Please set your exam date
Chemotherapy Agents and Oncology Pharmacology
Study Questions
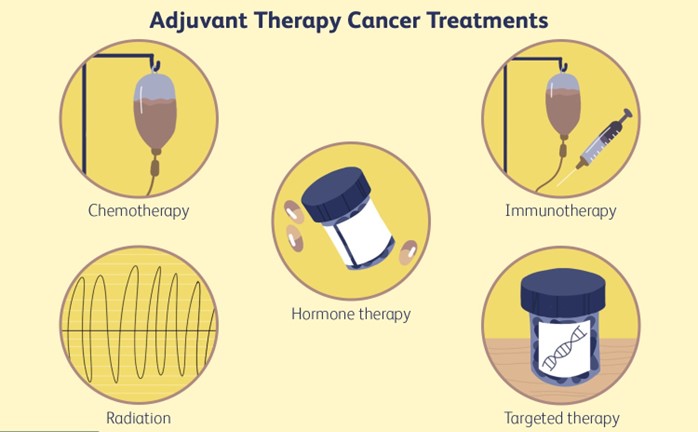
Introduction
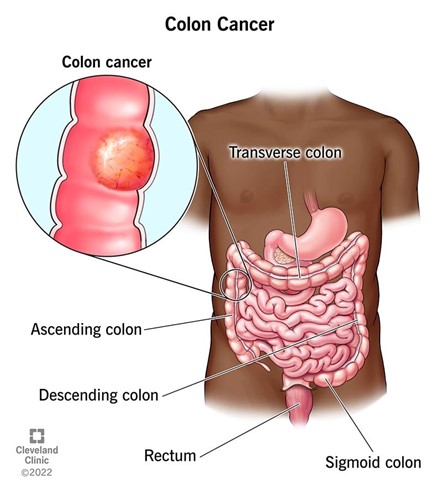
A nurse is caring for a client who is receiving adjuvant chemotherapy after surgery for colon cancer. The nurse should explain to the client that the purpose of this type of chemotherapy is to:
Explanation
Choice A reason:
This is incorrect because shrinking the tumor before surgery and making it easier to remove is the purpose of neoadjuvant chemotherapy, not adjuvant chemotherapy. Neoadjuvant chemotherapy is given before the primary treatment, while adjuvant chemotherapy is given after the primary treatment.
Choice B reason:
This is correct because eliminating any remaining cancer cells and preventing recurrence is the main goal of adjuvant chemotherapy. Adjuvant chemotherapy is given after the primary treatment, usually surgery, to lower the chance that the cancer will return and to improve the outcome of firstline treatment.
Choice C reason:
This is incorrect because inducing remission and reducing the tumor burden is the purpose of induction chemotherapy, not adjuvant chemotherapy. Induction chemotherapy is given as the firstline treatment to achieve a complete or partial response.
Choice D reason:
This is incorrect because relieving symptoms and improving quality of life is the purpose of palliative chemotherapy, not adjuvant chemotherapy. Palliative chemotherapy is given to patients with incurable or terminal cancer to reduce pain and suffering.
A nurse is reviewing the medication orders for a client who is receiving neoadjuvant chemotherapy for breast cancer. The nurse should identify that this client will receive chemotherapy drugs that are:
Explanation
Choice A reason:
This is incorrect because cell cyclespecific chemotherapy drugs are drugs that act on cancer cells during specific phases of the cell cycle. They have a narrow spectrum of activity because they only affect cells that are actively dividing. Cell cyclespecific drugs are not necessarily used for neoadjuvant chemotherapy.
Choice B reason:
This is incorrect because cell cyclenonspecific chemotherapy drugs are drugs that act on cancer cells regardless of their phase in the cell cycle. They have a broad spectrum of activity because they affect both dividing and nondividing cells. Cell cyclenonspecific drugs are not necessarily used for neoadjuvant chemotherapy.
Choice C reason:
This is incorrect because cell cyclespecific chemotherapy drugs are drugs that act on cancer cells during specific phases of the cell cycle. They have a broad spectrum of activity because they affect both dividing and nondividing cells. Cell cyclespecific drugs are not necessarily used for neoadjuvant chemotherapy.
Choice D reason:
This is incorrect because cell cyclenonspecific chemotherapy drugs are drugs that act on cancer cells regardless of their phase in the cell cycle. They have a narrow spectrum of activity because they only affect cells that are actively dividing. Cell cyclenonspecific drugs are not necessarily used for neoadjuvant chemotherapy.
Choice E reason:
This is correct because neoadjuvant chemotherapy is treatment with drugs before the main treatment, usually surgery or radiation therapy, to shrink the tumor and improve the outcome of the main treatment. Neoadjuvant chemotherapy can also help with surgical planning and early treatment of microscopic metastatic foci. Neoadjuvant chemotherapy is often given in combination with other modalities such as radiation or surgery.
A nurse is administering induction chemotherapy to a client who has acute myeloid leukemia (AML). The client asks the nurse what induction chemotherapy means. The nurse should respond by saying:
Explanation
Choice A reason:
This is incorrect because chemotherapy given before other treatments to shrink the leukemia cells is called neoadjuvant chemotherapy, not induction chemotherapy. Neoadjuvant chemotherapy is used to improve the outcome of the main treatment, such as surgery or radiation therapy.
Choice B reason:
This is incorrect because chemotherapy given after other treatments to kill any leftover leukemia cells is called adjuvant chemotherapy, not induction chemotherapy. Adjuvant chemotherapy is used to lower the chance of leukemia recurrence and improve the outcome of the firstline treatment.
Choice C reason:
This is correct because induction chemotherapy is the firstline or initial treatment of cancer, usually with high doses of anticancer drugs, before another treatment such as consolidation or postremission therapy. The goal of induction chemotherapy is to cure the cancer, destroy as many cancer cells as possible, suppress distant metastases, and shrink the tumor.
Choice D reason:
This is incorrect because chemotherapy given to control symptoms and improve quality of life is called palliative chemotherapy, not induction chemotherapy. Palliative chemotherapy is used for patients with incurable or terminal cancer to reduce pain and suffering.
A nurse is caring for a client who has ovarian cancer and is receiving palliative chemotherapy. The client tells the nurse that she feels hopeless and wonders why she is still taking the drugs. The nurse should respond by saying:
Explanation
Choice A reason:
This is incorrect because it may sound dismissive of the client's feelings and imply that palliative chemotherapy can only prolong life, not improve quality of life. Palliative chemotherapy is not meant to cure cancer or to extend life significantly, but to relieve the symptoms of cancer and improve quality of life.
Choice B reason:
This is incorrect because it may give false hope to the client and contradict the purpose of palliative chemotherapy. Palliative chemotherapy is unlikely to cure cancer or induce remission, even if the client responds well.
Choice C reason:
This is incorrect because it may suggest that the nurse does not support the client's decision to continue treatment or that palliative chemotherapy is futile. Palliative chemotherapy is optional and the client has the right to refuse treatment, but the nurse should respect the client's wishes and provide information and support.
Choice D reason:
This is correct because it shows empathy and compassion for the client's feelings and acknowledges the benefits of palliative chemotherapy. Palliative chemotherapy can relieve some of the symptoms and discomforts caused by cancer, such as pain, nausea, fatigue, etc.
A nurse is educating a client who has prostate cancer and is receiving salvage chemotherapy after failure of previous treatments. The nurse should inform the client that salvage chemotherapy:
Explanation
Choice A reason:
Salvage chemotherapy is not given to prevent relapse or progression of the disease, but rather to treat it when it has already relapsed or progressed. Preventive chemotherapy is usually given after the initial treatment has achieved a complete response, to reduce the risk of recurrence.
Choice B reason:
This is the correct answer. Salvage chemotherapy is given to control advanced or refractory disease, meaning that the disease has not responded to or has become resistant to previous treatments. Salvage chemotherapy aims to stabilize the disease, prevent further complications, and improve symptoms and quality of life. ³⁴
Choice C reason:
Salvage chemotherapy is not given to induce remission or reduce tumor burden, but rather to control it when it has already become unresponsive or resistant to previous treatments. Induction chemotherapy is usually given as the firstline treatment for aggressive cancers, to shrink the tumor before surgery or radiation therapy.
Choice D reason:
Salvage chemotherapy is not only given to relieve symptoms and improve quality of life, but also to control the disease and prevent further complications. Symptom relief and quality of life improvement are important goals of salvage chemotherapy, but they are not the only ones. ³⁴:

Cytotoxic Chemotherapy Drugs
A nurse is caring for a client who is receiving cyclophosphamide, an alkylating agent, as part of chemotherapy for lymphoma. The nurse should monitor the client for which of the following adverse effects of this drug?
Explanation
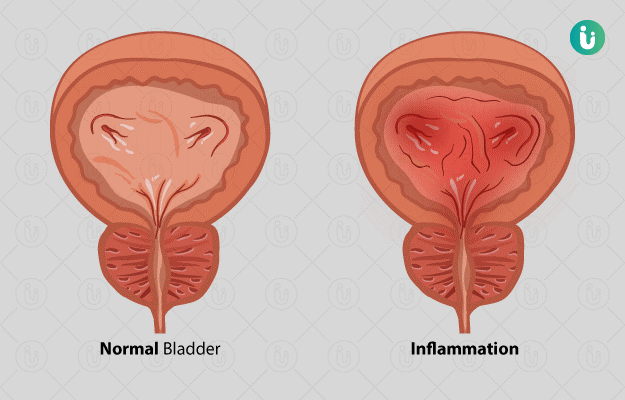
Choice A reason: Cyclophosphamide is an alkylating agent that can cause damage to the kidneys and bladder, leading to nephrotoxicity and hemorrhagic cystitis. Nephrotoxicity is the impairment of kidney function due to exposure to toxic substances, and hemorrhagic cystitis is the inflammation and bleeding of the bladder wall. The nurse should monitor the client's urine output, specific gravity, blood urea nitrogen, creatinine, and urinalysis for signs of renal impairment and hematuria. The nurse should also encourage the client to drink plenty of fluids, administer mesna (a protective agent), and alkalinize the urine to prevent these complications .
Choice B reason: Cardiotoxicity and extravasation injury are not common adverse effects of cyclophosphamide. Cardiotoxicity is the damage to the heart muscle caused by certain drugs, such as anthracyclines (e.g., doxorubicin) or trastuzumab. Extravasation injury is the leakage of a vesicant drug (a drug that causes tissue damage) into the surrounding tissues, causing pain, swelling, necrosis, and infection. Cyclophosphamide is not a vesicant drug, but vinca alkaloids (e.g., vincristine) or platinum compounds (e.g., cisplatin) are .
Choice C reason: Peripheral neuropathy and pulmonary fibrosis are not common adverse effects of cyclophosphamide. Peripheral neuropathy is the damage to the nerves of the peripheral nervous system, causing numbness, tingling, pain, or weakness in the hands or feet. Pulmonary fibrosis is the scarring of the lung tissue, causing shortness of breath, cough, and reduced oxygen levels. These complications are more likely to occur with drugs such as taxanes (e.g., paclitaxel) or bleomycin .
Choice D reason: Hepatotoxicity and gastrointestinal toxicity are not specific adverse effects of cyclophosphamide. Hepatotoxicity is the damage to the liver cells caused by certain drugs, such as methotrexate or acetaminophen. Gastrointestinal toxicity is the irritation of the mucous membranes of the digestive tract, causing nausea, vomiting, diarrhea, or mucositis. These side effects can occur with many chemotherapy drugs, but they are not unique to cyclophosphamide .
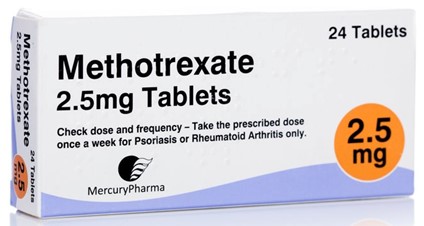
A nurse is administering methotrexate, an antimetabolite, to a client who has osteosarcoma. The nurse should identify that methotrexate can cause which of the following adverse effects? (Select all that apply.)
Explanation
Choice A reason: Methotrexate is an antimetabolite that inhibits the synthesis of DNA and RNA, which are essential for cell division and growth. Methotrexate affects rapidly dividing cells, such as those in the bone marrow, where blood cells are produced. This can lead to bone marrow suppression, which is the reduction of the number and function of blood cells, causing anemia, leukopenia, thrombocytopenia, or pancytopenia. The nurse should monitor the client's complete blood count, signs of infection, bleeding, or fatigue, and administer leucovorin (a rescue agent) to prevent or treat this complication .
Choice B reason: Ototoxicity is not a common adverse effect of methotrexate. Ototoxicity is the damage to the inner ear or auditory nerve caused by certain drugs, such as aminoglycosides (e.g., gentamicin) or loop diuretics (e.g., furosemide). Ototoxicity can cause hearing loss, tinnitus, vertigo, or balance problems .
Choice C reason: Gastrointestinal toxicity is a common adverse effect of methotrexate. Gastrointestinal toxicity is the irritation of the mucous membranes of the digestive tract, causing nausea, vomiting, diarrhea, or mucositis. Methotrexate can also cause hepatotoxicity, which is the damage to the liver cells. The nurse should monitor the client's liver function tests, weight, fluid intake and output, and nutritional status. The nurse should also provide antiemetics, mouth care, hydration, and small frequent meals to prevent or manage this complication .
Choice D reason: Neurotoxicity is not a common adverse effect of methotrexate. Neurotoxicity is the damage to the brain or nervous system caused by certain drugs, such as platinum compounds (e.g., cisplatin) or vinca alkaloids (e.g., vincristine). Neurotoxicity can cause confusion, seizures, peripheral neuropathy, or encephalopathy .
Choice E reason: Skin reactions are a common adverse effect of methotrexate. Skin reactions include rash, pruritus, photosensitivity, alopecia, or erythema multiforme. The nurse should inspect the client's skin regularly, provide skin care, avoid exposure to sunlight or ultraviolet light, and apply sunscreen and moisturizer to prevent or treat this complication .
A nurse is educating a client who has breast cancer and is receiving paclitaxel, a natural product, as part of chemotherapy. The nurse should instruct the client to report which of the following manifestations that indicate peripheral neuropathy?
Explanation
Choice A reason: Hearing loss is not a common side effect of paclitaxel, a natural product that interferes with the growth of cancer cells. Hearing loss may be caused by other factors, such as aging, exposure to loud noises, or ear infections.
Choice B reason: Chest pain and shortness of breath are not signs of peripheral neuropathy, but may indicate cardiac or pulmonary problems. Paclitaxel can cause hypersensitivity reactions, such as flushing, rash, and dyspnea, but these usually occur during or shortly after the infusion.
Choice C reason: Numbness and tingling in the hands and feet are symptoms of peripheral neuropathy, which is a common adverse effect of paclitaxel. Peripheral neuropathy is a condition that affects the nerves that carry messages to and from the brain and spinal cord. Paclitaxel can damage these nerves and cause sensory changes, such as numbness, tingling, burning, or pain. The client should report these symptoms to the provider, as they may require dose adjustment or discontinuation of the drug.
Choice D reason: Redness and swelling at the infusion site are not signs of peripheral neuropathy, but may indicate phlebitis or infiltration. Phlebitis is inflammation of the vein, which can cause pain, warmth, and redness along the vein. Infiltration is leakage of the drug into the surrounding tissue, which can cause swelling, pain, and skin damage. The nurse should monitor the infusion site for these complications and stop the infusion if they occur.

A nurse is caring for a client who has lung cancer and is receiving bleomycin, an antineoplastic antibiotic, as part of chemotherapy. The nurse should assess the client for which of the following signs and symptoms that indicate pulmonary fibrosis?
Explanation
Choice A reason: Cough, dyspnea, and crackles are signs and symptoms of pulmonary fibrosis, which is a serious and potentially fatal adverse effect of bleomycin, an antineoplastic antibiotic that inhibits DNA synthesis in cancer cells. Pulmonary fibrosis is a condition that causes scarring and thickening of the lung tissue, which reduces the lung's ability to exchange oxygen and carbon dioxide. The client should be monitored for pulmonary function tests and chest xrays before and during treatment with bleomycin, and the drug should be discontinued if pulmonary fibrosis develops.
Choice B reason: Nausea, vomiting, and diarrhea are not signs of pulmonary fibrosis, but may occur as common side effects of bleomycin and other chemotherapy drugs. The nurse should provide antiemetic drugs, fluids, and electrolytes to prevent dehydration and electrolyte imbalance in the client.
Choice C reason: Fever, chills, and sore throat are not signs of pulmonary fibrosis, but may indicate infection, which is a risk factor for clients receiving chemotherapy. Chemotherapy drugs can suppress the immune system and make the client more susceptible to infections. The nurse should monitor the client's temperature, white blood cell count, and cultures, and administer antibiotics as prescribed.
Choice D reason: Jaundice, dark urine, and claycolored stools are not signs of pulmonary fibrosis, but may indicate liver damage, which is another possible adverse effect of bleomycin. Bleomycin can cause hepatotoxicity, which is toxicity to the liver cells that can impair the liver's function. The nurse should monitor the client's liver function tests, such as serum bilirubin, alkaline phosphatase, and transaminases, and report any abnormalities to the provider.
A nurse is administering leuprolide, a hormone, to a client who has prostate cancer. The nurse should explain to the client that leuprolide works by:
Explanation
Choice A reason: Blocking the estrogen receptors on the cancer cells and inhibiting their growth is the mechanism of action of tamoxifen, a selective estrogen receptor modulator (SERM) that is used to treat breast cancer. Tamoxifen is not effective for prostate cancer, which is stimulated by testosterone, not estrogen.
Choice B reason: Stimulating the production of testosterone and increasing the sensitivity of the cancer cells to chemotherapy is not the mechanism of action of leuprolide, a hormone that is used to treat prostate cancer. Leuprolide does not increase testosterone, but decreases it. Increasing testosterone would worsen prostate cancer, not improve it.
Choice C reason: Suppressing the secretion of luteinizing hormone and reducing the level of testosterone is the mechanism of action of leuprolide, a gonadotropinreleasing hormone (GnRH) agonist that is used to treat prostate cancer. Leuprolide binds to the GnRH receptors in the pituitary gland and initially stimulates the release of luteinizing hormone (LH) and folliclestimulating hormone (FSH). However, with continuous administration, leuprolide desensitizes the receptors and inhibits the secretion of LH and FSH. This leads to a decrease in the production of testosterone by the testes, which reduces the growth of prostate cancer cells.
Choice D reason: Altering the metabolism of cortisol and inducing apoptosis of the cancer cells is not the mechanism of action of leuprolide, a hormone that is used to treat prostate cancer. Leuprolide does not affect cortisol, but testosterone. Cortisol is a glucocorticoid hormone that regulates stress response, inflammation, and metabolism. Apoptosis is a process of programmed cell death that can be triggered by some chemotherapy drugs, such as cisplatin and doxorubicin.
Targeted Therapy and Immunotherapy in Oncology
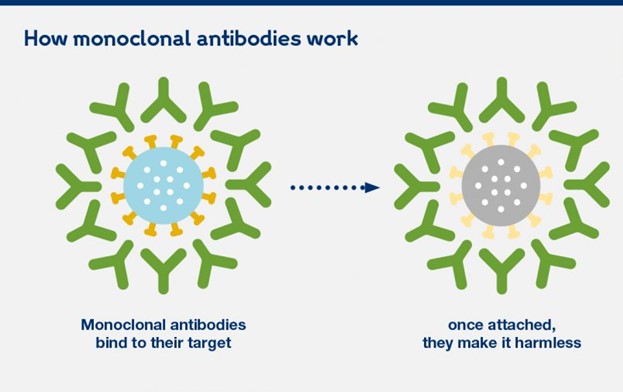
A nurse is caring for a client who is receiving rituximab, a monoclonal antibody, as part of targeted therapy for nonHodgkin's lymphoma. The nurse should monitor the client for which of the following adverse effects of this drug?
Explanation
Choice A reason:
Infusion reactions and allergic reactions are common and potentially serious adverse effects of rituximab, a monoclonal antibody that binds to the CD20 antigen on the surface of B lymphocytes and causes their destruction. Rituximab is used to treat nonHodgkin's lymphoma, a type of cancer that affects the lymphatic system. Infusion reactions can occur during or shortly after the administration of rituximab and may include fever, chills, rigors, hypotension, dyspnea, bronchospasm, angioedema, and anaphylaxis. Allergic reactions can occur within hours or days after the infusion and may include rash, urticaria, pruritus, and serum sickness. The nurse should monitor the client's vital signs, oxygen saturation, and symptoms during and after the infusion and administer premedications, such as antihistamines, corticosteroids, and acetaminophen, as prescribed.
Choice B reason:
Gastrointestinal toxicity and hepatotoxicity are not common adverse effects of rituximab, a monoclonal antibody that is used to treat nonHodgkin's lymphoma. Gastrointestinal toxicity and hepatotoxicity may be caused by other drugs, such as methotrexate and cyclophosphamide, which are often used in combination with rituximab. The nurse should monitor the client's liver function tests, such as serum bilirubin, alkaline phosphatase, and transaminases, and report any abnormalities to the provider.
Choice C reason:
Hypertension and bleeding are not common adverse effects of rituximab, a monoclonal antibody that is used to treat nonHodgkin's lymphoma. Hypertension and bleeding may be caused by other factors, such as renal impairment, coagulation disorders, or anticoagulant therapy. The nurse should monitor the client's blood pressure, urine output, creatinine clearance, coagulation studies, platelet count, and signs of bleeding.
Choice D reason:
Flulike symptoms and bone marrow suppression are not common adverse effects of rituximab, a monoclonal antibody that is used to treat nonHodgkin's lymphoma. Flulike symptoms and bone marrow suppression may be caused by other drugs, such as interferon alfa and vinblastine, which are also used to treat nonHodgkin's lymphoma. The nurse should monitor the client's temperature, white blood cell count, hemoglobin level, and symptoms of infection or anemia.
A nurse is administering erlotinib, a tyrosine kinase inhibitor, to a client who has lung cancer. The nurse should instruct the client to report which of the following adverse effects of this drug? (Select all that apply.)
Explanation
Choice A reason:
Diarrhea and abdominal pain are common and potentially serious adverse effects of erlotinib, a tyrosine kinase inhibitor that blocks the epidermal growth factor receptor (EGFR) and inhibits the growth and survival of cancer cells. Erlotinib is used to treat lung cancer, a type of cancer that affects the respiratory system. Diarrhea and abdominal pain can indicate gastrointestinal toxicity, which can lead to dehydration, electrolyte imbalance, and perforation. The client should report these symptoms to the provider and receive appropriate treatment, such as fluids, electrolytes, and antidiarrheal drugs.
Choice B reason:
Jaundice and dark urine are rare but serious adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Jaundice and dark urine can indicate liver damage, which can impair the liver's function and cause complications, such as bleeding, infection, and encephalopathy. The client should report these symptoms to the provider and have their liver function tests, such as serum bilirubin, alkaline phosphatase, and transaminases, monitored regularly.
Choice C reason:
Skin rash and dry skin are common and usually mild adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Skin rash and dry skin can occur because erlotinib affects the EGFR in the skin cells as well as the cancer cells. The client should report these symptoms to the provider and use moisturizers, sunscreen, and mild soap to prevent skin irritation and infection.
Choice D reason:
Chest pain and dyspnea are not common adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Chest pain and dyspnea may be caused by other factors, such as cardiac or pulmonary problems. The client should report these symptoms to the provider and have their cardiac and pulmonary function assessed.
Choice E reason:
Fever and chills are not common adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Fever and chills may indicate infection, which is a risk factor for clients receiving chemotherapy. Chemotherapy drugs can suppress the immune system and make the client more susceptible to infections. The client should report these symptoms to the provider and have their temperature, white blood cell count, and cultures monitored.
A nurse is educating a client who has colorectal cancer and is receiving bevacizumab, an angiogenesis inhibitor, as part of targeted therapy. The nurse should explain to the client that bevacizumab works by:
Explanation
Choice A reason:
Binding to specific antigens on cancer cells and triggering their destruction is the mechanism of action of monoclonal antibodies, such as rituximab and trastuzumab, that are used to treat some types of cancer, such as nonHodgkin's lymphoma and breast cancer. Monoclonal antibodies are proteins that recognize and attach to specific antigens on the surface of cancer cells and activate the immune system to destroy them.
Choice B reason:
Inhibiting the activity of enzymes that mediate cell growth and survival signals is the mechanism of action of tyrosine kinase inhibitors, such as erlotinib and imatinib, that are used to treat some types of cancer, such as lung cancer and chronic myeloid leukemia. Tyrosine kinase inhibitors are drugs that block the activity of enzymes called tyrosine kinases, which are involved in transmitting signals from growth factors and hormones to the cell nucleus.
Choice C reason:
Preventing the formation of new blood vessels that supply oxygen and nutrients to tumors is the mechanism of action of angiogenesis inhibitors, such as bevacizumab and sorafenib, that are used to treat some types of cancer, such as colorectal cancer and renal cell carcinoma. Angiogenesis inhibitors are drugs that interfere with the process of angiogenesis, which is the formation of new blood vessels from existing ones. Angiogenesis is essential for tumor growth and metastasis, as tumors need a constant supply of oxygen and nutrients to survive and spread.
Choice D reason:
Enhancing the immune system's ability to recognize and eliminate cancer cells is the mechanism of action of immunotherapy, such as interferon alfa and interleukin2, that are used to treat some types of cancer, such as melanoma and renal cell carcinoma. Immunotherapy is a type of treatment that uses substances produced by the body or made in a laboratory to boost or restore the immune system's function. Immunotherapy can stimulate the immune system to attack cancer cells or make them more visible to the immune system.
A nurse is caring for a client who has melanoma and is receiving interferon alfa2b, an immunomodulator, as part of immunotherapy. The client tells the nurse that he feels tired, achy, and feverish after each injection. The nurse should respond by saying:
Explanation
Choice A reason:
These are not normal side effects of interferon alfa2b, but symptoms of flulike syndrome, which is a common and potentially serious adverse effect of interferon alfa2b, an immunomodulator that enhances the immune system's ability to recognize and eliminate cancer cells. Interferon alfa2b is used to treat melanoma, a type of skin cancer that develops from melanocytes. Flulike syndrome can cause fever, chills, fatigue, myalgia, headache, and malaise. These symptoms may not go away after a few days, but may persist or worsen during the course of treatment.
Choice B reason:
These are not signs of an allergic reaction to interferon alfa2b, but symptoms of flulike syndrome caused by interferon alfa2b. An allergic reaction to interferon alfa2b would manifest as rash, urticaria, pruritus, angioedema, or anaphylaxis. The client should not stop taking interferon alfa2b without consulting the provider, as this may compromise the effectiveness of the treatment.
Choice C reason:
These are symptoms of flulike syndrome caused by interferon alfa2b. The nurse should explain to the client that flulike syndrome is a common adverse effect of interferon alfa2b and provide education on how to manage it. The nurse should advise the client to take acetaminophen as prescribed to reduce fever and pain, drink plenty of fluids to prevent dehydration, rest as needed to conserve energy, and report any severe or persistent symptoms to the provider.
Choice D reason:
These are not indications of bone marrow suppression caused by interferon alfa2b, but symptoms of flulike syndrome caused by interferon alfa2b. Bone marrow suppression is another possible adverse effect of interferon alfa2b, which can result in leukopenia, anemia, and thrombocytopenia. Bone marrow suppression can cause symptoms such as infection, bleeding, or pallor. The client should have their blood counts monitored regularly and receive supportive care as needed.
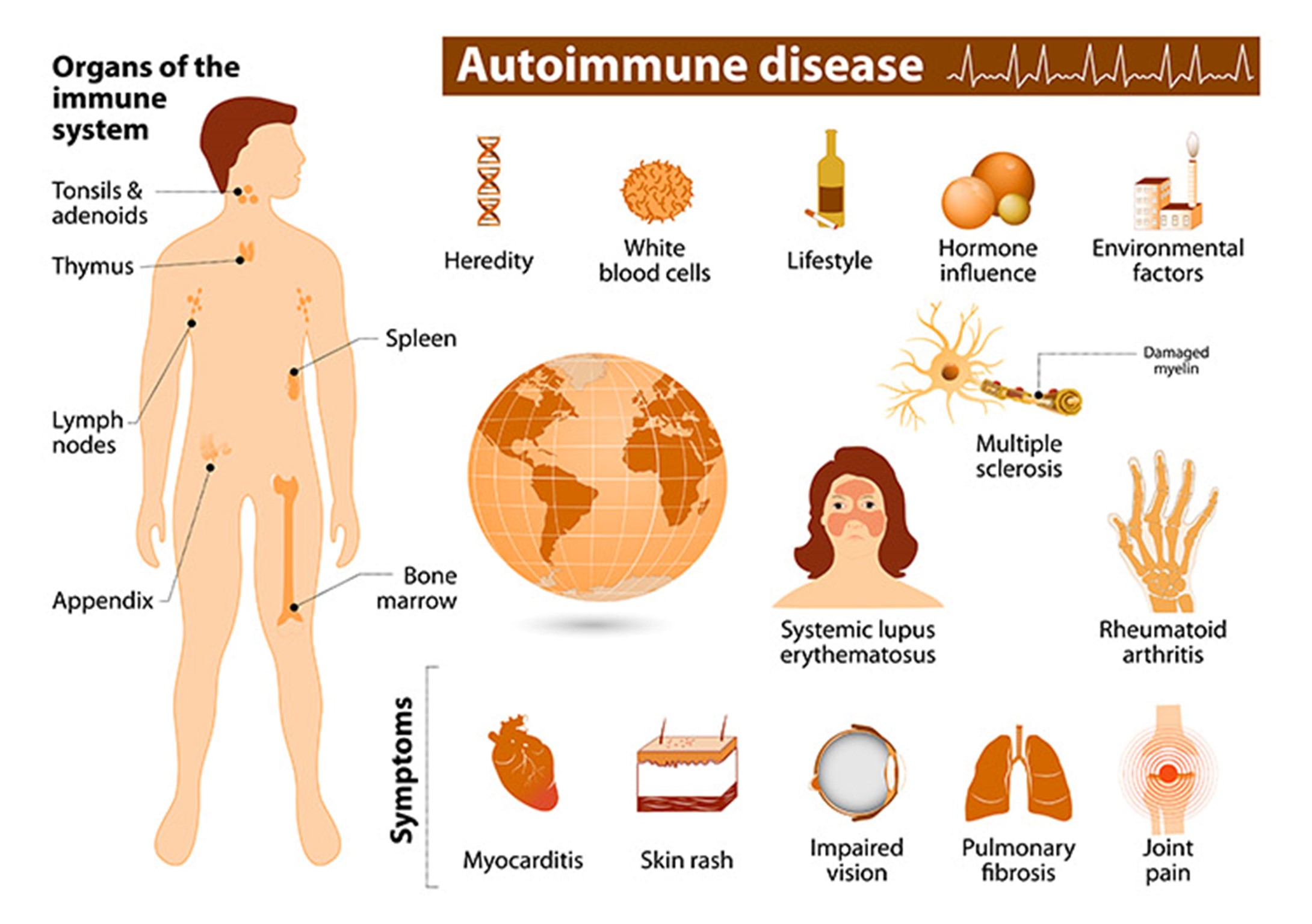
A nurse is administering nivolumab, a checkpoint inhibitor, to a client who has renal cell carcinoma. The nurse should identify that nivolumab can cause which of the following adverse effects?
Explanation
Choice A reason:
Cardiotoxicity and extravasation injury are not common adverse effects of nivolumab, a checkpoint inhibitor that blocks the programmed cell death1 (PD1) receptor and enhances the immune system's ability to recognize and eliminate cancer cells. Nivolumab is used to treat renal cell carcinoma, a type of kidney cancer that originates from the renal tubules. Cardiotoxicity and extravasation injury may be caused by other drugs, such as anthracyclines and vinca alkaloids, which are used to treat other types of cancer.
Choice B reason:
Peripheral neuropathy and pulmonary fibrosis are not common adverse effects of nivolumab, a checkpoint inhibitor that is used to treat renal cell carcinoma. Peripheral neuropathy and pulmonary fibrosis may be caused by other drugs, such as natural products and antineoplastic antibiotics, which are used to treat other types of cancer.
Choice C reason:
Autoimmune disorders and organ dysfunction are common and potentially serious adverse effects of nivolumab, a checkpoint inhibitor that is used to treat renal cell carcinoma. Autoimmune disorders and organ dysfunction can occur because nivolumab affects the PD1 receptor in the immune cells as well as the cancer cells. The PD1 receptor normally acts as a brake on the immune system and prevents it from attacking healthy tissues. By blocking the PD1 receptor, nivolumab can unleash the immune system and cause it to attack various organs, such as the skin, lungs, liver, kidneys, thyroid, pituitary gland, colon, and pancreas. The client should be monitored for signs and symptoms of autoimmune disorders and organ dysfunction, such as rash, pruritus, dyspnea, cough, jaundice, dark urine, fatigue, weight loss or gain, diarrhea, abdominal pain, and hypotension or hypertension. The client should receive corticosteroids or immunosuppressive drugs as prescribed to suppress the immune system and prevent further damage.
Choice D reason:
Thrombosis and teratogenicity are not common adverse effects of nivolumab, a checkpoint inhibitor that is used to treat renal cell carcinoma. Thrombosis and teratogenicity may be caused by other factors, such as coagulation disorders, genetic mutations, or pregnancy. The client should have their coagulation studies monitored regularly and receive anticoagulant therapy as prescribed to prevent thrombosis. The client should also avoid pregnancy while receiving nivolumab and use effective contraception methods.
Chemoprotective Agents and Bone Marrow Stimulants
A nurse is caring for a client who is receiving cyclophosphamide, an alkylating agent, as part of chemotherapy for ovarian cancer. The nurse should administer mesna, a chemoprotective agent, to the client to prevent which of the following adverse effects of cyclophosphamide?
Explanation
Choice A reason:
Cardiotoxicity is not a common adverse effect of cyclophosphamide, an alkylating agent that crosslinks DNA strands and prevents cell division. Cyclophosphamide is used to treat ovarian cancer, a type of cancer that affects the female reproductive organs. Cardiotoxicity may be caused by other drugs, such as anthracyclines and trastuzumab, which are used to treat other types of cancer.
Choice B reason:
Hemorrhagic cystitis is a common and potentially serious adverse effect of cyclophosphamide, an alkylating agent that is used to treat ovarian cancer. Hemorrhagic cystitis is inflammation and bleeding of the bladder, which can lead to infection, obstruction, and renal failure. Hemorrhagic cystitis is caused by the metabolite of cyclophosphamide, acrolein, which irritates the bladder lining. The nurse should administer mesna, a chemoprotective agent, to the client to prevent hemorrhagic cystitis. Mesna binds to acrolein and inactivates it, preventing it from damaging the bladder. The nurse should also encourage the client to drink plenty of fluids and void frequently to flush out the drug and its metabolites.
Choice C reason:
Nephrotoxicity is not a common adverse effect of cyclophosphamide, an alkylating agent that is used to treat ovarian cancer. Nephrotoxicity may be caused by other drugs, such as cisplatin and methotrexate, which are used to treat other types of cancer.
Choice D reason:
Neurotoxicity is not a common adverse effect of cyclophosphamide, an alkylating agent that is used to treat ovarian cancer. Neurotoxicity may be caused by other drugs, such as vincristine and paclitaxel, which are used to treat other types of cancer.
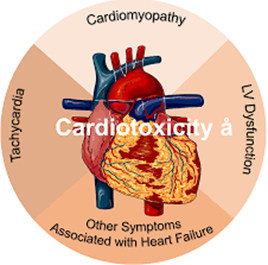
A nurse is caring for a client who is receiving doxorubicin, an anthracycline, as part of chemotherapy for breast cancer. The nurse should monitor the client for which of the following adverse effects of doxorubicin that can be reduced by dexrazoxane, a chemoprotective agent? (Select all that apply.)
Explanation
Choice A reason:
Bone marrow suppression is a common and potentially serious adverse effect of doxorubicin, an anthracycline that intercalates into DNA and inhibits the enzyme topoisomerase II, resulting in DNA damage and cell death. Doxorubicin is used to treat breast cancer, a type of cancer that affects the breast tissue. Bone marrow suppression can cause leukopenia, anemia, and thrombocytopenia, which can increase the risk of infection, bleeding, and fatigue. Dexrazoxane, a chemoprotective agent, does not prevent bone marrow suppression caused by doxorubicin. The nurse should monitor the client's blood counts regularly and provide supportive care as needed.
Choice B reason:
Cardiotoxicity is a rare but serious adverse effect of doxorubicin, an anthracycline that is used to treat breast cancer. Cardiotoxicity can cause acute or chronic heart failure, arrhythmias, and myocardial infarction. Cardiotoxicity is caused by the formation of free radicals that damage the cardiac muscle cells. Dexrazoxane, a chemoprotective agent, can reduce cardiotoxicity caused by doxorubicin. Dexrazoxane is an iron chelator that scavenges free radicals and protects the heart from oxidative stress. The nurse should monitor the client's cardiac function before and during treatment with doxorubicin and administer dexrazoxane as prescribed.
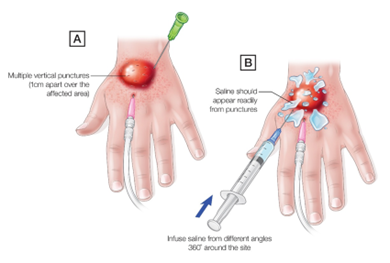
Choice C reason:
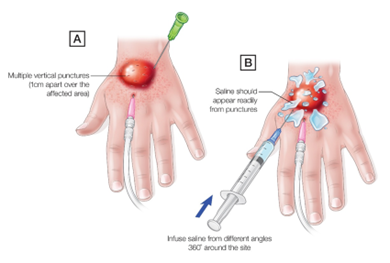
Extravasation injury is a rare but serious adverse effect of doxorubicin, an anthracycline that is used to treat breast cancer. Extravasation injury is leakage of the drug into the surrounding tissue, which can cause severe pain, swelling, blistering, necrosis, and ulceration. Extravasation injury is caused by the vesicant property of doxorubicin, which means that it can cause tissue damage if it escapes from the vein. Dexrazoxane, a chemoprotective agent, can reduce extravasation injury caused by doxorubicin. Dexrazoxane can prevent or limit tissue damage by inhibiting the enzyme topoisomerase II in the skin cells. The nurse should monitor the infusion site carefully and stop the infusion immediately if extravasation occurs. The nurse should also administer dexrazoxane as prescribed and follow the institutional protocol for extravasation management.
Choice D reason:
Alopecia is a common and usually mild adverse effect of doxorubicin, an anthracycline that is used to treat breast cancer. Alopecia is hair loss that can affect the scalp, eyebrows, eyelashes, and body hair. Alopecia is caused by the cytotoxic effect of doxorubicin on the hair follicles. Dexrazoxane, a chemoprotective agent, does not prevent alopecia caused by doxorubicin. The nurse should provide emotional support to the client and educate them on how to cope with hair loss, such as using wigs, hats, scarves, or makeup.
Choice E reason:
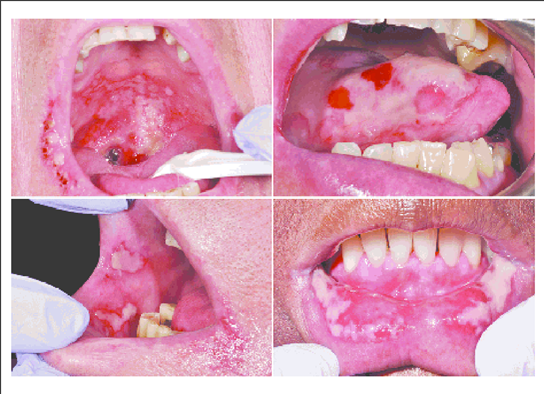
Mucositis is a common and potentially serious adverse effect of doxorubicin, an anthracycline that is used to treat breast cancer. Mucositis is inflammation and ulceration of the mucous membranes that line the mouth, throat, esophagus, stomach, and intestines. Mucositis can cause pain, difficulty swallowing, nausea, vomiting, diarrhea, and infection. Mucositis is caused by the cytotoxic effect of doxorubicin on the rapidly dividing cells of the mucous membranes. Dexrazoxane, a chemoprotective agent, does not prevent mucositis caused by doxorubicin. The nurse should assess the client's oral cavity regularly and provide oral hygiene as needed. The nurse should also advise the client to avoid spicy, acidic, or hot foods and drinks; use a soft toothbrush; rinse with saline or baking soda solution; and use topical analgesics or mouthwashes as prescribed.
A nurse is caring for a client who is receiving cisplatin, a platinum compound, as part of chemotherapy for lung cancer. The nurse should administer amifostine, a chemoprotective agent, to the client to protect which of the following organs from nephrotoxicity caused by cisplatin?
Explanation
Choice A reason:
The liver is not the organ that is protected by amifostine, a chemoprotective agent, from nephrotoxicity caused by cisplatin, a platinum compound that crosslinks DNA strands and prevents cell division. Cisplatin is used to treat lung cancer, a type of cancer that affects the respiratory system. The liver is not the primary target of cisplatin's toxicity, although it can cause hepatotoxicity in some cases. Amifostine does not prevent hepatotoxicity caused by cisplatin.
Choice B reason:
The kidneys are the organ that is protected by amifostine, a chemoprotective agent, from nephrotoxicity caused by cisplatin, a platinum compound that is used to treat lung cancer. Nephrotoxicity is a common and potentially serious adverse effect of cisplatin, which can cause acute or chronic renal failure, electrolyte imbalance, and metabolic acidosis. Nephrotoxicity is caused by the accumulation of cisplatin and its metabolites in the renal tubules, which leads to tubular damage and dysfunction. Amifostine can prevent or reduce nephrotoxicity caused by cisplatin. Amifostine is a prodrug that is converted to an active form by alkaline phosphatase in the normal tissues, but not in the tumor tissues. The active form of amifostine scavenges free radicals and protects the renal cells from oxidative stress.
Choice C reason:
The heart is not the organ that is protected by amifostine, a chemoprotective agent, from nephrotoxicity caused by cisplatin, a platinum compound that is used to treat lung cancer. The heart is not the primary target of cisplatin's toxicity, although it can cause cardiotoxicity in some cases. Amifostine does not prevent cardiotoxicity caused by cisplatin.
Choice D reason:
The lungs are not the organ that is protected by amifostine, a chemoprotective agent, from nephrotoxicity caused by cisplatin, a platinum compound that is used to treat lung cancer. The lungs are the primary site of action of cisplatin, as it kills the lung cancer cells. Amifostine does not protect the lung cancer cells from cisplatin's cytotoxic effect, as it does not reach them in its active form. Amifostine does not prevent pulmonary toxicity caused by cisplatin.
A nurse is educating a client who has colon cancer and is receiving chemotherapy that causes anemia. The nurse should explain to the client that epoetin alfa, a bone marrow stimulant, works by:
Explanation
Choice A reason:
Increasing the number of red blood cells in your blood is the mechanism of action of epoetin alfa, a bone marrow stimulant that is used to treat anemia caused by chemotherapy. Epoetin alfa is a synthetic form of erythropoietin, a hormone that stimulates the production of red blood cells in the bone marrow. Red blood cells are the cells that carry oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs. By increasing the number of red blood cells, epoetin alfa can improve the oxygencarrying capacity of the blood and reduce the symptoms of anemia, such as fatigue, weakness, and pallor.
Choice B reason:
Increasing the amount of iron in your blood is not the mechanism of action of epoetin alfa, a bone marrow stimulant that is used to treat anemia caused by chemotherapy. Iron is a mineral that is essential for the synthesis of hemoglobin, a protein that binds oxygen in the red blood cells. Iron deficiency can cause anemia, but it is not the main cause of anemia in clients receiving chemotherapy. Epoetin alfa does not increase the amount of iron in the blood, but it may increase the demand for iron, as more red blood cells are produced. The client may need to take iron supplements along with epoetin alfa to prevent iron deficiency.
Choice C reason:
Increasing the amount of oxygen in your blood is not the mechanism of action of epoetin alfa, a bone marrow stimulant that is used to treat anemia caused by chemotherapy. Oxygen is a gas that is inhaled from the air and diffuses into the blood through the lungs. The amount of oxygen in the blood depends on several factors, such as the atmospheric pressure, the respiratory rate, and the ventilationperfusion ratio. Epoetin alfa does not increase the amount of oxygen in the blood directly, but it can increase the oxygencarrying capacity of the blood indirectly, by increasing the number of red blood cells.
Choice D reason:
Increasing the number of platelets in your blood is not the mechanism of action of epoetin alfa, a bone marrow stimulant that is used to treat anemia caused by chemotherapy. Platelets are cell fragments that are involved in blood clotting and hemostasis. Thrombocytopenia is a condition that causes low platelet count and increases the risk of bleeding. Thrombocytopenia can be caused by chemotherapy, but it is not treated by epoetin alfa. Epoetin alfa does not increase the number of platelets in the blood, but it may increase the risk of thrombosis, as more red blood cells can make the blood more viscous. The client may need to take anticoagulant drugs along with epoetin alfa to prevent thrombosis.
A nurse is administering filgrastim, a bone marrow stimulant, to a client who has leukemia and is receiving chemotherapy that causes neutropenia. The nurse should monitor the client for which of the following adverse effects of filgrastim?
Explanation
Choice A reason:
Hypertension and headache are not common adverse effects of filgrastim, a bone marrow stimulant that is used to treat neutropenia caused by chemotherapy. Filgrastim is a synthetic form of granulocyte colonystimulating factor (GCSF), a hormone that stimulates the production of neutrophils, a type of white blood cell that fights infection, in the bone marrow. Hypertension and headache may be caused by other factors, such as stress, pain, or dehydration.
Choice B reason:
Diarrhea and abdominal pain are not common adverse effects of filgrastim, a bone marrow stimulant that is used to treat neutropenia caused by chemotherapy. Diarrhea and abdominal pain may be caused by other drugs, such as antibiotics or antineoplastic agents, that affect the gastrointestinal tract.
Choice C reason:
Fever and flulike symptoms are common and usually mild adverse effects of filgrastim, a bone marrow stimulant that is used to treat neutropenia caused by chemotherapy. Fever and flulike symptoms can occur because filgrastim stimulates the immune system and causes the release of cytokines, which are substances that mediate inflammation and immune response. The client should report these symptoms to the provider and receive appropriate treatment, such as acetaminophen, fluids, and rest.
Choice D reason:
Bleeding and bruising are not common adverse effects of filgrastim, a bone marrow stimulant that is used to treat neutropenia caused by chemotherapy. Bleeding and bruising may be caused by thrombocytopenia, a condition that causes low platelet count and increases the risk of bleeding. Thrombocytopenia can be caused by chemotherapy, but it is not treated by filgrastim. Filgrastim does not increase the number of platelets in the blood, but it may increase the risk of splenic rupture, as more white blood cells can enlarge the spleen. The client should have their platelet count and spleen size monitored regularly and report any signs of bleeding or abdominal pain.
Nursing Interventions
A nurse is preparing to administer chemotherapy to a patient who has lung cancer. Which of the following laboratory tests should the nurse review before giving the chemotherapy drugs?
Explanation
Choice A reason:
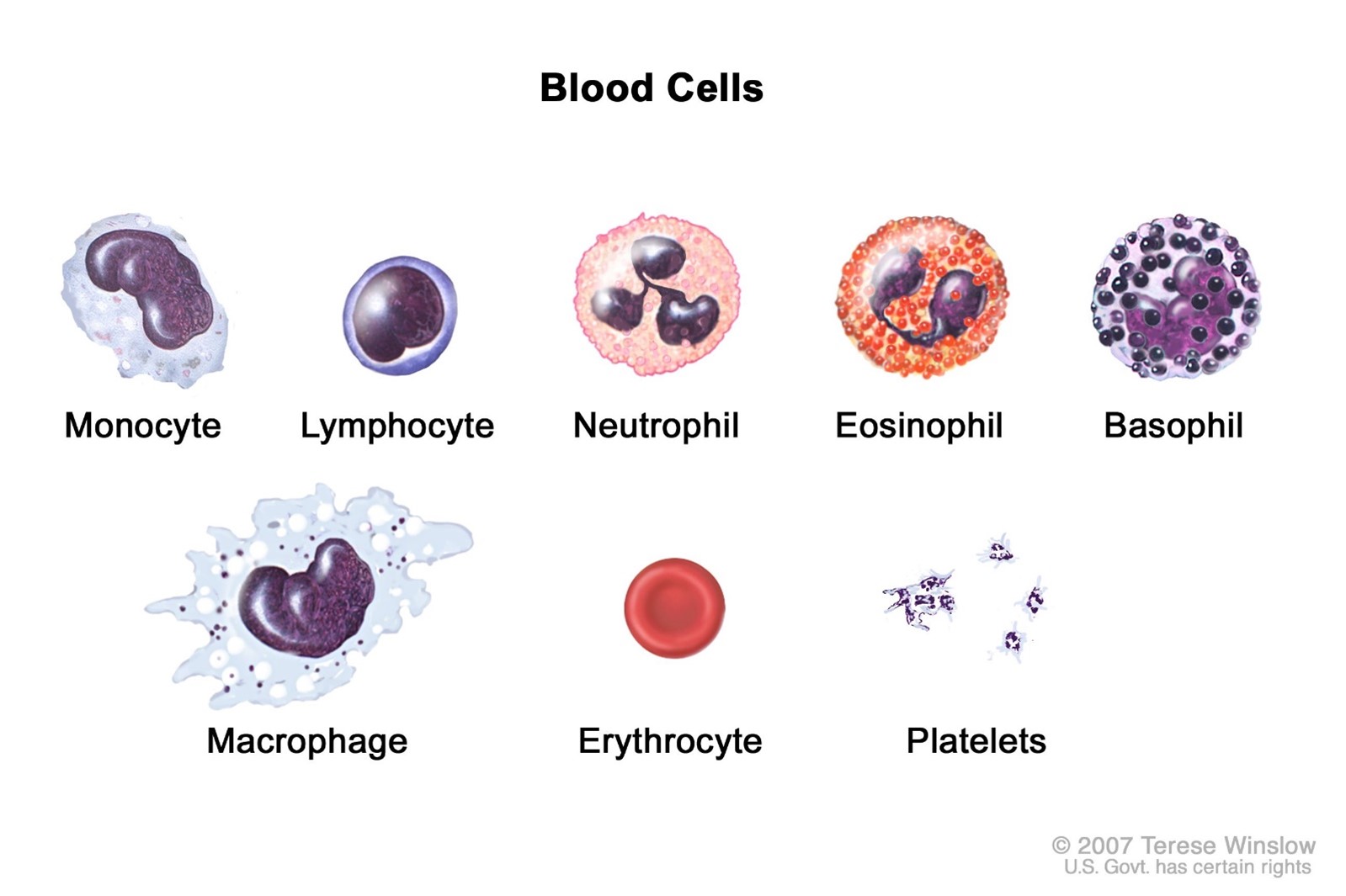
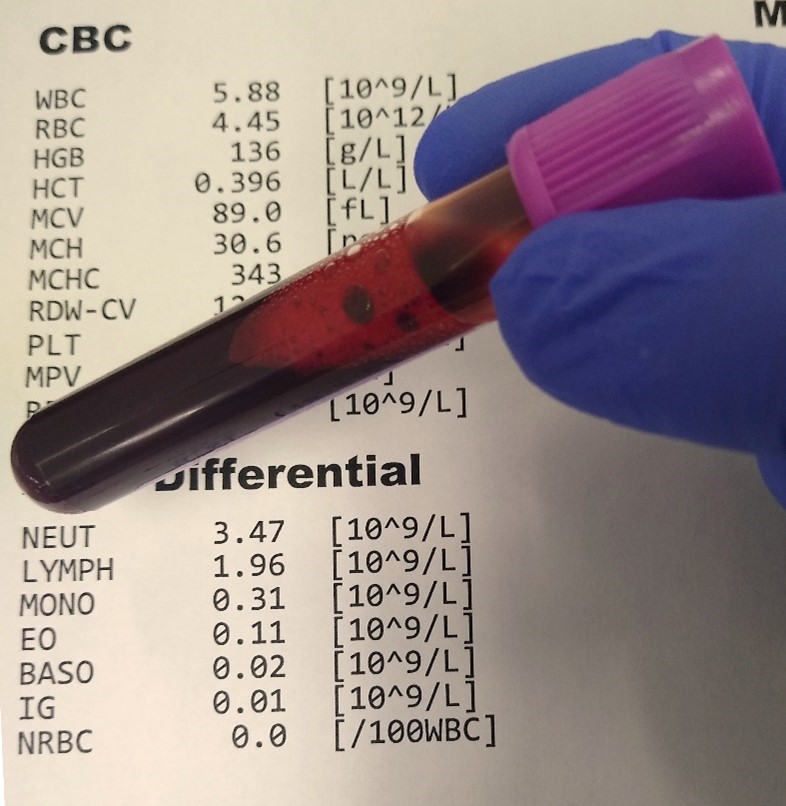
The nurse should review the complete blood count and differential before administering chemotherapy to a patient who has lung cancer. The complete blood count and differential measure the number and types of blood cells, such as red blood cells, white blood cells, and platelets. Chemotherapy drugs can cause bone marrow suppression, which can result in anemia, leukopenia, and thrombocytopenia. These conditions can increase the risk of infection, bleeding, and fatigue. The nurse should compare the patient's blood counts with the normal values and the provider's orders and report any abnormalities or contraindications to the provider.
Choice B reason:
The nurse should review the serum electrolytes and blood urea nitrogen before administering chemotherapy to a patient who has lung cancer. The serum electrolytes measure the levels of sodium, potassium, chloride, and bicarbonate in the blood. The blood urea nitrogen measures the amount of urea nitrogen, a waste product of protein metabolism, in the blood. Chemotherapy drugs can cause nephrotoxicity, which can impair the kidney's function and cause electrolyte imbalance, dehydration, and metabolic acidosis. The nurse should compare the patient's serum electrolytes and blood urea nitrogen with the normal values and the provider's orders and report any abnormalities or contraindications to the provider.
Choice C reason:
The nurse should review the liver function tests and serum bilirubin before administering chemotherapy to a patient who has lung cancer. The liver function tests measure the levels of enzymes and proteins that reflect the liver's function, such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), albumin, and total protein. The serum bilirubin measures the level of bilirubin, a pigment that is produced by the breakdown of red blood cells, in the blood. Chemotherapy drugs can cause hepatotoxicity, which can damage the liver cells and impair the liver's function. The nurse should compare the patient's liver function tests and serum bilirubin with the normal values and the provider's orders and report any abnormalities or contraindications to the provider.
Choice D reason:
All of the above laboratory tests are important to review before administering chemotherapy to a patient who has lung cancer. Chemotherapy drugs can cause various adverse effects that affect different organs and systems in the body. The nurse should monitor the patient's laboratory values closely and adjust the dosage or frequency of chemotherapy drugs as prescribed by the provider. The nurse should also provide supportive care and education to the patient to prevent or manage the adverse effects of chemotherapy.
A nurse is administering chemotherapy to a patient who has colon cancer via an intravenous (IV) line. The nurse should monitor the IV site closely for signs of extravasation, which is:
Explanation
Choice A reason:
This is the definition of extravasation, which is a rare but serious complication of intravenous chemotherapy. Extravasation can cause tissue damage or necrosis, especially if the drug is a vesicant (a highly toxic substance that causes blisters). The nurse should monitor the IV site closely for signs of extravasation, such as tingling, burning, swelling, redness, or discomfort. If extravasation occurs, the nurse should stop the infusion immediately and follow the appropriate protocol to minimize the harm.
Choice B reason:
This is the definition of thrombophlebitis, which is inflammation of a vein due to a blood clot. Thrombophlebitis can occur as a complication of IV therapy, but it is not the same as extravasation. The nurse should monitor the IV site for signs of thrombophlebitis, such as redness, warmth, and tenderness along the vein. If thrombophlebitis occurs, the nurse should discontinue the IV line and apply warm compresses to the affected area³.
Choice C reason:
This is the definition of infiltration, which is the leakage of fluid into the tissues due to a dislodged or punctured IV catheter. Infiltration can cause edema, pallor, and decreased skin temperature around the IV site. Infiltration can also occur as a complication of IV therapy, but it is not as serious as extravasation. The nurse should monitor the IV site for signs of infiltration, such as swelling, coolness, or dampness. If infiltration occurs, the nurse should stop the infusion and remove the IV line³.
Choice D reason:
This is the definition of occlusion, which is the blockage of an IV catheter by a precipitate (a solid substance that forms when two solutions are mixed). Occlusion can cause reduced or absent flow rate and increased pressure in the IV line. Occlusion can also occur as a complication of IV therapy, but it is not related to extravasation. The nurse should monitor the IV line for signs of occlusion, such as difficulty in flushing or infusing fluids. If occlusion occurs, the nurse should try to clear the catheter by flushing with saline or heparin³.
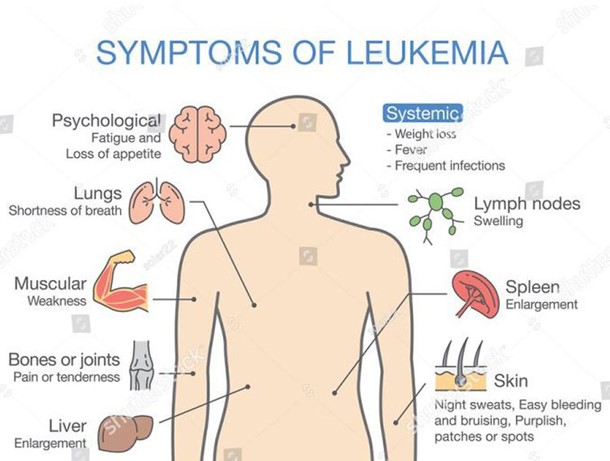
A nurse is caring for a patient who has leukemia and is receiving chemotherapy that causes bone marrow suppression. The nurse should assess the patient for which of the following manifestations that indicate bone marrow suppression?
Explanation
Choice B reason:
These are signs of infection, which can occur when the bone marrow is suppressed and cannot produce enough white blood cells to fight off germs. White blood cells are part of the immune system and help protect the body from infections. A low white blood cell count is called neutropenia, and it increases the risk of developing serious infections that may require hospitalization or antibiotics. The nurse should assess the patient for fever, chills, sore throat, or any other symptoms of infection and report them to the provider immediately³.
Choice A reason:
These are common side effects of chemotherapy, but they are not directly related to bone marrow suppression. Nausea, vomiting, and diarrhea can occur due to the effects of chemotherapy on the digestive system or the brain. They can also cause dehydration and electrolyte imbalance, which can affect the blood cells. The nurse should assess the patient for nausea, vomiting, and diarrhea and provide antiemetics, fluids, and electrolytes as ordered.
Choice C reason:
These are also common side effects of chemotherapy, but they are not directly related to bone marrow suppression. Hair loss, dry skin, and brittle nails can occur due to the effects of chemotherapy on the cells that produce hair and skin. They can also affect the patient's selfesteem and body image. The nurse should assess the patient for hair loss, dry skin, and brittle nails and provide supportive care and education.
Choice D reason:
These are signs of a cardiac problem, such as a heart attack or an arrhythmia. They are not directly related to bone marrow suppression. However, some chemotherapy drugs can affect the heart and cause cardiotoxicity, which can lead to heart failure or damage. The nurse should assess the patient for chest pain, dyspnea, and palpitations and report them to the provider immediately.
A nurse is providing supportive care to a patient who has lymphoma and is receiving chemotherapy that causes mucositis. The nurse should implement which of the following interventions to help the patient with mucositis?
Explanation
Choice D reason:
These are all interventions that can help the patient with mucositis, which is inflammation and ulceration of the mucous membranes in the mouth and throat. Mucositis can occur as a side effect of chemotherapy or radiotherapy that affects the rapidly dividing cells in the oral cavity. Mucositis can cause pain, difficulty swallowing, increased risk of infection, and reduced quality of life³.
Choice A reason:
Encouraging oral hygiene with a soft toothbrush or sponge and a mild mouthwash or saline solution can help prevent or reduce mucositis by keeping the mouth clean and moist. Oral hygiene can also prevent bacterial growth and infection in the mouth. The nurse should instruct the patient to avoid alcoholbased mouthwashes, as they can irritate the mucous membranes³.
Choice B reason:
Administering topical anesthetics or analgesics as prescribed can help relieve pain and discomfort caused by mucositis. Topical agents can numb the mouth and throat and allow the patient to eat and drink more comfortably. Systemic analgesics may also be needed for severe pain. The nurse should assess the patient's pain level and administer pain relief as ordered³.
Choice C reason:
Offering soft, bland, moist foods and fluids at room temperature or cooler can help the patient with mucositis by avoiding further irritation of the mucous membranes. Soft foods are easier to swallow and less likely to cause bleeding or damage to the ulcers. Bland foods are less likely to cause a burning sensation or inflammation. Moist foods and fluids can keep the mouth hydrated and prevent dryness. Room temperature or cooler foods and fluids can soothe the mouth and throat and reduce swelling³.
Conclusion
A nurse is caring for a patient who is receiving chemotherapy for lung cancer. The nurse should explain to the patient that chemotherapy is a type of treatment that:
Explanation
Choice B reason:
This is the definition of chemotherapy, which is a type of cancer treatment that uses drugs to kill cancer cells or slow down their growth. Chemotherapy drugs work by targeting the cell cycle, which is the process of cell division and replication. Cancer cells have an abnormal cell cycle that allows them to grow and multiply faster than normal cells. Chemotherapy drugs can interfere with different stages of the cell cycle and prevent cancer cells from completing it. This causes the cancer cells to die or stop growing³.
Choice A reason:
This is the definition of radiotherapy, which is another type of cancer treatment that uses highenergy radiation, such as Xrays or gamma rays, to destroy cancer cells and shrink tumors. Radiotherapy works by damaging the DNA of cancer cells, which prevents them from dividing and growing. Radiotherapy can be given externally or internally, depending on the location and size of the tumor.
Choice C reason:
This is the definition of immunotherapy, which is a newer type of cancer treatment that uses substances that stimulate the body's immune system to fight cancer cells and prevent metastasis. Immunotherapy works by enhancing the natural ability of the immune system to recognize and destroy cancer cells, or by providing artificial immune system components, such as antibodies or cytokines, that can target specific molecules on cancer cells.
Choice D reason:
This is the definition of targeted therapy, which is another newer type of cancer treatment that uses drugs that target specific molecules on cancer cells and block their growth and survival signals. Targeted therapy works by interfering with the pathways or processes that are essential for cancer cells to grow, spread, or resist other treatments. Targeted therapy drugs are often used in combination with other treatments, such as chemotherapy or immunotherapy.
A nurse is reviewing the medication orders for a patient who is receiving chemotherapy for breast cancer. The nurse should identify that some chemotherapy drugs are classified as cytotoxic, meaning that they: (Select all that apply.)
Explanation
Choice A reason:
Directly kill cancer cells or inhibit their replication. This is one of the main characteristics of cytotoxic drugs, which are drugs that destroy cells or prevent them from dividing. Cytotoxic drugs work by interfering with the cell cycle, which is the process of cell division and replication. Cancer cells have an abnormal cell cycle that allows them to grow and multiply faster than normal cells. Cytotoxic drugs can target different stages of the cell cycle and prevent cancer cells from completing it. This causes the cancer cells to die or stop growing.
Choice D reason:
Cause damage to normal cells that are rapidly dividing. This is one of the main side effects of cytotoxic drugs, which are not selective for cancer cells only. Cytotoxic drugs can also affect normal cells that are rapidly dividing, such as those in the bone marrow, hair follicles, gastrointestinal tract, and reproductive organs. This can cause symptoms such as anemia, hair loss, nausea, vomiting, diarrhea, infertility, and increased risk of infection.
Choice E reason:
Enhance the recovery of blood cells after chemotherapyinduced damage. This is one of the main benefits of cytotoxic drugs, which can help restore the normal function of the bone marrow after chemotherapy. Cytotoxic drugs can stimulate the production of blood cells, such as red blood cells, white blood cells, and platelets, which are essential for oxygen transport, immune response, and clotting. Cytotoxic drugs can also reduce the risk of bleeding and infection in patients who have low blood cell counts due to chemotherapy.
Choice B reason:
Selectively target specific molecules or pathways involved in cancer growth or evasion of the immune system. This is not a characteristic of cytotoxic drugs, but rather of targeted therapy drugs, which are another type of cancer treatment. Targeted therapy drugs work by interfering with specific molecules or pathways that are essential for cancer cells to grow, spread, or resist other treatments. Targeted therapy drugs are often used in combination with cytotoxic drugs or other treatments.
Choice C reason:
Protect normal cells from the toxic effects of chemotherapy drugs. This is not a characteristic of cytotoxic drugs, but rather of cytoprotective drugs, which are another type of cancer treatment. Cytoprotective drugs work by reducing the damage caused by cytotoxic drugs to normal cells and tissues. Cytoprotective drugs can also prevent or treat some of the side effects of cytotoxic drugs, such as nausea, vomiting, mouth sores, kidney damage, and nerve damage.
A nurse is administering chemotherapy to a patient who has colon cancer. The nurse should monitor the patient for which of the following adverse effects that are common to most chemotherapy drugs?
Explanation
Choice A reason:
These are two of the most common adverse effects of chemotherapy, which are caused by the damage to normal cells that are rapidly dividing. Bone marrow suppression is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. Gastrointestinal toxicity is the damage to the cells lining the mouth, stomach, and intestines. This can cause mouth sores, nausea, vomiting, diarrhea, and loss of appetite³.
Choice B reason:
These are not common adverse effects of most chemotherapy drugs, but rather of specific drugs that can affect the heart and lungs. Cardiotoxicity is the damage to the heart muscle or valves, which can cause heart failure or arrhythmias. Pulmonary fibrosis is the scarring of the lung tissue, which can cause shortness of breath and coughing. These adverse effects are more likely to occur with drugs such as anthracyclines (doxorubicin) and bleomycin.
Choice C reason:
These are not common adverse effects of most chemotherapy drugs, but rather of specific drugs that can affect the nerves and skin. Peripheral neuropathy is the damage to the nerves in the hands and feet, which can cause numbness, tingling, burning, or pain. Skin reactions are the changes in the skin appearance or texture, such as rash, dryness, or sensitivity. These adverse effects are more likely to occur with drugs such as taxanes (paclitaxel) and platinum drugs (cisplatin).
Choice D reason:
These are not common adverse effects of most chemotherapy drugs, but rather of specific drugs that can affect the kidneys and ears. Nephrotoxicity is the damage to the kidney cells or function, which can cause reduced urine output, swelling, or electrolyte imbalance. Ototoxicity is the damage to the inner ear or hearing nerve, which can cause hearing loss or ringing in the ears. These adverse effects are more likely to occur with drugs such as cisplatin and aminoglycosides (amikacin).
A nurse is educating a patient who has leukemia and is receiving chemotherapy about the use of filgrastim, a bone marrow stimulant, as part of the treatment. The nurse should tell the patient that filgrastim works by:
Explanation
Choice C reason:
This is the main function of filgrastim, which is a synthetic (manmade) form of a substance that is naturally produced in your body called a colony stimulating factor. Filgrastim helps the bone marrow to make new white blood cells, especially neutrophils, which are the most common type of white blood cells and play a key role in fighting infections. Filgrastim is used to treat neutropenia, which is a low level of neutrophils that can be caused by chemotherapy or other conditions. Filgrastim can reduce the risk of infection and the need for antibiotics in patients with neutropenia³.
Choice A reason:
This is not a function of filgrastim, but rather of cytoprotective drugs, which are another type of cancer treatment. Cytoprotective drugs work by protecting the kidneys from the harmful effects of chemotherapy drugs, such as cisplatin, which can cause nephrotoxicity (kidney damage). Cytoprotective drugs can prevent or treat nephrotoxicity by increasing urine output, binding to toxic substances, or providing antioxidants⁴.
Choice B reason:
This is not a function of filgrastim, but rather of erythropoietin, which is another type of colony stimulating factor. Erythropoietin stimulates the production of red blood cells in the bone marrow. Erythropoietin is used to treat anemia, which is a low level of red blood cells that can be caused by chemotherapy or other conditions. Erythropoietin can increase the oxygencarrying capacity of the blood and reduce the need for blood transfusions in patients with anemia⁵.
Choice D reason:
This is not a function of filgrastim, but rather of thrombopoietin, which is another type of colony stimulating factor. Thrombopoietin stimulates the production of platelets in the bone marrow. Platelets are cell fragments that help with blood clotting and prevent bleeding. Thrombopoietin is used to treat thrombocytopenia, which is a low level of platelets that can be caused by chemotherapy or other conditions. Thrombopoietin can reduce the risk of bleeding and bruising in patients with thrombocytopenia.
A nurse is providing supportive care to a patient who has lymphoma and is receiving chemotherapy that causes alopecia. The nurse should implement which of the following interventions to help the patient cope with alopecia?
Explanation
Choice D reason:
These are all interventions that can help the patient cope with alopecia, which is hair loss caused by chemotherapy. Alopecia is one of the most common and distressing side effects of chemotherapy, as it can affect the patient's selfesteem, body image, and social interactions. Alopecia is usually temporary and reversible, but it can take several months for the hair to grow back³.
Choice A reason:
Encouraging the patient to wear a wig, hat, scarf, or turban to cover the scalp can help the patient cope with alopecia by providing warmth, comfort, and protection from sun exposure. It can also help the patient feel more confident and attractive. The patient should choose a head covering that suits their personal style and preference. Some insurance companies may cover the cost of a wig if it is prescribed by a doctor³.
Choice B reason:
Advising the patient to avoid washing, brushing, or combing the hair excessively can help the patient cope with alopecia by reducing the amount of hair loss and breakage. The patient should use gentle hair care products and avoid harsh chemicals, heat, or styling tools. The patient should also avoid tight hairstyles or accessories that can pull or damage the hair³.
Choice C reason:
Suggesting the patient to cut the hair short before chemotherapy or shave the head after hair loss begins can help the patient cope with alopecia by giving them a sense of control and preparation. Cutting or shaving the hair can also make the hair loss less noticeable and easier to manage. The patient should consult with their doctor before cutting or shaving their hair, as some chemotherapy drugs may cause scalp sensitivity or irritation³.
More Questions
A nurse is caring for a client who has lung cancer and is receiving combination chemotherapy with cisplatin and etoposide. Which of the following interventions should the nurse implement to prevent nephrotoxicity from cisplatin?
Explanation
Choice D reason:
These are all interventions that can prevent nephrotoxicity from cisplatin, which is a potent and valuable chemotherapy drug that can cause kidney damage or failure. Nephrotoxicity is one of the most serious and doselimiting adverse effects of cisplatin, which can affect up to 30% of patients. Nephrotoxicity is caused by the accumulation of cisplatin in the renal tubular cells, leading to cell injury, inflammation, and ischemia³.
Choice A reason:
Administering mannitol as prescribed before cisplatin infusion can prevent nephrotoxicity by increasing urine output and reducing the concentration of cisplatin in the kidney. Mannitol is an osmotic diuretic that draws water from the extracellular space into the tubular lumen, thereby increasing urine volume and flow rate. Mannitol can also scavenge free radicals and reduce oxidative stress induced by cisplatin⁴.
Choice B reason:
Monitoring serum creatinine and blood urea nitrogen levels daily can prevent nephrotoxicity by detecting early signs of renal impairment and adjusting the dose of cisplatin accordingly. Serum creatinine and blood urea nitrogen are markers of kidney function that reflect the glomerular filtration rate (GFR). An increase in these levels indicates a decrease in GFR and a loss of kidney function. The dose of cisplatin should be reduced or withheld if serum creatinine or blood urea nitrogen levels rise above a certain threshold⁴.
Choice C reason:
Encouraging fluid intake of at least 3 L per day during treatment can prevent nephrotoxicity by maintaining adequate hydration and preventing dehydration. Hydration is essential for preventing cisplatininduced renal toxicity, as it dilutes the concentration of cisplatin in the kidney and enhances its elimination. Dehydration can increase the risk of nephrotoxicity by reducing renal blood flow and causing tubular obstruction by uric acid crystals. Fluid intake can be oral or intravenous, depending on the patient's condition⁴.
A nurse is caring for a client who has breast cancer and is receiving doxorubicin, cyclophosphamide, and paclitaxel as adjuvant chemotherapy. The nurse should monitor the client for cardiotoxicity from doxorubicin by assessing for which of the following signs and symptoms?
Explanation
Choice A reason:
These are signs of cardiotoxicity from doxorubicin, which is a potent anthracycline chemotherapy drug that can cause damage to the heart muscle or valves. Cardiotoxicity is one of the most serious and doselimiting adverse effects of doxorubicin, which can affect up to 20% of patients. Cardiotoxicity can manifest as acute or chronic heart failure, arrhythmias, or myocardial infarction. The nurse should monitor the client for chest pain, dyspnea, palpitations, and edema, which indicate reduced cardiac function and fluid overload. The nurse should also measure the client's blood pressure, heart rate, oxygen saturation, and electrocardiogram (ECG) regularly³.
Choice B reason:
These are common side effects of chemotherapy, but they are not directly related to cardiotoxicity from doxorubicin. Nausea, vomiting, diarrhea, and abdominal pain can occur due to the effects of chemotherapy on the digestive system or the brain. They can also cause dehydration and electrolyte imbalance, which can affect the heart function. The nurse should assess the client for nausea, vomiting, diarrhea, and abdominal pain and provide antiemetics, fluids, and electrolytes as ordered.
Choice C reason:
These are not common signs of cardiotoxicity from doxorubicin, but rather of peripheral neuropathy from paclitaxel, which is another chemotherapy drug that is used in combination with doxorubicin and cyclophosphamide for breast cancer. Peripheral neuropathy is the damage to the nerves in the hands and feet, which can cause numbness, tingling, burning, or pain. Peripheral neuropathy can affect the client's quality of life and ability to perform daily activities. The nurse should assess the client for peripheral neuropathy and provide pain relief and supportive care as needed.
Choice D reason:
These are not common signs of cardiotoxicity from doxorubicin, but rather of infection from bone marrow suppression caused by chemotherapy. Bone marrow suppression is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. Infection can occur when the white blood cell count is low and the immune system is weakened. The nurse should monitor the client for fever, chills, sore throat, and mouth ulcers, which indicate infection and report them to the provider immediately.
A nurse is caring for a client who has lymphoma and is receiving vincristine, prednisone, and rituximab as induction chemotherapy. The nurse should identify that vincristine can cause neurotoxicity and instruct the client to report which of the following manifestations?
Explanation
Choice D reason:
These are manifestations of neurotoxicity from vincristine, which is a chemotherapy drug that belongs to the vinca alkaloids. Vinca alkaloids work by binding to tubulin and inhibiting the formation of microtubules, which are essential for cell division and function. Neurotoxicity is one of the most common and doselimiting adverse effects of vincristine, which can affect up to 80% of patients. Neurotoxicity can manifest as peripheral neuropathy, which is the damage to the nerves in the hands and feet, causing numbness, tingling, burning, or pain. The nurse should monitor the client for peripheral neuropathy and provide pain relief and supportive care as needed³.
Choice A reason:
These are not manifestations of neurotoxicity from vincristine, but rather of paralytic ileus from vincristine. Paralytic ileus is the loss of intestinal motility, causing constipation, urinary retention, and abdominal distension. Paralytic ileus is another common adverse effect of vincristine, which can affect up to 40% of patients. Paralytic ileus is caused by the inhibition of microtubules in the smooth muscle cells of the intestine and bladder, leading to reduced peristalsis and urine flow. The nurse should monitor the client for paralytic ileus and provide laxatives, catheterization, and fluids as ordered⁴.
Choice B reason:
These are not manifestations of neurotoxicity from vincristine, but rather of ototoxicity from cisplatin, which is another chemotherapy drug that is used in combination with vincristine and prednisone for lymphoma. Ototoxicity is the damage to the inner ear or hearing nerve, causing hearing loss, tinnitus, and vertigo. Ototoxicity is one of the most serious and doselimiting adverse effects of cisplatin, which can affect up to 50% of patients. Ototoxicity is caused by the accumulation of cisplatin in the cochlea and vestibular system, leading to oxidative stress and cell death. The nurse should monitor the client for ototoxicity and provide hearing tests and vestibular rehabilitation as needed .
Choice C reason:
These are not manifestations of neurotoxicity from vincristine, but rather of ocular toxicity from rituximab, which is another chemotherapy drug that is used in combination with vincristine and prednisone for lymphoma. Ocular toxicity is the damage to the eyes or vision, causing blurred vision, photophobia, and eye irritation. Ocular toxicity is a rare but serious adverse effect of rituximab, which can affect up to 1% of patients. Ocular toxicity is caused by the infusionrelated reactions or immunemediated reactions induced by rituximab, leading to inflammation and edema in the eyes. The nurse should monitor the client for ocular toxicity and provide eye drops and steroids as ordered .
A nurse is caring for a client who has leukemia and is receiving cytarabine, an antimetabolite, as part of chemotherapy. Which of the following laboratory tests should the nurse monitor for adverse effects of this drug?
Explanation
Choice C reason:
This is the laboratory test that the nurse should monitor for adverse effects of cytarabine, which is an antimetabolite chemotherapy drug that works by slowing or stopping the growth of cancer cells. The main adverse effect of cytarabine is bone marrow suppression, which is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. The nurse should monitor the complete blood count and differential, which measure the number and type of blood cells in a sample of blood. The nurse should report any abnormal results to the provider and provide supportive care as ordered³.
Choice A reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of cisplatin, which is another chemotherapy drug that can cause kidney damage or failure. Cisplatin can accumulate in the kidney cells and cause oxidative stress and cell death. The nurse should monitor the serum creatinine and blood urea nitrogen levels, which are markers of kidney function that reflect the glomerular filtration rate (GFR). An increase in these levels indicates a decrease in GFR and a loss of kidney function. The nurse should report any abnormal results to the provider and provide fluids and electrolytes as ordered⁴.
Choice B reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of amphotericin B, which is an antifungal drug that can cause electrolyte imbalance. Amphotericin B can affect the transport of sodium and potassium across cell membranes and cause renal tubular acidosis. The nurse should monitor the serum potassium and magnesium levels, which are important electrolytes for nerve and muscle function. A decrease in these levels can cause muscle weakness, cramps, arrhythmias, and seizures. The nurse should report any abnormal results to the provider and provide supplements as ordered .
Choice D reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of methotrexate, which is another antimetabolite chemotherapy drug that can cause liver damage or failure. Methotrexate can interfere with the metabolism of folate and cause accumulation of toxic metabolites in the liver cells. The nurse should monitor the serum bilirubin and liver enzyme levels, which are markers of liver function that reflect the liver's ability to process bilirubin and other substances. An increase in these levels indicates liver injury or inflammation. The nurse should report any abnormal results to the provider and provide folinic acid as ordered .
A nurse is caring for a client who has ovarian cancer and is receiving vincristine, a natural product, as part of chemotherapy. Which of the following interventions should the nurse implement to prevent constipation from vincristine?
Explanation
Choice C reason:
This is the laboratory test that the nurse should monitor for adverse effects of cytarabine, which is an antimetabolite chemotherapy drug that works by slowing or stopping the growth of cancer cells. The main adverse effect of cytarabine is bone marrow suppression, which is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. The nurse should monitor the complete blood count and differential, which measure the number and type of blood cells in a sample of blood. The nurse should report any abnormal results to the provider and provide supportive care as ordered³.
Choice A reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of cisplatin, which is another chemotherapy drug that can cause kidney damage or failure. Cisplatin can accumulate in the kidney cells and cause oxidative stress and cell death. The nurse should monitor the serum creatinine and blood urea nitrogen levels, which are markers of kidney function that reflect the glomerular filtration rate (GFR). An increase in these levels indicates a decrease in GFR and a loss of kidney function. The nurse should report any abnormal results to the provider and provide fluids and electrolytes as ordered⁴.
Choice B reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of amphotericin B, which is an antifungal drug that can cause electrolyte imbalance. Amphotericin B can affect the transport of sodium and potassium across cell membranes and cause renal tubular acidosis. The nurse should monitor the serum potassium and magnesium levels, which are important electrolytes for nerve and muscle function. A decrease in these levels can cause muscle weakness, cramps, arrhythmias, and seizures. The nurse should report any abnormal results to the provider and provide supplements as ordered .
Choice D reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of methotrexate, which is another antimetabolite chemotherapy drug that can cause liver damage or failure. Methotrexate can interfere with the metabolism of folate and cause accumulation of toxic metabolites in the liver cells. The nurse should monitor the serum bilirubin and liver enzyme levels, which are markers of liver function that reflect the liver's ability to process bilirubin and other substances. An increase in these levels indicates liver injury or inflammation. The nurse should report any abnormal results to the provider and provide folinic acid as ordered .
A nurse is caring for a client who has colon cancer and is receiving dactinomycin, an antineoplastic antibiotic, as part of chemotherapy. The nurse should identify that dactinomycin can cause which of the following adverse effects? (Select all that apply.)
Explanation
Choice A reason:
Bone marrow suppression is an adverse effect of dactinomycin, which is an antineoplastic antibiotic that works by binding to DNA and inhibiting RNA synthesis. Bone marrow suppression is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. The nurse should monitor the complete blood count and differential, which measure the number and type of blood cells in a sample of blood. The nurse should report any abnormal results to the provider and provide supportive care as ordered³.
Choice B reason:
Skin reactions are an adverse effect of dactinomycin, which can cause inflammation, rash, acne, erythema multiforme, or increased pigmentation of previously irradiated skin. Skin reactions can occur due to the direct toxicity of dactinomycin on the skin cells or due to the hypersensitivity or allergic reactions induced by dactinomycin. The nurse should monitor the skin appearance and texture and report any changes to the provider. The nurse should also provide skin care and topical agents as ordered³.
Choice E reason:
Extravasation injury is an adverse effect of dactinomycin, which can occur when the drug leaks out of the vein into the surrounding tissue during intravenous infusion. Extravasation injury can cause severe pain, swelling, redness, blistering, ulceration, or necrosis of the affected tissue. The nurse should monitor the infusion site and stop the infusion immediately if extravasation occurs. The nurse should also elevate the affected limb and apply cold compresses as ordered. The nurse should consult with the provider for further management of extravasation injury³.
Choice C reason:
Cardiotoxicity is not an adverse effect of dactinomycin, but rather of doxorubicin, which is another antineoplastic antibiotic that can cause damage to the heart muscle or valves. Cardiotoxicity can manifest as acute or chronic heart failure, arrhythmias, or myocardial infarction. The nurse should monitor the blood pressure, heart rate, oxygen saturation, and electrocardiogram (ECG) regularly and report any abnormal findings to the provider .
Choice D reason:
Pulmonary fibrosis is not an adverse effect of dactinomycin, but rather of bleomycin, which is another antineoplastic antibiotic that can cause scarring of the lung tissue. Pulmonary fibrosis can manifest as shortness of breath, coughing, or reduced lung function. The nurse should monitor the respiratory rate, breath sounds, and chest xray regularly and report any abnormal findings to the provider .
A nurse is caring for a client who has breast cancer and is receiving trastuzumab, a monoclonal antibody, as part of targeted therapy. Which of the following assessments should the nurse perform before and during the infusion of this drug?
Explanation
Choice A reason:
Blood pressure and pulse should be monitored before and during the infusion of trastuzumab, as this drug can cause cardiomyopathy and heart failure in some patients. These are serious side effects that can affect the heart's ability to pump blood effectively.
Choice B reason:
Respiratory rate and oxygen saturation should be monitored before and during the infusion of trastuzumab, as this drug can cause infusion reactions and pulmonary toxicity in some patients³. These are serious side effects that can affect the lungs' ability to exchange oxygen and carbon dioxide.
Choice C reason:
Temperature and skin condition should be monitored before and during the infusion of trastuzumab, as this drug can cause fever, chills, rash, and infection in some patients. These are common side effects that can indicate an allergic reaction or an infection.
Choice D reason:
All of the above assessments should be performed before and during the infusion of trastuzumab, as this drug can cause various side effects that can affect the heart, lungs, skin, and immune system of the patient. The nurse should also monitor for other signs and symptoms such as nausea, vomiting, diarrhea, headache, cough, sore throat, etc. The nurse should report any abnormal findings to the doctor and intervene as needed.
A nurse is caring for a client who has chronic myeloid leukemia (CML) and is receiving imatinib, a tyrosine kinase inhibitor, as part of targeted therapy. Which of the following laboratory tests should the nurse monitor for adverse effects of this drug?
Explanation
Choice A reason:
Liver function tests should be monitored for adverse effects of imatinib, as this drug can cause hepatotoxicity and liver failure in some patients³⁴. These are serious side effects that can affect the liver's ability to metabolize drugs and toxins.
Choice B reason:
Serum electrolytes are not directly affected by imatinib, as this drug does not cause significant changes in sodium, potassium, calcium, or magnesium levels³. However, electrolyte imbalances may occur due to other factors such as dehydration, diarrhea, vomiting, or kidney problems.
Choice C reason:
Coagulation studies are not directly affected by imatinib, as this drug does not cause significant changes in prothrombin time, partial thromboplastin time, or international normalized ratio³. However, bleeding disorders may occur due to other factors such as thrombocytopenia, anemia, or vascular damage.
Choice D reason:
Liver function tests are the only laboratory tests that should be monitored for adverse effects of imatinib, as this drug can cause serious liver damage in some patients. The other tests are not directly affected by imatinib, but may be influenced by other factors or conditions. The nurse should also monitor for other signs and symptoms such as nausea, vomiting, diarrhea, rash, edema, fatigue, infection, etc. The nurse should report any abnormal findings to the doctor and intervene as needed.

A nurse is caring for a client who has multiple myeloma and is receiving thalidomide, an angiogenesis inhibitor, as part of targeted therapy. The nurse should instruct the client to report which of the following adverse effects of this drug? (Select all that apply.)
Explanation
Choice A reason:
Numbness, tingling, or pain in the extremities are signs of peripheral neuropathy, which is a common and serious side effect of thalidomide³. This condition can affect the nerves that control sensation and movement in the arms and legs, and can lead to permanent nerve damage if not treated.
Choice B reason:
Drowsiness, dizziness, or confusion are signs of central nervous system depression, which is a common and serious side effect of thalidomide³. This condition can affect the brain's ability to regulate alertness, cognition, and coordination, and can increase the risk of falls, accidents, and injuries.
Choice C reason:
Constipation, nausea, or vomiting are signs of gastrointestinal distress, which is a common and mild side effect of thalidomide. This condition can affect the digestive system's ability to process food and fluids, and can lead to dehydration, malnutrition, and electrolyte imbalance if not managed.
Choice D reason:
Swelling, redness, or warmth in the legs are not directly related to thalidomide use, but may indicate a deep vein thrombosis (DVT), which is a blood clot that forms in a vein deep in the body. Thalidomide can increase the risk of DVT by affecting the blood's ability to clot normally. A DVT can be lifethreatening if it breaks off and travels to the lungs, causing a pulmonary embolism.
Choice E reason:
Rash, itching, or hives are signs of allergic reaction, which is a rare but serious side effect of thalidomide³. This condition can affect the skin's immune response to the drug, and can lead to severe skin reactions such as StevensJohnson syndrome or toxic epidermal necrolysis if not treated.
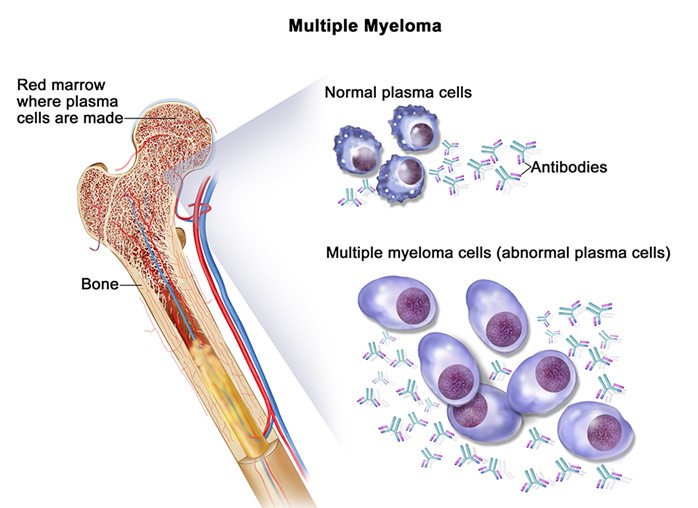
A nurse is caring for a client who has lymphoma and is receiving chemotherapy that causes thrombocytopenia. Which of the following drugs should the nurse administer to the client to stimulate the production of platelets in the bone marrow?
Explanation
Choice A reason:
Epoetin alfa (Epogen) is a drug that stimulates the production of red blood cells in the bone marrow, not platelets⁴. It is used to treat anemia caused by chemotherapy, chronic kidney disease, or other conditions.
Choice B reason:
Filgrastim (Neupogen) is a drug that stimulates the production of white blood cells in the bone marrow, not platelets⁴. It is used to prevent or treat neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice C reason:
Sargramostim (Leukine) is a drug that stimulates the production of white blood cells and red blood cells in the bone marrow, not platelets⁴. It is used to prevent or treat neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice D reason:
Oprelvekin (Neumega) is a drug that stimulates the production of platelets in the bone marrow⁴. It is used to prevent or treat thrombocytopenia caused by chemotherapy. It works by mimicking the action of thrombopoietin, a hormone that regulates platelet development.
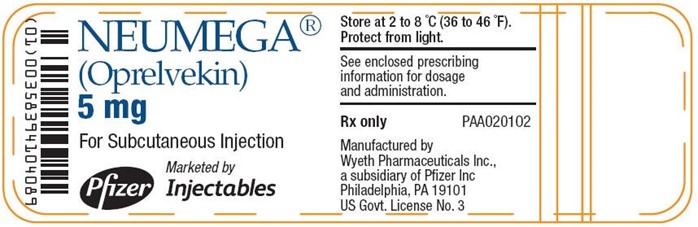
A nurse is caring for a client who has prostate cancer and is receiving chemotherapy that causes anemia and neutropenia. The nurse should identify that which of the following drugs can be used to treat both conditions by stimulating the production of red blood cells and neutrophils in the bone marrow? (Select all that apply.)
Explanation
Choice A reason:
Epoetin alfa (Epogen) is a drug that stimulates the production of red blood cells in the bone marrow, but not neutrophils. It is used to treat anemia caused by chemotherapy, chronic kidney disease, or other conditions.
Choice B reason:
Filgrastim (Neupogen) is a drug that stimulates the production of neutrophils in the bone marrow, but not red blood cells. It is used to prevent or treat neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice C reason:
Sargramostim (Leukine) is a drug that stimulates the production of both red blood cells and neutrophils in the bone marrow. It is used to prevent or treat anemia and neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice D reason:
Pegfilgrastim (Neulasta) is a drug that stimulates the production of both red blood cells and neutrophils in the bone marrow⁴. It is a longacting form of filgrastim that works in the same way but can be given less often. It is used to prevent or treat anemia and neutropenia caused by chemotherapy.
Choice E reason:
Darbepoetin alfa (Aranesp) is a drug that stimulates the production of red blood cells in the bone marrow, but not neutrophils. It is a longacting form of epoetin alfa that works in the same way but can be given less often. It is used to treat anemia caused by chemotherapy, chronic kidney disease, or other conditions.
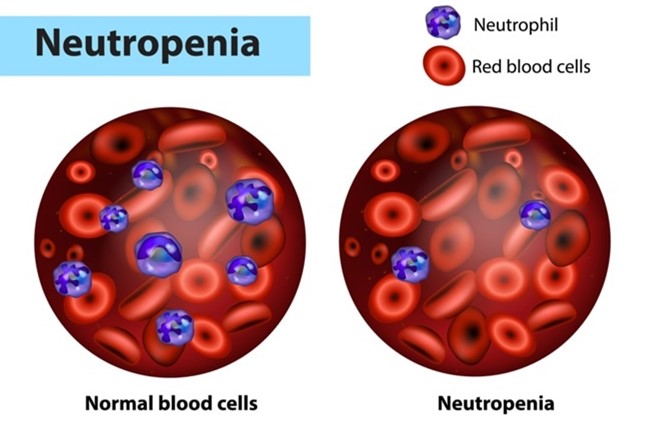
A nurse is caring for a patient who has cervical cancer and is receiving chemotherapy that causes anemia and fatigue. The nurse should instruct the patient to report which of the following manifestations that indicate anemia and fatigue? (Select all that apply.)
Explanation
Choice A reason:
Pallor and weakness are signs of anemia, as they indicate a low level of hemoglobin or red blood cells that carry oxygen to the tissues. Pallor is the loss of color in the skin, especially in the face, nails, and inside of the eyelids. Weakness is the feeling of having less energy or strength than usual.
Choice B reason:
Dizziness and headache are signs of anemia, as they indicate a low level of oxygen in the brain. Dizziness is the feeling of being lightheaded or unsteady. Headache is the pain or discomfort in the head, scalp, or neck.
Choice C reason:
Shortness of breath and tachycardia are signs of anemia, as they indicate a low level of oxygen in the lungs and heart. Shortness of breath is the feeling of not being able to breathe enough or catch your breath. Tachycardia is the abnormally fast or irregular heartbeat.
Choice D reason:
Constipation and abdominal pain are not directly related to anemia or fatigue, but may indicate other conditions such as dehydration, bowel obstruction, or infection. Constipation is the difficulty or infrequency in passing stools. Abdominal pain is the pain or discomfort in the stomach or belly area.
Choice E reason:
Difficulty sleeping and concentrating are not directly related to anemia or fatigue, but may indicate other conditions such as stress, depression, or anxiety. Difficulty sleeping is the trouble falling asleep or staying asleep. Difficulty concentrating is the trouble focusing on tasks or remembering things.
A nurse is caring for a patient who has cervical cancer and is receiving combination chemotherapy with doxorubicin and cyclophosphamide. Which of the following interventions should the nurse implement to prevent cardiotoxicity from doxorubicin?
Explanation
Choice A reason:
Administering dexrazoxane as prescribed before doxorubicin infusion can help prevent cardiotoxicity by inhibiting the formation of DNA doublestrand breaks mediated by topoisomerase II beta, which is a key mechanism of doxorubicininduced cardiac damage³. Dexrazoxane is a chelating agent that binds to iron and prevents the generation of reactive oxygen species that can cause oxidative stress and DNA damage⁴. Dexrazoxane is the only drug approved by the Food and Drug Administration (FDA) for the prevention of doxorubicin cardiotoxicity in patients with metastatic breast cancer who have received a cumulative dose of 300 mg/m2 or more⁵.
Choice B reason:
Monitoring electrocardiogram (ECG) and cardiac enzymes during treatment can help detect cardiotoxicity from doxorubicin, but not prevent it. ECG can show changes such as ST segment depression, T wave inversion, arrhythmias, or conduction abnormalities that indicate cardiac ischemia or injury. Cardiac enzymes such as troponin and creatine kinaseMB (CKMB) can show elevation that indicates myocardial damage or necrosis.
Choice C reason:
Assessing for signs and symptoms of heart failure such as dyspnea, edema, and crackles can help diagnose cardiotoxicity from doxorubicin, but not prevent it. Dyspnea is the difficulty or discomfort in breathing that indicates reduced cardiac output or pulmonary congestion. Edema is the swelling of the lower extremities or abdomen that indicates fluid retention or rightsided heart failure. Crackles are the abnormal lung sounds that indicate pulmonary edema or leftsided heart failure.
Choice D reason:
Administering dexrazoxane as prescribed before doxorubicin infusion is the only intervention that can prevent cardiotoxicity from doxorubicin. Monitoring ECG and cardiac enzymes during treatment and assessing for signs and symptoms of heart failure can help detect and treat cardiotoxicity, but not prevent it. Other strategies that may help prevent doxorubicin cardiotoxicity include limiting the cumulative dose of doxorubicin to less than 450 to 550 mg/m2, administering the drug as an infusion rather than an injection, using a liposomal formulation of doxorubicin, and using other agents with antioxidant or antiinflammatory properties⁴.
A nurse is caring for a patient who has prostate cancer and is receiving combination chemotherapy with docetaxel and prednisone. The nurse should instruct the patient to report which of the following adverse effects that indicate peripheral neuropathy? (Select all that apply.)
No explanation
Exams on Chemotherapy Agents and Oncology Pharmacology
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define chemotherapy and its goals, types, and mechanisms of action.
- Identify the major groups of chemotherapeutic agents and their indications, adverse effects, and nursing interventions.
- Explain the role of targeted therapy and immunotherapy in oncology and their benefits and challenges.
- Describe the use of chemoprotective agents and bone marrow stimulants in cancer treatment and their implications for nursing care.
- Apply the principles of safe handling, administration, and disposal of chemotherapy drugs.
Introduction
- Chemotherapy is the use of drugs to treat cancer by killing or inhibiting the growth of cancer cells.
- Chemotherapy can be used alone or in combination with other modalities such as surgery, radiation, biologic therapies, or targeted drug therapy.
- The goals of chemotherapy are to control the growth of cancer cells, achieve long-term survival or cure, or palliate symptoms, and improve quality of life.
- Chemotherapy can be classified into different types based on the timing, frequency, route, or purpose of administration. Some examples are:
- Adjuvant chemotherapy: given after surgery or radiation to eliminate any remaining cancer cells and prevent recurrence.
- Neoadjuvant chemotherapy: given before surgery or radiation to shrink the tumor and make it easier to remove or treat.
- Induction chemotherapy: given as the first line treatment to induce remission or reduce tumor burden.
- Maintenance chemotherapy: given after induction or remission to prevent relapse or progression.
- Salvage chemotherapy: given after failure of previous treatments to control advanced or refractory disease.
- Palliative chemotherapy: given to relieve symptoms and improve quality of life in incurable or terminal cases.
- Chemotherapy drugs act by interfering with the cell cycle, DNA synthesis, or cell division of cancer cells. However, they also affect normal cells that are rapidly dividing, such as those in the bone marrow, gastrointestinal tract, hair follicles, and reproductive organs. This causes various adverse effects such as:
- Bone marrow suppression: leads to anemia, leukopenia, thrombocytopenia, and increased risk of infection, bleeding, and fatigue.
- Gastrointestinal toxicity: leads to nausea, vomiting, diarrhea, constipation, mucositis, stomatitis, anorexia, and weight loss.
- Alopecia: leads to hair loss on the scalp and other body parts.
- Reproductive toxicity: leads to infertility, amenorrhea, oligospermia, teratogenicity, and sexual dysfunction.
- Other organ-specific toxicities: affect the liver, kidneys, heart, lungs, nervous system, skin, nails, eyes, ears, etc.
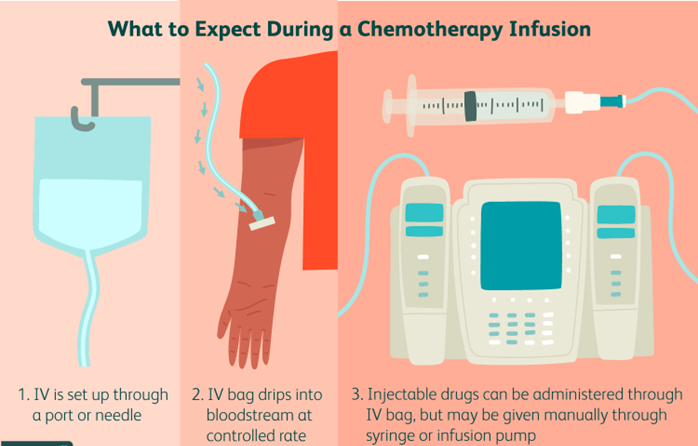
Cytotoxic Chemotherapy Drugs
- Cytotoxic chemotherapy drugs are traditional agents that directly kill cancer cells or inhibit their replication. They are classified into several major groups based on their chemical structure and mechanism of action. Some examples are:
- Alkylating agents: bind to DNA and crosslink strands, preventing DNA replication and transcription. Examples are cisplatin, cyclophosphamide, busulfan, etc. They are used for various solid tumors and hematologic malignancies. They can cause bone marrow suppression, nephrotoxicity, ototoxicity, neurotoxicity, hemorrhagic cystitis, etc.
- Antimetabolites: mimic natural metabolites and interfere with DNA synthesis or function. Examples are methotrexate, 5fluorouracil, cytarabine, etc. They are used for various solid tumors and hematologic malignancies. They can cause bone marrow suppression, gastrointestinal toxicity, hepatotoxicity, neurotoxicity, etc.
- Natural products: derived from natural sources such as plants or microorganisms and inhibit cell division (mitosis) or DNA synthesis. Examples are paclitaxel, vincristine, doxorubicin, etc. They are used for various solid tumors and hematologic malignancies. They can cause bone marrow suppression, peripheral neuropathy, cardiotoxicity, extravasation injury, etc.
- Antineoplastic antibiotics: derived from microorganisms and bind to DNA or RNA and inhibit their synthesis or function. Examples are dactinomycin, bleomycin, mitomycin C, etc. They are used for various solid tumors and hematologic malignancies. They can cause bone marrow suppression, pulmonary fibrosis, skin reactions, etc.
- Hormones: modulate the activity of hormonedependent tumors by blocking or stimulating hormone receptors or altering hormone synthesis. Examples are tamoxifen, leuprolide, prednisone, etc. They are used for breast, prostate, and endometrial cancers. They can cause menopausal symptoms, osteoporosis, hyperglycemia, etc.
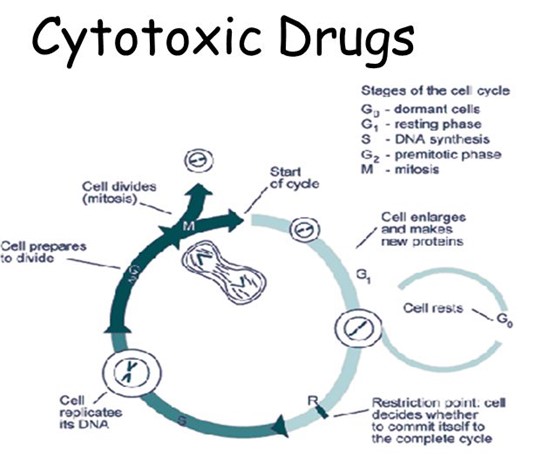
Targeted Therapy and Immunotherapy in Oncology
- Targeted therapy and immunotherapy are newer modalities that use biologic agents to selectively target specific molecules or pathways involved in cancer growth, survival, or evasion of the immune system. They have the potential to improve efficacy and reduce toxicity compared to cytotoxic chemotherapy drugs. Some examples are:
- Monoclonal antibodies: engineered proteins that bind to specific antigens on cancer cells or other molecules and trigger immune-mediated destruction, block growth signals, or deliver cytotoxic agents. Examples are rituximab, trastuzumab, cetuximab, etc. They are used for various solid tumors and hematologic malignancies. They can cause infusion reactions, allergic reactions, cardiotoxicity, etc.
- Tyrosine kinase inhibitors: small molecules that inhibit the activity of tyrosine kinases, which are enzymes that mediate intracellular signaling pathways involved in cell growth, survival, angiogenesis, and metastasis. Examples are imatinib, erlotinib, sunitinib, etc. They are used for various solid tumors and hematologic malignancies. They can cause gastrointestinal toxicity, hepatotoxicity, skin rash, etc.
- Angiogenesis inhibitors: agents that inhibit the formation of new blood vessels that supply oxygen and nutrients to tumors. Examples are bevacizumab, sorafenib, thalidomide, etc. They are used for various solid tumors and hematologic malignancies. They can cause hypertension, bleeding, thrombosis, etc.
- Immunomodulators: agents that enhance the immune system's ability to recognize and eliminate cancer cells. Examples are interferons, interleukins, vaccines, etc. They are used for various solid tumors and hematologic malignancies. They can cause flu-like symptoms, bone marrow suppression, autoimmune disorders, etc.
- Checkpoint inhibitors: agents that block the inhibitory signals that cancer cells use to evade the immune system's attack. Examples are ipilimumab, nivolumab, pembrolizumab, etc. They are used for various solid tumors and hematologic malignancies. They can cause immune-related adverse events such as colitis, hepatitis, pneumonitis, endocrinopathies, etc.
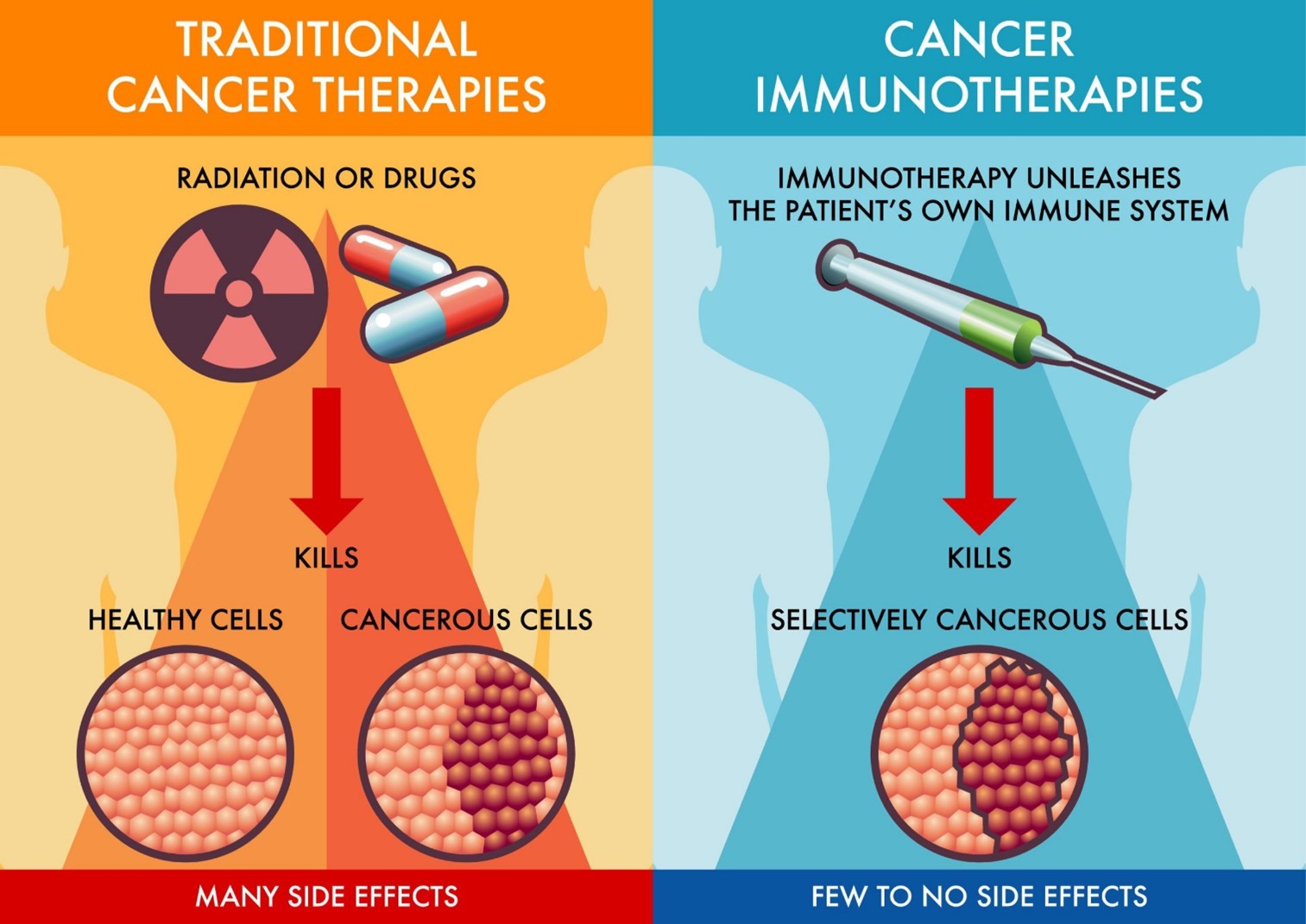
Chemoprotective Agents and Bone Marrow Stimulants
- Chemoprotective agents and bone marrow stimulants are adjunctive agents that are used to reduce the toxic effects of chemotherapy drugs on normal cells or to enhance their recovery after chemotherapyinduced damage.
- Chemoprotective agents are drugs that protect specific organs or tissues from the harmful effects of chemotherapy drugs by scavenging free radicals, inhibiting metabolic activation, enhancing detoxification, or increasing cellular resistance. Some examples are:
- Mesna (Mesnex): protects the bladder from hemorrhagic cystitis caused by cyclophosphamide or ifosfamide by binding to the toxic metabolites and inactivating them.³
- Dexrazoxane (Zinecard): protects the heart from cardiotoxicity caused by doxorubicin or other anthracyclines by chelating iron and preventing free radical formation.³
- Amifostine (Ethyol): protects the kidneys from nephrotoxicity caused by cisplatin or other platinum compounds by scavenging free radicals and enhancing cellular repair.³
- Bone marrow stimulants are drugs that stimulate the production of blood cells in the bone marrow by acting on specific growth factors or receptors. Some examples are:
- Epoetin alfa (Epogen): stimulates the production of red blood cells by binding to erythropoietin receptors on erythroid progenitor cells. It is used to treat chemotherapyinduced anemia.
- Filgrastim (Neupogen): stimulates the production of neutrophils by binding to granulocyte colonystimulating factor receptors on myeloid
- Filgrastim (Neupogen): stimulates the production of neutrophils by binding to granulocyte colony-stimulating factor receptors on myeloid progenitor cells. It is used to prevent or treat chemotherapy-induced neutropenia.
- Sargramostim (Leukine): stimulates the production of granulocytes and monocytes by binding to granulocyte-macrophage colony-stimulating factor receptors on myeloid progenitor cells. It is used to enhance bone marrow recovery after chemotherapy or bone marrow transplantation.
- Oprelvekin (Neumega): stimulates the production of platelets by binding to interleukin11 receptors on megakaryocyte progenitor cells. It is used to prevent or treat chemotherapyinduced thrombocytopenia.
Nursing Interventions
- Nursing interventions for chemotherapy patients include the following:
- Assess the patient's history, physical examination, laboratory tests, and tumor characteristics before, during, and after chemotherapy.
- Educate the patient and family about the chemotherapy regimen, its purpose, benefits, risks, side effects, and management strategies.
- Administer the chemotherapy drugs according to the prescribed protocol, route, dose, schedule, and precautions. Use proper equipment, technique, and personal protective equipment to prevent exposure, extravasation, or contamination.
- Monitor the patient's vital signs, fluid and electrolyte balance, nutritional status, weight, and urine output during and after chemotherapy. Report any signs of toxicity, infection, bleeding, or organ dysfunction.
- Provide supportive care to the patient such as pain management, antiemetics, antidiarrheals, laxatives, mouth care, skin care, hair care, etc. Encourage oral hygiene, hydration, nutrition, rest, and activity as tolerated.
- Teach the patient and family how to prevent or minimize complications such as infection, bleeding, anemia, fatigue, etc. Advise them to avoid crowds, sick people, raw foods, sharp objects, etc. Instruct them to report any fever, chills, sore throat, cough, shortness of breath, chest pain, abdominal pain, blood in urine or stool, bruising, etc.
- Dispose of the chemotherapy drugs and waste materials according to the institutional policies and guidelines. Follow the proper procedures for handling spills or accidents involving chemotherapy drugs.
Conclusion
- Chemotherapy is a major modality of cancer treatment that uses drugs to kill or inhibit cancer cells. It can be used alone or in combination with other modalities such as surgery, radiation, biologic therapies, or targeted drug therapy.
- Chemotherapy drugs can be classified into different types based on their mechanism of action. They include cytotoxic chemotherapy drugs that directly kill cancer cells or inhibit their replication; targeted therapy and immunotherapy that selectively target specific molecules or pathways involved in cancer growth or evasion of the immune system; chemoprotective agents that protect normal cells from the toxic effects of chemotherapy drugs; and bone marrow stimulants that enhance the recovery of blood cells after chemotherapyinduced damage.
- Chemotherapy drugs can cause various adverse effects on normal cells that are rapidly dividing such as those in the bone marrow, gastrointestinal tract, hair follicles, and reproductive organs. They can also affect other organs such as the liver, kidneys, heart, lungs, nervous system, etc. These adverse effects can be prevented or managed by using supportive care, chemoprotective agents, or bone marrow stimulants.
- Nursing interventions for chemotherapy patients include assessing, educating, administering, monitoring, providing supportive care, teaching, and disposing of chemotherapy drugs and waste materials. Nurses play a vital role in ensuring the safety, efficacy, and quality of life of chemotherapy patients.
Summary
- Chemotherapy is the use of drugs to treat cancer by killing or inhibiting cancer cells.
- Chemotherapy can be classified into different types based on the timing, frequency, route, or purpose of administration.
- Chemotherapy drugs can be classified into different groups based on their mechanism of action. They include:
- Cytotoxic chemotherapy drugs: alkylating agents, antimetabolites, natural products, antineoplastic antibiotics, hormones.
- Targeted therapy and immunotherapy: monoclonal antibodies, tyrosine kinase inhibitors, angiogenesis inhibitors, immunomodulators, checkpoint inhibitors.
- Chemoprotective agents: mesna, dexrazoxane, amifostine.
- Bone marrow stimulants: epoetin alfa, filgrastim, sargramostim, oprelvekin.
- Chemotherapy drugs can cause various adverse effects on normal cells and organs. These can be prevented or managed by using supportive care, chemoprotective agents, or bone marrow stimulants.
- Nursing interventions for chemotherapy patients include assessing, educating, administering, monitoring, providing supportive care, teaching, and disposing of chemotherapy drugs and waste materials.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Chemotherapy Agents and Oncology Pharmacology
This filled cannot be empty

