Please set your exam date
Antibiotics and Antimicrobial Agents
Study Questions
Introduction
A nurse is reviewing the mechanism of action of different antibiotic groups.
The nurse understands that which of the following antibiotics bind to the 30S ribosomal subunit of bacteria and interfere with protein synthesis?
Explanation
Amikacin (Amikin) is an aminoglycoside antibiotic that binds to the30S ribosomal subunitof bacteria and interferes with protein synthesis by causingmRNA misreadingandinhibiting 30S subunit assembly.
Choice A is wrong because cefazolin (Zolicef) is a cephalosporin antibiotic that binds to thepenicillin-binding proteinsof bacteria and interferes with cell wall synthesis by inhibitingpeptidoglycan cross-linking.
Choice C is wrong because ciprofloxacin (Cipro) is a fluoroquinolone antibiotic that binds to theDNA gyraseandtopoisomerase IVof bacteria and interferes with DNA replication by inhibitingDNA supercoiling.
Choice D is wrong because penicillin G (Pfizerpen) is a beta-lactam antibiotic that binds to thepenicillin-binding proteinsof bacteria and interferes with cell wall synthesis by inhibitingpeptidoglycan cross-linking.
Normal ranges for 30S ribosomal subunit are not applicable as it is a bacterial structure.
Normal ranges for antibiotics depend on the type, dose, route, frequency and duration of administration as well as the patient’s age, weight, renal function and infection site and severity.
A nurse is caring for a client who has a urinary tract infection caused by Escherichia coli. The provider has ordered sulfamethoxazole-trimethoprim (Bactrim) for the client. Which of the following actions should the nurse take? (Select all that apply).
Explanation
The nurse should instruct the client to drink plenty of fluids and advise the client to avoid sunlight exposure when taking sulfamethoxazole-trimethoprim (Bactrim).Drinking fluids can help prevent crystalluria and kidney damage caused by the medication.Avoiding sunlight exposure can prevent photosensitivity reactions that can cause skin rash, itching, or burning.
Choice A is wrong because sulfamethoxazole-trimethoprim does not affect blood glucose levels.This is a possible side effect of some other antibiotics, such as fluoroquinolones.
Choice D is wrong because sulfamethoxazole-trimethoprim can be taken with or without food.Taking it with food may help reduce nausea or stomach upset, but it is not necessary.
Choice E is wrong because sulfamethoxazole-trimethoprim does not affect platelet count.This is a possible side effect of some other antibiotics, such as penicillins or cephalosporins.
A nurse is administering imipenem-cilastatin (Primaxin) to a client who has a severe infection. The client asks the nurse why this medication is given in combination. The nurse should respond with which of the following statements?
Explanation
T
he combination of imipenem and cilastatin prevents the degradation of imipenem by renal enzymes.Imipenem is a carbapenem antibiotic that works by interfering with the bacteria’s cell wall.Cilastatin is a dehydropeptidase inhibitor that inhibits the metabolism of imipenem by renal brush-border enzymes, thus increasing imipenem concentrations in urine.
Choice A is wrong because the combination does not enhance the antimicrobial activity of imipenem, but rather preserves its activity by preventing its breakdown.
Choice B is wrong because the combination does not reduce the risk of allergic reactions to imipenem, but rather increases the risk of side effects such as diarrhea, rash, fever, and seizures.
Choice D is wrong because the combination does not lower the dosage requirement of imipenem, but rather allows for higher dosages to be administered depending on the organism sensitivity and the severity of infection.
A nurse is teaching a client who has a sinus infection about amoxicillin (Amoxil). Which of the following statements by the client indicates an understanding of the teaching?
Explanation
This statement indicates that the client understands that amoxicillin can reduce the effectiveness of oral contraceptives and increase the risk of unintended pregnancy.
Choice A is wrong because a rash can indicate an allergic reaction to amoxicillin, which can be life-threatening.The client should stop taking the medication and seek medical attention if a rash develops.
Choice B is wrong because the client should complete the full course of amoxicillin as prescribed, even if they feel better.Stopping the medication too soon can lead to bacterial resistance and recurrence of infection.
Choice D is wrong because amoxicillin does not cause stomach upset and does not need to be taken with an antacid.In fact, some antacids can interfere with the absorption of amoxicillin and reduce its effectiveness.
A nurse is caring for a client who has endocarditis and is receiving gentamicin (Garamycin) intravenously. Which of the following laboratory tests should the nurse monitor to assess for adverse effects of this medication?
Explanation
The nurse should monitor the serum creatinine level of the client who is receiving gentamicin because this medication can cause nephrotoxicity, which is damage to the kidneys.Serum creatinine is a marker of kidney function and it should be within the normal range of 0.6 to 1.2 mg/dL for adults.
If the serum creatinine level increases, it indicates that the kidneys are not filtering the waste products properly and the dose of gentamicin may need to be adjusted or discontinued.
Choice B. Serum potassium is wrong because gentamicin does not affect the potassium level in the blood.Potassium is an electrolyte that regulates the nerve and muscle function and it should be within the normal range of 3.5 to 5.0 mEq/L for adults.Abnormal potassium levels can be caused by other factors such as dehydration, kidney disease, diuretics, or acid-base imbalance.
Choice C. Serum albumin is wrong because gentamicin does not affect the albumin level in the blood.Albumin is a protein that helps maintain fluid balance and transport substances in the blood and it should be within the normal range of 3.5 to 5.0 g/dL for adults.Low albumin levels can be caused by other factors such as malnutrition, liver disease, inflammation, or blood loss.
Choice D. Serum bilirubin is wrong because gentamicin does not affect the bilirubin level in the blood.Bilirubin is a waste product of red blood cell breakdown and it should be within the normal range of 0.1 to 1.2 mg/dL for adults.
High bilirubin levels can be caused by other factors such as hemolysis, liver
Antimicrobial classifications
A nurse is caring for a client who has a viral infection. Which of the following antiviral groups inhibits viral DNA polymerase or reverse transcriptase enzymes that are essential for viral DNA or RNA synthesis?
Explanation
This is because nucleoside analogs inhibit viral DNA polymerase or reverse transcriptase enzymes that are essential for viral DNA or RNA synthesis.
Some possible explanations for the other choices are:
Choice B is wrong becauseNon-nucleoside reverse transcriptase inhibitors (NNRTIs) are wrong because they do not inhibit viral DNA polymerase, but rather bind directly to reverse transcriptase and block its activity.
Choice C is wrong becauseNucleotide reverse transcriptase inhibitors (NRTIs) are wrong because they are not nucleosides, but nucleotides that need to be phosphorylated before they can inhibit reverse transcriptase.
Choice D is wrong becauseProtease inhibitors (PIs) are wrong because they do not inhibit viral DNA polymerase or reverse transcriptase, but rather block the protease enzyme that cleaves viral proteins into functional units.
A nurse is caring for a client who has a viral infection. Which of the following antiviral groups bind to and inhibit viral reverse transcriptase enzyme that is essential for viral RNA synthesis? (Select all that apply)
Explanation
These are examples ofnon-nucleoside reverse transcriptase inhibitors (NNRTIs), which bind to and inhibit viral reverse transcriptase enzyme that is essential for viral RNA synthesis.NNRTIs block reverse transcriptase by binding directly to the enzyme and prevent the completion of DNA synthesis.
Choice D is wrong because rilpivirine (Edurant) is also an NNRTI, but it does not bind to the same site as efavirenz, nevirapine and etravirine.
Therefore, it is not part of the same antiviral group.
Choice E is wrong because nucleotide reverse transcriptase inhibitors (NRTIs) are different from NNRTIs.
NRTIs are analogues of the natural deoxynucleotides that compete with them for incorporation into the viral DNA chain.However, NRTIs lack a 3′-hydroxyl group on the deoxyribose moiety, which results in chain termination.
NRTIs do not bind to reverse transcriptase enzyme directly like NNRTIs do.
A nurse is caring for a client who has a viral infection. The client asks the nurse how nucleoside analogs work to treat viral infections. Which of the following statements by the nurse is correct?
Explanation
Nucleoside analogs are antiviral agents that resemble natural nucleosides and act by causing termination of the nascent DNA chain.They are used to treat various viral infections such as HIV, HBV, HCV, CMV, HSV and VZV.
Choice A is wrong because it describes the mechanism of action of non-nucleoside reverse transcriptase inhibitors (NNRTIs), which are another class of antiviral drugs that bind to and inhibit viral reverse transcriptase enzyme.
Choice B is wrong because it describes the mechanism of action of protease inhibitors (PIs), which are another class of antiviral drugs that inhibit viral protease enzyme that is essential for viral protein maturation and assembly.
Choice D is wrong because it describes the mechanism of action of fusion inhibitors (FIs), which are another class of antiviral drugs that prevent viral fusion with host cell membrane.
A nurse is caring for a client who has a viral infection and is taking an antiviral medication that inhibits the integrase enzyme that is essential for viral DNA integration into host cell genome. Which of the following antiviral groups does this medication belong to?
Explanation
Integrase strand transfer inhibitors (INSTIs) are a class of antiviral drugs that block the action of integrase, a viral enzyme that inserts the viral genome into the DNA of the host cell. This prevents the virus from replicating and infecting new cells.
Choice A is wrong because nucleotide reverse transcriptase inhibitors (NRTIs) are a class of antiviral drugs that block the action of reverse transcriptase, a viral enzyme that converts the viral RNA into DNA.
Choice B is wrong because non-nucleoside reverse transcriptase inhibitors (NNRTIs) are a class of antiviral drugs that also block the action of reverse transcriptase, but in a different way than NRTIs.They bind to a different site on the enzyme and cause it to change shape.
Choice D is wrong because protease inhibitors (PIs) are a class of antiviral drugs that block the action of protease, a viral enzyme that cleaves the viral polyprotein into functional units.This prevents the virus from assembling and maturing.
A nurse is caring for a client who has a fungal infection and is prescribed amphotericin. What adverse effects should the nurse monitor for in this client?
Explanation
Amphotericin B is a drug used to treat fungal infections, but it can cause kidney damage and electrolyte imbalance as a common side effect. The nurse should monitor the client’s urine output, creatinine, potassium, and magnesium levels.
Choice B is wrong because Ototoxicity is wrong because amphotericin B does not affect the ears or hearing.
Ototoxicity is more common with aminoglycosides, another class of antibiotics.
Choice C is wrong because Hepatotoxicity is wrong because amphotericin B does not cause liver damage.
Hepatotoxicity is more common with azoles, another class of antifungals.
Choice D is wrong because Thrombocytopenia is wrong because amphotericin B does not cause low platelet count.
Thrombocytopenia is more common with heparin, an anticoagulant drug.
A nurse is teaching a client who has a vaginal candidiasis infection about the use of miconazole cream. Which of the following instructions should the nurse include? (Select all that apply.).
Explanation
The nurse should instruct the client to avoid sexual intercourse until the infection is cleared, as it can cause irritation and inflammation of the vaginal mucosa and potentially transmit the infection to the partner.The nurse should also instruct the client to use a backup method of contraception if using oral contraceptives, as miconazole cream can reduce the effectiveness of hormonal contraceptives.
Choice A is wrong because the client should apply the cream twice a day for 7 days, not once a day.
Choice B is wrong because the client should not wash the applicator with soap and water after each use, as it can alter the pH of the vagina and promote fungal growth.
Choice E is wrong because bleeding or bruising are not common side effects of miconazole cream and are not related to vaginal candidiasis infection.
A nurse is reviewing the medication history of a client who has a fungal infection and is prescribed caspofungin. The nurse should identify that which of the following medications can interact with caspofungin?
Explanation
Cyclosporine can interact with caspofungin and increase its plasma concentration and risk of liver toxicity.Cyclosporine is a drug used to prevent organ rejection or suppress the immune system.
Choice B is wrong because warfarin does not have a significant interaction with caspofungin.Warfarin is a blood thinner that prevents blood clots.
Choice C is wrong because metformin does not have a significant interaction with caspofungin.Metformin is a drug used to lower blood sugar levels in diabetes.
Choice D is wrong because digoxin does not have a significant interaction with caspofungin.Digoxin is a drug used to treat heart failure and irregular heartbeat.
Caspofungin is an antifungal drug that belongs to the echinocandin class.It works by inhibiting the synthesis of a component of the fungal cell wall called beta-glucan.
It is used to treat various fungal infections such as candidemia, esophageal candidiasis, invasive aspergillosis, and febrile neutropenia
A nurse is educating a client who has tinea pedis about the use of terbinafine cream. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
This statement indicates that the client understands the proper use of terbinafine cream for tinea pedis, which is a fungal infection of the feet.Terbinafine cream is an antifungal agent that works by killing the fungus or preventing its growth.According to a study, terbinafine 1% cream applied once daily for 7 days is effective in treating interdigital tinea pedis, but some sources recommend applying it twice daily for 2 weeks.
Choice B is wrong because washing the feet with soap and water before applying the cream is not necessary and may cause irritation or dryness of the skin.
Choice C is wrong because covering the affected area with a bandage after applying the cream is not advised and may create a moist environment that favors fungal growth.
Choice D is wrong because itching or burning are common side effects of terbinafine cream and do not indicate an allergic reaction or a need to stop using the cream.However, if the symptoms are severe or persist, the client should contact their health care provider.
A nurse is caring for a client who has malaria and is prescribed chloroquine. What is the mechanism of action of this drug?
Explanation
Chloroquine inhibits heme polymerization in the parasite, which causes the accumulation of toxic heme and kills the parasite.
Choice B is wrong because chloroquine does not disrupt mitochondrial function in the parasite.
Choice C is wrong because chloroquine does not interfere with DNA synthesis in the parasite.
Choice D is wrong because chloroquine does not block calcium influx in the parasite.
Heme polymerization is the process of converting heme, a toxic byproduct of hemoglobin digestion, into hemozoin, a nontoxic pigment that can be stored by the parasite.Chloroquine forms a complex with heme and prevents it from polymerizing, thus disrupting the parasite’s metabolism and survival.
A nurse is administering albendazole to a client who has a tapeworm infection. The client asks how the drug works. Which of the following responses should the nurse give?
Explanation
Albendazole prevents the worm from absorbing glucose, which is its main source of energy.This leads to the worm’s death
Choice B is wrong because albendazole does not paralyze the worm’s muscles.It inhibits the formation of microtubules, which are important for cell division and movement
Choice C is wrong because albendazole does not dissolve the worm’s cuticle.
The cuticle is a protective layer that covers the worm’s body.Albendazole affects the internal cells of the worm, not the external ones
Choice D is wrong because albendazole does not stimulate the worm’s nervous system.It has the opposite effect of blocking the transmission of nerve impulses by interfering with tubulin, a protein that forms part of the nerve cells
A nurse is reviewing the medication history of a client who is prescribed atovaquone-proguanil for malaria prophylaxis.
Which of the following medications should the nurse identify as a potential interaction with atovaquone-proguanil?
Explanation
Rifampin is a drug that can interact with atovaquone-proguanil and reduce its effectiveness in preventing or treating malaria.Rifampin can lower the blood levels of atovaquone and proguanil by increasing their metabolism in the liver. Therefore, rifampin should be avoided or used with caution when taking atovaquone-proguanil.
Choice A is wrong because warfarin is not a known interaction with atovaquone-proguanil.
Warfarin is a blood thinner that can interact with many other drugs, but atovaquone-proguanil is not one of them.
Choice B is wrong because metformin is not a known interaction with atovaquone-proguanil.
Metformin is a drug that lowers blood sugar levels in people with diabetes.
It does not affect the metabolism or efficacy of atovaquone-proguanil.
Choice C is wrong because omeprazole is not a known interaction with atovaquone-proguanil.
Omeprazole is a drug that reduces stomach acid production and treats ulcers and reflux.
It does not interfere with the absorption or action of atovaquone-proguanil.
Mechanisms of action
A nurse is reviewing the mechanisms of action of different antimicrobial agents. The nurse understands that antibiotics that inhibit cell wall synthesis are most effective against which type of bacteria?
Explanation
This is because antibiotics that inhibit cell wall synthesis are most effective against bacteria that have a thick peptidoglycan layer in their cell wall, which is characteristic of gram-positive bacteria.Peptidoglycan is a polymer of glycan and peptides that gives the cell wall its strength and rigidity.Antibiotics that inhibit cell wall synthesis, such as β-lactams and glycopeptides, prevent the formation or cross-linking of the peptidoglycan layer, resulting in cell wall defects and bacterial lysis.
Choice B is wrong becauseGram-negative bacteria is wrong because gram-negative bacteria have a thin peptidoglycan layer and an outer membrane that protects them from antibiotics that target cell wall synthesis.Some gram-negative bacteria also have efflux pumps or β-lactamases that can expel or degrade these antibiotics.
Choice C is wrong becauseAnaerobic bacteria is wrong because anaerobic bacteria can be either gram-positive or gram-negative, and their susceptibility to antibiotics that inhibit cell wall synthesis depends on their cell wall structure and resistance mechanisms.
Choice D is wrong becauseAtypical bacteria is wrong because atypical bacteria are bacteria that lack a cell wall, such as Mycoplasma and Chlamydia.These bacteria are naturally resistant to antibiotics that inhibit cell wall synthesis, as they do not have a peptidoglycan layer to target.
A nurse is caring for a client who has a severe infection and is receiving a combination of antibiotics. The nurse knows that some antibiotics have synergistic effects when used together. Which of the following are examples of antibiotic combinations that have synergistic effects? (Select all that apply.)
Explanation
These are examples of antibiotic combinations that have synergistic effects, meaning they enhance each other’s bacterial killing when used together.
Choice A is correct because ampicillin and gentamicin are synergistic against enterococcal infections.
Ampicillin inhibits the cell wall synthesis of enterococci, while gentamicin damages their ribosomes and interferes with protein synthesis.
Choice B is correct because trimethoprim and sulfamethoxazole are synergistic against many gram-negative and gram-positive bacteria.
Trimethoprim inhibits the enzyme dihydrofolate reductase, while sulfamethoxazole inhibits the enzyme dihydropteroate synthase.
Both enzymes are involved in the synthesis of folic acid, which is essential for bacterial DNA replication.
Choice C is wrong because clindamycin and erythromycin are antagonistic, meaning they interfere with each other’s activity when used together.
Both antibiotics bind to the same site on the bacterial ribosome and block protein synthesis, but clindamycin has a higher affinity and displaces erythromycin.
Choice D is wrong because metronidazole and ciprofloxacin are not synergistic, but additive, meaning they have independent effects when used together.
Metronidazole damages the bacterial DNA by generating reactive oxygen species, while ciprofloxacin inhibits the enzyme DNA gyrase that unwinds the DNA for replication.
Choice E is wrong because vancomycin and rifampin are not synergistic, but indifferent, meaning they have no effect on each other’s activity when used together.
Vancomycin inhibits the cell wall synthesis of gram-positive bacteria by binding to the peptidoglycan precursors, while rifampin inhibits the bacterial RNA polymerase that transcribes DNA into RNA.
A nurse is teaching a client who has a urinary tract infection about the prescribed antibiotic, ciprofloxacin. The nurse instructs the client to avoid taking the medication with dairy products.
The client asks, “Why do I have to avoid dairy products?” What is the best response by the nurse?
Explanation
This means that less of the drug will get into your bloodstream and it may not work as well to treat your infection.According to one source, dairy products can reduce the bioavailability of ciprofloxacin by 30 to 36 percent and the peak concentration by 36 percent.
Choice A is wrong because dairy products do not increase the risk of kidney stones with this medication.
There is no evidence to support this claim.
Choice C is wrong because dairy products do not cause allergic reactions with this medication.
Allergic reactions are possible with any medication, but they are not related to dairy products.
Choice D is wrong because dairy products do not interfere with the metabolism of this medication in your liver.
Ciprofloxacin is mainly eliminated by the kidneys, not the liver.
To avoid this interaction, you should take ciprofloxacin at least 2 hours before or 6 hours after dairy products.
A nurse is monitoring a client who is receiving antiviral therapy for influenza.
The nurse expects that the antiviral drug will have which of the following effects?
Explanation
Antiviral drugs for influenza can reduce the duration and severity of symptoms by inhibiting the replication of the virus in the body.They are most effective when started within 48 hours of illness onset.
Choice A is wrong because antiviral drugs do not kill the influenza virus, but only prevent it from multiplying.
Choice C is wrong because antiviral drugs do not prevent the transmission of the virus to others, but only reduce the amount of virus shed by infected persons.People who take antiviral drugs should still practice good hygiene and avoid close contact with others.
Choice D is wrong because antiviral drugs do not stimulate the immune system to fight off the virus, but only interfere with the viral enzymes that are essential for viral replication.Antiviral drugs are not a substitute for vaccination, which can induce protective immunity against influenza.
A nurse is administering an antifungal medication to a client who has a systemic fungal infection.
The nurse understands that antifungal drugs have a higher risk of toxicity than antibacterial drugs because:
Explanation
This means that antifungal drugs have to target specific components of the fungal cell that are different from the human cell, such as the cell membrane or the cell wall.However, this also increases the risk of toxicity to human cells, especially those that have high turnover rates, such as liver and kidney cells.
Choice A is wrong because fungi do not have cell walls that are difficult to penetrate.Fungi have cell walls that are composed of chitin, glucan, and mannoproteins, which are different from the peptidoglycan cell walls of bacteria.
Antifungal drugs can target these components and disrupt the integrity of the fungal cell wall.
Choice B is wrong because fungi are not more resistant to drug therapy than bacteria.Fungi can develop resistance to antifungal drugs, but this is not a common mechanism of antifungal drug failure.Bacteria can also develop resistance to antibacterial drugs through various mechanisms, such as producing enzymes that degrade or modify the drugs, altering the target sites of the drugs, or pumping out the drugs from the cell.
Choice D is wrong because fungi do not mutate rapidly and develop drug resistance.
Fungi have a slower rate of mutation than bacteria because they have a more complex genome and a more efficient DNA repair system
Spectrum of activity
A nurse is reviewing the medication history of a client who has a urinary tract infection caused by Escherichia coli.
Which of the following antimicrobial agents should the nurse expect the provider to prescribe for this client?
Explanation
Amoxicillin-clavulanate is an antibiotic that belongs to the penicillin group and is effective against Escherichia coli, the most common cause of urinary tract infections (UTIs).It works by inhibiting the bacterial cell wall synthesis and preventing the bacteria from producing an enzyme that makes them resistant to penicillin.
Choice B is wrong becauseVancomycin is wrong because it is an antibiotic that is used to treat serious infections caused by gram-positive bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA).It is not effective against gram-negative bacteria, such as Escherichia coli.
Choice C is wrong becausePenicillin G is wrong because it is an antibiotic that is effective against some gram-positive bacteria, such as Streptococcus and Neisseria.However, many strains of Escherichia coli are resistant to penicillin G and can produce an enzyme called beta-lactamase that breaks down the antibiotic.
Choice D is wrong becauseAcyclovir is wrong because it is an antiviral drug that is used to treat infections caused by herpes simplex virus (HSV) and varicella-zoster virus (VZV).It has no activity against bacteria, such as Escherichia coli.
(Select all that apply) A client is receiving ciprofloxacin IV for a severe infection caused by Pseudomonas aeruginosa.
Which of the following laboratory tests should the nurse monitor for adverse effects of this medication?
Explanation
Ciprofloxacin is an antibiotic that can cause various side effects, some of which are serious and may be permanent.
The nurse should monitor the following laboratory tests for adverse effects of this medication:
• Liver function tests: Ciprofloxacin can cause hepatotoxicity, which is damage to the liver cells.Liver function tests can detect abnormal levels of enzymes or bilirubin that indicate liver injury.
• Serum creatinine levels: Ciprofloxacin can cause nephrotoxicity, which is damage to the kidney cells.
Serum creatinine levels can measure how well the kidneys are filtering waste products from the blood.Elevated serum creatinine levels indicate impaired kidney function.
• Complete blood count: Ciprofloxacin can cause hematologic disorders, such as anemia, leukopenia, thrombocytopenia, or pancytopenia.
A complete blood count can evaluate the number and quality of red blood cells, white blood cells, and platelets in the blood.Abnormal blood counts can increase the risk of bleeding, infection, or fatigue.
Choice B is wrong because ciprofloxacin does not affect blood glucose levels directly.
However, ciprofloxacin can interact with some oral antidiabetic drugs and increase the risk of hypoglycemia or hyperglycemia.Therefore, the nurse should monitor the blood glucose levels of diabetic patients who are taking ciprofloxacin and other antidiabetic drugs.
Choice E is wrong because ciprofloxacin does not affect thyroid function tests directly.
However, ciprofloxacin can interact with some thyroid hormone replacement drugs and decrease their absorption or efficacy.Therefore, the nurse should monitor the thyroid function tests of patients who are taking ciprofloxacin and thyroid hormone replacement drugs.
A nurse is teaching a client who has a fungal infection about fluconazole.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
This is because alcohol can increase the risk of liver damage and other side effects from fluconazole.Fluconazole is an antifungal medicine that is used to treat infections caused by fungus, such as yeast infections.
Choice A is wrong because fluconazole can be taken with or without food.
Food does not affect the absorption of the medicine.
Choice C is wrong because fluconazole can reduce the effectiveness of hormonal contraceptives, such as birth control pills, patches, rings, or injections.Therefore, a barrier method of contraception, such as condoms or diaphragms, should be used in addition to the hormonal method while taking fluconazole and for at least 1 week after the last dose.
Choice D is wrong because a rash can be a sign of a serious allergic reaction to fluconazole.
If a rash develops, the medication should not be stopped without consulting a doctor.Other symptoms of an allergic reaction include hives, itching, swelling, difficulty breathing, or fever.
A client is diagnosed with influenza A and is prescribed oseltamivir.
Which of the following statements by the client indicates a need for further education?
Explanation
This statement indicates a need for further education because oseltamivir does not prevent the transmission of influenza virus to others.Oseltamivir is an antiviral drug that can shorten the duration of symptoms, reduce the risk of complications, and work best if started within 48 hours of symptom onset. However, it does not eliminate the virus from the body or provide immunity against future infections.Therefore, the client should still practice good hygiene and avoid contact with others who are at high risk of influenza complications.
Choice A is wrong because oseltamivir can shorten the duration of symptoms by about one day if taken within 48 hours of symptom onset.
Choice C is wrong because oseltamivir works best if started within 48 hours of symptom onset, as it inhibits the viral replication and reduces the viral load.
Choice D is wrong because oseltamivir may cause nausea and vomiting as side effects in some people, especially if taken without food.These side effects are usually mild and transient and can be minimized by taking the medication with food or milk.
A nurse is caring for a client who has meningitis caused by Streptococcus pneumoniae. The provider orders penicillin G IV for this client.
Before administering the medication, which of the following actions should the nurse take?
Explanation
This is because penicillin G is a beta-lactam antibiotic that can cause severe allergic reactions in some people, such as anaphylaxis, rash, or angioedema. Therefore, the nurse should always check for any history of allergies before administering penicillin G or any other beta-lactam antibiotic.
Choice A is wrong because checking the client’s temperature is not a priority action before giving penicillin G.Although fever is a common sign of meningitis, it does not affect the administration of penicillin
Choice B is wrong because assessing the client’s level of consciousness is not a priority action before giving penicillin G.Although altered mental status is a common sign of meningitis, it does not affect the administration of penicillin
Choice D is wrong because obtaining a blood sample for culture and sensitivity is not a priority action before giving penicillin G.Although culture and sensitivity tests are important to identify the causative organism and the appropriate antibiotic, they should not delay the initiation of empiric therapy for meningitis.Penicillin G is effective against Streptococcus pneumoniae, which is the most common cause of bacterial meningitis in adults.
Commonly prescribed antimicrobial agents
A client with a bacterial skin infection is prescribed cephalexin (Keflex).
The nurse should instruct the client to report which adverse effect of this medication?
Explanation
A rash is a possible adverse effect of cephalexin (Keflex), a type of antibiotic used to treat bacterial skin infections.A rash may indicate an allergic reaction to the medication, which can be serious and require immediate medical attention.
Choice A is wrong because diarrhea is a common side effect of cephalexin that usually does not need medical attention unless it is severe or watery.
Choice B is wrong because headache is not a common or serious side effect of cephalexin.
Choice D is wrong because nausea is a common side effect of cephalexin that usually does not need medical attention unless it is persistent or severe.
A nurse is caring for a client with a bacterial respiratory tract infection who is receiving azithromycin (Zithromax).
Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A is correct because azithromycin can cause liver toxicity and hepatitis, so the nurse should monitor the client’s liver function tests.
Choice B is wrong because azithromycin can be taken with or without food.
Choice C is wrong because azithromycin does not interact with dairy products.
Choice D is correct because azithromycin can increase the risk of sunburn and photosensitivity, so the nurse should advise the client to use sunscreen and avoid excessive sun exposure.
Choice E is correct because azithromycin is a bacteriostatic antibiotic that requires the client to complete the full course of therapy to prevent bacterial resistance and recurrence of infection.
A nurse is teaching a client who has a bacterial urinary tract infection about nitrofurantoin (Macrobid).
Which of the following statements by the client indicates understanding of the teaching?
Explanation
This statement indicates that the client understands that nitrofurantoin (Macrobid) can cause gastrointestinal upset and taking it with food or milk can help reduce this side effect.
Choice B is wrong because drinking at least two liters of water daily is a general measure to prevent urinary tract infections (UTIs), not a specific instruction for nitrofurantoin.
Choice C is wrong because the client should complete the full course of antibiotics even if they feel better, to avoid recurrence or resistance of the infection.
Choice D is wrong because using a straw to drink this medication is not necessary or helpful.
Nitrofurantoin is an oral capsule, not a liquid.Using a straw may be advised for liquid medications that can stain the teeth, such as iron supplements.
A nurse is reviewing the medication history of a client who has a bacterial gastrointestinal infection and a prescription for metronidazole (Flagyl).
The nurse should identify that which of the following medications can interact with metronidazole?
Explanation
Warfarin (Coumadin) can interact with metronidazole (Flagyl) and increase the risk of bleeding.This is because metronidazole may inhibit the enzyme that metabolizes warfarin, leading to higher warfarin levels and enhanced anticoagulant effect.If a patient is taking warfarin and metronidazole, they may need a dose adjustment and frequent monitoring of their INR.They should also watch for any signs of bleeding or bruising and report them to their doctor.
Choice B is wrong because levothyroxine (Synthroid) does not have a significant interaction with metronidazole.
Choice C is wrong because lisinopril (Prinivil) does not have a significant interaction with metronidazole.
Choice D is wrong because omeprazole (Prilosec) does not have a significant interaction with metronidazole.
A nurse is preparing to administer ceftriaxone (Rocephin) to a client who has bacterial meningitis.
The nurse should recognize that this medication is effective against which type of bacteria?
Explanation
Ceftriaxone (Rocephin) is athird-generation cephalosporin antibioticthat works byinterfering with the formation of bacterial cell walls.It is effective againstgram-negative bacteria, such asNeisseria gonorrhoeaeandHaemophilus species, which are common causes of bacterial meningitis.
Choice A is wrong because ceftriaxone is less active againstgram-positive bacteria, such asStaphylococcusandStreptococcusspecies.
Choice C is wrong because ceftriaxone is not effective againstanaerobic bacteria, which are bacteria that do not require oxygen to grow.Anaerobic bacteria are usually treated withmetronidazoleorclindamycin.
Choice D is wrong because ceftriaxone can treat bothaerobicandanaerobicgram-negative bacteria, but not all aerobic bacteria are gram-negative.
Aerobic bacteria are bacteria that require oxygen to grow.Some examples of aerobic gram-positive bacteria areListeria monocytogenesandBacillus anthracis, which are resistant to ceftriaxone.
Indications for use
A nurse is reviewing the culture and sensitivity report of a client with a urinary tract infection. The report shows that the causative microorganism is Escherichia coli and it is sensitive to ciprofloxacin, nitrofurantoin, and trimethoprim-sulfamethoxazole.
Which of these antimicrobial agents is considered a narrow-spectrum drug?
Explanation
Nitrofurantoin is considered a narrow-spectrum drug because it is effective against only a limited range of bacteria, mainly gram-negative bacteria that cause urinary tract infections.
Some additional explanations are:
Choice A is wrong becauseCiprofloxacin is a broad-spectrum drug that can affect a wide range of bacteria, both gram-positive and gram-negative.
Choice C is wrong becauseTrimethoprim-sulfamethoxazole is also a broad-spectrum drug that can inhibit the growth of many types of bacteria, including some gram-positive and gram-negative bacteria.
Choice D is wrong because None of them is incorrect because nitrofurantoin is a narrow-spectrum drug as explained above.
Normal ranges for urinary tract infection microorganisms are:
• Escherichia coli: less than 10^5 CFU/mL
• Other bacteria: less than 10^4 CFU/mL
A nurse is caring for a client with sepsis who is receiving empiric therapy with a broad-spectrum antimicrobial agent.
The nurse knows that this type of therapy is indicated for which situations? (Select all that apply.)
Explanation
Empiric therapy with a broad-spectrum antimicrobial agent is indicated for situations when the causative microorganism is unknown, when the infection is severe or life-threatening, and when there is a need to cover multiple pathogens.
Choice D is wrong because empiric therapy with a broad-spectrum antimicrobial agent is not indicated for situations when there is a risk of resistance.On the contrary, this approach can drive antimicrobial overuse and resistance and should be accompanied by a commitment to de-escalation and antimicrobial stewardship.
Choice E is wrong because empiric therapy with a broad-spectrum antimicrobial agent is not indicated for situations when there is a synergistic effect between two or more agents.
Synergistic effect means that the combined effect of two or more agents is greater than the sum of their individual effects.
This may be desirable in some cases, but it is not a reason to use empiric therapy with a broad-spectrum antimicrobial agent.
A nurse is educating a client who has been prescribed amoxicillin for a sinus infection.
The client asks, “Why do I have to take this drug three times a day?” What is the best response by the nurse?
Explanation
This drug has a short half-life, so it needs to be taken frequently to maintain effective levels in your body.The half-life of amoxicillin is61.3 minutes, which means that half of the drug is eliminated from the body in about an hour. To keep a constant amount of the drug in the blood and tissues, it needs to be taken every 8 hours or three times a day.
Choice B is wrong because the minimum bactericidal concentration (MBC) is the lowest concentration of an antibiotic that kills 99.9% of bacteria.
Amoxicillin has a low MBC, which means it is effective at killing bacteria at low doses.
Choice C is wrong because the therapeutic index (TI) is the ratio of the toxic dose to the effective dose of a drug.
Amoxicillin has a high TI, which means it has a wide margin of safety and is unlikely to cause toxicity.
Choice D is wrong because the spectrum of activity refers to the range of bacteria that an antibiotic can kill or inhibit.
Amoxicillin has a broad spectrum of activity, which means it can target many types of bacteria, including gram-positive and gram-negative ones.
Normal ranges for amoxicillin are 5 to 25 mcg/mL for peak levels and less than 0.5 mcg/mL for trough levels.
Peak levels are measured 1 to 2 hours after taking the drug, and trough levels are measured just before the next dose.
A nurse is monitoring a client who is receiving vancomycin for a methicillin-resistant Staphylococcus aureus (MRSA) infection. The nurse notices that the client has developed flushing, rash, and pruritus on the face and neck.
What is the most appropriate action by the nurse?
Explanation
Slow down the infusion and administer an antihistamine.The client has developedred man syndrome, which is a common adverse reaction to vancomycin that occurs when the drug is infused too rapidly.It is not a serious or life-threatening condition and can be managed by slowing down the infusion rate and giving an antihistamine to relieve the symptoms.
Choice A is wrong because stopping the infusion and notifying the prescriber immediately is indicated for a severe allergic reaction or anaphylaxis, which is characterized by hypotension, bronchospasm, and laryngeal edema.
Red man syndrome does not cause these signs.
Choice C is wrong because continuing the infusion and documenting the findings is not appropriate for red man syndrome, which requires intervention to prevent further discomfort and complications.
Choice D is wrong because increasing the infusion rate and monitoring vital signs would worsen red man syndrome and increase the risk of ototoxicity and nephrotoxicity, which are serious adverse effects of vancomycin.
A nurse is preparing to administer gentamicin, an aminoglycoside antibiotic, to a client with a serious gram-negative infection.
The nurse understands that this class of antibiotics has a potential adverse effect on which organ system?
Explanation
Gentamicin is an aminoglycoside antibiotic that can causekidney damage, reduced urine output, blood in the urine, andnephrotoxicity.Patients with impaired renal function, advanced age, dehydration, and those who receive high doses or prolonged therapy are at an increased risk of toxicity.Serum concentrations of gentamicin should be monitored when feasible to assure adequate levels and to avoid potentially toxic levels.
Choice B is wrong because Hepatic is wrong because gentamicin does not have a significant adverse effect on the liver.However, some rare cases of transient hepatomegaly and splenomegaly have been reported.
Choice C is wrong because Cardiac is wrong because gentamicin does not directly affect the heart.However, it can cause electrolyte imbalance (low levels of calcium, potassium, or magnesium in the blood) which can affect the cardiac rhythm.It can also cause hypotension or hypertension in some cases.
Choice D is wrong because Hematologic is wrong because gentamicin does not cause blood disorders.However, it can cause anemia, leukopenia, granulocytopenia, and thrombocytopenia in patients with preexisting renal impairment or who receive concomitant therapy with other nephrotoxic or hematotoxic drugs.It can also cause bleeding due to hypoprothrombinemia in patients with renal failure or who are on anticoagulant therapy.
Adverse effects and toxicity
A nurse is reviewing the medication history of a client who is prescribed an antibiotic for a urinary tract infection. The nurse notes that the client has a history of allergic reactions to penicillins, cephalosporins, sulfonamides, and fluoroquinolones.
Which class of antibiotics should the nurse avoid administering to this client?
Explanation
The nurse should avoid administering macrolides to this client because they have a history of allergic reactions to penicillins, cephalosporins, sulfonamides, and fluoroquinolones.Macrolides are a class of antibiotics that have a similar structure and mechanism of action to penicillins and cephalosporins.Therefore, there is a risk of cross-reactivity and hypersensitivity reactions between these antibiotics.
Choice B is wrong because Tetracyclines is wrong because tetracyclines are a class of antibiotics that have a different structure and mechanism of action from penicillins, cephalosporins, sulfonamides, and fluoroquinolones.They are not likely to cause cross-reactivity or hypersensitivity reactions in this client.
Choice C is wrong because Aminoglycosides is wrong because aminoglycosides are a class of antibiotics that have a different structure and mechanism of action from penicillins, cephalosporins, sulfonamides, and fluoroquinolones.They are not likely to cause cross-reactivity or hypersensitivity reactions in this client.
Choice D is wrong because Glycopeptides is wrong because glycopeptides are a class of antibiotics that have a different structure and mechanism of action from penicillins, cephalosporins, sulfonamides, and fluoroquinolones.They are not likely to cause cross-reactivity or hypersensitivity reactions in this client.
(Select all that apply) A client is receiving vancomycin (Vancocin) for a severe infection caused by methicillin-resistant Staphylococcus aureus (MRSA).
The nurse monitors the client for signs of nephrotoxicity, which include:
Explanation
Elevated serum creatinine and decreased urine output are signs of nephrotoxicity, which is a potential adverse effect of vancomycin (Vancocin) therapy. Nephrotoxicity is damage to the kidneys caused by toxic substances.
Choice C is wrong because increased blood pressure is not a sign of nephrotoxicity.Hypotension may occur during vancomycin infusion, especially if it is given too rapidly.
Choice D is wrong because hematuria is not a sign of nephrotoxicity.
Hematuria is blood in the urine, which may indicate other problems such as urinary tract infection, kidney stones, or bladder cancer.
Choice E is wrong because tinnitus is not a sign of nephrotoxicity.Tinnitus is ringing or buzzing in the ears, which may indicate ototoxicity, another potential adverse effect of vancomycin therapy.
Ototoxicity is damage to the ears caused by toxic substances.
Normal ranges for serum creatinine are 0.6 to 1.2 mg/dL for men and 0.5 to 1.1 mg/dL for women.
Normal ranges for urine output are 800 to 2000 mL per day or 30 to 50 mL per hour.
A client develops diarrhea after taking amoxicillin (Amoxil) for a sinus infection. The nurse suspects that the diarrhea is caused by a superinfection of Clostridioides difficile (C. diff).
Which statement by the client supports this suspicion?
Explanation
This statement supports the suspicion of difficile infection, which is a common cause of antibiotic-associated diarrhea. Difficile infection can cause severe diarrhea and dehydration, lower abdominal pain and cramping, low-grade fever, nausea, and loss of appetite.The diarrhea is usually watery and has a very foul odor.
Choice A is wrong because taking probiotics to restore normal flora does not indicate C. difficile infection.Probiotics are live microorganisms that may help prevent or treat antibiotic-associated diarrhea by replenishing the good bacteria in the gut.
Choice C is wrong because abdominal cramps and bloating are nonspecific symptoms that can occur with many gastrointestinal disorders, not just difficile infection.
Choice D is wrong because loss of appetite and nausea are also nonspecific symptoms that can occur with many gastrointestinal disorders, not just difficile infection.
A nurse is teaching a client who is prescribed doxycycline (Vibramycin) for Lyme disease. The nurse instructs the client to avoid exposure to sunlight while taking this drug because it may cause photosensitivity.
Which statement by the client indicates understanding of this instruction?
Explanation
This statement indicates that the client understands that doxycycline can cause photosensitivity, which is a heightened skin sensitivity or unusual reaction when exposed to UV radiation from the sun or a tanning bed.Photosensitivity can cause damage at the DNA level, painful sunburn-like erythema, blistering, lichenoid eruptions, and photo-onycholysis.The client should avoid excessive sun exposure and use photoprotection methods against both UVB and UVA wavelengths.
Choice B is wrong because taking the drug at night before bed does not prevent photosensitivity during the day.The drug or its metabolites can remain in the skin for several days after ingestion.
Choice C is wrong because drinking plenty of fluids to prevent dehydration is not related to photosensitivity.
Dehydration can occur due to other causes such as vomiting, diarrhea, fever, or excessive sweating.
Choice D is wrong because stopping the drug if a rash develops is not advisable.
The rash could be a sign of photosensitivity or an allergic reaction, and the client should consult their doctor before discontinuing the medication.
Stopping the drug abruptly could also lead to treatment failure or bacterial resistance.
A nurse is caring for a client who has tuberculosis and is receiving isoniazid (INH), rifampin (Rifadin), pyrazinamide (PZA), and ethambutol (Myambutol).
The nurse monitors the client’s liver function tests and advises the client to avoid which substance while taking these drugs?
Explanation
The patient should avoid alcohol while taking these drugs because alcohol can increase the risk of liver toxicity.These drugs are metabolized by the liver and can cause hepatotoxicity, especially isoniazid and pyrazinamide.The nurse should monitor the patient’s liver function tests and advise the patient to report any signs of liver damage, such as dark urine, fatigue, or jaundice.
Choice B is wrong because Grapefruit juice is wrong because grapefruit juice does not interact with these drugs.
Grapefruit juice can affect the metabolism of some other drugs, such as statins, calcium channel blockers, or cyclosporine, but not antitubercular drugs.
Choice C is wrong because Milk is wrong because milk does not interact with these drugs.
Milk can reduce the absorption of some other drugs, such as tetracyclines or fluoroquinolones, but not antitubercular drugs.
Choice D is wrong because Caffeine is wrong because caffeine does not interact with these drugs.
Caffeine can increase the effects of some other drugs, such as theophylline or clozapine, but not antitubercular drugs.
Antimicrobial resistance
A nurse is caring for a client with a urinary tract infection caused by Escherichia coli. The client is prescribed ciprofloxacin, a fluoroquinolone antibiotic.
The nurse understands that this antibiotic works by which mechanism?
Explanation
Ciprofloxacin works by inhibiting DNA gyrase, a type II topoisomerase, and topoisomerase IV, enzymes necessary to separate bacterial DNA, thereby inhibiting cell division.
Choice A is wrong because ciprofloxacin does not inhibit cell wall synthesis.
That is the mechanism of action of beta-lactam antibiotics, such as penicillins and cephalosporins.
Choice B is wrong because ciprofloxacin does not inhibit protein synthesis.
That is the mechanism of action of macrolides, such as erythromycin and azithromycin.
Choice D is wrong because ciprofloxacin does not inhibit folic acid synthesis.
That is the mechanism of action of sulfonamides, such as sulfamethoxazole and trimethoprim.
A nurse is educating a client with tuberculosis about the importance of adhering to the prescribed regimen of rifampin, isoniazid, pyrazinamide, and ethambutol for six months.
The nurse should explain that this combination of drugs is necessary to:
Explanation
This means that the combination of drugs reduces the chances of the bacteria becoming resistant to one or more of the drugs, which would make the treatment ineffective.
Choice B is wrong because “enhance the selective toxicity of each drug” means that the drugs would target only the bacteria and not harm the host cells, which is not the main reason for using a combination of drugs.
Choice C is wrong because “increase the penetration of drugs into the lungs” means that the drugs would reach the site of infection more easily, which is not the main reason for using a combination of drugs.
Choice D is wrong because “reduce the adverse effects of each drug” means that the drugs would have less side effects when used together, which is not the main reason for using a combination of drugs.In fact, some of these drugs can have serious side effects such as liver damage, vision loss, or nerve damage.
Normal ranges for rifampin are 8-24 mcg/mL, for isoniazid are 1-6 mcg/mL, for pyrazinamide are 20-60 mcg/mL, and for ethambutol are 2-6 mcg/mL.
A client with a wound infection caused by methicillin-resistant Staphylococcus aureus (MRSA) asks the nurse how the bacteria became resistant to methicillin.
The nurse should respond by saying:
Explanation
The bacteria have an altered target site that methicillin cannot bind to.This means that the bacteria have changed their structure so that the antibiotic cannot attach to them and kill them.
Choice A is wrong because methicillin does not work by being broken down by an enzyme.Some other antibiotics, such as penicillin, can be inactivated by bacterial enzymes, but not methicillin.
Choice C is wrong because methicillin does not work by entering the bacterial cell.Some other antibiotics, such as tetracycline, can be expelled by bacterial membrane pumps, but not methicillin.
Choice D is wrong because methicillin does not work by blocking an alternative pathway.Some other antibiotics, such as sulfonamides, can be bypassed by bacterial alternative pathways, but not methicillin.
A nurse is administering gentamicin, an aminoglycoside antibiotic, to a client with a severe gram-negative infection. The nurse should monitor the client for signs of nephrotoxicity and ototoxicity, which are potential adverse effects of this antibiotic.
The nurse should also be aware that these adverse effects are:
Explanation
This means that the higher the dose and the longer the duration of aminoglycoside therapy, the greater the risk of nephrotoxicity and ototoxicity, which are damage to the kidneys and ears respectively.These adverse effects are irreversible because they cause permanent damage to the cells of these organs.
Choice A is wrong because dose-dependent and reversible implies that the adverse effects can be reversed by lowering the dose or stopping the therapy, which is not true for aminoglycosides.
Choice C is wrong because time-dependent and reversible implies that the adverse effects are related to the length of exposure and can be reversed by shortening the therapy, which is also not true for aminoglycosides.
Choice D is wrong because time-dependent and irreversible implies that the adverse effects are related to the length of exposure and cannot be reversed by shortening the therapy, which is partly true but not as accurate as choice B.
Normal ranges for BUN are 7 to 20 mg/dL and for creatinine are 0.6 to 1.2 mg/dL for men and 0.5 to 1.1 mg/dL for women.Signs of nephrotoxicity include increased BUN and creatinine levels, decreased urine output, proteinuria, hematuria, and casts in urine.Signs of ototoxicity include tinnitus, hearing loss, dizziness, vertigo, and headache
Nursing implications and patient education
A nurse is preparing to administer an antimicrobial agent to a patient who has a urinary tract infection. The nurse reviews the culture and sensitivity results and notes that the microorganism is resistant to the prescribed antimicrobial agent.
What is the most appropriate action by the nurse?
Explanation
Hold the antimicrobial agent and notify the prescriber of the resistance.This is because administering an antimicrobial agent that the microorganism is resistant to will not be effective and may increase the risk of medication toxicity. The prescriber should be informed so that they can order a different antimicrobial agent that is sensitive to the microorganism.
Choice A is wrong because administering the antimicrobial agent as ordered and monitoring for therapeutic effects will not treat the urinary tract infection (UTI) and may allow the infection to spread or worsen.
Choice C is wrong because administering a different antimicrobial agent that is sensitive to the microorganism without consulting the prescriber is outside the nurse’s scope of practice and may cause adverse effects or interactions.
Choice D is wrong because administering the antimicrobial agent with another medication to enhance its activity without consulting the prescriber is also outside the nurse’s scope of practice and may not be appropriate for the type of microorganism causing the UTI.
A nurse is educating a patient about the adverse effects of antimicrobial therapy.
Which of the following statements by the patient indicate a need for further teaching? (Select all that apply.)
Explanation
The correct answer is choice D and E and they indicate a need for further teaching.
Choice D is wrong because the patient should not stop taking the medication if they develop a rash or hives, but should report it to the provider immediately, as this could indicate a serious allergic reaction.
Choice E is wrong because the patient should not take an antacid if they have stomach upset, as this could interfere with the absorption of the antimicrobial drug.
Some additional information:
• Choice A is correct because drinking plenty of fluids can help prevent kidney damage from some antimicrobial drugs, such as aminoglycosides.
• Choice B is correct because ringing in the ears or hearing loss can be signs of ototoxicity from some antimicrobial drugs, such as vancomycin.
• Choice C is correct because some antimicrobial drugs, such as tetracyclines and sulfonamides, can increase the sensitivity to sunlight and cause sunburns.
• Normal ranges for kidney function tests are blood urea nitrogen (BUN) 7 to 20 mg/dL and creatinine 0.6 to 1.2 mg/dL.
• Normal ranges for liver function tests are alanine aminotransferase (ALT) 7 to 56 units/L and aspartate aminotransferase (AST) 10 to 40 units/L.
A nurse is caring for a patient who is receiving intravenous vancomycin for a severe infection. The patient complains of itching and flushing of the face, neck, and chest.
The nurse recognizes these symptoms as indicative of what?
Explanation
A red man syndrome is a reaction to the antibiotic vancomycin that causes flushing, itching, and sometimes hypotension and tachycardia. It is not a true allergic reaction, but rather a pseudoallergic or anaphylactoid reaction caused by the release of histamine from mast cells. It is more likely to occur when vancomycin is infused rapidly or at high doses.The symptoms usually resolve with slowing or stopping the infusion, and can be prevented by premedicating with antihistamines or extending the infusion time
Choice A is wrong because an allergic reaction to vancomycin would involve IgE-mediated hypersensitivity, which can cause urticaria, angioedema, bronchospasm, and anaphylaxis.An allergic reaction would not be dependent on the infusion rate or dose of vancomycin, and would require immediate discontinuation of the drug and treatment with epinephrine and other supportive measures
Choice B is wrong because a superinfection is a secondary infection that occurs when the normal flora of the body is disrupted by antibiotics, allowing opportunistic pathogens to proliferate. Common examples of superinfections are Clostridioides difficile colitis, oral or vaginal candidiasis, and methicillin-resistant Staphylococcus aureus infections. Superinfections do not cause flushing or itching, but rather symptoms related to the site of infection, such as diarrhea, abdominal pain, oral thrush, or skin lesions.Superinfections may require treatment with different antibiotics or antifungals
Choice C is wrong because a disulfiram-like reaction is a reaction that occurs when alcohol is consumed while taking certain drugs that inhibit the enzyme acetaldehyde dehydrogenase, which is responsible for metabolizing alcohol. This leads to the accumulation of acetaldehyde, which causes nausea, vomiting, headache, flushing, palpitations, and hypotension. Vancomycin does not cause a disulfiram-like reaction, but some other antibiotics such as metronidazole and cephalosporins do.A disulfiram-like reaction can be avoided by abstaining from alcohol while taking these drugs
A nurse is administering gentamicin, an aminoglycoside antibiotic, to a patient who has a gram-negative infection.
The nurse monitors the patient’s serum creatinine level as an indicator of what?
Explanation
Gentamicin is an aminoglycoside antibiotic that can cause nephrotoxicity, which is the damage of the kidney.Gentamicin induces nephrotoxicity by inhibiting protein synthesis in renal cells that specifically causes necrosis of cells in the renal proximal tubule, resulting in acute tubular necrosis, followed by acute renal failure.The nurse monitors the patient’s serum creatinine level as an indicator of nephrotoxicity because serum creatinine reflects the glomerular filtration rate (GFR) and kidney function.
Choice A is wrong because hepatotoxicity is the damage of the liver, not the kidney.
Gentamicin is not known to cause hepatotoxicity.
Choice C is wrong because neurotoxicity is the damage of the nervous system, not the kidney.
Gentamicin can cause neurotoxicity by affecting the neuromuscular junction and causing muscle weakness or paralysis, but this is not related to serum creatinine level.
Choice D is wrong because ototoxicity is the damage of the ear, not the kidney.
Gentamicin can cause ototoxicity by damaging the hair cells in the inner ear and causing hearing loss or balance problems, but this is not related to serum creatinine level.
Normal ranges for serum creatinine are 0.6 to 1.2 mg/dL for men and 0.5 to 1.1 mg/dL for women.
A nurse is teaching a patient who has been prescribed metronidazole, a nitroimidazole antibiotic, for a bacterial infection.
The nurse instructs the patient to avoid consuming what substance while taking this medication?
Explanation
The patient should avoid consuming alcohol while taking metronidazole, a nitroimidazole antibiotic, for a bacterial infection.This is because the combination of metronidazole and alcohol can cause a reaction (often referred to as a disulfiram-like reaction) in some people that may include nausea, vomiting, flushing, fast heart beat, and stomach cramps.This reaction can be severe and even fatal.It is best to avoid alcohol while taking metronidazole and for at least 3 days after the last dose.
Choice A is wrong because grapefruit juice does not interact with metronidazole.
Choice B is wrong because dairy products do not interact with metronidazole.
Choice D is wrong because caffeine does not interact with metronidazole.
Interactions and contraindications
A nurse is preparing to administer penicillin to a client who has a bacterial infection. The client also takes probenecid for gout.
What effect will probenecid have on the penicillin?
Explanation
It will increase the serum levels and half-life of penicillin.Probenecid inhibits the renal excretion of penicillin, which prolongs its action and increases its concentration in the blood. This can be beneficial for treating severe infections, but it also increases the risk of adverse effects and toxicity.
Choice B is wrong because probenecid does not affect the absorption or bioavailability of penicillin.
These factors depend on the route of administration and the formulation of the drug.
Choice C is wrong because probenecid does not enhance the bactericidal activity of penicillin.
Penicillin kills bacteria by interfering with their cell wall synthesis, which is independent of probenecid.
Choice D is wrong because probenecid does not reduce the risk of allergic reaction to penicillin.In fact, probenecid may increase the risk of hypersensitivity reactions by prolonging the exposure to penicillin.
Normal ranges for serum levels and half-life of penicillin vary depending on the type and dose of penicillin, but generally they are between 2 to 40 mcg/mL and 0.5 to 1.5 hours, respectively.
A nurse is caring for a client who is receiving vancomycin for a severe infection caused by methicillin-resistant Staphylococcus aureus (MRSA). The client also takes furosemide for heart failure.
Which of the following adverse effects should the nurse monitor for in this client? (Select all that apply.).
Explanation
Hearing loss and nephrotoxicity are possible adverse effects of vancomycin, especially when used with other drugs that can affect the kidneys or ears, such as furosemide. The nurse should monitor the client’s renal function tests, serum vancomycin levels, and hearing acuity while receiving this combination of drugs.
Choice C, red man syndrome, is a hypersensitivity reaction to vancomycin that causes flushing, itching, and rash on the face, neck, and upper body.It is not related to furosemide use and can be prevented by slowing the infusion rate of vancomycin.
Choice D, hypokalemia, is a low level of potassium in the blood that can be caused by furosemide, a loop diuretic that increases the excretion of potassium.However, vancomycin does not affect potassium levels and does not increase the risk of hypokalemia.
Choice E, thrombocytopenia, is a low level of platelets in the blood that can cause bleeding problems.
It is a rare side effect of vancomycin that occurs in less than 1% of patients.It is not related to furosemide use and does not occur more frequently with this combination of drugs.
A nurse is teaching a client who has a urinary tract infection (UTI) about trimethoprim/sulfamethoxazole. The client asks why he needs to take two antibiotics together.
What should the nurse say?
Explanation
The combination of trimethoprim and sulfamethoxazole has a synergistic effect that inhibits bacterial growth more effectively than either drug alone. This means that the two drugs work together to produce a greater effect than the sum of their individual effects.
Choice B is wrong because the combination of trimethoprim and sulfamethoxazole does not have an additive effect that reduces the dosage and frequency of administration of each drug.
The dosage and frequency of administration are determined by the severity of the infection, the renal function of the client, and the susceptibility of the bacteria.
Choice C is wrong because the combination of trimethoprim and sulfamethoxazole does not have an antagonistic effect that prevents the development of resistance to either drug.
Antagonistic effect means that one drug reduces or cancels out the effect of another drug.
The combination of trimethoprim and sulfamethoxazole may still cause resistance in some bacteria.
Choice D is wrong because the combination of trimethoprim and sulfamethoxazole does not have a selective effect that targets only the bacteria causing the UTI and spares the normal flora.
Selective effect means that a drug affects only certain types of cells or organisms.
The combination of trimethoprim and sulfamethoxazole is a broad-spectrum antibiotic that can affect both gram-positive and gram-negative bacteria, including some normal flora.
A nurse is administering tetracycline to a client who has acne vulgaris. The client tells the nurse that he usually takes calcium supplements with his meals.
How should the nurse respond?
Explanation
You should take calcium supplements at least 2 hours before or after tetracycline.This is because calcium can interfere with the absorption of tetracycline and reduce its effectiveness.
Choice A is wrong because taking calcium supplements with food does not prevent the interaction with tetracycline.
Choice B is wrong because avoiding calcium supplements altogether is not necessary and may deprive the client of an important nutrient.
Choice C is wrong because drinking plenty of water does not prevent the interaction with tetracycline either.
Normal ranges for calcium are 8.5 to 10.2 mg/dL for adults.Tetracycline is an antibiotic that is used to treat acne vulgaris and other infections.It should be taken on an empty stomach with a full glass of water.
A nurse is reviewing the medication history of a client who is prescribed azithromycin for a respiratory infection. The nurse notes that the client is also taking warfarin for atrial fibrillation.
What action should the nurse take?
Explanation
There is conflicting evidence about the interaction between azithromycin and warfarin.Some studies suggest that azithromycin does not affect warfarin metabolism or prothrombin time, while others report that azithromycin may enhance warfarin’s effects and increase the risk of bleeding or bruising.The FDA approved label revisions for azithromycin warn of a potential interaction with warfarin. Therefore, the nurse should inform the prescriber about this possible interaction and monitor the client’s prothrombin time or International Normalized Ratio (INR) periodically.
Choice B is wrong because it is not enough to instruct the client to monitor for signs of bleeding, such as bruising, hematuria, or melena.
The nurse should also inform the prescriber and check the client’s INR regularly.
Choice C is wrong because it is not advisable to advise the client to increase the intake of vitamin K-rich foods, such as green leafy vegetables, while taking azithromycin.
Vitamin K can reduce the effectiveness of warfarin and increase the risk of clotting.The client should maintain a consistent level of vitamin K intake throughout the treatment with warfarin.
Choice D is wrong because it is not relevant to the question.
Azithromycin does not affect hormonal contraception, such as pills, patches, or rings.The client does not need to use an alternative form of contraception, such as condoms, while taking azithromycin.
More questions on this topic
A nurse is preparing to administer ceftriaxone (Rocephin) to a client who has pneumonia caused by Streptococcus pneumoniae.
The nurse should recognize that ceftriaxone belongs to which generation of cephalosporins?
Explanation
Ceftriaxone belongs to the third-generation of cephalosporins.Third-generation cephalosporins have greater activity than the second-generation cephalosporins against certain gram-negative bacteria, such as Streptococcus pneumoniae.They are also more resistant to beta-lactamases, enzymes that can inactivate some cephalosporins.
Choice A is wrong because first-generation cephalosporins have less activity against gram-negative bacteria and are more susceptible to beta-lactamases.
Choice B is wrong because second-generation cephalosporins have less activity against Streptococcus pneumoniae than third-generation cephalosporins, and are also less resistant to beta-lactamases.
Choice D is wrong because fourth-generation cephalosporins have a broader spectrum of activity against gram-negative bacteria, including some that are resistant to third-generation cephalosporins, but they are not more effective against Streptococcus pneumoniae.
A nurse is caring for a client who has a severe infection and is receiving vancomycin (Vancocin).
The nurse should monitor the client for which of the following manifestations of ototoxicity?
Explanation
Vancomycin is an antibiotic that can cause ototoxicity, which is damage to the inner ear due to exposure to certain drugs.Ototoxicity can manifest as tinnitus (ringing in the ears), vertigo (dizziness), and hearing loss.Vancomycin ototoxicity is usually related to high serum levels of the drug and is more likely to occur in patients with renal impairment.Vancomycin can also potentiate the ototoxicity of other drugs, such as aminoglycosides.
Choice A is wrong because tinnitus is a possible manifestation of ototoxicity.
Choice B is wrong because vertigo is a possible manifestation of ototoxicity.
Choice C is wrong because hearing loss is a possible manifestation of ototoxicity.
A nurse is educating a client who has a respiratory infection and a new prescription for azithromycin (Zithromax).
Which of the following instructions should the nurse include? (Select all that apply).
Explanation
Choice A is wrong because azithromycin (Zithromax) should be takenwith foodto prevent stomach upset.
Choice B is correct because azithromycin can causeliver damageand the client should report any signs ofjaundiceordark urineas they may indicate liver problems.
Choice C is correct because azithromycin can interact withgrapefruit juiceand increase the risk ofside effectssuch as nausea, vomiting, diarrhea, headache and QT interval prolongation.
Choice D is correct because the client shouldcomplete the full course of therapyas prescribed to prevent bacterial resistance and recurrence of infection.
Choice E is wrong because azithromycin should be stored in arefrigeratorand discarded after 10 days if it is in a liquid form.
Which of the following antiviral medications inhibits neuraminidase enzyme?
Explanation
This is because oseltamivir is aneuraminidase inhibitor, which means it blocks the enzyme that helps the influenza virus to spread from cell to cell. By preventing the release of new virus particles, oseltamivir reduces the duration and severity of influenza infection.
Choice A is wrong becauseAcyclovir is wrong because it is anucleoside analogthat inhibits viral DNA synthesis.
It is effective against herpes simplex virus (HSV) and varicella zoster virus (VZV), but not against influenza virus.
Choice C is wrong because Efavirenz is wrong because it is a **non-nucleoside reverse transcript
Which of the following antiviral medications prevents viral fusion with host cell membrane?
Explanation
Maraviroc is aCCR5 coreceptor antagonistthat blocks the receptor site the HIV virus needs to interact with in order to enter the cell.It prevents viral fusion with host cell membrane by binding to the CCR5 receptor on CD4+ T cells and macrophages.
Choice B is wrong becauseAbacavir is wrong because it is anucleoside reverse transcriptase inhibitor (NRTI)that inhibits the enzyme reverse transcriptase, which converts viral RNA into DNA.
It does not prevent viral fusion with host cell membrane.
Choice C is wrong becauseDarunavir is wrong because it is aprotease inhibitor (PI)that inhibits the enzyme protease, which cleaves viral proteins into functional units.
It does not prevent viral fusion with host cell membrane.
Choice D is wrong becauseFosamprenavir is wrong because it is also aprotease inhibitor (PI)that inhibits the enzyme protease.
It does not prevent viral fusion with host cell membrane.
A nurse is caring for a client who has oral candidiasis and is prescribed nystatin suspension.
Which of the following actions should the nurse take?
Explanation
This is because nystatin suspension is an antifungal medication that works by coating the oral mucosa and killing the candida organisms.Swishing and swallowing the medication ensures that it reaches all the affected areas in the mouth and throat.
Choice B is wrong because administering the medication with a dropper to avoid aspiration is not necessary for a client who has oral candidiasis.
The client should be able to swish and swallow the medication without difficulty.
Choice C is wrong because diluting the medication with water before giving it to the client reduces its effectiveness and concentration.
The medication should be given undiluted for optimal results.
Choice D is wrong because giving the medication after meals to increase its effectiveness is not accurate.The medication should be given at least 30 minutes before or after meals to avoid interference with food or beverages.
A nurse is reviewing laboratory results for a client who has a fungal infection and is receiving itraconazole therapy.
Which of the following findings should alert the nurse to a potential adverse effect of this medication?
Explanation
This is because itraconazole can cause renal impairment and decreased urine output as an adverse effect.A normal serum creatinine level is 0.6 to 1.2 mg/dL for males and 0.5 to 1.1 mg/dL for females.
Choice B is wrong because decreased serum potassium level is not an adverse effect of itraconazole.Itraconazole can cause hypokalemia, which is a low level of potassium in the blood, but this is usually due to fluid retention and heart failure caused by the drug.A normal serum potassium level is 3.5 to 5.0 mEq/L.
Choice C is wrong because increased serum glucose level is not an adverse effect of itraconazole.Itraconazole can cause hyperglycemia, which is a high level of glucose in the blood, but this is usually due to diabetes mellitus or steroid use in patients taking the drug.A normal serum glucose level is 70 to 100 mg/dL.
Choice D is wrong because decreased white blood cell count is not an adverse effect of itraconazole.Itraconazole can cause leukopenia, which is a low level of white blood cells in the blood, but this is usually due to bone marrow suppression or infection in patients taking the drug.A normal white blood cell count is 4,500 to 11,000 cells/mm3.
A nurse is preparing to administer flucytosine to a client who has a systemic fungal infection.
Which of the following assessments should the nurse perform before giving this medication? (Select all that apply.).
Explanation
Flucytosine can cause bone marrow suppression and renal toxicity, so the nurse should monitor the client’s renal function tests and complete blood count before giving this medication.
These tests can help detect any signs of anemia, leukopenia, thrombocytopenia, or impaired kidney function that may require dose adjustment or discontinuation of the drug.
Choice A is wrong because flucytosine does not affect liver function significantly.Choice C is wrong because flucytosine does not cause changes in blood pressure.Choice E is wrong because flucytosine does not affect cardiac function or cause arrhythmias.
A nurse is caring for a client who has trichomoniasis and is prescribed tinidazole.
Which of the following instructions should the nurse give to the client?
Explanation
The client should avoid sexual intercourse until treatment is completed.This is because trichomoniasis is a sexually transmitted infection that can be passed between partners during penile-vaginal sex or through transmission of infected vaginal fluids or fomites among women who have sex with women. Therefore, abstaining from sex until both partners are cured can prevent reinfection and transmission.
Choice A is wrong because taking the medication with an antacid can reduce its absorption and effectiveness.Tinidazole should be taken with food to minimize gastrointestinal side effects.
Choice B is wrong because drinking plenty of fluids to prevent crystalluria is not relevant for tinidazole.
Crystalluria is a condition where crystals form in the urine, which can cause kidney stones or damage.This is a potential complication of some antibiotics, such as sulfonamides, but not tinidazole.
Choice D is wrong because chewing the tablets thoroughly before swallowing is not necessary for tinidazole.Tinidazole tablets are film-coated and can be swallowed whole with water.
Chewing the tablets may alter their release and absorption, and may also cause a bitter aftertaste.
A nurse is preparing to administer ivermectin to a client who has onchocerciasis (river blindness).
Which of the following adverse effects should the nurse monitor for in this client?
Explanation
A Mazzotti reaction is a severe inflammatory response that can occur after taking ivermectin for onchocerciasis (river blindness), a parasitic infection caused by Onchocerca volvulus.The reaction is due to the death of the microfilariae (larvae) of the parasite and can cause fever, rash, itching, joint pain, swollen lymph nodes, and eye inflammation.
Choice A is wrong because hypertension is not a common adverse effect of ivermectin.Hypotension, however, can occur in some cases.
Choice B is wrong because tinnitus is not a common adverse effect of ivermectin.Tinnitus is a ringing or buzzing sound in the ears that can be caused by various factors, such as exposure to loud noise, ear infections, or certain medications.
Choice D is wrong because Stevens-Johnson syndrome is not a common adverse effect of ivermectin.
Stevens-Johnson syndrome is a rare but serious skin reaction that can be triggered by infections or medications.
It causes blisters and peeling of the skin and mucous membranes.
A nurse is educating a group of travelers who are going to a region where malaria is endemic.
Which of the following antimalarial drugs should the nurse recommend for prophylaxis? (Select all that apply.).
Explanation
These are the antimalarial drugs that are recommended for prophylaxis by the CDC and other sources.
They are effective against the malaria parasites that are resistant to chloroquine and primaquine, which are the other two options.
Choice A is wrong because chloroquine is not effective in areas where chloroquine resistance is present, which is most of the malaria-endemic regions.
Choice B is wrong because primaquine is not used for prophylaxis, but for radical cure of vivax and ovale malaria.It also requires a test for glucose-6-phosphate dehydrogenase (G6PD) deficiency before use, as it can cause hemolysis in people with this condition.
Choice C is correct because mefloquine is a suppressive prophylactic that can be used in areas with chloroquine resistance.
A nurse is caring for a client who is receiving gentamicin, an aminoglycoside antibiotic, for a severe infection.
The nurse should monitor the client for which adverse effects of this drug? (Select all that apply.)
Explanation
Gentamicin is an aminoglycoside antibiotic that can causeototoxicity(damage to the inner ear) andnephrotoxicity(damage to the kidneys) as serious side effects. These effects may be irreversible and can occur even at therapeutic doses. Therefore, the nurse should monitor the client’s hearing, balance, urine output, and blood tests for kidney function while on this drug.
Choice C is wrong because gentamicin does not causehepatotoxicity(damage to the liver).
This is more common with other antibiotics such as isoniazid or rifampin.
Choice D is wrong because gentamicin does not causeneuromuscular blockade(paralysis of muscles).
This is more common with other aminoglycosides such as neomycin or tobramycin.
Choice E is wrong because gentamicin does not causethrombocytopenia(low platelet count).
This is more common with other drugs such as heparin or sulfonamides.
A nurse is teaching a client who has tuberculosis about the prescribed drug regimen, which includes isoniazid, rifampin, pyrazinamide, and ethambutol.
The nurse should instruct the client to report which signs or symptoms as possible adverse effects of these drugs? (Select all that apply.)
Explanation
Jaundice, vision changes and numbness in the hands or feet are possible adverse effects of the drugs used to treat tuberculosis.The nurse should instruct the client to report these signs or symptoms as they may indicate liver damage, optic neuritis or peripheral neuropathy respectively.
Choice C is wrong because hearing loss is not a common side effect of these drugs.Hearing loss may be caused by other drugs such as aminoglycosides.
Choice D is wrong because orange-colored urine is a harmless side effect of rifampin and does not need to be reported.
The nurse should inform the client about this expected change and reassure them that it is not harmful.
The normal ranges for liver function tests are:
• AST: 10-40 U/L
• ALT: 7-56 U/L
• ALP: 45-115 U/L
• Bilirubin: 0.1-1.2 mg/dL
The normal range for visual acuity is 20/20.
The normal range for sensation is intact and symmetrical in all extremities.
Which statement is true regarding narrow spectrum antibiotics?
Explanation
They are effective against a few types of organisms.Narrow spectrum antibiotics are antibiotics that work against a limited range of bacteria, usually either gram-positive or gram-negative.They are more specific and less likely to cause resistance or disrupt the normal flora.
Choice A) They are effective against gram-positive bacteria only.This is not true because some narrow spectrum antibiotics can also target gram-negative bacteria, such as aminoglycosides.
Choice B) They are effective against gram-negative bacteria only.This is not true because some narrow spectrum antibiotics can also target gram-positive bacteria, such as vancomycin.
Choice C) They are effective against one type of organism.This is too restrictive because narrow spectrum antibiotics can work against more than one type of organism, such as penicillins that target both streptococci and staphylococci.
Which term is used to describe an agent that inhibits bacterial growth but does not kill bacteria?
Explanation
A bacteriostatic agent is an agent that inhibits the growth or reproduction of bacteria, but does not kill them.
This means that the bacteria are still alive, but they cannot multiply or cause infection.
Choice A) Bactericidal is wrong because a bactericidal agent is an agent with the capability to kill bacteria.
This means that the bacteria are no longer alive or viable.
Choice C) Bacteriolytic is wrong because a bacteriolytic agent is an agent that causes the lysis or rupture of bacterial cells.
This means that the bacteria are destroyed and their contents are released.
Choice D) Bacteriophage is wrong because a bacteriophage is not an agent, but a type of virus that infects and replicates within bacteria.
This means that the bacteriophage uses the bacteria as hosts and may kill them or not depending on the type of infection.
Question 78.
The nurse is caring for a patient receiving vancomycin (Vancocin) for treatment of an infection caused by methicillin-resistant Staphylococcus aureus (MRSA).
Which assessment finding would indicate a potentially serious adverse reaction to this drug?
Explanation
These are signs ofototoxicity, a potentially serious adverse reaction to vancomycin (Vancocin) and other aminoglycosides.Ototoxicity can damage the inner ear and cause permanent hearing loss or balance problems.
Choice A is wrong because redness and itching at the infusion site are not specific to vancomycin (Vancocin) and could indicate a local irritation or an allergic reaction to any drug.
Choice B is wrong because flushing, rash, and pruritus on the face and upper torso are symptoms ofred man syndrome, a common but not serious side effect of vancomycin (Vancocin) that occurs due to rapid infusion and histamine release.Red man syndrome can be prevented by infusing the drug over at least 1 hour.
Choice C is wrong because nausea, vomiting, and abdominal cramps are not specific to vancomycin (Vancocin) and could be caused by many factors, such as infection, food poisoning, or other drugs.
Normal ranges for vancomycin (Vancocin) trough levels are 10 to 20 mcg/mL for most infections and 15 to 20 mcg/mL for serious infections such as osteomyelitis, endocarditis, or meningitis.Levels above 20 mcg/mL increase the risk of ototoxicity and nephrotoxicity.
Therefore, the nurse should monitor the patient’s trough levels regularly and report any abnormal findings to the prescriber.
The nurse is providing discharge teaching for a patient who will be taking oral linezolid (Zyvox) to treat a complicated skin infection caused by vancomycin-resistant enterococci (VRE).
Which statement by the patient indicates a need for further teaching?
Explanation
This statement indicates a need for further teaching because linezolid should be taken for the full prescribed course of treatment, even if the symptoms improve or resolve.Stopping the medication too soon can lead to bacterial resistance or recurrence of the infection.
Choice A is wrong because it is a correct statement.Linezolid can cause optic neuropathy or vision changes, so patients should report any changes in their vision to their doctor.
Choice B is wrong because it is a correct statement.
Linezolid can interact with foods that contain tyramine, such as cheese and red wine, and cause a hypertensive crisis.Patients should avoid eating foods that contain tyramine while taking linezolid and for two weeks after stopping the medication.
Choice C is wrong because it is a correct statement.Linezolid can be taken with or without food, but taking it on an empty stomach may help with absorption and effectiveness.
A nurse is administering penicillin to a client who has streptococcal pharyngitis. The nurse should monitor for which adverse effect of penicillin therapy?
Explanation
Anaphylaxis is a severe allergic reaction that can be life-threatening and requires immediate medical attention.Penicillin is one of the most common causes of anaphylaxis.Symptoms of anaphylaxis include difficulty breathing, swelling of the face, throat, or tongue, hives, itching, low blood pressure, and shock.
Choice A is wrong because hypokalemia (low potassium levels in the blood) is not a common or serious side effect of penicillin therapy.Hypokalemia can cause muscle weakness, cramps, irregular heartbeat, and fatigue.
Choice B is wrong because hyperglycemia (high blood sugar levels) is not a common or serious side effect of penicillin therapy.Hyperglycemia can cause thirst, frequent urination, blurred vision, and headaches.
Choice D is wrong because constipation is not a common or serious side effect of penicillin therapy.Constipation can cause abdominal pain, bloating, and difficulty passing stools.
A nurse is caring for a client who has tuberculosis and is prescribed rifampin, an antitubercular drug. The nurse should instruct the client about which potential side effect of rifampin?
Explanation
The nurse should instruct the client about this possibility and reassure them that it is harmless and will disappear when the medication is discontinued.
Choice B is wrong because metallic taste in mouth is not a side effect of rifampin, but of metronidazole, an antibiotic used to treat infections caused by anaerobic bacteria or protozoa.
Choice C is wrong because photosensitivity reaction is not a side effect of rifampin, but of tetracycline, an antibiotic used to treat acne and other infections.
Choice D is wrong because ototoxicity is not a side effect of rifampin, but of aminoglycosides, a class of antibiotics used to treat serious infections caused by gram-negative bacteria.
Ototoxicity can cause hearing loss or balance problems.
A nurse is teaching a client who has been prescribed tetracycline, a tetracycline antibiotic, for acne vulgaris.
Which of these instructions should the nurse include in the teaching? (Select all that apply.)
Explanation
The nurse should include these instructions in the teaching because:
• Tetracycline should be taken on an empty stomach to avoid interference with absorption.
• Dairy products should be avoided while taking this drug because they contain calcium, which can form insoluble complexes with tetracycline and reduce its effectiveness.
• Sunscreen or sun avoidance should be used while taking this drug because it can cause photosensitivity, which increases the risk of sunburn and skin damage.
• Plenty of fluids should be drunk while taking this drug because it can cause nephrotoxicity, which is damage to the kidneys.
Choice E is wrong because vaginal itching or discharge is not a common side effect of tetracycline.It may indicate a superinfection, which is a secondary infection caused by the disruption of normal flora by antibiotics.
This should be reported to the health care provider as soon as possible.
The nurse identifies which host factor as the most important when choosing an antimicrobial drug?
Explanation
This is because antibiotics act synergistically with the immune system to subdue infection, and it is critical for success that the host defenses are adequate.
Choice A is wrong becauseAge is wrong because age is a general factor that must be considered when choosing any medication, not just antimicrobials.
Choice C is wrong becauseGenetic heritage is wrong because genetic heritage is also a general factor that may affect the metabolism and excretion of medications, not the selection of antimicrobials.
Choice D is wrong becausePrevious medication reactions is wrong because previous medication reactions are also a general factor that may indicate allergies or intolerances to certain medications, not the selection of antimicrobials.
Normal ranges for immune function vary depending on the type and level of immunity measured, such as innate, adaptive, humoral or cellular immunity.Some common tests for immune function include complete blood count (CBC), immunoglobulin levels, complement levels, antibody titers and skin tests.
Normal ranges for these tests depend on the laboratory and the method used, but some examples are:
• CBC: white blood cell count 4.5-11 x 10^9/L; neutrophils 40-75%; lymphocytes 20-50%; monocytes 2-10%; eosinophils 1-6%; basophils 0-2%.
• Immunoglobulin levels: IgG 7-16 g/L; IgA 0.7-4 g/L; IgM 0.4-2.3 g/L; IgE 0-0.4 g/L.
• Complement levels: C3 0.9-1.8 g
The development of a new infection as a result of the elimination of normal flora by an antibiotic is referred to as what?
Explanation
A superinfection is defined as an infection that comes second to an initial infection and is often caused by the elimination of normal flora by an antibiotic.
Normal flora are the microorganisms that normally live in the human body and help prevent the growth of harmful pathogens.
When an antibiotic kills the normal flora, it creates an opportunity for other microorganisms to overgrow and cause a new infection.
Choice A is wrong because a resistant infection is an infection that does not respond to an antibiotic due to the presence of resistant bacteria.
Resistance can occur when bacteria mutate or acquire genes that make them able to survive the antibiotic.
Choice C is wrong because a nosocomial infection is an infection that is acquired in a hospital or health care setting.
Nosocomial infections can be caused by various factors, such as exposure to contaminated equipment, poor hygiene practices, or transmission from other patients or staff.
Choice D is wrong because an allergic reaction is an immune response to a foreign substance that is not harmful.
Allergic reactions can occur when a person is sensitive to an antibiotic or any other drug.
Symptoms of an allergic reaction may include rash, itching, swelling, or difficulty breathing.
(Select all that apply) A microbe acquires antibiotic resistance by which means?
Explanation
A microbe acquires antibiotic resistance by transferring DNA coding to other bacteria or by spontaneous mutation in the microbial genome.
These genetic changes allow the microbe to survive the effects of the antibiotic and pass on the resistance to its offspring.
ChoiceAis wrong because the host does not develop medication resistance, but the microbe does.
ChoiceBis wrong because the minimum bactericidal concentration (MBC) is the lowest concentration of an antibiotic needed to kill 99.9% of bacteria, not a mechanism of resistance.
ChoiceCis wrong because incorrect dosing does not cause ribosome mutations, but may promote the emergence of drug-resistant microbes by exposing them to suboptimal levels of the antibiotic.
Which statement is true regarding antimicrobial stewardship?
Explanation
Inappropriate antibiotic use leads to the emergence of resistance.This is a well-established fact that is supported by the CDC and other organizations.Resistance can occur when antibiotics are used unnecessarily, excessively, or incorrectly, and can lead to infections that are harder to treat and more costly.
Choice A is wrong because antibiotic guidelines in critical care do not necessarily reduce the hospital length of stay.Although some studies have suggested that adherence to pneumonia guidelines may improve outcomes in severe pneumonia, other studies have found no significant effect of antibiotic stewardship on hospital length of stay or mortality in critically ill patients.
Therefore, this statement is not universally true.
Choice C is wrong because antibiotic dosing has a significant effect on antimicrobial resistance.Optimal dosing of antibiotics can help eradicate infections, prevent relapse, and minimize the selection of resistant bacteria.Conversely, suboptimal dosing can lead to treatment failure, prolonged infection, and increased resistance.
Therefore, antibiotic dosing should be carefully adjusted according to the pharmacokinetic and pharmacodynamic properties of the drug and the patient.
Choice D is wrong because an antibiotic stewardship programme leads to a decrease in antimicrobial resistance, not an increase.An antibiotic stewardship programme is a coordinated effort to improve and measure the appropriate use of antibiotics by promoting the selection of the optimal drug regimen, dose, duration, and route of administration.Such programmes have been shown to reduce antibiotic consumption, resistance rates, adverse events, and costs in various settings.
Therefore, this statement is false.
Which antibiotics are classified as concentration-dependent antimicrobials?
Explanation
Gentamicin is an example of a concentration-dependent antimicrobial, which means that it achieves increasing bacterial kill with increasing levels of drug.The peak concentration and the area under the concentration curve (AUC) determine the efficacy of these antibiotics.Other examples of concentration-dependent antimicrobials include fluoroquinolones, daptomycin, aminoglycosides, and amphotericin
Choice A is wrong because ciprofloxacin is a fluoroquinolone, which is also a concentration-dependent antimicrobial.
Choice B is wrong because imipenem is a carbapenem, which is a type of beta-lactam antibiotic.Beta-lactams are time-dependent antimicrobials, which means that their bactericidal activity depends on the duration of the effective concentration.
Choice C is wrong because penicillin V is another type of beta-lactam antibiotic, which is also a time-dependent antimicrobial.
Choice D is wrong because metronidazole is a bactericidal agent that has both time- and concentration-dependent properties.However, it is not classified as a concentration-dependent antimicrobial according to the AMEG categorization of antibiotics in the European Union.
A nurse is preparing to administer vancomycin, a glycopeptide antibiotic, to a client with a severe infection caused by Clostridium difficile.
The nurse should select all that apply:
Explanation
Here is why:
• Choice A:Monitor the client’s serum creatinine level.
This is correct because vancomycin can cause nephrotoxicity (damage to the kidneys) and serum creatinine is a marker of kidney function.A high serum creatinine level indicates impaired kidney function and may require dose adjustment or discontinuation of vancomycin.
• Choice B:Monitor the client’s serum vancomycin level.
This is correct because vancomycin has a narrow therapeutic range, meaning that there is a small difference between the effective dose and the toxic dose.Monitoring the serum vancomycin level can help to ensure that the drug is within the therapeutic range and avoid toxicity or suboptimal efficacy.
• Choice C:Infuse the drug over at least 60 minutes.
This is correct because vancomycin can cause a hypersensitivity reaction called “red man syndrome” or “red neck syndrome”, which is characterized by flushing, itching, rash, hypotension and tachycardia.
This reaction is not an allergy but a result of histamine release due to rapid infusion of vancomycin.Infusing the drug over at least 60 minutes can reduce the risk of this reaction.
• Choice D:Observe the client for signs of ototoxicity.
This is incorrect because vancomycin is not known to cause ototoxicity (damage to the ears) in humans.Ototoxicity has been reported in animal studies and in vitro studies, but not in clinical trials or case reports involving humans.
Therefore, there is no need to monitor for signs of ototoxicity such as hearing loss, tinnitus or vertigo.
A patient has been prescribed azithromycin, a macrolide antibiotic, for a respiratory infection.
The nurse should instruct the patient to report which of the following signs or symptoms of a potential adverse effect?
Explanation
Azithromycin is a macrolide antibiotic that can cause a rare but serious side effect calledQT prolongation, which affects the electrical activity of the heart and can lead toirregular heartbeats, chest pain, and sudden cardiac death. The patient should report any signs of chest pain or palpitations to the doctor immediately.
Choice A is wrong because diarrhea is a common side effect of azithromycin that usually does not require medical attention unless it is severe or bloody.
Choice B is wrong because headache is also a common side effect of azithromycin that usually does not require medical attention unless it is severe or persistent.
Choice D is wrong because nausea is another common side effect of azithromycin that usually does not require medical attention unless it is severe or accompanied by vomiting.
A patient is receiving cefazolin, a first-generation cephalosporin, for a surgical prophylaxis.
The nurse should assess the patient for which of the following possible allergic reactions? (Select all that apply.)
Explanation
Cefazolin can cause serious or life-threatening allergic reactions in some patients, especially those with a history of penicillin allergy.The most common allergic reactions to cefazolin are immediate reactions, such as anaphylaxis, urticaria, bronchospasm, and angioedema.These reactions usually occur within one hour of the drug administration and may involve symptoms such as rash, itching, swelling, difficulty breathing, low blood pressure, and shock.Immediate reactions are mediated by immunoglobulin E (IgE) antibodies that bind to the drug and trigger the release of inflammatory mediators from mast cells and basophils.
Choice D is wrong because Stevens-Johnson syndrome is not a typical allergic reaction to cefazolin.
Stevens-Johnson syndrome is a rare and severe skin reaction that can be caused by various drugs, infections, or autoimmune diseases.
It involves blistering and peeling of the skin and mucous membranes, fever, malaise, and eye inflammation.
Stevens-Johnson syndrome is not mediated by IgE antibodies, but by other immune mechanisms that damage the skin cells.
Cefazolin is not known to cause Stevens-Johnson syndrome, although other cephalosporins have been reported to do so in rare cases.
A nurse is administering tetracycline, a broad-spectrum antibiotic, to a patient who has acne vulgaris.
The nurse should monitor the patient for which of the following adverse effects of this medication? (Select all that apply.)
Explanation
Tetracycline can causephotosensitivity, which means increased sensitivity to sunlight and risk of sunburn.It can also causesuperinfection, which means overgrowth of resistant bacteria or fungi in the mouth, intestines, or vagina.
Choice B is wrong because tetracycline can causetooth discolorationin children under 8 years old, not in adults.
Choice C is wrong because tetracycline can causehepatic impairmentonly in patients with preexisting liver disease or who take high doses for a long time.
Choice E is wrong because tetracycline can causebone marrow suppressiononly in patients with preexisting blood disorders or who take high doses for a long time.
A nurse is caring for a patient who is receiving gentamicin IV for treatment of endocarditis caused by gram-negative bacteria.
Which laboratory value should be monitored closely during gentamicin therapy?
Explanation
Gentamicin is an aminoglycoside antibiotic that can cause nephrotoxicity, which is damage to the kidneys.Serum creatinine is a measure of kidney function and should be monitored closely during gentamicin therapy. The normal range for serum creatinine is 0.6 to 1.2 mg/dL for men and 0.5 to 1.1 mg/dL for women.
Choice B is wrong because serum potassium is not affected by gentamicin.
The normal range for serum potassium is 3.5 to 5.0 mEq/L.
Choice C is wrong because serum calcium is not affected by gentamicin.
The normal range for serum calcium is 8.5 to 10.2 mg/dL.
Choice D is wrong because serum glucose is not affected by gentamicin.
The normal range for serum glucose is 70 to 110 mg/dL.
A nurse is reviewing the culture and sensitivity report of a patient who has a wound infection caused by Staphylococcus aureus.
The report indicates that the organism is sensitive to several antibiotics, including oxacillin, erythromycin, and clindamycin. Which antibiotic should be chosen for this patient? (Select all that apply.).
Explanation
Oxacillin, erythromycin and clindamycin are all antibiotics that are sensitive to Staphylococcus aureus according to the culture and sensitivity report.
This means that they can inhibit or kill the bacteria that are causing the wound infection.These antibiotics belong to different classes of drugs that have different mechanisms of action and spectrum of activity.
Choice D and E are wrong because vancomycin and linezolid are antibiotics that are usually reserved for more resistant strains of Staphylococcus aureus, such as methicillin-resistant Staphylococcus aureus (MRSA) or
Exams on Antibiotics and Antimicrobial Agents
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction
- Antimicrobial classifications
- Mechanisms of action
- Spectrum of activity
- Commonly prescribed antimicrobial agents
- Indications for use
- Adverse effects and toxicity
- Antimicrobial resistance
- Nursing implications and patient education
- Interactions and contraindications
- Conclusion
- More questions on this topic
- Summary
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Antimicrobial classifications: Understand the different classes of antimicrobial agents, including antibiotics, antivirals, antifungals, and antiparasitics.
- Mechanisms of action: Learn how different antimicrobial agents work to inhibit the growth or kill microorganisms, including their specific mechanisms of action against bacteria, viruses, fungi, or parasites.
- Spectrum of activity: Understand the range of microorganisms that are susceptible to specific antimicrobial agents, including broad-spectrum and narrow-spectrum agents.
- Commonly prescribed antimicrobial agents: Familiarize yourself with commonly used antimicrobial agents, such as penicillins, cephalosporins, antiretrovirals, antifungals, and antimalarials.
- Indications for use: Learn the appropriate indications for different antimicrobial agents, such as treating bacterial infections, viral infections, fungal infections, or parasitic infections.
- Pharmacokinetics: Understand the absorption, distribution, metabolism, and excretion (ADME) of antimicrobial agents, including factors that may affect their effectiveness or toxicity, such as food interactions or impaired renal or hepatic function.
- Adverse effects and toxicity: Be aware of the potential adverse effects and toxicities associated with specific antimicrobial agents, including allergic reactions, gastrointestinal disturbances, hepatotoxicity, nephrotoxicity, neurotoxicity, or bone marrow suppression.
- Antimicrobial resistance: Understand the concepts of antimicrobial resistance, including the mechanisms by which microorganisms become resistant to antimicrobial agents, the importance of proper antimicrobial stewardship, and strategies to prevent the development of resistance.
- Nursing implications and patient education: Be familiar with nursing responsibilities related to antimicrobial agent administration, such as assessing for allergies, monitoring for therapeutic effects, managing potential adverse effects, promoting adherence to the prescribed regimen, and educating patients about antimicrobial use, including the importance of completing the full course of treatment.
- Interactions and contraindications: Recognize potential drug interactions between antimicrobial agents and other medications, as well as contraindications for specific antimicrobial agents, such as pregnancy or known hypersensitivity.
Introduction
- Antimicrobial agents are substances that inhibit the growth or kill microorganisms, such as bacteria, viruses, fungi, or parasites
- Antimicrobial agents can be classified into different categories based on their chemical structure, mechanism of action, spectrum of activity, or target organism
- Some common classes of antimicrobial agents include antibiotics, antivirals, antifungals, and antiparasitics
- Antimicrobial agents are used to treat various types of infections caused by microorganisms, such as bacterial infections, viral infections, fungal infections, or parasitic infections
- Antimicrobial agents have different pharmacokinetic properties, such as absorption, distribution, metabolism, and excretion (ADME), that affect their effectiveness and toxicity
- Antimicrobial agents can cause adverse effects and toxicity in some patients, such as allergic reactions, gastrointestinal disturbances, hepatotoxicity, nephrotoxicity, neurotoxicity, or bone marrow suppression
- Antimicrobial resistance is a serious global health problem that occurs when microorganisms become resistant to antimicrobial agents due to genetic mutations or acquired mechanisms
- Antimicrobial stewardship is a strategy to optimize the use of antimicrobial agents to prevent the development and spread of resistance, improve patient outcomes, and reduce costs
- Nurses play a vital role in administering antimicrobial agents to patients, assessing for allergies, monitoring for therapeutic effects and adverse effects, promoting adherence to the prescribed regimen, educating patients about antimicrobial use, and preventing infection transmission
Antimicrobial classifications
Antibiotics
- Antibiotics are antimicrobial agents that are derived from living microorganisms, synthetic manufacturing, or genetic engineering. They are used to treat bacterial infections
- Antibiotics can be classified into different groups based on their chemical structure or mechanism of action. Some examples are:
|
Antibiotic group |
Examples |
Mechanism of action |
|
Aminoglycosides |
Amikacin (Amikin), gentamicin (Garamycin), kanamycin (Kantrex), neomycin (Mycifradin), streptomycin, tobramycin (TOBI, Tobrex) |
Bind to the 30S ribosomal subunit of bacteria and interfere with protein synthesis |
|
Carbapenems |
Doripenem (Doribax), ertapenem (Invanz), imipenem-cilastatin (Primaxin), meropenem (Merrem IV) |
Inhibit the synthesis of bacterial cell wall by binding to penicillin-binding proteins |
|
Cephalosporins |
Cefadroxil, cefazolin (Zolicef), cephalexin (Keflex), cefaclor (Ceclor), cefoxitin, cefprozil, cefuroxime (Zinacef), cefdinir, cefotaxime (Claforan), cefpodoxime (Vantin), ceftazidime (Ceptaz, Tazicef), ceftibuten (Cedax), ceftizoxime (Cefizox), ceftriaxone (Rocephin), cefditoren (Spectracef), cefepime (Maxipime), ceftaroline (Teflaro) |
Inhibit the synthesis of bacterial cell wall by binding to penicillin-binding proteins |
|
Fluoroquinolones |
Ciprofloxacin (Cipro), gemifloxacin (Factive), levofloxacin (Levaquin), moxifloxacin (Avelox), norfloxacin (Noroxin) |
Inhibit the activity of bacterial DNA gyrase and topoisomerase IV enzymes that are essential for DNA replication |
|
Penicillins and penicillinase-resistant antibiotics |
Amoxicillin (Amoxil), ampicillin (Omnipen), penicillin G (Pfizerpen), penicillin V (Veetids), dicloxacillin, nafcillin, oxacillin |
Inhibit the synthesis of bacterial cell wall by binding to penicillin-binding proteins |
|
Sulfonamides and trimethoprim |
Sulfamethoxazole-trimethoprim (Bactrim, Septra), sulfadiazine, sulfasalazine (Azulfidine) |
Inhibit the synthesis of folic acid, which is essential for bacterial DNA and RNA synthesis |
|
Tetracyclines |
Doxycycline (Doryx, Vibramycin), minocycline (Minocin), tetracycline (Sumycin) |
Bind to the 30S ribosomal subunit of bacteria and interfere with protein synthesis |
|
Macrolides |
Azithromycin (Zithromax), clarithromycin (Biaxin), erythromycin (Erythrocin) |
Bind to the 50S ribosomal subunit of bacteria and interfere with protein synthesis |
|
Lincosamides |
Clindamycin (Cleocin), lincomycin (Lincocin) |
Bind to the 50S ribosomal subunit of bacteria and interfere with protein synthesis |
|
Glycopeptides |
Vancomycin (Vancocin) |
Inhibit the synthesis of bacterial cell wall by binding to the D-alanyl-D-alanine terminus of peptidoglycan precursors |
|
Oxazolidinones |
Linezolid (Zyvox) |
Bind to the 50S ribosomal subunit of bacteria and interfere with protein synthesis |
|
Streptogramins |
Quinupristin-dalfopristin (Synercid) |
Bind to different sites on the 50S ribosomal subunit of bacteria and interfere with protein synthesis |
|
Lipopeptides |
Daptomycin (Cubicin) |
Insert into the bacterial cell membrane and cause depolarization and cell death |
Antivirals
- Antivirals are antimicrobial agents that are used to treat viral infections. They are usually specific for certain types of viruses.

- Antivirals can be classified into different groups based on their mechanism of action. Some examples are:
|
Antiviral group |
Examples |
Mechanism of action |
|
Nucleoside analogs |
Acyclovir (Zovirax), valacyclovir (Valtrex), famciclovir (Famvir), ganciclovir (Cytovene), valganciclovir (Valcyte) |
Inhibit viral DNA polymerase or reverse transcriptase enzymes that are essential for viral DNA or RNA synthesis |
|
Non-nucleoside reverse transcriptase inhibitors (NNRTIs) |
Efavirenz (Sustiva), nevirapine (Viramune), etravirine (Intelence), rilpivirine (Edurant) |
Bind to and inhibit viral reverse transcriptase enzyme that is essential for viral RNA synthesis |
|
Nucleotide reverse transcriptase inhibitors (NRTIs) |
Abacavir (Ziagen), didanosine (Videx), emtricitabine (Emtriva), lamivudine (Epivir), stavudine (Zerit), tenofovir disoproxil fumarate (Viread), zidovudine (Retrovir) |
Inhibit viral reverse transcriptase enzyme that is essential for viral RNA synthesis |
|
Protease inhibitors (PIs) |
Atazanavir (Reyataz), darunavir (Prezista), fosamprenavir (Lexiva), indinavir (Crixivan), lopinavir-ritonavir (Kaletra), nelfinavir (Viracept), ritonavir (Norvir), saquinavir (Invirase), tipranavir (Aptivus) |
Inhibit viral protease enzyme that is essential for viral protein maturation and assembly |
|
Integrase strand transfer inhibitors (INSTIs) |
Dolutegravir (Tivicay), elvitegravir (Vitekta), raltegravir (Isentress) |
Inhibit viral integrase enzyme that is essential for viral DNA integration into host cell genome |
|
Fusion inhibitors |
Enfuvirtide (Fuzeon) |
Prevent viral fusion with host cell membrane |
|
Entry inhibitors |
Maraviroc (Selzentry) |
Block viral entry by binding to host cell CCR5 co-receptor |
|
Neuraminidase inhibitors |
Oseltamivir (Tamiflu), zanamivir (Relenza) |
Inhibit viral neuraminidase enzyme that is essential for viral release from host cell |
|
Hepatitis C virus NS3/4A protease inhibitors |
Boceprevir (Victrelis), simeprevir (Olysio), telaprevir (Incivek) |
Inhibit viral NS3/4A protease enzyme that is essential for viral protein maturation and assembly |
|
Hepatitis C virus NS5A inhibitors |
Daclatasvir (Daklinza), ledipasvir, ombitasvir, velpatasvir |
Inhibit viral NS5A protein that is essential for viral replication and assembly |
|
Hepatitis C virus NS5B polymerase inhibitors |
Dasabuvir, sofosbuvir |
Inhibit viral NS5B polymerase enzyme that is essential for viral RNA synthesis |
Antifungals

- Antifungals are antimicrobial agents that are used to treat fungal infections. They can be classified into different groups based on their mechanism of action or target fungus. Some examples are:
|
Antifungal group |
Examples |
Mechanism of action |
|
Polyenes |
Amphotericin B, nystatin |
Bind to ergosterol in fungal cell membrane and cause leakage of cellular contents |
|
Azoles |
Fluconazole (Diflucan), itraconazole (Sporanox), ketoconazole, miconazole, voriconazole (Vfend) |
Inhibit the synthesis of ergosterol in fungal cell membrane by inhibiting the enzyme lanosterol 14-alpha-demethylase |
|
Echinocandins |
Anidulafungin (Eraxis), caspofungin (Cancidas), micafungin (Mycamine) |
Inhibit the synthesis of beta-glucan in fungal cell wall by inhibiting the enzyme beta-1,3-D-glucan synthase |
|
Allylamines and benzylamines |
Butenafine, naftifine, terbinafine (Lamisil) |
Inhibit the synthesis of ergosterol in fungal cell membrane by inhibiting the enzyme squalene epoxidase |
|
Pyrimidine analogs |
Flucytosine (Ancobon) |
Inhibit fungal DNA and RNA synthesis by interfering with the enzyme thymidylate synthetase |
Antiparasitic agents
- Antiparasitics are antimicrobial agents that are used to treat parasitic infections. They can be classified into different groups based on their mechanism of action or target parasites. Some examples are:
|
Antiparasitic group |
Examples |
Mechanism of action |
|
Antimalarials |
Chloroquine, hydroxychloroquine, mefloquine, primaquine, quinine, artemisinin derivatives, atovaquone-proguanil (Malarone) |
Interfere with various stages of the life cycle of Plasmodium parasites that cause malaria, such as heme polymerization, mitochondrial function, or DNA synthesis |
|
Antiprotozoals |
Metronidazole (Flagyl), tinidazole (Tindamax), nitazoxanide (Alinia), paromomycin, pentamidine, pyrimethamine-sulfadiazine, trimethoprim-sulfamethoxazole (Bactrim, Septra) |
Interfere with various metabolic pathways or cellular functions of protozoa, such as anaerobic respiration, DNA synthesis, or membrane integrity |
|
Anthelmintics |
Albendazole (Albenza), mebendazole (Vermox), ivermectin (Stromectol), praziquantel (Biltricide), pyrantel pamoate |
Interfere with various aspects of the nervous system or metabolism of helminths, such as neuromuscular transmission, glucose uptake, or calcium influx |
|
Ectoparasiticides |
Permethrin (Nix, Elimite), malathion (Ovide), lindane, benzyl benzoate, crotamiton (Eurax) |
Kill or repel ectoparasites, such as lice, scabies, or ticks, by affecting their nervous system or disrupting their cuticle |
Mechanisms of action
- Different antimicrobial agents have different mechanisms of action against microorganisms. Some common mechanisms are:

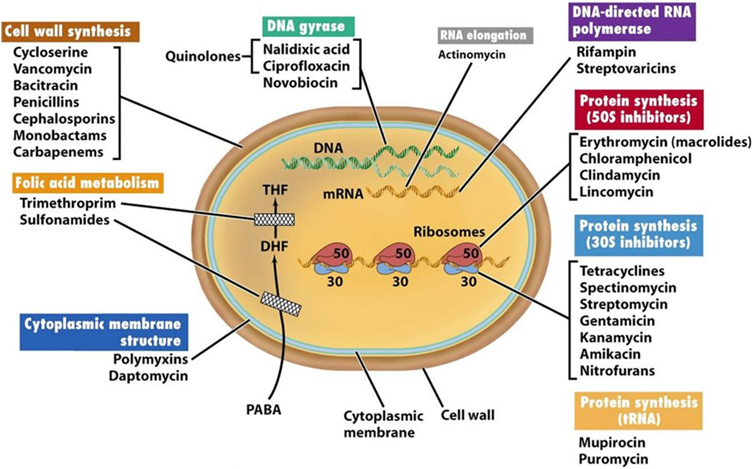
|
Mechanism of action |
Description |
Examples |
|
Inhibition of cell wall synthesis. |
Prevent the formation of peptidoglycan, a major component of the bacterial cell wall that provides strength and rigidity. This leads to cell lysis and death. |
Antibiotics that target penicillin-binding proteins, such as penicillins, cephalosporins, carbapenems, and monobactams; antibiotics that target D-alanyl-D-alanine residues, such as vancomycin and teicoplanin; antibiotics that target beta-1,3-D-glucan synthase, such as echinocandins |
|
Inhibition of protein synthesis |
Interfere with the function of ribosomes, the organelles that synthesize proteins in cells. This leads to impaired protein production and cell function. |
Antibiotics that bind to the 30S ribosomal subunit, such as aminoglycosides and tetracyclines; antibiotics that bind to the 50S ribosomal subunit, such as macrolides, lincosamides, chloramphenicol, and oxazolidinones; antibiotics that inhibit aminoacyl-tRNA binding to the ribosome, such as mupirocin and fusidic acid. |
|
Inhibition of nucleic acid synthesis. |
Interfere with the enzymes or substrates that are involved in the synthesis of DNA or RNA in cells. This leads to impaired replication and transcription of genetic material. |
Antibiotics that inhibit DNA gyrase and topoisomerase IV, such as fluoroquinolones; antibiotics that inhibit folic acid synthesis, such as sulfonamides and trimethoprim; antivirals that inhibit DNA polymerase or reverse transcriptase, such as nucleoside analogs and non-nucleoside analogs; antifungals that inhibit thymidylate synthetase, such as flucytosine |
|
Disruption of cell membrane function. |
Alter the permeability or integrity of the cell membrane of microorganisms. This leads to leakage of cellular contents and cell death. |
Antibiotics that bind to ergosterol in the fungal cell membrane, such as polyenes; antifungals that inhibit ergosterol synthesis in fungal cell membrane, such as azoles and allylamines; antivirals that prevent viral fusion with the host cell membrane, such as fusion inhibitors; antiparasitics that insert into the bacterial cell membrane and cause depolarization and cell death such as daptomycin and polymyxins |
|
Inhibition of metabolic pathways or cellular functions. |
Interfere with various biochemical processes or structures that are essential for the survival or growth of microorganisms. This leads to impaired cell function or death. |
Antiprotozoals that interfere with anaerobic respiration, such as metronidazole and tinidazole; antimalarials that interfere with heme polymerization, mitochondrial function, or DNA synthesis, such as chloroquine, mefloquine, primaquine, quinine, artemisinin derivatives, atovaquone-proguanil; anthelmintics that interfere with neuromuscular transmission, glucose uptake, or calcium influx, such as albendazole, mebendazole, ivermectin, praziquantel, pyrantel pamoate; ectoparasiticides that affect the nervous system or disrupt the cuticle of ectoparasites, such as permethrin, malathion, lindane, benzyl benzoate, crotamiton. |
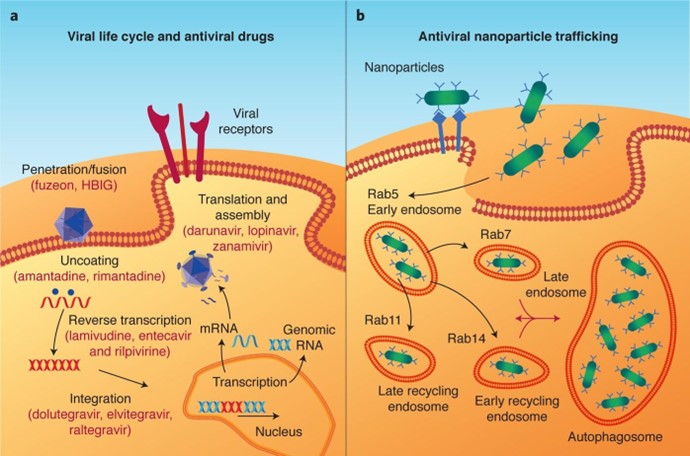
Spectrum of activity
- The spectrum of activity of an antimicrobial agent refers to the range of microorganisms that are susceptible to its action.
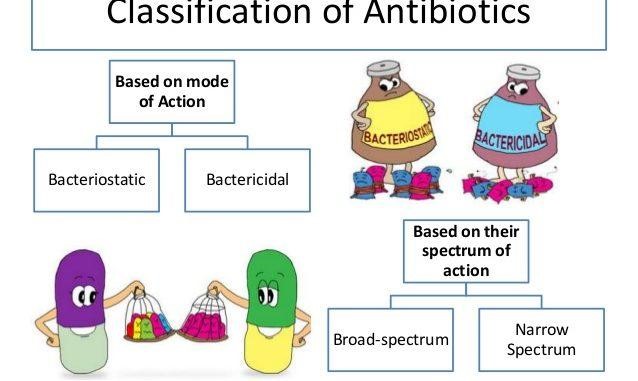
- Antimicrobial agents can have a broad-spectrum or a narrow-spectrum of activity.
- Broad-spectrum antimicrobial agents are effective against a wide variety of microorganisms, including both gram-positive and gram-negative bacteria. They are useful for treating infections caused by unknown or mixed microorganisms, or for preventing infections in immunocompromised patients. However, they may also kill normal flora and increase the risk of resistance.
- Narrow-spectrum antimicrobial agents are effective against a limited number of microorganisms, usually within a specific group or class. They are useful for treating infections caused by known or suspected microorganisms, or for minimizing the impact on normal flora and resistance. However, they may not cover all possible pathogens and require accurate identification and susceptibility testing.
- Some examples of broad-spectrum and narrow-spectrum antimicrobial agents are:
|
Antimicrobial agent |
Spectrum of activity |
|
Amoxicillin-clavulanate (Augmentin) |
Broad-spectrum antibiotic that covers many gram-positive and gram-negative bacteria, including some beta-lactamase producers |
|
Ciprofloxacin (Cipro) |
Broad-spectrum antibiotic that covers many gram-negative bacteria and some gram-positive bacteria |
|
Vancomycin (Vancocin) |
Narrow-spectrum antibiotic that covers only gram-positive bacteria |
|
Penicillin G (Pfizerpen) |
Narrow-spectrum antibiotic that covers mainly gram-positive bacteria and some gram-negative cocci |
|
Acyclovir (Zovirax) |
Narrow-spectrum antiviral that covers only herpes simplex virus (HSV) and varicella-zoster virus (VZV) |
|
Oseltamivir (Tamiflu) |
Narrow-spectrum antiviral that covers only influenza A and B viruses |
|
Fluconazole (Diflucan) |
Broad-spectrum antifungal that covers many yeasts and molds |
|
Amphotericin B |
Broad-spectrum antifungal that covers most fungi |
|
Metronidazole (Flagyl) |
Narrow-spectrum antiprotozoal that covers only anaerobic protozoa |
|
Chloroquine |
Narrow-spectrum antimalarial that covers only Plasmodium falciparum and Plasmodium vivax |
|
Albendazole (Albenza) |
Broad-spectrum anthelmintic that covers many nematodes and cestodes |
|
Praziquantel (Biltricide) |
Narrow-spectrum anthelmintic that covers only schistosomes and tapeworms |
|
Permethrin (Nix, Elimite) |
Broad-spectrum ectoparasiticide that covers many lice and scabies |
|
Benzyl benzoate |
Narrow-spectrum ectoparasiticide that covers only scabies |
Commonly prescribed antimicrobial agents
- Some commonly prescribed antimicrobial agents for different types of infections are:
|
Bacterial skin and soft tissue infections |
Cephalexin (Keflex), dicloxacillin, clindamycin (Cleocin), doxycycline (Vibramycin), trimethoprim-sulfamethoxazole (Bactrim, Septra), vancomycin (Vancocin) |
|
Bacterial respiratory tract infections |
Amoxicillin-clavulanate (Augmentin), azithromycin (Zithromax), cefdinir, ceftriaxone (Rocephin), clarithromycin (Biaxin), levofloxacin (Levaquin), moxifloxacin (Avelox) |
|
Bacterial urinary tract infections |
Nitrofurantoin (Macrobid), ciprofloxacin (Cipro), levofloxacin (Levaquin), trimethoprim-sulfamethoxazole (Bactrim, Septra) |
|
Bacterial gastrointestinal infections |
Metronidazole (Flagyl), ciprofloxacin (Cipro), levofloxacin (Levaquin), rifaximin (Xifaxan) |
|
Bacterial meningitis |
Ceftriaxone (Rocephin), cefotaxime (Claforan), vancomycin (Vancocin), ampicillin, meropenem (Merrem IV) |
|
Bacterial endocarditis |
Penicillin G (Pfizerpen), nafcillin, oxacillin, vancomycin (Vancocin), gentamicin (Garamycin), ceftriaxone (Rocephin) |
|
Bacterial sepsis |
Vancomycin (Vancocin), piperacillin-tazobactam (Zosyn), meropenem (Merrem IV), linezolid (Zyvox) |
|
Viral herpes infections |
Acyclovir (Zovirax), valacyclovir (Valtrex), famciclovir (Famvir) |
|
Viral influenza infections |
Oseltamivir (Tamiflu), zanamivir (Relenza) |
|
Viral hepatitis infections |
Pegylated interferon alfa, ribavirin, lamivudine (Epivir-HBV), adefovir dipivoxil (Hepsera), entecavir (Baraclude), telbivudine (Tyzeka), tenofovir disoproxil fumarate (Viread), boceprevir (Victrelis), simeprevir (Olysio), sofosbuvir (Sovaldi), ledipasvir-sofosbuvir (Harvoni), daclatasvir (Daklinza), ombitasvir-paritaprevir-ritonavir-dasabuvir (Viekira Pak) |
|
Viral human immunodeficiency virus (HIV) infections |
Combination antiretroviral therapy (cART) consisting of at least three antiviral agents from different classes, such as nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs), integrase strand transfer inhibitors (INSTIs), fusion inhibitors, entry inhibitors, or pharmacokinetic enhancers |
|
Fungal skin and nail infections |
Topical antifungals, such as clotrimazole, miconazole, ketoconazole, terbinafine, ciclopirox; oral antifungals, such as terbinafine, itraconazole, fluconazole |
|
Fungal oral and esophageal infections |
Nystatin, clotrimazole, fluconazole, itraconazole, voriconazole |
|
Fungal vaginal infections |
Clotrimazole, miconazole, terconazole, butoconazole, tioconazole; oral fluconazole |
|
Fungal systemic infections |
Amphotericin B, fluconazole, itraconazole, voriconazole, caspofungin, micafungin, anidulafungin |
|
Parasitic malaria infections |
Chloroquine, hydroxychloroquine, mefloquine, primaquine, quinine, artemisinin derivatives, atovaquone-proguanil |
|
Parasitic amoebiasis infections |
Metronidazole, tinidazole, paromomycin |
|
Parasitic giardiasis infections |
Metronidazole, tinidazole, nitazoxanide |
|
Parasitic trichomoniasis infections |
Metronidazole, tinidazole |
|
Parasitic toxoplasmosis infections |
Pyrimethamine-sulfadiazine, pyrimethamine-clindamycin, trimethoprim-sulfamethoxazole |
|
Parasitic leishmaniasis infections |
Sodium stibogluconate, amphotericin B, miltefosine, paromomycin |
|
Parasitic helminth infections |
Albendazole, mebendazole, ivermectin, praziquantel, pyrantel pamoate |
|
Parasitic ectoparasite infections |
Permethrin, malathion, lindane, benzyl benzoate, crotamiton |

Indications for use
- Different antimicrobial agents have different indications for use based on their spectrum of activity, efficacy, safety, and cost.
- The choice of antimicrobial agent depends on several factors, such as the type and severity of infection, the causative microorganism and its susceptibility, the patient’s medical history and allergies, the patient’s renal and hepatic function, the potential drug interactions and adverse effects, and the availability and affordability of the agent.
- Some general principles for selecting an appropriate antimicrobial agent are:
- Use culture and sensitivity testing to identify the causative microorganism and its susceptibility to various antimicrobial agents whenever possible.
- Use empiric therapy based on the most likely pathogens and local resistance patterns when culture and sensitivity testing is not available or delayed.
- Use narrow-spectrum antimicrobial agents when the causative microorganism is known or suspected to minimize the impact on normal flora and resistance.
- Use broad-spectrum antimicrobial agents when the causative microorganism is unknown or mixed, or when the infection is severe or life-threatening.
- Use combination therapy when there is a risk of resistance, when there is a synergistic effect between two or more agents, or when there is a need to cover multiple pathogens.
- Use monotherapy when there is no risk of resistance, when there is no synergistic effect between two or more agents, or when there is a need to avoid toxicity or interactions.
- Use the lowest effective dose and duration of therapy to achieve the desired therapeutic outcome and minimize the risk of adverse effects and resistance.
- Monitor the patient’s response to therapy by assessing clinical signs and symptoms, laboratory tests, and microbiological cultures.
- Adjust the therapy as needed based on the patient’s response, culture and sensitivity results, adverse effects, or drug interactions.
|
Antimicrobial agent |
Indications for use |
|
Amoxicillin-clavulanate (Augmentin) |
Bacterial skin and soft tissue infections, bacterial respiratory tract infections, bacterial urinary tract infections, bacterial otitis media, bacterial sinusitis |
|
Ciprofloxacin (Cipro) |
Bacterial urinary tract infections, bacterial gastrointestinal infections, bacterial prostatitis, bacterial anthrax, bacterial bone and joint infections |
|
Vancomycin (Vancocin) |
Bacterial endocarditis, bacterial meningitis, bacterial sepsis, bacterial pneumonia, bacterial osteomyelitis, bacterial skin and soft tissue infections caused by methicillin-resistant Staphylococcus aureus (MRSA) or other gram-positive bacteria |
|
Penicillin G (Pfizerpen) |
Bacterial endocarditis, bacterial meningitis, bacterial syphilis, bacterial streptococcal infections, bacterial tetanus |
|
Acyclovir (Zovirax) |
Viral herpes simplex virus (HSV) infections, viral varicella-zoster virus (VZV) infections |
|
Oseltamivir (Tamiflu) |
Viral influenza A and B infections |
|
Pegylated interferon alfa and ribavirin |
Viral hepatitis C infections |
|
Combination antiretroviral therapy (cART) |
Viral human immunodeficiency virus (HIV) infections |
|
Fluconazole (Diflucan) |
Fungal oral and esophageal infections, fungal vaginal infections, fungal systemic infections |
|
Amphotericin B |
Fungal systemic infections, fungal meningitis |
|
Metronidazole (Flagyl) |
Parasitic amoebiasis infections, parasitic giardiasis infections, parasitic trichomoniasis infections |
|
Chloroquine |
Parasitic malaria infections caused by Plasmodium falciparum and Plasmodium vivax |
|
Albendazole (Albenza) |
Parasitic helminth infections caused by nematodes and cestodes |
|
Permethrin (Nix, Elimite) |
Parasitic ectoparasite infections caused by lice and scabies |
Adverse effects and toxicity
- Antimicrobial agents can cause adverse effects and toxicity in some patients, which may limit their use or require dose adjustment or discontinuation.
- Some common adverse effects and toxicity of antimicrobial agents are:
|
Adverse effect or toxicity |
Description |
Examples |
|
Allergic reactions |
Hypersensitivity reactions occur when the immune system reacts to an antigen in the drug. They can range from mild to severe, such as rash, urticaria, angioedema, bronchospasm, anaphylaxis, or serum sickness. |
Penicillins, cephalosporins, sulfonamides, fluoroquinolones, vancomycin |
|
Gastrointestinal disturbances |
Irritation or inflammation of the gastrointestinal tract that causes symptoms such as nausea, vomiting, diarrhea, abdominal pain, or dyspepsia. They can be due to direct effects of the drug on the mucosa, alteration of normal flora, or superinfection by opportunistic pathogens. |
Antibiotics, especially broad-spectrum ones; antifungals; antiparasitics |
|
Hepatotoxicity |
Damage or injury to the liver cells that cause elevation of liver enzymes, such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), or bilirubin. It can be due to the direct effects of the drug on the hepatocytes, immune-mediated reactions, or metabolic idiosyncrasies. It can manifest as jaundice, hepatitis, cholestasis, or liver failure. |
Isoniazid (INH), rifampin (Rifadin), pyrazinamide (PZA), ethambutol (Myambutol), antiretrovirals, antifungals, antituberculars |
|
Nephrotoxicity |
Damage or injury to the kidney cells that cause elevation of serum creatinine or blood urea nitrogen (BUN), reduction of glomerular filtration rate (GFR), or alteration of urine output or composition. It can be due to direct effects of the drug on the nephrons, immune-mediated reactions, or obstruction of the urinary tract. It can manifest as acute kidney injury, chronic kidney disease, nephritis, or nephrotic syndrome. |
Aminoglycosides, vancomycin, amphotericin B, acyclovir, sulfonamides, antiretrovirals, antituberculars |
|
Neurotoxicity |
Damage or injury to the nervous system that causes symptoms such as headache, dizziness, confusion, seizures, peripheral neuropathy, or encephalopathy. It can be due to the direct effects of the drug on the neurons, accumulation of toxic metabolites, or interference with neurotransmission. It can manifest as central nervous system (CNS) toxicity or peripheral nervous system (PNS) toxicity. |
Isoniazid (INH), ethambutol (Myambutol), metronidazole (Flagyl), antiretrovirals, antifungals, antimalarials |
|
Bone marrow suppression |
Reduction or inhibition of the production of blood cells in the bone marrow that causes anemia, leukopenia, thrombocytopenia, or pancytopenia. It can be due to the direct effects of the drug on the hematopoietic stem cells, immune-mediated reactions, or interference with DNA synthesis. It can manifest as fatigue, weakness, pallor, infection, bleeding, or bruising. |
Chloramphenicol, trimethoprim-sulfamethoxazole (Bactrim, Septra), linezolid (Zyvox), antiretrovirals, antifungals, antituberculars |
|
Ototoxicity |
Damage or injury to the ear that causes hearing loss, tinnitus, vertigo, or balance problems. It can be due to the direct effects of the drug on the cochlea or vestibular apparatus in the inner ear, accumulation of toxic metabolites, or interference with blood flow. It can manifest as sensorineural hearing loss or vestibular dysfunction. |
Aminoglycosides, vancomycin, loop diuretics |
|
Photosensitivity |
Increased sensitivity to sunlight that causes skin reactions such as rash, erythema, pruritus, or blistering. It can be due to the direct effects of the drug on the skin, activation of photosensitizing agents by ultraviolet (UV) light, or immune-mediated reactions. It can manifest as phototoxicity or photoallergy. |
Tetracyclines, sulfonamides, fluoroquinolones, antifungals, antimalarials |
|
Disulfiram-like reaction |
A syndrome of flushing, headache, nausea, vomiting, palpitations, hypotension, or tachycardia that occurs when alcohol is consumed while taking certain drugs. It can be due to inhibition of the enzyme aldehyde dehydrogenase by the drug, which causes the accumulation of acetaldehyde in the blood. It can manifest as an unpleasant or dangerous reaction. |
Metronidazole (Flagyl), tinidazole (Tindamax), cephalosporins, antabuse |
|
Superinfection |
A secondary infection that occurs when the normal flora is disrupted by antimicrobial therapy, allowing opportunistic pathogens to overgrow and cause infection. It can affect various sites in the body, such as the oral cavity, the gastrointestinal tract, the vagina, or the skin. It can manifest as oral thrush, pseudomembranous colitis, vaginal candidiasis, or impetigo. |
Antibiotics, especially broad-spectrum ones; antifungals; antivirals |
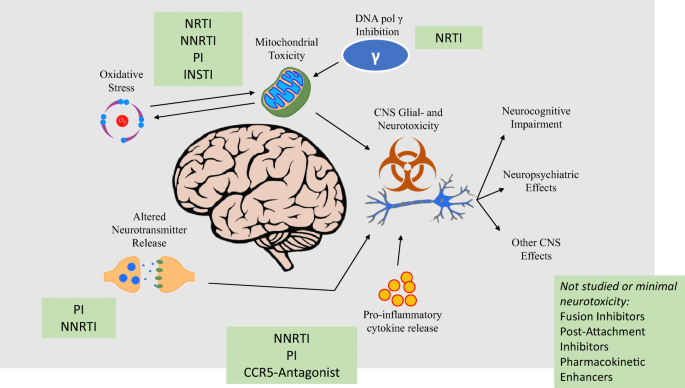

Antimicrobial resistance
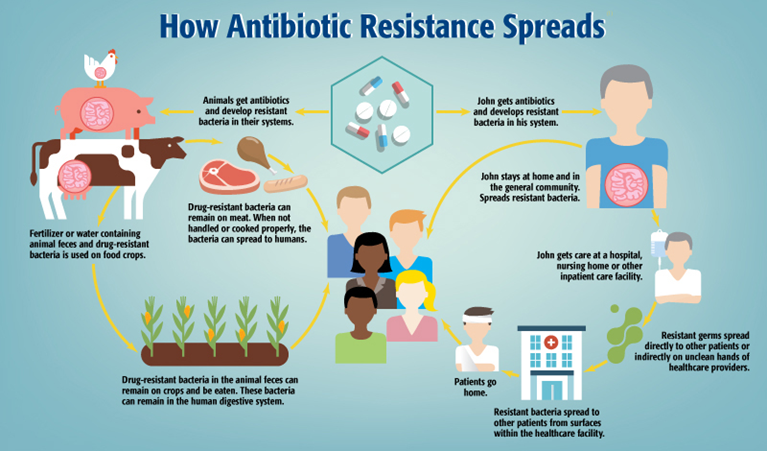
- Antimicrobial resistance is the ability of microorganisms to survive or grow in the presence of antimicrobial agents that would normally inhibit or kill them.
- Antimicrobial resistance is a serious global health problem that threatens the effectiveness of existing antimicrobial agents and increases the risk of morbidity and mortality from infections.
- Antimicrobial resistance can be intrinsic or acquired. Intrinsic resistance is the natural resistance of certain microorganisms to certain antimicrobial agents due to their inherent characteristics, such as lack of cell wall or target site. Acquired resistance is the resistance that develops in previously susceptible microorganisms due to genetic mutations or acquired mechanisms.
- Some common mechanisms of acquired resistance are:
- Enzymatic degradation or modification: The microorganism produces enzymes that degrade or modify the antimicrobial agent and render it inactive. For example, beta-lactamases are enzymes that hydrolyze beta-lactam antibiotics, such as penicillins and cephalosporins.
- Altered target site: The microorganism alters the structure or expression of the target site of the antimicrobial agent and reduces its affinity or binding. For example, methicillin-resistant Staphylococcus aureus (MRSA) has an altered penicillin-binding protein (PBP2a) that has a low affinity for beta-lactam antibiotics.
- Reduced permeability or increased efflux: The microorganism reduces the entry of the antimicrobial agent into the cell or increases its exit from the cell by altering the permeability or expression of membrane channels or pumps. For example, Pseudomonas aeruginosa has an outer membrane that limits the penetration of many antibiotics and efflux pumps that expel them from the cell.
- Bypassed metabolic pathway: The microorganism develops an alternative metabolic pathway that bypasses the inhibited step by the antimicrobial agent. For example, some bacteria can synthesize folic acid from exogenous sources instead of using their own pathway that is inhibited by sulfonamides and trimethoprim.
- Overproduction of target site: The microorganism overproduces the target site of the antimicrobial agent and saturates its binding capacity. For example, some bacteria can produce excess amounts of dihydrofolate reductase (DHFR) that is inhibited by trimethoprim.
- Acquisition of resistant genes: The microorganism acquires genes that confer resistance to the antimicrobial agent from other microorganisms by horizontal gene transfer mechanisms, such as plasmids, transposons, or bacteriophages. For example, some bacteria can acquire genes that encode for extended-spectrum beta-lactamases (ESBLs) or carbapenemases that confer resistance to a wide range of beta-lactam antibiotics.
- Antimicrobial resistance can be influenced by various factors, such as:
- Inappropriate use of antimicrobial agents: The misuse or overuse of antimicrobial agents, such as prescribing them for viral infections, using broad-spectrum agents when narrow-spectrum agents are sufficient, using suboptimal doses or durations, or not completing the full course of treatment, can increase the selective pressure and favor the survival and growth of resistant microorganisms.
- Lack of infection control measures: The poor implementation of infection control measures, such as hand hygiene, personal protective equipment, isolation precautions, sterilization, and disinfection, or waste management, can increase the transmission and spread of resistant microorganisms among patients, healthcare workers, and the environment.
- Lack of surveillance and reporting: The inadequate monitoring and reporting of antimicrobial resistance patterns and trends can limit the availability and accuracy of data to guide clinical decision-making and policy-making.
- Lack of research and development: The insufficient investment and innovation in developing new antimicrobial agents or alternative strategies to combat resistant microorganisms can limit the options and solutions to address the problem.
- Antimicrobial stewardship is a strategy to optimize the use of antimicrobial agents to prevent the development and spread of resistance, improve patient outcomes, and reduce costs.
- Antimicrobial stewardship involves various interventions and activities, such as:
- Developing and implementing evidence-based guidelines and protocols for antimicrobial prescribing and administration based on local resistance patterns and best practices.
- Educating and training health care providers and patients on the appropriate use of antimicrobial agents and the prevention of infections.
- Performing culture and sensitivity testing before initiating empiric therapy and adjusting therapy based on the results.
- Reviewing and de-escalating antimicrobial therapy based on clinical response, microbiological data, or adverse effects.
- Monitoring and evaluating the outcomes and impact of antimicrobial therapy on patient safety, quality of care, resistance patterns, and costs.
- Collaborating and communicating with multidisciplinary teams, including infectious disease specialists, pharmacists, microbiologists, infection control practitioners, and public health authorities.
Nursing implications and patient education
- Nurses play a vital role in administering antimicrobial agents to patients, assessing for allergies, monitoring for therapeutic effects and adverse effects, promoting adherence to the prescribed regimen, educating patients about antimicrobial use, and preventing infection transmission.
- Some nursing implications and patient education related to antimicrobial agent administration are:
- Assess the patient’s medical history, allergies, vital signs, laboratory tests, and culture and sensitivity results before initiating antimicrobial therapy.
- Administer the antimicrobial agent as prescribed by the route, dose, frequency, and duration indicated. Follow the manufacturer’s instructions for reconstitution, dilution, storage, and stability of the agent. Use aseptic technique and proper equipment for administration.
- Monitor the patient’s response to therapy by assessing clinical signs and symptoms, laboratory tests, and microbiological cultures. Report any changes or abnormalities to the prescriber.
- Monitor the patient for potential adverse effects and toxicity of the antimicrobial agent. Report any signs or symptoms of allergic reactions, gastrointestinal disturbances, hepatotoxicity, nephrotoxicity, neurotoxicity, bone marrow suppression, ototoxicity, photosensitivity, disulfiram-like reaction, or superinfection to the prescriber. Manage the adverse effects as ordered or as per protocol.
- Educate the patient about the purpose, benefits, and risks of antimicrobial therapy. Explain the mode of action, spectrum of activity, pharmacokinetics, adverse effects, and toxicity of the antimicrobial agent. Provide written information or instructions if available.
- Educate the patient about the importance of completing the full course of treatment as prescribed, even if symptoms improve or resolve. Explain the consequences of non-adherence, such as treatment failure, relapse, resistance, or adverse effects.
- Educate the patient about how to take the antimicrobial agent correctly and safely. Instruct the patient on how to measure or administer the dose accurately, how to store or dispose of the agent properly, and how to avoid or manage potential food or drug interactions. Provide examples of foods or drugs that may interact with the antimicrobial agent and advise the patient to consult the prescriber or pharmacist before taking any new medications, supplements, or herbal products.
- Educate the patient about how to prevent or reduce the risk of infection transmission. Instruct the patient on how to practice good hygiene, such as washing hands frequently, covering coughs and sneezes, and disposing of tissues properly. Advise the patient to avoid contact with people who are sick or have infections, and to seek medical attention if they develop signs or symptoms of infection. Inform the patient about any isolation precautions or infection control measures that are required during their treatment or hospitalization.
- Educate the patient about how to recognize and report any signs or symptoms of complications or adverse effects of antimicrobial therapy. Instruct the patient on how to monitor their temperature, pulse, blood pressure, urine output, weight, and blood glucose levels if indicated. Provide a list of signs or symptoms that require immediate medical attention, such as rash, hives, swelling, difficulty breathing, chest pain, palpitations, severe headache, confusion, seizures, hearing loss, tinnitus, vertigo, jaundice, dark urine, clay-colored stools, abdominal pain, nausea, vomiting, diarrhea, bleeding, bruising, or fever. Encourage the patient to contact the prescriber or pharmacist if they have any questions or concerns about their treatment.
Interactions and contraindications
- Antimicrobial agents can interact with other medications or substances and cause additive, synergistic, or antagonistic effects. These interactions can affect the pharmacokinetics or pharmacodynamics of the antimicrobial agent or the other medication or substance and result in increased or decreased efficacy or toxicity.
- Some common interactions of antimicrobial agents are:
|
Antimicrobial agent |
Interacting medication or substance |
Effect of interaction |
|
Penicillins |
Probenecid |
Increased serum levels and half-life of penicillins due to decreased renal excretion |
|
Cephalosporins |
Warfarin |
Increased risk of bleeding due to decreased vitamin K synthesis by normal flora |
|
Fluoroquinolones |
Antacids, iron supplements, calcium supplements |
Decreased absorption and bioavailability of fluoroquinolones due to chelation |
|
Tetracyclines |
Antacids, iron supplements, calcium supplements |
Decreased absorption and bioavailability of tetracyclines due to chelation |
|
Macrolides |
Theophylline, warfarin, carbamazepine |
Increased serum levels and toxicity of these drugs due to inhibition of cytochrome P450 enzymes by macrolides |
|
Sulfonamides |
Warfarin, phenytoin |
Increased serum levels and toxicity of these drugs due to displacement from plasma proteins by sulfonamides |
|
Trimethoprim |
Methotrexate |
Increased risk of bone marrow suppression due to additive inhibition of folic acid synthesis |
|
Aminoglycosides |
Loop diuretics |
Increased risk of ototoxicity and nephrotoxicity due to additive effects on the ear and kidney |
|
Vancomycin |
Loop diuretics, aminoglycosides, amphotericin B |
Increased risk of ototoxicity and nephrotoxicity due to additive effects on the ear and kidney |
|
Antiretrovirals |
Many drugs that are metabolized by cytochrome P450 enzymes, such as anticonvulsants, antidepressants, antifungals, antibiotics, anticoagulants, statins, oral contraceptives |
Increased or decreased serum levels and efficacy or toxicity of these drugs due to induction or inhibition of cytochrome P450 enzymes by antiretrovirals |
|
Antifungals |
Many drugs that are metabolized by cytochrome P450 enzymes, such as anticonvulsants, antidepressants, antibiotics, anticoagulants, statins, oral contraceptives |
Increased or decreased serum levels and efficacy or toxicity of these drugs due to inhibition of cytochrome P450 enzymes by antifungals |
|
Antimalarials |
Antacids, kaolin-pectin, cimetidine |
Decreased absorption and bioavailability of antimalarials due to chelation or increased gastric pH |
|
Antiprotozoals |
Alcohol, disulfiram |
Increased risk of disulfiram-like reaction due to inhibition of aldehyde dehydrogenase by antiprotozoals |
|
Anthelmintics |
Carbamazepine, phenytoin |
Decreased serum levels and efficacy of anthelmintics due to induction of cytochrome P450 enzymes by these drugs |
- Antimicrobial agents can have contraindications for use in certain patients or situations. These contraindications can be absolute or relative. Absolute contraindications are conditions that preclude the use of an antimicrobial agent because of a high risk of serious harm or death. Relative contraindications are conditions that require caution or dose adjustment when using an antimicrobial agent because of a moderate risk of harm or reduced efficacy.
- Some common contraindications of antimicrobial agents are:
|
Antimicrobial agent |
Contraindication |
Reason |
|
Penicillins |
History of severe allergic reaction (anaphylaxis) to penicillins or cephalosporins |
Cross-reactivity and risk of life-threatening hypersensitivity reaction |
|
Cephalosporins |
History of severe allergic reaction (anaphylaxis) to penicillins or cephalosporins |
Cross-reactivity and risk of life-threatening hypersensitivity reaction |
|
Fluoroquinolones |
Pregnancy, lactation, children under 18 years old |
Potential adverse effects on cartilage development and growth in fetuses and children |
|
Tetracyclines |
Pregnancy, lactation, children under 8 years old |
Potential adverse effects on bone and teeth development and staining in fetuses and children |
|
Macrolides |
History of QT prolongation, ventricular arrhythmias, or concurrent use of drugs that prolong QT interval |
Potential risk of cardiac arrhythmias due to QT prolongation by macrolides |
|
Sulfonamides |
History of severe allergic reaction (anaphylaxis, Stevens-Johnson syndrome, toxic epidermal necrolysis) to sulfonamides or sulfa-containing drugs |
Cross-reactivity and risk of life-threatening hypersensitivity reaction |
|
Trimethoprim |
Pregnancy, lactation, folate deficiency, megaloblastic anemia |
Potential adverse effects on fetal development and hematopoiesis due to inhibition of folic acid synthesis |
|
Aminoglycosides |
History of hearing loss, vestibular dysfunction, or renal impairment |
Potential risk of ototoxicity and nephrotoxicity due to accumulation of aminoglycosides in the ear and kidney |
|
Vancomycin |
History of hearing loss, vestibular dysfunction, or renal impairment |
Potential risk of ototoxicity and nephrotoxicity due to accumulation of vancomycin in the ear and kidney |
|
Antiretrovirals |
History of severe hypersensitivity reaction to any component of the antiretroviral regimen |
Risk of recurrence or worsening of hypersensitivity reaction |
|
Antifungals |
History of liver disease or impairment |
Potential risk of hepatotoxicity due to metabolism of antifungals in the liver |
|
Antimalarials |
History of retinal damage or impairment, psoriasis, porphyria, or glucose-6-phosphate dehydrogenase (G6PD) deficiency |
Potential risk of ocular toxicity, skin reactions, hemolysis, or methemoglobinemia due to effects of antimalarials on these organs or systems |
|
Antiprotozoals |
History of blood dyscrasias or neurological disorders |
Potential risk of bone marrow suppression or neurotoxicity due to effects of antiprotozoals on these systems |
|
Anthelmintics |
History of ocular or CNS cysticercosis caused by Taenia solium (pork tapeworm) |
Potential risk of inflammatory reactions or increased intracranial pressure due to death of the parasite in these sites |
|
Ectoparasiticides |
History of asthma, seizures, or skin irritation |
Potential risk of bronchospasm, convulsions, or dermatitis due to effects of ectoparasiticides on these systems |
Conclusion
- Antimicrobial agents are substances that inhibit the growth or kill microorganisms, such as bacteria, viruses, fungi, or parasites.
- Antimicrobial agents can be classified into different categories based on their chemical structure, mechanism of action, spectrum of activity, or target organism.
- Antimicrobial agents are used to treat various types of infections caused by microorganisms. The choice of antimicrobial agent depends on several factors, such as the type and severity
- Antimicrobial agents are substances that inhibit the growth or kill microorganisms, such as bacteria, viruses, fungi, or parasites.
- Antimicrobial agents can be classified into different categories based on their chemical structure, mechanism of action, spectrum of activity, or target organism.
- Antimicrobial agents are used to treat various types of infections caused by microorganisms. The choice of antimicrobial agent depends on several factors, such as the type and severity of infection, the causative microorganism and its susceptibility, the patient’s medical history and allergies, the patient’s renal and hepatic function, the potential drug interactions and adverse effects, and the availability and affordability of the agent.
- Antimicrobial agents have different pharmacokinetic properties, such as absorption, distribution, metabolism, and excretion (ADME), that affect their effectiveness and toxicity.
- Antimicrobial agents can cause adverse effects and toxicity in some patients, such as allergic reactions, gastrointestinal disturbances, hepatotoxicity, nephrotoxicity, neurotoxicity, bone marrow suppression, ototoxicity, photosensitivity, disulfiram-like reaction, or superinfection.
- Antimicrobial resistance is the ability of microorganisms to survive or grow in the presence of antimicrobial agents that would normally inhibit or kill them. Antimicrobial resistance is a serious global health problem that threatens the effectiveness of existing antimicrobial agents and increases the risk of morbidity and mortality from infections.
- Antimicrobial stewardship is a strategy to optimize the use of antimicrobial agents to prevent the development and spread of resistance, improve patient outcomes, and reduce costs.
- Nurses play a vital role in administering antimicrobial agents to patients, assessing for allergies, monitoring for therapeutic effects and adverse effects, promoting adherence to the prescribed regimen, educating patients about antimicrobial use, and preventing infection transmission.
- Antimicrobial agents can interact with other medications or substances and cause additive, synergistic, or antagonistic effects. These interactions can affect the pharmacokinetics or pharmacodynamics of the antimicrobial agent or the other medication or substance and result in increased or decreased efficacy or toxicity.
- Antimicrobial agents can have contraindications for use in certain patients or situations. These contraindications can be absolute or relative. Absolute contraindications are conditions that preclude the use of an antimicrobial agent because of a high risk of serious harm or death. Relative contraindications are conditions that require caution or dose adjustment when using an antimicrobial agent because of a moderate risk of harm or reduced efficacy.
Summary
- The main points of this topic are:
- Antimicrobial agents are substances that inhibit the growth or kill microorganisms.
- Antimicrobial agents can be classified into different categories based on their chemical structure, mechanism of action, spectrum of activity, or target organism.
- Antimicrobial agents are used to treat various types of infections caused by microorganisms.
- Antimicrobial agents have different pharmacokinetic properties that affect their effectiveness and toxicity.
- Antimicrobial agents can cause adverse effects and toxicity in some patients.
- Antimicrobial resistance is a serious global health problem that threatens the effectiveness of existing antimicrobial agents.
- Antimicrobial stewardship is a strategy to optimize the use of antimicrobial agents to prevent resistance, improve outcomes, and reduce costs.
- Nurses play a vital role in administering antimicrobial agents to patients, assessing for allergies
- Nurses play a vital role in administering antimicrobial agents to patients, assessing for allergies, monitoring for therapeutic effects and adverse effects, promoting adherence to the prescribed regimen, educating patients about antimicrobial use, and preventing infection transmission.
- Antimicrobial agents can interact with other medications or substances and cause additive, synergistic, or antagonistic effects. These interactions can affect the pharmacokinetics or pharmacodynamics of the antimicrobial agent or the other medication or substance and result in increased or decreased efficacy or toxicity.
- Antimicrobial agents can have contraindications for use in certain patients or situations. These contraindications can be absolute or relative. Absolute contraindications are conditions that preclude the use of an antimicrobial agent because of a high risk of serious harm or death. Relative contraindications are conditions that require caution or dose adjustment when using an antimicrobial agent because of a moderate risk of harm or reduced efficacy.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Antibiotics and Antimicrobial Agents
This filled cannot be empty

