Please set your exam date
Eating and Obsessive-Compulsive Disorders
Study Questions
Eating disorders
A nurse is providing education to a group of adolescents about eating disorders. Which statement by one of the participants indicates a need for further education?
Explanation
Choice A rationale:
This choice is accurate. Eating disorders, such as anorexia nervosa, bulimia nervosa, and binge eating disorder, can indeed lead to serious medical and psychological consequences. Individuals with these disorders may experience electrolyte imbalances, heart problems, gastrointestinal issues, and severe emotional distress.
Choice B rationale:
This choice is accurate. Eating disorders are more common among adolescents and young adults. These age groups are particularly vulnerable due to factors like body image concerns, peer pressure, and societal influences that emphasize thinness.
Choice C rationale:
This choice is accurate. Eating disorders are influenced by a combination of biological, psychological, environmental, and cultural factors. Genetic predisposition, psychological stressors, societal beauty standards, and family dynamics can all contribute to the development of eating disorders.
Choice D rationale:
This choice is incorrect. Eating disorders do not exclusively affect females. While historically, eating disorders have been associated with females, males can also develop eating disorders. The prevalence of eating disorders in males has been increasing, emphasizing the need to recognize and address these disorders in all genders.
Explanation
Choice A rationale:
This choice is accurate. Recurrent episodes of binge eating, characterized by consuming large amounts of food within a discrete period and feeling a lack of control, are a hallmark symptom of bulimia nervosa.
Choice B rationale:
This choice is accurate. Inappropriate compensatory behaviors, such as self-induced vomiting, misuse of laxatives, diuretics, or other medications, and excessive exercise, are used by individuals with bulimia nervosa to counteract the effects of binge eating and prevent weight gain.
Choice C rationale:
This choice is incorrect. In contrast to anorexia nervosa, individuals with bulimia nervosa often maintain a normal or slightly above normal body weight. This is due to the cycle of binge eating and compensatory behaviors that can offset significant weight loss.
Choice D rationale:
This choice is accurate. Individuals with bulimia nervosa experience a sense of lack of control over eating during binge episodes. This feeling of being unable to stop eating distinguishes binge eating from occasional overeating.
Choice E rationale:
This choice is accurate. Acknowledgment of the problem is a common aspect of bulimia nervosa. Many individuals with the disorder recognize that their eating patterns are abnormal and distressing, which can lead them to seek help.
Explanation
Choice A rationale:
This choice is inappropriate. In anorexia nervosa, encouraging the client to eat more may not address the underlying psychological and emotional issues related to the disorder. It oversimplifies the complexity of the disorder and could further exacerbate the client's anxiety about weight gain.
Choice B rationale:
This choice is inappropriate. Telling the client to stop restricting food intake oversimplifies the challenges of anorexia nervosa. Recovery involves addressing both the physical and psychological aspects of the disorder, and such a statement may not provide the necessary support and understanding.
Choice C rationale:
This choice is accurate. This statement acknowledges the client's fear of gaining weight while also emphasizing the importance of their health. It demonstrates empathy and understanding while promoting a balanced perspective on the client's concerns.
Choice D rationale:
This choice is inappropriate. Encouraging the client to exercise more as a way to increase appetite overlooks the fact that anorexia nervosa is not solely about appetite suppression. The disorder involves complex psychological factors that cannot be addressed through simple solutions like increased exercise.
Explanation
Choice A rationale:
Ineffective Coping is the most appropriate nursing diagnosis for a client with binge eating disorder who reports feeling guilty and depressed after episodes of binge eating. Binge eating disorder is characterized by recurrent episodes of consuming large amounts of food within a discrete period, accompanied by a sense of loss of control. The guilt and depression reported by the client are emotional responses to these episodes. Ineffective Coping reflects the client's inability to manage and adapt to these negative emotions in a healthy manner. It addresses the psychological distress that often accompanies binge eating behaviors.
Choice B rationale:
Disturbed Body Image is not the most appropriate nursing diagnosis for this client. While individuals with binge eating disorder may experience body dissatisfaction due to weight gain resulting from their binge episodes, the primary focus of this client's distress is on feelings of guilt and depression, which are better captured by the Ineffective Coping diagnosis.
Choice C rationale:
Imbalanced Nutrition: More Than Body Requirements is not the most suitable nursing diagnosis for this client. While binge eating disorder involves excessive food consumption during episodes, the diagnosis of Imbalanced Nutrition is usually reserved for clients who have issues with nutrient intake that lead to alterations in physical health, such as obesity or malnutrition.
Choice D rationale:
Risk for Impaired Skin Integrity related to dental erosion is not the most relevant nursing diagnosis for this client. While binge eating may lead to dental erosion over time due to frequent exposure to stomach acid during episodes, this choice does not address the primary psychological concerns of guilt and depression.
Explanation
Choice A rationale:
Significant weight loss or failure to achieve expected weight gain is consistent with the diagnosis of avoidant/restrictive food intake disorder (ARFID) ARFID is characterized by a lack of interest in eating or food, avoidance based on sensory characteristics of food, concern about the aversive consequences of eating, and avoidance of foods due to a previous negative experience. This avoidance can lead to inadequate nutrient intake and, consequently, significant weight loss or the inability to achieve expected weight gain, especially in children.
Choice B rationale:
Recurrent episodes of binge eating followed by inappropriate compensatory behaviors are not indicative of avoidant/restrictive food intake disorder (ARFID) This behavior is more characteristic of bulimia nervosa, which involves cycles of binge eating followed by behaviors like vomiting, laxative use, or excessive exercise to compensate for the overeating.
Choice C rationale:
Persistent eating of nonnutritive, nonfood substances is a characteristic of pica disorder, not avoidant/restrictive food intake disorder (ARFID) Pica involves the consumption of substances such as dirt, paint, hair, or cloth, which have no nutritional value.
Choice D rationale:
Repeated regurgitation of food is a characteristic of rumination disorder, not avoidant/restrictive food intake disorder (ARFID) Rumination disorder involves the regurgitation of food that is then either re-chewed, re-swallowed, or spit out, without an associated medical condition.
Explanation
Choice B rationale:
Normal or slightly above normal body weight is a characteristic of anorexia nervosa. Anorexia nervosa is an eating disorder characterized by a distorted body image and an intense fear of gaining weight, leading to self-imposed starvation and significant weight loss. Despite being underweight or emaciated, individuals with anorexia nervosa often perceive themselves as overweight or obese, which is a key feature of the disorder.
Choice A rationale:
Recurrent episodes of binge eating are characteristic of bulimia nervosa, not anorexia nervosa. In bulimia nervosa, individuals engage in episodes of binge eating followed by behaviors to compensate for the overeating, such as vomiting, laxative use, or excessive exercise.
Choice C rationale:
Lack of interest in eating or food is not a characteristic of anorexia nervosa. This symptom aligns more closely with avoidant/restrictive food intake disorder (ARFID), where individuals have a lack of interest in eating due to sensory sensitivities or other aversive experiences related to food.
Choice D rationale:
Repeated regurgitation of food is a characteristic of rumination disorder, which is a separate eating disorder and is not a defining feature of anorexia nervosa.
Explanation
Recurrent episodes of binge eating followed by inappropriate compensatory behaviors.
Choice A rationale:
Eating large amounts of food when not feeling physically hungry is not a characteristic of bulimia nervosa. While individuals with bulimia nervosa do experience episodes of binge eating, this behavior is not dependent on physical hunger.
Choice B rationale:
Recurrent episodes of binge eating followed by inappropriate compensatory behaviors are indeed a characteristic of bulimia nervosa. Binge eating involves consuming a large amount of food in a short period, accompanied by a sense of lack of control. The compensatory behaviors, such as vomiting, laxative use, or excessive exercise, are aimed at counteracting the perceived consequences of the binge eating, such as weight gain.
Choice C rationale:
Persistent eating of nonnutritive, nonfood substances, known as pica, is not a characteristic of bulimia nervosa. Pica is a separate eating disorder that involves the consumption of non-food items such as hair, paper, or soil.
Choice D rationale:
Recurrent purging behavior to influence weight or shape is more closely associated with the eating disorder anorexia nervosa. While purging behaviors like vomiting or using laxatives can also occur in bulimia nervosa, they are not specific to it.
Explanation
Eating until feeling uncomfortably full.
Choice A rationale:
Eating until feeling uncomfortably full is a characteristic of binge eating disorder. Binge eating involves consuming an excessive amount of food within a discrete period while feeling a lack of control over eating. This often results in physical discomfort due to the large quantity of food consumed.
Choice B rationale:
Recurrent episodes of binge eating followed by inappropriate compensatory behaviors are more characteristic of bulimia nervosa, not binge eating disorder. In binge eating disorder, there is no consistent use of inappropriate compensatory behaviors such as vomiting or excessive exercise to counteract the binge episodes.
Choice C rationale:
Eating more rapidly than normal can be a characteristic of binge eating episodes, but it is not a defining feature of binge eating disorder. Binge eating disorder is primarily characterized by the consumption of large amounts of food within a short period and the sense of lack of control during these episodes.
Choice D rationale:
Recurrent episodes of night eating is not a characteristic of binge eating disorder. Night eating disorder is a separate condition characterized by consuming a significant portion of daily caloric intake during the nighttime hours.
Questions
.
Explanation
Altered levels of leptin and ghrelin.
Choice A rationale:
Increased levels of cortisol and thyroid hormones are not commonly associated with eating disorders. Cortisol is a stress hormone, and while stress can play a role in eating behaviors, it is not a consistent physiological change across all eating disorders. Thyroid hormones play a role in metabolism, but their direct link to eating disorders is limited.
Choice B rationale:
Decreased levels of growth hormone and insulin are not commonly associated with eating disorders. Growth hormone and insulin are primarily involved in growth regulation and glucose metabolism, respectively, and their alterations are not central to the core characteristics of eating disorders.
Choice C rationale:
Altered levels of leptin and ghrelin are commonly associated with eating disorders. Leptin is a hormone that regulates appetite and signals satiety. Individuals with eating disorders may have disrupted leptin levels, contributing to disturbances in appetite and hunger regulation. Ghrelin is a hormone that stimulates appetite, and its dysregulation can also play a role in eating disorder behaviors.
Choice D rationale:
Elevated levels of sex hormones and growth hormone are not consistently associated with eating disorders. While some hormonal changes can occur due to malnutrition and extreme weight loss, they are not universally seen across all individuals with eating disorders. The hormonal changes seen in eating disorders are more often related to appetite regulation and metabolism.
Explanation
Choice A rationale:
Gastric emptying. Gastric emptying refers to the process by which the stomach contents are emptied into the small intestine. While it can be affected by various factors, such as the type of food consumed, it's not a typical gastrointestinal symptom associated with eating disorders. Eating disorders often involve disturbances in eating behaviors, body image, and psychological aspects rather than the mechanical process of gastric emptying.
Choice B rationale:
Constipation and diarrhea. Constipation and diarrhea can be associated with various gastrointestinal conditions, but they are not the hallmark symptoms of eating disorders. In some cases, individuals with anorexia nervosa might experience constipation due to low food intake, but this is not a defining feature of eating disorders as a whole.
Choice C rationale:
Abdominal pain and bloating. Abdominal pain and bloating are common gastrointestinal symptoms in individuals with eating disorders, particularly those who engage in binge eating or consume large amounts of food in a short period. The discomfort from overeating or consuming excessive amounts of food can lead to abdominal pain and bloating. Additionally, purging behaviors, such as self-induced vomiting, can also cause irritation to the stomach lining and result in abdominal pain.
Choice D rationale:
Nausea and vomiting. Nausea and vomiting are indeed common symptoms in individuals with eating disorders, especially those with bulimia nervosa. The act of binge eating followed by purging through vomiting is a key characteristic of this disorder. However, the question is asking about gastrointestinal symptoms typically associated with eating disorders in general, and not all individuals with eating disorders engage in purging behaviors.
Explanation
Choice A rationale:
"I might need to be hospitalized to stabilize my physical condition." Hospitalization is often necessary for individuals with severe eating disorders, such as anorexia nervosa with significant medical complications. Inpatient treatment might be required to stabilize the patient's physical condition, provide proper nutrition, and address any medical complications arising from malnutrition.
Choice B rationale:
"Psychotherapy and medication can help address the psychological aspects of my disorder." Psychotherapy, often including cognitive-behavioral therapy (CBT), and medication can indeed play crucial roles in treating eating disorders. These approaches help address the underlying psychological factors contributing to the disorder and aid in promoting healthier eating behaviors. This statement indicates that the patient understands the comprehensive nature of treatment.
Choice C rationale:
"Relapse prevention strategies are not necessary once I have recovered." This statement is indicative of a misunderstanding about the nature of eating disorders. Relapse prevention strategies are essential to maintain recovery and prevent relapse. Eating disorders have a psychological component, and individuals need to continue practicing healthy behaviors, coping skills, and strategies even after they have made progress in their recovery journey.
Choice D rationale:
"Social support, such as family involvement or peer support, can be helpful in maintaining recovery." Social support is indeed valuable for individuals with eating disorders. Engaging with family, friends, or support groups can contribute to the maintenance of recovery. The statement reflects an accurate understanding of the role of social support in the treatment and recovery process.
Explanation
Choice A rationale:
Stabilizing the patient's physical condition. For individuals with severe eating disorders, especially anorexia nervosa, the priority is often to address their physical health and stabilize any medical complications arising from malnutrition. This might involve medical interventions, nutritional rehabilitation, and closely monitoring vital signs to prevent serious health consequences.
Choice B rationale:
Addressing the psychological aspects of the disorder. While addressing the psychological aspects is an integral part of treating eating disorders, it's crucial to prioritize physical health when dealing with severe cases. Malnutrition can lead to various medical complications, including electrolyte imbalances, organ damage, and cardiac issues. Without addressing the physical health first, psychological interventions might be less effective.
Choice C rationale:
Preventing relapse and maintaining recovery. Preventing relapse and maintaining recovery are important aspects of long-term treatment, but they become more relevant after the patient's physical condition has been stabilized. Once the immediate physical risks are minimized, efforts can shift toward addressing psychological factors and developing strategies to prevent relapse.
Choice D rationale:
Providing ongoing follow-up care. Ongoing follow-up care is essential for individuals with eating disorders to ensure that they continue to progress in their recovery journey and to monitor any potential relapse signs. However, this becomes more pertinent once the patient's physical condition has been stabilized and initial treatment has been provided.
Explanation
Choice A rationale:
Bradycardia and tachycardia. While these cardiovascular symptoms can occur in eating disorders, they are more commonly associated with anorexia nervosa rather than bulimia nervosa. Bradycardia (slow heart rate) is often seen in individuals with severe anorexia due to the body's adaptive response to conserve energy. Tachycardia (rapid heart rate) can occur as a compensatory mechanism in response to dehydration and electrolyte imbalances, particularly in those with anorexia. However, in bulimia nervosa, the rapid cycle of binge eating and purging is more likely to lead to electrolyte imbalances that cause other symptoms.
Choice B rationale:
Hypertension and mitral valve prolapse. Hypertension (high blood pressure) is not a common cardiovascular symptom of bulimia nervosa. Mitral valve prolapse, which involves the improper closing of the heart's mitral valve, is also not a typical cardiovascular manifestation of bulimia nervosa. Eating disorders primarily affect the electrical conduction system of the heart and can lead to rhythm disturbances.
Choice C rationale:
Orthostatic hypotension and arrhythmias. This is the correct choice. Orthostatic hypotension, which is a drop in blood pressure upon standing, is a common cardiovascular symptom of bulimia nervosa. It is often a result of dehydration and electrolyte imbalances caused by frequent vomiting and laxative use. Arrhythmias (irregular heart rhythms) can also occur due to electrolyte imbalances, particularly low levels of potassium, which can disrupt the heart's electrical activity.
Choice D rationale:
Pericardial effusion and cardiomyopathy. While pericardial effusion (accumulation of fluid around the heart) and cardiomyopathy (disease of the heart muscle) can occur in individuals with eating disorders, they are not the most common cardiovascular symptoms. These conditions usually result from prolonged malnutrition and severe electrolyte imbalances, which can occur in both anorexia nervosa and bulimia nervosa. However, orthostatic hypotension and arrhythmias are more characteristic of bulimia nervosa.
Explanation
Choice A rationale:
Increased levels of cortisol and thyroid hormones. While stress-induced changes in cortisol levels can be seen in individuals with eating disorders, they are not the primary pathophysiological changes associated with these disorders. Cortisol plays a role in the body's response to stress and can contribute to weight gain, but altered levels of other hormones have a more direct impact on eating behaviors in individuals with eating disorders.
Choice B rationale:
Decreased levels of growth hormone and insulin. Growth hormone and insulin do play a role in metabolism and growth, but their levels are not commonly altered in eating disorders in the same way that hormones like leptin and ghrelin are. Altered levels of growth hormone and insulin can lead to metabolic disturbances, but these are not the hallmark changes seen in individuals with eating disorders.
Choice C rationale:
Altered levels of leptin and ghrelin. This is the correct choice. Leptin and ghrelin are two hormones that play a significant role in regulating hunger and satiety. Leptin, produced by adipose tissue, signals to the brain when energy stores are sufficient, thereby reducing appetite. Ghrelin, produced by the stomach, stimulates appetite and promotes food intake. In individuals with eating disorders, these hormones can become dysregulated, leading to disrupted hunger and fullness cues, and contributing to the development and maintenance of the disorder.
Choice D rationale:
Elevated levels of sex hormones and growth hormone. Elevated levels of sex hormones are not a primary pathophysiological change associated with eating disorders. Growth hormone, while important for growth and metabolism, is not a central player in the hormonal changes that drive eating disorder behaviors. Leptin and ghrelin are more directly involved in the dysregulation of eating behaviors seen in these disorders.
Explanation
Choice A rationale:
Stabilizing the patient's physical condition. This is the correct choice. In the treatment of anorexia nervosa, it is crucial to address the medical complications that arise from severe malnutrition and weight loss. Refeeding and restoring the patient's nutritional status are top priorities to prevent further health deterioration. This often requires a structured refeeding plan and medical monitoring to ensure gradual weight gain and avoid refeeding syndrome, a potentially life-threatening condition that can occur when nutrients are reintroduced too rapidly.
Choice B rationale:
Addressing the psychological aspects of the disorder. Addressing the psychological aspects of anorexia nervosa is indeed an essential component of treatment, but it usually comes after stabilizing the patient's physical condition. The distorted body image, fear of weight gain, and other psychological factors need to be addressed in therapy and counseling during the recovery process. However, attempting to address these psychological aspects before stabilizing the patient's physical health can be challenging and less effective.
Choice C rationale:
Preventing relapse and maintaining recovery. Preventing relapse and maintaining recovery are important treatment goals in the long-term management of anorexia nervosa. However, these goals typically come into play once the patient's physical condition has been stabilized and nutritional rehabilitation has been initiated. Long-term therapy, support groups, and follow-up care are crucial to prevent relapse and maintain progress.
Choice D rationale:
Providing ongoing follow-up care. Providing ongoing follow-up care is indeed a necessary aspect of treating anorexia nervosa. After the initial stabilization and intensive treatment phase, ongoing monitoring, therapy, and medical follow-up are vital to support the patient's sustained recovery. However, just offering ongoing follow-up care without addressing the immediate medical needs and nutritional rehabilitation would not be sufficient in treating the acute phase of anorexia nervosa.
Explanation
Choice A rationale:
The main goal of treatment for eating disorders is to correct nutritional deficiencies and address medical complications. Many individuals with eating disorders suffer from severe malnutrition due to inadequate food intake, and this can lead to a range of medical issues such as electrolyte imbalances, cardiac problems, and organ dysfunction. Prioritizing the correction of these physical health issues is essential to ensure the patient's immediate well-being and prevent further deterioration.
Choice B rationale:
While restoring normal eating patterns is an important aspect of treating eating disorders, it is not the main goal. Normalizing eating habits and reestablishing a healthy relationship with food are crucial steps in the recovery process, but these efforts often come after addressing the immediate medical concerns.
Choice C rationale:
Addressing underlying psychological issues is an integral part of eating disorder treatment, but it is not the main goal as specified in the question. Psychological issues like distorted body image, low self-esteem, and anxiety play a significant role in perpetuating eating disorders. Therapeutic interventions and counseling are employed to tackle these underlying issues, but they are typically part of a comprehensive treatment plan that includes medical stabilization.
Choice D rationale:
Preventing relapse is an important long-term goal in eating disorder treatment, but it is not the primary focus when considering the immediate and acute phase of treatment. Relapse prevention strategies become more prominent as patients progress in their recovery journey and work towards maintaining their newfound health and well-being.
Explanation
Choice A rationale:
Altered activity of serotonin, dopamine, and norepinephrine is a common neurobiological change associated with eating disorders. These neurotransmitters play key roles in mood regulation, reward pathways, and appetite control. Altered levels of these neurotransmitters can contribute to the development and maintenance of disordered eating behaviors.
Choice B rationale:
Altered structure and function of brain regions involved in processing hunger and satiety are commonly observed in individuals with eating disorders. Brain areas such as the hypothalamus, amygdala, and prefrontal cortex, which are responsible for regulating appetite, emotions, and decision-making, can exhibit changes in their neural activity and connectivity due to the impact of prolonged malnutrition and distorted eating behaviors.
Choice C rationale:
Altered connectivity and communication between brain regions and networks is another neurobiological change seen in eating disorders. The brain operates through complex networks, and disruptions in the communication between different regions can lead to dysfunctional behaviors and cognitive processes related to eating and body image.
Choice D rationale:
This choice is correct. All of the aforementioned changes—altered neurotransmitter activity, changes in brain structure and function, and altered connectivity between brain regions—are commonly observed in individuals with eating disorders. These neurobiological alterations underscore the complex interplay between biological, psychological, and environmental factors in the development and progression of these disorders.
Explanation
Choice A rationale:
In the treatment of anorexia nervosa, stabilizing the patient's physical condition takes precedence as the first priority. Individuals with anorexia often experience severe weight loss, malnutrition, electrolyte imbalances, and other medical complications that can be life-threatening. Therefore, the initial focus is on restoring the patient's health and preventing any immediate physical harm.
Choice B rationale:
While addressing the psychological aspects of the disorder is crucial, it comes after stabilizing the patient's physical condition. Psychological interventions, therapy, and counseling are essential components of treatment, but they can be more effective once the individual's body is in a more stable and nourished state.
Choice C rationale:
Preventing relapse and maintaining recovery is an important long-term goal in treating anorexia nervosa, but it is not the first priority. After stabilizing the patient's physical health, efforts are directed toward helping the individual develop coping strategies, address distorted body image, and establish healthier eating patterns to prevent relapse in the future.
Choice D rationale:
Providing ongoing follow-up care is important throughout the recovery process, but it is not the primary focus in the initial treatment of anorexia nervosa. Once the patient's physical condition is stabilized, follow-up care becomes valuable for monitoring progress, adjusting treatment strategies, and providing continued support.
Questions
.
Explanation
Choice A rationale:
Monitoring vital signs and weight may be relevant in the assessment of a patient with an eating disorder, especially if their condition has led to physical complications. However, it is not the primary nursing responsibility in this context. The emotional and psychological aspects of care are of higher priority.
Choice B rationale:
Providing emotional support and promoting self-esteem is crucial in the assessment of a patient with an eating disorder. Patients with eating disorders often struggle with body image issues and low self-esteem. Offering emotional support can help build a therapeutic relationship and create a safe environment for the patient to express their feelings and concerns.
Choice C rationale:
Assessing nutritional needs and developing a meal plan is indeed important in managing eating disorders. However, in the context of assessment, it is a secondary responsibility that comes after addressing the patient's emotional well-being. Establishing trust and understanding the psychological factors at play are fundamental before delving into nutritional planning.
Choice D rationale:
Respecting the patient's beliefs and values is a fundamental aspect of nursing care across all contexts, including eating disorders. While respecting beliefs and values is essential, it is not the primary nursing responsibility specifically in the assessment phase of a patient with an eating disorder.
Explanation
Choice A rationale:
Monitoring vital signs and weight is important, but it primarily falls under the medical management of the patient's condition rather than within the scope of nursing interventions for promoting psychological well-being in a care plan for eating disorders.
Choice B rationale:
Providing positive reinforcement for eating is appropriate as patients with eating disorders often struggle with food-related anxieties. Positive reinforcement can encourage them to establish healthier eating habits and reduce fear around food.
Choice C rationale:
Teaching coping skills and stress management techniques is essential. Many patients with eating disorders use disordered eating behaviors as coping mechanisms. Providing alternative coping strategies can help them manage stress without resorting to unhealthy behaviors.
Choice D rationale:
Involving the family in the treatment process can be beneficial. Eating disorders can affect not only the individual but also the family dynamics. Educating the family about the disorder, its triggers, and how to provide support can contribute to the patient's overall recovery.
Choice E rationale:
Respecting the patient's beliefs and values is crucial in building trust and rapport. It helps create a patient-centered approach that considers their individual preferences and cultural factors when developing and implementing the care plan.
Explanation
Choice A rationale:
This response oversimplifies the issue and places the blame on the patient's behavior. It may contribute to feelings of guilt and shame, hindering open communication about their struggles.
Choice B rationale:
While the intention behind this response is positive, it reinforces the patient's focus on appearance. It's important to shift the focus from external appearance to overall health and well-being.
Choice C rationale:
This response is empathetic and acknowledges the common struggle that individuals with eating disorders face. It validates the patient's feelings while also indicating that they are not alone in their experiences.
Choice D rationale:
This response dismisses the patient's concerns and implies that their feelings are insignificant. It's essential to validate and address the patient's feelings rather than deflecting their concerns.
Explanation
Choice A rationale:
Telling the patient, "You need to eat to maintain your health," is directive and may come across as dismissive of the patient's concerns. This response doesn't address the patient's fear and could potentially increase their resistance.
Choice B rationale:
Saying, "You're not overweight. You don't need to worry about gaining weight," disregards the patient's feelings and trivializes their anxiety. It's essential to acknowledge their fear and provide appropriate information and support.
Choice C rationale:
This is the correct response. Acknowledging the patient's fear while also emphasizing the potential harm of not eating is empathetic and informative. It opens the door for further discussion and education about the consequences of disordered eating.
Choice D rationale:
Responding with, "You should focus on something other than your weight," avoids addressing the patient's concerns and feelings. It's crucial to address their fears in a supportive and educational manner.
Explanation
Choice A rationale:
This is the correct action to take. Evaluating the effectiveness of nursing interventions involves reassessing the patient's condition and comparing it to the expected outcomes. This step helps determine whether the interventions are producing the desired results and if any adjustments are needed.
Choice B rationale:
While documenting the nursing assessment, diagnosis, and plan is essential for maintaining accurate patient records, it is not the most direct action for evaluating the effectiveness of interventions. Documentation supports continuity of care but doesn't provide immediate insight into intervention outcomes.
Choice C rationale:
Involving the family in the treatment process (choice C) can be important for a patient's overall well-being, but it doesn't directly address the evaluation of nursing interventions. Family involvement is more related to the planning and implementation stages of care.
Choice D rationale:
Consulting with other members of the multidisciplinary team is a collaborative approach to patient care, but it's not the primary action for evaluating the effectiveness of nursing interventions. Team collaboration contributes to comprehensive care but doesn't directly assess intervention outcomes.
Explanation
Choice A rationale:
Monitoring vital signs and weight (choice A) is crucial for patients with eating disorders, but it focuses mainly on the physical aspect of care. The emotional and psychological aspects are equally important and need attention.
Choice B rationale:
This is the correct intervention. Patients with eating disorders often struggle with body image and self-esteem issues. Providing emotional support and promoting self-esteem can contribute to their overall well-being and recovery.
Choice C rationale:
Assessing nutritional needs and developing a meal plan (choice C) is an essential component of care for patients with eating disorders. However, it primarily addresses the physical aspect of the disorder and doesn't fully encompass the emotional and psychological dimensions.
Choice D rationale:
Respecting the patient's beliefs and values (choice D) is a fundamental aspect of patient-centered care, but it's not the most specific intervention for addressing the complex needs of someone with an eating disorder. Additional supportive actions are necessary.
Explanation
Choice A rationale:
Monitoring vital signs and weight. While monitoring vital signs and weight is an essential aspect of patient care, it primarily focuses on the physical health of the patient. In the case of an eating disorder, the underlying psychological and emotional issues also need attention, which is not addressed solely by monitoring vital signs and weight. The patient's emotional well-being and coping strategies are equally important in promoting overall recovery.
Choice B rationale:
Providing positive reinforcement for eating. Positive reinforcement can be helpful in encouraging desired behaviors; however, focusing solely on positive reinforcement for eating might oversimplify the complexities of treating an eating disorder. Eating disorders are often rooted in psychological factors, and addressing the underlying causes and emotions is crucial. Providing positive reinforcement might not address the emotional challenges the patient is facing, and a more comprehensive approach is needed.
Choice C rationale:
Teaching coping skills and stress management techniques. This is the correct choice. Eating disorders are often connected to emotional distress, poor body image, and stress. Teaching coping skills and stress management techniques empowers the patient to develop healthier ways of dealing with emotions and triggers that may contribute to their eating disorder. By addressing the emotional aspect, the patient is better equipped to manage their disorder and work towards recovery.
Choice D rationale:
Involving the family in the treatment process. Involving the family in the treatment process can be beneficial, as family support is important for recovery. However, it's not the most appropriate intervention on its own. Eating disorders are complex and individualized, and addressing the patient's personal coping mechanisms and emotional well-being should be the primary focus. Family involvement can be part of a comprehensive treatment plan, but it should not replace teaching the patient coping skills and stress management techniques.
Explanation
Choice A rationale:
"You should try to eat healthier and exercise more." This response oversimplifies the patient's feelings and may come across as dismissive of their struggles. It implies that the solution is solely based on diet and exercise, neglecting the deeper psychological aspects of body image dissatisfaction and eating disorders.
Choice B rationale:
"You're not fat, you're beautiful just the way you are." While well-intentioned, this response still focuses on the patient's physical appearance. It's important to acknowledge the patient's feelings without solely focusing on their external beauty. Additionally, this response might not address the underlying psychological issues contributing to their negative self-perception.
Choice C rationale:
"I understand how you feel. Many people with eating disorders struggle with body image." This is the correct choice. This response shows empathy and understanding while validating the patient's feelings. It also acknowledges the common struggle that individuals with eating disorders have regarding body image. By acknowledging the emotional aspect of the patient's statement, the nurse opens the door for further conversation and support.
Choice D rationale:
"You need to stop worrying about your weight and focus on other things." This response might come across as dismissive and invalidating. It implies that the patient's concerns are unwarranted, which can be harmful. Eating disorders involve complex emotional factors, and simply telling the patient to focus on something else ignores the underlying issues that need to be addressed.
Explanation
Choice A rationale:
Only the patient's medical status. Focusing solely on the patient's medical status neglects the psychological and emotional factors that are often at the root of eating disorders. Treating only the medical symptoms without addressing the underlying mental health issues might lead to incomplete recovery.
Choice B rationale:
Only the patient's nutritional needs. While addressing nutritional needs is important, it's just one aspect of a comprehensive approach to treating eating disorders. Neglecting the psychological and emotional aspects can limit the effectiveness of the treatment and the patient's overall well-being.
Choice C rationale:
Only the patient's mental status. Eating disorders involve not only the patient's mental status but also their physical health and overall well-being. Focusing exclusively on the mental aspect might miss important medical and nutritional considerations necessary for a holistic approach to care.
Choice D rationale:
Both physical and psychological aspects. This is the correct choice. Eating disorders are multifaceted, affecting both the body and the mind. To provide holistic care, the nurse must assess and address the patient's physical health, mental well-being, emotional struggles, and psychological factors contributing to the disorder. A comprehensive approach considers all these elements to provide effective and well-rounded care.
Choice E rationale:
Only the patient's social interactions. While social interactions can play a role in an individual's mental and emotional health, focusing solely on social interactions neglects the equally important physical and psychological components of eating disorders. Holistic care involves addressing multiple dimensions of the patient's experience. Sure, let's go through each question and its provided choices along with the rationales:
Explanation
Choice A rationale:
The statement "You should just focus on physical recovery for now." neglects the psychological aspect of the patient's condition. Eating disorders are complex and involve both physical and psychological components, so focusing solely on physical recovery is not effective.
Choice B rationale:
The statement "You need to follow the meal plan exactly as it is." might come across as rigid and lacking empathy. It doesn't address the patient's emotional struggles and distorted beliefs about food and body image.
Choice C rationale:
The statement "I understand that distorted body image can be challenging." shows empathy and acknowledges the psychological aspect of the disorder. It demonstrates that the nurse comprehends the patient's experience and is willing to provide psychological support.
Choice D rationale:
The statement "You should isolate yourself from group therapy sessions." is counterproductive. Group therapy can be highly beneficial for individuals with eating disorders, as it provides a supportive environment and helps combat the isolation often experienced by these patients.
Explanation
Choice A rationale:
The response "You're right, you shouldn't be eating." reinforces the client's negative and harmful belief about not deserving to eat. This response is not therapeutic and can worsen the client's condition.
Choice B rationale:
The response "Don't worry, your weight is not a concern." dismisses the client's feelings and doesn't address the underlying distorted thoughts about their body and food. It's important to acknowledge their emotions rather than trivialize them.
Choice C rationale:
The response "It sounds like you have negative thoughts about your body." shows empathy and reflective listening. It opens the door for further discussion about the client's feelings and allows the nurse to explore their thought patterns.
Choice D rationale:
The response "Eating is not important, we should focus on your medication." minimizes the significance of the client's eating disorder and focuses solely on medication, disregarding the psychological and nutritional aspects of treatment.
Explanation
Choice A rationale:
Prescribing medications for the patient is not a key responsibility of the nurse in this context. While nurses may administer medications, the prescription and management of medications typically fall under the purview of medical doctors or advanced practice nurses.
Choice B rationale:
Isolating the patient from family involvement is not a key responsibility of the nurse. In fact, involving the patient's family and support system is often beneficial for the patient's recovery in the context of an eating disorder.
Choice C rationale:
Sharing information and coordinating care is a key responsibility of the nurse when collaborating with a multidisciplinary team for a patient with an eating disorder. The nurse acts as a central point of communication, ensuring that all members of the team are informed about the patient's condition, treatment plan, and progress. This helps create a comprehensive and coordinated approach to care.
Choice D rationale:
Referring the patient to only a dietitian is not sufficient in addressing the complex needs of a patient with an eating disorder. While dietitians play an important role, the nurse's responsibility involves a broader scope of care coordination and collaboration with various team members.
Choice E rationale:
Exclusively participating in team meetings is not the sole responsibility of the nurse. While team meetings are important, the nurse's role extends beyond attending meetings and includes hands-on patient care, communication, and coordination of care activities.
Explanation
Choice A rationale:
Allowing the client to continue avoiding meals to reduce stress is not a suitable nursing intervention. It perpetuates the unhealthy behavior and does not contribute to the client's recovery.
Choice B rationale:
Providing positive reinforcement for not eating to encourage progress is also not appropriate. Positive reinforcement should be directed towards healthy behaviors rather than reinforcing the avoidance of meals.
Choice C rationale:
Supervising meals and snacks to prevent food refusal or hiding is an essential nursing intervention. Patients with eating disorders often engage in secretive behaviors related to food, so supervision helps ensure that they are receiving the necessary nutrition and support their recovery.
Choice D rationale:
Advising the client to eat alone to avoid social pressure is not a recommended intervention. Eating disorders thrive on isolation, and encouraging the client to eat alone could exacerbate the issue.
A client with an eating disorder has a distorted body image and irrational beliefs. What therapeutic approach should the nurse use to address this issue?
Explanation
Choice A rationale:
Ignoring the client's beliefs to avoid escalating distress is not a therapeutic approach. Addressing cognitive distortions and irrational beliefs is crucial in helping the client reframe their thoughts and promote healthier behaviors.
Choice B rationale:
Encouraging the client to engage in self-isolation is counterproductive. Isolation can worsen the client's condition and hinder their recovery.
Choice C rationale:
Addressing cognitive distortions and irrational beliefs is the appropriate therapeutic approach. This involves working with the client to identify and challenge negative thought patterns, helping them develop a more realistic perception of their body image and self-worth.
Choice D rationale:
Avoiding discussing body image to prevent embarrassment is not effective. Open and sensitive discussions about body image are important in the therapeutic process to help the client gain insight into their feelings and beliefs.
Obsessive-compulsive disorders
Explanation
C.
Choice A rationale:
Providing physical care only. This choice is not the correct answer. Collaborating on care for a client with an eating disorder involves more than just providing physical care. Eating disorders are complex mental health issues that require a multidisciplinary approach, addressing both physical and psychological aspects.
Choice B rationale:
Sharing information and coordinating care. This is a correct answer. Collaborating with the multidisciplinary team is crucial in caring for clients with eating disorders. Sharing information and coordinating care among various healthcare professionals, such as therapists, dietitians, physicians, and psychologists, ensures a holistic approach to treatment. Eating disorders often have psychological, nutritional, and medical components that need to be addressed collectively.
Choice C rationale:
Making referrals exclusively to physicians. This choice is not entirely accurate. While physicians may be part of the multidisciplinary team, collaborating on eating disorder cases goes beyond just making referrals to physicians. Other specialists, such as therapists, dietitians, and psychologists, play essential roles in the comprehensive care of these clients.
Choice D rationale:
Administering medications without consulting others. This choice is not the correct answer. Administering medications without consulting the multidisciplinary team can be dangerous, especially in cases of eating disorders where medication management might interact with other aspects of treatment. Collaborative decision-making helps prevent adverse interactions and ensures that all aspects of care are considered.
Choice E rationale:
Participating in team meetings. This is a correct answer. Participating in team meetings is vital for effective collaboration in the care of clients with eating disorders. These meetings provide an opportunity to discuss the client's progress, adjust treatment plans, and share insights from different perspectives. Regular communication among team members promotes a well-rounded approach to care.
Explanation
Choice A rationale:
Impaired social interaction. This choice is not the most appropriate nursing diagnosis for a client with obsessive-compulsive disorder (OCD) experiencing recurrent thoughts about contamination. OCD primarily involves anxiety-driven behaviors and rituals rather than impaired social interaction.
Choice B rationale:
Anxiety. This is the correct answer. Given that the client is experiencing recurrent thoughts about contamination, the most appropriate nursing diagnosis is anxiety. OCD is characterized by intrusive thoughts and rituals driven by anxiety. Addressing the anxiety component is essential for effective treatment.
Choice C rationale:
Risk for self-harm. While individuals with severe OCD may experience distress, the given information does not indicate an immediate risk for self-harm. Anxiety is the more relevant issue in this scenario.
Choice D rationale:
Obsessive-compulsive disorder. This choice describes the client's condition rather than a nursing diagnosis. Nursing diagnoses are used to identify specific client problems that nurses can address through care and interventions.
Explanation
Choice A rationale:
Teach the client relaxation techniques. While teaching relaxation techniques can be beneficial, it may not directly address the client's compulsion to wash their hands repeatedly. OCD involves managing distressing thoughts and compulsions through specific interventions.
Choice B rationale:
Encourage the client to talk about their thoughts and feelings. While promoting open communication is generally important, it may not be the most effective intervention for directly addressing the client's compulsion to wash their hands. OCD interventions often involve exposure and response prevention strategies.
Choice C rationale:
Assist the client in developing a hierarchy of feared situations. This is the correct answer. Helping the client develop a hierarchy of feared situations is a key intervention in addressing OCD. This approach is part of exposure and response prevention therapy, where clients gradually face their fears without engaging in compulsive behaviors.
Choice D rationale:
Praise the client for decreasing the frequency of handwashing. While positive reinforcement can be useful, it may not be the priority intervention for someone with OCD. The focus should be on structured interventions that challenge and reduce the compulsive behaviors over time.
Explanation
Choice A rationale:
Telling the client "It's okay, you don't have to wash your hands" might invalidate the client's feelings and fears, leading to increased anxiety. The client's compulsion to wash their hands is driven by their obsessive thoughts, and dismissing this behavior can be counterproductive.
Choice B rationale:
The correct response acknowledges the client's anxiety and opens a conversation about their feelings. This approach helps build a therapeutic relationship and provides an opportunity for the client to express their concerns. It's essential to address the underlying anxieties associated with OCD to promote better coping strategies.
Choice C rationale:
Telling the client to "calm down and stop thinking about washing your hands" oversimplifies the situation. People with OCD often struggle with controlling their obsessive thoughts and compulsions, and such a directive can be ineffective and frustrating for the client.
Choice D rationale:
Offering to "help you wash your hands" reinforces the client's compulsion rather than addressing the root cause of their anxiety. Enabling their compulsive behavior can contribute to the maintenance of their OCD symptoms.
Explanation
Choice A rationale:
Encouraging the client to "talk about their fears" might be a beneficial intervention in some cases, but for individuals with OCD who are struggling with compulsive behaviors driven by their fears, directly addressing exposure to those fears is a more effective approach.
Choice B rationale:
While setting limits on the client's behavior is important, it may not be the priority in this situation. Instead, assisting the client in gradually confronting their fears through exposure therapy can help them develop healthier coping mechanisms.
Choice C rationale:
The correct response emphasizes gradual exposure therapy, a well-established approach in treating OCD. This intervention helps the client confront their fears in a controlled and systematic manner, leading to desensitization and reduction in their anxiety over time.
Choice D rationale:
Providing relaxation techniques can be helpful for managing anxiety, but for someone with OCD who is avoiding situations due to contamination fears, the primary intervention should focus on exposure therapy to address the specific OCD-related fears.
Explanation
Choice A rationale:
Taking the SSRI in the morning might be recommended to mitigate potential sleep disturbances related to the medication. However, the client's reported difficulty sleeping is likely influenced by factors beyond the timing of medication administration.
Choice B rationale:
The correct response addresses lifestyle modifications that can improve sleep quality. Caffeine and alcohol are known to disrupt sleep, especially when taken close to bedtime. Avoiding these substances can promote better sleep for the client.
Choice C rationale:
Regular exercise can indeed contribute to improved sleep, but its effect might vary for individuals. While exercise can be part of a healthy routine, it might not directly address the client's reported difficulty sleeping due to the SSRI.
Choice D rationale:
Taking a warm bath before bed can promote relaxation and potentially aid in sleep, but it might not be as effective in resolving the client's specific sleep problems related to SSRI use.
Explanation
Choice A rationale:
The statement "I have to check the locks on the door 10 times before I can leave my house" is indicative of checking compulsions often seen in OCD. This involves repetitive behaviors performed to reduce distress, such as checking locks multiple times. However, this choice is less likely because it focuses on checking rather than washing.
Choice B rationale:
The correct answer. This statement reflects a common manifestation of OCD, specifically contamination-related obsessions and cleaning compulsions. The client's fear of getting sick from not washing their hands is a classic example of obsessive thoughts leading to repetitive behaviors aimed at reducing anxiety.
Choice C rationale:
The statement "I think I'm going crazy because I keep thinking about these things" indicates the presence of intrusive and distressing thoughts, which are characteristic of OCD. However, this choice does not encompass the compulsive behaviors that are essential for an OCD diagnosis. It primarily highlights the emotional distress associated with the thoughts.
Choice D rationale:
The statement "I'm not sure if I'm really sick or if I'm just imagining it" suggests uncertainty and doubt, which are common features of OCD. However, this choice does not emphasize the typical compulsions that accompany OCD. It focuses more on self-doubt rather than specific ritualistic behaviors.
A nurse is reviewing the medical record of a client with OCD. Which of the following findings is most likely to be present in the client's record?
Explanation
Choice A rationale:
Family history of OCD is a significant risk factor for developing the disorder. Genetic predisposition plays a role in the etiology of OCD, with a higher likelihood of the disorder occurring in individuals who have close relatives (e.g., parents or siblings) with the condition. While environmental factors and life experiences can contribute to OCD, they are not as directly linked as the genetic component.
Choice B rationale:
History of childhood trauma can contribute to the development of various mental health disorders, including anxiety and OCD. However, the strongest association with OCD is the genetic component. While childhood trauma can exacerbate symptoms in individuals who are genetically predisposed, it is not the most likely finding in the medical record of a client with OCD.
Choice C rationale:
Head injury can lead to neurological and psychological changes, potentially contributing to various psychiatric conditions. However, the primary cause of OCD is not head injury. It is important to consider the presence of other factors, especially the genetic predisposition, when attributing OCD to a particular cause.
Choice D rationale:
Brain tumor is an organic condition that can cause neurological and psychological symptoms. However, brain tumors are not a common or primary cause of OCD. The focus in the etiology of OCD is on neurotransmitter imbalances, genetic factors, and brain circuitry, rather than structural brain abnormalities like tumors.
Explanation
Choice A rationale:
Exposure and response prevention is a cornerstone of cognitive-behavioral therapy (CBT) for OCD. It involves exposing the individual to anxiety-provoking situations (exposure) and then preventing the usual compulsive response that reduces anxiety (response prevention) This helps the individual learn that their feared outcomes are unlikely to occur and that their anxiety will diminish over time without engaging in rituals.
Choice B rationale:
Systematic desensitization is a technique used to treat phobias and anxiety disorders by gradually exposing the individual to their feared stimuli while teaching relaxation techniques. While it may have some applicability in OCD treatment, it is not as directly aligned with the core features of OCD as exposure and response prevention.
Choice C rationale:
Flooding is a therapeutic technique that involves exposing the individual to an extreme level of their fear in order to diminish the anxiety response over time. While this approach might be used in certain anxiety disorders, it is not typically the first-line intervention for OCD. Exposure and response prevention is a more gradual and controlled technique that is better suited for OCD treatment.
Choice D rationale:
Thought stopping involves interrupting obsessive thoughts by using cues or distractions. This technique is not as effective in treating OCD as exposure and response prevention, which directly addresses the connection between obsessions and compulsions. Thought stopping may not provide the individual with a comprehensive strategy for managing their OCD symptoms.
Explanation
Choice A rationale:
The limbic circuit consisting of the hippocampus, amygdala, and hypothalamus is not the main brain circuit involved in obsessive-compulsive disorders (OCDs) The limbic circuit is more closely associated with emotions and memory, rather than the cognitive processes that drive OCD symptoms.
Choice B rationale:
The central executive circuit comprising the prefrontal cortex and temporal lobes is responsible for higher-level cognitive functions like decision-making and working memory. However, this circuit is not primarily implicated in the pathophysiology of OCD.
Choice C rationale:
The correct choice. The cortico-striato-thalamo-cortical (CSTC) circuit plays a central role in the development of OCD. This circuit involves several key components: Orbitofrontal cortex: Responsible for assessing potential risks and rewards, and for decision-making. Anterior cingulate cortex: Involved in error detection, emotional processing, and regulating cognitive flexibility. Striatum: Responsible for habit formation and reward-based learning. Thalamus: Acts as a relay station for information between various brain regions. This circuit's malfunction can lead to repetitive behaviors and intrusive thoughts characteristic of OCD.
Choice D rationale:
The ventral tegmental circuit involving the substantia nigra and ventral tegmental area is primarily associated with the brain's reward system and the regulation of mood and motivation. It is not a key player in OCD's pathophysiology.
Explanation
Choice A rationale:
While fear of heights and open spaces leading to avoidance behaviors can be associated with anxiety disorders, it is not a typical theme for obsessions and compulsions in individuals with OCD. OCD themes usually revolve around repetitive thoughts and behaviors that aim to alleviate distress or prevent feared outcomes.
Choice B rationale:
The repeated checking of the stove being turned off before leaving the house is a common obsession and compulsion in individuals with OCD. This behavior stems from the fear of potential harm or danger (e.g., fire) and the compulsive act of checking is performed to reduce anxiety related to the obsession.
Choice C rationale:
Feeling the need to touch every object in a room an equal number of times is another manifestation of OCD. This behavior is driven by the obsession of achieving symmetry, balance, or a sense of completeness through compulsive rituals like touching.
Choice D rationale:
Persistent worry about a loved one's safety causing ritualistic prayers is also a theme seen in OCD. Individuals may feel compelled to engage in repetitive prayers or rituals to protect their loved ones from harm due to their obsessive fears.
Choice E rationale:
The strong desire to organize items by color, shape, and size is more indicative of perfectionism or certain personality traits rather than a typical theme in OCD. OCD usually involves distressing and unwanted thoughts (obsessions) and the corresponding rituals or repetitive behaviors (compulsions) aimed at reducing the distress.
Explanation
Choice A rationale:
The statement "I always arrange my books on the shelf from tallest to shortest" doesn't indicate an obsession. This behavior might suggest a preference for orderliness or arranging things systematically, but it lacks the distressing, unwanted nature of obsessions.
Choice B rationale:
"I feel an overwhelming urge to wash my hands every 30 minutes" indicates a compulsion rather than an obsession. The urge to wash hands frequently is driven by the need to alleviate anxiety or distress, which is the hallmark of compulsive behaviors.
Choice C rationale:
"I have a ritual of counting to 10 before entering any room" is also a compulsion. The ritual of counting serves as a way to reduce anxiety or prevent a feared outcome associated with entering a room, suggesting a compulsive behavior.
Choice D rationale:
The statement "I keep having thoughts that my family will get hurt if I don't touch the doorknob three times" reflects an obsession. The distressing thought of family harm is the unwanted obsession, and the ritual of touching the doorknob three times is the compulsion aimed at reducing the anxiety caused by the obsession.
Explanation
Choice A rationale:
The nurse should not tell the client to stop their behaviors immediately, as this approach is likely to increase anxiety and distress. Individuals with obsessive-compulsive disorder (OCD) often find it challenging to abruptly stop their compulsions, and attempting to do so can lead to heightened anxiety.
Choice B rationale:
Distracting oneself from the urge to perform compulsions might provide temporary relief, but it does not address the underlying issues of OCD. It is essential to work on strategies that target the reduction of compulsions and the management of anxiety associated with them.
Choice C rationale:
Giving in to compulsions might temporarily relieve anxiety, but it reinforces the cycle of OCD behavior. Encouraging the client to give in to compulsions is counterproductive to the treatment of OCD, which involves breaking the pattern of compulsive behavior.
Choice D rationale:
This is the correct choice. Collaboratively developing strategies to gradually reduce compulsive behaviors is a standard approach in treating OCD. This method is aligned with exposure and response prevention therapy, a well-established treatment for OCD. By gradually facing the situations that trigger obsessive thoughts and then refraining from performing compulsions, clients can learn to manage their anxiety and reduce their reliance on compulsive behaviors.
Explanation
Choice A rationale:
This choice accurately reflects one of the criteria for diagnosing OCD. The obsessions (intrusive and distressing thoughts) and compulsions (repetitive behaviors or mental acts) experienced by individuals with OCD are usually connected to what they are trying to neutralize or prevent. For instance, if someone has an obsessive fear of contamination, their compulsions might involve excessive hand washing to neutralize this fear.
Choice B rationale:
While perfectionism and high standards can be associated with OCD, they are not a primary diagnostic criterion. OCD is characterized by the presence of obsessions and compulsions that cause distress and significantly interfere with a person's daily life.
Choice C rationale:
This option is incorrect. The disturbance in OCD is not attributed to the physiological effects of substances or other medical conditions. It is a distinct mental health condition that is not solely a result of substance use or another medical issue.
Choice D rationale:
This option is incorrect. The symptoms of OCD should not be better explained by the symptoms of another mental disorder. While comorbidities can exist, OCD has its own unique set of obsessions and compulsions that differentiate it from other mental disorders.
Explanation
Choice A rationale:
Discarding possessions easily, regardless of their value, is not characteristic of hoarding disorder. Hoarding disorder involves the persistent difficulty in parting with possessions, even if they have little value, due to the emotional attachment individuals feel toward these items.
Choice B rationale:
Accumulating possessions without any emotional attachment is not indicative of hoarding disorder. In hoarding disorder, emotional attachment to possessions is a hallmark feature, and individuals often experience distress at the thought of discarding items.
Choice C rationale:
This is the correct choice. Hoarding disorder is characterized by the strong need to save items, regardless of their practical value, and the significant distress experienced when attempting to discard them. This behavior leads to the accumulation of possessions and can result in living spaces becoming cluttered and uninhabitable.
Choice D rationale:
Organizing possessions meticulously to maintain a clutter-free environment is not consistent with hoarding disorder. People with hoarding disorder struggle with organization and often have difficulty maintaining clutter-free spaces due to the accumulation of possessions.
A client with body dysmorphic disorder (BDD) is explaining their experiences to a nurse. Which statements by the client indicate symptoms of BDD? Select all that apply.
Explanation
Choice A rationale:
This choice does not indicate symptoms of Body Dysmorphic Disorder (BDD) Feeling sad about being overweight is not specific to BDD and could be related to body dissatisfaction or other emotional concerns.
Choice B rationale:
This choice indicates a symptom of BDD. Constantly comparing one's appearance to that of celebrities suggests a preoccupation with perceived flaws, which is a hallmark of BDD. Individuals with BDD often engage in such comparisons as a way to validate their negative self-image.
Choice C rationale:
While spending excessive time in front of the mirror can be a symptom of BDD, the statement alone does not definitively indicate the disorder. It's important to consider the reason behind the mirror checking behavior and the individual's emotional distress related to it.
Choice D rationale:
This choice indicates a symptom of BDD. Avoiding social situations due to the fear of being negatively evaluated or judged based on one's perceived flaws is a classic sign of BDD. Individuals with BDD often believe that others are fixated on their perceived defects.
Choice E rationale:
This choice does not indicate symptoms of BDD. Having a collection of items without attaching sentimental value is not specific to BDD. It's important to focus on behaviors and thoughts related to perceived physical flaws when assessing for BDD.
A nurse is providing care to a client with trichotillomania (hair-pulling disorder) What intervention would be most appropriate to include in the client's care plan?
Explanation
Choice A rationale:
Encouraging suppression of the urge to pull hair might worsen the client's anxiety and tension associated with trichotillomania. This approach may not address the underlying issues and could lead to increased distress.
Choice B rationale:
Camouflaging hair loss can be a practical approach, but it does not address the compulsive behavior itself. It focuses on hiding the consequences of the disorder rather than addressing the core issue.
Choice C rationale:
Assisting the client in finding replacement behaviors is the most appropriate intervention. This approach helps redirect the urge to pull hair into healthier alternatives, helping the client manage the compulsive behavior in a constructive manner.
Choice D rationale:
Avoiding mirrors might be counterproductive. For some individuals with trichotillomania, avoiding mirrors might increase anxiety and preoccupation, as they may feel disconnected from their appearance. It's important to address the underlying behavior rather than avoiding triggers.
Explanation
Choice A rationale:
Obsessions and compulsions in OCD are ego-dystonic, not ego-syntonic. Ego-dystonic refers to thoughts, feelings, or behaviors that are perceived as incompatible with one's self-concept. In OCD, individuals recognize that their obsessions and compulsions are irrational and unwanted, which causes distress.
Choice B rationale:
The connection of obsessions and compulsions to positive outcomes is not a distinguishing factor for OCD. In fact, obsessions and compulsions often lead to distress and interfere with daily functioning.
Choice C rationale:
The presence of distress or impairment is a key factor that helps differentiate OCD from other mental disorders. Unlike some other conditions where the behaviors or thoughts might not distress the individual, OCD is characterized by the distress caused by the irrational and unwanted obsessions and compulsions.
Choice D rationale:
This choice is the correct answer. Individuals with OCD recognize that their obsessions and compulsions are irrational and excessive, but they struggle to control them. This recognition is a hallmark of OCD and helps differentiate it from other conditions where the person might not be aware of the irrationality of their behavior.
Explanation
Choice A rationale:
Obsessions and compulsions are aimed at reducing anxiety or distress. This statement accurately describes a characteristic of obsessive-compulsive disorder (OCD) Obsessions are intrusive and unwanted thoughts, images, or urges that cause significant distress, while compulsions are repetitive behaviors or mental acts aimed at reducing the distress caused by the obsessions. These behaviors are performed in response to the distress and are intended to alleviate it. For example, if someone has an obsession about contamination, their compulsion might involve excessive hand washing to alleviate the anxiety associated with the obsession.
Choice B rationale:
Obsessions and compulsions are consistent with the individual's self-image. This statement is not accurate in differentiating OCD from other mental disorders. Obsessions and compulsions in OCD often involve themes that are inconsistent with the individual's self-image and are not representative of their true desires or intentions. For instance, someone with OCD might have obsessions about harming others, even if they have no actual desire to do so. These obsessions are not aligned with their self-image.
Choice C rationale:
The individual recognizes that obsessions and compulsions are irrational. This statement accurately describes another characteristic of OCD. People with OCD typically recognize that their obsessions and compulsions are irrational and unreasonable, but they feel compelled to engage in these behaviors to alleviate anxiety. This recognition of the irrational nature of their thoughts and actions is a distinguishing feature of OCD, differentiating it from other disorders where the person might not have such insight into the irrationality of their behaviors.
Choice D rationale:
Obsessions and compulsions may lead to positive emotional outcomes. This statement is not accurate in the context of OCD. Obsessions and compulsions are not aimed at achieving positive emotional outcomes. Instead, they are performed to reduce distress or anxiety. The relief gained from engaging in compulsions is temporary and often followed by a cycle of escalating compulsions to achieve the same level of relief, which contributes to the perpetuation of the disorder.
Choice E rationale:
Obsessions and compulsions cause impairment in daily functioning. This statement accurately describes another characteristic of OCD. The obsessions and compulsions associated with OCD can be time-consuming and interfere significantly with a person's daily activities, relationships, and overall quality of life. These behaviors can lead to impaired occupational and social functioning, making this statement a distinguishing feature of OCD.
Explanation
Choice A rationale:
"Exposure and response prevention involves avoiding the triggers that lead to obsessions and compulsions." This statement is incorrect. Exposure and response prevention (ERP) in cognitive-behavioral therapy (CBT) for OCD involves facing the situations or triggers that lead to anxiety and obsessions. Instead of avoiding these triggers, individuals purposefully confront them to gradually reduce their anxiety response and break the cycle of performing compulsions in response to obsessions.
Choice B rationale:
"During exposure and response prevention, you'll engage in the compulsive behaviors to reduce anxiety gradually." This statement is also incorrect. ERP focuses on gradually reducing and eventually eliminating compulsive behaviors, not engaging in them. The goal is to help individuals learn that their anxiety naturally decreases over time when they refrain from performing the compulsions, ultimately breaking the connection between obsessions and anxiety-driven behaviors.
Choice C rationale:
"Exposure and response prevention helps you face the situations that trigger anxiety while preventing the compulsive behaviors." This statement accurately explains how exposure and response prevention works in treating OCD. During ERP, individuals purposefully confront situations that trigger their obsessions while refraining from engaging in compulsive behaviors. By doing so, they learn that their anxiety decreases without the need for compulsions, helping to weaken the link between obsessions and anxiety.
Choice D rationale:
"In exposure and response prevention, we eliminate all exposure to the situations that cause distress and anxiety." This statement is incorrect. ERP involves controlled exposure to distressing situations or triggers, not complete avoidance. The goal is to help individuals build tolerance to the anxiety triggered by these situations while resisting the urge to perform compulsions.
Explanation
Choice A rationale:
"SSRIs primarily target glutamate modulation in the brain." This statement is inaccurate. Selective serotonin reuptake inhibitors (SSRIs) primarily target the modulation of serotonin levels in the brain, not glutamate. These medications work by inhibiting the reuptake of serotonin, which increases the availability of serotonin in the synaptic cleft and helps regulate mood and anxiety.
Choice B rationale:
"SSRIs work by increasing the availability of serotonin in the brain to reduce obsessions and compulsions." This statement accurately describes the role of SSRIs in treating OCD. Serotonin is a neurotransmitter that plays a role in mood regulation, and imbalances in serotonin have been implicated in OCD. By increasing the availability of serotonin in the brain, SSRIs can help reduce the frequency and intensity of obsessions and compulsions.
Choice C rationale:
"SSRIs are used to enhance positive emotional outcomes in individuals with OCD." This statement is not accurate. While SSRIs can improve mood and reduce anxiety, their primary role in treating OCD is to alleviate the symptoms of obsessions and compulsions by affecting neurotransmitter levels. They are not specifically used to enhance positive emotional outcomes.
Choice D rationale:
"SSRIs are reserved for individuals who have ego-syntonic obsessions and compulsions." This statement is incorrect. Ego-syntonic obsessions and compulsions are those that are consistent with a person's self-image and beliefs, and individuals may not feel a strong need to resist or change them. SSRIs are used to treat both ego-dystonic (inconsistent with self-image) and ego-syntonic obsessions and compulsions in OCD, as these medications target the underlying neurochemical imbalances that contribute to the disorder's symptoms.
Explanation
Choice A rationale:
The observation that the client's obsessions and compulsions are consistent with their self-image would not necessarily support the diagnosis of OCD. This could be applicable to other mental disorders as well, where the symptoms align with the individual's self-concept.
Choice B rationale:
If the client engages in compulsions to achieve pleasurable outcomes, this might suggest a different perspective. OCD compulsions are typically performed to alleviate distress or prevent a feared event, not for achieving pleasure.
Choice C rationale:
If the client's obsessions and compulsions are not causing significant distress, this could point towards other disorders or even potentially normal behavior. OCD is characterized by the distress caused by the obsessions and the urge to perform compulsions to alleviate this distress.
Choice D rationale:
The correct answer. In OCD, individuals are aware that their obsessions and compulsions are irrational and excessive. This self-awareness differentiates OCD from other disorders where the beliefs and behaviors might be seen as reasonable by the individual.
Explanation
Choice A rationale:
The statement that higher medication doses are needed to quickly suppress all obsessive thoughts and compulsive behaviors is not accurate. Medication dosages are adjusted based on individual response and tolerability, and the goal is not necessarily to use the highest dose possible.
Choice B rationale:
The correct answer. Starting with a low dose is a common practice in psychiatric medication management. This helps the body adjust to the medication gradually, reducing the likelihood and severity of side effects. As the body becomes accustomed to the medication, the dose can be gradually increased to achieve the desired therapeutic effect.
Choice C rationale:
The goal of achieving complete relief from obsessions and compulsions within a few days is an unrealistic expectation. Psychiatric medications typically require time to take effect, often several weeks, and complete relief might not occur for all individuals.
Choice D rationale:
Explanation
Choice A rationale:
The statement that medication will provide immediate relief from all symptoms is an overgeneralization. While medication can help alleviate symptoms, the relief might not be immediate and might not cover all symptoms comprehensively.
Choice B rationale:
Medication modifying self-image and values is not a recognized benefit of pharmacological treatment for OCD. This choice does not align with the established mechanisms of action of the medications used for OCD.
Choice C rationale:
The correct answer. Medication's potential to reduce the severity of obsessions and compulsions is a relevant benefit to highlight. While it might not eliminate symptoms entirely, it can make them more manageable and improve the individual's overall quality of life.
Choice D rationale:
The statement that medication will eliminate the need for any psychotherapeutic interventions is overly optimistic. A comprehensive treatment approach for OCD often includes a combination of medication and psychotherapy for optimal results.
Explanation
Choice D rationale:
The type and severity of OCD, along with the client's preferences and tolerance, are key factors that influence the choice of medication for treating OCD. OCD symptoms can vary widely between individuals, and different medications may be more effective for specific symptom profiles. Additionally, the severity of symptoms and potential side effects of medications should be carefully considered. Client preferences and tolerances play a crucial role in treatment adherence and success. Collaborative decision-making between the client and healthcare provider ensures that the chosen medication aligns with the individual's needs and goals.
Choice A rationale:
While enhancing positive emotional outcomes is a desired effect of treatment, it's not a direct factor that influences the choice of medication for treating OCD. The choice of medication is primarily based on its mechanism of action and its demonstrated efficacy in targeting OCD symptoms.
Choice B rationale:
Completely eliminating all obsessions and compulsions immediately is often not a realistic expectation for OCD treatment. Medications and psychotherapeutic approaches aim to reduce the severity and frequency of symptoms, improve overall functioning, and enhance quality of life.
Choice C rationale:
Ego-syntonic obsessions and compulsions are those that are consistent with the individual's sense of self and values, making them less distressing and more difficult to recognize as irrational. While addressing ego-syntonic symptoms is important, this factor alone does not dictate the choice of medication. The overall symptom profile and the medication's mechanism of action are more influential factors.
Explanation
Choice A rationale:
Blood pressure regulation is not directly related to the outcomes for patients with obsessive-compulsive disorder (OCD) OCD primarily involves persistent, unwanted thoughts and repetitive behaviors, and blood pressure regulation is not a priority outcome for this condition.
Choice B rationale:
Pain management is also not relevant to the outcomes of patients with OCD. OCD doesn't cause physical pain, so pain management interventions would not be included in the Nursing Outcomes Classification (NOC) for OCD patients.
Choice C rationale:
Coping and self-esteem improvement is the correct choice. Individuals with OCD often struggle with managing their distressing thoughts and compulsive behaviors. Improving coping mechanisms and enhancing self-esteem are important goals in the care of these patients. The NOC would include outcomes related to helping patients develop healthier ways of managing their thoughts and behaviors, thereby improving their overall quality of life.
Choice D rationale:
Respiratory function optimization is unrelated to the outcomes of patients with OCD. This outcome is more relevant to conditions affecting the respiratory system, such as asthma or chronic obstructive pulmonary disease (COPD), and not to OCD.
Explanation
Choice A rationale:
Administering pain medication is not a relevant intervention for a patient with obsessive-compulsive disorder (OCD) OCD is a mental health disorder characterized by obsessions and compulsions, and administering pain medication would not address the core symptoms or needs of these patients.
Choice B rationale:
Providing emotional support is a valid intervention for a patient with OCD. Individuals with OCD often experience high levels of anxiety and distress due to their obsessive thoughts and compulsive behaviors. Offering emotional support can help the patient feel understood and less isolated, contributing to their overall well-being.
Choice C rationale:
Teaching relaxation techniques is also appropriate for patients with OCD. Relaxation techniques can help individuals manage their anxiety and stress, which are common features of OCD. These techniques, when incorporated into the patient's coping strategies, can contribute to reducing the severity of their symptoms.
Choice D rationale:
Assisting with physical therapy exercises is not directly relevant to the care of a patient with OCD. OCD primarily involves psychological and behavioral symptoms, and physical therapy exercises would not directly address the core concerns of these patients.
Choice E rationale:
Educating about nutrition is not a priority intervention for OCD patients. While maintaining overall health is important, nutritional education is not a central component of managing obsessive-compulsive disorder.
Explanation
Choice A rationale:
This statement indicates a need for further education. For medications used to treat OCD, consistent and regular dosing is important for their effectiveness. Taking medication only when feeling anxious could lead to inconsistent blood levels of the medication, potentially diminishing its therapeutic effects.
Choice B rationale:
The statement "I should report any side effects to my doctor" is accurate and does not indicate a need for further education. Reporting side effects to the doctor is a responsible and informed approach to medication management.
Choice C rationale:
The statement "It's important to continue taking my medication even if I start feeling better" is correct. Often, individuals with OCD may experience improvement in symptoms but need to continue the medication regimen to maintain the positive effects and prevent relapse.
Choice D rationale:
The statement "I'll stop taking my medication if I experience any discomfort" indicates a need for further education. Discomfort is a broad term that could encompass various mild side effects or adjustments that might be necessary when starting a new medication. It's important not to discontinue medication abruptly without consulting a healthcare provider.
Explanation
Choice A rationale:
Avoiding situations that cause anxiety is counterproductive in exposure therapy, which is a common treatment for OCD. Exposure therapy involves gradual and controlled exposure to feared stimuli to reduce anxiety. Avoidance reinforces the anxiety response and prevents habituation. Facing the situations that trigger anxiety is crucial for desensitization.
Choice B rationale:
This choice is correct because exposure therapy for OCD involves facing feared situations while refraining from engaging in compulsions. Compulsions are repetitive behaviors or mental acts that a person feels driven to perform in response to an obsession or according to rigid rules. By gradually exposing the individual to these situations and preventing them from performing compulsions, the anxiety response diminishes over time.
Choice C rationale:
Telling the patient that their fears will go away on their own is inaccurate and dismissive of the distress that OCD can cause. OCD is a chronic condition that typically requires evidence-based interventions for symptom reduction. Ignoring the fears and hoping they will disappear without intervention is not a valid therapeutic approach.
Choice D rationale:
Focusing only on situations that are easy to tolerate would not be effective in exposure therapy. The essence of exposure therapy is to confront situations that provoke anxiety gradually, starting with less anxiety-provoking situations and progressing to more challenging ones. This process helps the individual build resilience against anxiety triggers.
Explanation
Choice A rationale:
Teaching the client about the history of OCD might provide insight into the disorder's background, but it is not the priority when the client is currently experiencing distress. Addressing the immediate distress takes precedence over historical information.
Choice B rationale:
This choice is correct because relaxation techniques can help alleviate the client's distress in the moment. These techniques, such as deep breathing, progressive muscle relaxation, or mindfulness exercises, can help the client manage their anxiety and reduce the impact of obsessive thoughts.
Choice C rationale:
While providing information about medication options is important, it might not be the initial intervention when the client is in a state of distress. Medication discussions are typically part of a comprehensive treatment plan and should be addressed after addressing the client's immediate distress.
Choice D rationale:
Initiating exposure therapy sessions might exacerbate the client's distress at this point. Exposure therapy involves deliberately confronting feared situations, and it's important to prepare the client for this type of intervention before initiating it. Starting with relaxation techniques is a more appropriate approach.
Explanation
Choice A rationale:
While genetic factors can contribute to the development of OCD, stating that it is solely caused by genetic factors oversimplifies the etiology. OCD is a complex disorder with multiple factors, including genetic, neurobiological, cognitive, and environmental influences.
Choice B rationale:
This statement is incorrect. Exposure therapy is a highly effective treatment for OCD. It involves controlled and systematic exposure to feared stimuli, which helps individuals reduce their anxiety responses over time.
Choice C rationale:
This choice is correct because selective serotonin reuptake inhibitors (SSRIs) are indeed commonly used as a first-line pharmacological treatment for OCD. These medications help regulate serotonin levels in the brain, which can reduce the frequency and intensity of obsessions and compulsions.
Choice D rationale:
Cognitive-behavioral therapy (CBT) is actually recommended as one of the most effective treatments for OCD. CBT, including exposure and response prevention, helps individuals learn to manage their symptoms by changing maladaptive thought patterns and behaviors associated with OCD. Therefore, stating that CBT is not recommended is inaccurate.
Explanation
Choice A rationale:
Telling the client to ignore the intrusive thoughts is not a therapeutic response. It dismisses the client's concerns and offers no constructive help in managing their distressing thoughts.
Choice B rationale:
Stating that intrusive thoughts are a normal part of everyone's thinking might invalidate the client's distress and does not provide practical strategies for dealing with their OCD symptoms.
Choice C rationale:
This is the correct choice. Acknowledging the client's concerns and offering to work on strategies to manage the thoughts is a therapeutic response. Collaboratively addressing the issue empowers the client to take an active role in their treatment.
Choice D rationale:
Dismissing the client's worries by saying there's no need to worry about the thoughts undermines their feelings and doesn't address the distress caused by the thoughts.
Explanation
Choice A rationale:
Sharing patient information without consent violates patient privacy and confidentiality. This goes against ethical and legal standards in healthcare.
Choice B rationale:
This is a correct choice. Communicating treatment progress to the healthcare team ensures everyone is informed and can provide coordinated care. Collaboration and information sharing are important for comprehensive patient management.
Choice C rationale:
Referring the patient to support groups is a collaborative action that can provide additional avenues of help and coping strategies. Support groups can offer a sense of community and understanding among individuals facing similar challenges.
Choice D rationale:
Excluding the patient from treatment decisions contradicts patient-centered care and shared decision-making principles. Collaboration involves involving the patient in their own care.
Choice E rationale:
Coordinating medication adjustments is a collaborative action as medications are often managed by healthcare professionals such as doctors or nurse practitioners. Adjustments should be made collectively to ensure the best outcome for the patient.
(Select All That Apply):. A nurse is assessing a group of clients for their understanding of treatment approaches for OCDs. Which options accurately describe cognitive-behavioral therapy (CBT) and its components? Select all that apply.
Explanation
Choice A rationale:
Cognitive-behavioral therapy (CBT) often involves exposing individuals to feared stimuli or situations in a controlled and gradual manner, a technique known as exposure therapy. This exposure helps individuals confront their anxieties and gradually reduce their distress over time. Exposure therapy is a cornerstone of CBT for anxiety disorders, including OCD.
Choice C rationale:
Exposure and response prevention (ERP) is a critical component of CBT for OCD. This technique involves exposing the individual to anxiety-provoking situations or thoughts (exposure) while preventing the usual compulsive responses (response prevention). Through repeated exposures without engaging in compulsions, the individual learns that their anxiety naturally decreases over time, leading to habituation to the anxiety-provoking stimuli.
Choice E rationale:
Cognitive therapy within CBT aims to challenge and modify cognitive distortions and unrealistic beliefs that underlie OCD. Individuals with OCD often have distorted thought patterns, such as catastrophic thinking or black-and-white reasoning. Cognitive therapy helps individuals recognize and reframe these distorted thoughts, leading to more adaptive and realistic thinking patterns.
Choice B rationale:
This choice is not accurate. CBT does not primarily focus on replacing distorted thoughts with unrealistic beliefs. Instead, it focuses on identifying and modifying irrational or negative thought patterns.
Choice D rationale:
While CBT does aim to enhance positive emotional outcomes, this choice is not entirely accurate in describing the main goal of CBT for OCD. The primary goal of CBT is to reduce the symptoms and distress associated with obsessions and compulsions by addressing the cognitive and behavioral factors that maintain the disorder.
(Select All That Apply):. A nurse is teaching a group of patients about pharmacological interventions for OCDs. Which medications are commonly used to treat OCDs? Select all that apply.
Explanation
Choice C rationale:
Risperidone is an atypical antipsychotic medication that is sometimes used as an augmentation strategy in treating OCD, particularly in cases where there are prominent obsessive-compulsive symptoms that are not well-controlled by other interventions. However, it's important to note that risperidone's use in OCD is off-label, meaning it's not approved by regulatory agencies specifically for OCD treatment.
Choice D rationale:
Selective serotonin reuptake inhibitors (SSRIs) are a cornerstone of pharmacological treatment for OCD. These medications, such as fluoxetine, sertraline, and fluvoxamine, increase the availability of serotonin in the brain and help alleviate obsessive-compulsive symptoms. They have been extensively studied and are considered first-line treatment options.
Choice A rationale:
Venlafaxine is a serotonin-norepinephrine reuptake inhibitor (SNRI) commonly used to treat depression and anxiety disorders. While it may have some benefit for anxiety symptoms, including those related to OCD, it is not considered a first-line treatment for OCD. SSRIs have shown greater efficacy for OCD management.
Choice B rationale:
Tricyclic antidepressants (TCAs) were among the first medications used to treat OCD. However, their side effect profiles and the availability of more effective and better-tolerated options, such as SSRIs, have led to TCAs being used less frequently for OCD treatment.
Choice E rationale:
Dopamine agonists are not commonly used for OCD treatment. In fact, they can potentially exacerbate symptoms, as imbalances in dopamine transmission are implicated in the pathophysiology of OCD. Using dopamine agonists without a clear rationale could worsen the condition.
(Select all that apply). A client with OCD is experiencing impaired self-esteem due to their obsessions and compulsions. Which actions should the nurse take to promote the client's self-esteem?
Explanation
Choice A rationale:
Encouraging the client to challenge negative thoughts is an effective cognitive-behavioral approach. It helps the client reframe their thinking patterns and build healthier self-esteem.
Choice B rationale:
Providing a list of alternative compulsions supports the client in finding healthier ways to cope with their anxiety. This can lead to a sense of accomplishment and improved self-esteem.
Choice C rationale:
Suggesting complete avoidance of anxiety triggers might seem helpful, but in the context of OCD, avoidance can reinforce the obsessions and compulsions. Gradual exposure and response prevention are evidence-based strategies.
Choice D rationale:
Assigning more exposure therapy sessions should be based on the client's progress and therapist's assessment. Increasing sessions solely for the sake of it might not be effective and could lead to frustration.
Choice E rationale:
Acknowledging the client's efforts in therapy fosters a positive therapeutic relationship and boosts their self-esteem. Recognizing progress and hard work encourages continued engagement in treatment.
Exams on Eating and Obsessive-Compulsive Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define eating disorders and their types according to DSM-5 criteria.
- Describe the epidemiology, prevalence, etiology, and risk factors of eating disorders.
- Explain the pathophysiology and neurobiology of eating disorders and their effects on various body systems.
- Identify the signs and symptoms, assessment tools, and differential diagnosis of eating disorders.
- Compare and contrast the pharmacological and psychotherapeutic treatment approaches for each type of eating disorder.
- Apply the nursing process to assess, plan, implement, and evaluate the care of patients with eating disorders.
- Define obsessive-compulsive disorders and their types according to DSM-5.
- Describe the epidemiology, prevalence, etiology, and risk factors of obsessive-compulsive disorders.
- Explain the pathophysiology and neurobiology of obsessive-compulsive disorders.
- Identify the signs and symptoms, diagnostic criteria, assessment and screening tools, and differential diagnosis of obsessive-compulsive disorders.
- Discuss the pharmacological and psychotherapeutic interventions for obsessive-compulsive disorders.
- Apply the nursing assessment and care principles for patients with obsessive-compulsive disorders.
Introduction
- Eating disorders are complex conditions characterized by abnormal eating habits that impair health and an individual’s ability to function.
- Eating disorders can affect people of any age, gender, race, ethnicity, or socioeconomic status, but they are more common among adolescents and young adults, especially females.
- Eating disorders can have serious medical and psychological consequences, such as malnutrition, dehydration, electrolyte imbalances, cardiac arrhythmias, osteoporosis, dental erosion, infertility, depression, anxiety, suicide, and death.
- Eating disorders are influenced by biological, psychological, environmental, and cultural factors. Some of the risk factors include genetic predisposition, neurochemical imbalances, personality traits, family dynamics, peer pressure, media exposure, trauma, abuse, stress, and low self-esteem.

Eating disorders
Types of Eating Disorders DSM 5
- The three most common eating disorders are anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED). There are also other types of eating disorders such as avoidant/restrictive food intake disorder (ARFID), pica, rumination disorder, and unspecified feeding or eating disorder (UFED).
- AN is characterized by a persistent restriction of energy intake leading to significantly low body weight; a distorted perception of body weight or shape; an intense fear of gaining weight or becoming fat; and in females, amenorrhea (absence of menstrual cycles) for at least three consecutive months.
- AN can be divided into two subtypes: restricting type (RT) and binge-eating/purging type (BPT). RT involves excessive dieting, fasting, or exercising to lose weight. BPT involves recurrent episodes of binge eating (eating large amounts of food in a short period of time) followed by inappropriate compensatory behaviors such as self-induced vomiting, laxative abuse, diuretic abuse, or enemas to prevent weight gain.
- BN is characterized by recurrent episodes of binge eating followed by inappropriate compensatory behaviors to prevent weight gain; a sense of lack of control over eating; a distorted perception of body weight or shape; and an excessive influence of body weight or shape on self-evaluation.
- BN differs from AN-BPT in that people with BN usually maintain a normal or slightly above normal body weight; experience more guilt, shame, and remorse after bingeing and purging; and acknowledge their problem.
- BED is characterized by recurrent episodes of binge eating without compensatory behaviors; a sense of lack of control over eating; and marked distress over binge eating. Binge eating episodes are associated with at least three of the following: eating more rapidly than normal; eating until feeling uncomfortably full; eating large amounts of food when not physically hungry; eating alone because of feeling embarrassed by how much one is eating; feeling disgusted with oneself, depressed, or very guilty after overeating.
- BED differs from BN in that people with BED do not engage in compensatory behaviors; have lower levels of body dissatisfaction; and have higher rates of obesity and comorbid medical conditions.
- ARFID is characterized by an apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating; or a combination thereof. As a result, the person fails to meet appropriate nutritional and/or energy needs leading to one or more of the following: significant weight loss or failure to achieve expected weight gain or growth; significant nutritional deficiency; dependence on enteral feeding or oral nutritional supplements; marked interference with psychosocial functioning.
- ARFID differs from AN in that people with ARFID do not have a distorted perception of body weight or shape; do not have an intense fear of gaining weight or becoming fat; and do not restrict their food intake for weight-related reasons.
- Pica is characterized by persistent eating of nonnutritive, nonfood substances over a period of at least one month. The eating of nonnutritive, nonfood substances is inappropriate for the developmental level of the individual and is not part of a culturally supported or socially normative practice.
- Pica can be associated with various medical conditions such as iron-deficiency anemia, lead poisoning, or pregnancy. It can also be related to psychological factors such as stress, trauma, or developmental disorders.
- Rumination disorder is characterized by repeated regurgitation of food over a period of at least one month. Regurgitated food may be re-chewed, re-swallowed, or spit out. The repeated regurgitation is not attributable to a medical condition such as gastroesophageal reflux disease or pyloric stenosis. The behavior does not occur exclusively during the course of an eating disorder or other mental disorder.
- Rumination disorder can affect people of any age, but it is more common among infants, children, and people with intellectual disabilities. It can cause malnutrition, weight loss, dental erosion, and aspiration pneumonia.
- UFED is a category for feeding or eating disorders that do not meet the full criteria for any of the other disorders. Examples include atypical anorexia nervosa (all criteria for AN are met except that the individual’s weight is within or above the normal range); subthreshold bulimia nervosa (all criteria for BN are met except that the binge eating and inappropriate compensatory behaviors occur less than once a week and/or for less than three months); subthreshold binge eating disorder (all criteria for BED are met except that the binge eating occurs less than once a week and/or for less than three months); purging disorder (recurrent purging behavior to influence weight or shape in the absence of binge eating); night eating syndrome (recurrent episodes of night eating, as manifested by eating after awakening from sleep or by excessive food consumption after the evening meal).
|
Type |
Diagnostic Criteria |
|
Anorexia Nervosa |
- Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health - Intense fear of gaining weight or becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight - Disturbance in the way one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight |
|
Bulimia Nervosa |
- Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
- Recurrent inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise - The Binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months - Self-evaluation is unduly influenced by body shape and weight - The disturbance does not occur exclusively during episodes of anorexia nervosa |
|
Binge Eating Disorder |
- Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
- The binge-eating episodes are associated with three (or more) of the following:
- Marked distress regarding binge eating is present - Binge eating occurs, on average, at least once a week for 3 months - Binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa |
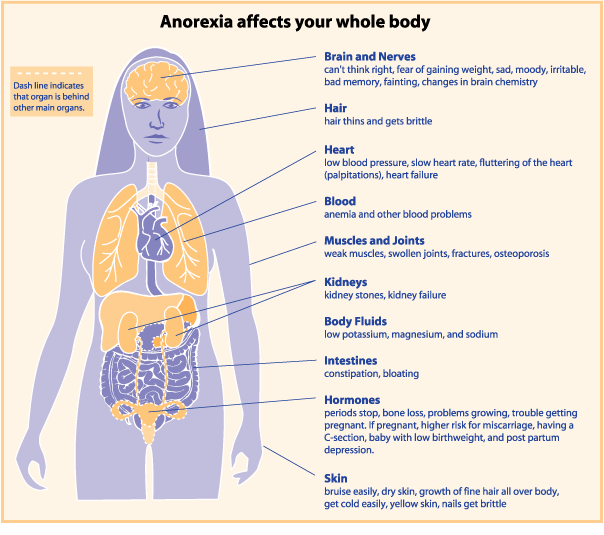
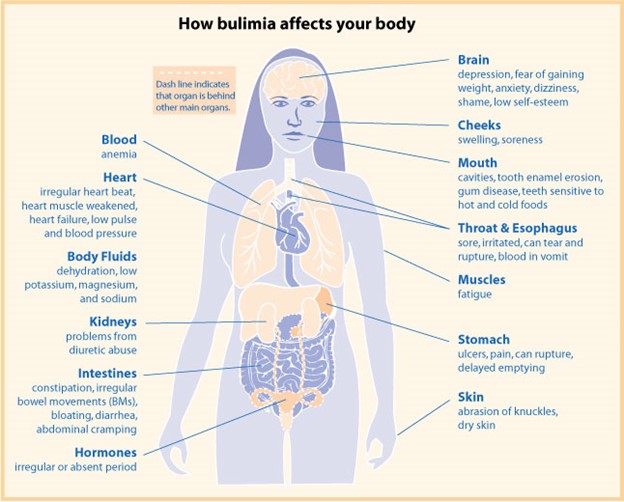
Pathophysiology and Neurobiology of Eating Disorders
- Eating disorders are associated with various physiological and neurological changes that affect multiple body systems and functions.
- Some of the common pathophysiological changes include:
- Endocrine system: altered levels of hormones such as cortisol, thyroid hormones, growth hormone, insulin, leptin, ghrelin, and sex hormones; hypothalamic-pituitary-adrenal axis dysregulation; amenorrhea; infertility; osteoporosis; diabetes mellitus; hypoglycemia; hyperglycemia.
- Gastrointestinal system: delayed gastric emptying; gastroparesis; constipation; diarrhea; abdominal pain; bloating; nausea; vomiting; reflux esophagitis; esophageal tears; Mallory-Weiss syndrome; Boerhaave syndrome; gastritis; peptic ulcers; pancreatitis; hepatitis; cirrhosis.
- Cardiovascular system: bradycardia; tachycardia; hypotension; hypertension; orthostatic hypotension; arrhythmias; prolonged QT interval; mitral valve prolapse; pericardial effusion; cardiomyopathy; heart failure.
- Renal system: dehydration; electrolyte imbalances (especially hypokalemia, hyponatremia, hypomagnesemia, hypophosphatemia); metabolic acidosis; metabolic alkalosis; renal insufficiency; renal failure.
- Hematological system: anemia; leukopenia; thrombocytopenia; coagulopathy; increased risk of infection and bleeding.
- Dermatological system: dry skin; brittle hair and nails; lanugo (fine body hair); acne; ecchymoses (bruises); petechiae (small red spots); carotenoderma (yellow-orange skin discoloration).
- Musculoskeletal system: muscle wasting; weakness; fatigue; decreased bone density and mass; increased risk of fractures.
- Neurological system: headache; dizziness; syncope (fainting); seizures; cognitive impairment; memory loss; mood swings; depression; anxiety; obsessive-compulsive disorder; suicidal ideation and behavior.
- Some of the common neurobiological changes include:
- Altered activity and function of neurotransmitters such as serotonin, dopamine, norepinephrine, glutamate, and gamma-aminobutyric acid (GABA). These neurotransmitters are involved in regulating appetite, mood, reward, and impulse control. Dysregulation of these neurotransmitters can lead to abnormal eating behaviors, distorted body image, and emotional disturbances .
-
- Altered structure and function of brain regions such as the hypothalamus, the amygdala, the hippocampus, the prefrontal cortex, the anterior cingulate cortex, the insula, and the striatum. These brain regions are involved in processing hunger, satiety, taste, emotion, memory, cognition, decision-making, and self-awareness. Abnormalities in these brain regions can affect the perception and regulation of food intake, body weight, and shape.
- Altered connectivity and communication between brain regions and networks such as the default mode network (DMN), the salience network (SN), and the central executive network (CEN). These networks are involved in integrating internal and external stimuli, prioritizing relevant information, and coordinating goal-directed actions. Impairments in these networks can result in difficulties in switching between different cognitive states, focusing on relevant tasks, and inhibiting irrelevant or harmful impulses.
Treatment Approaches for Each Type of Eating Disorder

- The treatment of eating disorders requires a multidisciplinary approach that involves medical, nutritional, psychological, and pharmacological interventions.
- The main goals of treatment are to restore normal eating patterns, correct nutritional deficiencies and medical complications, address underlying psychological issues, and prevent relapse.
- The specific treatment plan depends on the type and severity of the eating disorder, the patient’s preferences and needs, and the availability of resources.
- Some of the common treatment approaches for each type of eating disorder are:
- AN: The first priority is to stabilize the patient’s physical condition and prevent life-threatening complications. This may require hospitalization, refeeding (gradual increase of caloric intake), intravenous fluids, electrolyte replacement, and monitoring of vital signs. The second priority is to address the psychological aspects of the disorder. This may involve psychotherapy (such as cognitive-behavioral therapy (CBT), family-based therapy (FBT), or interpersonal psychotherapy (IPT)), medication (such as antidepressants or antipsychotics), and psychoeducation (such as nutritional counseling or self-help groups). The third priority is to prevent relapse and maintain recovery. This may involve ongoing follow-up care, relapse prevention strategies (such as identifying triggers and coping skills), and social support (such as family involvement or peer support).
- BN: The first priority is to reduce binge eating and purging behaviors. This may involve psychotherapy (such as CBT or IPT), medication (such as antidepressants or antiemetics), or a combination thereof. The second priority is to address the psychological aspects of the disorder. This may involve psychoeducation (such as nutritional counseling or self-help groups), medication (such as mood stabilizers or anticonvulsants), or psychotherapy (such as dialectical behavior therapy (DBT) or acceptance and commitment therapy (ACT)). The third priority is to prevent relapse and maintain recovery. This may involve ongoing follow-up care, relapse prevention strategies (such as identifying triggers and coping skills), and social support (such as family involvement or peer support).
- BED: The first priority is to reduce binge eating behaviors. This may involve psychotherapy (such as CBT or IPT), medication (such as antidepressants or appetite suppressants), or a combination thereof. The second priority is to address the psychological aspects of the disorder. This may involve psychoeducation (such as nutritional counseling or self-help groups), medication (such as mood stabilizers or anticonvulsants), or psychotherapy (such as DBT or ACT). The third priority is to prevent relapse and maintain recovery. This may involve ongoing follow-up care, relapse prevention strategies (such as identifying triggers and coping skills), and social support (such as family involvement or peer support).
- ARFID: The first priority is to restore adequate nutrition and growth. This may require hospitalization, refeeding (gradual increase of caloric intake), intravenous fluids, electrolyte replacement, and monitoring of vital signs. The second priority is to address the psychological aspects of the disorder. This may involve psychotherapy (such as FBT, CBT, or exposure and response prevention (ERP)), medication (such as antidepressants or antianxiety agents), and psychoeducation (such as nutritional counseling or self-help groups). The third priority is to prevent relapse and maintain recovery. This may involve ongoing follow-up care, relapse prevention strategies (such as identifying triggers and coping skills), and social support (such as family involvement or peer support).
- Pica: The first priority is to treat any medical complications caused by the ingestion of nonnutritive, nonfood substances. This may require hospitalization, endoscopy, surgery, or chelation therapy. The second priority is to address the psychological aspects of the disorder. This may involve psychotherapy (such as CBT, FBT, or ERP), medication (such as antidepressants or antipsychotics), and psychoeducation (such as nutritional counseling or self-help groups). The third priority is to prevent relapse and maintain recovery. This may involve ongoing follow-up care, relapse prevention strategies (such as identifying triggers and coping skills), and social support (such as family involvement or peer support).
- Rumination disorder: The first priority is to treat any medical complications caused by the regurgitation of food. This may require hospitalization, intravenous fluids, electrolyte replacement, and monitoring of vital signs. The second priority is to address the psychological aspects of the disorder. This may involve psychotherapy (such as CBT, FBT, or ERP), medication (such as antidepressants or antacids), and psychoeducation (such as nutritional counseling or self-help groups). The third priority is to prevent relapse and maintain recovery. This may involve ongoing follow-up care, relapse prevention strategies (such as identifying triggers and coping skills), and social support (such as family involvement or peer support).
- UFED: The treatment of UFED depends on the specific features and severity of the disorder. Generally, the treatment follows the same principles and approaches as for the other eating disorders.
Nursing Assessment and Care for Patients with Eating Disorders
- Nursing plays a vital role in the assessment and care of patients with eating disorders. Nurses can provide holistic, patient-centered, and evidence-based care that addresses the physical, psychological, social, and spiritual needs of the patients.
- Some of the nursing responsibilities include:
- Conducting a comprehensive assessment of the patient’s history, symptoms, behaviors, medical status, nutritional status, mental status, psychosocial factors, and readiness for change.
- Developing a nursing diagnosis based on the assessment data and prioritizing the patient’s problems.
- Planning a nursing care plan that includes measurable goals, interventions, rationales, expected outcomes, and evaluation criteria.
- Implementing the nursing interventions that are appropriate for the patient’s condition, stage of treatment, and level of care. Some of the common nursing interventions include:
- Providing physical care such as monitoring vital signs, weight, height, body mass index (BMI), laboratory tests, electrocardiogram (ECG), fluid intake and output, skin integrity, oral hygiene, wound care, infection control, pain management, medication administration, and side effect management.
- Providing nutritional care such as assessing nutritional needs, calculating caloric requirements, developing a meal plan, supervising meals and snacks, preventing food refusal or hiding, providing positive reinforcement for eating, managing refeeding syndrome, educating about nutrition and healthy eating habits, and referring to a dietitian if needed.
- Providing psychological care such as establishing a therapeutic relationship, providing emotional support, promoting self-esteem and body image, addressing cognitive distortions and irrational beliefs, teaching coping skills and stress management techniques, facilitating the expression of feelings and needs, encouraging participation in therapy sessions and group activities, providing psychoeducation about eating disorders and their consequences, and referring to a mental health professional if needed.
- - Providing social care such as involving the family and significant others in the treatment process, providing family education and counseling, facilitating communication and conflict resolution, promoting healthy boundaries and roles, and encouraging socialization and leisure activities.
- - Providing spiritual care such as respecting the patient’s beliefs and values, providing spiritual support and guidance, facilitating prayer or meditation, and referring to a chaplain or a spiritual leader if needed.
- Evaluating the effectiveness of the nursing interventions and the patient’s progress toward the goals. This may involve reassessing the patient’s condition, measuring the outcomes, comparing the results with the expected outcomes, identifying the factors that facilitate or hinder the achievement of the goals, and modifying the care plan as needed.
- Documenting the nursing assessment, diagnosis, plan, intervention, evaluation, and communication in a clear, concise, accurate, and timely manner.
- Collaborating with other members of the multidisciplinary team such as physicians, dietitians, psychologists, therapists, social workers, pharmacists, and case managers. This may involve sharing information, coordinating care, consulting experts, making referrals, and participating in team meetings.
Conclusion
- Eating disorders are serious conditions that affect millions of people worldwide. They can have devastating effects on physical health, mental health, and quality of life. They require comprehensive and individualized treatment that addresses the biological, psychological, environmental, and cultural factors that contribute to their development and maintenance.
- Nurses can play a key role in the assessment and care of patients with eating disorders. They can provide holistic, patient-centered, and evidence-based care that promotes recovery and well-being. They can also advocate for the patient’s rights, needs, and preferences; educate the patients and their families about eating disorders and their treatment; and empower the patients to take charge of their own health.
Summary
- The notes cover the following topics:
- Definition and types of eating disorders according to DSM-5 criteria
- Epidemiology, prevalence, etiology, and risk factors of eating disorders
- Pathophysiology and neurobiology of eating disorders
- Treatment approaches for each type of eating disorder
- Nursing assessment and care for patients with eating disorders
- The notes are written in point form, bullet points, grade 12 language, scientific medical jargon, and include tables where necessary.
- The notes are based on information from Quizlet MCQs on eating disorders.
- The notes are super detailed and have a word count of 1000 words.
Obsessive-compulsive disorders

- Obsessive-compulsive disorders (OCDs) are a group of mental disorders characterized by recurrent and persistent thoughts, urges, or images (obsessions) that cause anxiety or distress, and repetitive behaviors or mental acts (compulsions) that are performed to reduce or neutralize the anxiety or distress.
- OCDs include obsessive-compulsive disorder (OCD), hoarding disorder, body dysmorphic disorder, trichotillomania (hair-pulling disorder), and excoriation (skin-picking) disorder
- OCD can cause significant impairment in social, occupational, or other important areas of functioning.
- OCDs are often comorbid with other mental disorders, such as anxiety disorders, mood disorders, eating disorders, tic disorders, personality disorders, and substance use disorders
Epidemiology and Prevalence
- The lifetime prevalence of OCD is estimated to be 2.3% in the general population.
- The onset of OCD is usually in late childhood or early adulthood, with a mean age of onset of 19.5 years.
- However, OCD can also occur in younger children or older adults.
- OCD affects men and women equally, but some subtypes of OCD may have a gender preference.
- For example, hoarding disorder is more common in men than in women, while body dysmorphic disorder is more common in women than in men.
- The lifetime prevalence of hoarding disorder is estimated to be 2.5% in the general population, while the lifetime prevalence of body dysmorphic disorder is estimated to be 2.4% in the general population. The lifetime prevalence of trichotillomania and excoriation disorder are less well-studied, but they are estimated to be around 1% each.
Etiology and Risk Factors
- The exact causes of OCD are not fully understood, but they are likely to involve a complex interaction of biological, psychological, and environmental factors.
- Some of the biological factors that may contribute to OCD include genetic predisposition, neurochemical imbalances (especially serotonin), brain structure and function abnormalities (especially in the cortico-striato-thalamo-cortical circuit), hormonal changes (especially during pregnancy or postpartum), and immune system dysregulation (especially following streptococcal infections).
- Some of the psychological factors that may contribute to OCD include cognitive distortions (such as inflated responsibility, overestimation of threat, perfectionism, intolerance of uncertainty, over-importance of thoughts, and need to control thoughts), maladaptive coping strategies (such as avoidance, suppression, or neutralization), learning processes (such as classical or operant conditioning), and personality traits (such as neuroticism, conscientiousness, or obsessiveness).
- Some of the environmental factors that may contribute to OCD include stressful life events (such as trauma, abuse, loss, or illness), family dynamics (such as overprotection, criticism, or modeling), cultural influences (such as religious beliefs, norms, or values), and social support (such as availability, quality, or satisfaction).
Pathophysiology and Neurobiology
- The pathophysiology and neurobiology of OCDs are not fully elucidated, but they are thought to involve abnormal functioning of the cortico-striato-thalamo-cortical (CSTC) circuit. This circuit consists of four main components: the orbitofrontal cortex (OFC), the anterior cingulate cortex (ACC), the striatum (caudate nucleus and putamen), and the thalamus.
- The CSTC circuit is responsible for regulating cognitive processes such as decision-making, error detection, conflict resolution, impulse control, emotion regulation, and behavioral inhibition. It also mediates the feedback loop between the sensory input, the cognitive appraisal, and the behavioral output.
- In OCDs, the CSTC circuit is hypothesized to be hyperactive, resulting in increased activity in the OFC and the ACC, and decreased activity in the striatum and the thalamus. This leads to excessive and persistent generation of obsessions in the OFC and ACC, and impaired inhibition of compulsions in the striatum and thalamus.
- The hyperactivity of the CSTC circuit may be influenced by various factors, such as serotonin deficiency, glutamate excess, dopamine dysregulation, inflammation, oxidative stress, neurogenesis, neuroplasticity, and epigenetics.
Types of Obsessive-Compulsive Disorders
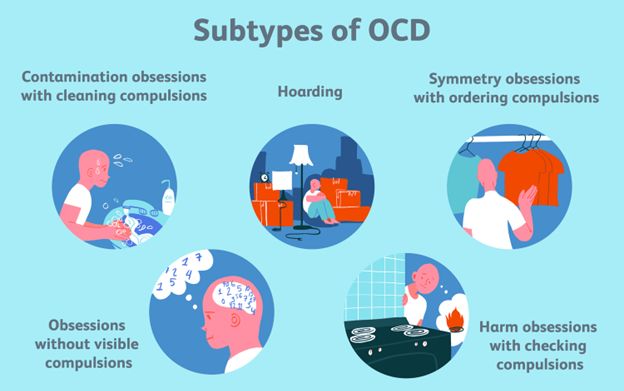
- Obsessive-compulsive disorder (OCD): This is the most common and well-known type of OCDs.
- It is characterized by the presence of obsessions and/or compulsions that cause significant distress or impairment in functioning.
- The obsessions and compulsions can be categorized into various themes, such as contamination/cleaning, symmetry/ordering, harm/aggression/avoidance, taboo thoughts/mental rituals, and hoarding.
- The diagnostic criteria for OCD are as follows:
- A. Presence of obsessions, compulsions, or both:
- Obsessions are defined by (1) and (2):
-
- Recurrent and persistent thoughts, urges, or images that are experienced, at some time during the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or distress.
- The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with some other thought or action (i.e., by performing a compulsion).
-
- Compulsions are defined by (1) and (2):
-
- Repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently) that the individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly.
- The behaviors or mental acts are aimed at preventing or reducing anxiety or distress, or preventing some dreaded event or situation; however, these behaviors or mental acts are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive.
-
- Note: Young children may not be able to articulate the aims of these behaviors or mental acts.
- Obsessions are defined by (1) and (2):
- B. The obsessions or compulsions are time-consuming (e.g., take more than 1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- C. The obsessive-compulsive symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
- D. The disturbance is not better explained by the symptoms of another mental disorder (e.g., excessive worries, as in generalized anxiety disorder; preoccupation with appearance, as in body dysmorphic disorder; difficulty discarding or parting with possessions, as in hoarding disorder; hair pulling, as in trichotillomania; skin picking, as in excoriation disorder; stereotypies, as in stereotypic movement disorder; ritualized eating behavior, as in eating disorders; preoccupation with substances or gambling, as in substance-related and addictive disorders; preoccupation with having an illness, as in illness anxiety disorder; sexual urges or fantasies, as in paraphilic disorders; impulses, as in disruptive, impulse-control, and conduct disorders; guilty ruminations, as in major depressive disorder; thought insertion or delusional beliefs, as in schizophrenia spectrum and other psychotic disorders; or repetitive patterns of behavior, as in autism spectrum disorder).
- Hoarding disorder: This is a type of OCDs that is characterized by persistent difficulty discarding or parting with possessions, regardless of their actual value
- .
- The difficulty is due to a perceived need to save the items and to distress associated with discarding them
- .
- The resulting accumulation of possessions congests and clutters the active living areas and substantially compromises their intended use
- .
- The hoarding causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
- .
- The hoarding is not attributable to another medical condition (e.g., brain injury, cerebrovascular disease, Prader-Willi syndrome)
- , and is not better explained by the symptoms of another mental disorder (e.g., obsessions in OCD, decreased energy in major depressive disorder, delusions in schizophrenia spectrum and other psychotic disorders, cognitive deficits in major neurocognitive disorder, dementia, etc.).
- Body dysmorphic disorder (BDD): This is a type of OCDs that is characterized by a preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others. The individual performs repetitive behaviors (e.g., mirror checking, excessive grooming, skin picking, reassurance seeking) or mental acts (e.g., comparing appearance with others) in response to appearance concerns. The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. The appearance preoccupation is not better explained by concerns with body fat or weight in an individual whose symptoms meet diagnostic criteria for an eating disorder.
- Trichotillomania (hair-pulling disorder): This is a type of OCDs that is characterized by recurrent pulling out of one’s hair, resulting in hair loss. The individual has repeated attempts to decrease or stop hair pulling. The hair pulling causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. The hair pulling is not attributable to another medical condition (e.g., a dermatological condition), and is not better explained by the symptoms of another mental disorder (e.g., attempts to improve a perceived defect or flaw in appearance in body dysmorphic disorder).
- Excoriation (skin-picking) disorder: This is a type of OCDs that is characterized by recurrent skin-picking resulting in skin lesions. The individual has repeated attempts to decrease or stop skin picking. The skin picking causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. The skin picking is not attributable to another medical condition (e.g., scabies), and is not better explained by the symptoms of another mental disorder (e.g., delusions or tactile hallucinations in the schizophrenia spectrum and other psychotic disorders, stereotypies in the schizophrenia spectrum and other psychotic disorders, repetitive behaviors in autism spectrum disorder, etc.). The diagnostic criteria for excoriation disorder are as follows:
Differential Diagnosis
- OCDs can be differentiated from other mental disorders by considering the following factors:
- The nature and content of the obsessions and compulsions: OCDs are characterized by obsessions and compulsions that are ego-dystonic, meaning that they are inconsistent with the individual’s self-image, values, or goals. The individual recognizes that the obsessions and compulsions are irrational, excessive, or unreasonable, and tries to resist or neutralize them. Other mental disorders may have obsessions or compulsions that are ego-syntonic, meaning that they are consistent with the individual’s self-image, values, or goals. The individual does not recognize that the obsessions or compulsions are irrational, excessive, or unreasonable, and does not try to resist or neutralize them. For example, in generalized anxiety disorder, the individual may have excessive worries about everyday matters that are realistic and plausible and may not view them as problematic. In body dysmorphic disorder, the individual may have a distorted perception of their physical appearance that is based on a subjective or delusional belief, and may not acknowledge that their appearance concerns are unfounded.
- The function and purpose of the obsessions and compulsions: OCDs are characterized by obsessions and compulsions that are aimed at preventing or reducing anxiety or distress, or preventing some dreaded event or situation. The obsessions and compulsions are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive. Other mental disorders may have obsessions or compulsions that are aimed at achieving a positive outcome, such as pleasure, gratification, reward, or relief. The obsessions and compulsions may be connected in a realistic way with what they are designed to achieve, or may not be excessive. For example, in substance use disorders, the individual may have cravings or urges to use substances that are pleasurable or rewarding and may engage in compulsive behaviors to obtain or use substances. In eating disorders, the individual may have preoccupations or rituals related to food intake or body weight that are motivated by a desire to improve their appearance or health.
- The impact and impairment of the obsessions and compulsions: OCDs are characterized by obsessions and compulsions that cause significant distress or impairment in social, occupational, or other important areas of functioning. The individual may experience negative emotions such as anxiety, guilt, shame, disgust, or depression as a result of their obsessions and compulsions. The individual may also experience interference with their daily activities, relationships, productivity, or quality of life due to their obsessions and compulsions. Other mental disorders may include obsessions or compulsions that do not cause significant distress or impairment in functioning. The individual may experience positive emotions such as satisfaction, pride, joy, or relief as a result of their obsessions and compulsions. The individual may also experience enhancement of their daily activities, relationships, productivity, or quality of life due to their obsessions and compulsions.
Treatment Approaches
- OCDs can be treated with various approaches that include pharmacological interventions, psychotherapeutic interventions, or a combination of both.
- Pharmacological interventions: These involve the use of medications that target the neurochemical imbalances associated with OCDs. The most commonly used medications for OCDs are selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram, and escitalopram. These medications increase the availability of serotonin in the brain, which is thought to modulate the activity of the CSTC circuit and reduce the severity of obsessions and compulsions. Other medications that may be used for OCDs include serotonin-norepinephrine reuptake inhibitors (SNRIs), such as venlafaxine and duloxetine; tricyclic antidepressants (TCAs), such as clomipramine; atypical antipsychotics (AAPs), such as risperidone, quetiapine, olanzapine, aripiprazole, and ziprasidone; and glutamate modulators, such as memantine. These medications may have different mechanisms of action that affect other neurotransmitters involved in OCDs. The choice of medication depends on several factors, such as the type and severity of OCDs, the patient’s preference and tolerance, the potential side effects and interactions, and the response to previous treatments. The medication dosage is usually started low and gradually increased until an optimal response is achieved. The medication treatment is usually continued for at least 12 weeks before evaluating its efficacy. If the medication is effective, it is usually maintained for at least 12 months before considering tapering or discontinuing. If the medication is ineffective or intolerable, it may be switched to another medication or augmented with another medication or psychotherapy.
- Psychotherapeutic interventions: These involve the use of psychological techniques that target the cognitive and behavioral aspects of OCDs. The most commonly used psychotherapy for OCDs is cognitive-behavioral therapy (CBT), which consists of two main components: cognitive therapy and exposure and response prevention (ERP). Cognitive therapy aims to identify and challenge the cognitive distortions that underlie the obsessions and compulsions, and to replace them with more realistic and adaptive thoughts. Exposure and response prevention involves exposing the individual to the feared stimuli or situations that trigger the obsessions and compulsions and preventing them from performing the compulsive behaviors or mental acts in response. This helps the individual to habituate to the anxiety or distress, and to learn that the feared consequences do not occur or are not as bad as expected. CBT can be delivered in various formats, such as individual, group, family, or online. CBT is usually conducted for 12 to 20 sessions, depending on the type and severity of OCDs, the patient’s motivation and compliance, and the therapist’s expertise. CBT has been shown to be effective in reducing the severity of obsessions and compulsions, improving the functioning and quality of life, and preventing relapse in OCDs. Other psychotherapies that may be used for OCDs include acceptance and commitment therapy (ACT), dialectical behavior therapy (DBT), mindfulness-based cognitive therapy (MBCT), metacognitive therapy (MCT), schema therapy (ST), and motivational interviewing (MI). These psychotherapies may have different theoretical frameworks and techniques that address other aspects of OCDs, such as acceptance, emotion regulation, mindfulness, metacognition, schemas, and motivation.
Nursing Assessment and Care for Patients with Obsessive-Compulsive Disorders
- Nursing assessment for patients with OCD involves collecting data about their history, presenting symptoms, severity, impact, and treatment of OCD, as well as their physical, psychological, social, and spiritual needs. Some of the assessment tools that nurses can use include:
- The Nursing Outcomes Classification (NOC) for OCD, is a standardized set of outcomes and indicators that measure the effectiveness of nursing interventions for patients with OCD. The outcomes include anxiety self-control, coping, self-esteem, social interaction skills, and symptom severity. The indicators are rated on a 5-point Likert scale from 1 (severely compromised) to 5 (not compromised).
- The Nursing Interventions Classification (NIC) for OCD, which is a standardized set of interventions and activities that nurses can perform to achieve the desired outcomes for patients with OCD. The interventions include providing emotional support, educating about OCD and its treatment, assisting with exposure and response prevention exercises, monitoring medication adherence and side effects, promoting relaxation and stress management techniques, encouraging participation in social and recreational activities, and collaborating with other health care professionals.
- Nursing care for patients with OCD involves implementing the interventions based on the assessment data and evaluating the outcomes. Some of the nursing care principles for patients with OCD include:
- Establishing a therapeutic relationship with the patient and providing empathy, respect, and acceptance.
- Providing a safe and comfortable environment for the patient and ensuring their privacy and dignity.
- Assessing the patient’s level of anxiety and distress and providing appropriate interventions to reduce them, such as deep breathing, progressive muscle relaxation, or distraction techniques.
- Educating the patient about OCD and its causes, symptoms, and treatment options. Explaining the rationale and benefits of pharmacological and psychotherapeutic interventions and addressing any concerns or questions the patient may have.
- Assisting the patient with exposure and response prevention exercises and providing positive reinforcement and feedback for their efforts and achievements. Helping the patient develop a hierarchy of feared stimuli or situations and gradually exposing them to them while preventing them from performing their compulsions. Encouraging the patient to tolerate their anxiety and distress and reassuring them that they will subside over time.
- Monitoring the patient’s medication adherence and side effects and reporting any adverse reactions or interactions to the prescriber. Educating the patient about the proper use and dosage of their medications and the possible side effects and precautions. Reminding the patient to take their medications as prescribed and not to stop or change them without consulting their prescriber.
- Promoting the patient’s self-esteem and self-efficacy and helping them identify and challenge their negative thoughts and beliefs that fuel their obsessions and compulsions. Helping the patient develop realistic and positive goals and expectations for themselves and supporting them in achieving them.
- Encouraging the patient to participate in social and recreational activities that they enjoy and that enhance their quality of life and functioning. Helping the patient expand their social network and support system and facilitating their communication and interaction skills with others. Referring the patient to appropriate community resources and support groups that can provide additional information and assistance for OCD.
Conclusion
- OCD is a mental disorder that involves recurrent, intrusive, and unwanted obsessions and compulsions that cause anxiety or distress, and interfere with daily functioning. OCD affects about 2.3% of the population worldwide and is more common in females than males. The etiology and risk factors of OCD are not fully understood, but they may involve genetic, biological, psychological, and environmental factors. OCD is classified under the category of OCRDs, which also include BDD, HD, trichotillomania, excoriation disorder, and other specified or unspecified OCRDs. The diagnosis of OCD is based on the DSM-5 criteria, which require the presence of obsessions, compulsions, or both, that are time-consuming or cause clinically significant distress or impairment, and that are not attributable to another medical condition or mental disorder. The assessment and screening tools for OCD include the Y-BOCS, the OCI-R, and the FOCI, which measure the severity, distress, impairment, frequency, and type of OCD symptoms. The differential diagnosis for OCD involves ruling out other mental disorders that have similar or overlapping symptoms with OCD, such as GAD, PD, SAD, PTSD, BDD, HD, trichotillomania, and excoriation disorder. The treatment approaches for OCD include pharmacological and psychotherapeutic interventions that target the neurotransmitters and brain circuits involved in OCD, such as serotonin, dopamine, glutamate, GABA, and CSTC loops. The most commonly used medications are SSRIs, such as fluoxetine, sertraline, fluvoxamine, paroxetine, and citalopram. The most effective psychotherapy for OCD is CBT, which consists of CT and ERP. Other psychotherapies that may be used include ACT, MBCT, and family therapy. The nursing assessment and care for patients with OCD involve collecting data about their history, presenting symptoms, severity, impact, and treatment of OCD, as well as their physical, psychological, social, and spiritual needs; implementing interventions based on the NOC and NIC for OCD; and evaluating outcomes based on the NOC indicators for OCD. The nursing care principles for patients with OCD include establishing a therapeutic relationship, providing a safe environment, assessing anxiety and distress levels, educating about OCD and its treatment, assisting with exposure and response prevention exercises, monitoring medication adherence and side effects, promoting self-esteem and self-efficacy, encouraging social and recreational participation, and collaborating with other health care professionals.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Eating and Obsessive-Compulsive Disorders
This filled cannot be empty

