Please set your exam date
Antihypertensives and Cardiovascular Medications
Study Questions
Introduction
A nurse is teaching a client with hypertension about antihypertensive drugs. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Antihypertensive drugs can lower blood pressure by affecting different parts of the cardiovascular system.This is a general statement that covers the various mechanisms of action of different classes of antihypertensive drugs, such as beta blockers, diuretics, ACE inhibitors, ARBs, calcium channel blockers, alpha blockers, and renin inhibitors.Each class of drugs has a different way of influencing the heart rate, blood vessel tone, blood volume, or hormonal activity that regulate blood pressure.
Choice A is wrong because antihypertensive drugs do not work by increasing the blood flow to the heart and kidneys.In fact, some antihypertensive drugs may decrease the blood flow to these organs as a side effect.
Choice C is wrong because antihypertensive drugs are not safe to use with any other medications or supplements.There are many potential drug interactions that can affect the efficacy or safety of antihypertensive drugs.For example, NSAIDs can reduce the blood pressure lowering effect of some antihypertensive drugs and increase the risk of kidney damage. Therefore, patients should always consult their doctor or pharmacist before taking any other medications or supplements with antihypertensive drugs.
Choice D is wrong because antihypertensive drugs will not cure hypertension if taken as prescribed.Hypertension is a chronic condition that requires lifelong management and lifestyle changes.Antihypertensive drugs can only control the blood pressure and prevent complications, but they do not address the underlying causes of hypertension.If patients stop taking their antihypertensive drugs, their blood pressure will likely rise again and increase the risk of heart attack, stroke, and kidney failure.
A nurse is reviewing the medication history of a client who has hypertension and is prescribed a calcium channel blocker. Which of the following medications should the nurse instruct the client to avoid? (Select all that apply.)
Explanation
The nurse should instruct the client to avoid grapefruit juice and St. John’s wort when taking a calcium channel blocker.
Here is why:
• Grapefruit juice can increase the blood levels of calcium channel blockers, which can lead to adverse effects such as hypotension, bradycardia, and edema.
The normal blood pressure range is 90/60 mmHg to 120/80 mmHg, and the normal heart rate range is 60 to 100 beats per minute.
• St.John’s wort can decrease the effectiveness of calcium channel blockers by inducing their metabolism in the liver.
This can reduce the therapeutic effect of lowering blood pressure and preventing angina.
• Ibuprofen, digoxin, and warfarin are not contraindicated with calcium channel blockers, but they should be used with caution and monitored closely for potential interactions.
Ibuprofen can increase the risk of bleeding when taken with warfarin, digoxin can increase the risk of arrhythmias when taken with calcium channel blockers, and warfarin can increase the risk of bleeding when taken with calcium channel blockers.
A nurse is caring for a client who has hypertension and is taking hydrochlorothiazide. The client reports muscle weakness and fatigue. Which of the following responses should the nurse make?
Explanation
Hydrochlorothiazide is a thiazide diuretic that lowers blood pressure by increasing urine output. However, it also causes potassium loss, which can lead to muscle weakness and fatigue.Therefore, the client should consume foods that are rich in potassium, such as bananas, oranges, potatoes, and spinach.
Choice A is wrong because drinking more fluids can increase blood volume and blood pressure, which is not desirable for a client who has hypertension.Dehydration is not a common side effect of hydrochlorothiazide.
Choice C is wrong because hydrochlorothiazide does not affect blood sugar levels directly. However, it can interact with some antidiabetic medications and increase the risk of hypoglycemia.Therefore, the client should monitor blood sugar levels regularly if taking both medications.
Choice D is wrong because hydrochlorothiazide does not increase sensitivity to sunlight. However, it can cause photosensitivity reactions in some clients, such as rash, itching, or redness of the skin. Therefore, the client should use sunscreen and wear protective clothing when exposed to sunlight.
A nurse is assessing a client who has hypertension and is taking an angiotensin-converting enzyme (ACE) inhibitor. Which of the following findings should the nurse report to the provider?
Explanation
A serum potassium level of 5.2 mEq/L.The nurse should report this finding to the provider because it indicateshyperkalemia, which is a potential adverse effect of ACE inhibitors. Hyperkalemia can cause cardiac arrhythmias and muscle weakness, and it requires prompt treatment.
Choice A is wrong because a dry cough is a common and benign side effect of ACE inhibitors. It does not indicate a serious problem and does not require reporting to the provider.
Choice B is wrong because a heart rate of 72/min is within the normal range of 60 to 100 beats per minute. It does not indicate any adverse effect of ACE inhibitors or hypertension.
Choice D is wrong because a blood pressure of 130/80 mm Hg is within the target range for a client who has hypertension. It indicates that the ACE inhibitor is effective in lowering the blood pressure and does not require reporting to the provider.
A nurse is providing dietary education to a client who has hypertension and hyperlipidemia. Which of the following foods should the nurse recommend to the client?
Explanation
Oatmeal is a good source of soluble fiber, which can help lower cholesterol levels and blood pressure. Oatmeal also has a low glycemic index, which means it does not cause rapid spikes in blood sugar levels. A client who has hypertension and hyperlipidemia should avoid foods that are high in saturated fat, sodium, and sugar, as they can worsen these conditions.
Choice A is wrong because whole milk is high in saturated fat, which can increase cholesterol levels and the risk of cardiovascular disease. A client who has hypertension and hyperlipidemia should choose low-fat or skim milk instead.
Choice B is wrong because salted nuts are high in sodium, which can increase blood pressure and fluid retention. A client who has hypertension and hyperlipidemia should choose unsalted nuts or seeds, which are rich in healthy fats, protein, and fiber.
Choice D is wrong because bacon is high in saturated fat, sodium, and nitrates, which can increase cholesterol levels, blood pressure, and inflammation. A client who has hypertension and hyperlipidemia should limit or avoid processed meats and choose lean sources of protein instead.
Medications for hypertension management
A nurse is teaching a middle-age client about hypertension. Which of the following information should the nurse include in the teaching?
Explanation
Diuretics are drugs that increase urine output and reduce fluid volume in the body. They lower blood pressure by decreasing the amount of sodium and water in the blood vessels, which reduces the pressure on the walls of the arteries. Diuretics are often the first-line therapy for hypertension, especially for older adults and African Americans.
Choice A is wrong because reaching the goal blood pressure depends on many factors, such as the severity of hypertension, the response to medication, and the lifestyle changes of the client. It may take longer than 2 months to achieve optimal blood pressure control.
Choice C is wrong because limiting alcohol consumption to three drinks a day is not enough to prevent or treat hypertension. Alcohol can raise blood pressure by interfering with the effects of medication, stimulating the nervous system, and increasing fluid retention. The recommended limit for alcohol intake is no more than one drink a day for women and two drinks a day for men.
Choice D is wrong because hypertension cannot be cured with medication. Hypertension is a chronic condition that requires lifelong management and monitoring. Medication can help lower blood pressure, but it does not address the underlying causes of hypertension, such as genetics, obesity, stress, or kidney disease. Lifestyle modifications, such as diet, exercise, weight loss, and smoking cessation, are also essential for preventing complications and improving quality of life.
Normal ranges for blood pressure are:
• Systolic: less than 120 mm Hg
• Diastolic: less than 80 mm Hg
Hypertension is defined as:
• Systolic: 130 mm Hg or higher
• Diastolic: 80 mm Hg or higher
A nurse is screening a male client for hypertension. The nurse should identify that which of the following actions by the client increase his risk for hypertension? (Select all that apply.)
Explanation
Drinking 36 oz beer daily and eating a diet high in sodium are actions that increase the risk for hypertension.
Here is why:
• Drinking too much alcohol can raise blood pressure and also damage the liver, brain, and heart.The American Heart Association recommends limiting alcohol intake to no more than one drink per day for women and two drinks per day for men.
• Eating a diet high in sodium can cause the body to retain fluid, which increases blood pressure.The American Heart Association recommends limiting sodium intake to no more than 2,300 mg per day, and ideally no more than 1,500 mg per day.
Choice A, B, and C are wrong because:
• Drinking 8 oz nonfat milk daily is not a risk factor for hypertension.In fact, dairy products may help lower blood pressure by providing calcium, potassium, and protein.
• Eating popcorn at the movie theater is not a risk factor for hypertension, unless the popcorn is heavily salted or buttered.Popcorn is a whole grain that can provide fiber and antioxidants.
• Walking 1 mile daily at 12 min/mile pace is not a risk factor for hypertension.On the contrary, physical activity can help lower blood pressure by strengthening the heart and blood vessels.
Normal blood pressure range is less than 120/80 mm Hg (millimeters of mercury).
Elevated blood pressure range is 120-129/less than 80 mm Hg.
Hypertension stage 1 range is 130-139/80-89 mm Hg.
Hypertension stage 2 range is 140 or higher/90 or higher mm Hg.Hypertensive crisis range is higher than 180/higher than 120 mm Hg.
A nurse is screening a male client for hypertension. The nurse should identify that which of the following actions by the client increase his risk for hypertension? (Select all that apply.)
Explanation
Captopril is a medication used to treat high blood pressure, heart failure, and kidney problems. It belongs to a class of drugs called angiotensin-converting enzyme (ACE) inhibitors, which work by relaxing blood vessels and lowering blood pressure. One of the common side effects of captopril is a dry cough, which may be caused by the accumulation of a substance called bradykinin in the lungs. A persistent cough may indicate that the medication is not well tolerated and may need to be changed.Therefore, the client should report any signs of a cough to their health care provider.
Choice A is wrong because captopril should be taken on an empty stomach, at least one hour before or two hours after meals.Food may decrease the absorption and effectiveness of captopril.
Choice B is wrong because captopril should not be stopped abruptly, even if the blood pressure becomes normal. Stopping captopril suddenly may cause a rebound increase in blood pressure and worsen the condition.Captopril should be taken regularly as prescribed, and only discontinued under the guidance of a health care provider.
Choice D is wrong because captopril should not be taken only when the client has symptoms of high blood pressure. High blood pressure is often asymptomatic, meaning that it does not cause any noticeable signs or symptoms. However, high blood pressure can damage the heart, kidneys, brain, and other organs over time.Therefore, captopril should be taken daily as a preventive measure to lower the risk of complications from high blood pressure.
Normal blood pressure range is less than 120/80 mm Hg (millimeters of mercury).
Elevated blood pressure range is 120-129/less than 80 mm Hg.
Stage 1 high blood pressure range is 130-139/80-89 mm Hg.
Stage 2 high blood pressure range is 140 or higher/90 or higher mm Hg.Hypertensive crisis range is 180 or higher/120 or higher mm Hg.
A client with hypertension is prescribed hydrochlorothiazide (HCTZ). Which of the following statements by the client indicates an understanding of the medication?
Explanation
All of the statements by the client indicate alack of understandingof the medication.
Here is why:
Choice A is wrong because hydrochlorothiazide (HCTZ) is a diuretic (water pill) that increases the amount of urine produced and excreted by the kidneys. Taking this medication at bedtime may cause frequent urination at night and disrupt the sleep cycle.It is recommended to take HCTZ in the morning or early afternoon.
Choice B is wrong because HCTZ is prescribed to treat high blood pressure (hypertension), which is a chronic condition that requires long-term management. Stopping the medication abruptly may cause a rebound increase in blood pressure and increase the risk of complications such as stroke, heart attack, or kidney failure.The client should continue taking HCTZ as directed by the doctor, even if the blood pressure becomes normal.
Choice C is wrong because a persistent cough is not a common side effect of HCTZ. A cough may be a sign of an allergic reaction, a respiratory infection, or another condition that needs medical attention. HCTZ may cause other side effects such as nausea, dizziness, headache, low blood pressure, low potassium levels, high calcium levels, or skin rash.The client should report any unusual or bothersome symptoms to the doctor.
Choice D is wrong because HCTZ is not a medication that can be taken as needed for symptoms of high blood pressure. High blood pressure often has no symptoms and can damage the blood vessels and organs over time. HCTZ works by reducing the fluid volume and pressure in the blood vessels.It needs to be taken regularly and consistently to maintain its effectiveness and prevent fluctuations in blood pressure. The client should be educated about the purpose, benefits, risks, and instructions of taking HCTZ. The client should also be advised to monitor their blood pressure, weight, fluid intake and output, and electrolyte levels while on this medication.The client should also be counseled about lifestyle modifications such as diet, exercise, stress management, and smoking cessation that can help lower blood pressure and improve overall health.
A nurse is caring for a client who is receiving nitroprusside for hypertensive crisis. Which of the following findings should indicate to the nurse that the client is experiencing an adverse effect of this medication?
Explanation
Nitroprusside is a vasodilator that lowers blood pressure by dilating blood vessels.It is used to treat hypertensive crisis, which is a life-threatening condition of very high blood pressure.However, nitroprusside can cause excessive hypotension, which is a serious side effect that can lead to irreversible ischemic injuries or death. Therefore, the nurse should monitor the client’s blood pressure continuously and adjust the infusion rate accordingly.
Choice B is wrong because Bradycardia is wrong because nitroprusside does not affect the heart rate directly.However, bradycardia can occur as a reflex response to hypotension, which is a possible adverse effect of nitroprusside. Therefore, the nurse should also monitor the client’s heart rate and rhythm.
Choice C is wrong because Tachycardia is wrong because nitroprusside does not cause tachycardia directly.However, tachycardia can occur as a compensatory mechanism to hypotension, which is a possible adverse effect of nitroprusside. Therefore, the nurse should also monitor the client’s heart rate and rhythm.
Choice D is wrong because Hypertension is wrong because nitroprusside is used to lower blood pressure, not to raise it.However, hypertension can occur if the infusion is stopped abruptly, which can cause rebound vasoconstriction and increased blood pressure. Therefore, the nurse should taper off the infusion gradually and avoid sudden discontinuation.
Normal ranges for blood pressure are systolic less than 120 mmHg and diastolic less than 80 mmHg.
Normal ranges for heart rate are 60 to 100 beats per minute.
A nurse is teaching a client who has stable angina about the use of sublingual nitroglycerin. Which of the following statements by the client indicates a need for further teaching?
Explanation
This statement indicates a need for further teaching because sublingual nitroglycerin tablets should not be swallowed, but dissolved under the tongue for rapid absorption and onset of action. Swallowing the tablet would reduce its effectiveness and delay its action.
Choice A is wrong because nitroglycerin tablets should be kept in a dark, glass bottle to protect them from light, heat, and moisture, which can degrade the drug.The bottle should be tightly closed and labeled with the date of opening.
Choice B is wrong because nitroglycerin tablets can be taken every 5 minutes for up to three doses if chest pain persists.If the pain is not relieved after three doses, the client should call 911 or seek emergency medical attention.
Choice D is wrong because nitroglycerin tablets have a short shelf life and should be replaced every 6 months or as indicated by the manufacturer.The client should check the expiration date and discard any unused tablets after 6 months.
A nurse is administering aspirin to a client who has angina and is at risk for myocardial infarction. Which of the following statements by the nurse explains the rationale for this medication?
Explanation
Aspirin is an antiplatelet drug that inhibits the aggregation of platelets and prevents the formation of thrombi, which can occlude the coronary arteries and cause angina or myocardial infarction.Aspirin is recommended for clients who have angina and are at risk for myocardial infarction as a secondary prevention measure.
Choice A is wrong because aspirin does not lower blood pressure or reduce cardiac workload.These effects are achieved by other drugs such as beta blockers, calcium channel blockers, or angiotensin-converting enzyme inhibitors.
Choice C is wrong because aspirin does not dilate the coronary arteries or increase blood flow to the heart.These effects are achieved by other drugs such as nitrates or calcium channel blockers.
Choice D is wrong because aspirin does not reduce inflammation or pain in the chest.These effects are achieved by other drugs such as nonsteroidal anti-inflammatory drugs or opioids.
A nurse is monitoring a client who is receiving intravenous heparin for angina and has a history of atrial fibrillation. Which of the following laboratory tests should the nurse use to evaluate the effectiveness of heparin therapy?
Explanation
Activated partial thromboplastin time (aPTT) is the laboratory test that the nurse should use to evaluate the effectiveness of heparin therapy.Heparin is an anticoagulant that works by helping antithrombin inactivate thrombin and factor Xa, reducing the production of fibrin and thus decreasing the formation of clots.The aPTT measures the time it takes for a clot to form in a sample of blood after adding certain substances.The normal range for aPTT is 25 to 35 seconds.A therapeutic level of heparin is 1.5 to 2.5 times the normal value, or 46 to 70 seconds.
Choice A is wrong because prothrombin time (PT) is a test that measures the time it takes for a clot to form in a sample of blood after adding tissue factor.PT is used to monitor warfarin therapy, not heparin therapy.The normal range for PT is 11 to 13 seconds.
Choice B is wrong because international normalized ratio (INR) is a standardized way of reporting the PT results, taking into account the variations in different laboratories and reagents.INR is also used to monitor warfarin therapy, not heparin therapy.The normal range for INR is 0.8 to 1.2.
Choice D is wrong because platelet count is a test that measures the number of platelets in a sample of blood.Platelets are cell fragments that help with blood clotting by sticking together and forming a plug at the site of injury.Platelet count is not directly related to heparin therapy, although heparin can cause a rare but serious adverse effect called heparin-induced thrombocytopenia (HIT), which is a drop in platelet count due to an immune reaction that leads to excessive clotting.The normal range for platelet count is 150,000 to 400,000/mm3.
Medications for arrhythmias
A nurse is caring for a client who is prescribed quinidine for the treatment of arrhythmias. Which of the following should the nurse monitor for as an adverse effect of this medication?
Explanation
Quinidine is an antiarrhythmic medication that can cause hypokalemia (low potassium levels) as an adverse effect. Potassium is an electrolyte that is important for the normal functioning of the heart and muscles.Hypokalemia can cause arrhythmias, muscle weakness, cramps, and fatigue.
Choice A is wrong because quinidine does not cause hypertension (high blood pressure).In fact, quinidine can lower blood pressure by dilating blood vessels and reducing the force of heart contractions.Normal blood pressure ranges are less than 120/80 mm Hg for systolic and diastolic pressures, respectively.
Choice B is wrong because quinidine does not cause hypoglycemia (low blood glucose levels).Quinidine does not affect insulin secretion or glucose metabolism.Normal blood glucose ranges are 70 to 99 mg/dL (3.9 to 5.5 mmol/L) before meals and less than 140 mg/dL (7.8 mmol/L) two hours after meals.
Choice D is wrong because quinidine does not cause hypernatremia (high sodium levels).Quinidine does not affect sodium balance or excretion. Sodium is another electrolyte that is important for fluid balance, nerve impulses, and muscle contractions.Hypernatremia can cause thirst, confusion, seizures, and coma.Normal sodium ranges are 135 to 145 mEq/L (135 to 145 mmol/L).
A nurse is caring for a client who is prescribed amiodarone for the treatment of arrhythmias. Which of the following should the nurse monitor for as an adverse effect of this medication? (Select all that apply)
Explanation
Amiodarone is a medication used to treat irregular heartbeats, but it can cause various adverse effects, such as:
• Photosensitivity, which means increased sensitivity of the skin to sunlight and risk of sunburn.
This can be prevented by wearing protective clothing and sunscreen when outdoors.
• Pulmonary toxicity, which means damage to the lungs that can cause inflammation, scarring, or difficulty breathing.
This can be fatal in some cases and requires regular monitoring of chest X-rays and pulmonary function tests.
• Thyroid dysfunction, which means abnormal levels of thyroid hormones that can affect metabolism, energy, and mood.
This can be either hypothyroidism (low thyroid hormone) or hyperthyroidism (high thyroid hormone) and requires regular monitoring of thyroid function tests.
Choice A and B are wrong because amiodarone can causebradycardia(slow heartbeat) andhypotension(low blood pressure), not the opposite.
These effects can be serious and require close monitoring of heart rate and blood pressure.
A nurse is caring for a client who is prescribed lidocaine for the treatment of arrhythmias. Which of the following should the nurse monitor for as an adverse effect of this medication?
Explanation
This is because lidocaine is a local anesthetic that can cause various side effects, some of which may be serious and require emergency medical help.These include difficulty breathing, swelling of the face, lips, tongue, or throat, twitching, tremors, seizure, a light-headed feeling, slow heart rate, weak pulse, weak or shallow breathing, and sudden feeling of warmth with muscle stiffness and pain.Dizziness is a common sign of central nervous system (CNS) excitation and/or depression caused by lidocaine.
Choice B is wrong because “My mouth feels dry” is wrong because dry mouth is not a typical side effect of lidocaine.Dry mouth can be caused by dehydration, medications, salivary gland problems, or other medical conditions.
Choice C is wrong because “My urine is dark” is wrong because dark urine is not a common side effect of lidocaine.Dark urine can be a sign of dehydration, liver problems, blood in the urine, or other health issues.Normal urine color ranges from clear to pale yellow.
Choice D is wrong because “I have a headache” is wrong because headache is not a usual side effect of lidocaine.Headache can be caused by many factors, such as stress, lack of sleep, dehydration, or other medical conditions.
Some additional sentences are:
assistantIf you are prescribed lidocaine for the treatment of arrhythmias, you should monitor for any signs of adverse effects and seek medical help if they occur.
You should also follow the dosage instructions carefully and avoid taking more than the recommended amount.Lidocaine can interact with some other medications, so you should inform your doctor about any other drugs you are taking.
A client who has been prescribed propranolol for the treatment of arrhythmias reports experiencing shortness of breath and difficulty breathing while lying down at night. Which of the following should the nurse instruct the client to do?
Explanation
This can help to elevate the chest and open up the airways, reducing shortness of breath and difficulty breathing.Propranolol is a beta blocker that can cause side effects such as slower heart rate, fatigue, dizziness, cold hands and feet, and Raynaud’s phenomenon. These side effects can worsen breathing problems, especially when lying down flat.
Choice B is wrong because sleeping on the left side may not be enough to improve breathing.It may also cause more pressure on the heart and lungs, which can affect blood circulation and oxygen delivery.
Choice C is wrong because sleeping on the right side may not be helpful for breathing either.Some research suggests that sleeping on the right side can make breathing more difficult for some people with obstructive sleep apnea.
Choice D is wrong because sleeping on the back can increase snoring, sleep apnea, and reflux symptoms, which can all interfere with breathing.Sleeping on the back can also cause the tongue and soft palate to block the airway, reducing oxygen intake.
A nurse is caring for a client who is prescribed verapamil for the treatment of arrhythmias. Which of the following should the nurse monitor for as an adverse effect of this medication?
Explanation
Verapamil is a medication that belongs to a class of drugs called calcium channel blockers, which are used to treat high blood pressure, angina, and arrhythmias. Verapamil works by relaxing the blood vessels and slowing down the heart rate, which lowers blood pressure and reduces the workload of the heart. However, verapamil can also affect the smooth muscles of the digestive tract, causing them to contract less frequently and forcefully.This can lead to constipation, which is a common side effect of verapamil.
Choice A is wrong because verapamil does not cause hypertension, but rather lowers blood pressure.In fact, verapamil can sometimes cause hypotension, which is abnormally low blood pressure.
Choice B is wrong because verapamil does not cause hyperkalemia, which is a high level of potassium in the blood.Verapamil can actually lower potassium levels by increasing its excretion in the urine.Hyperkalemia can be caused by other medications, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), or potassium-sparing diuretics.
Choice C is wrong because verapamil does not cause hypoglycemia, which is a low level of glucose in the blood.Verapamil does not affect insulin secretion or glucose metabolism.Hypoglycemia can be caused by other medications, such as insulin or sulfonylureas, or by fasting, alcohol consumption, or exercise.
The normal ranges for blood pressure, potassium, and glucose are as follows:
• Blood pressure: less than 120/80 mm Hg (millimeters of mercury) when fasting and less than 140/90 mm Hg two hours after eating for people without diabetes; less than 130/80 mm Hg for people with diabetes.
• Potassium: 3.6 to 5.2 mmol/L (millimoles per liter) or 3.6 to 5.2 mEq/L (milliequivalents per liter).
• Glucose: less than 100 mg/d
Medications for heart failure
A nurse is caring for a client with heart failure who is receiving furosemide (Lasix). Which of the following findings should indicate to the nurse that the medication is effective?
Explanation
Furosemide (Lasix) is a diuretic that helps reduce fluid overload and edema in clients with heart failure.Increased urine output indicates that the medication is effective in removing excess fluid from the body and improving cardiac function.
Choice B is wrong because Decreased blood pressure is wrong because furosemide (Lasix) does not directly lower blood pressure, although it may have a mild effect due to reduced blood volume.Decreased blood pressure may also indicate hypovolemia, dehydration, or shock, which are complications of heart failure and diuretic therapy.
Choice C is wrong because Increased heart rate is wrong because furosemide (Lasix) does not affect the heart rate, unless the client develops electrolyte imbalances or hypovolemia, which can cause tachycardia.Increased heart rate may also indicate worsening heart failure, as the heart tries to compensate for reduced cardiac output.
Choice D is wrong because Decreased respiratory rate is wrong because furosemide (Lasix) does not affect the respiratory rate, unless the client develops respiratory depression or alkalosis, which are rare side effects of the medication.Decreased respiratory rate may also indicate fatigue, sedation, or opioid overdose, which are not related to heart failure or diuretic therapy.
Normal ranges for urine output are 30 to 60 mL/hr for adults, blood pressure is 120/80 mm Hg or lower for normal and 140/90 mm Hg or higher for hypertension, heart rate is 60 to 100 beats/min for adults, and respiratory rate is 12 to 20 breaths/min for adults.
A nurse is caring for a client who has heart failure and is receiving spironolactone (Aldactone). Which of the following findings should indicate to the nurse that the client is experiencing an adverse effect of this medication? (Select all that apply)
Explanation
The correct answer is choice A. Hyperkalemia.Spironolactone is a potassium-sparing diuretic that prevents the body from absorbing too much salt and keeps the potassium levels from getting too low.However, this also means that it can cause high potassium levels (hyperkalemia) in some patients, especially those with kidney problems or taking other medications that affect potassium.Hyperkalemia can cause serious symptoms such as muscle weakness, irregular heartbeat, nausea, and paralysis.
Choice B is wrong becauseHypokalemia is wrong because spironolactone does not cause low potassium levels, but rather prevents them.
Choice C is wrong becauseGynecomastia is wrong because it is not a common adverse effect of spironolactone in women, but rather in men.Gynecomastia is the enlargement of breast tissue in males due to hormonal imbalance.
Choice D is wrong becauseMenorrhagia is wrong because it is not a common adverse effect of spironolactone in women, but rather in men.Menorrhagia is the excessive or prolonged bleeding during menstrual periods.
Choice E.Impotence is wrong because it is not a common adverse effect of spironolactone in women, but rather in men.Impotence is the inability to achieve or maintain an erection sufficient for sexual intercourse.
A client who has heart failure tells the nurse, “I have been taking my furosemide as prescribed, but I still feel short of breath.” Which of the following statements should the nurse make?
Explanation
You should notify your provider if you experience weight gain. This is because weight gain can indicate fluid retention, which can worsen heart failure and cause more shortness of breath. Furosemide is a diuretic that helps reduce fluid overload, but it may not be enough to control the symptoms of heart failure. Therefore, the provider may need to adjust the dose or add another medication.
Choice A is wrong because you should not increase your intake of foods high in potassium. Furosemide can cause potassium loss, but increasing potassium intake can lead to hyperkalemia, which can affect the heart rhythm and function. You should follow the provider’s advice on how much potassium to consume and have your potassium levels checked regularly.
Choice B is wrong because you should not decrease your intake of fluids. Dehydration can cause low blood pressure, kidney damage, and electrolyte imbalance, which can also affect the heart. You should drink enough fluids to stay hydrated, but not too much to cause fluid overload. The provider may give you a specific amount of fluid to drink per day based on your condition.
Choice D is wrong because you should not take your medication with food. Furosemide is best absorbed on an empty stomach, and food can interfere with its effectiveness. You should take furosemide at least one hour before or two hours after meals.
A nurse is caring for a client who has heart failure and is receiving captopril (Capoten). Which of the following statements by the client indicates an understanding of the medication?
Explanation
Captopril (Capoten) is an ACE inhibitor that can cause a dry, nonproductive cough as a side effect. This cough may be bothersome and interfere with the quality of life of the client.The client should inform the provider if this occurs, as the medication may need to be changed or adjusted.
Choice A is wrong because captopril should be taken one hour before meals, not with food.Food may decrease the absorption and effectiveness of the medication.
Choice B is wrong because captopril can cause hyperkalemia, or high levels of potassium in the blood, by decreasing aldosterone secretion.The client should avoid foods high in potassium, such as bananas, oranges, potatoes, and tomatoes, and have their potassium levels monitored regularly.
Choice D is wrong because captopril can cause hypotension, or low blood pressure, especially when the client first starts taking the medication or when the dose is increased.The client should take captopril in the morning or during the day, not at bedtime, to avoid orthostatic hypotension and falls.The client should also rise slowly from a sitting or lying position and report any symptoms of dizziness, lightheadedness, or fainting to the provider.
A nurse is caring for a client who has heart failure and is receiving lisinopril (Zestril). Which of the following findings should indicate to the nurse that the medication is effective?
Explanation
Choice B is wrong because Increased urine output.This indicates that the medication is effective in reducing the fluid overload and improving the renal perfusion in the client who has heart failure.
Choice A is wrong because decreased blood pressure is not a specific indicator of the medication’s effectiveness. Lisinopril (Zestril) is an angiotensin-converting enzyme (ACE) inhibitor that lowers blood pressure by blocking the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor.However, blood pressure can also be affected by other factors, such as dehydration, bleeding, or shock.
Choice C is wrong because increased heart rate is not a desired outcome of the medication. Lisinopril (Zestril) does not directly affect the heart rate, but it may cause reflex tachycardia as a compensatory mechanism for the reduced blood pressure.Increased heart rate can also worsen the cardiac workload and oxygen demand in the client who has heart failure.
Choice D is wrong because decreased respiratory rate is not a reliable sign of the medication’s effectiveness.Lisinopril (Zestril) may help reduce pulmonary congestion and dyspnea in the client who has heart failure, but respiratory rate can also be influenced by other factors, such as sedation, pain, or anxiety.
Normal ranges for vital signs are as follows:
• Blood pressure: 90/60 mm Hg to 120/80 mm Hg
• Heart rate: 60 to 100 beats per minute
• Respiratory rate: 12 to 20 breaths per minute
• Urine output: at least 30 mL per hour
More questions
A nurse is caring for a client who has hypertension and is prescribed metoprolol, a beta blocker. The nurse should monitor the client for which of the following adverse effects?
Explanation
This is because metoprolol is a beta blocker, which can block the beta-2 receptors in the lungs and cause constriction of the airways.This can lead to breathing problems such as shortness of breath, cough, and wheezing. Bronchospasm is more likely to occur in people who have asthma or chronic obstructive pulmonary disease (COPD).
Choice A is wrong because tachycardia, or fast heart rate, is not an adverse effect of metoprolol. In fact, metoprolol can lower the heart rate by blocking the beta-1 receptors in the heart.A normal resting heart rate for adults ranges from 60 to 100 beats per minute (bpm).Metoprolol can cause bradycardia, or slow heart rate, which can be a serious side effect if it is too low.
Choice B is wrong because hyperglycemia, or high blood sugar, is not an adverse effect of metoprolol. Metoprolol does not affect the insulin secretion or glucose metabolism in the body.A normal blood sugar level for adults without diabetes is less than 140 mg/dL (7.8 mmol/L) two hours after eating. Metoprolol can cause hypoglycemia, or low blood sugar, in people who have diabetes and take insulin or other glucose-lowering medications.This is because metoprolol can mask the symptoms of hypoglycemia, such as palpitations and tremors.
Choice D is wrong because hyperkalemia, or high potassium, is not an adverse effect of metoprolol. Metoprolol does not affect the potassium balance in the body.
A normal blood potassium level for adults is 3.6 to 5.2 millimoles per liter (mmol/L)
A nurse is evaluating a client who has hypertension and is taking lisinopril, an angiotensin II receptor blocker (ARB). Which of the following outcomes indicates that the medication is effective?
Explanation
The client has a blood pressure of 120/78 mm Hg. This indicates that the medication is effective because it lowers the blood pressure below the hypertensive levels.In adults 60 years of age or older, this is typically defined as a systolic pressure below 150 mm Hg and a diastolic pressure below 90 mm Hg.
Choice A is wrong because the client has no edema in the lower extremities. This is not a specific outcome of lisinopril, an angiotensin II receptor blocker (ARB). Edema can be caused by many factors, such as heart failure, kidney disease, or venous insufficiency. Lisinopril does not directly affect fluid retention or edema.
Choice B is wrong because the client has a urine output of 30 mL/hr. This is a low urine output that may indicate dehydration, kidney impairment, or urinary obstruction. Lisinopril is expected to increase urine output by reducing the blood pressure and improving the renal blood flow.
Choice D is wrong because the client has a serum creatinine level of 1.2 mg/dL. This is a high serum creatinine level that may indicate kidney damage or reduced kidney function. Lisinopril is expected to lower the serum creatinine level by preventing the progression of kidney disease and protecting the kidney from further injury.
Normal ranges of urine output, blood pressure, and serum creatinine are:
• Urine output: 800 to 2000 mL/day or 40 to 80 mL/hr
• Blood pressure: less than 120/80 mm Hg for adults
• Serum creatinine: 0.6 to 1.2 mg/dL for males and 0.5 to 1.1 mg/dL for females
A nurse is teaching a client who has hypertension and is prescribed nifedipine, a calcium channel blocker, about self-care measures. Which of the following instructions should the nurse include? (Select all that apply.)
Explanation
Nifedipine is a calcium channel blocker that lowers blood pressure by relaxing the blood vessels and reducing the workload of the heart.
The following instructions should be included in the teaching:
• Avoid drinking alcohol while taking this medication.Alcohol can increase the risk of side effects such as dizziness, flushing, headache, and low blood pressure.
• Monitor your blood pressure and pulse regularly.This will help to evaluate the effectiveness of the medication and detect any abnormal changes.Normal blood pressure for adults is less than 130/80 mm Hg and normal pulse rate is 60 to 100 beats per minute.
• Report any swelling in your ankles or feet to your provider.This can be a sign of fluid retention or heart failure, which are possible complications of nifedipine.
• Do not stop taking this medication abruptly.This can cause a rebound increase in blood pressure and chest pain.The dose should be tapered gradually under the supervision of the provider.
Choice E is wrong because chewing or crushing the sustained-release tablet can cause too much of the drug to be released at once, which can lead to overdose or severe side effects.
The tablet should be swallowed whole with a glass of water.
Which drug blocks the binding of angiotensin II to its receptors on blood vessels and adrenal glands, preventing its vasoconstrictive and aldosterone-stimulating effects?
Explanation
Angiotensin II receptor blockers (ARBs) block the binding of angiotensin II to its receptors on blood vessels and adrenal glands, preventing its vasoconstrictive and aldosterone-stimulating effects
Choice A is wrong because beta blockers do not block angiotensin II receptors, but rather beta-adrenergic receptors, which are involved in the sympathetic nervous system.Beta blockers reduce heart rate and blood pressure by inhibiting the effects of adrenaline and noradrenaline
Choice B is wrong because calcium channel blockers do not block angiotensin II receptors, but rather calcium channels, which are involved in the contraction of smooth muscle cells.Calcium channel blockers relax blood vessels and lower blood pressure by reducing the influx of calcium into the cells
Choice D is wrong because direct acting vasodilators do not block angiotensin II receptors, but rather act directly on the smooth muscle cells of blood vessels, causing them to relax and dilate.Direct acting vasodilators lower blood pressure by decreasing peripheral resistance
Which drug increases the excretion of water and sodium by the kidneys, reducing blood volume and blood pressure?
Explanation
Diuretics are drugs that increase the excretion of water and sodium by the kidneys, reducing blood volume and blood pressure.Diuretics lower blood pressure by dilating peripheral arterioles and decreasing blood volume by increasing the excretion of sodium and water.
Choice A is wrong because angiotensin-converting enzyme (ACE) inhibitors do not increase the excretion of water and sodium by the kidneys.ACE inhibitors block the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor and stimulator of aldosterone secretion.By reducing angiotensin II levels, ACE inhibitors lower blood pressure by dilating blood vessels and decreasing sodium and water retention.
Choice C is wrong because adrenergic drugs do not increase the excretion of water and sodium by the kidneys. Adrenergic drugs act on the sympathetic nervous system, which regulates heart rate, blood pressure, and other functions. Depending on the type and location of adrenergic receptors, adrenergic drugs can have different effects on blood pressure. Some adrenergic drugs can increase blood pressure by stimulating alpha receptors, which cause vasoconstriction.Other adrenergic drugs can decrease blood pressure by stimulating beta receptors, which cause vasodilation and decreased cardiac output.
Choice D is wrong because direct acting vasodilators do not increase the excretion of water and sodium by the kidneys. Direct acting vasodilators are drugs that relax the smooth muscle of blood vessels, causing them to widen and lower blood pressure.Direct acting vasodilators do not affect the renin-angiotensin-aldosterone system or the sympathetic nervous system, which regulate sodium and water balance.
Which drugs act on the sympathetic nervous system, which regulates blood pressure by controlling heart rate, cardiac output, vascular tone, and renin release?
Explanation
Adrenergic drugs.These are drugs that stimulate the sympathetic nervous system by mimicking or enhancing the effects of epinephrine and norepinephrine, the chemical messengers that activate adrenergic receptors.Adrenergic drugs can increase blood pressure, heart rate, cardiac output, vascular tone, and renin release by acting on different types of adrenergic receptors.
Choice A is wrong because beta blockers are drugs that inhibit the sympathetic nervous system by blocking the beta adrenergic receptors, which are responsible for increasing heart rate and contractility. Beta blockers can lower blood pressure and reduce cardiac workload.
Choice B is wrong because calcium channel blockers are drugs that inhibit the movement of calcium ions across the cell membrane of smooth muscle cells, which are found in blood vessels and the heart.Calcium channel blockers can relax blood vessels and lower blood pressure, as well as reduce heart rate and contractility.
Choice C is wrong because angiotensin II receptor blockers (ARBs) are drugs that block the action of angiotensin II, a hormone that causes vasoconstriction and stimulates the release of aldosterone, which increases sodium and water retention.
ARBs can lower blood pressure by dilating blood
A patient with atrial fibrillation has been prescribed digoxin (Lanoxin). The nurse should monitor which laboratory value to evaluate therapeutic effectiveness?
Explanation
Digoxin (Lanoxin) is a cardiac glycoside that is used to treat atrial fibrillation and heart failure.
It works by increasing the force of cardiac contraction and slowing down the heart rate.
However, digoxin can also cause toxicity, which can lead to life-threatening arrhythmias.
One of the risk factors for digoxin toxicity is hypokalemia, or low serum potassium level.
Potassium is an electrolyte that is essential for normal cardiac function and conduction.When the serum potassium level is low, digoxin binds more strongly to the cardiac cells and increases its effects, which can result in bradycardia, heart block, or ventricular tachycardia.
Therefore, the nurse should monitor the serum potassium level to evaluate the therapeutic effectiveness and safety of digoxin therapy.
Choice B) Serum sodium level is wrong because sodium is not directly related to digoxin action or toxicity.
Sodium is another electrolyte that is important for fluid balance and blood pressure regulation.However, sodium does not affect the binding of digoxin to the cardiac cells or its effects on the heart rate and contractility.
Therefore, the nurse does not need to monitor the serum sodium level to evaluate digoxin therapy.
Choice C) Serum magnesium level is wrong because magnesium is not directly related to digoxin action or toxicity.
Magnesium is another electrolyte that is involved in many enzymatic reactions and neuromuscular function.However, magnesium does not affect the binding of digoxin to the cardiac cells or its effects on the heart rate and contractility.
Therefore, the nurse does not need to monitor the serum magnesium level to evaluate digoxin therapy.
Choice D) Serum calcium level is wrong because calcium is not directly related to digoxin action or toxicity.
Calcium is another electrolyte that is essential for bone health and muscle contraction.However, calcium does not affect the binding of digoxin to the cardiac cells or its effects on the heart rate and contractility.
Therefore, the nurse does not need to monitor the serum calcium level to evaluate digoxin therapy.
The normal range for serum potassium level is 3.5-5.0 mEq
The nurse is caring for a patient with atrial fibrillation who has been prescribed warfarin (Coumadin). The patient’s INR level is 3.5, which is above therapeutic range. What action should the nurse take?
Explanation
Warfarin is an anticoagulant that prevents blood clots from forming or growing larger. It works by inhibiting the synthesis of vitamin K-dependent clotting factors in the liver. The INR (international normalized ratio) is a measure of how long it takes the blood to clot.The therapeutic range for INR depends on the indication for warfarin therapy, but for atrial fibrillation, it is usually between 2 and 3. An INR level of 3.5 is above the therapeutic range, which means the blood is too thin and the patient is at risk of bleeding. The nurse should hold the warfarin dose and notify the physician, who may order vitamin K to reverse the effects of warfarin.
Choice A) Administer vitamin K as ordered by physician is wrong because vitamin K is not indicated unless the physician orders it based on the patient’s condition and INR level.
Vitamin K is an antidote for warfarin overdose and can reverse its anticoagulant effects.
However, administering vitamin K without a physician’s order may cause the INR to drop below the therapeutic range and increase the risk of clotting.
Choice B) Administer heparin as ordered by physician is wrong because heparin is another anticoagulant that works by activating antithrombin, a natural inhibitor of clotting factors.
Heparin is used for acute treatment of thromboembolic disorders, such as deep vein thrombosis or pulmonary embolism.
It is not indicated for atrial fibrillation unless there is evidence of acute thrombosis.
Administering heparin to a patient with an elevated INR would increase the risk of bleeding.
Choice C) Administer warfarin as ordered by physician is wrong because warfarin is the cause of the elevated INR and should be withheld until the INR returns to the therapeutic range.
Continuing to administer warfarin would further increase the INR and the risk of bleeding.
The nurse is caring for a patient with atrial fibrillation who has been prescribed diltiazem (Cardizem). The patient reports feeling dizzy and lightheaded when standing up quickly from a sitting position or when getting out of bed in the morning. What action should the nurse take?
Explanation
This is because diltiazem (Cardizem) is a calcium channel blocker that lowers blood pressure and can cause orthostatic hypotension, which is a sudden drop in blood pressure when standing up from a sitting or lying position. This can lead to dizziness and lightheadedness, which can increase the risk of falls and injuries. Changing positions slowly can help prevent or reduce these symptoms by allowing the body to adjust to the change in blood pressure.
Choice A) Administer diltiazem as ordered by physician is wrong because it does not address the patient’s complaint of dizziness and lightheadedness, which are side effects of the medication.
The nurse should monitor the patient’s blood pressure and heart rate before and after administering diltiazem, and report any abnormal findings to the physician.
Choice C) Notify physician immediately is wrong because it is not necessary to notify the physician immediately for a common and mild side effect of diltiazem, unless the patient has other signs of severe hypotension, such as fainting, chest pain, or confusion.
The nurse should educate the patient about the possible side effects of diltiazem and how to prevent or manage them.
Choice D) Hold diltiazem and notify physician if symptoms persist is wrong because it is not appropriate to hold a prescribed medication without a valid reason or an order from the physician.
Holding diltiazem could cause the patient’s blood pressure to rise and increase the risk of complications from atrial fibrillation, such as stroke or heart failure.
The nurse should administer diltiazem as ordered and monitor the patient’s response.
A nurse is caring for a client who has heart failure and is receiving digoxin (Lanoxin). The nurse should monitor which of the following laboratory values to determine therapeutic effectiveness of this medication?
Explanation
The nurse should monitor the serum potassium level to determine the therapeutic effectiveness of digoxin (Lanoxin), a cardiac glycoside that improves the contractility and pumping ability of the heart. Digoxin has a narrow therapeutic range and can cause toxicity if the serum level is too high or if the patient has hypokalemia (low potassium).Hypokalemia can result from diuretic therapy, which is often prescribed for heart failure patients to reduce fluid overload.
Therefore, the nurse should monitor the serum potassium level and report any abnormal values to the provider.The normal potassium level is 3.5 to 5.0 mEq/L.
Choice B) Serum sodium level is wrong because sodium level is not directly affected by digoxin therapy.
Sodium level may be altered in heart failure patients due to fluid retention or diuretic use, but it does not indicate the effectiveness of digoxin.
Choice C) Serum magnesium level is wrong because magnesium level is not directly affected by digoxin therapy.
Magnesium level may be altered in heart failure patients due to diuretic use or renal impairment, but it does not indicate the effectiveness of digoxin.
Choice D) Serum calcium level is wrong because calcium level is not directly affected by digoxin therapy.
Calcium level may be altered in heart failure patients due to renal impairment or vitamin D deficiency, but it does not indicate the effectiveness of digoxin.
A nurse is caring for a client who has heart failure and is receiving carvedilol (Coreg). The nurse should monitor which of the following laboratory values to determine therapeutic effectiveness of this medication?
Explanation
The nurse should monitor the serum potassium level to determine the therapeutic effectiveness of carvedilol (Coreg), which is a beta-blocker that can lower the heart rate and blood pressure. Carvedilol can also cause hyperkalemia, which is a high level of potassium in the blood that can lead to cardiac arrhythmias and muscle weakness.Therefore, the nurse should monitor the serum potassium level and report any values above 5.0 mEq/L to the provider.
Choice B) Serum sodium level is wrong because carvedilol does not affect the sodium level significantly.Sodium level is more relevant for diuretics, which can cause hyponatremia (low sodium) or hypernatremia (high sodium) depending on the type and dose of the medication.
Choice C) Serum magnesium level is wrong because carvedilol does not affect the magnesium level significantly.
Magnesium level is more relevant for digoxin, which is another medication used for heart failure that can cause hypomagnesemia (low magnesium) or hypermagnesemia (high magnesium).Hypomagnesemia can increase the risk of digoxin toxicity, while hypermagnesemia can decrease the effectiveness of digoxin.
Choice D) Serum calcium level is wrong because carvedilol does not affect the calcium level significantly.
Calcium level is more relevant for calcium channel blockers, which are another class of medications used for heart failure that can lower the heart rate and blood pressure by blocking the entry of calcium into the cardiac and vascular smooth muscle cells.
Calcium channel blockers can cause hypocalcemia (low calcium) or hypercalcemia (high calcium), which can affect the cardiac contractility and conduction.
The normal ranges for serum electrolytes are:
• Potassium: 3.5 to 5.0 mEq/L
• Sodium: 135 to 145 mEq/L
• Magnesium: 1.5 to 2.5 mEq/L
• Calcium: 8.5 to 10.5 mg/dL
A nurse is caring for a client who has heart failure and is prescribed furosemide. Which of the following laboratory values should the nurse monitor closely?
Explanation
The nurse should monitor the client’s serum potassium level closely because furosemide is a loop diuretic that can cause hypokalemia, which increases the risk of cardiac arrhythmias and digitalis toxicity. The nurse should also monitor the client’s fluid status, blood pressure, and renal function.
Choice B is wrong because Serum calcium is wrong because furosemide does not affect calcium levels significantly. Calcium levels are more likely to be affected by thiazide diuretics, which can cause hypercalcemia.
Choice C is wrong because Serum albumin is wrong because furosemide does not affect albumin levels significantly. Albumin levels are more likely to be affected by liver disease, malnutrition, or nephrotic syndrome.
Choice D is wrong because Serum glucose is wrong because furosemide does not affect glucose levels significantly. Glucose levels are more likely to be affected by diabetes mellitus, corticosteroids, or stress.
Normal ranges for the laboratory values are:
• Serum potassium: 3.5-5.0 mEq/L
• Serum calcium: 8.5-10.5 mg/dL
• Serum albumin: 3.5-5.0 g/dL
• Serum glucose: 70-110 mg/dL
A nurse is teaching a client who has heart failure and is prescribed captopril. Which of the following instructions should the nurse include? (Select all that apply.).
Explanation
Captopril is an angiotensin-converting enzyme (ACE) inhibitor that is used to treat heart failure by lowering blood pressure and reducing the workload on the heart.
The nurse should include the following instructions when teaching a client who is prescribed captopril:
• Avoid salt substitutes that contain potassium.Captopril can increase the potassium levels in the blood, which can lead to hyperkalemia.Salt substitutes that contain potassium can further increase the risk of hyperkalemia, which can cause cardiac arrhythmias and muscle weakness.
• Report any dry cough to the provider.A dry cough is a common side effect of captopril and other ACE inhibitors.It is caused by the accumulation of bradykinin, a substance that dilates blood vessels and causes inflammation in the lungs.
The cough can be annoying and interfere with sleep and quality of life.The provider may switch the client to another type of medication if the cough is bothersome.
• Take the medication on an empty stomach.Food can decrease the absorption and effectiveness of captopril.The client should take the medication at least 1 hour before or 2 hours after meals.
• Rise slowly from a sitting or lying position.Captopril can cause orthostatic hypotension, which is a sudden drop in blood pressure when changing positions.
This can lead to dizziness, fainting, and falls.The client should rise slowly and sit on the edge of the bed for a few minutes before standing up.
Choice D is wrong because drinking at least 3 L of fluids per day is not recommended for clients with heart failure.
Excessive fluid intake can worsen the symptoms of heart failure, such as edema, shortness of breath, and fatigue.The client should limit fluid intake to 2 L or less per day, unless instructed otherwise by the provider.
A nurse is assessing a client who has heart failure and is receiving metoprolol. Which of the following statements by the client indicates a therapeutic effect of the medication?
Explanation
Choice B is wrong because “I can walk farther without getting tired.” This statement indicates a therapeutic effect of metoprolol, which is a beta-blocker that reduces the heart rate, blood pressure, and the workload of the heart.This helps to improve the blood flow and oxygen delivery to the heart and other organs, and reduces the symptoms of heart failure such as fatigue, dyspnea, and edema.
Choice A is wrong because “I have less swelling in my ankles.” This statement indicates a possible effect of a diuretic, which is a medication that reduces fluid retention and edema by increasing urine output.Metoprolol does not have a direct diuretic effect, although it may indirectly reduce fluid accumulation by improving cardiac function.
Choice C is wrong because “I don’t have chest pain anymore.” This statement indicates a possible effect of a nitrate, which is a medication that dilates the blood vessels and reduces the oxygen demand of the heart.Metoprolol may also help to prevent or treat angina by lowering the heart rate and blood pressure, but it is not the primary medication for chest pain relief.
Choice D is wrong because “I can breathe better at night.” This statement indicates a possible effect of an oxygen therapy, which is a treatment that delivers supplemental oxygen to the lungs and improves gas exchange.Metoprolol may also help to reduce dyspnea by improving cardiac function and reducing pulmonary congestion, but it is not the primary treatment for respiratory distress.
A nurse is evaluating a client who has heart failure and is receiving warfarin. Which of the following statements by the client indicates a need for further teaching?
Explanation
Choice B is wrong because “I will eat more green leafy vegetables.” This statement indicates a need for further teaching because green leafy vegetables are high in vitamin K, which can antagonize the effects of warfarin and increase the risk of clotting.The client should be advised to maintain a consistent intake of vitamin K and avoid sudden changes in their diet.
Choice A is wrong because using an electric razor for shaving is a safe practice for a client who is receiving warfarin, as it reduces the risk of bleeding from cuts or nicks.
Choice C is wrong because checking stools for blood is an important measure for a client who is receiving warfarin, as it can indicate gastrointestinal bleeding, which is a serious adverse effect of the medication.
Choice D is wrong because having blood drawn regularly is necessary for a client who is receiving warfarin, as it allows the monitoring of the international normalized ratio (INR), which reflects the degree of anticoagulation and guides the dosage adjustment of the medication.
The normal range for INR for a client who is receiving warfarin is 2 to 3, unless otherwise specified by the provider.
A nurse is planning to administer mannitol to a client who has heart failure and pulmonary edema. Which of the following actions should the nurse take before giving the medication?
Explanation
Mannitol is an osmotic diuretic that increases urine output and decreases intracranial pressure and intraocular pressure. The nurse should check the urine output before giving the medication to ensure adequate renal function and prevent fluid overload and electrolyte imbalance. The normal urine output is 0.5 to 1 mL/kg/hr.
Choice B is wrong because checking the blood pressure is not specific to mannitol administration. Mannitol can cause hypotension or hypertension depending on the fluid status of the client, but this is not the priority action before giving the medication.
Choice C is wrong because checking the blood glucose is not relevant to mannitol administration. Mannitol does not affect blood glucose levels.
Choice D is wrong because checking the oxygen saturation is not related to mannitol administration. Mannitol does not affect oxygen saturation levels.
The nurse is caring for a patient with chronic heart failure who has been prescribed digoxin (Lanoxin). The patient’s apical pulse rate is 58 beats/min. What should the nurse do next?
Explanation
Digoxin (Lanoxin) is a cardiac glycoside that is used to improve the contractility of the heart and slow down the heart rate in patients with chronic heart failure. However, digoxin has a narrow therapeutic range and can cause toxicity if the dose is too high or if the patient has low potassium levels. A normal serum digoxin level is 0.5 to 2 ng/mL and a normal serum potassium level is 3.5 to 5 mEq/L. A low heart rate (less than 60 beats/min) is a sign of digoxin toxicity and the nurse should withhold the medication and report it to the provider. The nurse should also check the patient’s serum digoxin and potassium levels to determine if they are within normal limits.
Choice A is wrong because administering the medication as ordered could worsen the patient’s condition and increase the risk of digoxin toxicity.
Choice C is wrong because checking the patient’s serum digoxin level is not enough to prevent digoxin toxicity. The nurse should also check the patient’s serum potassium level and heart rate before giving digoxin.
Choice D is wrong because giving an additional dose of digoxin could cause a fatal overdose and lead to cardiac arrest. The nurse should never give more than the prescribed dose of digoxin without consulting the provider.
The nurse is teaching a patient with heart failure about dietary modifications to reduce fluid retention and improve cardiac function. Which of the following foods should the nurse advise the patient to limit or avoid?
Explanation
The nurse should advise the patient with heart failure to limit or avoid canned soups and sauces because they are high in sodium, which can cause fluid retention and worsen cardiac function.Sodium intake should be restricted to less than 2 g per day for patients with heart failure.
Choice A is wrong because fresh fruits and vegetables are good sources of potassium, magnesium, and fiber, which are beneficial for heart health.Potassium and magnesium help regulate fluid and electrolyte balance, and fiber helps lower cholesterol and blood pressure.
Choice B is wrong because whole grains and cereals are also rich in fiber, as well as complex carbohydrates, which provide energy and prevent rapid fluctuations in blood glucose levels.Whole grains and cereals may also contain phytochemicals that have antioxidant and anti-inflammatory effects.
Choice C is wrong because lean meats and poultry are low in saturated fat and cholesterol, which can contribute to atherosclerosis and coronary artery disease. Lean meats and poultry provide protein, which is essential for tissue repair and wound healing.Protein intake should be adequate but not excessive for patients with heart failure, as too much protein can increase the workload of the kidneys.
The nurse is reviewing the discharge instructions with a patient who has heart failure and is prescribed losartan (Cozaar). Which of the following statements by the patient indicates understanding of the teaching? (Select all that apply.)
Explanation
Losartan (Cozaar) is an angiotensin II receptor blocker (ARB) that is used to treat heart failure by lowering blood pressure and reducing fluid retention.
Patients taking losartan should:
• Weigh themselves every morning and report any changes.
This helps to monitor fluid status and detect signs of worsening heart failure.Weight gain of more than 2 kg (4.4 lb) in a week or 1 kg (2.2 lb) in a day should be reported to the health care provider.
• Call their doctor if they have a sore throat or fever.This could indicate an infection or a rare but serious side effect of losartan called angioedema, which causes swelling of the face, lips, tongue, or throat.
The other choices are wrong because:
• Losartan does not need to be taken with food to prevent stomach upset.It can be taken with or without food.
• Losartan does not increase the sensitivity to sunlight.However, some other medications for heart failure, such as diuretics, may do so.
• Drinking plenty of fluids to stay hydrated is not recommended for patients with heart failure, as it may worsen fluid retention and overload the heart.Patients should follow their prescribed fluid restriction and limit their sodium intake.
Exams on Antihypertensives and Cardiovascular Medications
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Identify the main categories of antihypertensive drugs and their mechanisms of action
- Describe the common side effects and nursing implications of antihypertensive drugs
- Explain the difference between angina and myocardial infarction and the medications used to treat them
- Recognize the types of arrhythmias and the drugs used to correct them
- Understand the pathophysiology of heart failure and the drugs used to manage it
- Compare and contrast the different classes of diuretics and their effects on electrolytes and blood pressure
Introduction
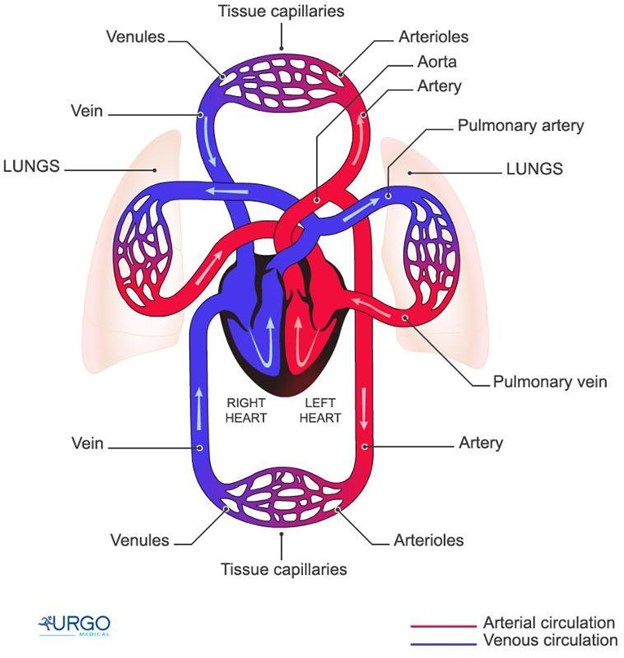
-Hypertension is a chronic condition characterized by elevated blood pressure, which increases the risk of cardiovascular and renal complications such as stroke, heart attack, heart failure, and kidney disease
-Antihypertensive drugs are medications that lower blood pressure by acting on different targets in the cardiovascular system, such as receptors, enzymes, hormones, or ion channels
-Cardiovascular medications are drugs that treat various disorders of the heart and blood vessels, such as angina, arrhythmias, heart failure, and hyperlipidemia
-The choice of medication depends on the type and severity of the condition, the patient’s characteristics and preferences, and the potential benefits and risks of each drug
Medications for hypertension management
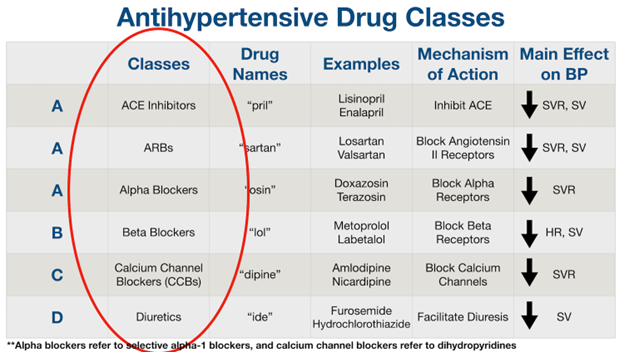
- Antihypertensive drugs can be classified into several categories based on their mechanisms of action:
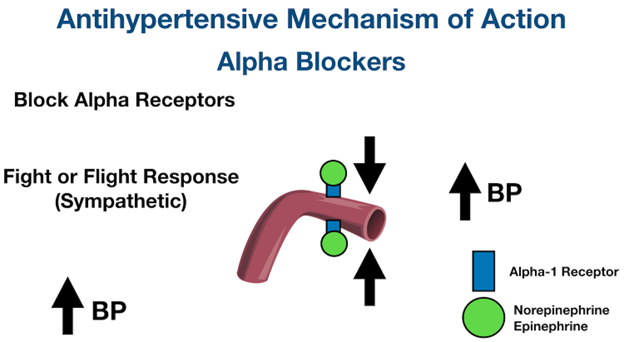
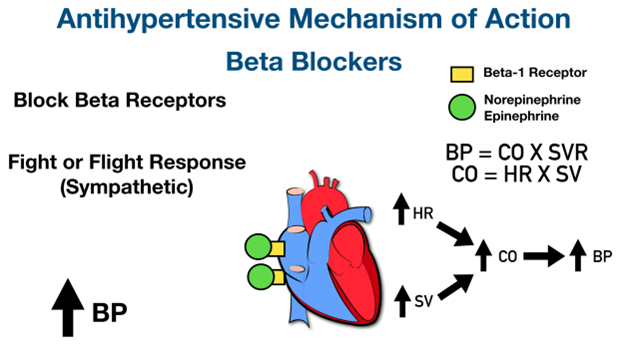
1. Adrenergic drugs: These drugs act on the sympathetic nervous system, which regulates blood pressure by controlling heart rate, cardiac output, vascular tone, and renin release. They include beta blockers, alpha blockers, centrally acting alpha 2 agonists, adrenergic neuron blockers, and alpha 1 and beta 1 blockers.
2. Direct acting vasodilators: These drugs relax the smooth muscle of the blood vessels, causing them to widen and lower blood pressure. They include hydralazine, minoxidil, nitroprusside, and diazoxide.
3. Angiotensin-converting enzyme (ACE) inhibitors: These drugs inhibit the enzyme that converts angiotensin I to angiotensin II, a potent vasoconstrictor and stimulator of aldosterone secretion. They include captopril, enalapril, lisinopril, ramipril, and others with the suffix -pril.
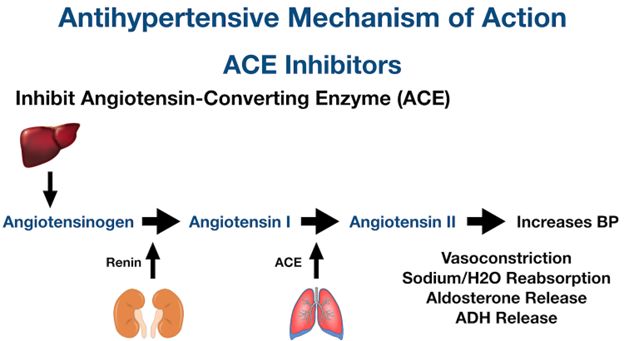
4. Angiotensin II receptor blockers (ARBs): These drugs block the binding of angiotensin II to its receptors on blood vessels and adrenal glands, preventing its vasoconstrictive and aldosterone-stimulating effects. They include losartan, valsartan, candesartan, irbesartan, and others with the suffix -sartan.
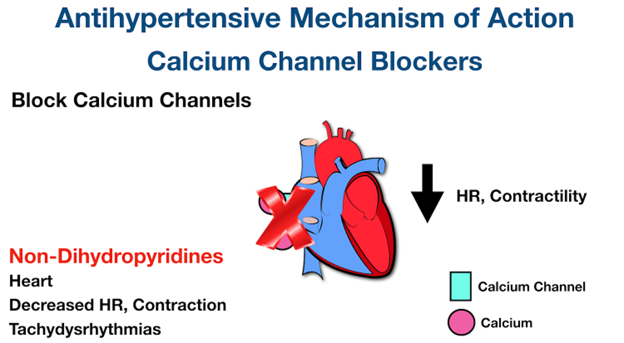
5. Calcium channel blockers: These drugs block the entry of calcium into cardiac and vascular smooth muscle cells, reducing their contractility and causing vasodilation. They include verapamil, diltiazem, nifedipine, amlodipine, felodipine, and others with the suffix -dipine.
-
- Diuretics: These drugs increase the excretion of water and sodium by the kidneys, reducing blood volume and blood pressure. They include thiazide diuretics (hydrochlorothiazide), loop diuretics (furosemide), potassium-sparing diuretics (spironolactone), osmotic diuretics (mannitol), and carbonic anhydrase inhibitors (acetazolamide).
- Direct renin inhibitors: These drugs inhibit renin, an enzyme that catalyzes the first step in the renin-angiotensin-aldosterone system (RAAS), which regulates blood pressure and fluid balance. They include aliskiren.
- The common side effects and nursing implications of antihypertensive drugs are summarized in the table below:
|
Category |
Common side effects |
Nursing implications |
|
Adrenergic drugs |
Hypotension, bradycardia, dizziness, fatigue, insomnia, edema |
Monitor vital signs and labs; do not abruptly stop beta blockers; teach patients to change positions slowly; avoid alcohol |
|
Direct acting vasodilators |
Hypotension, reflex tachycardia, headache, flushing |
Monitor vital signs; administer with beta blockers or diuretics to prevent reflex tachycardia; teach patients to report chest pain or palpitations |
|
ACE inhibitors |
Dry cough; hyperkalemia; angioedema; rash; hypotension |
Monitor vital signs; monitor potassium levels; teach patients to report swelling of face or throat; avoid salt substitutes |
|
ARBs |
Dizziness; headache; hypotension; hyperkalemia; angioedema |
Monitor vital signs; monitor potassium levels; teach patients to report swelling of face or throat; avoid salt substitutes |
|
Calcium channel blockers |
Hypotension; bradycardia; headache; flushing; edema |
Monitor vital signs; monitor for signs of heart failure; teach patients to report chest pain or dyspnea; avoid grapefruit juice |
|
Diuretics |
Hypotension; dehydration; electrolyte imbalance; polyuria |
Monitor vital signs; monitor fluid and electrolyte status; teach patients to weigh themselves daily and report weight gain or loss; teach patients to take diuretics in the morning |
|
Direct renin inhibitors |
Diarrhea; cough; angioedema; hyperkalemia |
Monitor vital signs; monitor potassium levels; teach patients to report swelling of face or throat |
Medications for angina
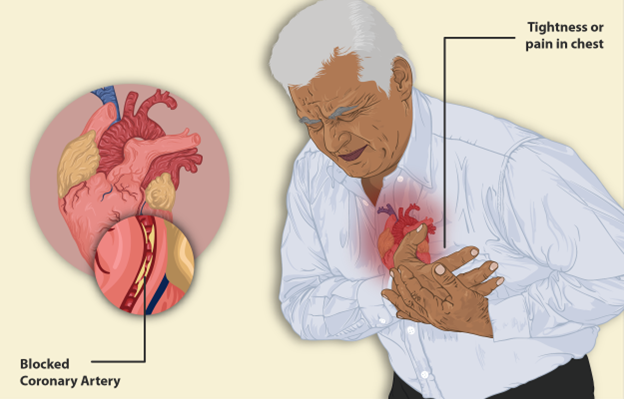
- Angina is a type of chest pain caused by reduced blood flow to the heart muscle, usually due to coronary artery disease
- Angina can be classified into stable angina, which occurs predictably with exertion or stress, and unstable angina, which occurs unpredictably and may indicate an impending myocardial infarction (MI)
- The medications used to treat angina are aimed at relieving the pain, improving blood flow, and preventing complications
- The main categories of drugs used for angina are:
- Nitrates: These drugs dilate the coronary arteries and peripheral veins, reducing the oxygen demand and increasing the oxygen supply to the heart. They include nitroglycerin, isosorbide dinitrate, and isosorbide mononitrate. They can be administered sublingually, orally, transdermally, or intravenously.
- Beta blockers: These drugs decrease the heart rate, contractility, and blood pressure, reducing the oxygen demand of the heart. They include propranolol, metoprolol, atenolol, and others with the suffix -olol. They are usually taken orally or intravenously.
- Calcium channel blockers: These drugs dilate the coronary arteries and peripheral arterioles, increasing the oxygen supply and reducing the oxygen demand of the heart. They include verapamil, diltiazem, nifedipine, amlodipine, and others with the suffix -dipine. They are usually taken orally or intravenously.
- Antiplatelet drugs: These drugs inhibit platelet aggregation and prevent thrombus formation in the coronary arteries. They include aspirin, clopidogrel, ticagrelor, and prasugrel. They are usually taken orally.
- Anticoagulant drugs: These drugs prevent clotting factors from forming clots in the blood vessels. They include heparin, enoxaparin, warfarin, dabigatran, rivaroxaban, and apixaban. They can be administered subcutaneously, intravenously, or orally.
- The common side effects and nursing implications of drugs for angina are summarized in the table below:
|
Category |
Common side effects |
Nursing implications |
|
Nitrates |
Headache; hypotension; reflex tachycardia; flushing |
Monitor vital signs; teach patients to sit or lie down when taking nitrates; teach patients to store nitrates in a dark container and replace them every 6 months; teach patients to take one nitroglycerin tablet sublingually every 5 minutes for up to three doses if angina occurs |
|
Beta blockers |
Hypotension; bradycardia; fatigue; dizziness; depression |
Monitor vital signs and labs; do not abruptly stop beta blockers; teach patients to change positions slowly; avoid alcohol |
|
Calcium channel blockers |
Hypotension; bradycardia; headache; flushing; edema |
Monitor vital signs; monitor for signs of heart failure; teach patients to report chest pain or dyspnea; avoid grapefruit juice |
|
Antiplatelet drugs |
Bleeding; bruising; gastrointestinal upset |
Monitor for signs of bleeding; teach patients to report any unusual bleeding or bruising; teach patients to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) and alcohol |
|
Anticoagulant drugs |
Bleeding; bruising; hematoma; anemia |
Monitor for signs of bleeding; monitor labs such as prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT); teach patients to report any unusual bleeding or bruising; teach patients to avoid foods high in vitamin K if taking warfarin |
Medications for arrhythmias
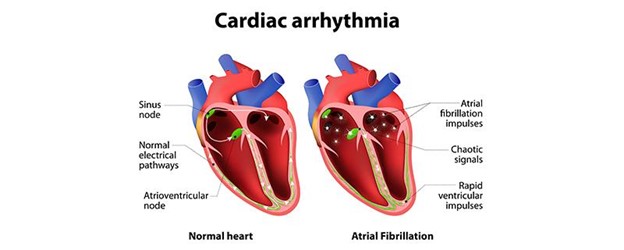
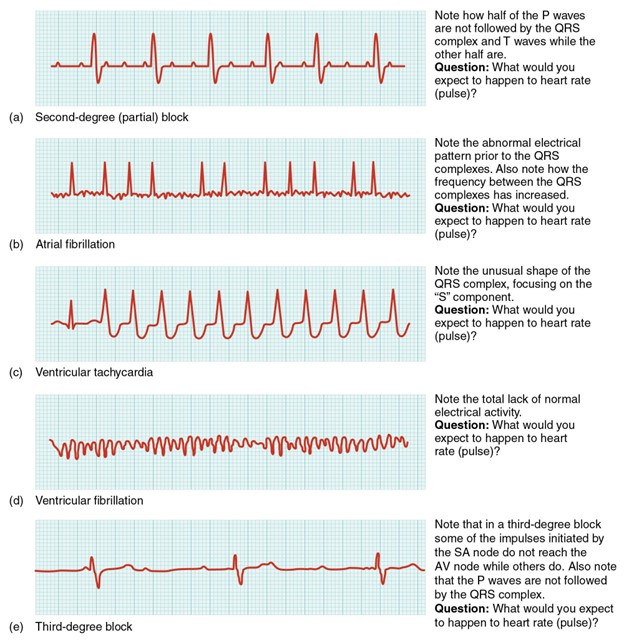
- Arrhythmias are abnormal heart rhythms that can affect the rate, regularity, or coordination of the cardiac cycle
- Arrhythmias can be classified into bradyarrhythmias, which are slow heart rhythms (<60 beats per minute), and tachyarrhythmias, which are fast heart rhythms (>100 beats per minute)
- Arrhythmias can also be classified by their origin, such as atrial, ventricular, or junctional
- The medications used to treat arrhythmias are aimed at restoring normal sinus rhythm, controlling the heart rate, and preventing complications such as stroke or cardiac arrest
- The main categories of drugs used for arrhythmias are:
- Sodium channel blockers: These drugs block the sodium channels in the cardiac cells, slowing down the conduction of electrical impulses and prolonging the refractory period. They include quinidine, procainamide, lidocaine, and flecainide. They are usually administered orally or intravenously.
- Beta blockers: These drugs decrease the heart rate, contractility, and conduction velocity by blocking the beta receptors in the cardiac cells. They include propranolol, metoprolol, atenolol, and others with the suffix -olol. They are usually taken orally or intravenously.
- Potassium channel blockers: These drugs block the potassium channels in the cardiac cells, prolonging the action potential and refractory period. They include amiodarone, sotalol, dofetilide, and ibutilide. They are usually administered orally or intravenously.
- Calcium channel blockers: These drugs block the calcium channels in the cardiac cells, slowing down the conduction velocity and reducing the automaticity. They include verapamil, diltiazem, and others with the suffix -dipine. They are usually taken orally or intravenously.
- Adenosine: This drug activates the adenosine receptors in the cardiac cells, slowing down the conduction velocity and reducing the automaticity. It is used to treat supraventricular tachycardia (SVT). It is administered intravenously as a rapid bolus injection.
- Digoxin: This drug inhibits the sodium-potassium ATPase pump in the cardiac cells, increasing the intracellular calcium and enhancing contractility. It also has a vagal effect that slows down the conduction velocity and reduces the automaticity. It is used to treat atrial fibrillation (AF) and heart failure. It is administered orally or intravenously.
- The common side effects and nursing implications of drugs for arrhythmias are summarized in the table below:
|
Category |
Common side effects |
Nursing implications |
|
Sodium channel blockers |
Hypotension; bradycardia; dizziness; nausea; vomiting; diarrhea; arrhythmias |
Monitor vital signs and electrocardiogram (ECG); monitor labs such as serum drug levels and liver function tests; teach patients to report any signs of toxicity such as blurred vision, tinnitus, or confusion |
|
Beta blockers |
Hypotension; bradycardia; fatigue; dizziness; depression |
Monitor vital signs and ECG; monitor labs such as serum drug levels and renal function tests; do not abruptly stop beta blockers; teach patients to change positions slowly; avoid alcohol |
|
Potassium channel blockers |
Hypotension; bradycardia; dizziness; nausea; vomiting; arrhythmias; pulmonary toxicity; thyroid dysfunction |
Monitor vital signs and ECG; monitor labs such as serum drug levels, thyroid function tests, and pulmonary function tests; teach patients to report any signs of toxicity such as dyspnea, cough, or weight gain |
|
Calcium channel blockers |
Hypotension; bradycardia; headache; flushing; edema |
Monitor vital signs and ECG; monitor for signs of heart failure; teach patients to report chest pain or dyspnea; avoid grapefruit juice |
|
Adenosine |
Flushing; chest pain; dyspnea; hypotension; bradycardia |
Monitor vital signs and ECG; administer as a rapid bolus injection followed by a saline flush; teach patients to expect transient side effects |
|
Digoxin |
Nausea; vomiting; anorexia; bradycardia; arrhythmias; visual disturbances |
Monitor vital signs and ECG; monitor labs such as serum digoxin levels and potassium levels; teach patients to report any signs of toxicity such as yellow-green halos, blurred vision, or confusion |
Medications for heart failure
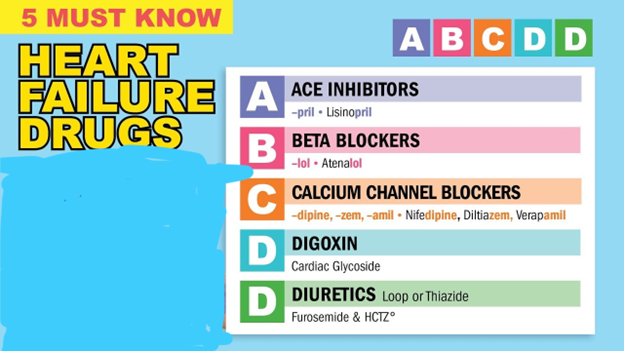
- Heart failure is a chronic condition characterized by the inability of the heart to pump enough blood to meet the body’s needs, resulting in fluid retention, edema, dyspnea, fatigue, and reduced exercise tolerance
- The medications used to treat heart failure are aimed at improving the cardiac function, reducing the preload and afterload, and preventing complications such as arrhythmias and thromboembolism
- The main categories of drugs used for heart failure are:
- Diuretics: These drugs increase the excretion of water and sodium by the kidneys, reducing the blood volume and the preload on the heart. They include thiazide diuretics (hydrochlorothiazide), loop diuretics (furosemide), potassium-sparing diuretics (spironolactone), osmotic diuretics (mannitol), and carbonic anhydrase inhibitors (acetazolamide).
- ACE inhibitors: These drugs inhibit the enzyme that converts angiotensin I to angiotensin II, a potent vasoconstrictor and stimulator of aldosterone secretion. They reduce the afterload on the heart by dilating the blood vessels and prevent the remodeling of the cardiac tissue by inhibiting the growth factors. They include captopril, enalapril, lisinopril, ramipril, and others with the suffix -pril.
- ARBs: These drugs block the binding of angiotensin II to its receptors on blood vessels and adrenal glands, preventing its vasoconstrictive and aldosterone-stimulating effects. They reduce the afterload on the heart by dilating the blood vessels and prevent the remodeling of the cardiac tissue by inhibiting the growth factors. They include losartan, valsartan, candesartan, irbesartan, and others with the suffix -sartan.
- Beta blockers: These drugs decrease the heart rate, contractility, and blood pressure by blocking the beta receptors in the cardiac cells. They reduce the oxygen demand of the heart and prevent the activation of the sympathetic nervous system, which can worsen heart failure. They include carvedilol, metoprolol, bisoprolol, and others with the suffix -olol.
- Digoxin: This drug inhibits the sodium-potassium ATPase pump in the cardiac cells, increasing the intracellular calcium and enhancing the contractility. It also has a vagal effect that slows down the conduction velocity and reduces
- Digoxin: This drug inhibits the sodium-potassium ATPase pump in the cardiac cells, increasing the intracellular calcium and enhancing the contractility. It also has a vagal effect that slows down the conduction velocity and reduces the automaticity. It is used to treat atrial fibrillation and heart failure. It is administered orally or intravenously.
- Vasodilators: These drugs dilate the blood vessels, reducing the preload and afterload on the heart. They include nitroglycerin, hydralazine, isosorbide dinitrate, and nitroprusside. They can be administered sublingually, orally, transdermally, or intravenously.
- Inotropic agents: These drugs increase the force of contraction of the heart muscle, improving the cardiac output and tissue perfusion. They include dobutamine, dopamine, and milrinone. They are administered intravenously.
- Anticoagulant and antiplatelet drugs: These drugs prevent clotting factors from forming clots in the blood vessels and inhibit platelet aggregation, reducing the risk of thromboembolism in patients with heart failure. They include heparin, enoxaparin, warfarin, dabigatran, rivaroxaban, apixaban, aspirin, clopidogrel, ticagrelor, and prasugrel. They can be administered subcutaneously, intravenously, or orally.
- The common side effects and nursing implications of drugs for heart failure are summarized in the table below:
|
Category |
Common side effects |
Nursing implications |
|
Diuretics |
Hypotension; dehydration; electrolyte imbalance; polyuria |
Monitor vital signs; monitor fluid and electrolyte status; teach patients to weigh themselves daily and report weight gain or loss; teach patients to take diuretics in the morning |
|
ACE inhibitors |
Dry cough; hyperkalemia; angioedema; rash; hypotension |
Monitor vital signs; monitor potassium levels; teach patients to report swelling of face or throat; avoid salt substitutes |
|
ARBs |
Dizziness; headache; hypotension; hyperkalemia; angioedema |
Monitor vital signs; monitor potassium levels; teach patients to report swelling of face or throat; avoid salt substitutes |
|
Beta blockers |
Hypotension; bradycardia; fatigue; dizziness; depression |
Monitor vital signs and labs; do not abruptly stop beta blockers; teach patients to change positions slowly; avoid alcohol |
|
Digoxin |
Nausea; vomiting; anorexia; bradycardia; arrhythmias; visual disturbances |
Monitor vital signs and ECG; monitor labs such as serum digoxin levels and potassium levels; teach patients to report any signs of toxicity such as yellow-green halos, blurred vision, or confusion |
|
Vasodilators |
Hypotension; reflex tachycardia; headache; flushing |
Monitor vital signs; administer with beta blockers or diuretics to prevent reflex tachycardia; teach patients to report chest pain or palpitations |
|
Inotropic agents |
Hypotension; tachycardia; arrhythmias; chest pain |
Monitor vital signs and ECG; monitor labs such as serum drug levels and renal function tests; teach patients to report any signs of chest pain or palpitations |
|
Anticoagulant and antiplatelet drugs |
Bleeding; bruising; hematoma; anemia |
Monitor for signs of bleeding; monitor labs such as prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT); teach patients to report any unusual bleeding or bruising; teach patients to avoid foods high in vitamin K if taking warfarin |
Summary
- Antihypertensive drugs lower blood pressure by acting on adrenergic receptors, direct vasodilators, ACE inhibitors, ARBs, calcium channel blockers, diuretics, or direct renin inhibitors
- Drugs for angina relieve chest pain by acting on nitrates, beta blockers, calcium channel blockers, antiplatelet drugs, or anticoagulant drugs
- Drugs for arrhythmias restore normal heart rhythm by acting on sodium channel blockers, beta blockers, potassium channel blockers, calcium channel blockers, adenosine, or digoxin
- Drugs for heart failure improve cardiac function by acting on diuretics, ACE inhibitors, ARBs, beta blockers, digoxin, vasodilators, inotropic agents, or anticoagulant and antiplatelet drugs
Conclusion
- Antihypertensive and cardiovascular medications are drugs that treat various disorders of the heart and blood vessels, such as hypertension, angina, arrhythmias, and heart failure
- These drugs act on different targets in the cardiovascular system, such as receptors, enzymes, hormones, or ion channels, to modify the blood pressure, blood flow, cardiac function, and clotting process
- These drugs have various side effects and nursing implications that require careful monitoring and patient education
- The choice of medication depends on the type and severity of the condition, the patient’s characteristics and preferences, and the potential benefits and risks of each drug
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Antihypertensives and Cardiovascular Medications
This filled cannot be empty

