Please set your exam date
PROM and PPROM
Study Questions
Introduction
A nurse is caring for a client who has PPROM at 34 weeks of gestation.
Which of the following interventions should the nurse implement? (Select all that apply.)
Explanation
Continuous fetal heart rate monitoring is indicated for clients who have PPROM to detect signs of fetal distress or infection.
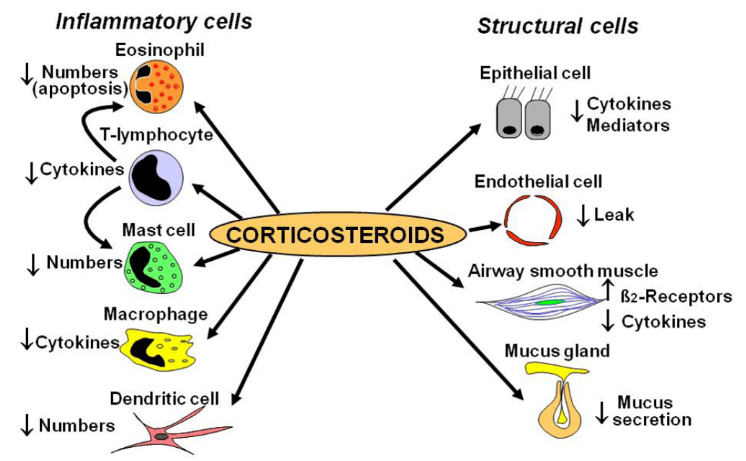
corticosteroids are recommended for clients who have PPROM between 24 and 34 weeks of gestation to enhance fetal lung maturity and reduce the risk of respiratory distress syndrome and other neonatal complications.
A nurse is reviewing the laboratory results of a client who has PROM at 38 weeks of gestation.
Which of the following findings indicates a risk for infection?
Explanation
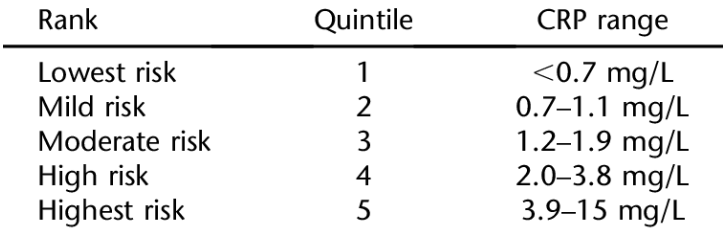
C-reactive protein (CRP) is a marker of inflammation and infection in the body.The normal range of CRP is less than 10 mg/L.A high level of CRP can be caused by bacterial or viral infections, autoimmune disorders, or tissue injury.
A nurse is teaching a client who has PROM about the possible complications for the fetus.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
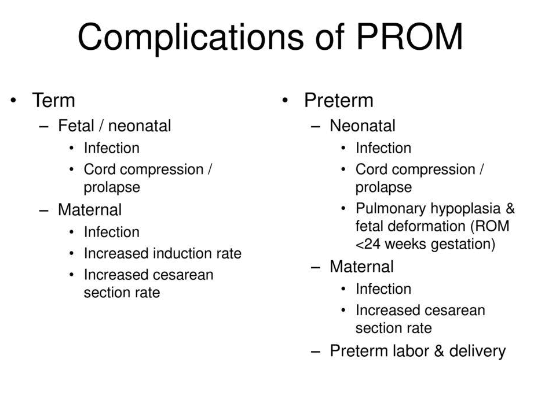
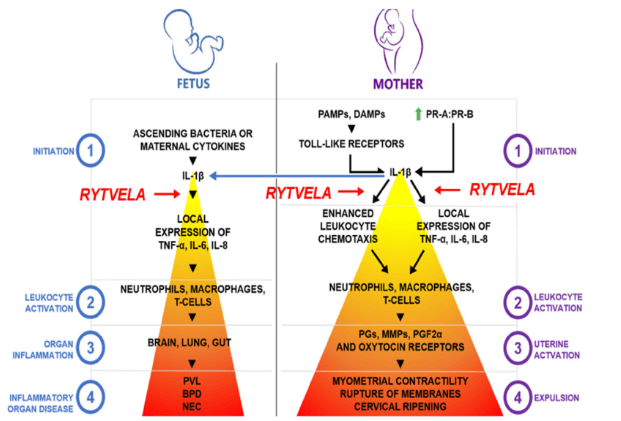
PROM can increase the risk ofintra-amniotic infectionwhich can lead toinflammation of the fetal lungsandrespiratory distress syndrome.
Normal ranges for fetal head circumference vary depending on gestational age and sex, but generally range from about 31 to 40 cm at term.
A nurse is assessing a client who has PPROM at 32 weeks of gestation and is receiving magnesium sulfate infusion for fetal neuroprotection.
Which of the following findings should the nurse report to the provider immediately?
Explanation
This is a sign of magnesium toxicity, which can occur when a client is receiving magnesium sulfate infusion for fetal neuroprotection.
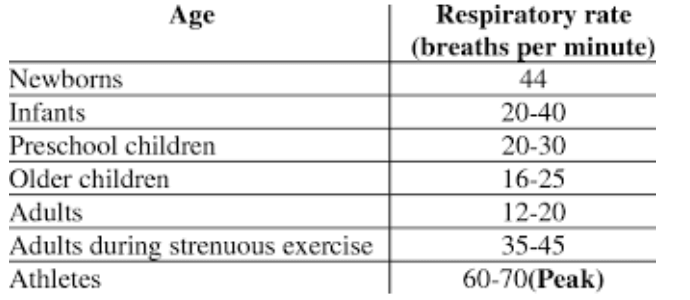
Magnesium sulfate can depress the central nervous system and respiratory system, leading to respiratory depression or arrest.The nurse should report this finding to the provider immediately and stop the infusion.
Causes and risk factors
A nurse is caring for a client who has a history of PROM in a previous pregnancy.
The nurse knows that this client is at a higher risk of developing which complication in the current pregnancy?
Explanation
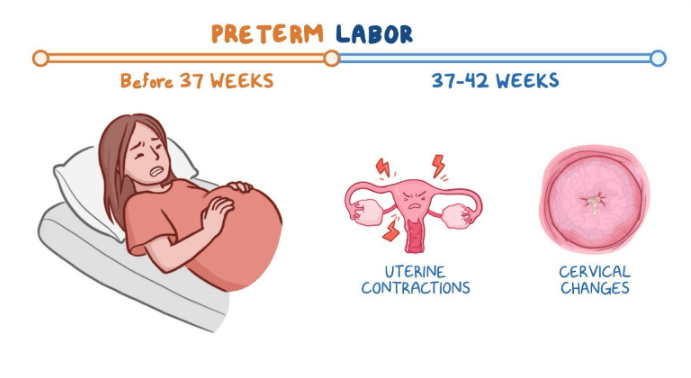
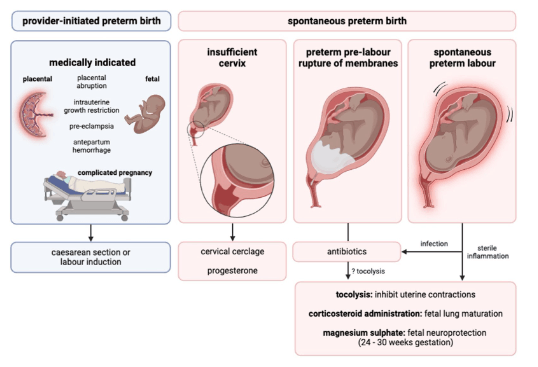
The client who has a history of PROM (premature rupture of membranes) in a previous pregnancy is at a higher risk of developing preterm labor in the current pregnancy.Preterm labor is when the baby is born before 37 weeks of gestation and can cause complications such as respiratory distress, low birth weight and infection.
A nurse is assessing a client who is at 34 weeks of gestation and reports a sudden gush of fluid from the vagina.
The nurse suspects that the client has PPROM.
Which of the following tests should the nurse perform to confirm the diagnosis?
Explanation
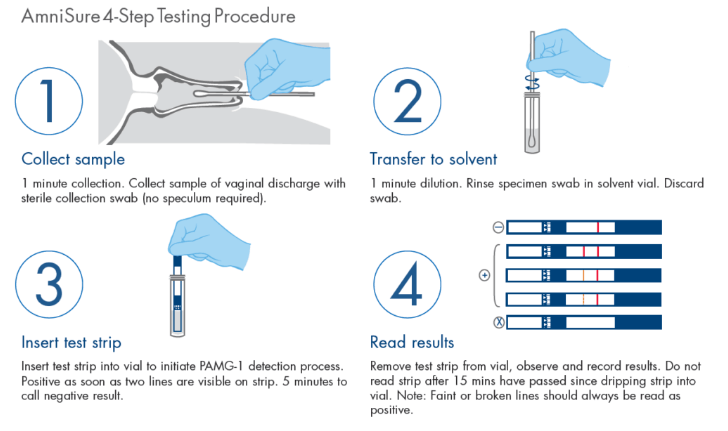
This is a rapid immunoassay test that detects placental alpha microglobulin-1 (PAMG-1) in vaginal fluid, which is a marker of fetal membrane rupture.It has high sensitivity and specificity and can be used in the presence of blood or other contaminants.
A nurse is teaching a pregnant client who smokes about the effects of smoking on the pregnancy.
The nurse should include that smoking increases the risk of which of the following conditions?
Explanation
Smoking increases the risk of various complications for both the mother and the fetus, such as:
• Intrauterine growth restriction: Smoking reduces blood flow and nutrient transfer to the fetus, resulting in small size for gestational age.
• Premature rupture of membranes: Smoking causes maternal vasoconstriction, decreases placental perfusion, and induces uterine contractions, which can lead to early rupture of the amniotic sac.
• Placental abruption: Smoking also increases the risk of placental detachment from the uterine wall, which can cause severe bleeding and fetal distress.
A nurse is reviewing the ultrasound report of a pregnant client who is at 28 weeks of gestation.
The report indicates that the client has polyhydramnios, which is an excess of amniotic fluid.
The nurse should recognize that this condition can cause which of the following complications? (Select all that apply.).
Explanation
Polyhydramnios is a condition where there is too much amniotic fluid in the uterus during pregnancy.This can cause various complications for both the mother and the fetus.
A nurse is caring for a client who has an incompetent cervix and is at 20 weeks of gestation.
The nurse should expect the provider to order which of the following interventions to prevent preterm birth and PPROM?
Explanation
Cerclage placement is a way of keeping the cervix closed during pregnancy to prevent premature birth and PPROM (preterm premature rupture of membranes) due to incompetent (weakened) cervix.A cerclage is the placement of a band or suture for reinforcement to help prevent the amniotic sac from “funneling” down into the cervix prematurely.
Clinical manifestations and Diagnostic tests
A nurse is caring for a client who has PPROM at 32 weeks of gestation.
Which of the following findings should alert the nurse to the possibility of chorioamnionitis?
Explanation
Maternal temperature of 38.2°C (100.8°F).This is because a high maternal temperature is a sign ofchorioamnionitis, which is a serious infection of the placental tissues that can occur in patients withPPROM(preterm premature rupture of membranes).Chorioamnionitis can be very dangerous for both mother and baby and requires immediate treatment with antibiotics and delivery.
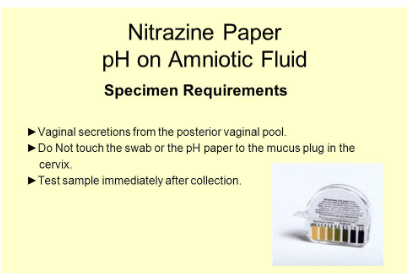
A nurse is performing a nitrazine paper test on a client who reports fluid leaking from the vagina.
The nurse observes that the paper remains yellow after contact with the fluid.
How should the nurse interpret this result?
Explanation
This is because the nitrazine paper test involves putting a drop of fluid obtained from the vagina onto paper strips containing nitrazine dye.
The strips change color depending on the pH of the fluid.The strips will turn blue if the pH is greater than 6.0, which is indicative of amniotic fluid.However, if the paper remains yellow after contact with the fluid, it means the pH is less than 6.0, which is indicative of urine or vaginal secretions.
Normal ranges for pH of vaginal fluid are 3.8 to 4.5, while normal ranges for pH of amniotic fluid are 7.0 to 7.5.
A nurse is reviewing the results of an AmniSure test on a client who has PROM at 36 weeks of gestation.
The test is positive for PAMG-1.
What does this result mean?
Explanation
The client has confirmed membrane rupture.This is because the AmniSure ROM Test detects the presence of PAMG-1 protein in the vaginal discharge of pregnant women, which is a marker of amniotic fluid.A positive test result means that the fetal membranes have ruptured and the amniotic fluid has leaked into the vagina.
A nurse is preparing to perform a ferning test on a client who has PPROM at 28 weeks of gestation.
Which of the following actions should the nurse take?
Explanation
A ferning test is used to detect the presence of amniotic fluid in the vagina, which can indicate preterm premature rupture of membranes (PPROM).To perform the test, the nurse should collect a sample of vaginal fluid with a sterile cotton swab and place it on a glass slide without a cover slip.Then, the nurse should examine the slide under low-power magnification and look for fern-like patterns that form when the fluid dries.
A nurse is assessing a client who has PROM at 34 weeks of gestation.
Which of the following ultrasound findings should the nurse report to the provider?
Explanation
This means that the fetus is positioned with its buttocks or feet towards the cervix, which can increase the risk of complications during delivery.The nurse should report this finding to the provider and prepare for a possible cesarean section.
Nursing interventions and Management
A nurse is preparing a client for an emergency cesarean birth due to umbilical cord prolapse.
Which of the following interventions should the nurse include in the preoperative care? (Select all that apply.).
Explanation
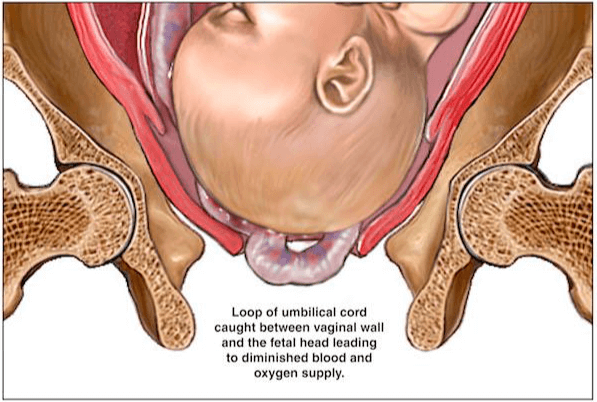
The correct answer is choice A, B and C. These interventions are part of the preoperative care for a client who is undergoing an emergency cesarean birth due to umbilical cord prolapse.Umbilical cord prolapse is a medical emergency that occurs when the umbilical cord slips through the cervix and into the vagina before the baby, causing fetal hypoxia.
Choice D is wrong because performing a leopold maneuver to determine fetal position is not necessary in this situation, as the fetal presentation is already known and the priority is to deliver the baby as soon as possible.
Choice E is wrong because applying an external fetal monitor to assess fetal heart rate is not sufficient in this situation, as the cord compression may cause severe bradycardia or variable decelerations.The nurse should manually lift the presenting part and hold it off the prolapsed cord while preparing for cesarean delivery.
A nurse is caring for a client with PPROM at 32 weeks of gestation.
The client asks the nurse why she needs to take corticosteroids.
The nurse’s best response is:
Explanation
corticosteroids can stimulate the production of surfactant, a substance that prevents the collapse of the alveoli in the lungs, and reduce the risk of respiratory distress syndrome, intraventricular hemorrhage, and neonatal death.
A nurse is performing a sterile speculum examination on a client with suspected PROM at 36 weeks of gestation.
The nurse observes a pool of clear fluid in the vagina.
What is the most appropriate action for the nurse to take next?
Explanation
A nitrazine test is a conventional test that uses pH testing of leaked amniotic fluid.Amniotic fluid is alkaline and turns the nitrazine paper blue, while vaginal secretions are acidic and turn the paper yellow or green.
A nurse is monitoring a client with PROM at 34 weeks of gestation who is receiving tocolytic therapy.
Which of the following findings would indicate a potential adverse effect of the medication?
Explanation
indicates a potential adverse effect of the medication.This could be a sign of infection or inflammation, which are common complications of preterm premature rupture of membranes (PPROM) and can lead to early delivery and neonatal morbidity.Tocolytic therapy aims to prolong the latency period and reduce the risks of prematurity, but it might also prolong fetal exposure to infection.
Normal ranges for maternal vital signs in pregnancy are:
• Heart rate: 60 to 100 beats per minute
• Blood pressure: less than 140/90 mmHg
• Temperature: 36.1°C to 37.2°C (97°F to 99°F)
• Respiratory rate: 16 to 20 breaths per minute
A nurse is educating a client with PPROM at 30 weeks of gestation who is being discharged home on bed rest with bathroom privileges.
Which of the following instructions should the nurse include in the teaching plan? (Select all that apply.).
Explanation
These are the instructions that the nurse should include in the teaching plan for a client with PPROM at 30 weeks of gestation who is being discharged home on bed rest with bathroom privileges.
A nurse is reviewing the laboratory results of a client with PROM at 38 weeks of gestation.
The nurse notes that the client has a positive culture for group B streptococcus.
What is the most likely implication of this finding for the client and the fetus?
Explanation
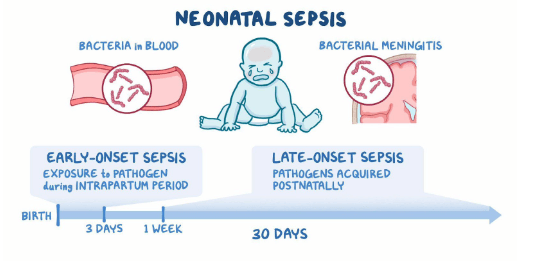
The client will need to receive intravenous antibiotics during labor and delivery to prevent neonatal sepsis.Group B streptococcus (GBS) is a type of bacteria that can be passed from a pregnant person to their baby during vaginal delivery and can cause serious infections in newborns.Antibiotics can significantly reduce the risk of the baby getting ill.
Potential Complications and Outcomes
A nurse is caring for a client who has PPROM at 32 weeks of gestation.
The nurse should monitor the client for which of the following signs of infection? (Select all that apply.).
Explanation
All are signs of infection that can occur in a client who has PPROM at 32 weeks of gestation.
Infection is a serious complication of PPROM that can affect both the mother and the baby.
A client who has PROM at 38 weeks of gestation is admitted to the labor and delivery unit.
The nurse should perform which of the following interventions first?
Explanation
PROM increases the risk of infection, cord compression, and fetal distress, so monitoring the fetal well-being is the priority intervention.
A nurse is teaching a pregnant client about the risk factors for PROM.
Which of the following statements by the client indicates a need for further teaching?
Explanation
Having sex as often as possible does not keep the cervix healthy and may increase the risk of premature rupture of membranes (PROM), which is when the amniotic sac breaks before labor begins.PROM can cause infection, premature birth and other complications for the mother and the baby.
A client who has PPROM at 28 weeks of gestation is receiving magnesium sulfate for fetal neuroprotection.
The nurse should monitor the client for which of the following adverse effects of magnesium sulfate?
Explanation
Magnesium sulfate is a drug that can reduce the risk of cerebral palsy in preterm infants when given to women at risk of early preterm birth.However, it can also cause adverse effects such as respiratory depression, hypotension, hypocalcemia, and loss of deep tendon reflexes in the mother.Therefore, the nurse should monitor the vital signs and reflexes of the woman receiving magnesium sulfate and stop the infusion if signs of toxicity appear.
A nurse is reviewing the electronic fetal monitor tracing of a client who has PROM at 34 weeks of gestation.
The nurse observes variable decelerations in the fetal heart rate.
The nurse should recognize that this finding indicates which of the following?
Explanation
Variable decelerations are abrupt drops in the fetal heart rate below baseline that last 15 seconds to less than two minutes.They are caused by reduced blood flow and oxygen delivery to the fetus due to umbilical cord compression.The onset, depth, and duration of variable decelerations vary with uterine contractions or fetal movement.
Summary
A nurse is teaching a pregnant woman who is at risk for pre-term labor.
Which of the following activities should the nurse instruct the woman to avoid?
Explanation
Sexual intercourse can trigger uterine contractions and increase the risk of preterm labor.
The nurse should instruct the woman to avoid sexual intercourse if she is at risk for preterm labor.
Choice A is wrong because drinking water is important for hydration and preventing dehydration, which can also cause uterine contractions.
Choice B is wrong because taking prenatal vitamins is essential for providing adequate nutrition and preventing deficiencies that can affect fetal development.
Choice D is wrong because performing fetal kick counts is a way of monitoring fetal well-being and detecting any signs of distress or reduced movement.
The nurse should encourage the woman to perform fetal kick counts regularly and report any concerns to her health care provider.
A nurse is providing discharge instructions to a client who had pre-term labor and was prescribed oral nifedipine.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Nifedipine is a calcium channel blocker that lowers blood pressure by relaxing the blood vessels.It can cause dizziness and orthostatic hypotension (a drop in blood pressure when standing up), so the client should avoid getting up suddenly from a lying or sitting position.
Choice A is wrong because grapefruit juice can increase the level of nifedipine in the blood and cause side effects such as headache, flushing, and swelling.
The client should avoid grapefruit and grapefruit juice while taking nifedipine.
Choice C is wrong because nifedipine does not affect the heart rate directly.
The client does not need to check the pulse before taking nifedipine, but should monitor the blood pressure regularly.
Choice D is wrong because nifedipine is prescribed to prevent pre-term labor by relaxing the uterine muscles.
The client should not stop taking nifedipine if contractions occur, but should contact the health care provider for further instructions.Stopping nifedipine suddenly can cause a rebound increase in blood pressure and chest pain.
A nurse is evaluating the effectiveness of antibiotic therapy for a client who has PPROM at 28 weeks of gestation.
Which of the following findings indicates a positive outcome?
Explanation
Increased amniotic fluid index indicates a positive outcome of antibiotic therapy for a client who has PPROM at 28 weeks of gestation.Antibiotics are used to prevent or treat infection and prolong pregnancy in women with PPROM.Infection can cause oligohydramnios (low amniotic fluid) which can lead to fetal complications such as cord compression, pulmonary hypoplasia and limb deformities.
Therefore, an increased amniotic fluid index suggests that the infection has been reduced or resolved and the risk of preterm birth has been lowered.
Normal ranges for amniotic fluid index are 5 to 25 cm.Normal ranges for maternal pulse rate are 60 to 100 beats per minute.Normal ranges for maternal leukocyte count are 4.5 to 11 x 10^9/L.
A nurse is providing discharge instructions to a client who has PPROM at 30 weeks of gestation and is on home bed rest.
Which of the following instructions should the nurse include?
Explanation
The nurse should include all of these instructions for a client who has PPROM at 30 weeks of gestation and is on home bed rest.
A nurse is preparing to administer betamethasone to a client who has PPROM at 26 weeks of gestation.
Which of the following statements by the nurse is appropriate?
Explanation
Betamethasone is a corticosteroid that is given to women who have PPROM (preterm prelabor rupture of membranes) at 24 to 36 weeks of gestation to reduce the risk of neonatal respiratory distress syndrome and other complications.It is given as two doses of 12 mg intramuscularly, 24 hours apart.
A nurse is caring for a client who has PPROM at 32 weeks of gestation and is receiving antibiotics prophylactically.
The nurse should monitor the client for which of the following signs of infection?
Explanation
This is because PPROM increases the risk of infection for both the mother and the baby, and infection can cause fetal tachycardia, maternal leukocytosis, and increased vaginal discharge.
Normal ranges for fetal heart rate are 110 to 160 beats per minute.
Normal ranges for maternal white blood cells are 4,500 to 11,000/mm3.
Normal ranges for vaginal discharge vary depending on the stage of pregnancy and other factors.
A nurse is caring for a client who has PPROM at 30 weeks of gestation and is receiving corticosteroids to enhance fetal lung maturity.
The nurse should explain to the client that the corticosteroids will have which of the following effects on the fetus?
Explanation
Corticosteroids have multiple effects on the fetus, including:
• Decreasing the risk of respiratory distress syndrome (RDS) by increasing the production of surfactant, a substance that helps the lungs expand and prevents them from collapsing.
• Reducing the incidence of intraventricular hemorrhage (IVH), a type of bleeding in the brain that can cause brain damage or death.
• Reducing the risk of necrotizing enterocolitis (NEC), a serious intestinal infection that can cause tissue death and perforation.
Normal ranges for gestational age are 37 to 42 weeks.
Normal ranges for fetal weight are 2.5 to 4.5 kg.
Normal ranges for fetal heart rate are 110 to 160 beats per minute.
Normal ranges for amniotic fluid index are 5 to 25 cm.
A nurse is caring for a client who has PPROM at 26 weeks of gestation and is on bed rest.
The nurse should instruct the client to report which of the following symptoms immediately?
Explanation
The nurse should instruct the client to report any symptoms of contractions, bleeding, or fever immediately, as they may indicate complications of PPROM such as preterm labor, placental abruption, or chorioamnionitis.
PPROM is the rupture of membranes before 37 weeks of gestation.
It occurs in 3% of pregnancies and is the leading cause of preterm delivery.It can lead to serious complications for both the mother and the fetus.PPROM at 26 weeks of gestation is considered extreme PPROM and has a high risk of neonatal morbidity and mortality.The management of PPROM depends on the gestational age, maternal and fetal condition, and availability of neonatal care.The client with PPROM at 26 weeks of gestation should be on bed rest and receive antibiotics, corticosteroids, and magnesium sulfate to prolong latency, reduce neonatal complications, and prevent cerebral palsy.
A nurse is caring for a client who is at 26 weeks of gestation and has PPROM.
Which of the following medications should the nurse expect to administer to the client? (Select all that apply.)
Explanation
Betamethasone, magnesium sulfate and ampicillin are medications that can be given to a client who has PPROM.
• Betamethasone is a corticosteroid that can help the baby’s lungs mature faster and reduce the risk of respiratory distress syndrome.It is usually given between 24 and 34 weeks of gestation.
• Magnesium sulfate is a tocolytic that can prevent preterm labor and reduce the risk of intraventricular hemorrhage and cerebral palsy in the baby.It is usually given for 24 to 48 hours after PPROM.
• Ampicillin is an antibiotic that can prevent or treat infection in the amniotic fluid, which is a common complication of PPROM.It can also prolong the latency period (the time between PPROM and delivery) and improve neonatal outcomes.
Normal ranges for gestational age are:
• 37 to 42 weeks for term pregnancy
• 34 to 36 weeks for late preterm pregnancy
• 32 to 33 weeks for moderate preterm pregnancy
• 28 to 31 weeks for very preterm pregnancy
• Less than 28 weeks for extremely preterm pregnancy
A nurse is teaching a client who is at 30 weeks of gestation and has PROM about the signs and symptoms of infection.
Which of the following should the nurse include in the teaching? (Select all that apply.)
Explanation
These are signs and symptoms of infection that can occur after PROM (prelabor rupture of membranes), which is the leakage of amniotic fluid before labor begins.Infection can be very dangerous for both the mother and the baby.
Normal ranges for gestational age are 37 to 42 weeks for term pregnancy and less than 37 weeks for preterm pregnancy.Normal ranges for fetal heart rate are 110 to 160 beats per minute.
A nurse is evaluating the understanding of a client who is at 32 weeks of gestation and has PPROM after providing discharge instructions.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The client should not use a tampon if they have any bleeding because it can increase the risk of infection.
A tampon can also interfere with the assessment of the amount and color of the bleeding.
A nurse is caring for a client with PROM who is receiving magnesium sulfate as a tocolytic agent.
Which of the following assessments should the nurse perform to monitor for magnesium toxicity?
Explanation
The nurse should perform all of the assessments listed to monitor for magnesium toxicity.
Magnesium sulfate is a drug that is given to prevent preterm labor by relaxing the uterine muscle.
However, it can also cause serious side effects such as weakness, low blood pressure, respiratory paralysis, and cardiac problems if the level of magnesium in the blood is too high.
The normal level of magnesium in the blood is about 1.5-2.5 mEq/L.Symptoms of toxicity may appear when the level reaches 4 mEq/L or higher.
A nurse is caring for a client with PPROM who is experiencing uterine contractions and signs of chorioamnionitis.
The nurse anticipates that the health care provider will order which of the following interventions?
Explanation
chorioamnionitis is a serious infection of the placental tissues that can cause fetal and maternal morbidity and mortality.The best management is to deliver the baby as soon as possible to prevent further complications.
Normal ranges for maternal blood C-reactive protein (CRP), procalcitonin and interleukin 6 (IL6) are:
• CRP: <10 mg/L
• Procalcitonin: <0.5 ng/mL
• IL6: <5 pg/mL
These markers may be elevated in chorioamnionitis, but they have low sensitivity and specificity for diagnosis.
A nurse is assessing a client with PROM who is at 37 weeks of gestation.
The nurse notes that the client has a foul-smelling vaginal discharge and a temperature of 38.2°C (100.8°F).
The nurse recognizes these findings as indicative of:
Explanation
Chorioamnionitis is an infection of the membranes containing the fetus and the amniotic fluid.It can occur when the membranes rupture before labor, especially if the rupture is prolonged or preterm.Chorioamnionitis can cause fever, foul-smelling vaginal discharge, abdominal pain, and fetal tachycardia.
Normal ranges for temperature are 36.5°C to 37.5°C (97.7°F to 99.5°F) and for fetal heart rate are 110 to 160 beats per minute.
A nurse is caring for a client who is at 26 weeks of gestation and has a diagnosis of PPROM.
Which of the following findings should the nurse report to the provider? (Select all that apply.).
Explanation
A temperature of 37.2°C (99°F) and uterine tenderness are signs of infection, which is a serious complication of PPROM.The normal temperature range during pregnancy is 36.4°C to 37.6°C (97.6°F to 99.6°F) orally.Uterine tenderness can indicate chorioamnionitis, which is an inflammation of the fetal membranes due to a bacterial infection.
A nurse is providing discharge instructions to a client who experienced PROM at 20 weeks of gestation and is on home bed rest.
Which of the following instructions should the nurse include?
Explanation
Drinking at least 2 L of fluids daily can help prevent dehydration and infection, which are possible complications of PROM (premature rupture of membranes).
Fluid intake also helps maintain amniotic fluid volume and fetal well-being.
A nurse is reviewing the laboratory results of a client who has PPROM at 30 weeks of gestation.
The nurse should expect to see which of the following values for the lecithin/sphingomyelin (L/S) ratio in the amniotic fluid?
Explanation
This value indicates a mature lecithin/sphingomyelin (L/S) ratio in the amniotic fluid, which reflects the fetal lung maturity and the low risk of respiratory distress syndrome (RDS) after birth.The L/S ratio is a test that measures the amount of lecithin and sphingomyelin, two types of phospholipids that are important for the formation of surfactant, a substance that prevents the lungs from collapsing.Lecithin increases and sphingomyelin stays constant as the fetus matures, so a higher L/S ratio indicates more surfactant and more lung development.A ratio of greater than 2:1 or 2.5:1 is 98% predictive of fetal lung maturity in most assays.
Exams on PROM and PPROM
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Define PROM and PPROM and their causes and risk factors.
-
Describe the clinical manifestations and diagnostic tests for PROM and PPROM.
-
Explain the nursing interventions and management for PROM and PPROM.
-
Identify the potential complications and outcomes of PROM and PPROM.
-
Educate the client and family about PROM and PPROM and their treatments.
-
Provide emotional support and reassurance to the client and family.
-
Collaborate with the interdisciplinary team to ensure optimal care for the client and fetus.
Introduction
-
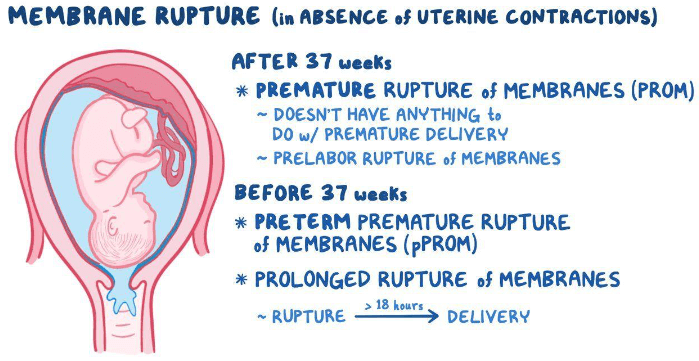
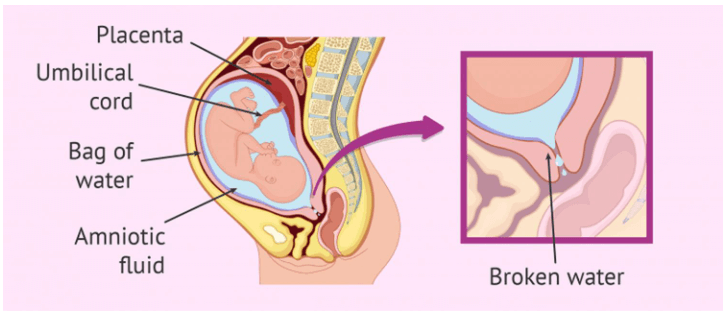
PROM stands for premature rupture of membranes, which is the rupture of the fetal membranes before the onset of labor.
-
If PROM occurs before 37 weeks of gestation, it is called preterm premature rupture of membranes (PPROM).
- PROM occurs in about 8 to 10 percent of all pregnancies and is associated with various complications for the mother and the fetus.
Causes and risk factors
-
The exact cause of PROM and PPROM is not always clear, but there are several conditions and factors that may contribute to membrane weakening and rupture.
-
Some of the causes and risk factors include:
-
History of PROM or PPROM in a previous pregnancy.
-
Genital or urinary tract infections, such as bacterial vaginosis, chlamydia, gonorrhea, or group B streptococcus.
-
Cigarette smoking.
-
Acute abdominal trauma.
-
Uterine overdistension, which can occur due to multiple pregnancy or polyhydramnios (excess amniotic fluid).
-
Malpresentation of the fetus, such as breech or transverse lie.
-
Incompetent cervix, which is a condition where the cervix dilates prematurely without contractions.
Clinical manifestations and Diagnostic tests
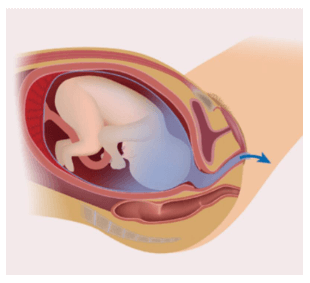
- The main clinical manifestation of PROM and PPROM is amniotic fluid leaking or gushing from the vagina. The fluid may be clear, yellowish, greenish, or blood-tinged depending on its composition.
-
Other signs and symptoms may include:
-
Absence or irregularity of uterine contractions.
-
Fetal heart rate changes, such as tachycardia or decelerations.
-
Maternal fever, chills, or malaise.
-
Foul-smelling vaginal discharge or amniotic fluid.
-
Abdominal tenderness or pain.
-
-
The diagnosis of PROM and PPROM is confirmed by the following tests:
- Nitrazine paper test: A strip of paper is placed in contact with the vaginal fluid. If the paper turns blue-green, it indicates that the fluid is alkaline and likely amniotic. If it remains yellow, it indicates that the fluid is acidic and likely urine or vaginal secretions.
-
Ferning test: A sample of vaginal fluid is placed on a microscope slide and allowed to dry. If fern-like patterns are seen under the microscope, it indicates that the fluid contains amniotic salts and proteins.
-
AmniSure test: A swab of vaginal fluid is tested for placental alpha microglobulin-1 (PAMG-1), a protein that is present in high concentrations in amniotic fluid. A positive result indicates membrane rupture
- Ultrasound: An ultrasound can measure the amount of amniotic fluid around the fetus. A low amount (oligohydramnios) may indicate membrane rupture. An ultrasound can also detect fetal position, placental location, and gestational age
Nursing interventions and Management
- The main goals of nursing care for clients with PROM and PPROM are to prevent infection, monitor maternal and fetal status, promote fetal lung maturity, and prepare for delivery if indicated
-
Some of the nursing interventions and management strategies include:
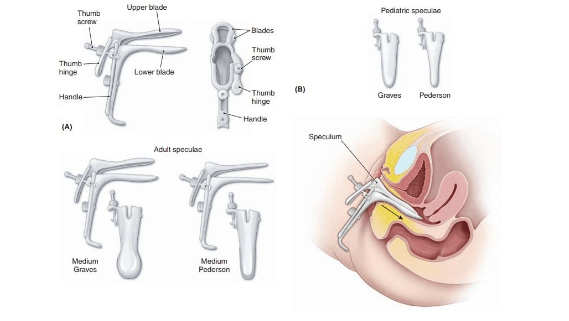
- Perform a sterile speculum examination to confirm membrane rupture and assess for pooling of amniotic fluid in the vagina. Avoid digital vaginal examinations unless absolutely necessary to reduce the risk of introducing infection
- Obtain vaginal and rectal cultures as prescribed to test for group B streptococcus, which can cause neonatal sepsis if transmitted during delivery. Administer antibiotics as prescribed to prevent or treat infection
-
Monitor maternal vital signs, especially temperature, every 4 hours or more frequently if indicated. Report any signs of infection, such as fever, tachycardia, leukocytosis, or foul-smelling discharge
-
Monitor fetal heart rate and uterine activity continuously or intermittently depending on gestational age and maternal condition. Report any signs of fetal distress, such as tachycardia, bradycardia, decelerations, or reduced variability .
-
Measure the amount and color of amniotic fluid leakage using a perineal pad. Report any changes in color or odor that may indicate infection or meconium staining (presence of fetal stool in amniotic fluid)
-

-
Administer corticosteroids as prescribed to enhance fetal lung maturity if gestational age is less than 34 weeks. Corticosteroids can reduce the risk of respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, and neonatal death in preterm infants
-
Administer tocolytics as prescribed to inhibit uterine contractions if gestational age is less than 34 weeks and there are no contraindications. Tocolytics can prolong pregnancy for up to 48 hours to allow time for corticosteroids to take effect or for maternal transfer to a facility with neonatal intensive care unit (NICU)
-
-
Maintain bed rest with bathroom privileges if there are no signs of labor or infection. Bed rest may reduce pressure on the cervix and prevent cord prolapse if there is significant loss of amniotic fluid. Encourage ambulation once labor begins or if fetal head is engaged
-
Provide comfort measures such as changing perineal pads frequently, applying ice packs to perineum if needed, wearing loose clothing, drinking plenty of fluids, and avoiding sexual intercourse or douching. These measures can help reduce irritation, discomfort, odor, dehydration, and infection risk
-
Educate the client and family about PROM and PPROM and their treatments. Explain the purpose and possible side effects of medications such as antibiotics, corticosteroids, and tocolytics. Teach them how to monitor for signs of infection, labor, cord prolapse, or fetal distress at home. Instruct them to report any changes in amniotic fluid leakage, vaginal bleeding, abdominal pain, fever, contractions, fetal movements, or umbilical cord protrusion immediately. Provide written instructions and contact numbers for emergency situations
-
Provide emotional support and reassurance to the client and family. Acknowledge their fears and concerns about preterm delivery, fetal well-being, NICU admission, or possible complications. Encourage them to express their feelings and ask questions. Provide information about available resources such as social workers, counselors, support groups, or online forums. Help them cope with uncertainty and plan for possible outcomes
-
Chorioamnionitis: An infection of the amniotic sac and fluid that can cause maternal fever, tachycardia, uterine tenderness, foul-smelling discharge, and leukocytosis. Chorioamnionitis can also increase the risk of postpartum endometritis, sepsis, hemorrhage, or thromboembolism
-
Placental abruption: A premature separation of the placenta from the uterine wall that can cause maternal bleeding, abdominal pain, uterine rigidity, and fetal distress. Placental abruption can also increase the risk of postpartum hemorrhage, anemia, shock, or disseminated intravascular coagulation (DIC)
Potential Complications and Outcomes
-
PROM and PPROM can lead to various complications for both the mother and the fetus depending on gestational age at rupture, infection status, and duration of latency period (time between rupture and delivery)
-
Preterm birth: Delivery before 37 weeks of gestation can result in various neonatal problems, such as respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, patent ductus arteriosus, retinopathy of prematurity, and neurodevelopmental impairment
- Umbilical cord prolapse: The umbilical cord may slip through the cervix and into the vagina before the fetal head, causing compression and reduced blood flow to the fetus. This can lead to fetal hypoxia, acidosis, or death
-
Fetal infection: The fetus may acquire infection from the mother through the placenta or during delivery. This can cause sepsis, pneumonia, meningitis, or long-term sequelae such as cerebral palsy or hearing loss
- Fetal deformities: Prolonged oligohydramnios due to membrane rupture before viability (< 24 weeks) can cause limb deformities (such as abnormal joint positioning) and pulmonary hypoplasia (underdevelopment of the lungs) due to compression of the fetus by the uterine wall. This condition is called Potter sequence or syndrome
-
-
The outcomes of PROM and PPROM depend on several factors, such as gestational age at rupture and delivery, infection status, latency period, fetal weight and maturity, and availability of neonatal intensive care
-
Generally, the earlier the rupture and delivery occur, the higher the risk of maternal and fetal morbidity and mortality
-
However, some studies have shown that expectant management (waiting for spontaneous labor) may improve neonatal outcomes compared to immediate delivery in selected cases of PPROM between 24 and 34 weeks of gestation
Conclusion
-
PROM and PPROM are common obstetric complications that can have significant implications for maternal and fetal health
-
Early diagnosis and management of PROM and PPROM are essential to prevent infection, promote fetal lung maturity, and prepare for delivery if indicated
-
Nursing care for clients with PROM and PPROM involves preventing infection, monitoring maternal and fetal status, providing comfort measures, educating the client and family, providing emotional support, and collaborating with the interdisciplinary team
Summary
-
PROM is the rupture of the fetal membranes before the onset of labor; PPROM is PROM before 37 weeks of gestation
-
PROM and PPROM may be caused by infection, trauma, smoking, uterine overdistension, malpresentation, or incompetent cervix
-
The main symptom of PROM and PPROM is amniotic fluid leakage from the vagina; other symptoms may include fever, foul-smelling discharge, abdominal pain, or fetal distress
-
The diagnosis of PROM and PPROM is confirmed by speculum examination, nitrazine paper test, ferning test, AmniSure test, or ultrasound
-
The nursing interventions and management for PROM and PPROM include antibiotics, corticosteroids, tocolytics, bed rest, comfort measures, client education, emotional support, and continuous monitoring
-
The potential complications of PROM and PPROM include chorioamnionitis, placental abruption, umbilical cord prolapse, fetal infection, preterm birth, fetal deformities, and intraventricular hemorrhage
-
The outcomes of PROM and PPROM depend on gestational age at rupture and delivery, infection status, latency period, fetal weight and maturity, and availability of neonatal intensive care
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on PROM and PPROM
This filled cannot be empty

