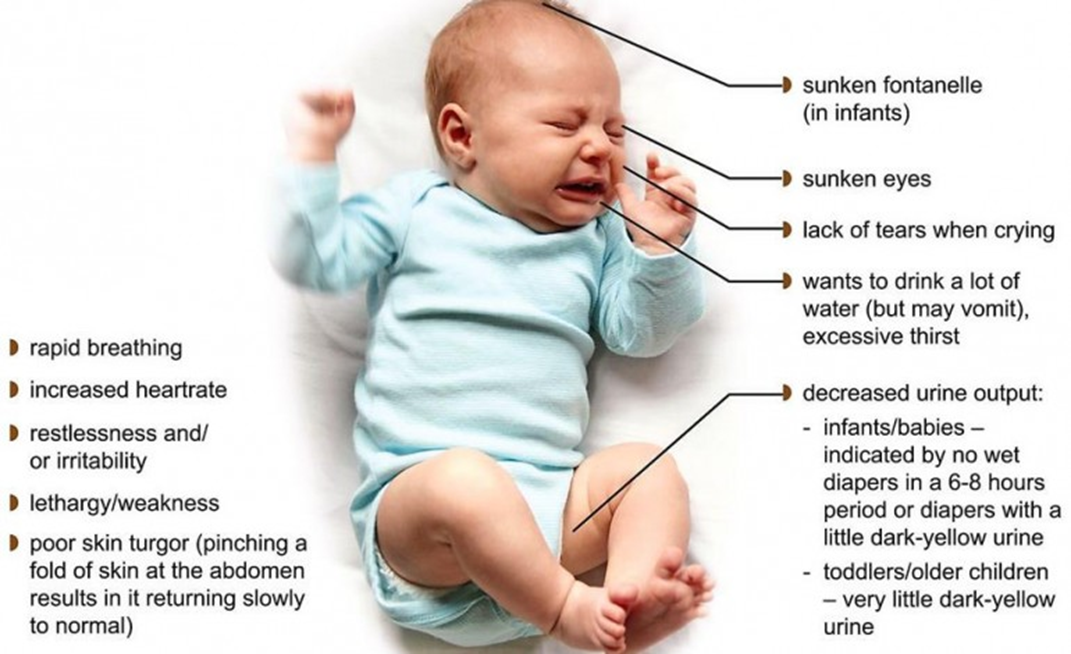
IV. Diagnostic Evaluation of Dehydration in Children: To diagnose dehydration in children, healthcare providers may assess the following parameters:
- Vital signs, including heart rate, blood pressure, and temperature.
- Physical examination findings, such as skin turgor and mucous membrane moisture.
- Laboratory tests, including complete blood count (CBC), electrolyte levels, and urine specific gravity.
- Assessing the child's history, including recent fluid intake, urine output, and presence of symptoms.
Nursing Assessment Dehydration in children:
- Physical examination: Assess the child's general appearance, skin turgor, mucous membranes, fontanelle (in infants), and capillary refill time.
- Vital signs: Monitor the child's heart rate, blood pressure, respiratory rate, and temperature.
- Fluid intake and output: Document the child's oral intake, urine output, and any signs of decreased urine output or increased fluid losses (e.g., vomiting, diarrhea).
- Weight: Monitor the child's weight to assess for any significant changes.
- Laboratory tests: Order and interpret relevant laboratory tests, such as complete blood count, electrolyte panel, and blood urea nitrogen (BUN) levels.
- Assess for signs of electrolyte imbalances: Check for symptoms like lethargy, muscle weakness, irritability, and abnormal heart rhythms.
Nursing Interventions Dehydration in children:
- Rehydration therapy: Administer oral rehydration solution (ORS) or intravenous fluids as prescribed by the healthcare provider.
- Monitor fluid balance: Measure and record the child's intake and output accurately.
- Provide comfort measures: Offer small, frequent sips of fluids, maintain a comfortable temperature, and provide adequate rest.
- Monitor vital signs: Regularly assess the child's heart rate, blood pressure, respiratory rate, and temperature.
- Educate the child and caregivers: Teach them about the importance of fluid intake, signs of dehydration, and how to prevent it.
Treatment and Management Dehydration in children:
- Fluid replacement: Ensure the child receives appropriate fluid replacement based on the severity of dehydration, age, and weight.
- Correct electrolyte imbalances: Administer electrolyte solutions or supplements as necessary.
- Continuously assess the child's hydration status: Monitor the child's response to treatment and adjust the plan accordingly.
- Collaborate with the healthcare team: Communicate with physicians, nutritionists, and other healthcare professionals to ensure comprehensive care.
Step-by-Step Calculation of Fluid Replacement in a Dehydrated Child
Dehydration in children can be a serious condition that requires prompt intervention. The calculation of fluid replacement in a dehydrated child involves several steps. Here is a step-by-step guide on how a nurse should calculate fluid replacement:
Step 1: Assess the Degree of Dehydration The nurse should assess the child's degree of dehydration based on clinical signs and symptoms, such as dry mucous membranes, decreased urine output, sunken fontanelle (in infants), and decreased skin turgor. The degree of dehydration is typically classified as mild (3-5% loss of body weight), moderate (6-9% loss of body weight), or severe (≥10% loss of body weight) .
Step 2: Calculate the Fluid Deficit To calculate the fluid deficit, the nurse needs to estimate the percentage of body weight lost due to dehydration. The following formulas can be used:
- Mild dehydration: Fluid deficit (in mL) = body weight (in kg) x 0.03
- Moderate dehydration: Fluid deficit (in mL) = body weight (in kg) x 0.06
- Severe dehydration: Fluid deficit (in mL) = body weight (in kg) x 0.1
For example, if a child weighs 10 kg and has moderate dehydration, the fluid deficit would be 10 kg x 0.06 = 600 mL .
Step 3: Calculate Maintenance Fluids Maintenance fluids are the amount of fluids required to meet the daily needs of the child. The nurse can use the Holliday-Segar method to calculate maintenance fluids:
- For the first 10 kg of body weight: 100 mL/kg/day
- For the next 10 kg of body weight: 50 mL/kg/day
- For each additional kg of body weight: 20 mL/kg/day
For example, if a child weighs 15 kg, the maintenance fluids would be calculated as follows:
- For the first 10 kg: 10 kg x 100 mL/kg/day = 1000 mL/day
- For the next 5 kg: 5 kg x 50 mL/kg/day = 250 mL/day
- Total maintenance fluids = 1000 mL/day + 250 mL/day = 1250 mL/day .
Step 4: Determine the Total Fluid Requirement To determine the total fluid requirement, the nurse should add the fluid deficit (step 2) to the maintenance fluids (step 3). Using the previous example, if the child has a fluid deficit of 600 mL and a maintenance fluid requirement of 1250 mL/day, the total fluid requirement would be 600 mL + 1250 mL = 1850 mL/day .
Step 5: Divide the Total Fluid Requirement The nurse should divide the total fluid requirement over a 24-hour period to determine the hourly rate. In this example, the total fluid requirement is 1850 mL/day, so the hourly rate would be 1850 mL/24 hours = approximately 77 mL/hour .
Step 6: Monitor and Adjust The nurse should closely monitor the child's fluid intake and output, as well as clinical signs of hydration status. Adjustments may be necessary based on the child's response to fluid replacement therapy.
It's important to note that these calculations are general guidelines, and individual patient factors should be considered. The nurse should consult with the healthcare team and follow institutional protocols for fluid replacement therapy in dehydrated children.
Intravenous fluids (IV) Fluids and their uses
Here is a table that summarizes the fluid, constituents, indications, and contraindications for the IV fluids (Intravenous fluids).
|
Fluid |
Constituents |
Indications |
Contraindications |
|
Normal saline (0.9% NaCl) |
Sodium 154 mEq/L. Chloride 154 mEq/L |
Hyponatremia, shock, maintenance fluids, dehydration |
Hypernatremia. fluid overload. heart failure Edema, heart disease, cardiac decompensation, primary or secondary aldosteronism |
|
Half normal saline (0.45% NaCl) |
Sodium 77 mEq/L. Chloride 77 mEq/L |
Fluid loss, mild hyponatremia, gastric fluid loss from vomiting or suction |
Hypovolemia. hyponatremia. increased intracranial pressure Liver disease, trauma, burns |
|
Lactated Ringer’s |
Sodium 130 mEq/L. Chloride 109 mEq/L. Potassium 4 mEq/L. Calcium 3 mEq/L. Lactate 28 mEq/L |
Fluid resuscitation, burns, lower GI fluid loss, acute blood loss, hypovolemia due to third-space fluid shifts |
Hyperkalemia. lactic acidosis. liver disease Renal failure, lactic acidosis, alkalosis |
|
D5W (5% dextrose in water) |
Dextrose 50 g/L. Water 950 mL |
To provide free water for cellular hydration. to supply calories (170 kcal/L). to dilute medications for IV administration Fluid loss and dehydration, hypernatremia |
Hyperglycemia. fluid overload. cerebral edema |
|
D10W (10% dextrose in water) |
Dextrose 100 g/L. Water 900 mL |
Water replacement, conditions where some nutrition with glucose is required to supply calories (340 kcal/L). to treat hypoglycemia |
Hyperglycemia. fluid overload. cerebral edema |
|
D20W (20% dextrose in water) |
Dextrose 200 g/L. Water 800 mL |
. to supply calories (680 kcal/L). to treat hypoglycemia |
Hyperglycemia. fluid overload. cerebral edema |
|
D50W (50% dextrose in water) |
Dextrose 500 g/L. Water 500 mL |
To provide free water for cellular hydration. to supply calories (1700 kcal/L). to treat severe hypoglycemia |
Hyperglycemia. fluid overload. cerebral edema |
|
Hypertonic sodium chloride solutions (3%. 5%. or 7.5% NaCl) |
Sodium 513-1286 mEq/L. Chloride 513-1286 mEq/L |
To treat severe hyponatremia and cerebral edema |
Hypernatremia. fluid overload. heart failure |
|
Albumin (5% or 25%) |
Human serum albumin derived from plasma donors |
To expand plasma volume and increase oncotic pressure in hypovolemic shock. burns. hypoalbuminemia |
Hypersensitivity to albumin or human plasma proteins |
|
Dextrans (Dextran-40 or Dextran-70) |
Glucose polymers of varying molecular weights suspended in isotonic or hypertonic saline or dextrose solutions |
To expand plasma volume and increase blood viscosity in hypovolemic shock and hemorrhage Plasma volume expansion, shock, thromboembolism prophylaxis |
Hypersensitivity to dextrans or corn products |
|
Gelatin (Gelofusine or Haemaccel) |
Degraded gelatin derived from bovine collagen suspended in isotonic saline or dextrose solutions |
To expand plasma volume and increase oncotic pressure in hypovolemic shock and hemorrhage |
Hypersensitivity to gelatin or bovine products |
|
Plasma protein fraction (Plasmanate or Plasmasteril) |
Human plasma proteins derived from plasma donors with sodium caprylate as a stabilizer |
To expand plasma volume and increase oncotic pressure in hypovolemic shock and burns |
Hypersensitivity to human plasma proteins or sodium caprylate |
Conclusion:
- Dehydration in children requires prompt assessment, intervention, and management to prevent complications and promote optimal health. Nurses play a critical role in recognizing and addressing dehydration in children, providing appropriate nursing care, and educating both the child and caregivers on preventive measures.
Summary:
- Understand the nursing assessment of dehydration in children.
- Identify appropriate nursing interventions for managing dehydration in children.
- Describe the treatment and management strategies for dehydration in children.
- Recognize the information commonly tested in ATI/HESI nursing proctored MCQ exams related to dehydration in children.
- Provide specific examples of nursing assessments, interventions, treatment, and management for dehydration in children.
- Include normal ranges for relevant parameters where applicable.
Allergies and Asthma in Children
Objectives:
- Understand the etiology of allergies and asthma in children.
- Explain the pathophysiology of allergies and asthma in children.
- Identify the clinical manifestations of allergies and asthma in children.
- Discuss the diagnostic evaluation methods for allergies and asthma in children.
- Provide normal ranges for relevant parameters.
- Understand the nursing assessment of allergies and asthma in children.
- Identify nursing interventions for managing allergies and asthma in children.
- Discuss the treatment and management strategies for allergies and asthma in children.
Introduction
- Allergies and asthma are common respiratory conditions that can affect children. They are often interrelated, with allergies being a common trigger for asthma symptoms. This comprehensive nursing note will provide detailed information on the etiology, pathophysiology, clinical manifestations, and diagnostic evaluation of allergies and asthma in children.
Etiology of Allergies and Asthma in Children:
- Allergies:
- Allergies in children are primarily caused by hypersensitivity reactions to certain substances, known as allergens.
- Common allergens include pollen, dust mites, pet dander, certain foods, and insect venom.
- Genetic factors, environmental exposures, and immune system dysregulation can contribute to the development of allergies in children.
- Asthma:
- Asthma in children is a chronic inflammatory disorder of the airways, characterized by recurrent episodes of wheezing, coughing, and shortness of breath.
- Both genetic and environmental factors play a role in the development of asthma.
- Exposure to allergens, respiratory infections, irritants (such as tobacco smoke), and exercise can trigger asthma symptoms in children.
Pathophysiology of Allergies and Asthma in Children:
- Allergies:
- Allergic reactions occur when the immune system overreacts to allergens, leading to the release of histamine and other inflammatory mediators.
- This immune response causes symptoms such as itching, hives, nasal congestion, and wheezing.
- IgE antibodies play a crucial role in the allergic response by binding to allergens and triggering the release of histamine.
Asthma:
- In asthma, chronic inflammation of the airways leads to increased airway sensitivity and hyperresponsiveness.
- Exposure to triggers, such as allergens or irritants, causes the airway muscles to contract (bronchoconstriction) and the airways to become inflamed and narrowed.
- This results in symptoms such as wheezing, coughing, and difficulty breathing.
Clinical Manifestations of Allergies and Asthma in Children:
- Allergies:
- Allergic rhinitis: Symptoms include nasal congestion, sneezing, itchy eyes, and runny nose.
- Atopic dermatitis: Manifestations include dry, itchy skin, redness, and rash.
- Allergic asthma: Symptoms include wheezing, coughing, shortness of breath, and chest tightness.
- Asthma:
- Wheezing: High-pitched whistling sound during expiration.
- Coughing: Persistent or recurrent cough, particularly at night or during physical activity.
- Shortness of breath: Difficulty breathing, with a feeling of tightness in the chest.
- Chest tightness: Sensation of pressure or squeezing in the chest.
Diagnostic Evaluation of Allergies and Asthma in Children:
- Allergies:
- Skin prick test: A small amount of allergen is placed on the skin, and the reaction is observed.
- Blood tests: Measure specific IgE antibodies to identify allergens.
- Elimination diet: Removing suspected allergens from the diet and monitoring symptom improvement.
- Asthma:
- Spirometry: Measures lung function, including forced expiratory volume in one second (FEV1) and forced vital capacity (FVC).
- Peak flow meter: Measures the maximum airflow during forced expiration and helps monitor asthma control.
- Allergy testing: Identifies specific allergens that may be triggering asthma symptoms.
Nursing Assessment of Allergies and Asthma in Children:
- Assessment of Allergies:
- Obtain a detailed medical history, including information about allergies, family history, and exposure to potential allergens.
- Assess for common symptoms of allergies, such as nasal congestion, sneezing, itching, and skin manifestations.
- Perform a physical examination, focusing on the respiratory system, skin, and mucous membranes.
- Conduct allergy testing, such as skin prick tests or blood tests, to identify specific allergens.
- Assessment of Asthma:
- Gather information about the child's medical history, including previous asthma episodes, triggers, and response to medications.
- Assess respiratory symptoms, including wheezing, coughing, shortness of breath, and chest tightness.
- Monitor lung function using spirometry or peak flow meter measurements.
- Evaluate the child's response to bronchodilators and other asthma medications.
Nursing Interventions for Allergies and Asthma in Children:
- Interventions for Allergies:
- Educate the child and family about allergen avoidance strategies, such as keeping the bedroom free of dust mites or avoiding specific foods.
- Administer prescribed antihistamines, nasal corticosteroids, or other allergy medications as ordered.
- Teach the child and family how to use an epinephrine auto-injector in case of severe allergic reactions.
- Provide emotional support and counseling to help the child cope with the impact of allergies on daily life.
- Interventions for Asthma:
- Teach the child and family about asthma triggers and how to avoid them, such as tobacco smoke, pet dander, or exercise-induced asthma triggers.
- Demonstrate and supervise The correct use of inhalers, spacers, and nebulizers.
- Develop an asthma action plan in collaboration with the healthcare provider, including steps to take during asthma exacerbations.
- Encourage regular follow-up visits to monitor asthma control and adjust treatment as needed.
Treatment and Management of Allergies and Asthma in Children:
- Treatment of Allergies:
- Avoidance of allergens is the primary approach in managing allergies.
- Medications such as antihistamines, nasal corticosteroids, and leukotriene inhibitors may be prescribed to relieve symptoms.
- Immunotherapy (allergy shots) may be recommended for children with severe allergies.
- Management of Asthma:
- Long-term control medications, such as inhaled corticosteroids, are prescribed to reduce airway inflammation and prevent asthma symptoms.
- Quick-relief medications, such as short-acting beta-agonists, are used to relieve acute symptoms during asthma attacks.
- Environmental modifications, such as removing allergens and improving indoor air quality, can help manage asthma symptoms.
- Regular monitoring of lung function and adherence to the asthma action plan are essential for effective management.
Conclusion
- In conclusion, nursing assessment plays a crucial role in identifying allergies and asthma in children. By conducting a comprehensive assessment, nurses can develop appropriate interventions and provide effective treatment and management strategies. Through education, support, and collaboration with healthcare providers, nurses can help children with allergies and asthma lead healthier lives.
Summary:
- Nursing assessment involves obtaining a detailed medical history, performing physical examinations, and conducting allergy and lung function tests.
- Nursing interventions include educating the child and family, administering medications, and providing emotional support.
- Treatment and management strategies include allergen avoidance, medication administration, and the development of asthma action plans.
- Regular monitoring and adherence to treatment plans are essential for effective management.
Diabetes Mellitus in Children
Objectives:
- Understand the etiology of diabetes mellitus in children.
- Explain the pathophysiology of diabetes mellitus in children.
- Identify the clinical manifestations of diabetes mellitus in children.
- Discuss the diagnostic evaluation of diabetes mellitus in children.
- Provide examples of commonly tested information in ATI/HESI nursing proctored MCQ exams in the topics above.
- Provide normal ranges for relevant parameters.
Introduction
- Diabetes mellitus is a chronic metabolic disorder characterized by hyperglycemia resulting from a defect in insulin secretion, insulin action, or both. In children, diabetes mellitus can have significant implications for growth, development, and overall well-being.
Etiology of Diabetes Mellitus in Children:
- Genetic factors: Children with a family history of diabetes have an increased risk of developing the condition.
- Autoimmune destruction of beta cells: In type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
- Environmental factors: Certain viral infections and dietary factors may trigger the development of diabetes in susceptible individuals.
Pathophysiology of Diabetes Mellitus in Children:
- Insulin deficiency: In type 1 diabetes, the destruction of beta cells leads to an absolute insulin deficiency.
- Insulin resistance: In type 2 diabetes, there is a combination of insulin resistance and impaired insulin secretion.
- Hyperglycemia: Insufficient insulin results in elevated blood glucose levels, leading to the characteristic symptoms of diabetes.
Clinical Manifestations of Diabetes Mellitus in Children:
- Polyuria: Increased urine production due to the osmotic diuretic effect of glucose.
- Polydipsia: Excessive thirst caused by dehydration secondary to polyuria.
- Polyphagia: Increased hunger as a result of the body's inability to utilize glucose properly.
- Weight loss: Despite increased appetite, children with diabetes may experience weight loss due to the breakdown of fats and proteins for energy.
- Fatigue: Reduced energy levels due to the body's inability to use glucose effectively.
Diagnostic Evaluation of Diabetes Mellitus in Children:
- Fasting plasma glucose: A fasting blood glucose level ≥126 mg/dL on two separate occasions indicates diabetes.
- Oral glucose tolerance test: A glucose level ≥200 mg/dL two hours after a glucose load confirms the diagnosis.
- Glycated hemoglobin (HbA1c): An HbA1c level ≥6.5% is indicative of diabetes.
- Urine analysis: Presence of glucose and ketones in the urine suggests uncontrolled diabetes.
Nursing Assessment Diabetes Mellitus in Children:
- Health history: Obtain a detailed history, including family history of diabetes, symptoms, and previous treatment.
- Physical examination: Assess for signs of hyperglycemia, such as polyuria, polydipsia, and weight loss.
- Blood glucose monitoring: Regularly monitor blood glucose levels to assess glycemic control.
- Urine analysis: Check for the presence of glucose and ketones in the urine.
- Growth and development assessment: Monitor growth patterns and assess for any delays or abnormalities.
- Psychosocial assessment: Evaluate the child's emotional well-being and coping mechanisms.
Nursing Interventions Diabetes Mellitus in Children:
- Education: Provide comprehensive education to the child and family about diabetes management, including blood glucose monitoring, insulin administration, and dietary modifications.
- Nutritional support: Collaborate with a dietitian to develop an individualized meal plan that promotes glycemic control and meets the child's nutritional needs.
- Insulin administration: Teach the child and family how to administer insulin injections or use insulin pumps accurately.
- Monitoring and management of complications: Regularly assess for complications such as hypoglycemia, hyperglycemia, and diabetic ketoacidosis (DKA) and intervene promptly.
- Psychosocial support: Offer emotional support and refer the child and family to appropriate resources, such as support groups or counseling services.
- Collaboration with healthcare team: Collaborate with healthcare providers, including endocrinologists, to ensure comprehensive and coordinated care.
Treatment and Management Diabetes Mellitus in Children:
- Insulin therapy: Insulin is the mainstay of treatment for children with diabetes mellitus. Different types of insulin may be prescribed, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin.
- Blood glucose monitoring: Regular monitoring of blood glucose levels helps guide insulin dosing and assess glycemic control.
- Dietary management: A balanced diet with appropriate carbohydrate counting and portion control is essential for glycemic control.
- Physical activity: Encourage regular physical activity as part of a healthy lifestyle and to improve insulin sensitivity.
- Complication prevention: Implement strategies to prevent acute complications such as hypoglycemia and DKA, as well as long-term complications like retinopathy and nephropathy.
- Regular follow-up: Schedule regular follow-up visits to monitor glycemic control, adjust treatment plans, and provide ongoing education and support.
Cystic Fibrosis in Children: Comprehensive Nursing Notes
Objectives:
- Understand the etiology of cystic fibrosis in children.
- Explain the pathophysiology of cystic fibrosis in children.
- Identify the clinical manifestations of cystic fibrosis in children.
- Describe the diagnostic evaluation methods for cystic fibrosis in children.
- Recognize the information commonly tested in ATI/HESI nursing proctored MCQ exams related to cystic fibrosis in children.
Introduction
- Cystic fibrosis (CF) is a genetic disorder that primarily affects the respiratory and digestive systems. It is characterized by the production of thick, sticky mucus that can obstruct the airways and impair the function of various organs. CF is caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, resulting in abnormal chloride transportation across cell membranes.
Introduction
- CF is an autosomal recessive genetic disorder.
- It occurs when a child inherits two copies of the defective CFTR gene, one from each parent.
- The most common mutation associated with CF is the deletion of phenylalanine at position 508 (F508del).
- Other less common mutations can also contribute to the development of CF.
Pathophysiology of Cystic Fibrosis in Children:
- The defective CFTR gene affects the production and function of the CFTR protein.
- The abnormal CFTR protein leads to impaired chloride and water transport across epithelial cells.
- This results in the production of thick, sticky mucus in various organs, particularly the lungs, pancreas, and intestines.
- The accumulation of mucus obstructs the airways, impairs digestion, and affects the function of other organs.
Clinical Manifestations of Cystic Fibrosis in Children: Respiratory System:
- Chronic cough, wheezing, and recurrent respiratory infections.
- Difficulty breathing, especially during physical activity.
- Clubbing of the fingers and toes due to chronic hypoxia.
- Nasal polyps and sinusitis.
Digestive System:
- Failure to thrive and poor weight gain.
- Steatorrhea (fatty stools) and malabsorption.
- Pancreatic insufficiency leading to malnutrition.
- Meconium ileus in newborns with CF.
Other Manifestations:
- Sweat electrolyte abnormalities, such as elevated chloride levels.
- Delayed puberty and infertility in males.
- Diabetes mellitus due to pancreatic dysfunction.
Diagnostic Evaluation of Cystic Fibrosis in Children:
- Newborn screening tests: Immunoreactive trypsinogen (IRT) and CFTR gene mutation analysis.
- Sweat chloride test: Elevated chloride levels confirm the diagnosis.
- Genetic testing: Identifies specific CFTR gene mutations.
- Pulmonary function tests: Measure lung function and assess respiratory impairment.
- Chest X-ray and CT scan: Evaluate lung structure and identify complications.
Nursing Assessment of Cystic Fibrosis in Children:
- Perform a thorough respiratory assessment, including auscultation of lung sounds, monitoring respiratory rate, and assessing for signs of respiratory distress.
- Assess the child's nutritional status, including weight, height, and body mass index (BMI).
- Monitor for signs of malabsorption, such as steatorrhea and poor weight gain.
- Evaluate the child's hydration status and monitor for electrolyte imbalances.
- Assess the child's psychological well-being and provide emotional support.
- Monitor for signs of complications, such as respiratory infections and gastrointestinal obstructions.
Nursing Interventions for Cystic Fibrosis in Children:
- Encourage and assist with airway clearance techniques, such as coughing and deep breathing exercises.
- Administer respiratory treatments as prescribed, such as chest physiotherapy and nebulized medications.
- Provide nutritional support, including a high-calorie, high-protein diet and pancreatic enzyme replacement therapy.
- Educate the child and family about infection prevention strategies, including hand hygiene and immunizations.
- Support the child's psychological well-being through therapeutic communication and counseling.
- Collaborate with the healthcare team to coordinate care and ensure comprehensive management of the child's condition.
Treatment and Management of Cystic Fibrosis in Children:
- Pharmacological interventions: Administer medications such as bronchodilators, mucolytics, and antibiotics as prescribed.
- Respiratory therapies: Implement airway clearance techniques, including chest physiotherapy, positive expiratory pressure devices, and high-frequency chest wall oscillation.
- Nutritional management: Provide a high-calorie, high-protein diet, pancreatic enzyme replacement therapy, and fat-soluble vitamin supplements.
- Exercise and physical activity: Encourage regular exercise to improve lung function and overall fitness.
- Infection prevention: Emphasize the importance of hand hygiene, immunizations, and avoiding exposure to respiratory infections.
- Psychosocial support: Offer emotional support, counseling, and resources for coping with the challenges of living with CF.
Conclusion
- Nurses play a vital role in the assessment, interventions, and management of children with cystic fibrosis. By understanding the unique needs of these patients and providing comprehensive care, nurses can contribute to improved outcomes and enhanced quality of life for children with CF.
Summary:
- Nursing assessment of children with CF involves respiratory, nutritional, and psychosocial evaluations.
- Nursing interventions include respiratory treatments, nutritional support, infection prevention, and psychological support.
- Treatment and management strategies for CF include pharmacological interventions, respiratory therapies, nutritional management, exercise, infection prevention, and psychosocial support.
Congenital Heart Defects in Children
Objectives:
- Understand the etiology of congenital heart defects in children.
- Explain the pathophysiology of congenital heart defects in children.
- Identify the clinical manifestations of congenital heart defects in children.
- Discuss the diagnostic evaluation of congenital heart defects in children.
- Recognize the commonly tested information in ATI/HESI nursing proctored MCQ exams for the above topics.
- Provide normal ranges for relevant parameters.
- Understand the importance of nursing assessment in congenital heart defects in children.
- Identify the key nursing interventions for children with congenital heart defects.
- Discuss the treatment and management approaches for children with congenital heart defects.
Introduction
- Congenital heart defects refer to structural abnormalities present at birth that affect the heart and its blood vessels. These defects can range from minor to severe, and they can significantly impact a child's health and well-being.
Etiology of Congenital Heart Defects in Children:
- Genetic factors: Certain genetic conditions, such as Down syndrome, are associated with an increased risk of congenital heart defects.
- Environmental factors: Exposure to certain medications, drugs, or infections during pregnancy can contribute to the development of congenital heart defects.
- Maternal health: Poorly controlled diabetes, obesity, and smoking during pregnancy can increase the risk of congenital heart defects.
- Chromosomal abnormalities: Changes in the structure or number of chromosomes can lead to congenital heart defects.
Pathophysiology of Congenital Heart Defects in Children:
- Abnormal heart development: During fetal development, errors in the formation of the heart can result in structural defects.
- Blood flow disturbances: Congenital heart defects can disrupt the normal flow of blood through the heart and blood vessels, leading to various complications.
- Oxygenation issues: Some defects can affect the oxygenation of the blood, resulting in inadequate oxygen supply to the body.
|
Common Childhood Congenital Heart Defects |
Symptoms |
Characteristic Heart Murmur |
Nursing Intervention |
|
Patent ductus arteriosus (PDA) |
Poor feeding, weight gain, or growth; fast breathing or breathlessness; easy tiring; sweating with exertion |
A continuous “machinery” murmur that is loudest below the left clavicle |
Administer diuretics, digoxin, and indomethacin as prescribed; monitor fluid balance and signs of heart failure; prepare for surgical ligation or transcatheter device closure if indicated |
|
Ventricular septal defect (VSD) |
May be asymptomatic or have signs of heart failure such as poor feeding, weight gain, or growth; fast breathing or breathlessness; easy tiring; sweating with exertion |
A harsh holosystolic murmur that is best heard at the left lower sternal border |
Administer diuretics, digoxin, and afterload-reducing agents as prescribed; monitor fluid balance and signs of heart failure; provide small, frequent feedings and supplemental oxygen as needed; prepare for surgical repair or transcatheter device closure if indicated |
|
Atrial septal defect (ASD) |
Difficulty breathing (dyspnea); frequent respiratory infections in children; feeling the heart beat (palpitations) in adults; shortness of breath with activity |
A systolic ejection murmur that is best heard at the left upper sternal border |
Monitor blood pressure and pulses in all extremities; administer antihypertensive medications as prescribed; provide rest and comfort measures; prepare for surgical repair or balloon angioplasty if indicated |
|
Coarctation of the aorta (COA) |
May have no symptoms or have high blood pressure in the arms, low blood pressure in the legs, headache, dizziness, fainting, nosebleeds, leg cramps, cold feet, or weak pulses |
A systolic ejection murmur that is best heard at the left upper sternal border and radiates to the back |
Monitor blood pressure and pulses in all extremities; administer antihypertensive medications as prescribed; provide rest and comfort measures; prepare for surgical repair or balloon angioplasty if indicated |
|
Tetralogy of Fallot (TOF) |
Cyanosis that worsens with crying or feeding; clubbing of fingers and toes; poor feeding, weight gain, or growth; polycythemia; hypercyanotic spells (“tet spells”) that cause sudden severe cyanosis, dyspnea, irritability, and loss of consciousness |
A harsh systolic ejection murmur that is best heard at the left upper sternal border |
Administer oxygen, morphine, propranolol, and fluids as prescribed during tet spells; monitor oxygen saturation and hematocrit levels; provide small, frequent feedings and supplemental oxygen as needed; prepare for surgical repair or palliative shunt placement if indicated |
|
Transposition of the great arteries (TGA) |
Severe cyanosis that does not improve with oxygen; poor feeding, weight gain, or growth; signs of heart failure such as tachypnea, tachycardia, hepatomegaly, and edema |
A single second heart sound (S2) and a systolic ejection murmur that is best heard at the left upper sternal border |
Administer prostaglandin E1 to maintain ductal patency; monitor oxygen saturation and blood gases; provide small, frequent feedings and supplemental oxygen as needed; prepare for balloon atrial septostomy or surgical correction if indicated |
Cyanotic and acyanotic congenital heart diseases
- Cyanotic and acyanotic congenital heart diseases are two types of heart defects that are present at birth. They affect the way blood flows through the heart and the rest of the body.
- Cyanotic congenital heart disease (CCHD) reduces the amount of oxygen delivered to the body, causing a bluish tint in the skin, lips, and nails (cyanosis). Acyanotic congenital heart disease (ACHD) does not interfere with the oxygen level in the blood, but it causes abnormal blood flow patterns in the heart or blood vessels.
- There are many kinds of CCHD and ACHD, each with different symptoms, causes, and treatments. Some of the most common ones are:
- Ventricular septal defect (VSD): A hole in the wall between the lower chambers of the heart (ventricles). It is an ACHD that causes a left-to-right shunt of blood, meaning that oxygen-rich blood from the left ventricle mixes with oxygen-poor blood from the right ventricle. This can lead to increased pressure and volume in the lungs and heart failure. VSD is the most common congenital heart defect.
- Atrial septal defect (ASD): A hole in the wall between the upper chambers of the heart (atria). It is also an ACHD that causes a left-to-right shunt of blood, similar to VSD. However, ASD usually causes less symptoms and complications than VSD because the pressure in the atria is lower than in the ventricles. ASD can increase the risk of stroke, arrhythmia, and pulmonary hypertension.
- Patent ductus arteriosus (PDA): A persistent opening between the aorta and the pulmonary artery. The ductus arteriosus is a normal fetal structure that allows blood to bypass the lungs before birth. It usually closes shortly after birth, but in some cases it remains open. This is another ACHD that causes a left-to-right shunt of blood, resulting in increased workload for the heart and lungs. PDA can cause symptoms such as poor feeding, rapid breathing, and sweating.
- Tetralogy of Fallot (TOF): A combination of four heart defects: a large VSD, a narrowing of the pulmonary valve or artery (pulmonary stenosis), an enlarged right ventricle, and a displaced aorta that overrides both ventricles. It is a CCHD that causes a right-to-left shunt of blood, meaning that oxygen-poor blood from the right ventricle flows into the aorta and the rest of the body. This can cause cyanosis, especially during episodes of crying or exertion (called “tet spells”). TOF can also cause poor growth, clubbing of fingers and toes, and heart murmur.
- Transposition of the great arteries (TGA): A reversal of the positions of the aorta and the pulmonary artery. The aorta arises from the right ventricle and carries oxygen-poor blood to the body, while the pulmonary artery arises from the left ventricle and carries oxygen-rich blood to the lungs. This is a CCHD that causes severe cyanosis and breathing difficulty soon after birth. TGA requires urgent surgery to correct the blood flow.
-
Type
Definition
Cause
Examples
Symptoms
Cyanotic
Heart defects that reduce the amount of oxygen in the blood, causing a bluish tint in the skin, lips, and nails
Abnormal blood flow from the right side of the heart to the left side, bypassing the lungs
Tetralogy of Fallot, transposition of the great arteries
Severe cyanosis, breathing difficulty, poor growth, clubbing of fingers and toes, heart murmur
Acyanotic
Heart defects that do not interfere with the oxygen level in the blood, but cause abnormal blood flow patterns in the heart or blood vessels
Abnormal blood flow from the left side of the heart to the right side, increasing the workload for the heart and lungs
Ventricular septal defect, atrial septal defect, patent ductus arteriosus
Mild or no cyanosis, fatigue, poor feeding, rapid breathing, sweating, heart murmur
Diagnostic Evaluation of Congenital Heart Defects in Children:
- Echocardiography: Ultrasound imaging of the heart to assess its structure and function.
- Electrocardiography (ECG): Recording the electrical activity of the heart to detect abnormalities.
- Chest X-ray: Imaging to evaluate the size and shape of the heart and detect any associated abnormalities.
- Cardiac catheterization: Invasive procedure to measure pressures and obtain detailed information about the heart's anatomy.
- Genetic testing: Identifying genetic abnormalities or syndromes associated with congenital heart defects.
Nursing Assessment of Congenital Heart Defects in Children:
- Physical examination: Assessing vital signs, heart sounds, and peripheral perfusion.
- Growth and development assessment: Monitoring weight, height, and developmental milestones.
- Oxygen saturation monitoring: Measuring the level of oxygen in the blood using pulse oximetry.
- Respiratory assessment: Assessing respiratory rate, effort, and presence of cyanosis.
- Feeding assessment: Evaluating feeding difficulties and growth patterns.
- Psychosocial assessment: Assessing the psychological and emotional well-being of the child and their family.
Nursing Interventions for Congenital Heart Defects in Children:
- Administering medications as prescribed: Examples include diuretics, vasodilators, and inotropic agents.
- Providing nutritional support: Collaborating with dieticians to ensure appropriate calorie intake and special dietary considerations.
- Promoting oxygenation: Assisting with oxygen therapy and monitoring oxygen saturation levels.
- Positioning for comfort: Teaching parents proper positioning techniques to optimize respiratory function.
- Educating the child and family: Providing information on the condition, treatment, and potential complications.
- Supporting psychosocial needs: Referring families to support groups and providing emotional support.
Treatment and Management of Congenital Heart Defects in Children:
- Surgical interventions: Examples include repair of septal defects, valve repair or replacement, and heart transplantation.
- Cardiac catheterization procedures: Used for diagnostic purposes or to perform interventions such as balloon valvuloplasty.
- Cardiac rehabilitation: Collaborating with physical therapists to optimize the child's physical function and quality of life.
- Medication management: Monitoring medication adherence and assessing for medication side effects.
Long-term monitoring: Regular follow-up appointments to assess cardiac function and detect any potential complications.
Conclusion
- Nursing assessment, interventions, and the overall treatment and management of children with congenital heart defects are essential for providing comprehensive and effective care. Nurses play a vital role in optimizing the health and well-being of these children and their families.
Summary:
- Nursing assessment includes physical examination, growth assessment, oxygen saturation monitoring, respiratory assessment, feeding assessment, and psychosocial assessment.
- Nursing interventions involve medication administration, nutritional support, oxygenation promotion, positioning, education, and psychosocial support.
- Treatment and management encompass surgical interventions, cardiac catheterization procedures, cardiac rehabilitation, medication management, and long-term monitoring.
Down Syndrome
Objectives:
- Understand the etiology of Down syndrome.
- Explain the pathophysiology of Down syndrome.
- Identify the clinical manifestations of Down syndrome.
- Discuss the diagnostic evaluation for Down syndrome.
- Familiarize with information commonly tested in ATI/HESI nursing proctored MCQ exams related to Down syndrome.
- Provide normal ranges for any applicable parameters.
Introduction:
- Down syndrome, also known as trisomy 21, is a genetic disorder caused by the presence of an extra copy of chromosome 21.
- This condition affects individuals both physically and intellectually, and it is the most common chromosomal disorder.
Etiology of Down syndrome:
- Down syndrome is primarily caused by an error in cell division, resulting in an extra copy of chromosome 21.
- There are three main types of Down syndrome: trisomy 21, translocation Down syndrome, and mosaic Down syndrome.
- Trisomy 21 is the most common type and occurs when there is an extra copy of chromosome 21 in every cell.
Pathophysiology of Down syndrome:
- The presence of an extra copy of chromosome 21 leads to an overexpression of genes, resulting in various physical and cognitive characteristics associated with Down syndrome.
- This additional genetic material affects the development of organs, leading to characteristic facial features, congenital heart defects, and other health issues.
- The cognitive impairment experienced by individuals with Down syndrome is attributed to the impact on brain development and functioning.
Clinical Manifestations of Down syndrome:
- Physical characteristics of Down syndrome include almond-shaped eyes, a flat nasal bridge, a small mouth, and a protruding tongue.
- Individuals with Down syndrome may also have low muscle tone, short stature, and a higher risk of developing certain medical conditions such as congenital heart defects, hearing loss, and thyroid disorders.
- Cognitive impairment is common, with varying degrees of intellectual disability observed among individuals with Down syndrome.
- Other clinical manifestations can include speech and language delays, delayed motor skills development, and sensory processing issues.
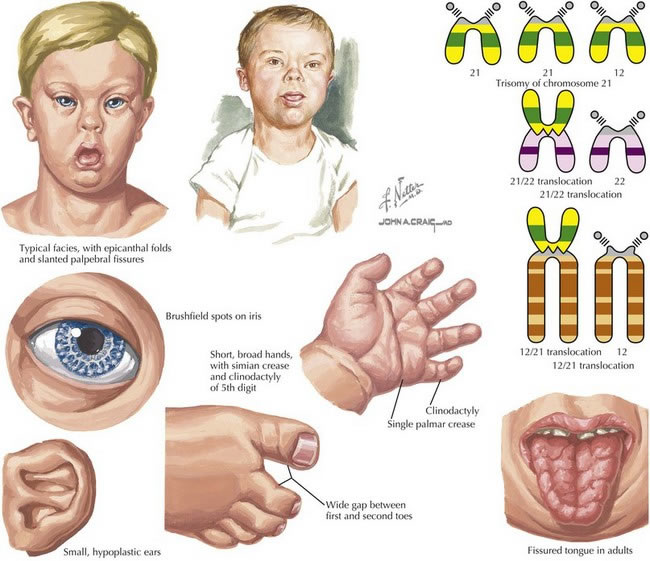
Diagnostic Evaluation of Down syndrome:
- Diagnosis of Down syndrome is usually made prenatally or after birth through genetic testing, such as amniocentesis or chorionic villus sampling.
- Physical examination and assessment of characteristic features are also important in diagnosing Down syndrome.
- Additional diagnostic evaluations may include echocardiography to evaluate heart abnormalities, hearing tests, and thyroid function tests.
Nursing Assessment Down Syndrome:
- Physical assessment:
- Observe for characteristic physical features, such as upward slanting eyes, a flat nasal bridge, and a small mouth.
- Assess for low muscle tone (hypotonia) and joint laxity.
- Evaluate growth parameters, including height, weight, and head circumference.
- Monitor for congenital anomalies, such as heart defects, gastrointestinal abnormalities, and hearing or vision impairments.
- Developmental assessment:
- Assess developmental milestones appropriate for the individual's age, considering the potential delays associated with Down syndrome.
- Evaluate cognitive abilities and intellectual functioning.
- Screen for speech and language delays.
- Assess fine and gross motor skills.
- Psychosocial assessment:
- Consider the emotional well-being of the individual and their family members.
- Evaluate the individual's social interactions and ability to form relationships.
- Assess the support systems available to the individual and their family.
Nursing Interventions Down Syndrome:
- Provide supportive care:
- Create a safe and nurturing environment for the individual, considering their specific needs and abilities.
- Educate caregivers on appropriate handling techniques, including proper positioning and feeding methods.
- Encourage regular physical activity and exercise to promote muscle tone and overall well-being.
- Promote cognitive development:
- Utilize age-appropriate educational materials and techniques to support learning.
- Use visual aids and assistive devices, if necessary, to enhance communication and understanding.
- Collaborate with educators and therapists to develop individualized educational plans and interventions.
- Monitor and manage health conditions:
- Regularly assess vital signs, including heart rate, blood pressure, and oxygen saturation levels.
- Implement preventive measures, such as immunizations and regular health screenings.
- Collaborate with healthcare providers to manage any chronic health conditions or complications.
- Provide emotional support:
- Offer counseling and guidance to individuals and their families, addressing any concerns or emotional challenges.
- Promote self-esteem and independence through positive reinforcement and encouragement.
- Connect families with support groups and resources in the community.
Treatment and Management Down Syndrome:
- Medical management:
- Address any associated health conditions or complications, such as congenital heart defects or gastrointestinal abnormalities, through appropriate medical interventions.
- Monitor and manage comorbidities, such as hypothyroidism, hearing loss, and visual impairments.
- Administer medications as prescribed, considering potential interactions and side effects.
- Early intervention:
- Encourage early intervention services, including physical therapy, occupational therapy, and speech therapy, to support optimal development.
- Collaborate with therapists and educators to implement individualized intervention plans.
- Education and advocacy:
- Educate individuals with Down syndrome and their families about their rights, resources, and available support networks.
- Advocate for inclusive educational opportunities and community integration.
- Facilitate communication and collaboration among healthcare providers, educators, and support services.
Conclusion:
- Down syndrome is a genetic disorder caused by an extra copy of chromosome 21, leading to various physical and cognitive characteristics.
- Early diagnosis and intervention are essential for individuals with Down syndrome to optimize their health and development.
- Nursing professionals play a crucial role in providing comprehensive care, support, and education to individuals with Down syndrome and their families.
- Providing comprehensive care to individuals with Down syndrome requires nurses to have a deep understanding of the condition's physical, developmental, and psychosocial aspects. By conducting thorough nursing assessments, implementing appropriate interventions, and collaborating with interdisciplinary teams, nurses can support individuals with Down syndrome in achieving their fullest potential and enhancing their overall quality of life.
Summary:
- Down syndrome is caused by an extra copy of chromosome 21.
- Etiology includes trisomy 21, translocation Down syndrome, and mosaic Down syndrome.
- Pathophysiology involves the overexpression of genes affecting physical and cognitive development.
- Clinical manifestations include characteristic facial features, low muscle tone, and cognitive impairment.
- Diagnostic evaluation includes genetic testing and physical examination.
- Commonly tested information includes screening tests, genetic counseling, and potential complications.
- Early intervention is crucial for optimal outcomes in individuals with Down syndrome.
- Down syndrome is a genetic disorder caused by the presence of an extra copy of chromosome 21.
- Nursing assessment for individuals with Down syndrome includes physical, developmental, and psychosocial evaluations.
- Nursing interventions focus on supportive care, cognitive development, health management, and emotional support.
- Treatment and management involve medical interventions, early intervention services, and education/advocacy efforts.
- Regular monitoring and collaboration with healthcare providers, educators, and support services are essential for comprehensive care.
Sickle Cell Disease
Objectives:
- Understand the etiology of sickle cell disease.
- Explain the pathophysiology of sickle cell disease.
- Identify the clinical manifestations of sickle cell disease.
- Describe the diagnostic evaluation of sickle cell disease.
- To understand the pathophysiology and etiology of sickle cell disease.
- To identify the signs and symptoms associated with sickle cell disease.
- To recognize the complications and potential risks of sickle cell disease.
- To develop appropriate nursing assessment skills for patients with sickle cell disease.
- To implement effective nursing interventions for patients with sickle cell disease.
- To understand the treatment and management strategies for sickle cell disease.
Introduction
Sickle cell disease is a genetic blood disorder characterized by abnormal hemoglobin production, leading to the formation of sickle-shaped red blood cells. This condition primarily affects individuals of African, Mediterranean, Middle Eastern, and Indian descent. It is important for healthcare professionals to have a comprehensive understanding of the etiology, pathophysiology, clinical manifestations, and diagnostic evaluation of sickle cell disease to provide effective care and support to affected individuals.
Etiology of Sickle Cell Disease:
- Sickle cell disease is caused by a mutation in the gene that codes for hemoglobin, known as HBB gene.
- The mutation results in the production of abnormal hemoglobin, called hemoglobin S.
- This genetic mutation is inherited in an autosomal recessive manner, requiring both parents to pass on the mutated gene for the disease to manifest.
Diagnostic Evaluation of Sickle Cell Disease:
- Hemoglobin electrophoresis: identifies the presence of abnormal hemoglobin S.
- Complete blood count: reveals anemia and other blood cell abnormalities.
- Peripheral blood smear: shows the presence of sickle-shaped red blood cells.
- Newborn screening: allows for early detection of sickle cell disease in newborns.
- Genetic testing: confirms the presence of the HBB gene mutation.
Table 1: Normal Ranges for Relevant Parameters
|
Parameter |
Normal Range |
|
Hemoglobin |
12-16 g/dL (male), 11.5-15.5 g/dL (female) |
|
Red Blood Cell Count |
4.5-5.5 million/mm³ (male), 4.0-5.0 million/mm³ (female) |
|
White Blood Cell Count |
4,500-11,000 cells/mm³ |
|
Platelet Count |
150,000-450,000/mm³ |
|
Hemoglobin Electrophoresis |
HbA (normal), HbS (elevated) |
- Table 2: Examples of Complications in Sickle Cell Disease
|
Organ Complication |
Examples |
|
Lungs |
Acute Chest Syndrome, Pulmonary Hypertension |
|
Kidneys |
Hematuria, Renal Failure |
|
Liver |
Cholelithiasis, Hepatic Sequestration |
|
Spleen |
Functional Asplenia, Increased Infection Risk |
- Table 3: Diagnostic Criteria for Sickle Cell Disease
|
Test |
Diagnostic Criteria |
|
Hemoglobin Electrophoresis |
Presence of Hemoglobin S |
|
Complete Blood Count |
Decreased Hemoglobin, Abnormal Red Blood Cell Indices |
|
Peripheral Blood Smear |
Presence of Sickled Red Blood Cells |
|
Newborn Screening |
Positive for Sickle Cell Disease |
|
Genetic Testing |
Identification of HBB Gene Mutation |
Nursing Assessment for Sickle Cell Disease:
- Detailed patient history, including family history of sickle cell disease
- Assessment of vital signs, including temperature, heart rate, blood pressure, and respiratory rate
- Evaluation of pain intensity and location
- Monitoring for signs and symptoms of vaso-occlusive crisis, such as joint pain, fever, and swelling
- Assessment of neurologic status, including cognitive function and sensory perception
- Evaluation of skin integrity, looking for ulcers or areas of tissue damage
- Monitoring for signs and symptoms of anemia, such as fatigue, pallor, and shortness of breath
- Assessment of nutritional status
- Evaluation of psychosocial well-being and coping mechanisms
Nursing Interventions Sickle Cell Disease
- Administering prescribed pain medications promptly and monitoring their effectiveness
- Encouraging adequate hydration to prevent dehydration and promote blood flow
- Educating patients on the importance of avoiding triggers for vaso-occlusive crises, such as extreme temperatures or physical exertion
- Providing emotional support and counseling to help patients cope with the chronic nature of the disease
- Assisting with activities of daily living and mobility to prevent complications and maintain independence
- Collaborating with other healthcare professionals to develop individualized care plans
- Educating patients and their families about the importance of regular follow-up appointments and adherence to prescribed treatment regimens
- Promoting self-care strategies, such as stress management and pain management techniques
Treatment and Management of Sickle Cell Disease:
- Blood transfusions to increase the number of healthy red blood cells
- Hydroxyurea therapy to reduce the frequency of pain crises and complications
- Antibiotics prophylaxis to prevent infections
- Pain management strategies, including nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids
- Oxygen therapy for patients with acute chest syndrome or respiratory distress
- Hematopoietic stem cell transplantation as a potential curative treatment option
- Genetic counseling and education for individuals and families affected by sickle cell disease
- Psychosocial support and counseling to address the emotional and psychological impact of the disease
Conclusion
Sickle cell disease is a complex condition that requires comprehensive nursing care and management. Nurses play a vital role in assessing, intervening, and educating patients with sickle cell disease to improve their quality of life and prevent complications. By understanding the pathophysiology, implementing appropriate interventions, and collaborating with the healthcare team, nurses can make a significant difference in the lives of individuals affected by sickle cell disease.
Summary
- Sickle cell disease is a genetic blood disorder characterized by abnormal hemoglobin.
- Nursing assessment includes patient history, vital signs, pain assessment, and monitoring for complications.
- Nursing interventions focus on pain management, hydration, education, and support.
- Treatment options include blood transfusions, hydroxyurea therapy, and antibiotics prophylaxis.
- Nurses play a crucial role in providing comprehensive care and support to patients with sickle cell disease.
Diabetic Ketoacidosis (DKA) in Children
Etiology of Diabetic Ketoacidosis (DKA) in Children
- Diabetic ketoacidosis (DKA) is a serious complication of diabetes mellitus in children, characterized by hyperglycemia, ketosis, and metabolic acidosis
- DKA occurs more frequently in children with type 1 diabetes mellitus (T1DM), but it can also occur in children with type 2 diabetes mellitus (T2DM) or gestational diabetes mellitus (GDM)
- The etiology of DKA in children involves a combination of factors, including insulin deficiency, increased counter-regulatory hormone levels, and dehydration
- Insulin deficiency, which can result from missed insulin doses, illness, or other factors, leads to uncontrolled glucose production by the liver and impaired glucose uptake by peripheral tissues, leading to hyperglycemia
- Increased counter-regulatory hormone levels, such as glucagon, cortisol, and growth hormone, further exacerbate hyperglycemia and stimulate lipolysis, leading to the production of ketone bodies
- Dehydration, which can result from osmotic diuresis and vomiting, further exacerbates the metabolic derangements in DKA by reducing renal perfusion and exacerbating acidosis
Pathophysiology of Diabetic Ketoacidosis (DKA) in Children
- The pathophysiology of DKA in children involves a complex interplay between insulin deficiency, increased counter-regulatory hormone levels, and metabolic acidosis
- Insulin deficiency leads to uncontrolled glucose production by the liver and impaired glucose uptake by peripheral tissues, leading to hyperglycemia
- Increased counter-regulatory hormone levels, such as glucagon, cortisol, and growth hormone, further exacerbate hyperglycemia and stimulate lipolysis, leading to the production of ketone bodies
- The accumulation of ketone bodies in the blood leads to metabolic acidosis, which can cause a range of symptoms, including Kussmaul breathing, nausea, vomiting, and altered mental status
- The acidosis also leads to electrolyte imbalances, such as hyperkalemia, hyponatremia, and hypophosphatemia, which can further exacerbate the metabolic derangements in DKA
Clinical Manifestations of Diabetic Ketoacidosis (DKA) in Children
- The clinical manifestations of DKA in children can vary depending on the severity and duration of the metabolic derangements
- The classic symptoms of DKA include polyuria, polydipsia, polyphagia, weight loss, fatigue, Kussmaul breathing, nausea, vomiting, and altered mental status
- Children with DKA may also present with signs of dehydration, such as dry mucous membranes, poor skin turgor, and tachycardia
- In severe cases, children with DKA may develop hypotension, shock, and cerebral edema, which can be life-threatening
Diagnostic Evaluation of Diabetic Ketoacidosis (DKA) in Children
- The diagnostic evaluation of DKA in children involves a combination of clinical findings, laboratory tests, and imaging studies to confirm the diagnosis and determine the severity of the metabolic derangements
- The initial laboratory evaluation of a child with suspected DKA includes blood levels of glucose, ketones, blood urea nitrogen, creatinine, electrolytes, calculated anion gap, arterial blood gases, osmolality, complete blood count with differential, blood cultures, and urine studies including ketones, urinalysis, and urine culture
- Imaging studies, such as chest radiography and computed tomography (CT) of the head, may be ordered to evaluate for complications such as pneumonia or cerebral edema
- The diagnosis of DKA is based on laboratory findings, including hyperglycemia (blood glucose level >11 mmol/L), ketosis (blood β-hydroxybutyrate level ≥3 mmol/L or moderate to high ketonuria), and metabolic acidosis (venous pH <7.3 or serum bicarbonate level <15 mmol/L)
Nursing Assessment DKA in children
- Assess the child's medical history, including any previous episodes of DKA, diabetes diagnosis, and current diabetes management. Note any recent illnesses, infections, or changes in medication or diet that may have contributed to the development of DKA
- Monitor the child's vital signs, paying close attention to heart rate, blood pressure, and respiratory rate. Elevated heart rate and decreased blood pressure may indicate dehydration, while rapid, deep respirations (Kussmaul respirations) are a compensatory mechanism for metabolic acidosis
- Check the child's capillary refill time to assess peripheral perfusion. Prolonged capillary refill time may indicate poor tissue perfusion and hypovolemia
- Assess the child's level of consciousness and mental status. DKA can lead to cerebral edema, which may manifest as changes in behavior, irritability, confusion, or lethargy
- Monitor the child's urine output. Decreased urine output may indicate hypovolemia and impaired renal function
- Assess the child's skin turgor and mucous membranes for signs of dehydration. Dry skin, cracked lips, and sunken eyes may be present in a dehydrated child
- Check the child's weight. Rapid weight loss may be a sign of DKA, and ongoing weight loss may indicate poor diabetes management
- Monitor the child's blood glucose levels. Hyperglycemia is a hallmark of DKA, with blood glucose levels typically exceeding 250 mg/dL (13.9 mmol/L)
- Monitor the child's electrolyte levels, including potassium, sodium, and bicarbonate. Hypokalemia is a common complication of DKA and may require supplementation
- Assess for signs of infection, as infections can trigger DKA in children with diabetes. Look for fever, elevated white blood cell count, and localized signs of infection
- Evaluate the child's respiratory status. Auscultate lung sounds for the presence of crackles, which may indicate pulmonary edema, a potential complication of DKA
- Assess the child's gastrointestinal status. Nausea, vomiting, and abdominal pain are common symptoms of DKA and may contribute to fluid and electrolyte imbalances
- Monitor the child's cardiac status. ECG changes, such as peaked T waves or widened QRS complexes, may indicate electrolyte imbalances, particularly hyperkalemia or hypokalemia
- Assess the child's fluid status. Evaluate skin turgor, mucous membranes, and fontanelle (in infants) for signs of dehydration. Monitor intake and output, and assess for signs of fluid overload, such as edema or crackles in the lungs
- Check for signs of metabolic acidosis. Assess the child's respiratory rate, depth, and pattern for Kussmaul respirations. Monitor arterial blood gas (ABG) values for a low pH and low bicarbonate level
- Assess the child's pain level. Abdominal pain is a common symptom of DKA and may require pain management interventions
- Evaluate the child's nutritional status. Assess the child's dietary intake, including the type and amount of carbohydrates consumed. Monitor for signs of malnutrition or poor growth in children with chronic diabetes
- Assess the child's family support system. Determine the level of understanding and involvement of the child's parents or caregivers in diabetes management. Provide education and support as needed
Nursing interventions for Diabetic Ketoacidosis (DKA) in children include:
- Assessing the patient: Check blood sugars, mental status, signs of infection, and urine output
- Stabilizing the patient: After initial stabilization of circulation, airway, and breathing, specific treatment of DKA requires correction of hyperglycemia with intravenous insulin, frequent monitoring, and replacement of electrolytes, mainly potassium, correction of hypovolemia with intravenous fluids, and correction of acidosis
- Administering insulin: IV insulin is the standard treatment for DKA as the patient needs insulin rapidly to decrease glucose
- Starting two large-bore IVs: This is necessary for fluid resuscitation and maintenance, insulin therapy, electrolyte replacement, and supportive care, which are the mainstays of management in DKA
- Administering fluids: Provide intravenous fluid replacement to restore peripheral circulation, renal perfusion, and electrolyte balance
- Monitoring fluid and electrolyte balance: Check electrolytes as potassium levels will drop with insulin treatment, and monitor for hypokalemia, hyponatremia, hypocalcemia, hypomagnesemia, and hypophosphatemia
- Educating the patient and family: Teach the patient on the importance of compliance with diabetic medications, the importance of follow-up, and how to recognize symptoms of DKA as well as prevent recurrences
- Coordinating with a diabetes educator: Patients who struggle with managing their diabetes may need education by a diabetes educator
- Monitoring for cerebral edema: Cerebral edema occurs in ~0.5% of children presenting in DKA, and it has a mortality of ~25%. At highest risk are (1) children newly diagnosed with diabetes, (2) younger children, and (3) children with the greatest degree of dehydration and acidosis
- Preventing falls and injuries: Patients with DKA may experience weakness and fatigue, often exacerbated by dehydration and electrolyte imbalances. To prevent falls and injuries, nurses should provide assistance with ambulation when necessary and ensure a safe environment
Treatment and Management of Diabetic Ketoacidosis (DKA) in Children
- The treatment and management of DKA in children involve a combination of interventions to correct fluid and electrolyte imbalances, reduce hyperglycemia, and prevent complications. The following are nursing interventions for the treatment and management of DKA in children:
- Fluid resuscitation: The initial management of DKA in children involves fluid resuscitation with 0.9% saline to restore intravascular volume and renal perfusion. The amount of fluid required depends on the degree of dehydration, which is typically 5-10% of body weight
- Electrolyte replacement: Electrolyte imbalances, particularly hypokalemia, are common in DKA and require replacement
- Potassium replacement should be initiated once urine output is established and serum potassium levels are known
- nsulin therapy: Insulin therapy is essential to normalize blood glucose levels and suppress ketogenesis. Insulin is typically administered intravenously, with the goal of reducing blood glucose levels by 50-75 mg/dL per hour
- Monitoring blood glucose and electrolyte levels: Blood glucose and electrolyte levels should be monitored frequently to guide insulin and electrolyte replacement therapy
- Monitoring for complications: Children with DKA are at risk for complications such as cerebral edema, hypokalemia, and aspiration pneumonia. Nurses should monitor for signs and symptoms of these complications and intervene promptly as needed.
- Patient and family education: Education is a critical component of DKA management, particularly for children with newly diagnosed diabetes. Nurses should provide education on diabetes management, including insulin therapy, dietary recommendations, and blood glucose monitoring
- Consultation with a diabetes educator: Children who struggle with diabetes management may benefit from consultation with a diabetes educator
- Coordination of outpatient care: After discharge, children with DKA require ongoing diabetes management and follow-up care. Nurses should coordinate with the pediatric diabetes care team to ensure appropriate outpatient care
- Prevention of recurrence: Children with DKA are at increased risk for recurrence, particularly if diabetes management is suboptimal. Nurses should provide education and support to prevent recurrence, including regular blood glucose monitoring, adherence to insulin therapy and dietary recommendations, and prompt recognition and treatment of any signs or symptoms of hyperglycemia or ketosis
Summary
- The treatment and management of DKA in children involve a combination of interventions to correct fluid and electrolyte imbalances, reduce hyperglycemia, and prevent complications.
- The initial management of DKA in children involves fluid resuscitation with 0.9% saline, electrolyte replacement, and insulin therapy.
- Blood glucose and electrolyte levels should be monitored frequently, and children should be monitored for complications such as cerebral edema, hypokalemia, and aspiration pneumonia.
- Education and support are critical components of DKA management, particularly for children with newly diagnosed diabetes.
- Children who struggle with diabetes management may benefit from consultation with a diabetes educator.
- After discharge, children with DKA require ongoing diabetes management and follow-up care to prevent recurrence
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Common Pediatric Conditions
This filled cannot be empty

