Please set your exam date
Umbilical cord prolapse
Study Questions
Introduction
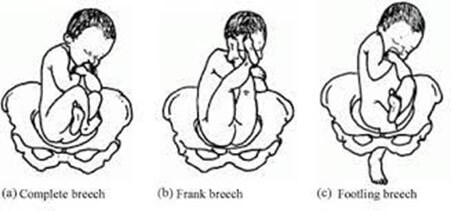
A nurse is caring for a client who is in labor and has a breech presentation.
The nurse knows that this client is at increased risk for which complication?
Explanation
The correct answer is choice B. Cord prolapse.
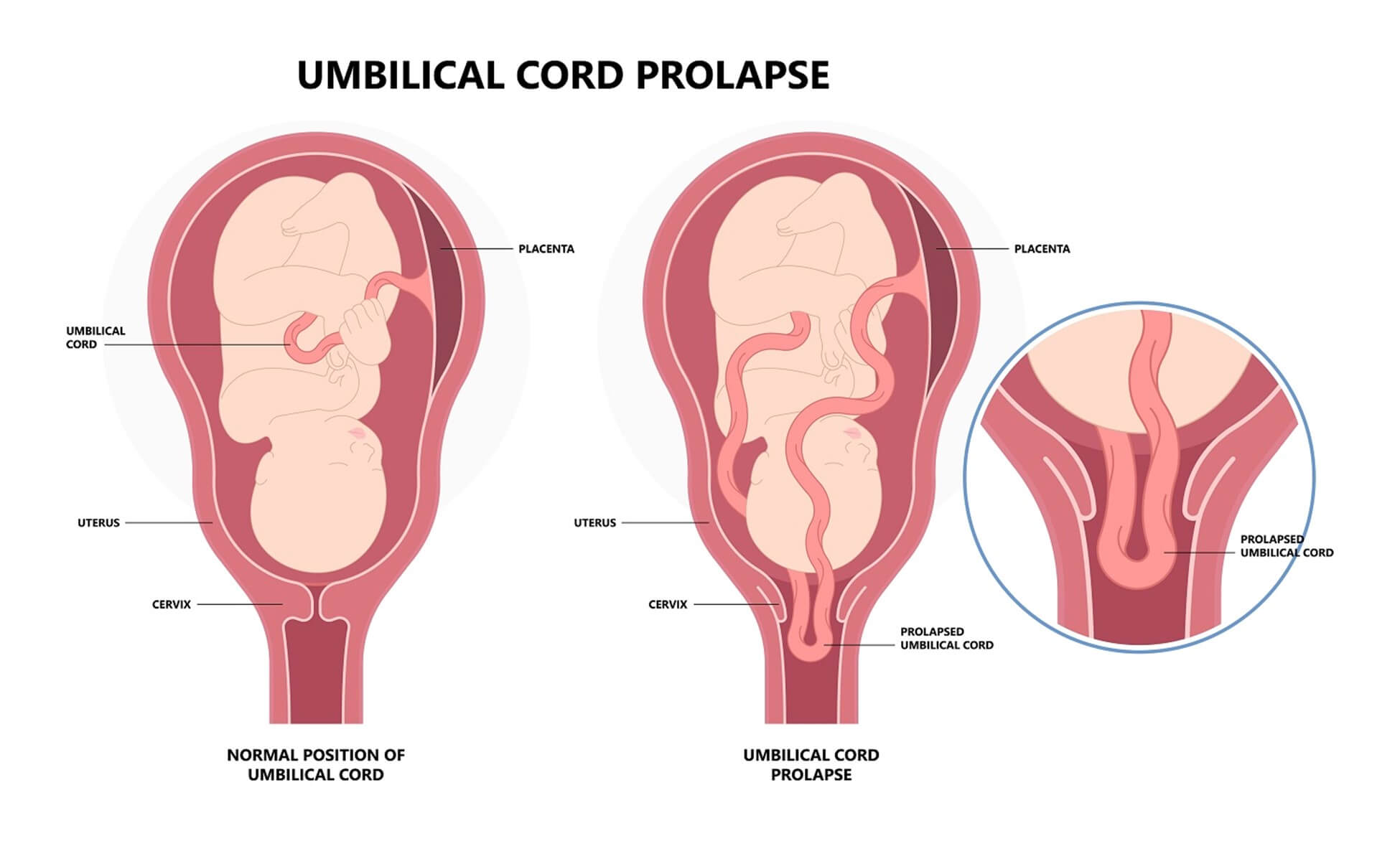
A cord prolapse occurs when the umbilical cord slips through the cervix and into the vagina before the baby during labor.
This can cause the cord to become compressed or twisted, cutting off the blood supply and oxygen to the baby.A cord prolapse is a medical emergency that requires immediate delivery by cesarean section.
Choice A is wrong because placenta previa is a condition where the placenta covers the opening of the cervix, not the baby’s position.Placenta previa can cause bleeding during pregnancy and labor, but it is not directly related to breech presentation.
Choice C is wrong because shoulder dystocia is a complication where the baby’s shoulder gets stuck behind the mother’s pubic bone during a head-first delivery.
This can cause injury to the baby’s nerves, bones, or brain.Shoulder dystocia is not a common complication of breech delivery.
Choice D is wrong because postpartum hemorrhage is excessive bleeding after delivery.
It can be caused by many factors, such as uterine atony, retained placenta, or lacerations.Postpartum hemorrhage is not more likely to occur with breech presentation than with vertex presentation.
Breech presentation can also increase the risk of other complications, such as congenital malformations, developmental dysplasia of the hip, and traumatic injuries.
Therefore, most breech babies are delivered by cesarean section to reduce
A nurse is monitoring the fetal heart rate of a client who has ruptured membranes.
The nurse notices severe variable decelerations on the monitor.
What is the most likely cause of this finding?
Explanation
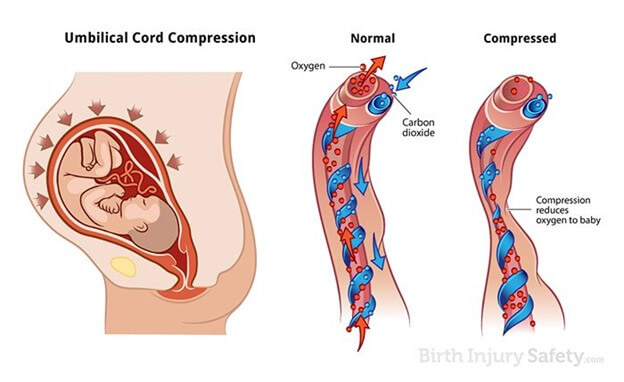
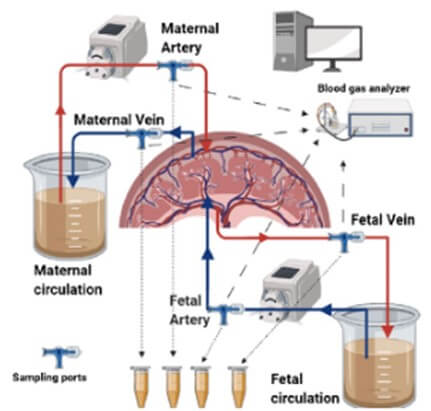
The correct answer is choice C. Umbilical cord compression.Variable decelerations are abrupt drops in the fetal heart rate below baseline that last 15 seconds to less than two minutes.They are caused by reduced blood flow and oxygen delivery to the fetus due to umbilical cord compression.The onset, depth, and duration of variable decelerations vary with uterine contractions or fetal movement.They can be periodic or episodic.
Choice A is wrong because fetal head compression causes early decelerations, which are symmetrical decreases and return-to-normal of the fetal heart rate that is linked to uterine contractions.Early decelerations are benign and do not affect fetal oxygenation.
Choice B is wrong because uteroplacental insufficiency causes late decelerations, which are gradual decreases in fetal heart rate after a uterine contraction.Late decelerations may indicate that a fetus has high levels of acid in the blood (a condition called impending fetal academia), which is often caused by a lack of oxygen.
Choice D is wrong because maternal hypotension can cause late decelerations, not variable decelerations.Maternal hypotension can reduce the blood flow to the placenta and affect fetal oxygenation.
A nurse is preparing a client for an emergency cesarean delivery due to cord prolapse.
What should the nurse do to relieve cord compression until the delivery?
Explanation
The correct answer is choice D. All of the above.
The nurse should do all of the following to relieve cord compression until the delivery:
• Apply gentle pressure to the presenting part with a sterile gloved hand.
This helps to lift the fetal head off the cord and restore blood flow.
• Elevate the client’s hips with pillows or a wedge.
This reduces the gravitational force on the cord and prevents further descent.
• Administer oxygen via facemask at 10 L/min.
This increases oxygen delivery to the fetus and reduces hypoxia.
A nurse is teaching a group of nursing students about cord prolapse.
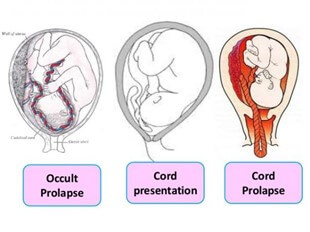
The nurse explains that cord prolapse can be classified into three types: overt, occult, and funis.
What is the difference between these types?
Explanation
The correct answer is choice A.Overt cord prolapse is when the cord is visible or palpable in the vagina, occult cord prolapse is when the cord is hidden within the uterus, and funis cord prolapse is when the cord is alongside but not below the presenting part.
Choice B is wrong because it reverses the definitions of overt and occult cord prolapse.
Choice C is wrong because it reverses the definitions of overt and funis cord prolapse.
Choice D is wrong because it does not match any of the definitions of cord prolapse types.
Normal ranges for umbilical cord length are 45 to 60 cm, and normal ranges for umbilical cord diameter are 1 to 2 cm.
A nurse is reviewing the risk factors for cord prolapse with a pregnant client who has polyhydramnios.
The nurse should inform the client that polyhydramnios increases the risk of cord prolapse by which mechanism?
Explanation
The correct answer is choice B. It creates more space for the cord to slip past the presenting part.Polyhydramnios is a condition where there is excessive accumulation of amniotic fluid during pregnancy.This can cause the fetus to be malpositioned or not engaged in the pelvis before labor, which increases the risk of cord prolapse.Cord prolapse is when the umbilical cord drops into the vagina ahead of the baby, which can compromise blood flow and oxygen delivery to the fetus.
Choice A is wrong because it is not the fetal movement that causes cord prolapse, but the displacement of the presenting part from the cervix.
Choice C is wrong because it is not the pressure on the membranes that causes cord prolapse, but the rupture of the membranes with a high or mobile presenting part.
Choice D is wrong because it is not the reduced cushioning effect of the amniotic fluid that causes cord prolapse, but the increased space for the cord to slip past the presenting part.
Risk factors and causes
A nurse is reviewing the risk factors for cord prolapse with a group of nursing students.
Which of the following statements by a student indicates an understanding of the teaching?
Explanation
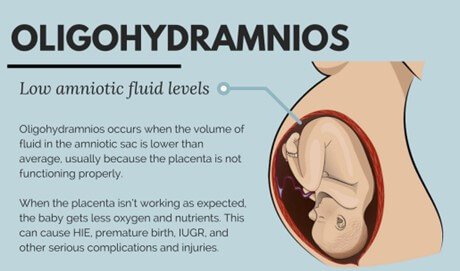
The correct answer is choice C. Cord prolapse is more likely to occur in clients who have oligohydramnios.
Oligohydramnios is a condition where there is too little amniotic fluid around the fetus.This can cause the umbilical cord to slip down into the cervix and vagina ahead of the baby during delivery.This can cut off the blood and oxygen supply to the baby and cause fetal distress.
Choice A is wrong because cord prolapse is more likely to occur in clients who have aplacenta previa, not a low-lying placenta.
Placenta previa is a condition where the placenta covers the cervix partially or completely.This can prevent the baby from descending into the pelvis and leave more space for the cord to prolapse.
Choice B is wrong because cord prolapse is more likely to occur in clients who have anon-vertex presentation, such as breech or transverse lie, not a vertex presentation.
A non-vertex presentation means that the baby’s head is not pointing down towards the birth canal.This can result in a smaller or irregularly shaped presenting part that does not fit snugly into the pelvis and allows the cord to slip past it.
Choice D is wrong because cord prolapse is more likely to occur in clients who have amultiple pregnancy, not a singleton
A nurse is assisting with the delivery of a client who has a breech presentation.
The nurse notices that the umbilical cord is protruding from the vagina.
Which of the following actions should the nurse take first?
Explanation
The correct answer is choice A. Apply pressure to the presenting part with gloved fingers.This is because applying pressure can prevent further compression of the umbilical cord and reduce the risk of fetal hypoxia (lack of oxygen).The umbilical cord can be flattened or twisted during delivery, which can cause nerve or brain damage.
Choice B is wrong because placing the client in Trendelenburg position (head down and feet up) may not be enough to relieve the cord compression and may cause discomfort or respiratory distress for the client.
Choice C is wrong because administering oxygen may not improve the fetal oxygenation if the cord is severely compressed.
Oxygen administration may also delay the urgent delivery of the baby.
Choice D is wrong because clamping and cutting the umbilical cord will cut off the fetal blood supply and oxygenation.
This can lead to fetal death or severe brain injury.
Normal ranges for umbilical cord pH are 7.18 to 7.38 for arterial blood and 7.28 to 7.45 for venous blood.
A nurse is monitoring the fetal heart rate of a client who has a suspected occult cord prolapse.
Which of the following findings should the nurse expect?
Explanation
The correct answer is choice D. Severe variable decelerations.
This is because occult cord prolapse occurs when the cord is compressed by the fetal presenting part, causing fetal hypoxemia.The fetal heart rate pattern may show severe bradycardia or severe variable decelerations, which indicate cord compression and fetal distress.
Choice A is wrong because episodic accelerations are normal and indicate fetal well-being.They are not associated with cord prolapse.
Choice B is wrong because fibrillation is a cardiac arrhythmia that affects the atria or ventricles of the heart.It is not a term used to describe fetal heart rate patterns.
Choice C is wrong because moderate tachycardia is a fetal heart rate above 160 beats per minute for more than 10 minutes.
It can be caused by maternal fever, infection, dehydration, fetal anemia, or fetal hypoxia.It is not a specific sign of cord prolapse.
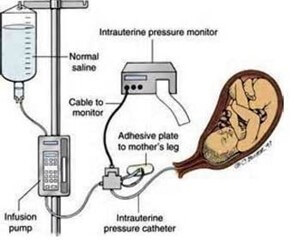
A nurse is preparing to perform an amnioinfusion for a client who has oligohydramnios and a cord compression.
Which of the following are appropriate steps for this procedure? (Select all that apply.)
Explanation
The correct answer is choice A, B, C and E. Here is why:
• Choice A is correct because informed consent is required before performing any invasive procedure, such as amnioinfusion.
• Choice B is correct because an intrauterine pressure catheter (IUPC) is needed to infuse fluid into the amniotic cavity and to monitor the uterine contractions.
• Choice C is correct because warmed sterile normal saline is the fluid of choice for amnioinfusion, as it mimics the natural amniotic fluid and reduces the risk of infection.
• Choice D is wrong because the client’s temperature should be monitored every 15 to 30 minutes, not every 4 hours, to detect any signs of infection or chorioamnionitis.
• Choice E is correct because the fetal heart rate and uterine activity should be assessed continuously to evaluate the fetal well-being and the effectiveness of amnioinfusion.
Amnioinfusion is a procedure that involves infusing fluid into the amniotic cavity to increase the amniotic fluid volume and to relieve umbilical cord compression.It can be used for clients who have oligohydramnios (low amniotic fluid) and cord compression, which can cause fetal growth restriction and abnormal fetal heart rate patterns.Amnioinfusion can improve the fetal blood flow and oxygenation by reducing the cord compression and variable decelerations.
Signs and symptoms
A nurse is caring for a client who is in labor and has a prolapsed umbilical cord.
Which of the following actions should the nurse take first?
Explanation
The correct answer is d. Call for assistance and prepare for an emergency cesarean delivery.
Rationale for Choice d:
- Emergency cesarean delivery is the definitive treatment for a prolapsed umbilical cord.It's crucial to expedite delivery to prevent fetal hypoxia and potential death.
- Any delay in delivery can have catastrophic consequences for the fetus.
- Calling for assistance immediately activates the necessary personnel and resources for a swift cesarean delivery.
- Prompt preparation ensures the operating room, anesthesia team, and surgical team are ready to proceed without delay.
Rationale for Choice a:
- Applying warm saline-soaked gauze to the exposed cord is a temporary measure to prevent cord compression and drying.
- It does not address the underlying issue of cord compression and compromised blood flow to the fetus.
- While this action is important, it should not take precedence over calling for assistance and preparing for emergency delivery.
Rationale for Choice b:
- Placing the client in Trendelenburg position (head down, feet up) was once thought to relieve pressure on the cord.
- However, current evidence does not support this practice.
- It can potentially worsen fetal distress by increasing venous return and cardiac output, leading to increased cord compression.
- It can also make it more difficult to monitor the fetal heart rate and perform a cesarean delivery.
Rationale for Choice c:
- Administering oxygen via face mask at 10 L/min may provide some benefit to the fetus by increasing maternal oxygen saturation.
- However, it does not address the primary issue of cord compression and compromised fetal blood flow.
- It should not be prioritized over calling for assistance and preparing for emergency delivery.
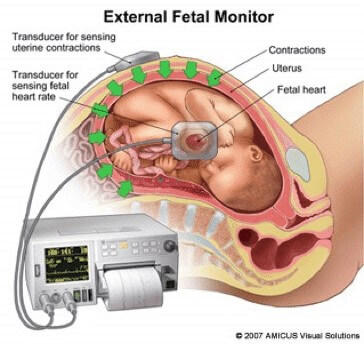
A nurse is reviewing the electronic fetal monitor (EFM) tracing of a client who is in labor and has ruptured membranes.
Which of the following findings should alert the nurse to the possibility of a cord prolapse?
Explanation
The correct answer is choice C. FHR of 80/min with severe variable decelerations.This indicates that the umbilical cord is prolapsed and compressed by the baby’s body, causing a decrease in blood and oxygen supply to the baby.A normal fetal heart rate is between 120 and 160 beats per minute.Severe variable decelerations are abrupt drops in the fetal heart rate that do not correspond to contractions.
Choice A is wrong because FHR of 160/min with accelerations is a normal finding that indicates a healthy baby.Accelerations are temporary increases in the fetal heart rate that usually occur with fetal movement or contractions.
Choice B is wrong because FHR of 120/min with early decelerations is also a normal finding that indicates a well-oxygenated baby.Early decelerations are gradual decreases in the fetal heart rate that mirror contractions and are caused by head compression.
Choice D is wrong because FHR of 140/min with late decelerations is an abnormal finding that indicates uteroplacental insufficiency, not cord prolapse.Late decelerations are gradual decreases in the fetal heart rate that occur after contractions and are caused by reduced blood flow to the placenta.
A nurse is teaching a group of pregnant clients about the risk factors for umbilical cord prolapse.
Which of the following factors should the nurse include? (Select all that apply.)
Explanation
The correct answer is choices A, B, C and E.These are all risk factors for umbilical cord prolapse, which is a complication that occurs when the umbilical cord drops through the cervix and into the vagina ahead of the baby during delivery.This can cause fetal hypoxia and distress by compressing the cord and reducing blood flow to the baby.
Choice A is correct because polyhydramnios, or excessive amniotic fluid around the fetus, can cause the cord to slip out when the membranes rupture.
Choice B is correct because breech presentation, or abnormal positioning of the baby, can make it easier for the cord to slip between and past the fetal feet and into the pelvis.
Choice C is correct because premature rupture of membranes, or breaking of the water before labor begins, can cause the cord to prolapse if the baby’s head is not well engaged in the pelvis.
Choice D is wrong because post-term pregnancy, or pregnancy that lasts longer than 42 weeks, is not a risk factor for umbilical cord prolapse.However, it can increase the risk of other complications such as fetal macrosomia, placental insufficiency and meconium aspiration.
Choice E is correct because multiple gestation, or having more than one baby in the uterus, can cause unstable lie, or frequent changes in the position of the baby.This can increase the risk of cord prolapse if the membranes rupture when the baby is not in a cephalic (head-down) position.
A nurse is performing a vaginal examination on a client who is in labor and has a prolapsed umbilical cord.
Which of the following actions should the nurse take to relieve cord compression?
Explanation
The correct answer is choice A. Push the presenting part upward with gloved fingers.This action can relieve cord compression and improve fetal oxygenation until an emergency cesarean section can be performed.
Choice B is wrong because pulling the cord gently to reduce tension can cause more damage to the umbilical vessels and increase the risk of fetal hemorrhage.
Choice C is wrong because clamping the cord with sterile forceps can cut off the blood supply to the fetus and cause fetal death.
Choice D is wrong because cutting the cord and tying it with sterile string can also cut off the blood supply to the fetus and cause fetal death.
Some additional information:
• A prolapsed umbilical cord is a rare but life-threatening obstetric emergency that occurs when the umbilical cord is abnormally positioned between the fetal presenting part and the cervix.
• The normal range of umbilical cord length is 40 to 60 cm.A longer cord can increase the risk of prolapse.
• The normal range of fetal heart rate is 110 to 160 beats per minute.A prolapsed cord can cause fetal bradycardia (slow heart rate) due to hypoxia.
A nurse is preparing a client who has a prolapsed umbilical cord for an emergency cesarean delivery.
Which of the following medications should the nurse anticipate administering to the client?
Explanation
Terbutaline is a medication that can relax the uterine muscles and reduce contractions.This can help relieve pressure on the prolapsed umbilical cord and restore blood flow to the baby while preparing for an emergency cesarean delivery.
Choice A is wrong because magnesium sulfate is used to prevent seizures in women with preeclampsia or eclampsia, not to treat umbilical cord prolapse.
Choice C is wrong because oxytocin is used to induce or augment labor, not to stop it.Oxytocin can increase contractions and worsen cord compression.
Choice D is wrong because methylergonovine is used to prevent or treat postpartum hemorrhage, not to treat umbilical cord prolapse.Methylergonovine can also increase contractions and worsen cord compression.

Nursing interventions and management
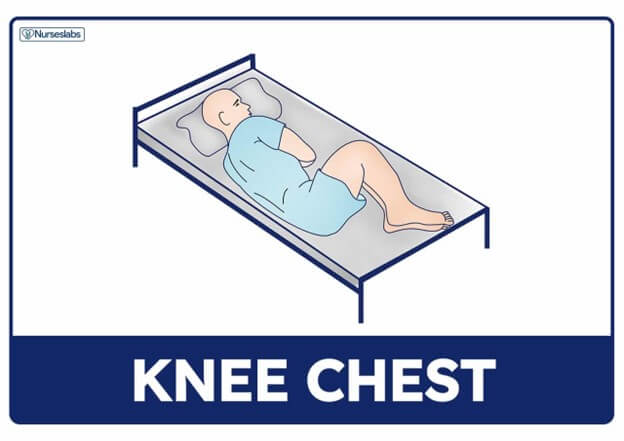
A nurse is caring for a client who is in labor and has a prolapsed umbilical cord.
Which of the following actions should the nurse take first?
Explanation
The correct answer is choice D. Reposition the client to a knee-chest position.This is because this position can reduce the pressure of the fetal presenting part on the prolapsed cord and improve fetal oxygenation.The nurse should also call for assistance and notify the provider, administer oxygen at 8 to 10 L/min via a face mask, and apply a warm, sterile, saline-soaked towel to the visible cord, but these are not the first actions to take.
Choice A is wrong because applying a warm, sterile, saline-soaked towel to the visible cord is not the first action to take.This intervention can prevent drying and atrophy of the umbilical vessels, but it does not relieve cord compression.
Choice B is wrong because administering oxygen at 8 to 10 L/min via a face mask is not the first action to take.This intervention can increase fetal oxygenation, but it does not relieve cord compression.
Choice C is wrong because calling for assistance and notifying the provider is not the first action to take.This intervention is necessary to prepare for emergency delivery, but it does not relieve cord compression.
A nurse is reviewing the risk factors for umbilical cord prolapse with a group of nursing students.
Which of the following factors should the nurse include? (Select all that apply.).
Explanation
The correct answer is choice A, B and E. Umbilical cord prolapse is a complication that occurs when the umbilical cord descends through the cervix before or with the presenting part of the fetus.
This can cause fetal hypoxia due to occlusion or vasospasm of the cord.
The risk factors for cord prolapse include:
• Premature rupture of membranes(choice A): This can cause the cord to slip past the fetal head or limbs when the amniotic fluid gushes out.
• Breech presentation(choice B): This is when the fetus is positioned with its feet or buttocks first.In a footling breech, the cord can easily slip between and past the fetal feet and into the pelvis.
• Cephalopelvic disproportion(choice C): This is when the fetal head is too large to fit through the maternal pelvis.This is not a risk factor for cord prolapse, as the fetal head usually prevents the cord from descending.
• Gestational diabetes(choice D): This is a condition where the mother has high blood sugar levels during pregnancy.This can cause macrosomia (large baby), but this is not a direct risk factor for cord prolapse.
• Hydramnios(choice E): This is a condition where there is excessive amniotic fluid around the fetus.This can create more space for the cord to move and prolapse, especially if there is a sudden loss of fluid.
Normal ranges for amniotic fluid index
A nurse is monitoring a client who is in labor and has meconium-stained amniotic fluid.
The nurse should identify that this finding can indicate which of the following conditions?
Explanation
The correct answer is choice A. Fetal hypoxia.Meconium-stained amniotic fluid is often caused by fetal hypoxia or other physiologic stress.Any reflexive “gasping” of the unborn fetus, due to hypoxia, can depress the fetal diaphragm mechanically, squeezing the contents of the bowels into the amniotic fluid.Meconium is a sign of fetal distress, either on-going or old.
Choice B. Fetal infection is wrong because meconium-stained amniotic fluid is not a direct indicator of fetal infection.However, fetal infection can cause fetal hypoxia and distress, which can lead to meconium passage.
Choice C. Fetal maturity is wrong because meconium-stained amniotic fluid is not a sign of fetal maturity.It is more common in full-term or post-term babies, but it can also occur in preterm babies.
Choice D. Fetal distress is wrong because it is too vague and nonspecific.Fetal distress can have many causes and manifestations, such as abnormal heart rate patterns, reduced fetal movements, or acidosis.
Meconium-stained amniotic fluid is one possible sign of fetal distress, but not the only one.

A nurse is performing a vaginal examination on a client who is in labor and notices a loop of umbilical cord protruding from the vagina.
Which of the following actions should the nurse take to relieve pressure on the cord?
Explanation
The correct answer is choice B. Place two fingers on either side of the cord and lift the fetal head off of it.
This action can relieve pressure on the cord and prevent fetal hypoxia until delivery can take place.
Choice A is wrong because pushing the cord back into the vagina can cause more damage to the cord and increase the risk of infection.
Choice C is wrong because clamping and cutting the cord will cut off the fetal blood supply and result in fetal death.
Choice D is wrong because pulling gently on the cord can cause cord avulsion or rupture of the uterus, both of which are life-threatening complications.
Normal ranges for umbilical cord pH are 7.18 to 7.38 and for umbilical cord base excess are -8 to +2 mmol/L.
: Cord Prolapse Nursing Management - RNpedia
Complications and outcomes
A nurse is caring for a client who is in labor and has a prolapsed umbilical cord.
Which of the following actions should the nurse take first?
Explanation
The correct answer is choice B. Place the client in a knee-chest position.This is because this position can reduce the pressure of the fetal presenting part on the prolapsed cord and improve fetal oxygenation.The nurse should also notify the provider and prepare for an emergency cesarean delivery, but this is not the first action to take.
Choice A is wrong because applying warm saline-soaked gauze to the exposed cord can prevent drying and atrophy of the cord, but it does not relieve cord compression.
Choice C is wrong because administering oxygen via face mask at 10 L/min can increase maternal oxygen saturation and fetal oxygen delivery, but it does not address the cause of cord prolapse.
Choice D is wrong because notifying the provider and preparing for an emergency cesarean delivery is a necessary action, but it is not the first priority.The nurse should first try to relieve cord compression by placing the client in a knee-chest position.
A nurse is reviewing the electronic fetal monitor tracing of a client who has a prolapsed umbilical cord.
Which of the following fetal heart rate patterns indicates cord compression and hypoxemia?
Explanation
The correct answer is choice D.Severe variable decelerations indicate cord compression and hypoxemia in a fetus with a prolapsed umbilical cord.Variable decelerations are abrupt decreases in fetal heart rate below the baseline, usually associated with uterine contractions.Severe variable decelerations are defined as having a nadir of less than 70 beats per minute or lasting longer than 60 seconds.
Choice A is wrong because episodic accelerations are transient increases in fetal heart rate above the baseline, usually indicating fetal well-being.
Choice B is wrong because fibrillation is an irregular and rapid contraction of the atria of the heart, which is not a normal fetal heart rate pattern.
Choice C is wrong because moderate tachycardia is a slightly elevated fetal heart rate above the normal range of 110 to 160 beats per minute, which may be caused by maternal fever, fetal infection, fetal anemia, or fetal hypoxia.
However, moderate tachycardia alone does not indicate cord compression and hypoxemia.
The normal range of fetal heart rate is 110 to 160 beats per minute.
A nurse is teaching a group of pregnant clients about the risk factors for umbilical cord prolapse.
Which of the following factors should the nurse include? (Select all that apply.)
Explanation
The correct answer is choices A, B and C. These are the risk factors for umbilical cord prolapse that the nurse should include in the teaching.Umbilical cord prolapse is where the umbilical cord descends through the cervix, with (or before) the presenting part of the fetus.It can cause fetal hypoxia and distress by occluding or compressing the blood flow to the fetus.
Choice A is correct because premature rupture of membranes, especially when the presenting part of the fetus is high in the pelvis, can allow the cord to slip down into the cervix and vagina.
Choice B is correct because breech presentation, such as a footling breech, can make it easy for the cord to slip between and past the fetal feet and into the pelvis.
Choice C is correct because polyhydramnios, or excessive amniotic fluid around the fetus, can create more space for the cord to move and prolapse.
Choice D is wrong because post-term pregnancy is not a risk factor for umbilical cord prolapse.Post-term pregnancy can cause other complications such as fetal macrosomia, placental insufficiency and meconium aspiration.
Choice E is wrong because multiple gestation is not a risk factor for umbilical cord prolapse.Multiple gestation can cause other complications such as preterm labor, preeclampsia and fetal growth restriction.
A nurse is assisting with the delivery of a client who has a prolapsed umbilical cord.
Which of the following interventions should the nurse perform to relieve cord compression until delivery?
Explanation
The correct answer is choice A. Elevate the presenting part with a sterile gloved hand.This intervention helps to relieve cord compression until delivery by preventing the fetus from pushing down on the cord.The umbilical cord is the lifeline of the fetus and any compression can cause fetal hypoxemia and distress.
Choice B is wrong because pushing the cord back into the vagina with gentle pressure can cause more damage to the cord and increase the risk of infection.
Choice C is wrong because clamping and cutting the cord as quickly as possible will cut off the fetal blood supply and oxygenation.
Choice D is wrong because wrapping the cord loosely around the fetal neck can cause strangulation and compromise fetal circulation.
A nurse is assessing a newborn who was delivered after a prolonged umbilical cord prolapse.
Which of the following findings should alert the nurse to possible neurological damage?
Explanation
The correct answer is choice A. Hypotonia.Hypotonia is a condition of low muscle tone and weakness that can indicate neurological damage due to lack of oxygen and blood flow to the brain.Umbilical cord prolapse is a rare but serious complication that occurs when the umbilical cord drops out of the cervix before the baby during delivery, which can compress the cord and reduce or stop the oxygen and nutrient supply to the baby.This can result in brain damage, cerebral palsy, or fetal death.
Choice B. Jaundice is wrong because jaundice is a common condition in newborns that causes yellowing of the skin and eyes due to high levels of bilirubin in the blood.
It is usually not a sign of neurological damage, but rather a result of immature liver function or increased breakdown of red blood cells.
Choice C. Tachypnea is wrong because tachypnea is a condition of rapid breathing that can indicate respiratory distress or infection in newborns.
It is not a specific sign of neurological damage, but rather a sign of inadequate oxygenation or ventilation.
Choice D. Petechiae is wrong because petechiae are small red or purple spots on the skin caused by bleeding under the skin.
They can occur in newborns due to trauma during delivery, low platelet count, infection, or clotting disorders.
They are not a sign of neurological damage, but rather a sign of bleeding or inflammation.
More questions on this topic
A patient’s umbilical cord prolapses during labor.
The nurse should place her in which position? (Select all that apply.).
Explanation
The correct answer is choice A and B. The nurse should place the patient in knee-chest or Trendelenburg position to relieve the pressure of the fetal presenting part on the prolapsed cord and improve fetal oxygenation.These positions also allow gravity to help keep the cord in the uterus and prevent further descent.
Choice C is wrong because supine position can worsen cord compression and compromise fetal blood flow.Choice D is wrong because lithotomy position can also increase cord descent and reduce fetal perfusion.Choice E is wrong because Sims position can cause cord prolapse if the membranes are intact or rupture spontaneously.
Normal ranges for fetal heart rate are 110 to 160 beats per minute.Cord prolapse can cause fetal bradycardia with decelerations during contractions due to cord compression.
This is a sign of fetal distress and requires immediate intervention.
The nurse suspects umbilical cord prolapse in a patient whose membranes have just ruptured because she notes which assessment finding?
Explanation
The correct answer is choice D. A loop of umbilical cord protruding from her vagina.This is a sign of umbilical cord prolapse, which is a medical emergency that occurs when the cord slips past the fetal presenting part and becomes compressed, reducing blood flow and oxygen to the fetus.The nurse should immediately call for help, place the woman in a knee-chest or Trendelenburg position, insert two fingers into the vagina and lift the presenting part off the cord, cover the cord with sterile saline-soaked gauze, administer oxygen, and prepare for an emergency cesarean delivery.
Choice A is wrong because a sudden increase in fetal heart rate variability is not a specific sign of cord prolapse.It may indicate fetal well-being or distress depending on the pattern and duration of the variability.
Choice B is wrong because a large amount of clear amniotic fluid is not a sign of cord prolapse.It may indicate rupture of membranes, which is a risk factor for cord prolapse if the presenting part is not engaged.
Choice C is wrong because a change in fetal heart rate from 140 to 90 bpm is not a sign of cord prolapse.It may indicate fetal bradycardia, which can have many causes such as hypoxia, acidosis, medication effects, or fetal sleep cycle.
The nurse recognizes that which fetal presentation increases a patient’s risk for umbilical cord prolapse? (Select all that apply).
Explanation
The correct answer is choice B, C, D and E.These are all fetal presentations that increase a patient’s risk for umbilical cord prolapse.Umbilical cord prolapse is when the umbilical cord comes out of the uterus with or before the presenting part of the baby.This can cause fetal hypoxia and brain damage due to cord compression.
Choice A is wrong because vertex presentation is the most common and normal fetal position, where the head is down and fully flexed.
This does not increase the risk of cord prolapse.
Normal ranges for fetal presentation are:
• Vertex: 95% of term deliveries.
• Breech: 3% to 4% of term deliveries.
• Transverse lie: 0.5% of term deliveries.
• Face: 0.2% of term deliveries.
• Brow: 0.1% of term deliveries.
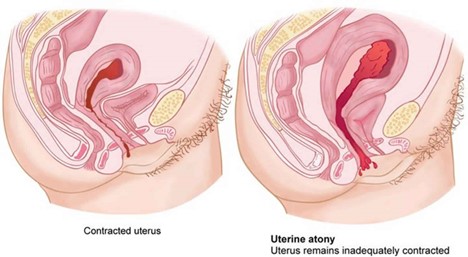
A nurse is caring for a client who has just delivered her second twin vaginally and notes that there is excessive bleeding from her vagina and that her uterus feels boggy on palpation.
The nurse should suspect which of the following complications?
Explanation
The correct answer is choice A. Uterine atony.
Uterine atony is the failure of the uterus to contract and retract after delivery, which can lead to excessive bleeding and hemorrhage.A boggy uterus on palpation is a sign of uterine atony.
Choice B. Uterine inversion is wrong because it is a rare complication in which the uterus turns inside out and protrudes through the cervix.It usually causes severe pain, shock, and hemorrhage.
Choice C. Uterine rupture is wrong because it is a life-threatening emergency in which the uterus tears open along the scar line of a previous cesarean delivery or other uterine surgery.It usually causes severe abdominal pain, fetal distress, and maternal hypovolemic shock.
Choice D. Uterine infection is wrong because it is an inflammation of the endometrium (the lining of the uterus) caused by bacteria.It usually causes fever, foul-smelling lochia, and lower abdominal tenderness.
Normal ranges for postpartum bleeding are about 500 ml for vaginal delivery and 1000 ml for cesarean delivery.The uterus should feel firm and midline at or below the umbilicus after delivery.
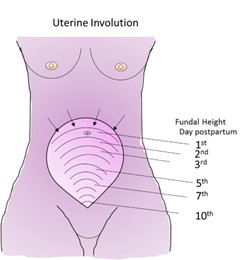
A nurse is assessing a client who had a vaginal delivery and notes that her fundus is firm, midline, and 2 cm below the umbilicus.
The nurse should document this finding as which of the following?
Explanation
The correct answer is choice A. Normal involution.
This means that the uterus is returning to its pre-pregnancy size and position after delivery.
The fundus is the upper part of the uterus and it should be firm, midline, and gradually descend into the pelvis.A fundus that is 2 cm below the umbilicus at 4 hours postpartum is within the normal range.
Choice B. Subinvolution is wrong because it refers to a delayed or incomplete involution of the uterus.
This can result in prolonged bleeding, infection, or retained placental fragments.A fundus that is above the umbilicus, boggy, or displaced to one side may indicate subinvolution.
Choice C. Retained placenta is wrong because it means that some or all of the placenta remains in the uterus after delivery.
This can cause heavy bleeding, infection, or uterine atony.A fundus that is high, soft, or tender may indicate retained placenta.
Choice D. Endometritis is wrong because it means that the lining of the uterus is inflamed due to infection.
This can cause fever, foul-smelling lochia, pelvic pain, or uterine tenderness.A fundus that is enlarged, tender, or malodorous may indicate endometritis.
Normal ranges for fundal height after delivery are:
• Immediately after delivery:
A nurse is providing discharge teaching to a client who had a cesarean delivery due to cord prolapse.
Which of the following instructions should the nurse include in the teaching?
Explanation
The correct answer is choiceA.
The nurse should instruct the client to avoid lifting anything heavier than the newborn for 6 weeks.This is because lifting heavy objects can strain the abdominal muscles and the incision site, and increase the risk of bleeding and infection.
ChoiceBis wrong because the nurse should advise the client to wait at least 4 to 6 weeks before resuming sexual intercourse.This is to allow the incision to heal and prevent infection and discomfort.
ChoiceCis wrong because the nurse should not recommend ibuprofen for pain relief as it can interfere with blood clotting and increase bleeding.The nurse should suggest acetaminophen or a prescribed analgesic instead.
ChoiceDis wrong because the nurse should not tell the client to report any foul-smelling vaginal discharge to the provider.
The client should expect some vaginal discharge (lochia) for several weeks after a cesarean delivery, which may have a mild odor.However, the nurse should instruct the client to report signs of infection such as fever, chills, redness, swelling, or increased pain at the incision site.
A patient’s umbilical cord prolapses during labor induction with oxytocin infusion.
Which action by the nurse takes priority?
Explanation
The correct answer is choice C. Apply pressure to presenting part with hand.
This is because cord prolapse is an emergency situation that requires immediate delivery to save the fetus.Applying pressure to the presenting part with hand can help relieve the compression of the cord and maintain fetal oxygenation until delivery.
Choice A is wrong because stopping oxytocin infusion will not prevent cord compression or fetal hypoxia.Oxytocin may be stopped after applying pressure to the presenting part and notifying the physician.
Choice B is wrong because placing the patient in knee-chest position may not be effective in relieving cord compression.
It may also be uncomfortable and difficult for the patient to maintain.A better position would be Trendelenburg or modified Sims.
Choice D is wrong because administering oxygen via non-rebreather mask is not a priority action.Oxygen may be given after applying pressure to the presenting part and notifying the physician, but it will not improve fetal oxygenation if the cord is compressed.

Which statement by a pregnant client indicates understanding of measures to prevent umbilical cord prolapse?
Explanation
The correct answer is choice C.“I will come to the hospital as soon as my water breaks.” This statement indicates understanding of measures to prevent umbilical cord prolapse, which is a complication that occurs when the umbilical cord drops out of the cervix before the baby during labor.This can cut off the baby’s blood and oxygen supply and cause permanent brain damage.Immediate delivery by C-section is usually necessary.
Choice A is wrong because squatting or sitting on hard surfaces does not increase the risk of umbilical cord prolapse.
Choice B is wrong because decreased fetal movement is not a sign of umbilical cord prolapse, but rather a sign of fetal distress that may have other causes.
Choice D is wrong because drinking plenty of fluids and resting on the left side are general measures to promote maternal and fetal well-being, but they do not prevent umbilical cord prolapse.
Some of the risk factors for umbilical cord prolapse include premature rupture of membranes, multiple pregnancy, breech presentation, excessive amniotic fluid, abnormal length of the umbilical cord and premature delivery.Some of the symptoms of umbilical cord prolapse include visible or palpable cord after water breaks, fetal heart rate abnormalities and maternal feeling of something coming out of the vagina.Umbilical cord prolapse can be diagnosed by physical examination, ultrasound or fetal heart rate monitoring.
Which condition increases the risk of occult umbilical cord prolapse?
Explanation
This is a condition where there is too little amniotic fluid around the fetus.This increases the risk of umbilical cord prolapse because the cord can easily slip past the presenting part of the fetus and into the cervix or vagina.
This can cause fetal hypoxia and distress due to compression or occlusion of the cord.
Choice A. Transverse lie is wrong because this is a condition where the fetus lies horizontally across the uterus.This can increase the risk of cord prolapse if the membranes rupture and the cord descends alongside or before the fetus.
Choice B. Macrosomia is wrong because this is a condition where the fetus is larger than average.This can decrease the risk of cord prolapse because the presenting part of the fetus is more likely to fill the pelvis and prevent the cord from slipping past.
Choice D. Placenta previa is wrong because this is a condition where the placenta covers part or all of the cervix.This can increase the risk of bleeding during labor, but not necessarily cord prolapse.
Which of these clients is at greatest risk for umbilical cord prolapse?
Explanation
The correct answer is choice C. A client who has oligohydramnios.
Oligohydramnios is a condition where there is too little amniotic fluid around the fetus.This can cause the umbilical cord to slip down into the cervix or vagina before the baby, resulting in cord prolapse.
Cord prolapse can cut off the blood and oxygen supply to the baby and cause fetal distress or death.
Choice A is wrong because a client who is pregnant with twins is not at greater risk for cord prolapse unless there is also malpresentation of the fetuses, such as breech or transverse lie.
Choice B is wrong because a client who has gestational hypertension is not at greater risk for cord prolapse unless there is also polyhydramnios, which is excessive amniotic fluid around the fetus.
Choice D is wrong because a client who has placenta previa is not at greater risk for cord prolapse unless there is also artificial rupture of membranes by doctors.
What is the most common cause of variable decelerations in fetal heart rate?
Explanation
The correct answer is choice B. Umbilical cord compression.Variable decelerations are the most common type of fetal deceleration and they are caused by compression of the umbilical cord.They vary in shape, duration, and intensity and may not have a constant relationship with uterine contractions.
Choice A is wrong because uteroplacental insufficiency is the cause of late decelerations, not variable decelerations.Uteroplacental insufficiency is a decrease in the blood flow to the placenta that reduces the amount of oxygen and nutrients transferred to the fetus.
Choice C is wrong because maternal hypotension is one of the possible causes of late decelerations, not variable decelerations.Maternal hypotension can reduce the uteroplacental blood flow and cause fetal hypoxia.
Choice D is wrong because fetal head compression is the cause of early decelerations, not variable decelerations.Early decelerations are benign and uniform in shape and they occur when the fetal head is pressed against the cervix during a uterine contraction.
What is an occult cord prolapse?
Explanation
The correct answer is choice B. The cord is hidden, often next to but not in front of the fetal head.This is called anoccult cord prolapseand it occurs when the umbilical cord descends alongside–but not past–the presenting part of the baby.Occult cords can occur with ruptured or intact membranes.They can cause hypoxia, brain injury, and permanent disability in a baby, so medical personnel must address them rapidly and appropriately.
Choice A is wrong because it describes anovert cord prolapse, which means that the cord slips down into your cervix and vagina ahead of your baby during delivery.This is a medical emergency that can cut off your baby’s blood and oxygen supply during delivery.
Choice C is wrong because it describes avisible cord prolapse, which is a type of overt cord prolapse where the cord is visible or palpable outside of the vagina.This is also a medical emergency that requires immediate delivery.
Choice D is wrong because it describes anuchal cord, which means that the cord is wrapped around the fetal neck or body.This is not a prolapse, but it can cause complications such as reduced blood flow, fetal distress, or umbilical cord strangulation.
A patient’s umbilical cord prolapses during labor induction with oxytocin infusion.
The nurse immediately places her hand into the vagina and pushes up on the presenting part to relieve pressure on the cord until an emergency cesarean delivery can be performed.
What should be done with the oxytocin infusion?
Explanation
The correct answer is choice C. Stop it completely.This is because oxytocin infusion can cause uterine hyperstimulation, which can worsen the cord compression and compromise fetal oxygenation.Stopping the oxytocin infusion can reduce the frequency and intensity of contractions and relieve pressure on the cord.
Choice A is wrong because increasing the oxytocin infusion rate can increase the risk of cord prolapse and fetal hypoxia.Choice B is wrong because decreasing the oxytocin infusion rate may not be enough to prevent cord compression and fetal distress.Choice D is wrong because maintaining the oxytocin infusion rate can prolong the labor and increase the chance of fetal compromise.
Which of the following patients is at highest risk for umbilical cord prolapse?
Explanation
The correct answer is choice D. A patient who is 34 weeks pregnant with a breech presentation and ruptured membranes.This is because breech presentation and ruptured membranes are both risk factors for umbilical cord prolapse, which is where the umbilical cord descends through the cervix and is alongside or below the presenting part of the fetus.This can cause fetal hypoxia and distress.
Choice A is wrong because a cephalic presentation and intact membranes are not risk factors for umbilical cord prolapse.
Choice B is wrong because although twins and ruptured membranes are risk factors for umbilical cord prolapse, the risk is lower than in choice D. Choice C is wrong because although a transverse lie is a risk factor for umbilical cord prolapse, the risk is lower than in choice D if the membranes are intact.
Which of the following statements by a patient indicates understanding of how to prevent umbilical cord prolapse?
Explanation
The correct answer is choice A. “I will avoid squatting or sitting on the toilet after my water breaks.” This statement indicates that the patient understands how to prevent umbilical cord prolapse, which is a rare but serious complication that occurs when the umbilical cord slips out of the cervix before the baby during labor.This can cut off the baby’s blood and oxygen supply and require immediate delivery.
Choice B is wrong because drinking plenty of fluids does not affect the amniotic fluid level, which is determined by the placenta and the baby’s kidneys.Excessive amniotic fluid (polyhydramnios) can actually increase the risk of umbilical cord prolapse.
Choice C is wrong because monitoring the baby’s movements does not prevent umbilical cord prolapse, although it can help detect fetal distress if the cord is compressed.Decreased fetal movements can have other causes besides cord prolapse, such as fetal sleep cycle, maternal medication, or placental insufficiency.
Choice D is wrong because sleeping on the left side does not prevent umbilical cord prolapse, although it can improve blood flow to the baby and reduce the risk of supine hypotension syndrome.Umbilical cord prolapse can occur regardless of the maternal position.
Normal ranges for amniotic fluid index (AFI) are 5 to 25 cm.Normal ranges for fetal heart rate (FHR) are 110 to 160 beats per minute (bpm).
Exams on Umbilical cord prolapse
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define cord prolapse and cord presentation
- Identify the risk factors and causes of cord prolapse
- Recognize the signs and symptoms of cord prolapse
- Describe the nursing interventions and management of cord prolapse
- Explain the complications and outcomes of cord prolapse
Introduction
- Cord prolapse is descent of the umbilical cord into the vagina ahead of the fetal presenting part with resulting compression of the cord between the presenting part and the maternal pelvis.
- Cord presentation is presence of the umbilical cord between the fetal presenting part and the cervix, with or without intact membranes.
- Cord prolapse is an emergency situation; immediate delivery will be attempted to save the fetus.
- Cord prolapse occurs in 1 of 200 pregnancies. The incidence is higher in the case of breech presentation (1 in 100).
- Perinatal mortality associated with cord prolapse is just over 9%.
Risk factors and causes
- Any condition that displaces the head or presenting part from the lower segment or cervix is a predisposing factor.
- Factors that are associated with cord prolapse are shown in table below.
|
Antenatal Risk Factors |
Intra-partum Risk Factors |
|
Non vertex presentation (transverse lie “back up” or breech) |
Artificial rupture of the membranes (especially with high presenting part) |
|
Unengaged presenting part eg Low-lying placenta, cervical fibroid etc |
Manual rotation or other vaginal manipulation of the fetus (eg internal podalic version, disimpaction of fetal head during rotational assisted delivery, placement of a fetal scalp electrode, insertion of an intrauterine pressure catheter or amnioinfusion catheter) |
|
Prematurity |
External Cephalic Version |
|
Polyhydramnios |
Large balloon catheter induction of labour |
|
Second twin |
Stabilising induction of labour |
|
Unstable lie is when the longitudinal axis of the fetus (lie) is changing repeatedly after 37+0 weeks |
Preterm premature rupture of membranes |
|
Multiparity |
Low birth weight |
|
Congenital abnormalities |
Cord abnormalities |
|
Male gender (if known) |
Signs and symptoms
- Cord prolapse may be occult or occur at any time in the labor process, even when the amniotic membranes are intact.
- Client reports feeling the cord within the vagina.
- Fetal bradycardia with deceleration during contraction.
- The umbilical cord can be seen or felt during a vaginal examination.
Nursing interventions and management
- Identify prolapsed cord and provide immediate intervention.
- Assess a laboring client often if the fetus is preterm or small for gestational age, if the fetal presenting part is not engaged, and if the membranes are ruptured.
- Periodically evaluate FHR, especially right after rupture of membranes (spontaneous or surgical), and again in 5 to 10 minutes.
- If prolapsed cord is identified, notify the physician and prepare for emergency cesarean birth.
- Using sterile gloved hand, insert 2 fingers into vagina, place finger on either side of cord, lift head from cord to stop compression.
- Reposition client knee-chest or Trendelenburg.
- Use warm, sterile saline soaked towel on visible cord to prevent cord drying up.
- Administer oxygen by face mask at 8 to 10 L/min as ordered.
- Start IV infusion or increase rate as ordered to maintain hydration and blood volume.
- Monitor maternal vital signs and FHR continuously until delivery.
Provide emotional support and reassurance to client and family.
Complications and outcomes
- Compression of the cord results in compromise or cessation of fetoplacental perfusion.
- This can lead to fetal hypoxia, acidosis, neurological damage, or death.
- The prognosis depends on the duration and severity of cord compression, gestational age, and mode and speed of delivery.
The perinatal mortality rate associated with cord prolapse ranges from 6% to 15%.
Summary
- Cord prolapse is an obstetric emergency that requires prompt recognition and intervention.
- It occurs when the umbilical cord descends into the vagina ahead of the fetal presenting part, causing compression and reduced blood flow.
- It is more common in non vertex presentations, unengaged presenting parts, prematurity, polyhydramnios, multiple gestations, unstable lie, and congenital anomalies.
- It presents with fetal bradycardia with decelerations, palpable or visible cord in vagina, and maternal sensation of cord.
- The nursing management includes notifying physician, preparing for cesarean section, relieving cord compression by manual elevation or maternal position change, applying warm saline compress to exposed cord, administering oxygen and IV fluids as ordered, monitoring maternal and fetal status, and providing emotional support.
- The complications include fetal hypoxia, acidosis, neurological damage, or death. The prognosis depends on various factors such as duration of compression, gestational age, and mode and speed of delivery.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Umbilical cord prolapse
This filled cannot be empty

