Please set your exam date
Pharmacology of Specific Body Systems
Study Questions
Introduction
A nurse is preparing to administer a beta-blocker to a client with hypertension. Which of the following actions should the nurse prioritize?
Explanation
B) Correct. Beta-blockers primarily affect the heart by decreasing heart rate and contractility. Before administering a beta-blocker, it is essential for the nurse to assess the client's heart rate and rhythm to ensure it is within an appropriate range. This is important because beta-blockers can further slow the heart rate and may be contraindicated in certain conditions, such as bradycardia or heart block.
A) Incorrect. Although checking the client's blood pressure is important, it is not the priority action when administering a beta-blocker.
C) Incorrect. Evaluating renal function is not directly related to the administration of a beta-blocker. However, renal function should be considered in the overall assessment of the client's health status.
D) Incorrect. Monitoring blood glucose levels is not directly related to the administration of a beta-blocker. This action is more relevant for clients with diabetes who are taking medications that can affect blood glucose levels.
A client with heart failure is prescribed digoxin. Which of the following assessment findings would require immediate nursing intervention?
Explanation
A) Correct. Digoxin is a cardiac glycoside, and hypokalemia increases the risk of digoxin toxicity. A serum potassium level of 3.2 mEq/L indicates hypokalemia and requires immediate nursing intervention. Hypokalemia can potentiate the effects of digoxin on cardiac conduction, leading to dysrhythmias.
B) Incorrect. A heart rate of 60 beats per minute is within the expected range for a client taking digoxin, as it is commonly used to control heart rate in certain cardiac conditions.
C) Incorrect. A systolic blood pressure of 100 mmHg may be within an acceptable range for a client with heart failure, depending on their baseline blood pressure and symptoms. It does not require immediate nursing intervention.
D) Incorrect. A digoxin level of 1.2 ng/mL is within the therapeutic range for digoxin. It does not require immediate nursing intervention.
A client who is taking warfarin asks the nurse about consuming foods high in vitamin K. Which of the following statements should the nurse include in the response?
Explanation
B) Correct. Clients taking warfarin should continue to eat foods high in vitamin K, but they should try to keep their intake consistent. Vitamin K plays a role in the synthesis of clotting factors, and warfarin works by inhibiting the action of vitamin K, thereby reducing the blood's ability to clot. Consistent vitamin K intake helps maintain a stable response to warfarin.
A) Incorrect. Avoiding foods high in vitamin K is not necessary, but consistency in vitamin K intake is important.
C) Incorrect. Increasing intake of foods high in vitamin K can counteract the effects of warfarin and increase the risk of blood clots.
D) Incorrect. Consuming unlimited amounts of foods high in vitamin K can interfere with the anticoagulant effects of warfarin and lead to inconsistent therapeutic response.
A nurse is caring for a client receiving intravenous heparin. Which of the following laboratory values should the nurse monitor to assess the client's response to therapy?
Explanation
C) Correct. Heparin primarily affects the intrinsic pathway of the coagulation cascade, and the activated partial thromboplastin time (aPTT) is the laboratory test used to monitor the client's response to heparin therapy. The aPTT provides information about the time it takes for the client's blood to clot and helps determine the appropriate heparin dosage.
A) Incorrect. Prothrombin time (PT) is used to monitor clients receiving warfarin therapy, not heparin.
B) Incorrect. International normalized ratio (INR) is also used to monitor clients receiving warfarin therapy, not heparin.
D) Incorrect. Platelet count is important to monitor for heparin-induced thrombocytopenia (HIT), a potential adverse effect of heparin therapy, but it does not directly assess the client's response to heparin therapy.
A nurse is caring for a client receiving angiotensin-converting enzyme (ACE) inhibitor therapy. Which of the following assessments should the nurse prioritize?
Explanation
B) Correct. ACE inhibitors can cause hyperkalemia as a side effect by inhibiting aldosterone secretion. Therefore, the nurse should prioritize assessing serum potassium levels regularly to monitor for hyperkalemia. This is particularly important in clients with pre-existing renal impairment or those taking other medications that can increase potassium levels.
A) Incorrect. ACE inhibitors do not directly affect blood glucose levels, although they may indirectly influence glycemic control in clients with diabetes.
C) Incorrect. Serum creatinine levels should be monitored regularly in clients receiving ACE inhibitors, as these medications can affect renal function. However, assessing serum potassium levels is a higher priority in this scenario.
D) Incorrect. White blood cell count is not directly related to ACE inhibitor therapy and does not require prioritization in this case.
A client is prescribed statin therapy to manage high cholesterol levels. Which of the following statements by the client indicates a need for further teaching?
Explanation
D) Correct. Statin therapy is usually a lifelong treatment for managing high cholesterol levels. Stopping the medication once cholesterol levels are normal can lead to a rebound increase in cholesterol levels and increase the risk of cardiovascular events. The client should be educated about the importance of continued adherence to statin therapy as prescribed by their healthcare provider.
A) Incorrect. Taking statin medication with the evening meal can optimize its effectiveness, as cholesterol synthesis typically occurs during nighttime.
B) Incorrect. Grapefruit can interfere with the metabolism of certain statins, leading to increased levels of the medication in the body. Therefore, it is important to avoid consuming grapefruit while taking statins.
C) Incorrect. Reporting muscle pain or weakness is crucial because statins can cause muscle-related side effects, including myopathy and rhabdomyolysis. Prompt reporting allows for early intervention or adjustment of the medication if necessary.
A nurse is caring for a client receiving intravenous nitroglycerin. Which of the following assessments should the nurse prioritize?
Explanation
A) Correct. Nitroglycerin is a vasodilator primarily used to reduce angina and improve cardiac blood flow. Monitoring the client's blood pressure is crucial to assess the medication's effectiveness and prevent hypotension, a potential adverse effect. Nitroglycerin can cause significant vasodilation, leading to a drop in blood pressure, and the nurse should closely monitor the client's blood pressure during therapy.
B) Incorrect. Although monitoring respiratory rate is important, it is not the priority assessment when caring for a client receiving intravenous nitroglycerin.
C) Incorrect. Oxygen saturation should be monitored for clients receiving nitroglycerin, but it is not the priority assessment in this scenario.
D) Incorrect. Blood glucose levels are not directly affected by nitroglycerin and do not require prioritization in this case.
Respiratory medications
A nurse is administering a bronchodilator medication to a client with asthma. Which of the following actions should the nurse prioritize?
Explanation
A) Correct. Assessing the client's respiratory status before administering a bronchodilator is essential to evaluate the client's baseline lung function and determine the effectiveness of the medication. This assessment helps the nurse identify any signs of respiratory distress or improvement and guides further interventions.
B) Incorrect. Checking blood glucose levels is not directly related to the administration of a bronchodilator medication.
C) Incorrect. Monitoring urine output is not specifically required for the administration of a bronchodilator medication.
D) Incorrect. Instructing the client to avoid caffeine-containing foods and beverages is not directly related to the administration of a bronchodilator medication. It may be more relevant for clients taking certain respiratory medications, such as methylxanthines like theophylline.
A client with chronic obstructive pulmonary disease (COPD) is prescribed an inhaled corticosteroid. Which of the following instructions should the nurse include when teaching the client about the medication?
Explanation
A) Correct. Instructing the client to rinse their mouth with water after each inhalation is important when using an inhaled corticosteroid. This action helps prevent the development of oral candidiasis (thrush), a potential side effect of inhaled corticosteroids.
B) Incorrect. Inhaled corticosteroids are maintenance medications for COPD and are not intended for use on an as-needed basis during acute exacerbations. Clients should have a separate rescue inhaler for acute symptom relief.
C) Incorrect. The use of a spacer device can improve the delivery of inhaled corticosteroids to the lungs, especially for clients who have difficulty coordinating inhaler use. Therefore, it is recommended to use a spacer device when using an inhaler.
D) Incorrect. Inhaled corticosteroids provide long-term control of symptoms in COPD but do not provide immediate relief. It may take several days to weeks of consistent use for the medication to reach its full therapeutic effect.
A nurse is caring for a client receiving theophylline therapy. Which of the following assessments should the nurse prioritize?
Explanation
B) Correct. Monitoring serum theophylline levels is crucial when caring for a client receiving theophylline therapy. Theophylline has a narrow therapeutic range, and monitoring blood levels helps ensure therapeutic effectiveness while minimizing the risk of toxicity. The nurse should assess the client's theophylline levels regularly and adjust the dosage as necessary.
A) Incorrect. While blood pressure monitoring is important, it is not the priority assessment specifically related to theophylline therapy.
C) Incorrect. Theophylline can affect liver function, but liver function tests are not the priority assessment in this case.
D) Incorrect. Pulmonary function tests are not directly related to theophylline therapy and do not require prioritization in this scenario.
A client is prescribed a metered-dose inhaler (MDI) and a dry powder inhaler (DPI). The client asks the nurse about the difference between the two types of inhalers. Which of the following responses by the nurse is correct?
Explanation
A) Correct. Metered-dose inhalers (MDIs) require the client to coordinate their breathing with inhalation. They release a measured dose of medication in aerosol form, and the client needs to inhale deeply at the same time to ensure the medication reaches the lungs. Dry powder inhalers (DPIs), on the other hand, do not require coordination of breathing and inhalation. The client simply needs to inhale forcefully to activate the powder dispersion.
B) Incorrect. MDIs contain a propellant that helps atomize the medication and facilitate its delivery into the lungs, but this is not the main difference between MDIs and DPIs.
C) Incorrect. DPIs deliver the medication in powder form, not mist form.
D) Incorrect. DPIs do not require the use of a spacer device, unlike MDIs, which can benefit from a spacer device to improve medication delivery.
A nurse is caring for a client who is receiving nebulized albuterol. Which of the following assessments should the nurse prioritize during and after the nebulization treatment?
Explanation
A) Correct. Monitoring the client's heart rate during and after nebulized albuterol treatment is essential. Albuterol is a beta-2 adrenergic agonist that can stimulate the sympathetic nervous system, leading to an increased heart rate (tachycardia). Monitoring the client's heart rate allows the nurse to assess for any potential adverse effects and determine the effectiveness of the medication.
B) Incorrect. Capillary refill time is not directly related to nebulized albuterol treatment and does not require prioritization in this scenario.
C) Incorrect. Bowel sounds are not directly affected by nebulized albuterol and do not require prioritization in this case.
D) Incorrect. Urine output is not directly affected by nebulized albuterol and does not require prioritization in this scenario.
A client with asthma is prescribed a leukotriene receptor antagonist. Which of the following statements by the client indicates a need for further teaching?
Explanation
C) Correct. Leukotriene receptor antagonists are not intended for immediate relief during an asthma attack. They are long-term control medications used to manage and prevent asthma symptoms. Clients should have a separate rescue inhaler for acute symptom relief.
A) Incorrect. Taking the medication on an empty stomach may enhance its absorption, although it can be taken with or without food.
B) Incorrect. Leukotriene receptor antagonists have been associated with mood changes, including depression and suicidal ideation. Therefore, it is important to notify the healthcare provider if any mood changes occur.
D) Incorrect. The client should continue using their other asthma medications as prescribed, as leukotriene receptor antagonists are often used as an adjunct therapy for asthma management.
A nurse is caring for a client receiving oral corticosteroid therapy. Which of the following assessments should the nurse prioritize?
Explanation
A) Correct. Monitoring blood glucose levels is crucial when caring for a client receiving oral corticosteroid therapy. Corticosteroids can increase blood glucose levels and may cause or worsen diabetes mellitus or steroid-induced hyperglycemia. The nurse should monitor the client's blood glucose levels regularly and collaborate with the healthcare team to manage any glucose abnormalities.
B) Incorrect. Oxygen saturation monitoring is important but is not the priority assessment specifically related to oral corticosteroid therapy.
C) Incorrect. Urinary output monitoring is not specifically required for oral corticosteroid therapy and does not require prioritization in this case.
D) Incorrect. Liver function tests are not directly related to oral corticosteroid therapy and do not require prioritization in this scenario.
Gastrointestinal medications
A nurse is administering a proton pump inhibitor (PPI) to a client with gastroesophageal reflux disease (GERD). Which of the following instructions should the nurse provide to the client?
Explanation
B) Correct. Proton pump inhibitors (PPIs) are most effective when taken on an empty stomach, about 30 minutes before a meal. This ensures optimal absorption and inhibits gastric acid secretion during mealtime.
A) Incorrect. PPIs do not need to be taken with a full glass of water. However, taking them with a small amount of water is recommended to aid in swallowing.
C) Incorrect. PPIs should not be crushed. They are usually in delayed-release or enteric-coated form to protect the medication from stomach acid and facilitate absorption in the small intestine.
D) Incorrect. Taking PPIs right before bedtime is not necessary or recommended unless specifically prescribed by the healthcare provider.
A nurse is caring for a client receiving a bowel cleansing agent in preparation for a colonoscopy. Which of the following assessments should the nurse prioritize?
Explanation
A) Correct. When a client is receiving a bowel cleansing agent, such as a laxative or oral sodium phosphate solution, monitoring electrolyte levels is crucial. These medications can cause electrolyte imbalances, especially hypokalemia, hyponatremia, and dehydration. The nurse should closely monitor the client's electrolyte levels and intervene appropriately to prevent complications.
B) Incorrect. Respiratory rate monitoring is important but is not the priority assessment specifically related to bowel cleansing agents.
C) Incorrect. Urine output monitoring is important but is not the priority assessment specifically related to bowel cleansing agents.
D) Incorrect. Blood glucose level monitoring is not directly affected by bowel cleansing agents and does not require prioritization in this scenario.
A nurse is preparing to administer a histamine-2 receptor antagonist (H2 blocker) to a client. Which of the following actions should the nurse take?
Explanation
D) Correct. H2 blockers, such as ranitidine or famotidine, are usually administered orally and do not require shaking. However, the nurse should monitor the client for signs of anaphylaxis, such as rash, itching, difficulty breathing, or swelling, as rare but serious allergic reactions can occur. Prompt recognition and intervention are essential in such cases.
A) Incorrect. H2 blockers can be taken with or without food, depending on the client's preference or specific instructions from the healthcare provider.
B) Incorrect. H2 blockers do not require shaking before administration.
C) Incorrect. H2 blockers are typically administered orally and are not given intravenously unless there are specific indications and healthcare provider orders.
A client is prescribed a bulk-forming laxative. Which of the following instructions should the nurse include when teaching the client about the medication?
Explanation
A) Correct. Bulk-forming laxatives, such as psyllium, should be taken with a full glass of water. This helps prevent the medication from swelling and causing an obstruction in the esophagus or gastrointestinal tract. It also aids in the formation of a soft, bulky stool.
B) Incorrect. Bulk-forming laxatives do not provide immediate relief. They work by increasing the bulk and water content of the stool, which takes time to produce a laxative effect.
C) Incorrect. Bulk-forming laxatives should not be crushed. They are typically available as granules or powder that can be mixed with liquid.
D) Incorrect. Bulk-forming laxatives can be taken at any time of the day, depending on the client's preference or specific instructions from the healthcare provider.
A nurse is caring for a client receiving sucralfate (Carafate) for the treatment of a duodenal ulcer. Which of the following instructions should the nurse provide to the client?
Explanation
C) Correct. Sucralfate (Carafate) forms a protective barrier over the ulcer, allowing it to heal. However, it can interact with antacids, reducing its effectiveness. Therefore, the client should avoid taking antacids within 30 minutes before or after sucralfate administration.
A) Incorrect. Sucralfate should be taken on an empty stomach, but this does not necessarily mean it needs to be taken in the morning before breakfast.
B) Incorrect. Sucralfate should be swallowed whole without chewing. Chewing the medication is not necessary and may interfere with its effectiveness.
D) Incorrect. Sucralfate can be taken multiple times a day, depending on the healthcare provider's instructions. It does not necessarily need to be taken at bedtime.
A nurse is teaching a client about the adverse effects of nonsteroidal anti-inflammatory drugs (NSAIDs). Which of the following adverse effects should the nurse include in the teaching?
Explanation
C) Correct. Gastrointestinal bleeding is a potential adverse effect of NSAID use. NSAIDs can cause irritation and damage to the lining of the stomach and intestines, leading to bleeding and ulcers.
A) Incorrect. Constipation is not a common adverse effect of NSAIDs. Instead, NSAIDs can cause gastrointestinal disturbances such as diarrhea or abdominal pain.
B) Incorrect. Hypotension is not a typical adverse effect of NSAIDs. However, some individuals may experience fluid retention and edema, which can lead to elevated blood pressure.
D) Incorrect. Bronchospasm is not directly associated with NSAIDs. However, individuals with a history of aspirin sensitivity or asthma may experience bronchospasm as a hypersensitivity reaction to NSAIDs.
A client is prescribed an antidiarrheal medication. The nurse should instruct the client to monitor for which of the following adverse effects?
Explanation
A) Correct. Antidiarrheal medications can cause constipation as an adverse effect.These medications slow down the movement of the gastrointestinal tract, which can lead to a delay in bowel movements and the potential for constipation.
B) Incorrect. Urinary retention is not a common adverse effect of antidiarrheal medications. Instead, urinary retention is associated with medications such as anticholinergics or opioids.
C ) Incorrect. Hypertension is not a typical adverse effect of antidiarrheal medications.
D) Incorrect. Diuresis, which refers to increased urine production, is not associated with antidiarrheal medications. Diuresis is more commonly associated with diuretic medications.
A nurse is administering an antacid medication to a client with gastroesophageal reflux disease (GERD). Which of the following instructions should the nurse provide to the client?
Explanation
D) Correct. Antacid medications can interfere with the absorption of other medications. Therefore, the client should be advised to avoid taking other medications within 1 hour of taking an antacid.
A) Incorrect. Antacid medications can be taken with or without food, depending on the client's preference or specific instructions from the healthcare provider.
B) Incorrect. Antacid medications do not need to be crushed before swallowing. They are typically available as tablets, chewable tablets, or liquids.
C) Incorrect. Taking antacid medication immediately before bedtime is not necessary or recommended unless specifically prescribed by the healthcare provider. The timing of antacid administration can vary based on the client's symptoms and medication regimen.
Nervous system medications
A nurse is caring for a client who is prescribed a benzodiazepine. Which of the following assessments should the nurse prioritize?
Explanation
C) Correct. Benzodiazepines are central nervous system depressants that can cause respiratory depression. Therefore, monitoring the client's respiratory rate is essential to ensure adequate oxygenation and identify any signs of respiratory compromise.
A) Incorrect. Blood pressure monitoring is important but is not the priority assessment specifically related to benzodiazepines.
B) Incorrect. Blood glucose levels are not directly affected by benzodiazepine use and do not require prioritization in this scenario.
D) Incorrect. While liver function tests may be relevant for some medications, it is not the priority assessment specifically related to benzodiazepines.
A nurse is caring for a client who is prescribed an acetylcholinesterase inhibitor. Which of the following statements should the nurse include in the client's education?
Explanation
A) Correct. Acetylcholinesterase inhibitors, such as donepezil or rivastigmine, are commonly prescribed to improve memory and cognitive function in clients with Alzheimer's disease. Educating the client about the therapeutic effects of the medication is important for promoting understanding and adherence.
B) Incorrect. Acetylcholinesterase inhibitors can be taken with or without food, and taking them with food may help reduce gastrointestinal side effects.
C) Incorrect. Acetylcholinesterase inhibitors do not provide immediate relief of symptoms. They need to be taken consistently over time to achieve the desired therapeutic effects.
D) Incorrect. Acetylcholinesterase inhibitors do not increase dopamine production. They work by inhibiting the breakdown of acetylcholine, a neurotransmitter involved in memory and cognitive function.
A client is prescribed a selective serotonin reuptake inhibitor (SSRI) for the treatment of depression. The nurse should monitor the client for which of the following potential adverse effects?
Explanation
D) Correct. Selective serotonin reuptake inhibitors (SSRIs) can cause sexual dysfunction as an adverse effect, including decreased libido, erectile dysfunction, or delayed ejaculation. It is important for the nurse to monitor the client for these potential adverse effects and provide appropriate support or interventions.
A) Incorrect. Hypertension is not a typical adverse effect of SSRIs. In fact, they are often used to manage anxiety disorders, which may contribute to reducing blood pressure.
B) Incorrect. Weight gain is a potential adverse effect of some antidepressant medications, but it is not specific to SSRIs.
C) Incorrect. Sedation is not a common adverse effect of SSRIs. In fact, SSRIs are generally considered to have a stimulating effect and may cause initial insomnia or agitation in some individuals.
A client is prescribed a muscle relaxant medication. The nurse should assess the client for which of the following potential adverse effects?
Explanation
C) Correct. Muscle relaxant medications can cause sedation as an adverse effect. These medications act on the central nervous system, leading to a relaxation of muscle tone, but they can also cause drowsiness and sedation.
A) Incorrect. Constipation is not a typical adverse effect of muscle relaxants. However, some muscle relaxants may have anticholinergic effects that can contribute to constipation.
B) Incorrect. Hypertension is not a common adverse effect of muscle relaxants. In fact, muscle relaxants can potentially lower blood pressure.
D) Incorrect. Bronchospasm is not directly associated with muscle relaxant use.
A nurse is caring for a client receiving an antiepileptic medication. Which of the following instructions should the nurse include in the client's teaching?
Explanation
B) Correct. Antiepileptic medications can cause drowsiness, dizziness, and impaired coordination. Therefore, the client should be advised to avoid driving or operating heavy machinery while taking the medication to prevent accidents or injuries.
A) Incorrect. The need to take the medication on an empty stomach depends on the specific medication and should be addressed based on the healthcare provider's instructions.
C) Incorrect. Antiepileptic medications should never be discontinued abruptly, as it can lead to seizure activity. The client should follow the healthcare provider's instructions for tapering off the medication, if necessary.
D) Incorrect. Alcohol can interact with antiepileptic medications and increase the risk of side effects or adverse reactions. Clients should be advised to avoid or limit alcohol consumption while taking these medications.
A client is prescribed a monoamine oxidase inhibitor (MAOI) for the treatment of depression. The nurse should instruct the client to avoid which of the following foods?
Explanation
B) Correct. Clients taking MAOIs should avoid aged cheese and other foods containing high levels of tyramine. Tyramine-rich foods can lead to a hypertensive crisis when combined with MAOIs, potentially causing severe increases in blood pressure.
A) Incorrect. Citrus fruits do not need to be avoided specifically when taking MAOIs.
C) Incorrect. Leafy green vegetables do not need to be avoided specifically when taking MAOIs.
D) Incorrect. Whole grains do not need to be avoided specifically when taking MAOIs.
A nurse is caring for a client who is prescribed a central nervous system stimulant. Which of the following assessments should the nurse prioritize?
Explanation
A) Correct. Central nervous system stimulants can increase heart rate and blood pressure. Monitoring the client's heart rate is essential to identify any cardiovascular side effects, such as tachycardia or arrhythmias.
B) Incorrect. While liver function tests may be relevant for some medications, it is not the priority assessment specifically related to central nervous system stimulants.
C) Incorrect. Urine output monitoring is important but is not the priority assessment specifically related to central nervous system stimulants.
D) Incorrect. Blood glucose levels are not directly affected by central nervous system stimulants and do not require prioritization in this scenario.
A client is prescribed a tricyclic antidepressant. The nurse should monitor the client for which of the following potential adverse effects?
Explanation
D) Correct. Tricyclic antidepressants can cause anticholinergic effects, including urinary retention. The nurse should monitor the client for any signs or symptoms of urinary retention and assess the client's ability to void.
A) Incorrect. Hypotension is a potential adverse effect of some antidepressant medications, but it is not specific to tricyclic antidepressants. In fact, tricyclic antidepressants can cause orthostatic hypotension, which is a drop in blood pressure upon standing.
B) Incorrect. Weight gain is a more common adverse effect of tricyclic antidepressants. Weight loss is not typically associated with these medications.
C) Incorrect. Insomnia is a potential adverse effect of tricyclic antidepressants, but it is not the most significant adverse effect associated with this class of medication. Sedation and drowsiness are more common adverse effects.
Endocrine medications
A nurse is preparing to teach a client about insulin administration. Which of the following statements should the nurse include in the teaching?
Explanation
A) Correct. The nurse should instruct the client to rotate injection sites to prevent lipohypertrophy, a condition characterized by fatty deposits at the injection sites that can affect insulin absorption.
B) Incorrect. Insulin should be injected into the subcutaneous tissue, not into the muscle. Injecting insulin into muscle can lead to faster absorption and potentially cause hypoglycemia.
C) Incorrect. Insulin should be stored in the refrigerator to maintain its potency. It should not be frozen or exposed to extreme heat.
D) Incorrect. Long-acting insulin and short-acting insulin should not be mixed in the same syringe unless specifically instructed by a healthcare provider. Mixing different types of insulin can alter their pharmacokinetics and effectiveness.
A client is prescribed levothyroxine sodium for the treatment of hypothyroidism. The nurse should instruct the client to take the medication at which of the following times?
Explanation
C) Correct. Levothyroxine sodium should be taken on an empty stomach, preferably 30 minutes to 1 hour before breakfast or at least 3-4 hours after the last meal. Food can interfere with the absorption of levothyroxine, reducing its effectiveness.
A) Incorrect. Taking levothyroxine before bedtime can disrupt sleep due to potential side effects, such as palpitations or insomnia.
B) Incorrect. Taking levothyroxine with meals can interfere with its absorption and reduce its effectiveness.
D) Incorrect. Levothyroxine should be taken at specific times to optimize its absorption and maintain consistent blood levels.
A nurse is reviewing the medication regimen of a client with diabetes who is also prescribed corticosteroids. The nurse should monitor the client for which of the following potential effects?
Explanation
C) Correct. Corticosteroids can increase blood glucose levels and lead to hyperglycemia. The nurse should monitor the client's blood glucose levels closely and adjust the diabetes management plan accordingly.
A) Incorrect. Corticosteroids can cause hyperglycemia, not hypoglycemia.
B) Incorrect. Hypotension is not a common adverse effect of corticosteroids.
D) Incorrect. Hyperkalemia is not directly associated with corticosteroid use.
A client is prescribed metformin for the treatment of type 2 diabetes. The nurse should instruct the client to monitor for which of the following adverse effects?
Explanation
C) Correct. Metformin is known to cause gastrointestinal upset, including symptoms such as nausea, vomiting, diarrhea, and abdominal discomfort. The client should be advised to monitor for these adverse effects and report them to the healthcare provider if they occur.
A) Incorrect. Hypoglycemia is not a common adverse effect of metformin when used as a monotherapy. However, if metformin is used in combination with other antidiabetic medications that can cause hypoglycemia, the risk may increase.
B) Incorrect. Weight gain is not typically associated with metformin. In fact, metformin may be associated with weight loss or weight stabilization in some individuals.
D) Incorrect. Bradycardia is not a known adverse effect of metformin.
A nurse is caring for a client who is receiving glucocorticoid therapy. The nurse should monitor the client for which of the following potential adverse effects?
Explanation
D) Correct. Glucocorticoid therapy can suppress the immune system, increasing the client's risk of infections and delaying wound healing. The nurse should monitor the client for signs of infection and educate the client about measures to prevent infection.
A) Incorrect. Hyperkalemia is not typically associated with glucocorticoid therapy. In fact, glucocorticoids can cause hypokalemia in some cases.
B) Incorrect. Hypotension is not a common adverse effect of glucocorticoid therapy.
C) Incorrect. Glucocorticoids can cause hypercalcemia, not hypocalcemia.
A client with hypothyroidism is prescribed levothyroxine sodium. The nurse should instruct the client to report which of the following symptoms, indicating a potential adverse effect of the medication?
Explanation
D) Correct. Levothyroxine sodium is used to treat hypothyroidism and aims to normalize thyroid hormone levels. However, excessive doses can lead to hyperthyroidism, characterized by symptoms such as tachycardia, palpitations, and tremors. The client should be instructed to report any signs of hyperthyroidism promptly.
A) Incorrect. Weight loss is a desired effect of levothyroxine therapy in individuals with hypothyroidism.
B) Incorrect. Constipation is a symptom associated with hypothyroidism and should improve with levothyroxine therapy.
C) Incorrect. Cold intolerance is a symptom associated with hypothyroidism and should improve with levothyroxine therapy.
A nurse is preparing to administer insulin lispro to a client with diabetes. The nurse should understand that insulin lispro has which of the following characteristics?
Explanation
A) Correct. Insulin lispro is a rapid-acting insulin with a rapid onset of action, typically within 15 minutes, and a short duration of action, lasting about 3-4 hours. It is used to control postprandial glucose levels.
B) Incorrect. Insulin lispro is not characterized by slow onset and long duration of action. This description more closely matches the characteristics of long-acting insulins.
C) Incorrect. Insulin lispro is not characterized by intermediate onset and duration of action. Intermediate-acting insulins, such as NPH insulin, have a slower onset and a longer duration of action.
D) Incorrect. Insulin lispro, like other insulins, has a peak action time. The peak action time refers to the time when the insulin has its maximum effect on lowering blood glucose levels.
Exams on Pharmacology of Specific Body Systems
Custom Exams
Login to Create a Quiz
Click here to loginCardiovascular Medications
Lessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Login to View Pharmacology of Specific Body Systems Study Video
Notes Highlighting is available once you sign in. Login Here.
Introduction

I. Introduction to Cardiovascular Medications
A. Importance of cardiovascular health
- Cardiovascular diseases are the leading cause of death worldwide
- Cardiovascular health refers to the function and condition of the heart and blood vessels
- Maintaining cardiovascular health can prevent or delay the onset of complications such as heart attack, stroke, heart failure, and arrhythmias
B. Role of medications in managing cardiovascular conditions
- Medications can help treat or control various cardiovascular conditions by affecting different aspects of the cardiovascular system
- Medications can reduce the risk of cardiovascular events by lowering blood pressure, cholesterol, or clotting factors
- Medications can relieve symptoms and improve quality of life by reducing chest pain, shortness of breath, or palpitations
- Medications can also have side effects and interactions that need to be monitored and managed
C. Categories of cardiovascular medications
- There are many types of cardiovascular medications with different mechanisms of action and indications
- Some of the major categories include antiplatelet agents, anticoagulants, betablockers, calcium channel blockers, ACE inhibitors, and ARBs
- Each category will be discussed in detail in the following sections
II. Antiplatelet Agents
A. Mechanism of action
- Antiplatelet agents prevent platelets from sticking together and forming clots in the blood vessels
- They work by inhibiting enzymes or receptors that are involved in platelet activation and aggregation
B. Commonly used medications
- Aspirin is a nonsteroidal antiinflammatory drug (NSAID) that inhibits cyclooxygenase-1 (COX-1), an enzyme that produces thromboxane A2, a potent platelet activator
- Clopidogrel is a thienopyridine that inhibits adenosine diphosphate (ADP) receptors on platelets, which are also involved in platelet activation and aggregation
C. Indications and contraindications
- Antiplatelet agents are indicated for patients with a history of or at high risk of arterial thrombosis, such as those with coronary artery disease (CAD), peripheral artery disease (PAD), cerebrovascular disease (CVD), or atrial fibrillation (AF)
- Antiplatelet agents are contraindicated for patients with active bleeding, peptic ulcer disease, severe liver disease, or hypersensitivity to the drugs
D. Adverse effects and monitoring
- The most common adverse effect of antiplatelet agents is bleeding, which can range from minor bruising to lifethreatening hemorrhage
- Other adverse effects include gastrointestinal upset, rash, headache, and liver dysfunction
- Monitoring parameters include bleeding time, platelet count, liver function tests, and signs and symptoms of bleeding
III. Anticoagulants
A. Mechanism of action
- Anticoagulants prevent clotting factors from forming or activating clots in the blood vessels
- They work by inhibiting enzymes or cofactors that are involved in the coagulation cascade
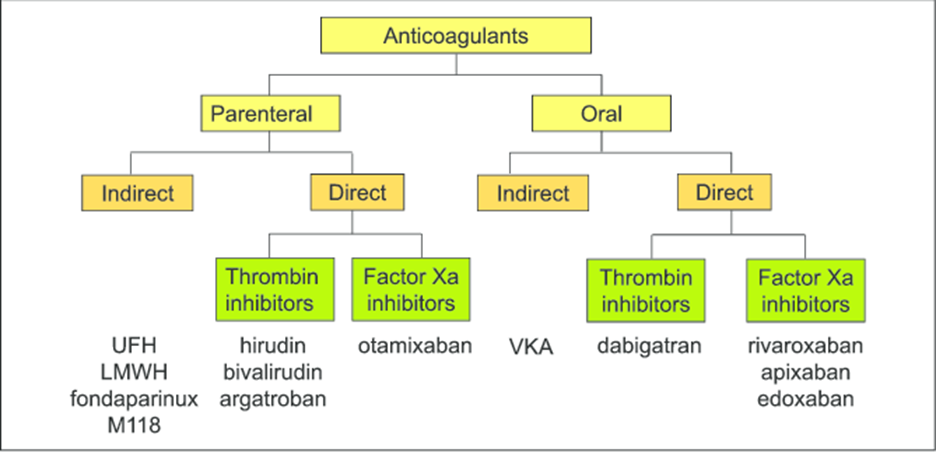
B. Types of anticoagulants
- Warfarin is a vitamin K antagonist that inhibits the synthesis of vitamin Kdependent clotting factors (II, VII, IX, X) and anticoagulant proteins (C and S)
- Heparin is a glycosaminoglycan that binds to antithrombin III (ATIII), a natural anticoagulant protein that inactivates thrombin and factor Xa
- Direct oral anticoagulants (DOACs) are newer drugs that directly inhibit either thrombin (e.g., dabigatran) or factor Xa (e.g., rivaroxaban, apixaban, edoxaban)
C. Indications and contraindications
- Anticoagulants are indicated for patients with a history of or at high risk of venous thromboembolism (VTE), such as those with deep vein thrombosis (DVT), pulmonary embolism (PE), or mechanical heart valves
- Anticoagulants are also indicated for some patients with AF, depending on their stroke risk factors
- Anticoagulants are contraindicated for patients with active bleeding, severe liver disease, or hypersensitivity to the drugs
D. Adverse effects and monitoring
- The most common adverse effect of anticoagulants is bleeding, which can range from minor bruising to lifethreatening hemorrhage
- Other adverse effects include skin necrosis, heparininduced thrombocytopenia (HIT), osteoporosis, and drug interactions
- Monitoring parameters include prothrombin time (PT) and international normalized ratio (INR) for warfarin, activated partial thromboplastin time (aPTT) and antiXa level for heparin, and renal function tests and signs and symptoms of bleeding for DOACs
E. Reversal agents
- Reversal agents are drugs that can reverse the anticoagulant effect of anticoagulants in case of emergency bleeding or surgery
- Reversal agents include vitamin K and fresh frozen plasma (FFP) for warfarin, protamine sulfate for heparin, idarucizumab for dabigatran, and andexanet alfa for factor Xa inhibitors
IV. Beta-Blockers
A. Mechanism of action
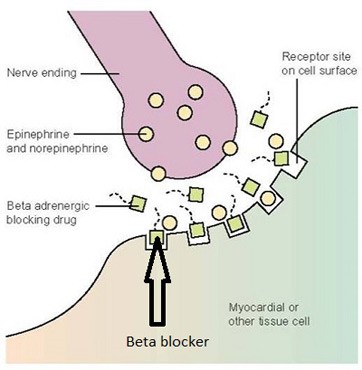
- Betablockers are drugs that block beta-adrenergic receptors on the heart and blood vessels, which are stimulated by catecholamines (e.g., epinephrine, norepinephrine)
- By blocking betaadrenergic receptors, beta-blockers reduce heart rate, contractility, and blood pressure, and decrease oxygen demand and arrhythmias
B. Commonly used beta-blockers
- Metoprolol is a selective beta1 blocker that mainly affects the heart
- Propranolol is a nonselective beta blocker that affects both the heart and the blood vessels
C. Indications and contraindications
- Betablockers are indicated for patients with hypertension, angina, myocardial infarction (MI), heart failure, or arrhythmias
- Betablockers are contraindicated for patients with bradycardia, heart block, cardiogenic shock, asthma, or hypersensitivity to the drugs
D. Adverse effects and monitoring
- The most common adverse effects of betablockers are bradycardia, hypotension, fatigue, dizziness, and bronchospasm
- Other adverse effects include depression, sexual dysfunction, hyperglycemia, and drug interactions
- Monitoring parameters include heart rate, blood pressure, electrocardiogram (ECG), blood glucose, and signs and symptoms of heart failure or asthma
E. Use in specific cardiovascular conditions
- In hypertension, betablockers lower blood pressure by reducing cardiac output and renin release
- In angina, betablockers reduce chest pain by decreasing oxygen demand and improving coronary blood flow
V. Calcium Channel Blockers

A. Mechanism of action
- Calcium channel blockers are drugs that block calcium channels on the heart and blood vessels, which are responsible for regulating muscle contraction and relaxation
- By blocking calcium channels, calcium channel blockers relax the smooth muscle of the blood vessels and reduce peripheral resistance and blood pressure
- Some calcium channel blockers also affect the cardiac muscle and reduce heart rate and contractility
B. Types of calcium channel blockers
- Dihydropyridines are calcium channel blockers that mainly affect the blood vessels (e.g., amlodipine, nifedipine)
- Nondihydropyridines are calcium channel blockers that affect both the blood vessels and the heart (e.g., diltiazem, verapamil)
C. Indications and contraindications
- Calcium channel blockers are indicated for patients with hypertension, angina, or arrhythmias
- Calcium channel blockers are contraindicated for patients with heart block, cardiogenic shock
VI. Angiotensin-Converting Enzyme (ACE) Inhibitors
A. Mechanism of action
- ACE inhibitors are drugs that inhibit the enzyme angiotensinconverting enzyme (ACE), which converts angiotensin I to angiotensin II.
- Angiotensin II is a hormone that causes vasoconstriction, sodium retention, and aldosterone secretion.
- By blocking the production of angiotensin II, ACE inhibitors lower blood pressure, reduce blood volume, and decrease the workload of the heart.
B. Commonly used ACE inhibitors
- Some of the commonly used ACE inhibitors are lisinopril (Prinivil), enalapril (Vasotec), captopril (Capoten), ramipril (Altace), and benazepril (Lotensin).
- They differ in their bioavailability, duration of action, and side effects.
C. Indications and contraindications
- ACE inhibitors are indicated for patients with hypertension, heart failure, myocardial infarction, diabetic nephropathy, and chronic kidney disease.
- They are contraindicated for patients with renal artery stenosis, hyperkalemia, angioedema, or hypersensitivity to ACE inhibitors.
D. Adverse effects and monitoring
- ACE inhibitors can cause adverse effects such as cough, hypotension, hyperkalemia, angioedema, rash, and renal impairment.
- They can also increase the risk of fetal harm in pregnant women. Patients taking ACE inhibitors should be monitored for blood pressure, serum potassium, serum creatinine, and signs of angioedema.
E. Use in specific cardiovascular conditions
- ACE inhibitors are effective in lowering blood pressure and preventing complications of hypertension such as stroke and kidney damage.
- They are also useful in improving the symptoms and survival of patients with heart failure by reducing the preload and afterload of the heart.
- They can prevent or treat myocardial infarction by preventing the remodeling of the heart muscle.
VII. Angiotensin II Receptor Blockers (ARBs)
A. Mechanism of action
- ARBs are drugs that block the angiotensin II receptors on the blood vessels and the adrenal glands.
- This prevents angiotensin II from exerting its effects of vasoconstriction, sodium retention, and aldosterone secretion.
- By blocking these effects, ARBs lower blood pressure, reduce blood volume, and decrease the workload of the heart.
B. Commonly used ARBs
- Some of the commonly used ARBs are losartan (Cozaar), valsartan (Diovan), candesartan (Atacand), irbesartan (Avapro), and telmisartan (Micardis). They differ in their potency, duration of action, and side effects.
C. Indications and contraindications
- ARBs are indicated for patients with hypertension, heart failure, myocardial infarction, diabetic nephropathy, and chronic kidney disease.
- They are contraindicated for patients with renal artery stenosis, hyperkalemia, angioedema, or hypersensitivity to ARBs.
D. Adverse effects and monitoring
- ARBs can cause adverse effects such as hypotension, hyperkalemia, angioedema, rash, and renal impairment.
- They can also increase the risk of fetal harm in pregnant women.
- Patients taking ARBs should be monitored for blood pressure, serum potassium, serum creatinine, and signs of angioedema.
E. Use in specific cardiovascular conditions
- ARBs are effective in lowering blood pressure and preventing complications of hypertension such as stroke and kidney damage.
- They are also useful in improving the symptoms and survival of patients with heart failure by reducing the preload and afterload of the heart.
- They can prevent or treat myocardial inf
VIII. Diuretics
- Drugs that increase urine output and decrease fluid volume in the body
- Mechanism of action: inhibit sodium and water reabsorption in the kidneys, leading to increased urine volume and decreased blood pressure
- Types of diuretics:
- Thiazide diuretics: act on the distal convoluted tubule of the nephron; examples include hydrochlorothiazide, chlorthalidone, and indapamide
- Loop diuretics: act on the ascending loop of Henle of the nephron; examples include furosemide, bumetanide, and torsemide
- Indications and contraindications:
- Indications: hypertension, heart failure, edema, renal failure, liver cirrhosis, hypercalcemia
- Contraindications: hypersensitivity, severe renal impairment, hypokalemia, hyponatremia, dehydration, pregnancy
- Adverse effects and monitoring:
- Adverse effects: electrolyte imbalance (especially hypokalemia), dehydration, hypotension, orthostatic hypotension, ototoxicity (especially with loop diuretics), hyperglycemia, hyperuricemia, allergic reactions
- Monitoring: blood pressure, weight, fluid intake and output, serum electrolytes (especially potassium), blood glucose, uric acid, renal function tests, hearing tests (especially with loop diuretics)
- Use in specific cardiovascular conditions:
- Hypertension: diuretics lower blood pressure by reducing blood volume and peripheral resistance; they are often used as firstline therapy or in combination with other antihypertensive drugs
- Heart failure: diuretics reduce preload and afterload by decreasing fluid volume and edema; they improve cardiac output and reduce symptoms of dyspnea and fatigue
IX. Statins and Lipid-Lowering Agents
- Drugs that lower cholesterol and triglyceride levels in the blood
- Mechanism of action: inhibit the enzyme HMGCoA reductase in the liver, which is responsible for cholesterol synthesis; they also increase the uptake of low-density lipoprotein (LDL) cholesterol by the liver cells and reduce the production of very-low-density lipoprotein (VLDL) cholesterol
- Commonly used statins: atorvastatin, simvastatin, rosuvastatin, pravastatin, lovastatin
- Indications and contraindications:
- Indications: hypercholesterolemia, dyslipidemia, prevention of cardiovascular events (e.g., myocardial infarction, stroke) in highrisk patients
- Contraindications: hypersensitivity, active liver disease or elevated liver enzymes, pregnancy or breastfeeding
- Adverse effects and monitoring:
- Adverse effects: myopathy (muscle pain or weakness), rhabdomyolysis (breakdown of muscle tissue), hepatotoxicity (liver damage), increased risk of diabetes mellitus, gastrointestinal disturbances (e.g., nausea, diarrhea), headache
- Monitoring: lipid profile (LDL cholesterol, total cholesterol, highdensity lipoprotein [HDL] cholesterol, triglycerides), liver function tests (alanine aminotransferase [ALT], aspartate aminotransferase [AST]), creatine kinase (CK), blood glucose
- Use in specific cardiovascular conditions:
- Hypercholesterolemia: statins lower LDL cholesterol levels and increase HDL cholesterol levels; they also reduce VLDL cholesterol and triglyceride levels; they are considered the most effective drugs for lowering cholesterol and preventing cardiovascular events
- Atherosclerosis: statins slow down the progression of plaque formation in the arteries by reducing cholesterol levels; they also have antiinflammatory and anti-thrombotic effects that may stabilize the plaques and prevent rupture
X. Other Cardiovascular Medications
- A variety of drugs that have different effects on the cardiovascular system
A. Nitrates:
- Drugs that dilate blood vessels by releasing nitric oxide (NO), a potent vasodilator
- Mechanism of action: relax smooth muscle cells in the walls of arteries and veins; reduce preload and afterload by decreasing venous return and arterial resistance; increase coronary blood flow by dilating coronary arteries
- Examples: nitroglycerin (sublingual, transdermal, intravenous), isosorbide dinitrate (oral), isosorbide mononitrate (oral)
- Indications and contraindications:
- Indications: angina pectoris (chest pain due to reduced blood flow to the heart), acute myocardial infarction, heart failure, pulmonary edema
- Contraindications: hypersensitivity, severe hypotension, shock, head trauma, increased intracranial pressure, concurrent use of phosphodiesterase5 inhibitors (e.g., sildenafil, tadalafil)
- Adverse effects and monitoring:
- Adverse effects: headache, hypotension, orthostatic hypotension, reflex tachycardia, flushing, dizziness, syncope, tolerance
- Monitoring: blood pressure, heart rate, pain relief, signs of hypoperfusion (e.g., confusion, cold extremities)
B. Antiarrhythmics:
- Drugs that correct abnormal heart rhythms by affecting the electrical activity of the cardiac cells
- Mechanism of action: vary depending on the class of antiarrhythmic drugs; generally, they act by blocking sodium channels, potassium channels, calcium channels, or beta receptors in the cardiac cells; they affect the rate and duration of depolarization and repolarization of the cardiac action potential
- Examples: lidocaine (class I), amiodarone (class III), verapamil (class IV), propranolol (class II)
- Indications and contraindications:
- Indications: various types of arrhythmias (e.g., atrial fibrillation, ventricular tachycardia, supraventricular tachycardia)
- Contraindications: hypersensitivity, heart block, bradycardia, hypotension, heart failureAdverse effects and monitoring:
- Adverse effects: bradycardia, hypotension, heart block, worsening of arrhythmias, proarrhythmia (new or more severe arrhythmias), nausea, vomiting, drowsiness, confusion
- Monitoring: electrocardiogram (ECG), blood pressure, heart rate, rhythm and symptoms of arrhythmias
C. Digoxin
- A cardiac glycoside that increases the force of myocardial contraction and decreases the conduction of electrical impulses through the AV node
- Used to treat heart failure and atrial fibrillation
- Has a narrow therapeutic index and requires careful monitoring of serum levels, heart rate, and signs of toxicity
- Side effects include nausea, vomiting, anorexia, bradycardia, arrhythmias, visual disturbances, and confusion
- Interacts with many drugs, including diuretics, beta blockers, calcium channel blockers, and antibiotics
D. Vasodilators
- Drugs that dilate blood vessels and reduce peripheral resistance
- Used to treat hypertension, angina pectoris, heart failure, and pulmonary hypertension
- Types of vasodilators include nitrates, hydralazine, minoxidil, and sodium nitroprusside
- Side effects include headache, hypotension, reflex tachycardia, flushing, dizziness, and edema
- May cause orthostatic hypotension and should be taken with caution in patients with renal or hepatic impairment
E. Other miscellaneous agents
- Drugs that have various effects on the cardiovascular system and are used for specific indications
- Examples include antiarrhythmics (e.g., amiodarone, lidocaine), anticoagulants (e.g., heparin, warfarin), antiplatelets (e.g., aspirin, clopidogrel), thrombolytics (e.g., alteplase, streptokinase), and lipidlowering agents (e.g., statins, fibrates)
- Each class of drugs has its own mechanism of action, pharmacokinetics, indications, contraindications, interactions, and adverse effects
- Patients should be educated about the purpose, dosage, administration, monitoring, and precautions of these drugs.
Respiratory medications
I. Introduction to Respiratory Medications
- Respiratory health is vital for oxygen delivery, gas exchange, and cellular function.
- Medications can help prevent, treat, and control respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and pneumonia.
- Respiratory medications can be classified into different categories based on their mechanism of action, route of administration, and duration of effect.
II. Bronchodilators
- Bronchodilators are medications that relax the smooth muscles of the airways and increase airflow to the lungs.
- There are three main types of bronchodilators: shortacting beta-agonists (SABAs), long-acting beta-agonists (LABAs), and anticholinergic bronchodilators.
A. Short-acting beta-agonists (SABAs)
- SABAs are bronchodilators that bind to beta2 receptors on the smooth muscles of the airways and cause them to relax.
- SABAs are commonly used as rescue medications for acute asthma attacks or exacerbations of COPD. They can also be used before exercise to prevent exerciseinduced bronchoconstriction.
- Examples of SABAs include albuterol, levalbuterol, and terbutaline.
- SABAs are contraindicated in patients with hypersensitivity to the medication or its components, cardiac arrhythmias, or uncontrolled hypertension.
- SABAs can cause adverse effects such as tachycardia, palpitations, tremors, nervousness, insomnia, and hypokalemia. Patients using SABAs should be monitored for vital signs, lung sounds, oxygen saturation, and serum potassium levels.
B. Long-acting beta-agonists (LABAs)
- LABAs are bronchodilators that bind to beta2 receptors on the smooth muscles of the airways and cause them to relax for a longer duration than SABAs.
- LABAs are commonly used as maintenance medications for chronic asthma or COPD. They are usually combined with inhaled corticosteroids (ICS) to enhance their efficacy and reduce the risk of adverse effects.
- Examples of LABAs include formoterol, salmeterol, and indacaterol.
- LABAs are contraindicated in patients with hypersensitivity to the medication or its components, cardiac arrhythmias, or uncontrolled hypertension. They should not be used as monotherapy for asthma or as rescue medications for acute symptoms.
- LABAs can cause adverse effects such as tachycardia, palpitations, tremors, nervousness, insomnia, and hypokalemia. Patients using LABAs should be monitored for vital signs, lung sounds, oxygen saturation, and serum potassium levels.
C. Anticholinergic bronchodilators
- Anticholinergic bronchodilators are medications that block the action of acetylcholine on the muscarinic receptors on the smooth muscles of the airways and cause them to relax.
- Anticholinergic bronchodilators are commonly used as maintenance medications for chronic asthma or COPD. They can also be used in combination with SABAs or LABAs for additive bronchodilation.
- Examples of anticholinergic bronchodilators include ipratropium bromide, tiotropium, and aclidinium.
- Anticholinergic bronchodilators are contraindicated in patients with hypersensitivity to the medication or its components, narrowangle glaucoma, or urinary retention.
- Anticholinergic bronchodilators can cause adverse effects such as dry mouth, blurred vision, constipation, urinary retention, and tachycardia. Patients using anticholinergic bronchodilators should be monitored for oral hygiene, eye exams, bowel movements, urine output, and heart rate.
III. Inhaled Corticosteroids (ICS)
- ICS are medications that reduce inflammation and mucus production in the airways by inhibiting the synthesis of inflammatory mediators such as cytokines and leukotrienes.
- ICS are commonly used as maintenance medications for chronic asthma or COPD. They are usually combined with LABAs to enhance their efficacy and reduce the risk of adverse effects.
- Examples of ICS include fluticasone, budesonide, mometasone, and ciclesonide.
- ICS are contraindicated in patients with hypersensitivity to the medication or its components, active or latent tuberculosis infection, fungal infection of the mouth or throat, or systemic steroid use within the past year.
- ICS can cause adverse effects such as oral candidiasis, hoarseness, cough, dysphonia, and adrenal suppression. Patients using ICS should be monitored for oral hygiene, voice quality, lung sounds, growth, and bone density.
VIII. Mucolytics and Expectorants
- Mucolytics are drugs that break down mucus and make it easier to cough up.
- Expectorants are drugs that increase the production and secretion of mucus and help clear the airways.
- Commonly used medications include acetylcysteine, which is a mucolytic, and guaifenesin, which is an expectorant.
- Indications for mucolytics and expectorants are conditions that cause thick and sticky mucus in the respiratory tract, such as chronic bronchitis, cystic fibrosis, and pneumonia.
- Contraindications for mucolytics and expectorants are hypersensitivity to the drugs, asthma, peptic ulcer disease, and bleeding disorders.
- Adverse effects of mucolytics and expectorants are nausea, vomiting, diarrhea, bronchospasm, rash, and allergic reactions. Monitoring for these effects is important.
IX. Inhaler Devices and Techniques
- Inhalers are devices that deliver medication directly to the lungs in the form of aerosol or powder.
- Metereddose inhalers (MDIs) are pressurized canisters that release a measured dose of medication with each actuation. They require coordination between inhalation and actuation.
- Dry powder inhalers (DPIs) are devices that contain medication in a powder form that is inhaled by the patient's breath. They do not require coordination but need sufficient inspiratory flow.
- Nebulizers are machines that convert liquid medication into a fine mist that is inhaled through a mouthpiece or mask. They do not require coordination but need a power source and take longer to administer.
- Proper inhalation techniques and patient education are essential for effective delivery of medication and prevention of complications. Some general principles are:
- Shake the inhaler before use
- Breathe out fully before inhaling
- Hold the inhaler upright and away from the mouth
- Place the mouthpiece between the lips and seal them tightly
- Press the canister (for MDIs) or inhale deeply (for DPIs) while breathing in slowly and steadily
- Hold the breath for 10 seconds after inhaling
- Wait for at least one minute between puffs
- Rinse the mouth after using inhaled corticosteroids
- Clean the inhaler regularly according to manufacturer's instructions
X. Other Respiratory Medications
- Antihistamines are drugs that block histamine receptors and reduce allergic symptoms such as sneezing, itching, runny nose, and watery eyes.
- Decongestants are drugs that constrict blood vessels in the nasal mucosa and reduce swelling and congestion.
- Antitussives are drugs that suppress cough reflex and reduce coughing.
- Oxygen therapy is the administration of supplemental oxygen to patients with hypoxemia (low blood oxygen levels).
Gastrointestinal medications
I. Introduction to Gastrointestinal Medications
- Gastrointestinal health is essential for digestion, absorption, and elimination of nutrients and waste.
- Medications can help treat various gastrointestinal conditions such as ulcers, reflux, nausea, vomiting, diarrhea, and constipation.
- Gastrointestinal medications can be classified into different categories based on their mechanism of action and therapeutic effects.
II. Acid-Reducing Agents
- These are medications that lower the amount of acid produced by the stomach.
- They are used to treat conditions such as gastroesophageal reflux disease (GERD), peptic ulcer disease (PUD), and ZollingerEllison syndrome (ZES).
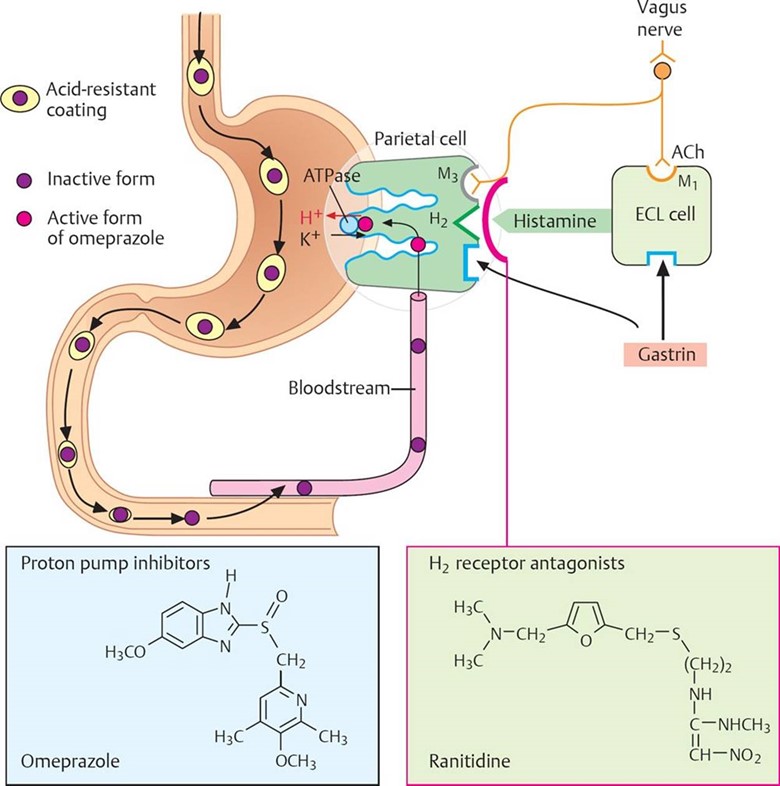
- There are three main types of acidreducing agents: proton pump inhibitors (PPIs), H2 receptor antagonists, and antacids.
A. Proton Pump Inhibitors (PPIs)
- These are medications that block the enzyme that pumps hydrogen ions into the stomach, thereby reducing acid secretion.
- Some examples of PPIs are omeprazole (Prilosec), esomeprazole (Nexium), lansoprazole (Prevacid), and pantoprazole (Protonix).
- PPIs are indicated for the treatment of GERD, PUD, ZES, and prevention of stress ulcers.
- PPIs are contraindicated in patients with hypersensitivity to the medication or its components, and in patients with liver impairment or osteoporosis.
- Some adverse effects of PPIs are headache, diarrhea, nausea, abdominal pain, and increased risk of fractures and infections.
- PPIs should be monitored for effectiveness, adverse effects, drug interactions, and adherence to therapy.
B. H2 Receptor Antagonists
- These are medications that block the histamine receptors on the parietal cells of the stomach, thereby reducing acid secretion.
- Some examples of H2 receptor antagonists are ranitidine (Zantac), famotidine (Pepcid), cimetidine (Tagamet), and nizatidine (Axid).
- H2 receptor antagonists are indicated for the treatment of GERD, PUD, ZES, and prevention of stress ulcers.
- H2 receptor antagonists are contraindicated in patients with hypersensitivity to the medication or its components, and in patients with renal or hepatic impairment.
- Some adverse effects of H2 receptor antagonists are headache, dizziness, diarrhea, constipation, and confusion.
- H2 receptor antagonists should be monitored for effectiveness, adverse effects, drug interactions, and adherence to therapy.
C. Antacids
- These are medications that neutralize the acid in the stomach by forming a salt and water.
- Some examples of antacids are aluminum hydroxide (Amphojel), calcium carbonate (Tums), magnesium hydroxide (Milk of Magnesia), and sodium bicarbonate (Baking Soda).
- Antacids are indicated for the treatment of mild to moderate GERD and PUD symptoms.
- Antacids are contraindicated in patients with hypersensitivity to the medication or its components, and in patients with renal failure or electrolyte imbalances.
- Some adverse effects of antacids are constipation, diarrhea, gas, bloating, and metabolic alkalosis.
- Antacids should be monitored for effectiveness, adverse effects, drug interactions, and adherence to therapy.
III. Antiemetics
- These are medications that prevent or treat nausea and vomiting by acting on different receptors in the brain or gastrointestinal tract.
- They are used to treat conditions such as motion sickness, chemotherapy-induced nausea and vomiting (CINV), postoperative nausea and vomiting (PONV), and gastroparesis.
- There are several types of antiemetics: serotonin antagonists, dopamine antagonists, antihistamines, anticholinergics, cannabinoids, corticosteroids, benzodiazepines, and neurokinin antagonists.
A. Serotonin Antagonists
- These are medications that block the serotonin receptors in the brain and gastrointestinal tract, thereby inhibiting the vomiting reflex.
- Some examples of serotonin antagonists are ondansetron (Zofran), granisetron (Kytril), dolasetron (Anzemet), and palonosetron (Aloxi).
- Serotonin antagonists are indicated for the prevention and treatment of CINV and PONV.
- Serotonin antagonists are contraindicated in patients with hypersensitivity to the medication or its components, and in patients with prolonged QT interval or cardiac arrhythmias.
- Some adverse effects of serotonin antagonists are headache, dizziness, constipation, diarrhea, and QT prolongation.
- Serotonin antagonists should be monitored for effectiveness, adverse effects, drug interactions, and adherence to therapy.
B. Dopamine Antagonists
- These are medications that block the dopamine receptors in the brain and gastrointestinal tract, thereby inhibiting the vomiting reflex.
- Some examples of dopamine antagonists are prochlorperazine (Compazine), metoclopramide (Reglan), promethazine (Phenergan), and haloperidol (Haldol).
- Dopamine antagonists are indicated for the prevention and treatment of CINV, PONV, and gastroparesis.
- Dopamine antagonists are contraindicated in patients with hypersensitivity to the medication or its components, and in patients with Parkinson's disease, seizure disorders, or bone marrow suppression.
- Some adverse effects of dopamine antagonists are sedation, drowsiness, extrapyramidal symptoms, tardive dyskinesia, hypotension, and anticholinergic effects.
- Dopamine antagonists should be monitored for effectiveness, adverse effects, drug interactions, and adherence to therapy.
C. Antihistamines
- These are medications that block the histamine receptors in the brain and inner ear, thereby inhibiting the vomiting reflex and reducing motion sickness.
- Some examples of antihistamines are dimenhydrinate (Dramamine), meclizine (Antivert), diphenhydramine (Benadryl), and hydroxyzine (Vistaril).
- Antihistamines are indicated for the prevention and treatment of motion sickness and PONV.
- Antihistamines are contraindicated in patients with hypersensitivity to the medication or its components, and in patients with glaucoma, urinary retention, or prostate enlargement.
- Some adverse effects of antihistamines are sedation, drowsiness, dry mouth, blurred vision, and urinary retention.
- Antihistamines should be monitored for effectiveness, adverse effects, drug interactions, and adherence to therapy.
IV. Laxatives
A. Bulk-forming laxatives
- Mechanism of action: absorb water and increase fecal mass, stimulating peristalsis
- Commonly used medications: psyllium, methylcellulose
- Indications: constipation, diverticular disease, irritable bowel syndrome
- Contraindications: bowel obstruction, fecal impaction, difficulty swallowing
- Adverse effects and monitoring: bloating, gas, abdominal discomfort, allergic reactions; monitor fluid intake and bowel movements
B. Stimulant laxatives
- Mechanism of action: increase intestinal motility and secretion of water and electrolytes into the colon
- Commonly used medications: bisacodyl, senna
- Indications: constipation, bowel preparation for surgery or diagnostic procedures
- Contraindications: bowel obstruction, appendicitis, ulcerative colitis, dehydration
- Adverse effects and monitoring: abdominal cramps, diarrhea, electrolyte imbalance, dependence; monitor fluid and electrolyte status and bowel movements
C. Osmotic laxatives
- Mechanism of action: draw water into the intestinal lumen, increasing intraluminal pressure and stimulating peristalsis
- Commonly used medications: lactulose, polyethylene glycol
- Indications: constipation, hepatic encephalopathy (lactulose), bowel preparation for colonoscopy (polyethylene glycol)
- Contraindications: bowel obstruction, renal impairment, dehydration
- Adverse effects and monitoring: abdominal cramps, flatulence, diarrhea, electrolyte imbalance; monitor fluid and electrolyte status and bowel movements
V. Anti-diarrheal Agents
A. Opioid Antimotility Agents
- Mechanism of action: activate opioid receptors in the gastrointestinal tract, reducing intestinal motility and increasing absorption of water and electrolytes
- Commonly used medications: loperamide, diphenoxylate/atropine
- Indications: diarrhea (acute or chronic), inflammatory bowel disease (loperamide)
- Contraindications: infectious diarrhea, pseudomembranous colitis, bowel obstruction
- Adverse effects and monitoring: drowsiness, dizziness, constipation, ileus; monitor bowel movements and signs of dehydration or toxicity
B. Adsorbents
- Mechanism of action: bind to toxins or bacteria in the gastrointestinal tract and facilitate their elimination in the stool
- Commonly used medications: bismuth subsalicylate
- Indications: diarrhea (acute or chronic), dyspepsia, Helicobacter pylori infection
- Contraindications: aspirin allergy, bleeding disorders, renal impairment
- Adverse effects and monitoring: black stools, black tongue, tinnitus, Reye's syndrome; monitor stool characteristics and signs of bleeding or toxicity
VI. Anti-inflammatory Agents
A. Corticosteroids
- Mechanism of action: suppress inflammation and immune response by inhibiting the synthesis of prostaglandins and leukotrienes
- Commonly used medications: prednisone, budesonide
- Indications: inflammatory bowel disease (Crohn's disease or ulcerative colitis), allergic reactions
- Contraindications: systemic fungal infections, peptic ulcer disease, diabetes mellitus
- Adverse effects and monitoring: hyperglycemia, osteoporosis, adrenal suppression, infection; monitor blood glucose levels, bone density tests, adrenal function tests and signs of infection
B. Aminosalicylates
- Mechanism of action: inhibit the synthesis of prostaglandins and leukotrienes in the colon mucosa
- Commonly used medications: mesalamine, sulfasalazine
- Indications: inflammatory bowel disease (Crohn's disease or ulcerative colitis), rheumatoid arthritis (sulfasalicylate)
- Contraindications: salicylate allergy, sulfonamide allergy, renal impairment
- Adverse effects and monitoring: nausea, vomiting, diarrhea, headache, rash, blood dyscrasias; monitor liver and kidney function tests and complete blood count
VII. Prokinetic Agents
- Mechanism of action: enhance gastric emptying and intestinal motility by stimulating dopamine or serotonin receptors in the gastrointestinal tract
- Commonly used medications: metoclopramide, domperidone
- Indications: gastroparesis, gastroesophageal reflux disease, nausea and vomiting
- Contraindications: bowel obstruction, perforation, hemorrhage, seizure disorders
- Adverse effects and monitoring: drowsiness, extrapyramidal symptoms, tardive dyskinesia, hyperprolactinemia; monitor neurological status and serum prolactin levels
Nervous system medications
I. Introduction to Nervous System Medications
- Nervous system health is essential for normal functioning of the body and mind
- Medications can help treat various nervous system conditions, such as pain, seizures, depression, and anxiety
- Nervous system medications can be classified into different categories based on their effects and targets
II. Analgesics and Pain Management
- Analgesics are medications that relieve pain by blocking pain signals or reducing inflammation
- There are three main types of analgesics: NSAIDs, opioids, and adjuvant analgesics
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- NSAIDs work by inhibiting the enzyme cyclooxygenase (COX), which produces prostaglandins that cause inflammation and pain
- Some common NSAIDs are ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin
- NSAIDs are used for mild to moderate pain, fever, and inflammatory conditions (e.g., arthritis, menstrual cramps)
- NSAIDs should not be used in people with allergies, ulcers, bleeding disorders, kidney or liver problems, or heart failure
- NSAIDs can cause adverse effects such as stomach irritation, bleeding, ulcers, kidney damage, and increased blood pressure
- NSAIDs should be monitored for signs of bleeding, renal impairment, and cardiovascular complications
B. Opioids
- Opioids work by binding to opioid receptors in the brain and spinal cord, which block pain signals and produce euphoria
- Some common opioids are morphine (MS Contin), oxycodone (OxyContin), hydrocodone (Vicodin), and fentanyl (Duragesic)
- Opioids are used for moderate to severe pain, especially in cancer and palliative care
- Opioids should not be used in people with respiratory depression, head injury, addiction history, or hypersensitivity
- Opioids can cause adverse effects such as sedation, respiratory depression, constipation, nausea, vomiting, itching, and dependence
- Opioids should be monitored for signs of overdose, respiratory depression, bowel function, and addiction
C. Adjuvant Analgesics
- Adjuvant analgesics are medications that have other primary uses but can also enhance pain relief
- Some common adjuvant analgesics are gabapentin (Neurontin), amitriptyline (Elavil), and ketamine (Ketalar)
- Adjuvant analgesics are used for neuropathic pain, chronic pain, and refractory pain
- Adjuvant analgesics should not be used in people with contraindications to their primary indications (e.g., seizure disorders for gabapentin, cardiac arrhythmias for amitriptyline)
- Adjuvant analgesics can cause adverse effects such as drowsiness, dizziness, dry mouth, weight gain, and hallucinations
- Adjuvant analgesics should be monitored for signs of toxicity, effectiveness, and interactions with other medications
III. Anticonvulsants
- Anticonvulsants are medications that prevent or reduce the frequency of seizures by stabilizing the electrical activity of neurons
- There are many types of anticonvulsants with different mechanisms of action and targets
- Some common anticonvulsants are phenytoin (Dilantin), valproic acid (Depakote), carbamazepine (Tegretol), and lamotrigine (Lamictal)
- Anticonvulsants are used for epilepsy and other seizure disorders, as well as bipolar disorder, migraine prevention, and neuropathic pain
- Anticonvulsants should not be used in people with hypersensitivity, liver or kidney impairment, blood disorders, or pregnancy
- Anticonvulsants can cause adverse effects such as drowsiness, ataxia, rash, nausea, vomiting, bone marrow suppression, and liver toxicity
- Anticonvulsants should be monitored for signs of therapeutic levels, toxicity, seizure control, and mood stability
IV. Anti-Parkinsonian Agents
A. Dopamine Agonists
- Stimulate dopamine receptors in the brain
- Used to treat Parkinson's disease and restless legs syndrome
- Examples: pramipexole, ropinirole
- Contraindicated in patients with psychosis, severe cardiovascular disease, or hypersensitivity
- Adverse effects: nausea, drowsiness, orthostatic hypotension, hallucinations, compulsive behaviors
- Monitor: blood pressure, renal function, mental status
- Levodopa/Carbidopa
- Precursor of dopamine that crosses the bloodbrain barrier
- Combined with carbidopa to prevent peripheral metabolism of levodopa
- Used to treat Parkinson's disease
- Contraindicated in patients with narrowangle glaucoma, melanoma, or hypersensitivity
- Adverse effects: nausea, dyskinesia, psychosis, dysrhythmias
- Monitor: liver function, hematologic parameters, mental status
V. Antidepressants
A. Selective Serotonin Reuptake Inhibitors (SSRIs)
- Inhibit the reuptake of serotonin in the synaptic cleft
- Used to treat major depressive disorder, anxiety disorders, obsessivecompulsive disorder, and post-traumatic stress disorder
- Examples: fluoxetine, sertraline
- Contraindicated in patients with bipolar disorder, seizure disorders, or hypersensitivity
- Adverse effects: insomnia, headache, sexual dysfunction, serotonin syndrome
B. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- SNRIs block the reabsorption of serotonin and norepinephrine in the brain, increasing their availability and enhancing mood and cognition.
- Common SNRIs include venlafaxine (Effexor) and duloxetine (Cymbalta).
- SNRIs are indicated for major depressive disorder, generalized anxiety disorder, neuropathic pain, and fibromyalgia. They are contraindicated in patients with uncontrolled hypertension, bleeding disorders, or hypersensitivity to the drug.
- Adverse effects of SNRIs may include nausea, headache, insomnia, dry mouth, sweating, and sexual dysfunction. SNRIs may also increase blood pressure and heart rate, and cause serotonin syndrome if combined with other serotonergic agents. Patients on SNRIs should be monitored for blood pressure, heart rate, mood changes, and signs of serotonin syndrome.
C. Tricyclic Antidepressants (TCAs)
- TCAs block the reuptake of serotonin and norepinephrine in the brain, as well as antagonize various receptors such as histamine, muscarinic, and alphaadrenergic receptors.
- Common TCAs include amitriptyline (Elavil) and nortriptyline (Pamelor).
- TCAs are indicated for major depressive disorder, especially with melancholic or atypical features, neuropathic pain, migraine prophylaxis, and nocturnal enuresis. They are contraindicated in patients with cardiac arrhythmias, recent myocardial infarction, glaucoma, urinary retention, or hypersensitivity to the drug.
- Adverse effects of TCAs may include sedation, weight gain, anticholinergic effects (dry mouth, blurred vision, constipation, urinary retention), orthostatic hypotension, and cardiac toxicity. TCAs may also lower the seizure threshold and cause serotonin syndrome if combined with other serotonergic agents. Patients on TCAs should be monitored for electrocardiogram (ECG) changes, blood pressure, anticholinergic effects, mood changes, and signs of serotonin syndrome.
VI. Anxiolytics and Sedatives
A. Benzodiazepines
- Benzodiazepines enhance the activity of gammaaminobutyric acid (GABA), the main inhibitory neurotransmitter in the brain, resulting in sedation, anxiolysis, muscle relaxation, and anticonvulsant effects.
- Common benzodiazepines include diazepam (Valium) and lorazepam (Ativan).
- Benzodiazepines are indicated for anxiety disorders, insomnia, alcohol withdrawal, seizures, muscle spasms, and preoperative sedation. They are contraindicated in patients with respiratory depression, sleep apnea, liver impairment, or hypersensitivity to the drug.
- Adverse effects of benzodiazepines may include drowsiness, confusion, ataxia, amnesia, dependence, tolerance, and withdrawal symptoms. Benzodiazepines may also potentiate the effects of other central nervous system (CNS) depressants such as alcohol and opioids. Patients on benzodiazepines should be monitored for respiratory rate, level of consciousness, mental status, and signs of abuse or withdrawal.
B. Non-Benzodiazepine Hypnotics
- Nonbenzodiazepine hypnotics act on a specific subtype of GABA receptors in the brain that are involved in sleep regulation.
- Common nonbenzodiazepine hypnotics include zolpidem (Ambien) and eszopiclone (Lunesta).
- Nonbenzodiazepine hypnotics are indicated for short-term treatment of insomnia. They are contraindicated in patients with respiratory depression, sleep apnea, liver impairment, or hypersensitivity to the drug.
- Adverse effects of nonbenzodiazepine hypnotics may include drowsiness, headache, dizziness, nausea, and complex sleep behaviors such as sleepwalking, sleep driving, or sleep eating.
- Nonbenzodiazepine hypnotics may also cause dependence, tolerance, and withdrawal symptoms.
- Patients on nonbenzodiazepine hypnotics should be monitored for respiratory rate, level of consciousness, mental status, and signs of abuse or withdrawal.
VII. Anti-Alzheimer's Medications
A. Cholinesterase Inhibitors
- Cholinesterase inhibitors prevent the breakdown of acetylcholine, a neurotransmitter involved in memory and cognition, by inhibiting the enzyme acetylcholinesterase in the brain.
- Common cholinesterase inhibitors include donepezil (Aricept) and rivastigmine (Exelon).
- Cholinesterase inhibitors are indicated for mild to moderate Alzheimer's disease.
- They are contraindicated in patients with bradycardia, sick sinus syndrome, peptic ulcer disease, or hypersensitivity to the drug.
- Adverse effects of cholinesterase inhibitors may include nausea, vomiting, diarrhea, anorexia, weight loss, and bradycardia.
- Cholinesterase inhibitors may also worsen symptoms of asthma, chronic obstructive pulmonary disease (COPD), or urinary obstruction.
- Patients on cholinesterase inhibitors should be monitored for heart rate, blood pressure, weight, gastrointestinal symptoms, and cognitive function.
B. N-Methyl-D-Aspartate (NMDA) Receptor Antagonists
- NMDA receptor antagonists block the activity of glutamate, an excitatory neurotransmitter that may cause neurotoxicity and neuronal death in Alzheimer's disease, by antagonizing the NMDA receptors in the brain.
- The only approved NMDA receptor antagonist for Alzheimer's disease is memantine (Namenda).
- Memantine is indicated for moderate to severe Alzheimer's disease. It is contraindicated in patients with renal impairment or hypersensitivity to the drug.
- Adverse effects of memantine may include dizziness, headache, confusion, constipation, and agitation. Memantine may also interact with other drugs that affect the pH of urine, such as sodium bicarbonate or acetazolamide. Patients on memantine should be monitored for renal function, mental status, and cognitive function.
Endocrine medications
I. Introduction to Endocrine Medications
- The endocrine system is a network of glands and hormones that regulate many vital functions in the body, such as metabolism, growth, reproduction, and stress response.
- Endocrine disorders can result from hormone deficiency, excess, or resistance, and can affect various organs and systems.
- Endocrine medications are drugs that either replace or modify the action of natural hormones, and are used to treat various endocrine conditions, such as hypothyroidism, hyperthyroidism, diabetes, adrenal insufficiency, and osteoporosis.
- Endocrine medications can be classified into different categories based on the hormone they target or mimic, such as thyroid medications, diabetes medications, adrenal medications, and calcium and vitamin D medications.
II. Thyroid Medications
- The thyroid gland is located in the neck and produces thyroid hormones (T3 and T4), which regulate the body's metabolism, growth, and development.
- Thyroid disorders can result from either underproduction (hypothyroidism) or overproduction (hyperthyroidism) of thyroid hormones, and can cause symptoms such as fatigue, weight changes, mood swings, and goiter.
- Thyroid medications are drugs that either replace or inhibit the production of thyroid hormones, and are used to treat hypothyroidism or hyperthyroidism.

A. Thyroid Hormone Replacement Therapy
- This is a type of medication that provides synthetic thyroid hormones to supplement the low levels of natural hormones in hypothyroid patients.
- The mechanism of action is to bind to thyroid hormone receptors in the target cells and activate the same metabolic processes as natural hormones.
- The most commonly used medication is levothyroxine (Synthroid), which is a synthetic form of T4 that is converted to T3 in the body.
- The indications for this therapy are hypothyroidism of any cause, such as Hashimoto's thyroiditis, iodine deficiency, or surgical removal of the thyroid gland.
- The contraindications for this therapy are hyperthyroidism, acute myocardial infarction, or hypersensitivity to the medication.
- The adverse effects of this therapy include symptoms of hyperthyroidism, such as palpitations, nervousness, insomnia, and heat intolerance. The therapy also requires regular monitoring of serum TSH levels to adjust the dosage accordingly.
B. Antithyroid Medications
- This is a type of medication that inhibits the synthesis or release of thyroid hormones in hyperthyroid patients.
- The mechanism of action is to interfere with the iodination of tyrosine residues in thyroglobulin, which is the precursor of thyroid hormones. Some medications also block the conversion of T4 to T3 in peripheral tissues.
- The most commonly used medications are methimazole (Tapazole) and propylthiouracil (PTU), which are thioamide derivatives that act on the thyroid gland.
- The indications for this therapy are hyperthyroidism of any cause, such as Graves' disease, toxic nodular goiter, or thyroid storm. The therapy can also be used as a preoperative preparation for thyroidectomy or as an adjunct to radioactive iodine therapy.
- The contraindications for this therapy are hypothyroidism, pregnancy (especially in the first trimester), or hypersensitivity to the medication.
- The adverse effects of this therapy include symptoms of hypothyroidism, such as lethargy, weight gain, depression, and cold intolerance. The therapy also carries a risk of agranulocytosis (a severe reduction in white blood cells), which requires periodic monitoring of blood counts. Other side effects include rash, pruritus, nausea, vomiting, and liver toxicity.
III. Diabetes Medications
- Diabetes mellitus is a chronic condition characterized by high blood glucose levels due to either insufficient insulin production (type 1 diabetes) or insulin resistance (type 2 diabetes).
- Diabetes can cause various complications such as cardiovascular disease, kidney disease, neuropathy, retinopathy, and foot ulcers.
- Diabetes medications are drugs that either increase insulin secretion or sensitivity, or lower blood glucose levels by other mechanisms. They are used to control blood glucose levels and prevent or delay diabetes complications.
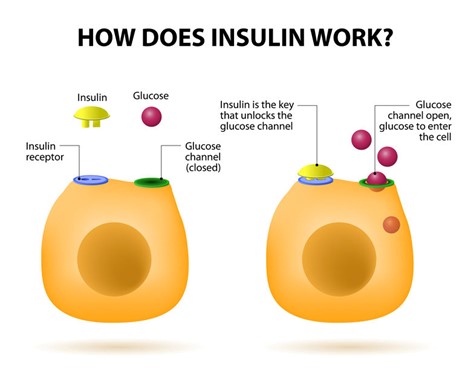
A. Insulin Therapy
- This is a type of medication that provides exogenous insulin to supplement or replace the endogenous insulin in diabetic patients.
- The mechanism of action is to bind to insulin receptors on the target cells and facilitate the uptake and utilization of glucose. Insulin also inhibits gluconeogenesis (the production of glucose from noncarbohydrate sources) and glycogenolysis (the breakdown of glycogen to glucose) in the liver and muscle.
- There are different types of insulin based on their onset, peak, and duration of action. The main types are rapidacting (e.g., lispro, aspart, glulisine), short-acting (e.g., regular), intermediate-acting (e.g., NPH), long-acting (e.g., glargine, detemir, degludec), and mixed (e.g., 70/30, 75/25, 50/50).
- The indications for this therapy are type 1 diabetes, type 2 diabetes that is not controlled by oral medications or lifestyle changes, gestational diabetes, diabetic ketoacidosis, or hyperglycemic hyperosmolar state.
- The contraindications for this therapy are hypoglycemia, allergy to insulin or its components, or concurrent use of drugs that may potentiate or antagonize the effects of insulin.
- The adverse effects of this therapy include hypoglycemia, which is a condition of low blood glucose levels that can cause symptoms such as sweating, trembling, hunger, confusion, and coma. Hypoglycemia can be treated by administering glucose or glucagon. Other side effects include weight gain, lipodystrophy (abnormal fat distribution at the injection site), allergic reactions, and hypokalemia (low potassium levels).
- Insulin administration requires proper injection technique, site rotation, storage, and disposal. Insulin also requires regular monitoring of blood glucose levels and adjustment of dosage based on factors such as diet, exercise, stress, and illness.
B. Oral Antidiabetic Medications
- This is a type of medication that lowers blood glucose levels by stimulating insulin secretion or enhancing insulin sensitivity in diabetic patients.
- The mechanism of action varies depending on the class of medication. The main classes are biguanides (e.g., metformin), sulfonylureas (e.g., glipizide, glyburide), meglitinides (e.g., repaglinide, nateglinide), thiazolidinediones (e.g., pioglitazone, rosiglitazone), alphaglucosidase inhibitors (e.g., acarbose, miglitol), dipeptidyl peptidase-4 inhibitors (e.g., sitagliptin, saxagliptin), sodium-glucose cotransporter 2 inhibitors (e.g., canagliflozin, dapagliflozin), and glucagon-like peptide 1 receptor agonists (e.g., exenatide, liraglutide).
- The indications for this therapy are type 2 diabetes that is not controlled by diet and exercise alone. Some medications can also be used in combination with insulin or other oral antidiabetic medications.
- The contraindications for this therapy depend on the class of medication. Some general contraindications are type 1 diabetes, diabetic ketoacidosis, severe renal or hepatic impairment, or hypersensitivity to the medication.
IV. Adrenal Medications
A. Glucocorticoids
- Mimic the effects of cortisol, a hormone produced by the adrenal cortex
- Suppress inflammation and immune responses, regulate glucose metabolism and stress response
- Commonly used medications include prednisone, hydrocortisone, dexamethasone, etc.
- Indicated for conditions such as asthma, rheumatoid arthritis, inflammatory bowel disease, adrenal insufficiency, etc.
- Contraindicated for patients with systemic fungal infections, hypersensitivity to the drugs, or peptic ulcer disease
- Adverse effects include hyperglycemia, osteoporosis, infection, weight gain, mood changes, etc.
- Monitoring includes blood glucose, bone density, signs of infection, electrolytes, etc.
B. Mineralocorticoids
- Mimic the effects of aldosterone, a hormone produced by the adrenal cortex
- Regulate sodium and water balance, blood pressure and potassium levels
- Commonly used medication is fludrocortisone
- Indicated for conditions such as Addison's disease, congenital adrenal hyperplasia, etc.
- Contraindicated for patients with hypertension, heart failure, renal insufficiency or hypokalemia
- Adverse effects include hypertension, edema, hypokalemia, cardiac enlargement, etc.
- Monitoring includes blood pressure, weight, fluid status, electrolytes, etc.
V. Calcium and Vitamin D Medications
A. Calcium Supplements
- Provide calcium ions for various physiological functions such as bone formation and maintenance, muscle contraction and nerve transmission
- Commonly used medications include calcium carbonate, calcium citrate, calcium gluconate, etc.
- Indicated for conditions such as osteoporosis prevention and treatment, hypocalcemia, etc.
- Contraindicated for patients with hypercalcemia, renal calculi or sarcoidosis
- Adverse effects include constipation, nausea, abdominal pain, kidney stones, etc.
- Monitoring includes serum calcium levels and renal function
B. Vitamin D Supplements
- Facilitate the absorption of calcium and phosphorus from the intestine and promote bone mineralization
- Commonly used medications include cholecalciferol (vitamin D3), calcitriol (active form of vitamin D), ergocalciferol (vitamin D2), etc.
- Indicated for conditions such as vitamin D deficiency or insufficiency, rickets, osteomalacia, etc.
- Contraindicated for patients with hypercalcemia or hypersensitivity to the drugs
- Adverse effects include hypercalcemia, hyperphosphatemia, anorexia, nausea, etc.
- Monitoring includes serum calcium and phosphorus levels and renal function.
- The adverse effects of this therapy also depend on the class of medication. Some common adverse effects are hypoglycemia, gastrointestinal disturbances (such as nausea, vomiting, diarrhea), weight gain or loss, edema (fluid retention), anemia (low red blood cell count), lactic acidosis (a serious condition of high blood lactate levels), hepatotoxicity (liver damage), pancreatitis (inflammation of the pancreas), urinary tract infections, and genital infections.
- Oral antidiabetic medications require regular monitoring of blood glucose levels and hemoglobin A1c levels (a measure of average blood glucose levels over three months). They also require adjustment of dosage based on factors such as renal or hepatic function, drug interactions, and adverse effects.
Conclusion
- Pharmacology is an essential part of nursing practice and requires a thorough understanding of the effects of drugs on the body systems.
- This study guide aims to help you review the key concepts and principles of pharmacology for specific body systems and prepare you for exams and clinical practice.
- By completing this study guide, you should be able to identify the main classes of drugs for each system, describe their pharmacokinetics and pharmacodynamics, and apply your knowledge to patient care situations.
Summary
- This study guide covers the pharmacology of five major body systems: cardiovascular, respiratory, gastrointestinal, nervous and endocrine.
- Each system has a different function and is affected by different types of medications.
- The study guide explains the mechanisms of action, indications, contraindications, adverse effects and interactions of the most common drugs used for each system.
- The study guide also provides examples of clinical scenarios and practice questions to test your knowledge and application skills.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Pharmacology of Specific Body Systems
This filled cannot be empty

