Please set your exam date
Mood Disorders and Suicide
Study Questions
Major depressive disorder (MDD)
Explanation
Choice A rationale:
MDD is actually more prevalent in younger adults, with the average age of onset being in the mid-20s to early 30s. The disorder can, however, occur at any age.
Choice B rationale:
MDD is a complex disorder influenced by a combination of genetic, environmental, and psychological factors. While genetics can play a role, it is not primarily caused by a single factor.
Choice C rationale:
Anhedonia is a term used to describe the diminished ability to experience pleasure or interest in previously enjoyed activities, which is a key characteristic of major depressive disorder. This symptom can significantly impact a person's quality of life and is one of the diagnostic criteria for MDD.
Choice D rationale:
For a diagnosis of MDD, a person must experience a persistent low mood or anhedonia (loss of interest or pleasure) along with other symptoms such as changes in appetite or weight, sleep disturbances, fatigue, feelings of worthlessness or guilt, difficulty concentrating, and in severe cases, thoughts of death or suicide. It's not sufficient to diagnose MDD based on just one symptom.
Explanation
Choice A rationale:
Increased interest in activities is not consistent with the clinical presentation of MDD. In fact, a hallmark symptom of MDD is anhedonia, which involves a reduced interest or pleasure in most activities.
Choice B rationale:
Weight gain is not typically associated with MDD. In contrast, significant changes in appetite and weight loss are more common symptoms, often accompanied by feelings of worthlessness or guilt related to body image.
Choice C rationale:
Excessive guilt and self-blame are common cognitive and emotional symptoms of MDD. Individuals with MDD tend to have a negative self-perception and may blame themselves for their difficulties.
Choice D rationale:
Insomnia, or difficulty falling asleep or staying asleep, is a common sleep disturbance associated with MDD. Sleep problems can exacerbate the symptoms of depression and impact overall well-being.
Choice E rationale:
Elevated mood and increased energy are actually more indicative of conditions like bipolar disorder or manic episodes, where there are distinct periods of abnormally elevated mood, known as mania or hypomania.
Explanation
Choice A rationale:
A manic episode is characterized by a distinct period of abnormally elevated, expansive, or irritable mood, often accompanied by increased energy, decreased need for sleep, and impulsive behavior. The client's description does not align with a manic episode.
Choice B rationale:
Bipolar disorder involves cycling between periods of mania or hypomania and depression. The client's statement does not provide evidence of mood cycling, which is characteristic of bipolar disorder.
Choice C rationale:
The client's statement directly describes anhedonia, which is a key characteristic of major depressive disorder (MDD). Anhedonia involves the inability to derive pleasure from activities that were previously enjoyable, and it is a central diagnostic criterion for MDD.
Choice D rationale:
Adjustment disorder is a condition characterized by emotional or behavioral symptoms that develop in response to a specific stressor. The client's statement is more indicative of a pervasive and ongoing lack of enjoyment, which aligns with the concept of anhedonia in MDD rather than the time-limited nature of adjustment disorder.
Explanation
Choice A rationale:
Signs of normal bereavement. Bereavement refers to the period of grief and mourning after the loss of a loved one. While fatigue and feelings of worthlessness can be experienced during bereavement, difficulty concentrating is not a typical sign. Additionally, bereavement-related symptoms typically improve over time as the individual processes their loss. The combination of extreme fatigue, difficulty concentrating, and thoughts of worthlessness suggests a more severe and persistent condition than normal bereavement.
Choice B rationale:
Symptoms of bipolar disorder. Bipolar disorder is characterized by alternating episodes of depression and mania (or hypomania). The client's symptoms of extreme fatigue, difficulty concentrating, and thoughts of worthlessness are primarily indicative of a depressive episode, which is only one aspect of bipolar disorder. Bipolar disorder requires the presence of manic or hypomanic episodes, which are not mentioned in the client's presentation.
Choice C rationale:
Indicators of substance-induced mood disorder. Substance-induced mood disorder occurs as a result of substance use or withdrawal and involves changes in mood and affect. While substances can lead to symptoms similar to depression, the combination of symptoms presented by the client (fatigue, difficulty concentrating, thoughts of worthlessness) is more indicative of a primary mood disorder rather than one directly caused by substance use.
Choice D rationale:
Criteria for diagnosing MDD according to DSM-5. The client's symptoms of extreme fatigue, difficulty concentrating, and thoughts of worthlessness align with the criteria for Major Depressive Disorder (MDD) as defined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). These criteria include the presence of specific symptoms for a specified duration, causing significant impairment in functioning. The symptoms should not be better explained by other conditions or substances. In this case, the client's presentation closely matches the criteria for diagnosing MDD.
Explanation
Choice A rationale:
"MDD is less severe than dysthymia but lasts for at least 2 years." This statement is incorrect. Major Depressive Disorder (MDD) is characterized by the presence of a major depressive episode, which can be severe and persistent, lasting for at least two weeks. Dysthymia, on the other hand, is a chronic but milder form of depression that lasts for at least two years, not MDD.
Choice B rationale:
"Dysthymia is characterized by alternating episodes of mania and depression." This statement is incorrect. Dysthymia is a chronic mood disorder characterized by a persistent low mood and other depressive symptoms. It does not involve alternating episodes of mania and depression. Alternating episodes of mania and depression are characteristic of bipolar disorder, not dysthymia.
Choice C rationale:
"Unlike MDD, dysthymia does not impair social or occupational functioning." This statement is incorrect. Both Major Depressive Disorder (MDD) and dysthymia can significantly impair social, occupational, and other areas of functioning. In fact, dysthymia's chronic nature often leads to long-term impairment in various aspects of an individual's life, similar to MDD.
Choice D rationale:
"Dysthymia is chronic and lasts for at least 2 years, but is less severe than MDD." This statement is accurate. Dysthymia is a chronic form of depression that persists for at least two years. While it may not exhibit the same level of severity as a major depressive episode, its long-term nature can still have a substantial impact on an individual's quality of life. This distinguishes it from MDD, which can have episodic occurrences.
Explanation
Choice A rationale:
Patient Health naire (PHQ-9). The PHQ-9 is a commonly used depression assessment tool that evaluates a patient's mood and depressive symptoms. It consists of nine questions that correspond to the nine criteria for diagnosing major depressive disorder (MDD) according to the DSM-5. The tool assesses various aspects of depression, such as mood, sleep disturbances, appetite changes, and more. It's a self-report questionnaire that helps clinicians assess the severity of a patient's depression and track their progress over time.
Choice B rationale:
Hamilton Depression Rating Scale (HAM-D). The Hamilton Depression Rating Scale (HAM-D) is another widely used tool for assessing the severity of depressive symptoms in patients with mood disorders. It contains multiple items that evaluate various aspects of depression, such as mood, feelings of guilt, suicidal ideation, and more. Unlike the PHQ-9, the HAM-D is typically administered by a trained clinician and is more extensive, making it suitable for clinical research and diagnosis but potentially less practical for routine screening.
Choice C rationale:
Beck Depression Inventory (BDI). The Beck Depression Inventory (BDI) is a self-report questionnaire designed to assess the presence and severity of depressive symptoms in individuals. It consists of 21 multiple-choice questions that cover various emotional, cognitive, and physical symptoms of depression. The BDI is useful for assessing the intensity of depression and changes in symptom severity over time. While a valuable tool, it's not the assessment tool most likely used in this scenario.
Choice D rationale:
Mini-Mental State Examination (MMSE). The Mini-Mental State Examination (MMSE) is not an appropriate tool for assessing depression. Instead, it's a brief cognitive screening test used to assess cognitive impairment and cognitive decline in individuals, especially in older adults. It evaluates aspects such as orientation, memory, attention, language, and visuospatial skills. It is not designed to assess mood, anxiety, or other emotional aspects related to depression.
Explanation
Choice A rationale:
Bipolar disorder involves distinct periods of both elevated mood (mania or hypomania) and depressive episodes. The scenario describes persistent feelings of sadness, guilt, worthlessness, weight loss, and insomnia, which are characteristic symptoms of major depressive disorder (MDD) but not necessarily indicative of bipolar disorder.
Choice B rationale:
An adjustment disorder is characterized by emotional or behavioral symptoms that arise within three months of experiencing a stressor (e.g., a major life change or event). The persistent feelings of sadness, guilt, worthlessness, weight loss, and insomnia described in the scenario are beyond the typical time frame for an adjustment disorder.
Choice C rationale:
The correct answer. Major depressive disorder (MDD) is characterized by persistent feelings of sadness, loss of interest or pleasure, changes in weight or appetite, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue, feelings of worthlessness or excessive guilt, difficulty concentrating, and recurrent thoughts of death or suicide. The client's symptoms align closely with the diagnostic criteria for MDD.
Choice D rationale:
A normal response to stress usually involves transient feelings of sadness or anxiety in response to a stressor. However, the client's symptoms of persistent feelings of sadness, guilt, worthlessness, weight loss, and insomnia are indicative of a more serious and prolonged condition like major depressive disorder (MDD).
Explanation
Choice A rationale:
The correct answer. A positive family history of mood disorders is a well-established risk factor for developing major depressive disorder (MDD). Genetic factors play a significant role in predisposing individuals to MDD, making it more likely to develop if there's a family history of mood disorders.
Choice B rationale:
Optimistic personality traits are not considered risk factors for developing major depressive disorder (MDD). In fact, having an optimistic personality might serve as a protective factor against developing MDD.
Choice C rationale:
The correct answer. Young age is a risk factor for developing MDD. Adolescents and young adults are particularly susceptible to the onset of depressive disorders due to hormonal changes, emotional challenges, and life transitions during this developmental stage.
Choice D rationale:
High socioeconomic status is not a consistent risk factor for developing major depressive disorder (MDD). While individuals from various socioeconomic backgrounds can develop MDD, the factors contributing to its development are more complex and not solely dependent on socioeconomic status.
Choice E rationale:
The correct answer. Chronic medical conditions are risk factors for developing major depressive disorder (MDD). The stress, emotional toll, and physiological effects of living with a chronic illness can contribute to the onset or exacerbation of depressive symptoms.
Explanation
Choice A rationale:
Symptoms of major depressive disorder (MDD) are characterized by causing significant distress, not mild distress. The distress associated with MDD is usually severe and impairs daily functioning.
Choice B rationale:
While insomnia is a common symptom of major depressive disorder (MDD), it is not necessary for the diagnosis. Other symptoms, such as changes in appetite, psychomotor agitation or retardation, fatigue, and diminished interest or pleasure, can also contribute to the diagnosis.
Choice C rationale:
The correct answer. Symptoms of major depressive disorder (MDD) must not be due to a medical condition. It's crucial to rule out medical conditions that can mimic depressive symptoms, such as hypothyroidism or certain neurological disorders.
Choice D rationale:
The presence of a manic or hypomanic episode would indicate a diagnosis of bipolar disorder, not major depressive disorder (MDD). Bipolar disorder involves distinct periods of both elevated mood and depressive episodes.
Choice E rationale:
The correct answer. To meet the diagnostic criteria for major depressive disorder (MDD) according to DSM-5, an individual must experience five or more symptoms of depression during a continuous two-week period. These symptoms must include either depressed mood or loss of interest/pleasure. The scenario did not specify all the symptoms, but the persistent feelings of sadness, guilt, worthlessness, weight loss, and insomnia described align with the criteria.
A nurse is assessing a client who has been experiencing persistent feelings of sadness, fatigue, and difficulty concentrating. The client denies any history of manic episodes. Which of the following conditions should the nurse consider as a possible differential diagnosis for this client?
Explanation
Choice A rationale:
Bipolar disorder involves both depressive episodes and manic episodes. The client in question denies any history of manic episodes, making bipolar disorder less likely as a diagnosis. Manic episodes are characterized by elevated mood, increased energy, impulsivity, and risky behavior.
Choice B rationale:
Dysthymia, also known as persistent depressive disorder, involves chronic feelings of sadness and a lack of interest or pleasure in activities. It is a milder form of depression that persists for at least two years in adults. The client's persistent feelings of sadness align more closely with the criteria for dysthymia.
Choice C rationale:
Substance-induced mood disorder occurs when the client's mood disturbances are a direct result of substance use or withdrawal. Since there is no mention of substance use or withdrawal in the client's history, this choice is less relevant to the scenario.
Choice D rationale:
Adjustment disorder is characterized by the development of emotional or behavioral symptoms in response to an identifiable stressor, and these symptoms typically resolve within six months of the stressor's resolution. In the scenario, there is no indication of a recent stressor, and the client's symptoms seem to be chronic rather than time-limited, making adjustment disorder less likely.
Explanation
Choice A rationale:
Genetic theory suggests that a person's genetic makeup can predispose them to develop depression, but it does not specifically address the role of neurotransmitters in depression. While genetics can contribute to the risk of major depressive disorder (MDD), this choice doesn't focus on the neurotransmitter imbalances.
Choice B rationale:
Neuroendocrine theory pertains to the role of hormones in depression, particularly abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis. While hormones play a role in mood regulation, this theory does not primarily revolve around neurotransmitter imbalances.
Choice C rationale:
Neurotransmitter theory proposes that an imbalance of neurotransmitters, such as serotonin, norepinephrine, and dopamine, contributes to the development of major depressive disorder. This theory aligns with the idea that these neurotransmitters are responsible for regulating mood, motivation, reward, cognition, and stress response.
Choice D rationale:
Environmental theory suggests that external factors, such as life events and stressors, contribute to the development of depression. While environment can indeed influence depression, it does not specifically address the neurotransmitter imbalances that are central to this question.
Explanation
Choice A rationale:
Social support refers to the network of family, friends, and community that provide emotional and practical assistance. Depression can be influenced by inadequate social support, as having a strong support system can buffer against the development and exacerbation of depressive symptoms.
Choice B rationale:
Personalization involves attributing external events to oneself, often in a negative manner. While this cognitive distortion is relevant to depression, it is not mentioned in the question stem and does not directly relate to cognitive processes influenced by depression.
Choice C rationale:
Cognitive distortions are irrational and negative thought patterns that are common in depression. These distortions contribute to the maintenance of depressive symptoms. Examples include all-or-nothing thinking, overgeneralization, and catastrophizing.
Choice D rationale:
Catastrophizing involves magnifying the negative significance of events. While it can contribute to depressive thought patterns, it is not as central to cognitive processes influenced by depression as cognitive distortions are.
Choice E rationale:
Interpersonal relationships are affected by depression and can also contribute to its development. The question does not focus on the effects of depression on relationships, but rather on the factors that can influence or be influenced by depression.
Explanation
Choice A rationale:
Chronic stress is known to activate the Hypothalamic-Pituitary-Adrenal (HPA) axis, which leads to increased cortisol production. While cortisol is important for various physiological functions, chronic elevation of cortisol due to stress can actually have detrimental effects on the brain. Elevated cortisol levels have been associated with impaired neurogenesis (the formation of new neurons) and synaptic plasticity (the ability of synapses to change and adapt), both of which play crucial roles in maintaining cognitive function and mental health.
Choice B rationale:
This statement is not accurate. Chronic stress typically leads to hyperactivity, not hypoactivity, of the HPA axis, resulting in increased levels of cortisol. The increased cortisol levels can negatively impact neurogenesis and synaptic plasticity, which are key factors in depression and cognitive function.
Choice C rationale:
This is the correct statement. Chronic stress triggers hyperactivity of the HPA axis, causing elevated levels of cortisol. While cortisol is meant to help the body cope with stress in the short term, chronic elevation can lead to adverse effects on the brain. High cortisol levels have been linked to impaired neurogenesis and synaptic plasticity, contributing to the development of depression and cognitive deficits.
Choice D rationale:
This statement is not accurate. Chronic stress tends to lead to hyperactivity of the HPA axis and elevated cortisol levels. Reduced cortisol levels, as suggested in this choice, are not commonly associated with chronic stress and its impact on depression.
Explanation
Choice A rationale:
Pharmacological interventions involve the use of medications to treat conditions like Major Depressive Disorder (MDD). This does not involve stimulating the brain electrically or magnetically. While antidepressant medications can have an impact on neuronal activity and neuroplasticity, they are not classified as brain stimulation therapies.
Choice B rationale:
This is the correct answer. Electroconvulsive therapy (ECT) is a treatment modality that involves passing an electrical current through the brain to induce a controlled seizure. This has been found to be effective in cases of severe depression where other treatments have not worked. Other somatic therapies might include repetitive transcranial magnetic stimulation (rTMS) and vagus nerve stimulation (VNS), both of which involve modulating brain activity through electrical or magnetic means.
Choice C rationale:
Psychotherapeutic interventions involve talking therapies aimed at addressing psychological and emotional issues. These therapies do not directly involve electrical or magnetic stimulation of the brain. While they can certainly lead to changes in neuronal activity and neuroplasticity, they are not the primary modalities for brain stimulation.
Choice D rationale:
Cognitive-behavioral therapy (CBT) is a specific type of psychotherapeutic intervention that focuses on changing thought patterns and behaviors. While CBT can lead to changes in brain activity and neuroplasticity, it does not involve direct brain stimulation through electrical or magnetic means like ECT or rTMS.
Explanation
Choice A rationale:
Increased appetite is not a commonly associated side effect of antidepressant medications. In fact, some antidepressants can lead to decreased appetite or weight loss as side effects.
Choice B rationale:
Hypertension (high blood pressure) is generally not a common side effect of most antidepressant medications. However, there are specific cases where certain antidepressants might have an impact on blood pressure, but it's not a typical side effect across the board.
Choice C rationale:
This is the correct statement. Insomnia, or difficulty sleeping, is a commonly reported side effect of many antidepressant medications. It can disrupt sleep patterns and lead to increased sleep difficulties, which might exacerbate existing sleep problems or contribute to new ones.
Choice D rationale:
Excessive energy is not a common side effect associated with antidepressant use. Antidepressants typically work to regulate mood and alleviate symptoms of depression, and excessive energy would not align with the expected effects of these medications.
Explanation
Choice A rationale:
Acetylcholine and gamma-aminobutyric acid (GABA) are not the primary neurotransmitters involved in regulating mood, motivation, reward, cognition, and stress response. Acetylcholine plays a role in memory and muscle control, while GABA is an inhibitory neurotransmitter that helps regulate anxiety and sleep. These neurotransmitters are not as closely associated with the functions mentioned in the question.
Choice B rationale:
Glutamate is a major excitatory neurotransmitter in the central nervous system, and epinephrine (also known as adrenaline) is a hormone that prepares the body for the fight-or-flight response. While both glutamate and epinephrine play important roles in various physiological responses, they are not primarily responsible for regulating mood, motivation, reward, cognition, and stress response as mentioned in the question.
Choice C rationale:
Serotonin, dopamine, and norepinephrine are all key neurotransmitters involved in the regulation of mood, motivation, reward, cognition, and stress response. These neurotransmitters have been extensively studied in the context of mood disorders like Major Depressive Disorder (MDD). Serotonin is often associated with feelings of well-being and happiness, dopamine is linked to pleasure and reward pathways, and norepinephrine is involved in the body's stress response. Imbalances in these neurotransmitters have been implicated in the development of mood disorders.
Choice D rationale:
Endorphins and oxytocin are important neurotransmitters, but they are not as directly related to the regulation of mood, motivation, reward, cognition, and stress response as the neurotransmitters mentioned in choice C. Endorphins are known for their role in pain modulation and feelings of pleasure, while oxytocin is often referred to as the "bonding hormone" and is associated with social connections and childbirth.
Explanation
Choice A rationale:
Positive life events, although beneficial, are not typically considered contributors to the development of depression. Positive events generally have a positive impact on mental health and may even serve as protective factors against depression.
Choice B rationale:
High income is not commonly recognized as a direct contributor to depression. In fact, higher income can provide access to better resources and opportunities that might contribute to better mental health outcomes.
Choice C rationale:
Lack of social support is a well-established factor contributing to the development of depression. Social support plays a crucial role in buffering against stress and providing individuals with a sense of belonging and emotional connection. A lack of strong social ties can lead to feelings of isolation and increase vulnerability to depression.
Choice D rationale:
Optimistic thinking is typically considered a protective factor against depression rather than a contributor to its development. Optimistic thinking involves a positive outlook on life and the expectation of positive outcomes, which can act as a resilience factor against depressive symptoms.
Explanation
Choice A rationale:
Genetic predisposition refers to a person's susceptibility to certain conditions based on their genetic makeup. While genetics can play a role in predisposing someone to depression, it is not considered a psychosocial factor. Genetic factors are biological in nature and do not directly involve social and psychological influences.
Choice B rationale:
The role of stress and life events is a significant psychosocial factor related to depression. Stressful life events, such as trauma, loss, or major life changes, can trigger or exacerbate depressive episodes in susceptible individuals. The interaction between these external stressors and an individual's psychological responses is a key aspect of psychosocial factors.
Choice C rationale:
Interpersonal relationships are another important psychosocial factor linked to depression. Poor interpersonal relationships, social isolation, and conflicts with friends or family can contribute to feelings of loneliness and despair, increasing the risk of developing depression.
Choice D rationale:
Cognitive factors, including negative thought patterns and distorted thinking, are considered psychosocial contributors to depression. Cognitive theories of depression emphasize how an individual's thought processes, self-perception, and interpretation of events can influence their emotional state. Dysfunctional thought patterns, such as excessive self-criticism or hopelessness, can contribute to the development and maintenance of depressive symptoms.
Choice E rationale:
Neurotransmitter imbalances are not psychosocial factors. They are more related to the biological underpinnings of depression rather than the social and psychological influences explored in psychosocial factors.
Explanation
Choice A rationale:
Electroconvulsive therapy (ECT) and other somatic therapies are considered main treatment options for Major Depressive Disorder (MDD). ECT involves passing electric currents through the brain to induce controlled seizures, and it's often used in severe cases of depression that haven't responded to other treatments. Somatic therapies encompass a range of interventions that directly target the body, such as transcranial magnetic stimulation (TMS) and vagus nerve stimulation (VNS). These treatments are supported by extensive research and clinical evidence, particularly for cases where pharmacological interventions haven't been effective or suitable.
Choice B rationale:
Pharmacological interventions are indeed a mainstay in MDD treatment. However, while they are effective for many individuals, they might not work for everyone and can have side effects. Hence, the treatment approach should be tailored to the individual's needs and preferences.
Choice C rationale:
Herbal supplements are not considered main treatment options for MDD according to established clinical guidelines. While some herbal supplements might have anecdotal support for mood enhancement, their efficacy and safety are not well-established through rigorous scientific research and clinical trials.
Choice D rationale:
Physical exercise has been shown to have a positive impact on mood and can be a beneficial adjunct to MDD treatment. However, it's typically not considered a standalone main treatment option. Rather, it's often recommended as a complementary approach alongside other evidence-based treatments.
Choice E rationale:
Mindfulness-based cognitive therapy (MBCT) is a psychological approach that combines mindfulness meditation with cognitive behavioral techniques. While MBCT has shown promise in preventing relapse for individuals with recurrent depression, it's usually used as a psychotherapeutic adjunct to other main treatments like pharmacological interventions or psychotherapy.
Explanation
Choice A rationale:
Depression is not solely caused by genetic factors. While genetics do play a role in predisposing individuals to depression, it's a complex interplay between genetic susceptibility and environmental influences that contribute to the development of the disorder.
Choice B rationale:
Genetic factors are not minor players in depression. Research suggests that genetics can significantly influence a person's susceptibility to depression. However, environmental factors, such as trauma, stress, and life experiences, also contribute substantially to the onset and course of depression.
Choice C rationale:
The relationship between genetics and depression is not as straightforward as specific genes causing depression independently of environmental factors. Depression is a multifactorial disorder influenced by a combination of genetic, biological, psychological, and environmental factors.
Choice D rationale:
This is the correct answer. Genetic factors do contribute to an individual's vulnerability to depression. Studies of families, twins, and heritability have demonstrated a genetic component to depression. However, it's crucial to recognize that genetic predisposition interacts with environmental factors. Trauma, loss, chronic stress, and other environmental triggers can precipitate depressive episodes in genetically susceptible individuals.
.
Bipolar disorder
Explanation
Choice A rationale:
The GAD-7 (Generalized Anxiety Disorder 7-item scale) is a self-report questionnaire designed to assess the severity of generalized anxiety symptoms. While anxiety and depression often coexist, the GAD-7 focuses on anxiety symptoms and wouldn't provide a comprehensive assessment of depression severity.
Choice B rationale:
The BAI (Beck Anxiety Inventory) is used to measure the severity of anxiety symptoms, not depression. It wouldn't be the appropriate tool for assessing depression in this context.
Choice C rationale:
This is the correct answer. The PHQ-9 (Patient Health naire-9) is a widely used self-report tool specifically designed to measure the severity of depressive symptoms. It covers various domains of depression, such as mood, sleep, appetite, and concentration, and is suitable for assessing the impact of depression on an individual's functioning.
Choice D rationale:
The CAGE questionnaire is used to assess alcohol misuse, not depression. It consists of four questions aimed at identifying potential alcohol-related problems. While substance use disorders can co-occur with depression, the CAGE is not the appropriate tool for assessing depression severity and impact.
Explanation
Choice A rationale:
Assessing the patient's medical history is crucial in understanding potential risk factors for suicide in patients with Major Depressive Disorder (MDD). Various medical conditions and medications can contribute to depression and increase the risk of suicidal ideation. By gathering this information, the nurse can identify any factors that might exacerbate the patient's condition.
Choice B rationale:
Monitoring the patient's response to treatment is essential for assessing the effectiveness of interventions and identifying any signs of worsening depression or increased suicidal risk. Certain treatments, like antidepressant medications, might initially increase the risk of suicide in some patients. Therefore, close monitoring is needed to ensure patient safety.
Choice C rationale:
Asking direct questions about suicidal thoughts is a critical component of assessing suicide risk in patients with MDD. Openly addressing this topic allows the nurse to gauge the patient's current state of mind, explore the presence and severity of suicidal ideation, and take appropriate actions if the patient expresses active suicidal thoughts.
Choice D rationale:
Providing a list of local crisis helplines can be beneficial, but it is not a component of the nursing assessment for suicide risk in patients with MDD. While offering resources is important, the immediate focus should be on assessing the patient's condition and potential risk factors.
Choice E rationale:
Encouraging the patient to isolate themselves is not an appropriate action when assessing suicide risk in patients with MDD. Social isolation can exacerbate depressive symptoms and increase the risk of suicide. Therefore, promoting social connection and support is essential, rather than encouraging isolation.
Explanation
Choice C rationale:
Responding with, "It sounds like you're feeling really hopeless right now," is an empathetic and therapeutic response. It reflects active listening and shows that the nurse acknowledges the client's feelings without making assumptions or offering false reassurance. This response validates the client's emotions and opens the door for further discussion, potentially leading to better understanding and support.
Choice A rationale:
Responding with, "Don't worry, things will get better soon," is dismissive and invalidating. It minimizes the client's feelings and offers premature reassurance without addressing the client's current emotional state.
Choice B rationale:
Responding with, "I know how you feel. I've been there too," shifts the focus from the client to the nurse. While sharing personal experiences can be helpful in certain contexts, it's important to prioritize the client's emotions and experiences first.
Choice D rationale:
Responding with, "You need to focus on the positive aspects of life," is directive and dismissive of the client's emotions. It implies that the client's feelings are invalid and suggests a solution without fully understanding the client's perspective.
Explanation
Choice C rationale:
The primary goal of establishing a therapeutic nurse-patient relationship in the context of caring for a patient with MDD is to promote trust, rapport, empathy, and communication. This relationship provides a safe and supportive environment for the patient to express their thoughts and feelings, which is essential for effective treatment and recovery.
Choice A rationale:
Providing constant reassurance to the patient oversimplifies the therapeutic relationship. While offering reassurance is part of the nurse's role, the relationship is multidimensional and involves active listening, understanding, and collaborative problem-solving beyond just providing reassurance.
Choice B rationale:
Offering advice and solutions to the patient's problems might be part of the therapeutic process, but it's not the primary goal of the nurse-patient relationship. The relationship focuses on fostering open communication and empowering the patient to explore their feelings and thoughts.
Choice D rationale:
Encouraging the patient to rely solely on the nurse for support is not the goal of the therapeutic relationship. Instead, the nurse aims to empower the patient to develop a network of support and coping strategies, both within and outside the healthcare setting. This approach enhances the patient's long-term resilience.
Explanation
Choice A rationale:
Taking the medication with alcohol is not recommended. Alcohol can interact negatively with antidepressants, including SSRIs (Selective Serotonin Reuptake Inhibitors). It can increase the risk of side effects and potentially reduce the effectiveness of the medication. In some cases, alcohol can also worsen depression symptoms.
Choice B rationale:
Avoiding taking the medication with food is not the best advice. While some medications might require specific instructions regarding food intake, SSRIs are generally taken with food to help minimize potential stomach upset. Therefore, instructing the client to take the medication with food would be more appropriate.
Choice C rationale:
(Correct Choice) Instructing the client to report any side effects or suicidal thoughts is crucial when starting antidepressant treatment. SSRIs and other antidepressants can have side effects, some of which might be serious or bothersome. Additionally, there's a potential risk of increased suicidal ideation, especially in the initial stages of treatment. Monitoring for any changes in mood, behavior, or physical symptoms is important for ensuring the client's safety.
Choice D rationale:
Stopping the medication if symptoms improve within a week is not recommended. It takes time for antidepressants to start showing their full effects. Improvements within the first week are unlikely to be significant, and stopping the medication abruptly can lead to a recurrence of symptoms or even withdrawal effects. The client should be advised to continue taking the medication as prescribed and to follow up with their healthcare provider if there are concerns.
Explanation
Choice A rationale:
Dry mouth is a common side effect of many medications, but it is not a distinctive side effect of SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors). Dry mouth is more commonly associated with medications that affect salivary gland function, such as anticholinergic drugs.
Choice B rationale:
Weight loss can indeed be a side effect of SNRIs. These medications can impact appetite and metabolism, leading to weight loss in some individuals. However, it is not the most common or distinctive side effect when compared to other options.
Choice C rationale:
Constipation is a side effect that can occur with SNRIs, but it's not as prevalent or characteristic as some other side effects. Constipation is often associated with medications that have anticholinergic effects, which SNRIs generally have to a lesser extent.
Choice D rationale:
(Correct Choice) Insomnia is a well-known side effect of SNRIs. These medications can affect sleep patterns and may cause difficulties falling asleep or staying asleep. This side effect is particularly relevant to discuss with patients because it can impact their quality of life and overall well-being.
Explanation
Choice A rationale:
Dairy products, in general, do not have a significant interaction with TCAs (Tricyclic Antidepressants). The concern with dairy products is usually related to their interaction with certain antibiotics. Therefore, avoiding dairy products is not necessary for someone taking TCAs.
Choice B rationale:
Fresh fruits do not have a notable interaction with TCAs. In fact, a diet rich in fresh fruits can be beneficial for overall health. There is no need to advise avoiding fresh fruits due to TCA use.
Choice C rationale:
(Correct Choice) Aged cheese should be avoided when taking TCAs. Aged cheeses, such as cheddar, blue cheese, and parmesan, contain tyramine, which can lead to a hypertensive crisis when consumed along with TCAs. This interaction is a result of the monoamine oxidase inhibitory effects of TCAs, which can lead to elevated levels of tyramine in the bloodstream.
Choice D rationale:
Leafy vegetables do not have a significant interaction with TCAs. Leafy vegetables are generally considered healthy and are not contraindicated when taking these medications. Therefore, there is no need for the client to avoid leafy vegetables due to TCA use.
Explanation
Choice A rationale:
The nurse should teach the patient to avoid foods rich in tyramine while on an MAOI antidepressant. MAOIs inhibit the enzyme monoamine oxidase, which breaks down tyramine in the body. Accumulation of tyramine can lead to hypertensive crisis due to excessive release of norepinephrine. Tyramine-rich foods include aged cheeses, cured meats, fermented foods, and certain beverages like wine and beer.
Choice B rationale:
The nurse should also teach the patient to avoid herbal supplements while on an MAOI antidepressant. Herbal supplements can interact with MAOIs and lead to potentially dangerous effects, including serotonin syndrome. Herbal supplements like St. John's wort, ginseng, and others may increase serotonin levels when combined with MAOIs.
Choice D rationale:
The nurse should instruct the patient to avoid over-the-counter pain relievers, particularly those containing pseudoephedrine or phenylephrine, while taking an MAOI antidepressant. These substances can also interact with MAOIs and result in hypertensive crisis due to increased release of norepinephrine.
Choice C rationale:
Choice C (Foods high in vitamin C) is not a concern when taking an MAOI antidepressant. Vitamin C-rich foods do not interact with MAOIs or pose a risk of hypertensive crisis. Thus, this choice is incorrect in the context of MAOI use.
Choice E rationale:
Choice E (Foods high in calcium) is also not a concern when taking an MAOI antidepressant. Calcium-rich foods do not have interactions with MAOIs that would result in hypertensive crisis. This choice is not relevant to MAOI medication.
Explanation
Choice B rationale:
Bupropion, an atypical antidepressant, indeed blocks the reuptake of both dopamine and norepinephrine. Unlike many other antidepressants, which primarily target serotonin, bupropion's mechanism of action involves increasing the levels of dopamine and norepinephrine in the brain.
Choice C rationale:
Mirtazapine, another atypical antidepressant, blocks serotonin and histamine receptors. By blocking histamine receptors, mirtazapine often leads to drowsiness, which can be a side effect of this medication.
Choice E rationale:
Atypical antidepressants are associated with common side effects such as dry mouth and blurred vision. These side effects are often due to their impact on various neurotransmitter systems, including histamine and acetylcholine. Choices A and D are incorrect because they misrepresent the mechanisms of atypical antidepressants.
Choice A rationale:
Choice A (They have the same mechanisms of action as SSRIs) is incorrect. Atypical antidepressants have different mechanisms of action compared to SSRIs. While SSRIs primarily target serotonin reuptake inhibition, atypical antidepressants like bupropion and mirtazapine have unique mechanisms involving other neurotransmitters.
Choice D rationale:
Choice D (Trazodone blocks the reuptake of serotonin only) is incorrect. Trazodone is an atypical antidepressant with a complex mechanism of action. It is an antagonist at certain serotonin receptors and inhibits serotonin reuptake, but it also has antagonistic effects on histamine receptors, which contribute to its sedative properties.
Explanation
Choice C rationale:
The nurse should emphasize the importance of reporting any side effects to the healthcare provider when educating a patient with MDD who has been prescribed an atypical antidepressant. Side effects can vary from person to person, and prompt reporting allows the healthcare provider to monitor and manage any adverse reactions effectively.
Choice A Rationale:
Choice A (Taking the medication only as needed) is incorrect because atypical antidepressants, like other antidepressants, need to be taken consistently as prescribed. Taking them as needed may not provide the sustained therapeutic levels required to manage MDD effectively.
Choice B Rationale:
Choice B (Taking the medication on an empty stomach) is not a key aspect of medication adherence for atypical antidepressants. While some medications do require administration on an empty stomach, this is not a general guideline for all antidepressants.
Choice D Rationale:
Choice D (Stopping the medication abruptly if side effects occur) is incorrect. Abruptly stopping an antidepressant, including atypical ones, can lead to withdrawal symptoms and a sudden return of depressive symptoms. Discontinuation should be done under the guidance of a healthcare professional and usually involves tapering the dose.
.
Explanation
Choice A rationale:
Increased sleep duration is not a characteristic of manic episodes in bipolar disorder. In fact, decreased need for sleep is a common symptom of manic episodes. Individuals experiencing a manic episode often report feeling restless and having a decreased need for sleep.
Choice B rationale:
Reduced goal-directed activity is not typical of manic episodes. During manic episodes, individuals often exhibit heightened goal-directed activity, excessive energy, and increased involvement in various activities. This can lead to a decreased ability to focus on one task at a time.
Choice C rationale:
Correct Choice In a manic episode, individuals may display a decreased need for social interaction. They might engage in excessive socializing, seek out new social interactions, and exhibit a heightened level of confidence in their ability to engage with others. This increased sociability can sometimes be characterized by rapid speech and impulsiveness in social situations.
Choice D rationale:
Feelings of sadness and hopelessness are not indicative of manic episodes. These emotions are more aligned with depressive episodes in bipolar disorder rather than manic ones. Manic episodes are characterized by elevated mood, increased energy, and a sense of euphoria or grandiosity.
Explanation
Choice A rationale:
Correct Choice Inflated self-esteem or grandiosity is a symptom commonly present during hypomanic episodes. Individuals experiencing a hypomanic episode often have an exaggerated sense of self-importance, believe they possess special abilities or talents, and may engage in grandiose plans.
Choice B rationale:
Marked impairment in social functioning is not a typical symptom of hypomanic episodes. While individuals in a hypomanic state may exhibit increased sociability, their social functioning is generally not impaired to the extent that it would be considered a defining characteristic of this episode. Hypomania is often associated with increased productivity and a generally positive mood.
Choice C rationale:
Correct Choice Decreased need for sleep is a symptom seen in hypomanic episodes. Individuals may feel rested with significantly less sleep than usual, yet they remain energetic and highly active. This is in contrast to depressive episodes where individuals often experience increased sleep and fatigue.
Choice D rationale:
Correct Choice Flight of ideas and racing thoughts are common symptoms of hypomanic episodes. Individuals may experience a rapid flow of thoughts, jumping from one idea to another quickly, and find it challenging to keep their thoughts focused on a single topic.
Choice E rationale:
Psychotic features like delusions are not typically associated with hypomanic episodes. Delusions are more commonly seen in severe manic episodes or mixed episodes where features of both mania and depression coexist.
Explanation
Choice A rationale:
Correct Choice Responding with empathy and reflecting the client's feelings is important in therapeutic communication. In this scenario, the client is exhibiting grandiose beliefs and a heightened sense of self-importance. The response acknowledges the client's feelings without necessarily agreeing or disagreeing, maintaining a nonjudgmental stance.
Choice B rationale:
While offering to listen and talk more is a good approach, the phrasing of this option, "I'm sorry you're feeling this way," could be perceived as dismissive or patronizing. It's important to provide a more empathetic and open response to the client's feelings.
Choice C rationale:
Responding with a contradictory statement might escalate the situation and potentially lead to a power struggle with the client. Challenging the client's beliefs directly could be counterproductive to building a therapeutic relationship.
Choice D rationale:
This response could be interpreted as confrontational and potentially distressing to the client. It's important to maintain a supportive and nonjudgmental stance when communicating with individuals experiencing manic or hypomanic episodes.
Explanation
Choice A rationale:
Antidepressants are not commonly used to reduce psychotic symptoms during manic episodes in bipolar disorder. Antidepressants are primarily used to manage depressive symptoms and may exacerbate manic symptoms if used alone.
Choice B rationale:
Mood stabilizers are an appropriate class of medications used to manage bipolar disorder. However, they are more focused on preventing mood swings and stabilizing the mood rather than directly reducing psychotic symptoms during manic episodes.
Choice C rationale:
Benzodiazepines are not typically used as a first-line treatment for reducing psychotic symptoms during manic episodes in bipolar disorder. They might have a sedative effect, but they are not the primary choice for managing acute manic symptoms.
Choice D rationale:
Antipsychotics are commonly used to reduce psychotic symptoms during manic episodes in bipolar disorder. They help to alleviate symptoms such as delusions, hallucinations, and disorganized thinking that can occur during manic episodes. Examples of antipsychotics used in this context include risperidone, olanzapine, and aripiprazole. These medications help stabilize the individual and manage the acute symptoms of mania.
Explanation
Choice A rationale:
Dialectical behavior therapy (DBT) is not commonly used as a psychotherapeutic intervention for managing bipolar disorder. DBT is often used to treat borderline personality disorder and focuses on emotional regulation and interpersonal skills.
Choice B rationale:
Cognitive-behavioral therapy (CBT) is commonly used as a psychotherapeutic intervention for managing bipolar disorder. It helps individuals identify and change negative thought patterns and behaviors, which can be valuable in managing both depressive and manic symptoms.
Choice C rationale:
Family-focused therapy (FFT) is commonly used as a psychotherapeutic intervention for managing bipolar disorder. It involves the family in the treatment process and aims to improve communication, problem-solving, and support within the family unit.
Choice D rationale:
Interpersonal and social rhythm therapy (IPSRT) is commonly used as a psychotherapeutic intervention for managing bipolar disorder. It focuses on stabilizing daily routines and sleep patterns, which can help prevent mood episodes and maintain stability.
Choice E rationale:
Exposure therapy is not commonly used for managing bipolar disorder. Exposure therapy is typically used to treat anxiety disorders, particularly phobias and post-traumatic stress disorder (PTSD), and involves gradually exposing individuals to their feared situations or memories to reduce anxiety.
Explanation
Choice A rationale:
While mood stabilizers are often used in combination with antidepressants for individuals with bipolar disorder, it's not an absolute requirement that antidepressants always be used alongside mood stabilizers. The choice to combine these medications depends on the individual's specific presentation and needs.
Choice B rationale:
Antidepressants can induce or worsen manic or hypomanic symptoms in individuals with bipolar disorder. This phenomenon is known as "switching" and can lead to a rapid shift from a depressive state to a manic or hypomanic state. Therefore, careful consideration is needed when prescribing antidepressants to individuals with bipolar disorder to avoid triggering manic episodes.
Choice C rationale:
Antidepressants are not the primary treatment for acute manic episodes in bipolar disorder. Antipsychotic medications and mood stabilizers are more commonly used to address the manic symptoms and stabilize the individual's mood during such episodes.
Choice D rationale:
Antidepressants, like all medications, have the potential for causing side effects. They can lead to a range of adverse effects, including gastrointestinal symptoms, changes in sleep patterns, and sexual dysfunction, among others. Monitoring for and managing these potential side effects is important in providing comprehensive care to individuals taking antidepressants.
Explanation
Choice A rationale:
Benzodiazepines can cause weight gain and increased appetite. Rationale: This statement is incorrect. Benzodiazepines are not typically associated with weight gain and increased appetite. Weight gain is more commonly associated with certain other psychotropic medications like some antipsychotics and mood stabilizers. Benzodiazepines primarily affect the central nervous system and are known for their sedative and anxiolytic properties rather than influencing appetite.
Choice B rationale:
Benzodiazepines are used to enhance the effects of dopamine in the brain. Rationale: This statement is incorrect. Benzodiazepines do not enhance the effects of dopamine in the brain. They work by enhancing the inhibitory effects of the neurotransmitter gamma-aminobutyric acid (GABA), which leads to sedative and calming effects. Dopamine is a separate neurotransmitter associated with reward, motivation, and movement control, and benzodiazepines do not directly influence its effects.
Choice C rationale:
Benzodiazepines are commonly prescribed as mood stabilizers. Rationale: This statement is incorrect. Benzodiazepines are not commonly prescribed as mood stabilizers. Mood stabilizers are a class of medications used to manage mood disorders like bipolar disorder. While benzodiazepines might be used in certain cases to manage anxiety or agitation associated with bipolar disorder, they are not considered primary mood stabilizers. Mood stabilizers like lithium, anticonvulsants (e.g., valproate, carbamazepine), and certain atypical antipsychotics are more commonly used for this purpose.
Choice D rationale:
Benzodiazepines may lead to cognitive impairment and dependence. Rationale: This statement is correct. Benzodiazepines are associated with potential cognitive impairment and the risk of dependence. These medications have sedative effects that can impact cognitive function, including memory and attention. Prolonged use of benzodiazepines can lead to physical and psychological dependence, making it important for healthcare providers to carefully assess and monitor their use in patients, particularly those with bipolar disorder.
.
Explanation
Choice A rationale:
The patient's thought content and organization. Rationale: While monitoring thought content and organization is important in psychiatric assessment, it is not directly related to observing and documenting the patient's mood state. Thought content and organization involve assessing the coherence, relevance, and logic of the patient's thoughts, which can provide insights into their cognitive functioning and potential psychiatric conditions like schizophrenia.
Choice B rationale:
The patient's physical vital signs and laboratory tests. Rationale: This choice is unrelated to the assessment of the patient's mood state. Vital signs and laboratory tests are essential in medical assessments, but when evaluating a patient with bipolar disorder, the focus should be on their psychological and emotional state rather than physical parameters.
Choice C rationale:
The patient's cognitive abilities, memory, and concentration. Rationale: While cognitive abilities, memory, and concentration are important factors to consider in a comprehensive mental status assessment, they are distinct from the patient's mood state. Cognitive assessment provides information about cognitive impairments that might accompany mood disorders, but it does not directly reflect the patient's current emotional state.
Choice D rationale:
The patient's mood state, such as euphoric, irritable, depressed, or mixed. Rationale: This statement is correct. Assessing and documenting the patient's mood state is crucial when evaluating individuals with bipolar disorder. The mood state can provide valuable information about the phase of the disorder (e.g., manic, hypomanic, depressive) and guide treatment decisions. Mood variations are a hallmark of bipolar disorder, and accurately identifying the patient's mood at the time of assessment is essential for effective care.
Explanation
Choice A rationale:
Coherence, logic, relevance, and organization. Rationale: This choice is related to assessing the thought process, but it does not accurately address the specific signs described in the scenario: flight of ideas, racing thoughts, and tangentiality. These are characteristic features of a manic or hypomanic episode in bipolar disorder and involve a rapid flow of thoughts, lack of focus, and difficulty maintaining a coherent and organized thought process.
Choice B rationale:
Flight of ideas, racing thoughts, and tangentiality. Rationale: This statement is correct. Flight of ideas, racing thoughts, and tangentiality are indicative of disorganized thought processes commonly seen in manic episodes of bipolar disorder. Flight of ideas refers to a rapid succession of thoughts that may be loosely connected. Racing thoughts involve a constant stream of rapid thoughts, often making it difficult for the individual to concentrate. Tangentiality refers to veering off-topic during conversation and difficulty sticking to the main point.
Choice C rationale:
Themes, topics, beliefs, and perceptions. Rationale: While understanding themes, topics, beliefs, and perceptions is important in a comprehensive psychiatric assessment, this choice does not address the specific signs of disorganized thought processes mentioned in the scenario. Themes and beliefs might be explored during a broader assessment, but flight of ideas, racing thoughts, and tangentiality are more indicative of the manic phase in bipolar disorder.
Choice D rationale:
Signs of delusions, hallucinations, paranoia. Rationale: Delusions, hallucinations, and paranoia are important aspects to assess in individuals with bipolar disorder, but they are not directly related to the disorganized thought processes described in the scenario. Delusions are false beliefs, hallucinations involve sensory perceptions without external stimuli, and paranoia is excessive distrust or suspicion. These symptoms are more characteristic of psychotic disorders or severe mood episodes but are not specific to the described thought process.
Explanation
Choice A rationale:
The statement "It's great that you're feeling this way. Your mood seems stable." is not appropriate because a rating of 9 on a scale of 1 to 10 indicates a high mood, not stability. The client's mood rating is actually quite elevated, not stable.
Choice B rationale:
The correct answer is B, "You must be feeling really low to rate your mood as 9." This response reflects an understanding of the mood rating scale where 1 is the lowest and 10 is the highest. By stating that the client must be feeling low to rate their mood as 9, the nurse is acknowledging the high mood level and prompting the client to further explore and discuss their feelings.
Choice C rationale:
The statement "Tell me more about why you rated your mood so high." is not the best choice here. The client's mood rating is high, not low, and asking them to explain why they rated their mood as high might not be accurate or therapeutic in this context.
Choice D rationale:
The statement "Your mood rating suggests that you're feeling depressed." is incorrect because a mood rating of 9 indicates a high mood, which is typically associated with mania or hypomania in bipolar disorder, rather than depression.
Explanation
Choice A rationale:
The correct answer is A, "The quality, intensity, range, and appropriateness of emotional expression." This choice reflects the comprehensive assessment of a patient's affect. The nurse should document aspects such as the quality (e.g., sad, angry, euphoric), intensity (e.g., blunted, intense), range (e.g., flat, labile), and appropriateness (e.g., congruent with the situation or not) of the patient's emotional expression.
Choice B rationale:
"Signs of flat, blunted, labile, or incongruent affect" are important to assess, but this choice is not as comprehensive as choice A. It focuses solely on specific features of affect without addressing the full spectrum of emotional expression.
Choice C rationale:
"The patient's thought content, such as themes, topics, and beliefs" is unrelated to assessing affect. Thought content pertains to the patient's cognitive processes and the content of their ideas, not their emotional expression.
Choice D rationale:
"Signs of flight of ideas, racing thoughts, tangentiality" pertain to thought processes, particularly in the context of assessing thought disorders like in bipolar disorder's manic phase. This is not directly related to the assessment of emotional expression.
Explanation
Choice A rationale:
The correct answer is A, "Orientation, memory, and attention." Impaired judgment and poor insight can be indicative of cognitive dysfunction in bipolar disorder. Assessing orientation (awareness of time, place, and person), memory (short-term and long-term memory abilities), and attention (ability to focus and concentrate) can provide insights into cognitive deficits that may be contributing to impaired judgment.
Choice B rationale:
"Physical vital signs and laboratory tests" are essential assessments, but they are not directly related to the cognitive abilities of the client. They focus on physiological aspects rather than cognitive functioning.
Choice C rationale:
"Coherence, logic, and continuity of thought" are aspects of thought processes, not cognitive abilities like memory and attention. These are more relevant to assessing thought disorders or psychosis.
Choice D rationale:
"Signs of confusion, disorientation, and amnesia" are relevant to cognitive assessment, but this choice does not cover the breadth of cognitive abilities encompassed by choice A.
Explanation
Choice A rationale:
Physical vital signs and body mass index (BMI) are important indicators of the patient's physical health. However, when assessing a patient with bipolar disorder, the focus should be on their psychosocial status rather than their physical health. Bipolar disorder primarily affects mood and emotions, so evaluating physical vital signs and BMI might not provide relevant information about the patient's psychosocial well-being.
Choice B rationale:
The patient's medication history and laboratory tests are crucial for understanding their medical treatment and potential physiological factors contributing to their bipolar disorder. However, this choice emphasizes the medical aspect rather than the psychosocial aspect of the patient's condition. While medication history and lab tests are important, they do not directly address the psychosocial evaluation that is required for understanding emotional expression in bipolar disorder.
Choice C rationale:
This is the correct choice. Bipolar disorder involves significant mood swings, from manic to depressive episodes. Assessing the quality, intensity, and range of emotional expression is essential to understand the patient's current emotional state, which is a fundamental aspect of their psychosocial well-being. It provides insight into potential mood fluctuations, which are characteristic of bipolar disorder.
Choice D rationale:
Social and emotional well-being is indeed crucial for individuals with bipolar disorder. However, this choice is too broad and general. The question specifically asks for an aspect related to psychosocial status that should be evaluated during the assessment. Choice C provides a more specific and relevant focus on emotional expression, which is directly tied to bipolar disorder symptoms.
Explanation
Choice A rationale:
Cognitive abilities, memory, and attention are important cognitive functions to assess in patients with bipolar disorder. However, when addressing aggressive behavior and impulsivity, the focus should be on observing and documenting behavioral aspects rather than cognitive functions. These cognitive functions might be affected, but they are not the primary aspects of interest in this context.
Choice B rationale:
The patient's mood state and affect are indeed important considerations, especially in the context of bipolar disorder. However, the question specifically asks about aggressive behavior and impulsivity. While mood and affect might influence behavior, they are not the same as behavior. Choice D directly addresses the aspects of behavior relevant to the situation.
Choice C rationale:
Physical height and weight are not directly relevant to the assessment of aggressive behavior and impulsivity in a client with bipolar disorder. These measurements are more related to physical health rather than the behavioral or psychosocial aspects of the patient's presentation.
Choice D rationale:
This is the correct choice. Aggressive behavior and impulsivity are behavioral manifestations that can provide important insights into the patient's mental state and psychosocial functioning. Observing and documenting activity level, speech pattern, and self-care behaviors can help understand the extent and nature of these behaviors, which are relevant to the client's bipolar disorder diagnosis.
Explanation
Choice A rationale:
Monitoring signs of psychomotor agitation is essential when assessing a patient with bipolar disorder. Psychomotor agitation can occur during manic episodes and is characterized by restlessness, increased activity, and difficulty sitting still. This is a behavioral manifestation closely tied to the patient's psychological state.
Choice B rationale:
Assessing the patient's memory and attention is important in understanding cognitive functioning. Bipolar disorder can have cognitive impacts, and assessing memory and attention can help identify potential deficits or changes in cognitive abilities that might accompany mood fluctuations.
Choice C rationale:
Documenting the patient's medication history is important for the overall care of a patient with bipolar disorder, but it primarily pertains to their medical management rather than the physical assessment aspect. Choices A, B, D, and E are more directly related to the physical and psychosocial assessment of the patient.
Choice D rationale:
Measuring vital signs and laboratory tests can provide valuable information about the patient's physical health, which can be affected by medications or coexisting medical conditions. This is important to ensure the patient's overall well-being and safety.
Choice E rationale:
Observing signs of impaired judgment is crucial in assessing a patient with bipolar disorder. Impaired judgment can be evident during manic episodes and might lead to risky behaviors. This aspect directly relates to the patient's mental state and psychosocial functioning.
Explanation
Choice A rationale:
Documenting signs of psychomotor agitation is crucial when assessing a client with bipolar disorder experiencing a mixed mood state. Psychomotor agitation is a hallmark of mixed states, which are characterized by the simultaneous presence of manic and depressive symptoms. Documenting these signs helps the nurse to monitor the severity of agitation, which can inform the treatment plan and interventions.
Choice B rationale:
Observing the patient's thought content is essential during a mixed mood state assessment. Clients in a mixed mood state may experience racing thoughts, flight of ideas, or rapid speech, which are indicative of the manic component. Conversely, they may also have negative and depressive thought content due to the depressive aspect. Assessing thought content helps the nurse understand the client's mental state and make appropriate clinical judgments.
Choice C rationale:
Assessing the patient's physical status is a high-priority assessment aspect. Clients in a mixed mood state can exhibit a range of physical symptoms, including changes in sleep patterns, appetite disturbances, and psychomotor agitation. These physical manifestations are integral to the overall presentation of the mixed mood state and contribute to the formulation of an effective care plan.
Choice D rationale:
Measuring the patient's weight and height is not directly relevant to assessing a client with bipolar disorder experiencing a mixed mood state. While monitoring a patient's weight and height might be important for general health assessments, they are not specific priorities when evaluating the symptoms of a mixed mood state.
Choice E rationale:
Monitoring signs of flat affect is not a primary priority when assessing a client with bipolar disorder experiencing a mixed mood state. Flat affect is more commonly associated with depressive states rather than mixed states. While it's important to consider affect, other symptoms like psychomotor agitation and thought content are more indicative of a mixed mood state.
Explanation
Choice B rationale:
Evaluating the effectiveness of interventions is the primary goal of the nursing process during the implementation phase for a patient with bipolar disorder. Bipolar disorder is a chronic condition that requires ongoing management, and interventions are implemented to address both manic and depressive symptoms. By evaluating the effectiveness of interventions, the nurse can determine if the patient's symptoms are improving, worsening, or remaining stable. This information guides further adjustments to the care plan, ensuring that the patient receives the most appropriate and beneficial treatment.
Choice A rationale:
Collecting data about the patient's physical status is an important aspect of the assessment phase, not the implementation phase, of the nursing process. While physical status assessment informs the development of the care plan, the primary focus of implementation is to put the planned interventions into action and evaluate their outcomes.
Choice C rationale:
Planning evidence-based interventions for the patient is a crucial step in the planning phase of the nursing process. During this phase, the nurse identifies interventions that are tailored to the patient's specific needs and based on evidence-based practice. Once the planning is complete, the nurse moves on to implementing the interventions and subsequently evaluating their effectiveness.
Choice D rationale:
Administering pharmacological treatments is an action that falls within the implementation phase of the nursing process. However, it is not the primary goal of this phase for a patient with bipolar disorder. While pharmacological treatments may be part of the interventions, the primary focus is on evaluating the outcomes of these interventions to ensure the patient's symptoms are being effectively managed.
.
A client in a manic episode is having difficulty concentrating and frequently changes topics during conversation. Which nursing response is appropriate in this situation?
Explanation
Choice A rationale:
This response is not appropriate as it may come across as confrontational and dismissive of the client's current state. The client's difficulty in concentrating is a symptom of their manic episode, and using such phrasing might increase their agitation and escalate the situation.
Choice B rationale:
"I'm here to listen. Let's try to stick to one topic at a time." This response acknowledges the client's difficulty while providing support and a gentle redirection to stay focused on one topic. It maintains a therapeutic and non-confrontational approach, promoting effective communication with the client.
Choice C rationale:
While it's important to ensure fair participation in group conversations, this response may not address the immediate need of the client in a manic episode. It could potentially trigger further irritability or resistance from the client.
Choice D rationale:
This response may be interpreted as the nurse not making an effort to understand the client's thoughts, which could exacerbate the client's frustration and hinder therapeutic communication. It lacks empathy and a collaborative approach.
A nurse is educating a support group about depressive episodes in bipolar disorder. Which statement accurately describes a symptom of a depressive episode?
Explanation
Choice A rationale:
This statement is not accurate for a depressive episode. Excessive involvement in risky activities is more characteristic of a manic episode in bipolar disorder, not a depressive one. Manic episodes are marked by increased energy levels and impulsivity.
Choice B rationale:
An increase in goal-directed activity is not a typical symptom of a depressive episode. Depressive episodes are associated with a decrease in energy, motivation, and interest in previously enjoyed activities, leading to reduced activity levels.
Choice C rationale:
A decreased need for sleep is more commonly associated with manic episodes, where individuals experience a reduced need for sleep due to heightened energy levels. In depressive episodes, sleep disturbances such as insomnia are more prevalent.
Choice D rationale:
Significant weight loss or gain without intentional effort is a possible symptom. Changes in appetite and weight are hallmark features of a depressive episode. Clients may experience a loss of interest in food and subsequently lose weight, or they might engage in "comfort eating," leading to weight gain.
A nurse is discussing treatment approaches for bipolar disorder with a client. Which class of medications is considered the gold standard for bipolar disorder treatment due to its efficacy in both acute and maintenance phases?
Explanation
Choice A rationale:
Antipsychotics are often used to manage acute manic episodes in bipolar disorder, but they are not considered the gold standard for overall treatment. They may have a role as adjunctive therapy or in specific situations, but they are not typically the primary choice for maintenance treatment.
Choice B rationale:
Antidepressants are used in bipolar disorder treatment, but they are often cautiously prescribed due to the risk of triggering manic episodes or rapid cycling. They are not considered the gold standard due to this potential for destabilization.
Choice C rationale:
Benzodiazepines may be used to manage acute agitation or anxiety in bipolar disorder, but they are not the gold standard for long-term treatment. Prolonged use can lead to dependence and may not address the underlying mood instability.
Choice D rationale:
Mood stabilizers. Mood stabilizers like lithium, valproate (divalproex), and lamotrigine are considered the gold standard for bipolar disorder treatment due to their efficacy in managing both acute episodes (manic, hypomanic, and depressive) and providing long-term stabilization. These medications help prevent relapses and mood swings by regulating neurotransmitters and stabilizing mood fluctuations.
Suicide
Explanation
Choice D rationale:
Suicidal ideation can be a symptom of various underlying mental health conditions. It is not a diagnosis in itself but rather a manifestation of an individual's thoughts about self-harm or suicide. Suicidal ideation can range from passive thoughts of death to active and detailed plans for self-harm. It is essential for healthcare professionals to recognize and assess suicidal ideation as it can indicate significant distress and potential risk.
Choice A rationale:
Suicidal ideation is not a diagnosis on its own. It is a symptom that indicates emotional or psychological distress. Diagnoses are typically related to specific mental health disorders (e.g., major depressive disorder, borderline personality disorder) that may or may not involve suicidal ideation.
Choice B rationale:
Suicidal ideation is not solely more common in older adults. It can affect individuals of all age groups, including children, adolescents, and adults. While the prevalence and characteristics of suicidal ideation may vary across age groups, it is not accurate to state that it is more common in older adults.
Choice C rationale:
Suicidal ideation does not always involve a detailed plan for self-harm. Suicidal ideation exists on a continuum, ranging from vague thoughts of death to well-formed plans for suicide. Some individuals may experience fleeting thoughts of wanting to die without having a detailed plan, while others may have specific plans and intent.
Explanation
Choice A rationale:
Being extroverted is not a common risk factor associated with suicide and suicidal ideation. Extroverted individuals typically have strong social interactions and connections, which are often considered protective factors against suicide.
Choice B rationale:
Having strong family support is not a common risk factor for suicide. In fact, strong family support is generally considered a protective factor that can mitigate the risk of suicidal thoughts and behaviors. Close familial relationships can provide emotional support and a sense of belonging.
Choice C rationale:
Experiencing chronic physical illness is a common risk factor for suicide. Chronic physical illness can lead to prolonged suffering, decreased quality of life, and feelings of hopelessness, which are all associated with an increased risk of suicidal ideation.
Choice D rationale:
Having a history of positive life events is not a common risk factor for suicide. Positive life events are more likely to act as protective factors against suicide, as they contribute to an individual's overall well-being and resilience.
Choice E rationale:
Suffering from a substance use disorder is a common risk factor for suicide. Substance abuse can impair judgment, increase impulsivity, exacerbate emotional distress, and weaken the individual's ability to cope effectively, all of which contribute to an elevated risk of suicidal thoughts and behaviors.
Explanation
Choice A rationale:
Telling the client that they shouldn't feel a certain way and suggesting that others care about them minimizes their emotions and can be invalidating. It's essential to acknowledge the client's feelings without dismissing them.
Choice B rationale:
Expressing understanding and acknowledging the overwhelming nature of grief is appropriate and empathetic. This response validates the client's emotions and creates a safe space for them to express their feelings.
Choice C rationale:
While the intention behind encouraging the client to stay strong for their children might be positive, it oversimplifies the complexity of grief and emotional responses. Grief is a personal experience, and implying that they should suppress their emotions for the sake of others is not ideal.
Choice D rationale:
Suggesting that the client avoid thinking about their loss or that time will heal their wounds can invalidate their current emotional state. Grief doesn't always follow a linear path, and minimizing the impact of the loss can hinder the client's healing process.
Explanation
Choice A rationale:
Dismissing the client's thoughts and labeling them as unhealthy might cause the client to feel judged or reluctant to share further. It's important to approach the situation with openness and empathy.
Choice B rationale:
While it's true that the client's thoughts might pass, this response doesn't address the client's feelings or encourage them to express themselves. It's important to engage in a more in-depth conversation to understand their emotions.
Choice C rationale:
Asking the client to elaborate on their thoughts and experiences opens the door for meaningful conversation and assessment. This response shows genuine interest in the client's well-being and allows the nurse to gather more information to determine the appropriate level of support.
Choice D rationale:
Telling the client that things will get better soon might come across as dismissive of their current struggles. It's important to validate their emotions and explore their feelings further rather than offering premature reassurances.
Explanation
Choice A rationale:
Advising the client to keep their feelings to themselves is not an appropriate intervention in this situation. Suicidal ideation is a serious concern, and keeping feelings hidden could potentially lead to the client not receiving the necessary support and intervention they need to stay safe.
Choice B rationale:
Encouraging the client to isolate themselves until they feel better is not an appropriate intervention either. Isolation can exacerbate feelings of hopelessness and increase the risk of acting on suicidal thoughts. Connecting with the client and providing a supportive environment is crucial.
Choice C rationale:
Asking the client directly if they are thinking about harming themselves is the most appropriate intervention. This approach helps the nurse assess the severity of the situation, open a dialogue about the client's feelings, and determine the level of risk. Direct communication allows for a better understanding of the client's mental state and the need for further intervention.
Choice D rationale:
Providing the client with alcohol or drugs to help them cope is a dangerous and inappropriate intervention. Substance use can further impair judgment and increase the risk of acting on suicidal thoughts. This action also fails to address the underlying issues contributing to the client's distress.
Explanation
Choice A rationale:
Engaging in team sports is generally a positive activity and does not typically indicate suicidal ideation. While team sports can have mental health benefits, it is important to focus on the other signs that are more strongly associated with potential suicide risk.
Choice B rationale:
Expressing feelings of hopelessness is a significant warning sign of suicidal ideation. When individuals consistently express a sense of hopelessness, it could indicate that they feel trapped in their current situation and may be contemplating suicide as a way out.
Choice C rationale:
Withdrawing from social activities is a red flag for potential suicidal ideation. Social withdrawal can be indicative of a lack of interest in activities once enjoyed, a desire to isolate oneself, and an increased sense of loneliness and isolation, all of which are concerning signs.
Choice D rationale:
Demonstrating good academic performance is generally not a strong indicator of suicidal ideation. It's important to consider other emotional and behavioral signs that are more closely related to mental distress.
Choice E rationale:
Participating in creative hobbies can be a warning sign of suicidal ideation, especially if there is a sudden loss of interest in activities that the person used to enjoy. Creative hobbies may serve as an outlet for emotions, and a decrease in engagement could signal emotional turmoil.
Explanation
Choice A rationale:
Leaving the client alone to give them space is not a suitable intervention for someone with a history of suicide attempts and depression. Isolation can increase the risk of acting on suicidal thoughts, and the client needs close monitoring and support during this vulnerable time.
Choice B rationale:
Removing any potential means of self-harm from the client's environment is essential. This intervention helps reduce the immediate risk by limiting access to harmful items. It's a crucial step in creating a safer environment for the client and preventing impulsive acts of self-harm.
Choice C rationale:
Encouraging the client to confront their feelings of hopelessness is important, but it should be done in a supportive and therapeutic manner. Simply telling someone to confront their feelings without appropriate guidance can be overwhelming and unproductive.
Choice D rationale:
Telling the client that they should be grateful for what they have minimizes their emotional experience and does not address the complexity of depression and suicidal ideation. This statement lacks empathy and understanding of the client's struggles.
Explanation
Choice A rationale:
Monitoring the client's access to lethal means is a crucial intervention to ensure the client's safety. This involves assessing the client's access to items that could be used for self-harm or suicide, such as medications, sharp objects, firearms, or other potentially dangerous items. By controlling the client's access to these means, the nurse can reduce the immediate risk of harm.
Choice D rationale:
Collaborating with the client's family and friends is essential in providing a supportive environment. These individuals can offer emotional support, encouragement, and supervision, which can contribute to the client's overall safety. The nurse can educate the client's support network about warning signs and appropriate responses, fostering a more secure environment.
Choice E rationale:
Administering sedative medications to keep the client calm is not a recommended intervention for ensuring the safety of a client displaying suicidal ideation. Sedative medications may temporarily mask the client's distress but will not address the underlying issues contributing to their suicidal thoughts. Moreover, sedatives can have side effects and potentially interact with other medications, further complicating the situation.
Explanation
Choice A rationale:
Exploring the client's feelings and thoughts about suicide is crucial to understanding their perspective, emotions, and reasons behind their thoughts. Openly discussing these feelings can help the client feel understood and validated, fostering a therapeutic relationship and potentially reducing their distress.
Choice B rationale:
Developing a safety plan with the client is essential. A safety plan outlines strategies the client can use when they experience suicidal thoughts or overwhelming emotions. It includes steps to manage their emotions, reach out for support, and avoid harmful behaviors. Having a concrete plan in place empowers the client to take control of their safety.
Choice E rationale:
Identifying the client's support systems and resources is important for their recovery. Building a network of people who can offer emotional support, as well as identifying professional resources such as therapists or support groups, can enhance the client's coping mechanisms and reduce feelings of isolation.
Explanation
Choice C rationale:
Collaborating with the client to develop a comprehensive aftercare plan is a priority nursing goal for a client who has recently attempted suicide and is now stabilized. Aftercare planning involves creating a structured plan that addresses the client's ongoing psychological, emotional, and social needs. This includes arranging follow-up therapy sessions, connecting with appropriate community resources, and involving the client in decisions regarding their care. Developing an aftercare plan aims to prevent further episodes of suicidal ideation and support the client's overall well-being. Isolating the client from friends and family, as mentioned in choice A, would be counterproductive. Isolation can exacerbate feelings of loneliness and hopelessness, potentially increasing the risk of further emotional distress. Encouraging the client to keep their feelings and experiences private, as suggested in choice B, is not in line with therapeutic practice. Open communication and sharing emotions with appropriate support systems are crucial for the client's healing process. Discharging the client home as soon as possible, as mentioned in choice D, without addressing the underlying issues and providing a comprehensive aftercare plan, could lead to a recurrence of suicidal thoughts and behaviors. It is essential to ensure the client's safety and well-being before considering discharge.
.
Explanation
Choice A rationale:
In the nursing process, the step of diagnosis involves collecting data about the patient's physical and mental health status, suicide risk level, protective factors, coping skills, and support system. This step is critical in identifying the patient's current condition, problems, and needs. By assessing these aspects, the nurse can accurately diagnose the patient's situation and develop an appropriate care plan. Suicide risk assessment is an essential component of this step, as it helps determine the severity of the patient's ideation and potential for harm.
Choice B rationale:
Planning is the phase of the nursing process where the nurse, in collaboration with the patient, sets goals and develops a strategy to address the identified problems. While planning does involve considering the patient's suicide risk assessment, it primarily focuses on outlining interventions and actions to achieve the desired outcomes. It does not encompass the comprehensive data collection and assessment of the patient's mental and physical health status that are central to the diagnosis phase.
Choice C rationale:
Implementation is the stage in the nursing process where the nurse carries out the planned interventions and treatments. It involves executing the care plan that was developed during the planning phase. While suicide risk factors and protective factors may influence the choice of interventions, implementation itself does not encompass the data collection and assessment aspects required to fully evaluate the patient's condition.
Choice D rationale:
Evaluation is the final step of the nursing process, during which the nurse assesses the effectiveness of the interventions and evaluates the patient's progress toward achieving the established goals. It involves comparing the patient's current status with the expected outcomes and making necessary adjustments to the care plan. While suicide risk assessment may play a role in evaluating the patient's response to interventions, it is not the primary focus of the evaluation phase, which is centered around the assessment of treatment outcomes.
Explanation
Choice A rationale:
Asking close-ended questions involves inquiring about specific information that can be answered with a brief response, such as "yes" or "no." While these questions have their place in assessment, they are not conducive to building rapport and trust in a therapeutic relationship. Open-ended questions encourage more extensive and meaningful communication.
Choice B rationale:
Reflecting back the patient's feelings and thoughts is a valuable skill in establishing a therapeutic relationship. It demonstrates that the nurse is actively listening and trying to understand the patient's perspective. This technique helps validate the patient's emotions and fosters a sense of trust and empathy.
Choice C rationale:
Imposing personal views and opinions goes against the principles of therapeutic communication. Nurses should maintain a nonjudgmental and objective stance to create a safe environment for patients to express themselves. Imposing personal views can hinder effective communication and damage the therapeutic relationship.
Choice D rationale:
Encouraging patient involvement in decision making empowers the patient and promotes their autonomy. Collaboration in care decisions enhances the patient's sense of control and ownership over their treatment. This approach is especially important when dealing with sensitive issues like suicide risk, as it helps the patient feel heard and respected.
Choice E rationale:
Disregarding patient preferences contradicts patient-centered care, which is a fundamental principle in nursing practice. Building a therapeutic relationship requires acknowledging and respecting the patient's preferences, values, and beliefs. Disregarding these aspects can lead to mistrust and hinder effective communication.
Explanation
Choice A rationale:
This statement is not accurate. The Columbia-Suicide Severity Rating Scale (C-SSRS) is not focused on assessing suicide-related thoughts and behaviors in the past year. Instead, it is designed to assess the severity of suicidal ideation and behavior over a specified time frame.
Choice B rationale:
This statement is not accurate. The C-SSRS is not a self-report questionnaire for depression and suicidal ideation in the past two weeks. It is a structured interview that involves a series of questions and prompts administered by a trained clinician to assess the severity of suicidal ideation and behavior.
Choice C rationale:
This statement is accurate. The Columbia-Suicide Severity Rating Scale (C-SSRS) guides the evaluation and triage of patients with suicidal ideation or behavior based on five steps: Determining the presence of active suicidal ideation. Assessing the intensity of ideation. Examining the presence and severity of any preparatory behavior. Evaluating the level of intent to die. Determining the lethality of the suicide plan. The C-SSRS is widely used in clinical and research settings to assess suicide risk and guide appropriate interventions.
Choice D rationale:
This statement is not accurate. The C-SSRS does not measure the severity and intensity of suicidal ideation and behavior in the past month. It focuses on assessing the severity of suicidal ideation and behavior based on the steps mentioned in choice C.
Explanation
Choice A rationale:
Active listening. Active listening is an important communication skill that involves attentively hearing and interpreting what the patient is saying. However, it doesn't specifically address the aspect of acknowledging the patient's feelings and thoughts as real and understandable without agreeing or disagreeing.
Choice B rationale:
Empowerment. Empowerment refers to the process of enabling and supporting patients to take control of their own health and make informed decisions. While this is an essential aspect of patient care, it doesn't directly address the skill of acknowledging the patient's feelings and thoughts without expressing agreement or disagreement.
Choice C rationale:
Validation. Validation involves recognizing and accepting the patient's feelings and thoughts as valid, even if you don't share the same perspective. It shows empathy and understanding without passing judgment. In the context of a patient with suicidal ideation, validation is crucial as it helps build trust and rapport, creating an environment where the patient feels heard and supported.
Choice D rationale:
Open-ended questions. Open-ended questions are inquiries that can't be answered with a simple "yes" or "no" and encourage patients to provide more detailed responses. While they are valuable for eliciting information, they don't specifically address the act of acknowledging the patient's feelings and thoughts as real and understandable without taking a stance.
Explanation
Choice A rationale:
Psychological needs are more important than physiological needs. This statement contradicts Maslow's hierarchy of needs. According to Maslow's theory, physiological needs, such as air, water, food, and shelter, are at the base of the hierarchy and must be satisfied before addressing higher-level psychological needs.
Choice B rationale:
Social isolation takes precedence over impaired coping. While social isolation can indeed have a significant impact on a person's well-being, Maslow's hierarchy places physiological needs as the foundation. Without satisfying basic physiological needs, addressing higher-level psychological and social needs becomes less effective.
Choice C rationale:
Physiological needs are more important than psychological needs. This choice aligns with Maslow's hierarchy of needs. The hierarchy starts with physiological needs as the most fundamental, followed by safety, belongingness and love, esteem, and finally, self-actualization. A person's physiological needs (like breathing, food, water, sleep) must be met before psychological needs (such as self-esteem, achievement) can be effectively addressed.
Choice D rationale:
Grieving is considered the highest priority diagnosis. Grieving, while important, isn't necessarily the highest priority diagnosis according to Maslow's hierarchy. It falls under psychological and emotional needs, which are secondary to physiological needs. Urgent physiological needs take precedence over emotional needs in this context.
Explanation
Choice A rationale:
Building rapport and trust with the patient. Building rapport and trust is a crucial aspect of the assessment phase, not the diagnosis phase, of the nursing process. While it's important to establish a strong nurse-patient relationship, the primary goal of the diagnosis phase is to identify and define the patient's health problems and needs.
Choice B rationale:
Identifying the nursing diagnoses related to suicide risk. The diagnosis phase involves analyzing the assessment data to identify and define the patient's health issues and needs. In the case of a patient at risk for suicide, it's essential to accurately identify the specific nursing diagnoses related to the suicide risk. This lays the foundation for developing an appropriate plan of care.
Choice C rationale:
Developing a plan of care for the patient's needs. While developing a plan of care is a critical step in the nursing process, it comes after the diagnosis phase. Once nursing diagnoses are identified, the nurse can then proceed to plan interventions and strategies to address the patient's needs.
Choice D rationale:
Evaluating the effectiveness of interventions. Evaluation is the final phase of the nursing process and occurs after interventions have been implemented. It involves determining whether the interventions have been successful in achieving the desired outcomes. The primary goal of the diagnosis phase is to identify the patient's health problems, not to evaluate interventions.
Explanation
Choice A rationale:
The nursing diagnosis "Impaired coping" signifies that the client is experiencing difficulty in dealing with stressors and challenges. While it's true that impaired coping can contribute to various negative outcomes, the most critical concern when dealing with a client diagnosed with impaired coping and suicidal ideation is the risk of self-inflicted harm, which aligns with choice A. Clients with impaired coping and suicidal ideation are at a heightened risk for engaging in self-destructive behaviors, including attempts at self-inflicted, life-threatening injury. This choice is the most relevant and urgent, as it directly addresses the potential harm the client may cause to themselves due to their impaired coping skills.
Choice B rationale:
Although feelings of aloneness can contribute to psychological distress and could potentially be relevant to the client's situation, choice B does not directly address the immediate risk of self-inflicted injury associated with impaired coping and suicidal ideation. The focus in this case should be on the client's safety and preventing self-harm.
Choice C rationale:
This choice accurately describes one aspect of impaired coping but does not specifically address the increased risk of self-inflicted harm or the severity of the situation presented in the question. While impaired coping does involve the inability to use appropriate skills to manage stressors, the urgency of addressing the immediate risk of self-inflicted injury takes precedence in this scenario.
Choice D rationale:
Negative self-evaluation may contribute to impaired coping, but the question specifically relates to the client's risk for self-inflicted, life-threatening injury. While negative self-evaluation could be part of the client's overall presentation, it's not the most direct or urgent concern in this situation.
Explanation
Choice B:
Encouraging active patient involvement.
Choice D:
Reflecting the patient's feelings and thoughts.
Choice A rationale:
Closed-ended questions often limit conversation and do not encourage deeper exploration of feelings or thoughts. In a therapeutic relationship with a patient at risk for suicide, the focus should be on open communication and building trust, which is not achieved through the use of closed-ended questions. Therefore, this choice is not suitable for building rapport and trust.
Choice B rationale:
Encouraging active patient involvement is crucial for establishing a therapeutic relationship. It empowers the patient to share their thoughts, concerns, and feelings openly. This choice promotes a sense of collaboration and trust between the nurse and the patient, creating a safe space for discussing sensitive topics like suicidal thoughts.
Choice C rationale:
Imposing personal opinions can create a power imbalance and hinder the therapeutic relationship. Patients should feel that their thoughts and feelings are respected and valued. Imposing personal opinions could alienate the patient and undermine the trust-building process.
Choice D rationale:
Reflecting the patient's feelings and thoughts involves active listening and showing empathy. This technique validates the patient's emotions and experiences, fostering a sense of understanding and trust. Reflecting feelings and thoughts demonstrates that the nurse is genuinely engaged and interested in the patient's perspective.
Choice E rationale:
Disregarding the patient's preferences goes against the principles of patient-centered care and building a therapeutic relationship. The patient's preferences and needs should be acknowledged and respected to establish trust and rapport. Disregarding preferences can lead to feelings of invalidation and hinder the development of a meaningful connection.
Explanation
Choice A:
Risk for suicide.
Choice B:
Ineffective family coping.
Choice C:
Chronic low self-esteem.
Choice A rationale:
This choice aligns with the primary concern of the patient being at risk for suicide, which is the focus of the assessment. Identifying this diagnosis is crucial for implementing appropriate interventions to ensure the patient's safety.
Choice B rationale:
Ineffective family coping could contribute to the patient's stressors and emotional state. It's relevant because the support system plays a significant role in a patient's mental health. However, it might not be as immediate a concern as the risk for suicide itself.
Choice C rationale:
Chronic low self-esteem is relevant to the patient's overall mental health and might contribute to their suicidal ideation. However, it might not directly address the immediate risk and urgency of the situation compared to the diagnosis of "Risk for suicide."
Choice D rationale:
Altered nutrition and risk for infection are not directly related to the primary concern of suicidal ideation and the associated nursing diagnoses. While they may be aspects of the patient's overall health, they are not the most pertinent concerns when addressing the risk of suicide.
Explanation
The client has a subjective state with limited personal choices.
Choice A rationale:
The client is at risk for self-inflicted, life-threatening injury. This choice does not accurately define the nursing diagnosis of "Hopelessness." While it is true that hopelessness can lead to self-harm or suicide, the nursing diagnosis focuses on the client's emotional state and personal choices rather than the immediate risk of injury.
Choice B rationale:
The client has a subjective state with limited personal choices. This choice accurately defines the nursing diagnosis of "Hopelessness." Hopelessness refers to the client's emotional state of feeling devoid of hope, often resulting in a perceived lack of personal choices and options. This sense of hopelessness can contribute to feelings of despair and potentially suicidal ideation.
Choice C rationale:
The client is unable to cope with stressors. This choice is not the most accurate definition of "Hopelessness." While hopelessness can certainly impact a client's ability to cope with stressors, the primary focus of the diagnosis is on the subjective emotional state and perceived lack of choices, rather than their coping abilities.
Choice D rationale:
The client experiences compromised family coping. This choice is not directly related to the nursing diagnosis of "Hopelessness." Family coping refers to how a family unit manages stressors together, whereas hopelessness pertains to an individual's emotional state and perceived choices.
.
Explanation
Collaborate with the patient and the healthcare team.
Choice A rationale:
Prioritize long-term goals over short-term outcomes. This choice is not the most appropriate principle to consider in the planning phase for a patient with suicidal ideation. While setting long-term goals is important, immediate safety and addressing the patient's emotional state take precedence in this situation.
Choice B rationale:
Develop a rigid and unchangeable plan of care. This choice is not suitable for a patient with suicidal ideation. Flexibility in the plan of care is essential to accommodate the patient's changing emotional state and needs. A rigid plan might not effectively address the dynamic nature of suicidal ideation.
Choice C rationale:
Focus only on the patient's physical health. This choice is not comprehensive enough for a patient with suicidal ideation. While physical health is important, addressing the patient's emotional well-being, safety, and mental health concerns should be a priority in the plan of care.
Choice D rationale:
Collaborate with the patient and the healthcare team. This choice is the most appropriate principle to consider. Collaboration involves actively involving the patient in the care planning process and working with the healthcare team to develop a holistic plan that addresses the patient's emotional, psychological, and safety needs. Inclusion of the patient's perspective enhances engagement and increases the likelihood of successful interventions.
Explanation
Choice A:
Administering prescribed antidepressant medication.
Choice B:
Creating a hope box for the client.
Choice C:
Teaching relaxation techniques to the client.
Choice E:
Providing crisis hotline numbers to the client.
Choice A rationale:
Administering prescribed antidepressant medication. This intervention can be included in the implementation phase of care for a client with expressed suicidal thoughts. Antidepressant medication, when prescribed by a healthcare provider, can help alleviate depressive symptoms and improve the client's overall mental state.
Choice B rationale:
Creating a hope box for the client. Creating a hope box, filled with personal mementos, coping strategies, and reminders of positive experiences, can provide the client with a tangible tool for managing moments of despair. This can contribute to the client's emotional well-being and resilience.
Choice C rationale:
Teaching relaxation techniques to the client. Teaching relaxation techniques, such as deep breathing, mindfulness, or progressive muscle relaxation, can equip the client with coping skills to manage anxiety, stress, and overwhelming emotions. These techniques can be valuable in preventing escalation of suicidal thoughts.
Choice D rationale:
Encouraging social isolation to prevent triggers. This choice is not appropriate for a client with expressed suicidal thoughts. Encouraging social isolation can exacerbate feelings of loneliness and hopelessness, potentially increasing the risk of self-harm. Social support and connection are essential protective factors.
Choice E rationale:
Providing crisis hotline numbers to the client. Supplying crisis hotline numbers ensures that the client has access to immediate support during times of distress. This intervention helps the client reach out for help when needed and promotes safety.
Explanation
Choice A rationale:
This statement indicates a clear and direct expression of suicidal ideation. The phrase "wish all of this would end" strongly implies a desire for one's life to end, which is a significant concern in assessing a patient with suicidal thoughts. Immediate intervention is necessary to ensure the patient's safety and address their emotional distress.
Choice B rationale:
This statement, "I have been feeling really down lately," expresses a general sense of sadness and low mood. While it suggests emotional distress, it does not explicitly convey a direct intention for self-harm or suicide. However, it should not be ignored and should be explored further during the assessment.
Choice C rationale:
"I've been making a list of things I want to do before I die" is a statement that may have different implications. While it could relate to the patient's interests and goals, it does not necessarily indicate a current intent for suicide. It is important to clarify the context and content of the list before drawing any conclusions.
Choice D rationale:
"I think things might get better if I reach out to my friends" suggests that the patient is considering seeking support from friends, which is generally a positive coping strategy. This statement does not express an immediate risk of self-harm or suicide. However, it's still essential to evaluate the patient's overall emotional state and social support.
Explanation
Choice A rationale:
This statement reflects a significant red flag for potential suicide risk. The client's acknowledgment of losing their job and perceiving their family would be better off without them suggests feelings of worthlessness and burden. These emotions are associated with an increased risk of self-harm or suicide. Immediate attention and intervention are necessary to address the client's distorted thoughts and emotions.
Choice B rationale:
"I enjoy spending time with my pet dog; it helps me relax" is not an alarming statement related to suicide risk. While it highlights a coping mechanism, it doesn't provide direct insight into the client's emotional state or thoughts about self-harm.
Choice C rationale:
"I have a supportive group of friends who are always there for me" indicates a positive aspect of the client's social support network. This statement does not raise immediate concerns about suicide risk. However, a comprehensive assessment should still explore the client's overall emotional well-being.
Choice D rationale:
"I find it challenging to express my emotions to others" suggests a difficulty in emotional expression, which can be relevant to the assessment but does not inherently indicate imminent suicide risk. It's important to further explore the client's reasons for struggling with emotional expression.
Explanation
Choice A rationale:
Identifying and challenging positive thoughts is a cognitive-behavioral strategy that can be beneficial for managing mental health, but it is not the top priority in suicide prevention education. While it contributes to overall emotional well-being, recognizing signs of suicide risk is more directly relevant to preventing self-harm.
Choice B rationale:
Recognizing the signs and symptoms of suicide risk is crucial for early intervention and support. Educating clients and their families about these signs, such as increased isolation, giving away possessions, or talking about death, enables them to identify when someone might be in danger and take appropriate action.
Choice C rationale:
Promoting alcohol consumption as a stress-relieving strategy is inappropriate in a suicide prevention context. Alcohol can exacerbate emotional distress and impair judgment, potentially leading to impulsive behaviors, including self-harm. This choice goes against safe and effective strategies for managing distress.
Choice D rationale:
Encouraging isolation during times of distress is counterproductive and potentially harmful. Isolation can exacerbate feelings of loneliness and hopelessness, increasing the risk of suicidal ideation and actions. Connecting with a support network is a more appropriate recommendation during times of distress.
Explanation
Choice A rationale:
Encouraging isolation to minimize potential stressors is not a appropriate intervention for a client with suicidal ideation. Isolation can exacerbate feelings of loneliness and hopelessness, which can further contribute to the client's distress.
Choice B rationale:
Assisting the client in creating a safety plan is a crucial intervention for a client with suicidal ideation. A safety plan helps the client identify strategies and resources to use when they experience overwhelming emotions or thoughts of self-harm. This plan provides a sense of control and practical steps to follow during times of crisis, promoting hope that they can manage their emotions and stay safe.
Choice C rationale:
Teaching the client relaxation techniques is a valuable intervention, but it may not directly address the immediate need for a safety plan. Relaxation techniques can be helpful for managing anxiety and stress, but they might not be sufficient to prevent self-harm or suicide attempts.
Choice D rationale:
Focusing solely on the client's past failures is counterproductive and can further erode the client's self-esteem and hope. It's important to focus on the client's strengths, coping skills, and the potential for positive change rather than dwelling on past difficulties.
Explanation
Choice A rationale:
Modifying the plan of care based on the patient's current status is a fundamental aspect of the evaluation phase. Patients' conditions can change, and the plan of care should be flexible enough to adapt to their evolving needs. By making necessary adjustments, the nurse ensures that the patient continues to receive appropriate and effective care.
Choice B rationale:
Comparing the patient's current status with baseline data only is insufficient for a comprehensive evaluation. Baseline data is useful for establishing a starting point, but it doesn't account for changes that may have occurred since then. Effective evaluation involves considering both baseline data and the patient's current condition.
Choice C rationale:
Disregarding the patient's feedback about their care is not appropriate during the evaluation phase. Patient feedback provides valuable insights into their experience, concerns, and whether the current plan of care is meeting their needs. Ignoring their feedback can lead to unaddressed issues and a lack of patient-centered care.
Choice D rationale:
Documenting outcomes without assessing the patient's response undermines the purpose of the evaluation phase. Evaluation involves not only documenting outcomes but also assessing how the patient has responded to interventions. This assessment informs whether the outcomes are positive, need adjustment, or require a different approach.
A nurse is providing care to a client with suicidal ideation. Select all the interventions that the nurse should include in the implementation phase of the client's care.
Explanation
A.Administering prescribed antidepressant medication,
B. Assisting the client in creating a hope box,
C. Teaching relaxation techniques to the client, and E. Providing education about the importance of follow-up care.
Choice A rationale:
Administering prescribed antidepressant medication is an important intervention for a client with suicidal ideation who may be experiencing underlying depression. Antidepressants can help alleviate depressive symptoms, which can contribute to an improved mental state and decreased risk of self-harm.
Choice B rationale:
Assisting the client in creating a hope box is a valuable intervention. A hope box is a collection of items that hold personal significance and provide comfort to the client during times of distress. This intervention encourages the client to focus on positive aspects of their life, fostering hope and resilience.
Choice C rationale:
Teaching relaxation techniques to the client equips them with coping strategies to manage stress and anxiety. These techniques can help the client regulate their emotions and reduce feelings of distress, which are essential for preventing suicidal ideation.
Choice D rationale:
Encouraging social isolation is not appropriate for a client with suicidal ideation. Isolation can exacerbate feelings of loneliness and hopelessness, increasing the risk of self-harm. Instead, promoting social connections and a supportive network can contribute to the client's well-being.
Choice E rationale:
Providing education about the importance of follow-up care is crucial for a client's ongoing well-being. Follow-up care ensures that the client continues to receive necessary support and interventions, reducing the risk of relapse and maintaining their progress toward recovery.
A client has expressed suicidal thoughts to the nurse. Select all the warning signs for suicide that the nurse should be aware of.
Explanation
Choice A rationale:
Expressing hopelessness or worthlessness is a significant warning sign for suicide. When a person communicates feelings of hopelessness or worthlessness, it indicates a deep emotional distress that may lead to suicidal thoughts or actions. This feeling of being trapped in a state of hopelessness can make suicide seem like the only way out. The nurse should be especially attentive when a client expresses such emotions and should take appropriate steps to assess and address their mental state.
Choice B rationale:
Engaging in positive coping strategies is not a warning sign for suicide. In fact, individuals who are actively using positive coping mechanisms are likely trying to manage stressors and emotional difficulties in a healthier way. These strategies can include seeking social support, practicing mindfulness, engaging in hobbies, and exercising. Positive coping strategies are indicative of an individual's effort to improve their mental well-being rather than a heightened risk of suicide.
Choice C rationale:
Increasing alcohol or drug use is a warning sign for suicide. Substance abuse can often be a way for individuals to numb emotional pain or distress. If someone is using alcohol or drugs as a means of escape, it can be a sign that they are struggling with their emotions and may be at an increased risk of suicidal ideation or behavior. It's important for the nurse to recognize this pattern and address the underlying emotional issues along with substance use.
Choice D rationale:
Talking about wanting to die is a warning sign for suicide. When an individual openly talks about wanting to die or expressing a desire to end their life, it's a serious indication of their mental state. Such statements should always be taken seriously, and appropriate assessments and interventions should be implemented to ensure the person's safety. This may involve involving mental health professionals or crisis intervention teams.
Choice E rationale:
Withdrawing or isolating oneself is a warning sign for suicide. Social withdrawal or isolation can be a sign that a person is experiencing emotional pain or struggling with their mental health. A sudden shift from being socially active to isolating oneself may indicate that the person is dealing with overwhelming emotions and could potentially be contemplating suicide as a way to escape their distress.
A nurse is teaching a client's family about suicide prevention. What information should the nurse emphasize when discussing resources for help and support?
Explanation
Choice A rationale:
The importance of isolation during times of distress is not accurate information. Isolation can exacerbate feelings of loneliness and hopelessness, potentially increasing the risk of suicidal thoughts. Encouraging isolation can prevent individuals from seeking help and support when they need it the most.
Choice B rationale:
The role of faith healing in preventing suicidal thoughts is not a universally applicable solution. While faith and spirituality can provide comfort and support to some individuals, it's important to recognize that suicide prevention requires a comprehensive approach that often involves professional intervention and evidence-based strategies. Relying solely on faith healing may neglect other important aspects of mental health care.
Choice C rationale:
Crisis hotline numbers, such as the National Suicide Prevention Lifeline, are crucial resources for individuals in crisis. These hotlines provide immediate access to trained professionals who can offer support, intervention, and referrals to mental health services. Sharing these hotline numbers empowers the client's family to take proactive steps in seeking help during times of crisis.
Choice D rationale:
The necessity of solving all life problems before seeking help is an unrealistic expectation. Mental health challenges, including suicidal thoughts, do not always correlate with external life problems. Waiting until all problems are solved could delay necessary intervention and support. It's essential to encourage seeking help early, even if all problems cannot be immediately resolved.
Exams on Mood Disorders and Suicide
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define mood disorders and their types, causes, symptoms, and complications.
- Identify the risk factors, assessment tools, and nursing diagnoses for mood disorders and suicide.
- Describe the nursing interventions, pharmacological management, and patient education for mood disorders and suicide.
- Evaluate the outcomes and effectiveness of nursing care for mood disorders and suicide.
- Apply critical thinking and clinical reasoning skills to prioritize, delegate, and collaborate in the care of patients with mood disorders and suicide.
- Demonstrate professional, ethical, and legal standards in the care of patients with mood disorders and suicide.
Major depressive disorder (MDD)

- Major depressive disorder (MDD) is a mood disorder characterized by persistent and pervasive feelings of sadness, hopelessness, guilt, worthlessness, anhedonia (loss of interest or pleasure in activities), and low self-esteem
- MDD affects about 7% of the population in a 1-year period, with higher rates in females, young adults, and people with low socioeconomic status
- MDD is associated with significant morbidity, mortality, disability, and reduced quality of life
- The etiology of MDD is multifactorial and complex, involving biological, psychological, social, and environmental factors
.- Some of the risk factors for developing MDD include family history of mood disorders, personal history of trauma or abuse, chronic medical conditions or pain, substance use disorders, stressful life events or losses, personality traits such as neuroticism or pessimism
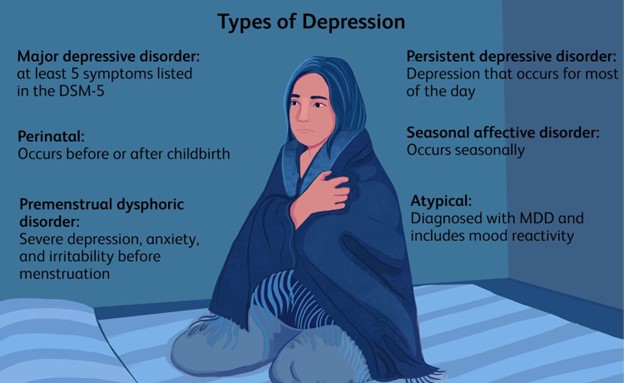
Clinical Presentation of MDD
- The signs and symptoms of MDD vary from person to person but generally include:
- Depressed mood most of the day, nearly every day
- Markedly diminished interest or pleasure in all or almost all activities most of the day
- Significant weight loss or weight gain (more than 5% of body weight in a month) or appetite changes
- Insomnia or hypersomnia (excessive sleeping)
- Psychomotor agitation or retardation (observable by others)
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Diminished ability to think or concentrate or indecisiveness
- Recurrent thoughts of death or suicide or suicide attempts
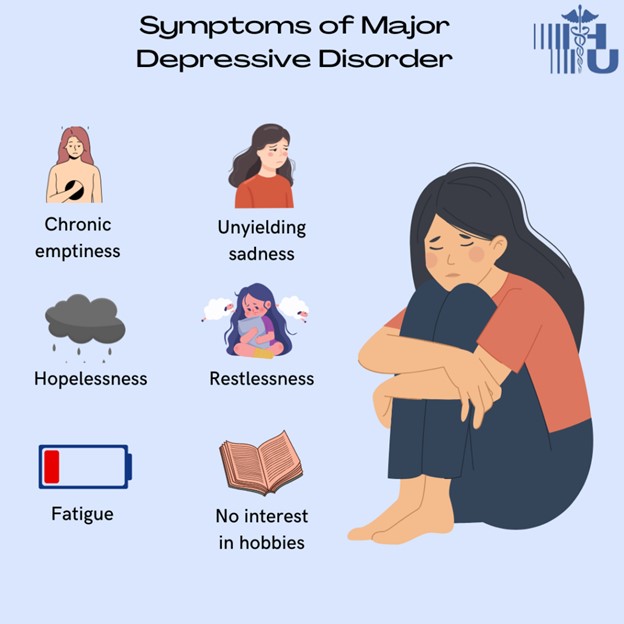
- The diagnostic criteria for MDD according to DSM-5 are
- Five or more of the above symptoms must be present during the same 2-week period and represent a change from previous functioning
- At least one of the symptoms must be either depressed mood or loss of interest or pleasure
- The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
- The symptoms are not due to the direct effects of a substance or a medical condition
- The symptoms are not better explained by another mental disorder
- There has never been a manic episode or a hypomanic episode
- The assessment and screening tools for MDD include
- Patient Health Questionnaire (PHQ-9): a 9-item self-report questionnaire that measures the severity of depression based on the DSM-5 criteria. A score of 10 or higher indicates moderate to severe depression.
- Hamilton Depression Rating Scale (HAM-D): a 17-item clinician-administered scale that evaluates various aspects of depression such as mood, anxiety, insomnia, somatic symptoms, etc. A score of 20 or higher indicates severe depression.
- Beck Depression Inventory (BDI): a 21-item self-report inventory that assesses cognitive, affective, behavioral, and somatic symptoms of depression. A score of 30 or higher indicates severe depression.
- The differential diagnosis for MDD includes:
- Bipolar disorder: characterized by episodes of mania (elevated mood) or hypomania (mild mania) alternating with episodes of depression. A history of manic or hypomanic episodes rules out MDD.
- Dysthymia: a chronic form of depression that lasts for at least 2 years but is less severe than MDD. Dysthymia can coexist with MDD as a double depression.
- Adjustment disorder: a reaction to a stressful life event that causes emotional distress and impairment in functioning. Adjustment disorder usually resolves within 6 months after the stressor is removed or adapted to.
- Bereavement: a normal and expected response to the loss of a loved one that involves grief and sadness. Bereavement can be complicated by MDD if the symptoms are persistent, severe, or interfere with daily functioning.
- Substance-induced mood disorder: a mood disturbance that is caused by the use or withdrawal of a substance such as alcohol, drugs, or medications. The mood symptoms usually remit when the substance is discontinued or detoxified.
- Mood disorder due to a general medical condition: a mood disturbance that is caused by a physical illness or injury that affects the brain or other organs. The mood symptoms usually improve when the medical condition is treated.
Pathophysiology and Neurobiology of MDD
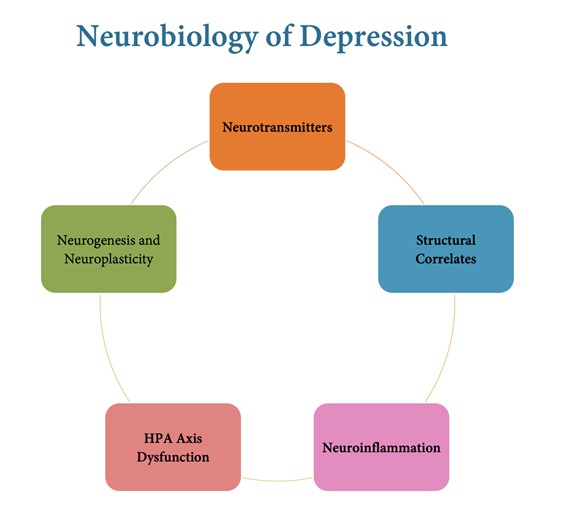
- The pathophysiology and neurobiology of MDD are not fully understood, but several theories have been proposed to explain the biological basis of depression. Some of the main theories are:
- Neurotransmitter theory: suggests that depression is caused by an imbalance of neurotransmitters such as serotonin, dopamine, and norepinephrine in the brain. These neurotransmitters are involved in regulating mood, motivation, reward, cognition, and stress response. Antidepressant medications work by increasing the availability of these neurotransmitters in the synaptic cleft.
- Neuroendocrine theory: suggests that depression is caused by dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, which is responsible for the stress response. Chronic stress can lead to hyperactivity of the HPA axis, resulting in elevated levels of cortisol, a stress hormone that can have negative effects on the brain and body. Cortisol can impair neurogenesis (the formation of new neurons), synaptic plasticity (the ability of neurons to change and adapt), and neurotrophic factors (substances that support neuronal growth and survival). Antidepressant medications work by normalizing the HPA axis function and reducing cortisol levels.
- Genetic theory: suggests that depression is influenced by genetic factors that make some individuals more vulnerable to developing depression. Several genes have been identified that are associated with depression, such as those involved in serotonin transporters, receptors, and enzymes. However, no single gene can cause depression, as environmental factors also play a role in gene expression and epigenetics (the modification of gene activity without changing the DNA sequence).
- Environmental theory: suggests that depression is influenced by environmental factors that interact with biological factors to trigger or exacerbate depression. Some of the environmental factors that can contribute to depression include trauma, abuse, neglect, poverty, social isolation, loss, conflict, etc. These factors can affect brain structure and function through neuroinflammation (the activation of immune cells in the brain), oxidative stress (the imbalance between free radicals and antioxidants), and mitochondrial dysfunction (the impairment of cellular energy production).
Psychosocial Factors and MDD
- The psychosocial factors and MDD are interrelated and mutually influence each other. Some of the psychosocial factors that can affect or be affected by depression are:
- Role of stress and life events: Stress is a subjective perception of a threat or challenge that exceeds one’s coping resources. Life events are significant occurrences that disrupt one’s routine or expectations. Both stress and life events can trigger or worsen depression by activating the biological pathways described above. However, not all stressors or life events lead to depression, as some individuals may have more resilience or protective factors than others.
- Cognitive factors: Cognitive factors refer to the way one thinks about oneself, others, and the world. Depression is associated with cognitive distortions (irrational or negative thoughts) such as overgeneralization (drawing broad conclusions from a single event), catastrophizing (exaggerating the worst possible outcome), personalization (blaming oneself for things beyond one’s control), etc. Depression is also associated with cognitive biases (selective attention or memory) such as negative filtering (focusing on the negative aspects of a situation), discounting the positive (minimizing or ignoring positive experiences), etc. These cognitive factors can maintain or reinforce depression by creating a negative feedback loop between thoughts, emotions, and behaviors.
- Interpersonal relationships: Interpersonal relationships refer to the connections one has with other people such as family, friends, partners, colleagues, etc. Depression can affect interpersonal relationships by causing social withdrawal, irritability, low self-esteem, poor communication, lack of intimacy, etc. These effects can lead to isolation, conflict, rejection, or loss of social support, which can further aggravate depression. On the other hand, interpersonal relationships can also help prevent or treat depression by providing emotional support, validation, feedback, companionship, etc.
Treatment Approaches for MDD
- The treatment approaches for MDD are based on the biopsychosocial model of depression, which recognizes the interplay between biological, psychological, and social factors in causing and treating depression.
- The main treatment modalities for MDD are:
- Pharmacological interventions: These include antidepressant medications that target the neurotransmitter systems involved in mood regulation, such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), monoamine oxidase inhibitors (MAOIs), and atypical antidepressants. Antidepressants can take several weeks to show their full effect and may cause side effects such as nausea, headache, insomnia, sexual dysfunction, etc. Antidepressants should be prescribed with caution in patients with bipolar disorder, suicidal ideation, or other medical conditions.
- Psychotherapeutic interventions: These include various forms of psychotherapy that aim to help patients understand and cope with their depression, change their negative thinking patterns, improve their interpersonal skills, and enhance their self-esteem. Some of the common types of psychotherapy for depression are cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), psychodynamic therapy, and mindfulness-based cognitive therapy (MBCT). Psychotherapy can be delivered individually or in groups and can be combined with pharmacotherapy for better outcomes.
- Electroconvulsive therapy (ECT) and other somatic therapies: These include procedures that stimulate the brain electrically or magnetically to induce changes in neuronal activity and neuroplasticity. ECT involves applying brief electrical currents to the scalp under general anesthesia to induce seizures. ECT is usually reserved for patients with severe, treatment-resistant, or psychotic depression, or those who are at high risk of suicide. ECT can cause memory loss and confusion as side effects. Other somatic therapies include transcranial magnetic stimulation (TMS), vagus nerve stimulation (VNS), and deep brain stimulation (DBS). These therapies are less invasive than ECT but have limited evidence of efficacy.
Nursing Assessment and Care for Patients with MDD
- Nursing assessment and care for patients with MDD involve the following steps:
- Nursing assessment tools: These include standardized scales such as PHQ-9, HAM-D, or BDI to measure the severity and impact of depression on the patient’s functioning. These tools can also help monitor the patient’s progress and response to treatment. Additionally, nurses should assess the patient’s medical history, medication use, substance use, suicidal risk, psychosocial factors, coping skills, and support system.
- Risk assessment for suicide and self-harm: This is a crucial part of nursing care for patients with MDD, as they have a higher risk of suicide than the general population. Nurses should ask direct questions about the patient’s suicidal thoughts, plans, means, intent, and previous attempts. Nurses should also look for warning signs such as hopelessness, isolation, giving away possessions, saying goodbye, etc. Nurses should provide a safe environment for the patient by removing any potential means of self-harm or suicide, such as sharp objects, medications, firearms, etc. Nurses should also implement a suicide prevention plan with the patient that includes identifying triggers, coping strategies, emergency contacts, and follow-up care.
- Developing a therapeutic nurse-patient relationship: This is an essential component of nursing care for patients with MDD, as it can foster trust, rapport, empathy, and communication between the nurse and the patient. Nurses should use active listening skills, open-ended questions, reflective statements, and nonverbal cues to convey interest, respect, and understanding. Nurses should also avoid giving false reassurance, advice, or criticism, as these can undermine the patient’s autonomy and self-efficacy. Nurses should encourage the patient to express their feelings, thoughts, and concerns, and validate their emotions without judgment. Nurses should also provide hope and optimism by highlighting the patient’s strengths, resources, and achievements.
- Pharmacological interventions and nursing considerations: These include administering antidepressant medications as prescribed, monitoring for therapeutic effects and adverse reactions, educating the patient about the medication regimen, and promoting medication adherence. Some of the nursing considerations for pharmacological interventions are:
- SSRIs: These are the first-line antidepressants for most patients with MDD. They work by blocking the reuptake of serotonin in the synaptic cleft, thereby increasing its availability. Examples of SSRIs are fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), and escitalopram (Lexapro). Some of the common side effects of SSRIs are nausea, diarrhea, headache, insomnia, sexual dysfunction, weight gain, and increased bleeding risk. A rare but serious adverse reaction is serotonin syndrome, which is caused by excessive serotonin levels in the brain. Serotonin syndrome can manifest as agitation, confusion, tremor, hyperthermia, tachycardia, hypertension, muscle rigidity, seizures, and coma. Serotonin syndrome can be triggered by taking SSRIs with other serotonergic agents such as MAOIs, TCAs, SNRIs, triptans (migraine medications), St. John’s wort (herbal supplement), etc. Nurses should monitor the patient for signs and symptoms of serotonin syndrome and report them immediately to the prescriber. Nurses should also teach the patient to avoid taking SSRIs with other serotonergic agents or alcohol, to take the medication at the same time every day with food or water, to not stop or change the dose without consulting the prescriber, and to report any side effects or suicidal thoughts.
- SNRIs: These are another class of antidepressants that work by blocking the reuptake of serotonin and norepinephrine in the synaptic cleft. Examples of SNRIs are venlafaxine (Effexor), duloxetine (Cymbalta), desvenlafaxine (Pristiq), and levomilnacipran (Fetzima). Some of the common side effects of SNRIs are similar to those of SSRIs, such as nausea, diarrhea, headache, insomnia, sexual dysfunction, weight gain, and increased bleeding risk. Additionally, SNRIs can cause increased blood pressure, heart rate, and sweating. A rare but serious adverse reaction is serotonin-norepinephrine syndrome, which is similar to serotonin syndrome but also involves norepinephrine excess. Serotonin-norepinephrine syndrome can be triggered by taking SNRIs with other serotonergic or noradrenergic agents such as MAOIs, TCAs, stimulants, opioids, etc. Nurses should monitor the patient for signs and symptoms of serotonin-norepinephrine syndrome and report them immediately to the prescriber. Nurses should also teach the patient to avoid taking SNRIs with other serotonergic or noradrenergic agents or alcohol, to take the medication at the same time every day with food or water, to not stop or change the dose without consulting the prescriber, and to report any side effects or suicidal thoughts.
- TCAs: These are an older class of antidepressants that work by blocking the reuptake of serotonin and norepinephrine in the synaptic cleft. Examples of TCAs are amitriptyline (Elavil), nortriptyline (Pamelor), imipramine (Tofranil), desipramine (Norpramin), and clomipramine (Anafranil). Some of the common side effects of TCAs are dry mouth, blurred vision, constipation, urinary retention, drowsiness, dizziness, weight gain, and cardiac arrhythmias. A rare but serious adverse reaction is TCA overdose, which can cause seizures, coma, and death. TCA overdose can be caused by taking too much TCA or by combining TCA with other drugs that increase its levels in the blood such as SSRIs, MAOIs, antihistamines, etc. Nurses should monitor the patient for signs and symptoms of TCA overdose and report them immediately to the prescriber. Nurses should also teach the patient to avoid taking TCAs with other drugs that increase its levels in the blood or alcohol, to take the medication at bedtime to avoid daytime sedation, to not stop or change the dose without consulting the prescriber, and to report any side effects or suicidal thoughts.
- MAOIs: These are another older class of antidepressants that work by inhibiting the enzyme monoamine oxidase (MAO) that breaks down serotonin, norepinephrine, and dopamine in the brain and other tissues. Examples of MAOIs are phenelzine (Nardil), tranylcypromine (Parnate), isocarboxazid (Marplan), and selegiline (Emsam). Some of the common side effects of MAOIs are insomnia, orthostatic hypotension, weight gain, sexual dysfunction, and headache. A rare but serious adverse reaction is hypertensive crisis, which is caused by a dangerous rise in blood pressure due to the interaction of MAOIs with tyramine, a substance found in certain foods and beverages. Tyramine can cause the release of large amounts of norepinephrine, leading to vasoconstriction and increased cardiac output. Hypertensive crisis can manifest as severe headache, chest pain, palpitations, nausea, vomiting, sweating, etc. Hypertensive crisis can be treated with phentolamine or nifedipine, which are vasodilators that lower blood pressure. Nurses should monitor the patient for signs and symptoms of hypertensive crisis and report them immediately to the prescriber. Nurses should also teach the patient to avoid taking MAOIs with other drugs that increase serotonin or norepinephrine levels in the blood such as SSRIs, SNRIs, TCAs, stimulants, opioids, etc., or alcohol. Nurses should also teach the patient to follow a low-tyramine diet that excludes foods and beverages such as aged cheese, pepperoni, salami, avocados, figs, bananas, smoked fish, protein supplements, beers, red wine, etc.
- Atypical antidepressants: These are a heterogeneous group of antidepressants that do not fit into the other classes and have different mechanisms of action. Examples of atypical antidepressants are bupropion (Wellbutrin), mirtazapine (Remeron), nefazodone (Serzone), trazodone (Desyrel), and vilazodone (Viibryd). Some of the common side effects of atypical antidepressants are nausea, dry mouth, drowsiness, insomnia, weight changes, sexual dysfunction, and headache. A rare but serious adverse reaction is serotonin syndrome or serotonin-norepinephrine syndrome when taken with other serotonergic or noradrenergic agents. Nurses should monitor the patient for signs and symptoms of these syndromes and report them immediately to the prescriber. Nurses should also teach the patient to avoid taking atypical antidepressants with other drugs that increase serotonin or norepinephrine levels in the blood or alcohol. Nurses should also teach the patient to take the medication as prescribed and to report any side effects or suicidal thoughts.
|
Class |
Mechanism of action |
Examples |
Common side effects |
|
SSRIs |
Block the reuptake of serotonin in the brain, increasing its availability |
Citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline |
Nausea, headache, insomnia, sexual dysfunction, weight gain |
|
SNRIs |
Block the reuptake of serotonin and norepinephrine in the brain, increasing their availability |
Duloxetine, venlafaxine, desvenlafaxine |
Nausea, headache, insomnia, sexual dysfunction, increased blood pressure |
|
TCAs |
Block the reuptake of norepinephrine and serotonin in the brain, increasing their availability. Also block other receptors such as histamine and acetylcholine |
Amitriptyline, clomipramine, desipramine, doxepin, imipramine, nortriptyline |
Dry mouth, blurred vision, constipation, urinary retention, drowsiness, weight gain, cardiac arrhythmias |
|
MAOIs |
Inhibit the enzyme monoamine oxidase that breaks down neurotransmitters such as dopamine, norepinephrine and serotonin in the brain |
Isocarboxazid, phenelzine, tranylcypromine |
Dizziness, headache, insomnia, weight gain. Can cause a dangerous rise in blood pressure if combined with certain foods or medications |
|
Atypical antidepressants |
Have different mechanisms of action than the other classes. Some examples are: Bupropion: blocks the reuptake of dopamine and norepinephrine Mirtazapine: blocks certain serotonin and histamine receptors Nefazodone: blocks the reuptake of serotonin and norepinephrine and certain serotonin receptors Trazodone: blocks the reuptake of serotonin and certain serotonin receptors Vortioxetine: blocks the reuptake of serotonin and modulates various serotonin receptors |
Vary depending on the drug. Some common ones are: Bupropion: insomnia, headache, nausea Mirtazapine: drowsiness, weight gain Nefazodone: drowsiness, nausea Trazodone: drowsiness, dry mouth Vortioxetine: nausea, headache |
Conclusion
- Major depressive disorder (MDD) is a common and serious mood disorder that affects millions of people worldwide.
- MDD is caused by a complex interplay of biological, psychological, and social factors that influence mood regulation.
- MDD is diagnosed based on the presence of five or more depressive symptoms for at least two weeks that cause significant distress or impairment in functioning.
- MDD is treated with a combination of pharmacological, psychotherapeutic, and somatic interventions that aim to restore neurotransmitter balance, cognitive functioning, and psychosocial well-being.
- Nursing care for patients with MDD involves assessing their depression severity, suicidal risk, and psychosocial factors, developing a therapeutic relationship, administering and monitoring antidepressant medications, and providing education and support.
Bipolar disorder
- Bipolar disorder, also known as manic-depressive illness, is a mental health condition that causes extreme shifts in mood, energy, activity, and behavior. People who have bipolar disorder experience episodes of intense highs, known as manic or hypomanic episodes, where they may feel overly energetic, euphoric, or irritable. These episodes alternate with periods of deep lows, or depressive episodes, where they may feel extremely sad, hopeless, and lethargic. The disorder can disrupt daily life, relationships, and decision-making. Understanding its varied manifestations, potential causes, nursing interventions, and available treatments is important in supporting those affected by this challenging condition.
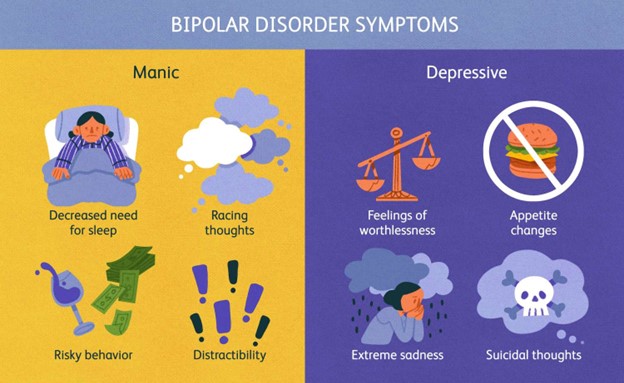
Types of Bipolar Disorder
- Bipolar disorder is classified into different types based on the severity and frequency of the mood episodes. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the main types of bipolar disorder are:
- Bipolar I disorder: This type is characterized by at least one manic episode that lasts for at least seven days or requires hospitalization. The manic episode may be preceded or followed by hypomanic or major depressive episodes. The symptoms of mania are severe enough to cause significant impairment in social or occupational functioning or to necessitate hospitalization. Some people with bipolar I disorder may also experience psychotic symptoms, such as delusions or hallucinations, during a manic episode.
- Bipolar II disorder: This type is characterized by at least one major depressive episode and at least one hypomanic episode, but no full-blown manic episodes. The symptoms of hypomania are less severe than those of mania and do not cause marked impairment in functioning or require hospitalization. However, the depressive episodes are usually more frequent and longer-lasting than those in bipolar I disorder.
- Cyclothymic disorder: This type is characterized by numerous periods of hypomanic symptoms and depressive symptoms that do not meet the criteria for a full episode. The symptoms must persist for at least two years in adults or one year in children or adolescents. The mood swings are usually mild to moderate in intensity and do not cause significant impairment in functioning.
- Other specified bipolar and related disorders: This category includes bipolar-like phenomena that do not meet the full criteria for any of the above types due to insufficient duration or severity. For example, a person may have a short-duration hypomanic episode (less than four days) or a hypomanic episode without prior major depression.
- Unspecified bipolar and related disorders: This category includes bipolar-like phenomena that cause clinically significant distress or impairment in functioning but do not meet the full criteria for any of the above types. For example, a person may have insufficient information to make a specific diagnosis or may have symptoms that do not fit into any of the above categories.
Pathophysiology and Neurobiology of Bipolar Disorder
- The exact cause of bipolar disorder is unknown, but it is likely influenced by a combination of genetic, environmental, and biological factors. Some of the possible factors are:
- Genetic factors: Bipolar disorder tends to run in families, suggesting a hereditary component. However, no single gene has been identified as responsible for the condition. Rather, it is likely that multiple genes interact with each other and with environmental factors to increase the risk of developing bipolar disorder. Some studies have suggested that genes involved in neurotransmitter systems (such as dopamine, serotonin, glutamate, and GABA), circadian rhythms (such as CLOCK), neurotrophic factors (such as BDNF), and immune system (such as IL-1) may play a role in bipolar disorder.
- Environmental factors: Stressful life events, such as trauma, abuse, loss, or conflict, may trigger or worsen mood episodes in people with bipolar disorder. However, not everyone who experiences stress develops bipolar disorder. Other environmental factors that may contribute to bipolar disorder include substance abuse (such as alcohol, cocaine, or cannabis), sleep deprivation or disruption (such as jet lag or shift work), hormonal changes (such as puberty or menopause), seasonal changes (such as winter depression), and medical conditions (such as thyroid disorders or neurological diseases).
- Biological factors: Bipolar disorder is associated with abnormalities in brain structure and function. Brain imaging studies have shown differences in the size, shape, activity, and connectivity of various brain regions involved in emotion regulation (such as prefrontal cortex, amygdala, hippocampus, thalamus) between people with bipolar disorder and healthy controls. These differences may reflect alterations in neuronal development (such as neurogenesis, synaptogenesis), plasticity (such as synaptic pruning), signaling (such as receptor density), and metabolism (such as oxidative stress) in the brain. Moreover, bipolar disorder is associated with changes in neurochemicals (such as neurotransmitters, hormones, and cytokines) that modulate mood, cognition, and behavior. For example, people with bipolar disorder may have dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, which controls the stress response and cortisol secretion. They may also have altered levels of monoamines (such as dopamine, serotonin, and norepinephrine), which are involved in reward, motivation, and mood. Additionally, they may have abnormal levels of glutamate and GABA, which are involved in excitatory and inhibitory neurotransmission, respectively. Furthermore, they may have impaired functioning of neurotrophic factors (such as BDNF), which are involved in neuronal survival, growth, and differentiation.
Signs and Symptoms of Manic, Hypomanic, and Depressive Episodes
- The signs and symptoms of bipolar disorder vary depending on the type and phase of the mood episode. The following are some of the common signs and symptoms of manic, hypomanic, and depressive episodes:
- Manic episode: A manic episode is a period of abnormally elevated, expansive, or irritable mood and increased goal-directed activity or energy that lasts for at least one week or requires hospitalization. During a manic episode, a person may exhibit at least three (or four if the mood is only irritable) of the following symptoms:
- Inflated self-esteem or grandiosity: The person may have an exaggerated sense of self-importance, power, or abilities. They may believe that they have special talents, connections, or insights that others do not have. They may also have unrealistic or delusional plans or goals.
- Decreased need for sleep: The person may feel rested after only a few hours of sleep or may not sleep at all. They may also have difficulty falling asleep or staying asleep due to racing thoughts or increased activity.
- More talkative than usual or pressure to keep talking: The person may speak rapidly, loudly, or incessantly. They may also interrupt others, dominate conversations, or change topics abruptly. They may have difficulty staying on one subject or following a logical sequence of ideas.
- Flight of ideas or subjective experience that thoughts are racing: The person may have a stream of thoughts that jump from one topic to another without any connection or coherence. They may also feel that their thoughts are moving too fast for them to keep up.
- Distractibility: The person may be easily sidetracked by irrelevant stimuli or have difficulty concentrating on one task or activity. They may also have trouble following instructions or completing assignments.
- Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation: The person may be excessively involved in multiple activities or projects that are often unrealistic or poorly planned. They may also be restless, fidgety, or hyperactive.
- Excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments): The person may act impulsively, recklessly, or irresponsibly without considering the consequences of their actions. They may also have poor judgment, insight, or impulse control.

- Hypomanic episode: A hypomanic episode is a period of abnormally elevated, expansive, or irritable mood and increased activity or energy that lasts for at least four consecutive days and is clearly different from the usual nondepressed mood. During a hypomanic episode, a person may exhibit at least three (or four if the mood is only irritable) of the same symptoms as in a manic episode. However, the symptoms are less severe than those in a manic episode and do not cause marked impairment in social or occupational functioning or require hospitalization. There are no psychotic features present during a hypomanic episode.
- Depressive episode: A depressive episode is a period of depressed mood or loss of interest or pleasure in most activities that lasts for at least two weeks and causes significant distress or impairment in functioning. During a depressive episode, a person may exhibit at least four of the following symptoms:
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite: The person may experience changes in their eating habits, appetite, or weight without any intentional effort to do so.
- Insomnia, hypersomnia, or other sleep disturbances: The person may have difficulty falling asleep , staying asleep, waking up too early, sleeping too much, or having poor quality of sleep.
- Psychomotor agitation , retardation , or other changes in physical activity: The person may be restless , fidgety , jittery , nervous , or agitated
Treatment Approaches for Bipolar Disorder
- The treatment of bipolar disorder involves a combination of pharmacological and psychotherapeutic interventions that aim to stabilize mood, prevent relapse, reduce symptoms, and improve functioning and quality of life.
- Pharmacological interventions: The main classes of medications used for bipolar disorder are mood stabilizers, antipsychotics, antidepressants, and benzodiazepines. The choice of medication depends on the type and phase of the mood episode, the patient’s response and tolerance, the presence of comorbidities, and the potential side effects.
- Mood stabilizers: These are medications that help prevent or reduce the frequency and severity of manic and depressive episodes. They include lithium, valproate, carbamazepine, lamotrigine, and some anticonvulsants. Lithium is considered the gold standard for bipolar disorder treatment, as it has proven efficacy in both acute and maintenance phases. However, lithium requires regular monitoring of blood levels, kidney function, thyroid function, and electrolytes, as it has a narrow therapeutic window and can cause toxicity or adverse effects.
- Antipsychotics: These are medications that help control psychotic symptoms, such as delusions or hallucinations, that may occur during manic or mixed episodes. They also have mood-stabilizing properties and can be used as monotherapy or adjunctive therapy for acute mania or depression. They include typical antipsychotics (such as haloperidol) and atypical antipsychotics (such as olanzapine, quetiapine, risperidone, aripiprazole, ziprasidone, and lurasidone). Antipsychotics can cause side effects such as weight gain, metabolic syndrome, extrapyramidal symptoms, tardive dyskinesia, sedation, and anticholinergic effects.
- Antidepressants: These are medications that help alleviate depressive symptoms, such as low mood, anhedonia, insomnia, and suicidal ideation. They include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs). Antidepressants are usually used in combination with mood stabilizers or antipsychotics to prevent or treat bipolar depression. However, antidepressants may also induce or worsen manic or hypomanic symptoms in some people with bipolar disorder, especially if used without a mood stabilizer.
- Benzodiazepines: These are medications that help reduce anxiety, agitation, insomnia, and muscle tension. They include diazepam, lorazepam, clonazepam, and alprazolam. Benzodiazepines are often used as adjunctive therapy for acute mania or mixed episodes to provide rapid relief of symptoms. However, benzodiazepines may also cause dependence, tolerance, withdrawal, sedation, cognitive impairment, and respiratory depression.
|
Class |
Examples |
How they work |
Side effects |
|
Mood stabilizers |
Lithium, valproate, lamotrigine, carbamazepine |
They help balance the levels of neurotransmitters in the brain and prevent mood swings |
Nausea, weight gain, tremor, thirst, kidney problems, rash, drowsiness, dizziness |
|
Antipsychotics |
Aripiprazole, olanzapine, quetiapine, risperidone, ziprasidone |
They block the effects of dopamine and serotonin in the brain and reduce psychotic symptoms such as delusions and hallucinations |
Weight gain, diabetes, high cholesterol, movement disorders, sedation, dry mouth, constipation |
|
Antidepressants |
Fluoxetine, sertraline, bupropion, venlafaxine |
They increase the levels of serotonin and/or norepinephrine in the brain and improve depressive symptoms |
Anxiety, insomnia, nausea, sexual dysfunction, headache, weight changes |
|
Benzodiazepines |
Alprazolam, clonazepam, lorazepam, diazepam |
They enhance the effects of a neurotransmitter called GABA in the brain and produce a calming effect |
Drowsiness, confusion, memory impairment, dependence, withdrawal symptoms |
- Psychotherapeutic interventions: These are non-pharmacological approaches that help enhance coping skills, psychoeducation, adherence to treatment, mood regulation, and social support for people with bipolar disorder. They include:
- Cognitive-behavioral therapy (CBT): This is a form of psychotherapy that helps identify and challenge negative or distorted thoughts and beliefs that contribute to mood swings and dysfunctional behaviors. CBT also teaches strategies to cope with stressors, manage emotions, solve problems, and prevent relapse.
- Interpersonal and social rhythm therapy (IPSRT): This is a form of psychotherapy that focuses on improving interpersonal relationships and stabilizing daily routines and rhythms. IPSRT helps people with bipolar disorder understand how their mood is influenced by their social environment and their biological clock. IPSRT also helps them establish regular patterns of sleep, activity, diet, and social interaction.
- Family-focused therapy (FFT): This is a form of psychotherapy that involves the participation of family members or significant others in the treatment of bipolar disorder. FFT helps educate the family about the nature and course of bipolar disorder, improve communication and problem-solving skills among family members, reduce family stress and conflict, and enhance family support and coping skills.
- Psychoeducation: This is a form of intervention that provides information and education about bipolar disorder, its symptoms, causes, treatment options, and prognosis. Psychoeducation helps increase the awareness and understanding of bipolar disorder among patients, families, and caregivers. It also helps improve treatment adherence, self-management, and prevention of relapse.
Nursing Assessment and Care for Patients with Bipolar Disorder
- The nursing process is a systematic and dynamic method of providing holistic care for patients with bipolar disorder. It involves four phases: assessment, planning, implementation, and evaluation.
- Assessment: This phase involves collecting data about the patient’s physical, psychological, social, and spiritual status. The nurse should assess the following aspects:
- Mood: The nurse should observe and document the patient’s mood state, such as euphoric, irritable, depressed, or mixed. The nurse should also ask the patient to rate their mood on a scale of 1 to 10, where 1 is the lowest and 10 is the highest.
- Behavior: The nurse should observe and document the patient’s behavior, such as activity level, speech pattern, impulsivity, aggression, self-care, hygiene, grooming, and dress. The nurse should also note any signs of psychomotor agitation or retardation.
- Thought process: The nurse should observe and document the patient’s thought process, such as coherence, logic, relevance, continuity, and organization. The nurse should also note any signs of flight of ideas, racing thoughts, tangentiality, circumstantiality, or loose associations.
- Thought content: The nurse should observe and document the patient’s thought content, such as themes, topics, beliefs, and perceptions. The nurse should also note any signs of delusions, hallucinations, paranoia, or suicidal or homicidal ideation.
- Affect: The nurse should observe and document the patient’s affect, such as the quality, intensity, range, appropriateness, and congruence of their emotional expression. The nurse should also note any signs of flat, blunted, labile, or incongruent affect.
- Cognition: The nurse should assess and document the patient’s cognitive abilities, such as orientation, memory, attention, concentration, judgment, insight, and abstract reasoning. The nurse should also note any signs of confusion, disorientation, amnesia, distractibility, impaired judgment, or poor insight.
- Physical: The nurse should assess and document the patient’s physical status, such as vital signs, weight, height, body mass index (BMI), laboratory tests (such as lithium level), and medication history. The nurse should also note any signs of dehydration, malnutrition, infection, injury, or toxicity.
- Psychosocial: The nurse should assess and document the patient’s psychosocial status,
Summary
- Bipolar disorder is a mental health condition that causes extreme shifts in mood, energy, activity, and behavior.
- Bipolar disorder is classified into different types based on the severity and frequency of the mood episodes: bipolar I disorder, bipolar II disorder, cyclothymic disorder, other specified bipolar and related disorders, and unspecified bipolar and related disorders.
- Bipolar disorder is influenced by a combination of genetic, environmental, and biological factors that affect brain structure and function.
- Bipolar disorder is diagnosed based on the DSM-5 criteria that specify the signs and symptoms of manic, hypomanic, and depressive episodes.
- Bipolar disorder is treated with a combination of pharmacological and psychotherapeutic interventions that aim to stabilize mood, prevent relapse, reduce symptoms, and improve functioning and quality of life.
- Bipolar disorder is managed with the nursing process that involves four phases: assessment, planning, implementation, and evaluation. The nurse should provide holistic care for the patient using evidence-based practices and clinical guidelines.
Suicide

- Suicide is the intentional act of killing oneself. It is a major public health problem that affects people of all ages, genders, races, and cultures. According to the World Health Organization, more than 700,000 people die by suicide every year worldwide, making it the second leading cause of death among 15-29-year-olds.
- Suicidal ideation, often called suicidal thoughts or ideas, is a broad term used to describe a range of contemplations, wishes, and preoccupations with death and suicide. Suicidal ideation can be passive or active, depending on the presence or absence of a plan to inflict lethal self-harm. Suicidal ideation is not a diagnosis, but a symptom of underlying mental health conditions, such as depression, anxiety, bipolar disorder, schizophrenia, substance use disorder, personality disorder, or post-traumatic stress disorder.
- The causes of suicide and suicidal ideation are complex and multifactorial. They involve biological, psychological, social, environmental, and situational factors that interact in different ways for each individual. Some of the common risk factors for suicide and suicidal ideation are:
- Previous suicide attempt or history of self-harm
- Family history of suicide or mental illness
- Chronic physical illness or pain
- Mental health disorders, especially mood disorders
- Substance use disorder or withdrawal
- Social isolation or lack of support
- Exposure to violence or abuse
- Loss of a loved one or a significant relationship
- Stressful life events or transitions
- Access to lethal means
- Hopelessness or helplessness
- Impulsivity or aggression
- Low self-esteem or self-worth
- Stigma or discrimination
- The warning signs of suicide and suicidal ideation are clues that indicate that a person may be thinking about or planning to end their life. They may be verbal, behavioral, or emotional. Some of the common warning signs are:
- Talking about wanting to die or kill oneself
- Looking for a way to kill oneself, such as searching online or obtaining a weapon
- Expressing feelings of hopelessness, worthlessness, guilt, shame, or despair
- Saying goodbye to family and friends or giving away prized possessions
- Withdrawing from social activities or isolating oneself
- Increasing the use of alcohol or drugs
- Showing changes in mood, such as sadness, anger, anxiety, or irritability
- Showing changes in sleep patterns, appetite, energy level, or hygiene
- Exhibiting reckless or risky behaviors, such as driving fast, having unprotected sex, or gambling excessively
- Losing interest in hobbies, work, school, or other aspects of life
Nursing Process in Suicide
- The nursing process is a systematic method of providing individualized care for patients with suicidal ideation or behavior. It consists of five steps: assessment, diagnosis, planning, implementation, and evaluation.
Assessment
- The assessment phase involves collecting data about the patient’s physical and mental health status, suicide risk level, protective factors, coping skills, and support system. The data can be obtained from various sources, such as interviews, observations, medical records, laboratory tests, and standardized tools. Some of the tools that can be used to assess suicide risk are:
- Columbia-Suicide Severity Rating Scale (C-SSRS): a clinician-administered scale that measures the severity and intensity of suicidal ideation and behavior in the past month.
- Patient Health Questionnaire-9 (PHQ-9): a self-report questionnaire that screens for depression and suicidal ideation in the past two weeks.
- Suicide Behaviors Questionnaire-Revised (SBQ-R): a self-report questionnaire that assesses suicide-related thoughts and behaviors in the past year.
- Suicide Assessment Five-step Evaluation and Triage (SAFE-T): a clinician-administered protocol that guides the evaluation and triage of patients with suicidal ideation or behavior based on five steps: identify risk factors, identify protective factors, conduct suicide inquiry, determine risk level and intervention, and document.
- The assessment phase also involves establishing a therapeutic relationship with the patient, which is essential for providing effective care and preventing suicide. The nurse should use the following skills to build rapport and trust with the patient:
- Active listening: paying attention to what the patient says and how they say it, using verbal and nonverbal cues to show interest and empathy, and reflecting back the patient’s feelings and thoughts.
- Open-ended questions: asking questions that allow the patient to express their feelings and thoughts in their own words, without leading or judging them.
- Validation: acknowledging the patient’s feelings and thoughts as real and understandable, without agreeing or disagreeing with them.
- Empowerment: encouraging the patient to take an active role in their care and recovery, by involving them in decision making, goal setting, and problem solving.
- Respect: showing respect for the patient’s dignity, autonomy, values, beliefs, and preferences, without imposing one’s own views or opinions.
- Honesty: being honest and transparent with the patient about the purpose and process of the assessment, the limits of confidentiality, and the possible outcomes and interventions.
Diagnosis
- The diagnosis phase involves analyzing the data collected from the assessment phase and identifying the nursing diagnoses that reflect the patient’s actual or potential problems related to suicide. The nursing diagnoses should be stated in terms of human responses (e.g., hopelessness, impaired coping) rather than medical diagnoses (e.g., depression, bipolar disorder). The nursing diagnoses should also be prioritized according to Maslow’s hierarchy of needs, which states that physiological needs (e.g., safety, air, water) are more important than psychological needs (e.g., love, esteem, self-actualization). Some of the common nursing diagnoses for patients with suicidal ideation or behavior are:
- Risk for suicide: at risk for self-inflicted, life-threatening injury
- Hopelessness: subjective state in which an individual sees few or no alternatives or personal choices available
- Impaired coping: inability to use appropriate skills to cope with stressors
- Chronic low self-esteem: long-standing negative self-evaluation or feelings about self or self-capabilities
- Social isolation: aloneness experienced by an individual as a negative or threatening state
- Ineffective family coping: compromised or disabled family coping
- Grieving: normal response to loss
Planning
- The planning phase involves developing a plan of care that specifies the goals, outcomes, and interventions for each nursing diagnosis. The plan of care should be individualized, holistic, and collaborative, involving the patient, the family, and other members of the health care team. The plan of care should also be flexible, realistic, and measurable, allowing for adjustments based on the patient’s changing needs and responses. Some of the general principles for planning care for patients with suicidal ideation or behavior are:
- Prioritize safety: ensure that the patient is safe from harm by removing any potential means of suicide (e.g., weapons, medications, sharp objects), providing constant or intermittent observation (depending on the risk level), implementing a no-suicide contract (a verbal or written agreement between the patient and the nurse that the patient will not harm themselves), and following institutional policies and protocols for suicide prevention.
- Promote recovery: provide evidence-based interventions that address the underlying causes and factors of suicide (e.g., mental health disorders, substance use disorders, psychosocial stressors), such as psychotherapy (e.g., cognitive-behavioral therapy, dialectical behavior therapy, interpersonal therapy), pharmacotherapy (e.g., antidepressants, mood stabilizers, antipsychotics), electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS), or ketamine infusion.
- Enhance coping: teach the patient positive coping skills that can help them manage their emotions, thoughts, and behaviors in stressful situations, such as relaxation techniques (e.g., deep breathing, progressive muscle relaxation, meditation), cognitive restructuring (e.g., identifying and challenging negative thoughts), problem-solving skills (e.g., defining the problem, generating alternatives, evaluating consequences), assertiveness skills (e.g., expressing one’s needs and rights respectfully), distraction techniques (e.g., engaging in hobbies, activities, or social interactions), or crisis hotline numbers (e.g., National Suicide Prevention Lifeline 1-800-273-TALK).
- Foster hope: help the patient develop a sense of hope for the future by identifying their strengths, values, goals, and reasons for living. Assist the patient in creating a hope box (a container filled with items that remind them of positive aspects of their life) or a safety plan (a written document that outlines steps to take when they feel suicidal) that they can use when they feel hopeless. Encourage the patient to participate in activities that give them meaning, purpose and joy, such as volunteering, spirituality, or hobbies. Provide positive feedback and praise for the patient’s efforts and achievements.
Implementation
- The implementation phase involves carrying out the interventions that were planned in the previous phase. The nurse should monitor the patient’s response to the interventions and document the outcomes. The nurse should also communicate and collaborate with other members of the health care team, such as physicians, psychologists, social workers, pharmacists, and case managers, to ensure continuity and quality of care. The nurse should also provide education and support to the patient and their family about suicide and its prevention, such as:
- The nature and causes of suicide and suicidal ideation
- The signs and symptoms of suicide risk and how to recognize them
- The treatment options and modalities for suicide prevention and recovery
- The coping skills and strategies to deal with stressors and emotions
- The resources and services available for help and support
- The importance of follow-up care and adherence to treatment plan
Evaluation
- The evaluation phase involves evaluating the effectiveness of the plan of care and determining whether the goals and outcomes were met. The nurse should compare the patient’s current status with the baseline data and the expected outcomes. The nurse should also solicit feedback from the patient and their family about their satisfaction with the care provided. Based on the evaluation results, the nurse should modify or revise the plan of care as needed to achieve optimal outcomes.
Conclusion
- Suicide is a serious and preventable public health problem that requires comprehensive and individualized nursing care. The nurse plays a vital role in assessing, intervening, and supporting patients with suicidal ideation or behavior. By using the nursing process, evidence-based interventions, and therapeutic communication skills, the nurse can help prevent suicide and promote safety and recovery for patients with suicidal ideation or behavior.
Summary
- Suicide is the intentional act of killing oneself. It is influenced by biological, psychological, social, environmental, and situational factors.
- Suicidal ideation is a broad term that describes a range of thoughts or wishes about death or suicide. It can be passive or active, depending on the presence or absence of a plan.
- The risk factors for suicide include previous suicide attempt, family history of suicide, mental health disorders, substance use disorders, chronic physical illness, social isolation, loss of a loved one, stressful life events, access to lethal means, hopelessness, impulsivity, low self-esteem, stigma.
- The warning signs for suicide include talking about wanting to die, looking for a way to kill oneself, expressing hopelessness or worthlessness, saying goodbye or giving away possessions, withdrawing or isolating oneself, increasing alcohol or drug use, showing mood changes or reckless behaviors.
- The nursing process is a systematic method of providing individualized care for patients with suicidal ideation or behavior. It consists of five steps: assessment, diagnosis, planning, implementation, and evaluation.
- The nursing interventions for patients with suicidal ideation or behavior include ensuring safety, providing evidence-based treatments, teaching coping skills, fostering hope, providing education and support, and evaluating outcomes.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Mood Disorders and Suicide
This filled cannot be empty

