Please set your exam date
Drug Interactions
Study Questions
Types of Drug Interactions
A nurse is preparing to administer warfarin to a client who also takes aspirin for arthritis pain. What action should the nurse take?
Explanation
Warfarin and aspirin are both anticoagulants that can increase the risk of bleeding. The nurse should hold the warfarin and notify the provider to avoid a potential drug interaction that could cause serious harm to the client.
b. Administering the warfarin as prescribed could result in excessive bleeding or haemorrhage.
c. Reducing the dose of warfarin by half is not appropriate without consulting the provider and monitoring the client's coagulation status.
d. Giving aspirin with food or milk may reduce gastric irritation but does not prevent the drug interaction with warfarin.
A client is prescribed phenytoin for seizure control. The client tells the nurse that they also take St. John's Wort for depression. What should the nurse teach the client?
Explanation
St. John's wort is a herbal supplement that can induce hepatic enzymes and increase the metabolism of phenytoin, reducing its serum levels and therapeutic effects. The nurse should teach the client to avoid taking St. John's wort with phenytoin and to consult the provider before using any herbal products.
a. St. John's wort does not increase the effectiveness of phenytoin but rather decreases it.
c. St. John's wort does not cause drowsiness when taken with phenytoin but rather may increase the risk of seizures due to reduced phenytoin levels.
d. St. John's wort does not cause hypertension when taken with phenytoin but rather may interact with other antihypertensive drugs and affect blood pressure.
A client is receiving gentamicin for a urinary tract infection. The client also takes furosemide for heart failure management. What adverse effect should the nurse monitor for in this client?
Explanation
Gentamicin and furosemide are both ototoxic drugs that can damage the inner ear and cause hearing loss, tinnitus, or vertigo when used together or at high doses. The nurse should monitor for signs of ototoxicity in this client and report any changes in hearing or balance to the provider.
b. Nephrotoxicity is a potential adverse effect of gentamicin and furosemide, but it is not specific to their combination.
c. Cardiotoxicity is not a common adverse effect of gentamicin or furosemide but rather may occur with other drugs that affect cardiac function, such as digoxin or beta-blockers
d. Cardiotoxicity is not a common adverse effect of gentamicin or furosemide but rather may occur with other drugs that affect cardiac function, such as digoxin or beta-blockers
A nurse is preparing to administer medication to a client. The nurse should be aware that which of the following factors can affect the absorption of the medication?
Explanation
The route of administration, the age of the client, and the presence of food in the stomach can all affect the absorption of a medication. For example, oral medications may be absorbed more slowly if taken with food, while intravenous medications are absorbed more quickly because they bypass the digestive system.
a. The route of administration can affect how quickly and completely a medication is absorbed.
b. Age can affect absorption because older adults may have decreased gastric motility and blood flow to the gastrointestinal tract.
c. The presence of food in the stomach can affect absorption by altering gastric pH and delaying gastric emptying. d. All of these factors can affect absorption.
A nurse is reviewing a client’s medication regimen and notes that the client is taking two medications that are both highly protein-bound. The nurse should recognize that this can result in which of the following?
Explanation
When two highly protein-bound medications are taken together, they can compete for binding sites on plasma proteins. This can result in an increased free fraction of one or both medications, leading to an increased risk of adverse effects, decreased effectiveness, and altered distribution.
a. An increased free fraction can result in higher plasma concentrations and an increased risk of adverse effects.
b. Competition for binding sites can decrease the effectiveness of one or both medications by decreasing their plasma concentrations.
c. Altered distribution can occur because changes in protein binding can affect how much medication is distributed to tissues. d. All of these effects can occur when two highly protein-bound medications are taken together.
A client is taking a medication that is metabolized by the liver. The nurse should recognize which of the following factors can affect the metabolism of this medication.
Explanation
The metabolism of a medication can be affected by several factors, including age, liver function, and genetic factors. For example, older adults may have decreased liver function, which can result in a slower metabolism and an increased risk of adverse effects.
a. Age can affect metabolism because liver function decreases with age.
b. Liver function is important for metabolism because many medications are metabolized by liver enzymes.
c. Genetic factors can affect metabolism because some individuals may have genetic variations that affect how they metabolize certain medications.
d. All of these factors can affect metabolism.
A nurse is administering two drugs to a patient and one drug induces the metabolism of another drug’s metabolic pathway. What effect will this have on plasma levels?
Explanation
Induction increases enzyme activity leading to faster metabolism and elimination of drugs resulting in lower plasma levels.
a. plasma levels will occur due to faster elimination of drugs.
b. Increasing plasma levels will not occur as induction increases enzyme activity leading to faster elimination of drugs.
c. No effect will not occur as induction increases enzyme activity leading to faster elimination of drugs.
d. Increasing half-life will not occur as induction increases enzyme activity leading to faster elimination of drugs.
A patient has been prescribed two drugs with opposing pharmacological actions. What effect will this have on their therapeutic effect?
Explanation
Drugs with opposing pharmacological actions will have an antagonistic effect decreasing their therapeutic effect.
a. Increasing therapeutic effect will not occur as drugs with opposing pharmacological actions will have an antagonistic effect decreasing their therapeutic effect.
b. Decreasing therapeutic effect will occur due to an antagonistic effect between drugs with opposing pharmacological actions.
c. No effect will not occur as drugs with opposing pharmacological actions will have an antagonistic effect decreasing their therapeutic effect.
d. Decreasing half-life will not occur as half-life is independent of pharmacological action.
A patient has been prescribed two drugs with one drug inhibiting another drug’s metabolic pathway. What effect will this have on plasma levels?
Explanation
Inhibition decreases enzyme activity leading to slower metabolism and elimination of drugs resulting in higher plasma levels.
a. Decreasing plasma levels will not occur as inhibition decreases enzyme activity leading to slower elimination of drugs.
b. Increasing plasma levels will occur due to slower elimination of drugs.
c. No effect will not occur as inhibition decreases enzyme activity leading to slower elimination of drugs.
d. Increasing half-life will not occur as inhibition decreases enzyme activity leading to slower elimination of drugs.
A patient has been prescribed two drugs with one drug increasing another drug’s excretion. What effect will this have on plasma levels?
Explanation
Increasing excretion leads to faster elimination of drugs resulting in lower plasma levels.
a. Decreasing plasma levels will occur due to faster elimination of drugs.
b. Increasing plasma levels will not occur as increasing excretion leads to faster elimination of drugs.
c. No effect will not occur as increasing excretion leads to faster elimination of drugs.
d. Increasing half life will not occur as increasing excretion leads to faster elimination of drugs.
A nurse is reviewing a client’s medication regimen and notes that the client is taking a medication that is known to be a substrate for CYP450 enzymes. The nurse should recognize that this can result in which of the following?
Explanation
CYP450 enzymes are responsible for metabolizing many medications. If a client is taking a medication that is a substrate for these enzymes, it can result in an increased risk of adverse effects, decreased effectiveness, and altered metabolism.
a. An increased risk of adverse effects can occur because changes in CYP450 enzyme activity can affect how quickly the medication is metabolized and eliminated from the body.
b. Decreased effectiveness can occur because changes in CYP450 enzyme activity can affect how much active drug is available to produce a therapeutic effect.
c. Altered metabolism can occur because changes in CYP450 enzyme activity can affect how the medication is metabolized and eliminated from the body.
d. All of these effects can occur when a client is taking a medication that is a substrate for CYP450 enzymes.
A nurse is preparing to administer a medication to a client who has renal impairment. The nurse should be aware that this can affect which pharmacokinetic process?
Explanation
Renal impairment can affect the excretion of medications because many medications are eliminated by the kidneys.
a. Absorption is not directly affected by renal impairment, although changes in fluid and electrolyte balance can indirectly affect absorption.
b. Distribution is not directly affected by renal impairment, although changes in fluid and electrolyte balance can indirectly affect distribution.
c. Metabolism is not directly affected by renal impairment, although changes in liver function can indirectly affect metabolism.
d. Excretion is directly affected by renal impairment because many medications are eliminated by the kidneys.
A nurse is preparing to administer a medication to a client. The nurse should be aware that which of the following factors can affect the absorption of the medication?
Explanation
The route of administration, the age of the client, and the presence of food in the stomach can all affect the absorption of a medication. For example, oral medications may be absorbed more slowly if taken with food, while intravenous medications are absorbed more quickly because they bypass the digestive system.
a. The route of administration can affect how quickly and completely a medication is absorbed.
b. Age can affect absorption because older adults may have decreased gastric motility and blood flow to the gastrointestinal tract.
c. The presence of food in the stomach can affect absorption by altering gastric pH and delaying gastric emptying.
d. All of these factors can affect absorption.
A nurse is reviewing a client's medication regimen and notes that the client is taking two medications that are both highly protein-bound. The nurse should recognize that this can result in which of the following?
Explanation
When two highly protein-bound medications are taken together, they can compete for binding sites on plasma proteins. This can result in an increased free fraction of one or both medications, leading to an increased risk of adverse effects, decreased effectiveness, and altered distribution.
a. An increased free fraction can result in higher plasma concentrations and an increased risk of adverse effects.
b. Competition for binding sites can decrease the effectiveness of one or both medications by decreasing their plasma concentrations.
c. Altered distribution can occur because changes in protein binding can affect how much medication is distributed to tissues.
d. All of these effects can occur when two highly protein-bound medications are taken together.
Factors Affecting Drug Interactions
A nurse is reviewing a client’s medication regimen and notes that the client is taking two medications with similar pharmacological actions. The nurse should recognize that this can result in which of the following?
Explanation
When two medications with similar pharmacological actions are taken together, their effects can be additive, resulting in an increased therapeutic effect.
a. An increased therapeutic effect can occur because the combined effect of the two medications is greater than the effect of either medication alone.
b. A decreased therapeutic effect is not likely to occur because the combined effect of the two medications is greater than the effect of either medication alone.
c. No change in therapeutic effect is not likely to occur because the combined effect of the two medications is greater than the effect of either medication alone.
d. An increased risk of adverse effects can occur if the combined effect of the two medications results in excessive drug action.
A nurse is reviewing a client’s medication regimen and notes that the client is taking two medications with opposing pharmacological actions. The nurse should recognize that this can result in which of the following?
Explanation
When two medications with opposing pharmacological actions are taken together, their effects can be antagonistic, resulting in a decreased therapeutic effect.
a. An increased therapeutic effect is not likely to occur because the opposing actions of the two medications can cancel each other out.
b. A decreased therapeutic effect can occur because the opposing actions of the two medications can cancel each other out.
c. No change in therapeutic effect is not likely to occur because the opposing actions of the two medications can cancel each other out.
d. An increased risk of adverse effects is not likely to occur because the opposing actions of the two medications can cancel each other out.
A nurse is preparing to administer medication to a client who has a history of drug allergies. The nurse should be aware that this can increase the client’s risk for which of the following?
Explanation
A history of drug allergies can increase a client’s risk for adverse drug reactions because allergic reactions are a type of adverse drug reaction.
a. Drug-drug interactions are not directly related to a history of drug allergies.
b. Drug-disease interactions are not directly related to a history of drug allergies.
c. Drug-food interactions are not directly related to a history of drug allergies.
d. Adverse drug reactions can occur as a result of an allergic reaction to a medication.
A patient has been prescribed two drugs with one being an agonist and another being an antagonist at the same receptor. What will be their combined effect?
Explanation
An antagonist will decrease an agonist’s action by competing for binding at the same receptor.
a. Increasing agonist’s action will not occur as an antagonist will decrease an agonist’s action by competing for binding at the same receptor.
b. Decreasing agonist’s action will occur due to competition for binding at the same receptor by an antagonist.
c. No change will not occur as an antagonist will decrease an agonist’s action by competing for binding at the same receptor.
d. Increasing antagonist’s action will not occur as an antagonist will decrease an agonist’s action by competing for binding at the same receptor.
A patient has been prescribed two drugs with one being an agonist and another being an inverse agonist at the same receptor. What will be their combined effect?
Explanation
An inverse agonist will decrease an agonist’s action by competing for binding at the same receptor and producing an opposite response.
a. Increasing agonist’s action will not occur as an inverse agonist will decrease an agonist’s action by competing for binding at the same receptor and producing an opposite response.
b. Decreasing agonist’s action will occur due to competition for binding at the same receptor by an inverse agonist and producing an opposite response.
c. No change will not occur as an inverse agonist will decrease an agonist’s action by competing for binding at the same receptor and producing an opposite response.
d. Increasing the inverse agonist’s action will not occur as an inverse agonist will decrease an agonist’s action by competing for binding at the same receptor and producing an opposite response.
A patient has been prescribed two drugs with one being an agonist and another being a partial agonist at the same receptor. What will be their combined effect?
Explanation
A partial agonist will decrease an agonist’s action by competing for binding at the same receptor and producing a submaximal response.
a. Increasing agonist’s action will not occur as a partial agonist will decrease an agonist’s action by competing for binding at the same receptor and producing a submaximal response.
b. Decreasing agonist’s action will occur due to competition for binding at the same receptor by a partial agonist and producing a submaximal response.
c. No change will not occur as a partial agonist will decrease an agonist’s action by competing for binding at the same receptor and producing a submaximal response.
d. Increasing partial agonist’s action will not occur as a partial agonist will decrease an agonist’s action by competing for binding at the same receptor and producing a submaximal response.
A patient has been prescribed two drugs with one being an antagonist and another being a partial agonist at the same receptor. What will be their combined effect?
Explanation
An antagonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
a. Increasing the antagonist’s action will not occur as an antagonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
b. Decreasing the antagonist’s action will not occur as an antagonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
c. No change will not occur as an antagonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
d. Increasing partial agonist’s action will occur due to competition for binding at the same receptor by an antagonist and decreasing the basal activity.
A patient has been prescribed two drugs with one being an inverse agonist and another being a partial agonist at the same receptor. What will be their combined effect?
Explanation
An inverse agonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
a. Increasing inverse agonist’s action will not occur as an inverse agonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
b. Decreasing the inverse agonist’s action will not occur as an inverse agonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
c. No change will not occur as an inverse agonist will increase a partial agonist’s action by competing for binding at the same receptor and decreasing the basal activity.
d. Increasing partial agonist’s action will occur due to competition for binding at the same receptor by an inverse agonist and decreasing the basal activity.
A patient has been prescribed two drugs with one being an antagonist and another being an inverse agonist at the same receptor. What will be their combined effect?
Explanation
An antagonist and an inverse agonist will have no combined effect as they both decrease the basal activity of the receptor.
a. Increasing antagonist action will not occur as both drugs decrease the basal activity of the receptor.
b. Decreasing antagonist action will not occur as both drugs decrease the basal activity of the receptor.
c. No change in effect will occur as both drugs decrease the basal activity of the receptor.
d. Increasing inverse agonist action will not occur as both drugs decrease the basal activity of the receptor.
A patient has been prescribed two drugs with one being an agonist and another being an antagonist at different receptors. What will be their combined effect?
Explanation
An agonist and an antagonist at different receptors will have no combined effect as they act on different receptors.
a. Additive effect will not occur as both drugs act on different receptors.
b. Synergistic effect will not occur as both drugs act on different receptors.
c. Antagonistic effect will not occur as both drugs act on different receptors.
d. No change in effect will occur as both drugs act on different receptors.
Contraindications to Drugs
A nurse is reviewing a client’s medication regimen and notes that the client has a history of liver disease. The nurse should recognize which of the following medications is contraindicated for this client.
Explanation
Acetaminophen is contraindicated in clients with liver disease because it is metabolized by the liver and can cause liver toxicity.
a. Acetaminophen is contraindicated in clients with liver disease because it can cause liver toxicity.
b. Ibuprofen is not contraindicated in clients with liver disease, although it should be used with caution because it can cause liver toxicity in high doses.
c. Aspirin is not contraindicated in clients with liver disease, although it should be used with caution because it can cause liver toxicity in high doses.
d. Naproxen is not contraindicated in clients with liver disease, although it should be used with caution because it can cause liver toxicity in high doses.
A nurse is reviewing a client’s medication regimen and notes that the client has a history of renal impairment. The nurse should recognize which of the following medications is contraindicated for this client.
Explanation
Metformin is contraindicated in clients with renal impairment because it is eliminated by the kidneys and can accumulate to toxic levels if renal function is impaired.
a. Metformin is contraindicated in clients with renal impairment because it can accumulate to toxic levels if renal function is impaired.
b. Glipizide is not contraindicated in clients with renal impairment, although it should be used with caution because it can cause hypoglycemia if renal function is impaired.
c. Glyburide is not contraindicated in clients with renal impairment, although it should be used with caution because it can cause hypoglycemia if renal function is impaired.
d. Pioglitazone is not contraindicated in clients with renal impairment, although it should be used with caution because it can cause fluid retention if renal function is impaired.
A patient has been prescribed a drug that interacts with alcohol.What should they avoid?
Explanation
Wine contains alcohol and should be avoided when taking drugs that interact with alcohol.
a. Wine contains alcohol and should be avoided when taking drugs that interact with alcohol.
b. Bananas do not contain alcohol and do not need to be avoided when taking drugs that interact with alcohol.
c. Oranges do not contain alcohol and do not need to be avoided when taking drugs that interact with alcohol.
d. Apples do not contain alcohol and do not need to be avoided when taking drugs that interact with alcohol.
A patient has been prescribed a drug that interacts with caffeine. What should they avoid?
Explanation
Coffee is high in caffeine and should be avoided when taking drugs that interact with caffeine.
a. Coffee is high in caffeine and should be avoided when taking drugs that interact with caffeine.
b. Bananas are not high in caffeine and do not need to be avoided when taking drugs that interact with caffeine.
c. Oranges are not high in caffeine and do not need to be avoided when taking drugs that interact with caffeine.
d. Apples are not high in caffeine and do not need to be avoided when taking drugs that interact with caffeine.
A patient has been prescribed a drug that interacts with sodium. What should they avoid?
Explanation
Salt is high in sodium and should be avoided when taking drugs that interact with sodium.
a. Salt is high in sodium and should be avoided when taking drugs that interact with sodium.
b. Bananas are not high in sodium and do not need to be avoided when taking drugs that interact with sodium.
c. Oranges are not high in sodium and do not need to be avoided when taking drugs that interact with sodium.
d. Apples are not high in sodium and do not need to be avoided when taking drugs that interact with sodium.
A patient has been prescribed a drug that interacts with iron. What should they avoid?
Explanation
Red meat is high in iron and should be avoided when taking drugs that interact with iron.
a. Red meat is high in iron and should be avoided when taking drugs that interact with iron.
b. Bananas are not high in iron and do not need to be avoided when taking drugs that interact with iron.
c. Oranges are not high in iron and do not need to be avoided when taking drugs that interact with iron.
d. Apples are not high in iron and do not need to be avoided when taking drugs that interact with iron.
A patient has been prescribed a drug that interacts with vitamin C. What should they avoid?
Explanation
Oranges are high in vitamin C and should be avoided when taking drugs that interact with vitamin C.
a. Oranges are high in vitamin C and should be avoided when taking drugs that interact with vitamin C.
b. Bananas are not high in vitamin C and do not need to be avoided when taking drugs that interact with vitamin C.
c. Milk is not high in vitamin C and does not need to be avoided when taking drugs that interact with vitamin C.
d. Apples are not high in vitamin C and do not need to be avoided when taking drugs that interact with vitamin C.
A nurse is reviewing a client’s medication regimen and notes that the client has a history of peptic ulcer disease. The nurse should recognize which of the following medications is contraindicated for this client.
Explanation
Ibuprofen is contraindicated in clients with peptic ulcer disease because it can irritate the stomach lining and exacerbate the condition.
a. Ibuprofen is contraindicated in clients with peptic ulcer disease because it can irritate the stomach lining and exacerbate the condition.
b. Acetaminophen is not contraindicated in clients with peptic ulcer disease because it does not irritate the stomach lining.
c. Aspirin is contraindicated in clients with peptic ulcer disease because it can irritate the stomach lining and exacerbate the condition.
d. Naproxen is contraindicated in clients with peptic ulcer disease because it can irritate the stomach lining and exacerbate the condition.
A nurse is reviewing a client’s medication regimen and notes that the client has a history of heart failure. The nurse should recognize which of the following medications is contraindicated for this client.
Explanation
Pioglitazone is contraindicated in clients with heart failure because it can cause fluid retention, which can exacerbate heart failure.
a. Metoprolol is not contraindicated in clients with heart failure, although it should be used with caution because it can decrease cardiac output.
b. Lisinopril is not contraindicated in clients with heart failure, although it should be used with caution because it can cause hypotension.
c. Furosemide is not contraindicated in clients with heart failure, although it should be used with caution because it can cause electrolyte imbalances.
d. Pioglitazone is contraindicated in clients with heart failure because it can cause fluid retention, which can exacerbate heart failure.
A patient has been prescribed a drug that interacts with potassium. What should they avoid?
Explanation
Bananas are high in potassium and should be avoided when taking drugs that interact with potassium.
a. Bananas are high in potassium and should be avoided when taking drugs that interact with potassium.
b. Salt is not high in potassium and does not need to be avoided when taking drugs that interact with potassium.
c. Oranges are not high in potassium and do not need to be avoided when taking drugs that interact with potassium.
d. Apples are not high in potassium and do not need to be avoided when taking drugs that interact with potassium.
Drug-Food Interactions
A nurse is reviewing a client’s medication regimen and notes that the client is taking a medication that should be taken on an empty stomach. The nurse should instruct the client to take the medication for how long before or after eating.
Explanation
Medications that should be taken on an empty stomach should generally be taken 1 hour before or 2 hours after eating to ensure optimal absorption.
a. Taking the medication 15 minutes before or after eating may not provide enough time for the stomach to empty.
b. Taking the medication 30 minutes before or after eating may not provide enough time for the stomach to empty.
c. Taking the medication 1 hour before or 2 hours after eating provides enough time for the stomach to empty and ensures optimal absorption.
d. Taking the medication 2 hours before or after eating may provide enough time for the stomach to empty, but it is not necessary to wait this long.
A nurse is reviewing a client’s medication regimen and notes that the client is taking a medication that can interact with grapefruit juice. The nurse should instruct the client to avoid consuming grapefruit juice for how long before and after taking the medication?
Explanation
Grapefruit juice can interact with certain medications by inhibiting the CYP3A4 enzyme, which is responsible for metabolizing many medications. To avoid this interaction, clients should avoid consuming grapefruit juice for at least 4 hours before and after taking the medication.
a. Avoiding grapefruit juice for only 15 minutes before and after taking the medication may not provide enough time to prevent an interaction.
b. Avoiding grapefruit juice for only 30 minutes before and after taking the medication may not provide enough time to prevent an interaction.
c. Avoiding grapefruit juice for only 1 hour before and after taking the medication may not provide enough time to prevent an interaction.
d. Avoiding grapefruit juice for at least 4 hours before and after taking the medication provides enough time to prevent an interaction.
A patient has been prescribed a drug that interacts with vitamin K. What food should they avoid?
Explanation
Spinach is high in vitamin K and should be avoided when taking drugs that interact with vitamin K.
a. Spinach is high in vitamin K and should be avoided when taking drugs that interact with vitamin K.
b. Bananas are not high in vitamin K and do not need to be avoided when taking drugs that interact with vitamin K.
c. Oranges are not high in vitamin K and do not need to be avoided when taking drugs that interact with vitamin K.
d. Apples are not high in vitamin K and do not need to be avoided when taking drugs that interact with vitamin K.
A patient has been prescribed a drug that interacts with tyramine. What food should they avoid?
Explanation
Cheese is high in tyramine and should be avoided when taking drugs that interact with tyramine.
a. Cheese is high in tyramine and should be avoided when taking drugs that interact with tyramine.
b. Bananas are not high in tyramine and do not need to be avoided when taking drugs that interact with tyramine.
c. Oranges are not high in tyramine and do not need to be avoided when taking drugs that interact with tyramine.
d. Apples are not high in tyramine and do not need to be avoided when taking drugs that interact with tyramine.
A patient has been prescribed a drug that interacts with calcium. What food should they avoid?
Explanation
Milk is high in calcium and should be avoided when taking drugs that interact with calcium.
a. Milk is high in calcium and should be avoided when taking drugs that interact with calcium.
b. Bananas are not high in calcium and do not need to be avoided when taking drugs that interact with calcium.
c. Oranges are not high in calcium and do not need to be avoided when taking drugs that interact with calcium.
d. Apples are not high in calcium and do not need to be avoided when taking drugs that interact with calcium.
A patient has been prescribed a drug that interacts with caffeine. What food should they avoid?
Explanation
Coffee is high in caffeine and should be avoided when taking drugs that interact with caffeine.
a. Coffee is high in caffeine and should be avoided when taking drugs that interact with caffeine.
b. Bananas are not high in caffeine and do not need to be avoided when taking drugs that interact with caffeine.
c. Oranges are not high in caffeine and do not need to be avoided when taking drugs that interact with caffeine.
d. Apples are not high in caffeine and do not need to be avoided when taking drugs that interact with caffeine.
A patient has been prescribed a drug that interacts with alcohol. What food should they avoid?
Explanation
Wine contains alcohol and should be avoided when taking drugs that interact with alcohol.
a. Wine contains alcohol and should be avoided when taking drugs that interact with alcohol.
b. Bananas do not contain alcohol and do not need to be avoided when taking drugs that interact with alcohol.
c. Oranges do not contain alcohol and do not need to be avoided when taking drugs that interact with alcohol.
d. Apples do not contain alcohol and do not need to be avoided when taking drugs that interact with alcohol.
A patient has been prescribed a drug that interacts with sodium. What food should they avoid?
Explanation
Salt is high in sodium and should be avoided when taking drugs that interact with sodium.
a. Salt is high in sodium and should be avoided when taking drugs that interact with sodium.
b. Bananas are not high in sodium and do not need to be avoided when taking drugs that interact with sodium.
c. Oranges are not high in sodium and do not need to be avoided when taking drugs that interact with sodium.
d. Apples are not high in sodium and do not need to be avoided when taking drugs that interact with sodium.
A patient has been prescribed a drug that interacts with iron. What food should they avoid?
Explanation
Red meat is high in iron and should be avoided when taking drugs that interact with iron.
a. Red meat is high in iron and should be avoided when taking drugs that interact with iron.
b. Bananas are not high in iron and do not need to be avoided when taking drugs that interact with iron.
c. Oranges are not high in iron and do not need to be avoided when taking drugs that interact with iron.
d. Apples are not high in iron and do not need to be avoided when taking drugs that interact with iron.
A patient has been prescribed a drug that interacts with vitamin C. What food should they avoid?
Explanation
Oranges are high in vitamin C and should be avoided when taking drugs that interact with vitamin C.
a. Oranges are high in vitamin C and should be avoided when taking drugs that interact with vitamin C.
b. Bananas are not high in vitamin C and do not need to be avoided when taking drugs that interact with vitamin C.
c. Milk is not high in vitamin C and does not need to be avoided when taking drugs that interact with vitamin C.
d. Apples are not high in vitamin C and do not need to be avoided when taking drugs that interact with vitamin C.
Exams on Drug Interactions
Custom Exams
Login to Create a Quiz
Click here to loginDrug Interactions
Lessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Login to View Drug Interactions Study Video
Notes Highlighting is available once you sign in. Login Here.
Introduction
- Drug interactions occur when the effects of one drug are altered by the presence of another drug, food, or substance.
- Interactions can lead to increased or decreased drug efficacy, toxicity, or the emergence of new side effects.
- Understanding drug interactions is essential for healthcare professionals to ensure patient safety and optimize therapeutic outcomes.
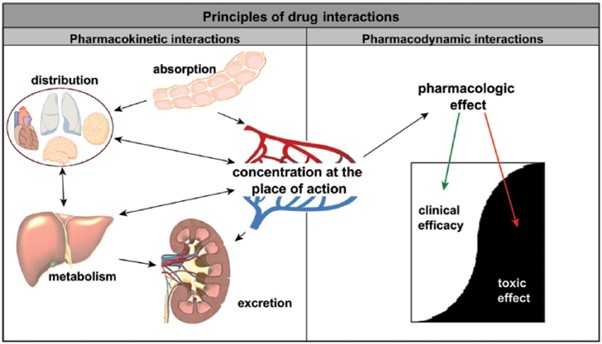
Types of Drug Interactions
A. Pharmacokinetic Interactions
1. Absorption
- Interference with drug absorption, e.g., antacids reducing the absorption of certain antibiotics.
- Examples: Tetracycline antibiotics with antacids, iron supplements, or dairy products.
2. Distribution
- Alterations in drug distribution, e.g., displacement from protein-binding sites by another drug.
- Examples: Warfarin displacement by aspirin, leading to increased bleeding risk.
3. Metabolism
- Inhibition or induction of drug metabolism by interacting substances, affecting drug levels.
- Examples: Grapefruit juice inhibiting the metabolism of certain statins, leading to increased statin levels and potential toxicity.
4. Elimination
- Interference with drug elimination, leading to increased or decreased drug levels.
- Examples: Probenecid reducing renal clearance of penicillin, resulting in increased penicillin levels.
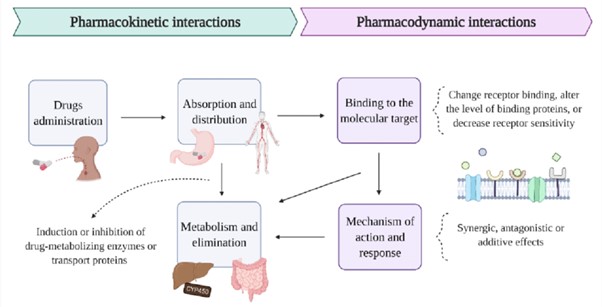
B. Pharmacodynamic Interactions
A. Additive Effects
- Additive effects occur when two drugs with similar pharmacological actions are combined, resulting in enhanced therapeutic effects.
- The combined effect is equal to the sum of the effects of each drug used alone.
- Examples:
Combining two antihypertensive drugs, such as an angiotensin-converting enzyme (ACE) inhibitor and a diuretic, to achieve better blood pressure control.
Using opioid analgesics in combination with non-opioid analgesics for more effective pain relief.
B. Synergistic Effects
- Synergistic effects occur when two drugs interact to produce an effect greater than the sum of their individual effects.
- The combined effect is more potent or more beneficial than what would be expected from each drug alone.
- Examples:
Combining an antibiotic with a beta-lactamase inhibitor enhances the antibacterial activity against resistant bacteria.
Administering opioids with sedatives or anaesthetics to achieve a deeper level of anaesthesia during surgery.
C. Antagonistic Effects
Antagonistic effects occur when two drugs interact and their combined effect is less than the sum of their individual effects.
The interaction may result in reduced therapeutic effects or increased toxicity.
Examples:
Combining an opioid antagonist with opioids to reverse their effects in cases of overdose or respiratory depression.
Using a beta-blocker in combination with a beta-agonist may lead to diminished bronchodilator response.
Factors Affecting Drug Interactions
A. Polypharmacy
- Polypharmacy refers to the concurrent use of multiple medications by a patient.
- Taking multiple medications increases the risk of drug interactions.
- The likelihood of drug interactions is further influenced by the number of medications used, their pharmacological properties, and the duration of therapy.
B. Pharmacokinetics
1. Absorption
- Variations in drug absorption can affect the extent and rate of drug interactions.
- Factors influencing drug absorption include route of administration, gastric pH, gastrointestinal motility, and the presence of food or other drugs that affect absorption.
2. Distribution
- Drug distribution can be influenced by protein binding, tissue binding, and volume of distribution.
- Drug interactions may occur if a drug displaces another drug from protein-binding sites, leading to increased free drug concentrations and potential toxicity.
3. Metabolism
- Drug metabolism primarily occurs in the liver through various enzymatic pathways.
- Enzyme induction or inhibition by other drugs can alter the metabolism of a drug, affecting its efficacy and safety.
- Genetic variations in drug-metabolizing enzymes (pharmacogenetics) can also contribute to individual variability in drug interactions.
3. Elimination
- Drug elimination primarily occurs via renal excretion, but it can also involve hepatic metabolism, biliary excretion, or other routes.
- Drugs that undergo renal excretion may interact with other drugs that affect renal function or compete for renal clearance.
C. Pharmacodynamics
- Pharmacodynamics refers to the study of a drug's effects on the body and the relationship between drug concentration and response.
- Variations in pharmacodynamic interactions can arise from drug-receptor interactions, additive or synergistic effects, or opposing actions.
D. Patient-Specific Factors
1. Age
- Age-related changes in pharmacokinetics and pharmacodynamics can influence the occurrence and severity of drug interactions.
- Pediatrics and geriatrics populations are particularly vulnerable to drug interactions due to altered drug metabolism and organ function.
2. Comorbidities and Organ Dysfunction
- Patients with underlying medical conditions, such as liver or kidney disease, may have impaired drug metabolism or elimination, increasing the risk of drug interactions.
- Organ dysfunction can alter drug distribution, metabolism, and excretion, affecting the likelihood and consequences of drug interactions.
3. Genetics and Pharmacogenetics
- Genetic variations can influence drug metabolism, receptor interactions, and drug transporters, leading to individual variability in drug interactions.
- Pharmacogenetic testing can help identify patients at risk for specific drug interactions based on their genetic profiles.
4. Concurrent Medications and Substances
- The concomitant use of multiple medications increases the potential for drug interactions.
- Drug interactions can occur between prescription medications, over-the-counter drugs, herbal supplements, and recreational substances.
- Certain substances, such as alcohol or tobacco, can also influence drug interactions.
Assessing and Managing Drug Interactions
A. Patient Assessment
- Collecting a thorough medical history, including current medications, allergies, and medical conditions.
- Identifying potential contraindications and interactions based on patient-specific factors.
B. Drug Information Resources
- Utilizing reliable drug information resources, such as drug interaction databases and clinical decision support systems.
- These resources provide comprehensive information on potential drug interactions and management strategies.
C. Communication and Collaboration
- Effective communication between healthcare professionals, including prescribers, pharmacists, and nurses, to discuss and manage potential drug interactions.
- Collaborative efforts ensure patient safety and optimize medication therapy.
V. Strategies to Minimize Drug Interactions
A. Medication Reconciliation
- Regularly reviewing and updating the patient's medication profile to identify potential interactions.
- Involves comparing the patient's current medication list with the prescribed medications.
B. Patient Education
- Providing patients with information on potential drug interactions and the importance of disclosing all medications, including over-the-counter drugs and herbal supplements.
- Encouraging patients to consult healthcare professionals before starting or stopping any medications.
C. Dose Adjustment
- Modifying medication doses based on known interactions to minimize adverse effects.
- Individualizing therapy based on patient factors, such as age, renal function, and concomitant medications.
D. Therapeutic Drug Monitoring
- Monitoring drug levels in the blood to ensure therapeutic efficacy and minimize toxicity in the presence of potential interactions.
- Adjusting medication doses based on therapeutic drug monitoring results.
VI. Conclusion
- Understanding and managing drug interactions are crucial for healthcare professionals to provide safe and effective pharmacotherapy.
- Assessing patient-specific factors, utilizing drug information resources, and promoting interdisciplinary collaboration are key to minimizing the risk of drug interactions and optimizing patient outcomes.
Contraindications to Drugs
I. Introduction
- Contraindications to drugs refer to specific situations or conditions in which the use of a particular drug is potentially harmful or not recommended.
- Understanding contraindications is essential for healthcare professionals to ensure safe and effective medication use.
II. General Contraindications
A. Absolute Contraindications
- Absolute contraindications indicate situations where the use of a drug is strictly prohibited due to the potential for severe harm or life-threatening effects.
- Examples:
- Allergy or Hypersensitivity: Patients with a known allergy or hypersensitivity to the drug or its components should avoid its use.
- Pregnancy and Lactation: Drugs known to have teratogenic effects or pose significant risks to the fetus or breastfeeding infants should be avoided.
- Severe Organ Dysfunction: Drugs that are primarily metabolized or eliminated by a dysfunctional organ may accumulate, leading to toxicity.
B. Relative Contraindications
- Relative contraindications suggest caution in using a drug due to the potential for increased risk or unfavourable outcomes. The decision to use the drug should be carefully evaluated on a case-by-case basis.
- Examples:
- Pre-existing Medical Conditions: Certain medical conditions, such as cardiovascular disease, respiratory disorders, or psychiatric disorders, may require caution or specific dose adjustments due to the potential for exacerbation or complications.
- Age-related Considerations: Pediatric and geriatric populations may have specific contraindications due to differences in drug metabolism, organ function, or susceptibility to adverse effects.
- Drug Interactions: Concurrent use of drugs with known interactions or overlapping mechanisms of action may lead to adverse effects or reduced efficacy.
III. Contraindications to Specific Drugs
A. Examples of Commonly Used Drugs and their Contraindications
- Aspirin (acetylsalicylic acid)
- Contraindications:
- Active peptic ulcer disease
- Hemophilia or other bleeding disorders
- Hypersensitivity to aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs)
- Contraindications:
- Warfarin
- Contraindications:
- Active bleeding or hemorrhagic tendencies
- Severe liver or kidney dysfunction
- Pregnancy (especially during the first trimester)
- Contraindications:
- ACE inhibitors (e.g., lisinopril)
- Contraindications:
- History of angioedema related to ACE inhibitor use
- Bilateral renal artery stenosis
- Pregnancy
- Contraindications:
- Statins (e.g., atorvastatin, simvastatin)
- Contraindications:
- Active liver disease or unexplained persistent elevations in liver function tests
- Pregnancy or breastfeeding
- Concomitant use of certain medications, such as cyclosporine or gemfibrozil
- Contraindications:
B. Importance of Drug-Specific Contraindications
- Each drug has specific contraindications based on its mechanism of action, pharmacokinetics, and potential adverse effects.
- Healthcare professionals must be familiar with drug-specific contraindications to make informed decisions about drug therapy.
IV. Identifying and Managing Contraindications
A. Thorough Patient Assessment
- Conduct a comprehensive patient assessment, including medical history, current medications, allergies, and pregnancy or breastfeeding status, to identify potential contraindications.
B. Consultation and Collaboration
- Collaborate with prescribers, pharmacists, and specialists to verify and confirm contraindications.
- Seek expert advice when needed to ensure appropriate decision-making.
C. Risk-Benefit Evaluation
- Consider the potential benefits and risks associated with the drug use in light of the identified contraindications.
- Weigh the potential benefits against the potential harm to determine if the drug should be used or alternative options should be considered.
D. Patient Education
- Communicate and educate patients about the contraindications associated with their prescribed medications.
- Emphasize the importance of adhering to contraindication recommendations and reporting any adverse effects or concerns promptly.
V. Conclusion
- Contraindications to drugs play a crucial role in ensuring safe and effective medication use.
- Understanding general contraindications and drug-specific contraindications is vital for healthcare professionals to make informed decisions, minimize potential harm, and optimize therapeutic outcomes.
Drug-Food Interactions
I. Introduction
- Drug-food interactions occur when the administration of certain foods or beverages affects the absorption, metabolism, distribution, or elimination of drugs, leading to altered therapeutic outcomes or increased risk of adverse effects.
- Understanding drug-food interactions is crucial for healthcare professionals to ensure safe and effective medication use.
II. Types of Drug-Food Interactions
A. Food Interfering with Absorption
1. Delayed Absorption
- Some foods can delay drug absorption by slowing gastric emptying or affecting gastrointestinal motility.
- Examples: High-fat meals can delay the absorption of certain antibiotics, such as tetracyclines.
2. Enhanced Absorption
- Certain foods or substances can enhance drug absorption by altering gastric pH or stimulating gastrointestinal motility.
- Examples: Citrus fruits or acidic beverages can enhance the absorption of iron supplements.
B. Food Interfering with Metabolism
1. Inhibition of Drug Metabolism
- Certain foods or beverages can inhibit drug-metabolizing enzymes, leading to increased drug levels and potential toxicity.
- Examples: Grapefruit juice inhibits the metabolism of some statins, increasing the risk of myopathy or rhabdomyolysis.
2. Induction of Drug Metabolism
- Some foods can induce drug-metabolizing enzymes, leading to decreased drug levels and reduced therapeutic efficacy.
- Examples: St. John's wort induces cytochrome P450 enzymes, potentially reducing the effectiveness of oral contraceptives or anticoagulants.
C. Food Interfering with Drug Distribution
- Certain foods or substances can bind to drugs or alter their distribution within the body, affecting their pharmacokinetic properties.
- Examples: High calcium foods can bind to tetracycline antibiotics, reducing their absorption and effectiveness.
III. Factors Influencing Drug-Food Interactions
A. Pharmacokinetic Factors
- Drug properties such as solubility, stability, and pH can influence the occurrence and extent of drug-food interactions.
- The route of administration and the timing of drug and food ingestion also play a role.
B. Individual Variability
- Individual factors such as age, genetics, and underlying health conditions can influence the susceptibility to drug-food interactions.
- Individuals with compromised gastrointestinal function, liver or kidney dysfunction, or specific genetic variations may be more susceptible.
C. Dietary Factors
- The composition and characteristics of the ingested food or beverages can affect drug interactions.
- Factors such as the quantity consumed, fat content, acidity, and specific nutrients can impact drug absorption, metabolism, or distribution.
IV. Management and Prevention of Drug-Food Interactions
A. Patient Education
- Educate patients about potential drug-food interactions and the importance of following specific dietary instructions provided with their medications.
- Encourage patients to consult healthcare professionals or pharmacists if they have questions or concerns about drug-food interactions.
B. Timing of Medication Administration
- Instruct patients to take medications as directed, either with or without food, as specified by healthcare professionals.
- Certain medications may require specific timing in relation to meals to optimize absorption or minimize interactions.
C. Medication Alternatives
- Consider alternative medications or dosage forms that have fewer or no significant interactions with food if a drug-food interaction poses a significant risk.
- For example, enteric-coated formulations may be used to bypass the stomach and minimize interactions with certain foods.
D. Collaboration with Healthcare Team
- Collaborate with other healthcare professionals, including prescribers and pharmacists, to identify potential drug-food interactions and optimize medication therapy.
- Consult reliable drug information resources and guidelines to guide decision-making.
V. Conclusion
- Drug-food interactions can have significant implications for medication efficacy and safety.
- Understanding the different types of drug-food interactions, and factors influencing their occurrence, and implementing appropriate management strategies are essential in ensuring optimal therapeutic outcomes and patient safety.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Drug Interactions
This filled cannot be empty

