Please set your exam date
Introduction
Study Questions
Introduction
A nurse is teaching a group of community members about the importance of first aid. Which of the following statements by the nurse is appropriate?
Explanation
Choice A Reason: This statement is incorrect because first aid is not a substitute for professional medical care, but a bridge to keep the victim alive and stable until help arrives.
Choice B Reason: This statement is incorrect because first aid is not only for comfort, but also for life-saving interventions in emergency situations.
Choice C Reason: This statement is incorrect because first aid is an essential skill for everyone, not just health professionals, as anyone can encounter an emergency situation.
Choice D Reason: This statement is correct because it summarizes the definition and benefits of first aid as given in the text. First aid is a way to prevent the person's condition from worsening and keep them alive until help arrives. This statement reflects the purpose and scope of first aid as described in the text.
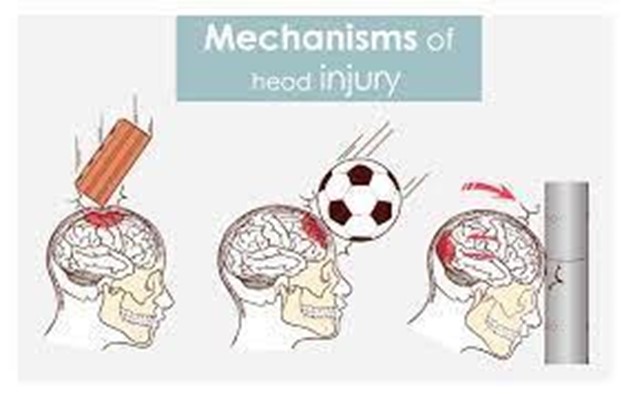
A nurse is assessing a victim who has fallen from a ladder and hit his head. Which of the following actions should the nurse perform as part of the primary assessment? (Select all that apply.)
Explanation
Choice A Reason: This action is correct because checking for responsiveness is the first step in assessing an unconscious or unresponsive victim.
Choice B Reason: This action is correct because calling for help and activating EMS is the second step in assessing an emergency situation.
Choice C Reason: This action is correct because opening the airway is the third step in assessing a victim who is not breathing or has abnormal breathing.
Choice D Reason: This action is incorrect because checking for bleeding is part of the secondary assessment, which involves checking for other injuries or illnesses that are not immediately life-threatening.
Choice E Reason: This action is incorrect because monitoring level of consciousness is part of the ongoing assessment, which involves observing for changes in the victim's condition until help arrives or the victim recovers.
A nurse is providing first aid to a client who has a deep cut on his arm from a kitchen knife. The client says, "I don't want you to touch me or put anything on my wound." How should the nurse respond?
Explanation
Choice A Reason: This response is incorrect because it does not respect the client's right to refuse first aid and may sound threatening or coercive.
Choice B Reason: This response is incorrect because it does not acknowledge the client's concern or consent and may sound dismissive or paternalistic.
Choice C Reason: This response is correct because it respects the client's right to refuse first aid and informs them of the risks of refusing care. It's your right to refuse first aid, but I need to explain the possible consequences of your decision. This response respects the client's autonomy and informs them of the risks of refusing care.
Choice D Reason: This response is incorrect because it does not address the client's concern or consent and may sound arrogant or condescending.
A nurse is performing CPR on a victim who has no pulse and is not breathing. The nurse has an AED available. What should the nurse do next?
Explanation
Choice A Reason: This action is incorrect because stopping CPR can reduce the chances of survival for the victim.
Choice B Reason: This action is correct because continuing CPR and attaching the AED pads to the victim's chest follows the steps for performing CPR and using AED as described in the text. Continue CPR and attach the AED pads to the victim's chest. This action follows the steps for performing CPR and using AED as described in the text.
Choice C Reason: This action is incorrect because giving two rescue breaths can delay the use of the AED, which can be more effective than rescue breaths in restoring a normal heart rhythm.
Choice D Reason: This action is incorrect because checking the victim's pulse can waste time and interrupt CPR, which should continue until the AED is ready.
A nurse is caring for a client who has a second-degree burn on his hand from touching a hot iron. Which of the following interventions should the nurse perform?
Explanation
Choice A Reason: This action is incorrect because applying ice to a burn can cause more damage to the skin and tissues.
Choice B Reason: Cover the burn with a sterile dressing. This intervention protects the burn from infection and further injury, as recommended in the text. This action is correct because covering the burn with a sterile dressing protects it from infection and further injury, as recommended in the text.
Choice C Reason: This action is incorrect because breaking the blisters and applying ointment can increase the risk of infection and delay healing.
Choice D Reason: This action is correct but not specific to a second-degree burn. Elevating an injured part can reduce swelling and pain, but it is not a priority intervention for a burn.
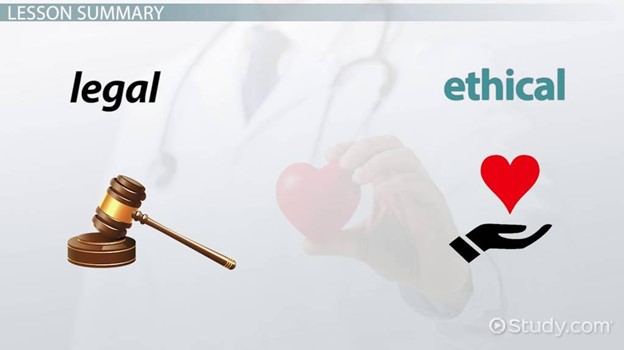
Legal and Ethical Aspects of First Aid
A nurse is providing first aid to a client who has a minor cut on his finger. The client tells the nurse that he does not want any treatment and asks the nurse to leave him alone. What should the nurse do?
Explanation
Choice A Reason: This action is incorrect because it violates the client's right to refuse first aid and may cause harm or resentment.
Choice B Reason: This action is correct because it respects the client's right to refuse first aid and documents his refusal as required by law. Respect the client's right to refuse first aid and document his refusal. This action follows the ethical principle of autonomy and the legal aspect of refusal as described in the text.
Choice C Reason: This action is incorrect because it does not respect the client's right to refuse first aid and may be seen as coercive or manipulative.
Choice D Reason: This action is incorrect because it is unnecessary and inappropriate for a minor injury that does not pose a serious threat to the client's health.
A nurse is providing first aid to a child who has fallen from a bicycle and has a head injury. The child is unconscious and has no identification. The nurse should obtain consent for first aid from: (Select all that apply.)
Explanation
Choice A Reason: This choice is correct because the child's parent or guardian is the legal representative of the child and can give consent for first aid.
Choice B Reason: This choice is incorrect because the child's teacher or coach is not authorized to give consent for first aid unless they have a written permission from the parent or guardian.
Choice C Reason: This choice is incorrect because the child's friend or sibling is not authorized to give consent for first aid unless they are an adult and have a written permission from the parent or guardian.
Choice D Reason: This choice is incorrect because the child's physician or nurse practitioner is not present at the scene and cannot give consent for first aid over the phone or online.
Choice E Reason: This choice is correct because if the child's parent or guardian is unavailable, the nurse can provide first aid based on implied consent, assuming that an unconscious person would give consent if they were able.
A nurse is providing first aid to a client who has a severe allergic reaction to a bee sting. The client has difficulty breathing and swelling of the face and throat. The nurse has an epinephrine auto-injector and asks the client for consent to use it. The client says, "No, I don't want any drugs. Just leave me alone." How should the nurse respond?
Explanation
Choice A Reason: This response is incorrect because it does not inform the client of the possible consequences of their decision and may imply that the nurse is abandoning them.
Choice B Reason: This response is incorrect because it does not respect the client's right to refuse first aid and may sound threatening or coercive.
Choice C Reason: This response is correct because it respects the client's right to refuse first aid and informs them of their decision's possible consequences.
Choice D Reason: This response is incorrect because it does not address the client's concern or consent and may sound dismissive or paternalistic.
A nurse is providing first aid to a client who has fainted in a crowded mall. The nurse checks the client's pulse and finds it to be weak and rapid. The nurse elevates the client's legs and loosens any tight clothing. The nurse also asks the bystanders to move away and give the client some space. The nurse hears one of the bystanders say:
Explanation
Choice A Reason: This statement is incorrect because giving water or juice to a fainting victim can cause choking or aspiration.
Choice B Reason: This statement is correct because it indicates that the bystander is concerned and willing to assist the nurse if needed.
Choice C Reason: This statement is incorrect because calling 911 right away may not be necessary for a fainting victim who may recover quickly.
Choice D Reason: This statement is incorrect because giving candy to a fainting victim can cause choking or aspiration, and low blood sugar may not be the cause of fainting.
A nurse is providing first aid to a client who has accidentally cut his finger with a kitchen knife. The nurse cleans the wound with soap and water and applies pressure with a clean cloth to stop the bleeding. The nurse then covers the wound with a sterile dressing and advises the client to seek medical attention if needed. The nurse should also document:
Explanation
Choice A Reason: This choice is correct because it includes all the relevant information for legal and ethical documentation of first aid as described in the text.
Choice B Reason: This choice is incorrect because it only includes some of the assessment findings but not the other information required for documentation.
Choice C Reason: This choice is incorrect because it includes unnecessary or irrelevant information that may violate confidentiality or privacy.
Choice D Reason: This choice is incorrect because it includes unnecessary or irrelevant information that may not affect wound care or outcome.
Primary and Secondary Assessment
A nurse is providing first aid to a client who has been involved in a car accident. The nurse should perform a primary assessment to check for which of the following conditions?
Explanation
Choice A Reason: This choice is incorrect because fractures or dislocations are not life-threatening and do not affect the ABCs of the primary assessment.
Choice B Reason: This choice is incorrect because head or spinal injuries are not life-threatening and do not affect the ABCs of the primary assessment.
Choice C Reason: This choice is correct because severe bleeding or shock are life-threatening and affect the victim's circulation, which is one of the ABCs of the primary assessment.
Choice D Reason: This choice is incorrect because burns or wounds are not life-threatening and do not affect the ABCs of the primary assessment.
A nurse is providing first aid to a client who has fainted in a crowded mall. The nurse should perform a secondary assessment to check for which of the following conditions? (Select all that apply.)
Explanation
Choice A Reason: This choice is incorrect because airway obstruction is a life-threatening condition that should be checked and treated in the primary assessment.
Choice B Reason: This choice is incorrect because breathing arrest is a life-threatening condition that should be checked and treated in the primary assessment.
Choice C Reason: This choice is incorrect because circulatory arrest is a life-threatening condition that should be checked and treated in the primary assessment.
Choice D Reason: This choice is correct because head injury is a possible cause or complication of fainting that is not immediately life-threatening but requires further evaluation and care.
Choice E Reason: This choice is correct because dehydration is a possible cause or complication of fainting that is not immediately life-threatening but requires further evaluation and care.
A nurse is providing first aid to a client who has been bitten by a snake. The nurse should call 911 and perform a primary assessment to check for signs of anaphylaxis, such as:
Explanation
Choice A Reason: This choice is correct because difficulty breathing is caused by swelling of the airways or bronchospasm that restricts airflow.
Choice B Reason: This choice is correct because swelling of face, lips, tongue, or throat is caused by fluid accumulation in the tissues that can block the airway.
Choice C Reason: This choice is correct because hives or itching are caused by histamine release that triggers an inflammatory response in the skin.
Choice D Reason: This choice is correct because it includes all of the signs of anaphylaxis as described in the text.
A nurse is providing first aid to a client who has a burn on his arm from touching a hot stove. The nurse should perform a secondary assessment to determine the severity of the burn by checking for which of the following factors?
Explanation
Choice A Reason: This choice is correct because the depth of the burn indicates how many layers of skin are damaged and how likely it is to heal.
Choice B Reason: This choice is correct because the size of the burn indicates how much body surface area is affected and how much fluid loss and heat loss may occur.
Choice C Reason: This choice is correct because the location of the burn indicates how vulnerable it is to infection and how it may affect the function of vital organs or structures.
Choice D Reason: This choice is correct because it includes all of the factors that affect the severity of the burn as described in the text.
A nurse is providing first aid to a client who has ingested a large amount of alcohol and is vomiting. The nurse should perform a primary assessment to check for which of the following conditions?
Explanation
Choice A Reason: This choice is incorrect because dehydration is not life-threatening and does not affect the ABCs of the primary assessment.
Choice B Reason: This choice is incorrect because hypothermia is not life-threatening and does not affect the ABCs of the primary assessment.
Choice C Reason: This choice is correct because aspiration is life-threatening and affects the victim's airway, which is one of the ABCs of the primary assessment.
Choice D Reason: This choice is incorrect because alcohol poisoning is not life-threatening and does not affect the ABCs of the primary assessment.
Cardiopulmonary Resuscitation (CPR) and Automated External Defibrillator (AED)
A nurse is providing CPR to a client who has no pulse and is not breathing. The nurse should give two breaths after every:
Explanation
Choice A Reason: This choice is incorrect because giving two breaths after every 10 compressions would interrupt the chest compressions too frequently and reduce blood flow.
Choice B Reason: This choice is incorrect because giving two breaths after every 15 compressions would interrupt the chest compressions too frequently and reduce blood flow.
Choice C Reason: This choice is correct because giving two breaths after every 30 compressions is the recommended ratio of compressions to breaths for CPR as described in the text.
Choice D Reason: This choice is incorrect because giving two breaths after every 50 compressions would delay the ventilation too long and cause hypoxia.
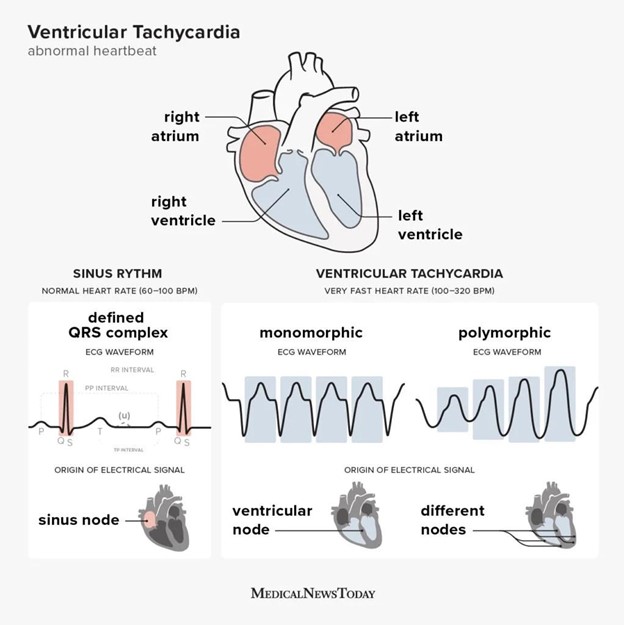
A nurse is using an AED on a client who has ventricular fibrillation. The nurse should attach the AED pads to which of the following locations on the client's chest? (Select all that apply.)
Explanation
Choice A Reason: This choice is correct because it places one pad on the upper right side below the collarbone, which is close to the right ventricle of the heart.
Choice B Reason: This choice is correct because it places one pad on the lower left side below the nipple, which is close to the left ventricle of the heart.
Choice C Reason: This choice is incorrect because it places one pad on the lower right side above the navel, which is too far from the heart and may interfere with abdominal organs.
Choice D Reason: This choice is incorrect because it places one pad on the upper left side above the nipple, which is too high and may interfere with lung tissue.
Choice E Reason: This choice is incorrect because it places one pad on the lower left side above the hip, which is too far from the heart and may interfere with pelvic organs.
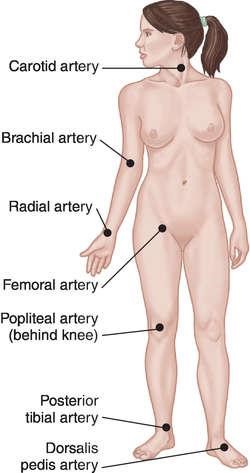
A nurse is providing CPR to a child who has no pulse and is not breathing. The nurse should check for a brachial pulse by feeling:
Explanation
Choice A Reason: This choice is incorrect because it describes the location of the carotid artery, which is used to check for a pulse in an adult.
Choice B Reason: This choice is correct because it describes the location of the brachial artery, which is used to check for a pulse in a child or an infant.
Choice C Reason: This choice is incorrect because it describes the location of the radial artery, which is used to check for a pulse in an adult or a conscious child.
Choice D Reason: This choice is incorrect because it describes the location of the popliteal artery, which is not used to check for a pulse in CPR.
A nurse is using an AED on a client who has ventricular tachycardia. The nurse turns on the AED and follows the voice prompts. The AED says:
Explanation
Choice A Reason: This choice is correct because it indicates that the AED has detected a shockable rhythm and is preparing to deliver a shock to the client's heart.
Choice B Reason: This choice is incorrect because it indicates that the AED has detected a non-shockable rhythm and advises the nurse to check for a pulse and start CPR if needed.
Choice C Reason: This choice is incorrect because it indicates that the AED has encountered a problem and advises the nurse to check for proper electrode placement and call for help.
Choice D Reason: This choice is incorrect because it indicates that the AED has detected a normal rhythm and advises the nurse to check for breathing and give oxygen if needed.
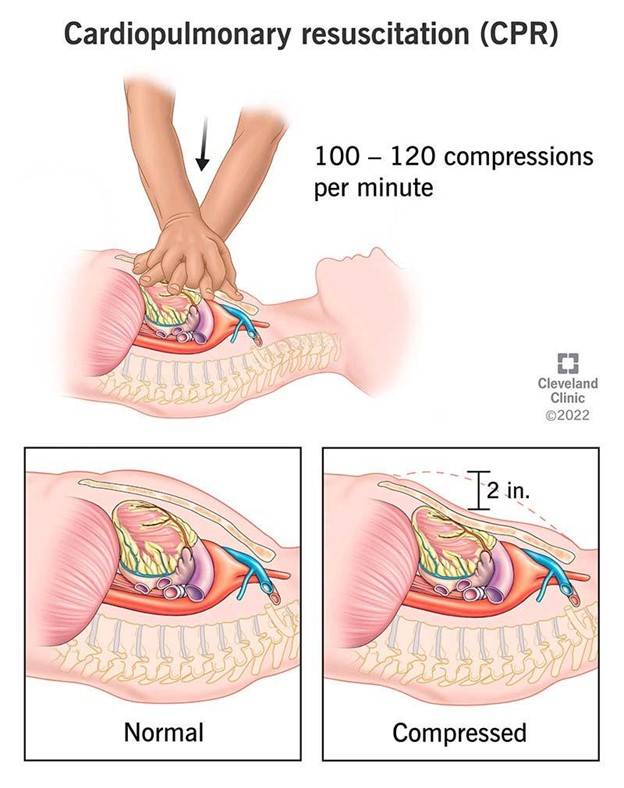
A nurse is providing CPR to an adult who is unconscious and not breathing. The nurse should compress the chest at a rate of:
Explanation
Choice A Reason: This choice is incorrect because compressing the chest at a rate of 60 to 80 compressions per minute is too slow and may not provide adequate blood flow.
Choice B Reason: This choice is incorrect because compressing the chest at a rate of 80 to 100 compressions per minute is too slow and may not provide adequate blood flow.
Choice C Reason: This choice is correct because compressing the chest at a rate of 100 to 120 compressions per minute is the recommended rate of chest compressions for CPR as described in the text.
Choice D Reason: This choice is incorrect because compressing the chest at a rate of 120 to 140 compressions per minute is too fast and may not allow the chest to recoil fully after each compression.
Wound Care and Bleeding Control
A nurse is caring for a client who has a deep laceration on the forearm. The nurse notices that the wound is oozing dark red blood. What type of bleeding is this?
Explanation
Choice A Reason: Arterial bleeding is bright red and spurts from a wound, not dark red and oozing.
Choice B Reason: Venous bleeding is characterized by a steady flow of dark red blood from a wound, which matches the description in the question.
Choice C Reason: Capillary bleeding is slow and oozes from a wound, but it is usually lighter in color than venous bleeding.
Choice D Reason: Hemorrhagic bleeding is severe and life-threatening, and it can be arterial or venous, but it is not a specific type of bleeding.
A nurse is teaching a group of students about wound care and bleeding control. Which of the following statements should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A Reason: Alcohol should not be used to clean a wound, as it can damage healthy tissue and delay healing. Soap and water or saline solution are preferred.
Choice B Reason: The frequency of dressing changes depends on the type and condition of the wound, but it should not be done more often than necessary, as it can disrupt healing and increase the risk of infection.
Choice C Reason: Applying direct pressure to a wound with a clean cloth or bandage is the most effective way to stop the bleeding, as it compresses the blood vessels and prevents further blood loss.
Choice D Reason: Elevating the injured part above the level of the heart can help reduce blood loss by gravity, as it lowers the blood pressure in the injured area and reduces blood flow.
Choice E Reason: Using a tourniquet as the first option to control bleeding is not recommended, as it can cause tissue damage and necrosis by cutting off blood supply to the limb. It should only be used as a last resort when other methods fail, and it should be loosened every 10 minutes to check for signs of circulation.
A nurse is assessing a client who has an infected wound on the leg. The nurse observes that the wound has yellow-green drainage, foul odor, and increased pain. The nurse asks the client how they feel about their wound. Which of the following statements by the client indicates a need for further intervention?
Explanation
Choice A Reason: Worrying about wound healing is a normal reaction, but it does not indicate a need for further intervention, unless it affects the client's mood or coping skills.
Choice B Reason: Feeling embarrassed by how a wound looks and smells is also a normal reaction, but it does not indicate a need for further intervention, unless it affects the client's self-esteem or social interactions.
Choice C Reason: Taking antibiotics as prescribed by a doctor is an appropriate action for an infected wound, as it helps prevent or treat bacterial infection.
Choice D Reason: Cleaning a wound with hydrogen peroxide every day can harm healthy tissue and delay healing, as well as increase the risk of infection by altering the pH balance of the wound environment. This indicates a need for further intervention by the nurse.
A nurse is preparing to dress a wound on a client's abdomen. The nurse notices that the wound edges are approximated, the wound bed is pink, and there is no drainage or signs of infection. The nurse selects a transparent film dressing for the wound. What is the rationale for this choice?
Explanation
Choice A Reason: A transparent film dressing protects the wound from contamination and allows oxygen to reach the wound, which promotes healing. This is the rationale for this choice.
Choice B Reason: A transparent film dressing does not absorb any drainage, so it is not suitable for wounds that are wet or exudative. A hydrocolloid or foam dressing would be more appropriate for these types of wounds, as they absorb excess drainage and provide a moist environment for healing.
Choice C Reason: A transparent film dressing does not debride any necrotic tissue, so it is not suitable for wounds that are infected or have slough or eschar. A hydrogel or enzymatic dressing would be more appropriate for these types of wounds, as they debride necrotic tissue and stimulate granulation tissue formation.
Choice D Reason: A transparent film dressing does not compress the wound, so it is not suitable for wounds that are bleeding or have edema. A gauze or elastic bandage would be more appropriate for these types of wounds, as they compress the wound and prevent bleeding and edema.
A nurse is caring for a client who has a gunshot wound on the chest. The nurse observes that the client's breathing is rapid and shallow, the pulse is weak and thready, and the blood pressure is low. The nurse suspects that the client has developed a tension pneumothorax. What should the nurse do first?
Explanation
Choice A Reason: Administering oxygen via nasal cannula may help improve oxygenation, but it does not address the underlying cause of tension pneumothorax, which is increased pressure in the chest cavity.
Choice B Reason: Inserting a chest tube in the affected side may help drain air and fluid from the pleural space and restore lung expansion, but it requires sterile equipment and preparation, which may delay treatment.
Choice C Reason: Performing needle decompression in the second intercostal space at the midclavicular line on the affected side can release the trapped air and relieve the pressure in the chest cavity, which can improve ventilation and circulation. This is a rapid and effective intervention that can be done with minimal equipment and preparation.
Choice D Reason: Applying an occlusive dressing over the wound may help prevent air from entering or escaping from the pleural space, but it does not remove any existing air that has already caused tension pneumothorax.
Nursing Interventions on First Aid
A nurse is providing first aid to a client who has a deep laceration on the lower leg and is bleeding profusely. Which of the following actions should the nurse take first?
Explanation
Choice A Reason: The nurse should apply direct pressure to the wound with a clean cloth or gauze to control bleeding as the first priority. This action can reduce blood loss and prevent shock.
Choice B Reason: The nurse should elevate the leg above the level of the heart after applying direct pressure to the wound. This action can help reduce swelling and bleeding by decreasing venous pressure.
Choice C Reason: The nurse should wrap the wound with a sterile dressing after controlling bleeding and elevating the leg. This action can protect the wound from infection and further injury.
Choice D Reason: The nurse should call for EMS if the bleeding is severe, does not stop, or if there are signs of shock, such as pale skin, rapid pulse, low blood pressure, or altered mental status. The nurse should not leave the client alone while waiting for EMS.
A nurse is teaching a group of students about first aid for fractures. Which of the following statements should the nurse include as a correct guideline? (Select all that apply.)
Explanation
Choice A Reason: The nurse should splint the injured part in the position it was found to prevent further damage to the nerves, blood vessels, and soft tissues. The nurse should not attempt to realign or move the fractured bone unless there is no pulse distal to the injury.
Choice B Reason: The nurse should check for pulses, sensation, and movement distal to the injury before and after splinting to assess for neurovascular compromise. The nurse should report any changes or abnormalities to EMS or a health care provider.
Choice C Reason: The nurse should apply ice packs to the injured area for 20 minutes every hour to reduce pain, swelling, and inflammation. The nurse should wrap the ice pack in a cloth or towel to prevent frostbite.
Choice D Reason: The nurse should not manipulate or move the fractured bone to align it with the normal anatomy unless there is no pulse distal to the injury. This action can cause more damage and complications, such as bleeding, infection, nerve injury, or compartment syndrome.
Choice E Reason: The nurse should immobilize the joints above and below the fracture site to prevent movement of the fractured bone and reduce pain and muscle spasm. The nurse should use a rigid material, such as a board, cardboard, or metal rod, to splint the injured part.
A client is brought to the emergency department after ingesting an unknown amount of acetaminophen tablets. What should the nurse say to obtain information about the poisoning?
Explanation
Choice A Reason: The nurse should ask how many tablets did the client take and when did they take them to determine the dose and time of ingestion of acetaminophen. This information can help estimate the risk of toxicity and guide treatment options.
Choice B Reason: The nurse should not ask why did the client take acetaminophen tablets as this question may imply judgment or blame and discourage honest communication. The nurse should focus on assessing and managing the poisoning rather than exploring its cause.
Choice C Reason: The nurse should ask about allergies or medical conditions that may affect treatment decisions, but this question is not specific to acetaminophen poisoning. The nurse should prioritize obtaining information about the poisoning first.
Choice D Reason: The nurse should ask about symptoms or discomfort that may indicate toxicity or complications of acetaminophen poisoning, such as nausea, vomiting, abdominal pain, jaundice, or confusion. However, this question is less important than knowing how much and when acetaminophen was ingested.
A client who has a severe peanut allergy is experiencing an anaphylactic reaction after eating a cookie that contained peanut butter. The nurse administers epinephrine to the client and monitors their vital signs. What should the nurse expect the client to say after receiving epinephrine?
Explanation
Choice A Reason: The nurse should not expect the client to say that they feel much better after receiving epinephrine, as this medication may not reverse the anaphylactic reaction completely or prevent its recurrence. The nurse should continue to monitor the client for signs of respiratory distress, hypotension, or shock.
Choice B Reason: The nurse should expect the client to say that they feel very shaky and nervous after receiving epinephrine, as this medication is a sympathomimetic agent that stimulates the adrenergic receptors and causes side effects such as tremors, anxiety, palpitations, tachycardia, and hypertension. The nurse should reassure the client that these effects are normal and temporary.
Choice C Reason: The nurse should not expect the client to say that they feel very sleepy and tired after receiving epinephrine, as this medication is a stimulant that increases alertness and energy. The nurse should assess the client for hypoxia, hypoglycemia, or cerebral edema if they report feeling drowsy or lethargic.
Choice D Reason: The nurse should not expect the client to say that they feel very thirsty and dry after receiving epinephrine, as this medication does not cause dehydration or fluid loss. The nurse should assess the client for other causes of thirst or dry mouth, such as diabetes mellitus, diabetes insipidus, or anticholinergic medications.
A nurse is performing CPR on a client who has no pulse and no breathing. The nurse attaches an AED to the client and follows the voice prompts. Which of the following actions should the nurse take when using an AED?
Explanation
Choice A Reason: The nurse should remove any clothing or jewelry from the chest area before attaching an AED to ensure good contact between the electrode pads and the skin. However, this action is not part of using an AED but rather preparing for its use.
Choice B Reason: The nurse should place one electrode pad on the upper right chest and one on the lower left chest when using an AED to deliver an electrical shock across the heart muscle and restore a normal rhythm. However, this action is not specific to using an AED but rather applying its electrode pads.
Choice C Reason: The nurse should press the shock button when instructed by the AED to deliver an electrical shock to the client if indicated by the device's analysis of the cardiac rhythm. This action is specific to using an AED and can be lifesaving for clients who have ventricular fibrillation or ventricular tachycardia.
Choice D Reason: The nurse should not continue chest compressions while the AED analyzes the rhythm or delivers a shock, as this can interfere with the device's function and accuracy. The nurse should stop chest compressions and ensure that no one is touching the client when prompted by the AED.
Conclusion
A nurse is teaching a group of students about the importance of first aid. Which of the following statements by the nurse is correct?
Explanation
First aid can help prevent further injury or damage to the victim
Choice A is incorrect because first aid can be performed by anyone who has the knowledge and skills to do so.
Choice C is incorrect because first aid is not a substitute for professional medical care, but a bridge to keep the victim alive and stable until help arrives.
Choice D is incorrect because first aid involves a systematic primary and secondary assessment approach to first identify and treat the most urgent problems.
A client is involved in a car accident and suffers multiple injuries. The nurse arrives at the scene and performs a primary assessment. Which of the following actions should the nurse do first? (Select all that apply)
Explanation
These are the steps of the primary assessment, which aims to identify and treat life-threatening conditions such as cardiac arrest, respiratory arrest, severe bleeding, or shock. Choice E is incorrect because controlling bleeding is part of the secondary assessment, which is done after the primary assessment.
A nurse is caring for a victim who has a deep wound on his leg. The nurse applies direct pressure and elevates the wound to control bleeding. The victim says, "I'm feeling dizzy and cold." What should the nurse do next?
Explanation
Check for signs of shock. Shock is a life-threatening condition that occurs when there is inadequate blood flow to vital organs. It can result from severe bleeding, dehydration, infection, or trauma. The symptoms of shock include dizziness, cold and clammy skin, rapid and weak pulse, shallow breathing, nausea, and confusion.
Choice A is incorrect because a tourniquet should only be used as a last resort when other methods of controlling bleeding fail or are not possible.
Choice B is incorrect because covering the wound with a sterile dressing is done after bleeding is controlled and does not address the victim's symptoms.
Choice C is incorrect because giving water to a victim who may have internal bleeding or abdominal injuries can worsen their condition.
A nurse is performing CPR on a victim who has no pulse and no breathing. The nurse notices that an automated external defibrillator (AED) is available nearby. What should the nurse do?
Explanation
The correct answer is C. Use the AED after completing five cycles of CPR. An AED is a device that can deliver an electric shock to restore a normal heart rhythm in victims of cardiac arrest. It should be used as soon as possible, but not at the expense of interrupting chest compressions for too long. The recommended sequence is to perform five cycles of CPR (30 compressions and two breaths), then use the AED, then resume CPR until the AED advises another shock or until help arrives. Choice A is incorrect because stopping CPR for more than 10 seconds can reduce the chances of survival. Choice B is incorrect because waiting for another rescuer to use the AED can delay defibrillation and reduce its effectiveness. Choice D is incorrect because alternating between CPR and AED every two minutes can disrupt the rhythm of chest compressions and decrease blood flow to vital organs.
A nurse is caring for a victim who has a minor burn on his arm caused by hot water. The nurse knows that first aid for burns includes which of the following actions?
Explanation
Remove any clothing or jewelry from the burn area. This can help prevent further damage or infection by reducing contact with heat sources or irritants.
Choice A is incorrect because applying ice or cold water to a burn can cause more tissue damage or hypothermia.
Choice C is incorrect because applying butter or oil to a burn can trap heat and increase inflammation and infection.
Choice D is incorrect because covering the burn area with cotton or wool can stick to the wound and cause pain and infection.
Summary
A nurse is teaching a first aid class to a group of high school students. The nurse asks one of the students to demonstrate how to perform abdominal thrusts (Heimlich maneuver) on a choking victim. Which of the following actions by the student indicates a need for further instruction?
Explanation
Choice A Reason: This action is correct because it positions the student behind the victim and allows him to perform abdominal thrusts.
Choice B Reason: This action is correct because it places the fist above the navel and below the xiphoid process, where the thrusts can dislodge the object.
Choice C Reason: This action is correct because it pulls the fist inward and upward, creating a strong pressure in the abdomen that can expel the object.
Choice D Reason: This action is incorrect because it does not recognize the need to change the intervention if the victim becomes unconscious. The student repeats the thrusts until the object is expelled or the victim becomes unconscious. This action indicates a need for further instruction because if the victim becomes unconscious, the student should lower them to the ground, call 911, and start CPR.
A nurse is providing first aid to a client who has a puncture wound on his foot from stepping on a nail. The nurse cleans the wound with soap and water and applies a sterile dressing. The nurse should also advise the client to:
Explanation
Choice A Reason: This advice is not specific to a puncture wound. Taking ibuprofen for pain relief may be helpful, but it is not a priority intervention.
Choice B Reason: This advice is incorrect because soaking the foot in warm water can increase the risk of infection and delay healing.
Choice C Reason: This advice is correct because getting a tetanus booster shot if needed can prevent tetanus, a serious bacterial infection that affects the nervous system.
Choice D Reason: This advice is incorrect because avoiding wearing shoes until the wound heals can expose the wound to dirt and bacteria and cause more complications.
A nurse is providing first aid to a client who has a nosebleed. The nurse should instruct the client to:
Explanation
Choice A Reason: This action is incorrect because tilting the head back can cause blood to go down the throat and increase the risk of choking or vomiting.
Choice B Reason: This action is correct because tilting the head forward and pinching the nostrils together helps to stop the bleeding and prevent blood from going down the throat.
Choice C Reason: This action is incorrect because blowing the nose forcefully can dislodge any clots and worsen the bleeding, and applying ice to the bridge of the nose may not be effective.
Choice D Reason: This action is incorrect because breathing through the mouth can dry out the nasal passages and delay healing, and applying pressure to the upper lip may not be effective.
A nurse is providing first aid to a client who has a sprained ankle. The nurse should apply which of the following interventions?
Explanation
Choice A Reason: This choice is correct because rest, ice, compression, and elevation (RICE) helps to reduce swelling, pain, and inflammation of a sprained ankle.
Choice B Reason: This choice is incorrect because heat, massage, exercise, and immobilization (HMEI) can increase swelling, pain, and inflammation of a sprained ankle.
Choice C Reason: This choice is incorrect because flexion, extension, rotation, and stabilization (FERS) can cause further damage to a sprained ankle.
Choice D Reason: This choice is incorrect because traction, reduction, splinting, and alignment (TRSA) are not indicated for a sprained ankle.
A nurse is providing first aid to a client who has been bitten by a dog. The nurse should take which of the following actions? (Select all that apply.)
Explanation
Choice A Reason: This choice is correct because washing the wound with soap and water helps to remove dirt and bacteria and prevent infection.
Choice B Reason: This choice is incorrect because applying an antibiotic ointment to the wound may not be necessary or effective for a dog bite wound.
Choice C Reason: This choice is correct because covering the wound with a sterile dressing helps to protect it from further contamination and injury.
Choice D Reason: This choice is correct because reporting the incident to the local health department helps to track and prevent rabies transmission.
Choice E Reason: This choice is incorrect because administering rabies vaccine to the client may not be indicated or available for a dog bite wound.
A nurse is providing first aid to a client who has a head injury from falling off a ladder. The nurse should monitor the client for signs of increased intracranial pressure (ICP), such as:
Explanation
Choice A Reason: This choice is correct because headache is caused by pressure on pain-sensitive structures in the brain.
Choice B Reason: This choice is correct because dilated pupils are caused by pressure on cranial nerves that control eye movement and pupil size.
Choice C Reason: This choice is correct because slurred speech is caused by pressure on areas of the brain that control language and speech.
Choice D Reason: This choice is correct because it includes all of the signs of increased intracranial pressure (ICP) as described in the text.
A nurse is providing first aid to a client who has a sprained ankle from playing soccer. The nurse should apply which of the following interventions?
Explanation
Choice A Reason: This choice is correct because rest, ice, compression, and elevation (RICE) helps to reduce swelling, pain, and inflammation of a sprained ankle.
Choice B Reason: This choice is incorrect because heat, massage, exercise, and immobilization (HMEI) can increase swelling, pain, and inflammation of a sprained ankle.
Choice C Reason: This choice is incorrect because flexion, extension, rotation, and stabilization (FERS) can cause further damage to a sprained ankle.
Choice D Reason: This choice is incorrect because traction, reduction, splinting, and alignment (TRSA) are not indicated for a sprained ankle.
A nurse is providing first aid to a client who has been stung by a bee and has a history of severe allergic reactions. The nurse should monitor the client for signs of anaphylaxis, such as: (Select all that apply.)
Explanation
Choice A Reason: This choice is correct because difficulty breathing is caused by swelling of the airways or bronchospasm that restricts airflow.
Choice B Reason: This choice is correct because swelling of face, lips, tongue, or throat is caused by fluid accumulation in the tissues that can block the airway.
Choice C Reason: This choice is correct because hives or itching are caused by histamine release that triggers an inflammatory response in the skin.
Choice D Reason: This choice is correct because nausea or vomiting are caused by histamine release that affects the gastrointestinal tract.
Choice E Reason: This choice is correct because dizziness or fainting are caused by low blood pressure or reduced blood flow to the brain.
A nurse is using an AED on a child who has ventricular fibrillation. The nurse should use which of the following types of AED pads?
Explanation
Choice A Reason: This choice is incorrect because adult pads are too large for a child's chest and may deliver too much electricity, which can damage the heart.
Choice B Reason: This choice is correct because child pads are specially designed for children between 1 and 8 years old and deliver a lower dose of electricity than adult pads.
Choice C Reason: This choice is incorrect because infant pads are too small for a child's chest and may not deliver enough electricity, which can fail to restart the heart.
Choice D Reason: This choice is incorrect because using any pads may not be appropriate or effective for a child's chest size and heart condition.
A nurse is providing CPR to an infant who has no pulse and is not breathing. The nurse should give two breaths by:
Explanation
Choice A Reason: This choice is incorrect because pinching the nose shut may obstruct the airway or cause air leakage.
Choice B Reason: This choice is correct because opening the mouth and sealing the mouth over both mouth and nose allows the nurse to deliver adequate ventilation to an infant's small airway.
Choice C Reason: This choice is incorrect because opening both mouth and nose may cause air leakage or reduce the pressure of ventilation.
Choice D Reason: This choice is incorrect because pinching both mouth and nose shut may obstruct the airway or cause trauma to the tissues.
A nurse is caring for a client who has an abdominal stab wound. The nurse notes that there is bright red blood spurting from the wound site. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A Reason: Applying direct pressure over the wound site with a sterile gauze pad can help control the bleeding by compressing the blood vessels. This is an appropriate action for arterial bleeding, which is bright red and spurts from a wound.
Choice B Reason: Elevating the client's legs above the level of the heart can help increase venous return and cardiac output, but it is not recommended for abdominal injuries, as it can increase intra-abdominal pressure and worsen bleeding or organ damage.
Choice C Reason: Applying ice packs around the wound site can help reduce inflammation and pain, but it is not recommended for bleeding wounds, as it can cause vasoconstriction and impair blood flow to the injured area.
Choice D Reason: Covering the wound site with an occlusive dressing can help prevent air from entering the abdominal cavity and causing a pneumoperitoneum, which can impair breathing and circulation. This is an appropriate action for penetrating wounds, such as stab wounds.
Choice E Reason: Checking the client's distal pulses frequently can help monitor the perfusion of the extremities and detect signs of shock or compartment syndrome. Shock is a condition in which there is inadequate tissue perfusion due to blood loss or other causes. Compartment syndrome is a condition in which there is increased pressure within a muscle compartment due to swelling or bleeding, which can compromise blood flow and nerve function.
A nurse is caring for a client who has a pressure ulcer on the sacrum. The nurse observes that the wound has yellow slough, red granulation tissue, and black eschar. The nurse should use which of the following types of dressings to debride the wound?
Explanation
Choice A Reason: Hydrogel dressings are water-based gels that provide moisture and hydration to the wound bed. They are suitable for wounds that are dry and have minimal drainage, such as partial-thickness burns or radiation injuries.
Choice B Reason: Foam dressings are soft, absorbent pads that provide cushioning and insulation to the wound bed. They are suitable for wounds that have moderate to heavy drainage, such as venous ulcers or surgical wounds.
Choice C Reason: Alginate dressings are fiber-based dressings that form a gel when in contact with wound exudate. They are suitable for wounds that have heavy drainage or bleeding, such as diabetic ulcers or arterial ulcers.
Choice D Reason: Enzymatic dressings are topical agents that contain enzymes that break down necrotic tissue and slough in the wound bed. They are suitable for wounds that have mixed necrotic and viable tissue, such as pressure ulcers with yellow slough, red granulation tissue, and black eschar.
A nurse is caring for a client who has a surgical wound on the abdomen. The nurse notes that the wound edges are separated and there is pink, shiny tissue protruding from the wound. The nurse should document this finding as which of the following types of wound dehiscence?
Explanation
Choice A Reason: Partial-thickness wound dehiscence is a type of wound dehiscence in which the wound edges separate but only involve the epidermis and dermis layers of the skin. The wound bed is usually moist and red, but there is no organ protrusion.
Choice B Reason: Full-thickness wound dehiscence is a type of wound dehiscence in which the wound edges separate and involve all layers of the skin and underlying tissues. The wound bed may have granulation tissue or necrotic tissue, but there is no organ protrusion.
Choice C Reason: Evisceration is a type of wound dehiscence in which the wound edges separate and the visceral organs protrude from the wound. This is a medical emergency that requires immediate intervention to prevent organ damage and infection.
Choice D Reason: Infection is not a type of wound dehiscence, but it can be a cause or a complication of wound dehiscence. Signs of infection include fever, pain, swelling, redness, warmth, pus, or foul odor.
Exams on Introduction
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define first aid and its purposes
- Describe the legal and ethical aspects of providing first aid
- Explain the steps of primary and secondary assessment in an emergency situation
- Identify the signs and symptoms of life-threatening conditions and the appropriate first aid interventions
- Demonstrate the skills of cardiopulmonary resuscitation (CPR) and automated external defibrillator (AED) use
- Discuss the principles of wound care and bleeding control
Introduction
First aid is the immediate, temporary assistance given to a person who is injured or has become ill. It includes:
- Assessing the victim for life-threatening conditions
- Performing appropriate interventions to sustain life
- Keeping the person in the best possible condition until the assistance of EMS is obtained
First aid can save lives, prevent complications, and reduce pain and suffering. It is an essential skill for nurses and other health professionals, as well as for the general public.

Legal and Ethical Aspects of First Aid
When providing first aid, it is important to be aware of the legal and ethical implications of your actions. Some of the key points are:
- Good Samaritan laws: These are enacted in most states to protect health professionals from legal liability when providing emergency first aid. They require that you follow a reasonable and prudent course of action, that you obtain verbal consent from the victim if possible, and that you do not abandon the victim until someone with comparable or better training takes over.
- Consent: The victim must give verbal permission for you to provide first aid. If the victim is unconscious, the law assumes that they would give consent if they were able. If the victim is a minor, you should obtain consent from a parent or guardian if possible. If not, you can provide first aid based on implied consent.
- Refusal: The victim has the right to refuse first aid or any part of it. You should respect their wishes and document their refusal. You should also inform them of the possible consequences of refusing care.
- Confidentiality: You should respect the privacy of the victim and not disclose any personal or medical information to anyone who is not involved in their care.
- Documentation: You should record your actions and observations in a clear and accurate manner. You should include the date, time, location, victim’s name, consent, assessment findings, interventions, outcomes, and any referrals or follow-up.
You should include the date, time, location, victim's name, consent, assessment findings, interventions, outcomes, and any referrals or follow-up.
Primary and Secondary Assessment
When you encounter an emergency situation, you should follow these steps:
1. Check for safety: Make sure the scene is safe for you and the victim. Remove any hazards or move to a safer location if possible.
2. Call for help: Call 911 or activate EMS as soon as possible. Give them your location, number of victims, nature of injury or illness, and any other relevant information.
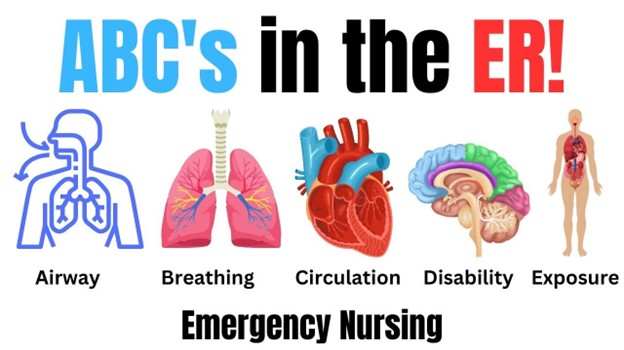
3. Care for life-threatening conditions: Perform a primary assessment to identify and treat any conditions that threaten the victim’s airway, breathing, or circulation (ABCs). These include:
- Airway obstruction: Check if the victim is choking or has anything blocking their airway. If so, perform abdominal thrusts (Heimlich maneuver) or chest thrusts to dislodge the object.
- Breathing arrest: Check if the victim is breathing by looking, listening, and feeling for signs of breathing. If not, perform rescue breathing by giving two breaths every five seconds for an adult or one breath every three seconds for a child or infant.
- Circulatory arrest: Check if the victim has a pulse by feeling for a carotid pulse in an adult or a brachial pulse in a child or infant. If not, perform chest compressions by pushing hard and fast on the center of the chest at a rate of 100 to 120 compressions per minute for all ages.
- Severe bleeding: Check if the victim has any bleeding that is spurting, soaking through dressings, or endangering their life. If so, apply direct pressure to the wound with a clean cloth or bandage. If possible, elevate the injured part above the level of the heart. If bleeding does not stop, apply pressure to a pressure point near the wound or use a tourniquet as a last resort.
4. Provide additional care: Perform a secondary assessment to identify and treat any other injuries or illnesses that are not immediately life-threatening. These include:
- Head injury: Check if the victim has any signs of skull fracture, such as deformity, swelling, bruising, bleeding, or cerebrospinal fluid leakage from the ears or nose. If so, do not move their head or neck unless necessary. Apply a sterile dressing to any open wounds and monitor their level of consciousness.
- Spinal injury: Check if the victim has any signs of spinal cord damage, such as numbness, tingling, weakness, paralysis, or loss of bladder or bowel control. If so, do not move their head or neck unless necessary. Stabilize their head and neck with your hands or a rigid object and monitor their breathing and circulation.
- Fracture: Check if the victim has any signs of broken bones, such as deformity, swelling, bruising, pain, or inability to move the affected part. If so, do not move the injured part unless necessary. Splint the fracture with a rigid object and padding and elevate the injured part if possible. Apply ice to reduce swelling and pain.
- Dislocation: Check if the victim has any signs of joint displacement, such as deformity, swelling, bruising, pain, or inability to move the affected part. If so, do not move the injured part unless necessary. Splint the dislocation in the position found and apply ice to reduce swelling and pain.
- Sprain: Check if the victim has any signs of ligament injury, such as swelling, bruising, pain, or difficulty moving the affected part. If so, apply the RICE method: Rest the injured part, Ice it for 20 minutes every hour, Compress it with an elastic bandage, and Elevate it above the level of the heart.
- Wound: Check if the victim has any cuts, scrapes, punctures, or burns on their skin. If so, clean the wound with soap and water or saline solution and cover it with a sterile dressing. Change the dressing as needed and watch for signs of infection, such as redness, warmth, pus, or fever.
- Burn: Check if the victim has any damage to their skin caused by heat, chemicals, electricity, or radiation. If so, classify the burn according to its depth:
- First-degree burn: Affects only the outer layer of skin (epidermis). Causes redness, pain, and mild swelling. Treat by cooling the burn with water or a cold compress for 10 to 15 minutes and applying aloe vera gel or antibiotic ointment.
- Second-degree burn: Affects both the outer and inner layer of skin (dermis). Causes blisters, severe pain, and moderate swelling. Treat by cooling the burn with water or a cold compress for 10 to 15 minutes and covering it with a sterile dressing. Do not break the blisters or apply ointment.
- Third-degree burn: Affects all layers of skin and may damage underlying tissues. Causes charred, white, or black skin that is dry and painless. Treat by covering the burn with a sterile dressing and seeking immediate medical attention. Do not cool the burn or remove any clothing that is stuck to it.
- Poisoning: Check if the victim has ingested, inhaled, absorbed, or injected any substance that is harmful to their body. If so,
- Call poison control center at 1-800-222-1222 for advice
- Follow their instructions on whether to induce vomiting or not
- Provide supportive care such as fluids, oxygen, or antidotes
- Monitor their vital signs and level of consciousness
- Allergic reaction: Check if the victim has any signs of hypersensitivity to a substance they have been exposed to. If so,
- Remove the source of allergen if possible
- Give them antihistamines or epinephrine if they have them
- Monitor their breathing and circulation
- Seek immediate medical attention if they have signs of anaphylaxis
- Anaphylaxis: A severe allergic reaction that can cause shock and death. Signs include:
- Difficulty breathing
- Swelling of face, lips, tongue, or throat
- Hives or itching
- Nausea or vomiting
- Dizziness or fainting
- Rapid pulse or low blood pressure
Cardiopulmonary Resuscitation (CPR) and Automated External Defibrillator (AED)
CPR is a basic emergency procedure for life support that consists of chest compressions and rescue breaths. It is performed when a person’s heart stops beating or when they are not breathing normally.
AED is a device that delivers an electric shock to the heart to restore its normal rhythm. It is used when a person’s heart stops beating due to ventricular fibrillation (VF) or ventricular tachycardia (VT).
The steps for performing CPR and using AED are:
- Check for responsiveness: Tap the person’s shoulder and shout “Are you OK?” If they do not respond,
- Call for help: Call 911 or activate EMS and get an AED if available
- Open the airway: Tilt their head back and lift their chin up
- Check for breathing: Look, listen, and feel for signs of breathing for no more than 10 seconds. If they are not breathing normally,
- Give two breaths: Pinch their nose shut and seal your mouth over theirs. Blow into their mouth for one second and watch their chest rise. Give another breath and let their chest fall.
- Check for pulse: Feel for a carotid pulse in an adult or a brachial pulse in a child or infant for no more than 10 seconds. If they have no pulse or you are not sure,
- Start chest compressions: Place the heel of one hand on the center of their chest and the other hand on top. Push hard and fast at a rate of 100 to 120 compressions per minute and a depth of at least 2 inches for an adult, 2 inches for a child, or 1.5 inches for an infant. Allow the chest to recoil fully after each compression.
- Continue CPR: Follow the ratio of 30 compressions to 2 breaths for all ages. If you are alone, perform five cycles of CPR (about two minutes) before leaving to get help or an AED. If you have an AED, use it as soon as possible.
- Use AED: Turn on the AED and follow the voice prompts. Attach the pads to the person’s bare chest as shown on the diagram. Make sure no one is touching the person and say “Clear!” Press the analyze button and let the AED check the person’s heart rhythm. If the AED advises a shock, make sure no one is touching the person and say “Clear!” Press the shock button and deliver the shock. If the AED does not advise a shock, resume CPR immediately.
- Repeat until help arrives: Continue CPR and use AED until the person shows signs of life, such as breathing, coughing, or moving; trained medical personnel take over; you are too exhausted to continue; or the scene becomes unsafe.
Wound Care and Bleeding Control
A wound is any break in the skin or underlying tissues caused by trauma or disease. Wounds can be classified according to their cause, depth, appearance, or infection status.
Bleeding is the loss of blood from blood vessels due to injury or disease. Bleeding can be classified according to its source, rate, or appearance.
The principles of wound care and bleeding control are:
- Stop the bleeding: Apply direct pressure to the wound with a clean cloth or bandage. If possible, elevate the injured part above the level of the heart. If bleeding does not stop, apply pressure to a pressure point near the wound or use a tourniquet as a last resort.
- Clean the wound: Wash the wound with soap and water or saline solution to remove any dirt or debris. Do not use alcohol, hydrogen peroxide, or iodine as they can damage healthy tissue and delay healing.
- Dress the wound: Cover the wound with a sterile dressing to protect it from infection and further injury. Change the dressing as needed and watch for signs of infection, such as redness, warmth, pus, or fever.
- Seek medical attention: Depending on the severity of the wound, you may need to seek medical attention for stitches, antibiotics, tetanus shot, or other treatments.

Nursing Interventions on First Aid
Some of the nursing interventions on first aid are:
- Assess the victim’s condition and prioritize the most urgent problems
- Call for help and activate the emergency medical services (EMS) if needed
- Provide basic life support (BLS) by performing cardiopulmonary resuscitation (CPR) and using automated external defibrillator (AED) if indicated
- Control bleeding by applying direct pressure, elevation, pressure points, or tourniquet
- Clean and dress wounds to prevent infection and further injury
- Stabilize fractures, dislocations, and sprains by splinting, immobilizing, and elevating the injured part
- Manage head and spinal injuries by maintaining a patent airway, monitoring level of consciousness, and preventing movement of the head and neck
- Treat burns by cooling, covering, and elevating the affected area
- Manage poisoning by identifying the source, calling poison control center, and providing supportive care
- Manage allergic reactions by removing the allergen, administering antihistamines or epinephrine, and monitoring breathing and circulation
- Monitor vital signs and level of consciousness until help arrives or the victim recovers
- Document the first aid given and the outcome of the intervention

Conclusion
- First aid is a crucial skill that can make a difference between life and death, recovery and disability, or comfort and pain in emergency situations
- First aid requires knowledge, skills, judgment, and confidence to assess and care for the victim in a safe, legal, and ethical manner
- First aid involves a systematic approach of primary and secondary assessment to identify and treat the most urgent problems first
- First aid includes performing CPR and using AED when the victim’s heart stops beating or when they are not breathing normally
- First aid also includes controlling bleeding and caring for wounds to prevent infection, shock, and further damage
- First aid is not a substitute for professional medical care, but a bridge to keep the victim alive and stable until help arrives
Summary
- First aid is the immediate, temporary assistance given to a person who is injured or has become ill
- Legal and ethical aspects of first aid include Good Samaritan laws, consent, refusal, confidentiality, and documentation
- Primary assessment involves checking for life-threatening conditions such as airway obstruction, breathing arrest, circulatory arrest, and severe bleeding
- Secondary assessment involves checking for other injuries or illnesses such as head injury, spinal injury, fracture, dislocation, sprain, wound, burn, poisoning, allergic reaction, or anaphylaxis
- CPR is a basic emergency procedure for life support that consists of chest compressions and rescue breaths
- AED is a device that delivers an electric shock to the heart to restore its normal rhythm
- Wound care and bleeding control involve stopping the bleeding, cleaning the wound, dressing the wound, and seeking medical attention
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Introduction
This filled cannot be empty

