Please set your exam date
Analgesics and Pain Management Medications
Study Questions
Introduction
A nurse is caring for a client who has chronic low back pain and is prescribed acetaminophen 650 mg every 4 hours as needed. Which of the following statements by the client indicates a need for further teaching by the nurse?
Explanation
Taking acetaminophen with food is not necessary to prevent stomach upset, unlike some other pain relievers such as aspirin or ibuprofen.Acetaminophen can be taken with or without food.
Choice A is wrong because it is true that the maximum daily dose of acetaminophen should not exceed 4,000 mg to avoid liver damage.
Choice B is wrong because it is true that alcohol should be avoided while taking acetaminophen, as it can increase the risk of liver toxicity.
Choice C is wrong because it is true that acetaminophen content should be checked in other medications, such as cold and flu remedies, to avoid accidental overdose.
A nurse is preparing to administer fentanyl patches to a client who has cancer pain. The client asks the nurse how long it will take for the patches to work. Which of the following responses should the nurse make?
Explanation
You may need supplemental pain medication for the first day.This is because fentanyl patches are used for long-lasting pain relief for constant, around-the-clock cancer pain, but they take some time to reach their full effect.According to one source, it can take up to 24 hours for the fentanyl patch to reach steady-state plasma concentrations. Therefore, you may need additional painkillers for breakthrough pain during the first day of using the patch.
Choice A is wrong because you should not feel some pain relief within 15 minutes. Fentanyl patches are not immediate acting and they do not work that fast.Fentanyl nasal sprays, lollipops, injections, sublingual tablets and sprays are immediately acting and used for breakthrough pain.
Choice B is wrong because you will not have maximum pain relief after one patch change.Fentanyl patches are usually changed every 72 hours, but the pain relief does not depend on how many times you change the patch. It depends on the dose of fentanyl that is appropriate for your level of pain.
Choice D is wrong because you will not have a constant level of pain relief throughout the day.Fentanyl patches provide steady-state plasma concentrations of fentanyl, but this does not mean that your pain will be constant. Your pain may vary depending on different factors such as movement, activity, stress, or other causes.You may still need breakthrough pain medication as needed.
A nurse is assessing a client who has a history of chronic pain and is using a transcutaneous electrical nerve stimulation (TENS) unit at home. The client reports that the TENS unit is not helping with the pain anymore.
Which of the following actions should the nurse take?
Explanation
Instruct repositioning the electrodes to different locations on the skin.This is because the electrical impulses from the TENS unit may lose their effectiveness over time if they stimulate the same nerve endings repeatedly.By changing the location of the electrodes, the TENS unit can target different nerves and provide more pain relief.
Choice A is wrong because increasing the intensity of the electrical stimulation may cause skin irritation, discomfort, or even burns.The intensity should be adjusted to a comfortable level that does not cause pain or muscle twitching.
Choice B is wrong because discontinuing the use of the TENS unit for a week may result in increased pain and reduced function.The TENS unit should be used as prescribed by the doctor or physical therapist for optimal pain management.
Choice C is wrong because applying ice packs to the skin before using the TENS unit may reduce blood flow and impair nerve conduction.The skin should be clean and dry before applying the electrodes.
A nurse is educating a client who has fibromyalgia about pain management strategies. Which of the following interventions should the nurse include in the teaching?
Explanation
The nurse should include all of the following interventions in the teaching for a client who has fibromyalgia:
• Perform stretching exercises daily.Stretching can help improve flexibility, reduce stiffness, and relieve pain.
• Apply heat packs to painful areas.Heat can help reduce muscle tension and increase blood flow, which can also ease pain.
• Limit intake of caffeine and alcohol.Caffeine and alcohol can interfere with sleep quality, which is important for managing fibromyalgia symptoms.
Choice A is wrong because it is only one of the possible interventions, not the only one.
Choice B is wrong for the same reason.
Choice C is wrong because it does not address the physical aspects of fibromyalgia pain management.
A nurse is reviewing the medication administration record of a client who is receiving morphine sulfate 10 mg IV every 2 hours as needed for severe postoperative pain.
Which of the following medications should the nurse identify as an adjuvant analgesic that can enhance the effect of morphine? (Select all that apply)
Explanation
Amitriptyline, dexamethasone and gabapentin are examples of adjuvant analgesics, which are drugs that are not primarily designed to control pain but have an analgesic effect on their own or when used with other pain medications.They are especially useful for neuropathic pain and pain syndromes like fibromyalgia.
Choice C is wrong because ondansetron is an antiemetic, which is used to treat nausea and vomiting, not pain.
Choice E is wrong because lidocaine is a local anaesthetic, which blocks nerve impulses in a specific area of the body, not a systemic analgesic.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
A nurse is caring for a patient who is taking NSAIDs for arthritis.
Which of the following is a common side effect of NSAIDs?
Explanation
Gastrointestinal irritation is a common side effect of NSAIDs.NSAIDs can cause stomach problems such as indigestion, nausea, vomiting, diarrhoea, constipation, bleeding and ulcers.Taking NSAIDs with food, milk or antacids may help reduce these side effects.
Choice A is wrong because hypertension is not a common side effect of NSAIDs.However, NSAIDs can increase blood pressure in some people, especially if they have high blood pressure or take blood pressure medications.
Choice B is wrong because hypotension is not a common side effect of NSAIDs.NSAIDs do not lower blood pressure, but they may reduce the effect of some blood pressure medications.
Choice D is wrong because bradycardia is not a common side effect of NSAIDs.NSAIDs do not affect the heart rate, but they may increase the risk of heart attack and stroke in some people, especially if they have heart disease or take high doses for a long time.
A nurse is caring for a patient who is taking NSAIDs for arthritis. The patient reports experiencing gastrointestinal irritation after taking the medication.
Which of the following statements by the patient indicates an understanding of the teaching?
Explanation
The patient should report any signs of gastrointestinal bleeding to their healthcare provider. NSAIDs can cause gastrointestinal irritation by blocking the COX-1 enzyme, which protects the lining of the stomach from acid.This can lead to ulcers and internal bleeding in some cases.Therefore, the patient should be aware of the symptoms of gastrointestinal bleeding, such as black or bloody stools, abdominal pain, or vomiting blood.
Choice A is wrong because taking NSAIDs on an empty stomach can increase the risk of gastrointestinal irritation and ulcers.The patient should take NSAIDs with food or milk to reduce stomach acid exposure.
Choice B is wrong because avoiding alcohol while taking NSAIDs is not enough to prevent gastrointestinal irritation.Alcohol can also irritate the stomach lining and increase the risk of bleeding, but it does not eliminate the effect of NSAIDs on the COX-1 enzyme.
Choice D is wrong because taking NSAIDs with antacids may not prevent gastrointestinal irritation and ulcers.Antacids can neutralize some of the stomach acids, but they do not affect the COX-1 enzyme or the prostaglandins that protect the stomach lining.The patient may need a prescription medication such as a proton pump inhibitor or misoprostol to reduce the risk of NSAID-induced ulcers.
A client is prescribed selective COX-2 inhibitors for pain relief.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
These medications have less gastrointestinal and bleeding side effects than nonselective COX inhibitors.This is because selective COX-2 inhibitors block only COX-2 enzymes, which are mainly involved in inflammation, and do not affect COX-1 enzymes, which help protect the stomach and intestinal lining and control blood clotting.
Choice A is wrong because these medications do not block both COX-1 and COX-2 enzymes, but only COX-2 enzymes.
Choice B is wrong because it is an incomplete statement.These medications do block only COX-2 enzymes, but this does not explain how they differ from nonselective COX inhibitors.
Choice D is wrong because it is a potential adverse effect of these medications, not a benefit.These medications may increase the risk of cardiovascular events such as myocardial infarction and stroke by reducing the production of prostacyclin, which inhibits platelet aggregation and vasodilation.
A nurse is caring for a patient who is prescribed nonselective COX inhibitors for pain relief.
Which of the following statements by the nurse indicates an understanding of the medication?
Explanation
Nonselective COX inhibitors are indicated for mild to moderate pain caused by inflammation, injury, surgery, dysmenorrhea, headache, fever, and cancer. This statement reflects an understanding of the medication’s mechanism of action and indications.
Choice A is wrong because nonselective COX inhibitors block both COX-1 and COX-2 enzymes.Blocking COX-1 can cause gastrointestinal and bleeding side effects.
Choice B is wrong because nonselective COX inhibitors have more gastrointestinal and bleeding side effects than selective COX-2 inhibitors.This is because selective COX-2 inhibitors spare the COX-1 enzyme that protects the stomach and intestinal lining.
Choice D is wrong because nonselective COX inhibitors are not available in intravenous or intra-articular forms.Only selective COX-2 inhibitors such as celecoxib have these formulations.
A nurse is caring for a patient who is taking NSAIDs for arthritis.
Which of the following instructions should the nurse include in the teaching? Select all that apply.
Explanation
The nurse should instruct the patient to take NSAIDs with food or milk and avoid alcohol while taking NSAIDs.This is because NSAIDs can cause stomach irritation, ulcers and bleeding by interfering with the protective lining of the stomach.Taking NSAIDs with food or milk can help reduce this risk, while alcohol can increase it.
Choice C is wrong because taking NSAIDs on an empty stomach can increase the risk of stomach problems.Choice D is correct but not complete, as the nurse should also teach the patient how to prevent gastrointestinal bleeding, not just report it.Choice E is wrong because taking NSAIDs with antacids can reduce their effectiveness and increase the risk of kidney problems.
Acetaminophen
A nurse is reviewing the medication history of a client who has a prescription for acetaminophen.
Which of the following medications should the nurse identify as increasing the risk of hepatotoxicity when taken with acetaminophen?
Explanation
Carbamazepine is an anticonvulsant drug that can induce the activity of cytochrome P450 enzymes in the liver.These enzymes are responsible for metabolizing acetaminophen into a toxic intermediate called N-acetyl-p-benzoquinone imine (NAPQI), which can cause liver injury by depleting glutathione and covalently binding to cellular proteins. Therefore, taking carbamazepine with acetaminophen can increase the risk of hepatotoxicity by enhancing the formation of NAPQI.
Choice A is wrong because warfarin is an anticoagulant drug that does not affect the metabolism of acetaminophen.However, acetaminophen can increase the anticoagulant effect of warfarin by inhibiting its metabolism, which can increase the risk of bleeding.
Choice C is wrong because furosemide is a diuretic drug that does not interact with acetaminophen.However, furosemide can cause dehydration and electrolyte imbalance, which can affect liver function and increase the susceptibility to acetaminophen-induced liver injury.
Choice D is wrong because ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that does not affect the metabolism of acetaminophen.However, ibuprofen can cause gastrointestinal irritation and renal impairment, which can also increase the risk of acetaminophen-induced liver injury.Additionally, taking both acetaminophen and ibuprofen can increase the risk of overdose and toxicity.
A nurse is teaching a client who has a new prescription for acetaminophen about the signs of overdose.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
This statement indicates that the client understands that abdominal pain and nausea are signs of acetaminophen overdose, which can cause liver damage.
The client should seek medical attention immediately if these symptoms occur.
Choice B is wrong because drinking plenty of fluids does not prevent kidney damage from acetaminophen overdose.In fact, dehydration can worsen the toxicity of acetaminophen.
Choice C is wrong because acetaminophen does not cause hypoglycemia (low blood sugar).Hypoglycemia is more likely to occur with drugs that lower blood sugar, such as insulin or sulfonylureas.
Choice D is wrong because acetaminophen does not cause dry mouth or sore throat.These are not signs of acetaminophen overdose and do not require medical attention.
A nurse is caring for a client who has arthritis and takes acetaminophen daily for pain relief. The client asks the nurse why acetaminophen does not reduce the inflammation in his joints.
Which of the following responses should the nurse give?
Explanation
Acetaminophen works by blocking prostaglandins in your brain, but not in your peripheral tissues. Prostaglandins are substances that cause pain and inflammation. By blocking them in the brain, acetaminophen reduces the perception of pain, but does not affect the inflammation in the joints.
Choice B is wrong because acetaminophen does not inhibit cyclooxygenase-2 (COX-2) enzyme, which is involved in the synthesis of prostaglandins. COX-2 inhibitors are a different class of drugs that can reduce both pain and inflammation.
Choice C is wrong because acetaminophen does not decrease the production of leukotrienes, which are another type of inflammatory mediators. Leukotriene inhibitors are used to treat asthma and allergic rhinitis.
Choice D is wrong because acetaminophen does not reduce the activity of natural killer cells, which are part of the immune system and can destroy infected or abnormal cells.
Natural killer cells are not directly related to pain or inflammation.
A nurse is administering acetaminophen to a child who has a fever caused by immunization.
Which of the following forms of acetaminophen should the nurse use?
Explanation
The nurse should use oral liquid acetaminophen to administer the drug to a child who has a fever caused by immunization.This is because oral liquid is easier to swallow and measure for children than oral tablets or capsules.Oral liquid acetaminophen also has a faster onset of action than rectal suppositories.
Choice A is wrong because oral tablets are not suitable for children who may have difficulty swallowing pills.Crushing the tablets may alter the drug’s effectiveness or cause adverse effects.
Choice C is wrong because rectal suppositories are not the preferred route of administration for acetaminophen in children.Rectal suppositories may cause irritation, leakage, or expulsion of the drug.They also have a slower onset of action and variable absorption than oral liquid.
Choice D is wrong because intravenous injection is not an over-the-counter form of acetaminophen.Intravenous injection is a prescription form that is used for severe pain or fever in hospitalized patients.It also requires special equipment and monitoring that are not available at home.
A nurse is preparing to administer acetaminophen to a client who has a fever.
Which of the following actions should the nurse take? (Select all that apply)
Explanation
• Choice B: Assess the client’s liver function tests.This is correct because acetaminophen is metabolized by the liver and can cause liver injury in the case of overdose or in patients with compromised liver function.Therefore, the nurse should check the client’s baseline liver function tests and monitor them for any signs of hepatotoxicity, such as elevated liver enzymes.
• Choice C: Verify the dosage with another nurse.This is correct because acetaminophen is a high-alert medication that requires a second nurse to verify the dosage calculation prior to administration.
This is to ensure client safety and prevent medication errors, such as giving too much or too little of the drug.
• Choice D: Ask the client about any allergies.This is correct because acetaminophen can cause allergic reactions in some people, such as rash, itching, swelling, or anaphylaxis.
Therefore, the nurse should ask the client about any history of allergies to acetaminophen or other medications before giving the drug.
• Choice E: Monitor the client’s temperature.This is correct because acetaminophen is used to reduce fever, and the nurse should monitor the client’s temperature to evaluate the effectiveness of the drug and adjust the dosage accordingly.
• Choice A: Check the client’s blood pressure.This is wrong because acetaminophen does not affect blood pressure significantly, and checking the client’s blood pressure is not a priority action when administering acetaminophen for fever.
The nurse should focus on other vital signs, such as temperature, pulse, and respiratory rate.
Normal ranges for liver function tests are:
• AST: 10 to 40 U/L
• ALT: 7 to 56 U/L
• ALP: 45 to 115 U/L
• Bilirubin: 0.1 to 1.2 mg/dL
Opioid Analgesics
A nurse is caring for a client who is receiving intravenous morphine for postoperative pain.
The nurse should monitor the client for which adverse effects of morphine?
Explanation
Morphine is an opioid analgesic that can cause respiratory depression by decreasing the sensitivity of the respiratory centre in the brainstem to carbon dioxide levels. This can lead to hypoventilation, hypoxia, and even death if not treated promptly.
Choice B is wrong because hyperthermia is not a common adverse effect of morphine.Morphine can cause sweating and flushing, but it does not increase body temperature.
Choice C is wrong because tachycardia is not a common adverse effect of morphine.Morphine can cause bradycardia by stimulating the vagus nerve and reducing sympathetic activity.
Choice D is wrong because hypertension is not a common adverse effect of morphine.Morphine can cause hypotension by dilating peripheral blood vessels and reducing cardiac output.
A nurse is administering nalbuphine to a client who has moderate pain. The client asks the nurse how this drug works.
What should the nurse say?
Explanation
Nalbuphine is a mixed opioid agonist-antagonist that binds to and activates kappa receptors, producing pain relief and sedation and blocking mu receptors, preventing respiratory depression. This makes it a safer option than pure opioid agonists for clients who have moderate pain and are at risk of respiratory complications.
Choice A is wrong because it describes the mechanism of action of pure opioid agonists, such as morphine or fentanyl, which bind to and activate both mu and kappa receptors, producing strong pain relief and sedation, but also respiratory depression and dependence.
Choice B is wrong because it describes the mechanism of action of partial opioid agonists, such as buprenorphine or tramadol, which bind to and partially activate mu receptors, producing moderate pain relief and less respiratory depression than pure opioid agonists, but also less analgesia.
Choice D is wrong because it describes the mechanism of action of opioid antagonists, such as naloxone or naltrexone, which bind to and block both mu and kappa receptors, reversing the effects of other opioids, but also precipitating withdrawal symptoms.
A nurse is preparing to administer codeine to a client who has a cough. The client asks the nurse why codeine is used for cough suppression.
What should the nurse say?
Explanation
Codeine acts on opioid receptors in your brainstem to suppress the activity of your cough centre and decrease your urge to cough. This is how codeine works as an antitussive or cough suppressant.
Choice A is wrong because codeine does not block pain signals from reaching your cough centre.Codeine blocks pain signals from reaching your brain and spinal cord, which is how it works as an analgesic or pain reliever.
Choice B is wrong because codeine does not act on opioid receptors in your lungs.Codeine does not reduce inflammation or mucus production that triggers your cough reflex.
Choice D is wrong because codeine does not act on opioid receptors in your throat.Codeine does not numb the nerve endings that stimulate your cough reflex.
A nurse is reviewing the medication history of a client who is prescribed buprenorphine for chronic pain.
The nurse should identify that which medication can interact with buprenorphine and increase the risk of serotonin syndrome?
Explanation
Fluoxetine can interact with buprenorphine and increase the risk of serotonin syndrome. Serotonin syndrome is a serious drug reaction that occurs when there is too much serotonin in the body. It can cause symptoms such as agitation, confusion, muscle rigidity, fever, seizures and coma.
Choice B is wrong because metformin is not known to have any serotonergic effects or interact with buprenorphine.
Choice C is wrong because omeprazole is not known to have any serotonergic effects or interact with buprenorphine.
Choice D is wrong because lisinopril is not known to have any serotonergic effects or interact with buprenorphine.
A nurse is teaching a client who has chronic pain about the use of transdermal fentanyl.
Which statements by the client indicate understanding of the teaching? Select all that apply.
Explanation
The client should change the patch every 72 hours and apply it to a clean, dry, and hairless area of skin. This ensures that the patch adheres well and delivers the medication at a steady rate.
Choice C is wrong because the client should not cut the patch in half.This can damage the patch and cause fentanyl to leak out or be absorbed too quickly.
Choice D is wrong because the client should avoid exposing the patch to heat sources, such as heating pads, electric blankets, saunas, or hot tubs.Heat can increase the absorption of fentanyl and cause an overdose.
Choice E is wrong because the client should dispose of the used patch by folding it onto itself and placing it in a sealed container or a special disposal pouch.Flushing the patch down the toilet can contaminate the water supply and pose a risk to others.
Mixed Agonists/Antagonists
A nurse is caring for a client who has cancer and is receiving buprenorphine (Buprenex) for pain management.
The nurse should monitor the client for which of the following adverse effects of this medication?
Explanation
Buprenorphine is an opioid medication that can cause respiratory depression, constipation, and dysphoria as adverse effects. Respiratory depression is a serious condition that can lead to coma and death if not treated promptly. Constipation is a common side effect of opioids that can cause discomfort and bowel obstruction. Dysphoria is a state of unease or dissatisfaction that can affect the mood and mental health of the patient.
Choice A is wrong because respiratory depression is not the only adverse effect of buprenorphine.
Choice B is wrong because constipation is not the only adverse effect of buprenorphine.
Choice C is wrong because dysphoria is not the only adverse effect of buprenorphine.
A nurse is preparing to administer butorphanol (Stadol) to a client who has severe pain after surgery. The client tells the nurse that he has been taking morphine (Duramorph) for several months for chronic back pain.
Which of the following responses should the nurse make?
Explanation
You might experience some withdrawal symptoms when you receive this medication.This is because butorphanol (Stadol) is anagonist-antagonist opioidthat can causeabstinence syndromein opioid-dependent clients. Abstinence syndrome is a group of symptoms that occur when a person who is physically dependent on opioids suddenly stops taking them.Some of the symptoms include vomiting, abdominal cramps, hypertension, fever, and anxiety.
Choice B is wrong because you will not need a higher dose of this medication to achieve pain relief.Butorphanol (Stadol) is a potent analgesic that can provide effective pain relief at lower doses than morphine.
Choice C is wrong because you can take this medication if you have a history of opioid dependence, but you should be monitored for signs of withdrawal and adverse effects.Butorphanol (Stadol) has a lower risk of abuse and respiratory depression than morphine.
Choice D is wrong because you will not have less risk of respiratory depression with this medication.Butorphanol (Stadol) can still cause respiratory depression, especially if taken with other CNS depressants or at high doses.You should have your respiratory rate checked before and after receiving this medication, and an opioid antagonist such as naloxone should be available in case of overdose.
A nurse is reviewing the medical record of a client who is receiving nalbuphine (Nubain) for postoperative pain.
The nurse should identify that which of the following findings is a contraindication for this medication?
Explanation
The client has a history of asthma.This is a contraindication for nalbuphine (Nubain) because it can cause significant respiratory depression and exacerbate bronchospasm.Nalbuphine is also contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
Choice B is wrong because a blood pressure of 150/90 mm Hg is not a contraindication for nalbuphine.Nalbuphine has minimal effects on blood pressure and heart rate.
Choice C is wrong because a heart rate of 100/min is not a contraindication for nalbuphine.Nalbuphine has minimal effects on blood pressure and heart rate.
Choice D is wrong because a history of glaucoma is not a contraindication for nalbuphine.Nalbuphine does not increase intraocular pressure.
A nurse is administering dezocine (Dalgan) to a client who has moderate pain due to kidney stones.
The nurse should explain to the client that this medication works by which of the following mechanisms?
Explanation
Dezocine is apartial agonist of the μ-opioid receptorand anantagonist of the κ-opioid receptor.It binds with stereospecific receptors at many sites within the central nervous system (CNS) to alter processes affecting both the perception of pain and the emotional response to pain.
Choice A is wrong because dezocine does not block the transmission of pain impulses in the spinal cord.
That is the mechanism of action of local anesthetics.
Choice C is wrong because dezocine does not inhibit prostaglandin synthesis in peripheral tissues.
That is the mechanism of action of nonsteroidal anti-inflammatory drugs (NSAIDs).
Choice D is wrong because dezocine does not stimulate endorphin release in the central nervous system.
A nurse is teaching a client who has chronic pain about using a transdermal patch of pentazocine (Talwin).
Which of the following instructions should the nurse include? (Select all that apply.)
Explanation
The correct answers are Choices A, B, C, and E.
Choice A rationale:Applying the patch to a clean, dry, hairless area of skin is crucial for the proper absorption of the medication. The skin acts as a barrier to the outside environment and also as a reservoir for the slow release of the drug from the patch. If the skin is not clean, substances on the skin could interact with the medication and alter its absorption. If the skin is not dry, the patch may not adhere properly, which could lead to it falling off and the medication not being delivered. Hair on the skin can also interfere with the patch’s adhesion and the medication’s absorption.
Choice B rationale:Changing the patch every 24 hours is important to ensure a consistent delivery of the medication. The medication in the patch is designed to be released slowly over a certain period of time, typically 24 hours. After this time, the patch may not have enough medication left to provide effective pain relief. Additionally, the adhesive on the patch may not last longer than 24 hours, so the patch could fall off.
Choice C rationale:Removing the old patch before applying a new one is necessary to prevent an overdose of the medication. If the old patch is left on, the remaining medication in the old patch could be absorbed along with the medication in the new patch, leading to a higher dose than intended. This could result in side effects or a potentially dangerous overdose.
Choice D rationale:Disposing of the used patch in a sharps container is not necessary. Sharps containers are typically used for objects that can puncture the skin, such as needles. A used transdermal patch does not pose this risk. However, it is important to dispose of the patch safely where children or pets cannot reach it, as it may still contain some medication.
Choice E rationale:Avoiding exposing the patch to heat sources is important because heat can increase the absorption of the medication, which could lead to an overdose. Heat sources can include heating pads, hot tubs, heated water beds, heat or tanning lamps, saunas, hot baths, and direct sunlight.
Adjuvant Analgesics
A nurse is caring for a client who has neuropathic pain due to diabetic neuropathy.
Which of the following adjuvant analgesics can the nurse administer to this client?
Explanation
Amitriptyline is a tricyclic antidepressant that can be used as an adjuvant analgesic for neuropathic pain.It works by inhibiting the reuptake of serotonin and norepinephrine, which are neurotransmitters involved in pain modulation.
Choice B.Etidronate is wrong because it is a bisphosphonate that is used to treat osteoporosis and Paget’s disease of bone, not neuropathic pain.
Choice C.Methylphenidate is wrong because it is a stimulant that is used to treat attention deficit hyperactivity disorder (ADHD) and narcolepsy, not neuropathic pain.
Choice D.Hydroxyzine is wrong because it is an antihistamine that is used to treat allergic reactions, anxiety, and insomnia, not neuropathic pain.
A nurse is preparing to administer pamidronate to a client who has bone pain due to metastatic cancer.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The client should not take pamidronate with food because it can decrease the absorption of the medication and reduce its effectiveness.The client should take pamidronate on an empty stomach at least 2 hours before or after eating.
Choice A is wrong because drinking plenty of water before and after receiving pamidronate can help prevent dehydration and kidney damage.
Choice B is wrong because having a dental check-up before starting pamidronate can help prevent osteonecrosis of the jaw.
A nurse is reviewing the medication history of a client who has chronic pain and is prescribed dexamethasone as an adjuvant analgesic.
Which of the following statements by the client should alert the nurse to a possible adverse effect of this medication?
Explanation
This statement by the client should alert the nurse to a possible adverse effect of dexamethasone, which ishyperglycemia.Dexamethasone is a steroid medication that has analgesic, antiemetic, and anti-inflammatory properties, but it can also increase blood glucose levels by stimulating gluconeogenesis and reducing insulin sensitivity. The nurse should monitor the client’s blood glucose levels and report any signs of hyperglycemia, such as polydipsia, polyphagia, and polyuria.
Choice B is wrong because insomnia is a common side effect of dexamethasone, but not a serious adverse effect. The nurse should advise the client to take dexamethasone in the morning to reduce the risk of insomnia and to avoid caffeine and alcohol before bedtime.
Choice C is wrong because tingling and numbness in the feet are not related to dexamethasone use.They could indicate peripheral neuropathy, which could have other causes such as diabetes, vitamin B12 deficiency, or nerve compression. The nurse should assess the client’s feet for sensation, circulation, and skin integrity and refer the client to a neurologist if needed.
Choice D is wrong because bruising on the arms and legs is also a common side effect of dexamethasone, but not a serious adverse effect.Dexamethasone can cause skin thinning and fragility, which can lead to easy bruising and delayed wound healing. The nurse should instruct the client to avoid trauma to the skin and to apply pressure to any bleeding sites. Normal ranges for blood glucose are 70-110 mg/dL (3.9-6.1 mmol/L) for fasting and <140 mg/dL (<7.8 mmol/L) for postprandial.
A nurse is educating a client who has fibromyalgia about the use of pregabalin as an adjuvant analgesic.
Which of the following information should the nurse include in the education?
Explanation
Pregabalin can cause drowsiness, so avoid driving or operating machinery.This is a common side effect of pregabalin, which is a drug that is used to treat the pain of fibromyalgia.Pregabalin works by reducing the abnormal electrical activity in the brain that causes pain.
Choice A is wrong because pregabalin does not cause bone marrow suppression.This is a serious side effect of some other drugs, such as chemotherapy agents, but not pregabalin.
Choice B is wrong because pregabalin can cause weight gain, not weight loss.This is another common side effect of pregabalin, which may affect about 1 in 18 people who take it. Therefore, patients should monitor their weight and nutritional intake while taking pregabalin.
Choice D is wrong because pregabalin does not cause rash.This is a rare side effect of some other drugs, such as antibiotics, but not pregabalin.However, if patients develop any signs of allergic reaction to pregabalin, such as swelling of the face, lips, tongue, or throat, they should stop taking it and notify their provider immediately.
(Select all that apply) A nurse is teaching a client who has cancer pain about the use of adjuvant analgesics.
Which of the following statements should the nurse include in the teaching?
Explanation
Adjuvant analgesics are drugs that are not primarily designed to control pain, but have an analgesic effect on their own or when used with other pain medications.They are especially useful for neuropathic pain and pain syndromes like fibromyalgia.They can also help with cancer pain by reducing the dose or side effects of opioids, treating various types of pain that are difficult to manage with conventional analgesics, enhancing the efficacy of nonopioids or opioids, and relieving associated symptoms of pain such as anxiety or insomnia.
Choice C is wrong because adjuvant analgesics cannot cure the underlying cause of pain.They only help to manage the pain and improve the quality of life of the patient.
Routes, Doses, Onset, Duration, Peak, and Half-life of Various Analgesics
A nurse is teaching a client about the advantages and disadvantages of different routes of administration for analgesics.
Which of the following statements by the client indicates a need for further teaching?
Explanation
Rectal analgesics arenotfaster than oral ones but they may be uncomfortable.Rectal analgesics have a slower onset of action and lower bioavailability than oral analgesics.They may be useful when the oral route is contraindicated or unavailable, but they are not preferred by most patients.
Choice A is correct because oral analgesics are convenient and widely available, but they may irritate the stomach or cause gastrointestinal bleeding, especially NSAIDs.
Choice C is correct because intravenous analgesics are the most reliable and fast-acting route of administration, but they may cause infection or thrombophlebitis at the injection site.
Choice D is correct because intramuscular analgesics are the most precise route of administration in terms of dosage, but they may cause pain, hematoma, or nerve damage at the injection site.
A nurse is caring for a client who has severe pain and is receiving intravenous analgesics.
The client asks the nurse, “How long will it take for this medication to work?” What is the best response by the nurse?
Explanation
This is because intravenous analgesics have a rapid onset of action, usually within 1 to 2 minutes, and a peak effect at 2 to 6 minutes.The duration of action depends on the type and dose of the analgesic, but it is typically 30 to 60 minutes.
Choice A is wrong because it will not take that long for intravenous analgesics to work.
Choice C is wrong because it will take much longer than the actual onset of action.
Choice D is wrong because it will take much longer than the peak effect and the duration of action.
A nurse is administering a rectal analgesic to a client who cannot swallow or has nausea or vomiting.
The client says, “I don’t like this way of taking medication. Is there another option?” What is the best response by the nurse?
Explanation
This is because a transdermal patch can deliver a steady dose of analgesic through the skin without the need for swallowing or rectal administration.A transdermal patch may also have fewer side-effects than other routes of administration.
Choice A is wrong because an oral analgesic may not be suitable for a client who cannot swallow or has nausea or vomiting.An oral analgesic may also interact with other medications or food.
Choice C is wrong because an intramuscular injection may be painful, invasive, and cause bleeding or infection.An intramuscular injection may also require frequent administration and monitoring.
Choice D is wrong because a nasal spray may not be effective for severe pain or chronic conditions.A nasal spray may also cause irritation, congestion, or bleeding in the nasal passages.
A nurse is reviewing the pharmacokinetics of different routes of administration for analgesics with a nursing student.
The nurse asks the student, “Which route has the fastest onset and peak of action?” What is the correct answer by the student?
Explanation
This is because the intravenous route delivers the drug directly into the bloodstream, bypassing the first-pass metabolism in the liver and the absorption barriers in the gastrointestinal tract.This results in a faster onset and peak of action compared to other routes.
Choice A. Oral route is wrong because the oral route involves swallowing the drug, which then passes through the stomach and intestines before reaching the bloodstream.This route has a slower onset and peak of action due to factors such as gastric emptying time, food intake, and first-pass metabolism.
Choice B. Rectal route is wrong because the rectal route involves inserting the drug into the rectum, where it is absorbed by the rectal mucosa and enters the systemic circulation.This route has a similar onset and peak of action to the oral route but may have better absorption and less first-pass metabolism.
Choice D. Intramuscular route is wrong because the intramuscular route involves injecting the drug into a muscle, where it is absorbed by the capillaries and enters the bloodstream. This route has a slower onset and peak of action than the intravenous route, but faster than the oral and rectal routes.The rate of absorption depends on factors such as blood flow, muscle mass, and injection site.
A nurse is preparing to administer an oral analgesic to a client with moderate pain.
Which of the following factors should the nurse consider when choosing the appropriate dose and formulation? (Select all that apply)
Explanation
The onset, peak, duration and first-pass metabolism of the analgesic are important factors to consider when choosing the appropriate dose and formulation for a client with moderate pain.The onset determines how quickly the analgesic will start to relieve pain, the peak determines when the analgesic will have its maximum effect, the duration determines how long the analgesic will last, and the first-pass metabolism determines how much of the analgesic will be available in the systemic circulation after passing through the liver.
These factors affect the efficacy and safety of the analgesic.
Choice E is wrong because the gastrointestinal tolerance of the analgesic is not a factor that affects the dose and formulation of the oral analgesic.The gastrointestinal tolerance refers to how well the client can tolerate the side effects of the analgesic, such as nausea, vomiting, constipation or ulceration.
This factor may influence the choice of the analgesic, but not its dose and formulation.
Nursing Assessments, Interventions, and Education for Patients Receiving Analgesics
A nurse is preparing to administer acetaminophen to a client who has a fever.
Which of the following actions should the nurse take? (Select all that apply.)
Explanation
The nurse should take the following actions when administering acetaminophen to a client who has a fever:
• Check the client’s liver function testsbecause acetaminophen can cause hepatotoxicity and liver damage, especially in clients who have preexisting liver disease or who take high doses of the medication.
• Assess the client’s pain levelbecause acetaminophen is also an analgesic that can reduce pain and discomfort associated with fever.
• Monitor the client’s fluid intake and outputbecause fever can cause dehydration and fluid loss, and acetaminophen can also affect renal function and urine output.
• Ask the client about any history of alcohol usebecause alcohol can increase the risk of liver damage from acetaminophen, and clients who consume more than three alcoholic drinks per day should avoid taking acetaminophen.
Choice E is wrong because grapefruit juice does not interact with acetamin
A nurse is assessing a client who is receiving morphine sulfate for pain relief.
Which of the following findings indicates a potential adverse effect of the medication?
Explanation
This indicates a potential adverse effect of morphine sulfate, which is respiratory depression.Morphine sulfate can suppress the respiratory centre in the brainstem and decrease the rate and depth of breathing.A normal respiratory rate for an adult is 12 to 20 breaths/min.
Choice B is wrong because blood pressure of 130/80 mmHg is within the normal range for an adult.Morphine sulfate can lower blood pressure by dilating blood vessels, but this is not a serious adverse effect unless it causes hypotension or shock.
Choice C is wrong because a heart rate of 72 beats/min is within the normal range for an adult.Morphine sulfate can slow down the heart rate by stimulating the vagus nerve, but this is not a serious adverse effect unless it causes bradycardia or cardiac arrest.
Choice D is wrong because a temperature of 37°C (98.6°F) is within the normal range for an adult.Morphine sulfate does not affect body temperature significantly unless it causes an allergic reaction or overdose.
A nurse is teaching a client who has chronic low back pain about nonpharmacological pain management strategies.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
This statement indicates an understanding of the teaching because stretching exercises are one of the recommended nonpharmacological pain management strategies for chronic low back pain.Stretching exercises can improve flexibility, mobility, and blood circulation, as well as reduce muscle tension and stiffness.
Choice A is wrong because applying a heating pad to the back for 30 minutes every hour can cause skin burns and inflammation.Heat therapy should be used for no more than 15 to 20 minutes at a time, and only after 48 hours of injury.
Choice C is wrong because taking a hot bath with Epsom salt before going to bed can also cause skin irritation and dehydration.Epsom salt has not been proven to have any benefits for chronic low back pain.
Choice D is wrong because listening to some relaxing music while lying down is not a specific nonpharmacological pain management strategy for chronic low back pain.Although music can be a form of distraction and relaxation, it does not address the underlying causes of chronic low back pain, such as poor posture, muscle weakness, or inflammation.Music therapy may be more effective for other types of chronic pain, such as cancer-related pain.
A nurse is caring for a client who is receiving ibuprofen for arthritis pain.
The nurse should monitor the client for which of the following adverse effects of the medication?
Explanation
This is a sign oftinnitus, which is a common adverse effect of ibuprofen.Tinnitus can indicatesalicylism, a condition caused by excessive intake of salicylates, such as ibuprofen.Salicylism can also causefever, diaphoresis, nausea, and dizziness.
Choice B is wrong because “I have trouble sleeping at night.” is not a typical adverse effect of ibuprofen. It may be related to other factors, such as pain, stress, or caffeine intake.
Choice C is wrong because “I have dry mouth and thirst.” is not a typical adverse effect of ibuprofen. It may be related to dehydration, diabetes, or other medications.
Choice D is wrong because “I have blurred vision and headache.” is not a typical adverse effect of ibuprofen. It may be related to eye strain, migraine, or high blood pressure.
Some other serious side effects of ibuprofen that need immediate medical attention include:asthma, wheezing and shortness of breath; swelling of the face, lips or tongue, which may cause difficulty breathing or swallowing; black poo or blood in your vomit, which can be signs of bleeding in your stomach; swollen ankles, blood in your pee or not peeing at all, which can be signs of a kidney problem.
A nurse is reviewing the medication administration record of a client who is receiving tramadol for moderate pain.
The nurse should identify that which of the following medications can interact with tramadol and increase the risk of serotonin syndrome?
Explanation
Fluoxetine can interact with tramadol and increase the risk of serotonin syndrome. Serotonin syndrome is a serious drug reaction that occurs when there is too much serotonin in the body.It can cause symptoms such as agitation, confusion, muscle rigidity, seizures, and coma.
Choice A is wrong because omeprazole is not known to affect serotonin levels or interact with tramadol.
Choice B is wrong because metformin is not known to affect serotonin levels or interact with tramadol.
Choice D is wrong because lisinopril is not known to affect serotonin levels or interact with tramadol.
Fluoxetine is a selective serotonin reuptake inhibitor (SSRI) that increases the amount of serotonin available in the brain.
Tramadol is an opioid pain medication that also has some serotonin and norepinephrine reuptake inhibitory effects.When these two drugs are taken together, they can cause a buildup of excess serotonin that can lead to serotonin syndrome.
This is a rare but potentially life-threatening condition that requires immediate medical attention.
Normal ranges of serotonin in the blood are between 101 and 283 nanograms per milliliter (ng/mL).
Serotonin syndrome can occur when serotonin levels exceed 500 ng/mL.
Pain Assessment Tools and Scale Conclusion
A nurse is teaching a patient how to use a numeric rating scale (NRS) to assess pain intensity.
Which of the following statements by the nurse is appropriate?
Explanation
This statement is appropriate because it uses theNumeric Pain Rating Scale (NPRS)orNumerical Rating Scale (NRS), which is a subjective measure of pain intensity in adults, including those with chronic pain. It is a segmented numeric version of the visual analogue scale (VAS) in which a respondent selects a whole number from 0 (no pain at all) to 10 (worst imaginable pain).The scale is anchored by terms describing pain severity extremes.It can help assess the extent of pain, improve communication with healthcare providers, guide the diagnostic process, and track the progression of pain.
Choice B is wrong because it asks about the pain in the last 24 hours, which is not consistent with the NPRS.The NPRS usually asks about the pain intensity “in the last 24 hours” or average pain intensity, but not both.
Choice C is wrong because it uses a different scale, the visual analogue scale (VAS), which is a continuous line with no numbers or segments.The respondent marks a line on this scale to show how much pain they have right now.
Choice D is wrong because it uses another scale, the verbal rating scale (VRS), which is a list of words that describe different levels of pain intensity, such as mild, moderate, severe, etc.The respondent chooses a word from this list that best describes their pain right now.
A nurse is assessing a patient who has acute postoperative pain.
The nurse asks the patient to describe the quality of the pain. Which of the following responses by the patient indicates pain quality?
Explanation
Pain quality is the description of how the pain feels, such as throbbing, burning, stabbing, etcChoice A indicates pain quality by using the word “throbbing” to describe the sensation in the wound.
Choice B is wrong because it indicates pain onset, not pain quality. Pain onset is when the pain started or how long it lasts.
Choice C is wrong because it indicates pain effect, not pain quality. The pain effect is how the pain makes the person feel emotional, such as anxious, depressed, angry, etc.
Choice D is wrong because it indicates pain relief, not pain quality. Pain relief is what makes the pain go away or reduce in intensity. Normal ranges for pain intensity are usually measured on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain imaginableNormal ranges for pain quality are subjective and depend on the person’s experience and perception of pain.
A nurse is evaluating a patient’s response to analgesic therapy.
The nurse asks the patient if there is any change in the pain relief after taking the medication. Which of the following responses by the patient indicates a positive outcome of analgesic therapy?
Explanation
A positive outcome of analgesic therapy is to reduce pain to a tolerable level, not to eliminate it completely.
Choice A is wrong because it may indicate overmedication or adverse effects of the analgesic.
Choice C is wrong because it indicates inadequate pain relief and the need for a different or higher dose of analgesic.
Choice D is wrong because it indicates the side effects of the analgesic that may interfere with the patient’s quality of life.
A nurse is caring for a patient who has dementia and reports pain in the lower extremities.
The nurse observes that the patient grimaces and rubs his legs frequently. Which of the following behavioral pain assessment tools and scales should the nurse use to measure the patient’s pain level?
Explanation
The PAINAD scale is a behavioral pain assessment tool that is designed for patients with advanced dementia who cannot communicate verbally. The PAINAD scale evaluates five indicators of pain: breathing, vocalization, facial expression, body language, and consolability. Each indicator is scored from 0 to 2, and the total score ranges from 0 to 10.A higher score indicates more severe pain.
Choice A is wrong because the FLACC scale is a behavioural pain assessment tool that is used for children aged 2 months to 7 years who are unable to report their pain.The FLACC scale evaluates five categories of pain: face, legs, activity, cry, and consolability.
Choice C is wrong because the PASS scale is a behavioral pain assessment tool that is used for patients who are sedated or unconscious.The PASS scale evaluates four indicators of pain: movement of limbs, facial grimacing, muscle tension, and compliance with ventilation.
Choice D is wrong because the CAS scale is a behavioral pain assessment tool that is used for children aged 1 to 18 years who are awake and alert. The CAS scale evaluates six categories of pain: vocal, facial, activity, body and limbs, physiological, and consolability
A nurse is caring for a patient who has chronic back pain due to osteoarthritis.
Which of the following pain assessment tools and scales should the nurse use to measure multiple aspects of the patient’s pain experience and impact? (Select all that apply.)
Explanation
The McGill Pain Questionnaire (MPQ) and the Brief Pain Inventory (BPI) are pain assessment tools that measure multiple aspects of the patient’s pain experience and impact.The MPQ evaluates the sensory, affective, and evaluative dimensions of pain, as well as the pain intensity and location.The BPI assesses the severity of pain, the interference of pain with daily activities, and the response to pain treatment.
Choice C is wrong because the Wong-Baker FACES Pain Rating Scale (WBFPRS) is a simple tool that uses facial expressions to rate pain intensity from 0 to 10. It does not measure other aspects of pain such as quality, location, or impact.
Choice D is wrong because the Pain Disability Index (PDI) is a tool that measures the degree of functional impairment due to chronic pain. It does not measure the pain intensity or quality.
Choice E is wrong because the Faces Pain Scale (FPS) is another tool that uses facial expressions to rate pain intensity from 0 to 10. It is similar to the WBFPRS but does not use numbers. It also does not measure other aspects of pain such as quality, location, or impact.
More questions on this topics
A nurse is caring for a patient who reports pain in his left leg that he rates as an 8 on a scale from 0 to 10 and states that he feels tingling and numbness in his toes.
The patient has an order for morphine sulfate 2 mg IV bolus PRN every two hours for pain greater than 7, last administered three hours ago, and ibuprofen 400 mg PO PRN every four hours for pain less than or equal to 7, last administered six hours ago.
What action should the nurse take first?
Explanation
The correct answer is choice C. Assess the patient’s leg for circulation, sensation, and movement.
This is because the patient’s symptoms of pain, tingling, and numbness in his left leg could indicate a potential complication of impaired blood flow or nerve damage after surgery.The nurse should prioritize assessing the patient’s leg for any signs of compromised circulation, sensation, or movement before administering any pain medication.
Choice A is wrong because administering morphine sulfate 2 mg IV bolus without assessing the patient’s leg could mask the symptoms of a serious problem and delay appropriate interventions.Morphine sulfate is a potent opioid analgesic that can cause respiratory depression, sedation, and constipation.
Choice B is wrong because administering ibuprofen 400 mg PO without assessing the patient’s leg could also mask the symptoms of a serious problem and delay appropriate interventions.Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can cause gastrointestinal bleeding, renal impairment, and increased risk of cardiovascular events.
Choice D is wrong because reassessing the patient’s pain in 15 minutes without assessing the patient’s leg could result in the worsening of the patient’s condition and increased risk of complications.The nurse should not delay assessing the patient’s leg for any signs of impaired circulation, sensation, or movement.
A nurse is caring for a patient who has been receiving morphine via PCA pump following abdominal surgery two days ago and is scheduled to be switched to oral analgesics today.
The patient’s current settings are a demand dose of 1 mg, a lockout interval of 10 minutes, a four-hour limit of 30 mg, and a basal rate of 2 mg/hr.
The patient reports satisfactory pain relief with these settings and has received an average of 20 mg of morphine per four-hour period in addition to the basal rate over the past day.
The provider orders oxycodone/acetaminophen (Percocet) 5/325 mg PO every six hours PRN for pain, starting today at noon, and discontinues the PCA pump at that time.
What action should the nurse take?
Explanation
The correct answer is choice B. Administer Percocet every six hours around the clock for two days.
This is because the patient has been receiving a continuous infusion of morphine via a PCA pump, which means that they have a steady level of opioids in their system.
If the PCA pump is discontinued abruptly and the patient is switched to oral analgesics PRN, they may experience withdrawal symptoms and inadequate pain relief.
Therefore, the patient needs to receive a scheduled dose of oral opioids for at least two days to prevent a sudden drop in opioid blood concentration and to maintain adequate analgesia.
After two days, the patient’s pain level and opioid requirement may be reassessed and the oral analgesics may be tapered or given PRN as needed.
Choice A is wrong because a higher dose of Percocet is not necessary if the patient reports satisfactory pain relief with the current PCA settings.The equivalent oral dose of morphine for the patient’s average PCA consumption is about 120 mg per day (20 mg x 6 doses), which is equivalent to about 80 mg of oxycodone per day (1.5 x 120 mg).
The prescribed dose of Percocet is 20 mg of oxycodone per day (5 mg x 4 doses), which is about 25% of the patient’s previous opioid requirement.This reduction is appropriate to account for incomplete cross-tolerance between different opioids.
Choice C is wrong because stopping morphine one hour before giving Percocet will not prevent a gap in analgesia.The half-life of morphine is about 2 to 4 hours, which means that it takes about 10 to 20 hours for morphine to be eliminated from the body.
Therefore, stopping morphine one hour before giving Percocet will not significantly reduce the morphine blood concentration and will not avoid the risk of additive effects or overdose.
Choice D is wrong because giving Percocet only if the patient reports breakthrough pain will not provide adequate pain relief for the patient who has been receiving a continuous infusion of morphine via a PCA pump.
The patient may experience withdrawal symptoms and increased pain sensitivity if the opioid blood concentration drops suddenly.
Therefore, the patient needs to receive a scheduled dose of oral opioids for at least two days to prevent a gap in analgesia and to allow a smooth transition from IV to oral opioids.
A nurse is teaching a client who has chronic pain about nonpharmacological pain management techniques.
Which of the following statements by the client indicates an understanding of the teaching? (Select all that apply.).
Explanation
The correct answer is choice A, C and E. These statements indicate that the client understands the teaching about nonpharmacological pain management techniques.
• Choice A is correct becausemeditationcan help the client relax and cope with pain by reducing stress and anxiety.
• Choice C is correct becausedistractioncan help the client divert attention from pain by engaging in enjoyable or stimulating activities.
• Choice E is correct becauseheatcan help the client soothe the painful area by increasing blood flow and relaxing muscles.
• Choice B is wrong becausecold packsshould not be applied to the painful area for more than15 minutesat a time, as they can cause tissue damage or frostbite.
• Choice D is wrong becausemassageshould not be done with firm pressure, as it can aggravate the pain or cause injury.Gentle massage may be beneficial for some clients.
A client with osteoarthritis has been prescribed celecoxib (Celebrex). The nurse should instruct the client to report which of the following adverse effects immediately?
Explanation
The correct answer is choice C) Chest pain.
This is because chest pain can be a sign of a serious cardiovascular event, such as a heart attack or stroke, which can be fatal.
Celecoxib is a nonsteroidal anti-inflammatory drug (NSAID) that belongs to the class of cyclooxygenase-2 (COX-2) inhibitors.These drugs can increase the risk of cardiovascular thrombotic events, especially in patients with a history of heart disease or risk factors.
Therefore, the nurse should instruct the client to report chest pain immediately and seek emergency medical attention.
Choice A) Constipation is wrong because it is not a common or serious side effect of celecoxib.
Constipation can be caused by many factors, such as diet, dehydration, lack of exercise, or other medications.It can be managed by increasing fluid and fiber intake, using laxatives or stool softeners as needed, and consulting a doctor if it persists or worsens.
Choice B) Nausea is wrong because it is a common but mild side effect of celecoxib that usually goes away with time or can be reduced by taking the medication with food or milk.
Nausea is not a sign of a serious adverse reaction and does not require immediate medical attention.
Choice D) Headache is wrong because it is also a common but mild side effect of celecoxib that can be treated with over-the-counter pain relievers, such as acetaminophen or ibuprofen.
However, the client should avoid taking aspirin or other NSAIDs with celecoxib, as this can increase the risk of gastrointestinal bleeding and ulcers
Which statement made by a client taking aspirin indicates an understanding of its use?
Explanation
The correct answer is choice D) “Aspirin can cause gastrointestinal bleeding.”
This is because aspirin is a salicylate that works by reducing substances in the body that cause pain, fever, and inflammation, but also prevents blood clots from forming in the arteries.This can increase the risk of bleeding, especially in the stomach or gut.
Choice A) “Aspirin can be taken with alcohol.” is wrong because alcohol can also increase the risk of bleeding and interact with aspirin.
Choice B) “Aspirin can be taken on an empty stomach.” is wrong because aspirin can irritate the stomach lining and cause heartburn, nausea, or vomiting.It is better to take aspirin with food or water.
Choice C) “Aspirin can be taken with antacids.” is wrong because antacids can reduce the effectiveness of aspirin and interfere with its absorption.It is better to avoid taking antacids within two hours of taking aspirin.
A nurse is caring for a client who has rheumatoid arthritis and has been prescribed ibuprofen (Advil).
Which of the following instructions should the nurse include in the teaching? Select all that apply.
Explanation
The correct answer is choiceA,B , andD.
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can cause gastric irritation and bleeding.Therefore, the nurse should instruct the client to take ibuprofen with food or milk to reduce the risk of stomach ulcers.The nurse should also advise the client to avoid alcohol while taking ibuprofen, as alcohol can increase the risk of gastrointestinal bleeding and liver damage.Additionally, the nurse should tell the client to report any signs of gastrointestinal bleeding, such as black or tarry stools, abdominal pain, or vomiting blood, to the healthcare provider immediately.
ChoiceCis wrong because taking ibuprofen on an empty stomach can increase the risk of gastric irritation and bleeding.
ChoiceEis wrong because taking ibuprofen with antacids can reduce the effectiveness of ibuprofen and interfere with its absorption.Antacids can also cause adverse effects such as diarrhea, constipation, or electrolyte imbalance.
Therefore, the nurse should not recommend taking ibuprofen with antacids.
A nurse is caring for a client who has chronic hepatitis C and reports taking acetaminophen daily for headaches. The nurse should monitor the client for which of the following adverse effects?
Explanation
The correct answer is choice A. Hepatic necrosis.Acetaminophen (APAP) is a common cause of drug-induced liver injury and can lead to hepatic necrosis, especially in patients who have chronic hepatitis C.APAP is metabolized by the liver and produces a toxic intermediate called N-acetyl-p-benzoquinone imine (NAPQI), which can deplete glutathione and damage hepatocytes.Patients who have chronic hepatitis C may have reduced glutathione levels and increased oxidative stress, making them more susceptible to APAP toxicity.
Choice B. Pulmonary fibrosis is wrong because APAP does not cause pulmonary fibrosis.
Pulmonary fibrosis is a chronic lung disease that involves scarring of the lung tissue and impaired gas exchange.Some drugs that can cause pulmonary fibrosis are amiodarone, bleomycin, methotrexate and nitrofurantoin.
Choice C. Pancreatitis is wrong because APAP does not cause pancreatitis.
Pancreatitis is an inflammation of the pancreas that can result from gallstones, alcohol abuse, hypertriglyceridemia, hypercalcemia, infections, trauma or certain medications.
Some drugs that can cause pancreatitis are azathioprine, valproic acid, didanosine and pentamidine.
Choice D. Cardiac dysrhythmias is wrong because APAP does not cause cardiac dysrhythmias.
Cardiac dysrhythmias are abnormal heart rhythms that can result from electrolyte imbalances, ischemia, myocardial infarction, heart failure, congenital defects or certain medications.
Some drugs that can cause cardiac dysrhythmias are digoxin, quinidine, sotalol and erythromycin.
A nurse is providing discharge teaching to a client who has a prescription for acetaminophen and hydrocodone (Vicodin). Which of the following instructions should the nurse include in the teaching?
Explanation
The correct answer is choice A. Avoid driving while taking this medication.The nurse should instruct the client to avoid driving or operating heavy machinery while taking acetaminophen and hydrocodone (Vicodin) because these medications can cause drowsiness, dizziness, and impaired mental function.The nurse should also warn the client about the risk of addiction, overdose, and death from misuse of this medication.
Choice B is wrong because taking this medication on an empty stomach can increase the risk of nausea and vomiting.The nurse should advise the client to take this medication with food or milk to prevent stomach upset.
Choice C is wrong because increasing the intake of foods rich in vitamin K is not relevant to taking acetaminophen and hydrocodone (Vicodin).Vitamin K is involved in blood clotting and may interact with some anticoagulant medications, but not with this medication.
Choice D is wrong because limiting fluid intake to prevent fluid retention is not necessary for a client taking acetaminophen and hydrocodone (Vicodin).This medication does not cause fluid retention or edema.The nurse should encourage the client to drink plenty of fluids to prevent constipation, which is a common side effect of opioid medications.
A nurse is reviewing laboratory results for a client who takes acetaminophen for osteoarthritis pain management. Which of the following findings should alert the nurse to possible hepatotoxicity? (Select all that apply.) .
Explanation
The correct answer is choice A, B, and C. These are all liver enzymes that can indicate hepatotoxicity (liver damage) from acetaminophen overdose.
The normal ranges for these enzymes are:
• AST: 10 to 40 U/L
• ALT: 7 to 56 U/L
• ALP: 45 to 115 U/L
Choice D and E are wrong because they are indicators of renal function, not liver function.
The normal ranges for these values are:
• BUN: 7 to 20 mg/dL
• Creatinine: 0.6 to 1.2 mg/dL
A nurse is caring for a client who has a sickle cell crisis and is receiving morphine via patient-controlled analgesia (PCA) pump.
Which assessment finding indicates that the PCA pump is effective?
Explanation
The correct answer is choice A. The client reports a pain level of 4 on a scale of 0 to 10.This indicates that the PCA pump is effective in reducing the client’s pain, which is the primary symptom of sickle cell crisis.
Choice B is wrong because a respiratory rate of 12 breaths per minute is normal and does not indicate the effectiveness of the PCA pump.
Choice C is wrong because a blood pressure of 140/90 mm Hg is high and may indicate hypertension, which is a complication of sickle cell disease.
Choice D is wrong because a pulse oximetry reading of 95% is normal and does not indicate the effectiveness of the PCA pump.
Normal ranges for vital signs are:
• Respiratory rate: 12-20 breaths per minute
• Blood pressure: <120/80 mm Hg
• Pulse oximetry: >95%
A nurse is teaching a client who has cancer pain about the use of oral oxycodone with acetaminophen (Percocet).
Which statement by the client indicates a need for further teaching?
Explanation
The correct answer is choice C.The client should take this medicationregularlyas prescribed to maintain a steady level of analgesia and prevent breakthrough pain.
Taking the medication only when the pain is severe can lead to inadequate pain relief and increased side effects.
Choice A is wrong because drinking plenty of fluids and eating high-fiber foods can help prevent constipation, which is a common adverse effect of opioids.
Choice B is wrong because avoiding driving or operating heavy machinery is a safety precaution for clients taking opioids, as they can cause drowsiness and impaired judgment.
Choice D is wrong because reporting any signs of allergic reaction is an important instruction for clients taking any medication, especially opioids, which can cause severe hypersensitivity reactions.
A nurse is caring for a patient who is receiving epidural analgesia with buprenorphine (Buprenex). Which assessment finding would indicate that an adverse effect may be occurring?
Explanation
The correct answer is choice A) Respiratory rate: 10 breaths/min.This indicates that the patient may be experiencing respiratory depression, which is a serious adverse effect of buprenorphine and other opioids.
Respiratory depression can lead to hypoxia, brain damage, or death if not treated promptly.
The normal respiratory rate for adults is 12 to 20 breaths/min.
Choice B) Blood pressure: 110/70 mm Hg is wrong because this is within the normal range for adults, which is 90/60 to 120/80 mm Hg.Buprenorphine can cause hypotension as a side effect, but this is not evident in this case.
Choice C) Heart rate: 72 beats/min is wrong because this is also within the normal range for adults, which is 60 to 100 beats/min.Buprenorphine can cause bradycardia as a side effect, but this is not evident in this case.
Choice D) Temperature: 37°C is wrong because this is the normal body temperature for humans.Buprenorphine can cause hyperthermia as a side effect, but this is not evident in this case.
A patient who is addicted to heroin is admitted to the hospital for treatment of an infection. The patient is prescribed methadone (Dolophine) as part of a detoxification program. What is the rationale for using methadone in this patient?
Explanation
The correct answer is choice B.Methadone blocks the euphoric effects of heroin and discourages its use.Methadone is a synthetic opioid analgesic that produces a cross-tolerance to other narcotics, thereby preventing the user from feeling the high of heroin.Methadone also reduces withdrawal symptoms and cravings for heroin.
Choice A is wrong because methadone does not prevent withdrawal symptoms, but rather reduces them.
Choice C is wrong because methadone does not stimulate opioid receptors, but rather occupies them and blocks their activation by heroin.
Choice D is wrong because methadone does not reverse the respiratory depression caused by heroin overdose, but rather carries a risk of overdose itself.
A patient who has chronic low back pain is prescribed oxycodone (OxyContin) for long-term use.
Which of the following interventions should the nurse implement to prevent complications from this medication? (Select all that apply.)
Explanation
The correct answer is choice B and C.Oxycodone (OxyContin) is a potent opioid analgesic that can causeconstipation,drowsiness,nausea,pruritus, andvomitingas common side effects.
To prevent constipation, the patient should be encouraged to drink plenty of fluids and eat high-fiber foods.To prevent respiratory depression and sedation, the patient should be advised to avoid alcohol and other CNS depressants while taking oxycodone.
Choice A is wrong because monitoring vital signs regularly is not specific to oxycodone use, but rather a general nursing intervention for any patient with chronic pain.
Choice D is wrong because acetaminophen (Tylenol) can interact with oxycodone and increase the risk of liver damage.
The patient should not take any other pain medications without consulting the prescriber.
Choice E is wrong because a patient-controlled analgesia (PCA) pump is not used for long-term pain management, but rather for acute or postoperative pain.Oxycodone (OxyContin) is formulated as an extended-release tablet that provides sustained pain relief for up to 12 hours.
A patient with chronic back pain is prescribed gabapentin as an adjuvant analgesic. The nurse should instruct the patient to report which of the following adverse effects?
Explanation
The correct answer is choice A.Blurred vision is a common side effect of gabapentin and should be reported to the doctor.
Blurred vision can affect the patient’s ability to perform daily activities and may indicate a serious problem with the eyes or the brain.
Choice B is wrong because constipation is not a common side effect of gabapentin.
Constipation can be caused by other factors such as diet, dehydration, or lack of physical activity.
Choice C is wrong because dry mouth is a common side effect of gabapentin and does not usually require medical attention.
Dry mouth can be relieved by drinking water, chewing sugar-free gum, or using saliva substitutes.
Choice D is wrong because tinnitus is not a common side effect of gabapentin.
Tinnitus is a ringing or buzzing sound in the ears that can be caused by many conditions such as ear infections, hearing loss, or exposure to loud noises.
A patient with cancer-related bone pain is receiving etidronate as an adjuvant analgesic. The nurse should monitor the patient for which of the following laboratory values?
Explanation
The correct answer is choice A. Serum calcium.Etidronate is a bisphosphonate that inhibits bone resorption and reduces the risk of skeletal complications in patients with cancer-related bone pain.However, it can also cause hypocalcemia (low serum calcium levels) as a side effect, which can lead to muscle spasms, numbness, tingling, seizures, and cardiac arrhythmias.
Therefore, the nurse should monitor the patient’s serum calcium levels regularly and supplement with calcium and vitamin D if needed.
Choice B. Serum potassium is wrong because etidronate does not affect potassium levels.Potassium is mainly regulated by the kidneys and can be altered by renal impairment, dehydration, acid-base imbalance, or medications such as diuretics or potassium-sparing agents.
Choice C. Serum creatinine is wrong because etidronate does not affect creatinine levels.
Creatinine is a waste product of muscle metabolism that is excreted by the kidneys.It reflects the glomerular filtration rate (GFR) and can be elevated in renal dysfunction or dehydration.
Choice D. Serum albumin is wrong because etidronate does not affect albumin levels.
Albumin is a protein that is synthesized by the liver and helps maintain fluid balance and transport substances in the blood.It can be decreased in liver disease, malnutrition, inflammation, or protein-losing conditions.
(Select all that apply) A patient with postoperative pain is prescribed hydroxyzine as an adjuvant analgesic. The nurse should teach the patient about which of the following benefits of this medication.
Explanation
The correct answer is choice A, B, D, and E.Hydroxyzine is an antihistamine that hasantiemeticandsedativeeffects that are thought to be mediated by its actions in the brain.It can alsodecrease anxietyrelated to pain by inhibiting the hypothalamic H-1 histamine receptors.Hydroxyzine may also have apotentiatingeffect on other analgesics, although the evidence for this is not conclusive.
Choice C is wrong because hydroxyzine does not have any anti-inflammatory properties.It is a competitive antagonist of histamine H1-receptors, not a cyclooxygenase inhibitor.
The nurse is preparing to administer morphine sulfate, an opioid analgesic, to a client who reports pain at level 8 on a scale of 0 to 10. Which action should the nurse take first?
Explanation
The correct answer is choice B. Check the client’s allergy history.
This is because morphine sulfate is a medication that can cause severe allergic reactions in some people, such as anaphylaxis, which can be life-threatening.
Therefore, the nurse should always check the client’s allergy history before administering any medication, especially opioids.
Choice A is wrong because assessing the client’s respiratory rate is not the first action the nurse should take.
Although morphine sulfate can cause respiratory depression, which is a serious side effect that needs to be monitored, the nurse should first ensure that the client is not allergic to the medication.
Choice C is wrong because reviewing the client’s medication record is not the first action the nurse should take.
Although morphine sulfate can interact with other medications, such as sedatives, antidepressants, or alcohol, which can increase the risk of respiratory depression or overdose, the nurse should first ensure that the client is not allergic to the medication.
Choice D is wrong because verifying the dosage with another nurse is not the first action the nurse should take.
Although morphine sulfate is a high-alert medication that requires double-checking to prevent medication errors, the nurse should first ensure that the client is not allergic to the medication.
The nurse is caring for a client who has been prescribed acetaminophen, a non-opioid analgesic, for mild pain. Which laboratory test result should the nurse monitor closely in this client?
Explanation
The correct answer is choice D. Serum bilirubin.The nurse should monitor the client’s serum bilirubin level closely because acetaminophen, a non-opioid analgesic, can cause hepatotoxicity and acute liver failure in cases of overdose.
Serum bilirubin is a marker of liver function and damage.
A high level of serum bilirubin indicates jaundice, a sign of liver injury.
Choice A is wrong because serum creatinine is a marker of kidney function and damage.Acetaminophen has limited nephrotoxicity compared to NSAIDs.
Choice B is wrong because serum potassium is not directly affected by acetaminophen.
Serum potassium is an electrolyte that reflects fluid and acid-base balance in the body.
Choice C is wrong because serum albumin is a protein that is synthesized by the liver.
Although serum albumin may be low in chronic liver disease, it is not a sensitive indicator of acute liver injury caused by acetaminophen overdose.
Normal ranges for serum bilirubin are 0.3 to 1.2 mg/dL for adults and 1 to 12 mg/dL for newborns.
Normal ranges for serum creatinine are 0.6 to 1.2 mg/dL for men and 0.5 to 1.1 mg/dL for women.
Normal ranges for serum potassium are 3.5 to 5 mEq/L for adults and children.
Normal ranges for serum albumin are 3.4 to 5.4 g/dL for adults and children.
A nurse is educating a client about ibuprofen, a nonsteroidal anti-inflammatory drug (NSAID), that has been prescribed for moderate pain and inflammation. Which of the following instructions should the nurse include? (Select all that apply.).
Explanation
The correct answer is choice A, B, C, and D.Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that has anti-inflammatory, analgesic, and antipyretic effects.It works by inhibiting the synthesis of prostaglandins, which are involved in inflammation, pain, and fever.However, ibuprofen can also cause adverse effects such as gastric irritation, bleeding complications, renal impairment, and hypersensitivity reactions.
Therefore, the nurse should instruct the client to:
• Take ibuprofen with food or milk to prevent gastric irritation.This will reduce the direct contact of the drug with the stomach lining and decrease the risk of ulcers and bleeding.
• Drink at least 2 liters of fluid per day to prevent renal impairment.This will help maintain adequate hydration and renal perfusion and prevent the accumulation of ibuprofen in the kidneys.
• Avoid alcohol and other NSAIDs to prevent bleeding complications.Alcohol and other NSAIDs can increase the risk of gastric bleeding by interfering with the protective effects of prostaglandins on the stomach mucosa.
• Report any signs of hypersensitivity such as rash, itching, or wheezing.These may indicate an allergic reaction to ibuprofen that can be serious or life-threatening.
Choice E is wrong because ibuprofen does not affect blood pressure significantly.However, some other NSAIDs such as celecoxib may increase the risk of cardiovascular events such as thrombosis, myocardial infarction, and stroke.Therefore, clients with hypertension or cardiovascular disease should use NSAIDs with caution and monitor their blood pressure regularly.
The primary health care provider instructs the nurse to obtain the patient’s pain level every four hours. Which actions by the nurse help facilitate the pain assessment? Select all that apply.
Explanation
The correct answer is choice A, B, C and E.These actions by the nurse help facilitate the pain assessment by using a consistent and clear method to measure the patient’s pain level, enhancing the visibility and understanding of the scale, repeating the information for clarity and accuracy, and giving the patient enough time to respond without rushing or interrupting.
Choice D is wrong because asking about the present level of pain rather than the pain history is more relevant for pain management, not the pain assessment.The pain history provides valuable information about the onset, duration, frequency, quality, intensity, location, and aggravating or relieving factors of the pain.
Which component of pain assessment is addressed by asking a client to rate his or her current level of discomfort on a scale of 0-10?
Explanation
The correct answer is choice A. Intensity.Intensity is one of the key components of pain assessmentand it is measured by asking a client to rate his or her current level of discomfort on a scale of 0-10.
This helps to quantify the severity of pain and monitor its changes over time.
Choice B. Quality is wrong because quality refers to the nature or characteristics of pain, such as burning, stabbing, throbbing, etc.It is usually assessed by asking the client to describe the pain in his or her own words.
Choice C.Onset is wrong because onset refers to the time when the pain started or what triggered it.It is usually assessed by asking the client about the mechanism of injury or etiology of pain, if identifiable.
Choice D.Duration is wrong because duration refers to how long the pain lasts or how often it occurs.It is usually assessed by asking the client about the course or temporal pattern of pain, such as constant, intermittent, or episodic.
A nurse is caring for an older adult client who has difficulty communicating verbally due to aphasia following a stroke.
Which of the following strategies should the nurse use to assess this client’s pain? (Select all that apply.)
Explanation
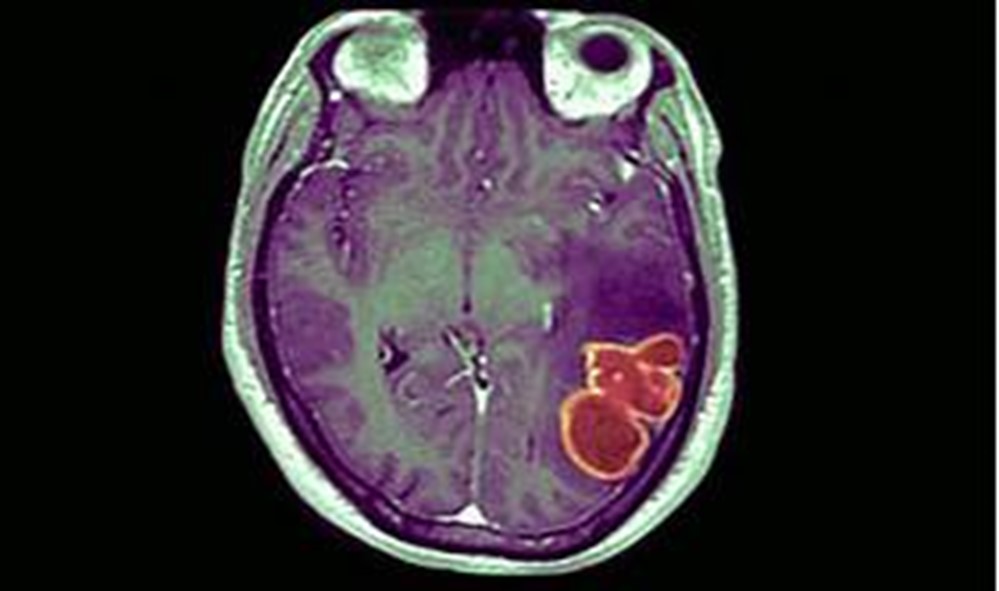
The correct answer is choice A, B, C, and E. The nurse should use the following strategies to assess this client’s pain:
• Ask yes or no questions: This can help the client to communicate their pain level and location with minimal language difficulty.
• Use a visual analog scale (VAS): This is a self-report pain scale that uses a line with endpoints labeled as “no pain” and “worst pain imaginable”.The client can point to a position on the line that corresponds to their pain intensity.VAS has been shown to be feasible, valid, and reliable for stroke patients with mild-to-moderate aphasia.
• Observe for nonverbal cues: This can include facial expressions, body movements, vocalizations, and changes in vital signs that may indicate pain.Nonverbal cues are especially important for clients with severe aphasia who cannot use self-report scales.
• Involve family members or caregivers: They can provide information about the client’s pain history, preferences, and behaviors that may indicate pain.They can also help the nurse to communicate with the client and interpret their responses.
Choice D is wrong because open-ended questions require more complex language skills and may frustrate the client with aphasia.The nurse should use simple and direct questions that can be answered with yes or no, gestures, or pointing.
A nurse is caring for a patient who has been prescribed fentanyl patches for chronic cancer pain management at home. Which statement by the patient indicates that he understands how to use this medication safely?
Explanation
The correct answer is choice C.The patient should remove the old patch before applying a new one to avoid overdose and adverse effects of fentanyl.Fentanyl patches are designed to deliver a constant amount of opioid analgesic over a period of time, usually 72 hours.
Therefore, changing the patch every other day (choice A) would result in inadequate pain relief and withdrawal symptoms.
Applying the patch to a hairy area (choice B) would interfere with the absorption of the drug and reduce its effectiveness.
Cutting the patch in half (choice D) would damage the integrity of the patch and cause erratic or rapid release of the drug, which could be fatal.Fentanyl patches should be applied to a clean, dry, hairless area of intact skin on the upper torso or upper arm.
A nurse is administering naloxone to a patient who has overdosed on heroin. What is the expected outcome of this intervention?
Explanation
The correct answer is choice D. The patient will experience improved mental status and oxygenation.This is because naloxone is a medication that can rapidly reverse an opioid overdose by blocking the effects of opioids and restoring normal breathing.Naloxone can be given as a nasal spray or an injection.
Choice A is wrong because naloxone does not increase euphoria and sedation, but rather reverses them by blocking opioid receptors.
Choice B is wrong because naloxone does not cause severe withdrawal symptoms and agitation, but rather mild to moderate ones that are not life-threatening.
Choice C is wrong because naloxone does not decrease respiratory rate and blood pressure, but rather increases them by reversing opioid overdose.
Normal ranges for respiratory rate are 12 to 20 breaths per minute and for blood pressure are 90/60 mmHg to 120/80 mmHg.
A nurse is educating a patient who has been prescribed aspirin for the prevention of cardiovascular events. Which of the following instructions should the nurse include? (Select all that apply.)
Explanation
The correct answer is choice A, B, C and E.Aspirin is a medication that can prevent cardiovascular events by inhibiting platelet aggregation and reducing inflammation.
However, aspirin also has some side effects that the patient should be aware of and report to the doctor if they occur.
Choice A is correct because taking aspirin with food or milk can reduce the risk of stomach irritation and ulcers that aspirin can cause.
Choice B is correct because aspirin can increase the risk of bleeding and bruising due to its antiplatelet effect.The patient should monitor for signs of bleeding such as black, tarry stools, bloody or cloudy urine, vomiting of blood or material that looks like coffee grounds, and unusual bleeding or bruising.
Choice C is correct because taking other NSAIDs (nonsteroidal anti-inflammatory drugs) concurrently with aspirin can increase the risk of stomach ulcers and bleeding.
NSAIDs include ibuprofen, naproxen, diclofenac, and others.
Choice D is wrong because tinnitus (ringing in the ears) is a sign of aspirin toxicity and should not be ignored.The patient should stop taking aspirin and seek medical attention if they experience tinnitus, confusion, hallucinations, rapid breathing, or seizures.
Choice E is correct because enteric-coated tablets can reduce the gastric irritation caused by aspirin by delaying its release until it reaches the small intestine.However, enteric-coated tablets may not be as effective as regular tablets in preventing cardiovascular events.
Exams on Analgesics and Pain Management Medications
Routes, Doses, Onset, Duration, Peak, and Half-life of Various Analgesics
Review Practice Mode Take ExamCustom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Acetaminophen
- Opioid Analgesics
- Mixed Agonists/Antagonists
- Adjuvant Analgesics
- Routes, Doses, Onset, Duration, Peak, and Half-life of Various Analgesics
- Nursing Assessments, Interventions, and Education for Patients Receiving Analgesics
- Pain Assessment Tools and Scale Conclusion
- Conclusion
- Summary
- More questions on this topics
Notes Highlighting is available once you sign in. Login Here.
Objectives
- The types, mechanisms, indications, side effects, and interactions of different classes of analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, opioids, mixed agonists/antagonists, and adjuvants.
- The signs and symptoms, causes, prevention, and treatment of opioid overdose, tolerance, dependence, and withdrawal.
- The routes, doses, onset, duration, peak, and half-life of various analgesics.
- The nursing assessments, interventions, and education for patients receiving analgesics.
- The pain assessment tools and scales used to evaluate pain intensity, quality, location, and relief.
- Demonstrate critical thinking and clinical judgment in managing pain for patients with different conditions and needs.
Introduction
- Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage.
- Pain management is the process of providing medical care that alleviates or reduces pain.
- Pain management involves pharmacological and non-pharmacological interventions.
- Pharmacological interventions include analgesics, which are medications that relieve pain.
- Analgesics are classified into three main categories: nonopioids, opioids, and adjuvants.
- Nonopioids include acetaminophen and NSAIDs, which are effective for mild to moderate pain and have anti-inflammatory and antipyretic properties.
- Opioids include morphine, fentanyl, oxycodone, hydrocodone, codeine, and others, which are effective for moderate to severe pain and act on opioid receptors in the brain and spinal cord
- Adjuvants include antidepressants, anticonvulsants, corticosteroids, local anaesthetics, and others, which have either independent or additive analgesic effects when used with opioids or nonopioids.
- The choice of analgesic depends on several factors, such as the type, intensity, duration, location, cause, and response to pain; the patient’s age, weight, medical history, and allergies; the availability, cost, and safety of the medication; and the patient’s preference and values.
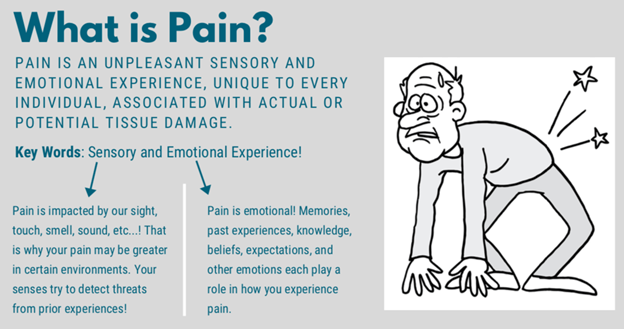
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- NSAIDs are a group of medications that inhibit cyclooxygenase (COX) enzymes, which are involved in the synthesis of prostaglandins. Prostaglandins are inflammatory mediators that sensitize nerve endings to pain stimuli.
- NSAIDs have analgesic (pain-relieving), anti-inflammatory (reducing swelling and redness), and antipyretic (lowering fever) effects.
- NSAIDs are indicated for mild to moderate pain caused by inflammation (e.g., arthritis), injury (e.g., sprain), surgery (e.g., dental extraction), dysmenorrhea (menstrual cramps), headache (e.g., migraine), fever (e.g., infection), and cancer (e.g., bone metastasis).
- NSAIDs are available in oral (tablet or capsule), topical (gel or cream), rectal (suppository), intravenous (injection), or intra-articular (into a joint) forms.
- NSAIDs can be divided into two subclasses: nonselective COX inhibitors and selective COX-2 inhibitors. Nonselective COX inhibitors block both COX-1 and COX-2 enzymes. COX-1 is responsible for protecting the gastric mucosa, regulating platelet aggregation, and maintaining renal function. COX-2 is induced by inflammation and mediates pain and fever. Selective COX-2 inhibitors block only COX-2 enzymes and have less gastrointestinal and bleeding side effects than nonselective COX inhibitors. However, selective COX-2 inhibitors may increase the risk of cardiovascular events such as myocardial infarction and stroke.
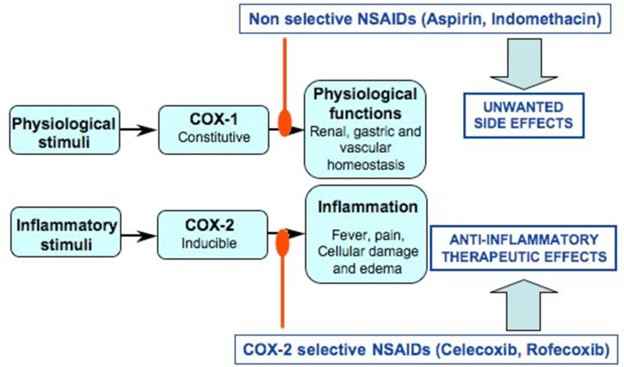
- Examples of nonselective COX inhibitors include aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), ketorolac (Toradol), indomethacin (Indocin), diclofenac (Voltaren), and meloxicam (Mobic). Examples of selective COX-2 inhibitors include celecoxib (Celebrex) and etoricoxib (Arcoxia)
- The common side effects of NSAIDs include gastrointestinal irritation, ulceration, bleeding, and perforation; renal impairment; fluid retention and edema; hypertension; and increased risk of cardiovascular events.
- The contraindications and precautions for NSAIDs include allergy, asthma, peptic ulcer disease, bleeding disorders, renal or hepatic impairment, heart failure, hypertension, pregnancy, lactation, and children under 18 years old.
- The interactions of NSAIDs include increased bleeding risk with anticoagulants, antiplatelets, corticosteroids, and alcohol; decreased effectiveness of antihypertensives and diuretics; increased toxicity of lithium, methotrexate, and digoxin; and increased risk of nephrotoxicity with aminoglycosides.
Acetaminophen
- Acetaminophen (Tylenol) is a medication that inhibits prostaglandin synthesis in the central nervous system, but not in the peripheral tissues. It has analgesic and antipyretic effects, but not anti-inflammatory effects.

- Acetaminophen is indicated for mild to moderate pain caused by headache, muscle ache, arthritis, menstrual cramps, toothache, and cold; and for fever caused by infection or immunization.
- Acetaminophen is available in oral (tablet, capsule, liquid), rectal (suppository), intravenous (injection), or combination forms. Many over-the-counter and prescription medications contain acetaminophen as an ingredient, such as cold and flu remedies, cough syrups, and opioid analgesics.
- The common side effects of acetaminophen are rare and mild, such as rash, nausea, vomiting, and headache. However, a serious side effect of acetaminophen is hepatotoxicity (severe liver damage), which can occur with overdose or chronic use. Hepatotoxicity can lead to liver failure, coma, and death.
- The contraindications and precautions for acetaminophen include allergy, severe liver disease or failure, alcoholism, malnutrition, pregnancy, lactation, and children under 2 years old.
- The interactions of acetaminophen include increased risk of hepatotoxicity with alcohol, barbiturates, carbamazepine, phenytoin, and rifampin; decreased effectiveness of warfarin; and increased risk of nephrotoxicity with loop diuretics.
Opioid Analgesics
- Opioid analgesics are a group of medications that act on opioid receptors in the brain and spinal cord to produce analgesia, sedation, euphoria, and respiratory depression.
- Opioid receptors are classified into three types: mu, kappa, and delta. Mu receptors are responsible for most of the analgesic and adverse effects of opioids, such as respiratory depression, constipation, miosis (pupil constriction), pruritus (itching), dependence, and tolerance.
- Kappa receptors mediate analgesia and sedation in the spinal cord and some adverse effects such as dysphoria (unpleasant mood), hallucinations, and miosis. Delta receptors have less clinical significance but may modulate mood and analgesia.
- Opioid analgesics are indicated for moderate to severe pain caused by various conditions, such as trauma, surgery, cancer, myocardial infarction, and sickle cell crisis.
- They are also used for cough suppression and diarrhoea control in some cases. Opioids are the mainstay of treatment for acute pain and cancer pain but should be used cautiously for chronic non-cancer pain due to the risk of addiction and misuse
- Opioid analgesics are available in oral (tablet, capsule, liquid), rectal (suppository), intravenous (injection), intramuscular (injection), subcutaneous (injection), transdermal (patch or film), nasal (spray), sublingual (tablet or film), buccal (tablet or film), or epidural (injection) forms
- Opioid analgesics can be classified into four groups based on their receptor affinity and activity: pure agonists, partial agonists, mixed agonists/antagonists, and pure antagonists. Pure agonists bind to and activate mu and kappa receptors, producing strong analgesia and sedation.
- Partial agonists bind to and partially activate mu receptors, producing moderate analgesia and less respiratory depression than pure agonists. Mixed agonists/antagonists bind to and activate kappa receptors while antagonizing or partially activating mu receptors, produces moderate analgesia and less euphoria and dependence than pure agonists.
- Pure antagonists bind to and block mu and kappa receptors, reversing the effects of opioid agonists
- Examples of pure agonists include morphine, fentanyl, oxycodone, hydrocodone, codeine, hydromorphone, methadone, meperidine, and tramadol. Examples of partial agonists include buprenorphine and nalbuphine. Examples of mixed agonists/antagonists include pentazocine, butorphanol, and dezocine. Examples of pure antagonists include naloxone, naltrexone, and nalmefene
- The common side effects of opioid analgesics include respiratory depression, sedation, constipation, nausea, vomiting, pruritus, urinary retention, miosis, orthostatic hypotension, cough suppression, and biliary spasm
- The contraindications and precautions for opioid analgesics include allergy, severe respiratory depression or failure, severe asthma or bronchospasm, increased intracranial pressure or head injury, paralytic ileus or bowel obstruction, pregnancy, lactation, children under 18 years old (except for some specific indications), elderly or debilitated patients, renal or hepatic impairment, history of substance abuse or dependence, and concurrent use of other central nervous system depressants
- The interactions of opioid analgesics include increased sedation and respiratory depression with alcohol, benzodiazepines, barbiturates, antihistamines, and other opioids; decreased analgesic effect with opioid antagonists; increased risk of serotonin syndrome with selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, and other serotonergic agents; increased risk of seizures with tramadol and meperidine; decreased metabolism and increased toxicity of opioids with inhibitors of cytochrome P450 enzymes, such as cimetidine, erythromycin, ketoconazole, and grapefruit juice
Mixed Agonists/Antagonists
- Mixed agonists/antagonists are a group of medications that have both agonist and antagonist activity at different opioid receptors. They are also called partial agonist-antagonists or balanced analgesics.
- Mixed agonists/antagonists have analgesic and sedative effects similar to pure agonists, but with a lower risk of respiratory depression, euphoria, dependence, and tolerance. However, they may also cause dysphoria (unpleasant mood), hallucinations, anxiety, and confusion in some patients. They may also precipitate withdrawal symptoms in patients who are physically dependent on pure agonists.
- Mixed agonists/antagonists are indicated for moderate to severe pain caused by various conditions, such as trauma, surgery, cancer, and labor. They are also used for anesthesia and detoxification in some cases. They are not recommended for chronic pain management due to the risk of ceiling effect (a limit to the analgesic effect regardless of dose increase) and psychotomimetic effects (disturbance of perception and cognition)
- Mixed agonists/antagonists are available in oral (tablet), intravenous (injection), intramuscular (injection), subcutaneous (injection), transdermal (patch), nasal (spray), or epidural (injection) forms
- Examples of mixed agonists/antagonists include pentazocine (Talwin), butorphanol (Stadol), nalbuphine (Nubain), buprenorphine (Buprenex, Subutex), and dezocine (Dalgan)
- The common side effects of mixed agonists/antagonists include respiratory depression, sedation, constipation, nausea, vomiting, pruritus, urinary retention, miosis, orthostatic hypotension, cough suppression, biliary spasm, dysphoria, hallucinations, anxiety, confusion, and withdrawal symptoms.
- The contraindications and precautions for mixed agonists/antagonists include allergy, severe respiratory depression or failure, severe asthma or bronchospasm, increased intracranial pressure or head injury, paralytic ileus or bowel obstruction, pregnancy (except for buprenorphine), lactation, children under 18 years old (except for some specific indications), elderly or debilitated patients, renal or hepatic impairment, history of substance abuse or dependence, and concurrent use of other central nervous system depressants or pure opioid agonists.
- The interactions of mixed agonists/antagonists include increased sedation and respiratory depression with alcohol, benzodiazepines, barbiturates, antihistamines, and other opioids; decreased analgesic effect with opioid antagonists; increased risk of serotonin syndrome with selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, and other serotonergic agents; increased risk of seizures with tramadol and meperidine; decreased metabolism and increased toxicity of opioids with inhibitors of cytochrome P450 enzymes, such as cimetidine, erythromycin, ketoconazole, and grapefruit juice.
Adjuvant Analgesics
- Adjuvant analgesics are a group of medications that have primary indications other than pain relief but have either independent or additive analgesic effects when used with opioids or nonopioids. They are also called coanalgesics or adjunctive analgesics.

- Adjuvant analgesics are indicated for various types of pain that are difficult to treat with conventional analgesics alone, such as neuropathic pain (caused by nerve damage or dysfunction), cancer pain (especially bone pain), chronic pain (such as fibromyalgia), and postoperative pain. They are also used to enhance the efficacy of opioids or nonopioids, reduce their side effects or doses, and treat the underlying cause or associated symptoms of pain.
- Adjuvant analgesics are available in oral (tablet, capsule, liquid), topical (patch, cream, gel), intravenous (injection), intramuscular (injection), subcutaneous (injection), or epidural (injection) forms.
- Examples of adjuvant analgesics include antidepressants, anticonvulsants, corticosteroids, local anaesthetics, alpha2-adrenergic agonists, N-methyl-D-aspartate (NMDA) receptor antagonists, muscle relaxants, bisphosphonates, and cannabinoids.
- The common side effects of adjuvant analgesics vary depending on the class and individual medication but may include sedation, drowsiness, dizziness, confusion, nausea, vomiting, constipation, dry mouth, weight gain, sexual dysfunction, hypotension, bradycardia, cardiac arrhythmias, seizures, rash, bleeding, osteoporosis, hyperglycemia, immunosuppression, infection, and dependence.
- The contraindications and precautions for adjuvant analgesics vary depending on the class and individual medication but may include allergy, pregnancy, lactation, children under 18 years old (except for some specific indications), elderly or debilitated patients, renal or hepatic impairment, history of substance abuse or dependence, and concurrent use of other medications that may interact with them.
- The interactions of adjuvant analgesics vary depending on the class and individual medication but may include increased sedation and respiratory depression with opioids and other central nervous system depressants; increased risk of serotonin syndrome with opioids and other serotonergic agents; increased risk of bleeding with anticoagulants and antiplatelets; decreased metabolism and increased toxicity of opioids and other medications with inhibitors of cytochrome P450 enzymes; decreased effectiveness of oral contraceptives; and increased risk of cardiac arrhythmias with drugs that prolong the QT interval.
Routes, Doses, Onset, Duration, Peak, and Half-life of Various Analgesics
- The route of administration of an analgesic refers to the way the medication is delivered into the body. The route affects the onset (how quickly the medication starts to work), the peak (when the medication reaches its highest concentration and effect), the duration (how long the medication lasts), and the dose (how much medication is needed) of the analgesic.
- The oral route is the most common and convenient way of taking analgesics, especially for mild to moderate pain. However, the oral route has some disadvantages, such as slow and variable absorption, first-pass metabolism (reduction of drug concentration by the liver before reaching the systemic circulation), and gastrointestinal irritation. The onset of oral analgesics ranges from 15 to 60 minutes, the peak ranges from 30 minutes to 4 hours, and the duration ranges from 2 to 12 hours, depending on the drug and formulation.
- The rectal route is an alternative to the oral route for patients who cannot swallow or have nausea or vomiting. The rectal route has a faster absorption than the oral route, but it is also variable and unpredictable. The onset of rectal analgesics ranges from 15 to 30 minutes, the peak ranges from 30 minutes to 2 hours, and the duration ranges from 2 to 8 hours, depending on the drug and formulation.
- The intravenous route is the fastest and most reliable way of delivering analgesics, especially for severe pain or breakthrough pain (a sudden increase in pain intensity). The intravenous route bypasses the first-pass metabolism and allows precise control of drug dosage and titration. The onset of intravenous analgesics ranges from 1 to 5 minutes, the peak ranges from 5 to 15 minutes, and the duration ranges from 1 to 6 hours, depending on the drug and infusion rate.
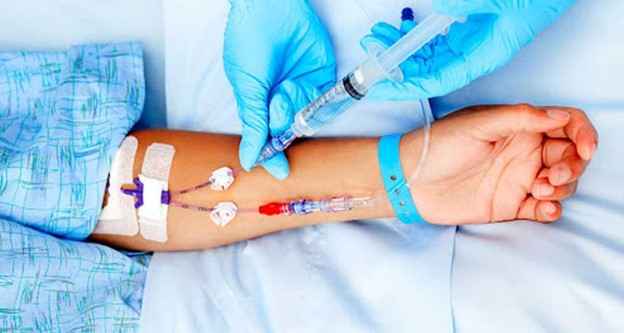
- The intramuscular route is a less common and less preferred way of delivering analgesics, as it is more painful and less predictable than the intravenous route. The intramuscular route has a slower absorption than the intravenous route, but it is also affected by blood flow, muscle mass, injection site, and volume of the drug. The onset of intramuscular analgesics ranges from 10 to 30 minutes, the peak ranges from 30 minutes to 2 hours, and the duration ranges from 2 to 8 hours, depending on the drug and injection site.
- The subcutaneous route is similar to the intramuscular route in terms of absorption and variability, but it is less painful and more convenient for patients who need frequent or continuous administration of analgesics. The subcutaneous route can be used with syringes or infusion pumps. The onset of subcutaneous analgesics ranges from 10 to 30 minutes, the peak ranges from 30 minutes to 2 hours, and the duration ranges from 2 to 8 hours, depending on the drug and infusion rate.
- The transdermal route is a noninvasive and convenient way of delivering analgesics through patches or films that adhere to the skin. The transdermal route provides sustained release of drugs into the systemic circulation and provides a steady state of drug concentration. The transdermal route is useful for patients who need long-term or continuous administration of analgesics, such as those with chronic pain or cancer pain. However, the transdermal route has some disadvantages, such as delayed onset and offset, skin irritation or allergy, and difficulty in titrating the dose. The onset of transdermal analgesics ranges from 2 to 12 hours, the peak ranges from 12 to 24 hours, and the duration ranges from 48 to 72 hours, depending on the drug and patch.
- The nasal route is a noninvasive and rapid way of delivering analgesics through sprays that are absorbed by the nasal mucosa. The nasal route is useful for patients who need immediate or breakthrough relief of pain, such as those with migraine or cancer pain. However, the nasal route has some disadvantages, such as nasal irritation, bleeding, congestion, or infection; variable absorption; and limited availability of drugs. The onset of nasal analgesics ranges from 5 to 15 minutes, the peak ranges from 15 to 30 minutes, and the duration ranges from 2 to 4 hours, depending on the drug and spray.
- The sublingual or buccal route is a noninvasive and fast way of delivering analgesics through tablets or films that are placed under the tongue or between the cheek and gum. The sublingual or buccal route bypasses the first-pass metabolism and allows rapid absorption of drugs into the systemic circulation. The sublingual or buccal route is useful for patients who need immediate or breakthrough relief of pain, such as those with cancer pain. However, the sublingual or buccal route has some disadvantages, such as oral irritation, dry mouth, taste disturbance, and limited availability of drugs. The onset of sublingual or buccal analgesics ranges from 5 to 15 minutes, the peak ranges from 15 to 30 minutes, and the duration ranges from 2 to 4 hours, depending on the drug and formulation.
- The epidural route is an invasive and specialized way of delivering analgesics through injections into the epidural space (the space between the dura mater and the vertebral column). The epidural route provides localized analgesia to a specific region of the body without affecting other areas. The epidural route is useful for patients who need continuous or intermittent administration of analgesics for severe pain, such as those undergoing surgery, labour and delivery, or cancer pain.
- However, the epidural route has some disadvantages, such as requiring a skilled practitioner to perform the procedure; risk of infection, bleeding, nerve damage, or spinal headache; and potential complications such as hypotension, respiratory depression, urinary retention, nausea, vomiting, pruritus, or motor block.
- The onset of epidural analgesics ranges from 10 to 20 minutes, the peak ranges from 20 to 60 minutes, and the duration ranges from 2 to 24 hours, depending on the drug and infusion rate
- The dose of an analgesic refers to the amount of medication that is given to a patient at one time. The dose depends on several factors, such as the type, intensity, duration, location, cause, and response to pain; the patient’s age, weight, medical history, and allergies; the availability, cost, and safety of the medication; and the patient’s preference and values.
- The dose should be individualized for each patient and adjusted according to the patient’s response and tolerance. The dose should be titrated to achieve optimal pain relief with minimal side effects.
- The dose should be given at regular intervals or as needed to maintain adequate pain control. The dose should be reduced or discontinued gradually to prevent withdrawal symptoms or rebound pain
- The onset of an analgesic refers to how quickly the medication starts to work after administration. The onset depends on several factors, such as the route, formulation, absorption, distribution, and metabolism of the medication; the type, intensity, duration, location, cause, and response to pain; and the patient’s age, weight, medical history, allergies; and concurrent use of other medications.
- The onset should be considered when choosing an appropriate analgesic for a patient’s pain level and condition. The onset should be monitored to evaluate the effectiveness of the analgesic and adjust
- The half-life of an analgesic refers to the time it takes for the concentration of the medication in the blood to decrease by half. The half-life depends on several factors, such as the route, formulation, absorption, distribution, metabolism, and excretion of the medication; the patient’s age, weight, medical history, allergies; and concurrent use of other medications that may affect the clearance of the drug.
- The half-life affects the frequency and duration of administration of the analgesic. The half-life should be considered when choosing an appropriate analgesic for a patient’s pain level and condition. The half-life should be monitored to avoid accumulation or withdrawal of the drug in the body.
See Table 11.1 for a comparison of the routes, doses, onset, duration, peak, and half-life of some common analgesics. Note that these values are approximate and may vary depending on individual factors and sources. Always check the drug label and reference for specific information before administering any medication.
|
Analgesic |
Route |
Dose |
Onset |
Duration |
Peak |
Half-life |
|---|---|---|---|---|---|---|
|
Acetaminophen |
Oral |
325-1000 mg every 4-6 hours (max 4000 mg/day) |
15-60 min |
3-4 hours |
30-60 min |
2-3 hours |
|
Acetaminophen |
Rectal |
650 mg every 4-6 hours (max 4000 mg/day) |
15-30 min |
3-4 hours |
30-60 min |
2-3 hours |
|
Acetaminophen |
IV |
1000 mg every 6 hours or 650 mg every 4 hours (max 4000 mg/day) |
5-10 min |
4-6 hours |
15 min |
2-3 hours |
|
Aspirin |
Oral |
325-650 mg every 4-6 hours (max 4000 mg/day) |
15-30 min |
4-6 hours |
1-2 hours |
2-3 hours |
|
Ibuprofen |
Oral |
200-800 mg every 4-6 hours (max 3200 mg/day) |
15-30 min |
4-6 hours |
1-2 hours |
2-4 hours |
|
Naproxen |
Oral |
250-500 mg every 12 hours (max 1500 mg/day) |
30 min -1 hour |
12-24 hours |
2-4 hours |
12-17 hours |
Nursing Assessments, Interventions, and Education for Patients Receiving Analgesics
- Nursing assessments for patients receiving analgesics include the following:
- Assess the patient’s pain level, quality, location, duration, frequency, and relief using a valid and reliable pain assessment tool or scale, such as the numeric rating scale, the visual analogue scale, the faces pain scale, or the FLACC scale.
- Assess the patient’s medical history, allergies, current medications, vital signs, and laboratory results to identify any contraindications, precautions, or interactions for analgesic therapy.
- Assess the patient’s response to previous analgesic therapy, including the type, dose, route, frequency, effectiveness, and side effects of the medication.
- Assess the patient’s preferences and values regarding pain management, including their expectations, goals, beliefs, fears, and coping strategies.
- Assess the patient’s risk factors for opioid misuse, abuse, addiction, overdose, or withdrawal, such as a history of a substance use disorder, mental health disorder, chronic pain condition, or family or social environment. Use a validated screening tool or questionnaire, such as the Opioid Risk Tool or the Screener and Opioid.
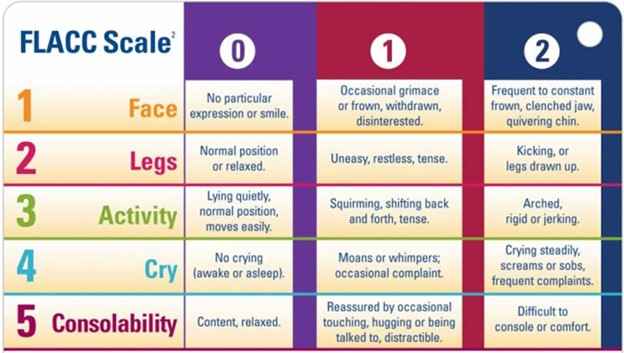
- Nursing interventions for patients receiving analgesics include the following:
- Administer the prescribed analgesic according to the five rights of medication administration: right patient, right drug, right dose, right route, and the right time.
- Monitor the patient’s pain level and relief before and after administering the analgesic using the same pain assessment tool or scale. Document the pain assessment and intervention in the patient’s record.
- Monitor the patient’s vital signs and oxygen saturation before and after administering the analgesic. Report any abnormal findings or changes to the health care provider.
- Monitor the patient’s side effects and adverse reactions to the analgesic. Report any severe or unexpected symptoms to the health care provider. Manage mild or common side effects with appropriate interventions, such as providing fluids and fibre for constipation, antiemetics for nausea and vomiting, antihistamines for pruritus, and stool softeners or laxatives for opioid-induced bowel dysfunction.
- Monitor the patient’s signs and symptoms of opioid overdose, tolerance, dependence, or withdrawal. Report any concerning findings to the health care provider. Treat opioid overdose with naloxone (Mucomyst), a pure opioid antagonist that reverses the effects of opioids. Taper off opioids gradually to prevent withdrawal symptoms. Refer patients with opioid use disorder to addiction treatment programs.
- Educate the patient and family about pain management, including the causes, types, and consequences of pain; the goals, options, and benefits of analgesic therapy; the risks, side effects, and precautions of analgesic therapy; the proper use, storage, and disposal of analgesics; the signs and symptoms of overdose, tolerance, dependence, or withdrawal; and the available resources and support for pain management. Encourage the patient and family to ask questions and express their concerns about pain management.
Pain Assessment Tools and Scale Conclusion
- Pain assessment tools and scales are instruments that help measure and quantify pain intensity, quality, location, and relief. Pain assessment tools and scales are essential for evaluating the patient’s pain level, response to analgesic therapy, and need for adjustment of the pain management plan. Pain assessment tools and scales should be valid, reliable, consistent, and appropriate for the patient’s age, cognitive ability, language, and culture.
- Pain assessment tools and scales can be classified into three types: unidimensional, multidimensional, and behavioural. Unidimensional pain assessment tools and scales measure only one aspect of pain, such as intensity or severity. Multidimensional pain assessment tools and scales measure multiple aspects of pain, such as intensity, quality, location, duration, frequency, interference, coping, and affect. Behavioural pain assessment tools and scales measure the observable signs and behaviours of pain, such as facial expressions, body movements, vocalizations, and physiological changes.
- Examples of unidimensional pain assessment tools and scales include the numeric rating scale (NRS), the visual analogue scale (VAS), the faces pain scale (FPS), the verbal rating scale (VRS), the verbal descriptor scale (VDS), the colour analogue scale (CAS), and the Wong-Baker FACES pain rating scale (WBFPRS).
- These tools and scales use numbers, words, pictures, or colours to represent different levels of pain intensity or severity. The patient is asked to choose or mark the option that best describes their pain level. The NRS is a horizontal or vertical line with numbers from 0 to 10 or 1 to 10, where 0 or 1 means no pain and 10 means worst possible pain.
- The VAS is a horizontal or vertical line with no numbers or words, where one end means no pain and the other end means the worst possible pain.
- The patient is asked to mark a point on the line that corresponds to their pain level. The FPS is a horizontal line with six faces that show different expressions of pain, from no pain to very much pain. The patient is asked to point to the face that matches their pain level.
- The VRS is a list of words that describe different levels of pain intensity or severity, such as none, mild, moderate, severe, or excruciating. The patient is asked to choose the word that best describes their pain level. The VDS is a list of words that describe different qualities of pain, such as sharp, dull, throbbing, burning, or stabbing.
- The patient is asked to choose the word that best describes their pain quality. The CAS is a horizontal line with colours that represent different levels of pain intensity or severity, such as blue for no pain, green for mild pain, yellow for moderate pain, orange for severe pain, and red for worst possible pain.
- The patient is asked to mark a point on the line that corresponds to their pain level. The WBFPRS is a horizontal line with six faces that show different expressions of pain, from no hurt to hurts worst. The patient is asked to point to the face that matches their hurt level.
Examples of multidimensional pain assessment tools and scales include the McGill Pain
Questionnaire (MPQ), the Brief Pain Inventory (BPI), the Pain Disability Index (PDI), the Pain Catastrophizing Scale (PCS), and the Pain Anxiety Symptoms Scale (PASS). These tools and scales use multiple questions or items to measure different aspects of pain experience and impact.
- The patient is asked to rate or answer each question or item using numbers, words, pictures, or colours. The MPQ is a questionnaire that measures three dimensions of pain: sensory (what the pain feels like), affective (how the pain makes you feel emotionally), and evaluative (how bad the pain is overall). The patient is asked to choose words from a list that describe their pain in each dimension.
- The BPI is a questionnaire that measures four dimensions of pain: severity (how much it hurts), interference (how much it affects your daily activities), location (where it hurts), and relief (how much it improves with treatment). The patient is asked to rate their pain in each dimension using numbers from 0 to 10 or 1 to 10.
- The PDI is a questionnaire that measures how much pain interferes with the patient’s daily activities, such as work, household chores, social activities, sleep, and mood. The patient is asked to rate their pain interference in each activity using numbers from 0 to 10, where 0 means no interference and 10 means complete interference. The PCS is a questionnaire that measures how much the patient tends to magnify, ruminate, or feel helpless about their pain.
- The patient is asked to rate their agreement with each statement using numbers from 0 to 4, where 0 means not at all and 4 means all the time. The PASS is a questionnaire that measures how much the patient experiences anxiety symptoms related to their pain, such as fear, avoidance, escape, cognitive anxiety, and physiological anxiety. The patient is asked to rate the frequency of each symptom using numbers from 0 to 5, where 0 means never and 5 means always
- Examples of behavioural pain assessment tools and scales include the FLACC scale, the Checklist of Nonverbal Pain Indicators (CNPI), the Pain Assessment in Advanced Dementia (PAINAD) scale, and the Critical-Care Pain Observation Tool (CPOT). These tools and scales use observation of the patient’s facial expression, body movement, vocalization, and physiological changes to infer their pain level.
- These tools and scales are useful for patients who cannot communicate verbally or cognitively, such as infants, children, older adults with dementia, or critically ill patients. The FLACC scale is a tool that uses five categories of behaviour: face, legs, activity, cry, and controllability. Each category is scored from 0 to 2, where 0 means no pain and 2 means severe pain.
- The total score ranges from 0 to 10. The CNPI is a tool that uses six indicators of nonverbal pain: vocal complaints, facial grimaces or winces, bracing, rubbing, restlessness, and vocalizations. Each indicator is scored as present or absent. The total score ranges from 0 to 6. The PAINAD scale is a tool that uses five items of pain behaviour: breathing, negative vocalization, facial expression, body language, and controllability. Each item is scored from 0 to 2, where 0 means no pain and 2 means severe pain.
- The total score ranges from 0 to 10. The CPOT is a tool that uses four indicators of pain behaviour: facial expression, body movements, muscle tension, and compliance with the ventilator or vocalization. Each indicator is scored from 0 to 2 or from 0 to 3, where 0 means no pain and 2 or 3 means severe pain. The total score ranges from 0 to 8 or from 0 to 10.
Summary
asdgvfqefgqe
Conclusion
- Analgesics are medications that relieve pain by acting on different mechanisms and targets in the body. Analgesics are classified into three main categories: nonopioids, opioids, and adjuvants.
- Nonopioids include acetaminophen and NSAIDs, which inhibit prostaglandin synthesis and have analgesic and antipyretic effects, but not anti-inflammatory effects in the case of acetaminophen.
- Opioids include pure agonists, partial agonists, mixed agonists/antagonists, and pure antagonists, which act on opioid receptors in the brain and spinal cord and produce analgesia, sedation, euphoria, and respiratory depression.
- Adjuvants include antidepressants, anticonvulsants, corticosteroids, local anaesthetics, alpha2-adrenergic agonists, NMDA receptor antagonists, muscle relaxants, bisphosphonates, and cannabinoids, which have either independent or additive analgesic effects when used with opioids or nonopioids.
- The choice of analgesic depends on several factors, such as the type, intensity, duration, location, cause, and response to pain; the patient’s age, weight, medical history, and allergies; the availability, cost, and safety of the medication; and the patient’s preference and values.
- The route of administration of an analgesic affects the onset (how quickly the medication starts to work), the peak (when the medication reaches its highest concentration and effect), the duration (how long the medication lasts), and the dose (how much medication is needed) of the analgesic.
- The dose of an analgesic should be individualized for each patient and adjusted according to the patient’s response and tolerance.
- The half-life of an analgesic affects the frequency and duration of administration of the analgesic. The half-life depends on several factors, such as the route, formulation, absorption, distribution, metabolism, and excretion of the medication; the patient’s age, weight, medical history, allergies; and concurrent use of other medications that may affect the clearance of the drug.
- Nursing assessments for patients receiving analgesics include pain assessment, medical history, allergies, current medications, vital signs, laboratory results, response to previous analgesic therapy, preference and values regarding pain management, and risk factors for opioid misuse, abuse, addiction, overdose, or withdrawal.
- Nursing interventions for patients receiving analgesics include administering the prescribed analgesic according to the five rights of medication administration, monitoring the patient’s pain level and relief, vital signs and oxygen saturation, side effects and adverse reactions, signs and symptoms of opioid overdose, tolerance, dependence, or withdrawal, educating the patient and family about pain management, and referring patients with opioid use disorder to addiction treatment programs.
- Pain assessment tools and scales are instruments that help measure and quantify pain intensity, quality, location, and relief. Pain assessment tools and scales can be classified into three types: unidimensional, multidimensional, and behavioural. Unidimensional pain assessment tools and scales measure only one aspect of pain, such as intensity or severity.
- Multidimensional pain assessment tools and scales measure multiple aspects of pain, such as intensity, quality, location, duration, frequency, interference, coping, and affect. Behavioural pain assessment tools and scales measure the observable signs and behaviours of pain, such as facial expressions, body movements, vocalizations, and physiological changes.
Summary
- Analgesics are medications that relieve pain by acting on different mechanisms and targets in the body.
- Nonopioids include acetaminophen and NSAIDs, which inhibit prostaglandin synthesis and have analgesic and antipyretic effects, but not anti-inflammatory effects in the case of acetaminophen.
- Opioids include pure agonists, partial agonists, mixed agonists/antagonists, and pure antagonists, which act on opioid receptors in the brain and spinal cord and produce analgesia, sedation, euphoria, and respiratory depression.
- Adjuvants include antidepressants, anticonvulsants, corticosteroids, local anaesthetics, alpha2-adrenergic agonists, NMDA receptor antagonists, muscle relaxants, bisphosphonates, and cannabinoids, which have either independent or additive analgesic effects when used with opioids or nonopioids.
- The choice of analgesic depends on several factors, such as the type, intensity, duration, location, cause, and response to pain; the patient’s age, weight, medical history, and allergies; the availability, cost, and safety of the medication; and the patient’s preference and values.
- The route of administration of an analgesic affects the onset (how quickly the medication starts to work), the peak (when the medication reaches its highest concentration and effect), the duration (how long the medication lasts), and the dose (how much medication is needed) of the analgesic.
- The dose of an analgesic should be individualized for each patient and adjusted according to the patient’s response and tolerance.
- The half-life of an analgesic affects the frequency and duration of administration of the analgesic. The half-life depends on several factors, such as the route, formulation, absorption, distribution, metabolism, and excretion of the medication; the patient’s age, weight, medical history, allergies; and concurrent use of other medications that may affect the clearance of the drug.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Analgesics and Pain Management Medications
This filled cannot be empty

