Please set your exam date
Nursing Care of Hospitalized Children
Study Questions
Admission and discharge procedures
A nurse is admitting a 4-year-old child to the pediatric unit. What is the best way to obtain the child's cooperation during the admission process?
Explanation
Choice A reason: This is not a good way to obtain the child's cooperation, as it may make the child feel ashamed or guilty for expressing emotions. It also does not address the child's fears or concerns.
Choice B reason: This may be a helpful strategy to reward the child for cooperation, but it is not the best way to obtain it. It may also create unrealistic expectations or dependence on external rewards.
Choice C reason: This is the best way to obtain the child's cooperation, as it shows respect for the child's cognitive and emotional development. It also helps the child understand what is happening and why and reduces anxiety and fear.
Choice D reason: This is not a good way to obtain the child's cooperation, as it may overwhelm or confuse the child. It also does not involve the child in his or her own care.
A nurse is reviewing the medical history of a 6-month-old infant who is being admitted to the pediatric unit. What information should the nurse obtain from the parents? (Select all that apply.)
Explanation
Choice A reason: The infant's immunization status is important information to obtain, as it may indicate the risk of vaccine-preventable diseases or adverse reactions to vaccines.
Choice B reason: The infant's birth weight and length are not relevant information to obtain, as they do not reflect the current growth and development of the infant.
Choice C reason: The infant's feeding and sleeping patterns are important information to obtain, as they may indicate nutritional status, growth rate, comfort level, and potential problems such as reflux, colic, or sleep apnea.
Choice D reason: The infant's developmental milestones are important information to obtain, as they may indicate normal or abnormal development, cognitive abilities, motor skills, and social-emotional functioning.
Choice E reason: The infant's family history of allergies is important information to obtain, as it may indicate genetic predisposition or environmental triggers for allergic reactions or asthma.
A nurse is performing a physical assessment on a 2-year-old toddler who is being admitted to the pediatric unit. What statement by the nurse would be most appropriate to elicit cooperation from the toddler?
Explanation
Choice A reason: This statement by the nurse may not be appropriate for a 2-year-old toddler, as it does not offer any choice or control to the toddler. It may also sound scary or intimidating to the toddler.
Choice B reason: This statement by the nurse would be most appropriate for a 2-year-old toddler, as it offers a limited choice and a sense of control to the toddler. It also shows respect for the toddler's preferences and autonomy.
Choice C reason: This statement by the nurse may not be appropriate for a 2-year-old toddler, as it does not offer any choice or control to the toddler. It may also sound demanding or threatening to the toddler.
Choice D reason: This statement by the nurse may not be appropriate for a 2-year-old toddler, as it does not relate to the physical assessment. It may also distract or confuse the toddler from what is being done.
A nurse is preparing to discharge a 10-year-old child from the pediatric unit after an appendectomy. What statement by the child would indicate that he or she understands the discharge instructions?
Explanation
Choice A reason: This statement by the child would indicate that he or she does not understand the discharge instructions, as it may be too soon to resume normal activities and socialization. The child may need to rest and recover for a few days or weeks, depending on the healing process and the physician's advice.
Choice B reason: This statement by the child would indicate that he or she understands the discharge instructions, as it shows compliance with the prescribed medication regimen. The child may need to take antibiotics or pain relievers to prevent infection or manage pain.
Choice C reason: This statement by the child would indicate that he or she does not understand the discharge instructions, as it may not reflect the dietary restrictions or recommendations after an appendectomy. The child may need to avoid spicy, fatty, or high-fiber foods and drink plenty of fluids to promote bowel function and healing.
Choice D reason: This statement by the child would indicate that he or she does not understand the discharge instructions, as it may not reflect the wound care or dressing changes after an appendectomy. The child may need to keep the incision site clean and dry, change the bandage as instructed, and report any signs of infection or bleeding.
A nurse is transferring a 12-year-old child from the pediatric unit to the intensive care unit (ICU) after a severe asthma attack. What is the most important information that the nurse should communicate to the ICU staff during the handoff report?
Explanation
Choice A reason: This information is important but not the most important for the nurse to communicate during the handoff report. It may be already available in the electronic health record or the transfer form.
Choice B reason: This information is the most important for the nurse to communicate during the handoff report, as it reflects the current clinical status and stability of the child. It may also indicate any changes or interventions that are needed in the ICU.
Choice C reason: This information is important but not the most important for the nurse to communicate during the handoff report. It may be already available in the electronic health record or the medication administration record.
Choice D reason: This information is important but not the most important for the nurse to communicate during the handoff report. It may be more relevant for the psychosocial assessment and support of the child and family in the ICU.
A nurse is admitting a 3-year-old child who has pneumonia to a pediatric unit. Which of the following actions should the nurse take first?
Explanation
Choice A reason: This action should be taken first by the nurse, as it provides essential data about the child's condition and helps identify any signs of deterioration or complications.
Choice B reason: This action should be taken by the nurse after obtaining a set of baseline vital signs, as it provides more comprehensive data about the child's physical status and helps identify any abnormalities or problems.
Choice C reason: This action should be taken by the nurse after performing a head-to-toe physical assessment, as it provides additional data about the child's risk of infection or adverse reactions to vaccines.
Choice D reason: This action should be taken by the nurse after reviewing the child's immunization record, as it provides important data about the child's risk of allergic reactions or drug interactions.
A nurse is discharging a 5-year-old child who has diabetes mellitus from a pediatric unit. Which of the following statements by the parent indicates a need for further teaching?
Explanation
Choice A reason: This statement by the parent indicates an understanding of the teaching, as it shows adherence to the recommended blood glucose monitoring schedule.
Choice B reason: This statement by the parent indicates an understanding of the teaching, as it shows adherence to the prescribed insulin regimen.
Choice C reason: This statement by the parent indicates an understanding of the teaching, as it shows awareness of how to treat hypoglycemia.
Choice D reason: This statement by the parent indicates a need for further teaching, as it shows a lack of understanding of the importance of dietary management for diabetes mellitus. The child should follow a balanced and consistent carbohydrate diet that matches the insulin dose and activity level.
A nurse is transferring a 7-year-old child who has cystic fibrosis from the pediatric unit to the respiratory unit. What information should the nurse include in the handoff report? (Select all that apply.)
Explanation
Choice A reason: This information is important but not specific for the nurse to include in the handoff report. It may be already available in the electronic health record or the transfer form.
Choice B reason: This information is specific and essential for the nurse to include in the handoff report, as it reflects the main problem and intervention for the child who has cystic fibrosis.
Choice C reason: This information is specific and essential for the nurse to include in the handoff report, as it reflects the routine and ongoing care for the child who has cystic fibrosis.
Choice D reason: This information is specific and essential for the nurse to include in the handoff report, as it reflects the secondary problem and intervention for the child who has cystic fibrosis.
Choice E reason: This information is specific and essential for the nurse to include in the handoff report, as it reflects the holistic and individualized care for the child who has cystic fibrosis.
Questions on Discharge Procedures
A nurse is preparing to discharge a child who has undergone a tonsillectomy. What is the most important discharge instruction that the nurse should give to the child and family?
Explanation
Choice A reason: This instruction is important but not the most important for the nurse to give to the child and family, as it helps prevent Reye syndrome, a rare but serious condition that can affect the brain and liver.
Choice B reason: This instruction is important but not the most important for the nurse to give to the child and family, as it helps promote hydration and healing of the throat.
Choice C reason: This instruction is the most important for the nurse to give to the child and family, as it helps detect postoperative hemorrhage, a potentially life-threatening complication of tonsillectomy.
Choice D reason: This instruction is important but not the most important for the nurse to give to the child and family, as it helps identify infection or inflammation of the throat or ears.
A nurse is discharging a child who has asthma from a pediatric unit. What information should the nurse include in the discharge plan and home care education? (Select all that apply.)
Explanation
Choice A reason: This information should be included in the discharge plan and home care education, as it helps ensure safe and effective medication management for asthma.
Choice B reason: This information should be included in the discharge plan and home care education, as it helps monitor and control asthma symptoms and guide appropriate actions based on the severity of the condition.
Choice C reason: This information should be included in the discharge plan and home care education, as it helps prevent or reduce exposure to allergens or irritants that can trigger or worsen asthma symptoms.
Choice D reason: This information is not specific for the discharge plan and home care education for asthma, as it applies to all children regardless of their health condition.
Choice E reason: This information should be included in the discharge plan and home care education, as it helps provide timely and appropriate medical attention in case of an acute asthma attack that does not respond to home treatment.
A nurse is discharging a child who has cystic fibrosis from a pediatric unit. What statement by the child indicates a need for further teaching?
Explanation
Choice A reason: This statement by the child indicates an understanding of the teaching, as it shows awareness of the importance of chest physiotherapy for cystic fibrosis.
Choice B reason: This statement by the child indicates an understanding of the teaching, as it shows awareness of the importance of pancreatic enzyme replacement for cystic fibrosis.
Choice C reason: This statement by the child indicates a need for further teaching, as it shows a misunderstanding of the dietary recommendations for cystic fibrosis. The child should drink plenty of fluids but avoid foods that are high in salt, as they can worsen dehydration and electrolyte imbalance.
Choice D reason: This statement by the child indicates an understanding of the teaching, as it shows awareness of the importance of infection prevention for cystic fibrosis.
A nurse is discharging a child who has diabetes mellitus from a pediatric unit. What statement by the child indicates that he or she understands the discharge instructions?
Explanation
Choice A reason: This statement by the child indicates a partial understanding of the discharge instructions, as it shows awareness of the importance of blood glucose monitoring for diabetes mellitus. However, the child may also need to check his or her blood sugar level at other times, such as before bedtime, before exercise, or when sick.
Choice B reason: This statement by the child indicates a need for further teaching, as it shows a misunderstanding of the proper technique for insulin administration for diabetes mellitus. The child should rotate the injection sites to prevent lipodystrophy, a condition that causes lumps or dents in the skin.
Choice C reason: This statement by the child indicates an understanding of the discharge instructions, as it shows awareness of the importance of dietary management for diabetes mellitus. The child should follow a balanced and consistent carbohydrate diet that matches the insulin dose and activity level.
Choice D reason: This statement by the child indicates an understanding of the discharge instructions, as it shows awareness of the signs and symptoms of hyperglycemia, a condition that occurs when the blood sugar level is too high and can lead to diabetic ketoacidosis, a serious complication of diabetes mellitus.
A nurse is discharging a child who has sickle cell anemia from a pediatric unit. What is the most important discharge instruction that the nurse should give to the child and family?
Explanation
Choice A reason: This instruction is important but not the most important for the nurse to give to the child and family, as it helps prevent vaso-occlusive crises, which are episodes of severe pain caused by blocked blood vessels due to sickled red blood cells.
Choice B reason: This instruction is important but not the most important for the nurse to give to the child and family, as it helps prevent hemolytic crises, which are episodes of rapid red blood cell destruction due to dehydration or infection.
Choice C reason: This instruction is important but not the most important for the nurse to give to the child and family, as it helps prevent megaloblastic anemia, which is a type of anemia caused by folic acid deficiency due to increased red blood cell production.
Choice D reason: This instruction is the most important for the nurse to give to the child and family, as it helps prevent sequestration crises, which are episodes of life-threatening organ damage caused by pooling of blood in the spleen or liver due to sickled red blood cells.
A nurse is admitting a child who has leukemia to a pediatric unit. Which of the following actions should the nurse take first?
Explanation
Choice A reason: This action should be taken first by the nurse, as it helps protect the child from exposure to infections that can be life-threatening due to immunosuppression caused by leukemia.
Choice B reason: This action should be taken by the nurse after placing the child in a private room with reverse isolation precautions, as it provides important data about the type and severity of leukemia and the risk of bleeding or infection.
Choice C reason: This action should be taken by the nurse after obtaining a complete blood count with differential and platelet count, as it helps correct anemia or thrombocytopenia that may result from leukemia or its treatment.
Choice D reason: This action should be taken by the nurse after administering packed red blood cells or platelets as ordered by the physician, as it helps provide information and support to the child and family who may be experiencing fear, anxiety, or grief.
A nurse is discharging a child who has undergone a cardiac catheterization from a pediatric unit. Which of the following statements by the parent indicates an understanding of the discharge instructions?
Explanation
Choice A reason: This statement by the parent indicates a need for further teaching, as it shows a misunderstanding of the wound care instructions. The dressing on the insertion site should be removed after 24 hours and replaced with a band-aid.
Choice B reason: This statement by the parent indicates an understanding of the discharge instructions, as it shows awareness of how to monitor and prevent complications such as infection or hemorrhage.
Choice C reason: This statement by the parent indicates a need for further teaching, as it shows a lack of understanding of the activity restrictions. The child should avoid strenuous activities and exercise for at least one week or until cleared by the physician.
Choice D reason: This statement by the parent indicates a need for further teaching, as it shows a misunderstanding of the pain management instructions. The child should not take aspirin or ibuprofen, as they can increase the risk of bleeding. The child should take acetaminophen or other prescribed medications for pain relief.
A nurse is admitting a child who has appendicitis to a pediatric unit. What information should the nurse obtain from the child and family? (Select all that apply.)
Explanation
Choice A reason: This information should be obtained from the child and family, as it helps assess the severity and progression of appendicitis and its complications.
Choice B reason: This information should be obtained from the child and family, as it helps evaluate the bowel function and rule out other causes of abdominal pain such as constipation or diarrhea.
Choice C reason: This information should be obtained from the child and family, as it helps identify any risk factors or contraindications for treatment such as allergic reactions, drug interactions, vaccine-preventable diseases, or previous abdominal surgeries.
Choice D reason: This information should be obtained from the child and family, as it helps determine the nutritional status and fluid balance of the child and prepare for surgery if indicated.
Choice E reason: This information is not specific for the admission and discharge of a child who has appendicitis, as it does not affect the diagnosis or treatment of the condition. It may be more relevant for other gastrointestinal disorders.
Questions on Chain of infection and modes of transmission and Risk factors and sources of infection in hospitalized children
Infection Control
A nurse is teaching a group of parents about the chain of infection and how to prevent it. The nurse should explain that the first link in the chain of infection is which of the following?
Explanation
Choice A reason: This is the correct answer, as the infectious agent is the microorganism that causes the infection, such as bacteria, viruses, fungi, or parasites.
Choice B reason: This is not the correct answer, as the reservoir is the second link in the chain of infection. It is the place where the infectious agent lives and grows, such as humans, animals, plants, soil, or water.
Choice C reason: This is not the correct answer, as the portal of exit is the third link in the chain of infection. It is the way that the infectious agent leaves the reservoir, such as through body fluids, skin, mucous membranes, or respiratory tract.
Choice D reason: This is not the correct answer, as the mode of transmission is the fourth link in the chain of infection. It is the way that the infectious agent travels from one host to another, such as through direct or indirect contact, droplet, airborne, vector, or vehicle transmission.
Explanation
Choice A reason: This factor may have contributed to the development of an HAI, as children have immature immune systems that make them more susceptible to infections.
Choice B reason: This factor may have contributed to the development of an HAI, as children may be exposed to other infected patients or health care workers who can transmit microorganisms through direct or indirect contact.
Choice C reason: This factor may have contributed to the development of an HAI, as children may use contaminated medical devices or equipment that can introduce microorganisms into their body, such as catheters, ventilators, or intravenous lines.
Choice D reason: This factor may have contributed to the development of an HAI, as children may contact environmental surfaces or objects that can harbor microorganisms, such as bed rails, tables, toys, or books.
Choice E reason: This factor may not have contributed to the development of an HAI, as CAIs are infections that are acquired outside of health care settings. However, CAIs may increase the risk of HAIs if they are not treated properly or if they cause complications.
Explanation
Choice A reason: This statement by the nurse would be most appropriate to educate the child and family about chickenpox, as it accurately describes the infectious agent and mode of transmission for this condition.
Choice B reason: This statement by the nurse would not be appropriate to educate the child and family about chickenpox, as it incorrectly describes the infectious agent and mode of transmission for this condition. Chickenpox is not caused by a bacterium or spread through contaminated food or water.
Choice C reason: This statement by the nurse would not be appropriate to educate the child and family about chickenpox, as it incorrectly describes the infectious agent and mode of transmission for this condition. Chickenpox is not caused by a fungus or spread through inhalation of spores from soil or plants.
Choice D reason: This statement by the nurse would not be appropriate to educate the child and family about chickenpox, as it incorrectly describes the infectious agent and mode of transmission for this condition. Chickenpox is not caused by a parasite or spread through bites from mosquitoes or ticks.
A nurse is caring for a child who has a community-acquired infection (CAI). Which of the following actions should the nurse take to prevent the spread of infection to other patients or healthcare workers?
Explanation
Choice A reason: This is the correct answer, as standard precautions are the minimum infection control practices that should be used for all patients, regardless of their diagnosis or infection status. They include hand hygiene, use of personal protective equipment, safe injection practices, safe handling of potentially contaminated equipment or surfaces, and respiratory hygiene and cough etiquette. A private room may also help reduce the exposure of other patients or health care workers to the infectious agent.
Choice B reason: This is not the correct answer, as contact precautions are additional infection control practices that should be used for patients who have infections that can be spread by direct or indirect contact with the patient or their environment. They include wearing gloves and gowns, using dedicated equipment, and limiting patient movement outside the room. A semi-private room may also increase the risk of cross-contamination between patients.
Choice C reason: This is not the correct answer, as airborne precautions are additional infection control practices that should be used for patients who have infections that can be spread by small droplets that remain in the air for long periods of time and can be inhaled by others. They include wearing a respirator, placing the patient in a negative pressure room with an air filtration system, and limiting patient movement outside the room.
Choice D reason: This is not the correct answer, as droplet precautions are additional infection control practices that should be used for patients who have infections that can be spread by large droplets that are generated by coughing, sneezing, or talking and can be transmitted to others who are within 3 feet of the patient. They include wearing a surgical mask, placing the patient in a private room or cohorting with other patients with the same infection, and limiting patient movement outside the room. A positive pressure room may also increase the risk of spreading the infection to other areas of the hospital.
Explanation
Choice A reason: This statement by the nurse would be appropriate to include in the teaching, as it helps prevent the transmission of microorganisms through hand contact.
Choice B reason: This statement by the nurse would be appropriate to include in the teaching, as it helps prevent the transmission of microorganisms through personal items.
Choice C reason: This statement by the nurse would be appropriate to include in the teaching, as it helps prevent the transmission of microorganisms through respiratory droplets.
Choice D reason: This statement by the nurse would be most appropriate to include in the teaching, as it helps prevent the occurrence and spread of common infectious diseases that can cause serious complications or death. Vaccination is one of the most effective ways to protect oneself and others from CAIs.
Questions on Standard and transmission-based precautions
A nurse is caring for a patient who has a urinary tract infection (UTI). What type of personal protective equipment (PPE) should the nurse wear when performing urinary catheter care for this patient?
Explanation
Choice A reason: This is the correct answer, as gloves and gown are the appropriate PPE to wear when performing urinary catheter care for a patient who has a UTI. Gloves protect the nurse's hands from exposure to urine, which may contain infectious agents. Gown protects the nurse's clothing and skin from contamination by urine or other body fluids.
Choice B reason: This is not the correct answer, as gloves and mask are not the appropriate PPE to wear when performing urinary catheter care for a patient who has a UTI. Mask protects the nurse's mouth and nose from exposure to respiratory droplets, which are not a mode of transmission for UTIs.
Choice C reason: This is not the correct answer, as gloves and eye protection are not the appropriate PPE to wear when performing urinary catheter care for a patient who has a UTI. Eye protection protects the nurse's eyes from exposure to splashes or sprays of blood or body fluids, which are unlikely to occur during urinary catheter care.
Choice D reason: This is not the correct answer, as gloves only are not sufficient PPE to wear when performing urinary catheter care for a patient who has a UTI. Gloves protect the nurse's hands from exposure to urine, but they do not protect the nurse's clothing and skin from contamination by urine or other body fluids.
Explanation
Choice A reason: This action should be taken as part of standard precautions, as it helps prevent the transmission of microorganisms through hand contact.
Choice B reason: This action should be taken as part of standard precautions, as it helps prevent the transmission of microorganisms through exposure to blood or body fluids.
Choice C reason: This action should be taken as part of standard precautions, as it helps prevent the transmission of microorganisms through respiratory droplets.
Choice D reason: This action is not part of standard precautions, but rather part of transmission-based precautions. It helps prevent the transmission of microorganisms through direct or indirect contact, airborne, or droplet routes.
Choice E reason: This action should be taken as part of standard precautions, as it helps prevent the transmission of microorganisms through environmental surfaces or objects.
Explanation
Choice A reason: This statement by the nurse would not be appropriate to educate the patient and family about TB, as it incorrectly describes the infectious agent and mode of transmission for this condition. TB is not caused by a virus or spread through direct contact with skin lesions or respiratory droplets.
Choice B reason: This statement by the nurse would be most appropriate to educate the patient and family about TB, as it accurately describes the infectious agent and mode of transmission for this condition. TB is caused by a bacterium called Mycobacterium tuberculosis that can spread through inhalation of small droplets that remain in the air for long periods of time after an infected person coughs, sneezes, or speaks.
Choice C reason: This statement by the nurse would not be appropriate to educate the patient and family about TB, as it incorrectly describes the infectious agent and mode of transmission for this condition. TB is not caused by a fungus or spread through contact with soil or plants that are contaminated with spores.
Choice D reason: This statement by the nurse would not be appropriate to educate the patient and family about TB, as it incorrectly describes the infectious agent and mode of transmission for this condition. TB is not caused by a parasite or spread through ingestion of contaminated food or water.
A nurse is implementing transmission-based precautions for a patient who has measles. What type of personal protective equipment (PPE) should the nurse wear when entering the patient's room?
Explanation
Choice A reason: This is not the correct answer, as gloves and gown are not sufficient PPE to wear when entering the room of a patient who has measles. Gloves protect the nurse's hands from exposure to blood or body fluids, and gown protects the nurse's clothing and skin from contamination by blood or body fluids, but they do not protect the nurse's respiratory tract from exposure to airborne droplets that contain the measles virus.
Choice B reason: This is not the correct answer, as gloves and mask are not sufficient PPE to wear when entering the room of a patient who has measles. Gloves protect the nurse's hands from exposure to blood or body fluids, and mask protects the nurse's mouth and nose from exposure to large droplets that are generated by coughing, sneezing, or talking, but they do not protect the nurse's respiratory tract from exposure to small droplets that remain in the air for long periods of time and can be inhaled by others.
Choice C reason: This is not the correct answer, as gloves and eye protection are not sufficient PPE to wear when entering the room of a patient who has measles. Gloves protect the nurse's hands from exposure to blood or body fluids, and eye protection protects the nurse's eyes from exposure to splashes or sprays of blood or body fluids, but they do not protect the nurse's respiratory tract from exposure to airborne droplets that contain the measles virus.
Choice D reason: This is the correct answer, as gloves and respirator are the appropriate PPE to wear when entering the room of a patient who has measles. Gloves protect the nurse's hands from exposure to blood or body fluids, and respirator protects the nurse's respiratory tract from exposure to airborne droplets that contain the measles virus. A respirator is a device that filters out at least 95% of airborne particles and fits tightly around the face.
A nurse is caring for a patient who has Clostridium difficile infection (CDI). What type of transmission-based precautions should the nurse implement for this patient?
Explanation
Choice A reason: This is the correct answer, as contact precautions are indicated for patients who have infections that can be spread by direct or indirect contact with the patient or their environment. CDI is caused by a bacterium that produces spores that can contaminate surfaces or objects and can be transmitted through hand contact.
Choice B reason: This is not the correct answer, as droplet precautions are indicated for patients who have infections that can be spread by large droplets that are generated by coughing, sneezing, or talking and can be transmitted to others who are within 3 feet of the patient. CDI is not spread by respiratory droplets.
Choice C reason: This is not the correct answer, as airborne precautions are indicated for patients who have infections that can be spread by small droplets that remain in the air for long periods of time and can be inhaled by others. CDI is not spread by airborne droplets.
Choice D reason: This is not the correct answer, as neutropenic precautions are indicated for patients who have low white blood cell counts and are at risk of developing infections from normal flora or environmental sources. CDI is not caused by normal flora or environmental sources, but by an overgrowth of a bacterium that is usually present in small amounts in the intestine.
A nurse is caring for a patient who has a methicillin-resistant Staphylococcus aureus (MRSA) infection.
Which of the following actions should the nurse take to prevent cross-contamination?
Explanation
Choice A reason: This action should be taken by the nurse to prevent cross-contamination, as it helps protect the nurse and other patients from exposure to MRSA, which can be transmitted through direct or indirect contact with infected skin or wounds.
Choice B reason: This action should be taken by the nurse to prevent cross-contamination, as it helps prevent the transmission of MRSA, which can survive on surfaces or objects for long periods of time.
Choice C reason: This action should be taken by the nurse to prevent cross-contamination, as it helps eliminate MRSA, which can be resistant to many disinfectants and antibiotics.
Choice D reason: This is the correct answer, as all of the above actions should be taken by the nurse to prevent cross-contamination. MRSA is a serious and potentially life-threatening infection that can cause skin and soft tissue infections, bloodstream infections, pneumonia, or surgical site infections.
A nurse is caring for a patient who has influenza. What type of transmission-based precautions should the nurse implement for this patient?
Explanation
Choice A reason: This is not the correct answer, as contact precautions are indicated for patients who have infections that can be spread by direct or indirect contact with the patient or their environment. Influenza is not spread by contactbut by respiratory droplets.
Choice B reason: This is the correct answer, as droplet precautions are indicated for patients who have infections that can be spread by large droplets that are generated by coughing, sneezing, or talking and can be transmitted to others who are within 3 feet of the patient. Influenza is caused by a virus that can spread through respiratory droplets.
Choice C reason: This is not the correct answer, as airborne precautions are indicated for patients who have infections that can be spread by small droplets that remain in the air for long periods of time and can be inhaled by others. Influenza is not spread by airborne droplets, unless it is a novel strain that has the potential to cause a pandemic.
Choice D reason: This is not the correct answer, as neutropenic precautions are indicated for patients who have low white blood cell counts and are at risk of developing infections from normal flora or environmental sources. Influenza is not caused by normal flora or environmental sources, but by a virus that can infect the respiratory tract.
Explanation
Choice A reason: This statement by the nurse would be appropriate to include in the teaching, as it helps prevent the transmission of microorganisms through hand contact between the health care workers and the patient or their equipment.
Choice B reason: This statement by the nurse would be appropriate to include in the teaching, as it helps prevent the transmission of microorganisms through self-inoculation of the mucous membranes with unwashed hands.
Choice C reason: This statement by the nurse may not be appropriate to include in the teaching, as it may not be feasible or realistic for the patient or family to keep their room clean and tidy and dispose of any waste properly. This may be more of a responsibility of the environmental services staff.
Choice D reason: This statement by the nurse would be appropriate to include in the teaching, as it helps detect and treat any HAIs early and prevent complications or spread of infection.
Choice E reason: This statement by the nurse would be appropriate to include in the teaching, as it helps reduce the exposure of the patient to potential sources of infection from visitors and protect them from transmitting any infection to others.
Questions on Safety measures
Safety measures
Explanation
Choice A reason: This is not the appropriate nursing intervention, as it may increase the risk of injury, agitation, or psychological trauma in the child. Restraints should only be used as a last resort and with a physician's order.
Choice B reason: This is not the appropriate nursing intervention, as it may not prevent the child from falling out of bed or wandering around the unit. Bed alarms are useful for alerting the staff, but they do not stop the child from moving.
Choice C reason: This is a possible nursing intervention, as it may facilitate closer observation and monitoring of the child. However, it may not address the underlying cause of the child's restlessness or agitation.
Choice D reason: This is the most appropriate nursing intervention, as it may reduce the child's boredom, anxiety, or fear and provide a sense of security and comfort. Diversionary activities may include toys, games, books, or music that are suitable for the child's age and developmental level. Parental supervision may also help prevent falls by assisting the child with toileting, positioning, or ambulation.
Explanation
Choice A reason: This action should be taken by the nurse to prevent medication errors, as it helps ensure that the medication is correct in terms of name, dose, route, time, and patient.
Choice B reason: This action should be taken by the nurse to prevent medication errors, as it helps ensure that the medication is measured and administered accurately and safely. Oral syringes or droppers are more precise and easier to use than cups or spoons for liquid medication.
Choice C reason: This action should be taken by the nurse to prevent medication errors, as it helps ensure that the medication dosage and calculation are correct and appropriate for the patient's weight and age. Another nurse can act as a double-check and catch any potential errors or discrepancies.
Choice D reason: This action should be taken by the nurse to prevent medication errors, as it helps ensure that the medication is given to the right patient. Comparing the infant's identification band with the MAR and asking the parent to confirm the infant's name are two ways of verifying the patient's identity.
Choice E reason: This action should not be taken by the nurse to prevent medication errors, as it may alter the effectiveness, absorption, or taste of the medication. Crushing or dissolving tablets or capsules and mixing them with formula or juice may also cause choking or aspiration in infants. The nurse should only administer medications that are in liquid form or prescribed to be crushed or dissolved.
A nurse is caring for a child who has a central venous catheter (CVC) in place. What type of equipment-related injury is the child most at risk for and what action should the nurse take to prevent it?
Explanation
Choice A reason: This is not the correct answer, as the malfunction is not the most common type of equipment-related injury for a child who has a CVC. Malfunctions may occur due to mechanical failure, occlusion, infection, or thrombosis of the CVC, but it can be prevented or detected by regular assessment and maintenance of the CVC.
Choice B reason: This is not the correct answer, as misuse is not the most common type of equipment-related injury for a child who has a CVC. Misuse may occur due to human error, lack of knowledge, or inappropriate use of the CVC, but it can be prevented or corrected by following the standard guidelines and policies for CVC care.
Choice C reason: This is the correct answer, as disconnection is the most common type of equipment-related injury for a child who has a CVC. Disconnection may occur due to accidental removal, breakage, or loosening of the CVC connections, and it can cause serious complications such as hemorrhage or air embolism. The nurse should secure the CVC connections with tape or clamps and monitor the child for signs of bleeding or air embolism, such as hypotension, tachycardia, dyspnea, chest pain, cyanosis, or altered mental status.
Choice D reason: This is not the correct answer, as entanglement is not the most common type of equipment-related injury for a child who has a CVC. Entanglement may occur due to excessive or tangled tubing that can interfere with the child's mobility or comfort, but it can be prevented or minimized by organizing the tubing and keeping it away from the child's reach and movement.
Explanation
Choice A reason: This statement by the nurse would not indicate that the procedure is done correctly and safely, as it does not describe the correct anatomical landmark for a lumbar puncture. The needle should be inserted between the fourth and fifth lumbar vertebrae, not the third and fourth, to avoid damaging the spinal cord.
Choice B reason: This statement by the nurse would indicate that the procedure is done correctly and safely, as it describes the correct position for a lumbar puncture. The lateral recumbent position with flexion of the spine helps expose the intervertebral spaces and facilitate the insertion of the needle.
Choice C reason: This statement by the nurse would not indicate that the procedure is done correctly and safely, as it describes the post-procedure care, not the procedure itself. Applying a sterile dressing and monitoring for signs of infection or bleeding are important steps to prevent complications after a lumbar puncture, but they do not ensure that the procedure is done correctly and safely.
Choice D reason: This statement by the nurse would not indicate that the procedure is done correctly and safely, as it describes the pre-procedure and intra-procedure care, not the procedure itself. Giving pain medication and asking for pain or discomfort are important steps to reduce anxiety and discomfort during a lumbar puncture, but they do not ensure that the procedure is done correctly and safely.
A nurse is caring for a child who has a burn injury on the left arm. What type of procedure-related injury is the child most at risk for and what action should the nurse take to prevent it?
Explanation
Choice A reason: This is not the correct answer, as pain is not the most common type of procedure-related injury for a child who has a burn injury. Pain is an expected outcome of a burn injury and its treatment, but it can be managed with appropriate analgesics and non-pharmacological interventions.
Choice B reason: This is not the correct answer, as bleeding is not the most common type of procedure-related injury for a child who has a burn injury. Bleeding may occur during debridement or grafting of the wound, but it can be controlled with pressure dressing and hemostatic agents.
Choice C reason: This is the correct answer, as infection is the most common type of procedure-related injury for a child who has a burn injury. Infection may occur due to loss of skin barrier, exposure to microorganisms, or impaired immune response. The nurse should clean and dress the wound with sterile technique and monitor the child's temperature and white blood cell count to prevent or detect infection.
Choice D reason: This is not the correct answer, as allergic reaction is not the most common type of procedure-related injury for a child who has a burn injury. Allergic reaction may occur due to hypersensitivity to medications, dressings, or grafts, but it can be prevented or treated with antihistamines or corticosteroids.
Explanation
Choice A reason: This action should be taken by the nurse to prevent equipment-related injuries, as it helps ensure that the traction is effective and does not cause any complications such as nerve damage, muscle spasms, or skin breakdown.
Choice B reason: This action should be taken by the nurse to prevent equipment-related injuries, as it helps prevent pressure ulcers, infection, or inflammation of the skin under the traction device.
Choice C reason: This action should be taken by the nurse to prevent equipment-related injuries, as it helps assess the blood flow, sensation, and movement of the affected extremity and detect any signs of impaired circulation, nerve compression, or compartment syndrome.
Questions on Types and examples of play and distraction techniques
Play and distraction techniques
A nurse is planning to use therapeutic play with a child who is scheduled for a blood draw. What type of play would be most appropriate for this purpose and why?
Explanation
Choice A reason: This is the correct answer, as role play is a type of therapeutic play that helps the child cope with a specific health problem or procedure. Role play allows the child to express their fears, ask questions, and gain mastery over the situation.
Choice B reason: This is not the correct answer, as board game is a type of recreational play that provides fun, enjoyment, or entertainment for the child. Board game may distract the child from their anxiety, but it does not address their specific concerns or prepare them for the procedure.
Choice C reason: This is not the correct answer, as art activity is a type of developmental play that supports the child's growth and development according to their age and stage. Art activity may help the child express their emotions, but it does not provide them with information or skills to cope with the procedure.
Choice D reason: This is not the correct answer, as music activity is a type of multimodal play that uses more than one type of play or more than one mode of delivery. Music activity may soothe the child and reduce their pain perception, but it does not familiarize them with the procedure or allow them to participate in it.
A nurse is caring for a child who is hospitalized for a chronic illness. The nurse wants to use recreational play to provide fun and enjoyment for the child. What type of play would be most suitable for this purpose and why?
Explanation
Choice A reason: This is the correct answer, as video game is a type of recreational play that provides fun, enjoyment, or entertainment for the child. Video game can also enhance the child's cognitive, motor, and social skills, as well as provide a sense of control and escape from reality.
Choice B reason: This is not the correct answer, as puzzle is a type of developmental play that supports the child's growth and development according to their age and stage. Puzzle can also provide fun and enjoyment for the child, but it may not be as engaging or stimulating as video game.
Choice C reason: This is not the correct answer, as storytelling is a type of therapeutic play that helps the child cope with a specific health problem or procedure. Storytelling can also provide fun and enjoyment for the child, but it may not be as interactive or exciting as video game.
Choice D reason: This is not the correct answer, as puppet show is a type of multimodal play that uses more than one type of play or more than one mode of delivery. Puppet show can also provide fun and enjoyment for the child, but it may not be as accessible or convenient as video game.
Explanation
Choice A reason: This type of play would be appropriate for this purpose, as it helps support the child's physical development and coordination, especially for infants and toddlers who are in the sensorimotor stage of cognitive development.
Choice B reason: This type of play would be appropriate for this purpose, as it helps support the child's cognitive and emotional development, especially for preschoolers who are in the preoperational stage of cognitive development and use symbolic play to represent their thoughts and feelings.
Choice C reason: This type of play would not be appropriate for this purpose, as it is more suitable for older children who are in the concrete operational or formal operational stages of cognitive development and can understand and follow rules and logic. Games with rules may also be too competitive or stressful for a child who is undergoing chemotherapy.
Choice D reason: This type of play would be appropriate for this purpose, as it helps support the child's social and moral development, especially for school-age children who are in the conventional stage of moral development and value social interactions and norms.
Choice E reason: This type of play would be appropriate for this purpose, as it helps support the child's self-esteem and coping skills, especially for adolescents who are in the postconventional stage of moral development and value individuality and autonomy. Solitary play may also provide a sense of relaxation and distraction for a child who is undergoing chemotherapy.
A nurse is using multimodal play with a child who is hospitalized for asthma. What type of play would be most effective for this purpose and why?
Explanation
Choice A reason: This is not the correct answer, as music and art are not the most effective types of multimodal play for a child who is hospitalized for asthma. Music and art may provide relaxation, distraction, or emotional expression for the child, but they do not address their specific health problem or teach them how to cope with it.
Choice B reason: This is the correct answer, as storytelling and puppet show are effective types of multimodal play for a child who is hospitalized for asthma. Storytelling and puppet show can help the child understand their condition, learn coping strategies, express their fears or concerns, and gain mastery over the situation.
Choice C reason: This is not the correct answer, as video game and board game are not the most effective types of multimodal play for a child who is hospitalized for asthma. Video game and board game may provide fun, enjoyment, or entertainment for the child, as well as enhance their cognitive, motor, and social skills, but they may not be as engaging or interactive as storytelling and puppet show.
Choice D reason: This is not the correct answer, as role play and sensorimotor play are not the most effective types of multimodal play for a child who is hospitalized for asthma. Role play and sensorimotor play may help the child practice their skills, improve their coordination, and reduce their anxiety, but they may not be as creative or imaginative as storytelling and puppet show.
A nurse is planning to use play and distraction techniques for a child who is undergoing a painful procedure. Which of the following principles should the nurse follow when choosing the appropriate technique? (Select all that apply.)
Explanation
Choice A reason: This is correct. The technique should be child-centered and tailored to the child's preferences and needs, such as their favorite toys, games, or music.
Choice B reason: This is correct. The technique should be developmentally appropriate and match the child's cognitive and emotional level, such as their attention span, language skills, or coping strategies.
Choice C reason: This is correct. The technique should be culturally sensitive and respect the child's values and beliefs, such as their religious practices, family roles, or communication styles.
Choice D reason: This is correct. The technique should be evidence-based and supported by research and clinical guidelines, such as the best practices for pain management, anxiety reduction, or procedural preparation.
Choice E reason: This is correct. The technique should be collaborative and involve the child, family, and health care team, such as their parents, siblings, or nurses.
A nurse is evaluating the effectiveness of play and distraction techniques for a child who is undergoing a medical procedure. Which of the following tools and methods can the nurse use to measure the outcomes of play and distraction techniques? (Select all that apply.)
Explanation
Choice A reason: This is correct. Self-report scales are valid and reliable measures that assess the child's pain intensity, anxiety level, or satisfaction with the technique, such as the Wong-Baker FACES Pain Rating Scale¹, the State-Trait Anxiety Inventory for Children², or the Child Satisfaction with Play Technique Scale³.
Choice B reason: This is correct. Behavioral observation scales are objective and standardized measures that observe the child's facial expressions, body movements, or vocalizations during the procedure, such as the FLACC Scale, the Child Facial Coding System, or the Non-communicating Children's Pain Checklist.
Choice C reason: This is correct. Physiological indicators are accurate and sensitive measures that monitor the child's heart rate, blood pressure, or oxygen saturation before, during, and after the procedure using devices such as a pulse oximeter, a sphygmomanometer, or an electrocardiogram.
Choice D reason: This is correct. Qualitative feedback is an in-depth and rich source of information that collects the child's comments, feelings, or suggestions about the technique using methods such as interviews, focus groups, or open-ended questions.
Choice E reason: This is correct. Quantitative data is a numerical and statistical source of information that analyzes the child's length of stay,
medication use, or complication rate after the procedure using methods such as charts, records, or databases.
A nurse is using play and distraction techniques for a child who is receiving an intravenous injection. Which of the following statements by the nurse is most appropriate to use as a distraction technique?
Explanation
Choice A reason: This is incorrect. Telling the child that the injection will hurt can increase their fear and anticipation of pain, and may also damage the trust between the nurse and the child.
Choice B reason: This is incorrect. Offering the child to watch a video on a tablet may not be effective as a distraction technique, as the child may still be aware of the procedure and may not be able to focus on the video.
Choice C reason: This is correct. Asking the child to name the animals on a poster is an example of a distraction technique that can divert the child's attention from the procedure and reduce their anxiety and pain.
Choice D reason: This is incorrect. Criticizing or minimizing the child's feelings can make them feel ashamed or guilty, and may also worsen their emotional distress.
A nurse is using play and distraction techniques for a child who is having a dressing change. Which of the following statements by the child indicates that the technique is effective?
Explanation
Choice A reason: This is incorrect. Saying that they don't want to be touched or asking the nurse to go away is an indication that the child is feeling anxious and defensive, and not distracted from the procedure.
Choice B reason: This is incorrect. Expressing fear or pleading with the nurse not to hurt them is an indication that the child is feeling anxious and fearful, and not distracted from the procedure.
Choice C reason: This is correct. Showing interest and pride in making a bracelet with beads is an indication that the child is engaged in
the play activity and distracted from the procedure.
Choice D reason: This is incorrect. Asking the nurse to hurry up and finish is an indication that the child is feeling impatient and uncomfortable, and not distracted from the procedure.
A nurse is educating a parent about how to use play and distraction techniques for their child who has chronic pain. Which of the following information should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A reason: This is correct. Play and distraction techniques can help reduce pain by stimulating endorphins in the brain, which are natural painkillers that block pain signals.
Choice B reason: This is correct. Play and distraction techniques can help improve mood by increasing serotonin levels in the brain, which are neurotransmitters that regulate mood, sleep, appetite, and memory.
Choice C reason: This is correct. Play and distraction techniques can help enhance coping by providing a sense of control and mastery, which can increase self-esteem, confidence, and resilience.
Choice D reason: This is correct. Play and distraction techniques can help promote healing by improving blood flow and oxygen delivery, which can facilitate tissue repair, wound healing, and infection prevention.
Choice E reason: This is correct. Play and distraction techniques can help prevent infection by boosting immune system function, which can fight off pathogens, inflammation, and disease.
A nurse uses guided imagery as a play technique for a 10-year-old client who has cancer. The nurse asks
the client to imagine being in a place where he feels happy and safe. Which of
the following actions should
the nurse take next?
Explanation
Choice A reason: This is correct. Asking the client to describe what he sees, hears, smells, and feels in that place is the next action that the nurse should take when using guided imagery as a play technique. This can help the client to focus on the sensory details of the imagined place and enhance the relaxation and distraction effects of the technique.
Choice B reason: This is incorrect. Asking the client to rate his pain level on a scale of 0 to 10 is not the next action that the nurse should take when using guided imagery as a play technique. This can interrupt the flow of the technique and remind the client of his pain.
Choice C reason: This is incorrect. Asking the client to draw a picture of that place is not the next action that the nurse should take when using guided imagery as a play technique. This can distract the client from the mental imagery and reduce the effectiveness of the technique.
Choice D reason: This is incorrect. Asking the client to repeat positive affirmations about that place is not the next action that
the nurse should take when using guided imagery as a play technique. This can be done after the technique is completed, but not during it.
Questions on conclusion
Explanation
Choice A reason: Egocentrism and magical thinking are characteristics of the preschool stage, not the school-age stage.
Choice B reason: Concrete operations and conservation are characteristics of the school-age stage, which involves logical thinking and understanding of physical properties.
Choice C reason: Formal operations and abstract reasoning are characteristics of the adolescent stage, not the school-age stage.
Choice D reason: Identity formation and peer pressure are characteristics of the adolescent stage, not the school-age stage.
Explanation
Choice A reason: Providing written instructions and verbal explanations to the parents is an important action to ensure understanding and compliance with the discharge plan.
Choice B reason: Teaching the child how to change the dressing and monitor for signs of infection is not appropriate for a 4-year-old child, who may not have the cognitive or motor skills to perform these tasks. The parents should be taught how to do these instead.
Choice C reason: Encouraging the parents to let the child resume normal activities as tolerated is an important action to promote recovery and prevent complications such as constipation or adhesions.
Choice D reason: Giving the child a stuffed animal or a toy as a reward for being brave is an important action to provide positive reinforcement and reduce anxiety or fear associated with hospitalization or surgery.
Choice E reason: Referring the child to a support group or a counselor if needed is not a necessary action for a 4-year-old child who had surgery for appendicitis, unless there are signs of emotional distress or trauma that require professional intervention.
Coping strategies
A nurse is caring for a hospitalized child who is experiencing stress due to a chronic illness. Which of the following factors should the nurse consider when assessing the child's coping process and responses? (Select all that apply.)
Explanation
Choice A reason: This is correct. The child's developmental stage and cognitive abilities can affect how they perceive, understand, and cope with stressors. For example, younger children may have more difficulty expressing their feelings or understanding their condition than older children.
Choice B reason: This is correct. The child's personality and temperament traits can influence how they react to and cope with stressors. For example, some children may be more resilient, optimistic, or adaptable than others.
Choice C reason: This is correct. The child's family structure and support system can impact how they cope with stressors. For example, children who have supportive and involved parents or siblings may cope better than those who have absent or dysfunctional family members.
Choice D reason: This is correct. The child's cultural background and values can affect how they cope with stressors. For example, some cultures may have different beliefs, practices, or expectations regarding health, illness, or coping.
Choice E reason: This is correct. The child's physical environment and comfort level can influence how they cope with stressors. For example, children who have a familiar, safe, and comfortable environment may cope better than those who have a strange, noisy, or painful environment.
A nurse is teaching a hospitalized child who is undergoing chemotherapy how to use problem-focused coping strategies to deal with the stress of the treatment. Which of the following strategies should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A reason: This is correct. Asking questions and seeking information about the treatment process and outcomes is a problem-focused coping strategy that can help the child understand what to expect and how to prepare for the treatment.
Choice B reason: This is incorrect. Practicing relaxation techniques such as deep breathing or guided imagery before and during the treatment is an emotion-focused coping strategy that can help the child regulate or reduce the emotional impact of the problem.
Choice C reason: This is correct. Setting realistic goals and planning actions to achieve them is a problem-focused coping strategy that can help the child take control of the situation and make progress toward the desired outcome.
Choice D reason: This is incorrect. Expressing emotions and feelings about the treatment to a trusted person or a support group is an emotion-focused coping strategy that can help the child cope with the feelings associated with the problem.
Choice E reason: This is correct. Seeking help and assistance from healthcare professionals or family members when needed is a problem-focused coping strategy that can help the child access resources and support that can facilitate solving the problem.
A nurse is using emotion-focused coping strategies to help a hospitalized child who is feeling anxious and scared about an upcoming surgery. Which of the following statements by the nurse is most appropriate to use as an emotion-focused coping strategy?
Explanation
Choice A reason: This is incorrect. Telling the child that they don't have to worry about anything or that the surgery will go well is not an effective emotion-focused coping strategy, as it may dismiss or invalidate the child's feelings.
Choice B reason: This is incorrect. Offering to explain what will happen during the surgery is not an emotion-focused coping strategy, but rather a problem-focused coping strategy that can help the child to understand the situation.
Choice C reason: This is correct. Asking the child how they are feeling right now is an example of an emotion-focused coping strategy that can help the child express their emotions and feelings about the surgery.
Choice D reason: This is incorrect. Asking the child why they are so nervous or saying that it's not a big deal is not an effective emotion-focused coping strategy, as it may criticize or minimize the child's feelings.
A nurse is assessing a hospitalized child who is using play as a coping strategy to deal with the stress of hospitalization. Which of the following statements by the child indicates that the play is effective as a coping strategy?
Explanation
Choice A reason: This is incorrect. Saying that they hate the place or want to go home is an indication that the child is feeling unhappy and dissatisfied with the hospitalization, and not using play as a coping strategy.
Choice B reason: This is incorrect. Saying that they are bored or have nothing to do is an indication that the child is feeling uninterested and unmotivated by the play activity, and not using it as a coping strategy.
Choice C reason: This is correct. Showing interest and creativity in making a card for the doctor is an indication that the child is engaged in
the play activity and using it as a coping strategy to deal with the stress of hospitalization.
Choice D reason: This is incorrect. Asking the nurse to leave them alone or saying that they don't want to play is an indication that the child is feeling isolated and withdrawn from the play activity, and not using it as a coping strategy.
A nurse is planning interventions for a hospitalized child who is using coping strategies to deal with the stress of hospitalization. Which of the following principles and guidelines should the nurse follow when planning coping interventions? (Select all that apply.)
Explanation
Choice A reason: This is correct. The interventions should be based on the individual needs and preferences of the child, such as their interests, hobbies, or goals.
Choice B reason: This is correct. The interventions should be consistent with the developmental stage and cognitive abilities of the child, such as their language skills, attention span, or reasoning abilities.
Choice C reason: This is correct. The interventions should be flexible and adaptable to changing situations and circumstances, such as different procedures, staff, or environments.
Choice D reason: This is incorrect. The interventions should not be limited to one type of coping strategy, but rather include both problem-focused and emotion-focused coping strategies, as they can complement each other and enhance coping outcomes.
Choice E reason: This is correct. The interventions should be evaluated by measuring the effectiveness and outcomes of coping strategies, such as pain relief, anxiety reduction, mood improvement, or adaptation enhancement.
A nurse is caring for a hospitalized child who has been diagnosed with cancer. The nurse observes that the child often plays with dolls and pretends to be a doctor who treats sick patients. The nurse should identify that this type of play is an example of which of the following coping strategies?
Explanation
Choice A reason: This is correct. Playing with dolls and pretending to be a doctor who treats sick patients is an example of problem-focused coping, which aims to change or solve the problem that causes stress. By doing this, the child can gain a sense of control and mastery over their situation and prepare for their treatment.
Choice B reason: This is incorrect. Emotion-focused coping aims to regulate or reduce
the emotional impact of the problem, not change or solve it. Examples of emotion-focused coping include expressing feelings, seeking comfort, or using relaxation techniques.
Choice C reason: This is incorrect. Cognitive restructuring is a coping strategy that involves changing the way one thinks about the problem, not playing or pretending. Examples of cognitive restructuring include challenging negative thoughts, reframing the situation, or using positive affirmations.
Choice D reason: This is incorrect. Social support is a coping strategy that involves seeking help or assistance from others, not playing or pretending. Examples of social support include talking to a friend, family member, or counselor, joining a support group, or asking for advice.
A nurse is teaching a hospitalized child who has diabetes how to use emotion-focused coping strategies to deal with the stress of the disease. Which of the following strategies should the nurse include in the teaching?
Explanation
Choice A reason: This is incorrect. Monitoring blood glucose levels and administering insulin injections as prescribed is an example of a problem-focused coping strategy that aims to change or solve the problem that causes stress, not regulate or reduce it.
Choice B reason: This is incorrect. Learning about diabetes and its complications and prevention methods is an example of a problem-focused coping strategy that aims to change or solve the problem that causes stress, not regulate or reduce it.
Choice C reason: This is correct. Writing a journal or a diary about their feelings and experiences with diabetes is an example of an emotion-focused coping strategy that can help the child to regulate or reduce the emotional impact of the disease. By doing this, the child can express their emotions, vent their frustrations, and reflect on their coping process.
Choice D reason: This is incorrect. Joining a diabetes club or a peer group with other children who have diabetes is an example of a social support strategy that involves seeking help or assistance from others, not regulating or reducing emotions.
A nurse is evaluating the outcomes of coping strategies for a hospitalized child who is recovering from surgery. Which of the following outcomes indicate that the coping strategies are effective? (Select all that apply.)
Explanation
Choice A reason: This is correct. The child reporting less pain and discomfort after using relaxation techniques is an outcome that indicates that the coping strategy is effective, as it can reduce the physical impact of the surgery.
Choice B reason: This is correct. The child showing more interest and participation in play activities and school work is an outcome that indicates that the coping strategy is effective, as it can improve the psychological and behavioral impact of the surgery.
Choice C reason: This is correct. The child expressing more positive and optimistic thoughts and feelings about their recovery is an outcome that indicates that the coping strategy is effective, as it can enhance the emotional and cognitive impact of the surgery.
Choice D reason: This is incorrect. The child developing a fever and an infection at the surgical site is not an outcome that indicates that the coping strategy is effective, but rather a complication that may indicate ineffective coping or poor healing.
Choice E reason: This is correct. The child having a shorter length of stay and fewer complications after the surgery is an outcome that indicates that the coping strategy is effective, as it can facilitate the physiological and clinical impact of the surgery.
A nurse is caring for a hospitalized child who is experiencing stress due to a traumatic injury. Which of the following developmental factors should the nurse consider when assessing the child's coping process and responses?
Explanation
Choice A reason: This is correct. The child's age and understanding of the injury and its consequences are developmental factors that the nurse should consider when assessing the child's coping process and responses. For example, younger children may have more difficulty expressing their feelings or comprehending their situation than older children.
Choice B reason: This is incorrect. The child's temperament and personality traits that influence their reactions to stress are not developmental factors, but rather personality factors that the nurse should consider when assessing the child's coping process and responses.
Choice C reason: This is incorrect. The child's family structure and support system that affect their coping resources are not developmental factors, but rather family factors that the nurse should consider when assessing the child's coping process and responses.
Choice D reason: This is incorrect. The child's cultural background and values that shape their coping beliefs and practices are not developmental factors, but rather cultural factors that the nurse should consider when assessing the child's coping process and responses.
A nurse is teaching a hospitalized child who is undergoing dialysis how to use emotion-focused coping strategies to deal with the stress of the procedure. Which of the following strategies should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A reason: This is incorrect. Asking questions and seeking information about the procedure process and outcomes is a problem-focused coping strategy that aims to change or solve the problem that causes stress, not regulate or reduce it.
Choice B reason: This is correct. Practicing relaxation techniques such as deep breathing or guided imagery before and during the procedure is an emotion-focused coping strategy that can help the child regulate or reduce the emotional impact of the problem.
Choice C reason: This is incorrect. Setting realistic goals and planning actions to achieve them is a problem-focused coping strategy that aims to change or solve the problem that causes stress, not regulate or reduce it.
Choice D reason: This is correct. Expressing emotions and feelings about the procedure to a trusted person or a support group is an emotion-focused coping strategy that can help the child cope with the feelings associated with the problem.
Choice E reason: This is incorrect. Seeking help and assistance from health care professionals or family members when needed is a problem-focused coping strategy that aims to change or solve
the problem that causes stress, not regulate or reduce it.
A nurse is planning interventions for a hospitalized child who is using coping strategies to deal with the stress of hospitalization. Which of the following principles and guidelines should the nurse follow when planning coping interventions? (Select all that apply.)
Explanation
Choice A reason: This is correct. The interventions should be based on the individual needs and preferences of the child, such as their interests, hobbies, or goals.
Choice B reason: This is correct. The interventions should be consistent with the developmental stage and cognitive abilities of the child, such as their language skills, attention span, or reasoning abilities.
Choice C reason: This is correct. The interventions should be flexible and adaptable to changing situations and circumstances, such as different procedures, staff, or environments.
Choice D reason: This is incorrect. The interventions should not be limited to one type of coping strategy, but rather include both problem-focused and emotion-focused coping strategies, as they can complement each other and enhance coping outcomes.
Choice E reason: This is correct. The interventions should be evaluated by measuring the effectiveness and outcomes of coping strategies, such as pain relief, anxiety reduction, mood improvement, or adaptation enhancement.
A nurse is caring for a hospitalized child who has been diagnosed with leukemia. The nurse observes that the child often plays with stuffed animals and pretends to be a teacher who teaches them about health and wellness. The nurse should identify that this type of play is an example of which of the following coping strategies?
Explanation
Choice A reason: This is correct. Playing with stuffed animals and pretending to be a teacher who teaches them about health and wellness is an example of problem-focused coping, which aims to change or solve the problem that causes stress. By doing this, the child can gain a sense of control and mastery over their situation and prepare for their treatment.
Choice B reason: This is incorrect. Emotion-focused coping aims to regulate or reduce the emotional impact of the problem, not change or solve it. Examples of emotion-focused coping include expressing feelings, seeking comfort, or using relaxation techniques.
Choice C reason: This is incorrect. Cognitive restructuring is a coping strategy that involves changing the way one thinks about the problem, not playing or pretending. Examples of cognitive restructuring include challenging negative thoughts, reframing the situation, or using positive affirmations.
Choice D reason: This is incorrect. Social support is a coping strategy that involves seeking help or assistance from others, not playing or pretending. Examples of social support include talking to a friend, family member, or counselor, joining a support group, or asking for advice.
A nurse is teaching a hospitalized child who has asthma how to use problem-focused coping strategies to deal with the stress of the disease. Which of the following strategies should the nurse include in the teaching?
Explanation
Choice A reason: This is correct. Monitoring peak flow and oxygen saturation levels and using inhalers as prescribed is a problem-focused coping strategy that can help the child control their asthma symptoms and prevent exacerbations.
Choice B reason: This is correct. Learning about asthma and its triggers and prevention methods is a problem-focused coping strategy that can help the child understand their disease and how to avoid or manage it.
Choice C reason: This is incorrect. Writing a journal or a diary about their feelings and experiences with asthma is an emotion-focused coping strategy that can help the child regulate or reduce the emotional impact of the disease.
Choice D reason: This is incorrect. Joining an asthma club or a peer group with other children who have asthma is a social support strategy that involves seeking help or assistance from others, not changing or solving the problem.
A nurse is evaluating the outcomes of coping strategies for a hospitalized child who is recovering from a burn injury. Which of the following outcomes indicate that the coping strategies are effective? (Select all that apply.)
Explanation
Choice A reason: This is correct. The child reporting less pain and discomfort after using relaxation techniques is an outcome that indicates that the coping strategy is effective, as it can reduce the physical impact of the injury.
Choice B reason: This is correct. The child showing more interest and participation in play activities and school work is an outcome that indicates that the coping strategy is effective, as it can improve the psychological and behavioral impact of the injury.
Choice C reason: This is correct. The child expressing more positive and optimistic thoughts and feelings about their recovery is an outcome that indicates that the coping strategy is effective, as it can enhance the emotional and cognitive impact of the injury.
Choice D reason: This is incorrect. The child developing an infection and scarring at the burn site is not an outcome that indicates that
the coping strategy is effective, but rather a complication that may indicate ineffective coping or poor healing.
Choice E reason: This is correct. The child having a shorter length of stay and fewer complications after the injury is an outcome that indicates that the coping strategy is effective, as it can facilitate the physiological and clinical impact of the injury.
Conclusion
Explanation
Choice A reason: Asking the parents to leave the room until the child calms down is not an appropriate action, as it may increase the child's anxiety and distress, which can worsen respiratory status. The parents should be allowed to stay with the child and provide comfort and reassurance.
Choice B reason: Placing the child in a prone position with the head elevated is not an appropriate action, as it may compromise airway patency and ventilation. The child should be placed in a semi-Fowler's position or upright on the lap of a parent or caregiver.
Choice C reason: Administering oxygen via nasal cannula at 2 L/min is an appropriate action, as it can improve oxygenation and reduce respiratory distress in a child with bronchiolitis. The oxygen flow rate should be adjusted according to pulse oximetry readings and clinical signs.
Choice D reason: Offering the child a pacifier or a bottle of juice is not an appropriate action, as it may increase the risk of aspiration and dehydration in a child with respiratory distress. The child should be given small amounts of clear fluids by mouth or intravenously if oral intake is inadequate.
Explanation
Choice A reason: This is the correct definition of standard precautions, which are the basic level of infection control that should be used for the care of all patients in all healthcare settings.
Choice B reason: This is the definition of bloodborne pathogen standard, which is a specific type of standard precaution that applies to occupational exposure to blood or other potentially infectious materials.
Choice C reason: This is the definition of transmission-based precautions, which are additional infection control measures that are used for patients who are known or suspected to have infections that are spread by airborne, droplet, or contact routes.
Choice D reason: This is the definition of isolation precautions, which are a subset of transmission-based precautions that involve separating patients who have certain infections from others to prevent cross-contamination.
Explanation
Choice A reason: Praising the child for being independent and responsible is not an appropriate action, as it may encourage the child to perform activities that are beyond their physical abilities or safety limits. The nurse should assess the child's developmental level and provide appropriate guidance and supervision.
Choice B reason: Reminding the child to use the call bell before getting out of bed is an appropriate action, as it can prevent falls and injuries in a child with a fractured femur. The nurse should also instruct the child on how to use assistive devices such as crutches or a walker if indicated.
Choice C reason: Moving the items to the other side of the bed to prevent falls is not an appropriate action, as it may make them inaccessible to the child and increase their frustration or dependence. The nurse should ensure that the items are within reach and secure on the bedside table.
Choice D reason: Checking the child's identification band and allergy status is not an appropriate action, as it is not related to the safety issue of falls. The nurse should perform this action as part of routine care and medication administration.
Explanation
Choice A reason: Airborne precautions are indicated for patients who have infections that are spread by small droplet nuclei that can remain suspended in the air and travel over long distances, such as chickenpox, tuberculosis, or measles.
Choice B reason: Droplet precautions are indicated for patients who have infections that are spread by large droplet particles that travel up to 3 feet from the source, such as influenza, pertussis, or meningitis.
Choice C reason: Contact precautions are indicated for patients who have infections that are spread by direct or indirect contact with the patient or their environment, such as scabies, impetigo, or Clostridium difficile.
Choice D reason: Neutropenic precautions are indicated for patients who have low white blood cell counts and are at high risk of acquiring infections from others, such as those undergoing chemotherapy or bone marrow transplantation.
Explanation
Choice A reason: Dehydration is a common and serious complication of rotavirus gastroenteritis, which causes vomiting, diarrhea, and loss of fluids and electrolytes. The nurse should monitor the infant's intake and output, weight, vital signs, skin turgor, mucous membranes, fontanelles, and urine specific gravity.
Choice B reason: Hypoglycemia is not a typical complication of rotavirus gastroenteritis, unless there is severe malnutrition or insulin overdose. The nurse should monitor the infant's blood glucose levels if indicated by signs such as lethargy, jitteriness, or seizures.
Choice C reason: Hyperkalemia is not a typical complication of rotavirus gastroenteritis, unless there is renal failure or excessive potassium intake. The nurse should monitor the infant's serum potassium levels if indicated by signs such as muscle weakness, arrhythmias, or cardiac arrest.
Choice D reason: Metabolic alkalosis is not a typical complication of rotavirus gastroenteritis, unless there is excessive vomiting or bicarbonate intake. The nurse should monitor the infant's serum pH and bicarbonate levels if indicated by signs such as confusion, tremors, or tetany.
Explanation
Choice A reason: Washing hands and the child's hands frequently and thoroughly is an effective way to prevent the transmission of communicable diseases by removing germs and reducing contamination.
Choice B reason: Avoiding sharing personal items such as toothbrushes, cups, or utensils with the child is an effective way to prevent the transmission of communicable diseases by avoiding contact with saliva or other bodily fluids that may contain germs.
Choice C reason: Keeping the child away from other children who have signs of illness such as fever, cough, or rash is an effective way to prevent the transmission of communicable diseases by avoiding exposure to infectious agents that may be spread by airborne, droplet, or contact routes.
Choice D reason: Immunizing the child according to the recommended schedule and catch-up guidelines is an effective way to prevent the transmission of communicable diseases by stimulating the immune system to produce antibodies that protect against specific diseases.
Choice E reason: Giving the child antibiotics whenever they have a sore throat, earache, or runny nose is not an effective way to prevent the transmission of communicable diseases, as antibiotics are only effective against bacterial infections and not viral infections. Moreover, overuse or misuse of antibiotics can lead to antibiotic resistance and adverse effects.
Further questions
Summary
A nurse is caring for a child who has chickenpox, a communicable disease caused by the varicella-zoster virus. Which of the following transmission-based precautions should the nurse implement for this patient?
Explanation
Choice A reason: Contact precautions are used for patients who have infections that can be spread by direct or indirect contact with the patient or the patient's environment. Examples of infections that require contact precautions are scabies, impetigo, and Clostridium difficile.
Choice B reason: Droplet precautions are used for patients who have infections that can be spread by large respiratory droplets that are generated by coughing, sneezing, or talking. Examples of infections that require droplet precautions are influenza, pertussis, and meningitis.
Choice C reason: Airborne precautions are used for patients who have infections that can be spread by small airborne particles that can remain suspended in the air and travel over long distances. Examples of infections that require airborne precautions are tuberculosis, measles, and chickenpox.
Choice D reason: Vector-borne precautions are used for patients who have infections that can be spread by insects or animals that carry the infectious agent. Examples of infections that require vector-borne precautions are malaria, Lyme disease, and rabies.
A nurse is teaching a group of parents about the risk factors for infection in hospitalized children. Which of the following statements should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A reason: Children who have chronic conditions such as asthma or diabetes are more prone to infection because their immune system may be compromised or weakened by their underlying disease.
Choice B reason: Children who receive immunizations on time are less likely to get infected because they have developed immunity against certain diseases that can be prevented by vaccines.
Choice C reason: Children who have invasive devices such as catheters or IV lines are at increased risk of infection because these devices can introduce microorganisms into the body or create a portal of entry for infection.
Choice D reason: Children who share a room with another patient are more exposed to infection because they may come in contact with the infectious agent from the other patient or the environment.
Choice E reason: Children who have visitors or family members who are sick should not be in contact with them because they may transmit the infection to the child or vice versa.
A nurse is performing hand hygiene before entering a patient's room. The nurse's hands are not visibly soiled. Which of the following statements should the nurse make to explain the rationale for hand hygiene?
Explanation
Choice A reason: Hand hygiene is the most effective way to prevent the spread of infection because it removes or kills microorganisms that may be present on the hands and prevents their transmission to others.
Choice B reason: Hand hygiene is required by the hospital policy and accreditation standards, but this is not the primary rationale for hand hygiene. The policy and standards are based on evidence and best practices that support hand hygiene as an infection control measure.
Choice C reason: Hand hygiene is a courtesy to the patient and shows respect, but this is not the main reason for hand hygiene. The main reason is to protect the patient and oneself from infection.
Choice D reason: Hand hygiene is a personal habit that I learned from my parents, but this is not a valid explanation for hand hygiene. Hand hygiene is based on scientific principles and guidelines, not personal preferences or traditions.
A nurse is preparing to administer medication to a child who is hospitalized with an infection. The nurse scans the patient's identification bracelet and verifies the medication order. Which of the following statements should the nurse make to ensure patient safety?
Explanation
Choice A reason: Asking the patient to tell their name and date of birth is a way to confirm their identity and match it with the medication order. This is one of the steps of the "five rights" of medication administration, which are the right patient, the right drug, the right dose, the right route, and the right time.
Choice B reason: Asking the patient about their allergies or adverse reactions to medications is important, but it is not a way to ensure patient safety in terms of identification. The nurse should have checked the patient's allergy status before preparing the medication.
Choice C reason: Asking the patient how they feel today and if they have any pain or discomfort is a way to assess their condition and provide comfort measures, but it is not a way to ensure patient safety in terms of identification. The nurse should have done this assessment earlier in the shift or during the medication administration process.
Choice D reason: Asking the patient what is the name of the medication and why they are taking it is a way to educate them about their treatment and check their understanding, but it is not a way to ensure patient safety in terms of identification. The nurse should have done this education before or after giving the medication.
A nurse is cleaning a child's room after discharge. The child had an infection that required contact precautions. Which of the following actions should the nurse take to prevent environmental contamination?
Explanation
Choice A reason: Wearing gloves and a gown while handling the soiled linens and disposing of them in a biohazard bag is an appropriate action to prevent environmental contamination. This follows the standard precautions for contact with blood or body fluids and the transmission-based precautions for contact with infectious agents.
Choice B reason: Wearing a mask and eye protection while wiping the surfaces and equipment with a disinfectant solution is not necessary for contact precautions. This would be indicated for droplet or airborne precautions, where respiratory droplets or particles may be present.
Choice C reason: Wearing sterile gloves and a surgical mask while removing any sharps or needles and placing them in a puncture-resistant container is not required for contact precautions. This would be indicated for situations where there is a risk of exposure to bloodborne pathogens or other infectious materials.
Choice D reason: Wearing a respirator and a face shield while spraying an aerosol sanitizer in the air and on the curtains is not recommended for contact precautions. This would be indicated for airborne precautions, where small airborne particles may be present. However, spraying an aerosol sanitizer is not an effective way to disinfect the environment, as it may create aerosols that can spread infection.
A nurse is caring for a child who has pertussis, also known as whooping cough, which is caused by Bordetella pertussis bacteria. Which of the following types of isolation should the nurse use for this patient?
Explanation
Choice A reason: Contact isolation is used for patients who have infections that can be spread by direct or indirect contact with the patient or their environment. Pertussis is not transmitted by contact, but by respiratory droplets.
Choice B reason: Droplet isolation is used for patients who have infections that can be spread by large respiratory droplets that are generated by coughing, sneezing, or talking. Pertussis is transmitted by respiratory droplets, so droplet isolation is appropriate.
Choice C reason: Airborne isolation is used for patients who have infections that can be spread by small airborne particles that can remain suspended in the air and travel over long distances. Pertussis is not transmitted by airborne particles, but by respiratory droplets.
Choice D reason: Protective isolation is used for patients who have compromised immune systems and are at risk of acquiring infections from others. Pertussis does not require protective isolation, as it does not pose a threat to immunocompromised patients.
A nurse is teaching a parent about immunizations for children. Which of the following statements by the parent indicates an understanding of the teaching?
Explanation
Choice A reason: The MMR vaccine, which protects against measles, mumps, and rubella, is given in two doses, but not before starting school. The first dose is given at 12 to 15 months of age, and the second dose is given at 4 to 6 years of age.
Choice B reason: The DTaP vaccine, which protects against diphtheria, tetanus, and pertussis, is given in five doses, but not at age 11. The first three doses are given at 2, 4, and 6 months of age, the fourth dose is given at 15 to 18 months of age, and the fifth dose is given at 4 to 6 years of age. A booster dose of Tdap, which is a similar vaccine for older children and adults, is given at 11 to 12 years of age.
Choice C reason: The hepatitis B vaccine, which protects against hepatitis B virus infection, is given in three doses in the first year of life. The first dose is given at birth, the second dose is given at 1 to 2 months of age, and the third dose is given at 6 to 18 months of age.
Choice D reason: The varicella vaccine, which protects against chickenpox, is given in two doses, but not at age 12. The first dose is given at 12 to 15 months of age, and the second dose is given at 4 to 6 years of age.
A nurse is reviewing the laboratory results of a child who has an infection. Which of the following findings should the nurse report to the provider? (Select all that apply.)
Explanation
Choice A reason: A white blood cell count (WBC) of 12,000/mm3 is within the normal range for children aged 2 to 6 years. A WBC count above this range may indicate an infection or inflammation.
Choice B reason: An erythrocyte sedimentation rate (ESR) of 40 mm/h is elevated for children aged 2 to 6 years. The normal range for this age group is 0 to 20 mm/h. An ESR above this range may indicate an infection or inflammation.
Choice C reason: A C-reactive protein (CRP) level of 8 mg/L is elevated for children aged 2 to 6 years. The normal range for this age group is less than 1 mg/L. A CRP level above this range may indicate an infection or inflammation.
Choice D reason: A blood culture positive for Staphylococcus aureus indicates a bacterial infection in the bloodstream. This can be a serious condition that requires prompt treatment with antibiotics.
Choice E reason: A urine culture negative for Escherichia coli indicates no bacterial infection in the urinary tract. This is a normal finding that does not require further action.
A nurse is teaching a group of parents about the chain of infection. Which of the following statements by one of the parents indicates a need for further teaching?
Explanation
Choice A reason: This is a correct statement. The infectious agent is the microorganism that causes the disease, such as bacteria, viruses, fungi, or parasites.
Choice B reason: This is a correct statement. The reservoir is where the microorganism lives and grows, such as humans, animals, plants, soil, or water.
Choice C reason: This is an incorrect statement. The portal of exit is how the microorganism leaves the body of the reservoir, not how it enters the body of the host. The portal of entry is how the microorganism enters the body of the host.
Choice D reason: This is a correct statement. The susceptible host is someone who is at risk for getting the infection, such as children, elderly, immunocompromised, or malnourished people.
A nurse is caring for a child who has chickenpox. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A reason: This is an incorrect action. The nurse should place the child in a private room with negative air pressure only if the child has an airborne infection, such as tuberculosis or measles. Chickenpox is transmitted by both airborne and contact routes, so a private room with positive air pressure is sufficient.
Choice B reason: This is a correct action. The nurse should wear gloves and a gown when entering the room to prevent contact transmission of chickenpox.
Choice C reason: This is a correct action. The nurse should apply calamine lotion to the skin lesions to relieve itching and prevent scratching.
Choice D reason: This is a correct action. The nurse should administer acyclovir as prescribed to reduce viral shedding and shorten the duration of symptoms.
Choice E reason: This is an incorrect action. The nurse should not give aspirin for fever and pain relief to a child who has chickenpox, because it can increase the risk of Reye syndrome, a rare but serious condition that affects the liver and brain.
A nurse is assessing a child who has been admitted with a urinary tract infection (UTI). Which of the following statements by the child's parent indicates a possible source of infection?
Explanation
Choice A reason: This is not a possible source of infection. Wiping from front to back after using
the toilet can prevent bacteria from entering the urinary tract and causing infection.
Choice B reason: This is not a possible source of infection. Drinking plenty of water and cranberry juice every day can help flush out bacteria from
the urinary tract and prevent infection.
Choice C reason: This is a possible source of infection. Taking bubble baths with toys can introduce bacteria into
the urinary tract and cause infection.
Choice D reason: This is not a possible source of infection. Wearing cotton underwear and loose-fitting pants can allow air circulation and prevent moisture buildup in
the genital area, which can reduce
the risk of infection.
A nurse is planning care for a child who has pertussis (whooping cough). Which of
the following interventions should be included in
the plan?
Explanation
Choice A reason: This is not a priority intervention. The nurse should encourage oral fluids and soft foods to prevent dehydration and maintain nutrition, but this is not as important as monitoring the child for respiratory distress.
Choice B reason: This is an incorrect intervention. The nurse should not administer antitussive medication to a child who has pertussis, because it can suppress the cough reflex and increase the risk of mucus accumulation and airway obstruction.
Choice C reason: This is not a priority intervention. The nurse should provide humidified oxygen via nasal cannula to moisten the airways and ease breathing, but this is not as important as monitoring the child for respiratory distress.
Choice D reason: This is a priority intervention. The nurse should monitor the child for signs of respiratory distress, such as cyanosis, tachypnea, retractions, or nasal flaring, because pertussis can cause severe coughing spells that can interfere with breathing.
A nurse is evaluating the effectiveness of infection control education for a group of parents of hospitalized children. Which of the following statements by one of the parents indicates an understanding of the teaching?
Explanation
Choice A reason: This is a correct statement. The parent indicates an understanding of the teaching by stating that they will wash their hands with soap and water before and after visiting their child, which is a key component of standard precautions and infection control.
Choice B reason: This is an incorrect statement. The parent does not need to wear a mask and gloves when they enter their child's room, unless their child has a known or suspected infection that requires transmission-based precautions.
Choice C reason: This is an incorrect statement. The parent should not bring fresh flowers and balloons for their child, because they can harbor microorganisms and allergens that can cause infection or irritation.
Choice D reason: This is an incorrect statement. The parent should not share their child's toys with other children in the ward, because they can transmit microorganisms and cause cross-infection.
A nurse is caring for a 4-year-old child who has been diagnosed with rotavirus gastroenteritis. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A reason: This is a correct action. The nurse should administer oral rehydration solution as prescribed to prevent dehydration and electrolyte imbalance.
Choice B reason: This is a correct action. The nurse should monitor the child's weight and intake and output to assess fluid status and hydration level.
Choice C reason: This is a correct action. The nurse should isolate the child from other children in the unit to prevent transmission of rotavirus, which is highly contagious.
Choice D reason: This is an incorrect action. The nurse does not need to collect stool specimens for culture and sensitivity, because rotavirus gastroenteritis is diagnosed by antigen detection tests or polymerase chain reaction (PCR) tests.
Choice E reason: This is a correct action. The nurse should teach the parents about proper hand hygiene to prevent infection and cross-contamination.
A nurse is caring for a 2-year-old child who has impetigo contagiosa on his face
and hands. Which of the following actions should
the nurse take?
Explanation
Choice A reason: This is a correct action. The nurse should apply topical antibiotics to the lesions twice a day to treat the infection and prevent its spread.
Choice B reason: This is an incorrect action. The nurse should not cover the lesions with sterile gauze dressings, because this can create a moist environment that promotes bacterial growth and delays healing.
Choice C reason: This is not a priority action. The nurse should wash the lesions with warm water and soap daily to remove crusts and debris, but this is not as important as applying topical antibiotics.
Choice D reason: This is not a priority action. The nurse should trim the child's fingernails and discourage scratching to prevent skin damage and secondary infection, but this is not as important as applying topical antibiotics.
A nurse is reviewing the immunization record of a 6-month-old infant who is due for a well-child visit. Which of the following vaccines should the nurse expect to administer? (Select all that apply.)
Explanation
Choice A reason: This is the correct vaccine. The nurse should expect to administer rotavirus vaccine to a 6-month-old infant, as the third dose of this vaccine is given at 6 months of age.
Choice B reason: This is the correct vaccine. The nurse should expect to administer diphtheria, tetanus, and acellular pertussis vaccine to a 6-month-old infant, as the third dose of this vaccine is given at 6 months of age.
Choice C reason: This is the correct vaccine. The nurse should expect to administer Haemophilus influenzae type b vaccine to a 6-month-old infant, as the third dose of this vaccine is given at 6 months of age.
Choice D reason: This is an incorrect vaccine. The nurse should not expect to administer measles, mumps, and rubella vaccine to a 6-month-old infant, as the first dose of this vaccine is given at 12 months of age.
Choice E reason: This is a correct vaccine. The nurse should expect to administer pneumococcal conjugate vaccine to a 6-month-old infant, as the third dose of this vaccine is given at 6 months of age.
Exams on Nursing Care of Hospitalized Children
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- To describe the admission and discharge procedures for pediatric patients in hospitals.
- To identify the common reasons and challenges for hospitalization of children.
- To explain the role of the nurse in providing family-centered care and promoting the child’s well-being during hospitalization.
- To discuss the developmental, emotional, and psychosocial needs of hospitalized children and their families.
- To apply the nursing process and evidence-based practice to plan, implement, and evaluate care for hospitalized children.
- To recognize the potential complications and risks of hospitalization for children and implement preventive and therapeutic measures.
- To define infection, colonization, and communicable disease and explain their differences.
- To describe the chain of infection and the modes of transmission of infectious agents.
- To identify the risk factors and sources of infection in hospitalized children.
- To discuss the standard and transmission-based precautions for preventing and controlling infection in hospitalized children.
- To explain the principles and techniques of hand hygiene, personal protective equipment, environmental cleaning, and waste disposal in infection control.
- To apply the nursing process in caring for hospitalized children with infectious or communicable diseases.
- To define safety and explain its importance in the nursing care of hospitalized children.
- To identify the common hazards and risks for injury or harm in hospitalized children.
- To describe the strategies and interventions to prevent or minimize the potential for injury or harm in hospitalized children.
- To apply the principles of patient safety and quality improvement in the nursing care of hospitalized children.
- To evaluate the effectiveness and outcomes of safety measures in the nursing care of hospitalized children.
- To educate the child and family about safety issues and prevention measures in hospitalized children.
- To define play and distraction techniques and explain their importance in the nursing care of hospitalized children.
- To identify the benefits and outcomes of play and distraction techniques for hospitalized children.
- To describe the types and examples of play and distraction techniques for hospitalized children.
- To apply the principles and guidelines of play and distraction techniques in nursing care of hospitalized children.
- To evaluate the effectiveness and satisfaction of play and distraction techniques in the nursing care of hospitalized children.
- To define coping and explain its importance in nursing care of hospitalized children.
- To identify the factors that influence the coping process and responses of hospitalized children.
- To describe the types and examples of coping strategies for hospitalized children.
- To apply the principles and guidelines of coping assessment and intervention in the nursing care of hospitalized children.
- To educate the child and family about coping issues and resources in nursing care of hospitalized children.
Introduction
- Hospitalization is a stressful and disruptive experience for children and their families.
- Children may face separation from their parents, siblings, friends, and familiar environment; loss of control and autonomy; exposure to painful or invasive procedures; fear of unknown outcomes; and disruption of their normal routines and activities.
- These factors can affect the child’s physical, cognitive, emotional, and social development, as well as their coping skills and resilience.
- Therefore, nurses who care for hospitalized children need to have specialized knowledge, skills, and attitudes to provide safe, effective, and holistic care that meets the unique needs of each child and family.
- Safety is the prevention of errors and adverse events that may cause injury or harm to patients, staff, or visitors in health care settings1.
- Safety is a vital aspect of nursing care for hospitalized children because they are more vulnerable to hazards and risks due to their developmental stage, cognitive level, physical size, curiosity, and dependence on others2.
- Coping is the process of managing or adapting to stressors or challenges that threaten one’s well-being or functioning1.
- Coping is important in nursing care of hospitalized children because it can help to reduce the negative effects of hospitalization, such as pain, anxiety, fear, anger, sadness, boredom, loneliness, isolation, loss of control, loss of identity, loss of routine, loss of peers, etc.2.
- Coping can also promote positive outcomes of hospitalization, such as resilience, self-esteem, self-efficacy, competence, mastery, autonomy, social support, etc.2.

Admission and discharge procedures
Admission Procedures
The admission process is the first step in establishing a trusting relationship between the nurse, the child, and the family. The nurse should perform the following tasks during admission:
- Verify the child’s identity and assess his or her clinical status.
- Make the child as comfortable as possible and provide appropriate pain relief if needed.
- Introduce the child and family to the staff, roommates, and environment.
- Orient the child and family to the unit policies, routines, facilities, and resources.
- Provide supplies and special equipment needed for daily care, such as diapers, toys, books, games, etc.
- Review the child’s medical history, medication list, allergies, immunizations, growth charts, developmental milestones, etc.
- Obtain baseline vital signs, height, weight, head circumference (for infants), pain score, etc. Normal ranges for vital signs vary by age group. Table 1 shows some examples of normal ranges for different age groups1.
|
Age Group |
Heart Rate (beats/min) |
Respiratory Rate (breaths/min) |
Blood Pressure (mm Hg) |
|
Newborn |
100-160 |
30-60 |
60-90/20-60 |
|
Infant |
100-150 |
25-50 |
70-95/35-65 |
|
Toddler |
90-140 |
20-40 |
80-105/40-70 |
|
Preschooler |
80-110 |
20-30 |
85-110/45-75 |
|
School-age |
75-100 |
15-25 |
90-115/50-80 |
|
Adolescent |
60-90 |
12-20 |
95-120/55-85 |
- Perform a comprehensive physical assessment using a systematic approach. Use developmentally appropriate techniques to elicit cooperation from the child. For example, use distraction, play, or storytelling to reduce anxiety or fear; allow the child to touch or examine equipment before use; explain procedures in simple terms; praise the child for cooperation; etc.
- Collect specimens for laboratory tests as ordered by the physician. Follow standard precautions and infection control measures when handling specimens. Label specimens correctly and transport them to the laboratory promptly.
- Administer medications as ordered by the physician. Follow the six rights of medication administration: right patient, right drug, right dose, right route, right time, right documentation. Use pediatric-specific dosing formulas or charts to calculate drug doses based on the child’s weight or body surface area. Use appropriate devices or techniques to administer medications to children. For example, use oral syringes or droppers for liquid medications; crush tablets or open capsules and mix with food or liquid if allowed; apply topical medications with gloves or cotton swabs; etc.
- Initiate intravenous (IV) therapy as ordered by the physician. Select an appropriate IV site based on the child’s age, condition, and type of infusion. Use an aseptic technique to insert an IV catheter and secure it with tape or dressing. Monitor the IV site for signs of infiltration, phlebitis, infection, or extravasation. Adjust the IV flow rate according to the physician’s order or protocol. Use an infusion pump or controller to deliver accurate and safe IV fluids or medications.
- Implement other interventions as ordered by the physician or indicated by the child’s condition. For example,
- Apply oxygen therapy if the child has hypoxia or respiratory distress. Use an appropriate device to deliver oxygen at the prescribed concentration. Monitor the child’s oxygen saturation level using a pulse oximeter. Assess the child’s respiratory rate, depth, rhythm, effort, breath sounds, etc.
- Insert a nasogastric (NG) tube if the child has vomiting, gastric decompression, feeding intolerance, malnutrition, etc. Use a measuring tape to determine the correct length of insertion based on the child’s nose-to-ear-to-xiphoid process distance. Use a syringe to aspirate gastric contents and check pH level to confirm proper placement. Secure the NG tube with tape or dressing. Monitor the NG tube function, output, patency, etc.
- Insert a urinary catheter if the child has urinary retention, obstruction, infection, incontinence, etc. Use an appropriate size and type of catheter based on the child’s age, gender, and condition. Use an aseptic technique to insert the catheter and collect urine. Secure the catheter with tape or dressing. Monitor the catheter function, output, patency, etc.
- Document all admission data and interventions in the child’s medical record. Use clear, concise, accurate, and timely language. Follow the SOAP format: subjective data (what the child or family says), objective data (what the nurse observes or measures), assessment (what the nurse concludes or diagnoses), and plan (what the nurse plans to do or has done).
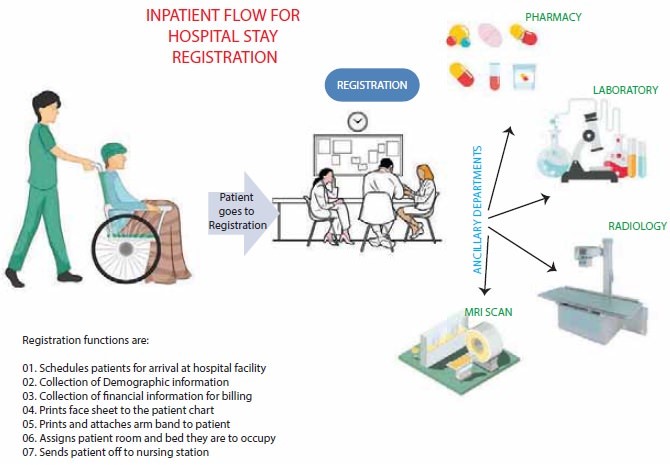
Discharge Procedures
The discharge process is the final step in ensuring a smooth transition from hospital to home for the child and family. The nurse should perform the following tasks during discharge:
- Review the child’s progress and readiness for discharge with the healthcare team. Ensure that the child has met the discharge criteria, such as stable vital signs, adequate pain control, improved symptoms, normal laboratory values, etc.
- Obtain a discharge order from the physician. The order should include the date and time of discharge, the mode of transportation, the destination, and any follow-up instructions or referrals.
- Educate the child and family about the discharge plan and home care. Use developmentally appropriate methods to teach the child and family about the diagnosis, treatment, medications, diet, activity, wound care, infection prevention, signs of complications, when to seek medical attention, etc. Use teach-back or return-demonstration techniques to evaluate the child and family’s understanding and ability to perform home care. Provide written instructions and contact information for questions or concerns.
- Arrange for any necessary equipment, supplies, or services for home care. For example,
- Order a home health nurse or therapist if the child needs skilled care at home.
- Order a durable medical equipment (DME) company to deliver oxygen tanks, infusion pumps, feeding tubes, etc.
- Order a pharmacy to deliver medications or supplies for home use.
- Coordinate with social workers or case managers to arrange for financial assistance, transportation, respite care, etc.
- Reconcile the child’s medications before discharge. Compare the medications that the child was taking before admission with those that he or she will be taking after discharge. Identify any discrepancies or changes and communicate them to the child and family. Provide a complete and accurate list of medications that the child will be taking at home, including names, doses, routes, frequencies, indications, side effects, interactions, etc.
- Perform a final physical assessment and vital signs check on the child. Ensure that the child is stable, comfortable, and ready for discharge. Remove any IV lines, catheters, dressings, etc . that are no longer needed. Apply bandages or ointments as needed. Assist the child with dressing and personal hygiene.
- Collect any valuables or belongings that were stored in the hospital. Return them to the child and family. Check that nothing is left behind in the room.
- Escort the child and family to the exit. Help them with loading their belongings into their vehicle or arranging for transportation. Thank them for choosing your hospital and wish them well.
- Document all discharge data and interventions in the child’s medical record. Use clear, concise, accurate, and timely language. Follow the SOAP format: subjective data (what the child or family says), objective data (what the nurse observes or measures), assessment (what the nurse concludes or diagnoses), and plan (what the nurse plans to do or has done).
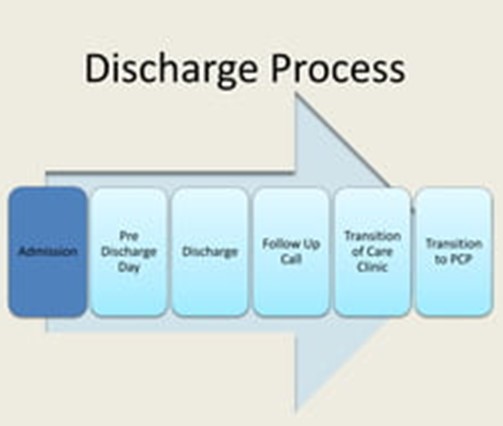
Infection Control
- Infection is the invasion of body tissue by microorganisms with the potential to cause illness or disease1.
- Colonization is the presence of microorganisms on or in a host without causing signs or symptoms of infection2.
- Communicable disease is an infectious disease that can be transmitted from one person to another through direct or indirect contact2.
- Infection control is the practice of preventing and reducing the spread of infections in healthcare settings2.
- Infection control is important for hospitalized children because they are more vulnerable to infections due to their immature immune system, frequent exposure to invasive procedures, and contact with other sick children1.
Chain of infection and modes of transmission
- The chain of infection is a model that describes how an infection occurs and spreads. It consists of six links: infectious agent, reservoir, portal of exit, mode of transmission, portal of entry, and susceptible host2.
- Infectious agent is a microorganism that causes the infection, such as bacteria, viruses, fungi, or parasites2.
- Reservoir is the place where the infectious agent lives and multiplies, such as humans, animals, soil, water, or medical equipment2.
- Portal of exit is the way the infectious agent leaves the reservoir, such as through respiratory secretions, blood, urine, feces, or wounds2.
- The mode of transmission is the way the infectious agent travels from the reservoir to the susceptible host. There are four main modes: contact (direct or indirect), droplet, airborne, and vector-borne2.
- Portal of entry is the way the infectious agent enters the susceptible host, such as through mucous membranes, skin breaks, or injection sites2.
- Susceptible host is a person who is at risk of getting infected by the infectious agent. Factors that affect susceptibility include age, immunization status, health condition, and medication use2.
Risk factors and sources of infection in hospitalized children
- Hospitalized children are at risk of acquiring two types of infections: healthcare-associated infections (HAIs) and community-acquired infections (CAIs)1.
- HAIs are infections that occur during or after receiving health care services. They are also called nosocomial infections. Examples of HAIs include catheter-associated urinary tract infections (CAUTIs), central line-associated bloodstream infections (CLABSIs), surgical site infections (SSIs), ventilator-associated pneumonia (VAP), and Clostridioides difficile infection (CDI)2.
- CAIs are infections that are acquired outside of healthcare settings. They are also called community-acquired infections. Examples of CAIs include respiratory tract infections (RTIs), gastrointestinal infections (GIs), skin and soft tissue infections (SSTIs), and meningitis1.
- The sources of infection in hospitalized children may vary depending on the type and location of infection. Some common sources are:
- Other infected patients or healthcare workers
- Contaminated medical devices or equipment
- Environmental surfaces or objects
- Visitors or family members
- Animals or insects
- Food or water
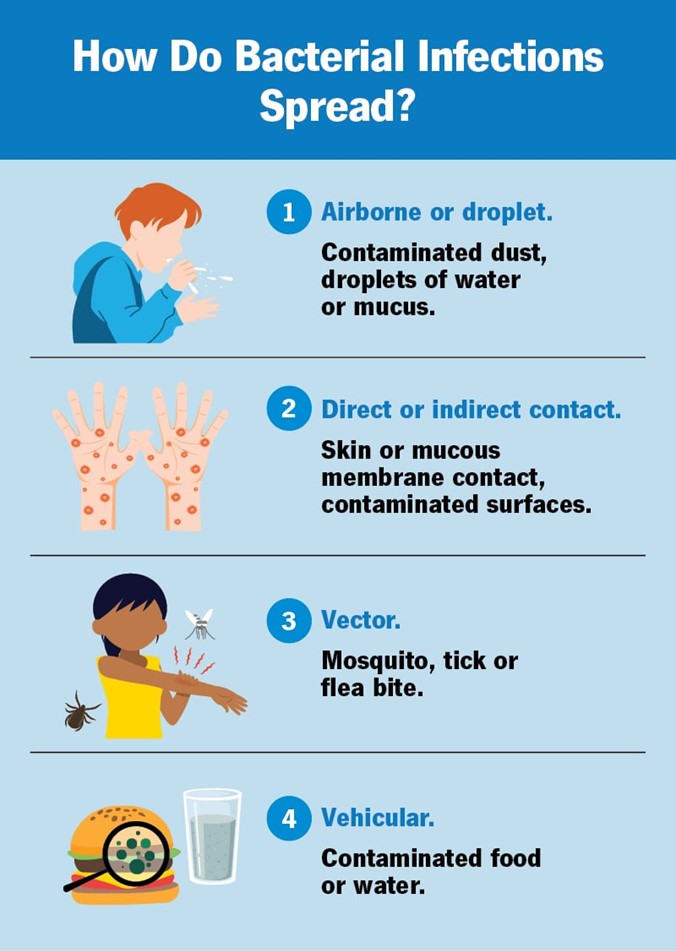
Standard and transmission-based precautions
- Standard precautions are the basic level of infection control that should be used for all patients regardless of their diagnosis or presumed infection status. They are based on the principle that all blood, body fluids, secretions, excretions, non-intact skin, and mucous membranes may contain infectious agents2. Standard precautions include:
- Hand hygiene: washing hands with soap and water or using alcohol-based hand rub before and after patient contact, after removing gloves, after contact with potentially infectious materials, and before performing invasive procedures2.
- Personal protective equipment (PPE): wearing gloves, gowns, masks, eye protection, or face shields as appropriate to prevent exposure to blood or body fluids2.
- Respiratory hygiene/cough etiquette: covering mouth and nose when coughing or sneezing, using tissues and disposing them properly, wearing a mask if possible, and maintaining a distance of at least 3 feet from others2.
- Patient placement: assigning patients to private rooms if possible or cohorting them with other patients with the same infection. Isolating patients who pose a risk of transmitting airborne or droplet infections2.
- Environmental cleaning: cleaning and disinfecting frequently touched surfaces and equipment with appropriate agents. Following manufacturer’s instructions for reprocessing reusable medical devices2.
- Waste disposal: disposing of sharps, infectious, and hazardous waste in designated containers. Following local regulations for waste management2.
- Linen handling: handling soiled linen with minimal agitation and wearing gloves and gowns. Placing linen in leak-proof bags and transporting them to laundry facilities2.
- Patient care equipment: using disposable or dedicated equipment for each patient if possible. Cleaning and disinfecting equipment between patient use if shared2.
- Patient education: educating patients and families about the signs and symptoms of infection, the modes of transmission, the prevention measures, and the treatment options1.
- Transmission-based precautions are additional infection control measures that should be used for patients with known or suspected infections that are transmitted by contact, droplet, or airborne routes. They are based on the type of microorganism and the mode of transmission. They are used in addition to standard precautions2. Transmission-based precautions include:
- Contact precautions: used for patients with infections that are spread by direct or indirect contact with the patient or the patient’s environment. Examples of infections that require contact precautions are MRSA, VRE, ESBL, CDI, RSV, scabies, and impetigo2. Contact precautions include:
- Wearing gloves and gowns when entering the patient’s room or having contact with the patient or the patient’s environment2.
- Using disposable or dedicated patient care equipment. Cleaning and disinfecting non-disposable equipment before use on another patient2.
- Placing the patient in a private room or cohorting them with other patients with the same infection. Limiting the movement of the patient outside the room2.
- Educating the patient and family about the infection and the prevention measures1.
- Droplet precautions: used for patients with infections that are spread by large respiratory droplets that are generated by coughing, sneezing, or talking. Examples of infections that require droplet precautions are influenza, pertussis, mumps, rubella, and meningococcal disease2. Droplet precautions include:
- Wearing a mask when entering the patient’s room or having contact with the patient within 3 feet2.
- Wearing eye protection or a face shield if there is a risk of splashes or sprays of respiratory secretions2.
- Placing the patient in a private room or cohorting them with other patients with the same infection. Limiting the movement of the patient outside the room. If the patient needs to be transported, having them wear a mask if possible2.
- Educating the patient and family about the infection and the prevention measures1.
- Airborne precautions: used for patients with infections that are spread by small respiratory droplets that remain suspended in the air and can be inhaled by others. Examples of infections that require airborne precautions are tuberculosis, measles, chickenpox, and disseminated herpes zoster2. Airborne precautions include:
- Wearing a respirator (such as N95) when entering the patient’s room or having contact with the patient2.
- Placing the patient in a private room with negative air pressure and 6 to 12 air changes per hour. Keeping the door closed at all times. Limiting the movement of the patient outside the room. If the patient needs to be transported, having them wear a mask if possible2.
- Educating the patient and family about the infection and the prevention measures1.
- Contact precautions: used for patients with infections that are spread by direct or indirect contact with the patient or the patient’s environment. Examples of infections that require contact precautions are MRSA, VRE, ESBL, CDI, RSV, scabies, and impetigo2. Contact precautions include:
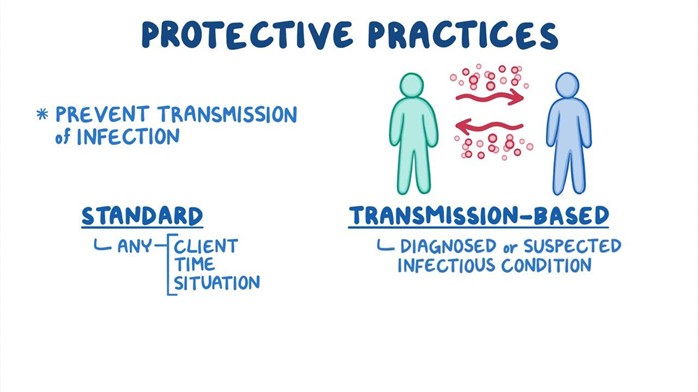
Safety measures
- Some of the common hazards and risks for injury or harm in hospitalized children are:
- Falls: the most frequent cause of injury in hospitalized children. Factors that increase the risk of falls include age, mobility, medication use, medical devices, environmental factors, and parental supervision2.
- Medication errors: the administration of incorrect medication or dosage to a patient. Factors that increase the risk of medication errors include lack of standardization, communication barriers, calculation errors, look-alike or sound-alike drugs, and high-alert medications1.
- Infection: the invasion of body tissue by microorganisms with potential to cause illness or disease. Factors that increase the risk of infection include immature immune system, frequent exposure to invasive procedures, contact with other sick children, and poor infection control practices2.
- Equipment-related injuries: the damage or harm caused by medical devices or equipment. Factors that increase the risk of equipment-related injuries include malfunction, misuse, disconnection, entanglement, electrical shock, or burns2.
- Procedure-related injuries: the damage or harm caused by diagnostic or therapeutic procedures. Factors that increase the risk of procedure-related injuries include pain, bleeding, bruising, infection, allergic reaction, or complications2.
- Physical restraint injuries: the damage or harm caused by the use of devices or methods to restrict a patient’s movement. Factors that increase the risk of physical restraint injuries include skin breakdown, nerve damage, circulation impairment, aspiration, suffocation, or psychological distress1.
- Safety measures are the strategies and interventions to prevent or minimize the potential for injury or harm in hospitalized children. They are based on the principles of patient safety and quality improvement. They include:
- Assessment: collecting data about the child’s health status, developmental stage, cognitive level, risk factors for injury or harm, and safety needs. Using standardized tools such as pediatric fall risk assessment scale (PFRA), pediatric early warning score (PEWS), pediatric sedation scale (PSS), etc.2.
- Planning: setting goals and outcomes for safety and quality improvement. Developing policies and protocols for safety measures. Providing resources and equipment for safety measures. Collaborating with other health care professionals and agencies for safety measures1.
- Implementation: carrying out the planned interventions to achieve the desired outcomes. Applying the strategies and interventions for safety measures such as:
- Fall prevention: using age-appropriate crib and bedding; securing equipment and cords; maintaining bed in low position; keeping crib rails up when parent not at bedside; establishing list of approved visitors; staff communication when parent leaves; adolescent issues3.
- Medication administration: following the six rights of medication administration (right patient, right drug, right dose, right route, right time, right documentation); using barcode scanning; double-checking calculations; avoiding abbreviations; labeling syringes; using smart pumps; reporting errors1.
- Infection control: following standard and transmission-based precautions; performing hand hygiene; wearing personal protective equipment (PPE); cleaning and disinfecting environmental surfaces and equipment; disposing of waste properly; educating patients and families1.
- Equipment safety: checking equipment function and calibration; following manufacturer’s instructions; securing tubing and wires; monitoring alarms and settings; removing unnecessary equipment; reporting malfunction2.
- Procedure safety: obtaining informed consent; verifying patient identity; marking operative site; using time-out before procedure; monitoring vital signs; managing pain; preventing complications1.
- Restraint safety: using restraints only as a last resort; obtaining order from provider; choosing least restrictive type and size; applying restraints correctly; monitoring skin integrity; removing one restraint at a time on a regular basis1.
- Evaluation: measuring the effectiveness and outcomes of safety measures. Comparing the actual outcomes with the expected outcomes. Evaluating the child’s progress toward the goals and modifying the plan of care as needed. Evaluating the child’s satisfaction with the care and identifying areas for improvement. Evaluating the quality and safety of safety measures and reporting any errors or adverse events.
- Education: educating the child and family about safety issues and prevention measures. Providing information and instructions about safety measures. Encouraging participation and feedback from the child and family. Reinforcing positive behaviors and correcting unsafe behaviors. Providing resources and referrals for safety measures.

Play and distraction techniques
- Play is an essential part of childhood that supports the development of physical, cognitive, social, and emotional skills. It is also a way of expressing feelings, coping with stress, and having fun1.
- Distraction is a psychological strategy that involves shifting the child’s attention from a painful or stressful stimulus to a more pleasant or engaging one. It is based on the idea that pain and anxiety are influenced by cognitive and emotional factors2.
- Play and distraction techniques are important in the nursing care of hospitalized children because they can help to reduce pain, anxiety, fear, boredom, and loneliness. They can also promote coping, adaptation, healing, and well-being3.
Types and examples of play and distraction techniques
- Play and distraction techniques can be classified into different types according to their purpose, content, format, or mode. Some of the types and examples are:
- Therapeutic play: play that is designed to help the child cope with a specific health problem or procedure. Examples of therapeutic play are:
- Medical play: play that involves using medical equipment or dolls to simulate a medical procedure or situation. It can help the child to understand, prepare, or rehearse for a procedure or situation.
- Expressive play: play that involves using art, music, drama, or storytelling to express feelings, thoughts, or experiences. It can help the child to communicate, vent, or resolve emotional issues.
- Guided imagery: play that involves using mental images or stories to create a relaxing or pleasant scenario. It can help the child to relax, visualize, or imagine a positive outcome.
- Recreational play: play that is designed to provide fun, enjoyment, or entertainment for the child. Examples of recreational play are:
- Games: play that involves following rules, competing, or cooperating with others. It can help the child to have fun, challenge oneself, or socialize with others.
- Toys: play that involves using objects that are designed for amusement or stimulation. It can help the child to have fun, explore, or learn new skills.
- Books: play that involves reading or listening to stories that are written or told for pleasure or education. It can help the child to have fun, escape reality, or learn new information.
- Developmental play: play that is designed to support the child’s growth and development according to their age and stage. Examples of developmental play are:
- Sensorimotor play: play that involves using sensory and motor skills to interact with the environment. It can help the child to develop physical abilities, coordination, and perception. Examples of sensorimotor play are bubbles, balls, blocks, etc.
- Cognitive play: play that involves using mental skills to solve problems, make decisions, or acquire knowledge. It can help the child to develop intellectual abilities, reasoning, and memory. Examples of cognitive play are puzzles, cards, board games, etc.
- Social play: play that involves using interpersonal skills to relate with others. It can help the child to develop social abilities, communication, and empathy. Examples of social play are role-playing, puppets, dolls, etc.
- Multimodal play: play that involves using more than one type of play or more than one mode of delivery. It can help the child to benefit from multiple aspects of play and distraction techniques. Examples of multimodal play are:
- Video games: play that involves using electronic devices to interact with a virtual world. It can combine elements of therapeutic (e.g., virtual reality), recreational (e.g., action), cognitive (e.g., strategy), and social (e.g., multiplayer) play.
- Music therapy: play that involves using music as a medium for expression, communication, or relaxation. It can combine elements of therapeutic (e.g., songwriting), recreational (e.g., listening), cognitive (e.g., learning), and social (e.g., singing) play.

Benefits and outcomes of play and distraction techniques
- Play and distraction techniques can have positive effects on the child’s physical, psychological, and behavioral outcomes. Some of the benefits and outcomes are:
- Reduced pain perception and intensity: play and distraction techniques can decrease the child’s awareness of pain by competing with the pain signals in the brain. They can also reduce the child’s emotional response to pain by enhancing positive emotions and reducing negative emotions.
- Reduced anxiety and fear: play and distraction techniques can lower the child’s stress level by providing a sense of control, security, and comfort. They can also reduce the child’s anticipatory anxiety and fear by diverting attention from the threatening stimulus or situation.
- Increased coping and adaptation: play and distraction techniques can enhance the child’s coping skills by providing opportunities to express feelings, vent frustrations, and resolve conflicts. They can also facilitate the child’s adaptation to the hospital environment by providing familiarity, continuity, and normalcy.
- Improved healing and well-being: play and distraction techniques can promote the child’s healing process by stimulating the immune system, increasing blood flow, and releasing endorphins. They can also improve the child’s well-being by supporting growth, development, learning, and socialization.
Principles and guidelines of play and distraction techniques
- Play and distraction techniques should be based on the following principles and guidelines in the nursing care of hospitalized children:
- Child-centered: play and distraction techniques should be tailored to the child’s preferences, interests, needs, and abilities. They should respect the child’s autonomy, dignity, and rights. They should involve the child in the planning, implementation, and evaluation of play and distraction techniques.
- Developmentally appropriate: play and distraction techniques should match the child’s developmental stage, cognitive level, and emotional maturity. They should support the child’s growth and development. They should use language and materials that are suitable for the child’s age and stage.
- Culturally sensitive: play and distraction techniques should consider the child’s cultural background, beliefs, values, and practices. They should respect the child’s diversity and individuality. They should use culturally relevant and respectful play and distraction techniques.
- Evidence-based: play and distraction techniques should be based on the best available scientific evidence and clinical expertise. They should follow the standards and guidelines of professional organizations and agencies. They should use valid and reliable tools and methods to measure the effectiveness and outcomes of play and distraction techniques.
- Collaborative: play and distraction techniques should involve collaboration with the child, family, health care team, and community. They should foster communication, coordination, and cooperation among all stakeholders. They should seek feedback and input from the child and family. They should refer to other resources or services as needed.
Effectiveness and satisfaction of play and distraction techniques
- The effectiveness and satisfaction of play and distraction techniques can be evaluated by using various tools and methods to measure the physical, psychological, and behavioral outcomes of play and distraction techniques. Some of the tools and methods are:
- Pain scales: tools that measure the child’s pain perception and intensity. Examples of pain scales are:
- Faces pain scale-revised (FPS-R): a tool that uses six faces with different expressions to indicate pain levels from 0 (no pain) to 10 (very much pain). It is suitable for children aged 4 years or older.
- FLACC scale: a tool that uses five categories (face, legs, activity, cry, consolability) to score pain behaviors from 0 (no pain) to 10 (severe pain). It is suitable for children aged 2 months to 7 years or older.
- Numeric rating scale (NRS): a tool that uses a number line from 0 (no pain) to 10 (worst possible pain) to rate pain intensity. It is suitable for children aged 8 years or older.
- Anxiety scales: tools that measure the child’s anxiety level or state. Examples of anxiety scales are:
- State-trait anxiety inventory for children (STAIC): a tool that uses two subscales (state anxiety and trait anxiety) to assess how anxious the child feels at a given moment or in general. It is suitable for children aged 9 to 12 years.
- Children’s fear scale (CFS): a tool that uses a single item with five faces ranging from happy to terrified to indicate fear level from 0 (no fear) to 4 (very much fear). It is suitable for children aged 4 to 16 years.
- Modified Yale preoperative anxiety scale (mYPAS): a tool that uses five domains (activity, vocalizations, emotional expressivity, state of apparent arousal, use of parents) to score preoperative anxiety from 22.5 (no anxiety) to 100 (extreme anxiety). It is suitable for children aged 2 to 12 years.
- Satisfaction surveys: tools that measure the child’s or family’s satisfaction with the care or service provided. Examples of satisfaction surveys are:
- Pediatric quality of life inventory (PedsQL): a tool that uses four subscales (physical functioning, emotional functioning, social functioning, school functioning) to assess health-related quality of life from 0 (poor) to 100 (excellent). It is suitable for children aged 2 to 18 years.
- Child health questionnaire-parent form (CHQ-PF50): a tool that uses 15 subscales (physical functioning, role/social limitations-emotional/behavioral, role/social limitations-physical, bodily pain/discomfort, behavior, mental health, self-esteem, general health perceptions, parental impact-emotional, parental impact-time, family activities, family cohesion, change in health) to assess health status from 0 (poor) to 100 (excellent). It is suitable for parents of children aged 5 to 18 years.
- Client satisfaction questionnaire-8 (CSQ-8): a tool that uses eight items with four-point Likert scales to measure satisfaction with service quality from 8 (low) to 32 (high). It is suitable for adults or adolescents.
- Pain scales: tools that measure the child’s pain perception and intensity. Examples of pain scales are:
Education
- Education is an essential component of play and distraction techniques in the nursing care of hospitalized children. It involves providing information and instructions about play and distraction techniques to the child and family. It also involves encouraging participation and feedback from the child and family. Some of the principles and guidelines of education are:
- Assess the child’s and family’s learning needs, readiness, and preferences. Use developmentally appropriate, culturally sensitive, and evidence-based methods and materials.
- Explain the purpose, benefits, and outcomes of play and distraction techniques. Provide examples of play and distraction techniques that are suitable for the child’s age, stage, and condition.
- Demonstrate how to use play and distraction techniques effectively. Allow the child and family to practice play and distraction techniques under supervision. Provide positive reinforcement and constructive feedback.
- Evaluate the child’s and family’s understanding and satisfaction with play and distraction techniques. Address any questions or concerns. Modify the education plan as needed.
- Document the education process and outcomes. Communicate with other healthcare professionals and agencies as needed.
Coping strategies
Factors that influence the coping process and responses
- The coping process and responses of hospitalized children are influenced by various factors, such as:
- Developmental stage: the child’s age and level of cognitive, emotional, and social development. It affects the child’s understanding of the hospitalization, the stressors they face, and the coping strategies they use. For example, younger children may have more difficulty in comprehending the reasons and procedures of hospitalization, may perceive more threats and fears, and may use more behavioral or emotional coping strategies, such as crying, clinging, or regressing. Older children may have more ability to understand and communicate their needs and feelings, may face more challenges in maintaining their identity and routine, and may use more cognitive or problem-solving coping strategies, such as seeking information, planning, or negotiating.
- Personality: the child’s temperament, traits, and characteristics. It affects the child’s perception of the hospitalization, the stressors they encounter, and the coping strategies they prefer. For example, some children may be more optimistic, resilient, or adaptable, and may cope better with hospitalization. Some children may be more pessimistic, anxious, or rigid, and may cope worse with hospitalization.
- Family: the child’s primary source of support, attachment, and guidance. It affects the child’s emotional state, the stressors they experience, and the coping strategies they learn. For example, some families may be more supportive, involved, or consistent, and may help the child to cope better with hospitalization. Some families may be less supportive, distant, or inconsistent, and may hinder the child to cope worse with hospitalization.
- Culture: the child’s background, beliefs, values, and practices. It affects the child’s expectations of the hospitalization, the stressors they face, and the coping strategies they use. For example, some cultures may have more positive or respectful attitudes toward healthcare providers and institutions and may facilitate the child to cope better with hospitalization. Some cultures may have more negative or distrustful attitudes toward healthcare providers and institutions and may impede the child to cope worse with hospitalization.
- Environment: the physical and social surroundings of the child in the hospital. It affects the child’s comfort level, the stressors they encounter, and the coping strategies they access. For example, some environments may be more child-friendly, stimulating, or familiar, and may enhance the child to cope better with hospitalization. Some environments may be less child-friendly, boring, or strange, and may diminish the child to cope worse with hospitalization.
Types and examples of coping strategies
- Coping strategies are the methods or techniques that the child uses to manage or adapt to stressors or challenges. They can be classified into two main types: problem-focused and emotion-focused.
- Problem-focused coping strategies are those that aim to change or solve the problem that causes stress. They involve using cognitive or behavioral skills to deal with the situation. Examples of problem-focused coping strategies are:
- Seeking information: the child asks questions, reads books, watches videos, or searches online to learn more about the hospitalization, the procedures, or the condition.
- Planning: the child sets goals, makes plans, or prepares for the hospitalization, the procedures, or the condition.
- Negotiating: the child expresses opinions, preferences, or needs to the health care providers, parents, or peers. The child tries to reach an agreement or compromise with them.
- Problem-solving: the child identifies the problem, generates possible solutions, evaluates the pros and cons of each solution, chooses the best solution, and implements it.
- Emotion-focused coping strategies are those that aim to regulate or reduce the emotional distress caused by the problem. They involve using psychological or physiological skills to cope with the feelings. Examples of emotion-focused coping strategies are:
- Relaxation: the child uses breathing exercises, progressive muscle relaxation, guided imagery, meditation, or yoga to calm down, relax, or reduce tension.
- Positive self-talk: the child uses affirmations, statements, or thoughts that are positive, encouraging, or optimistic to boost confidence, motivation, or hope.
- Emotional expression: the child uses art, music, drama, writing, or talking to express feelings, thoughts, or experiences related to the hospitalization, the procedures, or the condition.
- Social support: the child seeks comfort, advice, or help from parents, siblings, friends, health care providers, or other supportive people. The child also gives support to others who are in similar situations.
- Problem-focused coping strategies are those that aim to change or solve the problem that causes stress. They involve using cognitive or behavioral skills to deal with the situation. Examples of problem-focused coping strategies are:
Principles and guidelines of coping assessment and intervention
- Coping assessment and intervention are the processes of evaluating and enhancing the child’s coping skills and responses. They should be based on the following principles and guidelines in nursing care of hospitalized children:
- Individualized: coping assessment and intervention should be tailored to the child’s unique characteristics, needs, and preferences. They should consider the child’s developmental stage, personality, family, culture, and environment. They should involve the child in the assessment and intervention process.
- Holistic: coping assessment and intervention should address the child’s physical, psychological, social, and spiritual aspects of coping. They should consider the child’s strengths and weaknesses, resources and barriers, goals and expectations, beliefs and values. They should use a multidisciplinary approach to coping assessment and intervention.
- Evidence-based: coping assessment and intervention should be based on the best available scientific evidence and clinical expertise. They should follow the standards and guidelines of professional organizations and agencies. They should use valid and reliable tools and methods to assess and intervene in the child’s coping skills and responses.
- Collaborative: coping assessment and intervention should involve collaboration with the child, family, health care team, and community. They should foster communication, coordination, and cooperation among all stakeholders. They should seek feedback and input from the child and family. They should refer to other resources or services as needed.
Effectiveness and outcomes of coping strategies
- The effectiveness and outcomes of coping strategies can be evaluated by using various tools and methods to measure the physical, psychological, social, and spiritual outcomes of coping strategies. Some of the tools and methods are:
- Physiological measures: tools that measure the child’s physiological responses to stress or coping, such as heart rate, blood pressure, respiratory rate, oxygen saturation, cortisol level, etc.
- Psychological measures: tools that measure the child’s psychological states or traits related to stress or coping, such as mood, affect, self-esteem, self-efficacy, resilience, etc.
- Behavioral measures: tools that measure the child’s behavioral actions or reactions related to stress or coping, such as compliance, cooperation, participation, aggression, withdrawal, etc.
- Spiritual measures: tools that measure the child’s spiritual beliefs or practices related to stress or coping, such as faith, hope, meaning, purpose, prayer, meditation, etc.
Education
- Education is an essential component of coping strategies in nursing care of hospitalized children. It involves providing information and instructions about coping strategies to the child and family. It also involves encouraging participation and feedback from the child and family. Some of the principles and guidelines of education are:
- Assess the child’s and family’s learning needs, readiness, and preferences. Use developmentally appropriate, culturally sensitive, and evidence-based methods and materials.
- Explain the purpose, benefits, and outcomes of coping strategies. Provide examples of coping strategies that are suitable for the child’s age, stage, condition, and preference.
- Demonstrate how to use coping strategies effectively. Allow the child and family to practice coping strategies under supervision. Provide positive reinforcement and constructive feedback.
- Evaluate the child’s and family’s understanding and satisfaction with coping strategies. Address any questions or concerns. Modify the education plan as needed.
- Document the education process and outcomes. Communicate with other healthcare professionals and agencies as needed.
Conclusion
- The admission and discharge procedures for pediatric patients in hospitals are important aspects of nursing care that require specialized knowledge, skills, and attitudes.
- The nurse should provide family-centered care and promote the child’s well-being during hospitalization by addressing their developmental, emotional, and psychosocial needs.
- The nurse should also apply the nursing process and evidence-based practice to plan, implement, and evaluate care for hospitalized children by using appropriate techniques, devices, and interventions.
- Infection control is a vital aspect of nursing care for hospitalized children.
- It involves understanding the concepts of infection, colonization, and communicable disease; the chain of infection and the modes of transmission; the risk factors and sources of infection; and the standard and transmission-based precautions.
- It also involves applying the nursing process in assessing, diagnosing, planning, implementing, and evaluating the care of children with infectious or communicable diseases.
- By following these principles and techniques, nurses can prevent and reduce the spread of infections, protect themselves and others from exposure, and promote optimal health outcomes for children.
- Safety is a vital aspect of nursing care for hospitalized children.
- It involves identifying the common hazards and risks for injury or harm in hospitalized children, such as falls, medication errors, infection, equipment-related injuries, procedure-related injuries, and physical restraint injuries.
- It also involves applying strategies and interventions to prevent or minimize the potential for injury or harm in hospitalized children, such as fall prevention, medication administration, infection control, equipment safety, procedure safety, and restraint safety.
- By following these principles and techniques, nurses can prevent and reduce errors and adverse events, protect themselves and others from exposure, and promote optimal health outcomes for children.
Summary
- Infection is the invasion of body tissue by microorganisms with the potential to cause illness or disease.
- Colonization is the presence of microorganisms on or in a host without causing signs or symptoms of infection.
- Communicable disease is an infectious disease that can be transmitted from one person to another through direct or indirect contact.
- The chain of infection consists of six links: infectious agent, reservoir, portal of exit, mode of transmission, portal of entry, and susceptible host.
- The modes of transmission are contact (direct or indirect), droplet, airborne, and vector-borne.
- The risk factors for infection in hospitalized children include age, immunization status, chronic conditions, medications, invasive devices, etc.
- The sources of infection in hospitalized children include other infected patients or health care workers, contaminated medical devices or equipment, environmental surfaces or objects, visitors or family members, animals or insects, food or water.
- Standard precautions are the basic level of infection control that should be used for all patients regardless of their diagnosis or presumed infection status. They include hand hygiene, PPE, respiratory hygiene/cough etiquette, patient placement, environmental cleaning, waste disposal, linen handling, patient care equipment, and patient education.
- Transmission-based precautions are additional infection control measures that should be used for patients with known or suspected infections that are transmitted by contact (gloves and gowns), droplet (mask), or airborne (respirator) routes. They include patient isolation or cohorting.
- The nursing process is a systematic method of providing individualized care to patients based on their needs and responses. It consists of five steps: assessment (collecting data), diagnosis (identifying problems), planning (setting goals and interventions), implementation (carrying out interventions), and evaluation (measuring effectiveness).
- Safety is the prevention of errors and adverse events that may cause injury or harm to patients, staff, or visitors in healthcare settings.
- Hospitalized children are more vulnerable to hazards and risks due to their developmental stage, cognitive level, physical size, curiosity, and dependence on others.
- The common hazards and risks for injury or harm in hospitalized children are falls, medication errors, infection, equipment-related injuries, procedure-related injuries, and physical restraint injuries.
- The strategies and interventions to prevent or minimize the potential for injury or harm in hospitalized children are assessment, planning, implementation, evaluation, and education.
- The implementation of safety measures includes fall prevention, medication administration, infection control, equipment safety, procedure safety, and restraint safety.
- The evaluation of safety measures includes measuring the effectiveness and outcomes of safety measures, comparing the actual outcomes with the expected outcomes, evaluating the child’s progress toward the goals and modifying the plan of care as needed, evaluating the child’s satisfaction with the care and identifying areas for improvement, evaluating the quality and safety of safety measures and reporting any errors or adverse events.
- The education of safety measures includes educating the child and family about safety issues and prevention measures, providing information and instructions about safety measures, encouraging participation and feedback from the child and family, reinforcing positive behaviors and correcting unsafe behaviors, and providing resources and referrals for safety measures.
- Play is an essential part of childhood that supports the development of physical, cognitive, social, and emotional skills. It is also a way of expressing feelings, coping with stress, and having fun.
- Distraction is a psychological strategy that involves shifting the child’s attention from a painful or stressful stimulus to a more pleasant or engaging one. It is based on the idea that pain and anxiety are influenced by cognitive and emotional factors.
- Play and distraction techniques are important in the nursing care of hospitalized children because they can help reduce pain, anxiety, fear, boredom, and loneliness. They can also promote coping, adaptation, healing, and well-being.
- The types of play and distraction techniques for hospitalized children are therapeutic (e.g., medical play), recreational (e.g., games), developmental (e.g., sensorimotor play), and multimodal (e.g., video games).
- The principles and guidelines of play and distraction techniques in nursing care of hospitalized children are child-centered, developmentally appropriate, culturally sensitive, evidence-based, and collaborative.
- The effectiveness and satisfaction of play and distraction techniques can be evaluated by using various tools and methods to measure the physical, psychological, and behavioral outcomes of play and distraction techniques, such as pain scales, anxiety scales, and satisfaction surveys.
- The education of play and distraction techniques involves providing information and instructions about play and distraction techniques to the child and family. It also involves encouraging participation and feedback from the child and family.
- Coping is the process of managing or adapting to stressors or challenges that threaten one’s well-being or functioning.
- Coping is important in the nursing care of hospitalized children because it can help to reduce the negative effects of hospitalization (e.g., pain) and promote positive outcomes of hospitalization (e.g., resilience).
- The factors that influence the coping process and responses are developmental stage (e.g., age), personality (e.g., temperament), family (e.g., support), culture (e.g., beliefs), environment (e.g., surroundings).
- The types of coping strategies are problem-focused (e.g., seeking information) and emotion-focused (e.g., relaxation).
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Nursing Care of Hospitalized Children
This filled cannot be empty

