Please set your exam date
Fluid and Electrolytes
Study Questions
Distribution of Body Fluids
A nurse is teaching a client about the importance of maintaining fluid and electrolyte balance. Which of the following statements by the client indicates a need for further teaching?
Explanation
Choice A reason:
This statement is correct. Fluids and electrolytes help transport nutrients and oxygen to the cells by maintaining blood volume and pressure. They also help maintain the acid-base balance of the blood and other body fluids.
Choice B reason:
This statement is correct. Fluids and electrolytes help regulate body temperature by allowing heat to be distributed evenly throughout the body and by facilitating sweating, which cools the body. They also help lubricate the joints by providing synovial fluid, which reduces friction and inflammation.
Choice C reason:
This statement is correct. Fluids and electrolytes help digest food by providing saliva, gastric juice, bile, pancreatic juice, and intestinal secretions, which break down food and absorb nutrients. They also help excrete wastes from the body by forming urine, feces, sweat, and breath, which eliminate excess fluids, electrolytes, toxins, and carbon dioxide.
Choice D reason:
This statement indicates a need for further teaching. Fluids and electrolytes do not help increase body fat or lower blood pressure. Body fat is determined by the balance between calorie intake and expenditure, not by fluid intake. Blood pressure is influenced by many factors, such as cardiac output, vascular resistance, blood volume, and hormone levels, not by fluid intake alone. Fluid intake can affect blood pressure only if it causes overhydration or dehydration, which are both abnormal conditions that should be avoided.
A nurse is assessing a client who has dehydration. Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
Choice A reason:
Decreased skin turgor is a sign of dehydration because the skin loses elasticity when the body loses water. The nurse can assess this by pinching the skin on the back of the hand or the forehead and observing how quickly it returns to its normal position. If it takes longer than a few seconds, it indicates decreased skin turgor.
Choice B reason:
Increased heart rate is a sign of dehydration because the heart has to work harder to pump blood when the blood volume is low. The body also tries to compensate for the fluid loss by increasing the heart rate and constricting the blood vessels.
Choice C reason:
Crackles in the lungs are not a sign of dehydration, but rather a sign of fluid overload or pulmonary edema. Crackles are caused by fluid accumulation in the alveoli, which interferes with gas exchange and produces a crackling sound when breathing. This choice is incorrect.
Choice D reason:
Low urine output is a sign of dehydration because the kidneys try to conserve water by producing less urine. The urine also becomes more concentrated and darker in color when the body is dehydrated.
Choice E reason:
Dry mucous membranes are a sign of dehydration because the body loses moisture from the mouth, nose, and eyes when it is dehydrated. The nurse can assess this by looking at the lips, tongue, and oral cavity for dryness and cracking.
A nurse is caring for a client who has a high fever and is at risk for fluid volume deficit. The nurse should monitor the client for which of the following signs of fluid loss?
Explanation
Choice A reason: Feeling thirsty all the time is a sign of dehydration, not fluid loss. Dehydration occurs when the body does not have enough water and other fluids to carry out its normal functions. Dehydration can be caused by excessive sweating, vomiting, diarrhea, fever, or decreased water intake.
Choice B reason:
Gaining 2 pounds since yesterday is a sign of fluid retention, not fluid loss. Fluid retention occurs when the body holds on to extra water and salt in the tissues or blood vessels. Fluid retention can be caused by heart failure, kidney disease, liver disease, hormonal changes, or certain medications.
Choice C reason:
Having trouble breathing when lying down is a sign of orthopnea, not fluid loss. Orthopnea is a condition where a person feels short of breath when lying flat. Orthopnea can be caused by heart failure, lung disease, obesity, or sleep apnea.
Choice D reason:
Feeling dizzy when standing up is a sign of orthostatic hypotension, which is a possible sign of fluid loss. Orthostatic hypotension is a condition where the blood pressure drops when changing position from lying or sitting to standing. This can cause dizziness, lightheadedness, or fainting. Orthostatic hypotension can be caused by hypovolemia, which is a decrease in the volume of blood in the body due to fluid loss. Fluid loss can occur from bleeding, vomiting, diarrhea, sweating, or burns.
A nurse is reviewing the laboratory results of a client who has metabolic acidosis. The nurse should expect to see which of the following changes in the client's electrolyte levels?
Explanation
Choice A reason:
Decreased sodium is not a typical feature of metabolic acidosis. Sodium levels may be low, normal or high depending on the cause and severity of the acidosis, as well as the fluid status of the patient. Sodium is not directly involved in the acid-base balance of the body.
Choice B reason:
Increased potassium is a common finding in metabolic acidosis, especially in renal failure. This is because acidosis causes hydrogen ions to move into cells in exchange for potassium ions, which move out of cells into the blood. Also, impaired kidney function reduces the excretion of potassium in the urine.
Choice C reason:
Decreased calcium is not a typical feature of metabolic acidosis. Calcium levels may be low, normal or high depending on the cause and severity of the acidosis, as well as the presence of other disorders affecting calcium metabolism. Calcium is not directly involved in the acid-base balance of the body.
Choice D reason:
Increased chloride is a feature of normal anion gap metabolic acidosis, also known as hyperchloremic acidosis. This is because chloride replaces bicarbonate as the major anion in the blood when bicarbonate is lost or consumed by acids. However, increased chloride is not a feature of high anion gap metabolic acidosis, which is caused by accumulation of organic acids such as ketones or lactate.
A nurse is educating a client who has heart failure about the effects of diuretics on fluid and electrolyte balance. The nurse should instruct the client to report which of the following symptoms to the provider?
Explanation
Choice A reason:
Muscle weakness is a symptom of hypokalemia, which is a low level of potassium in the blood. Potassium is an important electrolyte that helps regulate the function of the heart and muscles. Diuretics can cause potassium loss through increased urine output, which can lead to hypokalemia. Hypokalemia can affect the heart rhythm and cause muscle cramps, weakness, fatigue, and constipation. Therefore, the client should report muscle weakness to the provider as it may indicate a need for potassium supplementation or a change in diuretic therapy.
Choice B reason:
Nausea and vomiting are not specific symptoms of diuretic use or fluid and electrolyte imbalance. They can be caused by many other factors, such as infection, food poisoning, medication side effects, or psychological stress. Nausea and vomiting can also lead to dehydration and electrolyte imbalance if not treated promptly. Therefore, the client should drink plenty of fluids and seek medical attention if nausea and vomiting persist or are severe, but they are not directly related to diuretic use or heart failure.
Choice C reason:
Headache and blurred vision are not common symptoms of diuretic use or fluid and electrolyte imbalance. They can be caused by many other factors, such as high blood pressure, migraine, eye strain, or neurological disorders. Headache and blurred vision can also be signs of a serious condition, such as stroke or brain tumor, that requires immediate medical attention. Therefore, the client should report headache and blurred vision to the provider as soon as possible, but they are not directly related to diuretic use or heart failure.
Choice D reason:
Constipation and abdominal pain are not common symptoms of diuretic use or fluid and electrolyte imbalance. They can be caused by many other factors, such as dietary changes, lack of fiber, medication side effects, or bowel obstruction. Constipation and abdominal pain can also be signs of a serious condition, such as appendicitis or diverticulitis, that requires immediate medical attention. Therefore, the client should report constipation and abdominal pain to the provider as soon as possible, but they are not directly related to diuretic use or heart failure.
A nurse is caring for a client who has fluid overload due to renal failure. Which of the following interventions should the nurse include in the plan of care?
Explanation
Choice A reason:
Administering IV fluids as prescribed is not an appropriate intervention for a client who has fluid overload due to renal failure. IV fluids will increase the fluid volume and worsen the condition. The nurse should monitor the client's fluid intake and output, and report any signs of fluid overload to the provider.
Choice B reason:
Restricting sodium intake is an appropriate intervention for a client who has fluid overload due to renal failure. Sodium causes water retention and increases the fluid volume in the body. The nurse should limit the client's sodium intake to less than 2 g per day, and avoid foods that are high in sodium, such as canned soups, processed meats, cheese, and salted snacks.
Choice C reason:
Elevating the head of the bed is an appropriate intervention for a client who has fluid overload due to renal failure. Elevating the head of the bed helps to reduce the pressure on the lungs and improve the client's breathing. The nurse should also monitor the client's respiratory status, and administer oxygen therapy as prescribed.
Choice D reason:
Encouraging ambulation is not an appropriate intervention for a client who has fluid overload due to renal failure. Ambulation may increase the workload on the heart and lungs, and exacerbate the symptoms of fluid overload. The nurse should assist the client with activities of daily living, and provide rest periods between activities.
Electrolytes
A nurse is reviewing the laboratory results of a client who has fluid volume excess. Which of the following electrolytes is most likely to be elevated in this client?
Explanation
Choice A reason:
Sodium is the most likely electrolyte to be elevated in a client who has fluid volume excess. This is because fluid volume excess, or hypervolemia, is caused by an increase in total body sodium content and an increase in total body water. Sodium is the main electrolyte that regulates fluid balance in the body. When sodium levels are high, the body retains water to dilute it. This leads to fluid overload and edema. Therefore, a client with fluid volume excess would have high sodium levels in their blood.
Choice B reason:
Potassium is not likely to be elevated in a client who has fluid volume excess. Potassium is mainly found inside the cells, and its levels are regulated by the kidneys. Potassium levels can be affected by acid-base balance, insulin, aldosterone, and cell damage. A client with fluid volume excess may have low potassium levels due to dilution or increased excretion by the kidneys.
Choice C reason:
Calcium is not likely to be elevated in a client who has fluid volume excess. Calcium is mostly bound to albumin, a protein in the blood. Calcium levels can be affected by parathyroid hormone, vitamin D, phosphate, and albumin levels. A client with fluid volume excess may have low calcium levels due to dilution or low albumin levels.
Choice D reason:
Magnesium is not likely to be elevated in a client who has fluid volume excess. Magnesium is mainly found inside the cells and bones, and its levels are regulated by the kidneys. Magnesium levels can be affected by renal function, intestinal absorption, hormonal factors, and medications. A client with fluid volume excess may have low magnesium levels due to dilution or increased excretion by the kidneys.
A nurse is teaching a client who has chronic kidney disease about the importance of limiting phosphate intake. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
Dairy products like milk and cheese are high in phosphorus, which can cause bone loss and cardiovascular problems in clients who have chronic kidney disease. Therefore, avoiding or limiting these foods can help reduce phosphate intake and prevent complications.
Choice B reason:
Salt substitutes often contain potassium, which can accumulate in the blood and cause hyperkalemia in clients who have chronic kidney disease. Hyperkalemia can lead to cardiac arrhythmias and muscle weakness. Therefore, using salt substitutes instead of regular salt is not a good idea.
Choice C reason:
Orange juice and grapefruit juice are both high in potassium, which can cause hyperkalemia in clients who have chronic kidney disease. Therefore, drinking either of these juices does not indicate an understanding of the importance of limiting phosphate intake.
Choice D reason:
Fruits and vegetables like bananas and spinach are also high in potassium, which can cause hyperkalemia in clients who have chronic kidney disease. Moreover, some fruits and vegetables are also high in oxalate, which can increase the risk of kidney stones. Therefore, eating more fruits and vegetables like bananas and spinach does not indicate an understanding of the importance of limiting phosphate intake.
A nurse is assessing a client who has hypocalcemia. Which of the following findings should the nurse expect?
Explanation
Choice A reason:
Muscle weakness is not a typical symptom of hypocalcemia. Muscle weakness can be caused by many other conditions, such as electrolyte imbalance, dehydration, or muscle injury. Hypocalcemia usually causes muscle cramps or spasms, especially in the back and legs.
Choice B reason:
Constipation is not a common symptom of hypocalcemia. Constipation can be caused by many other factors, such as diet, medication, or lack of physical activity. Hypocalcemia usually affects the nervous system and the muscles, not the digestive system.
Choice C reason:
Facial twitching is a characteristic symptom of hypocalcemia. Facial twitching is also known as Chvostek's sign, which is a test to diagnose hypocalcemia. It involves tapping the facial nerve near the ear and observing if the facial muscles contract involuntarily. Facial twitching occurs because hypocalcemia makes the nerves and muscles more excitable and sensitive to stimulation.
Choice D reason:
Decreased deep tendon reflexes are not a sign of hypocalcemia. Decreased deep tendon reflexes can be caused by many other conditions, such as peripheral neuropathy, spinal cord injury, or hypothyroidism. Hypocalcemia usually causes increased deep tendon reflexes, which is also known as Trousseau's sign. It involves inflating a blood pressure cuff on the arm and observing if the hand and fingers curl inward. This happens because hypocalcemia reduces the threshold for nerve and muscle activation.
A nurse is preparing to administer magnesium sulfate intravenously to a client who has preeclampsia. Which of the following actions should the nurse take?
Explanation
-
Choice A reason: Dilute the medication in normal saline solution. This is incorrect because magnesium sulfate should be diluted in lactated Ringer's solution, not normal saline solution.
-
Choice B reason:
-
Infuse the medication over 10 minutes. This is incorrect because magnesium sulfate should be infused over 20 to 30 minutes.
-
Choice C reason:
-
Monitor the client's blood pressure every 15 minutes. This is incorrect because monitoring the client's blood pressure every 15 minutes is not enough to prevent or detect complications of preeclampsia or magnesium sulfate therapy. The nurse should also monitor the client's respiratory rate, deep tendon reflexes, urine output, and serum magnesium levels.
-
Choice D reason:
-
Have calcium gluconate available as an antidote. This is correct because calcium gluconate is the antidote for magnesium toxicity, which can cause respiratory depression, cardiac arrest, and coma. Magnesium toxicity can occur if the client has renal impairment, receives too high a dose, or has a low urine output. The nurse should have calcium gluconate readily available and administer it intravenously if signs of magnesium toxicity occur.
Fluid Pressures/Movements (Starling's Law)
A nurse is reviewing the laboratory results of a client who has dehydration. Which of the following findings indicates an increase in osmolality?
Explanation
Choice A reason: Serum sodium 140 mEq/L is a normal value and does not indicate an increase in osmolality. Osmolality is the concentration of dissolved particles in a fluid. Sodium is one of the main electrolytes that affect osmolality, but a normal sodium level does not necessarily mean a normal osmolality.
Choice B reason:
Serum potassium 4.0 mEq/L is also a normal value and does not indicate an increase in osmolality. Potassium is another electrolyte that affects osmolality, but it has a smaller effect than sodium. A normal potassium level does not necessarily mean a normal osmolality.
Choice C reason:
Serum glucose 90 mg/dL is also a normal value and does not indicate an increase in osmolality. Glucose is another substance that affects osmolality, but it has a smaller effect than electrolytes. A normal glucose level does not necessarily mean a normal osmolality.
Choice D reason:
Serum urea nitrogen 25 mg/dL is an elevated value and indicates an increase in osmolality. Urea nitrogen is a waste product of protein metabolism that is excreted by the kidneys. Urea nitrogen is one of the main substances that affect osmolality, along with sodium and glucose. An elevated urea nitrogen level means that the blood is more concentrated and has less water. This can be caused by dehydration, which is a common condition in clients who have dehydration. Dehydration leads to an increase in serum osmolality and activation of antidiuretic hormone (ADH), which results in urinary concentration. Therefore, choice D is the correct answer.
A nurse is caring for a client who has a severe burn injury and is receiving intravenous fluid replacement therapy. Which of the following actions should the nurse take to monitor fluid shifts in this client? (Select all that apply.)
Explanation
Choice A reason:
Measure intake and output. This is a correct action because it helps to monitor the fluid balance and renal function of the client who has a severe burn injury and is receiving intravenous fluid replacement therapy. Fluid shifts can cause hypovolemia, dehydration, electrolyte imbalances, and renal failure in burn patients. Measuring intake and output can help to detect these complications and adjust the fluid therapy accordingly.
Choice B reason:
Assess skin turgor. This is an incorrect action because it is not a reliable indicator of fluid status in burn patients. Burn injuries can damage the skin and alter its elasticity, making skin turgor assessment inaccurate. Other methods of assessing hydration, such as mucous membranes, capillary refill, and urine specific gravity, are more appropriate for burn patients.
Choice C reason:
Check blood pressure. This is a correct action because it helps to monitor the hemodynamic status and perfusion of the client who has a severe burn injury and is receiving intravenous fluid replacement therapy. Fluid shifts can cause hypotension, shock, and organ damage in burn patients. Checking blood pressure can help to detect these complications and adjust the fluid therapy accordingly.
Choice D reason:
Weigh the client daily. This is a correct action because it helps to monitor the fluid balance and nutritional status of the client who has a severe burn injury and is receiving intravenous fluid replacement therapy. Fluid shifts can cause weight changes, edema, and protein loss in burn patients. Weighing the client daily can help to detect these complications and adjust the fluid therapy accordingly.
Choice E reason:
Monitor serum albumin levels. This is a correct action because it helps to monitor the fluid balance and protein status of the client who has a severe burn injury and is receiving intravenous fluid replacement therapy. Fluid shifts can cause hypoalbuminemia, which can lead to edema, decreased oncotic pressure, and impaired wound healing in burn patients. Monitoring serum albumin levels can help to detect this complication and adjust the fluid therapy accordingly.
A nurse is teaching a client who has heart failure about the importance of limiting sodium intake. The client asks, "How does sodium affect my condition?” Which of the following responses should the nurse make?
Explanation
Choice A reason:
Sodium attracts water and increases the fluid volume in your blood vessels. This is the correct answer because sodium is an electrolyte that helps regulate the balance of fluids in the body. When there is too much sodium in the blood, it draws water from the cells and tissues into the blood vessels, increasing the blood volume and pressure. This puts extra strain on the heart and can worsen heart failure symptoms.
Choice B reason:
Sodium causes water to move out of your cells and into your urine. This is incorrect because sodium does not cause water to move out of the cells and into the urine. In fact, sodium can cause water retention by stimulating the release of antidiuretic hormone (ADH), which reduces urine output and increases blood volume.
Choice C reason:
Sodium stimulates your kidneys to retain water and decrease urine output. This is incorrect because sodium does not directly stimulate the kidneys to retain water and decrease urine output. However, sodium can indirectly affect the kidney function by increasing the blood volume and pressure, which can damage the kidney cells and impair their ability to filter waste and excess fluid from the body.
Choice D reason:
Sodium interferes with the action of your heart medications. This is incorrect because sodium does not interfere with the action of your heart medications. However, some heart medications, such as diuretics, can cause sodium loss in the urine, which can lead to low blood sodium levels (hyponatremia) This can cause symptoms such as confusion, weakness, nausea, and muscle cramps. Therefore, it is important to monitor your sodium intake and blood levels while taking heart medications.
A nurse is preparing to administer intravenous fluids to a client who has hypovolemia due to vomiting and diarrhea. The nurse should anticipate using which of the following types of solutions?
Explanation
Choice A reason:
A hypertonic solution is one that has a higher concentration of solutes than the blood plasma. Administering a hypertonic solution to a client who has hypovolemia would cause water to move out of the cells and into the blood vessels, resulting in cellular dehydration and increased blood pressure. This could worsen the client's condition and cause complications such as cerebral edema, pulmonary edema, or heart failure.
Choice B reason:
A hypotonic solution is one that has a lower concentration of solutes than the blood plasma. Administering a hypotonic solution to a client who has hypovolemia would cause water to move from the blood vessels into the cells, resulting in cellular swelling and decreased blood pressure. This could also worsen the client's condition and cause complications such as fluid overload, hyponatremia, or hemolysis.
Choice C reason:
An isotonic solution is one that has the same concentration of solutes as the blood plasma. Administering an isotonic solution to a client who has hypovolemia would help restore the fluid volume and maintain the osmotic pressure of the blood. This could improve the client's condition and prevent complications such as shock, acidosis, or organ failure. Examples of isotonic solutions are 0.9% sodium chloride (normal saline) and lactated Ringer's solution.
Choice D reason:
A colloid solution is one that contains large molecules that do not cross the capillary membrane. Administering a colloid solution to a client who has hypovolemia would increase the oncotic pressure of the blood and draw water from the interstitial space into the blood vessels. This could also improve the client's condition and prevent complications such as shock, acidosis, or organ failure. Examples of colloid solutions are albumin, dextran, and hetastarch.
A nurse is assessing a client who has fluid overload. Which of the following findings should the nurse expect?
Explanation
Choice A reason:
Increased hematocrit is not a finding of fluid overload, but rather of dehydration. Hematocrit is the percentage of red blood cells in the blood volume. When the blood volume decreases due to fluid loss, the hematocrit increases.
Choice B reason:
Decreased heart rate is not a finding of fluid overload, but rather of fluid deficit. When the blood volume increases due to fluid retention, the heart rate increases to maintain cardiac output.
Choice C reason:
Crackles in the lungs are a finding of fluid overload. Crackles are caused by fluid accumulation in the alveoli, which interferes with gas exchange and produces a crackling sound on auscultation.
Choice D reason:
Sunken eyeballs are not a finding of fluid overload, but rather of dehydration. Sunken eyeballs are caused by loss of subcutaneous fat and tissue turgor due to fluid loss. Some additional sentences are.
Regulating Body Fluids
A nurse is caring for a client who has a fluid imbalance due to excessive vomiting. The nurse should monitor the client for which of the following electrolyte imbalances?
Explanation
Choice A reason:
Hyponatremia is a condition of low sodium level in the blood, which can result from excessive vomiting. Sodium is an important electrolyte that helps regulate fluid balance, nerve and muscle function, and blood pressure. When a person vomits, they lose sodium and water from the stomach, which can lead to dehydration and hyponatremia. Symptoms of hyponatremia include confusion, headache, weakness, nausea, muscle cramps, and seizures.
Choice B reason:
Hyperkalemia is a condition of high potassium level in the blood, which can result from kidney failure, certain medications, or excessive intake of potassium-rich foods. Potassium is an important electrolyte that helps regulate heart rhythm, muscle contraction, and nerve impulses. When a person has hyperkalemia, they may experience irregular heartbeat, chest pain, muscle weakness, numbness, or paralysis. Vomiting does not usually cause hyperkalemia unless the person has other risk factors.
Choice C reason:
Hypercalcemia is a condition of high calcium level in the blood, which can result from hyperparathyroidism, certain cancers, or excessive intake of calcium or vitamin D supplements. Calcium is an important electrolyte that helps regulate bone health, blood clotting, muscle contraction, and nerve function. When a person has hypercalcemia, they may experience nausea, vomiting, constipation, abdominal pain, confusion, lethargy, kidney stones, or cardiac arrhythmias. Vomiting does not usually cause hypercalcemia unless the person has other risk factors.
Choice D reason:
Hypomagnesemia is a condition of low magnesium level in the blood, which can result from malnutrition, alcoholism, diarrhea, diuretics, or certain medications. Magnesium is an important electrolyte that helps regulate muscle and nerve function, blood pressure, blood sugar, and protein synthesis. When a person has hypomagnesemia, they may experience muscle twitching, cramps, tremors, seizures, irregular heartbeat, or changes in mental status. Vomiting does not usually cause hypomagnesemia unless the person has other risk factors.
A nurse is reviewing the laboratory results of a client who has chronic kidney disease. Which of the following electrolytes should the nurse expect to be elevated in this client? (Select all that apply.)
Explanation
Choice A reason:
Sodium is not likely to be elevated in a client who has chronic kidney disease because the kidneys tend to lose sodium along with water. Sodium levels may be low (hyponatremia) or normal in these clients, depending on their fluid status and dietary intake.
Choice B reason:
Potassium is likely to be elevated in a client who has chronic kidney disease because the kidneys are unable to excrete excess potassium. Potassium levels may be high (hyperkalemia) or normal in these clients, depending on their medication use and dietary intake.
Choice C reason:
Calcium is not likely to be elevated in a client who has chronic kidney disease because the kidneys are unable to activate vitamin D, which is needed for calcium absorption. Calcium levels may be low (hypocalcemia) or normal in these clients, depending on their parathyroid hormone levels and supplementation.
Choice D reason:
Phosphorus is likely to be elevated in a client who has chronic kidney disease because the kidneys are unable to excrete excess phosphorus. Phosphorus levels may be high (hyperphosphatemia) or normal in these clients, depending on their dietary intake and phosphate binders.
Choice E reason:
Magnesium is likely to be elevated in a client who has chronic kidney disease because the kidneys are unable to excrete excess magnesium. Magnesium levels may be high (hypermagnesemia) or normal in these clients, depending on their dietary intake and antacid use.
A nurse is teaching a client who has heart failure about the renin-angiotensin-aldosterone system. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
This system helps to increase my blood pressure when it is too low. This is correct because the renin-angiotensin-aldosterone system (RAAS) is a mechanism that regulates arterial blood pressure by increasing sodium and water retention, vasoconstriction, and cardiac output.
Choice B reason:
This system helps to decrease my blood volume when it is too high. This is incorrect because the RAAS does the opposite of this. It increases blood volume by stimulating the secretion of aldosterone, which causes the kidneys to reabsorb sodium and water.
Choice C reason:
This system helps to regulate my blood pH when it is too acidic. This is incorrect because the RAAS does not directly affect blood pH. Blood pH is regulated by the respiratory and renal systems, which adjust the levels of carbon dioxide and bicarbonate in the blood.
Choice D reason:
This system helps to lower my potassium level when it is too high. This is incorrect because the RAAS does not directly lower potassium levels. Potassium levels are regulated by the kidneys, which excrete excess potassium in the urine. However, aldosterone, which is part of the RAAS, can indirectly affect potassium levels by increasing sodium reabsorption and potassium secretion in the distal tubules of the kidneys.
A nurse is assessing a client who has hypocalcemia. Which of the following findings should the nurse expect?
Explanation
Choice A reason:
A positive Chvostek's sign is a facial twitch that occurs when the facial nerve is tapped. This is a sign of hypocalcemia, which causes increased neuromuscular excitability. According to index 2, a nurse can assess for Chvostek's sign by tapping the cheek just below the temple. If the facial muscles contract, the sign is positive.
Choice B reason:
Decreased deep tendon reflexes are not a sign of hypocalcemia, but rather of hypercalcemia, which causes decreased neuromuscular excitability. According to index 5, symptoms of hypercalcemia include muscle weakness, fatigue, constipation, nausea, vomiting, and confusion.
Choice C reason:
Muscle weakness is also not a sign of hypocalcemia, but rather of hyperkalemia, which causes impaired muscle contraction. According to index 1, a nurse can assess for muscle weakness by testing the client's grip strength and ability to lift the legs against resistance. If the client has difficulty performing these tasks, they may have hyperkalemia.
Choice D reason:
Hypoactive bowel sounds are not a sign of hypocalcemia, but rather of ileus, which is a paralysis of the intestinal muscles that causes obstruction. Ileus can be caused by various factors, such as surgery, infection, medication, or electrolyte imbalance. According to index 6, symptoms of ileus include abdominal pain, distension, nausea, vomiting, and constipation.
A nurse is preparing to administer intravenous magnesium sulfate to a client who has preeclampsia. The nurse should monitor the client for which of the following adverse effects of magnesium toxicity?
Explanation
Choice A reason:
Tachycardia is not a sign of magnesium toxicity. Magnesium sulfate can cause bradycardia or slow heart rate as a side effect.
Choice B reason:
Diarrhea is not a sign of magnesium toxicity. Magnesium sulfate can cause constipation or decreased bowel movements as a side effect.
Choice C reason:
Respiratory depression is a sign of magnesium toxicity. Magnesium sulfate can cause decreased respiratory rate or difficulty breathing as a side effect. This is a serious complication that requires immediate intervention by the nurse, such as discontinuing the infusion and administering calcium gluconate as an antidote.
Choice D reason:
Hyperthermia is not a sign of magnesium toxicity. Magnesium sulfate can cause hypothermia or low body temperature as a side effect.
Regulation of Electrolytes
A nurse is caring for a client who has a low serum sodium level. Which of the following actions should the nurse take?
Explanation
Choice A reason:
Restricting the client's fluid intake is not appropriate for a client who has a low serum sodium level. This could worsen the client's condition by increasing the relative concentration of sodium in the blood. Fluid restriction is indicated for clients who have a high serum sodium level.
Choice B reason:
Administering a hypertonic saline solution IV is the correct action for a nurse to take for a client who has a low serum sodium level. This will help increase the serum sodium level by drawing water out of the cells and into the blood. Hypertonic saline solutions are used to treat severe cases of hyponatremia.
Choice C reason:
Encouraging the client to eat foods high in potassium is not relevant for a client who has a low serum sodium level. Potassium is another electrolyte that affects the fluid balance in the body, but it does not directly affect the serum sodium level. Foods high in potassium are recommended for clients who have a low serum potassium level.
Choice D reason:
Monitoring the client for signs of hypernatremia is not necessary for a client who has a low serum sodium level. Hypernatremia is a condition of high serum sodium level, which is opposite to the client's condition. Signs of hypernatremia include thirst, dry mucous membranes, confusion, and seizures.
A nurse is reviewing the laboratory results of a client who has a high serum potassium level. Which of the following factors can cause hyperkalemia? (Select all that apply.)
Explanation
Choice A reason:
Renal failure. This is a common cause of hyperkalemia because the kidneys are responsible for excreting excess potassium from the body. When the kidneys are damaged or impaired, they cannot filter out enough potassium, leading to its accumulation in the blood.
Choice B reason:
Diuretic therapy. This is not a cause of hyperkalemia, but rather a potential treatment for it. Diuretics are medications that increase urine output and help remove excess fluid and electrolytes from the body. Some diuretics, such as thiazides and loop diuretics, can also lower potassium levels by increasing its loss in urine. However, other diuretics, such as potassium-sparing diuretics, can cause hyperkalemia by reducing potassium excretion.
Choice C reason:
Acidosis. This is a condition where the blood pH is lower than normal, indicating an excess of acid in the body. Acidosis can cause hyperkalemia by shifting potassium from the cells to the blood in exchange for hydrogen ions. This is a mechanism to buffer the acid and maintain the electrical balance across the cell membrane.
Choice D reason:
Insulin deficiency. This is a condition where the body does not produce enough insulin, a hormone that regulates blood glucose levels. Insulin deficiency can cause hyperkalemia by impairing the uptake of glucose and potassium into the cells. Insulin normally stimulates the activity of sodium-potassium pumps that transport sodium out of the cells and potassium into the cells.
Choice E reason:
Tissue injury. This is a condition where there is damage or destruction of body tissues due to trauma, infection, inflammation, or ischemia (lack of blood supply) Tissue injury can cause hyperkalemia by releasing potassium from the injured cells into the blood. This can occur in conditions such as burns, crush injuries, rhabdomyolysis (muscle breakdown), hemolysis (red blood cell breakdown), or tumor lysis syndrome (cancer cell breakdown)
A nurse is teaching a client who has osteoporosis about calcium supplements. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
Taking calcium supplements with milk is not recommended because milk contains phosphorus, which can interfere with calcium absorption.
Choice B reason:
Eating spinach while taking calcium supplements is not a problem, as spinach is a good source of calcium and other nutrients. However, spinach also contains oxalates, which can bind to calcium and reduce its absorption. Therefore, spinach should not be the only source of calcium in the diet.
Choice C reason:
Taking calcium supplements with vitamin D is the best option, as vitamin D helps the body absorb and use calcium more effectively. Vitamin D can be obtained from sunlight exposure, fortified foods, or supplements.
Choice D reason:
Limiting caffeine intake while taking calcium supplements is a good idea, but not the most important one. Caffeine can increase calcium excretion in the urine, but this effect can be offset by consuming adequate amounts of calcium from food or supplements.
A nurse is assessing a client who has hypomagnesemia. Which of the following findings should the nurse expect?
Explanation
Choice A reason:
Hypotension is not an expected finding for a client who has hypomagnesemia. Hypotension is more likely to occur with hypovolemia, which is a decrease in the amount of fluid in the blood vessels. Hypomagnesemia is a decrease in the amount of magnesium in the blood, which affects neuromuscular function and can cause muscle spasms, tremors, and seizures.
Choice B reason:
Bradycardia is not an expected finding for a client who has hypomagnesemia. Bradycardia is a slow heart rate, usually below 60 beats per minute. Hypomagnesemia can cause cardiac arrhythmias, such as tachycardia (fast heart rate), premature ventricular contractions (PVCs), and torsades de pointes (a type of ventricular tachycardia)
Choice C reason:
Muscle weakness is not an expected finding for a client who has hypomagnesemia. Muscle weakness is more likely to occur with hypermagnesemia, which is an excess of magnesium in the blood. Hypermagnesemia can cause decreased neuromuscular excitability and reduced muscle contraction.
Choice D reason:
Tetany is an expected finding for a client who has hypomagnesemia. Tetany is a condition characterized by involuntary muscle contractions, often affecting the hands and feet. It is caused by low levels of calcium or magnesium in the blood, which interfere with normal nerve impulses.
A nurse is preparing to administer IV fluids to a client who has dehydration. The nurse should select a solution that contains which of the following electrolytes to regulate ECF balance and vascular volume?
Explanation
Choice A reason:
Potassium is the major cation in the intracellular fluid (ICF), not the extracellular fluid (ECF) It is important for nerve and muscle function, but it does not regulate ECF balance and vascular volume.
Choice B reason:
Calcium is a cation that is mostly found in bones and teeth, but also plays a role in muscle contraction, blood clotting, and enzyme activity. It does not regulate ECF balance and vascular volume.
Choice C reason:
Chloride is the correct answer. It is the major anion in the ECF and it helps to maintain osmotic pressure, acid-base balance, and fluid volume. It often accompanies sodium in fluid replacement therapy.
Choice D reason:
Phosphate is an anion that is mostly found in bones and teeth, but also participates in energy metabolism, acid-base balance, and nucleic acid synthesis. It does not regulate ECF balance and vascular volume.
Factors Affecting Body Fluid, Electrolyte Fluid Imbalances
A nurse is assessing a client who has dehydration. Which of the following findings should the nurse expect?
Explanation
Choice A reason:
Decreased hematocrit is not a finding of dehydration, but rather of overhydration or hemodilution. Hematocrit is the percentage of red blood cells in the blood volume. When the blood volume is reduced due to dehydration, the hematocrit increases, not decreases.
Choice B reason:
Increased urine specific gravity is a finding of dehydration, as it indicates that the urine is more concentrated due to less water in the body. Urine specific gravity is a measure of the density of urine compared to water. Normal urine specific gravity ranges from 1.005 to 1.030. When the body is dehydrated, the kidneys reabsorb more water and produce less urine, resulting in higher urine specific gravity.
Choice C reason:
Decreased serum sodium is not a finding of dehydration, but rather of hyponatremia or low sodium level in the blood. Serum sodium is the amount of sodium in the blood plasma. Normal serum sodium ranges from 135 to 145 mEq/L. When the body is dehydrated, the serum sodium increases, not decreases, because there is less water to dilute the sodium concentration.
Choice D reason:
Increased capillary refill time is a finding of dehydration, as it indicates that the blood flow to the peripheral tissues is impaired due to low blood volume. Capillary refill time is the time it takes for the color to return to the nail bed after applying pressure. Normal capillary refill time is less than 3 seconds. When the body is dehydrated, the blood pressure drops and the heart rate increases to maintain adequate perfusion to vital organs, resulting in longer capillary refill time.
A nurse is caring for a client who has overhydration. Which of the following interventions should the nurse implement? (Select all that apply.)
Explanation
Choice A reason:
Monitoring intake and output is an important intervention for a client who has overhydration because it helps to assess the fluid balance and the effectiveness of treatment. The nurse should measure and record all sources of fluid intake and output, including oral, intravenous, tube feeding, urine, stool, wound drainage, and other losses.
Choice B reason:
Restricting fluid intake as prescribed is another intervention for a client who has overhydration because it helps to reduce the excess fluid volume and prevent further complications. The nurse should follow the prescribed fluid restriction and educate the client and family about the rationale and guidelines for fluid restriction.
Choice C reason:
Administering diuretics as prescribed is a pharmacological intervention for a client who has overhydration because it helps to increase urine output and eliminate excess fluid and sodium from the body. The nurse should monitor the client's response to diuretics, such as urine output, weight, blood pressure, electrolytes, and kidney function.
Choice D reason:
Elevating the head of the bed is a comfort measure for a client who has overhydration because it helps to improve breathing and reduce pulmonary congestion caused by fluid accumulation in the lungs. The nurse should elevate the head of the bed to at least 30 degrees or more, depending on the client's tolerance and preference.
Choice E reason:
Encouraging ambulation is not an appropriate intervention for a client who has overhydration because it may worsen the fluid overload and increase the risk of complications such as heart failure, pulmonary edema, or cerebral edema. The nurse should limit the client's physical activity and provide rest periods to conserve energy and reduce oxygen demand.
A nurse is teaching a client who has fluid volume overload about dietary modifications. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
Limiting salt intake to 2 grams per day is a good dietary modification for a client who has fluid volume overload, but it is not the best answer. Salt (sodium) can cause the body to retain water and increase the fluid volume in the bloodstream and tissues. Reducing salt intake can help prevent or reduce fluid overload, but it may not be enough by itself.
Choice B reason:
Drinking at least 3 liters of water every day is a bad dietary modification for a client who has fluid volume overload. This would increase the fluid intake and worsen the condition. A client who has fluid volume overload should limit their fluid intake to avoid excess fluid accumulation in the body. The amount of fluid restriction depends on the severity of the condition and the client's weight, urine output, and other factors.
Choice C reason:
Avoiding foods that are high in potassium is a bad dietary modification for a client who has fluid volume overload. Potassium is an essential mineral that helps regulate the balance of fluids and electrolytes in the body. A client who has fluid volume overload may have low potassium levels due to diuretic therapy, kidney problems, or other causes. Low potassium levels can cause muscle weakness, irregular heartbeat, and other complications. A client who has fluid volume overload should eat foods that are high in potassium, such as bananas, potatoes, tomatoes, oranges, and spinach, unless they have a medical condition that requires potassium restriction.
Choice D reason:
Using herbs and spices instead of salt to season food is the best dietary modification for a client who has fluid volume overload. This would help reduce the sodium intake and prevent or decrease fluid retention in the body. Herbs and spices can also add flavor and variety to the diet without adding calories or fat. Some examples of herbs and spices that can be used instead of salt are garlic, onion, ginger, basil, oregano, rosemary, thyme, parsley, cilantro, mint, lemon, lime, vinegar, pepper, chili, cumin, curry, turmeric, paprika, cinnamon, nutmeg, and cloves.
A client who has fluid volume deficit is receiving IV fluids. The nurse notices that the client has crackles in the lungs, dyspnea, and increased blood pressure. Which of the following actions should the nurse take first?
Explanation
Choice A reason: Slow down the infusion rate. This is the correct answer because the client is showing signs of fluid volume overload, which can result from rapid or excessive infusion of IV fluids. Slowing down the infusion rate can help prevent further fluid accumulation in the lungs and reduce the risk of pulmonary edema, which can impair gas exchange and cause respiratory distress.
Choice B reason:
Check the client's weight. This is not the correct answer because checking the client's weight is not a priority action in this situation. Although weight changes can reflect fluid balance, they are not an immediate indicator of fluid overload or deficit. The nurse should check the client's weight daily at the same time, but not before addressing the acute respiratory symptoms.
Choice C reason:
Notify the provider. This is not the correct answer because notifying the provider is not the first action that the nurse should take. The nurse should first implement independent nursing interventions to stabilize the client's condition, such as slowing down the infusion rate, elevating the head of the bed, and administering oxygen as needed. The nurse should notify the provider after assessing the client and intervening appropriately.
Choice D reason:
Raise the client's legs. This is not the correct answer because raising the client's legs can worsen fluid overload by increasing venous return to the heart and lungs. The nurse should avoid this position for clients who have crackles in the lungs, dyspnea, and increased blood pressure, as these are signs of fluid volume excess.
A nurse is reviewing the laboratory results of a client who has overhydration. Which of the following values should the nurse expect?
Explanation
-
Choice A reason:
-
Serum osmolality 280 mOsm/kg is not a sign of overhydration. Serum osmolality measures the concentration of dissolved particles in the blood. Normal serum osmolality ranges from 275 to 295 mOsm/kg. Overhydration causes serum osmolality to decrease because of the excess water in the blood.
-
Choice B reason:
-
Serum sodium 150 mEq/L is not a sign of overhydration. Serum sodium measures the amount of sodium (salt) in the blood. Normal serum sodium ranges from 135 to 145 mEq/L. Overhydration causes serum sodium to decrease because of the dilution of sodium by excess water. This condition is called hyponatremia and can affect brain function.
-
Choice C reason:
-
Hemoglobin 18 g/dL is not a sign of overhydration. Hemoglobin is a protein in red blood cells that carries oxygen. Normal hemoglobin ranges from 12 to 16 g/dL for women and from 14 to 18 g/dL for men. Overhydration does not directly affect hemoglobin levels, but it can cause hemodilution, which is a decrease in the concentration of hemoglobin due to increased plasma volume.
-
Choice D reason:
-
Urine specific gravity 1.005 is a sign of overhydration. Urine specific gravity measures the concentration of urine compared to water. Normal urine specific gravity ranges from 1.010 to 1.030. Overhydration causes urine specific gravity to decrease because of the excess water in the urine. This indicates that the kidneys are excreting more water than solutes.
Causes of Electrolyte Imbalances
A nurse is caring for a client with hypernatremia. Which of the following actions should the nurse take?
Explanation
Choice A reason:
Administering hypertonic saline solution IV is not appropriate for a client with hypernatremia, because it will increase the serum sodium level and worsen the condition. Hypertonic saline is only used in severe cases of hyponatremia, when the serum sodium level is very low.
Choice B reason:
Encouraging the client to drink caffeinated beverages is not helpful for a client with hypernatremia, because caffeine can act as a diuretic and cause further fluid loss and dehydration. The client should be encouraged to drink water or hypotonic fluids to dilute the sodium concentration in the blood.
Choice C reason:
Monitoring the client's serum sodium level is the correct action for the nurse to take, because it will help to evaluate the effectiveness of the treatment and detect any changes in the client's condition. The normal serum sodium level is 135 to 145 mEq/L (135 to 145 mmol/L) The nurse should monitor the client's serum sodium level frequently and report any abnormal values to the provider.
Choice D reason:
Increasing the client's sodium intake is contraindicated for a client with hypernatremia, because it will raise the serum sodium level and aggravate the symptoms. The client should avoid foods high in sodium, such as processed meats, cheese, canned soups, and salty snacks.
A nurse is reviewing the laboratory results of a client with hyponatremia. Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
Choice A reason:
Serum sodium level less than 135 mEq/L. This is an expected finding of hyponatremia, which is a condition of low sodium concentration in the blood. Sodium is an electrolyte that helps regulate fluid balance, nerve impulses, and muscle contractions. Hyponatremia can result from excessive fluid intake, diuretic use, vomiting, diarrhea, or kidney disease.
Choice B reason:
Serum osmolality less than 280 mOsm/kg. This is an expected finding of hyponatremia, which is a measure of the concentration of solutes in the blood. Osmolality reflects the body's ability to maintain fluid balance and hydration status. Hyponatremia causes a decrease in osmolality due to dilution of the blood by excess water.
Choice C reason:
Urine specific gravity less than 1.010. This is an expected finding of hyponatremia, which is a measure of the concentration of solutes in the urine. Specific gravity reflects the kidney's ability to concentrate or dilute urine. Hyponatremia causes a decrease in specific gravity due to increased urine output and water excretion.
Choice D reason:
Urine sodium level greater than 20 mEq/L. This is an expected finding of hyponatremia, which is a measure of the amount of sodium excreted in the urine. Sodium excretion reflects the kidney's ability to regulate sodium balance and fluid volume. Hyponatremia causes an increase in urine sodium level due to impaired sodium reabsorption and increased sodium loss.
Choice E reason:
Serum potassium level greater than 5 mEq/L. This is not an expected finding of hyponatremia, but rather a finding of hyperkalemia, which is a condition of high potassium concentration in the blood. Potassium is an electrolyte that helps regulate cardiac and neuromuscular function. Hyperkalemia can result from renal failure, acidosis, tissue injury, or medications that affect potassium excretion or shift.
A nurse is teaching a client with diabetes insipidus about the causes of hypernatremia. Which of the following statements by the client indicates a need for further teaching?
Explanation
Choice A reason:
Avoiding foods that are high in protein is not necessary for a client with diabetes insipidus. Protein intake does not affect the serum sodium level or the urine output in this condition. Therefore, this statement does not indicate a need for further teaching.
Choice B reason:
Drinking water whenever thirsty is not adequate for a client with diabetes insipidus. This condition causes excessive urine output and dehydration, which can lead to hypernatremia (high sodium level in the blood) The client should drink fluids according to a prescribed schedule and monitor the urine specific gravity to prevent fluid imbalance. Therefore, this statement indicates a need for further teaching.
Choice C reason:
Taking the prescribed medication as directed is important for a client with diabetes insipidus. The medication is usually a synthetic form of antidiuretic hormone (ADH), which helps the kidneys retain water and reduce urine output. This can prevent dehydration and hypernatremia. Therefore, this statement does not indicate a need for further teaching.
Choice D reason:
Limiting the intake of salt and salty foods is advisable for a client with diabetes insipidus. Salt intake can increase the serum sodium level and worsen the fluid imbalance. The client should follow a low-sodium diet and avoid processed foods, canned foods, and table salt. Therefore, this statement does not indicate a need for further teaching.
A nurse is assessing a client with syndrome of inappropriate anti-diuretic hormone (SIADH) Which of the following statements by the client indicates a possible complication of hyponatremia?
Explanation
Choice A reason:
A headache that won't go away is a possible complication of hyponatremia, which is a low level of sodium in the blood. Hyponatremia can cause brain swelling, which can lead to headaches, confusion, seizures, and coma.
Choice B reason:
Feeling very thirsty all the time is not a complication of hyponatremia, but rather a symptom of diabetes insipidus, which is a condition that causes the body to produce large amounts of dilute urine and lose water. Diabetes insipidus occurs when there is a deficiency of antidiuretic hormone (ADH), which is the opposite of SIADH.
Choice C reason:
Having trouble sleeping at night is not a complication of hyponatremia, but rather a common problem that can have many causes, such as stress, anxiety, caffeine, noise, or medication. Having trouble sleeping at night is not directly related to SIADH or sodium levels.
Choice D reason:
Losing weight recently is not a complication of hyponatremia, but rather a possible sign of fluid loss or dehydration. Fluid loss can occur in conditions that cause excessive urination, such as diabetes insipidus or diuretic use. Fluid loss can also cause hyponatremia, but it is not caused by SIADH.
A nurse is planning care for a client with hypocalcemia. Which of the following interventions should the nurse include in the plan?
Explanation
-
Choice A reason:
-
Administering calcium supplements orally or IV is not an appropriate intervention for a client with hypocalcemia. Calcium supplements can cause hypercalcemia, which can lead to cardiac arrhythmias, kidney stones, and constipation. Calcium supplements should only be given if the hypocalcemia is severe or symptomatic and under the supervision of a physician.
-
Choice B reason:
-
Monitoring the client for signs of tetany and seizures is an appropriate intervention for a client with hypocalcemia. Hypocalcemia can cause increased neuromuscular excitability, which can manifest as muscle spasms, cramps, twitching, or convulsions. Tetany is a condition where the muscles contract involuntarily and can affect the hands, feet, face, or larynx. Seizures are a result of abnormal electrical activity in the brain that can be triggered by low calcium levels. The nurse should monitor the client for these signs and intervene promptly to prevent complications.
-
Choice C reason:
-
Providing a high-phosphorus diet is not an appropriate intervention for a client with hypocalcemia. Phosphorus and calcium have an inverse relationship in the body, meaning that when one is high, the other is low. A high-phosphorus diet can lower the serum calcium level further and worsen the hypocalcemia. The nurse should advise the client to avoid foods high in phosphorus, such as dairy products, meat, poultry, fish, eggs, nuts, seeds, beans, and cola drinks.
-
Choice D reason:
-
Avoiding stimulating the facial nerve is not an appropriate intervention for a client with hypocalcemia. Stimulating the facial nerve can elicit a positive Chvostek's sign, which is a facial twitching that occurs when the nerve is tapped near the ear. A positive Chvostek's sign indicates hypocalcemia and increased neuromuscular irritability. However, avoiding stimulating the facial nerve does not prevent or treat hypocalcemia. The nurse should monitor the client for other signs of hypocalcemia and administer calcium as prescribed.
Nursing Assessment of Fluid and Electrolyte Imbalances
A nurse is assessing a client who has fluid volume deficit. Which of the following findings should the nurse expect?
Explanation
Choice A reason:
Increased skin turgor is not a sign of fluid volume deficit, but rather a sign of normal hydration. Skin turgor is the elasticity of the skin that allows it to return to its original shape after being pinched. Fluid volume deficit causes decreased skin turgor, which means the skin stays tented or takes longer to flatten after being pinched.
Choice B reason:
Hypertension is not a sign of fluid volume deficit, but rather a sign of fluid volume excess. Fluid volume deficit causes hypotension, which means low blood pressure. Fluid volume excess causes hypertension, which means high blood pressure. This is because fluid volume affects the amount of blood in the vessels and the pressure it exerts on the vessel walls.
Choice C reason:
Tachycardia is a sign of fluid volume deficit. Tachycardia means fast heart rate, usually more than 100 beats per minute. Fluid volume deficit causes tachycardia because the heart has to pump faster and harder to compensate for the low blood volume and maintain adequate blood flow to the vital organs.
Choice D reason:
Crackles in the lungs are not a sign of fluid volume deficit, but rather a sign of fluid volume excess or pulmonary edema. Crackles are abnormal lung sounds that indicate fluid accumulation in the alveoli or air sacs of the lungs. Fluid volume deficit does not cause fluid accumulation in the lungs, but rather dehydration of the lung tissues. Some additional information: Fluid volume deficit, also known as dehydration, is a condition where the body loses more fluids than it takes in. This can result from excessive vomiting, diarrhea, sweating, burns, hemorrhage, or diuretic use. Fluid volume excess, also known as overhydration or hypervolemia, is a condition where the body retains more fluids than it needs. This can result from excessive fluid intake, kidney failure, heart failure, liver cirrhosis, or steroid use. Fluid balance is essential for maintaining homeostasis and normal functioning of the body systems. Fluid balance is regulated by various mechanisms such as thirst, urine output, hormones, and electrolytes.
A nurse is caring for a client who has fluid volume excess. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A reason:
Monitoring daily weight is an important action for the nurse to take because it reflects the fluid status of the client. A sudden increase in weight indicates fluid retention, while a sudden decrease indicates fluid loss. The nurse should weigh the client at the same time every day, using the same scale and clothing.
Choice B reason:
Restricting sodium intake is another action that the nurse should take because sodium attracts water and increases fluid volume. The nurse should limit or avoid foods that are high in sodium, such as processed meats, canned soups, cheese, pickles, and salty snacks. The nurse should also educate the client about reading food labels and choosing low-sodium alternatives.
Choice C reason:
Administering diuretics as prescribed is a third action that the nurse should take because diuretics increase urine output and reduce fluid volume. The nurse should monitor the client's electrolyte levels, blood pressure, and urine output before and after giving diuretics. The nurse should also inform the client about the possible side effects of diuretics, such as dehydration, hypotension, hypokalemia, and ototoxicity.
Choice D reason:
Encouraging oral fluids is not an action that the nurse should take because it would worsen the fluid volume excess. The nurse should limit or restrict oral fluids as ordered by the provider. The nurse should also measure and record all fluid intake and output accurately.
Choice E reason:
Elevating the head of the bed is a fourth action that the nurse should take because it improves respiratory function and reduces pulmonary congestion. The nurse should elevate the head of the bed to at least 30 degrees or more, depending on the client's comfort and tolerance. The nurse should also monitor the client's oxygen saturation, breath sounds, and dyspnea.
A nurse is teaching a client who has chronic kidney disease about dietary modifications. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
A client who has chronic kidney disease should limit the intake of bananas and oranges because they are high in potassium, which can accumulate in the blood and cause hyperkalemia. Hyperkalemia can lead to cardiac arrhythmias and muscle weakness.
Choice B reason:
A client who has chronic kidney disease should not drink at least 3 liters of water every day because this can cause fluid overload and hypertension. Fluid overload can worsen the kidney function and increase the risk of heart failure and pulmonary edema. Hypertension can damage the blood vessels and organs.
Choice C reason:
A client who has chronic kidney disease should not eat more cheese and yogurt because they are high in phosphorus, which can bind with calcium and cause hypocalcemia and hyperphosphatemia. Hypocalcemia can lead to muscle cramps, tetany, and osteoporosis. Hyperphosphatemia can cause soft tissue calcification and itching.
Choice D reason:
A client who has chronic kidney disease should not use salt substitutes instead of table salt because they often contain potassium chloride, which can also increase the potassium level in the blood and cause hyperkalemia. Salt substitutes are not recommended for clients who have kidney disease or who are on potassium-sparing diuretics.
A nurse is evaluating a client who has dehydration and is receiving IV fluid therapy. Which of the following statements by the client indicates a positive outcome of the therapy?
Explanation
Choice A reason:
Feeling less thirsty is a sign of improved hydration status and a positive outcome of IV fluid therapy. Thirst is a subjective symptom of dehydration that is triggered by increased osmolality of the blood or decreased blood volume. When IV fluids are administered, they restore the fluid balance and reduce the thirst sensation.
Choice B reason:
Urine that is dark and concentrated is a sign of inadequate hydration and a negative outcome of IV fluid therapy. Urine color and concentration are influenced by the amount of fluid intake and output. When a person is dehydrated, the kidneys conserve water and produce less urine that is more concentrated and darker in color. When IV fluids are administered, they increase the urine output and dilute the urine, making it lighter in color.
Choice C reason:
A heart rate of 110 beats per minute is a sign of tachycardia and a negative outcome of IV fluid therapy. Tachycardia is an abnormal increase in heart rate that can be caused by dehydration, among other factors. Dehydration reduces the blood volume and lowers the blood pressure, which triggers the heart to beat faster to maintain adequate perfusion to the vital organs. When IV fluids are administered, they increase the blood volume and pressure and normalize the heart rate.
Choice D reason:
Having a headache and dizziness is a sign of cerebral dehydration and a negative outcome of IV fluid therapy. Headache and dizziness are common symptoms of dehydration that result from reduced blood flow to the brain and increased osmolality of the blood. When IV fluids are administered, they improve the cerebral perfusion and osmotic balance and relieve the headache and dizziness.
A nurse is planning care for a client who has hypernatremia. Which of the following interventions should the nurse include in the plan?
Explanation
-
Choice A reason:
-
Administering hypotonic IV fluids is an appropriate intervention for a client who has hypernatremia. Hypotonic fluids have a lower concentration of solutes than the blood, so they can help dilute the excess sodium and rehydrate the cells.
-
Choice B reason:
-
Monitoring blood glucose levels is not directly related to hypernatremia, although it may be indicated for other reasons, such as diabetes. Hypernatremia can be caused by uncontrolled diabetes, but it is not a consequence of high blood glucose levels.
-
Choice C reason:
-
Providing oral care every 4 hours is a supportive measure for a client who has hypernatremia, but it is not a specific intervention to correct the electrolyte imbalance. Oral care can help relieve thirst and dry mouth, which are common symptoms of hypernatremia, but it does not address the underlying cause of fluid loss or sodium gain.
-
Choice D reason:
-
Increasing dietary intake of potassium is not helpful for a client who has hypernatremia. Potassium is another electrolyte that plays a role in fluid balance and nerve function, but it is not affected by hypernatremia. In fact, increasing potassium intake may worsen the condition by causing further dehydration or hyperkalemia (high potassium levels)
Promoting Fluid and Electrolyte Balance
A nurse is caring for a client who has dehydration and is receiving dextrose 5% in water (D5W) intravenously. The nurse should monitor the client for which of the following complications of this type of solution?
Explanation
Choice A reason: Hyperglycemia. This is incorrect because dextrose 5% in water (D5W) is not likely to cause hyperglycemia in a dehydrated client. D5W is a hypotonic solution that provides free water and glucose to the body. The glucose is rapidly metabolized by the cells, leaving only water in the intravascular space. This water then moves into the intracellular and interstitial compartments, rehydrating the tissues. Therefore, D5W does not increase the blood glucose level significantly in a dehydrated client.
Choice B reason:
Hyperkalemia. This is incorrect because dextrose 5% in water (D5W) does not contain any potassium or other electrolytes. Hyperkalemia is a condition of high potassium level in the blood, which can be caused by renal failure, acidosis, tissue injury, or excessive intake of potassium-rich foods or supplements. D5W does not affect the potassium level in the blood.
Choice C reason:
Fluid overload. This is correct because dextrose 5% in water (D5W) can cause fluid overload in a client who has impaired fluid regulation mechanisms, such as heart failure, kidney disease, or liver disease. Fluid overload is a condition of excess fluid volume in the body, which can lead to edema, hypertension, dyspnea, crackles, jugular venous distension, and pulmonary congestion. D5W can cause fluid overload by expanding the intravascular volume and shifting water into the interstitial and intracellular spaces.
Choice D reason:
Metabolic acidosis. This is incorrect because dextrose 5% in water (D5W) does not cause metabolic acidosis in a dehydrated client. Metabolic acidosis is a condition of low pH and low bicarbonate level in the blood, which can be caused by diabetic ketoacidosis, lactic acidosis, renal failure, diarrhea, or ingestion of toxic substances. D5W does not affect the pH or bicarbonate level in the blood.
A nurse is preparing to administer lactated Ringer's (LR) solution to a client who has hypovolemia due to third-space shifting. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A reason:
Assess the client's blood pressure and pulse frequently. This is correct because a client who has hypovolemia due to third-space shifting has lost fluid from the intravascular space to the interstitial space, resulting in decreased blood volume and pressure. The nurse should monitor the client's vital signs to assess the response to fluid replacement and detect any signs of fluid overload or electrolyte imbalance.
Choice B reason:
Monitor the client's serum electrolyte levels. This is correct because lactated Ringer's solution contains sodium, chloride, potassium, calcium, and lactate, which are important electrolytes for maintaining fluid balance, acid-base balance, nerve conduction, muscle contraction, and cellular function. The nurse should monitor the client's serum electrolyte levels to ensure they are within normal range and to identify any abnormalities that may require intervention.
Choice C reason:
Warm the solution to body temperature before infusion. This is incorrect because warming the solution is not necessary and may cause hemolysis (destruction of red blood cells) or bacterial growth. The nurse should infuse the solution at room temperature or use a fluid warmer device if indicated.
Choice D reason:
Use a filter needle when drawing the solution from the bag. This is incorrect because using a filter needle is not required when drawing the solution from the bag. A filter needle is used to remove particles or air bubbles from a vial or ampule before injection. The nurse should use a sterile spike to pierce the bag and connect it to the IV tubing.
Choice E reason:
Check the solution for cracks or leaks. This is incorrect because checking the solution for cracks or leaks is not specific to lactated Ringer's solution. The nurse should check any IV fluid for cracks or leaks before administration to prevent contamination or infection. The nurse should also check the expiration date, color, clarity, and label of the solution before use.
A nurse is teaching a client who has diabetes mellitus about fluid and electrolyte balance. The nurse should instruct the client to increase fluid intake before, during, and after active exercise for which of the following reasons?
Explanation
Choice A reason:
To prevent hypernatremia and dehydration. This is the correct reason because exercise increases fluid loss through sweating and breathing, which can lead to dehydration and high sodium levels in the blood (hypernatremia) Dehydration and hypernatremia can cause symptoms such as thirst, confusion, weakness, and seizures. Therefore, increasing fluid intake before, during, and after active exercise can help maintain fluid and electrolyte balance in clients who have diabetes mellitus.
Choice B reason:
To dilute excess glucose and ketones in the blood. This is not a correct reason because increasing fluid intake does not lower blood glucose or ketone levels significantly. Clients who have diabetes mellitus should monitor their blood glucose and ketone levels regularly and adjust their insulin dosage and carbohydrate intake accordingly. Fluid intake alone is not enough to prevent hyperglycemia or ketoacidosis, which are serious complications of diabetes mellitus.
Choice C reason:
To promote renal perfusion and urine output. This is not a correct reason because increasing fluid intake does not improve kidney function or urine output in clients who have diabetes mellitus. Clients who have diabetes mellitus are at risk of developing diabetic nephropathy, which is a chronic kidney disease caused by damage to the blood vessels and glomeruli of the kidneys. Diabetic nephropathy can lead to reduced renal perfusion and urine output, as well as proteinuria, edema, hypertension, and renal failure. Therefore, increasing fluid intake does not prevent or treat diabetic nephropathy.
Choice D reason:
To replace lost electrolytes and prevent acidosis. This is not a correct reason because increasing fluid intake does not replenish electrolytes or prevent acidosis in clients who have diabetes mellitus. Clients who have diabetes mellitus are at risk of developing diabetic ketoacidosis (DKA), which is a life-threatening condition caused by insufficient insulin production or utilization, resulting in high blood glucose and ketone levels. DKA causes metabolic acidosis, which lowers the pH of the blood and body fluids. DKA also causes electrolyte imbalances, such as low potassium, sodium, chloride, and bicarbonate levels. Therefore, increasing fluid intake does not correct the metabolic acidosis or electrolyte imbalances caused by DKA.
A client who has Addison's crisis is receiving dextrose 5% in normal saline intravenously. The client asks the nurse why this type of solution is used. Which of the following responses should the nurse give?
Explanation
Choice A reason:
This is incorrect because dextrose 5% in normal saline is a hypertonic solution that will increase the blood sugar level, not lower it. Patients with Addison's crisis have low cortisol levels, which can impair glucose metabolism and cause hypoglycemia, so they need glucose supplementation.
Choice B reason:
This is partially correct because dextrose 5% in normal saline will provide some nutrition with glucose, but this is not the main reason for using this solution in Addison's crisis. Patients with Addison's crisis have low aldosterone levels, which can cause hyponatremia and hypovolemia, so they need sodium and fluid replacement.
Choice C reason:
This is correct because dextrose 5% in normal saline will correct the low sodium level caused by aldosterone deficiency in Addison's crisis. Sodium is essential for maintaining blood pressure, fluid balance, and nerve and muscle function. Dextrose 5% in normal saline will also increase the blood volume and prevent dehydration and shock.
Choice D reason:
This is partially correct because dextrose 5% in normal saline will increase the blood volume, but this is not the only solution that can do that. Other isotonic or hypertonic solutions can also expand the intravascular space. Dextrose 5% in normal saline is preferred in Addison's crisis because it also provides glucose and sodium, which are both deficient in this condition.
A nurse is reviewing the laboratory results of a client who has diabetic ketoacidosis (DKA) and is receiving 0.45% sodium chloride (1/2 normal saline) intravenously. Which of the following findings indicates that the therapy is effective?
Explanation
Choice A reason:
Decreased serum osmolarity. This is the correct answer because the goal of therapy for diabetic ketoacidosis (DKA) is to restore fluid and electrolyte balance, correct acidosis, and lower blood glucose levels. 0.45% sodium chloride (1/2 normal saline) is a hypotonic solution that helps to rehydrate the intracellular and extracellular compartments and reduce the serum osmolarity, which is elevated in DKA due to hyperglycemia and dehydration.
Choice B reason:
Increased urine specific gravity. This is incorrect because urine specific gravity reflects the concentration of solutes in the urine. In DKA, urine specific gravity is usually high due to osmotic diuresis caused by hyperglycemia and ketonuria. Effective therapy for DKA should lower the urine specific gravity as the blood glucose level and hydration status improve.
Choice C reason:
Decreased serum bicarbonate level. This is incorrect because serum bicarbonate level reflects the metabolic component of acid-base balance. In DKA, serum bicarbonate level is low due to increased production of ketoacids that consume bicarbonate as a buffer. Effective therapy for DKA should increase the serum bicarbonate level as the acidosis is corrected by insulin and fluid administration.
Choice D reason:
Increased serum potassium level. This is incorrect because serum potassium level is affected by several factors in DKA, such as insulin deficiency, acidosis, osmotic diuresis, and fluid therapy. In DKA, serum potassium level may be normal or high initially due to the shift of potassium from the intracellular to the extracellular space, but the total body potassium is depleted. Effective therapy for DKA should normalize the serum potassium level by replacing potassium losses and correcting the factors that cause potassium shift.
Techniques of Peripheral and Central Vascular Access
A nurse is caring for a client who has a peripheral venous access in the cephalic vein. The nurse notices that the site is red, warm, and tender to touch. The nurse should suspect that the client has developed:
Explanation
Choice A reason: Infiltration. This is when the IV fluid leaks into the surrounding tissue, causing swelling, coolness, and pallor. This does not match the symptoms of redness, warmth, and tenderness.
Choice B reason:
Extravasation. This is when the IV fluid is a vesicant, meaning it can cause tissue damage or necrosis if it leaks into the surrounding tissue. This can cause pain, burning, blistering, or skin sloughing. This does not match the symptoms of redness, warmth, and tenderness.
Choice C reason:
Phlebitis. This is when the vein becomes inflamed due to mechanical, chemical, or bacterial irritation. This can cause redness, warmth, tenderness, and a palpable cord along the vein. This matches the symptoms of the client.
Choice D reason:
Thrombophlebitis. This is when a blood clot forms in the vein, causing inflammation and obstruction. This can cause pain, swelling, redness, warmth, and a palpable cord along the vein. However, this is more likely to occur in larger veins such as the femoral or saphenous veins, not in the cephalic vein.
A nurse is preparing to administer intravenous fluids to a client who has a central venous access in the internal jugular vein. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A reason:
Incorrect. Checking the patency of the catheter by flushing it with normal saline is not necessary for a central venous access device (CVAD) that is already in place and functioning. Flushing is done before and after each medication administration or every 8 hours when medications are not being given.
Choice B reason:
Correct. Using aseptic technique when accessing the catheter is essential to prevent catheter-related bloodstream infections (CRBSIs), which are a serious complication of CVADs. The nurse should wear gloves, mask, and gown and use sterile equipment when changing the dressing or tubing.
Choice C reason:
Incorrect. Applying pressure dressing over the insertion site is not recommended for a CVAD in the internal jugular vein. Pressure dressings can increase the risk of thrombosis and occlusion of the catheter. A transparent semipermeable dressing is preferred to allow for visualization of the site and prevent moisture accumulation.
Choice D reason:
Correct. Monitoring the client for signs of infection and air embolism is a vital action for the nurse to take when caring for a client with a CVAD. Signs of infection include fever, chills, redness, swelling, drainage, or tenderness at the insertion site. Signs of air embolism include dyspnea, chest pain, hypotension, tachycardia, or altered mental status. The nurse should promptly report any abnormal findings to the provider.
Choice E reason:
Correct. Changing the dressing and tubing according to facility protocol is another important action for the nurse to take to maintain the patency and integrity of the CVAD and prevent complications. The dressing should be changed every 5 to 7 days or more frequently if it becomes loose, wet, or soiled. The tubing should be changed every 72 to 96 hours or per manufacturer's recommendations.
A nurse is teaching a client who has a peripheral venous access about the signs and symptoms of infiltration. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
This is incorrect because a burning sensation at the site is more likely to indicate phlebitis, which is inflammation of the vein, rather than infiltration, which is leakage of fluid into the surrounding tissue.
Choice B reason:
This is incorrect because blood leaking from the site is more likely to indicate a hematoma, which is a collection of blood outside the blood vessel, rather than infiltration.
Choice C reason:
This is correct because swelling and coolness around the site are common signs and symptoms of infiltration. Infiltration occurs when the IV fluid leaks into the surrounding tissue, causing edema and reduced blood flow.
Choice D reason:
This is incorrect because difficulty moving the arm is more likely to indicate nerve damage or compartment syndrome, which are serious complications of IV therapy, rather than infiltration.
A nurse is administering an antineoplastic medication to a client who has a central venous access in the subclavian vein. The nurse should monitor the client for extravasation, which can cause:
Explanation
Choice A reason:
Fever and chills are not signs of extravasation, but rather of infection or an allergic reaction to the antineoplastic medication.
Choice B reason:
Nausea and vomiting are common side effects of antineoplastic medications, but they are not caused by extravasation. Extravasation is the leakage of the medication into the surrounding tissues.
Choice C reason:
Tissue necrosis and deformity are possible consequences of extravasation, especially with vesicant drugs that can cause severe tissue damage. The nurse should monitor the client for pain, swelling, redness, or blistering at the infusion site and stop the infusion immediately if extravasation is suspected.
Choice D reason:
Hypotension and tachycardia are not specific signs of extravasation, but rather of shock or hemorrhage. The nurse should monitor the client's vital signs and report any abnormal findings to the primary health care provider.
A nurse is reviewing the medical record of a client who has a history of thrombophlebitis. The nurse should identify that which of the following factors increases the risk of developing this complication?
Explanation
Choice A reason:
Dehydration is not a risk factor for thrombophlebitis, which is inflammation of a vein due to a blood clot. Dehydration can cause hemoconcentration, which increases the risk of thrombosis, but not necessarily thrombophlebitis.
Choice B reason:
Immobility is a risk factor for thrombophlebitis, as it reduces blood flow and increases the chance of clot formation in the veins. Immobility can also impair the function of the calf muscles, which normally help pump blood back to the heart.
Choice C reason:
Hyperglycemia is not a risk factor for thrombophlebitis, although it can increase the risk of other vascular complications, such as atherosclerosis and peripheral arterial disease. Hyperglycemia can damage the endothelial lining of the blood vessels, but this does not directly cause thrombophlebitis.
Choice D reason:
Hypertension is not a risk factor for thrombophlebitis, although it can increase the risk of other cardiovascular problems, such as stroke and heart failure. Hypertension can increase the pressure and stress on the arterial walls, but this does not affect the venous system where thrombophlebitis occurs.
More questions on this topic
A nurse is caring for a client who has metabolic alkalosis and is receiving sodium chloride and potassium chloride IV fluids. The nurse should monitor for which of the following complications of this therapy?
Explanation
Choice A reason:
Hypernatremia is not a likely complication of sodium chloride and potassium chloride IV fluids, because these fluids do not contain excessive amounts of sodium. Hypernatremia is more likely to occur with hypertonic saline solutions or excessive sodium intake.
Choice B reason:
Hypokalemia is not a likely complication of sodium chloride and potassium chloride IV fluids, because these fluids contain potassium, which can help prevent or correct hypokalemia. Hypokalemia is more likely to occur with diuretic therapy, vomiting, or diarrhea.
Choice C reason:
Hyperchloremic acidosis is a likely complication of sodium chloride and potassium chloride IV fluids, because these fluids can increase the serum chloride level and lower the serum bicarbonate level, resulting in a metabolic acidosis. Hyperchloremic acidosis can also worsen the client's existing metabolic alkalosis by impairing the renal excretion of hydrogen ions.
Choice D reason:
Hypochloremic alkalosis is not a likely complication of sodium chloride and potassium chloride IV fluids, because these fluids do not cause a loss of chloride or an increase in bicarbonate. Hypochloremic alkalosis is more likely to occur with vomiting, gastric suctioning, or diuretic therapy.
A nurse is evaluating the effectiveness of IV fluid therapy for a client who has dehydration. Which of the following findings indicates improvement?
Explanation
Choice A reason:
Decreased urine specific gravity indicates improvement in hydration status. Urine specific gravity is a measure of the concentration of solutes in the urine. It reflects the ability of the kidney to concentrate or dilute urine. A high urine specific gravity (>1.030) indicates concentrated urine, which can be caused by dehydration, reduced renal blood flow, or increased fluid loss. A low urine specific gravity (<1.010) indicates diluted urine, which can be caused by overhydration, diuretic use, or impaired renal function. A normal urine specific gravity ranges from 1.010 to 1.030.
Choice B reason:
Increased hematocrit level indicates worsening of dehydration. Hematocrit is the percentage of red blood cells in the total blood volume. It is affected by the plasma volume and the number of red blood cells. A high hematocrit (>47% for males and >42% for females) indicates hemoconcentration, which can be caused by dehydration, polycythemia, or hypoxia. A low hematocrit (<37% for males and <32% for females) indicates hemodilution, which can be caused by overhydration, anemia, or hemorrhage. A normal hematocrit ranges from 37% to 47% for males and 32% to 42% for females.
Choice C reason:
Decreased skin turgor indicates persistent dehydration. Skin turgor is the elasticity of the skin that reflects its hydration status. It is assessed by pinching a fold of skin on the chest, abdomen, or forearm and releasing it. Normally, the skin should return to its original position in less than 3 seconds. If the skin remains elevated or takes longer to return, it indicates poor skin turgor, which can be caused by dehydration, aging, or edema.
Choice D reason:
Increased serum osmolarity indicates worsening of dehydration. Serum osmolarity is a measure of the concentration of solutes in the blood plasma. It reflects the balance between water and electrolytes in the body fluids. A high serum osmolarity (>300 mOsm/kg) indicates hyperosmolarity, which can be caused by dehydration, hypernatremia, hyperglycemia, or mannitol infusion. A low serum osmolarity (<280 mOsm/kg) indicates hypoosmolarity, which can be caused by overhydration, hyponatremia, syndrome of inappropriate antidiuretic hormone secretion (SIADH), or diuretic use. A normal serum osmolarity ranges from 280 to 300 mOsm/kg.
A nurse is planning care for a client who has hyponatremia and is receiving IV fluid therapy with 3% sodium chloride solution. Which of the following interventions should the nurse include in the plan? (Select all that apply.)
Explanation
Choice A reason:
Administer the solution via a central line. This is correct because 3% sodium chloride solution is a hypertonic solution that can cause phlebitis and tissue damage if infused peripherally. A central line can deliver the solution more safely and effectively.
Choice B reason:
Monitor serum sodium levels every 4 hours. This is correct because serum sodium levels can indicate the effectiveness of the therapy and the risk of complications such as hypernatremia or cerebral edema. The normal range of serum sodium is 135 to 145 mEq/L.
Choice C reason:
Titrate the infusion rate according to urine output. This is incorrect because the infusion rate of 3% sodium chloride solution should be titrated according to serum sodium levels, not urine output. Urine output can be affected by other factors such as renal function, fluid intake, and diuretics.
Choice D reason:
Assess for signs of fluid overload. This is correct because 3% sodium chloride solution can cause fluid shifts from the intracellular and interstitial spaces to the intravascular space, leading to fluid overload. Signs of fluid overload include cough, dyspnea, crackles, tachypnea, tachycardia, elevated blood pressure, bounding pulse, elevated central venous pressure (CVP), weight gain, edema, neck and hand vein distention, altered level of consciousness, and decreased hematocrit.
Choice E reason:
Keep an accurate intake and output record. This is correct because intake and output records can help monitor the fluid balance and identify any excesses or deficits. Intake includes oral fluids, intravenous fluids, tube feedings, and blood products. Output includes urine, stool, vomitus, drainage, and insensible losses.
A nurse is caring for a client who has diabetic ketoacidosis and is receiving an insulin infusion and IV fluids containing dextrose and normal saline. The nurse should monitor for which of the following complications of fluid therapy?
Explanation
Choice A reason:
Hypernatremia is not a likely complication of fluid therapy for diabetic ketoacidosis (DKA) Hypernatremia occurs when there is a loss of water or an excess of sodium in the body. Fluid therapy for DKA usually involves normal saline and dextrose, which do not cause hypernatremia. In fact, fluid therapy may help correct the dehydration and hyperosmolality that are associated with DKA.
Choice B reason:
Hyperkalemia is also not a likely complication of fluid therapy for DKA. Hyperkalemia occurs when there is an excess of potassium in the blood. Fluid therapy for DKA usually involves insulin infusion, which helps lower the potassium level by driving it into the cells. Insulin also helps lower the blood glucose level and reverse the acidosis that are characteristic of DKA.
Choice C reason:
Fluid volume deficit is a common manifestation of DKA, not a complication of fluid therapy. Fluid volume deficit occurs when there is a loss of fluid and electrolytes from the body due to osmotic diuresis, vomiting, and increased respiratory rate. Fluid therapy for DKA aims to restore the fluid volume and correct the electrolyte imbalances that result from fluid loss.
Choice D reason:
Cerebral edema is a potential complication of fluid therapy for DKA, especially in children and young adults. Cerebral edema occurs when there is an increase in intracranial pressure due to swelling of the brain tissue. Fluid therapy for DKA may cause cerebral edema by altering the osmotic gradient between the blood and the brain, leading to fluid shifts into the brain cells. Cerebral edema can cause neurological symptoms such as headache, confusion, seizures, and coma.
A nurse is administering albumin to a client who has hypovolemic shock due to hemorrhage. The nurse understands that albumin is which of the following types of solutions?
Explanation
Choice A reason:
Crystalloid solutions are fluids that contain electrolytes and can diffuse across semipermeable membranes. They are used to treat dehydration, electrolyte imbalances, and hypovolemia. However, they are not as effective as colloids in expanding the intravascular volume and maintaining the blood pressure. Therefore, choice A is incorrect.
Choice B reason:
Colloid solutions are fluids that contain large molecules such as proteins, starches, or gelatin that cannot cross the capillary membrane. They exert an osmotic pressure that draws fluid from the interstitial and intracellular spaces into the intravascular space. They are used to treat hypovolemic shock, burns, and hemorrhage. Albumin is a type of colloid solution that is derived from human plasma and contains 5% or 25% protein. It increases the plasma volume and the blood pressure by increasing the oncotic pressure. Therefore, choice B is correct.
Choice C reason:
Hypertonic solutions are fluids that have a higher osmolarity than the blood plasma. They draw water out of the cells and into the intravascular space. They are used to treat hyponatremia, cerebral edema, and severe dehydration. However, they can cause fluid overload, hypertension, and cellular dehydration if given in excess. Therefore, choice C is incorrect.
Choice D reason:
Hypotonic solutions are fluids that have a lower osmolarity than the blood plasma. They provide free water and electrolytes to the cells and the interstitial space. They are used to treat hypernatremia, cellular dehydration, and fluid loss due to burns or diuresis. However, they can cause fluid shifts from the intravascular space to the interstitial and intracellular spaces, resulting in hypovolemia, hypotension, and edema. Therefore, choice D is incorrect.
A nurse is evaluating the effectiveness of fluid therapy for a client who has hypernatremia. Which of the following findings indicates improvement? (Select all that apply.)
Explanation
Choice A reason:
Decreased thirst. This is a sign of improvement because hypernatremia causes increased thirst due to high sodium levels in the blood. Decreased thirst indicates that the fluid therapy has restored the normal balance of sodium and water in the body.
Choice B reason:
Increased urine output. This is a sign of improvement because hypernatremia can cause decreased urine output due to dehydration or kidney dysfunction. Increased urine output indicates that the fluid therapy has replenished the body's water and helped the kidneys excrete excess sodium.
Choice C reason:
Decreased serum sodium level. This is a sign of improvement because hypernatremia is defined as a serum sodium level higher than 145 mEq/L. Decreased serum sodium level indicates that the fluid therapy has diluted the blood and lowered the sodium concentration to within the normal range.
Choice D reason:
Increased level of consciousness. This is a sign of improvement because hypernatremia can cause confusion, lethargy, or coma due to the effects of high sodium levels on the brain. Increased level of consciousness indicates that the fluid therapy has improved the brain function and reduced the risk of brain injury.
Choice E reason:
Decreased edema. This is not a sign of improvement because hypernatremia does not cause edema, which is the accumulation of fluid in the interstitial spaces. Edema is more likely to occur in conditions such as hypervolemia (excess fluid volume) or hyponatremia (low sodium levels) Decreased edema may indicate that the fluid therapy has caused fluid overload or electrolyte imbalance, which can be harmful.
A nurse is caring for a client who has metabolic alkalosis as a result of prolonged nasogastric suctioning. The nurse should expect which of the following arterial blood gas values?
Explanation
Choice A reason:
pH 7.50, PaCO2 40 mm Hg, HCO3- 30 mEq/L. This choice is correct because it shows a high pH, a normal PaCO2, and a high HCO3-, which are consistent with metabolic alkalosis. Metabolic alkalosis occurs when there is a loss of acid or a gain of base in the body fluids, such as from prolonged nasogastric suctioning. The kidneys try to compensate by excreting more bicarbonate, but this process is slow and incomplete.
Choice B reason:
pH 7.35, PaCO2 35 mm Hg, HCO3- 24 mEq/L. This choice is incorrect because it shows normal values for pH, PaCO2, and HCO3-, which indicate no acid-base imbalance. A client with metabolic alkalosis would have an elevated pH and bicarbonate level.
Choice C reason:
pH 7.25, PaCO2 50 mm Hg, HCO3- 26 mEq/L. This choice is incorrect because it shows a low pH, a high PaCO2, and a normal HCO3-, which are consistent with respiratory acidosis. Respiratory acidosis occurs when there is impaired gas exchange or hypoventilation, leading to an accumulation of carbon dioxide in the blood. The kidneys try to compensate by retaining more bicarbonate, but this process is slow and incomplete.
Choice D reason:
pH 7.30, PaCO2 30 mm Hg, HCO3- 18 mEq/L. This choice is incorrect because it shows a low pH, a low PaCO2, and a low HCO3-, which are consistent with metabolic acidosis. Metabolic acidosis occurs when there is a gain of acid or a loss of base in the body fluids, such as from diabetic ketoacidosis or diarrhea. The lungs try to compensate by increasing the rate and depth of breathing to expel more carbon dioxide, but this process is fast and limited.
A nurse is reviewing the laboratory report of a client who has diabetic ketoacidosis (DKA) Which of the following findings should the nurse expect?
Explanation
Choice A reason:
Serum glucose 600 mg/dL. This is an expected finding for a client who has diabetic ketoacidosis (DKA) DKA results from a deficiency of insulin, which leads to hyperglycemia and ketosis. The normal range for serum glucose is 70 to 110 mg/dL.
Choice B reason:
Serum bicarbonate 28 mEq/L. This is not an expected finding for a client who has DKA. A client who has DKA experiences ketosis, which results in ketones in the urine and blood. The nurse should expect a client who has DKA to have an HCO3- less than 15 mEq/L. This decreased value is due to an increased production of ketones, which results in metabolic acidosis. The normal range for serum bicarbonate is 22 to 26 mEq/L.
Choice C reason:
Serum potassium 2.5 mEq/L. This is not an expected finding for a client who has DKA. A client who has DKA experiences osmotic diuresis and subsequent dehydration, which can cause electrolyte imbalances. The nurse should expect a client who has DKA to have elevated serum potassium levels due to the movement of potassium from the intracellular to the extracellular space in response to acidosis. The normal range for serum potassium is 3.5 to 5 mEq/L.
Choice D reason:
Serum sodium 150 mEq/L. This is not an expected finding for a client who has DKA. A client who has DKA experiences osmotic diuresis and subsequent dehydration, which can cause electrolyte imbalances. The nurse should expect a client who has DKA to have decreased serum sodium levels due to the dilutional effect of excess glucose in the blood. The normal range for serum sodium is 136 to 145 mEq/L.
A nurse is providing discharge instructions to a client who has chronic heart failure and is prescribed furosemide, a loop diuretic. Which of the following dietary modifications should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A reason:
Furosemide is a potassium-wasting diuretic that may reduce the potassium level in your blood. To counteract the loss of potassium, you should try to eat enough potassium-rich foods in your diet. Some examples of potassium-rich foods include bananas, orange juice, apricots, acorn squash, butternut squash, Hubbard squash, prunes, raisins, and bran products.
Choice B reason:
Furosemide is used to treat high blood pressure and edema by causing the kidneys to get rid of unneeded water and salt from the body into the urine. To enhance the effect of furosemide and prevent fluid retention, you should decrease intake of foods high in sodium. Some examples of sodium-rich foods include processed meats, canned soups, pickles, cheese, salted nuts, and snack foods.
Choice C reason:
Furosemide does not affect the calcium level in your blood significantly. Therefore, there is no need to increase intake of foods high in calcium when taking furosemide. However, you should still consume adequate amounts of calcium for your bone health and other functions. Some examples of calcium-rich foods include milk, yogurt, cheese, broccoli, kale, and fortified cereals.
Choice D reason:
Furosemide does not affect the protein level in your blood significantly. Therefore, there is no need to decrease intake of foods high in protein when taking furosemide. However, you should still consume moderate amounts of protein for your muscle health and other functions. Some examples of protein-rich foods include eggs, fish, poultry, meat, beans, nuts, and seeds.
Choice E reason:
Furosemide can cause dehydration and electrolyte imbalance by increasing urine output. Therefore, you should increase intake of fluids as tolerated to prevent these complications. You should drink enough water to keep your urine clear or pale yellow. You should also avoid alcohol and caffeine as they can worsen dehydration.
A nurse is caring for a client who has metabolic acidosis and is receiving sodium bicarbonate IV bolus and infusion to correct the pH imbalance. Which of the following laboratory values should the nurse monitor to evaluate the effectiveness of the therapy?
Explanation
Choice A reason:
Serum sodium is not directly related to the acid-base balance of the body. Sodium bicarbonate therapy does not affect the serum sodium level significantly. Therefore, monitoring serum sodium is not an effective way to evaluate the effectiveness of the therapy.
Choice B reason:
Serum potassium is inversely related to the serum pH. As the pH increases, the potassium level decreases, and vice versa. Sodium bicarbonate therapy raises the pH and lowers the potassium level. Therefore, monitoring serum potassium is important to prevent hypokalemia, but it does not directly reflect the acid-base balance of the body.
Choice C reason:
Serum chloride is inversely related to the serum bicarbonate level. As the bicarbonate level increases, the chloride level decreases, and vice versa. Sodium bicarbonate therapy increases the bicarbonate level and decreases the chloride level. Therefore, monitoring serum chloride is important to prevent hypochloremia, but it does not directly reflect the acid-base balance of the body.
Choice D reason:
Serum bicarbonate is directly related to the acid-base balance of the body. The normal range of serum bicarbonate is 22 to 26 mEq/L. In metabolic acidosis, the bicarbonate level is low, and in metabolic alkalosis, it is high. Sodium bicarbonate therapy aims to increase the bicarbonate level and correct metabolic acidosis. Therefore, monitoring serum bicarbonate is the most effective way to evaluate the effectiveness of the therapy.
A nurse is reviewing the laboratory results of a client who has chronic kidney disease and notes that the serum phosphate level is elevated. The nurse should anticipate that which of the following electrolyte levels will be decreased?
Explanation
Choice A reason: Sodium. Sodium is not affected by serum phosphate level in chronic kidney disease (CKD) patients. Sodium level is mainly regulated by the renin-angiotensin-aldosterone system and the antidiuretic hormone. Sodium level can be altered by fluid intake, fluid loss, diuretics, or salt restriction, but not by phosphate level.
Choice B reason:
Magnesium. Magnesium is also not affected by serum phosphate level in CKD patients. Magnesium level is mainly influenced by dietary intake, intestinal absorption, renal excretion, and exchange with bone and soft tissues. Magnesium level can be altered by malnutrition, malabsorption, diarrhea, vomiting, diuretics, or alcoholism, but not by phosphate level.
Choice C reason:
Calcium. Calcium is the correct answer because calcium and phosphate have an inverse relationship in the body. When serum phosphate level is elevated, as in CKD patients, serum calcium level tends to decrease. This is because high phosphate level binds to calcium and forms insoluble complexes that are deposited in soft tissues and bones. This reduces the amount of free calcium in the blood and triggers the secretion of parathyroid hormone (PTH), which further lowers the calcium level by increasing its excretion in the urine.
Choice D reason:
Bicarbonate. Bicarbonate is not directly affected by serum phosphate level in CKD patients. Bicarbonate level is mainly determined by the acid-base balance in the body. Bicarbonate level can be altered by metabolic acidosis or alkalosis, respiratory acidosis or alkalosis, renal failure, or diarrhea, but not by phosphate level.
A nurse is providing dietary teaching to a client who has hypocalcemia due to hypoparathyroidism. Which of the following foods should the nurse recommend? (Select all that apply.)
Explanation
Choice A reason:
Cheese is a good source of calcium, which is essential for bone health and muscle contraction. Calcium also helps regulate the heart rhythm and blood clotting. Cheese can provide about 200 mg of calcium per ounce.
Choice B reason:
Broccoli is a cruciferous vegetable that contains goitrogens, which are substances that can interfere with thyroid hormone synthesis and cause or worsen hypothyroidism. Hypothyroidism can lead to low levels of parathyroid hormone (PTH), which is responsible for maintaining calcium balance in the body. Therefore, broccoli should be avoided or limited by clients who have hypocalcemia due to hypoparathyroidism.
Choice C reason:
Almonds are rich in magnesium, which is a mineral that helps regulate calcium absorption and metabolism. Magnesium also plays a role in nerve and muscle function, blood pressure, and blood sugar control. Almonds can provide about 80 mg of magnesium per ounce.
Choice D reason:
Bananas are high in potassium, which is a mineral that can affect the balance of calcium in the body. High levels of potassium can cause hyperkalemia, which can lower the serum calcium level by increasing the renal excretion of calcium and decreasing the release of PTH. Therefore, bananas should be avoided or limited by clients who have hypocalcemia due to hypoparathyroidism.
Choice E reason:
Sardines are a type of oily fish that contain vitamin D, which is a fat-soluble vitamin that helps increase the intestinal absorption of calcium and phosphorus. Vitamin D also works with PTH to regulate the bone resorption and formation of calcium. Sardines can provide about 250 IU of vitamin D per 3 ounces.
A nurse is caring for a client who has dehydration due to vomiting and diarrhea. The client's blood pressure is 90/60 mm Hg, pulse is 110/min, and respirations are 22/min. The nurse should anticipate a prescription for which of the following types of IV fluids?
Explanation
Choice A reason:
Dextrose 5% in water (D5W) is a hypotonic solution that provides free water and calories, but no electrolytes. It is used to treat hypernatremia and cellular dehydration, but it can cause fluid shifts from the intravascular to the intracellular space, leading to cerebral edema and decreased blood pressure. This is not appropriate for a client who has dehydration due to vomiting and diarrhea, as they need to restore their intravascular volume and electrolyte balance.
Choice B reason:
Lactated Ringer's (LR) is an isotonic solution that contains sodium, chloride, potassium, calcium, and lactate. It is used to treat fluid loss from burns, trauma, surgery, or sepsis. It also helps to correct metabolic acidosis by providing bicarbonate precursors. This is the best choice for a client who has dehydration due to vomiting and diarrhea, as they need to replace their fluid and electrolyte losses and maintain their acid-base balance.
Choice C reason:
Dextrose 5% in 0.45% sodium chloride (D5W/0.45% NaCl) is a hypertonic solution that provides free water, calories, and sodium. It is used to treat hypovolemia and hyponatremia, but it can cause fluid shifts from the intracellular to the intravascular space, leading to cellular dehydration and increased blood pressure. This is not appropriate for a client who has dehydration due to vomiting and diarrhea, as they already have low blood pressure and cellular dehydration.
Choice D reason:
Dextrose 5% in lactated Ringer's (D5LR) is a hypertonic solution that provides free water, calories, sodium, chloride, potassium, calcium, and lactate. It is used to treat hypovolemia and metabolic acidosis, but it can cause fluid shifts from the intracellular to the intravascular space, leading to cellular dehydration and increased blood pressure. This is not appropriate for a client who has dehydration due to vomiting and diarrhea, as they already have low blood pressure and cellular dehydration.
A nurse is evaluating a client who has fluid volume overload and received furosemide 40 mg IV bolus 1 hr ago. Which of the following findings indicates that the medication was effective?
Explanation
Choice A reason:
The client reports increased thirst. This is not an indication that the medication was effective, because increased thirst can be a sign of dehydration or electrolyte imbalance caused by excessive diuresis. Furosemide can cause loss of water and sodium, potassium, calcium, magnesium, and chloride in the urine.
Choice B reason:
The client's urine output is 250 mL/hr. This is an indication that the medication was effective, because furosemide is a loop diuretic that inhibits the reabsorption of sodium and water in the ascending limb of the loop of Henle, resulting in increased urine output and decreased fluid volume. A normal urine output is about 30 to 60 mL/hr, so a urine output of 250 mL/hr indicates a significant diuretic effect.
Choice C reason:
The client's heart rate is 100/min. This is not an indication that the medication was effective, because a high heart rate can be a sign of hypovolemia, hypotension, or cardiac stress caused by furosemide. Furosemide can lower the blood pressure and reduce the preload and afterload on the heart, but it can also trigger compensatory mechanisms such as increased sympathetic activity and renin-angiotensin-aldosterone system activation, which can increase the heart rate.
Choice D reason:
The client's weight is unchanged. This is not an indication that the medication was effective, because weight loss is expected with furosemide therapy due to fluid removal. Furosemide can cause a rapid and significant reduction in fluid volume, which can be measured by daily weight changes. A weight loss of 1 kg corresponds to a fluid loss of about 1 L.
A nurse is planning care for a client who has overhydration and hyponatremia. Which of the following actions should the nurse include in the plan? (Select all that apply.)
Explanation
Choice A reason:
Monitoring neurological status is a priority intervention for a client who has overhydration and hyponatremia because these conditions can cause cerebral edema, increased intracranial pressure, and altered mental status. The nurse should assess the client for signs of confusion, lethargy, seizures, and coma, and report any changes to the provider.
Choice B reason:
Administering sodium polystyrene sulfonate is not indicated for a client who has overhydration and hyponatremia. This medication is used to treat hyperkalemia by exchanging sodium ions for potassium ions in the intestine. It has no effect on sodium levels or fluid balance.
Choice C reason:
Providing oral hygiene frequently is a supportive intervention for a client who has overhydration and hyponatremia, but it is not a priority. Oral hygiene can help prevent dry mouth, infections, and discomfort caused by fluid retention and electrolyte imbalance. However, it does not address the underlying causes or complications of the disorder.
Choice D reason:
Restricting sodium intake as prescribed is an essential intervention for a client who has overhydration and hyponatremia. Sodium intake can affect the serum sodium level and the fluid balance in the body. Excessive sodium intake can worsen fluid retention and edema, while inadequate sodium intake can exacerbate hyponatremia. The nurse should follow the provider's orders regarding sodium restriction and educate the client on how to avoid high-sodium foods and beverages.
Choice E reason:
Encouraging foods high in protein is not appropriate for a client who has overhydration and hyponatremia. Protein intake can affect the serum osmolality and the fluid distribution in the body. High-protein foods can increase the osmotic pressure in the blood vessels, drawing more fluid from the interstitial and intracellular spaces. This can worsen overhydration and hyponatremia by diluting the serum sodium level further. The nurse should consult with a dietitian regarding the optimal protein intake for the client.
A patient has been admitted with a potassium level of 6.8 mEq/L. The nurse would expect which of the following electrocardiogram (ECG) changes as a result of this laboratory value?
Explanation
Choice A reason:
U waves are not a sign of high potassium level, but rather of low potassium level (hypokalemia) Hypokalemia can cause ST segment depression, T wave flattening or inversion, and prominent U waves.
Choice B reason:
Absent P waves are not a sign of high potassium level, but rather of a severe conduction block or atrial fibrillation. High potassium level can cause P wave widening or flattening, and PR prolongation, but not complete disappearance of P waves.
Choice C reason:
Elevated T waves are the most common and earliest sign of high potassium level (hyperkalemia) Hyperkalemia can cause tall, peaked, symmetric T waves that may merge with the QRS complex. This is the correct answer.
Choice D reason:
Inverted QRS complexes are not a sign of high potassium level, but rather of ventricular arrhythmias or myocardial infarction. High potassium level can cause QRS widening and bizarre QRS morphology, but not inversion.
The nurse is caring for a patient who has been vomiting and has diarrhea for 3 days and now has muscle weakness and paresthesias in his hands and feet, along with an irregular pulse rate and rhythm, and shallow respirations with crackles on auscultation of his lungs bilaterally. The nurse suspects that these symptoms are most likely due to which electrolyte imbalance?
Explanation
Choice A: Hypercalcemia. This is a condition of having too much calcium in the blood. It can cause muscle weakness, constipation, nausea, vomiting, confusion, and irregular heartbeat. However, it does not typically cause paresthesias (tingling or numbness), diarrhea, or crackles in the lungs.
Choice B:
Hypokalemia. This is a condition of having too low potassium in the blood. It can cause muscle weakness, paresthesias, irregular heartbeat, shallow respirations, and increased risk of digoxin toxicity (a medication used to treat heart failure) It can also cause vomiting and diarrhea, which can worsen the potassium loss. This choice matches the symptoms of the patient.
Choice C:
Hypermagnesemia. This is a condition of having too much magnesium in the blood. It can cause muscle weakness, nausea, vomiting, low blood pressure, bradycardia (slow heart rate), and respiratory depression. However, it does not usually cause paresthesias, diarrhea, or crackles in the lungs.
Choice D:
Hypophosphatemia. This is a condition of having too low phosphate in the blood. It can cause muscle weakness, bone pain, rickets (softening of bones), and impaired cellular function. However, it does not typically cause paresthesias, irregular heartbeat, shallow respirations, or crackles in the lungs.
A nurse is caring for a client who has hypomagnesemia due to chronic alcohol use disorder. Which of the following actions should the nurse take?
Explanation
Choice A reason:
Administer magnesium sulfate IV. This is correct because magnesium sulfate is the treatment of choice for severe hypomagnesemia. It can rapidly increase the blood level of magnesium and correct the symptoms of deficiency.
Choice B reason:
Monitor the client's blood pressure and heart rate. This is incorrect because monitoring vital signs is not a specific intervention for hypomagnesemia. However, it is important to monitor the client for signs of hypotension and bradycardia, which can occur as adverse effects of magnesium sulfate therapy.
Choice C reason:
Encourage the client to increase intake of green leafy vegetables. This is correct because green leafy vegetables are rich sources of dietary magnesium. Increasing the intake of magnesium-rich foods can help prevent or treat mild hypomagnesemia.
Choice D reason:
Prepare to administer calcium gluconate IV. This is incorrect because calcium gluconate is not indicated for hypomagnesemia. Calcium gluconate is used to treat hypocalcemia, which can occur as a complication of hypomagnesemia. However, calcium gluconate should not be given until the magnesium level is corrected, as low magnesium can impair the response to calcium.
Choice E reason:
Assess the client for Chvostek's sign and Trousseau's sign. This is correct because Chvostek's sign and Trousseau's sign are clinical tests for neuromuscular irritability, which can occur in hypomagnesemia. Chvostek's sign is elicited by tapping the facial nerve in front of the ear and observing for facial twitching. Trousseau's sign is elicited by inflating a blood pressure cuff above the systolic pressure for 3 minutes and observing for carpal spasm.
A nurse is reviewing laboratory results for a client who has hypokalemia. Which of the following findings should the nurse expect?
Explanation
Choice A: Decreased serum pH. This is incorrect because hypokalemia usually causes increased serum pH, not decreased. This is because low potassium levels can lead to metabolic alkalosis, a condition where the blood is too alkaline due to loss of acid from the body. This can happen in cases of vomiting, diuretic use, or mineralocorticoid excess.
Choice B:
Increased serum calcium. This is incorrect because hypokalemia does not directly affect serum calcium levels. However, hypokalemia can cause hypomagnesemia, or low magnesium levels, which can in turn cause hypercalcemia, or high calcium levels. This is because magnesium is needed for the secretion of parathyroid hormone (PTH), which regulates calcium balance in the body. Low magnesium levels can lead to increased PTH secretion and increased calcium reabsorption from the bones and kidneys.
Choice C:
Decreased serum magnesium. This is correct because hypokalemia and hypomagnesemia often occur together, especially in cases of chronic diarrhea, malabsorption, alcoholism, or diuretic use. This is because potassium and magnesium are both lost in the urine or stool when these conditions are present. Hypomagnesemia can also cause hypokalemia by impairing the reabsorption of potassium in the kidneys and increasing the entry of potassium into the cells.
Choice D:
Increased serum bicarbonate. This is incorrect because hypokalemia usually causes decreased serum bicarbonate, not increased. This is because low potassium levels can lead to metabolic acidosis, a condition where the blood is too acidic due to accumulation of acid in the body. This can happen in cases of diabetic ketoacidosis, renal tubular acidosis, or chronic kidney disease.
A nurse is caring for a client who has metabolic acidosis due to diabetic ketoacidosis (DKA) Which of the following manifestations should the nurse monitor?
Explanation
Choice A reason:
Kussmaul respirations are a type of deep, rapid breathing that occurs in response to metabolic acidosis. The body tries to compensate for the excess acid by blowing off carbon dioxide through the lungs. Kussmaul respirations are a common manifestation of diabetic ketoacidosis (DKA), which is a severe form of metabolic acidosis caused by the accumulation of ketones in the blood. The nurse should monitor the client's respiratory rate, depth, and pattern, as well as the arterial blood gas results, to assess the severity of metabolic acidosis and the effectiveness of treatment.
Choice B reason:
Bradypnea is a condition of abnormally slow breathing, usually less than 12 breaths per minute. Bradypnea can result from respiratory acidosis, which is a condition of excess carbon dioxide in the blood due to hypoventilation or impaired gas exchange. Bradypnea is not a manifestation of metabolic acidosis, which is a condition of excess acid in the blood due to increased production or decreased elimination of hydrogen ions. Therefore, choice B is incorrect.
Choice C reason:
Muscle spasms are involuntary contractions of the skeletal muscles that can cause pain and discomfort. Muscle spasms can result from hypocalcemia, which is a condition of low calcium levels in the blood. Hypocalcemia can occur in metabolic acidosis due to the binding of calcium with excess hydrogen ions, reducing the availability of free calcium for muscle contraction. However, muscle spasms are not a specific or common manifestation of metabolic acidosis, and they can have other causes such as dehydration, electrolyte imbalance, or muscle injury. Therefore, choice C is incorrect.
Choice D reason:
Numbness and tingling of extremities are sensations of reduced or abnormal feeling in the arms or legs. Numbness and tingling can result from hypokalemia, which is a condition of low potassium levels in the blood. Hypokalemia can occur in metabolic acidosis due to the movement of potassium from the intracellular to the extracellular space in exchange for hydrogen ions, which are then excreted by the kidneys. However, numbness and tingling are not specific or common manifestations of metabolic acidosis, and they can have other causes such as nerve compression, peripheral neuropathy, or hyperventilation. Therefore, choice D is incorrect.
A nurse is assessing a client who has fluid overload. Which of the following findings should the nurse report to the provider? (Select all that apply.)
Explanation
Choice A reason:
Jugular vein distension is a sign of fluid overload because it indicates increased pressure in the right atrium and superior vena cava due to excess blood volume.
Choice B reason:
Weight gain of 2 kg in one day is a sign of fluid overload because it reflects fluid retention in the body. A weight gain of 1 kg (2.2 lb) is equivalent to 1 L of fluid.
Choice C reason:
Decreased hematocrit is a sign of fluid overload because it indicates hemodilution or dilution of the blood due to excess fluid in the intravascular space.
Choice D reason:
Bounding pulse is a sign of fluid overload because it reflects increased cardiac output and stroke volume due to excess blood volume.
Choice E reason:
Flat neck veins are not a sign of fluid overload, but rather a sign of fluid deficit or dehydration. In fluid overload, neck veins will be distended or elevated.
The nurse is caring for a patient with severe burns who is receiving IV fluid resuscitation with lactated Ringer's solution. The nurse understands that this type of solution is used for this patient because it:
No explanation
The nurse is preparing to hang a bag of 0.9% sodium chloride (normal saline) for a patient who has hyponatremia. The nurse knows that this type of solution is:
Explanation
Choice A reason: This is incorrect because 0.9% sodium chloride (normal saline) is an isotonic solution, not a hypotonic one. Isotonic solutions have the same concentration of solutes as blood plasma and do not cause fluid movement across the cell membrane.
Choice B reason:
This is incorrect because 0.9% sodium chloride (normal saline) is an isotonic solution, not a hypertonic one. Hypertonic solutions have a higher concentration of solutes than blood plasma and cause fluid to move out of the cells and into the vascular space.
Choice C reason:
This is correct because 0.9% sodium chloride (normal saline) is an isotonic solution that will expand the vascular space by adding fluid without changing the concentration of solutes. This is useful for patients with hyponatremia (low sodium level in the blood) who need to restore their fluid and electrolyte balance.
Choice D reason:
This is incorrect because 0.9% sodium chloride (normal saline) is an isotonic solution that will expand the vascular space by adding fluid without changing the concentration of solutes. It will not have no effect on fluid movement, as it will increase the intravascular volume.
A nurse is administering dextrose 10% in water (D10W) to a patient who needs some nutrition with glucose. Which of the following assessments should the nurse perform? (Select all that apply.)
Explanation
Choice A reason:
The nurse should monitor blood glucose levels because dextrose 10% in water (D10W) is a hypertonic solution that contains glucose and can raise the blood sugar level of the patient. The nurse should check the blood glucose level before and after administering D10W to prevent hyperglycemia or hypoglycemia.
Choice B reason:
The nurse should check for signs of phlebitis at the IV site because D10W is acidic and can cause venous irritation. Phlebitis is inflammation of the vein that can result from chemical, mechanical or bacterial causes. Signs of phlebitis include pain, redness, swelling, warmth and tenderness at the IV site.
Choice C reason:
The nurse should assess for fluid overload because D10W is quickly metabolized, leaving behind water that can move into the interstitial space. Fluid overload can cause edema, dyspnea, crackles, distended neck veins, increased blood pressure and decreased urine output. The nurse should monitor the intake and output, vital signs, weight and breath sounds of the patient.
Choice D reason:
The nurse does not need to evaluate serum sodium levels because D10W does not contain sodium or affect the sodium balance of the patient. D10W is used to provide some nutrition with glucose, not to correct electrolyte imbalances.
Choice E reason:
The nurse does not need to observe for signs of hypoglycemia because D10W is unlikely to cause hypoglycemia unless there is a sudden interruption or discontinuation of the infusion. Hypoglycemia is a low blood sugar level that can cause shakiness, diaphoresis, confusion, weakness, hunger and headache. The nurse should monitor the blood glucose level and administer D10W at a steady rate to prevent hypoglycemia.
The nurse is caring for a patient with an IV infusion in his left arm that was started 2 hours ago in the emergency department (ED) The patient complains of pain at the IV site and rates it as an 8 on a scale of 0 to 10. The nurse assesses the site and notes edema, erythema, and coolness to touch around the insertion site. What is the most appropriate action by the nurse?
Explanation
Choice A reason:
Applying warm compresses to the site and elevating the arm may help to reduce pain and swelling, but they do not address the underlying cause of the problem, which is likely infiltration or phlebitis of the IV site. Infiltration occurs when the IV fluid leaks into the surrounding tissue, causing edema, coolness, and pallor. Phlebitis occurs when the vein becomes inflamed, causing pain, erythema, and warmth. Both conditions require immediate removal of the IV catheter and restarting a new IV in another site.
Choice B reason:
Slowing down the infusion rate and documenting the findings may be appropriate actions after removing the IV catheter and starting a new IV in another site, but they are not sufficient to resolve the problem. Slowing down the infusion rate may reduce the discomfort and prevent further complications, but it does not stop the leakage or inflammation of the IV site. Documenting the findings is important for legal and quality improvement purposes, but it does not provide any intervention for the patient's pain or risk of infection.
Choice C reason:
Stopping the infusion, removing the IV catheter, and starting a new IV in another site is the most appropriate action by the nurse. This action prevents further damage to the tissue or vein, reduces the risk of infection, and restores adequate IV access for fluid and medication administration. The nurse should also apply a sterile dressing to the affected site, monitor for signs of infection or complications, and notify the physician if needed. This is the correct answer.
Choice D reason:
Notifying the physician and obtaining an order for an antihistamine is not an appropriate action by the nurse. This action implies that the patient is having an allergic reaction to the IV fluid or medication, which is not supported by the assessment findings. An antihistamine may help to reduce itching or swelling, but it does not address the cause of the pain or prevent further tissue or vein damage. The nurse should notify the physician after removing the IV catheter and starting a new IV in another site, and only if there are signs of infection or complications that require medical intervention.
The nurse is preparing to insert a central venous catheter into a patient's right internal jugular vein using ultrasound guidance. What is an important step that the nurse should perform before inserting the catheter?
Explanation
Choice A reason: Shaving the hair around the insertion site is not recommended because it can cause skin irritation and increase the risk of infection.
Choice B reason:
Obtaining informed consent from the patient is important, but it is not a step that the nurse should perform before inserting the catheter. Informed consent should be obtained by the physician or advanced practice nurse who will perform the procedure.
Choice C reason:
Administering prophylactic antibiotics to the patient is not a routine practice for central venous catheter insertion. Antibiotics may be indicated for patients with certain risk factors, such as immunosuppression, but they should be prescribed by the physician or advanced practice nurse.
Choice D reason:
Placing the patient in Trendelenburg position is an important step that the nurse should perform before inserting the catheter. This position helps to distend the jugular vein and reduce the risk of air embolism during catheter insertion.
The nurse is monitoring a patient who has a central venous catheter in place for signs of complications. Which of the following are potential complications of central venous catheters? (Select all that apply.)
Explanation
Choice A reason: Pneumothorax: This is a condition where air accumulates in the pleural space, causing the lung to collapse. It can occur during insertion of a central venous catheter if the needle or catheter punctures the lung or the pleura.
Choice B reason:. Air embolism. This is a condition where air bubbles enter the bloodstream and obstruct blood flow. It can occur during insertion, removal or maintenance of a central venous catheter if air enters the catheter or the vein.
Choice C reason:. Catheter-related bloodstream infection. This is an infection that occurs when microorganisms colonize the catheter or the insertion site and enter the bloodstream. It can cause fever, chills, sepsis and other serious complications. It can be prevented by using strict aseptic technique and following infection control guidelines.
Choice D reason:. Catheter occlusion. This is a condition where the catheter lumen becomes blocked by blood clots, fibrin sheaths, precipitates or kinks. It can impair the infusion or withdrawal of fluids and medications. It can be prevented by flushing the catheter regularly with saline or heparin solutions.
Choice E reason: Hematoma formation. This is a condition where blood accumulates under the skin or in the tissues around the insertion site. It can occur due to bleeding from the punctured vein or artery, or from trauma to the site. It can cause pain, swelling, bruising and infection.
Exams on Fluid and Electrolytes
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
- Objectives
- Introduction (Homeostasis)
- Fluids and Electrolytes
- Distribution of Body Fluids
- Electrolytes
- Fluid Pressures/Movements (Starling's Law)
- Routes of Transport of Body Fluid
- Regulating Body Fluids
- Regulation of Electrolytes
- Factors Affecting Body Fluid, Electrolyte Fluid Imbalances
- Causes of Electrolyte Imbalances
- Nursing Assessment of Fluid and Electrolyte Imbalances
- NANDA Nursing Diagnoses
- Promoting Fluid and Electrolyte Balance
- Techniques of Peripheral and Central Vascular Access
- Common Complications of Intravenous Fluid Infusion
- More questions on this topic
Notes Highlighting is available once you sign in. Login Here.
Objectives
Objectives
-
Discuss the function, distribution, movement, and regulation of fluids and electrolytes in the body.
-
Describe the regulation of acid-base balance in the body, including the role of the lungs, kidneys.
-
Identify factors affecting normal body fluid& electrolyte.
-
Discuss the risk factors for and the causes and effects of fluid & electrolyte
-
Collect assessment data related to the client's fluid, electrolyte, and acid-base balance.
-
Identify examples of nursing diagnoses, outcomes, and interventions for clients with altered fluid, and electrolyte balance.
-
Teach clients measures to maintain fluid and electrolyte.
-
Implement measures to correct imbalances of fluids and electrolytes.
-
Evaluate the effect of nursing interventions on the client's fluid, electrolyte.
-
Verbalize the steps used in:
-
Starting an intravenous infusion
-
Monitoring an intravenous infusion
-
Changing an intravenous container, tubing, and dressing
-
- Decreased bone density results in osteoporosis
- Decreased muscle mass results in sarcopenia
- Decreased joint mobility results in stiffness and pain
- Decreased height due to vertebral compression fractures
Neurological System
- Decreased brain weight and volume results in decreased number of neurons
- Decreased neurotransmitter production results in decreased nerve conduction velocity
- Decreased cerebral blood flow results in decreased oxygen delivery to brain cells
- Decreased sensory perception results in impaired vision, hearing, smell, touch and pain sensation
- Decreased cognitive function results in slowed reaction time, memory loss and decreased learning ability
Sensory System
- Decreased visual acuity results in presbyopia, cataracts, glaucoma and macular degeneration
- Decreased hearing acuity results in presbycusis, tinnitus and hearing loss
- Decreased olfactory acuity results in anosmia and decreased smell sensation
- Decreased gustatory acuity results in ageusia and decreased taste sensation
- Decreased tactile acuity results in decreased touch and pain sensation
Introduction (Homeostasis)
-
Body works best when some conditions are kept within normal. e.g. body temperature, blood electrolytes values as (sodium, potassium & calcium), blood pH, & blood volume.
-
To keep the condition as close to normal as possible is called Homeostasis:
-
Homeostasis means keeping everything normal
-
Diseases and daily factors can create imbalances such as:
-
Excessive temperatures
-
Vigorous activity
-
Use of diuretics.
-
-
Fluids and Electrolytes Necessary for organs to perform work
Water
-
50% to 60% of healthy adult weight
-
An infant has considerably more body fluid and ECF than an adult.
-
Age, Sex, and amount of fat cells affect body water.
-
Women and obese people have less body water
Total Body Fluids in Human Body
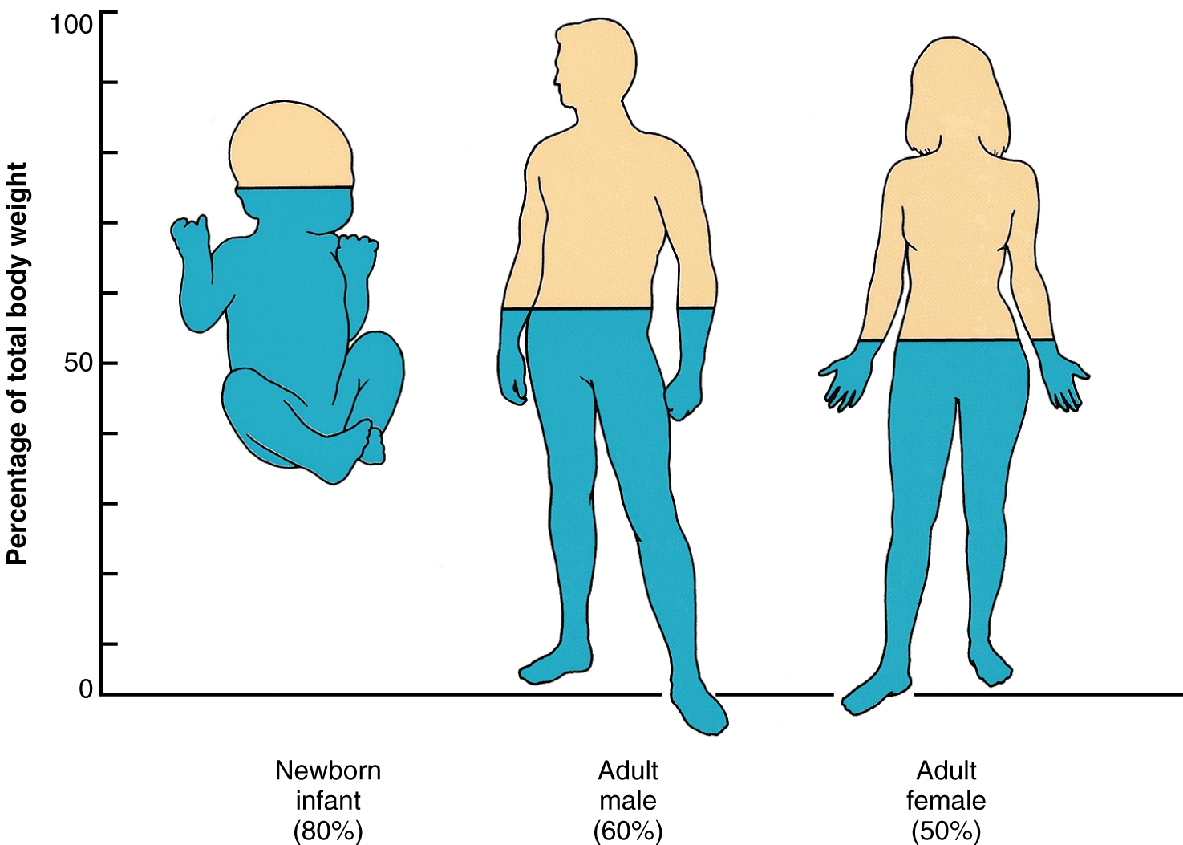
Functions of body water:
-
Transport nutrients, electrolytes, and O2 to the cells
-
Excretion of wastes
-
Regulates body temperature
-
Lubricates joints and membranes
-
Medium for food digestion
Fluids and Electrolytes
Fluids and Electrolytes
Necessary for organs to perform work
Water
-
50% to 60% of healthy adult weight
-
An infant has considerably more body fluid and ECF than an adult.
-
Age, Sex, and amount of fat cells affect body water.
-
Women and obese people have less body water
Total Body Fluids in Human Body
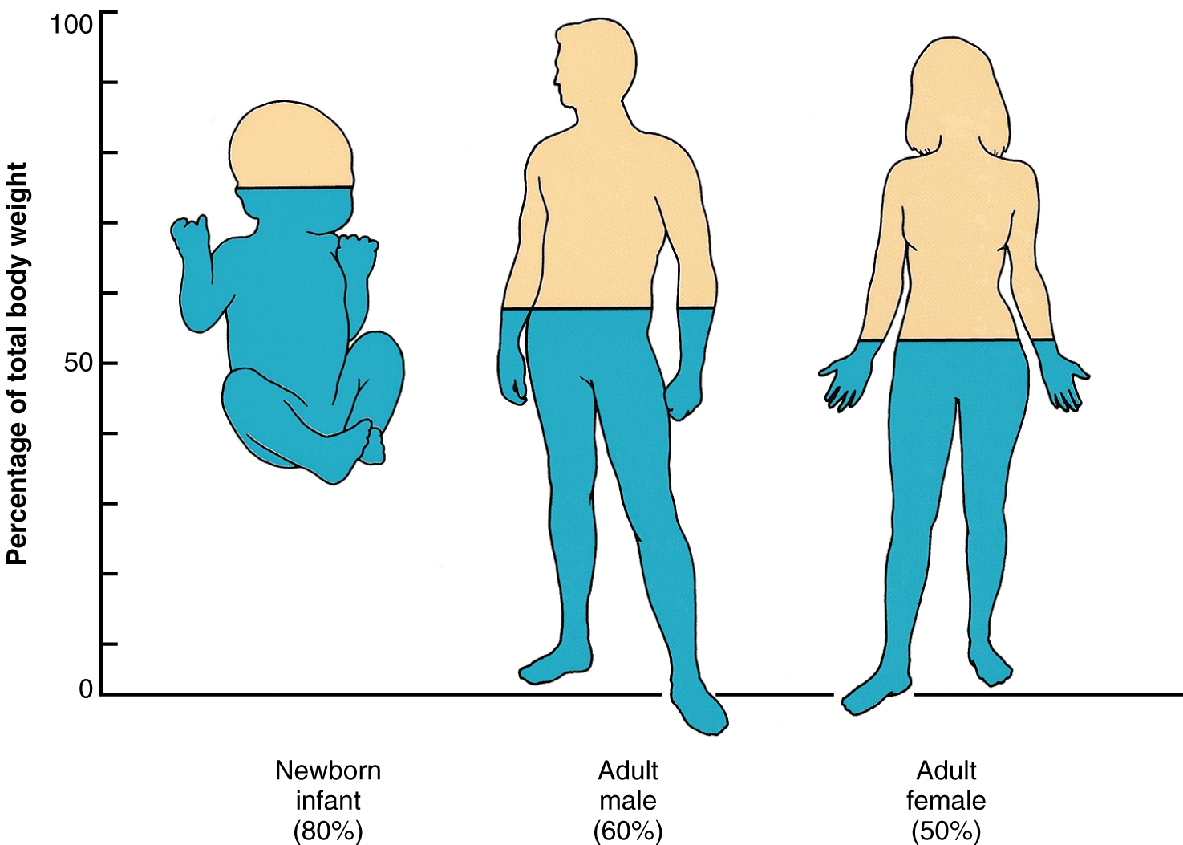
Functions of body water:
-
Transport nutrients, electrolytes, and O2 to the cells
-
Excretion of wastes
-
Regulates body temperature
-
Lubricates joints and membranes
-
Medium for food digestion
Distribution of Body Fluids
Body fluid is made up of water and certain dissolved substances called electrolytes.
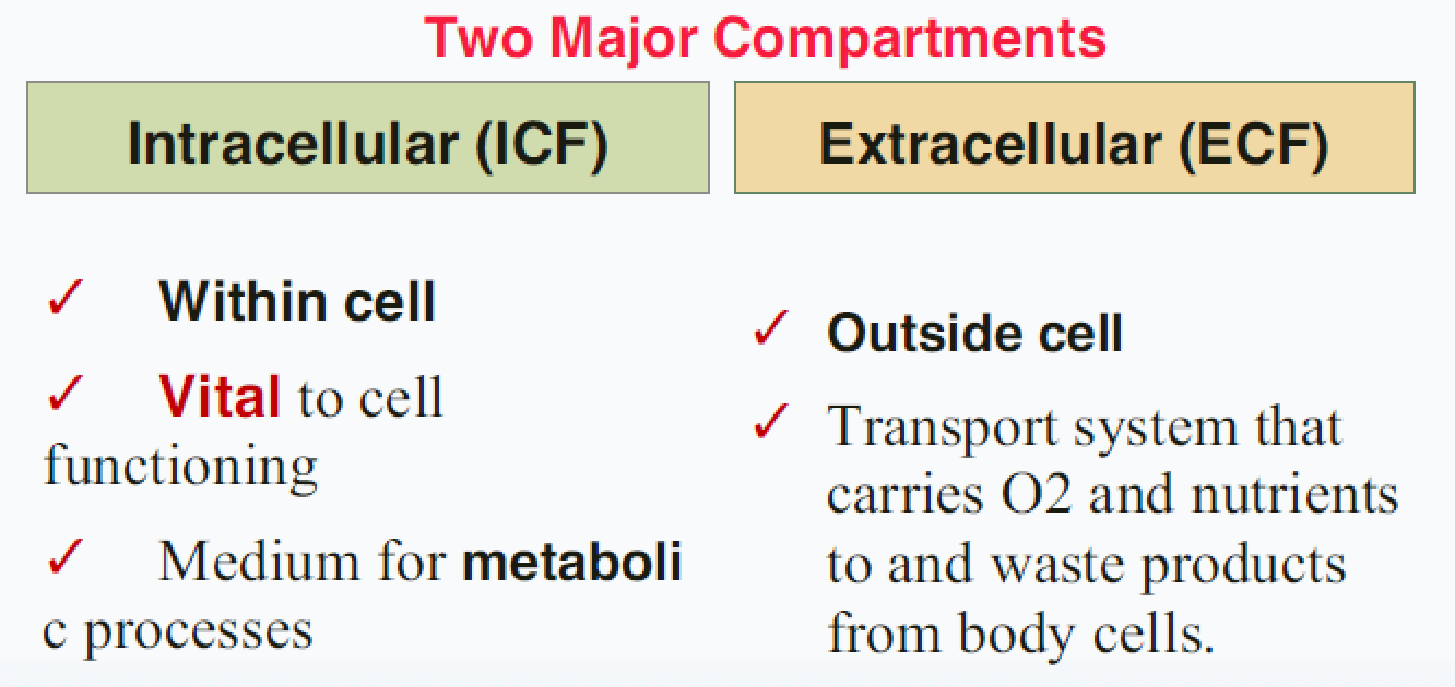
ECF two main compartments:
-
Intravascular fluids (Plasma 20%) found within the vascular system.
-
Interstitial (75%) found surrounding the cells.
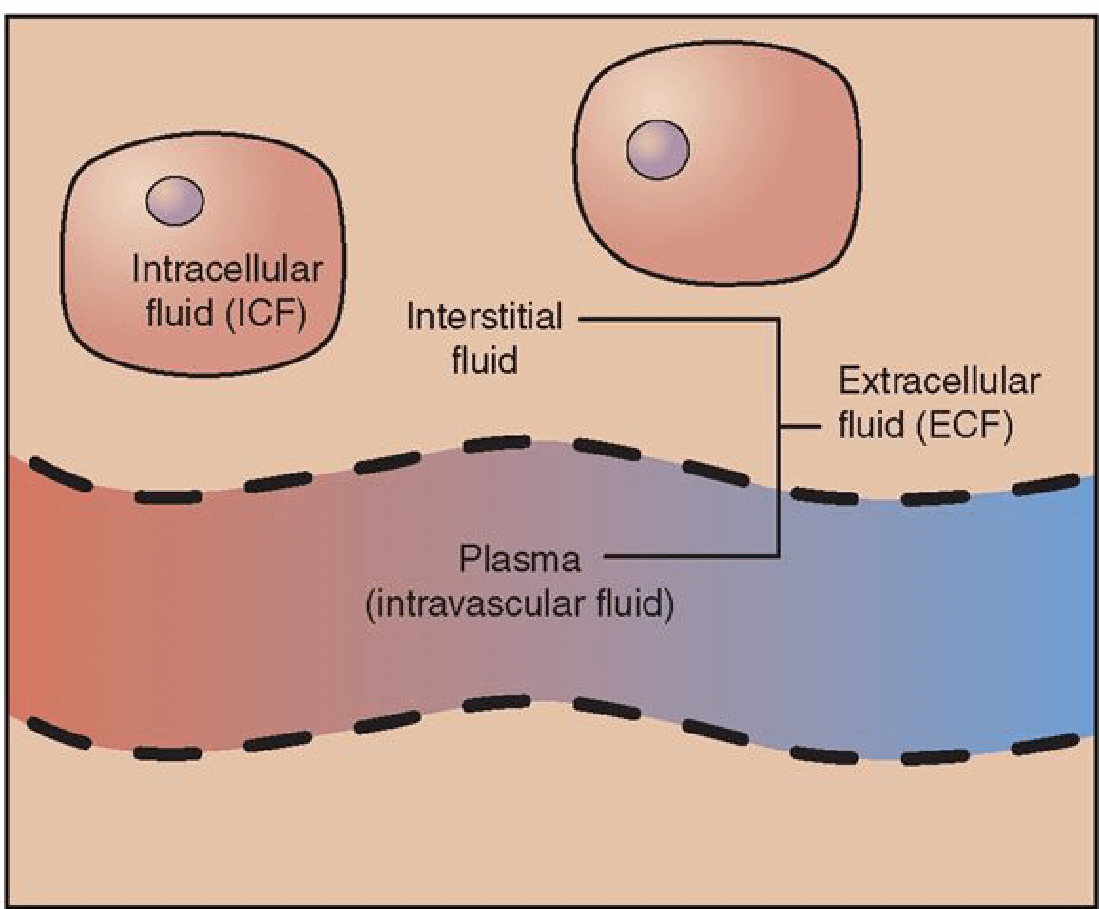
Electrolytes
Positively charged: ions are called cations and include:
-
Sodium (Na +) a major electrolyte in ECF
-
Potassium (K+) a major electrolyte in ICF
-
Calcium (Ca ++)
-
Magnesium (Mg ++)
Negatively charged: ions are called anions and include:
-
Chloride (Cl) a major electrolyte in ECF
-
Phosphate (HPO4) a major electrolyte in ICF
-
Bicarbonate (HCO3)
-
Sulfate (SO4)
Functions of Electrolytes
|
Promote |
Promote neuromuscular reaction |
|
Maintain |
Maintain body fluid volume and osmolarity |
|
Distribute |
Distribute body water between fluid compartments (balance) |
|
Regulate |
Regulate acid-base balance |
Fluid Pressures/Movements (Starling's Law)
-
ECF and ICF fluid shifts occur related to changes in pressure within the compartments
-
Fluid flows only when there is a difference in pressure
Osmolality:
-
Concentration of a solution determined by the number of dissolved particles per kilogram of water. Controls water movement and distribution in body fluid compartments (275-295mmol/L)
Movement of Body Fluids and Electrolytes Solutes (substances dissolved in a liquid)
Crystalloids (salts that dissolve readily into true solutions)
Colloids (substances such as large protein molecules that do not readily dissolve into true solutions)
Solvent (is the component of a solution that can dissolve a solute)
Materials are transported between cellular and extracellular spaces through several routes including:
-
Diffusion
-
Osmosis
-
Filtration
-
Active transport
Routes of Transport of Body Fluid Diffusion:
-
Water move across a semi permeable membrane from an area of high solute concentration to one of lower solute concentration.
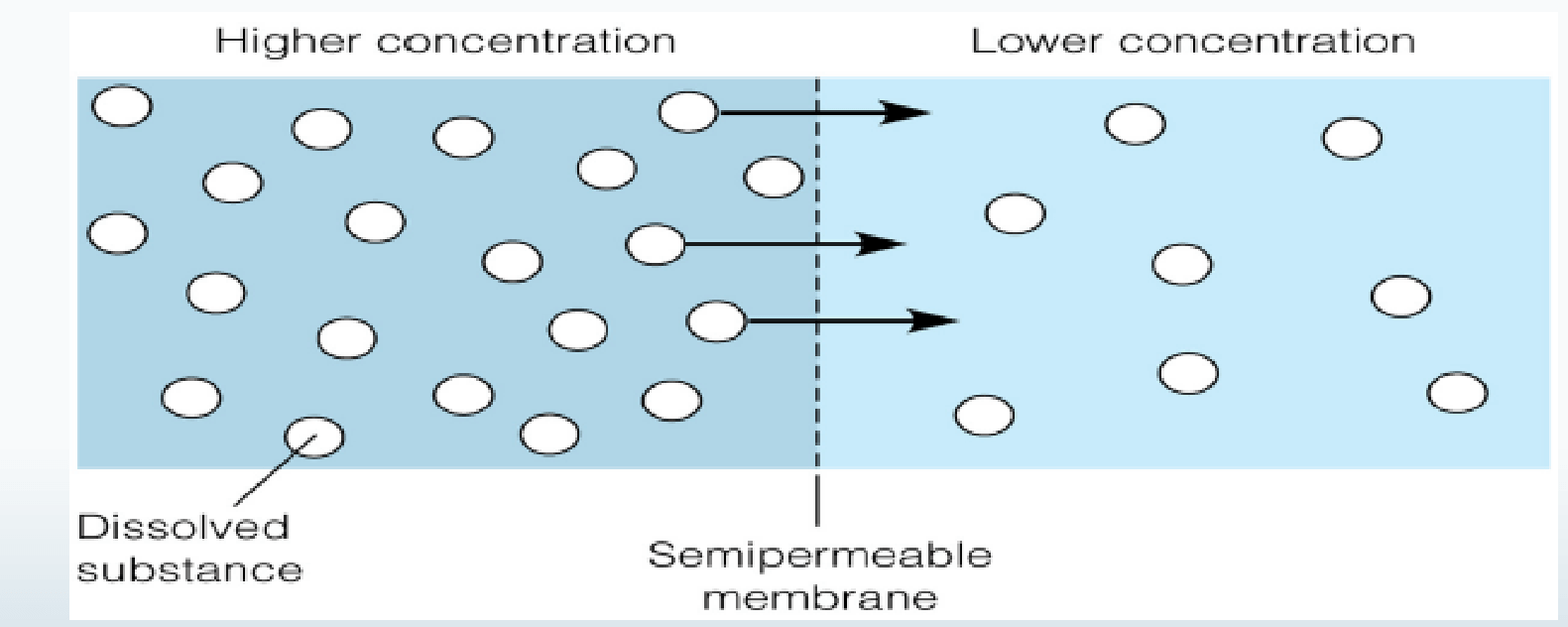
Osmosis:
-
Movement of water across a semi permeable membrane from a less concentrated solution to a more concentrated solution thereby.
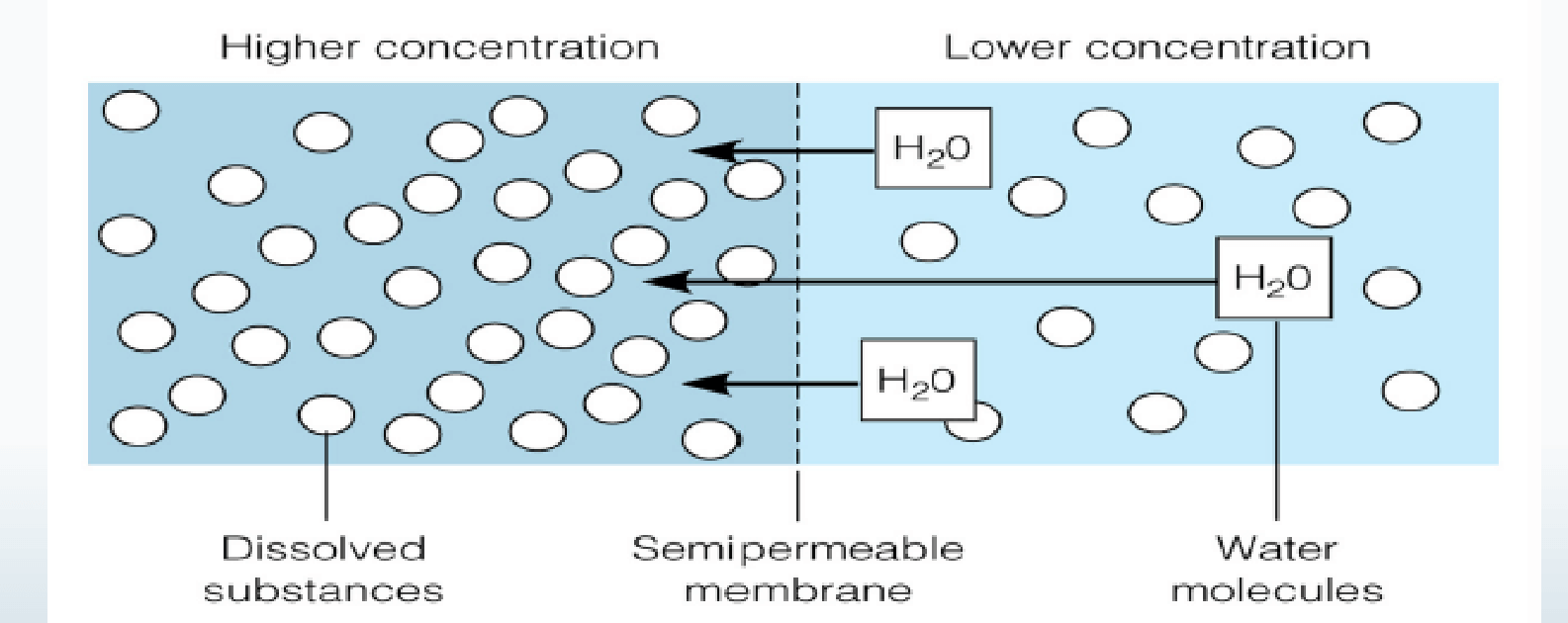
Filtration:
-
Fluids and solutes move together across a membrane from an area of higher pressure to an area of a lower pressure.
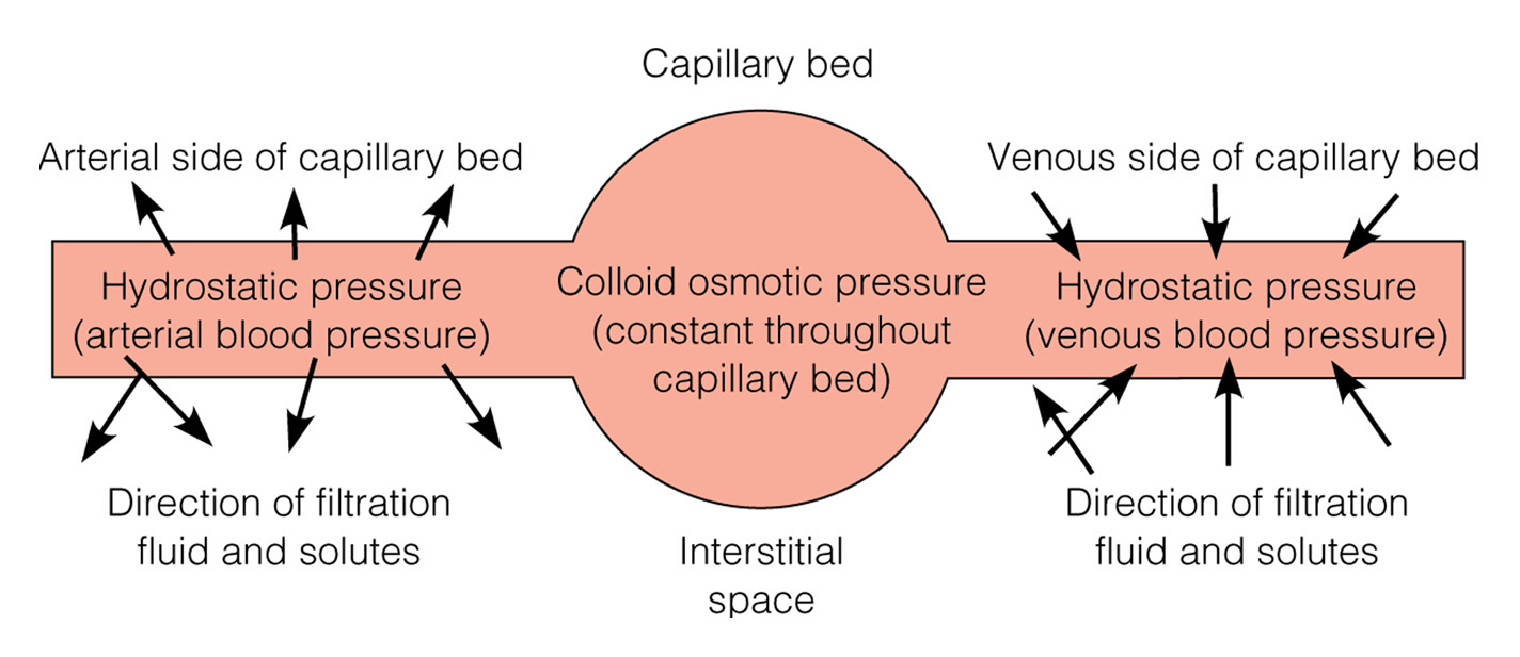
Active Transport:
-
Movement of solutes across cell membranes from a less concentrated solution to a more concentrated solution.
-
Importance in maintaining the differences in sodium and potassium ion concentration of ECF and ICF.
-
Na+ concentration are higher in ECF and K+ concentrations are higher in ICF .
-
To maintain these proportions, an active transport mechanism (Na+- K+ pump) is activated.
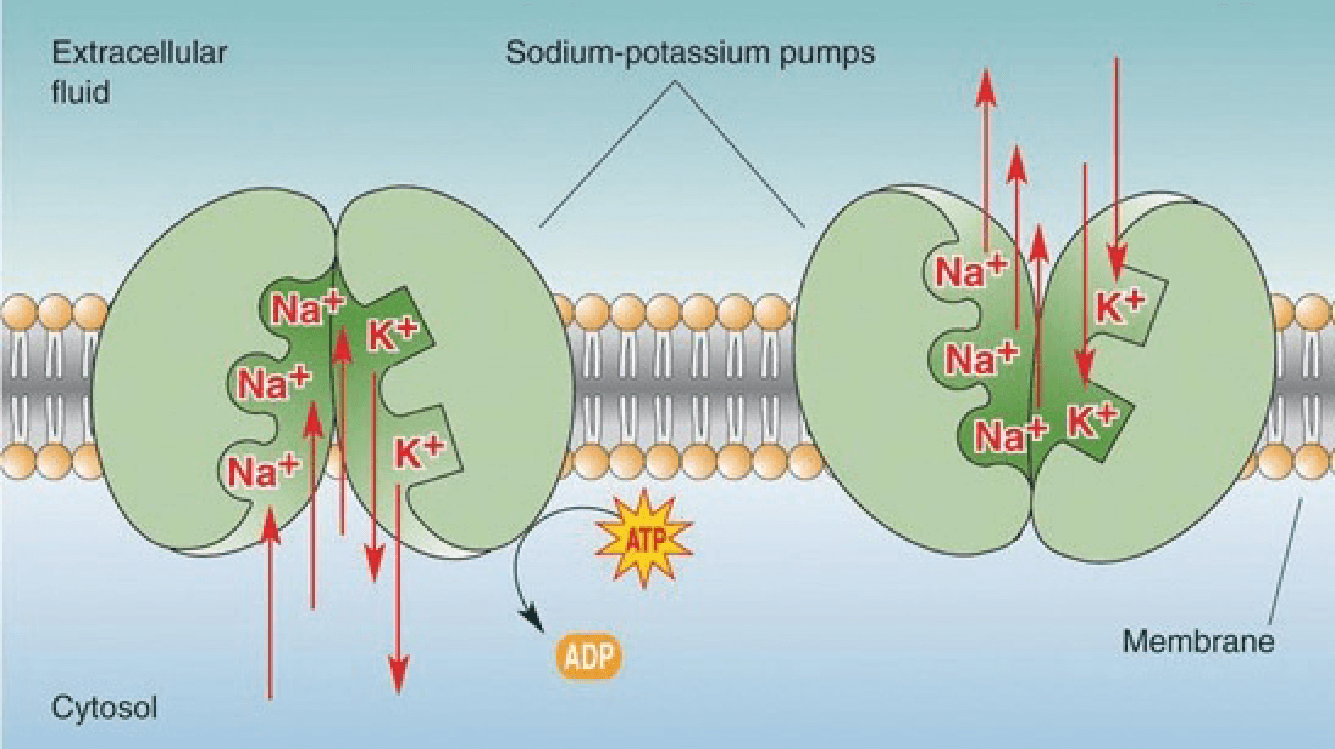
Diffusion vs Active Transport:
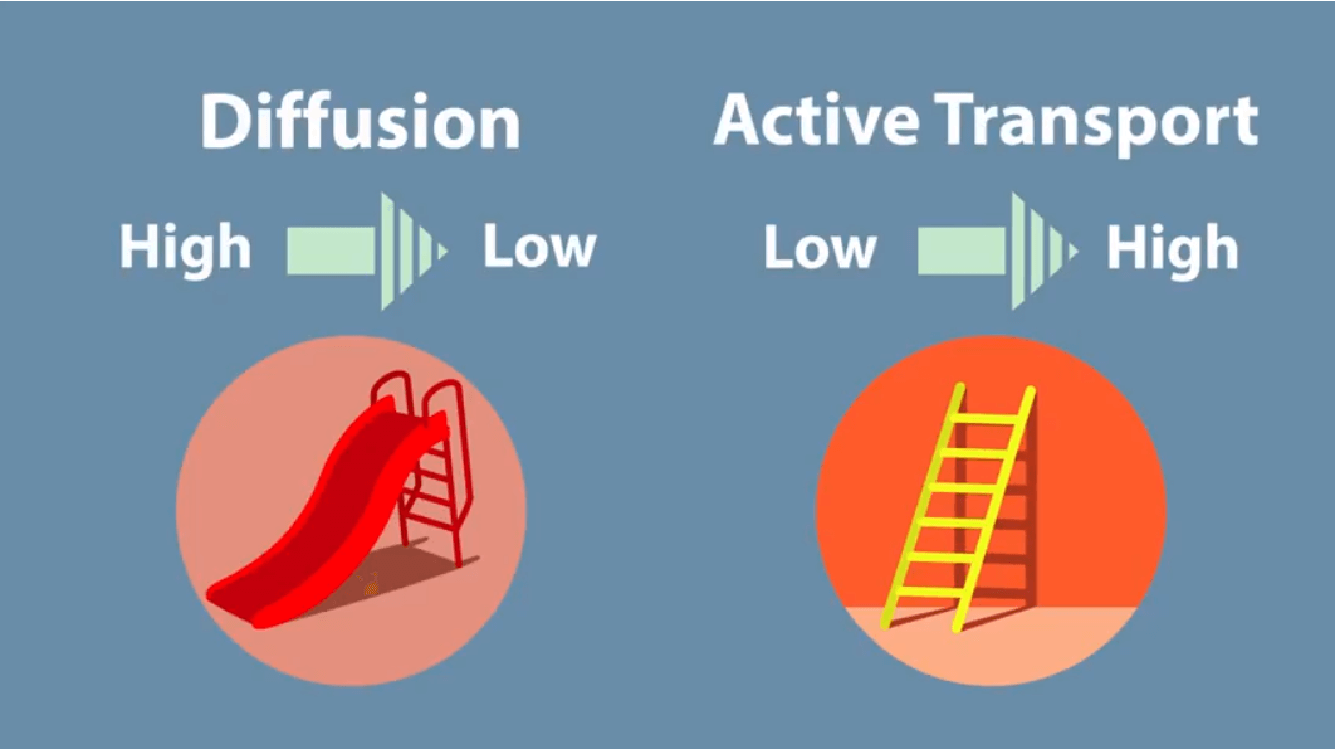
Routes of Transport of Body Fluid
Routes of Transport of Body Fluid
Diffusion:
-
Water move across a semi permeable membrane from an area of high solute concentration to one of lower solute concentration.
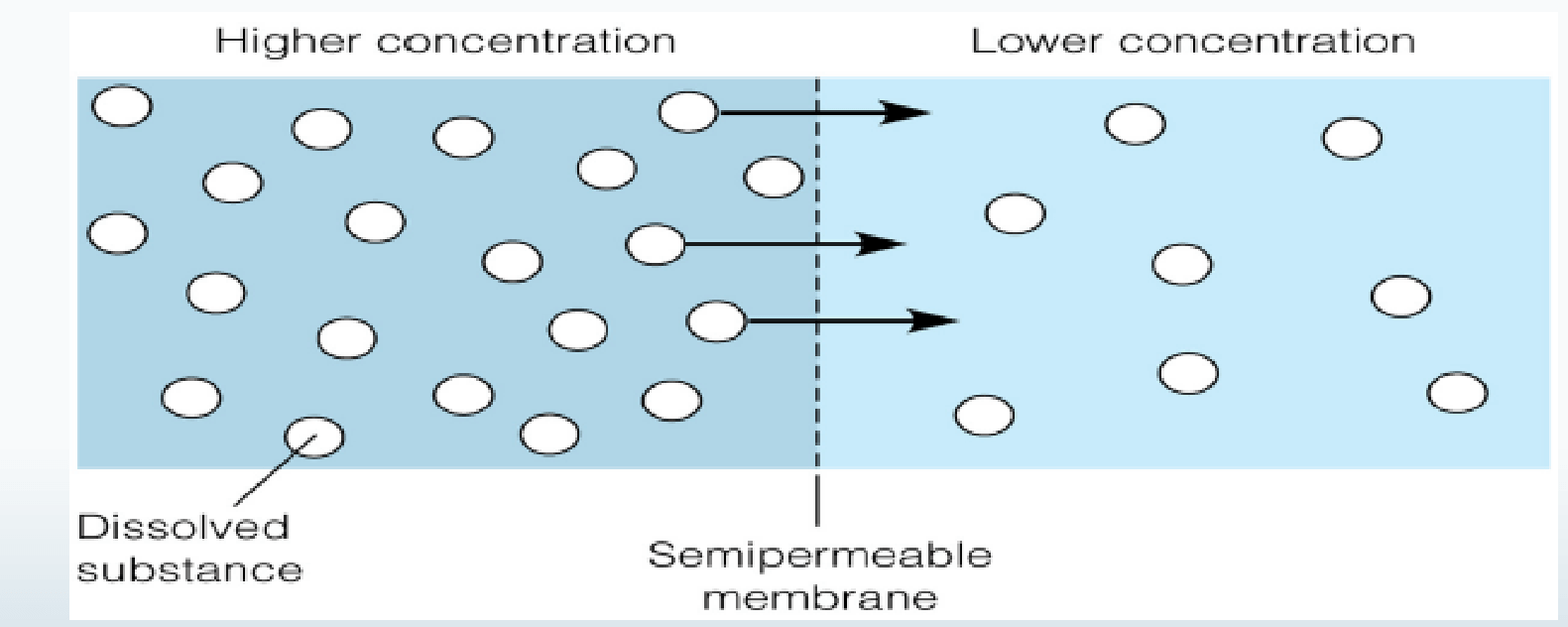
Osmosis:
-
Movement of water across a semi permeable membrane from a less concentrated solution to a more concentrated solution thereby.
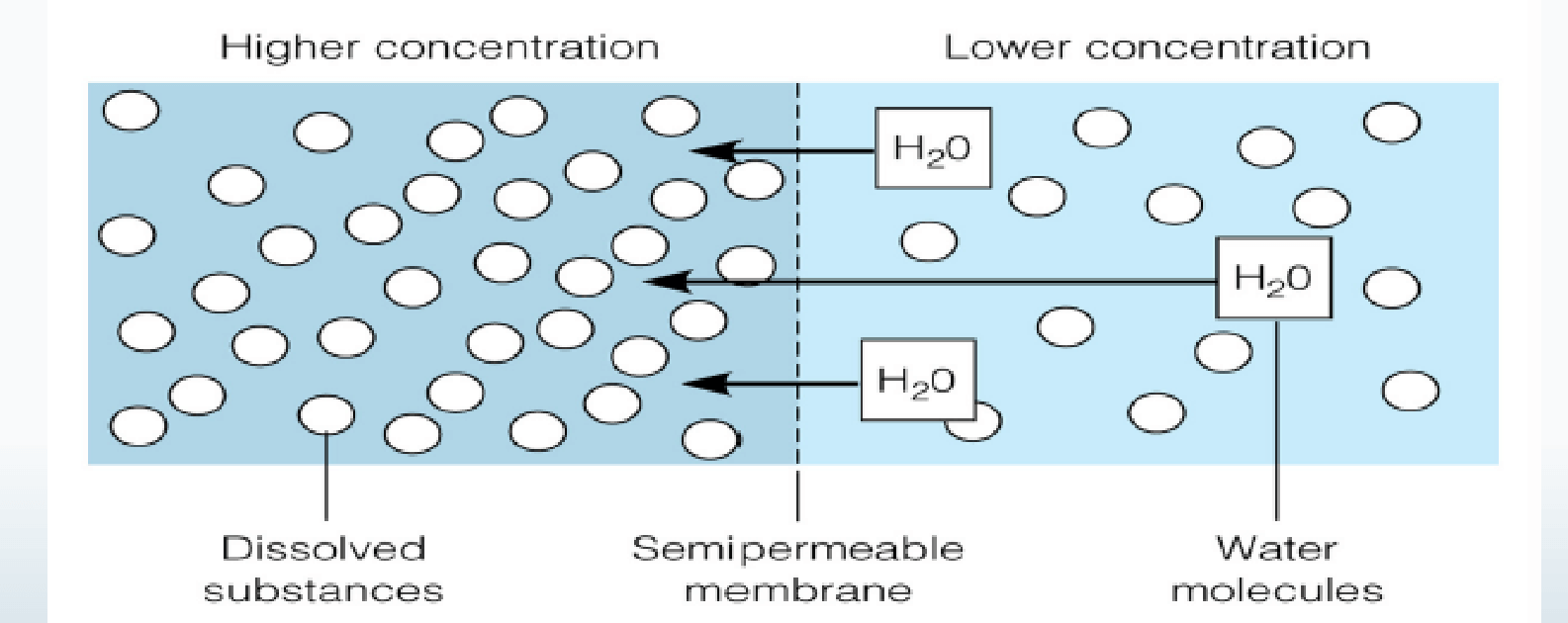
Filtration:
-
Fluids and solutes move together across a membrane from an area of higher pressure to an area of a lower pressure.
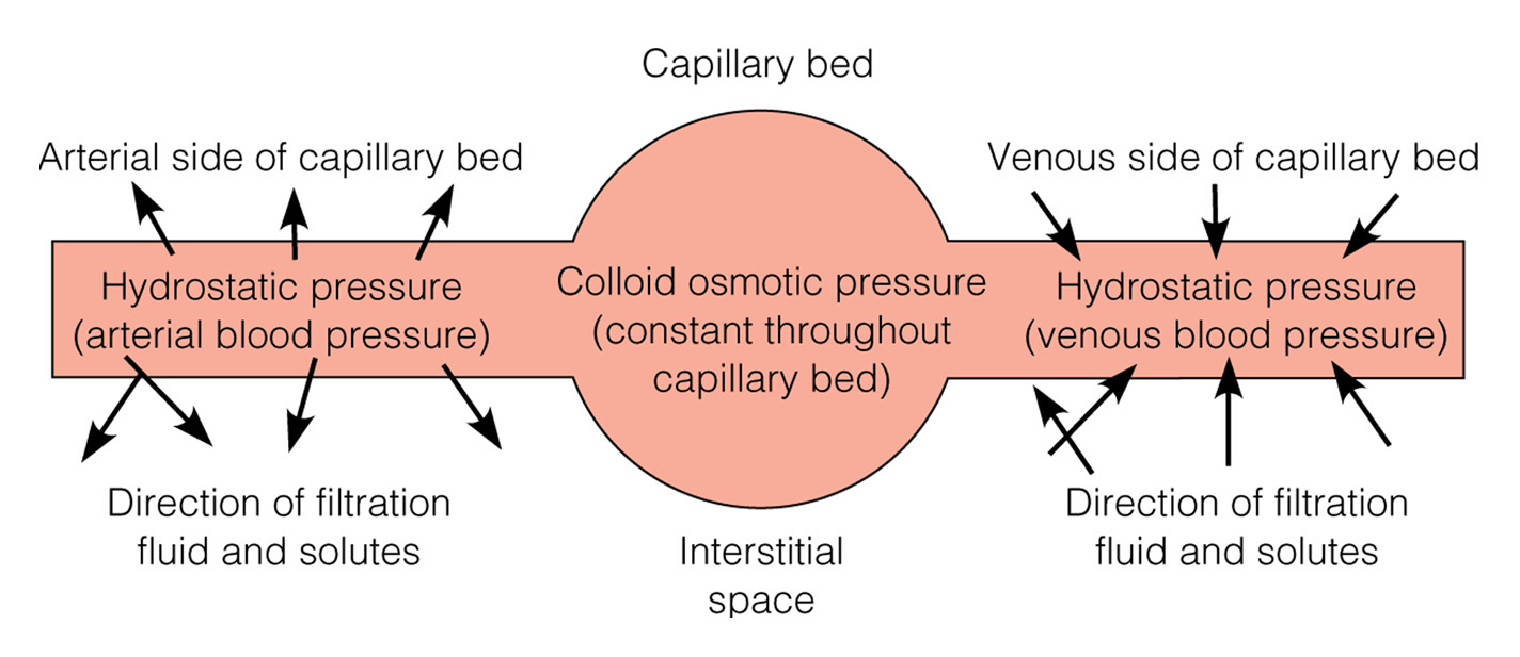
Active Transport:
-
Movement of solutes across cell membranes from a less concentrated solution to a more concentrated solution.
-
Importance in maintaining the differences in sodium and potassium ion concentration of ECF and ICF.
-
Na+ concentration are higher in ECF and K+ concentrations are higher in ICF .
-
To maintain these proportions, an active transport mechanism (Na+- K+ pump) is activated.
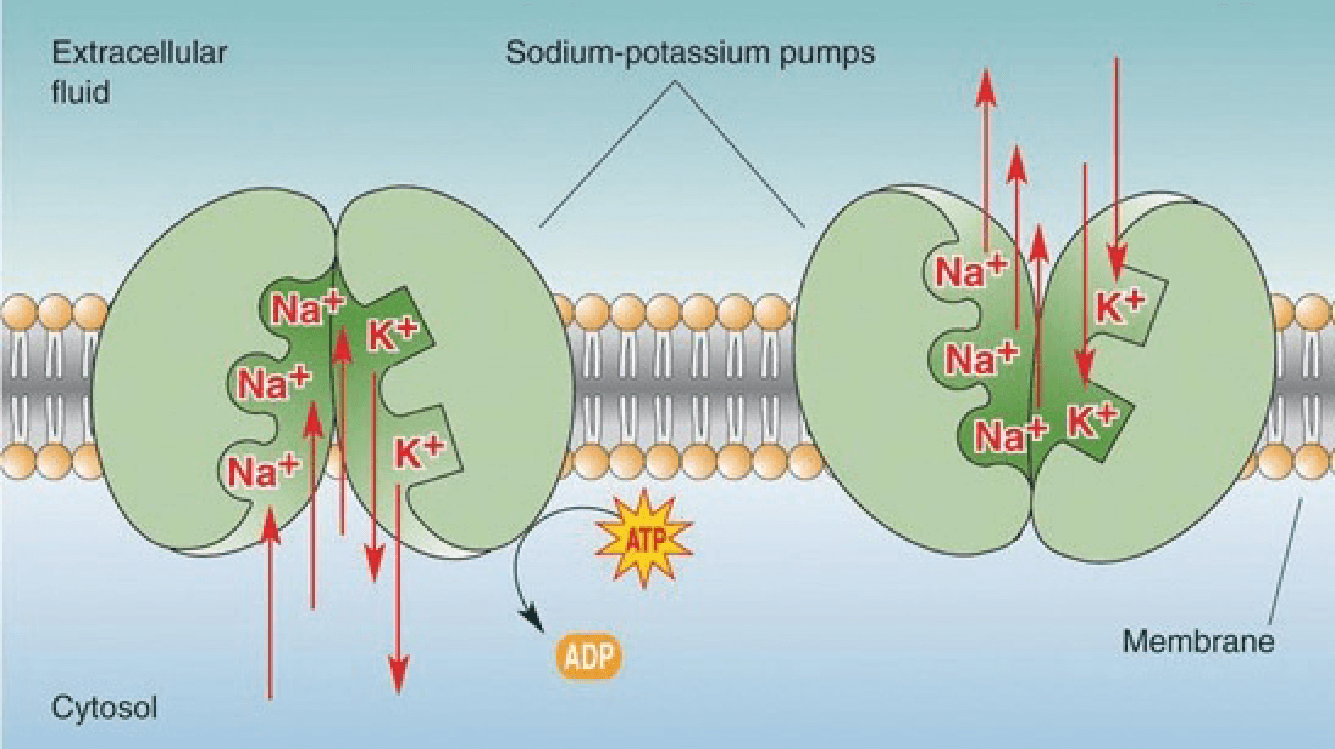
Diffusion vs Active Transport:
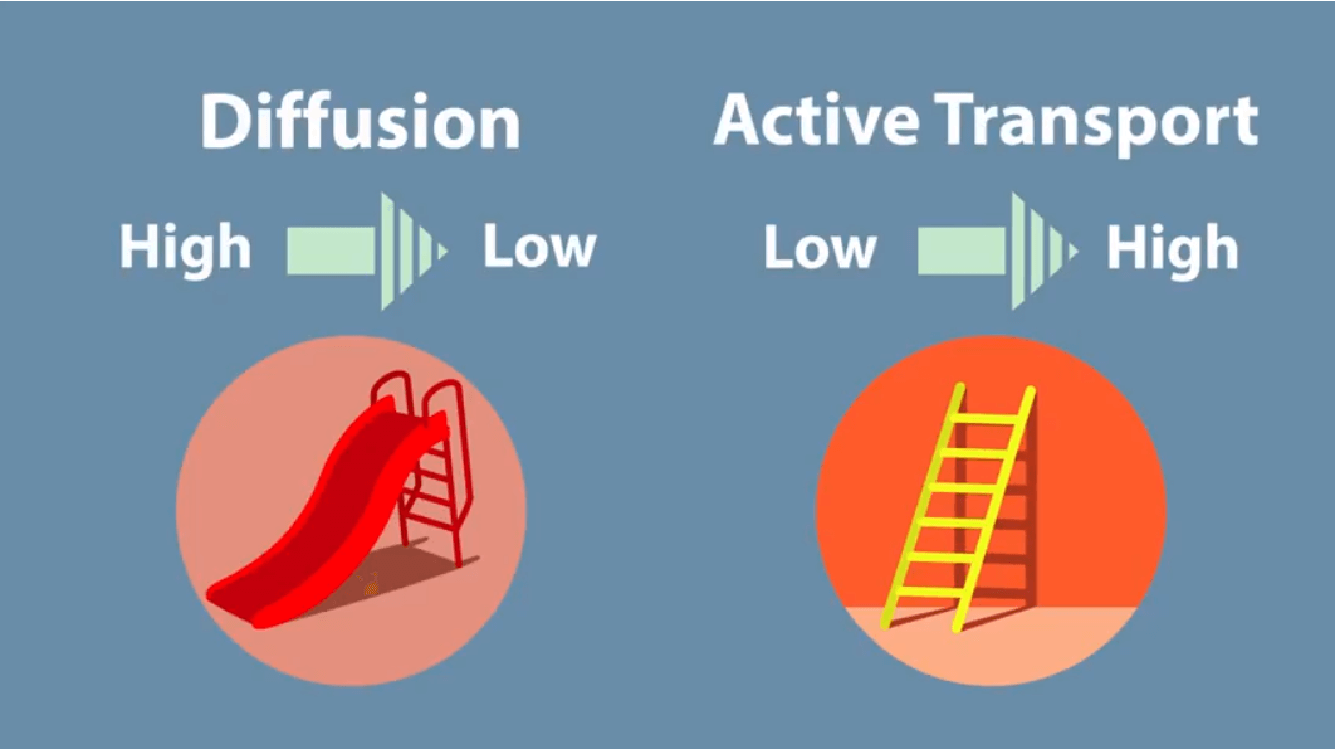
Regulating Body Fluids
Homeostasis is maintained through:
-
Fluid intake regulation
-
Thirst mechanism
-
Hormonal regulation
-
Antidiuretic hormone (ADH)
-
Renin-angiotensin-aldosterone system
-
Atrial natriuretic factor
-
Fluid output regulation
-
Kidneys (1200-1500 mL of urine produced daily)
-
Insensible loss skin (500 - 600 mL of fluid lost daily)
-
Lung (500 mL loss of water daily)
-
GI tract
Regulation of Electrolytes Major Cations in body fluids
-
Sodium (Na+)
-
Potassium (K+)
-
Calcium (Ca++)
-
Magnesium (Mg++)
Electrolyte - Normal Range
|
Electrolyte |
Normal Value |
Function |
|
Sodium |
135-145 mEq/L |
Regulates fluid volume and osmolarity; involved in nerve impulse transmission and muscle contraction |
|
Potassium |
3.5-5 mEq/L |
Maintains intracellular osmolarity; involved in nerve impulse transmission and muscle contraction; regulates acid-base balance |
|
Calcium |
8.5-10.5 mg/dL |
Forms bones and teeth; involved in nerve impulse transmission and muscle contraction; regulates blood clotting and enzyme activity |
|
Magnesium |
1.5-2.5 mEq/L |
Involved in nerve impulse transmission and muscle contraction; regulates enzyme activity and protein synthesis |
|
Phosphorus |
2.5-4.5 mg/dL |
Forms bones and teeth; involved in energy metabolism and acid-base balance |
|
Chloride |
95-105 mEq/L |
Maintains extracellular osmolarity; involved in acid-base balance and gastric acid production |
|
Bicarbonate |
23-30 mEq/L |
Maintains acid-base balance; acts as a buffer in the blood |
Regulation of Electrolytes
|
Electrolyte |
Regulation |
Function |
|
Sodium (Na+) |
- Renal reabsorption or excretion - Aldosterone increases Na+ reabsorption in collecting duct of nephrons |
- Regulating ECF volume and distribution - Maintaining blood volume - Transmitting nerve impulses and contracting muscles |
|
Potassium (K+) |
- Renal excretion - Aldosterone increases K+ excretion - Movement into and out of cells - Insulin helps move K+ into cells; tissue damage and acidosis shift K+ out of cells into ECF |
- Maintaining ICF osmolality - Transmitting nerve and other electrical impulses - Regulating cardiac impulse transmission and muscle contraction |
|
Calcium (Ca2+) |
- Redistribution between bones and ECF - Parathyroid hormone and calcitriol increase serum Ca2+ levels; calcitonin decreases serum levels |
- Skeletal and smooth muscle function - Regulating acid-base balance - Forming bones and teeth - Transmitting nerve impulses - Regulating muscle contractions - Maintaining cardiac pacemaker (automaticity) - Blood clotting |
|
Magnesium (Mg2+) |
- Conservation and excretion by kidneys - Intestinal absorption increased by vitamin D and parathyroid hormone |
- Intraocular metabolism - Operating sodium-potassium pump - Relaxing muscle contractions - Transmitting nerve impulses - Regulating cardiac function |
|
Chloride (Cl-) |
- Excreted and reabsorbed along with sodium in the kidneys - Aldosterone increases chloride reabsorption with sodium |
- Regulating ECF balance and vascular volume - Regulating acid-base balance |
|
Bicarbonate (HCO3-) |
- Excretion and reabsorption along with sodium in the kidneys - Regeneration by kidneys |
- Major body buffer involved in acid-base regulation - Buffer in oxygen-carbon dioxide exchange in RBCs |
|
Phosphate (PO4-) |
- Parathyroid hormone decreases serum levels by increasing renal excretion - Reciprocal relationship with calcium: increasing serum calcium decreases phosphate levels; decreasing serum calcium increases phosphate |
- Forming bones and teeth - Metabolizing carbohydrate, protein, and fat - Cellular metabolism; producing ATP and DNA - Muscle, nerve, and RBC function |
Body fluids are normally slightly alkaline, between: pH of 7.35 and 7.45
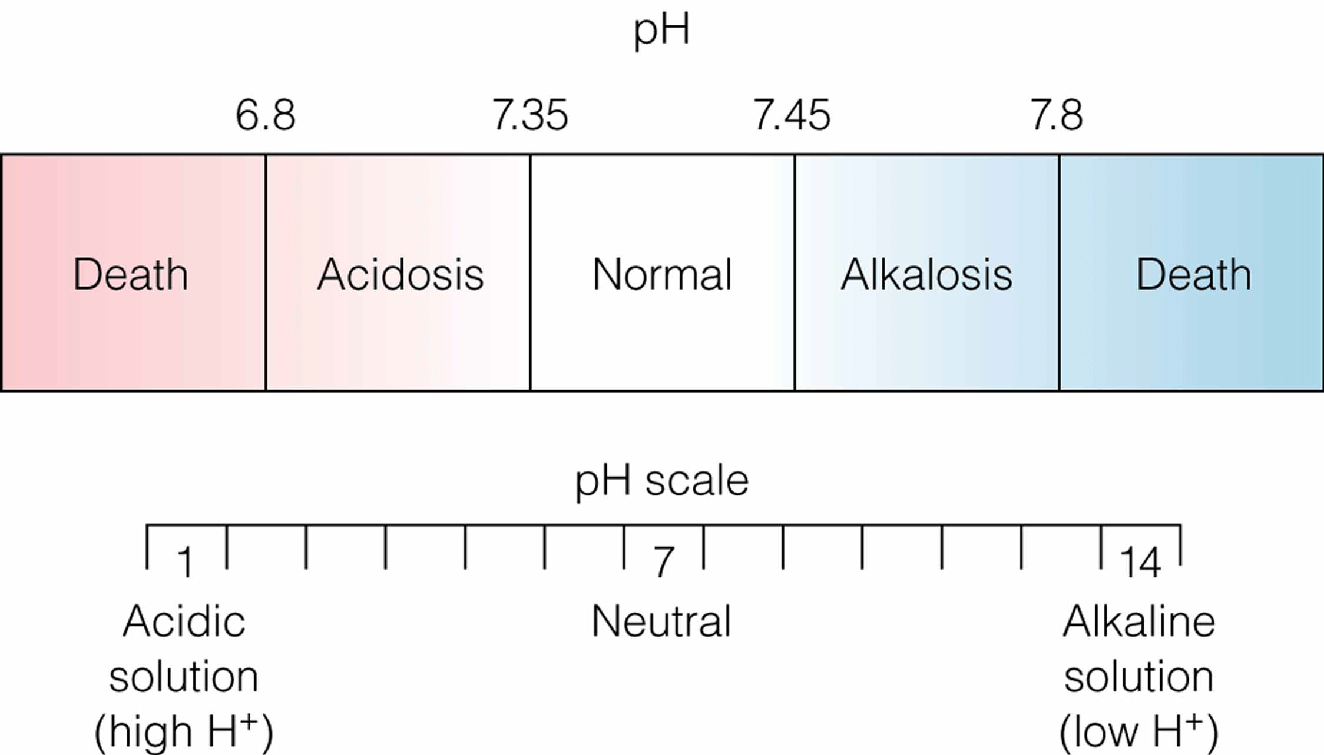
-
Factors Affecting Body Fluid, Electrolyte Age
-
Sex and body size
-
Health Condition
-
Medications
-
Environmental temperature
-
Lifestyle
-
Diet
-
Exercise
-
Stress
-
Alcohol consumption
-
Factors Affecting Body Fluid, Electrolyte Fluid Imbalances
Dehydration
-
Hyper-osmolar loss of only water leaving the client with excess sodium
Overhydration
-
Hypo-osmolar gain of only water leaving low osmolality and low serum sodium levels
Fluid volume overload
-
Bounding pulse
-
Distended neck & peripheral veins
-
Dyspnea; orthopnea
-
Pulmonary edema
-
Polyuria
-
Peripheral edema
-
Possible cerebral edema.
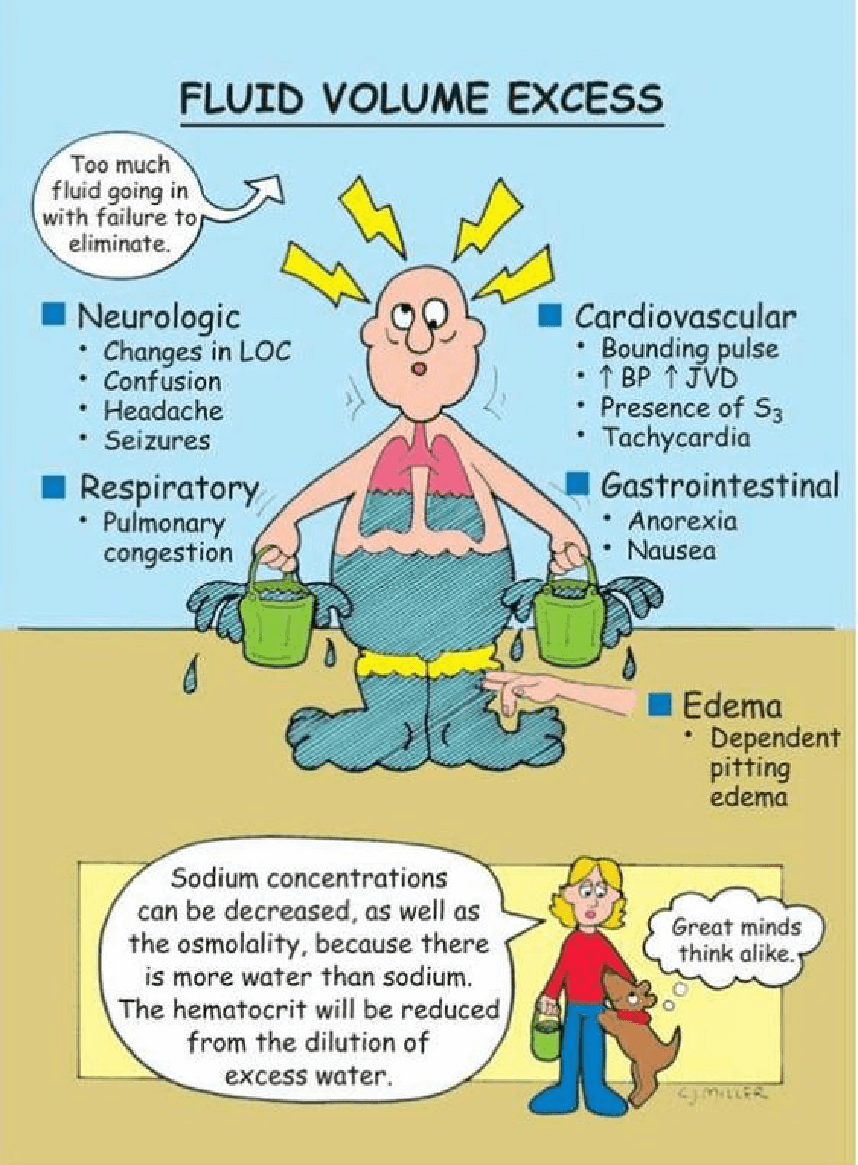
Figure 52-11: Evaluation of edema. B, Four-point scale for grading edema.
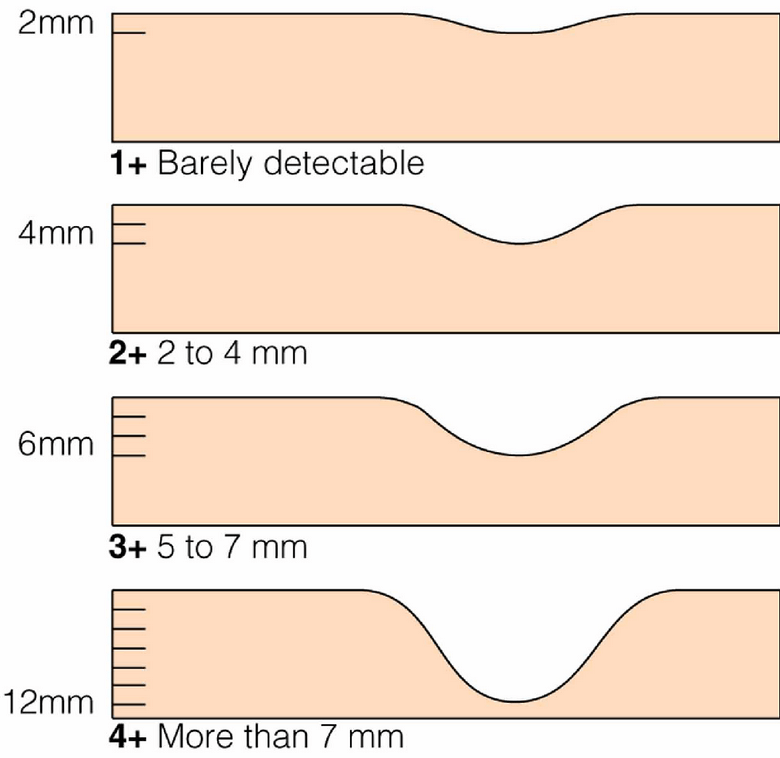
Fluid Volume Deficit
-
Poor skin turgor is associated with decreased urine output.
-
Sunken eyes In infants, sunken fontanels:
-
Low blood pressure Rapid heartbeat Rapid breathing
-
No tears when crying
-
Fever
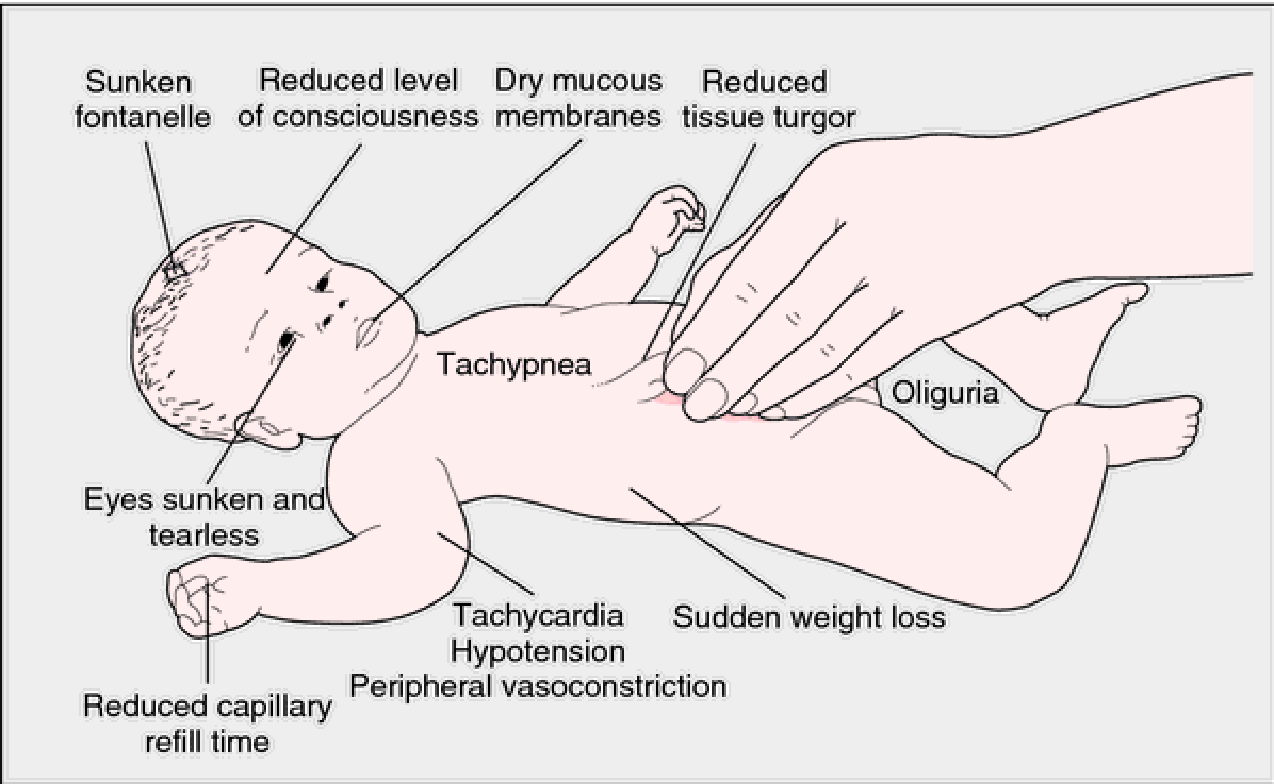
Causes of Electrolyte Imbalances
-
Excessive sweating
-
Fluid loss leading to dehydration
-
Excessive vomiting
-
Diuretics like Lasix (K+ depletion)
-
Massive blood loss
-
Dehydration may go unnoticed in hot, dry climates
-
Renal failure
|
Electrolyte |
Derangement |
Causes |
Signs and Symptoms |
Treatment |
Nursing Interventions |
|
Sodium |
Hypernatremia (high sodium) (>145 mEq/L) |
- Diarrhea, vomiting, fever, burns - Diabetes insipidus, kidney disease - High-protein diet, osmotic diuretics - Impaired thirst or mental judgment |
- Excessive thirst - Extreme fatigue, lethargy - Confusion, seizures, coma - Muscle twitching or spasms |
- Treat underlying cause - Replace water deficit with oral or IV fluids - Correct sodium level gradually to avoid cerebral edema |
- Monitor vital signs, fluid status, urine output - Assess neurological and mental status - Provide oral care and hydration - Educate patient on sodium restriction and fluid intake |
|
Sodium |
Hyponatremia (low sodium) (<135 mEq/L) |
- Diuretics, antidepressants, pain medications - Syndrome of inappropriate anti-diuretic hormone (SIADH) - Heart failure, liver cirrhosis, kidney disease - Excessive water intake or retention |
- Headache, nausea, vomiting - Muscle weakness, cramps - Confusion, irritability, restlessness - Seizures, coma |
- Treat underlying cause - Restrict water intake or administer diuretics - Correct sodium level gradually to avoid osmotic demyelination syndrome |
- Monitor vital signs, fluid status, urine output - Assess neurological and mental status - Provide oral care and hydration - Educate patient on fluid restriction and sodium intake |
|
Potassium |
Hyperkalemia (high potassium) (>5 mEq/L) |
- Renal failure, adrenal insufficiency - Acidosis, tissue injury, hemolysis - Potassium-sparing diuretics, ACE inhibitors - Excessive potassium intake or supplements |
- Muscle weakness, paralysis - Nausea, abdominal cramps - Cardiac arrhythmias, cardiac arrest - Paresthesia, anxiety |
- Treat underlying cause - Administer calcium gluconate to stabilize cardiac membrane - Administer insulin and glucose to shift potassium into cells - Administer sodium bicarbonate to correct acidosis |
- Monitor vital signs, cardiac rhythm, ECG changes - Assess muscle strength and reflexes - Monitor potassium level and renal function tests - Educate patient on potassium restriction and medication use |
|
Potassium |
Hypokalemia (low potassium) (<3.5 mEq/L) |
- Diarrhea, vomiting, laxative abuse - Metabolic alkalosis - Diuretics, corticosteroids - Insufficient potassium intake or absorption |
- Muscle weakness, fatigue - Constipation - Cardiac arrhythmias - Paresthesia |
- Treat underlying cause - Replace potassium orally or intravenously - Monitor potassium level and adjust dose accordingly - Correct acid-base imbalance if present |
- Monitor vital signs, cardiac rhythm,< ECG changes - Assess muscle strength and reflexes - Monitor potassium level and renal function tests - Educate patient on potassium-rich foods and medication use |
|
Calcium |
Hypercalcemia (high calcium) (>10.5 mg/dL) |
- Hyperparathyroidism - Malignancy - Vitamin D excess - Thiazide diuretics, lithium, antacids |
- Nausea, vomiting, anorexia - Polyuria, dehydration - Confusion, lethargy, coma - Kidney stones, bone pain |
- Treat underlying cause - Hydrate with saline infusion - Administer loop diuretics to increase calcium excretion - Administer bisphosphonates, calcitonin, or glucocorticoids to lower calcium level |
- Monitor vital signs, fluid status, urine output - Assess neurological and mental status - Monitor calcium level and renal function tests - Educate patient on calcium restriction and hydration |
|
Calcium |
Hypocalcemia (low calcium) (<8.5 mg/dL) |
- Hypoparathyroidism - Vitamin D deficiency - Renal failure - Magnesium deficiency, phosphate excess |
- Muscle cramps, tetany, spasms - Paresthesia, numbness - Cardiac arrhythmias - Positive Chvostek’s or Trousseau’s sign |
- Treat underlying cause - Replace calcium orally or intravenously - Administer vitamin D to enhance absorption - Correct magnesium or phosphate imbalance if present |
- Monitor vital signs, cardiac rhythm,< ECG changes - Assess muscle strength and reflexes - Monitor calcium level and other electrolytes - Educate patient on calcium-rich foods and supplements |
|
Magnesium |
Hypermagnesemia (high magnesium) (>2.5 mEq/L) |
- Renal failure - Adrenal insufficiency - Magnesium-containing antacids or laxatives - Excessive magnesium infusion |
- Hypotension, bradycardia - Muscle weakness, paralysis - Respiratory depression - Lethargy, coma |
- Treat underlying cause - Discontinue magnesium intake or infusion - Administer calcium gluconate to antagonize effects on cardiac muscle - Administer loop diuretics or dialysis to increase magnesium excretion |
- Monitor vital signs, cardiac rhythm,< ECG changes - Assess muscle strength and reflexes - Monitor magnesium level and renal function tests - Educate patient on magnesium restriction and medication use |
Be Alert
Hyperkalemia is usually more dangerous because cardiac arrest is more frequently associated with high serum potassium levels.
Potassium may be given intravenously for severe hypokalemia.
-
It must always be diluted appropriately and never be given IV push.
-
Potassium that is to be given IV should be mixed in the pharmacy and double-checked prior to administration by two nurses.
-
The usual concentration of IV potassium is 2O to 4O mEq/L.
Hypocalcemia
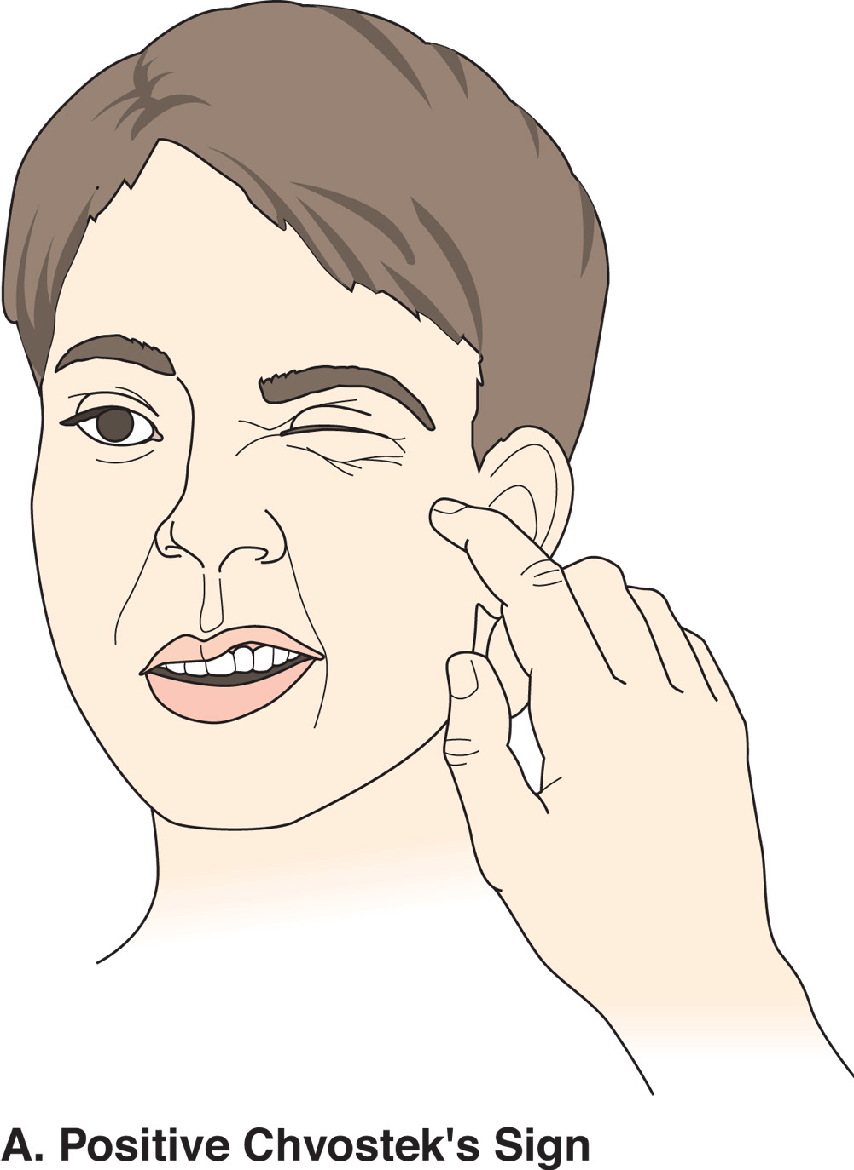
Hypocalcemia
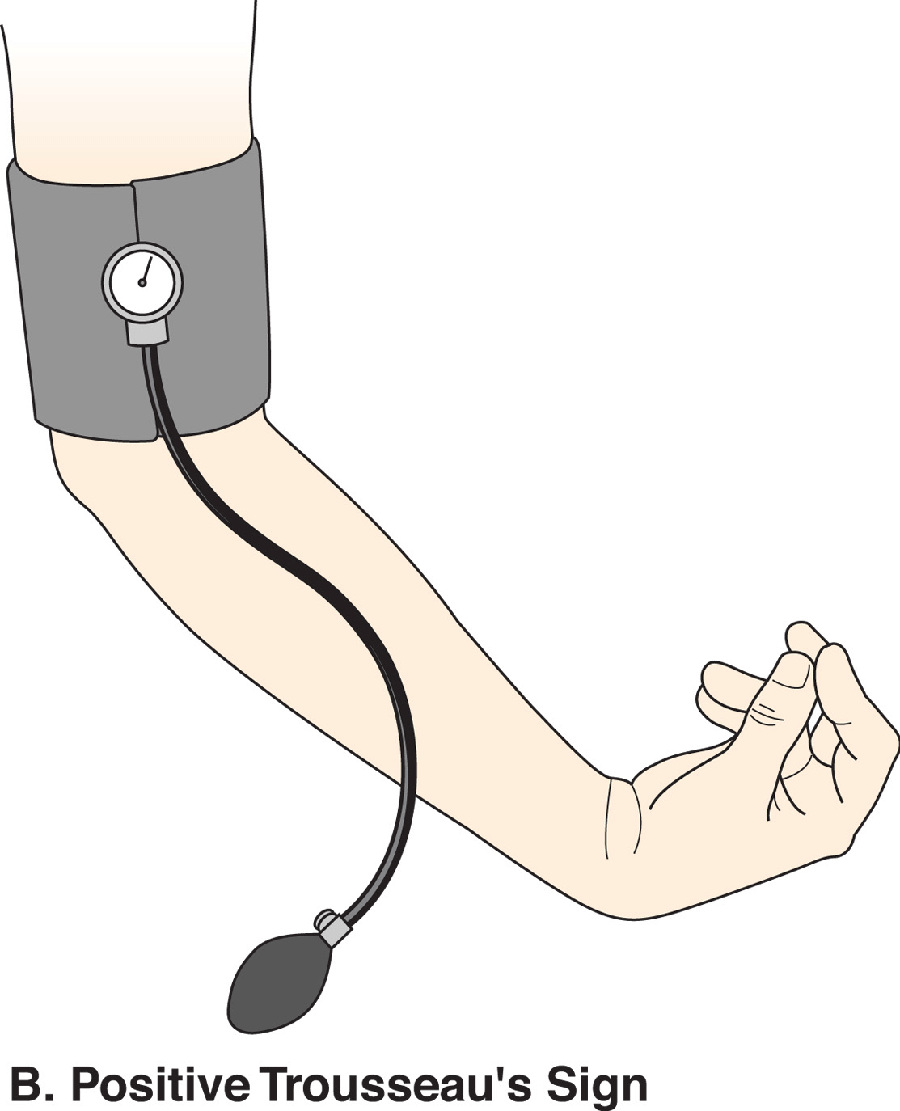
Nursing Assessment of Fluid and Electrolyte Imbalances
-
Chronic diseases
-
Acute conditions
-
Medications
-
Age:
-
Very old or very young
-
-
Inability to access food and fluids
Physical Assessment:
-
Skin
-
Mucus membranes
-
Eyes
-
Fontanels (infants)
-
Cardiovascular system
-
Respiratory system
-
Neurologic
Clinical Measurements:
-
Daily weights:
-
At the same time each day
-
Wearing the same or similar clothing
-
On the same scale
-
-
Vital signs
-
Fluid intake/output
Intake to be Recorded:
-
Oral fluids
-
Foods that are or become liquid at room temperature
-
Tube feedings
-
Parenteral feedings
-
IV medications
-
Catheter or tube irrigation
Output to be Recorded:
-
Urinary output
-
Vomitus and liquid feces
-
Tube drainage
-
Wound and Fistula Drainage
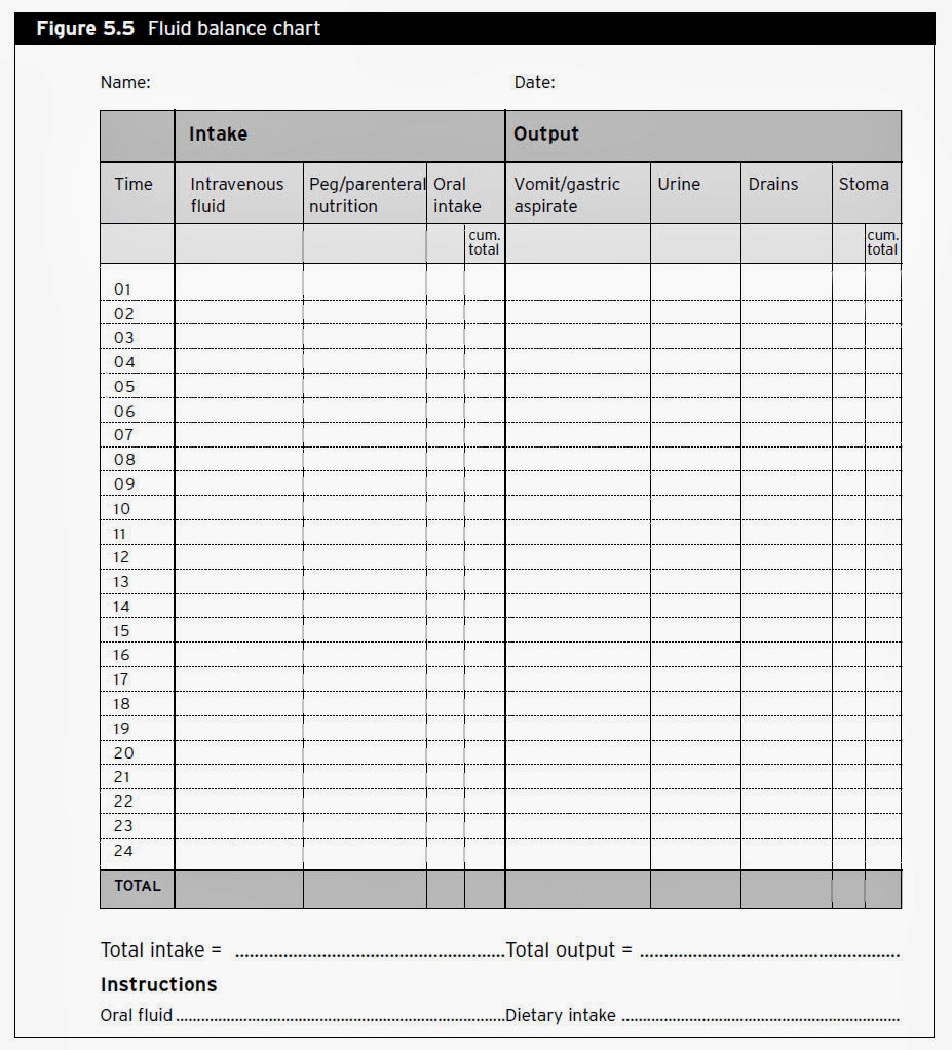
NANDA Nursing Diagnoses
-
Deficient Fluid Volume
-
Excess Fluid Volume
-
Risk for Imbalanced Fluid Volume
-
Risk for Deficient Fluid volume
-
Impaired Gas Exchange
Planning
-
Maintain or restore normal fluid balance.
-
Maintain or restore normal balance of electrolytes.
-
Maintain or restore gas exchange and oxygenation.
-
Prevent associated risks:
-
Tissue breakdown
-
Decreased cardiac output
-
Confusion and other neurologic signs.
-
Implementing
-
Fluid intake modifications
-
Dietary changes
-
Oral electrolyte supplements
-
Parenteral fluid and electrolyte, and blood replacement.
Others:
- Providing skin care and oral hygiene
- Positioning the client appropriately
- Scheduling rest periods
Promoting Fluid and Electrolyte Balance
-
Consume 6-8 glasses water daily
-
Avoid foods with excess salt, sugar, caffeine
-
Eat well-balanced diet
-
Increase fluid intake before, during, and after active exercise
-
Replace lost electrolytes
Correcting Imbalances
Types of Intravenous Solution
Isotonic
-
Same salt concentration as cells and blood.
-
Has normal osmolarity (275 to 295 m0sm/kg)
Hypotonic
-
Fewer dissolved particles (like salt and other electrolytes) than is found in body cells and blood.
-
Has lower osmolarity (<270)
Hypertonic
-
Higher salt concentration than body cells and blood.
-
Has higher osmolarity (>300)
-
IV solutions with very high (>500 mEq/L) should only be
-
given via central lines.
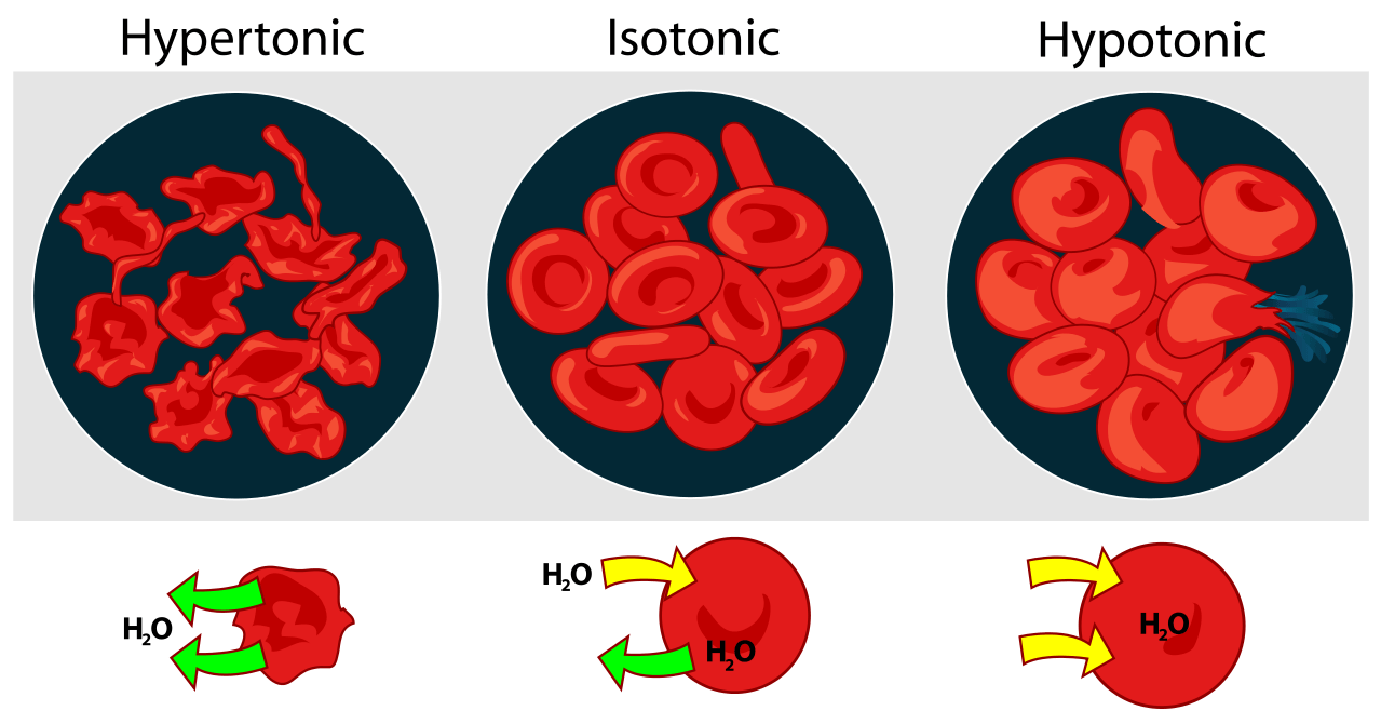
|
Hypertonic |
Isotonic |
Hypotonic |
|
Type |
Solution |
Use |
|
Hypertonic |
Dextrose 5% in 0.45% normal saline |
Later in DKA treatment |
|
Hypertonic |
Dextrose 5% in normal saline |
Temporary treatment for shock if plasma expanders aren’t available<br>Addison’s crisis |
|
Hypertonic |
Dextrose 10% in water |
Water replacement<br>Condition where some nutrition with glucose is required |
|
Isotonic |
Dextrose 5% in water (D5W) |
Fluid loss<br>Dehydration<br>Hypernatremia |
|
Isotonic |
0.9% sodium chloride (Normal Saline) (NaCl) |
Shock<br>Hyponatremia<br>Blood transfusions<br>Resuscitation<br>Fluid challenge<br>DKA |
|
Isotonic |
Lactated Ringer’s (LR) |
Dehydration<br>Burns<br>Lower GI fluid loss<br>Acute blood loss<br>Hypovolemia due to third-space shifting |
|
Hypotonic |
0.45% sodium chloride (1/2 normal saline) |
Water replacement<br>DKA<br>Gastric fluid loss from NG or vomiting |
Techniques of Peripheral and Central Vascular Access
A peripheral venous access:
-
Is placed into a peripheral vein in order to administer medication or fluids.
-
Cephalic, basilic, median, humeral and femoral vein.
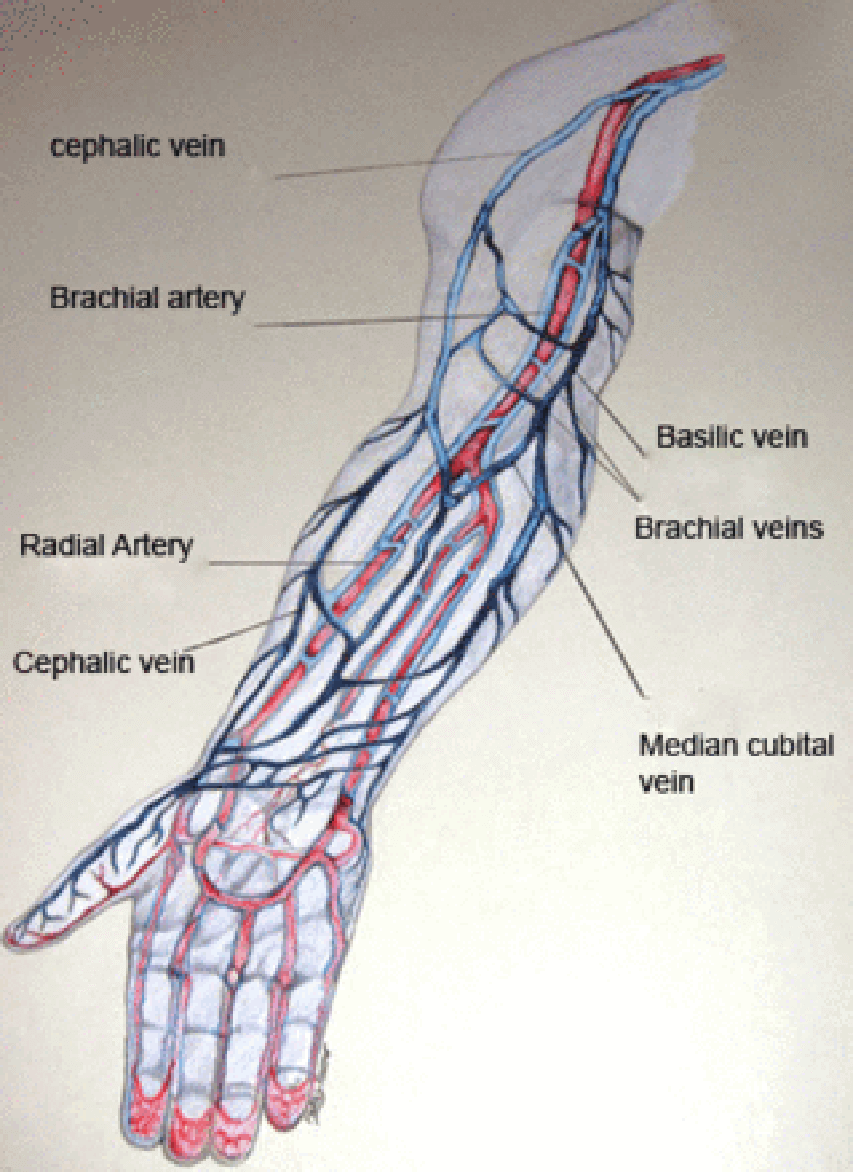
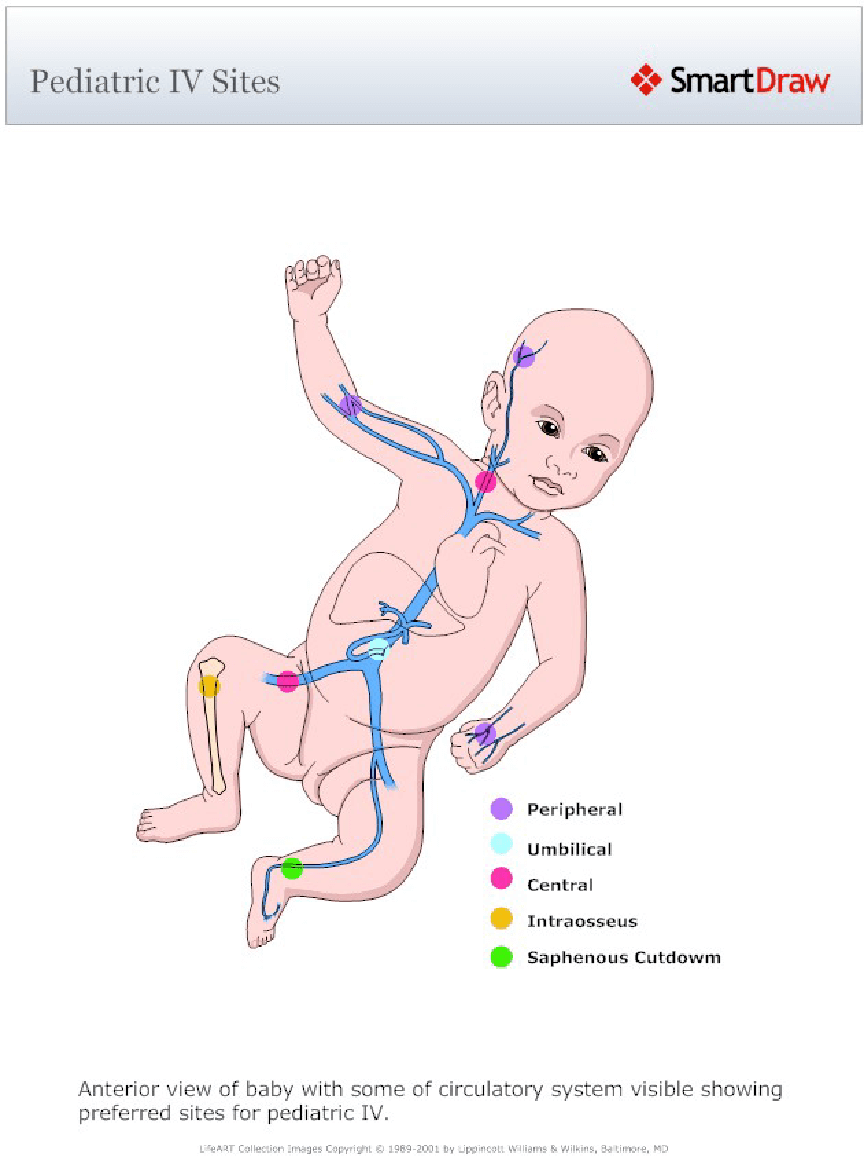
Central venous access:
-
Inserted in a central vein
-
Usually internal jugular vein of the neck or the subclavian vein of the chest.
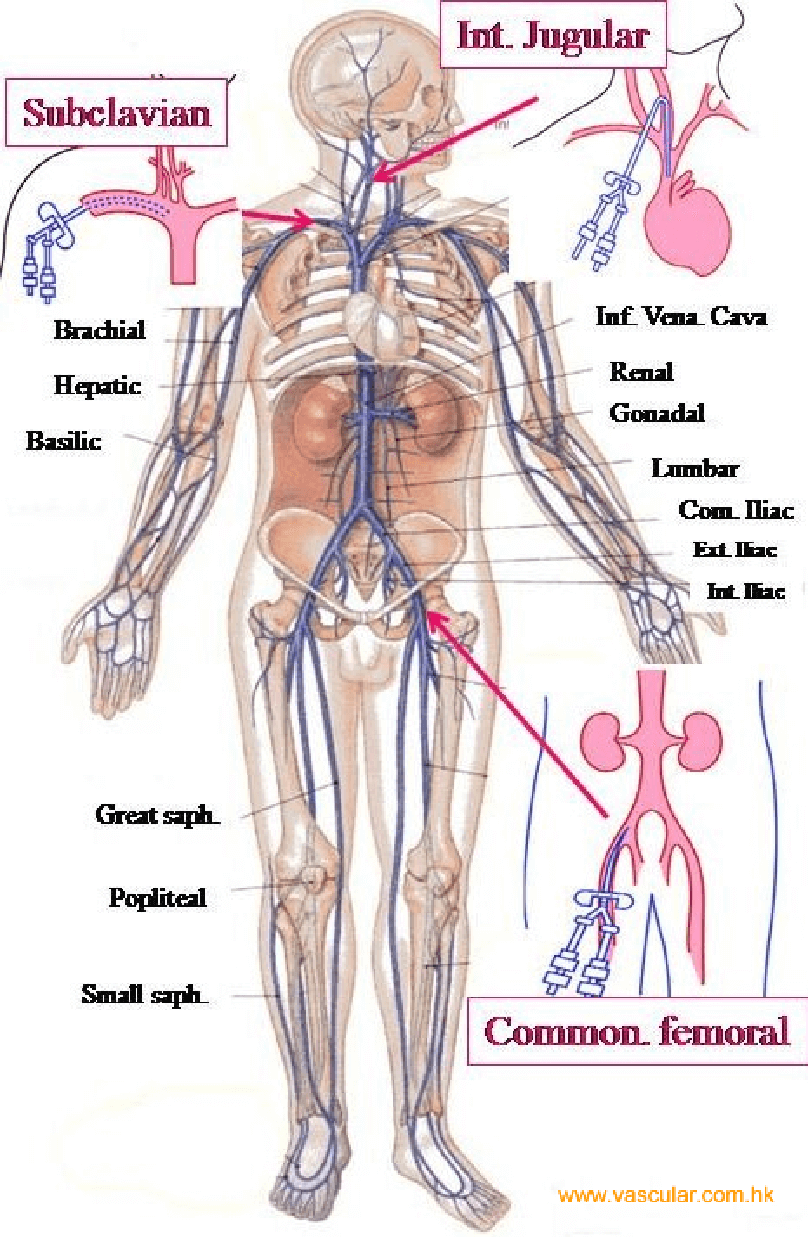
-
Common Complications of Intravenous Fluid Infusion Phlebitis/Thrombophlebitis:
-
Occur more frequently.
-
Phlebitis is inflammation of the vein.
-
Thrombophlebitis is inflammation associated with a thrombus.
-
Infiltration:
-
Infusion of fluid and/or medication outside the intravascular space, into the surrounding soft tissue.
-
Swelling of the soft tissue surrounding the IV, the skin feels cool, firm and pale.
-
Extravasation
-
The leaking of solution or vesicant drugs(antineoplastics) into surrounding tissue.
-
Cause severe local tissue damage.
-
Result in:
-
Delayed healing
-
Infection
-
Tissue necrosis
-
Deformity
-
Loss of function
-
Amputation.
Common Complications of Intravenous Fluid Infusion
1. Phlebitis/Thrombophlebitis:
-
Occur more frequently.
-
Phlebitis is inflammation of the vein.
-
Thrombophlebitis is inflammation associated with a thrombus.
2. Infiltration:
-
Infusion of fluid and/or medication outside the intravascular space, into the surrounding soft tissue.
-
Swelling of the soft tissue surrounding the IV, the skin feels cool, firm and pale.
3. Extravasation
-
The leaking of solution or vesicant drugs(antineoplastics) into surrounding tissue.
-
Cause severe local tissue damage.
-
Result in:
- Delayed healing
- Infection
- Tissue necrosis
- Deformity
- Loss of function
- Amputation.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Fluid and Electrolytes
This filled cannot be empty

