Please set your exam date
Pre-eclampsia, Eclampsia
Study Questions
Fetal Complications
A nurse is caring for a client who is 32 weeks pregnant and has been diagnosed with mild preeclampsia.
Which of the following interventions should the nurse include in the plan of care? Select all that apply.
Explanation
The correct answer is choice A, C and D. Here is why:
• Choice A is correct because monitoring blood pressure and urine protein daily is a standard intervention for mild preeclampsia to detect any worsening of the condition.
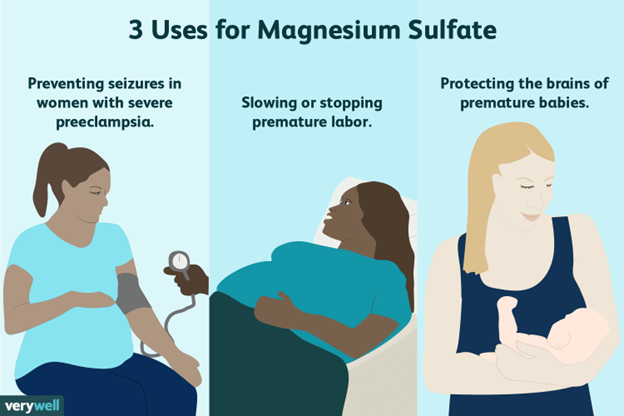
• Choice B is wrong because magnesium sulfate is not prescribed for mild preeclampsia, but for severe preeclampsia or eclampsia to prevent seizures.
• Choice C is correct because encouraging bedrest in left lateral position can improve uteroplacental perfusion and reduce blood pressure in mild preeclampsia.
• Choice D is correct because teaching the client to report headache or visual changes can help identify signs of severe preeclampsia or impending eclampsia, which require immediate medical attention.
• Choice E is wrong because restricting fluid intake to 1.5 L per day is not indicated for mild preeclampsia and can cause dehydration and electrolyte imbalance.
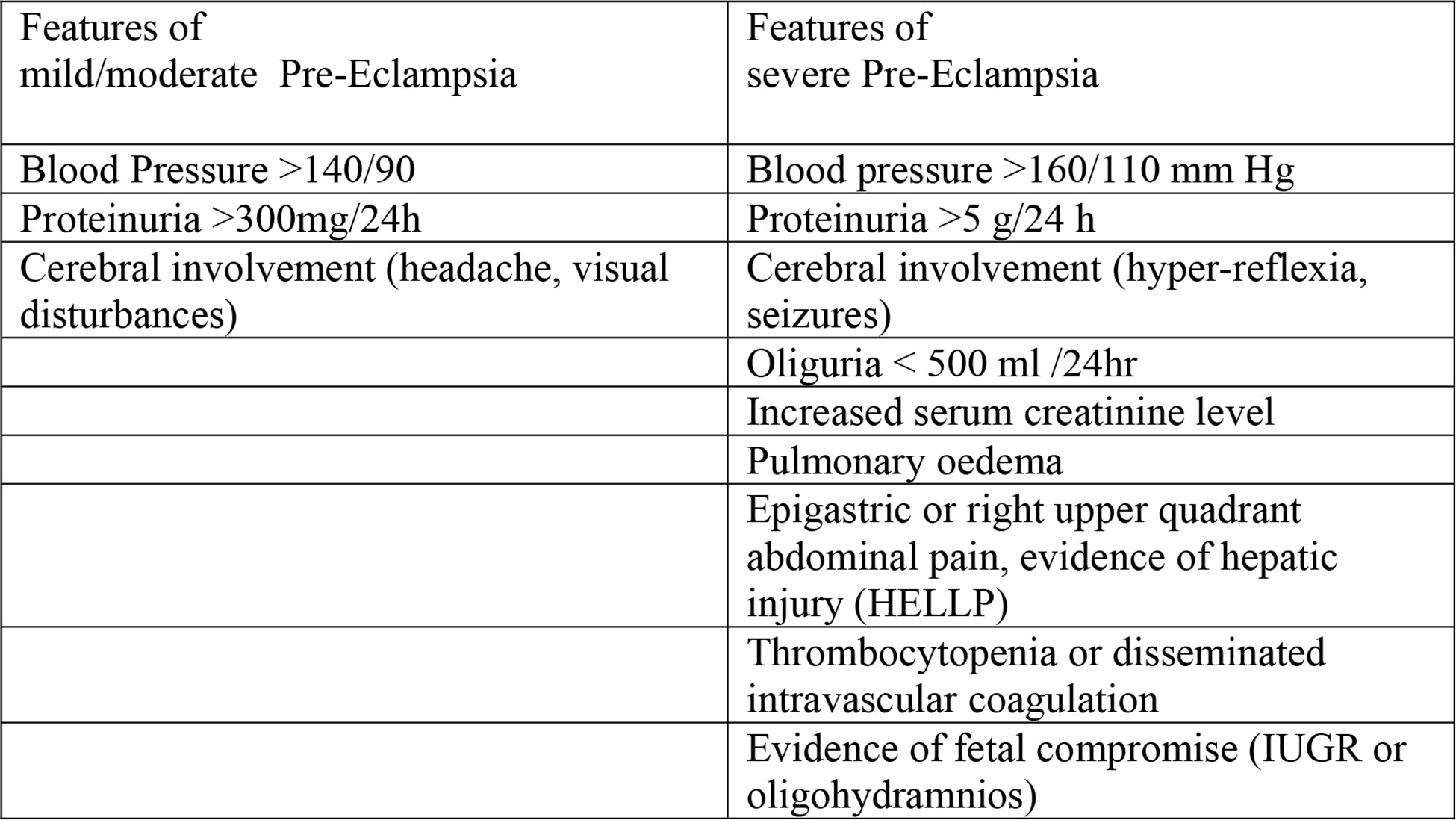
Normal ranges for blood pressure and urine protein in pregnancy are:
• Blood pressure: less than 140/90 mmHg
• Urine protein: less than 300 mg/24 hours
A nurse is reviewing the laboratory results of a client who is 36 weeks pregnant and has severe preeclampsia.
Which of the following findings should the nurse report to the provider immediately?
Explanation
A platelet count of 100,000/mm3 is below the normal range of 150,000 to 450,000/mm3 and indicates thrombocytopenia.Thrombocytopenia is a common coagulation abnormality in preeclampsia and can increase the risk of bleeding complications.
The nurse should report this finding to the provider immediately.
Choice B is wrong because a serum creatinine of 0.8 mg/dL is within the normal range of 0.5 to 1.1 mg/dL for women and does not indicate renal impairment.
Choice C is wrong because a serum uric acid of 6 mg/dL is within the normal range of 2.4 to 6 mg/dL for women and does not indicate hyperuricemia.
Choice D is wrong because a serum albumin of 3.5 g/dL is within the normal range of 3.4 to 5.4 g/dL for adults and does not indicate hypoalbuminemia.
A nurse is preparing to administer an IV infusion of magnesium sulfate to a client who is 38 weeks pregnant and has eclampsia.
Which of the following actions should the nurse take?
Explanation
All of the above.
The nurse should take all of the following actions when administering an IV infusion of magnesium sulfate to a client who has eclampsia:
• Use an infusion pump to regulate the flow rate.
This ensures that the client receives the correct dose of magnesium sulfate and prevents overdose or underdose.Magnesium sulfate is given as a loading dose of 4 g in normal saline solution, followed by a maintenance infusion of 1 to 2 g/h by controlled infusion pump.
• Monitor the client’s deep tendon reflexes hourly.
This is a way to assess the client’s neuromuscular status and detect signs of magnesium toxicity, such as hyporeflexia or areflexia.Magnesium sulfate can cause muscle weakness and respiratory depression if the serum level is too high.
• Keep calcium gluconate readily available.
This is the antidote for magnesium toxicity and should be given if the client develops signs of respiratory depression, cardiac arrhythmias, or loss of consciousness.Calcium gluconate is given as 10 mL of 10% solution IV push over 3 to 5 minutes.
Choice A is wrong because using an infusion pump is not enough to ensure safe administration of magnesium sulfate.
The nurse should also monitor the client’s vital signs, urine output, and serum magnesium level regularly.
Choice B is wrong because monitoring the client’s deep tendon reflexes is not enough to prevent or treat eclamptic seizures.
The nurse should also observe the client for signs of headache, visual disturbances, epigastric pain, or altered mental status.
Choice C is wrong because keeping calcium gluconate available is not enough to prevent complications of magnesium sulfate therapy.
The nurse should also be prepared to manage air circulation.
A nurse is teaching a prenatal class about the risk factors for preeclampsia and eclampsia.
Which of the following statements by a class participant indicates a need for further teaching?
Explanation
“I should take low-dose aspirin every day to prevent preeclampsia.” This statement indicates a need for further teaching because low-dose aspirin is not recommended for all pregnant women, but only for those who have a high risk of developing preeclampsia.Low-dose aspirin may have side effects such as bleeding, allergic reactions, or stomach ulcers.
The nurse should explain that low-dose aspirin is prescribed by the health care provider only after weighing the benefits and risks for each individual case.
Choice A is wrong because eating foods that are high in salt may increase blood pressure and fluid retention, which are signs of preeclampsia.The nurse should advise the client to limit salt intake and avoid processed foods that contain a lot of sodium.
Choice B is wrong because having a family history of preeclampsia is one of the risk factors for developing this condition.
The nurse should encourage the client to inform the doctor about any family history of preeclampsia, as well as other risk factors
A nurse is assessing a client who is 34 weeks pregnant and has mild preeclampsia.
Which of the following findings should alert the nurse to possible progression to severe preeclampsia?
Explanation
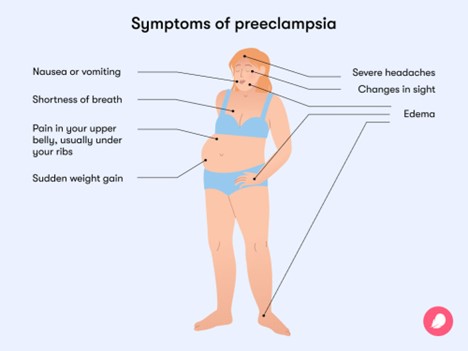
Epigastric pain is a sign of severe preeclampsia, which indicates possible damage to the liver.Severe preeclampsia can also cause high blood pressure, proteinuria, headaches, changes in vision, sensitivity to light, fatigue, nausea/vomiting, infrequent urination, or a tendency to bruise easily.
B. Weight gain of 2 kg in one week.Statement is wrong because weight gain of 2 kg in one week is not a sign of severe preeclampsia, but rather a normal occurrence during pregnancy.
C. Facial edema.Statement is wrong because facial edema is a sign of mild preeclampsia, not severe preeclampsia.Mild preeclampsia is characterized by high blood pressure and protein in the urine.
D. Urine output of 40 mL/hr.
Statement is wrong because urine output of 40 mL/hr is not a sign of severe preeclampsia, but rather a normal range for urine output during pregnancy.
Normal urine output ranges from 30 to 60 mL/hr for adults.
More Questions on this Topic
A nurse is providing discharge instructions to a client who had preeclampsia and delivered her baby 2 days ago.
Which of the following instructions should the nurse include?
Explanation
The nurse should instruct the client to report any headache or visual changes to the doctor immediately, as these are signs of worsening preeclampsia that can lead to serious complications such as stroke, eclampsia, or HELLP syndrome.Preeclampsia can persist or even begin after delivery, most often within 48 hours, so the client should monitor her blood pressure and symptoms until they resolve.
Choice A is wrong because the client should not stop taking her blood pressure medication without consulting her doctor.Blood pressure medication helps lower the blood pressure and protects the organs from damage.The blood pressure usually returns to normal within several days to weeks after delivery, but some clients may need medication for longer.
Choice B is wrong because the client should not avoid breastfeeding her baby unless there is a medical reason to do so.Breastfeeding has many benefits for both the mother and the baby, and does not affect the blood pressure or the preeclampsia.
Choice D is wrong because the client should not limit her fluid intake to prevent fluid overload.Fluid overload is not a common complication of preeclampsia, and limiting fluids can cause dehydration and affect the milk supply for breastfeeding.
The client should drink enough fluids to stay hydrated and follow a balanced diet.
A nurse is assessing a client who is 24 weeks pregnant and has preeclampsia.
Which of the following findings should the nurse report to the provider as a manifestation of severe preeclampsia?
Explanation
This is a manifestation of severe preeclampsia that indicates liver involvement and can precede a seizure.
The nurse should report this finding to the provider immediately and prepare for possible delivery of the baby.
Choice A is wrong because blood pressure of 150/90 mm Hg is a sign of mild preeclampsia, not severe.Severe preeclampsia is diagnosed when the systolic pressure is 160 mm Hg or higher or the diastolic pressure is 110 mm Hg or higher.
Choice B is wrong because urine protein of 2+ is also a sign of mild preeclampsia, not severe.Severe preeclampsia is diagnosed when the urine protein is 3+ or higher.
Choice D is wrong because facial edema is a common finding in normal pregnancy and does not indicate severe preeclampsia.Other signs of severe preeclampsia include headache, blurred vision, oliguria, thrombocytopenia, and pulmonary edema.
A nurse is administering magnesium sulfate IV to a client who has severe preeclampsia.
Which of the following assessments should the nurse perform to monitor for magnesium toxicity? Select all that apply.
Explanation
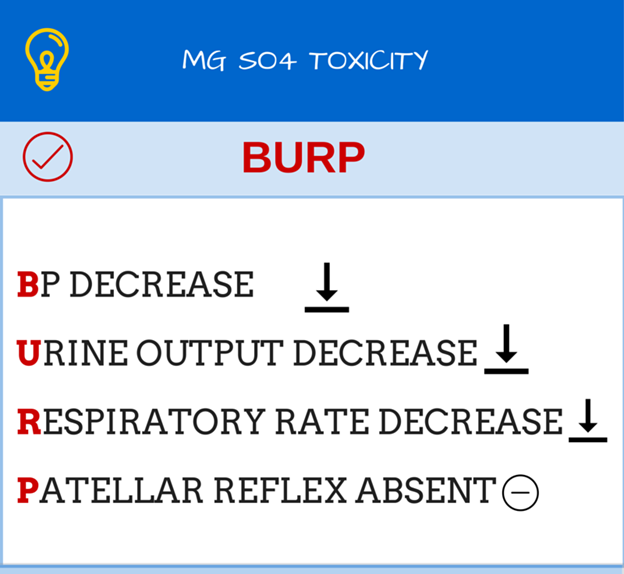
The correct answer is choice A, B, C and E.The nurse should monitor for magnesium toxicity by assessing the deep tendon reflexes, respiratory rate, urine output and serum magnesium level of the client who has severe preeclampsia and is receiving magnesium sulfate IV.Magnesium toxicity can cause life-threatening complications such as hypotension, areflexia (loss of DTRs), respiratory depression, respiratory arrest, oliguria, shortness of breath, chest pains, slurred speech and cardiac arrest.The nurse should also have calcium chloride ready as an antidote for magnesium toxicity.
Choice D is wrong because fetal heart rate is not a direct indicator of magnesium toxicity.However, the nurse should still monitor the fetal heart rate and uterine activity per the Electronic Fetal Monitoring (EFM) Guideline.
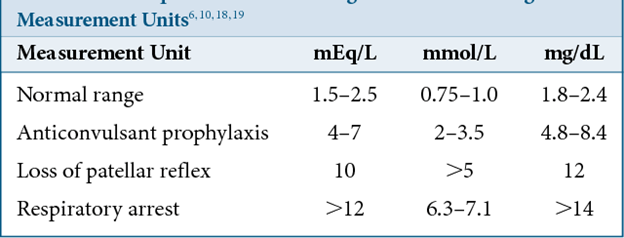
Normal ranges for the assessments are:
• Deep tendon reflexes: 1+ to 4+ (normal to hyperactive)
• Respiratory rate: 12 to 20 breaths per minute
• Urine output: at least 30 mL per hour
• Serum magnesium level: 4 to 7 mg/dL (therapeutic range for preeclampsia)
A nurse is caring for a client with severe pre-eclampsia who is receiving magnesium sulfate.
Which assessment finding would indicate that the client is experiencing magnesium toxicity?
Explanation
Respiratory rate of 10 breaths/minute.This indicates that the client is experiencingmagnesium toxicity, which can causemuscle weakness,difficulty breathing, andcardiac arrest.The normal respiratory rate for adults is 12 to 20 breaths/minute.
Choice B is wrong because deep tendon reflexes of 2+ are normal and do not indicate magnesium toxicity.
Choice C is wrong because urinary output of 40 mL/hour is within the normal range of 30 to 50 mL/hour.Magnesium toxicity can cause urine retention, not increased output.
Choice D is wrong because serum magnesium level of 6 mEq/L is within the normal range of 1.7 to 2.3 mEq/L.Magnesium toxicity occurs when the level is above 2.6 mEq/L.
A nurse is evaluating the effectiveness of magnesium sulfate therapy for a client with pre-eclampsia.
Which outcome would indicate that the therapy is successful?
Explanation
The client has no seizures or eclampsia.This outcome would indicate that the magnesium sulfate therapy is successful because magnesium sulfate is a mineral that reduces seizure risks in women with preeclampsia.
Some additional information for the other choices are:
• Choice B. The client delivers a healthy baby vaginally.
This outcome is desirable but not directly related to the effectiveness of magnesium sulfate therapy.Magnesium sulfate can help prolong a pregnancy for up to two days to allow drugs that speed up the baby’s lung development to be administered, but it does not guarantee a vaginal delivery or a healthy baby.
• Choice C. The client has normal blood pressure and urine output.
This outcome is also desirable but not directly related to the effectiveness of magnesium sulfate therapy.
Magnesium sulfate may help reduce blood pressure in some cases, but it is not the primary treatment for hypertension in preeclampsia.Other medications such as antihypertensives are usually prescribed for that purpose.Urine output should be monitored closely while receiving magnesium sulfate therapy, as a decrease may indicate toxicity or kidney impairment.Urine output should be at least 30 mL/hour while administering magnesium sulfate.
• Choice D. The client has improved liver function and platelet count.
This outcome is also desirable but not directly related to the effectiveness of magnesium sulfate therapy.
Magnesium sulfate does not affect liver function or platelet count in preeclampsia.These parameters may improve after delivery of the placenta, which is the main cause of preeclampsia.
Normal ranges for blood pressure, urine output, liver function and platelet count are:
• Blood pressure: less than 140/90 mm Hg
• Urine output: at least 30 mL/hour
• Liver function: AST and ALT less than 40 U/L, LDH less than 600 U/L, bilirubin less than 1.2 mg/dL
• Platelet count: 150,000 to 450,000 per microliter of blood
A nurse is teaching a pregnant client about the risk factors for pre-eclampsia.
Which of the following should the nurse include? (Select all that apply).
Explanation
The correct answer is choices B, C, D, and E.These are all risk factors for pre-eclampsia according to various sources.
Choice A is wrong because age over 35 years is not a risk factor for pre-eclampsia by itself, although it may be associated with other conditions that increase the risk, such as chronic hypertension or diabetes.
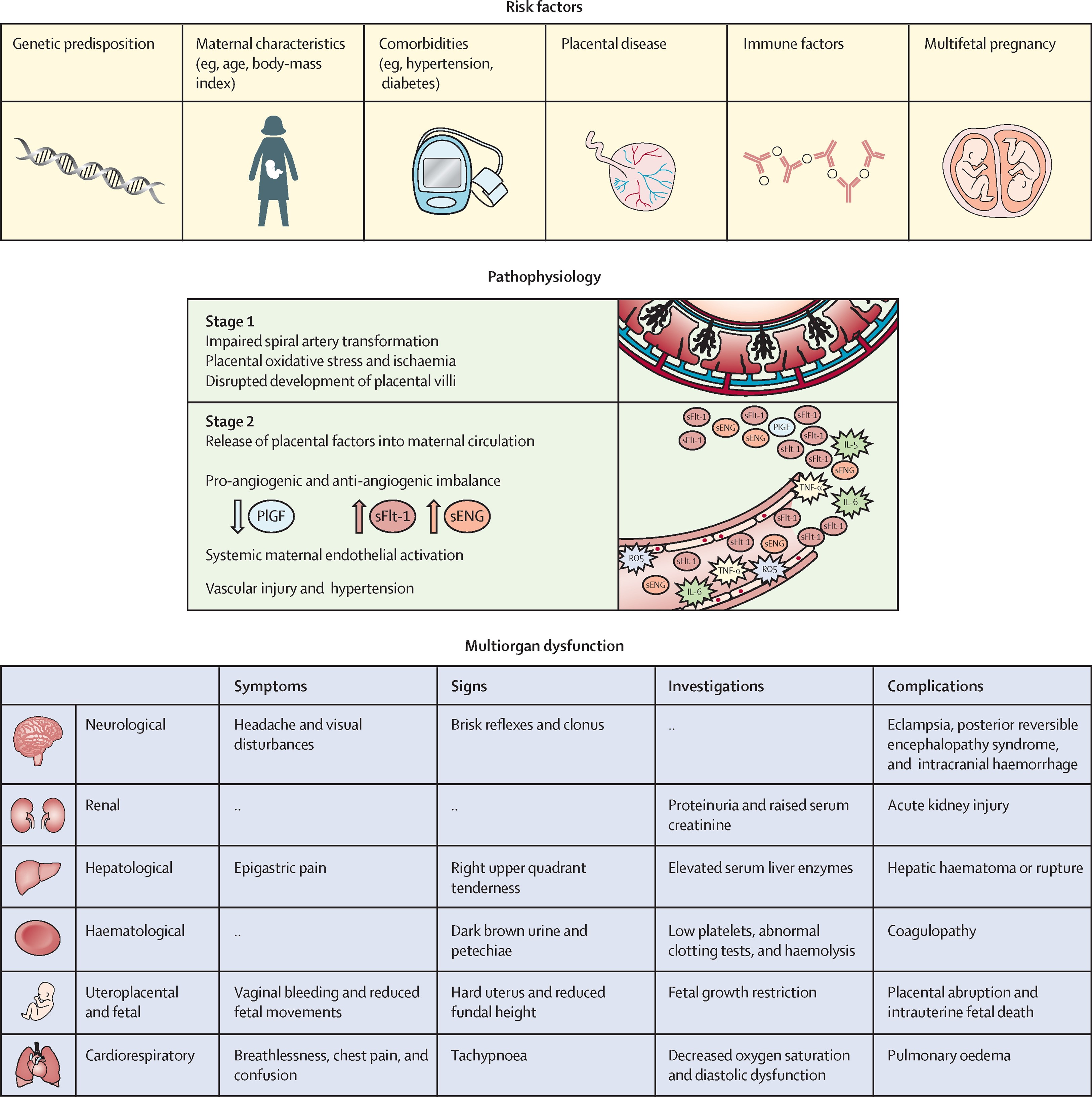
Pre-eclampsia is a complication of pregnancy that involves high blood pressure, protein in the urine, and organ damage.It can affect both the mother and the fetus and can lead to serious complications such as eclampsia (seizures), placental abruption, and stillbirth.It is more common in first pregnancies, especially with a new partner, because of the immune response to the foreign fetal antigens.Obesity, diabetes mellitus, and multiple gestation are also risk factors because they increase the metabolic and vascular demands on the placenta and the mother.
Normal ranges for blood pressure and proteinuria in pregnancy are:
• Blood pressure: less than 140/90 mmHg
• Proteinuria: less than 300 mg/24 hours or less than 30 mg/dL on a random urine sample
A nurse is monitoring a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously.
Which of the following assessments is the most important for the nurse to perform?
Explanation
Level of consciousness.
This is because magnesium sulfate, which is given to prevent seizures in severe preeclampsia, can cause respiratory depression and coma if the dose is too high.Therefore, the nurse should monitor the client’s level of consciousness and respiratory rate closely and report any signs of toxicity to the provider.
Choice A is wrong because hourly intake and output is not the most important assessment for this client.However, the nurse should monitor the urinary output as a sign of renal function and fluid balance and report any output less than 30 ml per hour.
Choice B is wrong because deep tendon reflexes are not the most important assessment for this client.However, the nurse should check the reflexes as a sign of neuromuscular irritability and report any hyperreflexia or clonus.
Choice C is wrong because lung sounds are not the most important assessment for this client.However, the nurse should auscultate the lungs as a sign of pulmonary edema and report any crackles or wheezes.
A nurse is caring for a client with severe pre-eclampsia who is being induced with oxytocin.
The nurse notes that the client’s contractions are occurring every 2 minutes and lasting 90 seconds.
The fetal heart rate is 160 beats/minute with late decelerations.
What is the priority nursing action?
Explanation
The correct answer is d. Notify the health care provider.
Rationale for Choice A:
- Increasing the rate of oxytocin infusion is contraindicated in this situation.
- Oxytocin stimulates uterine contractions,and the client is already experiencing excessively frequent and prolonged contractions.
- Increased oxytocin could further compromise uteroplacental blood flow and exacerbate fetal distress.
- It could also put the client at higher risk for uterine rupture,a serious complication associated with oxytocin use.
Rationale for Choice B:
- While administering oxygen is a common intervention for fetal distress,it's not the priority action in this case.
- Late decelerations in fetal heart rate are typically caused by uteroplacental insufficiency,which means the fetus isn't receiving adequate oxygen and nutrients from the placenta.
- Oxygen administered to the mother may not significantly improve fetal oxygenation if the underlying issue is impaired placental perfusion.
Rationale for Choice C:
- Turning the client to her left side is a recommended position to improve placental blood flow.
- However,in this situation,it's not the priority action given the presence of late decelerations and excessive uterine contractions.
- It may be a helpful adjunct measure,but it won't address the primary cause of fetal distress.
Rationale for Choice D:
- Notifying the health care provider is the most crucial action because:
- The client has severe pre-eclampsia,a serious condition that requires close monitoring and management.
- The frequent and prolonged contractions,along with late decelerations in the fetal heart rate,indicate potential fetal distress.
- The health care provider needs to be aware of these changes to make timely decisions regarding interventions,such as:
- Adjusting the oxytocin infusion
- Expediting delivery if necessary
- Implementing other measures to improve fetal well-being
- Closely monitoring the mother's condition to prevent complications of pre-eclampsia
A nurse is providing discharge instructions to a client who had severe pre-eclampsia and delivered a healthy baby at 34 weeks of gestation.
Which of the following statements by the client indicates a need for further teaching?
Explanation
“I will resume my normal activities as soon as possible.” This statement indicates a need for further teaching because a woman who had severe pre-eclampsia should rest more often and avoid strenuous activities until her blood pressure is normal and stable.She should also follow up with her doctor regularly and monitor her blood pressure at home.
Choice A is wrong because it is important to monitor blood pressure at home for a few weeks after having pre-eclampsia.
This can help detect any signs of worsening hypertension or organ damage.
Choice B is wrong because it is advisable to call the doctor if there are any headaches or vision changes, as these could be signs of brain injury or eclampsia.
Eclampsia is a serious complication of pre-eclampsia that causes seizures.
Choice C is wrong because some over-the-counter pain medications, such as ibuprofen, can increase blood pressure and should be avoided by women with pre-eclampsia.However, acetaminophen (Tylenol) is usually safe to take for mild pain relief.
Normal ranges for blood pressure during pregnancy are less than 140/90 mmHg.Normal ranges for protein in urine during pregnancy are less than 300 mg in 24 hours.
A nurse is caring for a client who is receiving magnesium sulfate for severe preeclampsia.
Which of the following actions should the nurse take?
Explanation
Administer calcium gluconate as an antidote if toxicity occurs.Magnesium sulfate is a mineral that reduces seizure risks in women with severe preeclampsia.However, it can also cause side effects and toxicity, such as respiratory depression, muscle weakness, and cardiac arrest.Calcium gluconate is an antidote that can reverse the effects of magnesium sulfate and restore normal neuromuscular function.
Choice B is wrong because magnesium sulfate does not affect blood glucose levels.
There is no need to monitor the client’s blood glucose level every 4 hours.
Choice C is wrong because the infusion should be discontinued if the client’s respiratory rate is below 12/min, not 16/min.
A low respiratory rate indicates respiratory depression, which is a sign of magnesium toxicity.
Choice D is wrong because the infusion rate should not be increased if the client’s urine output is above 30 mL/hr.Urine output should be at least 30 mL/hr while administering magnesium sulfate to prevent accumulation of the drug in the body.
Increasing the infusion rate can increase the risk of toxicity.
A nurse is teaching a client who is at risk for developing preeclampsia.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
“I should take a baby aspirin every day as prescribed.” Taking a baby aspirin daily has been shown to reduce the risk of developing preeclampsia by about 15%.If you have risk factors for preeclampsia, your healthcare provider may recommend starting aspirin in early pregnancy (by 12 weeks gestation).
Choice A is wrong because avoiding foods that are high in sodium does not prevent preeclampsia.Sodium intake does not affect blood pressure in pregnancy.
Choice B is wrong because lying on your left side for at least 2 hours a day does not prevent preeclampsia.However, lying on your left side may help improve blood flow to your placenta and your baby.
Choice C is wrong because checking your blood pressure at home every day does not prevent preeclampsia.However, monitoring your blood pressure at home may help detect signs of preeclampsia early and alert you to seek medical attention if needed.
A nurse is assessing a client who has severe preeclampsia and is receiving magnesium sulfate via continuous IV infusion.
Which of the following findings should alert the nurse to suspect magnesium toxicity?
Explanation
Respiratory rate 10/min.This indicatesmuscle weaknessanddifficulty breathing, which are symptoms ofmagnesium toxicity.Magnesium sulfate is a medication that can cause magnesium overdose if given in excess or if the patient has impaired kidney function.
Choice B.Urine output 40 mL/hr is wrong because this is within the normal range for urine output, which is 30 to 50 mL/hr.Urine output may decrease in severe cases of magnesium toxicity due to urine retention.
Choice C. Patellar reflex 2+ is wrong because this is a normal finding for the knee-jerk reflex.A low or absent patellar reflex may indicate magnesium toxicity, as it reflectsmuscle weaknessandnerve dysfunction.
Choice D.Serum magnesium level 4.5 mEq/L is wrong because this is within the normal range for serum magnesium, which is 1.7 to 2.3 mEq/L.Serum magnesium levels above 2.6 mEq/L can indicate hypermagnesemia or magnesium overdose.
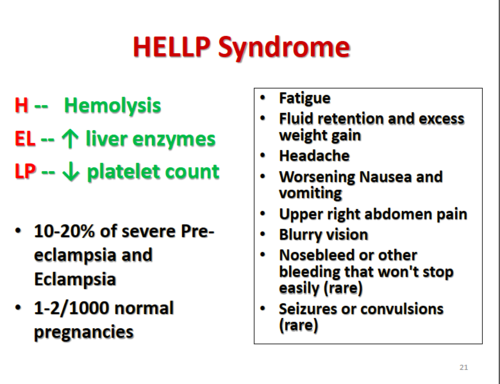
A nurse is caring for a client who has a diagnosis of HELLP syndrome.
The nurse should monitor the client for which of the following complications? (Select all that apply.)
Explanation
The correct answer is choice A, C, D and E. Here is why:
• Choice A is correct becausedisseminated intravascular coagulation (DIC)is a blood clotting disorder that can develop as a complication of HELLP syndrome.DIC can result in excessive bleeding or blood clots in various organs.
• Choice B is wrong becauseacute kidney injuryis not a common complication of HELLP syndrome.However, preeclampsia can cause kidney damage and proteinuria (high levels of protein in the urine).
• Choice C is correct becausepulmonary edemais a condition where fluid accumulates in and around the lungs, impairing oxygen absorption.It can occur as a complication of HELLP syndrome due to high blood pressure and fluid overload.
• Choice D is correct becauseplacental abruptionis a condition where the placenta separates from the uterus before delivery.
It can cause severe bleeding and fetal distress.It can occur as a complication of HELLP syndrome due to high blood pressure and abnormal blood clotting.
• Choice E is correct becausefetal growth restrictionis a condition where the fetus does not grow as expected.It can occur as a complication of HELLP syndrome due to reduced blood flow and oxygen delivery to the placenta.
Normal ranges for liver enzymes are:
• Alanine aminotransferase (ALT): 7 to 55 units per liter (U/L)
• Aspartate aminotransferase (AST): 8 to 48 U/L
• Alkaline phosphatase (ALP): 45 to 115 U/L
Normal range for platelet count is:
• 150,000 to 450,000 platelets per microlitre.
A nurse is providing discharge teaching to a client who had HELLP syndrome and a cesarean birth.
The nurse should instruct the client to report which of the following findings to the provider?
Explanation
Headache unrelieved by analgesics.This is because headache is a common symptom of HELLP syndrome, a rare pregnancy complication that can cause high blood pressure, seizures, stroke or liver rupture.HELLP syndrome is a type of preeclampsia and has similar symptoms.
Choice A is wrong because breast engorgement is a normal postpartum condition that occurs when the breasts are full of milk and become swollen and tender.
It is not related to HELLP syndrome.
Choice B is wrong because lochia rubra for 3 days postpartum is a normal finding that indicates the shedding of the uterine lining after delivery.
It is not related to HELLP syndrome.
Choice D is wrong because perineal discomfort is a common postpartum discomfort that results from the stretching and tearing of the perineal tissues during vaginal delivery.
It is not related to HELLP syndrome.
Normal ranges for blood pressure are less than 120/80 mmHg, for platelet count are 150,000 to 450,000 per microliter, and for liver enzymes are 7 to 56 units per liter for AST and 0 to 35 units per liter for ALT.
A nurse is providing discharge teaching to a client who had pre-eclampsia and delivered a healthy newborn.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
The client should have a follow-up visit with the provider in a week.This is because preeclampsia can persist or develop after delivery and requires close monitoring of blood pressure and signs of organ injury.
Choice A is wrong because vaginal bleeding is normal after delivery and does not indicate a complication of preeclampsia.
Choice B is wrong because the client should not stop taking blood pressure medication without consulting the provider.Preeclampsia can cause hypertension that may need treatment even after delivery.
Choice C is wrong because breastfeeding is not contraindicated for women with preeclampsia.Breastfeeding may even lower blood pressure and help the uterus contract.
A nurse is caring for a client who has severe pre-eclampsia and is receiving hydralazine IV.
Which of the following adverse effects should the nurse monitor for?
Explanation
Hydralazine can causetachycardia(fast heart rate) as a common side effect.
This is because hydralazine lowers blood pressure by relaxing blood vessels, which can make the heart beat faster to compensate.
Choice B is wrong because hydralazine does not causehyperglycemia(high blood sugar).
Hydralazine is not known to affect glucose metabolism or insulin secretion.
Choice C is wrong because hydralazine does not causehypokalemia(low potassium levels).
Hydralazine is not a diuretic and does not increase potassium excretion.
Choice D is wrong because hydralazine does not causeconstipation.Hydralazine can causediarrheaas a common side effect, but not constipation.
A nurse is evaluating the effectiveness of magnesium sulfate therapy for a client who has eclampsia.
Which of the following outcomes indicates that the therapy is successful?
Explanation
The client has no seizures.Magnesium sulfate therapy is used to prevent seizures in women with preeclampsia and eclampsia.Seizures are a life-threatening complication of eclampsia and indicate a failure of therapy.
Choice B is wrong because diuresis is not a goal of magnesium sulfate therapy.Diuresis may indicate fluid overload or renal impairment, which are complications of preeclampsia and eclampsia.
Choice C is wrong because improved fetal movement is not a direct outcome of magnesium sulfate therapy.Fetal movement may be affected by many factors, such as gestational age, maternal position, and fetal well-being.
Choice D is wrong because increased platelet count is not a result of magnesium sulfate therapy.Platelet count may be decreased in preeclampsia and eclampsia due to disseminated intravascular coagulation, which is a serious complication that requires prompt treatment.
Normal ranges for blood pressure are less than 140/90 mm Hg, for proteinuria are less than 300 mg/24 hours, for platelet count are 150,000 to 400,000/mm3, and for serum magnesium are 1.5 to 2.5 mEq/L.
A nurse is assessing a client with severe pre-eclampsia who is receiving magnesium sulfate infusion.
Which finding should alert the nurse to suspect magnesium toxicity?
Explanation
Respiratory rate of 10 breaths/min.
This is a sign ofmagnesium toxicity, which can occur when a client receives magnesium sulfate infusion for severe pre-eclampsia.Magnesium toxicity can causemuscle weakness,difficulty breathing,irregular heartbeats, andcardiac arrest.
Choice B is wrong because deep tendon reflexes of 2+ are normal and do not indicate magnesium toxicity.
Choice C is wrong because urine output of 40 mL/hour is adequate and does not indicate magnesium toxicity.
The minimum urine output for an adult is 30 mL/hour.
Choice D is wrong because serum magnesium level of 6 mEq/L is within the normal range of 1.7 to 2.3 mEq/L and does not indicate magnesium toxicity.Magnesium levels above 2.6 mEq/L can indicate hypermagnesemia.
A nurse is caring for a client with eclampsia who is having a tonic-clonic seizure.
Which action should the nurse take first?
Explanation
Turn the client to the side.This is because turning the client to the side will prevent aspiration of secretions or vomitus and maintain a patent airway during a seizure.
This is the most important and immediate action to take for a client with eclampsia who is having a tonic-clonic seizure.
Choice A is wrong because administering oxygen via face mask is not the first priority and may not be feasible during a seizure.Oxygen therapy may be indicated after the seizure to improve oxygenation and fetal well-being.
Choice C is wrong because inserting an oral airway is contraindicated during a seizure as it may cause injury to the oral mucosa or trigger a gag reflex.An oral airway may be used after the seizure if the client is unconscious and has a compromised airway.
Choice D is wrong because giving a loading dose of magnesium sulfate is not the first action to take, although it is an important intervention to prevent further seizures and lower blood pressure in eclampsia.Magnesium sulfate should be administered intravenously after securing the airway and ensuring adequate ventilation.
A nurse is providing discharge instructions to a client who had severe pre-eclampsia and delivered a healthy baby at 36 weeks of gestation.
The nurse should instruct the client to report which symptom to the provider as a possible sign of postpartum pre-eclampsia?
Explanation
Headache that does not respond to analgesics.This is a possible sign of postpartum pre-eclampsia, a rare condition that occurs when a woman has high blood pressure and excess protein in her urine soon after childbirth.Postpartum pre-eclampsia can cause seizures and other serious complications if not treated.
Choice B is wrong because breast engorgement and tenderness are normal symptoms of breastfeeding and do not indicate postpartum pre-eclampsia.
Choice C is wrong because lochia rubra with small clots is a normal discharge of blood and tissue from the uterus after delivery and does not indicate postpartum pre-eclampsia.
Choice D is wrong because perineal pain and swelling are common after vaginal delivery and do not indicate postpartum pre-eclampsia.
Normal ranges for blood pressure are below 120/80 mm Hg and for protein in urine are below 150 mg/day.
A nurse is reviewing the laboratory results of a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously.
Which of the following results should the nurse notify the provider about? (Select all that apply.)
Explanation
The correct answer is choice C and E.A platelet count of 100,000/mm3 is low and indicates a risk of bleeding due to preeclampsia.A urine output of 20 mL/hour is also low and suggests kidney impairment due to magnesium sulfate therapy.
Both of these results should be reported to the provider as they may require intervention.
Choice A is wrong because a serum creatinine of 1.2 mg/dL is within the normal range of 0.6 to 1.3 mg/dL for womenand does not indicate kidney dysfunction.
Choice B is wrong because liver enzymes of 40 U/L are within the normal range of 7 to 55 U/L for women and do not indicate liver damage.
Choice D is wrong because a coagulation profile of 12 seconds is within the normal range of 11 to 13.5 seconds for women and does not indicate a clotting disorder.
A nurse is planning to administer hydralazine to a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously.
Which of the following actions should the nurse take before giving the medication? (Select all that apply.)
Explanation
The correct answer is choice A and E. The nurse should check the client’s blood pressure and magnesium level before giving hydralazine to a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously.
• Choice A is correct because hydralazine is an antihypertensive drug that lowers blood pressure by relaxing blood vessels.The nurse should monitor the client’s blood pressure before and after giving hydralazine to ensure that it is within the target range and to avoid hypotension or rebound hypertension.
• Choice B is wrong because pulse oximetry is not directly related to hydralazine administration or pre-eclampsia.Pulse oximetry measures the oxygen saturation of hemoglobin in the blood and can be affected by factors such as anemia, hypothermia, nail polish, or movement.
The nurse should monitor the client’s pulse oximetry as part of routine care, but it is not a priority before giving hydralazine.
• Choice C is wrong because checking the client’s reflexes is not directly related to hydralazine administration or pre-eclampsia.Reflexes are assessed to monitor for signs of magnesium toxicity, which can cause muscle weakness, respiratory depression, and cardiac arrest.
The nurse should check the client’s reflexes as part of routine care, but it is not a priority before giving hydralazine.
• Choice D is wrong because checking the client’s urine specific gravity is not directly related to hydralazine administration or pre-eclampsia.Urine specific gravity measures the concentration of solutes in the urine and can be affected by factors such as hydration status, renal function, or diuretic use.
The nurse should monitor the client’s urine specific gravity as part of routine care, but it is not a priority before giving hydralazine.
• Choice E is correct because magnesium sulfate is a drug that prevents and treats seizures in women with severe pre-eclampsia or eclampsia.The nurse should monitor the client’s magnesium level before and after giving magnesium sulfate to ensure that it is within the therapeutic range and to avoid magnesium toxicity.
A nurse is educating a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously about the possible side effects of the medication.
Which of the following statements should the nurse include in the teaching?
Explanation
“You may feel warm and flushed while receiving this medication.” This is a common side effect of magnesium sulfate therapy, which is used to prevent seizures in women with severe pre-eclampsia.Magnesium sulfate can also help prolong a pregnancy for up to two days by relaxing the uterus.
Choice B is wrong because magnesium sulfate can cause fluid retention and swelling, not dehydration.Choice C is wrong because magnesium sulfate can cause drowsiness and lethargy, not insomnia and restlessness.Choice D is wrong because magnesium sulfate can cause decreased blood pressure and heart rate, not inflammation and infection at the infusion site.
Normal ranges for blood pressure are below 140/90 mm Hg, for platelet count are 150,000 to 450,000 per microliter of blood, and for protein in urine are less than 300 milligrams per day.
(select all that apply) A nurse is reviewing the laboratory results of a client with eclampsia who is receiving magnesium sulfate.
Which of the following values should the nurse report to the provider? (Select all that apply.)
Explanation
The correct answer is A and B. A. Serum magnesium level of 8 mg/dL
This statement is correct because a serum magnesium level of 8 mg/dL (6.6 mmol/L) is within the therapeutic range for eclampsia treatment, which is 3.5 to 7 mEq/L (4.2 to 8.4 mg/dL) according to some sources, or 1.5 to 3.5 mmol/L according to others.A serum magnesium level above 8 mEq/L (10 mmol/L) can cause areflexia, respiratory paralysis, and cardiac arrest.
B. Serum calcium level of 7 mg/dL
This statement is correct because a serum calcium level of 7 mg/dL (1.75 mmol/L) is below the normal range of 8.5 to 10.2 mg/dL (2.12 to 2.55 mmol/L), which indicates hypocalcemia.Hypocalcemia is a common side effect of magnesium sulfate therapy, as magnesium competes with calcium for binding sites on plasma proteins and cell membranes, and also inhibits the release of parathyroid hormone.
C. Serum creatinine level of 1.2 mg/dL
This statement is wrong because a serum creatinine level of 1.2 mg/dL (106 umol/L) is within the normal range of 0.6 to 1.3 mg/dL (53 to 115 umol/L) for women.Serum creatinine level reflects kidney function, and renal impairment can affect the clearance of magnesium sulfate and increase the risk of toxicity.
D. Serum potassium level of 3.8 mEq/L
This statement is wrong because a serum potassium level of 3.8 mEq/L (3.8 mmol/L) is within the normal range of 3.5 to 5 mEq/L (3.5 to 5 mmol/L) for adults.Serum potassium level reflects electrolyte balance, and hypokalemia or hyperkalemia can affect cardiac function and muscle contraction.
E. Serum sodium level of 140 mEq/L
This statement is wrong because a serum sodium level of 140 mEq/L (140 mmol/L) is within the normal range of 135 to 145 mEq/L (135 to 145 mmol/L) for adults.Serum sodium level reflects fluid balance, and hyponatremia or hypernatremia can affect brain function and blood pressure.
A nurse is caring for a client with eclampsia who is receiving magnesium sulfate and has a magnesium level of 10 mg/dL.
Which of the following medications should the nurse have available as an antidote?
Explanation
Calcium gluconate is the antidote for magnesium sulfate overdose.Magnesium sulfate blocks calcium, so calcium gluconate can reverse the effect of an overdose.
The other choices are not antidotes for magnesium sulfate.Choice A, naloxone, is the antidote for narcotics or opioid overdose.Choice B, flumazenil, is the antidote for benzodiazepine overdose.Choice D, protamine sulfate, is the antidote for heparin overdose.The normal range of magnesium level is 1.5 to 2.5 mEq/L, so a level of 10 mg/dL indicates toxicity.
A nurse is evaluating the effectiveness of magnesium sulfate therapy for a client with eclampsia.
Which of the following findings indicates a therapeutic response?
Explanation
Absence of seizures indicates a therapeutic response to magnesium sulfate therapy for a client with eclampsia.Magnesium sulfate is used to prevent seizures in women with preeclampsia, a complication of pregnancy characterized by high blood pressure and organ dysfunction.Magnesium sulfate may act as a vasodilator, an anticonvulsant, and a protector of the blood-brain barrier.
Choice B is wrong because a decrease in urine output may indicate renal impairment, which is a complication of preeclampsia and eclampsia.
Choice C is wrong because an increase in deep tendon reflexes may indicate hyperreflexia, which is a sign of increased neuromuscular irritability and a risk factor for seizures.
Choice D is wrong because an increase in respiratory rate may indicate respiratory distress, which can be caused by pulmonary edema, another complication of preeclampsia and eclampsia.
Normal ranges for urine output are 0.5 to 1 mL/kg/hour, for deep tendon reflexes are 1+ to 2+, and for respiratory rate are 12 to 20 breaths per minute.
A nurse is caring for a client who has severe preeclampsia and is receiving magnesium sulfate via continuous IV infusion.
Which of the following findings should the nurse identify as an indication of magnesium sulfate toxicity?
Explanation
Urinary output of 100 mL in 4 hr is an indication of magnesium sulfate toxicity.Magnesium sulfate is used to prevent seizures in women with severe preeclampsia or eclampsia.Taking too much magnesium can be life-threatening to both mother and child.
Choice B is wrong because
Choice C is wrong because patellar reflex of +2 is normal and not a sign of toxicity.Loss of deep tendon reflexes can occur with magnesium overdose.
Choice D is wrong because serum magnesium level of 4 mEq/L is normal and not a sign of toxicity.Toxic levels are usually above 8 mEq/L.
A nurse is caring for a client who has eclampsia and is receiving magnesium sulfate and hydralazine.
The client’s blood pressure is 150/90 mmHg, pulse is 88/min, respirations are 18/min, and oxygen saturation is 97%.
The nurse notes that the client’s deep tendon reflexes are absent.
Which of the following actions should the nurse take?
Explanation
Stop the magnesium sulfate infusion.
The client is showing signs of magnesium toxicity, such as absent deep tendon reflexes, which can lead to respiratory depression and cardiac arrest.
Magnesium sulfate is an anticonvulsant that is used to prevent seizures in eclampsia, but it can also cause vasodilation and hypotension.
The nurse should stop the infusion and monitor the client’s vital signs and neurological status.
Choice B. Increase the rate of the hydralazine infusion is wrong because hydralazine is an antihypertensive that lowers blood pressure.
The client’s blood pressure is already within the normal range for eclampsia (140/90 to 160/110 mmHg), so increasing the rate of hydralazine could cause hypotension and compromise placental perfusion.
Choice C. Administer calcium gluconate IV push is wrong because calcium gluconate is an antidote for magnesium toxicity, but it should not be given IV push.
It should be given slowly over 10 to 20 minutes to avoid cardiac arrhythmias and bradycardia.
Choice D. Prepare for immediate delivery of the fetus is wrong because delivery of the fetus is not indicated at this time.
The client’s vital signs are stable and there is no evidence of fetal distress or placental abruption.
Delivery of the fetus is the definitive treatment for eclampsia, but it should be done when the maternal and fetal conditions are optimal.
A nurse is reviewing the electronic health record of a client who has severe preeclampsia and is being induced with oxytocin.
Which of the following findings should the nurse report to the provider immediately?
Explanation
Epigastric pain and nausea.This is because epigastric pain and nausea are signs of severe preeclampsia that indicate liver involvement and possible hepatic rupture.
This is a medical emergency that requires immediate intervention to prevent maternal and fetal complications.
Choice A is wrong because contractions lasting 90 seconds and occurring every 2 minutes are normal during labor induction with oxytocin and do not indicate severe preeclampsia.
Choice B is wrong because fetal heart rate baseline of 140/min with moderate variability is a reassuring sign of fetal well-being and does not indicate severe preeclampsia.
Choice C is wrong because cervical dilation of 4 cm and effacement of 50% are normal findings during labor induction and do not indicate severe preeclampsia.
A nurse is monitoring a client with severe pre-eclampsia who is receiving magnesium sulfate infusion.
What is the antidote for magnesium sulfate toxicity?
Explanation
Calcium gluconate is the antidote for magnesium sulfate toxicity because it reverses the effects of magnesium on the neuromuscular and cardiovascular systems.
Magnesium sulfate can cause respiratory depression, hypotension, bradycardia, and cardiac arrest in high doses.
Choice B. Naloxone is wrong because it is the antidote for opioid overdose, not magnesium sulfate toxicity.
Naloxone blocks the opioid receptors and restores breathing and consciousness.
Choice C. Flumazenil is wrong because it is the antidote for benzodiazepine overdose, not magnesium sulfate toxicity.
Flumazenil binds to the benzodiazepine receptors and reverses the sedative and hypnotic effects.
Choice D. Protamine sulfate is wrong because it is the antidote for heparin overdose, not magnesium sulfate toxicity.
Protamine sulfate neutralizes the anticoagulant effect of heparin and prevents bleeding.
Normal ranges for magnesium are 1.5 to 2.5 mEq/L or 0.75 to 1.25 mmol/L.
A nurse is evaluating the effectiveness of magnesium sulfate therapy for a client with eclampsia.
What clinical indicator would suggest that the therapy is successful?
Explanation
Magnesium sulfate therapy is used to prevent seizures in women with preeclampsia, a complication of pregnancy characterized by high blood pressure and organ dysfunction.Seizures are a sign of eclampsia, a severe form of preeclampsia that can be life-threatening.
Therefore, if the therapy is successful, the woman should not have any seizures.
Choice B.Absence of proteinuria is wrong because proteinuria, or excess protein in urine, is a possible sign of preeclampsia, not eclampsia.
Proteinuria may not disappear even after magnesium sulfate therapy.
Choice C.Absence of edema is wrong because edema, or swelling, is a common symptom of pregnancy and may not be related to preeclampsia or eclampsia.
Edema may not disappear even after magnesium sulfate therapy.
Choice D.Absence of headache is wrong because headache is a symptom of preeclampsia, not eclampsia.
Headache may not disappear even after magnesium sulfate therapy.
Normal ranges for blood pressure are below 140/90 mm Hg and for protein in urine are below 300 mg per 24 hours.
A nurse is caring for a client with HELLP syndrome who is receiving a blood transfusion.
What nursing interventions are appropriate for this client? Select all that apply.
Explanation
The correct answer is choice A and C. A client with HELLP syndrome is at risk for bleeding, liver damage, and fluid overload or transfusion reaction.Therefore, the nurse should monitor vital signs and urine output to assess for signs of shock, hemorrhage, or renal failure.The nurse should also check for signs of fluid overload or transfusion reaction such as dyspnea, crackles, edema, fever, chills, or rash.
Choice B is wrong because corticosteroids are not indicated for clients with HELLP syndrome unless they have severe thrombocytopenia or need to delay delivery for fetal lung maturity.Corticosteroids may worsen the liver function and increase the risk of infection.
Choice D is wrong because encouraging oral intake of fluids and electrolytes may exacerbate fluid overload and hypertension in clients with HELLP syndrome.Fluid restriction and diuretics may be prescribed to reduce the risk of pulmonary edema and cerebral edema.
Choice E is wrong because maintaining bed rest and a quiet environment may not be sufficient to prevent the progression of HELLP syndrome.The definitive treatment for HELLP syndrome is delivery of the fetus and placenta as soon as possible.Bed rest and a quiet environment may help reduce blood pressure and stress, but they are not the main interventions for this condition.
A nurse is caring for a client who is at 28 weeks of gestation and has a blood pressure of 160/100 mm Hg.
The nurse should anticipate a prescription for which of the following medications?
Explanation
Labetalol is an antihypertensive drug that can lower blood pressure in pregnant women with preeclampsia.Preeclampsia is a condition that causes high blood pressure and proteinuria after 20 weeks of gestation.
Choice A is wrong because hydralazine is not recommended as a first-line treatment for preeclampsia due to its potential adverse effects on maternal and fetal outcomes.
Choice B is wrong because nifedipine is not licensed for use in pregnancy and may interact with magnesium sulfate, which is an anticonvulsant medication used to prevent or treat seizures in severe preeclampsia.
Choice D is wrong because methyldopa is not effective for acute blood pressure control and may cause adverse effects such as depression, sedation, and hemolytic anemia.
A nurse is reviewing the discharge instructions for a client who had severe preeclampsia and delivered her baby at 34 weeks of gestation by cesarean birth.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
The client will have to monitor her blood pressure at home for a month after delivery because preeclampsia can persist or develop for the first time after delivery.The client should seek medical care if she has signs of postpartum preeclampsia, such as severe headaches, vision changes, severe belly pain, nausea and vomiting.
Choice A is wrong because magnesium sulfate is an anticonvulsant medication that is given to prevent seizures in women with severe preeclampsia during labor and usually for 24 hours after delivery.
It is not needed for another week.
Choice C is wrong because breastfeeding is not contraindicated in women with preeclampsia.Breastfeeding may even lower the blood pressure and help with bonding.
Choice D is wrong because contraception is not related to preeclampsia.The client should discuss with her healthcare provider about the best contraceptive method for her based on her medical history and preferences.
A nurse is evaluating the fetal status of a client who has preeclampsia and is receiving magnesium sulfate.
Which of the following findings should the nurse report to the provider as a sign of fetal compromise?
Explanation
Oligohydramnios on ultrasound.Oligohydramnios is a condition where the amniotic fluid volume is less than expected for gestational age.It can be a sign of fetal compromise due to various causes, such as renal abnormalities, placental insufficiency, premature rupture of membranes, or chromosomal anomalies.Oligohydramnios can lead to complications such as fetal deformities, preterm birth, infection, or stillbirth.
Choice A is wrong because a fetal heart rate of 140 beats/min is within the normal range for most of pregnancy.
Choice B is wrong because fetal movement of 10 times in an hour is also within the normal range and indicates fetal well-being.
Choice D is wrong because a reactive nonstress test is a reassuring sign that the fetus is not hypoxic or stressed.
Normal ranges:
• Amniotic fluid index (AFI): 5-25 cm
• Fetal heart rate: 110-160 beats/min
• Fetal movement: at least 10 movements in 2 hours
• Nonstress test: at least two accelerations of fetal heart rate of 15 beats/min for 15 seconds or more in 20 minutes
Introduction
A nurse is caring for a client with pre-eclampsia who is receiving magnesium sulfate.
What is the rationale for administering this medication?
Explanation
To prevent seizures.Magnesium sulfate is given to reduce central nervous system irritability and prevent seizures in clients with preeclampsia.Preeclampsia is a hypertensive disorder that occurs after 20 weeks of gestation and is characterized by elevated blood pressure, proteinuria, edema, headache, epigastric pain, and vision changes.
Choice B is wrong because magnesium sulfate does not lower blood pressure.Some antihypertensive drugs might be given to manage blood pressure in clients with preeclampsia.
Choice C is wrong because magnesium sulfate does not increase urine output.In fact, it can cause urinary retention and oliguria as adverse effects.
Choice D is wrong because magnesium sulfate does not promote fetal lung maturity.
It is given to prevent maternal complications, not fetal ones.Corticosteroids might be given to promote fetal lung maturity if delivery is anticipated before 34 weeks of gestation.
A nurse is assessing a client with severe pre-eclampsia who reports a headache and blurred vision.
What other sign or symptom would indicate a worsening of the condition?
Explanation
Epigastric pain is a sign of worsening pre-eclampsia that indicates liver damage.It can also be associated with HELLP syndrome, a severe complication of pre-eclampsia that involves hemolysis, elevated liver enzymes and low platelet count.
Choice B is wrong because facial edema is a common symptom of pregnancy and not specific to pre-eclampsia.
Choice C is wrong because proteinuria is a diagnostic criterion for pre-eclampsia, but not a sign of worsening condition.
Choice D is wrong because brisk reflexes are a normal finding in pregnancy and do not indicate pre-eclampsia severity.
Normal ranges for blood pressure are below 140/90 mmHg, and for proteinuria are less than 300 mg in 24-hour urine collection.
A nurse is teaching a client with mild pre-eclampsia about the signs and symptoms that she should report to the health care provider.
Which of the following should the nurse include? (Select all that apply)
Explanation
The correct answer is choice A and B.Sudden weight gain and decreased fetal movement are signs of pre-eclampsia, a condition that develops in pregnant women and is marked by high blood pressure and presence of proteins in urine.Pre-eclampsia can affect the blood supply to the placenta and the growth of the baby.
Choice C is wrong because vaginal bleeding is not a symptom of pre-eclampsia, but it may indicate other problems such as placental abruption or miscarriage.
Choice D is wrong because nausea and vomiting are not specific symptoms of pre-eclampsia, but they may occur in some cases.However, excessive vomiting and nausea may be a sign of severe pre-eclampsia.
A nurse is preparing to administer an antihypertensive medication to a client with pre-eclampsia.
What is the goal of pharmacological therapy for this condition?
Explanation
To prevent blood pressure from exceeding 160/110 mmHg.The goal of pharmacological therapy for pre-eclampsia is to prevent severe hypertension that can lead to complications such as stroke, kidney failure, or placental abruption.
Choice A is wrong because maintaining blood pressure below 140/90 mmHg is the target for normal hypertension, not pre-eclampsia.
Choice B is wrong because reducing blood pressure by 25% within one hour is too rapid and can compromise blood flow to the placenta and the fetus.
Choice C is wrong because keeping diastolic blood pressure between 80 and 100 mmHg is not specific enough and does not account for the systolic blood pressure, which is also important.
A nurse is reviewing the laboratory results of a client with pre-eclampsia.
Which of the following findings would indicate a risk of disseminated intravascular coagulation (DIC)?
Explanation
Decreased fibrinogen level.This indicates that the client has a risk of disseminated intravascular coagulation (DIC), which is a condition where the blood clots abnormally and causes bleeding in various organs.Fibrinogen is a protein that is essential for blood clotting, and a low level means that the clotting factors are being consumed faster than they can be produced.
Choice A is wrong because elevated platelet count is not a sign of DIC, but rather of normal pregnancy or other conditions that cause thrombocytosis.Platelets are blood cells that help form clots, and a high count means that there is an increased production or decreased destruction of platelets.
Choice C is wrong because increased prothrombin time (PT) is not a specific sign of DIC, but rather of any condition that affects the extrinsic pathway of coagulation.PT measures how long it takes for the blood to clot by adding tissue factor, which activates factor VII.A prolonged PT means that there is a deficiency or dysfunction of factor VII or other factors in the common pathway (X, V, II, I).
Choice D is wrong because reduced partial thromboplastin time (PTT) is not a sign of DIC, but rather of hypercoagulable states or antiphospholipid syndrome.PTT measures how long it takes for the blood to clot by adding phospholipids and an activator, which activate factor XII.A shortened PTT means that there is an increased activity or presence of factor XII or other factors in the intrinsic or common pathway.
Risk Factors
A nurse is reviewing the medical history of a client who is 32 weeks pregnant and has mild preeclampsia.
Which of the following factors in the client’s history increases her risk for developing this condition? Select all that apply.
Explanation
The correct answer is choices B, C, D and E.These are all factors that increase the risk of developing preeclampsia according to various sources.
Choice A is wrong because maternal age of 37 years old is not a risk factor for preeclampsia by itself.However, advanced maternal age (over 40) is associated with a higher risk.
Some of the other risk factors for preeclampsia that are not mentioned in the question are:
• First pregnancy with current partner
• Family history of preeclampsia
• African American ethnicity
• History of certain health conditions, such as migraines, diabetes, rheumatoid arthritis, lupus, scleroderma, urinary tract infections, gum disease, polycystic ovary syndrome, multiple sclerosis, gestational diabetes, and sickle cell disease
• Pregnancy resulting from egg donation, donor insemination, or in vitro fertilization
Normal ranges for blood pressure and proteinuria in pregnancy are:
• Blood pressure: less than 140/90 mm Hg
• Proteinuria: less than 300 mg/24 hours or less than 30 mg/dL in a random urine sample
A nurse is caring for a client who is 36 weeks pregnant and has severe preeclampsia.
The client reports having a severe headache and blurred vision.
The nurse should recognize that these symptoms indicate which of the following complications?
Explanation
Cerebral edema.This is because severe headache and blurred vision are signs of increased intracranial pressure due to swelling of the brain, which can occur in severe preeclampsia.Cerebral edema is a serious complication that can lead to seizures, stroke or death.
Choice A.Pulmonary edema is wrong because it would cause shortness of breath, coughing and chest pain, not headache and blurred vision.
Choice C.Placental abruption is wrong because it would cause abdominal pain, vaginal bleeding and uterine tenderness, not headache and blurred vision.
Choice D.Hepatic rupture is wrong because it would cause epigastric or right upper quadrant pain, nausea and vomiting, not headache and blurred vision.Hepatic rupture is also a rare complication of preeclampsia.
A nurse is preparing to administer magnesium sulfate IV to a client who is 38 weeks pregnant and has eclampsia.
What is the main purpose of this medication for this client?
Explanation
To prevent seizures.Magnesium sulfate is a medication that is used to relax the uterus and prevent seizures in clients with preeclampsia or eclampsia.
It does not lower the blood pressure, induce labor, or increase urine output.
Choice A is wrong because magnesium sulfate does not lower the blood pressure.Other medications, such as labetalol or hydralazine, are used to treat hypertension in preeclampsia.
Choice C is wrong because magnesium sulfate does not induce labor.In fact, it may delay labor by inhibiting uterine contractions.
Choice D is wrong because magnesium sulfate does not increase urine output.It may cause fluid retention and edema, which are signs of magnesium toxicity.The nurse should monitor the client’s urine output, respiratory rate, deep tendon reflexes, and serum magnesium levels while on magnesium sulfate therapy.
A nurse is monitoring a client who is 34 weeks pregnant and has mild preeclampsia.
Which of the following laboratory tests should the nurse review to assess for end-organ damage in this client?
Explanation
Liver enzymes and platelets. The nurse should review these laboratory tests to assess for end-organ damage in a client with mild preeclampsia because they indicate the status of the liver and the coagulation system, which are often affected by this condition.
Choice A is wrong because hemoglobin and hematocrit are not specific indicators of end-organ damage in preeclampsia. They may be elevated due to hemoconcentration from fluid retention or decreased due to hemolysis.
Choice C is wrong because blood glucose and ketones are not related to preeclampsia. They are more relevant for gestational diabetes mellitus, which is a different complication of pregnancy.
Choice D is wrong because creatinine and blood urea nitrogen are not the most sensitive markers of end-organ damage in preeclampsia. They may be elevated due to renal impairment, but proteinuria is a more classic sign of preeclampsia.
Normal ranges for liver enzymes and platelets are:
• AST: 10-40 U/L
• ALT: 7-56 U/L
• ALP: 44-147 U/L
• LDH: 140-280 U/L
• Platelets: 150,000-400,000/mm3
Liver enzymes and platelets.The nurse should review these laboratory tests to assess for end-organ damage in a client with mild preeclampsia because they indicate the status of the liver and the coagulation system, which are often affected by this condition.
Choice A is wrong because hemoglobin and hematocrit are not specific indicators of end-organ damage in preeclampsia.They may be elevated due to hemoconcentration from fluid retention or decreased due to hemolysis.
Choice C is wrong because blood glucose and ketones are not related to preeclampsia.They are more relevant for gestational diabetes mellitus, which is a different complication of pregnancy.
Choice D is wrong because creatinine and blood urea nitrogen are not the most sensitive markers of end-organ damage in preeclampsia.They may be elevated due to renal impairment, but proteinuria is a more classic sign of preeclampsia.
Normal ranges for liver enzymes and platelets are:
• AST: 10-40 U/L
• ALT: 7-56 U/L
• ALP: 44-147 U/L
• LDH: 140-280 U/L
• Platelets: 150,000-400,000/mm3
A nurse is teaching a client who is 28 weeks pregnant and has gestational hypertension about the signs and symptoms of preeclampsia.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
The client should report any changes in the baby’s movements to the doctor, as this could indicate fetal distress due to reduced blood flow to the placenta.
Choice A is wrong because swelling in the hands and feet is a common symptom of pregnancy and not necessarily a sign of preeclampsia.
However, if the swelling is sudden or severe, the client should seek medical attention.
Choice B is wrong because checking blood pressure at home every day is not a reliable way to monitor for preeclampsia.
Blood pressure can vary throughout the day and may be affected by other factors such as stress, activity, or medication.The client should have regular prenatal visits with a health care provider who can measure blood pressure and perform other tests to detect preeclampsia.
Choice D is wrong because weighing oneself every week and reporting any sudden weight gain is not enough to prevent or diagnose preeclampsia.
Weight gain during pregnancy can also be influenced by fluid retention, diet, or other factors.The client should also look out for other signs and symptoms of preeclampsia, such as severe headaches, vision changes, abdominal pain, or reduced urine output.
Clinical Features
A nurse is caring for a client with mild pre-eclampsia who has a blood pressure of 150/95 mmHg, proteinuria of 400 mg/24 hours, and edema of the face and hands.
Which intervention is the priority for this client?
Explanation
Encourage bed rest in a left lateral position.
This is because bed rest can lower blood pressure and improve blood flow to the placenta and the fetus.The left lateral position reduces pressure on the inferior vena cava, a large vein that carries blood from the lower body to the heart.
Choice A is wrong because magnesium sulfate is used to prevent seizures in severe preeclampsia or eclampsia, not mild preeclampsia.
Choice B is wrong because monitoring the fetal heart rate and movement is important, but not the priority for this client.
Choice D is wrong because educating the client about the signs of eclampsia is not urgent and may not prevent the progression of preeclampsia.Some signs of eclampsia are severe headaches, blurred vision, nausea, vomiting, abdominal pain and seizures.
A nurse is caring for a client with mild pre-eclampsia who has a blood pressure of 150/95 mmHg, proteinuria of 400 mg/24 hours, and edema of the face and hands.
Which intervention is the priority for this client?
Explanation
This is because bed rest can lower blood pressure and improve blood flow to the placenta and the fetus.The left lateral position reduces pressure on the inferior vena cava, a large vein that carries blood from the lower body to the heart.
Choice A is wrong because magnesium sulfate is used to prevent seizures in severe preeclampsia or eclampsia, not mild preeclampsia.
Choice B is wrong because monitoring the fetal heart rate and movement is important, but not the priority for this client.
Choice D is wrong because educating the client about the signs of eclampsia is not urgent and may not prevent the progression of preeclampsia.Some signs of eclampsia are severe headaches, blurred vision, nausea, vomiting, abdominal pain and seizures.
A nurse is reviewing the laboratory results of a client with severe pre-eclampsia who is receiving magnesium sulfate.
Which finding would indicate a therapeutic level of magnesium sulfate?
Explanation
This indicates a therapeutic level of magnesium sulfate for a client with severe pre-eclampsia who is receiving magnesium sulfate.According to some sources, the effective therapeutic serum magnesium level is 1.8–3.0 mmol/L, which corresponds to 4.2–7 mg/dL or 3.5–7 mEq/L.
Choice B is wrong because serum calcium level of 8.5 mg/dL is within the normal range and does not indicate the effect of magnesium sulfate.
Choice C is wrong because serum creatinine level of 1.2 mg/dL is within the normal range and does not indicate the effect of magnesium sulfate.
Choice D is wrong because serum potassium level of 3.5 mEq/L is at the lower end of the normal range and does not indicate the effect of magnesium sulfate.
A nurse is preparing to administer hydralazine to a client with pre-eclampsia who has a blood pressure of 180/110 mmHg.
What is the rationale for using this medication?
Explanation
This is the rationale for using this medication in a client with pre-eclampsia who has a blood pressure of 180/110 mmHg.High blood pressure in pre-eclampsia can cause damage to the kidneys, liver, brain, and other organs, and can also increase the risk of complications for the baby.
Therefore, lowering blood pressure with hydralazine can help prevent or reduce these adverse outcomes.
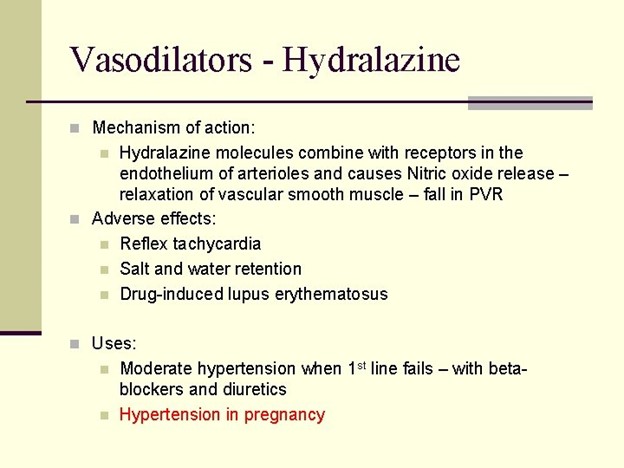
Choice A is wrong because hydralazine does not reduce cerebral edema or prevent seizures.These are symptoms of eclampsia, a more severe form of pre-eclampsia that requires different treatment.
Choice B is wrong because hydralazine does not increase uteroplacental perfusion or fetal oxygenation.These are affected by other factors such as the placental function, maternal position, and fetal well-being.
Choice C is wrong because hydralazine does not decrease proteinuria or prevent renal damage.
Proteinuria is a sign of kidney impairment that occurs in pre-eclampsia, but it is not directly affected by hydralazine.Renal damage can be prevented by controlling blood pressure and avoiding nephrotoxic drugs.
A nurse is assessing a client with pre-eclampsia who is receiving oxytocin for labor induction.
Which finding would alert the nurse to suspect that the client is developing HELLP syndrome?
Explanation
This is because HELLP syndrome is a complication of pregnancy that affects the liver and blood clotting.It can cause liver damage, bleeding problems, and high blood pressure.Epigastric pain or right upper quadrant pain is a sign of liver injury or rupture.
Choice B is wrong because blurred vision or flashes of light are symptoms of preeclampsia, not HELLP syndrome.
Preeclampsia is a condition that causes high blood pressure and protein in the urine during pregnancy.It can lead to HELLP syndrome, but not all women with preeclampsia develop HELLP syndrome.
Choice C is wrong because decreased urinary output or oliguria are also symptoms of preeclampsia, not HELLP syndrome.
Oliguria means producing less than 400 mL of urine in 24 hours.It can indicate kidney damage or failure due to high blood pressure or proteinuria.
Choice D is wrong because hyperreflexia or clonus are also symptoms of preeclampsia, not HELLP syndrome.
Hyperreflexia means having exaggerated reflexes, while clonus means having involuntary muscle spasms.
They can indicate nervous system involvement or seizures due to high
A nurse is providing discharge instructions to a client who had pre-eclampsia and delivered a healthy baby.
Which statement by the client indicates a need for further teaching?
Explanation
The client should not resume normal activities as soon as she gets home because she is still at risk for complications from preeclampsia.She should rest as directed by her healthcare provider and avoid strenuous activities that may increase her blood pressure.
Choice A is wrong because monitoring blood pressure at home is a recommended practice for clients who had preeclampsia.It can help detect any signs of worsening hypertension or organ damage.
Choice B is wrong because reporting any headache, vision changes, or abdominal pain to the doctor is a crucial step to prevent serious complications from preeclampsia.These symptoms may indicate damage to the brain, eyes, or liver and require immediate medical attention.
Choice D is wrong because continuing to take prenatal vitamins and iron supplements is beneficial for the client’s recovery and health.Prenatal vitamins can provide essential nutrients that may be lacking in the diet, and iron supplements can prevent or treat anemia that may result from blood loss during delivery.
A nurse is caring for a client with severe pre-eclampsia who is receiving magnesium sulfate.
Which of the following findings would indicate magnesium toxicity and require immediate intervention?
Explanation
A. Urinary output of 25 mL/hour.This indicates magnesium toxicity and requires immediate intervention because it means the kidneys are not functioning properly and magnesium is not being excreted.Magnesium toxicity can cause life-threatening complications such as respiratory depression, cardiac arrest, and coma.
B. Respiratory rate of 14 breaths/minute is normal and does not indicate magnesium toxicity.A respiratory rate of less than 12 breaths/minute or more than 20 breaths/minute would be abnormal and require further assessment.
C. Deep tendon reflexes 1+ are normal and do not indicate magnesium toxicity.A loss of deep tendon reflexes or clonus would indicate magnesium toxicity and require immediate intervention.
D. Serum magnesium level of 6 mg/dL is within the therapeutic range for preeclampsia and does not indicate magnesium toxicity.
The therapeutic range for preeclampsia is 4 to 7 mg/dL.A serum magnesium level of more than 8 mg/dL would indicate magnesium toxicity and require immediate intervention.
A nurse is assessing a client with severe pre-eclampsia who reports a severe headache and blurred vision.
The nurse notes that the client has hyperreflexia with clonus.
What is the most likely explanation for these findings?
Explanation
The most likely explanation for the client's findings of severe headache, blurred vision, hyperreflexia, and clonus in the context of severe pre-eclampsia is A. Cerebral edema.
Pre-eclampsia is a pregnancy-related condition characterized by high blood pressure (hypertension) and signs of organ damage, most commonly affecting the liver and kidneys. Severe pre-eclampsia can lead to complications such as eclampsia, which is characterized by seizures. The symptoms described by the client, including severe headache and blurred vision, are consistent with neurological manifestations associated with severe pre-eclampsia.
Hyperreflexia refers to an exaggerated reflex response, and clonus refers to rhythmic contractions of a muscle when it is passively stretched. Both hyperreflexia and clonus are indicative of central nervous system (CNS) hyperexcitability. Cerebral edema, which is the swelling of the brain due to fluid accumulation, can lead to increased intracranial pressure and neurological symptoms such as headache, vision changes, hyperreflexia, and clonus.
While other complications such as pulmonary edema (B), hemolysis (C), and thrombocytopenia (D) can occur in severe pre-eclampsia, they are not directly associated with the reported symptoms of severe headache, blurred vision, hyperreflexia, and clonus.
Pre-eclampsia is a pregnancy-related condition characterized by high blood pressure (hypertension) and signs of organ damage, most commonly affecting the liver and kidneys. Severe pre-eclampsia can lead to complications such as eclampsia, which is characterized by seizures. The symptoms described by the client, including severe headache and blurred vision, are consistent with neurological manifestations associated with severe pre-eclampsia.
Hyperreflexia refers to an exaggerated reflex response, and clonus refers to rhythmic contractions of a muscle when it is passively stretched. Both hyperreflexia and clonus are indicative of central nervous system (CNS) hyperexcitability. Cerebral edema, which is the swelling of the brain due to fluid accumulation, can lead to increased intracranial pressure and neurological symptoms such as headache, vision changes, hyperreflexia, and clonus.
While other complications such as pulmonary edema (B), hemolysis (C), and thrombocytopenia (D) can occur in severe pre-eclampsia, they are not directly associated with the reported symptoms of severe headache, blurred vision, hyperreflexia, and clonus.
A nurse is reviewing the laboratory results of a client with severe pre-eclampsia.
Which of the following results would indicate hepatic involvement? (Select all that apply.)
Explanation
The correct answer is choice B, C and D. These results indicate hepatic involvement because they are elevated above the normal ranges.According to, the normal ranges for AST, ALT and LDH are:
• AST: 8 to 48 U/L
• ALT: 7 to 55 U/L
• LDH: 122 to 222 U/L
Choice A is wrong because serum creatinine is not a marker of liver function, but of kidney function.The normal range for serum creatinine is 0.6 to 1.3 mg/dL for adults.
Choice E is wrong because platelet count is not a marker of liver function, but of blood clotting ability.The normal range for platelet count is 150 to 450 x 10^9/L.
A nurse is preparing to administer hydralazine to a client with severe pre-eclampsia who has a blood pressure of 170/110 mmHg.
What is the expected outcome of this medication?
Explanation
To lower blood pressure.Hydralazine is an antihypertensive drug that is used to treat severe hypertension in pre-eclampsia.It works by relaxing the blood vessels and reducing the resistance to blood flow.
This helps to lower the blood pressure and prevent complications such as stroke, kidney damage, or placental abruption.
Choice A is wrong because hydralazine does not prevent seizures.
Seizures are a symptom of eclampsia, a more severe form of pre-eclampsia.To prevent seizures, magnesium sulfate is usually given intravenously.
Choice C is wrong because hydralazine does not increase urine output.In fact, it may cause fluid retention and edema as a side effect.Diuretics are drugs that increase urine output, but they are not recommended for pre-eclampsia because they may worsen the condition by reducing blood volume and placental perfusion.
Choice D is wrong because hydralazine does not improve placental perfusion.
Placental perfusion is the blood flow to the placenta, which provides oxygen and nutrients to the fetus.
Placental perfusion may be impaired in pre-eclampsia due to abnormal development of the placental blood vessels.Hydralazine does not affect the placental blood vessels directly, but it may improve placental perfusion indirectly by lowering the maternal blood pressure and reducing the risk of abruption.
However, this is not the primary or expected outcome of hydralazine therapy.
A nurse is educating a client with mild pre-eclampsia about the signs and symptoms that she should report to her health care provider.
Which of the following should the nurse include? (Select all that apply.)
Explanation
The correct answer is choice C and D.Epigastric pain and decreased fetal movement are signs of severe pre-eclampsia that indicate damage to the liver and placenta respectively.These symptoms should be reported to the health care provider immediately as they may lead to serious complications such as eclampsia, HELLP syndrome, placental abruption or fetal growth restriction.
Choice A is wrong because sudden weight gain is a common symptom of mild pre-eclampsia that does not necessarily require immediate attention.However, it should be monitored regularly along with blood pressure and urine protein levels.
Choice B is wrong because swelling of the face and hands is also a common symptom of mild pre-eclampsia that does not indicate severe organ damage.It may be caused by fluid retention or edema.
Choice E is wrong because vaginal bleeding is not a typical symptom of pre-eclampsia.It may be a sign of other pregnancy complications such as placenta previa, placental abruption or cervical infection.
A nurse is caring for a client who has severe preeclampsia and is receiving magnesium sulfate infusion.
Which of the following assessments is most important for the nurse to monitor?
Explanation
Deep tendon reflexes.
The nurse should monitor the client’s deep tendon reflexes to assess for signs of magnesium toxicity, which can cause respiratory depression, cardiac arrest, and coma.Magnesium sulfate is given to prevent seizures in clients with severe preeclampsia, but it can also have adverse effects on the neuromuscular system.
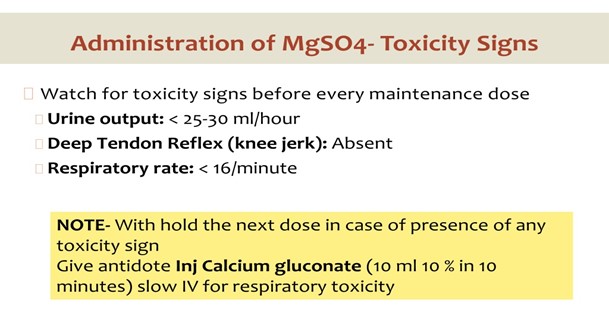
Choice A is wrong because blood pressure is not the most important assessment for a client receiving magnesium sulfate.
Blood pressure is a manifestation of preeclampsia, but it does not indicate magnesium toxicity.
Choice B is wrong because urine output is not the most important assessment for a client receiving magnesium sulfate.
Urine output should be at least 25 to 30 mL/hr to promote adequate excretion of magnesium, but it does not reflect the level of magnesium in the blood.
Choice D is wrong because fetal heart rate is not the most important assessment for a client receiving magnesium sulfate.
Fetal heart rate is important to monitor for signs of fetal distress, but it does not indicate maternal magnesium toxicity.
A client who is 36 weeks pregnant is admitted to the hospital with a diagnosis of eclampsia.
She has a history of chronic hypertension and gestational diabetes.
The nurse anticipates that the client will receive which of the following medications to prevent seizures?
Explanation
Magnesium sulfate.Magnesium sulfate is thedrug of choiceto prevent and treat seizures in people with severe preeclampsia and eclampsia.It is an anticonvulsant medication that reduces the risk of eclampsia by 50%.
Choice A is wrong because hydralazine is a blood pressure medication that can lower blood pressure in people with preeclampsia or eclampsia, but it does not prevent seizures.
Choice B is wrong because nifedipine is another blood pressure medication that can lower blood pressure in people with preeclampsia or eclampsia, but it does not prevent seizures.
Choice D is wrong because diazepam is an anticonvulsant medication that was previously used to treat eclamptic seizures, but it has been replaced by magnesium sulfate as the preferred drug due to its better safety and efficacy.Diazepam can also cause sedation and respiratory depression in the mother and the fetus.
Normal ranges for blood pressure are below 140/90 mm Hg, for proteinuria are below 300 mg/24 hours, for platelet count are 150,000 to 450,000 per microliter, for liver enzymes are 7 to 56 units per liter for alanine aminotransferase (ALT) and 10 to 40 units per liter for aspartate aminotransferase (AST), and for magnesium levels are 1.5 to 2.5 mEq/L.
A nurse is reviewing the laboratory results of a client who has mild preeclampsia.
Which of the following findings would indicate a need for further evaluation?
Explanation
Serum creatinine of 1.2 mg/dL.This indicates a need for further evaluation because it is above the normal range of 0.6 to 1.1 mg/dL for women and suggests kidney impairment.Preeclampsia can affect the kidneys and other organs.
Choice A is wrong because a platelet count of 150,000/mm3 is within the normal range of 150,000 to 450,000/mm3.
Choice C is wrong because proteinuria of 1+ on dipstick is expected in mild preeclampsia.
Choice D is wrong because serum albumin of 3.5 g/dL is within the normal range of 3.4 to 5.4 g/dL.
A nurse is providing discharge teaching to a client who had preeclampsia and delivered a healthy baby at 38 weeks of gestation.
Which of the following instructions should the nurse include in the teaching?
Explanation
Report any headache that is not relieved by acetaminophen.This is because a headache that persists despite taking pain medication can be a sign of increased blood pressure or brain swelling, which are serious complications of preeclampsia.
Choice B is wrong because some vaginal bleeding for up to 6 weeks postpartum is normal and expected for any woman who has given birth, regardless of whether she had preeclampsia or not.
Choice C is wrong because resuming sexual activity as soon as you feel comfortable is also a normal recommendation for any woman who has given birth, unless there are other medical reasons to avoid it.
Choice D is wrong because drinking at least 3 liters of fluid per day to prevent dehydration is not necessary for a woman who had preeclampsia.In fact, drinking too much fluid can worsen the swelling and fluid retention that are common in preeclampsia.
(Select all that apply) A nurse is assessing a client who is 32 weeks pregnant and has a diagnosis of severe preeclampsia.
Which of the following findings should the nurse report to the provider immediately?
Explanation
The correct answer is choice A, B, D and E. These are all signs of severe preeclampsia that indicate organ damage and require immediate medical attention.According to Mayo Clinic, preeclampsia is a complication of pregnancy that causes high blood pressure, protein in the urine, or other signs of organ damage after 20 weeks of gestation.
Choice A is correct because epigastric pain can indicate liver damage or bleeding in the abdomen due to preeclampsia.
Choice B is correct because blurred vision or light sensitivity can indicate brain damage or increased pressure in the skull due to preeclampsia.
Choice C is wrong because facial edema is a common symptom of normal pregnancy and does not necessarily indicate preeclampsia.
Choice D is correct because hyperreflexia can indicate nervous system damage or increased pressure in the skull due to preeclampsia.
Choice E is correct because oliguria can indicate kidney damage or decreased blood flow to the kidneys due to preeclampsia.
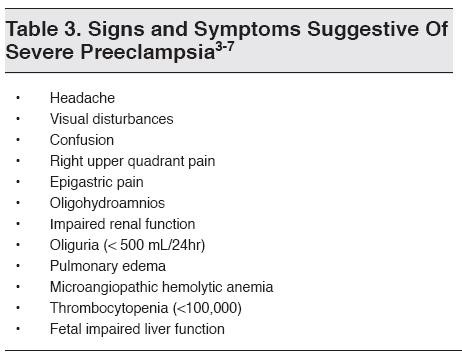
HELLP Syndrome
A nurse is caring for a client with HELLP syndrome.
Which of the following laboratory tests should the nurse monitor closely?
Explanation
Coagulation profile.This is because HELLP syndrome is a pregnancy complication that involveshemolysis(breaking down of red blood cells),elevated liver enzymes(indicating liver injury) andlow platelet count(impairing blood clotting).A coagulation profile can help monitor these abnormalities and assess the risk of bleeding or clotting complications.
Choice A is wrong because blood glucose is not directly affected by HELLP syndrome, although it may be elevated in women with gestational diabetes or pre-existing diabetes.
Choice B is wrong because serum creatinine is a marker of kidney function, not liver function.However, kidney function may also be impaired in women with preeclampsia or eclampsia, which are associated with HELLP syndrome.
Choice D is wrong because thyroid function is not related to HELLP syndrome.Thyroid disorders may occur in pregnancy, but they have different symptoms and causes.
A client with HELLP syndrome reports severe epigastric pain and nausea.
The nurse should suspect that the client is experiencing:
Explanation
Hepatic rupture.The client with HELLP syndrome is experiencing severe epigastric pain and nausea due to liver damage caused by hemolysis, elevated liver enzymes and low platelets.Hepatic rupture is a life-threatening complication of HELLP syndrome that can cause bleeding and shock.
Choice B.Pancreatitis is wrong because it is not a common complication of HELLP syndrome and it usually causes more diffuse abdominal pain rather than localized epigastric pain.
Choice C.Gastric ulcer is wrong because it is not associated with HELLP syndrome and it does not explain the other symptoms such as hemolysis, elevated liver enzymes and low platelets.
Choice D.Cholecystitis is wrong because it is not related to HELLP syndrome and it usually causes right upper quadrant pain rather than epigastric pain.
Normal ranges for liver enzymes are AST < 40 IU/L and ALT < 56 IU/L.Normal range for platelet count is 150-400 x 10⁹/L.
A nurse is reviewing the discharge instructions for a client who had HELLP syndrome during pregnancy.
Which of the following statements by the client indicates a need for further teaching?
Explanation
“I will resume my oral contraceptive pills as soon as possible.”
This statement indicates a need for further teaching because oral contraceptive pills are not recommended for women who had HELLP syndrome during pregnancy.Oral contraceptive pills can increase the risk of blood clots and high blood pressure, which can be dangerous for women with a history of HELLP syndrome.
Women who had HELLP syndrome should consult their provider about alternative methods of contraception that are safer for them.
The other statements are correct and do not indicate a need for further teaching:
• A.“I will need to have regular blood pressure checks for a few weeks.” This statement is correct because women who had HELLP syndrome are at risk of developing high blood pressure or preeclampsia after delivery and need to monitor their blood pressure regularly.
• B.“I will avoid taking any nonsteroidal anti-inflammatory drugs (NSAIDs).” This statement is correct because NSAIDs can interfere with platelet function and increase the risk of bleeding, which can be harmful for women who had HELLP syndrome.
• D.“I will report any signs of bleeding or infection to my provider.” This statement is correct because women who had HELLP syndrome are at risk of developing complications such as hemorrhage, infection, liver rupture, or stroke and need to seek medical attention if they notice any signs of bleeding or infection.
Normal ranges:
• Blood pressure: less than 140/90 mmHg
• Platelet count: 150,000 to 450,000 per microliter of blood
• Liver enzymes: AST (aspartate aminotransferase) less than 40 U/L; ALT (alanine aminotransferase) less than 40 U/L
• Hemoglobin: 12 to 16 g/dL for women
A nurse is preparing to administer magnesium sulfate to a client with HELLP syndrome.
Which of the following actions should the nurse take? (Select all that apply.)
Explanation
The correct answer is choice A, B, C and D. Here is why:
• Choice A is correct becausemonitoring the client’s deep tendon reflexesis a way to assess the client’s neuromuscular status and the risk of magnesium toxicity.Magnesium sulfate can cause muscle weakness and decreased reflexes.
• Choice B is correct becausechecking the client’s urine output every houris a way to monitor the client’s renal function and fluid balance.Magnesium sulfate is excreted by the kidneys and can cause oliguria and fluid overload.
• Choice C is correct becauseadministering calcium gluconate as an antidote if neededis a way to treat magnesium toxicity.Calcium gluconate reverses the effects of magnesium sulfate on the neuromuscular and cardiovascular systems.
• Choice D is correct becausekeeping a bag of 0.9% sodium chloride solution at the bedsideis a way to prepare for possible complications of magnesium sulfate therapy such as hypotension, pulmonary edema, or cardiac arrest.Normal saline can help restore blood pressure and fluid balance.
• Choice E is wrong becauseflushing the IV line with heparin before and after infusionis not necessary or recommended for magnesium sulfate administration.Heparin is an anticoagulant that can increase the risk of bleeding and is not compatible with magnesium sulfate.
A nurse is providing education to a pregnant client who is at risk for developing HELLP syndrome.
Which of the following information should the nurse include?
Explanation
HELLP syndrome can occur before or after delivery.
Explanation:
• HELLP syndrome is a rare pregnancy complication that is a type of preeclampsia.It stands for hemolysis (breaking down of red blood cells), elevated liver enzymes (indicating liver damage), and low platelet count (affecting blood clotting).
• HELLP syndrome usually occurs during the third trimester of pregnancy, but it can also develop in the first week after childbirth (postpartum preeclampsia).
• The other statements are wrong because:
➤ B.HELLP syndrome is not caused by a bacterial infection, but by unknown factors that may involve abnormal placental development.
➤ C.HELLP syndrome cannot be prevented by taking folic acid supplements, but by early diagnosis and treatment of preeclampsia.
➤
D. HELLP syndrome is treated with corticosteroids and antihypertensives, but only as supportive measures to manage the symptoms and complications.The definitive treatment is delivery of the baby as soon as possible.
• Normal ranges for some of the tests used to diagnose HELLP syndrome are:
➤ Lactate dehydrogenase (LDH): 140 to 280 U/L
➤ Aspartate transaminase (AST): 10 to 40 U/L
➤ Platelet count: 150 to 450 x 10^9/L
Diagnostic Criteria and Investigations
A nurse is reviewing the results of a 24-hour urine collection for a client who is 32 weeks pregnant and has suspected pre-eclampsia.
Which of the following findings indicates proteinuria?
Explanation
Protein excretion of 450 mg indicates proteinuria.Proteinuria is the presence of excess protein in the urine, which can be a sign of kidney damage or disease.Normal protein excretion in a 24-hour urine collection is less than 150 mg.
Choice A is wrong because protein excretion of 150 mg is within the normal range.
Choice B is wrong because protein excretion of 250 mg is slightly above the normal range, but not enough to indicate proteinuria.
Choice C is wrong because protein excretion of 350 mg is also above the normal range, but not enough to indicate proteinuria.
Preeclampsia is a condition that affects some pregnant women, usually after 20 weeks of pregnancy.It causes high blood pressure and proteinuria, which can harm both the mother and the baby.A 24-hour urine collection is a simple lab test that measures what’s in the urine and checks kidney function.The test is done by collecting all the urine passed in a 24-hour period in a special container that must be kept cool until returned to the lab.
A nurse is performing a non-stress test (NST) for a client who is 34 weeks pregnant and has pre-eclampsia.
Which of the following fetal heart rate patterns indicates a reactive test?
Explanation
Two or more accelerations of at least 15 beats/min above baseline lasting for at least 15 seconds in a 20-minute period.This indicates a reactive test, which means that the fetus is well oxygenated and not in distress.
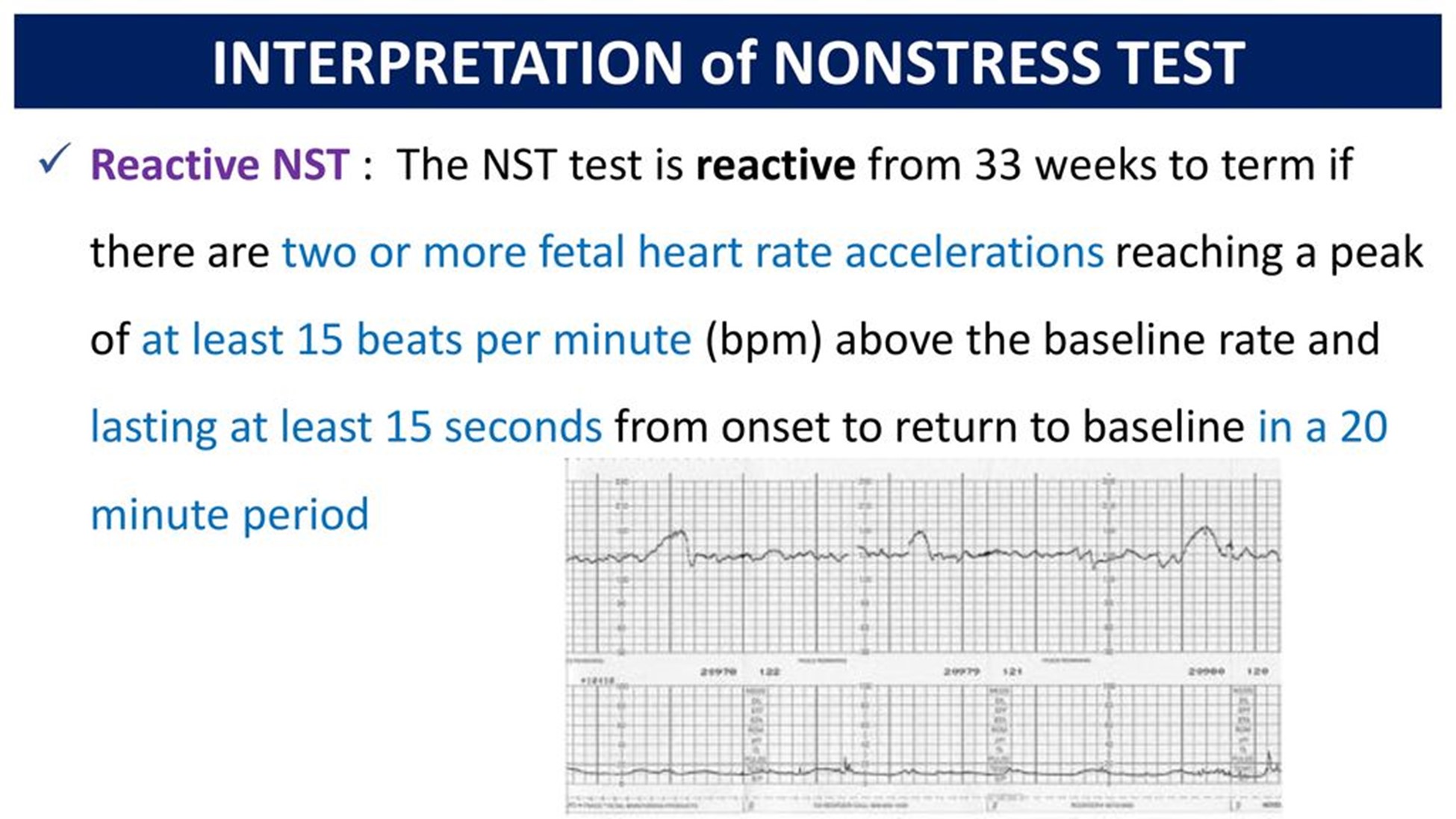
Choice B is wrong because no accelerations or decelerations in a 20-minute period indicate a non-reactive test, which may suggest fetal hypoxia or acidosis.
Choice C is wrong because one acceleration of at least 10 beats/min above baseline lasting for at least 10 seconds in a 20-minute period is the criterion for a reactive test for gestational age less than 32 weeks, not 34 weeks.
Choice D is wrong because variable decelerations with normal variability in a 20-minute period indicate cord compression or fetal head compression, not a reactive test.
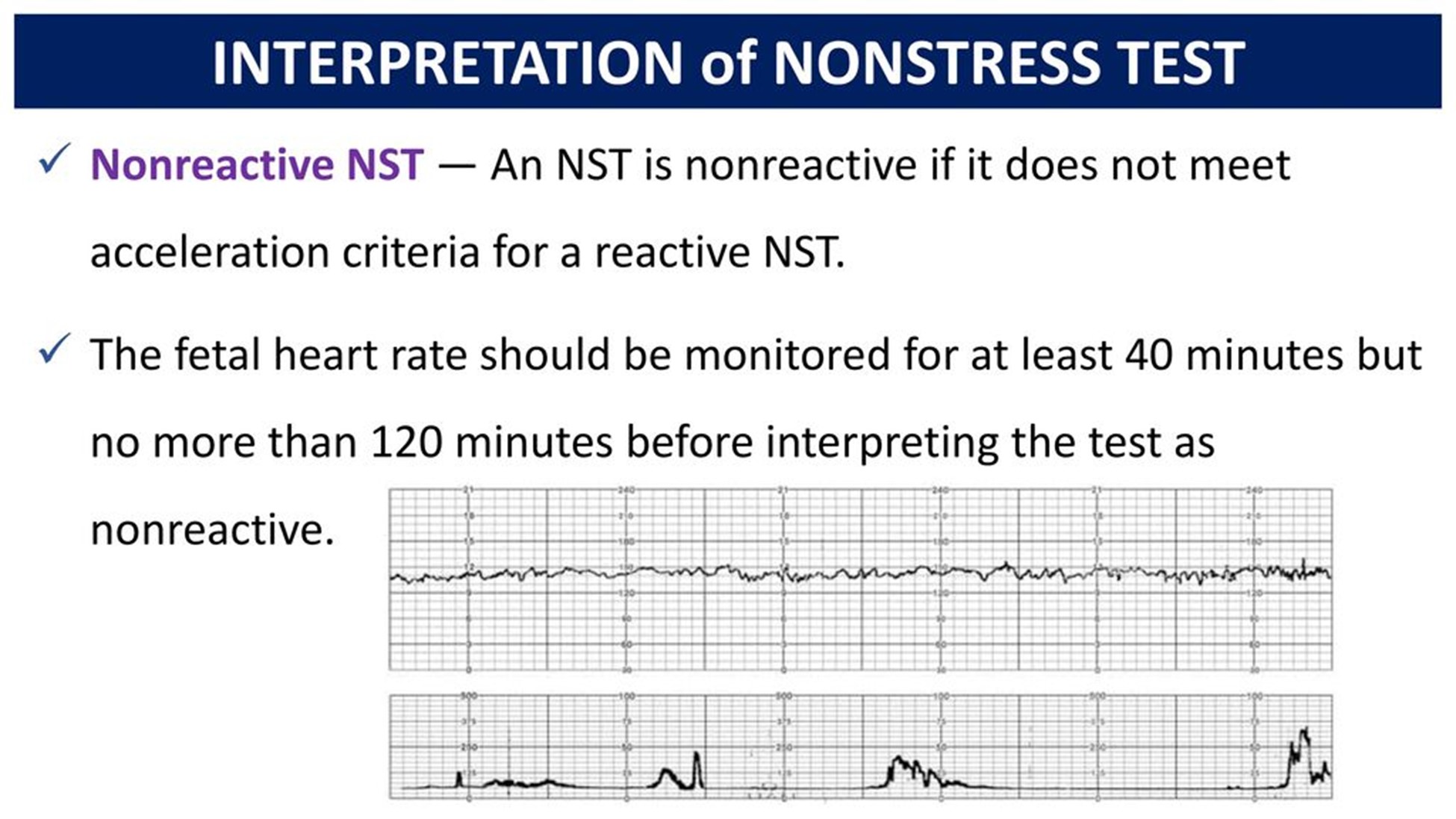
A nurse is preparing to administer magnesium sulfate IV to a client who has severe pre-eclampsia.
Which of the following actions should the nurse take? (Select all that apply.)
Explanation
The correct answer is choice A, B, C and E.The nurse should monitor the client’s deep tendon reflexes hourly because magnesium sulfate can cause neuromuscular blockade and decreased reflexes.The nurse should keep calcium gluconate readily available because it is the antidote for magnesium toxicity.The nurse should maintain a urine output of at least 40 mL/hr because magnesium is excreted by the kidneys and low urine output can indicate renal impairment or fluid overload.The nurse should check the client’s blood pressure every 15 minutes because magnesium sulfate can cause hypotension and preeclampsia can cause hypertension.
Choice D is wrong because the medication should not be infused via a peripheral IV line, but rather through a central line or a large-bore IV catheter to prevent tissue damage.
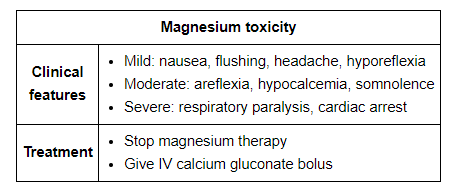
A nurse is assessing a client who has eclampsia and is receiving magnesium sulfate IV.
Which of the following findings should alert the nurse to suspect magnesium toxicity?
Explanation
This indicates that the client has respiratory depression, which is a sign of magnesium toxicity.Magnesium sulfate is given to prevent and treat seizures in clients with eclampsia, but it can also cause adverse effects such as hypotension, decreased urine output, absent or diminished reflexes, and cardiac arrest.
Choice B is wrong because urine output of 50 mL/hr is within the normal range and does not indicate magnesium toxicity.The nurse should monitor the client’s urine output closely and report any decrease below 30 mL/hr.
Choice C is wrong because serum magnesium level of 6 mg/dL is within the therapeutic range of 4 to 7 mg/dL for clients receiving magnesium sulfate.The nurse should monitor the client’s serum magnesium level regularly and report any increase above 8 mg/dL, which indicates toxicity.
Choice D is wrong because patellar reflex of 2+ is normal and does not indicate magnesium toxicity.The nurse should assess the client’s deep tendon reflexes frequently and report any decrease or absence of reflexes, which indicates toxicity.
A nurse is caring for a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously.
What is the primary reason for administering magnesium sulfate to this client?
Explanation
A. To prevent seizures.
Magnesium sulfate is a mineral that can reduce seizure risks in women with severe preeclampsia.It is often given intravenously and can also be used to prolong pregnancy for up to two days.Magnesium sulfate is also used to prevent and manage seizures in women with postpartum preeclampsia.
• Statement B is wrong because magnesium sulfate does not lower blood pressure.It may be given along with medications that help reduce blood pressure.
• Statement C is wrong because magnesium sulfate does not induce labor.It may be given to delay delivery for up to 48 hours to allow time for the administration of drugs that speed up the baby’s lung development.
• Statement D is wrong because magnesium sulfate does not reduce edema.Edema is a common symptom of preeclampsia, but it is not a direct cause of complications.
A nurse is monitoring a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously.
Which of the following signs indicates magnesium toxicity and requires immediate intervention?
Explanation
According to Mayo Clinic, loss of reflexes is a sign of magnesium toxicity and requires immediate intervention.
Other signs of magnesium toxicity include:
• Decreased urine output
• Difficulty breathing
• Drowsiness or confusion
• Low blood pressure
• Slow heart rate
• Weakness
Choice B is wrong because headache is not a sign of magnesium toxicity.
It may be a symptom of preeclampsia or other conditions, but it does not indicate an overdose of magnesium sulfate.
Choice C is wrong because nausea is not a sign of magnesium toxicity.
It may be a side effect of magnesium sulfate or a symptom of preeclampsia or other conditions, but it does not indicate an overdose of magnesium sulfate.
Choice D is wrong because blurred vision is not a sign of magnesium toxicity.
It may be a symptom of preeclampsia or other conditions, but it does not indicate an overdose of magnesium sulfate.
A nurse is preparing to administer antihypertensive therapy to a client with severe pre-eclampsia.
Which of the following blood pressure readings is the target goal for this client?
Explanation
The target blood pressure goal for a client with severe pre-eclampsia is less than 160/110 mmHg.
This is because lowering the blood pressure too much or too fast can compromise the placental perfusion and fetal oxygenation.
Choice A is wrong because it is the target blood pressure goal for a client with chronic hypertension or gestational hypertension without severe features.
Choice B is wrong because it is the target blood pressure goal for a client with mild pre-eclampsia.
Choice D is wrong because it is too high and can increase the risk of maternal and fetal complications such as stroke, eclampsia, placental abruption, and fetal growth restriction.
Normal blood pressure ranges are less than 120/80 mmHg for systolic and diastolic pressures respectively.
A nurse is administering corticosteroids to a client with severe pre-eclampsia who is 32 weeks pregnant.
What is the main purpose of giving corticosteroids to this client?
Explanation
To accelerate fetal lung maturity.Corticosteroids are given to pregnant women with severe pre-eclampsia who are at risk of preterm delivery to help the development of the fetus’s lungs and reduce the risk of respiratory distress syndrome.
This can improve the survival and health outcomes of the newborn.
Choice A is wrong because corticosteroids do not reduce inflammation in pre-eclampsia.They are used for other inflammatory conditions such as asthma or arthritis.
Choice B is wrong because corticosteroids do not prevent infection in pre-eclampsia.They can actually increase the risk of infection by suppressing the immune system.
Choice D is wrong because corticosteroids do not increase platelet count in pre-eclampsia.They can actually decrease the platelet count by causing thrombocytopenia.
A nurse is assessing the fetal heart rate and uterine activity of a client with severe pre-eclampsia who is receiving magnesium sulfate intravenously.
Which of the following findings should the nurse report to the provider immediately?
Explanation
C. Fetal heart rate decelerations.
Fetal heart rate decelerations are temporary drops in the fetal heart rate that can indicate fetal distress or lack of oxygen.There are three types of decelerations: early, late and variable.Early decelerations are benign and caused by compression of the fetus’s head during a uterine contraction.Late decelerations are caused by uteroplacental insufficiency, which is a decrease in blood flow to the placenta.Variable decelerations are the most common type and vary in shape, duration and intensity.They are often caused by cord compression or other factors that affect fetal oxygenation.
•
A. Fetal heart rate of 140 beats per minute.
Statement is wrong because this is a normal fetal heart rate.The normal range for fetal heart rate is 120-160 beats per minute.
•
B. Uterine contractions every 10 minutes.
Statement is wrong because this is a normal frequency for uterine contractions during early labor.
The normal range for uterine contractions is 5-10 minutes apart.
•
D. Uterine contractions lasting 60 seconds.
Statement is wrong because this is a normal duration for uterine contractions during active labor.
The normal range for uterine contractions is 45-90 seconds long.
A nurse is caring for a client with eclampsia who is receiving magnesium sulfate intravenously.
Which of the following findings indicates magnesium toxicity?
Explanation
Fetal heart rate decelerations indicate a possible compromise of fetal oxygenation and should be reported to the provider immediately.Decelerations can be caused by various factors such as cord compression, uterine hyperstimulation, maternal hypotension, or placental abruption.
Choice A is wrong because a fetal heart rate of 140 beats per minute is within the normal range of 110 to 160 beats per minute.
Choice B is wrong because uterine contractions every 10 minutes are not abnormal in a client with severe pre-eclampsia who is receiving magnesium sulfate.Magnesium sulfate is used to prevent seizures and lower blood pressure in pre-eclampsia, but it does not stop labor.
Choice D is wrong because uterine contractions lasting 60 seconds are not a sign of …
A nurse is preparing to administer hydralazine to a client with eclampsia who has a blood pressure of 180/120 mmHg.
What is the rationale for administering this medication?
Explanation
To increase placental perfusion.
Hydralazine is an antihypertensive drug that dilates the blood vessels and lowers the blood pressure.By doing so, it improves the blood flow to the placenta and reduces the risk of fetal hypoxia and growth restriction.
Choice A is wrong because hydralazine does not prevent cerebral edema.
Cerebral edema is a complication of severe preeclampsia or eclampsia that can cause seizures, headaches, and visual disturbances.Hydralazine may lower the blood pressure and reduce the risk of stroke, but it does not directly affect the brain swelling.
Choice B is wrong because hydralazine does not reduce uterine contractions.
Uterine contractions are stimulated by oxytocin and prostaglandins, which are not affected by hydralazine.Hydralazine may cause reflex tachycardia, which can increase the cardiac output and uterine blood flow, but it does not alter the uterine muscle activity.
Choice D is wrong because hydralazine does not promote diuresis.
Diuresis is the increased production of urine by the kidneys.
Hydralazine may cause fluid retention and edema by activating the renin-angiotensin-aldosterone system, which increases sodium and water reabsorption.Hydralazine may also cause a decrease in renal perfusion and glomerular filtration rate, which can impair the kidney function and urine output.
A nurse is assessing a client with eclampsia who is having a seizure.
Which of the following actions should the nurse take first?
Explanation
Turn the client to the side.This is because turning the client to the side will prevent aspiration and maintain a patent airway during a seizure.
Some possible explanations for the other choices are:
• Choice B. Insert an oral airway.This is wrong because inserting an oral airway during a seizure can cause injury to the client’s mouth or teeth, and it can also stimulate the gag reflex and increase the risk of vomiting and aspiration.
• Choice C. Administer oxygen via face mask.This is wrong because administering oxygen via face mask during a seizure can be difficult and ineffective, as the client may not be able to breathe through the mask or may dislodge it with their movements.Oxygen can be given after the seizure has stopped, if needed.
• Choice D. Document the duration of the seizure.
This is wrong because documenting the duration of the seizure is not a priority action during a seizure.The nurse should first ensure the client’s safety and airway patency, and then document the seizure characteristics after it has ended.
A nurse is teaching a client with eclampsia about the purpose of corticosteroid therapy.
Which of the following statements by the client indicates understanding of the teaching?
Explanation
“This medication will help my baby’s lungs develop faster.” Corticosteroid therapy is given to pregnant clients with eclampsia to accelerate fetal lung maturity and reduce the risk of respiratory distress syndrome in the newborn.
Some possible explanations for the other choices are:
• Choice A is wrong because corticosteroids do not lower blood pressure.Antihypertensive drugs such as hydralazine or labetalol are used to treat hypertension in eclampsia.
• Choice B is wrong because corticosteroids do not prevent seizures.Magnesium sulfate is the drug of choice for seizure prophylaxis and treatment in eclampsia.
• Choice D is wrong because corticosteroids do not reduce inflammation in the body.They may have anti-inflammatory effects in some conditions, but their main purpose in eclampsia is to enhance fetal lung development.
Normal ranges for blood pressure and proteinuria in pregnancy are:
• Blood pressure: less than 140/90 mm Hg
• Proteinuria: less than 300 mg/24 hours or less than 1+ on dipstick
(select all that apply) A nurse is planning care for a client with eclampsia who is scheduled for delivery as soon as possible.
Which of the following interventions should the nurse include in the plan? (Select all that apply.)
Explanation
Answer is A and C. Eclampsia is a life-threatening complication of pregnancy that causes seizures due to severe hypertension.The nurse should monitor the fetal heart rate and uterine activity continuously to assess for signs of fetal distress or placental abruption.The nurse should also maintain a dark and quiet environment to reduce stimuli that might trigger seizures.
Statement B is wrong because administering oxytocin to augment labor can increase the risk of uterine rupture and placental abruption in a patient with eclampsia.
Statement D is wrong because encouraging oral fluids and a high-protein diet can worsen the fluid retention and renal impairment in a patient with eclampsia.
Statement E is wrong because assessing for signs of placental abruption is not enough.The nurse should also monitor the vital signs, urine output, neurological status, and laboratory values of the patient with eclampsia.
Normal ranges for blood pressure are less than 120/80 mmHg for non-pregnant adults and less than 140/90 mmHg for pregnant women.Normal ranges for protein in urine are less than 150 mg/day for non-pregnant adults and less than 300 mg/day for pregnant women.
A nurse is caring for a client with HELLP syndrome who is receiving magnesium sulfate intravenously.
What is the main purpose of this medication?
Explanation
Maintain a dark and quiet environment.This intervention helps to reduce sensory stimulation and prevent seizures in a client with eclampsia.
Choice A is wrong becausemonitoring fetal heart rate and uterine activity continuouslyis not a priority intervention for a client with eclampsia.The priority is to prevent seizures and control blood pressure.
Choice B is wrong becauseadministering oxytocin to augment laboris contraindicated in a client with eclampsia.Oxytocin can increase blood pressure and cause uterine hyperstimulation, which can worsen the condition and endanger the mother and the fetus.
Choice D is wrong becauseencouraging oral fluids and a high-protein dietis not appropriate for a client with eclampsia.
The client should be kept NPO to prevent aspiration in case of a seizure.A high-protein diet can increase the risk of renal failure and hepatic dysfunction.
Choice E is wrong becauseassessing for signs of placental abruptionis not a specific intervention for a client with eclampsia.Placental abruption can occur as a complication of eclampsia, but it is not the main focus of care.
A nurse is reviewing the laboratory results of a client with HELLP syndrome.
Which of the following findings would indicate hemolysis?
Explanation
Elevated serum lactate dehydrogenase (LDH) indicates hemolysis, which is one of the components of HELLP syndrome.Hemolysis is the destruction of red blood cells that occurs when they pass through damaged blood vessels.
Choice A is wrong because elevated serum creatinine indicates kidney dysfunction, which is not specific for hemolysis.
Choice C is wrong because elevated serum alkaline phosphatase (ALP) indicates liver damage, which is another component of HELLP syndrome, but not specific for hemolysis.
Choice D is wrong because elevated serum uric acid indicates increased purine metabolism, which can be associated with preeclampsia and HELLP syndrome, but not specific for hemolysis.
Management Principles and Nursing Interventions
A nurse is caring for a client with mild pre-eclampsia who is at 32 weeks of gestation.
The nurse should anticipate administering which medication to the client?
Explanation
Betamethasone.This is because betamethasone is a corticosteroid that can help speed up the fetal lung development and reduce the risk of respiratory distress syndrome in preterm babies.
A client with mild pre-eclampsia who is at 32 weeks of gestation may need to deliver early if the condition worsens, so betamethasone can help prepare the baby for birth.
Choice A is wrong because magnesium sulfate is used to prevent seizures in women with severe preeclampsia or eclampsia, not mild preeclampsia.Magnesium sulfate can also prolong pregnancy for up to two days, but it does not improve fetal outcomes.
Choice C is wrong because oxytocin is a hormone that stimulates uterine contractions and induces labor.Oxytocin is not indicated for mild preeclampsia unless there are other reasons to deliver the baby urgently.
Choice D is wrong because misoprostol is a medication that can cause cervical ripening and uterine contractions.Misoprostol is used for medical abortion, induction of labor, or management of postpartum hemorrhage.It is not used for mild preeclampsia unless there are other indications for delivery.
A nurse is teaching a client with mild pre-eclampsia about dietary modifications.
Which statement by the client indicates a need for further teaching?
Explanation
“I should limit my salt intake to less than 5 grams per day.” This statement indicates a need for further teaching because clients with mild pre-eclampsia do not need to restrict their salt intake.Salt restriction can lead to low blood volume and decreased placental perfusion.A regular diet with adequate protein and calories is recommended for clients with mild pre-eclampsia.
Choice B is wrong because drinking at least 2 liters of water every day can help prevent dehydration and maintain blood volume.
Choice C is wrong because avoiding foods and drinks that contain caffeine can help lower blood pressure and reduce the risk of seizures.
Choice D is wrong because increasing protein intake to 100 grams per day can help replenish the protein lost in urine due to proteinuria.Protein also helps maintain plasma oncotic pressure and prevent edema.
Normal ranges for salt intake are about 6 grams per day for healthy adults.
Normal ranges for protein intake are about 0.8 grams per kilogram of body weight per day for healthy adults.
A nurse is monitoring the fetal well-being of a client with mild pre-eclampsia who is at 28 weeks of gestation.
Which test should the nurse perform at least every two weeks to assess the fetal growth and oxygenation?
Explanation
A biophysical profile is a test that combines a nonstress test with an ultrasound to assess the fetal well-being and oxygenation.A biophysical profile evaluates five parameters: fetal breathing movements, fetal body movements, fetal tone, amniotic fluid volume, and fetal heart rate reactivity.
Each parameter is scored 0 or 2, and the total score ranges from 0 to 10.A score of 8 to 10 is considered normal, indicating adequate oxygenation and low risk of asphyxia.
Choice A is wrong because a nonstress test is a test that measures the fetal heart rate response to fetal movements.It does not assess the fetal growth or oxygenation directly.
Choice C is wrong because an amniocentesis is a test that involves inserting a needle into the amniotic sac to obtain a sample of amniotic fluid for genetic or biochemical analysis.It does not assess the fetal growth or oxygenation directly.
Choice D is wrong because an umbilical artery doppler is a test that uses ultrasound to measure the blood flow in the umbilical artery.
It can detect placental insufficiency or fetal growth restriction.
A nurse is reviewing the laboratory results of a client with mild pre-eclampsia who is at 30 weeks of gestation.
Which finding should the nurse report to the provider immediately?
Explanation
Serum creatinine of 1.2 mg/dL.This indicates impaired kidney function, which is a serious complication of pre-eclampsia and should be reported to the provider immediately.
Choice A is wrong because a platelet count of 150,000/mm3 is within the normal range (150,000-400,000/mm3) and does not indicate a problem.
Choice C is wrong because a serum uric acid of 6 mg/dL is also within the normal range (2.4-6.0 mg/dL for women) and does not indicate a problem.
Choice D is wrong because a serum albumin of 3.5 g/dL is slightly below the normal range (3.5-5.0 g/dL), but not significantly enough to cause concern.Albumin levels can decrease due to various factors, such as malnutrition, inflammation, or fluid overload.
A nurse is preparing to administer antihypertensive medication to a client with mild pre-eclampsia who is at 34 weeks of gestation.
The nurse should avoid giving which medication to the client?
Explanation
Enalapril is an angiotensin-converting enzyme (ACE) inhibitor that can cause fetal renal damage and oligohydramnios.It should be avoided in pregnancy, especially in the second and third trimesters.
Choice A is wrong because methyldopa is a centrally acting antihypertensive drug that is safe and effective for treating mild to moderate hypertension in pregnancy.
Choice B is wrong because nifedipine is a calcium channel blocker that can lower blood pressure and prevent seizures in women with severe pre-eclampsia.
Choice C is wrong because hydralazine is a vasodilator that can reduce blood pressure and prolong pregnancy in women with severe pre-eclampsia.
A nurse is preparing to administer corticosteroids to a client with HELLP syndrome who is 32 weeks pregnant.
What is the rationale for this intervention?
Explanation
To accelerate fetal lung maturity.This is because corticosteroids are given to pregnant women with HELLP syndrome who are at risk of preterm delivery to help the lungs of the fetus to mature and prevent respiratory distress syndrome.
According to the health search result from Focus Medica, HELLP syndrome is a life-threatening condition that occurs in pregnant women or soon after delivery.This can cause high blood pressure, seizures, stroke or liver rupture.
Choice A is wrong because corticosteroids do not reduce inflammation in the liver, but rather increase the risk of liver injury by elevating liver enzymes.
Choice C is wrong because corticosteroids do not increase maternal blood pressure, but rather decrease it by acting as antihypertensives.
Choice D is wrong because corticosteroids do not prevent fetal growth restriction, but rather may cause it by reducing placental blood flow and fetal nutrition.
A nurse is monitoring a client with HELLP syndrome for signs of magnesium toxicity.
Which of the following assessments would indicate the need for calcium gluconate as an antidote?
Explanation
Loss of reflexes.This is because magnesium toxicity can cause neuromuscular blockade and respiratory depression, which can be reversed by calcium gluconate as an antidote.
Choice B.Brisk tendon reflexes is wrong because magnesium toxicity usually causes diminished or absent reflexes.
Choice C.Hypertension is wrong because magnesium toxicity usually causes hypotension.
Choice D. Proteinuria is wrong because magnesium toxicity does not affect urine protein levels.Proteinuria is a sign of preeclampsia, not magnesium toxicity.
A nurse is planning care for a client with HELLP syndrome who has signs of severe anemia, coagulopathy, and bleeding.
Which of the following interventions should the nurse anticipate?
No explanation
Intrapartum Management
A nurse is caring for a client with pre-eclampsia who is receiving magnesium sulfate intravenously.
Which of the following assessments is the most important for the nurse to monitor?
Explanation
Deep tendon reflexes are important to monitor because they indicate the level of neuromuscular irritability caused by magnesium sulfate therapy.Magnesium sulfate is a mineral that reduces seizure risks in women with preeclampsia.A healthcare provider will give the medication intravenously.If the deep tendon reflexes are absent or diminished, it may indicate magnesium toxicity, which can cause respiratory depression, cardiac arrest, and coma.
Other statement options:
•
A. Blood pressure: Blood pressure is a major sign of preeclampsia, but it is not the most important assessment to monitor when receiving magnesium sulfate therapy.Blood pressure may be controlled by other antihypertensive medications.
•
C. Fetal heart rate: Fetal heart rate is important to monitor for fetal well-being, but it is not directly affected by magnesium sulfate therapy.Fetal heart rate may be monitored by nonstress test or biophysical profile.
•
D. Urine output: Urine output is important to monitor for kidney function, but it is not the most important assessment to monitor when receiving magnesium sulfate therapy.Urine output may be measured by urine analysis or 24-hour urine sample.
Normal ranges:
• Blood pressure: less than 140/90 mm Hg
• Deep tendon reflexes: 2+ (normal) or 3+ (brisk) on a scale of 0 to 4
• Fetal heart rate: 110 to 160 beats per minute
• Urine output: at least 30 mL per hour
A client with eclampsia has a seizure during labor.
Which of the following actions should the nurse take first?
Explanation
Turn the client to the side.This is because turning the client to the side will prevent aspiration and maintain a patent airway, which is the priority intervention for a client who has a seizure.
Some possible explanations for the other choices are:
• Choice B. Administer oxygen via face mask.
This is not the first action because oxygen administration alone will not prevent aspiration or ensure a patent airway.Oxygen may be given after turning the client to the side and assessing the respiratory status.
• Choice C. Give additional magnesium sulfate.
This is not the first action because magnesium sulfate is used to prevent seizures in clients with eclampsia, not to treat them once they occur.Magnesium sulfate may be given after stabilizing the client and checking the serum magnesium level, which should be between 4 to 7 mg/dL (3.3 to 5.8 mEq/L) for therapeutic effect.
• Choice D. Document the duration and characteristics of the seizure.
This is not the first action because documentation is important but not urgent in this situation.The nurse should document the seizure after providing immediate care and notifying the provider.
A nurse is preparing to administer hydralazine to a client with pre-eclampsia who has a blood pressure of 170/112 mmHg.
Which of the following parameters should the nurse monitor before and after giving the medication? (Select all that apply.)
Explanation
Hydralazine is a medication that lowers blood pressure by relaxing the blood vessels.It is used to treat hypertension in pre-eclampsia, a condition that causes high blood pressure and proteinuria in pregnant women.Hydralazine can cause side effects such as palpitations, tachycardia, chest pain, and headache.
Therefore, the nurse should monitor the heart rate before and after giving the medication to assess the effectiveness and safety of the treatment.
Choice B. Respiratory rate is wrong because hydralazine does not affect the respiratory system directly.However, if the blood pressure is too low, it can cause difficulty breathing or shortness of breath.
This is a sign of hypotension or shock and requires immediate medical attention.
Choice C. Temperature is wrong because hydralazine does not cause fever or affect the body temperature.However, some people may experience a feeling of warmth or flushing after taking hydralazine.
This is a normal reaction and does not indicate a problem.
Choice D. Oxygen saturation is wrong because hydralazine does not affect the oxygen level in the blood.
However, if the blood pressure is too low, it can cause decreased blood flow to the vital organs, which can lead to hyp
A nurse is reviewing the laboratory results of a client with pre-eclampsia who is scheduled for induction of labor.
Which of the following findings indicates a risk for disseminated intravascular coagulation (DIC)?
Explanation
D-dimer level of 0.8 mcg/mL.
D-dimer is a protein fragment that is produced when a blood clot dissolves.A high level of D-dimer indicates a risk for disseminated intravascular coagulation (DIC), a condition in which blood clots form throughout the body and block blood flow to vital organs.
Choice A is wrong because platelet count of 150,000/mm3 is within the normal range for adults, which is between 150,000 and 450,000 platelets/mcL.Platelet count may decrease in DIC due to excessive clotting and consumption of platelets.
Choice B is wrong because fibrinogen level of 300 mg/dL is within the normal range for adults, which is between 200 and 400 mg/dL.
Fibrinogen is a protein that helps blood clotting.Fibrinogen level may increase in DIC due to inflammation and tissue injury.
Choice C is wrong because prothrombin time of 15 seconds is within the normal range for adults, which is between 11 and 13.5 seconds.
Prothrombin time measures how long it takes for blood to clot.Prothrombin time may increase in DIC due to depletion of clotting factors.
A nurse is teaching a client with pre-eclampsia about the signs and symptoms of magnesium toxicity.
Which of the following statements by the client indicates a need for further teaching?
Explanation
“I should not worry if I do not feel my baby move as much as before.” This statement indicates a need for further teaching because decreased fetal movement is a sign of fetal distress and should be reported to the nurse immediately.
Magnesium toxicity can affect the fetal central nervous system and cause hypotonia and reduced activity.
Choice A is wrong because difficulty breathing is a sign of magnesium toxicity and should be reported to the nurse.
Magnesium can depress the respiratory system and cause respiratory failure.
Choice B is wrong because warmth and flushing are common side effects of magnesium infusion and do not indicate toxicity.
They are caused by the vasodilatory effect of magnesium on the blood vessels.
Choice C is wrong because blurred vision and headache are signs of severe pre-eclampsia and should be reported to the nurse.
They indicate increased blood pressure and possible cerebral edema.
Postpartum Management
A nurse is caring for a client who has postpartum pre-eclampsia.
Which of the following interventions should the nurse include in the plan of care? Select all that apply.
Explanation
The correct answer is choice B and E. The nurse should administer magnesium sulfate as prescribed and provide health education and counselling on the signs and symptoms of postpartum pre-eclampsia.
Choice A is wrong because the nurse should monitor blood pressure more frequently than every 4 hours, preferably every 15 minutes until stable, then every hour.
Choice C is wrong because the nurse should avoid early ambulation and mobilization, as they can increase blood pressure and risk of seizures.
Choice D is wrong because breastfeeding is not contraindicated in postpartum pre-eclampsia, unless the mother is taking antihypertensive medication that is not compatible with breastfeeding.
Postpartum pre-eclampsia is a rare condition that occurs when a woman has high blood pressure and protein in her urine or other signs of organ damage after giving birth.It can lead to serious complications such as seizures, stroke, kidney failure, and death if not treated promptly.Normal blood pressure ranges are less than 120/80 mm Hg for systolic and diastolic pressures respectively.
A nurse is reviewing the laboratory results of a client who has postpartum pre-eclampsia.
Which of the following findings should the nurse report to the provider?
Explanation
Serum uric acid of 8 mg/dL.This is because postpartum preeclampsia is a condition that causes high blood pressure and excess protein in the urine after childbirth.It can also affect other organs such as the liver and kidneys.One of the signs of kidney impairment is elevated serum uric acid levels.Normal serum uric acid levels range from 2.4 to 6 mg/dL for women.
Choice A is wrong because platelet count of 150,000/mm3 is within the normal range of 150,000 to 450,000/mm3.
Platelets are the cells that help blood clot.A low platelet count can indicate a risk of bleeding complications.
Choice B is wrong because serum creatinine of 1.2 mg/dL is within the normal range of 0.6 to 1.3 mg/dL for women.
Creatinine is a waste product that is filtered by the kidneys.A high serum creatinine level can indicate kidney dysfunction.
Choice D is wrong because serum albumin of 4 g/dL is within the normal range of 3.4 to 5.4 g/dL.
Albumin is a protein that helps regulate fluid balance in the body.A low serum albumin level can indicate liver damage or fluid leakage from blood vessels.
A nurse is teaching a client who has postpartum pre-eclampsia about the potential effects of this condition on future pregnancies.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
“I will have a higher risk of having pre-eclampsia or eclampsia in my next pregnancy.” This statement indicates an understanding of the teaching because postpartum pre-eclampsia is a rare condition that occurs when you have high blood pressure and excess protein in your urine soon after childbirth.It increases the risk of developing preeclampsia or gestational hypertension in subsequent pregnancies.Preeclampsia is a serious condition of high blood pressure during pregnancy that can cause complications for the mother and the baby.
Choice A is wrong because aspirin is not a treatment for postpartum pre-eclampsia, but a preventive measure for preeclampsia during pregnancy in women who are at high risk for it.Aspirin may reduce the risk of preeclampsia and related complications by inhibiting platelet aggregation and inflammation.However, aspirin may not work for women with chronic hypertension.
Choice B is wrong because postpartum pre-eclampsia does not affect the risk of developing gestational diabetes in the next pregnancy.
Gestational diabetes is a condition where the blood sugar level becomes too high during pregnancy due to hormonal changes and insulin resistance.
The risk factors for gestational diabetes include obesity, family history of diabetes, previous history of gestational diabetes, polycystic ovary syndrome, and certain ethnic groups.
Choice C is wrong because postpartum pre-eclampsia does not require a cesarean delivery for the next pregnancy.
Cesarean delivery is a surgical procedure
A nurse is assessing a client who has postpartum pre-eclampsia and is receiving magnesium sulfate intravenously.
Which of the following findings should alert the nurse to suspect magnesium toxicity?
Explanation
Respiratory rate of 10/min.This is because a decreased respiratory rate is a sign of magnesium toxicity, which can occur when a client receives magnesium sulfate intravenously to treat pre-eclampsia.Magnesium sulfate can depress the central nervous system and affect the respiratory center in the brain.
Choice B is wrong because urine output of 40 mL/hour is normal for a postpartum client and does not indicate magnesium toxicity.
Choice C is wrong because deep tendon reflexes of 2+ are normal and do not indicate magnesium toxicity.Magnesium toxicity can cause loss of deep tendon reflexes or hyporeflexia.
Choice D is wrong because serum magnesium level of 6 mg/dL is within the therapeutic range of 4 to 7 mg/dL for a client receiving magnesium sulfate.Magnesium toxicity can occur when the serum magnesium level exceeds 8 mg/dL.
A nurse is preparing to administer an antihypertensive medication to a client who has postpartum pre-eclampsia.
Which of the following medications should the nurse have available as an antidote in case of an adverse reaction?
Explanation
Sodium nitroprusside.
This is an antihypertensive medication that can lower blood pressure rapidly and can cause hypotension, cyanide toxicity, or thiocyanate toxicity as adverse reactions.The antidote for sodium nitroprusside toxicity is sodium thiosulfate, which can be administered intravenously.
Choice A is wrong because naloxone is an antidote for opioid overdose, not antihypertensive medication.
Choice B is wrong because flumazenil is an antidote for benzodiazepine overdose, not antihypertensive medication.
Choice D is wrong because sodium bicarbonate is an antidote for acidosis, not antihypertensive medication.
Complications and Outcomes
A nurse is caring for a client with severe pre-eclampsia who is receiving magnesium sulfate infusion.
What is the rationale for administering this medication?
Explanation
To prevent seizures.Magnesium sulfate is given prophylactically to prevent seizures in clients with severe preeclampsia.Seizures are a sign of eclampsia, which is a life-threatening complication of preeclampsia.
Choice B is wrong because magnesium sulfate does not lower blood pressure.Some antihypertensive drugs might be given to manage blood pressure in clients with preeclampsia.
Choice C is wrong because magnesium sulfate does not increase urine output.In fact, it can cause oliguria or renal failure as adverse effects.
Choice D is wrong because magnesium sulfate does not improve placental perfusion.It may actually decrease placental blood flow and cause fetal distress.Delivery of the baby is the only cure for preeclampsia.
A nurse is reviewing the laboratory results of a client with eclampsia who has developed disseminated intrasvascular coagulation (DIC).
What findings would the nurse expect to see? Select all that apply.
Explanation
The correct answer is choice A, C and E. A client with eclampsia who has developed disseminated intravascular coagulation (DIC) would have decreased platelet count, prolonged prothrombin time (PT) and prolonged activated partial thromboplastin time (aPTT).These findings indicate that the client has excessive clotting and bleeding due to the consumption of clotting factors and platelets.
Choice B is wrong because increased fibrinogen level is not a sign of DIC.
Fibrinogen is a precursor of fibrin, which forms the meshwork of clots.In DIC, fibrinogen is converted to fibrin and then degraded by fibrinolysis, resulting in decreased fibrinogen level.
Choice D is wrong because decreased fibrin degradation products (FDPs) or D-dimer are not a sign of DIC.
FDPs or D-dimer are fragments of fibrin that are released when clots are broken down by fibrinolysis.
A nurse is assessing a client with mild pre-eclampsia at 34 weeks of gestation.
What signs and symptoms would indicate worsening of the condition? Select all that apply.
Explanation
The correct answer is choices A, B and C.These are signs and symptoms of severe preeclampsia that indicate worsening of the condition and require immediate medical attention.
Choice A is correct because a headache that does not respond to acetaminophen may indicate increased intracranial pressure due to cerebral edema.
Choice B is correct because blurred vision or scotoma (spots in the visual field) may indicate retinal damage or detachment due to hypertension.
Choice C is correct because epigastric pain or right upper quadrant pain may indicate liver ischemia or rupture due to vasospasm and edema.
Choice D is wrong because weight gain of 2 lbs in one week is normal for a pregnant woman at 34 weeks of gestation.Weight gain of more than 4 lbs in one week should be reported to the physician.
Choice E is wrong because swelling of the ankles and feet is common in pregnancy and does not necessarily indicate preeclampsia.Swelling of the face, eyes, or hands should be reported to the physician.
A nurse is preparing to administer an antihypertensive medication to a client with severe pre-eclampsia.
What blood pressure parameters should the nurse aim for?
Explanation
Systolic < 160 mmHg and diastolic < 110 mmHg.This is the blood pressure goal for a client with severe pre-eclampsia who is receiving antihypertensive medication.
The goal is to lower the blood pressure enough to prevent maternal complications such as stroke, seizure, or organ damage, but not too much to compromise fetal perfusion.
Choice A is wrong because systolic < 120 mmHg and diastolic < 80 mmHg are the normal blood pressure ranges for a healthy adult.
This goal is too low for a client with severe pre-eclampsia and may cause fetal hypoxia.
Choice B is wrong because systolic < 140 mmHg and diastolic < 90 mmHg are the blood pressure ranges for a client with mild hypertension.
This goal is also too low for a client with severe pre-eclampsia and may not prevent maternal complications.
Choice D is wrong because systolic < 180 mmHg and diastolic < 120 mmHg are the thresholds for initiating antihypertensive therapy in a client with severe pre-eclampsia.
This goal is too high for a client who is already receiving antihypertensive medication and may not adequately lower the blood pressure.
A nurse is educating a client with pre-eclampsia about the importance of fetal kick counts.
How many fetal movements should the client report in one hour?
Explanation
At least 6 fetal movements should be reported in one hour.
This is because fetal kick counts are a way to monitor the fetus’s health and well-being.A decrease in fetal movements may indicate fetal distress or problems with the placenta.Pre-eclampsia is a condition that affects the blood pressure and the kidneys of the pregnant person and can cause complications for both the person and the fetus.
Choice A is wrong because at least 2 fetal movements in one hour is too low and may suggest a lack of oxygen and nutrients to the fetus.
Choice B is wrong because at least 4 fetal movements in one hour is also too low and may indicate a problem with the pregnancy.
Choice D is wrong because at least 8 fetal movements in one hour is higher than the recommended minimum and may not be realistic for some fetuses.
Exams on Pre-eclampsia, Eclampsia
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Fetal Complications
- More Questions on this Topic
- Sample SubTopic
- Objectives
- Introduction
- Risk Factors
- Clinical Features
- HELLP Syndrome
- Diagnostic Criteria and Investigations
- Management Principles and Nursing Interventions
- Intrapartum Management
- Postpartum Management
- Complications and Outcomes
- Summary
Notes Highlighting is available once you sign in. Login Here.
Objectives
By the end of this note, you should be able to:
- Define pre-eclampsia and eclampsia and explain their pathophysiology
- Identify the risk factors and clinical features of pre-eclampsia and eclampsia
- Describe the diagnostic criteria and investigations for pre-eclampsia and eclampsia
- Outline the management principles and nursing interventions for pre-eclampsia and eclampsia
- Recognize the complications and outcomes of pre-eclampsia and eclampsia for the mother and the baby
- Provide health education and counselling for women with pre-eclampsia and eclampsia
- Apply critical thinking and clinical reasoning skills to case scenarios involving pre-eclampsia and eclampsia
Introduction
Pre-eclampsia is a pregnancy-specific condition characterized by new-onset hypertension and proteinuria after 20 weeks of gestation or during the postpartum period in a previously normotensive client. Hypertension is defined as a systolic blood pressure (SBP) of 140 mmHg or higher or a diastolic blood pressure (DBP) of 90 mmHg or higher on two occasions at least four hours apart. Proteinuria is defined as a urinary protein excretion of 300 mg or more in 24 hours or a urine protein-to-creatinine ratio of 0.3 or more. Pre-eclampsia can be classified as mild or severe based on the severity of hypertension, proteinuria, and other signs and symptoms.
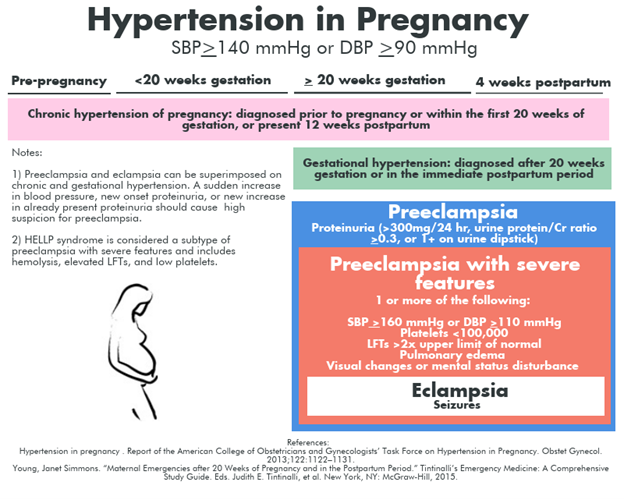
Eclampsia is when a client with pre-eclampsia develops generalized seizures that are not attributable to other causes. Eclampsia can occur before, during, or after delivery.
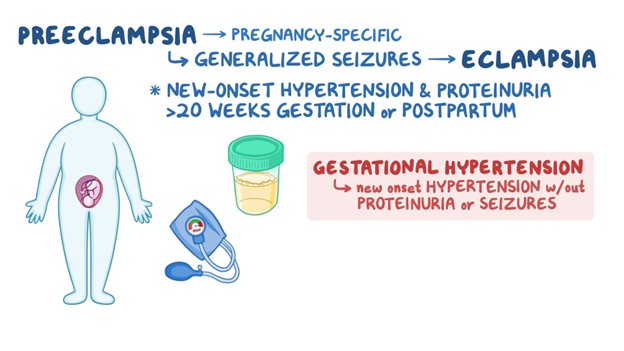
Pre-eclampsia and eclampsia are serious complications of pregnancy that can affect both the mother and the baby. They are part of a spectrum of hypertensive disorders of pregnancy that also include gestational hypertension, chronic hypertension, and chronic hypertension with superimposed pre-eclampsia.
The exact cause of pre-eclampsia and eclampsia is unknown, but it is thought to involve abnormal placentation, endothelial dysfunction, inflammation, oxidative stress, and genetic factors. The placenta is a temporary organ that develops in the uterus during pregnancy, and connects the pregnant client with the fetus. It provides oxygen and nutrients to the fetus and removes waste products from the fetal blood. The placenta is attached to the uterine wall by spiral arteries that dilate during pregnancy to increase blood flow to the placenta. In pre-eclampsia, there is incomplete remodeling of the spiral arteries, resulting in reduced placental perfusion and hypoxia. This triggers the release of placental factors that cause widespread endothelial damage, vasoconstriction, increased vascular permeability, platelet aggregation, coagulation activation, and oxidative stress. These changes lead to multi-organ dysfunction and increased risk of maternal and fetal morbidity and mortality.
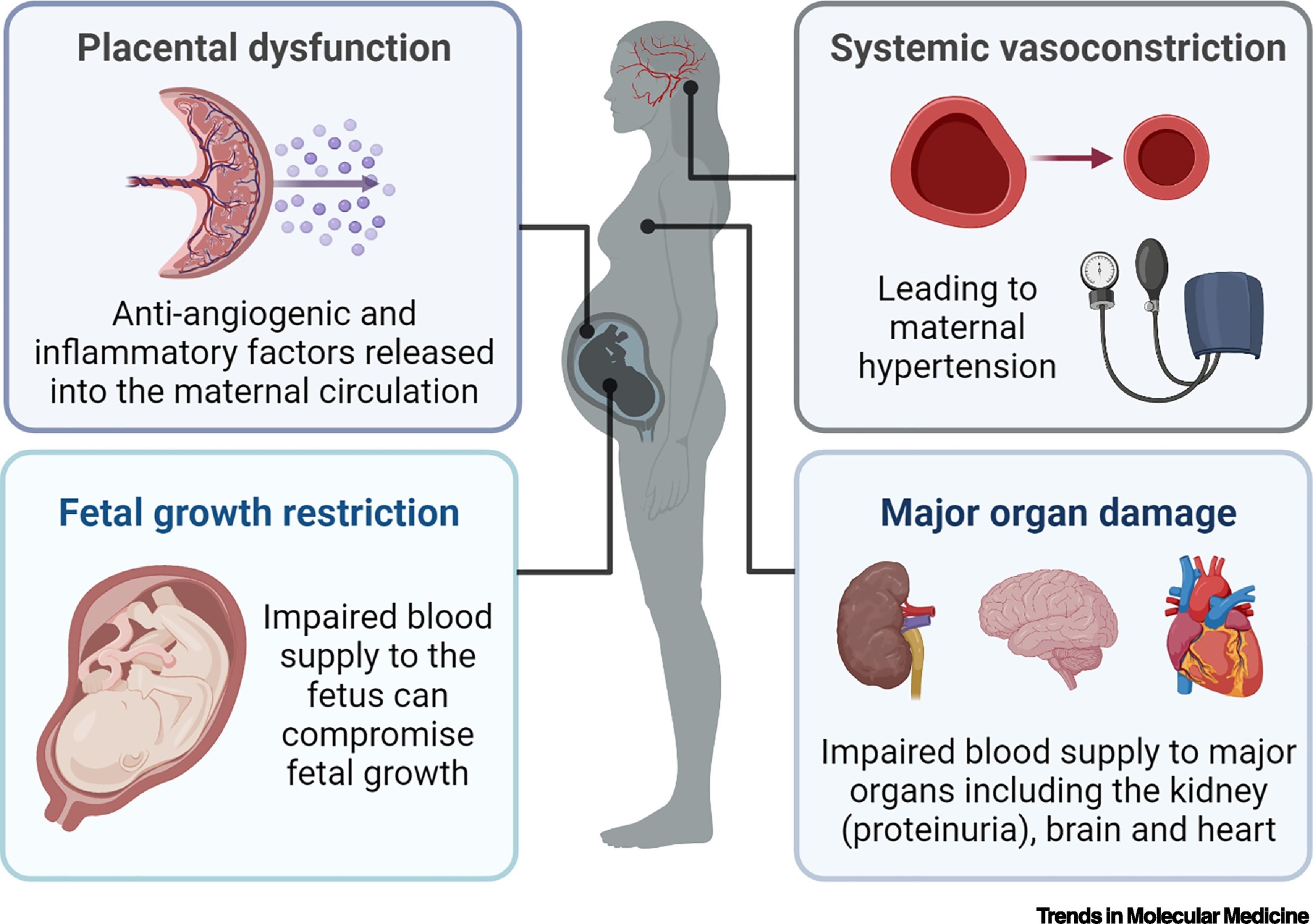 Questions
Questions
Risk Factors
Some factors that increase the risk of developing pre-eclampsia and eclampsia include:
- Nulliparity (first pregnancy)
- Multiple gestation (twins, triplets, etc.)
- Maternal age <20 years or >35 years
- Obesity (body mass index >30 kg/m2)
- Pre-existing medical conditions (e.g., chronic hypertension, diabetes mellitus, renal disease, autoimmune disease)
- History of pre-eclampsia or eclampsia in previous pregnancy or family history
- Pregnancy interval >10 years
- Assisted reproductive technology (e.g., in vitro fertilization)
- Placental abnormalities (e.g., molar pregnancy, placenta previa)
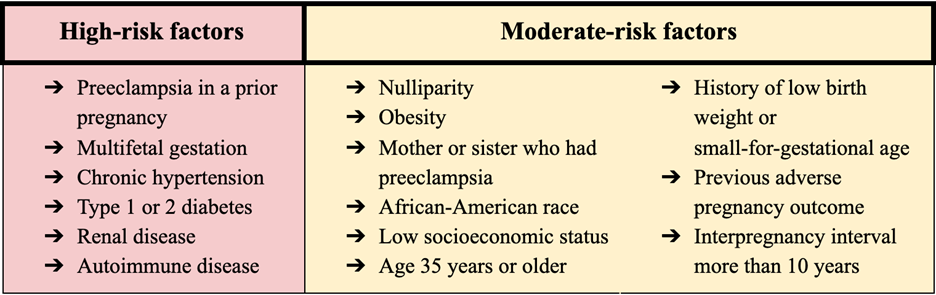
Clinical Features
The clinical features of pre-eclampsia and eclampsia vary depending on the severity of the condition and the organs involved. Some common signs and symptoms include:
Mild pre-eclampsia
Mild Pre-eclampsia
- SBP 140-159 mmHg or DBP 90-109 mmHg on two occasions at least four hours apart
- Proteinuria ≥300 mg/24 hours or urine protein-to-creatinine ratio ≥0.3
- Edema (swelling) of the face, hands, or feet
- Weight gain >0.5 kg/week
- Headache
- Visual disturbances (e.g., blurred vision, flashes, spots)
- Nausea or vomiting
- Epigastric pain or right upper quadrant pain
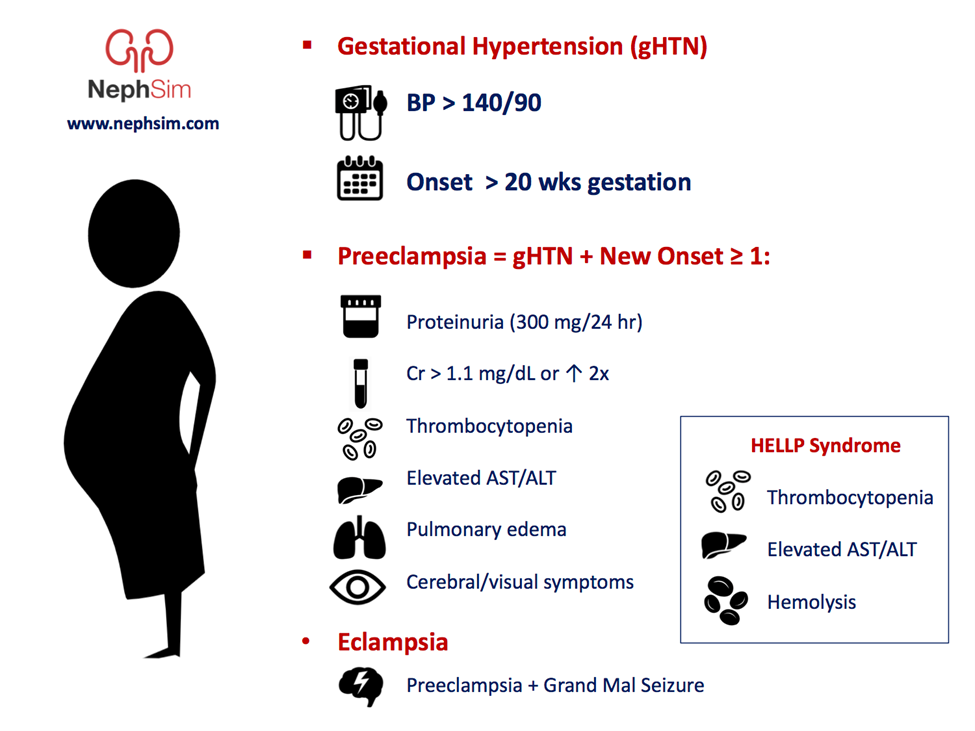
Severe pre-eclampsia
Severe Pre-eclampsia
- SBP ≥160 mmHg or DBP ≥110 mmHg on two occasions at least four hours apart
- Proteinuria ≥5 g/24 hours or urine protein-to-creatinine ratio ≥3.5
- Oliguria (<500 mL/24 hours)
- Serum creatinine >1.2 mg/dL
- Thrombocytopenia (<100 x 10^9/L)
- Elevated liver enzymes (aspartate aminotransferase [AST] or alanine aminotransferase [ALT] >70 U/L)
- Hemolysis (elevated lactate dehydrogenase [LDH] >600 U/L)
- Pulmonary edema (shortness of breath, crackles on auscultation)
- Cerebral edema (severe headache, altered mental status)
- Hyperreflexia (increased deep tendon reflexes) with clonus (rhythmic muscle contractions)
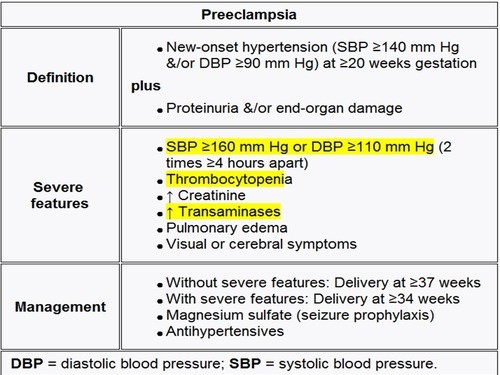
Eclampsia
Eclampsia
- Generalized tonic-clonic seizures lasting 15 seconds to 2 minutes
- Postictal state (confusion, drowsiness, amnesia) lasting up to 30 minutes
HELLP Syndrome
HELLP Syndrome
HELLP syndrome is a severe variant of pre-eclampsia that involves hemolysis (H), elevated liver enzymes (EL), and low platelets (LP). It occurs in about 10% of clients with severe pre-eclampsia. It can present with similar signs and symptoms as severe pre-eclampsia, but may also include:
- Jaundice (yellowing of the skin and eyes)
- Anemia (pallor, fatigue, weakness)
- Bleeding tendencies (petechiae, ecchymoses, epistaxis)
- Hematuria (blood in urine)
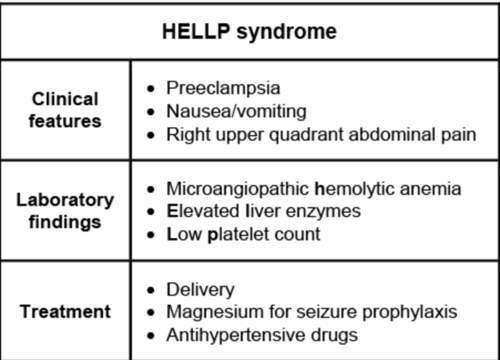
Diagnostic Criteria and Investigations
Diagnostic Criteria and Investigations
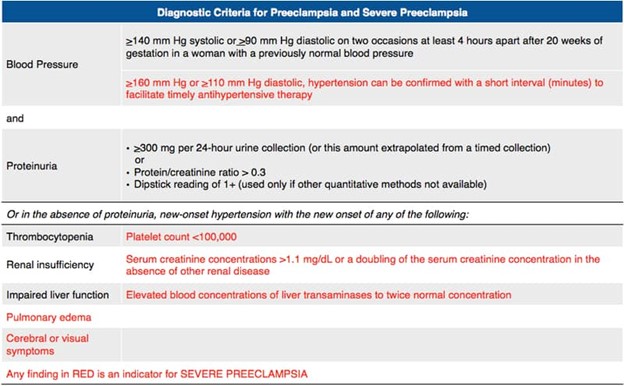
The diagnosis of pre-eclampsia is based on clinical findings of hypertension and proteinuria after 20 weeks of gestation or during the postpartum period in a previously normotensive client. The diagnosis of eclampsia is based on clinical findings of seizures in a client with pre-eclampsia.
Some investigations that may be performed to confirm the diagnosis and assess the severity of pre-eclampsia and eclampsia include:
Blood Tests
To evaluate renal function:
- Serum creatinine
- Blood urea nitrogen (BUN)
To evaluate liver function:
- AST
- ALT
To evaluate hematologic function:
- Complete blood count (CBC) with differential
- Platelet count
- LDH
To evaluate coagulation function:
- Prothrombin time (PT)
- Partial thromboplastin time (PTT)
- Fibrinogen
To evaluate electrolyte balance:
- Sodium
- Potassium
- Chloride
- Bicarbonate
Urine Tests
To quantify proteinuria:
- 24-hour urine collection for protein excretion
- Urine protein-to-creatinine ratio
To detect hematuria:
- Urinalysis with microscopic examination
Imaging Tests
To assess fetal well-being:
- Ultrasound for fetal growth, amniotic fluid volume, placental location, umbilical artery Doppler flow
- Non-stress test (NST) for fetal heart rate reactivity
- Biophysical profile (BPP) for fetal movement, tone, breathing, heart rate reactivity, amniotic fluid volume
To assess maternal cerebral edema:
- Computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of the head
Management Principles and Nursing Interventions
Management Principles and Nursing Interventions
The only definitive treatment for pre-eclampsia and eclampsia is delivery of the fetus and placenta. However, the timing and mode of delivery depend on several factors such as gestational age, fetal maturity, maternal condition, and availability of resources. The goal is to balance the risks and benefits for both the mother and the baby.
Some general principles for managing pre-eclampsia and eclampsia include:
Antepartum Management: For mild pre-eclampsia
Antepartum Management: For mild pre-eclampsia:
- Monitor blood pressure at least twice weekly
- Monitor urine protein at least weekly
- Monitor fetal growth and well-being at least every two weeks
- Advise bed rest at home or hospitalization depending on maternal-fetal status
- Advise dietary salt
- Advise dietary salt restriction to <5 g/day
- Advise fluid intake of 1.5-2 L/day
- Advise avoidance of alcohol, tobacco, and caffeine
- Advise regular antenatal visits and reporting of any worsening symptoms
- Administer corticosteroids (e.g., betamethasone) if gestational age is <34 weeks to accelerate fetal lung maturity
- Consider antiplatelet therapy (e.g., low-dose aspirin) to reduce the risk of placental thrombosis and improve uteroplacental blood flow
- Consider antihypertensive therapy (e.g., methyldopa, nifedipine, hydralazine, labetalol) if blood pressure is persistently >150/100 mmHg or if there are signs of end-organ damage
- Plan for delivery at 37 weeks of gestation or earlier if maternal-fetal condition deteriorates
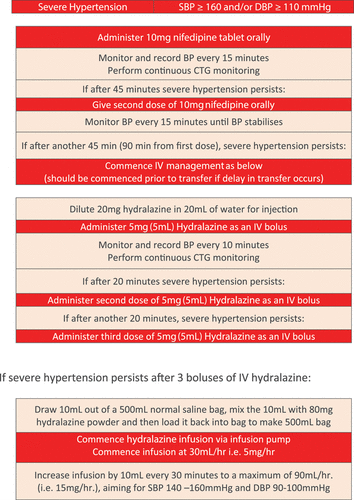
Antepartum Management: For severe pre-eclampsia
Antepartum Management: For severe pre-eclampsia:
- Hospitalize the client and monitor blood pressure, urine output, fetal heart rate, and uterine activity continuously
- Monitor laboratory tests (e.g., serum creatinine, liver enzymes, platelet count, coagulation profile) daily or more frequently as needed
- Administer magnesium sulfate intravenously to prevent seizures and lower blood pressure
- Monitor for magnesium toxicity (e.g., loss of reflexes, reduced urine output, respiratory depression, cardiac arrhythmias) and have calcium gluconate available as an antidote
- Administer antihypertensive therapy (e.g., hydralazine, labetalol) to lower blood pressure to <160/110 mmHg
- Administer corticosteroids (e.g., betamethasone) if gestational age is <34 weeks to accelerate fetal lung maturity
- Plan for delivery as soon as possible after maternal stabilization and fetal maturity assessment
Antepartum Management: For HELLP syndrome
Antepartum Management: For HELLP syndrome:
- Hospitalize the client and monitor blood pressure, urine output, fetal heart rate, and uterine activity continuously
- Monitor laboratory tests (e.g., serum creatinine, liver enzymes, platelet count, coagulation profile) daily or more frequently as needed
- Administer magnesium sulfate intravenously to prevent seizures and lower blood pressure
- Monitor for magnesium toxicity (e.g., loss of reflexes, reduced urine output, respiratory depression, cardiac arrhythmias) and have calcium gluconate available as an antidote
- Administer antihypertensive therapy (e.g., hydralazine, labetalol) to lower blood pressure to <160/110 mmHg
- Administer corticosteroids (e.g., betamethasone) if gestational age is <34 weeks to accelerate fetal lung maturity and improve platelet count
- Consider transfusion of packed red blood cells, fresh frozen plasma, or platelets if there are signs of severe anemia, coagulopathy, or bleeding
- Plan for delivery as soon as possible after maternal stabilization and fetal maturity assessment
Intrapartum Management
Antepartum Management: For eclampsia
Antepartum Management: For eclampsia:
- Protect the client from injury during seizures and maintain a patent airway
- Administer oxygen via face mask at 10 L/min
- Administer magnesium sulfate intravenously to stop seizures and lower blood pressure
- Monitor for magnesium toxicity (e.g., loss of reflexes, reduced urine output, respiratory depression, cardiac arrhythmias) and have calcium gluconate available as an antidote
- Administer antihypertensive therapy (e.g., hydralazine, labetalol) to lower blood pressure to <160/110 mmHg
- Administer corticosteroids (e.g., betamethasone) if gestational age is <34 weeks to accelerate fetal lung maturity
- Plan for delivery as soon as possible after maternal stabilization and fetal maturity assessment
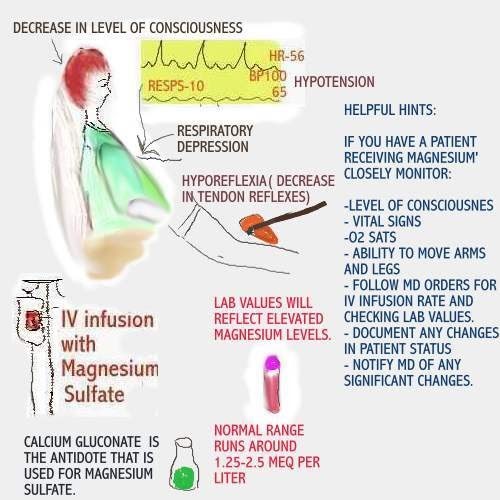
Intrapartum Management
The mode of delivery for clients with pre-eclampsia and eclampsia depends on several factors such as gestational age, fetal presentation, cervical status, maternal condition, and availability of resources. The goal is to achieve a safe vaginal delivery whenever possible.
Some general principles for managing pre-eclampsia and eclampsia during labor and delivery include
- Maintain intravenous access and administer fluids cautiously to avoid fluid overload
- Monitor vital signs, urine output, fetal heart rate, and uterine activity frequently
- Administer magnesium sulfate intravenously to prevent seizures and lower blood pressure
- Monitor for magnesium toxicity (e.g., loss of reflexes, reduced urine output, respiratory depression, cardiac arrhythmias) and have calcium gluconate available as an antidote
- Administer antihypertensive therapy (e.g., hydralazine, labetalol) to lower blood pressure to <160/110 mmHg
- Administer oxytocin intravenously to augment labor if indicated and not contraindicated
- Consider induction of labor with prostaglandins or mechanical methods if the cervix is unfavorable for vaginal delivery
- Consider cesarean section if vaginal delivery is not feasible or there are signs of fetal distress or maternal deterioration
- Provide pain relief with epidural anesthesia if possible and not contraindicated
- Provide emotional support and reassurance to the client and family
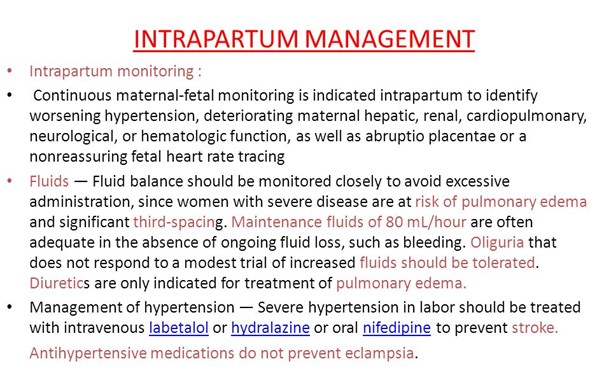
Postpartum Management
Postpartum Management
The risk of complications from pre-eclampsia and eclampsia does not end with delivery. Some clients may develop postpartum pre-eclampsia or eclampsia, which can occur up to six weeks after delivery. Therefore, close monitoring and follow-up care are essential for these clients.
Some general principles for managing pre-eclampsia and eclampsia in the postpartum period include:
- Monitor blood pressure, urine output, neurological status, and laboratory tests daily or more frequently as needed
- Continue magnesium sulfate intravenously for 24 hours after delivery or the last seizure, whichever is later
- Continue antihypertensive therapy (e.g., methyldopa, nifedipine, hydralazine, labetalol) until blood pressure is stable below 140/90 mmHg
- Encourage early ambulation and mobilization to prevent thromboembolism
- Promote breastfeeding if possible and not contraindicated
- Provide health education and counselling on the following topics:
- The signs and symptoms of postpartum pre-eclampsia or eclampsia and when to seek medical attention
- The importance of regular blood pressure monitoring and follow-up visits
- The potential effects of pre-eclampsia or eclampsia on future pregnancies and the need for preconception counselling
- The possible impact of pre-eclampsia or eclampsia on mental health and well-being and the availability of support resources
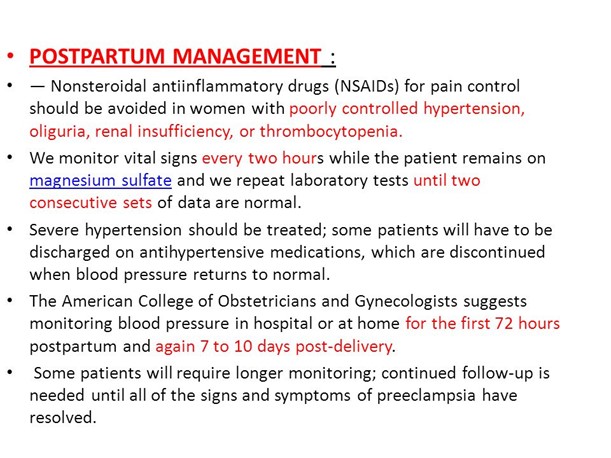
Complications and Outcomes
Complications and Outcomes
Pre-eclampsia and eclampsia can have serious consequences for both the mother and the baby. Some of the possible complications include:
Maternal complications
Maternal Complications
- Stroke (cerebrovascular accident)
- Intracranial hemorrhage
- Retinal detachment
- Pulmonary edema
- Acute respiratory distress syndrome (ARDS)
- Acute kidney injury (AKI)
- Hepatic rupture or infarction
- Disseminated intravascular coagulation (DIC)
- Placental abruption (premature separation of the placenta from the uterine wall)
- Maternal death
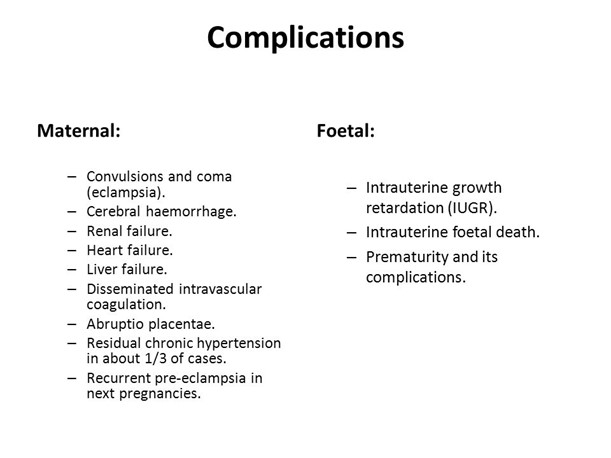
Fetal complications
Fetal Complications
- Intrauterine growth restriction (IUGR)
- Oligohydramnios (reduced amniotic fluid volume)
- Fetal hypoxia or acidosis
- Fetal distress or demise
- Preterm birth
- Neonatal intensive care unit (NICU) admission
- Perinatal death
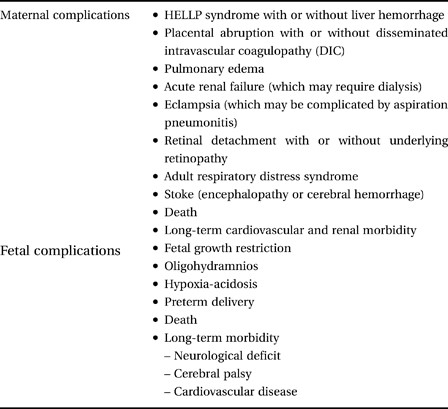
Conclusion
The outcomes of pre-eclampsia and eclampsia depend on several factors such as gestational age, severity of the condition, response to treatment, and availability of resources. The prognosis is generally better if the condition is detected early and managed appropriately. Most clients recover fully within six weeks after delivery. However, some clients may have long-term sequelae such as chronic hypertension, renal impairment, cardiovascular disease, or psychological distress. Similarly, some babies may have long-term complications such as neurodevelopmental delay, cerebral palsy, or learning disabilities.
Summary
- Pre-eclampsia is a pregnancy-specific condition characterized by new-onset hypertension and proteinuria after 20 weeks of gestation or during the postpartum period in a previously normotensive client.
- Eclampsia is when a client with pre-eclampsia develops generalized seizures that are not attributable to other causes.
- Pre-eclampsia and eclampsia are part of a spectrum of hypertensive disorders of pregnancy that also include gestational hypertension, chronic hypertension, and chronic hypertension with superimposed pre-eclampsia.
- The exact cause of pre-eclampsia and eclampsia is unknown, but it is thought to involve abnormal placentation, endothelial dysfunction, inflammation, oxidative stress, and genetic factors.
- The clinical features of pre-eclampsia and eclampsia vary depending on the severity of the condition and the organs involved. Some common signs and symptoms include headache, visual disturbances, epigastric pain, edema, oliguria, thrombocytopenia, elevated liver enzymes, hemolysis, pulmonary edema, cerebral edema, hyperreflexia with clonus, and seizures.
- The diagnosis of pre-eclampsia is based on clinical findings of hypertension (>140/90 mmHg)and proteinuria (>300 mg/24 hours) after 20 weeks of gestation or during the postpartum period in a previously normotensive client.
- The diagnosis of eclampsia is based on clinical findings of seizures in a client with pre-eclampsia.
- Some investigations that may be performed to confirm the diagnosis and assess the severity of pre-eclampsia
- Some investigations that may be performed to confirm the diagnosis and assess the severity of pre-eclampsia and eclampsia include blood tests (e.g., serum creatinine, liver enzymes, platelet count, coagulation profile), urine tests (e.g., 24-hour urine collection for protein excretion, urine protein-to-creatinine ratio), and imaging tests (e.g., ultrasound for fetal growth and well-being, CT or MRI scan for maternal cerebral edema).
- The only definitive treatment for pre-eclampsia and eclampsia is delivery of the fetus and placenta. However, the timing and mode of delivery depend on several factors such as gestational age, fetal maturity, maternal condition, and availability of resources. The goal is to balance the risks and benefits for both the mother and the baby.
- Some general principles for managing pre-eclampsia and eclampsia include antepartum management (e.g., monitoring blood pressure and urine protein, advising bed rest or hospitalization, administering corticosteroids, antiplatelet therapy, or antihypertensive therapy), intrapartum management (e.g., maintaining intravenous access and administering fluids cautiously, monitoring vital signs and fetal heart rate, administering magnesium sulfate, antihypertensive therapy, or oxytocin), postpartum management (e.g., monitoring blood pressure and neurological status, continuing magnesium sulfate or antihypertensive therapy, encouraging early ambulation and breastfeeding), and health education and counselling (e.g., informing about the signs and symptoms of postpartum pre-eclampsia or eclampsia, the importance of regular follow-up visits, the potential effects on future pregnancies and mental health).
- Pre-eclampsia and eclampsia can have serious consequences for both the mother and the baby. Some of the possible complications include stroke, intracranial hemorrhage, retinal detachment, pulmonary edema, acute kidney injury, hepatic rupture or infarction, disseminated intravascular coagulation, placental abruption, maternal death, intrauterine growth restriction, oligohydramnios, fetal hypoxia or acidosis, fetal distress or demise, preterm birth, neonatal intensive care unit admission, and perinatal death.
- The outcomes of pre-eclampsia and eclampsia depend on several factors such as gestational age, severity of the condition, response to treatment, and availability of resources. The prognosis is generally better if the condition is detected early and managed appropriately. Most clients recover fully within six weeks after delivery. However, some clients may have long-term sequelae such as chronic hypertension, renal impairment, cardiovascular disease, or psychological distress. Similarly, some babies may have long-term complications such as neurodevelopmental delay, cerebral palsy, or learning disabilities.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Pre-eclampsia, Eclampsia
This filled cannot be empty

