Please set your exam date
Pediatric Emergency Care
Study Questions
Pediatric Basic Life Support
During pediatric basic life support (BLS), what is the correct compression depth for chest compressions in infants?
Explanation
A. The correct compression depth for infants during pediatric BLS is approximately 1 inch (2.5 cm).
B. 1.5 inches (4 cm) is the correct compression depth for children (ages 1 to puberty).
C. 2 inches (5 cm) is the correct compression depth for adult patients.
D. 2.5 inches (6.5 cm) is not the recommended compression depth for any age group in BLS.
Which of the following maneuvers is recommended to open the airway in a neonate during resuscitation?
Explanation
A. Head tilt-chin lift is used for older children and adults, not for neonates.
B. Jaw thrust is the recommended maneuver to open the airway in neonates to avoid putting pressure on the soft tissues of the neck.
C. Neck extensionof the head is not appropriate maneuvers for neonatal airway management.
D. Hyperextension of the head is not appropriate maneuvers for neonatal airway management.
Which of the following is a sign of effective ventilation in a newborn during neonatal resuscitation?
Explanation
A. Decreased heart rate indicates ineffective ventilation and is a sign of inadequate oxygenation.
B. Cyanosis suggests inadequate oxygenation and is not a sign of effective ventilation.
C. Chest movement and a rising heart rate are signs of effective ventilation in a newborn during neonatal resuscitation.
D. Gasping respirations are not a reliable indicator of effective ventilation and may indicate cardiac arrest.
What is the correct compression-to-ventilation ratio for one-rescuer infant CPR?
Explanation
A. 15:2 is the compression-to-ventilation ratio for two-rescuer infant CPR.
B. The correct compression-to-ventilation ratio for one-rescuer infant CPR is 30:2.
C. 30:1 is the compression-to-ventilation ratio for one-rescuer adult CPR.
D. 5:1 is not a standard compression-to-ventilation ratio for any age group in CPR.
What is the recommended depth for chest compressions in newborns during neonatal resuscitation?
Explanation
A. 1 inch (2.5 cm) is the recommended compression depth for infants during pediatric BLS.
B. The correct compression depth for newborns during neonatal resuscitation is approximately 1.5 inches (4 cm).
C. 2 inches (5 cm) is the correct compression depth for adult patients.
D. 2.5 inches (6.5 cm) is not the recommended compression depth for any age group in BLS.
What is the initial step in neonatal resuscitation when the newborn is not breathing and has a heart rate below 100 beats per minute?
Explanation
A. Administering positive-pressure ventilation is the initial step in neonatal resuscitation for a newborn not breathing or having a heart rate below 100 beats per minute.
B. Initiating chest compressions is the next step if positive-pressure ventilation is not effective.
C. Administering epinephrine is part of the advanced steps in neonatal resuscitation after positive-pressure ventilation and chest compressions.
D. Inserting an advanced airway device is part of the advanced steps in neonatal resuscitation after positive-pressure ventilation, chest compressions, and administering epinephrine.
Which of the following medications is indicated for use in neonatal resuscitation to treat bradycardia?
Explanation
A. Naloxone is used to reverse opioid overdose and is not indicated for bradycardia in neonatal resuscitation.
B. Atropine is used in neonatal resuscitation to treat bradycardia and increase the heart rate.
C. Epinephrine is used in neonatal resuscitation for severe bradycardia or cardiac arrest not responding to ventilation and chest compressions.
D. Albuterol is a bronchodilator and is not indicated for bradycardia in neonatal resuscitation.
What is the recommended rate of chest compressions in neonatal resuscitation?
Explanation
A. 60-80 compressions per minute is the recommended rate of chest compressions for older children and adults in CPR.
B. 80-100 compressions per minute is the recommended rate of chest compressions for infants in CPR.
C. The recommended rate of chest compressions in neonatal resuscitation is 100-120 compressions per minute.
D. 120-140 compressions per minute is not a standard rate of chest compressions in neonatal resuscitation.
Which of the following maneuvers is recommended to open the airway in a newborn during neonatal resuscitation?
Explanation
A. Head tilt-chin lift is used for older children and adults, not for newborns.
B. Jaw thrust is the recommended maneuver to open the airway in newborns to avoid putting pressure on the soft tissues of the neck.
C. Neck extension and D. Hyperextension of the head are not appropriate maneuvers for newborn airway management.
What is the correct sequence of steps in neonatal resuscitation according to the American Heart Association guidelines?
Explanation
A. The correct sequence of steps in neonatal resuscitation according to the American Heart Association guidelines is Airway, Breathing, Chest compressions, Drugs, and Defibrillation (if indicated).
B. Chest compressions are performed after airway and breathing interventions, not before.
C. Breathing and airway interventions are prioritized before chest compressions.
D. Defibrillation, if indicated, is performed after the initial steps of neonatal resuscitation, including airway, breathing, and chest compressions. Drugs are administered after defibrillation if necessary.
Pediatric Advanced Life Support (PALS)
During pediatric advanced life support (PALS), what is the correct medication for treating ventricular fibrillation in a child?
Explanation
A. Adenosine is used for supraventricular tachycardias, not ventricular fibrillation.
B. Amiodarone is the medication of choice for treating ventricular fibrillation in pediatric advanced life support.
C. Atropine is used for symptomatic bradycardia, not ventricular fibrillation.
D. Epinephrine is used for pulseless rhythms and severe bradycardia, not ventricular fibrillation.
What is the correct compression depth for chest compressions in pediatric advanced life support (PALS)?
Explanation
A. 1/2 to 1 inch (1.25 to 2.5 cm) is the recommended compression depth for infants during pediatric CPR.
B. 1 to 1.5 inches (2.5 to 4 cm) is the recommended compression depth for children (ages 1 to puberty) during pediatric CPR.
C. The correct compression depth for chest compressions in pediatric advanced life support (PALS) is 1.5 to 2 inches (4 to 5 cm).
D. 2 to 2.5 inches (5 to 6.5 cm) is the recommended compression depth for adult patients during CPR.
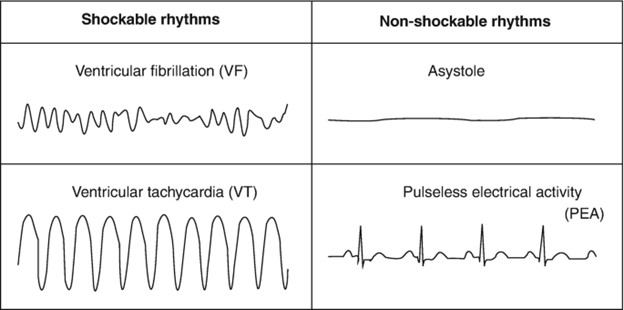
Which of the following rhythms is treated with synchronized cardioversion in pediatric advanced life support (PALS)?
Explanation
A. Ventricular fibrillation and B. Pulseless ventricular tachycardia are treated with defibrillation, not synchronized cardioversion.
C. Supraventricular tachycardia with poor perfusion is treated with synchronized cardioversion in pediatric advanced life support (PALS).
D. Asystole does not respond to cardioversion and is managed with advanced life support interventions.
What is the initial dose of epinephrine in pediatric advanced life support (PALS) for a child in cardiac arrest?
Explanation
A. 0.01 mg/kg is the correct dose of epinephrine in neonatal resuscitation, not for pediatric advanced life support.
B. The initial dose of epinephrine in pediatric advanced life support (PALS) for a child in cardiac arrest is 0.1 mg/kg.
C. 0.5 mg/kg and D. 1 mg/kg are not appropriate doses for pediatric cardiac arrest situations.
Which of the following maneuvers is recommended to open the airway in a child during pediatric advanced life support (PALS)?
Explanation
A. Head tilt-chin lift is the recommended maneuver to open the airway in children during pediatric advanced life support (PALS).
B. Jaw thrust is used when there is suspicion of a cervical spine injury; otherwise, head tilt-chin lift is preferred.
C. Neck extension and D. Hyperextension of the head are not appropriate maneuvers for pediatric airway management.
What is the recommended rate of chest compressions in pediatric advanced life support (PALS) for children and infants?
Explanation
A. 60-80 compressions per minute is the recommended rate of chest compressions for older children and adults in CPR.
B. 80-100 compressions per minute is the recommended rate of chest compressions for infants in CPR.
C. The recommended rate of chest compressions in pediatric advanced life support (PALS) for children and infants is 100-120 compressions per minute.
D. 120-140 compressions per minute is not a standard rate of chest compressions in pediatric advanced life support.
Which of the following is an indication for using an advanced airway device in pediatric advanced life support (PALS)?
Explanation
A. Mild respiratory distress does not require an advanced airway device; oxygen supplementation and monitoring may be sufficient.
B. Ineffective bag-mask ventilation is an indication for using an advanced airway
device in pediatric advanced life support (PALS).
C. Initial assessment of a non-breathing child requires basic airway management techniques before considering advanced airway devices.
D. Effective spontaneous breathing does not require an advanced airway device.
What is the correct sequence of actions in pediatric advanced life support (PALS) for a child with a pulseless ventricular tachycardia?
Explanation
A. The correct sequence of actions in pediatric advanced life support (PALS) for a child with a pulseless ventricular tachycardia is Defibrillation, epinephrine, amiodarone.
B. Epinephrine is administered after the first defibrillation, followed by amiodarone if the rhythm persists.
C. Amiodarone is given after the first shock and epinephrine if the rhythm persists.
D. Defibrillation is the first step, followed by amiodarone, and then epinephrine if necessary.
Which of the following is a common cause of pediatric cardiac arrest?
Explanation
A. Hyperventilation, C. Bradycardia, and D. Trauma can lead to pediatric cardiac arrest, but respiratory failure is a common cause.
B. Respiratory failure, such as in cases of severe asthma or pneumonia, can lead to hypoxia and subsequently cardiac arrest in children.
What is the correct depth for chest compressions in pediatric advanced life support (PALS) for children and infants?
Explanation
A. 1/2 to 1 inch (1.25 to 2.5 cm) is the recommended compression depth for infants during pediatric CPR.
B. 1 to 1.5 inches (2.5 to 4 cm) is the recommended compression depth for children (ages 1 to puberty) during pediatric CPR.
C. The correct compression depth for chest compressions in pediatric advanced life support (PALS) for children and infants is 1.5 to 2 inches (4 to 5 cm).
D. 2 to 2.5 inches (5 to 6.5 cm) is the recommended compression depth for adult patients during CPR.
Pediatric Emergencies
A 2-year-old child is brought to the emergency room with high fever, irritability, and a rash. The nurse suspects bacterial meningitis. What is the appropriate intervention?
Explanation
A. Administering an antipyretic without further evaluation is not appropriate for a suspected case of bacterial meningitis.
B. Performing a lumbar puncture to analyze cerebrospinal fluid and starting antibiotics is the standard intervention for suspected bacterial meningitis.
C. Administering an antihistamine is not the appropriate intervention for bacterial meningitis, which is a bacterial infection of the meninges.
D. Ordering a head CT scan is not the first-line diagnostic test for suspected bacterial meningitis. A lumbar puncture is the diagnostic procedure of choice.
A child with known peanut allergy accidentally ingests peanuts and develops severe difficulty in breathing, facial swelling, and hives. What is the priority action by the nurse?
Explanation
A. Administering an antipyretic is not appropriate for anaphylaxis, a severe allergic reaction that requires immediate intervention.
B. Administering epinephrine is the first-line treatment for anaphylaxis. After administering epinephrine, calling for emergency medical assistance is crucial.
C. Offering a cold drink is not the appropriate intervention for anaphylaxis and will not address the life-threatening symptoms.
D. Providing a heating pad is not relevant to the situation and will not address the symptoms of anaphylaxis.
A 3-year-old child is suspected of ingesting an unknown substance. What action should the nurse take first?
Explanation
A. Administering ipecac syrup to induce vomiting is no longer recommended as a first-aid measure for poisoning. The Poison Control Center should be consulted first for guidance.
B. Calling the Poison Control Center is the first action to take in case of suspected poisoning. They provide expert guidance on managing poisoning cases.
C. Administering activated charcoal can be done under the guidance of the Poison Control Center, but it is not the first action to take.
D. Performing abdominal thrusts is used for foreign body airway obstruction, not poisoning.
A parent brings in a 1-year-old child who is coughing and choking. The child is unable to breathe, cry, or make any sound. What should the nurse do first?
Explanation
A. Performing back blows and chest thrusts is the appropriate intervention for foreign body airway obstruction in an infant who is unable to breathe, cry, or make any sound.
B. Abdominal thrusts are used for conscious adults and children over 1 year old with foreign body airway obstruction.
C. Administering a drink is not appropriate and can worsen the situation by causing further obstruction.
D. Performing a finger sweep of the mouth can push the object farther down the airway and is not recommended.
A 5-year-old child falls from a tree and loses consciousness briefly. The child wakes up but appears drowsy and confused. What is the priority action by the nurse?
Explanation
A. Applying a cold compress can provide comfort but is not the priority action for a child with head trauma and altered mental status.
B. Administering pain medication is not the priority; the child needs a thorough evaluation and possible imaging studies to assess for head injury.
C. Monitoring closely is important, but with the history of head trauma, immediate medical evaluation is crucial to rule out any serious injury.
D. Transporting the child to the emergency department immediately is the priority to ensure proper assessment and management of head trauma.
A 8-year-old child with a history of heart disease suddenly becomes pale, lethargic, and complains of chest pain. Vital signs show tachycardia and weak pulses. What is the likely cause of the child's symptoms?
Explanation
A. Febrile seizure presents with sudden convulsions and fever in children and does not cause pale, lethargic symptoms with chest pain and tachycardia.
B. Hypoglycemia can cause weakness and altered mental status, but it does not typically present with chest pain, tachycardia, and weak pulses.
C. Cardiogenic shock, often seen in children with heart disease, can present with pale, lethargic appearance, chest pain, tachycardia, and weak pulses due to poor cardiac output.
D. Foreign body aspiration can cause sudden respiratory distress and choking, but it does not present with chest pain, pale appearance, tachycardia, and weak pulses.
A 6-year-old child is found unconscious and not breathing. What is the initial action by the nurse?
Explanation
A. Administering epinephrine is part of advanced life support protocols and is done after initiating chest compressions and rescue breaths in pediatric cardiac arrest.
B. Initiating chest compressions and rescue breaths is the immediate action for an unconscious child who is not breathing.
C. Checking for a pulse is not the first step in pediatric cardiac arrest. Starting chest compressions and rescue breaths takes priority.
D. Calling for emergency medical assistance should be done simultaneously with starting chest compressions and rescue breaths.
A nurse is caring for a child with suspected septic shock. Which intervention is a priority in managing this condition?
Explanation
A. Administering pain medication is not the priority in septic shock. Prompt administration of antibiotics and fluids is crucial to address the underlying infection and support hemodynamic stability.
B. Administering antibiotics and fluids is the priority intervention in managing septic shock. Early initiation of appropriate antibiotics and fluid resuscitation are key components of septic shock management.
C. Providing antipyretics can be done to address fever, but it is not the priority in managing septic shock.
D. Elevating the head of the bed may be done for comfort or respiratory support but is not the priority in septic shock management.
A 10-year-old child is suspected of ingesting an unknown amount of acetaminophen. What intervention should the nurse anticipate?
Explanation
A. Administration of an antidote, such as N-acetylcysteine (NAC), is the specific treatment for acetaminophen poisoning if given within the appropriate timeframe after ingestion.
B. Inducing vomiting is not recommended as a first-line intervention for acetaminophen poisoning due to the risk of aspiration.
C. Administering activated charcoal can be considered in certain cases of poisoning, but it is not specific for acetaminophen poisoning.
D. Administering laxatives is not the appropriate intervention for acetaminophen poisoning.
A nurse is caring for a child in status epilepticus. What is the priority action by the nurse?
Explanation
A. Administering an antipyretic is not the priority in managing status epilepticus. Controlling the seizure activity takes precedence.
B. Administering intravenous diazepam or lorazepam is the first-line treatment for status epilepticus to stop ongoing seizures.
C. Administering oral phenytoin is not appropriate in the acute management of status epilepticus. Intravenous benzodiazepines are the preferred initial treatment.
D. Administering an antihistamine is not the appropriate intervention for status epilepticus. Intravenous benzodiazepines are used to stop the seizure activity.
A 4-year-old child is brought to the emergency room with a fever, sore throat, and difficulty swallowing. The nurse suspects streptococcal pharyngitis. What is the appropriate intervention?
Explanation
A. Administering a broad-spectrum antibiotic without confirmation of streptococcal infection is not appropriate and can contribute to antibiotic resistance.
B. Antiviral medications are not effective against bacterial infections such as streptococcal pharyngitis.
C. Performing a throat culture or rapid strep test is the appropriate intervention to confirm the diagnosis of streptococcal pharyngitis. If positive, antibiotic treatment can be initiated.
D. Administering a pain reliever can provide symptomatic relief but does not confirm the diagnosis. Throat culture or rapid strep test is necessary.
A 2-year-old child with a history of asthma is experiencing difficulty breathing, wheezing, and a persistent cough. What is the priority intervention by the nurse?
Explanation
A. Administering a bronchodilator inhaler, such as albuterol, is the priority intervention for a child with asthma experiencing difficulty breathing, wheezing, and coughing.
B. Antihistamines are not the primary treatment for acute asthma exacerbations.
C. Mucolytic medications can help thin mucus but are not the first-line treatment for acute asthma symptoms.
D. Cough suppressants are not recommended for children with asthma as they can worsen respiratory distress.
A 6-month-old infant is brought to the emergency room with signs of dehydration, sunken fontanelles, and decreased urine output. What is the priority nursing intervention?
Explanation
A. Offering oral rehydration solution (ORS) may not be effective for severe dehydration in an infant who is unable to drink or tolerate oral fluids.
B. Administering intravenous fluids is the priority intervention for a severely dehydrated infant to restore fluid balance and prevent complications.
C. Monitoring vital signs is important but does not address the immediate need for fluid replacement in severe dehydration.
D. Obtaining a urine sample is not the priority; intravenous fluids should be initiated promptly in a severely dehydrated infant.
A 5-year-old child is experiencing a febrile seizure. What is the nurse's immediate action?
Explanation
A. Administering a fever reducer is not the immediate action during a febrile seizure.
B. Placing the child in a tub of cold water is not recommended. The best approach is to keep the child safe and monitor them during the seizure.
C. Placing the child on the side helps prevent choking and aspiration during a seizure. This is the immediate action to take during a febrile seizure.
D. Administering an antiepileptic medication is not necessary during a febrile seizure, which is usually a brief and self-limiting event.
A 7-year-old child sustains a deep cut on the arm while playing outside. The wound is bleeding heavily. What is the nurse's initial action?
Explanation
A. Applying a tourniquet is not the initial action for controlling bleeding. Direct pressure and elevation are more appropriate.
B. Applying direct pressure and elevating the arm above the level of the heart help control bleeding from the wound.
C. Cleaning the wound with alcohol can wait until after bleeding is controlled. Direct pressure and elevation are the immediate priorities.
D. Administering an oral pain reliever is not the immediate concern; controlling bleeding and preventing infection are the priorities.
A 9-month-old infant is brought to the emergency room with suspected poisoning. What action should the nurse take first?
Explanation
A. Administering activated charcoal can be done under the guidance of the Poison Control Center, but it is not the first action to take.
B. Inducing vomiting is not recommended as a first-line intervention for poisoning and should not be done without consulting the Poison Control Center.
C. Contacting the Poison Control Center is the first and most important action in cases of suspected poisoning. They provide expert guidance on managing poisoning cases.
D. Administering syrup of ipecac is no longer recommended as a first-aid measure for poisoning. The Poison Control Center should be consulted first.
A 3-year-old child is brought to the emergency room with a head injury after falling from a height. The child is unconscious and not breathing. What is the nurse's immediate action?
Explanation
A. Administering rescue breaths is the immediate action for an unconscious child who is not breathing. CPR should be initiated immediately.
B. Checking for a pulse can be done after initiating rescue breaths and chest compressions.
C. Initiating chest compressions is part of CPR but should be preceded by rescue breaths.
D. Initiating abdominal thrusts is used for foreign body airway obstruction, not for an unconscious child with a head injury and respiratory distress.
A 6-year-old child with diabetes experiences symptoms of hypoglycemia, including irritability, shakiness, and confusion. What is the appropriate intervention?
Explanation
A. Administering insulin is not appropriate for hypoglycemia; it would further lower blood sugar levels.
B. Administering a high-sugar snack or drink is the appropriate intervention for hypoglycemia to raise blood sugar levels quickly.
C. Administering a pain reliever is not the appropriate intervention for hypoglycemia.
D. Administering a sedative is not the appropriate intervention for hypoglycemia and can mask symptoms.
A 10-year-old child is found unconscious in the water after a near-drowning incident. What is the nurse's immediate action?
Explanation
A. Administering rescue breaths and chest compressions is the immediate action for an unconscious child found after a near-drowning incident. CPR should be initiated immediately.
B. Placing the child in the recovery position is not appropriate for an unconscious child requiring CPR.
C. Initiating abdominal thrusts is used for foreign body airway obstruction, not for an unconscious child found after a near-drowning incident.
D. Administering a sedative is not the appropriate intervention for an unconscious child and can further depress respiratory function.
A 8-year-old child is brought to the emergency room with a deep cut on the leg. The wound is bleeding profusely. What is the nurse's initial action?
Explanation
A. Applying a tourniquet is not the initial action for controlling bleeding. Direct pressure and elevation are more appropriate.
B. Applying direct pressure and elevating the leg above the level of the heart help control bleeding from the wound.
C. Cleaning the wound with alcohol can wait until after bleeding is controlled. Direct pressure and elevation are the immediate priorities.
D. Administering an oral pain reliever is not the immediate concern; controlling bleeding and preventing infection are the priorities.
Exams on Pediatric Emergency Care
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
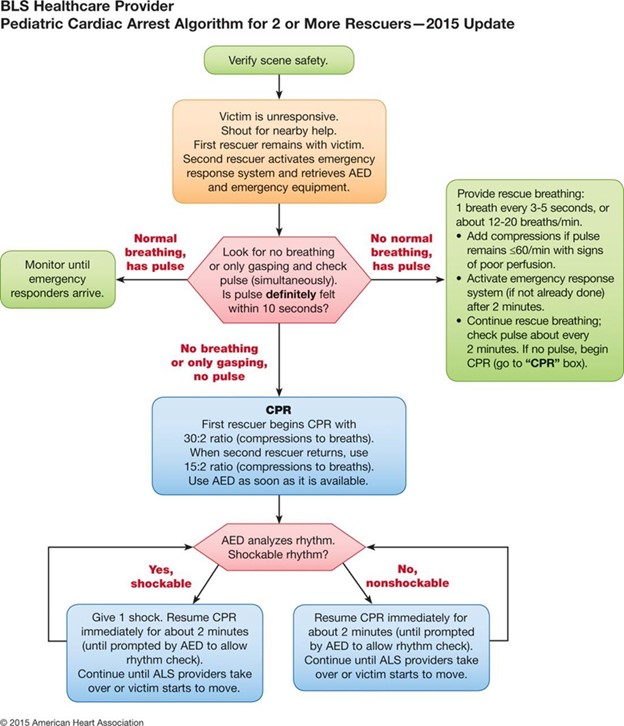
Pediatric Basic Life Support
Pediatric Basic Life Support (BLS) and Neonatal Resuscitation are indispensable skills for healthcare professionals, ensuring timely and effective interventions during pediatric emergencies.
Pediatric Assessment
- Scene Safety and Initial Assessment:
- Ensure Safety: Assess the safety of the scene for both rescuer and child.
- Assess Responsiveness: Check the child's responsiveness by tapping and shouting.
- Airway Management: Open the airway using appropriate maneuvers based on age (head-tilt-chin-lift for children and jaw-thrust for infants).
- Breathing Assessment:
- Check Breathing: Assess breathing by observing chest rise and fall, listening for breath sounds, and feeling for airflow.
- Ventilation: If breathing is absent or inadequate, provide rescue breaths using a bag-mask device with proper-sized masks for infants and children.
- Circulation Assessment:
- Check Pulse: Assess the pulse (carotid for infants, femoral for older children) for no more than 10 seconds.
- Chest Compressions: If pulse is absent, initiate chest compressions at a rate of 100-120 compressions per minute using appropriate techniques for infants and older children.
Neonatal Resuscitation
- Initial Steps:
- Clear Airway: Clear the neonate's airway using a bulb syringe to remove mucus and amniotic fluid.
- Provide Stimulation: Provide tactile stimulation (rubbing the back or feet) to stimulate breathing.
- Positive Pressure Ventilation (PPV):
- Bag-Mask Ventilation: Use a neonatal bag-mask device to provide PPV if the newborn is not breathing or has inadequate breathing efforts.
- Proper Technique: Ensure a proper seal and deliver gentle breaths, observing for chest rise.
- Chest Compressions for Neonates:
- Indications: Initiate chest compressions if the heart rate remains below 60 bpm despite adequate ventilation.
- Technique: Use two fingers in the center of the chest, compressing to approximately one-third the depth of the chest.
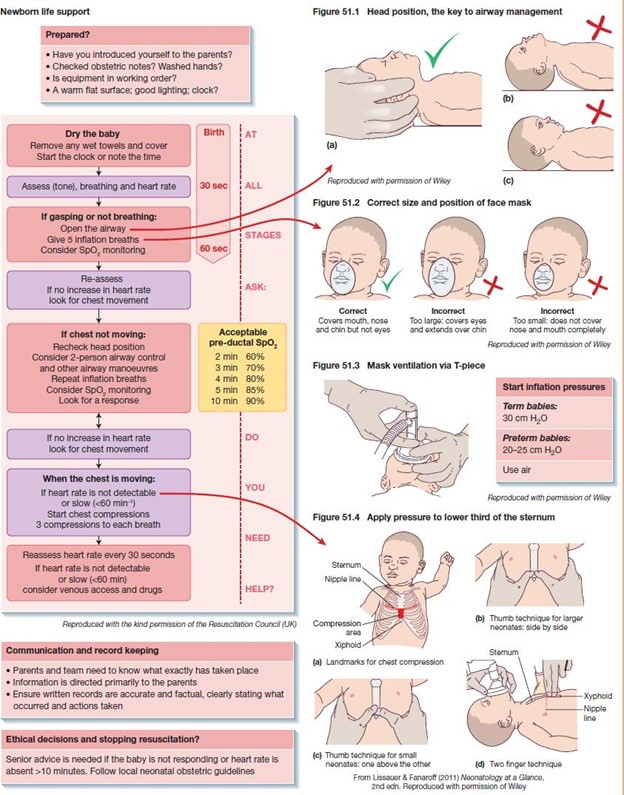
Special Considerations
- Choking Management:
- Perform back blows and chest thrusts (for infants) or abdominal thrusts (for older children) if conscious and choking.
- Medications and Advanced Interventions:
- Epinephrine: Administer epinephrine for bradycardia unresponsive to ventilation and chest compressions.
- Advanced Airways: Consider advanced airway interventions such as endotracheal intubation for prolonged resuscitation efforts.
Team Dynamics
- Effective Communication:
- Clear Communication: Maintain clear and concise communication within the resuscitation team.
- Designated Roles: Assign specific roles (compressor, ventilator, medication administration) for efficient teamwork.
- Team Leader Role:
- Leadership: Appoint a team leader responsible for decision-making and coordination of efforts.
- Direction: Provide direction to team members, ensuring adherence to protocols and guidelines.
Post-Resuscitation Care
- Continuous Monitoring:
- Vital Signs: Continuously monitor vital signs, oxygen saturation, and cardiac rhythm.
- Clinical Assessment: Perform regular clinical assessments to gauge the child's overall condition.
- Transportation and Handoff:
- Transition of Care: Ensure a seamless transition of care during handoffs between healthcare providers.
- Documentation: Document all interventions, responses, and changes in the child's condition for accurate medical records.
Conclusion
In summary, pediatric BLS and neonatal resuscitation demand a comprehensive understanding of assessment techniques, interventions, and team dynamics. Healthcare professionals must master these skills to provide optimal care, ensuring the best possible outcomes for pediatric and neonatal patients in emergencies.
Pediatric Advanced Life Support (PALS)
Pediatric Advanced Life Support (PALS) is an advanced resuscitation course designed for healthcare professionals involved in caring for critically ill or injured infants and children.
The course is structured to equip healthcare providers with the knowledge and skills necessary to manage pediatric emergencies effectively.
Pediatric Assessment
- Primary Survey:
- A for Airway: Ensure a patent airway, using appropriate maneuvers (head-tilt-chin-lift for children and jaw-thrust for infants).
- B for Breathing: Assess breathing, administer oxygen if necessary, and provide ventilatory support using bag-mask ventilation or advanced airway devices.
- C for Circulation: Evaluate the child's circulation, assess pulses, and initiate chest compressions if needed.
- D for Disability: Evaluate the child's neurological status, including level of consciousness, pupil size, and motor responses.
- E for Exposure: Assess for signs of trauma, temperature abnormalities, and exposure to toxins.
- Secondary Survey:
- Focused History: Obtain a focused medical history from caregivers, emphasizing current illness, medications, and allergies.
- Physical Examination: Conduct a thorough physical examination, including heart and lung sounds, and assess for signs of shock or respiratory distress.
Interventions
- Airway Management:
- Endotracheal Intubation: Consider intubation for children with severe respiratory distress or failure.
- Supraglottic Airway Devices: Use supraglottic airway devices as an alternative airway management option.
- Ventilatory Support:
- Mechanical Ventilation: Initiate mechanical ventilation for children with respiratory failure or inadequate gas exchange.
- Capnography: Use capnography to monitor the effectiveness of ventilation and confirm correct placement of the endotracheal tube.
- Circulatory Support:
- Intravenous Access: Establish intravenous access for fluid resuscitation and administration of medications.
- Vasoactive Medications: Administer vasoactive medications such as epinephrine and dopamine in cases of shock and hemodynamic instability.
- Medications:
- Epinephrine: Administer epinephrine for pulseless arrest and severe bradycardia.
- Antiarrhythmics: Use antiarrhythmic medications like amiodarone or lidocaine for shock-refractory ventricular fibrillation or pulseless ventricular tachycardia.
Special Considerations
Cardiac Arrest Algorithms:
- Shockable Rhythms: Follow specific algorithms for pulseless ventricular tachycardia and ventricular fibrillation, emphasizing prompt defibrillation and high-quality CPR.
- Non-Shockable Rhythms: Implement guidelines for pulseless electrical activity (PEA) and asystole, focusing on reversible causes and appropriate interventions.
Post-Resuscitation Care:
- Therapeutic Hypothermia: Consider therapeutic hypothermia for children who remain comatose after resuscitation from cardiac arrest.
- Neurological Monitoring: Continuously monitor neurological status, including pupillary responses and Glasgow Coma Scale (GCS) scores.
Team Dynamics
- Effective Communication:
- Closed-Loop Communication: Use closed-loop communication to ensure accurate and clear communication among team members.
- Team Leader Role: Designate a team leader responsible for coordinating efforts, making decisions, and ensuring adherence to protocols.
- Debriefing:
- Post-Event Debriefing: Conduct a debriefing session after the resuscitation event to review the case, identify areas for improvement, and enhance team performance.
Conclusion
In conclusion, pediatric ALS demands a sophisticated understanding of pediatric assessment, advanced airway management, pharmacological interventions, and effective team dynamics. Healthcare professionals must master these skills to deliver high-quality care during pediatric emergencies, ultimately improving outcomes and saving young lives.
Pediatric Emergencies
Pediatric emergencies demand swift and precise actions from healthcare providers. Recognizing the signs and symptoms of various pediatric emergencies is crucial for timely intervention, which can significantly impact outcomes.
Fever and Febrile Seizures
- Recognition:
- Fever: Elevated body temperature, often indicative of an underlying infection or illness.
- Febrile Seizures: Seizures occurring in association with a high fever, often seen in children between 6 months and 5 years of age.
- Management:
- Fever: Focus on fever management with antipyretics (such as acetaminophen) and adequate hydration.
- Febrile Seizures: Ensure the child's safety during the seizure, protect the airway, and monitor vital signs. Post-seizure, assess for any signs of serious illness or complications.
Anaphylaxis
- Recognition:
- Rapid Onset: Sudden and severe onset of symptoms, including difficulty breathing, swelling of the face and throat, and a rapid, weak pulse.
- Trigger: Often triggered by allergens such as certain foods, insect stings, or medications.
- Management:
- Epinephrine: Administer epinephrine immediately via auto-injector to reverse symptoms.
- Airway Management: Ensure a patent airway, administer supplemental oxygen, and be prepared for advanced airway interventions if necessary.
Poisoning
- Recognition:
- Various Symptoms: Symptoms can range from nausea and vomiting to confusion, seizures, or loss of consciousness.
- History: Obtain a thorough history, including potential exposure to toxic substances.
- Management:
- Activated Charcoal: Administer activated charcoal if indicated and within the appropriate timeframe.
- Supportive Care: Provide supportive care, maintain airway, and administer antidotes if available for specific toxins.
Foreign Body Aspiration
- Recognition:
- Sudden Choking: Sudden onset of coughing, gagging, or wheezing, indicating a possible foreign body aspiration.
- Ineffective Cough: Inability to cough forcefully, suggesting airway obstruction.
- Management:
- Back Blows and Abdominal Thrusts: Perform back blows and abdominal thrusts (Heimlich maneuver) to dislodge the foreign body.
- Advanced Airway Management: If unsuccessful, consider advanced airway techniques or chest thrusts in infants.
Head Trauma
- Recognition:
- Altered Mental Status: Any alteration in consciousness, from mild confusion to loss of consciousness.
- Vomiting: Persistent vomiting following a head injury may indicate increased intracranial pressure.
- Management:
- Stabilization: Stabilize the cervical spine if trauma is suspected and maintain a patent airway.
- Neurological Assessment: Conduct a thorough neurological assessment, including Glasgow Coma Scale (GCS) scoring.
- Imaging: Consider imaging studies (CT scan) based on clinical assessment and guidelines.
Shock
- Recognition:
- Hypotension: Low blood pressure, weak or absent pulses, and tachycardia.
- Altered Perfusion: Cool, clammy skin, delayed capillary refill, and altered mental status.
- Management:
- Fluid Resuscitation: Administer fluid boluses (normal saline) for hypovolemic shock.
- Inotropic Support: Consider inotropic support (epinephrine, dopamine) for cardiogenic shock.
- Identify and Treat Underlying Cause: Identify and treat the underlying cause, whether it's sepsis, dehydration, or cardiac dysfunction.
Cardiac Arrest
- Recognition:
- Absence of Pulse: Verify absence of pulse and unresponsiveness.
- Initiate CPR: Begin high-quality CPR immediately, emphasizing chest compressions and ventilation.
- Management:
- Defibrillation: Use an AED to deliver shocks in case of shockable rhythms (ventricular fibrillation, pulseless ventricular tachycardia).
- Medications: Administer epinephrine and antiarrhythmic medications per guidelines.
- Advanced Airway: Consider advanced airway management (endotracheal intubation) for sustained cardiac arrest.
Conclusion
In summary, recognizing and effectively managing pediatric emergencies requires knowledge, skills, and rapid decision-making.
Healthcare providers must be well-versed in these guidelines to provide optimal care, ultimately improving outcomes for pediatric patients during critical situations.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Pediatric Emergency Care
This filled cannot be empty

