Please set your exam date
Pathophysiology of the Gastrointestinal System
Study Questions
Gastroenteritis
Explanation
A) Correct. Gastroenteritis is most commonly caused by viral infections, such as norovirus or rotavirus.
B) Incorrect. While bacterial infections can cause gastroenteritis, they are not the sole cause.
C) Incorrect. Parasitic infections are less common causes of gastroenteritis compared to viral and bacterial infections.
D) Incorrect. Fungal infections are rare causes of gastroenteritis and are not considered primary pathogens.
Explanation
A) Correct. Adequate fluid intake is crucial in managing gastroenteritis to prevent dehydration.
B) Incorrect. Spicy foods can exacerbate gastrointestinal symptoms and should be avoided.
C) Incorrect. Dairy products can aggravate symptoms of gastroenteritis, so it's recommended to avoid them until recovery.
D) Incorrect. Bland, easily digestible foods are recommended for individuals with gastroenteritis to help minimize irritation to the gastrointestinal tract.
Explanation
A) Incorrect. Antidiarrheal medications can be considered but are not the first-line treatment for severe cases of gastroenteritis.
B) Correct. Rehydration is the primary intervention for clients with severe abdominal pain and signs of dehydration due to gastroenteritis.
C) Incorrect. Increasing fiber intake is not recommended in the acute phase of gastroenteritis, as it may exacerbate symptoms.
D) Incorrect. Fasting is not recommended in gastroenteritis; rehydration and appropriate nutrition are crucial.
Explanation
A) Incorrect. Mild abdominal cramping and bloating are common symptoms of gastroenteritis and may not require immediate intervention.
B) Incorrect. While absence of bowel movements for 24 hours is concerning, it may not be an immediate emergency compared to other options.
C) Correct. The presence of blood in stool or dark, tarry stools indicates potential gastrointestinal bleeding, which requires immediate attention.
D) Incorrect. Nausea and occasional vomiting are common symptoms of gastroenteritis and may not be an immediate concern.
Explanation
A) Incorrect. Viral gastroenteritis primarily affects the small intestine, not the large intestine.
B) Incorrect. Viral gastroenteritis is caused by viruses, not bacterial toxins.
C) Correct. Viral gastroenteritis leads to inflammation of the stomach and small intestine linings.
D) Incorrect. Blood in the stool is not a typical symptom of viral gastroenteritis; it is more commonly seen in certain bacterial infections.
Explanation
A) Correct. Many bacteria that cause gastroenteritis release toxins that directly damage the gastrointestinal lining.
B) Incorrect. While invasion of cells can occur with certain bacteria, it is not the primary mechanism of action for all bacterial gastroenteritis.
C) Incorrect. While inflammation is a common response to bacterial infection, it may not be the primary mechanism of all cases of bacterial gastroenteritis.
D) Incorrect. Disruption of normal gut flora is more commonly associated with certain types of antibiotics rather than the direct mechanism of bacteria causing gastroenteritis.
Explanation
A) Correct. Parasitic gastroenteritis is commonly transmitted through consumption of contaminated food and water.
B) Incorrect. Respiratory droplets are not the primary mode of transmission for parasitic gastroenteritis.
C) Incorrect. Direct contact with infected individuals may transmit some infections, but it is not the primary mode of transmission for parasitic gastroenteritis.
D) Incorrect. Insect vectors are more commonly associated with the transmission of certain diseases, such as malaria, rather than parasitic gastroenteritis.
Explanation
A) Incorrect. Electrolytes are primarily absorbed in the small intestine, not the large intestine.
B) Correct. Gastroenteritis can lead to electrolyte imbalances, especially when there is excessive vomiting and diarrhea, as these processes result in the loss of important electrolytes.
C) Incorrect. Gastroenteritis can lead to electrolyte imbalances, so electrolyte levels may not remain stable in affected individuals.
D) Incorrect. Electrolytes play a crucial role in various physiological processes, and their imbalance is a significant aspect of the pathophysiology of gastroenteritis.
A nurse is explaining the inflammatory response in the context of gastroenteritis. What statement by the nurse is accurate?
Explanation
A) Incorrect. While antibodies play a role in the immune response, they are not the primary mediators of inflammation in gastroenteritis.
B) Correct. Inflammation in gastroenteritis is a protective response against invading pathogens and helps to clear the infection.
C) Incorrect. Inflammation in gastroenteritis can occur in both the stomach and the small intestine, not just the large intestine.
D) Incorrect. Inflammatory cells, such as white blood cells, play a significant role in the inflammatory response in gastroenteritis. They are responsible for targeting and destroying pathogens.
Explanation
A) Correct. Headache can be a symptom of dehydration, which is a common complication of gastroenteritis due to fluid loss through diarrhea and vomiting.
B) Incorrect. Muscle weakness is not a typical symptom of gastroenteritis.
C) Incorrect. Visual disturbances are not typically associated with gastroenteritis.
D) Incorrect. Chest pain is not a common symptom of gastroenteritis.
Explanation
A) Correct. Skin turgor and mucous membranes are important indicators of hydration status, which is a critical concern in clients with gastroenteritis.
B) Incorrect. While blood pressure and heart rate are important vital signs, they may not provide immediate information about the client's hydration status.
C) Incorrect. Urinary output and specific gravity are important indicators of renal function, but they may not provide immediate information about the client's hydration status.
D) Incorrect. Respiratory rate and lung sounds are important assessments, but they may not provide immediate information about the client's hydration status.
Explanation
A) Incorrect. Reintroducing regular foods should be done cautiously and not solely based on the client's desire.
B) Correct. It is important to wait until diarrhea has completely stopped to ensure the client's digestive system has had time to recover.
C) Incorrect. While it is important for symptoms like nausea and abdominal pain to have resolved, focusing on the cessation of diarrhea is particularly crucial.
D) Incorrect. Reintroducing regular foods should be done cautiously and not solely based on the client's tolerance.
Explanation
A) Correct. Dry lips and a sunken fontanelle are signs of severe dehydration in an infant and require immediate attention.
B) Incorrect. While decreased urine output is a concern, it may not necessitate immediate reporting if it is only slightly decreased.
C) Incorrect. Mild irritability during feedings is a symptom of discomfort but may not necessitate immediate reporting.
D) Incorrect. Occasional vomiting after feeds is a common symptom of gastroenteritis and may not necessitate immediate reporting.
Explanation
A) Correct. This advice encourages the client to monitor their temperature and take appropriate action if it rises significantly.
B) Incorrect. While a fever is expected with gastroenteritis, it can still be managed to improve the client's comfort.
C) Incorrect. Ibuprofen may not be the best choice for everyone, and it's important to specify a temperature threshold for intervention.
D) Incorrect. A fever of 100°F (37.8°C) is not a critical threshold that would necessitate an immediate visit to the emergency room.
Explanation
A) Correct. Severe bacterial gastroenteritis can lead to significant fluid and electrolyte imbalances, including hypokalemia, which can be life-threatening.
B) Incorrect. Hypertension is not a typical complication of gastroenteritis.
C) Incorrect. Hypernatremia, or high sodium levels, is not a common complication of gastroenteritis.
D) Incorrect. Hyperglycemia, or high blood sugar levels, is not a typical complication of gastroenteritis.
Explanation
A) Incorrect. While viral gastroenteritis can lead to complications, chronic kidney disease is not a typical outcome.
B) Correct. One potential complication of viral gastroenteritis is the development of electrolyte imbalances, such as low potassium levels, due to excessive vomiting and diarrhea.
C) Incorrect. Permanent changes in vision are not associated with viral gastroenteritis.
D) Incorrect. While complications are not extremely common, they can occur, especially in severe cases.
Explanation
A) Correct. Dehydration is a significant concern in elderly individuals with gastroenteritis due to their reduced reserve and increased vulnerability to fluid and electrolyte imbalances.
B) Incorrect. Hyperactivity is not a typical complication of gastroenteritis, especially in the elderly population.
C) Incorrect. Hypothermia is not a typical complication of gastroenteritis, especially in the absence of other underlying conditions.
D) Incorrect. Hypertension is not a typical complication of gastroenteritis.
Explanation
A) Incorrect. While gastroenteritis can lead to complications, permanent damage to the liver and kidneys is not a typical long-term effect.
B) Correct. One possible long-term effect of gastroenteritis is the development of irritable bowel syndrome (IBS), which can lead to chronic gastrointestinal symptoms.
C) Incorrect. Chronic fatigue may occur during the acute phase of gastroenteritis, but it is not a typical long-term effect.
D) Incorrect. While long-term effects are not extremely common, they can occur, especially in cases of severe or prolonged gastroenteritis.
Explanation
A) Correct. Severe viral gastroenteritis can lead to malnutrition due to the inability to absorb nutrients properly during the acute phase.
B) Incorrect. Hypernatremia, or high sodium levels, is not a common complication of gastroenteritis.
C) Incorrect. Hypotension, or low blood pressure, may occur in severe cases, but it is not a typical complication during recovery.
D) Incorrect. Urinary retention is not a typical complication of gastroenteritis.
Explanation
A) Incorrect. Avoiding fluids can lead to dehydration. It's important to maintain hydration, especially in cases of gastroenteritis.
B) Correct. Clear fluids like water, broth, and oral rehydration solutions help replace lost fluids and electrolytes, preventing dehydration.
C) Incorrect. Caffeinated beverages can lead to further dehydration due to their diuretic effect, so they should be avoided.
D) Incorrect. Fruit juices and carbonated beverages can exacerbate gastrointestinal symptoms and are not recommended during the acute phase of gastroenteritis.
Explanation
A) Incorrect. Spicy and greasy foods can exacerbate gastrointestinal symptoms and should be avoided during the recovery phase of gastroenteritis.
B) Correct. Dairy products can be hard to digest for some individuals with gastroenteritis, so it's recommended to avoid them until symptoms completely resolve.
C) Incorrect. While fiber is important for a balanced diet, increasing fiber intake may exacerbate symptoms in the acute phase of gastroenteritis.
D) Incorrect. Large amounts of fatty foods can be difficult to digest and may worsen gastrointestinal symptoms, so they should be avoided during recovery.
Explanation
A) Incorrect. While antidiarrheal medications can provide relief, they should be used with caution as they can potentially prolong the infection by preventing the body from expelling the infectious agent.
B) Correct. It's generally recommended to avoid using antidiarrheal medications in cases of infectious gastroenteritis, as they can impede the body's natural defense mechanism of expelling the infectious agent through diarrhea.
C) Incorrect. Antidiarrheal medications may be prescribed by a healthcare provider in specific cases, but they are not recommended as a first-line treatment for infectious gastroenteritis.
D) Incorrect. Antidiarrheal medications can be used in both children and adults, but they should be used with caution and under the guidance of a healthcare provider.
Explanation
A) Correct. Severe bacterial gastroenteritis may require treatment with antibiotics to target the specific bacterial infection.
B) Incorrect. While fluid replacement is important, administering the appropriate antibiotic is the priority for severe bacterial gastroenteritis.
C) Incorrect. In severe cases, a clear liquid diet may be recommended initially to allow the digestive system to rest and recover.
D) Incorrect. While rest is important, administering the appropriate antibiotic is crucial in cases of severe bacterial gastroenteritis.
Explanation
A) Incorrect. Being symptom-free for only 24 hours may not be sufficient to ensure full recovery from gastroenteritis.
B) Correct. It is important to wait until all symptoms, including diarrhea, vomiting, and abdominal pain, have completely resolved before returning to work to prevent the spread of infection.
C) Incorrect. Returning to work when only feeling slightly better may risk spreading the infection to others.
D) Incorrect. 48 hours of symptom improvement may not be sufficient to ensure full recovery from gastroenteritis. It is important to wait until all symptoms have completely resolved.
Explanation
A) Incorrect. Avoiding hand hygiene is not an effective way to prevent gastroenteritis; in fact, it increases the risk of infection.
B) Correct. Proper hand hygiene, including washing hands frequently, especially before handling food, is a key measure in preventing the spread of gastroenteritis.
C) Incorrect. Consuming undercooked meats and unpasteurized dairy products can actually increase the risk of gastroenteritis due to potential bacterial contamination.
D) Incorrect. Sharing personal items can increase the risk of spreading gastroenteritis, as the virus or bacteria can be easily transmitted through shared items.
Explanation
A) Incorrect. Limiting hand hygiene is not a recommended practice; in fact, it increases the risk of infection.
B) Incorrect. While vaccinations are important for overall health, there is no specific vaccine for all types of gastroenteritis.
C) Incorrect. Encouraging children to share personal items can increase the risk of spreading gastroenteritis.
D) Correct. Practicing good hand hygiene and proper food handling are essential measures to prevent the spread of gastroenteritis, especially in young children who may be more susceptible to infections.
Explanation
A) Incorrect. Well water can become contaminated, especially during outbreaks, and is not inherently immune to contamination.
B) Correct. Boiling well water for at least one minute can help kill harmful microorganisms, making it safer to use during a gastroenteritis outbreak.
C) Incorrect. It is important to take precautions with well water during a gastroenteritis outbreak, as it can be a potential source of contamination.
D) Incorrect. Using well water directly from the source without any treatment can pose a risk of gastroenteritis if the water is contaminated.
Explanation
A) Incorrect. Avoiding hand hygiene is not an effective way to prevent gastroenteritis; in fact, it increases the risk of infection.
B) Incorrect. Sharing personal items can increase the risk of spreading gastroenteritis, as the virus or bacteria can be easily transmitted through shared items.
C) Incorrect. While alcohol-based hand sanitizers can be used in the absence of soap and water, they are not as effective as proper handwashing.
D) Correct. Proper hand hygiene, especially after using the restroom, is crucial in preventing the spread of gastroenteritis, as it reduces the risk of contaminating hands with potentially infectious agents.
A client recovering from gastroenteritis asks the nurse about when it is safe to resume normal activities. What is the nurse's best response?
Explanation
A) Incorrect. Resuming normal activities when only feeling slightly better may risk spreading the infection to others.
B) Correct. It's important to wait until all symptoms, including diarrhea, vomiting, and abdominal pain, have completely resolved before resuming normal activities to prevent the spread of infection.
C) Incorrect. Being symptom-free for only 24 hours may not be sufficient to ensure full recovery from gastroenteritis.
D) Incorrect. Antibiotics are not always prescribed for gastroenteritis, and resuming normal activities should be based on symptom resolution, not antibiotic use.
Explanation
A) Incorrect. While stress and anxiety can exacerbate symptoms of GERD, they are not the primary cause. The underlying cause of heartburn in GERD is the reflux of stomach acid into the esophagus.
B) Correct. Heartburn in GERD is caused by the backflow of stomach acid into the esophagus, leading to irritation and discomfort.
C) Incorrect. While spicy foods can trigger heartburn in some individuals, they are not the primary cause of GERD. The underlying issue is the reflux of stomach acid.
D) Incorrect. An overproduction of bile in the stomach is not a direct cause of GERD. The condition is primarily related to the reflux of stomach acid.
Explanation
A) Incorrect. While exercise is important for overall health, strenuous exercise immediately after meals may exacerbate symptoms of GERD.
B) Incorrect. Lying down immediately after meals can lead to increased reflux and heartburn. It is advisable to remain upright for a period after eating.
C) Correct. Eating smaller, more frequent meals can help prevent excessive stomach distention, reducing the likelihood of acid reflux and heartburn.
D) Incorrect. High-fat meals can lead to delayed gastric emptying, potentially worsening symptoms of GERD. It is recommended to consume lower-fat meals.
Explanation
A) Incorrect. Untreated GERD is not directly associated with the development of gallstones.
B) Correct. Untreated GERD can lead to complications such as esophagitis (inflammation of the esophagus), ulcers in the esophagus, and strictures (narrowing of the esophagus). These complications can significantly impact a client's health.
C) Incorrect. Untreated GERD does not lead to the formation of kidney stones.
D) Incorrect. Untreated GERD is not directly associated with the development of high blood pressure.
Explanation
A) Incorrect. Consuming large meals can lead to increased pressure on the lower esophageal sphincter, potentially exacerbating symptoms of GERD.
B) Correct. Avoiding lying down for at least 2 hours after meals can help prevent acid reflux and heartburn by allowing the stomach to properly digest food.
C) Incorrect. Spicy foods can trigger heartburn in some individuals, so they should be avoided or consumed in moderation in those with GERD.
D) Incorrect. Engaging in vigorous exercise immediately after meals may exacerbate symptoms of GERD. It is advisable to wait until digestion is underway before participating in strenuous physical activity.
Explanation
A) Incorrect. Elevating the head of the bed is not primarily related to improving blood circulation in the legs.
B) Incorrect. While good digestion is important, elevating the head of the bed primarily helps prevent the reflux of stomach acid into the esophagus.
C) Correct. Elevating the head of the bed can help prevent stomach acid from flowing back into the esophagus, reducing the likelihood of acid reflux and heartburn.
D) Incorrect. Elevating the head of the bed is not typically associated with alleviating joint pain and stiffness.
Gastroesophageal reflux disease
Explanation
A) Incorrect. GERD is associated with specific risk factors, and it is not a random occurrence.
B) Correct. Being overweight or obese increases the likelihood of developing GERD because excess abdominal fat can put pressure on the stomach, leading to increased reflux of stomach acid into the esophagus.
C) Incorrect. While there may be some genetic predisposition to GERD, it is not primarily caused by genetic factors passed down in families.
D) Incorrect. While spicy foods can exacerbate symptoms of GERD in some individuals, they are not the main risk factor for developing the condition.
Explanation
A) Incorrect. A frequent exercise routine is not a risk factor for GERD; in fact, regular exercise can be beneficial in managing GERD.
B) Incorrect. While smoking is a risk factor for many health conditions, it is not a specific risk factor for GERD.
C) Incorrect. Consistent consumption of high-fiber foods is generally beneficial for digestive health and is not a risk factor for GERD.
D) Correct. A hiatal hernia can increase the risk of GERD because it can weaken the lower esophageal sphincter, allowing stomach acid to reflux into the esophagus.
Explanation
A) Incorrect. Eating meals at regular intervals can impact GERD. Smaller, more frequent meals are recommended to help prevent excessive stomach distention.
B) Correct. Frequent consumption of caffeine and alcohol can relax the lower esophageal sphincter, increasing the risk of GERD.
C) Incorrect. Being underweight or having a low BMI is not a typical risk factor for GERD. In fact, being overweight or obese is more commonly associated with the condition.
D) Incorrect. Occasional stress may not be a significant risk factor for GERD. However, chronic stress can potentially exacerbate symptoms.
Explanation
A) Incorrect. Regular exercise is generally beneficial for overall health and is not a risk factor for GERD.
B) Incorrect. Smoking is a known risk factor for GERD, as it can relax the lower esophageal sphincter and increase acid reflux.
C) Correct. Pregnancy can increase the risk of GERD due to the pressure exerted on the abdomen by the growing uterus. This pressure can lead to increased reflux of stomach acid.
D) Incorrect. Consuming a high-fiber diet is generally recommended for digestive health and is not considered a risk factor for GERD.
Explanation
A) Incorrect. Avoiding acidic foods is not a recognized risk factor for GERD.
B) Incorrect. While occasional stress may not be a significant risk factor, chronic stress can potentially exacerbate symptoms of GERD.
C) Correct. Being pregnant or obese increases the risk of developing GERD due to increased pressure on the abdomen, which can lead to increased reflux of stomach acid.
D) Incorrect. Regular use of over-the-counter antacids may be indicative of pre-existing GERD, but it is not a risk factor for developing the condition.
Explanation
A) Incorrect. While excessive stomach acid can contribute to GERD symptoms, it is not the primary cause. The weakening of the lower esophageal sphincter is the central issue.
B) Correct. GERD is primarily caused by the weakening of the lower esophageal sphincter (LES), a muscular ring that normally prevents stomach acid from flowing back into the esophagus.
C) Incorrect. A deficiency of digestive enzymes is not the primary cause of GERD.
D) Incorrect. GERD is not primarily related to a bacterial infection in the esophagus. It is primarily related to the dysfunction of the lower esophageal sphincter.
Explanation
A) Incorrect. Increased production of digestive enzymes is not a primary factor in weakening the lower esophageal sphincter (LES) in GERD.
B) Correct. In GERD, the relaxation of the diaphragm muscle can contribute to the weakening of the lower esophageal sphincter (LES), allowing stomach acid to reflux into the esophagus.
C) Incorrect. Enhanced contraction of the LES is not a contributing factor to GERD. It is actually the weakening or relaxation of the LES that leads to GERD.
D) Incorrect. Elevated levels of bile in the stomach are not a primary factor in weakening the LES in GERD.
Explanation
A) Incorrect. While excessive stomach acid can contribute to GERD symptoms, it is not the primary cause. The weakening of the lower esophageal sphincter is the central issue.
B) Incorrect. Stomach acid is not involved in neutralizing alkaline substances in the esophagus. Its primary role is in digestion.
C) Correct. In GERD, stomach acid refluxes back into the esophagus due to the weakened lower esophageal sphincter (LES), leading to irritation and discomfort.
D) Incorrect. Stomach acid production may be excessive or it may reflux back into the esophagus in individuals with GERD. It is not completely normal in this context.
Explanation
A) Incorrect. Weakening of the lower esophageal sphincter (LES) does not lead to a significant decrease in stomach acid production.
B) Correct. When the LES weakens, it allows stomach contents, including acid, to flow back into the esophagus, resulting in the characteristic symptoms of GERD.
C) Incorrect. Weakening of the LES is not associated with an overproduction of digestive enzymes in the stomach.
D) Incorrect. The diaphragm muscle is not directly involved in the weakening of the LES in GERD. It is primarily related to the relaxation of the LES.
Explanation
A) Incorrect. Lying down after a meal can actually worsen GERD symptoms, as it can lead to increased pressure on the abdomen, potentially resulting in more acid reflux.
B) Incorrect. Lying down does not facilitate the passage of food from the stomach to the small intestine; in fact, it can increase the likelihood of acid reflux.
C) Correct. Lying down after a meal can increase pressure on the abdomen, which can lead to more acid reflux into the esophagus, exacerbating GERD symptoms.
D) Incorrect. Lying down after a meal can impact GERD symptoms, as it can lead to increased pressure on the abdomen and potentially worsen acid reflux.
Explanation
A) Incorrect. While GERD can potentially lead to respiratory symptoms, such as cough and shortness of breath, the most common symptoms are related to the gastrointestinal tract, such as heartburn and regurgitation.
B) Correct. Common symptoms of GERD include heartburn (a burning sensation in the chest), regurgitation (the return of stomach contents into the mouth or throat), and chest pain.
C) Incorrect. Joint pain and muscle weakness are not typical symptoms of GERD. The condition primarily affects the gastrointestinal tract.
D) Incorrect. While a persistent sore throat can be associated with GERD, it is not the main symptom. Heartburn and regurgitation are more commonly reported.
Explanation
A) Incorrect. Increased blood pressure readings may not be directly related to GERD. They may be a separate issue and should be assessed independently.
B) Correct. Persistent cough and hoarseness are symptoms that can be associated with GERD. Acid reflux into the throat can lead to irritation and inflammation, resulting in a chronic cough and hoarseness.
C) Incorrect. Cold and clammy skin are not typical symptoms of GERD. These symptoms may be indicative of other conditions or factors.
D) Incorrect. Blurred vision and dizziness are not typically associated with GERD. These symptoms may be related to other health issues.
Explanation
A) Incorrect. Excessive sweating and chills are not typical nighttime symptoms of GERD. These may be indicative of other health issues.
B) Correct. GERD can lead to symptoms such as coughing, choking, and difficulty swallowing, particularly at night. Acid reflux can worsen when lying down, leading to these nighttime symptoms.
C) Incorrect. GERD can indeed cause symptoms at night, especially when lying down. These symptoms may include coughing, choking, and difficulty swallowing.
D) Incorrect. Severe abdominal pain is not a typical nighttime symptom of GERD. This type of pain may be indicative of other conditions.
Explanation
A) Incorrect. Excessive thirst and frequent urination are not typical symptoms of GERD. These may be indicative of other health issues, such as diabetes.
B) Incorrect. Difficulty in concentrating and memory problems are not commonly associated with GERD. These symptoms may be indicative of other conditions.
C) Correct. Chest pain that may mimic a heart attack is a symptom that can occur in GERD. It is important for the nurse to differentiate between GERD-related chest pain and cardiac-related chest pain.
D) Incorrect. Increased sensitivity to light and noise are not typical symptoms of GERD. These symptoms may be related to other health issues.
Explanation
A) Incorrect. In severe cases of GERD, it can lead to difficulty swallowing and a sensation of food sticking in the throat. This is known as dysphagia.
B) Correct. In severe cases of GERD, it can lead to difficulty swallowing (dysphagia) and a sensation of food sticking in the throat, which may require further evaluation and management.
C) Incorrect. While GERD can impact appetite, difficulty swallowing and a sensation of food sticking in the throat are more specific symptoms related to swallowing.
D) Incorrect. Symptoms related to swallowing, such as difficulty and sensation of food sticking, can be associated with severe cases of GERD. It is important to recognize and address these symptoms.
Explanation
A) Incorrect. An upper gastrointestinal (GI) series involves X-ray imaging of the esophagus, stomach, and small intestine with the use of a contrast material. It does not provide direct visualization or allow for tissue biopsies.
B) Incorrect. Esophageal manometry measures the pressure and coordination of the muscles in the esophagus. It does not provide direct visualization or allow for tissue biopsies.
C) Correct. Upper endoscopy (EGD) involves the insertion of a flexible tube with a camera through the mouth and into the esophagus, stomach, and duodenum. It allows for direct visualization and tissue biopsies to assess for any abnormalities or signs of GERD.
D) Incorrect. 24-hour pH monitoring measures the amount of acid in the esophagus over a 24-hour period. It does not provide direct visualization or allow for tissue biopsies.
Explanation
A) Incorrect. Upper endoscopy (EGD) involves the direct visualization of the esophagus, stomach, and duodenum using a flexible tube with a camera. It does not measure muscle pressure and coordination.
B) Correct. Esophageal manometry is a diagnostic test that measures the pressure and coordination of the muscles in the esophagus. It helps evaluate the function of the esophageal muscles and the lower esophageal sphincter.
C) Incorrect. 24-hour pH monitoring measures the amount of acid in the esophagus over a 24-hour period. It does not assess muscle pressure and coordination.
D) Incorrect. An upper gastrointestinal (GI) series involves X-ray imaging of the esophagus, stomach, and small intestine with the use of a contrast material. It does not measure muscle pressure and coordination.
Explanation
A) Incorrect. An upper gastrointestinal (GI) series involves X-ray imaging of the esophagus, stomach, and small intestine with the use of a contrast material. It does not measure acid levels over a 24-hour period.
B) Incorrect. Esophageal manometry measures the pressure and coordination of the muscles in the esophagus. It does not measure acid levels over a specific time frame.
C) Incorrect. Upper endoscopy (EGD) involves the direct visualization of the esophagus, stomach, and duodenum using a flexible tube with a camera. It does not measure acid levels over a 24-hour period.
D) Correct. 24-hour pH monitoring is a diagnostic test that measures the amount of acid in the esophagus over a 24-hour period. It helps assess the frequency and severity of acid reflux.
Explanation
A) Correct. An upper gastrointestinal (GI) series involves X-ray imaging of the esophagus, stomach, and small intestine using a contrast material. It is useful for detecting structural abnormalities and evaluating the function of the digestive tract.
B) Incorrect. Esophageal manometry measures the pressure and coordination of the muscles in the esophagus. It does not involve X-ray imaging.
C) Incorrect. Upper endoscopy (EGD) involves the direct visualization of the esophagus, stomach, and duodenum using a flexible tube with a camera. It does not use X-ray imaging with contrast material.
D) Incorrect. 24-hour pH monitoring measures the amount of acid in the esophagus over a 24-hour period and does not involve X-ray imaging.
Explanation
A) Incorrect. An upper gastrointestinal (GI) series involves X-ray imaging of the esophagus, stomach, and small intestine with the use of a contrast material. It does not allow for direct visualization.
B) Incorrect. Esophageal manometry measures the pressure and coordination of the muscles in the esophagus. It does not provide direct visualization.
C) Incorrect. 24-hour pH monitoring measures the amount of acid in the esophagus over a 24-hour period. It does not involve direct visualization.
D) Correct. Upper endoscopy (EGD) involves the insertion of a flexible tube with a camera through the mouth and into the esophagus, stomach, and duodenum, allowing for direct visualization of the gastrointestinal tract. It also allows for tissue biopsies if needed.
Explanation
A) Incorrect. Regular physical exercise is generally beneficial for overall health, including digestive health. It is not recommended to avoid exercise entirely.
B) Correct. Elevating the head of the bed by about 6-8 inches can help prevent stomach acid from flowing back into the esophagus during sleep, reducing nighttime reflux symptoms.
C) Incorrect. Consuming large meals can increase the risk of acid reflux. It is recommended to eat smaller, more frequent meals to help manage GERD.
D) Incorrect. Spicy and acidic foods can exacerbate symptoms of GERD in many individuals. It is generally recommended to avoid or limit consumption of these foods.
Explanation
A) Correct. Caffeine, chocolate, and peppermint can relax the lower esophageal sphincter (LES) and contribute to acid reflux. Advising the client to limit or avoid these items is beneficial in managing GERD.
B) Incorrect. Consuming large meals can increase the risk of acid reflux. It is recommended to eat smaller, more frequent meals to help manage GERD.
C) Incorrect. Citrus fruits and tomatoes are acidic and can exacerbate GERD symptoms in some individuals. It is generally recommended to limit their consumption.
D) Incorrect. Specific dietary modifications are important in managing GERD. Advising the client to make appropriate changes in their diet can help alleviate symptoms.
Explanation
A) Correct. Antacids are over-the-counter medications that can help neutralize stomach acid and provide short-term relief of GERD symptoms.
B) Incorrect. Proton pump inhibitors (PPIs) are effective medications for GERD, but they are typically taken on a regular basis for long-term management, not for immediate relief of symptoms.
C) Incorrect. H2 receptor antagonists (H2RAs) are another type of medication that can help reduce stomach acid production and provide relief from GERD symptoms.
D) Incorrect. Over-the-counter medications can be helpful in managing GERD symptoms. However, it's important for the client to use them according to the recommended dosage and guidelines.
Explanation
A) Correct. Alcohol can relax the lower esophageal sphincter (LES) and increase the risk of acid reflux, so it is recommended to avoid alcohol altogether to manage GERD.
B) Incorrect. Even one or two alcoholic beverages can contribute to GERD symptoms, so it is generally advised to avoid alcohol.
C) Incorrect. Alcohol can exacerbate GERD symptoms, so it is not recommended to consume it without moderation.
D) Incorrect. Limiting alcohol intake is important, but the recommended limit for those with GERD is typically lower than four drinks per day. It's generally advised to avoid alcohol or consume it in very limited quantities.
Explanation
A) Incorrect. Lying down flat immediately after meals can increase the risk of acid reflux. It is recommended to stay upright to allow gravity to help prevent reflux.
B) Correct. Maintaining an upright position for at least 2-3 hours after eating can help prevent stomach acid from flowing back into the esophagus, reducing the risk of reflux.
C) Incorrect. Sitting with legs crossed does not have a direct impact on GERD symptoms. It is more important to focus on maintaining an upright position.
D) Incorrect. Lying on the right side does not specifically aid in gastric emptying in the context of GERD management. Staying upright after meals is generally more effective.
Explanation
A) Incorrect. High-fiber foods like fruits and vegetables are generally beneficial for overall health and digestion. They are not typically associated with exacerbating GERD symptoms.
B) Correct. Fatty and fried foods can lead to delayed gastric emptying, which can contribute to acid reflux. It is advisable to limit or avoid these types of foods in the management of GERD.
C) Incorrect. Lean protein sources like chicken and fish are generally well-tolerated and do not typically worsen GERD symptoms.
D) Incorrect. Whole grains like brown rice and whole wheat bread are generally considered healthy and are not typically associated with exacerbating GERD symptoms.
Explanation
A) Incorrect. Eating three large meals per day can increase the risk of acid reflux. It is generally recommended to have smaller, more frequent meals to help manage GERD.
B) Correct. Having the last meal of the day at least 2-3 hours before bedtime allows for better digestion and reduces the likelihood of nighttime reflux.
C) Incorrect. Frequent snacking throughout the day may increase the overall volume of food consumed, which can contribute to acid reflux.
D) Incorrect. Consuming a large breakfast and a light dinner is not a universal recommendation for managing GERD. It is more important to focus on smaller, well-balanced meals spread throughout the day.
Explanation
A) Incorrect. Taking the PPI immediately before bedtime may not provide the same level of effectiveness as taking it with the first meal of the day.
B) Correct. Proton pump inhibitors (PPIs) are typically most effective when taken with the first meal of the day, on an empty stomach, as this allows for optimal absorption.
C) Incorrect. Consistency in timing is important, but taking the PPI with the first meal of the day is specifically recommended for best results.
D) Incorrect. Taking the PPI 30 minutes after a meal may not be as effective as taking it with the first meal of the day on an empty stomach.
A client with GERD asks the nurse about recommended beverages. What advice should the nurse provide?
Explanation
A) Incorrect. Coffee and tea can be acidic and may contribute to GERD symptoms. It is advisable to consume them in moderation.
B) Correct. Low-fat milk and non-citrus fruit juices are generally well-tolerated and less likely to exacerbate GERD symptoms compared to acidic or high-fat beverages.
C) Incorrect. While some beverages can exacerbate GERD symptoms, it is not necessary to avoid all types of beverages. Making specific, informed choices about beverages is more appropriate.
D) Incorrect. Herbal teas with mint can relax the lower esophageal sphincter and potentially worsen GERD symptoms. Chamomile tea may be soothing for some individuals, but it is not universally recommended for GERD.
A client is curious about a test that allows for direct visualization of the esophagus, stomach, and duodenum. What test is the client referring to?
Explanation
A) Incorrect. An upper gastrointestinal (GI) series involves X-ray imaging of the esophagus, stomach, and small intestine with the use of a contrast material. It does not allow for direct visualization.
B) Incorrect. Esophageal manometry measures the pressure and coordination of the muscles in the esophagus. It does not provide direct visualization.
C) Incorrect. 24-hour pH monitoring measures the amount of acid in the esophagus over a 24-hour period. It does not involve direct visualization.
D) Correct. Upper endoscopy (EGD) involves the insertion of a flexible tube with a camera through the mouth and into the esophagus, stomach, and duodenum, allowing for direct visualization of the gastrointestinal tract. It also allows for tissue biopsies if needed.
Peptic ulcer disease
Explanation
A) Correct. Peptic ulcers are most commonly associated with an overproduction of stomach acid, which can erode the protective mucosal lining.
B) Incorrect. Autoimmune reactions are not the primary cause of peptic ulcers. They are more closely linked to factors like acid production and bacterial infection.
C) Incorrect. While bacterial infection with H. pylori can contribute to the development of peptic ulcers, it is not the primary mechanism.
D) Incorrect. Inadequate blood supply to the stomach (ischemia) is not the primary mechanism of peptic ulcers. Acid overproduction and other factors play a more significant role.
Explanation
A) Correct. H. pylori is a bacterium that can directly damage the mucosal lining of the stomach, making it more susceptible to ulcers.
B) Incorrect. While H. pylori can lead to increased acid production, its primary mechanism in ulcer development is direct damage to the stomach lining.
C) Incorrect. H. pylori primarily affects the stomach lining, rather than weakening the overall immune system.
D) Incorrect. H. pylori does not primarily disrupt blood flow to the stomach. Its main impact is on the mucosal lining.
Explanation
A) Incorrect. Prostaglandins do not promote acid production; in fact, they can help regulate acid secretion.
B) Correct. Prostaglandins are protective substances that play a crucial role in maintaining the integrity of the stomach lining and promoting mucosal defense mechanisms.
C) Incorrect. While prostaglandins have various roles in the immune system, they do not primarily stimulate the immune system to fight off bacterial infections in the stomach.
D) Incorrect. Prostaglandins do play a role in regulating blood flow, but their primary function in the stomach is mucosal protection, rather than preventing ischemia.
Explanation
A) Incorrect. NSAIDs can lead to increased stomach acid production, but their primary mechanism in ulcer development is direct damage to the stomach lining.
B) Incorrect. NSAIDs do inhibit the action of prostaglandins, but this is not their primary role in ulcer development.
C) Correct. NSAIDs can directly damage the stomach lining, which makes it more vulnerable to the development of ulcers.
D) Incorrect. NSAIDs do not promote the growth of H. pylori. Their mechanism in ulcer development is related to direct damage to the stomach lining.
A nurse is explaining the role of lifestyle factors in the pathophysiology of peptic ulcer disease. What information should the nurse include?
Explanation
A) Correct. Excessive stress and anxiety can stimulate the release of certain hormones that increase stomach acid production, potentially contributing to the development of peptic ulcers.
B) Incorrect. While spicy foods can exacerbate existing ulcers, they are not a major factor in the development of peptic ulcers.
C) Incorrect. While regular exercise has numerous health benefits, it is not a primary factor in preventing the development of peptic ulcers.
D) Incorrect. Alcohol consumption can contribute to the risk of peptic ulcers, particularly in excessive amounts, due to its potential to irritate the stomach lining and increase acid production.
Explanation
A diet high in fiber and low in fat is generally considered healthy, but it is not specifically associated with an increased or decreased risk of peptic ulcer disease.
Choice B reason:
Smoking and alcohol consumption are indeed risk factors for peptic ulcer disease. They can contribute to the development and exacerbation of ulcers.
Choice C reason:
This statement is correct. The use of NSAIDs, such as aspirin and ibuprofen, and Helicobacter pylori infection are well-established risk factors for peptic ulcer disease.
Choice D reason:
While stress and emotional factors may exacerbate peptic ulcer symptoms, they are not the primary cause of the condition. The primary causes are H. pylori infection and the use of NSAIDs.
Explanation
This question is relevant to assess for gastrointestinal symptoms, as changes in bowel movements may indicate issues with digestion or absorption.
Choice B reason:
Family history of heart disease is not directly related to peptic ulcer disease. However, it is essential for overall health assessment and risk factor identification.
Choice C reason:
Swelling or edema in the legs may be indicative of cardiovascular or circulatory issues, but it is not directly related to peptic ulcer disease.
Choice D reason:
The frequency of consuming high-fiber foods is not specifically related to peptic ulcer disease. However, diet history is essential for overall health assessment.
Explanation
Taking the PPI with meals is not the most effective timing for acid suppression. PPIs work best when taken on an empty stomach.
Choice B reason:
This statement is correct. PPIs are most effective when taken on an empty stomach, about 30 minutes before a meal. This allows the medication to be absorbed and inhibit acid secretion in the stomach before food intake.
Choice C reason:
While consistency in medication timing is important, taking the PPI at any time of the day may not optimize its effectiveness.
Choice D reason:
Taking the PPI before bedtime may not provide the best acid suppression throughout the day. Taking it on an empty stomach before a meal is a more appropriate approach.
Explanation
This statement describes an esophagoscopy, not an endoscopy. An endoscopy examines the upper gastrointestinal tract, including the stomach and duodenum.
Choice B reason:
This statement describes a colonoscopy, not an endoscopy. An endoscopy does not involve the lower gastrointestinal tract.
Choice C reason:
This statement describes an ultrasound, not an endoscopy. An endoscopy is a direct visualization procedure.
Choice D reason:
This statement is correct. An endoscopy involves inserting a fleble tube (endoscope) with a camera on the end through the mouth to examine the stomach and duodenum. It is a commonly used procedure to assess and diagnose peptic ulcer disease.
A nurse is providing dietary education to a client with peptic ulcer disease. Which of the following dietary modifications should the nurse recommend to the client?
Explanation
Increasing the intake of spicy foods can exacerbate symptoms in a client with peptic ulcer disease, as they can irritate the stomach lining and increase acid production.
Choice B reason:
This statement is correct. Consuming small, frequent meals throughout the day can help reduce stomach distention and pressure, minimizing the symptoms of peptic ulcer disease.
Choice C reason:
Avoiding fluids with meals is not a standard recommendation for peptic ulcer disease. Adequate hydration is important, and drinking fluids with meals should not significantly affect stomach distention.
Choice D reason:
Citrus fruits and juices are acidic and can aggravate the stomach lining in a client with peptic ulcer disease. It is best to avoid or limit their consumption.
Explanation
This statement is correct. Family history and genetic factors are considered significant risk factors for peptic ulcer disease. A positive family history increases the likelihood of developing the condition.
Choice B reason:
Excessive consumption of fresh fruits and vegetables is not a risk factor for peptic ulcer disease. In fact, a diet rich in fruits and vegetables is generally associated with a lower risk of developing peptic ulcers.
Choice C reason:
Regular exercise and maintaining a healthy weight are not considered risk factors for peptic ulcer disease. These factors are essential for overall health but are not directly related to ulcer development.
Choice D reason:
While stress and emotional factors may exacerbate peptic ulcer symptoms, they are not the primary cause of the condition. The primary causes are Helicobacter pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Explanation
Consumption of spicy foods and carbonated beverages may exacerbate symptoms in individuals with peptic ulcer disease, but they are not direct risk factors for developing the condition.
Choice B reason:
Regular consumption of yogurt and probiotics may promote gastrointestinal health, but they are not specifically risk factors for peptic ulcer disease.
Choice C reason:
Frequent use of antacids for heartburn relief may indicate underlying acid-related issues, but it is not a risk factor for peptic ulcer disease.
Choice D reason:
This statement is correct. Long-term use of NSAIDs is a well-established risk factor for peptic ulcer disease. NSAIDs can irritate the stomach lining and increase the risk of ulcer formation.
Explanation
While Helicobacter pylori is a type of bacteria, it is not typically transmitted through food and does not directly cause peptic ulcer disease.
Choice B reason:
This statement is incorrect. Helicobacter pylori infection is indeed associated with an increased risk of peptic ulcer disease.
Choice C reason:
This statement is correct. Helicobacter pylori infection can weaken the stomach lining by producing substances that can damage the mucous layer, leading to increased vulnerability to acid and contributing to ulcer formation.
Choice D reason:
Helicobacter pylori infection is not caused by excessive consumption of spicy foods. The infection is typically acquired through person-to-person transmission, such as through contaminated water or food, and is unrelated to diet choices.
Explanation
Taking NSAIDs with alcohol can increase the risk of gastrointestinal irritation and ulcer development. Alcohol should be avoided while taking NSAIDs.
Choice B reason:
Taking NSAIDs on an empty stomach can increase the risk of irritation and ulcer formation. To minimize this risk, NSAIDs should be taken with food or milk.
Choice C reason:
This statement is correct. Using NSAID patches or creams can provide pain relief without affecting the gastrointestinal tract, reducing the risk of peptic ulcer development.
Choice D reason:
While a high-fiber diet is generally beneficial for digestive health, it does not specifically counteract the effects of NSAIDs on the stomach lining.
Explanation
Frequent consumption of spicy foods or citrus fruits can irritate the stomach lining and increase the risk of peptic ulcer development.
Choice B reason:
Family history of lung diseases is not directly related to the risk of peptic ulcer disease. However, family history of peptic ulcers or gastrointestinal conditions is relevant for risk assessment.
Choice C reason:
Experiencing frequent headaches is not a direct risk factor for peptic ulcer disease. However, the nurse should assess for other risk factors and medical history during the health screening.
Choice D reason:
Regular physical exercise is important for overall health, but it is not a direct risk factor for peptic ulcer disease. The nurse should focus on risk factors related to diet, medication use, and other medical conditions.
Explanation
This statement is correct. Right upper quadrant abdominal pain that radiates to the right shoulder is a hallmark symptom of cholecystitis. The pain is typically sudden, severe, and constant, and it is often triggered by a fatty meal.
Choice B reason:
Left lower quadrant abdominal pain with rebound tenderness is not characteristic of cholecystitis. It may indicate other conditions, such as diverticulitis or appendicitis.
Choice C reason:
Midline epigastric pain aggravated by lying down is more indicative of gastroesophageal reflux disease (GERD) rather than cholecystitis.
Choice D reason:
Diffuse abdominal pain with a low-grade fever may be seen in various conditions, but it does not specifically point to cholecystitis.
Explanation
Elevated white blood cell count may indicate inflammation or infection, but it is not directly related to jaundice and dark-colored urine, which are characteristic of increased bilirubin levels.
Choice B reason:
Impaired blood clotting is not directly related to jaundice and dark-colored urine. It may be a concern in liver disease but does not explain the specific manifestations mentioned in the question.
Choice C reason:
This statement is correct. Jaundice and dark-colored urine are indicative of increased bilirubin levels in the blood, which can occur in cholecystitis due to obstruction of the bile ducts.
Choice D reason:
Elevated serum amylase is more associated with pancreatitis rather than cholecystitis. It is not directly related to the clinical manifestations described.
Explanation
Nausea and vomiting after meals are common symptoms in acute cholecystitis, but they do not indicate a severe complication. They are typical manifestations of gallbladder inflammation.
Choice B reason:
Mild right upper quadrant pain may be present in acute cholecystitis, but it does not suggest a severe complication.
Choice C reason:
Referred pain to the left shoulder (Kehr's sign) is a classic symptom of splenic rupture or other conditions involving the spleen, not directly related to cholecystitis.
Choice D reason:
This statement is correct. High fever and chills may indicate the presence of infection and sepsis, which can be severe complications of acute cholecystitis.
Explanation
This statement is correct. Chronic cholecystitis can lead to impaired gallbladder emptying, resulting in difficulties in digesting fats. Indigestion and bloating after meals are common manifestations of this problem.
Choice B reason:
Excessive stomach acid production is more associated with conditions like GERD or peptic ulcer disease, and it is not directly related to chronic cholecystitis.
Choice C reason:
Inflammation of the small intestine may cause abdominal pain, diarrhea, or malabsorption issues, but it is not specifically related to the symptoms described in the question.
Choice D reason:
Decreased production of pancreatic enzymes may lead to malabsorption issues and cause symptoms like diarrhea and steatorrhea. However, it is not the primary cause of indigestion and bloating after meals in chronic cholecystitis.
A nurse is assessing a client suspected of having acute cholecystitis. Which of the following techniques should the nurse use to elicit Boas' sign?
Explanation
Percussion of the left lower quadrant is not relevant to assess for Boas' sign, which involves the right upper quadrant.
Choice B reason:
Deep palpation of the epigastric region is not associated with Boas' sign. Boas' sign involves palpation of the right subscapular area.
Choice C reason:
This statement is correct. Boas' sign is elicited by palpating the right upper quadrant during inspiration. The client may experience referred pain to the right subscapular area, indicating irritation of the phrenic nerve by the inflamed gallbladder.
Choice D reason:
Auscultation of the left upper quadrant is not relevant to assessing for Boas' sign, which involves the right upper quadrant.
Explanation
Abdominal CT scan can provide detailed images, but it is not typically the first-line imaging study for diagnosing cholecystitis. It may be used if complications are suspected.
Choice B reason:
MRI of the gallbladder can provide high-resolution images, but it is not the first-line imaging study for diagnosing cholecystitis.
Choice C reason:
This statement is correct. Abdominal ultrasound is the first-line imaging study for diagnosing cholecystitis. It can visualize the gallbladder, detect gallstones, and assess for signs of inflammation, such as gallbladder wall thickening and pericholecystic fluid.
Choice D reason:
ERCP is an invasive procedure used to visualize the biliary and pancreatic ducts, but it is not typically used as a first-line diagnostic test for cholecystitis.
Explanation
Fasting for 12 hours before an abdominal ultrasound is not necessary. Abdominal ultrasound does not require an empty stomach.
Choice B reason:
Drinking water is not typically restricted before an abdominal ultrasound. In fact, drinking water can improve image quality in some cases.
Choice C reason:
This statement is correct. There are no special preparations required for an abdominal ultrasound. The procedure is non-invasive and does not involve any special preparation or fasting.
Choice D reason:
Avoiding pain medications is not necessary before an abdominal ultrasound. The client can continue taking prescribed medications as usual.
Explanation
Elevated serum amylase levels are more indicative of pancreatitis, not cholecystitis.
Choice B reason:
Increased serum creatinine levels are suggestive of kidney dysfunction and are not directly related to cholecystitis.
Choice C reason:
This statement is correct. Cholecystitis is associated with inflammation and infection, which can lead to an elevated white blood cell count (leukocytosis).
Choice D reason:
Low serum bilirubin levels are not consistent with cholecystitis, which can cause obstructive jaundice and elevated bilirubin levels due to bile duct obstruction.
Explanation
Visualizing blood flow in the liver is not the purpose of a HIDA scan. This type of scan is primarily used to assess the biliary system.
Choice B reason:
This statement is correct. A HIDA scan is used to assess the function and patency of the bile ducts. It involves injecting a radioactive tracer that is taken up by the liver and excreted into the bile. The scan can visualize the flow of bile and detect any obstruction or abnormality in the biliary system.
Choice C reason:
Evaluating the motility of the small intestine is not the purpose of a HIDA scan. It is used specifically for assessing the biliary system.
Choice D reason:
Providing detailed images of the pancreas is not the primary purpose of a HIDA scan, although it can sometimes provide some information about the pancreas if the tracer reaches the duodenum and enters the common bile duct.
A client is undergoing an abdominal computed tomography (CT) scan to evaluate suspected cholecystitis. The client expresses concern about potential radiation exposure. Which of the following responses should the nurse provide?
Explanation
CT scans use X-rays, not magnetic fields, to create detailed cross-sectional images of the body. They involve radiation exposure.
Choice B reason:
This statement is correct. While CT scans use X-rays, the amount of radiation used in modern CT machines is relatively low and considered safe. The benefits of the diagnostic information obtained from the scan usually outweigh the risks associated with the small amount of radiation exposure.
Choice C reason:
The speed of the scan does not impact the radiation exposure. The amount of radiation used in a CT scan remains the same regardless of the scan duration.
Choice D reason:
CT scans use X-rays, not sound waves. Sound waves are used in ultrasound imaging, not in CT scans.
Explanation
Avoiding NSAIDs is essential for clients with peptic ulcer disease as they can worsen the condition and increase the risk of bleeding.
Choice B reason:
Following a low-fat diet does not directly impact stomach acid production, but it can help prevent irritation to the stomach lining by reducing the intake of potentially irritating foods.
Choice C reason:
This statement is correct. Proton pump inhibitors (PPIs) are commonly prescribed to reduce stomach acid production and promote ulcer healing. It is crucial for the client to continue taking PPIs as directed by their healthcare provider.
Choice D reason:
This statement is incorrect and indicates a need for further teaching. Alcohol can irritate the stomach lining and exacerbate peptic ulcer disease. Clients with peptic ulcers should avoid or minimize alcohol consumption.
Explanation
Administering antacids one hour before meals would be less effective in providing pain relief during mealtime when stomach acid production is increased.
Choice B reason:
This statement is correct. Administering antacids with meals helps neutralize stomach acid during the digestion process and provides pain relief for clients with peptic ulcer disease.
Choice C reason:
Administering antacids two hours after meals may not effectively reduce pain during the mealtime when stomach acid production is at its peak.
Choice D reason:
Administering antacids at bedtime may help with overnight acid reduction, but it may not adequately address pain during meals when acid production is higher.
Explanation
Antibiotics do not directly heal the ulcer or reduce stomach acid production. They are prescribed specifically to treat Helicobacter pylori (H. pylori) infection, a common cause of peptic ulcers.
Choice B reason:
This statement is correct. Antibiotics are prescribed to treat H. pylori infection, which is a major cause of peptic ulcers. By eliminating the bacterial infection, the ulcer has a better chance of healing and preventing recurrence.
Choice C reason:
Antibiotics do not promote blood clotting or reduce the risk of bleeding from the ulcer. Other medications may be prescribed to manage bleeding if it occurs.
Choice D reason:
Antibiotics do not relax stomach muscles or alleviate abdominal pain. Pain relief is typically achieved through acid-reducing medications and other pain management strategies.
Explanation
Recovering fully within 1-2 weeks after surgery for a peptic ulcer perforation may be overly optimistic. The recovery time is typically longer and depends on the individual's health status and the extent of the surgery.
Choice B reason:
This statement is correct. The recovery time after surgery for a peptic ulcer perforation varies depending on factors such as the type of surgery performed, the extent of the perforation, and the client's overall health. It may take several weeks to months for the client to fully recover.
Choice C reason:
Resuming normal activities immediately after surgery for a peptic ulcer perforation is not advisable. Clients usually require a period of rest and limited activity to allow proper healing.
Choice D reason:
Recovering fully in 6 months may be an extended recovery period. While some clients may experience a longer recovery, it is not a standard time frame for everyone.
A nurse is providing dietary instructions to a client with peptic ulcer disease. Which of the following dietary modifications should the nurse recommend to promote ulcer healing?
Explanation
Increasing intake of spicy foods is not recommended for clients with peptic ulcer disease, as they can irritate the stomach lining and exacerbate symptoms.
Choice B reason:
This statement is correct. Consuming frequent, small meals throughout the day helps prevent prolonged periods of fasting, which can reduce stomach acid production and irritation to the stomach lining. It also aids in maintaining steady blood sugar levels.
Choice C reason:
Drinking caffeinated beverages can increase stomach acid production and may worsen symptoms in clients with peptic ulcer disease. It is best to avoid or limit caffeinated drinks.
Choice D reason:
High-fiber foods can be beneficial for overall digestive health, but they are not specifically recommended for promoting ulcer healing. In some cases, high-fiber foods may need to be avoided if they cause discomfort.
Explanation
Mild bloating and gas after meals may be common gastrointestinal symptoms but are not specific warning signs of complications related to peptic ulcer disease.
Choice B reason:
This statement is correct. Black, tarry stools (melena) or vomiting blood (hematemesis) are potential signs of gastrointestinal bleeding, a serious complication of peptic ulcer disease. Clients should seek immediate medical attention if they experience these symptoms.
Choice C reason:
Occasional heartburn may occur during the course of ulcer healing but is not considered a warning sign of complications.
Choice D reason:
Feeling fatigued and sleepy after meals is not typically associated with peptic ulcer disease or its complications.
Explanation
A perforated peptic ulcer can lead to localized peritonitis, which may cause abdominal rigidity and guarding, rather than hypoactive bowel sounds.
Choice B reason:
Reduced abdominal tenderness is not expected in a client with a perforated peptic ulcer. Abdominal tenderness is likely to be present due to inflammation and irritation of the peritoneal lining.
Choice C reason:
Elevated blood pressure is not a typical finding in a client with a perforated peptic ulcer. The client may experience hypotension due to fluid loss and hemorrhage.
Choice D reason:
This statement is correct. A perforated peptic ulcer can cause increased abdominal rigidity due to the inflammation and irritation of the peritoneal lining. The abdomen may feel tense and rigid upon palpation.
Explanation
Taking NSAIDs with food can help reduce stomach irritation and the risk of developing peptic ulcers.
Choice B reason:
This statement is correct. Dark, tarry stools may indicate gastrointestinal bleeding, a potential complication of peptic ulcer disease. The client should promptly notify their healthcare provider if they experience this symptom.
Choice C reason:
This statement is incorrect and indicates a need for further education. While antacids can provide temporary relief from heartburn, they do not address the underlying issue of stomach irritation caused by NSAIDs. The client should avoid NSAIDs or discuss alternative pain management strategies with their healthcare provider.
Choice D reason:
Avoiding alcohol is advisable while on NSAIDs as alcohol can increase the risk of gastrointestinal bleeding and worsen peptic ulcer disease.
Explanation
Assessing for signs of fluid overload is a priority when administering PPIs intravenously, as these medications can increase the risk of fluid retention in some clients.
Choice B reason:
Monitoring liver function test results is important for clients taking certain medications, but it is not the priority when administering PPIs to this client.
Choice C reason:
Elevating the head of the client's bed is a standard measure to prevent aspiration and improve digestion, but it is not the priority in this scenario.
Choice D reason:
Checking for drug interactions with other medications is essential for safe medication administration, but it is not the priority when administering PPIs intravenously to this client.
A client with peptic ulcer disease is scheduled for an upper gastrointestinal endoscopy. The client asks the nurse about the purpose of the procedure. Which of the following responses should the nurse provide?
Explanation
Choice A Reason:
This statement is correct. An upper gastrointestinal endoscopy is a diagnostic procedure that uses a fleble tube with a camera (endoscope) to visualize the esophagus, stomach, and duodenum. It helps identify abnormalities, such as peptic ulcers, inflammation, or tumors.
Choice B reason:
Assessing blood flow to the intestines and colon is not the purpose of an upper gastrointestinal endoscopy. This procedure focuses on the upper digestive tract.
Choice C reason:
Evaluating kidney function and the urinary system is unrelated to an upper gastrointestinal endoscopy, which focuses on the upper digestive tract.
Choice D reason:
Diagnosing conditions in the lower digestive tract is not the purpose of an upper gastrointestinal endoscopy. Lower digestive tract evaluations are typically done using colonoscopy or sigmoidoscopy.
Explanation
Choice A reason:
This statement is correct. Sucralfate is best taken on an empty stomach at least 1 hour before meals to allow it to form a protective barrier over the ulcer and provide optimal therapeutic effects.
Choice B reason:
Crushing sucralfate tablets is not recommended, as it may interfere with the medication's ability to adhere to the ulcer site and provide protection.
Choice C reason:
Taking sucralfate with antacids may reduce its effectiveness, as antacids can interfere with its therapeutic actions. It is best to take sucralfate separately from antacids.
Choice D reason:
It is essential to avoid taking sucralfate with other medications, especially those that require an acidic environment for absorption. This is because sucralfate can decrease the absorption of certain drugs.
Explanation
Choice A reason:
Eating a large, well-balanced meal during mealtimes may exacerbate abdominal pain for the client with peptic ulcer disease. Instead, the client should be encouraged to eat smaller, more frequent meals to reduce stomach acid production.
Choice B reason:
This statement is correct. Administering prescribed antacids 30 minutes before meals can help reduce stomach acid levels during digestion and alleviate the client's pain.
Choice C reason:
Instructing the client to lie flat immediately after eating is not recommended, as it may increase the risk of reflux and worsen the client's symptoms.
Choice D reason:
Providing the client with spicy foods is not advisable, as they can irritate the stomach lining and worsen symptoms for the client with peptic ulcer disease.
Explanation
Choice A reason:
This statement is correct. H2 receptor blockers can sometimes cause an increase in serum potassium levels. The nurse should monitor the client's potassium levels closely to detect any abnormalities.
Choice B reason:
H2 receptor blockers do not typically affect blood glucose levels, so monitoring blood glucose is not the priority in this scenario.
Choice C reason:
H2 receptor blockers are not known to have a significant impact on serum creatinine levels, so monitoring creatinine is not the priority in this case.
Choice D reason:
H2 receptor blockers are not known to affect the CBC, so monitoring the complete blood count is not the priority for this client.
Explanation
Choice A reason:
Hypertension and increased heart rate are not early signs of gastrointestinal bleeding. In fact, hypotension and tachycardia are more common signs of significant blood loss.
Choice B reason:
Abdominal distention and bloating are not typical early signs of gastrointestinal bleeding. These symptoms may occur due to other gastrointestinal issues but are not specific to bleeding.
Choice C reason:
This statement is correct. Melena, or black, tarry stools, is a classic sign of upper gastrointestinal bleeding and indicates the presence of partially digested blood in the stool.
Choice D reason:
Hyperactive bowel sounds are not early signs of gastrointestinal bleeding. Bowel sounds may be hyperactive or hypoactive depending on the severity of the bleeding and associated factors.
A client with peptic ulcer disease is prescribed misoprostol. Which of the following information should the nurse include in the client's medication education?
Explanation
Choice A reason:
Misoprostol is not an antibiotic. It is a synthetic prostaglandin used to protect the stomach lining and prevent peptic ulcers, particularly in clients taking nonsteroidal anti-inflammatory drugs (NSAIDs).
Choice B reason:
Misoprostol should be taken with meals to minimize gastrointestinal side effects. Taking it on an empty stomach may increase the risk of adverse effects.
Choice C reason:
This statement is correct. Misoprostol is contraindicated during pregnancy and can cause uterine contractions and birth defects. Clients taking misoprostol should use effective contraception to prevent pregnancy.
Choice D reason:
Misoprostol is not used to reduce stomach acid production. Instead, it helps protect the stomach lining by increasing mucus production and promoting bicarbonate secretion.
Explanation
Choice A reason:
This statement is correct. Smoking and excessive alcohol intake can irritate the stomach lining and increase the risk of peptic ulcer recurrence. Avoiding these substances is important for promoting healing and preventing further damage.
Choice B reason:
Consuming a high-fat diet is not recommended for peptic ulcer prevention. High-fat foods can stimulate acid production and worsen symptoms for clients with peptic ulcers.
Choice C reason:
Engaging in strenuous exercise immediately after meals is not advisable, as it can increase the risk of acid reflux and worsen symptoms for clients with peptic ulcers.
Choice D reason:
Regular use of NSAIDs can increase the risk of developing peptic ulcers and is not a preventive strategy for clients with a history of peptic ulcer disease.
Explanation
Choice A reason:
This statement is incorrect and indicates a need for further education. PPIs should be taken on an empty stomach, at least 30 minutes before meals, to allow for optimal absorption and effectiveness.
Choice B reason:
This statement is correct. Clients should continue taking the PPI for the full duration as prescribed, even if they start to feel better, to prevent ulcer recurrence.
Choice C reason:
This statement is correct. PPIs can decrease calcium absorption and increase the risk of osteoporosis in some clients. Increasing calcium intake or taking calcium supplements may be necessary for clients on long-term PPI therapy.
Choice D reason:
This statement is correct. Antacids can interfere with the action of PPIs, and clients should avoid taking them together. If needed, antacids should be taken at least 1 hour before or after the PPI.
Explanation
Choice A reason:
Limiting fiber-rich foods is not a recommended preventive strategy for peptic ulcer disease. In fact, fiber can aid digestion and promote bowel regularity, which may be beneficial for some clients with peptic ulcers.
Choice B reason:
This statement is correct. Spicy and acidic foods can irritate the stomach lining and increase stomach acid production, potentially worsening symptoms for clients with peptic ulcers.
Choice C reason:
Increasing consumption of carbonated beverages is not advised, as they can cause bloating and increased gas production, which may exacerbate symptoms for clients with peptic ulcers.
Choice D reason:
Caffeine-containing beverages should be limited or avoided, as caffeine can stimulate gastric acid secretion and may worsen symptoms for clients with peptic ulcers.
Explanation
Choice A reason:
Avoiding all dairy products is not a preventive measure for H. pylori reinfection. Dairy consumption does not play a significant role in H. pylori colonization or infection.
Choice B reason:
This statement is correct. H. pylori is primarily transmitted through the oral-oral or fecal-oral route. Practicing strict hand hygiene, especially after using the restroom and before eating, can help reduce the risk of transmission and reinfection.
Choice C reason:
Including raw vegetables in the diet is not a specific preventive measure for H. pylori reinfection. A balanced diet that promotes overall gut health may be beneficial, but raw vegetables alone do not prevent H. pylori reinfection.
Choice D reason:
Taking over-the-counter antacids regularly is not a preventive strategy for H. pylori reinfection. Antacids do not target the bacterium and are not effective in eradicating H. pylori.
A client with a history of peptic ulcer disease is prescribed sucralfate as part of the preventive treatment plan. Which of the following instructions should the nurse provide to the client about taking sucralfate?
Explanation
Choice A reason:
Taking sucralfate with meals is not recommended, as it can reduce its effectiveness. Sucralfate should be taken on an empty stomach, at least 1 hour before meals, to allow it to form a protective barrier over the ulcerated areas.
Choice B reason:
Crushing sucralfate tablets is not advised, as it can interfere with the medication's ability to adhere to the ulcer site and provide protection.
Choice C reason:
This statement is correct. Taking antacids with sucralfate can reduce its effectiveness, as antacids can interfere with its therapeutic actions. Clients should avoid taking antacids together with sucralfate.
Choice D reason:
Sucralfate does not typically cause drowsiness, so taking it before bedtime is not necessary for this medication. It should be taken at regular intervals during the day as prescribed.
Gastrointestinal bleeding
Explanation
Rationale
A) Incorrect. While infections can cause gastrointestinal symptoms, they are not the primary cause of gastroesophageal bleeding. The erosion of blood vessels is a more common cause.
B) Correct. Gastroesophageal bleeding often occurs due to the erosion of blood vessels in the esophagus or stomach lining, which can be caused by conditions such as peptic ulcers, esophagitis, or varices.
C) Incorrect. Psychological stress and anxiety are not primary causes of gastroesophageal bleeding. Physical factors and underlying conditions play a more significant role.
D) Incorrect. Excessive physical activity and strenuous exercise are not common causes of gastroesophageal bleeding. The erosion of blood vessels and underlying medical conditions are more relevant factors.
Explanation
Rationale
A) Incorrect. History of allergies and sensitivities is not a significant risk factor for gastroesophageal bleeding.
B) Correct. Chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs) is a significant risk factor for gastroesophageal bleeding. NSAIDs can irritate the lining of the stomach and esophagus, potentially leading to bleeding.
C) Incorrect. Regular consumption of probiotic supplements is not a known risk factor for gastroesophageal bleeding.
D) Incorrect. High intake of vitamin C-rich foods is not a significant risk factor for gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Abdominal pain and bloating are not the main signs and symptoms of gastroesophageal bleeding. They may be associated with other gastrointestinal conditions.
B) Incorrect. Difficulty concentrating and memory problems are not typically associated with gastroesophageal bleeding. These symptoms may be indicative of other health issues.
C) Correct. One of the main signs of gastroesophageal bleeding is the presence of bloody or black, tarry stools (melena). This indicates that blood has passed through the digestive tract.
D) Incorrect. Skin rash and itching are not typical signs of gastroesophageal bleeding. These symptoms may be associated with other conditions.
Explanation
Rationale
A) Incorrect. NSAIDs can increase the risk of gastroesophageal bleeding. Continuing their use without precautions can be detrimental.
B) Correct. Avoiding or limiting the use of NSAIDs and considering alternative pain management methods can help reduce the risk of gastroesophageal bleeding.
C) Incorrect. NSA
IDs can increase the risk of gastroesophageal bleeding, especially with long-term use. They should be used cautiously.
D) Incorrect. Using NSAIDs liberally, especially without consideration of the potential risks, can increase the likelihood of gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Consuming alcohol, even in moderation, can contribute to gastroesophageal bleeding. It is advisable to limit or avoid alcohol.
B) Correct. Maintaining a healthy, balanced diet with an emphasis on foods rich in fiber and nutrients can help support digestive health and reduce the risk of gastroesophageal bleeding.
C) Incorrect. Increasing the use of NSAIDs for pain management can increase the risk of gastroesophageal bleeding. Alternative pain management methods should be considered.
D) Incorrect. Engaging in high-intensity exercise is important for cardiovascular health, but it is not directly related to the prevention of gastroesophageal bleeding. Dietary modifications and careful medication management are more relevant in this context.
Explanation
Rationale
A) Correct. A history of heavy alcohol consumption is a known risk factor for gastroesophageal bleeding. Alcohol can irritate the gastrointestinal tract and contribute to bleeding.
B) Incorrect. Regular consumption of probiotic supplements is not a primary risk factor for gastroesophageal bleeding.
C) Incorrect. While a sedentary lifestyle can contribute to overall health issues, it is not a direct risk factor specifically for gastroesophageal bleeding.
D) Incorrect. A history of allergies and sensitivities is not a common risk factor for gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Regular consumption of low-fat dairy products is not a significant risk factor for gastroesophageal bleeding.
B) Correct. Chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs) is a significant risk factor for gastroesophageal bleeding. NSAIDs can irritate the gastrointestinal tract and increase the risk of bleeding.
C) Incorrect. Engaging in regular moderate exercise is generally beneficial for overall health and well-being, but it is not a significant risk factor for gastroesophageal bleeding.
D) Incorrect. Consuming a diet rich in fruits and vegetables is generally considered healthy and is not a significant risk factor for gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. NSAIDs can increase the risk of gastroesophageal bleeding, especially with regular use. Continuing their use without precautions can be detrimental.
B) Correct. Avoiding or limiting the use of NSAIDs and considering alternative pain management methods can help reduce the risk of gastroesophageal bleeding.
C) Incorrect. Engaging in intense physical activity can be beneficial for overall health, but it is not directly related to the prevention of gastroesophageal bleeding.
D) Incorrect. Increasing the consumption of alcoholic beverages can actually contribute to gastroesophageal bleeding. It is advisable to limit or avoid alcohol.
Explanation
Rationale
A) Correct. A history of allergies and sensitivities is not a significant risk factor for gastroesophageal bleeding.
B) Incorrect. Chronic use of proton pump inhibitors (PPIs) is not a known risk factor for gastroesophageal bleeding. In fact, PPIs are often prescribed to help manage conditions that may lead to bleeding.
C) Incorrect. Regular consumption of herbal teas is not a known risk factor for gastroesophageal bleeding.
D) Incorrect. Previous surgery for a broken bone is not related to the risk of gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Consuming alcohol, even in moderation, can contribute to gastroesophageal bleeding. It is advisable to limit or avoid alcohol.
B) Correct. Maintaining a healthy, balanced diet with an emphasis on foods rich in fiber and nutrients can help support digestive health and reduce the risk of gastroesophageal bleeding.
C) Incorrect. Engaging in high-intensity exercise is important for cardiovascular health, but it is not directly related to the prevention of gastroesophageal bleeding. Dietary modifications and careful medication management are more relevant in this context.
D) Incorrect. Seeking medical attention for minor aches and pains is important for overall health and well-being and is not a risk factor for gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Bacterial infections are not the primary cause of gastroesophageal bleeding. It is more commonly related to the integrity of blood vessel walls.
B) Correct. Gastroesophageal bleeding is primarily caused by the weakening of blood vessel walls in the esophagus or stomach. Conditions like peptic ulcers, esophagitis, or varices can lead to this weakening.
C) Incorrect. While psychological stress and anxiety can have an impact on overall health, they are not the leading factors contributing to gastroesophageal bleeding.
D) Incorrect. Excessive physical activity and strenuous exercise are not the primary triggers for gastroesophageal bleeding. The integrity of blood vessel walls plays a more significant role.
Explanation
Rationale
A) Incorrect. While certain bacterial infections can lead to gastrointestinal issues, they are not a primary factor in the development of gastroesophageal bleeding.
B) Correct. Chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs) is a significant factor contributing to gastroesophageal bleeding. NSAIDs can irritate the gastrointestinal tract, potentially leading to bleeding.
C) Incorrect. Psychological stress and anxiety are not the primary factors that weaken blood vessel walls in the esophagus leading to gastroesophageal bleeding.
D) Incorrect. Engaging in intense physical activity and strenuous exercise is not the main cause of weakened blood vessels in gastroesophageal bleeding. It is primarily related to the integrity of blood vessel walls and underlying conditions.
Explanation
Rationale
A) Incorrect. Gastroesophageal bleeding is not primarily related to the accumulation of gas and bloating in the digestive tract. It is related to blood vessel integrity.
B) Correct. Gastroesophageal bleeding occurs when weakened blood vessel walls lead to the escape of blood into the digestive tract. This blood can be expelled in vomit (hematemesis) or in stool (melena).
C) Incorrect. Psychological stress and anxiety can impact overall health, but they do not directly cause gastroesophageal bleeding.
D) Incorrect. Excessive physical activity and strenuous exercise do not directly cause gastroesophageal bleeding. It is primarily related to the integrity of blood vessel walls.
Explanation
Rationale
A) Incorrect. Excessive stomach acid can contribute to gastrointestinal issues, but it is not the primary factor in gastroesophageal bleeding. Weakened blood vessel walls are more significant.
B) Correct. Gastroesophageal bleeding is primarily caused by the weakening of blood vessel walls in the esophagus or stomach lining. Conditions like peptic ulcers, esophagitis, or varices can lead to this weakening.
C) Incorrect. Psychological stress and anxiety can impact overall health, but they do not directly cause weakened blood vessel walls leading to gastroesophageal bleeding.
D) Incorrect. Vigorous coughing and respiratory distress are not the primary causes of gastroesophageal bleeding. The integrity of blood vessel walls is more relevant.
Explanation
Rationale
A) Incorrect. Engaging in regular, moderate physical activity is generally beneficial for overall health, but it is not the primary factor in strengthening blood vessel walls related to gastroesophageal bleeding.
B) Correct. Excessive physical activity and strenuous exercise can
contribute to weakened blood vessel walls, which is a significant factor in gastroesophageal bleeding.
C) Incorrect. Psychological stress and anxiety associated with physical activity are not the primary triggers for gastroesophageal bleeding.
D) Incorrect. While diet can play a role in gastrointestinal health, it is not the primary factor related to weakened blood vessel walls leading to gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Severe headache and dizziness are not common symptoms of gastroesophageal bleeding. These symptoms may be indicative of other health issues.
B) Incorrect. Abdominal pain, bloating, and discomfort are not the main symptoms of gastroesophageal bleeding. They may be associated with other gastrointestinal conditions.
C) Incorrect. Difficulty concentrating and memory problems are not typically associated with gastroesophageal bleeding. These symptoms may be indicative of other health issues.
D) Correct. One of the main symptoms of gastroesophageal bleeding is the presence of bloody or black, tarry stools (melena). This indicates that blood has passed through the digestive tract.
Explanation
Rationale
A) Correct. In gastroesophageal bleeding, changes in blood pressure and heart rate may occur due to blood loss. These vital signs should be closely monitored.
B) Incorrect. Joint pain and swelling are not typical symptoms of gastroesophageal bleeding. They may be indicative of other health issues.
C) Incorrect. Visual disturbances and blurred vision are not common symptoms of gastroesophageal bleeding. These symptoms may be indicative of other health issues.
D) Incorrect. Elevated blood glucose levels are not directly related to gastroesophageal bleeding. They may be indicative of other health issues.
Explanation
Rationale
A) Correct. Signs of shock in gastroesophageal bleeding may include pale skin, rapid breathing, confusion, and other indicators of inadequate tissue perfusion due to blood loss.
B) Incorrect. Joint pain and stiffness are not typical signs of shock in gastroesophageal bleeding. They may be indicative of other health issues.
C) Incorrect. Visual disturbances and blurred vision are not common signs of shock in gastroesophageal bleeding. They may be indicative of other health issues.
D) Incorrect. Elevated blood pressure and heart rate are not typical signs of shock in gastroesophageal bleeding. In fact, blood pressure may decrease as a result of blood loss.
Explanation
Rationale
A) Incorrect. Kidney stones are not a direct complication of gastroesophageal bleeding. They are unrelated conditions.
B) Incorrect. Peptic ulcers can be a cause of gastroesophageal bleeding, but they are not a complication of the bleeding itself.
C) Correct. Anemia can result from gastroesophageal bleeding due to the loss of red blood cells. This can lead to symptoms such as fatigue, weakness, and pallor.
D) Incorrect. Migraine headaches are not a direct complication of gastroesophageal bleeding. They are unrelated conditions.
Explanation
Rationale
A) Incorrect. Consuming alcohol, even in moderation, can contribute to gastroesophageal bleeding. It is advisable to limit or avoid alcohol.
B) Correct. Maintaining a healthy, balanced diet with an emphasis on foods rich in fiber and nutrients can help support digestive health and reduce the risk of gastroesophageal bleeding.
C) Incorrect. Engaging in high-intensity exercise is important for cardiovascular health, but it is not directly related to the prevention of gastroesophageal bleeding. Dietary modifications and careful medication management are more relevant in this context.
D) Incorrect. Seeking medical attention for minor aches and pains is important for overall health and well-being and is not a risk factor for gastroesophageal bleeding.
Explanation
Rationale
A) Correct. A complete blood count (CBC) is an important diagnostic test for gastroesophageal bleeding as it helps assess for anemia resulting from blood loss.
B) Incorrect. An electrocardiogram (ECG) is not a primary diagnostic test for gastroesophageal bleeding. It is used to assess cardiac function.
C) Incorrect. A urine test is not the main diagnostic test for gastroesophageal bleeding. It is used to detect various urinary conditions.
D) Incorrect. A skin biopsy is not commonly performed to diagnose gastroesophageal bleeding. It is used to assess skin changes and conditions.
Explanation
Rationale
A) Correct. An upper gastrointestinal (GI) endoscopy is a direct visualization procedure that allows healthcare providers to examine the esophagus and stomach for any signs of bleeding or other abnormalities.
B) Incorrect. Magnetic resonance imaging (MRI) is a non-invasive imaging technique that may be used for various medical conditions, but it is not the primary test for visualizing the gastrointestinal tract in cases of bleeding.
C) Incorrect. A chest X-ray may be performed for different purposes, but it is not the primary test for visualizing the esophagus and stomach.
D) Incorrect. Positron emission tomography (PET) scans are used to detect metabolic activity in the body and are not typically used as a primary diagnostic test for gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Esophageal manometry measures the pressure and coordination of the muscles in the esophagus. It is not a test involving contrast material.
B) Incorrect. An upper gastrointestinal (GI) series involves swallowing a contrast material, but it is not the primary test for visualizing the esophagus and stomach in cases of bleeding.
C) Incorrect. Endoscopic ultrasound involves the use of an endoscope and ultrasound to visualize the gastrointestinal tract, but it does not typically involve swallowing a contrast material.
D) Correct. A barium swallow study, or upper GI series, involves swallowing a contrast material (barium) that coats the inside of the esophagus and stomach, allowing for better visualization during X-rays.
Explanation
Rationale
A) Correct. Capsule endoscopy involves swallowing a small wireless capsule that contains a camera to capture images as it passes through the gastrointestinal tract. It is useful for visualizing areas that are not easily reached with traditional endoscopy.
B) Incorrect. Upper gastrointestinal (GI) endoscopy involves using a flexible tube with a camera to directly visualize the esophagus and stomach.
C) Incorrect. Esophageal manometry measures the pressure and coordination of the muscles in the esophagus. It does not involve placing a wireless capsule.
D) Incorrect. Endoscopic ultrasound involves the use of an endoscope and ultrasound to visualize the gastrointestinal tract, but it does not involve placing a wireless capsule.
Explanation
Rationale
A) Incorrect. Capsule endoscopy involves swallowing a small wireless capsule with a camera to capture images as it passes through the gastrointestinal tract. It does not evaluate the pressure and coordination of the esophageal muscles.
B) Incorrect. Upper gastrointestinal (GI) endoscopy involves using a flexible tube with a camera to directly visualize the esophagus and stomach. It does not evaluate the esophageal muscle function.
C) Correct. Esophageal manometry is a diagnostic test that evaluates the pressure and coordination of the muscles in the esophagus. It is useful in assessing conditions related to esophageal motility.
D) Incorrect. Endoscopic ultrasound involves the use of an endoscope and ultrasound to visualize the gastrointestinal tract, but it does not evaluate the pressure and coordination of the esophageal muscles.
Explanation
Rationale
A) Incorrect. Taking over-the-counter NSAIDs can exacerbate gastroesophageal bleeding as they may irritate the gastrointestinal tract. It is advisable to avoid them in this situation.
B) Correct. Seeking immediate medical attention is crucial if a client experiences symptoms of gastroesophageal bleeding such as vomiting blood (hematemesis) or passing dark, tarry stools (melena). This ensures timely evaluation and treatment.
C) Incorrect. Engaging in high-intensity exercise may exacerbate the bleeding and is not recommended as part of the initial management of gastroesophageal bleeding.
D) Incorrect. Increasing alcohol consumption can contribute to gastroesophageal bleeding, so it is important to avoid alcohol in this situation.
Explanation
Rationale
A) Correct. Lying down and remaining still can help reduce blood flow during episodes of bleeding. This is an important first step in managing gastroesophageal bleeding at home.
B) Incorrect. Administering aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) can exacerbate gastroesophageal bleeding and is not recommended.
C) Incorrect. It is important for the client to stay hydrated, even during episodes of bleeding. Avoiding food or fluid intake can lead to dehydration and further complications.
D) Incorrect. Chewing on ice chips is not a recommended intervention for managing gastroesophageal bleeding. It is important to seek immediate medical attention.
Explanation
Rationale
A) Incorrect. Increasing intake of spicy foods can irritate the gastrointestinal tract and potentially worsen gastroesophageal bleeding. It is not recommended.
B) Correct. Avoiding hot beverages and foods can help prevent further irritation of the gastrointestinal lining, which is important for managing gastroesophageal bleeding.
C) Incorrect. Consuming large quantities of alcohol can contribute to gastroesophageal bleeding and is not recommended.
D) Correct. Incorporating iron-rich foods in the diet is important for supporting recovery from anemia, which can occur due to blood loss from gastroesophageal bleeding.
Explanation
Rationale
A) Correct. Nonsteroidal anti-inflammatory drugs (NSAIDs) can increase the risk of gastrointestinal bleeding and should be avoided in individuals with gastroesophageal bleeding.
B) Incorrect. While anticoagulants can increase the risk of bleeding, their use and management should be determined by a healthcare provider based on individual circumstances.
C) Incorrect. Proton pump inhibitors (PPIs) are actually used to reduce stomach acid production and can be beneficial in the management of gastroesophageal bleeding.
D) Incorrect. Antibiotics are not typically contraindicated for gastroesophageal bleeding. They may be prescribed if there is evidence of bacterial infection.
Explanation
Rationale
A) Incorrect. Maintaining a low-fiber diet is not typically recommended for managing gastroesophageal bleeding. A balanced diet with emphasis on fiber-rich foods is generally advised.
B) Correct. Regular follow-up appointments with a healthcare provider are important for monitoring any recurrence of bleeding or complications associated with gastroesophageal bleeding.
C) Incorrect. While physical activity is important for overall health, intense physical activity is not specifically indicated for preventing further bleeding in individuals with gastroesophageal bleeding.
D) Incorrect. Seeking immediate medical attention for any symptoms of gastroesophageal bleeding is crucial for timely evaluation and treatment. Delaying medical care can lead to complications.
Explanation
Rationale
A) Correct. Lifting heavy objects or engaging in strenuous physical activities can increase blood pressure and strain, potentially exacerbating gastroesophageal bleeding. It is important to avoid such activities.
B) Incorrect. Engaging in intense aerobic exercise may increase blood pressure and should be avoided to prevent exacerbation of gastroesophageal bleeding.
C) Incorrect. Taking hot baths is not specifically related to managing gastroesophageal bleeding. It is important to focus on activities that do not exacerbate bleeding.
D) Incorrect. While a diet high in fiber and roughage is generally beneficial for digestive health, it is not directly related to preventing further bleeding in cases of gastroesophageal bleeding.
Explanation
Rationale
A) Correct. Monitoring vital signs, especially blood pressure and heart rate, is crucial for assessing the client's hemodynamic stability and response to treatment for gastroesophageal bleeding.
B) Incorrect. Administering aspirin regularly is contraindicated in cases of gastroesophageal bleeding, as it can exacerbate bleeding.
C) Incorrect. Encouraging rigorous physical activities is not recommended for clients with gastroesophageal bleeding, as it can increase the risk of bleeding and further complications.
D) Incorrect. Allowing the client to self-administer medications without supervision may not be safe, especially in cases of gastroesophageal bleeding where careful medication management is essential.
Explanation
Rationale
A) Incorrect. Increasing intake of foods high in fiber and fluids is generally beneficial for digestive health, but it may not specifically prevent further bleeding in cases of gastroesophageal bleeding.
B) Incorrect. Consuming spicy foods can potentially irritate the gastrointestinal tract, which may exacerbate gastroesophageal bleeding. It is not recommended.
C) Incorrect. Limiting fluid intake is not advisable, as it may lead to dehydration. It is important to stay adequately hydrated, especially in cases of bleeding.
D) Correct. Avoiding alcohol and caffeine is important in managing gastroesophageal bleeding, as they can contribute to further bleeding and irritation of the gastrointestinal tract.
Explanation
Rationale
A) Correct. Proton pump inhibitors (PPIs) are commonly used to reduce stomach acid production, which can help prevent further bleeding in cases of gastroesophageal bleeding.
B) Incorrect. Anticoagulants may be used for specific medical conditions, but they are not typically administered to prevent further bleeding in cases of gastroesophageal bleeding.
C) Incorrect. Nonsteroidal anti-inflammatory drugs (NSAIDs) can exacerbate gastroesophageal bleeding and are generally avoided in this situation.
D) Incorrect. Antibiotics may be prescribed if there is evidence of bacterial infection, but they are not used specifically to prevent further bleeding in cases of gastroesophageal bleeding.
Explanation
Rationale
A) Incorrect. Taking over-the-counter NSAIDs can exacerbate gastroesophageal bleeding and is not recommended.
B) Incorrect. Seeking immediate medical attention for any symptoms of gastroesophageal bleeding is crucial for timely evaluation and treatment. Delaying medical care can lead to complications.
C) Correct. Seeking regular follow-up appointments with a healthcare provider is important for ongoing monitoring and management of gastroesophageal bleeding to prevent complications and ensure appropriate treatment.
D) Incorrect. Engaging in high-intensity exercise is not specifically indicated for preventing further bleeding in individuals with gastroesophageal bleeding. It may even exacerbate the bleeding.
Pancreatitis
Explanation
A) Incorrect. GERD primarily involves acid reflux and heartburn, not severe upper abdominal pain.
B) Incorrect. PUD is characterized by ulcers in the stomach or duodenum, which may cause pain, but it typically doesn't present with severe upper abdominal pain and nausea.
C) Correct. Pancreatitis is characterized by severe upper abdominal pain, nausea, and vomiting. It is often a result of inflammation of the pancreas.
D) Incorrect. Gastritis involves inflammation of the stomach lining and can cause abdominal discomfort, but it is not typically associated with severe upper abdominal pain.
Explanation
A) Incorrect. Alcohol abuse is indeed a significant risk factor for pancreatitis, especially when consumed excessively.
B) Correct. Excessive alcohol intake is a well-known risk factor for the development of both acute and chronic pancreatitis.
C) Incorrect. Drug abuse can also contribute to the development of pancreatitis, but alcohol consumption is a recognized risk factor.
D) Incorrect. Moderate alcohol consumption is less likely to lead to pancreatitis compared to heavy or excessive drinking, but it still carries some risk.
Explanation
A) Incorrect. Continuing with the regular diet, especially without modifications, may exacerbate symptoms in a client with acute pancreatitis.
B) Incorrect. While a clear liquid diet may be indicated initially, it is not the long-term dietary recommendation for someone with acute pancreatitis.
C) Incorrect. A high-fat, low-carbohydrate diet is not recommended for someone with pancreatitis, as it can exacerbate symptoms.
D) Correct. Starting with a low-fat, bland diet and gradually advancing as tolerated is a common dietary recommendation for clients with acute pancreatitis. This approach allows the pancreas to rest and recover.
Explanation
A) Correct. Elevated levels of serum amylase are indicative of pancreatic inflammation and are a common diagnostic marker for pancreatitis.
B) Incorrect. Elevated serum creatinine levels may be seen in kidney dysfunction but are not specific to pancreatitis.
C) Incorrect. Hemoglobin levels may be affected in various conditions, but they are not a specific marker for pancreatitis.
D) Incorrect. Platelet counts may be affected in different medical conditions, but they are not specific to pancreatitis.
Explanation
A) Incorrect. Pancreatitis is associated with several potential complications, including pancreatic pseudocysts.
B) Correct. One potential complication of pancreatitis is the development of pancreatic pseudocysts, which are collections of fluid and tissue debris that form in or around the pancreas.
C) Incorrect. While gallstones can contribute to pancreatitis, they are not a complication that arises from pancreatitis itself.
D) Incorrect. Hypertension is not a typical complication of pancreatitis. There are other potential complications that are more directly related to the condition.
Explanation
A) Incorrect. Excessive alcohol consumption is a significant risk factor for the development of pancreatitis.
B) Correct. Having a history of gallstones or gallbladder disease increases the risk of pancreatitis, as gallstones can obstruct the pancreatic duct, leading to inflammation.
C) Incorrect. Being physically inactive is not a direct risk factor for pancreatitis, but other factors such as obesity and high triglyceride levels, which may be associated with inactivity, can contribute to the risk.
D) Incorrect. Age and gender can play a role in the risk of developing pancreatitis. Older age and being male are associated with an increased risk.
Explanation
A) Incorrect. While family history of diabetes is a relevant factor for assessing diabetes risk, it is not a direct risk factor for pancreatitis.
B) Correct. Recent unexplained weight loss can be an indicator of underlying pancreatic issues, including pancreatitis.
C) Incorrect. History of asthma is not directly related to the risk of developing pancreatitis.
D) Incorrect. Frequent dental check-ups are not a direct risk factor for pancreatitis.
Explanation
A) Incorrect. Smoking is not a direct risk factor for pancreatitis, but it poses other serious health risks.
B) Correct. Excessive alcohol consumption is a significant risk factor for pancreatitis. Advising the client to limit alcohol intake can help reduce the risk.
C) Incorrect. Engaging in regular exercise is generally beneficial for overall health, but it may not directly impact the risk of developing pancreatitis.
D) Incorrect. Consuming a high-fat diet can contribute to the risk of pancreatitis, especially if it leads to obesity or high triglyceride levels.
Explanation
A) Incorrect. A history of lung cancer is not directly associated with an increased risk of pancreatitis.
B) Correct. Chronic liver disease, including conditions like cirrhosis, can increase the risk of pancreatitis due to shared factors and pathways related to liver and pancreatic function.
C) Incorrect. Having a strong family history of skin conditions is not a direct risk factor for pancreatitis.
D) Incorrect. Being a vegetarian is not a direct risk factor for pancreatitis. However, certain dietary habits within a vegetarian diet (e.g., high fat or alcohol consumption) could contribute to the risk.
Explanation
A) Incorrect. Diabetes can impact the pancreas, potentially increasing the risk of pancreatitis.
B) Correct. Having diabetes can increase the risk of developing pancreatitis. Diabetes can affect the pancreas and its functions, potentially contributing to the development of pancreatitis.
C) Incorrect. Diabetes is associated with an increased risk of pancreatitis, rather than a reduction in risk.
D) Incorrect. The relationship between diabetes and pancreatitis is understood, and it is known that diabetes can be a risk factor for pancreatitis.
Explanation
A) Incorrect. Pancreatitis is not primarily caused by a bacterial infection in the pancreas. Infections can be secondary complications in some cases.
B) Correct. The main cause of pancreatitis is inflammation and damage to the pancreatic tissue, often due to factors like gallstones, alcohol abuse, or certain medications.
C) Incorrect. While excessive production of digestive enzymes can contribute to pancreatitis, it is not the primary cause.
D) Incorrect. A lack of blood flow to the pancreas (ischemia) can be a contributing factor in some cases, but it is not the primary cause of pancreatitis.
Explanation
A) Incorrect. Autodigestion is not related to insulin release from the pancreas.
B) Correct. Autodigestion is the process in which pancreatic enzymes are prematurely activated within the pancreas, leading to the digestion and damage of pancreatic tissue.
C) Incorrect. Autodigestion is actually a harmful process that leads to further damage of the pancreas, rather than a protective mechanism.
D) Incorrect. The process of converting food into absorbable nutrients occurs in the small intestine, not the pancreas.
Explanation
A) Incorrect. Bile duct obstruction can be a contributing factor in the development of acute pancreatitis.
B) Correct. Bile duct obstruction can lead to the backup of bile and digestive enzymes in the pancreas, which can contribute to the development of pancreatitis.
C) Incorrect. Bile duct obstruction can be associated with both acute and chronic pancreatitis, depending on the underlying cause.
D) Incorrect. Bile duct obstruction primarily affects the flow of bile, not the production of insulin by the pancreas.
Explanation
A) Incorrect. Trypsin is not a hormone responsible for regulating blood sugar levels.
B) Correct. Trypsin is a digestive enzyme produced by the pancreas. When it is prematurely activated within the pancreas, it can lead to tissue damage, contributing to the development of pancreatitis.
C) Incorrect. Trypsin is not a neurotransmitter; it is a digestive enzyme.
D) Incorrect. Trypsin is not responsible for regulating the production of bile in the pancreas.
Explanation
A) Incorrect. High levels of calcium in the blood (hypercalcemia) are not a direct cause of pancreatitis.
B) Incorrect. Low levels of calcium in the blood (hypocalcemia) are not directly associated with an increased risk of developing pancreatitis.
C) Correct. In pancreatitis, calcium can accumulate in the pancreas and form deposits, contributing to tissue damage and inflammation.
D) Incorrect. Calcium does play a role in the development and progression of pancreatitis, particularly in the form of calcium deposits within the pancreatic tissue.
Explanation
A) Incorrect. GERD primarily involves acid reflux and heartburn, not severe upper abdominal pain.
B) Incorrect. PUD is characterized by ulcers in the stomach or duodenum, which may cause pain, but it typically doesn't present with severe upper abdominal pain and nausea.
C) Correct. Pancreatitis is characterized by severe upper abdominal pain, nausea, and vomiting. It is often a result of inflammation of the pancreas.
D) Incorrect. Gastritis involves inflammation of the stomach lining and can cause abdominal discomfort, but it is not typically associated with severe upper abdominal pain.
Explanation
A) Incorrect. Visual disturbances are not typically associated with pancreatitis. They may be related to other conditions or causes.
B) Incorrect. Severe lower back pain is not a characteristic symptom of pancreatitis. It may be indicative of other issues.
C) Correct. Jaundice, characterized by yellowing of the skin and eyes, can occur in pancreatitis due to the obstruction of the bile duct by inflamed pancreatic tissue.
D) Incorrect. Tingling in the extremities is not a common symptom of pancreatitis. It may be indicative of nerve-related issues or other conditions.
Explanation
A) Incorrect. GERD primarily involves acid reflux and heartburn, not severe upper abdominal pain.
B) Incorrect. PUD is characterized by ulcers in the stomach or duodenum, which may cause pain, but it typically doesn't present with severe upper abdominal pain and nausea.
C) Correct. Pancreatitis is characterized by severe upper abdominal pain, nausea, and vomiting. It is often a result of inflammation of the pancreas.
D) Incorrect. Gastritis involves inflammation of the stomach lining and can cause abdominal discomfort, but it is not typically associated with severe upper abdominal pain.
Explanation
A) Incorrect. Alcohol abuse is indeed a significant risk factor for pancreatitis, especially when consumed excessively.
B) Correct. Excessive alcohol intake is a well-known risk factor for the development of both acute and chronic pancreatitis.
C) Incorrect. Drug abuse can also contribute to the development of pancreatitis, but alcohol consumption is a recognized risk factor.
D) Incorrect. Moderate alcohol consumption is less likely to lead to pancreatitis compared to heavy or excessive drinking, but it still carries some risk.
Explanation
A) Incorrect. Continuing with the regular diet, especially without modifications, may exacerbate symptoms in a client with acute pancreatitis.
B) Incorrect. While a clear liquid diet may be indicated initially, it is not the long-term dietary recommendation for someone with acute pancreatitis.
C) Incorrect. A high-fat, low-carbohydrate diet is not recommended for someone with pancreatitis, as it can exacerbate symptoms.
D) Correct. Starting with a low-fat, bland diet and gradually advancing as tolerated is a common dietary recommendation for clients with acute pancreatitis. This approach allows the pancreas to rest and recover.
Explanation
A) Correct. Elevated levels of serum amylase are indicative of pancreatic inflammation and are a common diagnostic marker for pancreatitis.
B) Incorrect. Elevated serum creatinine levels may be seen in kidney dysfunction but are not specific to pancreatitis.
C) Incorrect. Hemoglobin levels may be affected in various conditions, but they are not a specific marker for pancreatitis.
D) Incorrect. Platelet counts may be affected in different medical conditions, but they are not specific to pancreatitis.
Explanation
A) Incorrect. Pancreatitis is associated with several potential complications, including pancreatic pseudocysts.
B) Correct. One potential complication of pancreatitis is the development of pancreatic pseudocysts, which are collections of fluid and tissue debris that form in or around the pancreas.
C) Incorrect. While gallstones can contribute to pancreatitis, they are not a complication that arises from pancreatitis itself.
D) Incorrect. Hypertension is not a typical complication of pancreatitis. There are other potential complications that are more directly related to the condition.
Explanation
A) Incorrect. Excessive alcohol consumption is a significant risk factor for the development of pancreatitis.
B) Correct. Having a history of gallstones or gallbladder disease increases the risk of pancreatitis, as gallstones can obstruct the pancreatic duct, leading to inflammation.
C) Incorrect. Being physically inactive is not a direct risk factor for pancreatitis, but other factors such as obesity and high triglyceride levels, which may be associated with inactivity, can contribute to the risk.
D) Incorrect. Age and gender can play a role in the risk of developing pancreatitis. Older age and being male are associated with an increased risk.
Explanation
A) Incorrect. While family history of diabetes is a relevant factor for assessing diabetes risk, it is not a direct risk factor for pancreatitis.
B) Correct. Recent unexplained weight loss can be an indicator of underlying pancreatic issues, including pancreatitis.
C) Incorrect. History of asthma is not directly related to the risk of developing pancreatitis.
D) Incorrect. Frequent dental check-ups are not a direct risk factor for pancreatitis.
Explanation
A) Incorrect. Smoking is not a direct risk factor for pancreatitis, but it poses other serious health risks.
B) Correct. Excessive alcohol consumption is a significant risk factor for pancreatitis. Advising the client to limit alcohol intake can help reduce the risk.
C) Incorrect. Engaging in regular exercise is generally beneficial for overall health, but it may not directly impact the risk of developing pancreatitis.
D) Incorrect. Consuming a high-fat diet can contribute to the risk of pancreatitis, especially if it leads to obesity or high triglyceride levels.
Explanation
A) Incorrect. A history of lung cancer is not directly associated with an increased risk of pancreatitis.
B) Correct. Chronic liver disease, including conditions like cirrhosis, can increase the risk of pancreatitis due to shared factors and pathways related to liver and pancreatic function.
C) Incorrect. Having a strong family history of skin conditions is not a direct risk factor for pancreatitis.
D) Incorrect. Being a vegetarian is not a direct risk factor for pancreatitis. However, certain dietary habits within a vegetarian diet (e.g., high fat or alcohol consumption) could contribute to the risk.
Explanation
A) Incorrect. Diabetes can impact the pancreas, potentially increasing the risk of pancreatitis.
B) Correct. Having diabetes can increase the risk of developing pancreatitis. Diabetes can affect the pancreas and its functions, potentially contributing to the development of pancreatitis.
C) Incorrect. Diabetes is associated with an increased risk of pancreatitis, rather than a reduction in risk.
D) Incorrect. The relationship between diabetes and pancreatitis is understood, and it is known that diabetes can be a risk factor for pancreatitis.
Explanation
A) Incorrect. Pancreatitis is not primarily caused by a bacterial infection in the pancreas. Infections can be secondary complications in some cases.
B) Correct. The main cause of pancreatitis is inflammation and damage to the pancreatic tissue, often due to factors like gallstones, alcohol abuse, or certain medications.
C) Incorrect. While excessive production of digestive enzymes can contribute to pancreatitis, it is not the primary cause.
D) Incorrect. A lack of blood flow to the pancreas (ischemia) can be a contributing factor in some cases, but it is not the primary cause of pancreatitis.
Explanation
A) Incorrect. Autodigestion is not related to insulin release from the pancreas.
B) Correct. Autodigestion is the process in which pancreatic enzymes are prematurely activated within the pancreas, leading to the digestion and damage of pancreatic tissue.
C) Incorrect. Autodigestion is actually a harmful process that leads to further damage of the pancreas, rather than a protective mechanism.
D) Incorrect. The process of converting food into absorbable nutrients occurs in the small intestine, not the pancreas.
Explanation
A) Incorrect. Bile duct obstruction can be a contributing factor in the development of acute pancreatitis.
B) Correct. Bile duct obstruction can lead to the backup of bile and digestive enzymes in the pancreas, which can contribute to the development of pancreatitis.
C) Incorrect. Bile duct obstruction can be associated with both acute and chronic pancreatitis, depending on the underlying cause.
D) Incorrect. Bile duct obstruction primarily affects the flow of bile, not the production of insulin by the pancreas.
Explanation
A) Incorrect. Trypsin is not a hormone responsible for regulating blood sugar levels.
B) Correct. Trypsin is a digestive enzyme produced by the pancreas. When it is prematurely activated within the pancreas, it can lead to tissue damage, contributing to the development of pancreatitis.
C) Incorrect. Trypsin is not a neurotransmitter; it is a digestive enzyme.
D) Incorrect. Trypsin is not responsible for regulating the production of bile in the pancreas.
Explanation
A) Incorrect. High levels of calcium in the blood (hypercalcemia) are not a direct cause of pancreatitis.
B) Incorrect. Low levels of calcium in the blood (hypocalcemia) are not directly associated with an increased risk of developing pancreatitis.
C) Correct. In pancreatitis, calcium can accumulate in the pancreas and form deposits, contributing to tissue damage and inflammation.
D) Incorrect. Calcium does play a role in the development and progression of pancreatitis, particularly in the form of calcium deposits within the pancreatic tissue.
Explanation
A) Incorrect. GERD primarily involves acid reflux and heartburn, not severe upper abdominal pain.
B) Incorrect. PUD is characterized by ulcers in the stomach or duodenum, which may cause pain, but it typically doesn't present with severe upper abdominal pain and nausea.
C) Correct. Pancreatitis is characterized by severe upper abdominal pain, nausea, and vomiting. It is often a result of inflammation of the pancreas.
D) Incorrect. Gastritis involves inflammation of the stomach lining and can cause abdominal discomfort, but it is not typically associated with severe upper abdominal pain.
Explanation
A) Incorrect. Visual disturbances are not typically associated with pancreatitis. They may be related to other conditions or causes.
B) Incorrect. Severe lower back pain is not a characteristic symptom of pancreatitis. It may be indicative of other issues.
C) Correct. Jaundice, characterized by yellowing of the skin and eyes, can occur in pancreatitis due to the obstruction of the bile duct by inflamed pancreatic tissue.
D) Incorrect. Tingling in the extremities is not a common symptom of pancreatitis. It may be indicative of nerve-related issues or other conditions.
Explanation
A) Incorrect. Continuing with the regular diet, especially without modifications, may exacerbate symptoms in a client with acute pancreatitis.
B) Incorrect. While a clear liquid diet may be indicated initially, it is not the long-term dietary recommendation for someone with acute pancreatitis.
C) Incorrect. A high-fat, low-carbohydrate diet is not recommended for someone with pancreatitis, as it can exacerbate symptoms.
D) Correct. Starting with a low-fat, bland diet and gradually advancing as tolerated is a common dietary recommendation for clients with acute pancreatitis. This approach allows the pancreas to rest and recover.
Explanation
A) Incorrect. While elevated serum amylase and lipase levels can be indicative of pancreatitis, they are not definitive indicators. Additional assessments and clinical findings are necessary for a confirmed diagnosis.
B) Incorrect. While normal levels of serum amylase and lipase may make pancreatitis less likely, they do not completely rule out the possibility of the condition.
C) Correct. Elevated serum amylase and lipase levels are commonly seen in pancreatitis, but they are not exclusive to this condition. Further assessment, including clinical signs and imaging, is needed for a definitive diagnosis.
D) Incorrect. Monitoring serum amylase and lipase levels is an important aspect of evaluating pancreatitis, as they can provide valuable information about pancreatic function.
Explanation
A) Incorrect. Pancreatitis is associated with several potential complications, including pancreatic pseudocysts.
B) Correct. One potential complication of pancreatitis is the development of pancreatic pseudocysts, which are collections of fluid
and tissue debris that form in or around the pancreas.
C) Incorrect. While gallstones can contribute to pancreatitis, they are not a complication that arises from pancreatitis itself.
D) Incorrect. Hypertension is not a typical complication of pancreatitis. There are other potential complications that are more directly related to the condition.
Explanation
A) Correct. Imaging studies like ultrasound, CT scan, and MRI are commonly used to visualize the pancreas and assess for signs of inflammation or other abnormalities.
B) Incorrect. While blood tests are important in the diagnostic process, they are not the primary tests for diagnosing pancreatitis. Elevated levels of amylase and lipase are commonly seen, but they are not exclusive to pancreatitis.
C) Incorrect. While a pancreatic biopsy may be performed in some cases, it is not considered the gold standard for diagnosing pancreatitis. It is usually reserved for more complex or uncertain cases.
D) Incorrect. There are specific diagnostic tests for pancreatitis, including imaging studies and blood tests. Clinical symptoms are important, but they alone are not sufficient for a definitive diagnosis.
Explanation
A) Incorrect. Serum amylase and lipase tests do not directly visualize the pancreas. They measure enzyme levels that can indicate pancreatic inflammation.
B) Correct. Serum amylase and lipase tests are important diagnostic tools for pancreatitis. Elevated levels of these enzymes can indicate pancreatic inflammation.
C) Incorrect. Serum amylase and lipase tests are not used to assess blood sugar levels. They are specific to measuring pancreatic enzyme levels.
D) Incorrect. Serum amylase and lipase tests are primarily used to assess pancreatic function and diagnose pancreatitis, not to identify gallbladder issues.
Explanation
A) Incorrect. ERCP is not a surgical procedure for removing a portion of the pancreas. It is an endoscopic procedure.
B) Correct. ERCP involves passing a flexible tube with a camera through the mouth to visualize and, if needed, treat issues in the pancreas and bile ducts.
C) Incorrect. ERCP is not a blood test. It is an endoscopic procedure used to directly visualize the pancreas and bile ducts.
D) Incorrect. ERCP does involve the use of imaging, but it is done through an endoscope with a camera, not through X-rays.
Explanation
A) Incorrect. Serum amylase is a commonly used test for pancreatitis, but it is not as specific or sensitive as some other tests.
B) Incorrect. Serum lipase is also used in the diagnosis of pancreatitis, but endoscopic ultrasound (EUS) is considered more sensitive and specific.
C) Incorrect. Abdominal ultrasound is a valuable imaging tool for visualizing the pancreas, but it may not always provide as detailed information as an endoscopic ultrasound.
D) Correct. Endoscopic ultrasound (EUS)
is considered a highly specific and sensitive indicator of pancreatic injury. It allows for detailed imaging of the pancreas and surrounding structures.
Explanation
A) Correct. A CT scan is a valuable diagnostic tool for pancreatitis. It provides detailed images of the pancreas and adjacent structures, aiding in the diagnosis and assessment of the severity of pancreatitis.
B) Incorrect. While a CT scan can visualize blood vessels, it is not used specifically to assess blood flow in the pancreas.
C) Incorrect. A CT scan does not measure levels of pancreatic enzymes; it provides imaging of the pancreas.
D) Incorrect. A CT scan is used for imaging internal structures like the pancreas, not for assessing lung function.
Explanation
A) Incorrect. Continuing with the regular diet, especially without modifications, may exacerbate symptoms in a client with acute pancreatitis.
B) Incorrect. While a clear liquid diet may be indicated initially, it is not the long-term dietary recommendation for someone with acute pancreatitis.
C) Incorrect. A high-fat, low-carbohydrate diet is not recommended for someone with pancreatitis, as it can exacerbate symptoms.
D) Correct. Starting with a low-fat, bland diet and gradually advancing as tolerated is a common dietary recommendation for clients with acute pancreatitis. This approach allows the pancreas to rest and recover.
Explanation
A) Incorrect. Resuming regular exercise immediately after discharge may not be advisable, especially if it places additional stress on the pancreas. The client should follow medical recommendations for activity.
B) Correct. Avoiding alcohol and smoking is crucial for preventing further stress and damage to the pancreas, which can exacerbate pancreatitis.
C) Incorrect. Consuming high-fat foods is not recommended for pancreatitis, as they can exacerbate symptoms. The emphasis should be on a low-fat, bland diet.
D) Incorrect. Monitoring blood sugar levels may be necessary, especially if the client has developed diabetes as a result of pancreatitis or has pre-existing diabetes.
Explanation
A) Incorrect. While certain pain medications may need to be used cautiously in pancreatitis, it is not necessary to avoid all pain medications. The healthcare provider will determine appropriate options.
B) Incorrect. NSAIDs should generally be avoided in pancreatitis, as they can exacerbate the condition.
C) Correct. Pain management for pancreatitis may include medications like acetaminophen or opioids, prescribed by the healthcare provider as needed.
D) Incorrect. While some herbal remedies and alternative therapies may provide complementary support, they should not be the sole or primary method of pain relief in pancreatitis.
Explanation
A) Correct. Monitoring blood glucose levels is crucial in severe pancreatitis, as it can lead to the development of diabetes or exacerbate existing diabetes.
B) Incorrect. While blood pressure should be monitored, it is not the primary focus in severe pancreatitis.
C) Incorrect. Respiratory rate is important, but it is not the primary focus in severe pancreatitis.
D) Incorrect. Body temperature is relevant, but it is not the primary focus in severe pancreatitis.
Explanation
A) Incorrect. Pancreatitis is associated with several potential complications, including pancreatic pseudocysts.
B) Correct. One potential complication of pancreatitis is the development of pancreatic pseudocysts, which are collections of fluid and tissue debris that form in or around the pancreas.
C) Incorrect. While gallstones can contribute to pancreatitis, they are not a complication that arises from pancreatitis itself.
D) Incorrect. Hypertension is not a typical complication of pancreatitis. There are other potential complications that are more directly related to the condition.
Explanation
A) Incorrect. Alcohol does not promote healing of the pancreas; in fact, it can worsen inflammation and complications.
B) Correct. Abstaining from alcohol is crucial in pancreatitis, as it can exacerbate inflammation of the pancreas and lead to further complications.
C) Incorrect. Even moderate alcohol intake is not advisable in pancreatitis, as any amount of alcohol can potentially worsen the condition.
D) Incorrect. Alcohol does have an impact on pancreatitis, and it can worsen the condition. Abstaining from alcohol is a critical aspect of treatment.
Explanation
A) Incorrect. The supine position with legs elevated is not typically recommended for a client with pancreatitis, as it may not provide optimal comfort or relief.
B) Correct. The left lateral decubitus position can help alleviate discomfort in clients with pancreatitis by reducing pressure on the pancreas and promoting drainage of pancreatic enzymes.
C) Incorrect. While the High Fowler's position may be suitable for some conditions, it may not be the most comfortable position for a client with pancreatitis.
D) Incorrect. The prone position is not typically recommended for clients with pancreatitis, as it may not provide the necessary comfort and relief.
Explanation
A) Incorrect. Limiting fluid intake can lead to dehydration, which is particularly important to avoid in clients with pancreatitis.
B) Incorrect. While hydration is important, consuming an excessive amount of water can potentially stress the kidneys.
C) Correct. It's important for clients with pancreatitis to maintain adequate fluid intake to prevent dehydration. However, excessive amounts of fluids should be avoided, as they can potentially worsen the condition.
D) Incorrect. Avoiding all fluids until symptoms completely resolve is not advisable, as it may lead to dehydration and exacerbate the condition.
Explanation
A) Correct. Applying a heating pad to the abdomen can help alleviate discomfort in clients with pancreatitis by promoting relaxation and improving blood flow to the area.
B) Incorrect. Regularly administering over-the-counter pain relievers may not be appropriate, as they can have side effects and may not adequately address the pain associated with chronic pancreatitis.
C) Incorrect. Consuming high-fat foods is not advisable for clients with pancreatitis, as they can exacerbate symptoms.
D) Incorrect. Limiting physical activity may not be the most effective approach for managing pain in clients with chronic pancreatitis. Gentle movement and exercise, as tolerated, can be beneficial.
Explanation
A) Incorrect. Even moderate alcohol intake is not advisable in pancreatitis, as any amount of alcohol can potentially worsen the condition.
B) Correct. Abstaining from alcohol is crucial in pancreatitis, as it can exacerbate inflammation of the pancreas and lead to further complications.
C) Incorrect. Consuming alcohol, even in small amounts, is not recommended for individuals with pancreatitis.
D) Incorrect. Alcohol intake should be completely avoided, not just restricted during acute flare-ups, to prevent exacerbation of pancreatitis.
Appendicitis
Explanation
A) Incorrect. This statement provides incorrect information about appendicitis. It describes cholecystitis, an inflammation of the gallbladder.
B) Correct. This statement accurately describes appendicitis as an inflammation of the appendix, a small pouch located in the lower right side of the abdomen. This condition can lead to serious complications if not promptly treated.
C) Incorrect. This statement describes a condition involving ulcers in the stomach lining, which is not appendicitis.
D) Incorrect. This statement describes gastroenteritis, an infection of the small intestine, which is different from appendicitis.
Explanation
A) Incorrect. Rebound tenderness in the lower right abdomen is a later sign of appendicitis and may not be present in the early stages.
B) Incorrect. Severe, sudden-onset abdominal pain in the upper abdomen is not a typical early symptom of appendicitis. The pain usually starts around the navel and then migrates to the lower right abdomen.
C) Incorrect. Diarrhea and frequent bowel movements are not typically associated with early-stage appendicitis.
D) Correct. Nausea and loss of appetite are common early symptoms of appendicitis. As inflammation progresses, other symptoms like abdominal pain and tenderness may develop.
Explanation
A) Incorrect. This statement provides incorrect information about the location of the appendix. The appendix is not located in the upper left quadrant.
B) Incorrect. The appendix is not situated in the lower left quadrant near the sigmoid colon. Its typical location is in the lower right quadrant.
C) Correct. The appendix is usually located in the lower right quadrant of the abdomen, near the right hip bone. This is a key anatomical feature when assessing for appendicitis.
D) Incorrect. The appendix is not found in the upper right quadrant near the liver. Its location is in the lower right quadrant.
Explanation
A) Incorrect. Mild, intermittent abdominal pain that lasts for several days may be a sign of various conditions, but it is not the characteristic presentation of appendicitis.
B) Correct. Severe, constant abdominal pain that starts around the navel and then migrates to the lower right abdomen is a classic symptom of appendicitis. This requires prompt medical attention.
C) Incorrect. Occasional bloating and gas after meals are not specific symptoms of appendicitis.
D) Incorrect. Muscle soreness in the upper back is not typically associated with appendicitis. It may be indicative of other issues.
Explanation
A) Incorrect. Applying a heating pad may provide temporary relief but will not address the underlying cause of appendicitis. It is important to seek medical attention.
B) Incorrect. Taking over-the-counter laxatives is not recommended for suspected appendicitis. It is important to seek proper medical evaluation and treatment.
C) Incorrect. Avoiding solid foods may lead to dehydration and is not recommended. It is important to maintain hydration and seek prompt medical attention.
D) Correct. This option emphasizes the importance of seeking immediate medical attention if the client experiences worsening pain, fever, or vomiting, as these could be signs of a progressing appendicitis and require urgent evaluation and treatment.
Explanation
A) Incorrect. Having a high-fiber diet rich in fruits and vegetables is generally considered beneficial for digestive health, but it is not a recognized risk factor for appendicitis.
B) Correct. A history of previous episodes of appendicitis is a known risk factor. Once a person has had appendicitis, they are at a higher risk of experiencing it again in the future.
C) Incorrect. Engaging in regular physical exercise and maintaining a healthy weight are positive lifestyle choices but are not considered risk factors for appendicitis.
D) Incorrect. Frequent consumption of spicy foods is not identified as a risk factor for appendicitis.
Explanation
A) Incorrect. While gastrointestinal bleeding is a separate concern, it is not a recognized risk factor specifically for appendicitis.
B) Incorrect. Being a non-smoker is a positive health behavior but is not identified as a risk factor for appendicitis.
C) Correct. Having a history of ulcerative colitis, which is an inflammatory bowel disease, is a potential predisposing condition for developing appendicitis.
D) Incorrect. Maintaining a vegetarian diet is generally considered a healthy dietary choice but is not identified as a specific risk factor for appendicitis.
Explanation
A) Incorrect. Being physically active and participating in regular exercise are generally positive behaviors for overall health but are not identified as risk factors for appendicitis.
B) Correct. Having a family history of appendicitis is a recognized risk factor. Genetics can play a role in predisposing individuals to develop appendicitis.
C) Incorrect. Consuming a diet low in processed foods and high in fiber is generally considered beneficial for digestive health but is not specifically identified as a risk factor for appendicitis.
D) Incorrect. Avoiding the use of nonsteroidal anti-inflammatory drugs (NSAIDs) is advisable for some individuals but is not considered a specific risk factor for appendicitis.
Explanation
A) Correct. Appendicitis is most common in adolescents and young adults, although it can occur at any age.
B) Incorrect. While appendicitis can occur in middle-aged adults, it is most commonly seen in adolescents and young adults.
C) Incorrect. Appendicitis is less common in senior citizens, but it can still occur in this age group.
D) Incorrect. Age does impact the risk of developing appendicitis, with the highest incidence occurring in adolescents and young adults.
Explanation
A) Correct. Being male is identified as a risk factor for appendicitis. Males have a slightly higher incidence of appendicitis compared to females.
B) Incorrect. While appendicitis can occur in both males and females, being female is not identified as a specific risk factor for the condition.
C) Incorrect. Gender does influence the risk of developing appendicitis, with males being at slightly higher risk.
D) Incorrect. Having a history of allergies is not recognized as a risk factor for appendicitis.
Explanation
A) Incorrect. This statement provides an inaccurate explanation of the development of appendicitis. It does not primarily result from an accumulation of stool.
B) Correct. Appendicitis is typically caused by an infection, often due to obstruction of the appendix by fecal material, lymphoid hyperplasia, or a foreign body. This leads to inflammation of the appendix.
C) Incorrect. Excessive alcohol consumption is not a recognized cause of appendicitis.
D) Incorrect. While genetics may play a role in certain cases, the primary cause of appendicitis is infection and subsequent inflammation.
Explanation
A) Correct. If appendicitis is left untreated, the inflamed appendix can eventually rupture or perforate, leading to the spread of infection and potential development of peritonitis.
B) Incorrect. Without intervention, appendicitis typically does not resolve on its own. Instead, it can lead to complications.
C) Incorrect. The appendix does not typically reduce in size over time without treatment. In fact, it can become more inflamed and enlarged.
D) Incorrect. While the immune system does respond to the infection, untreated appendicitis can lead to serious complications, including perforation, rather than strengthening the immune system.
Explanation
A) Incorrect. Appendicitis is primarily caused by infection and subsequent inflammation, not an allergic reaction.
B) Correct. An infection can lead to the obstruction of the appendix, causing an increase in pressure within the appendix. This increased pressure leads to inflammation and the characteristic symptoms of appendicitis.
C) Incorrect. While infection can lead to inflammation and dilation of the appendix, the primary mechanism is obstruction due to the infection.
D) Incorrect. The infection itself does not directly damage the nerves in the appendix. The pain associated with appendicitis is a result of the inflammation and increased pressure.
Explanation
A) Correct. In the early stages of appendicitis, inflammation leads to irritation of the abdominal lining, resulting in symptoms like nausea and loss of appetite.
B) Incorrect. Rebound tenderness is a later sign of appendicitis and may not be present in the early stages.
C) Incorrect. Fever and an elevated white blood cell count typically occur as the infection progresses, which is a later stage of appendicitis.
D) Incorrect. Severe, constant abdominal pain in the lower right quadrant is a classic symptom, but it tends to develop after the initial nausea and loss of appetite.
Explanation
A) Incorrect. While chronic abdominal pain can be a complication of appendicitis, the primary concern with delayed surgery is the risk of appendix rupture.
B) Correct. Without timely intervention, an inflamed appendix may rupture, leading to the spread of infection and potentially serious complications like peritonitis.
C) Incorrect. Appendicitis typically does not resolve on its own without intervention.
D) Incorrect. Delaying surgery is not recommended, as it increases the risk of appendix rupture and the spread of infection. Prompt surgical intervention is crucial.
Explanation
A) Incorrect. While sharp, stabbing pain in the lower right abdomen is a characteristic symptom of appendicitis, it tends to develop as the condition progresses.
B) Correct. Nausea and loss of appetite are common early symptoms of appendicitis. Inflammation in the early stages can lead to irritation of the abdominal lining, resulting in these symptoms.
C) Incorrect. Severe, constant pain radiating to the back is not a typical early sign of appendicitis. This type of pain is more commonly associated with other conditions.
D) Incorrect. Feeling bloated and experiencing excessive gas are not specific early signs of appendicitis. These symptoms may be present in various digestive conditions.
Explanation
A) Correct. Rebound tenderness in the lower right abdomen is a hallmark symptom that often occurs in the later stages of appendicitis. It indicates peritoneal irritation and is a sign of potential appendix perforation.
B) Incorrect. While severe, constant abdominal pain in the lower right quadrant is a characteristic symptom of appendicitis, it may occur in both early and later stages.
C) Incorrect. A low-grade fever and elevated white blood cell count are indicative of an inflammatory response and may occur in the later stages of appendicitis, but they are not as specific as rebound tenderness.
D) Incorrect. Diarrhea and frequent bowel movements are not typically associated with appendicitis. Constipation is a more common gastrointestinal symptom in this condition.
Explanation
A) Incorrect. The pain associated with appendicitis is not typically felt in the upper left abdomen near the stomach.
B) Incorrect. The lower left abdomen near the sigmoid colon is not the typical location for appendicitis-related pain.
C) Correct. The characteristic location of pain in appendicitis is in the lower right abdomen, near the right hip bone. This is a key clinical feature used in assessment.
D) Incorrect. The pain of appendicitis is not typically centered in the upper right abdomen near the liver.
Explanation
A) Incorrect. Severe, constant abdominal pain in the lower right quadrant is indicative of appendicitis, but it does not specifically indicate perforation.
B) Incorrect. While an elevated heart rate and blood pressure may be present in response to pain or infection, they are not specific indications of appendix perforation.
C) Incorrect. Rebound tenderness in the lower right abdomen is an important clinical sign of appendicitis but is not specific to perforation.
D) Correct. Fever and signs of sepsis, including an elevated temperature, increased heart rate, and other systemic symptoms, can indicate the presence of infection due to appendix perforation.
Explanation
A) Incorrect. Applying a heating pad may provide temporary relief but will not address the underlying cause of appendicitis. It is important to seek medical attention.
B) Incorrect. Taking over-the-counter laxatives is not recommended for suspected appendicitis. It is important to seek proper medical evaluation and treatment.
C) Incorrect. Avoiding food and liquids can lead to dehydration and is not recommended. It is important to maintain hydration and seek prompt medical attention.
D) Correct. This option emphasizes the importance of seeking immediate medical attention if the client experiences worsening pain, fever, or vomiting, as these could be signs of a progressing appendicitis and require urgent evaluation and treatment.
Explanation
A) Incorrect. While ultrasound can be used in the evaluation of appendicitis, it is not considered the most definitive test. It may be less accurate in certain cases, such as in individuals with obesity.
B) Correct. A CT scan is considered the most definitive test for diagnosing appendicitis. It provides detailed images of the appendix and surrounding structures, allowing for accurate assessment.
C) Incorrect. Blood tests for infection markers, such as white blood cell count and C-reactive protein, can support the diagnosis of appendicitis, but they are not as definitive as a CT scan.
D) Incorrect. Abdominal X-rays are not typically used as a primary diagnostic tool for appendicitis. They may be performed to rule out other conditions, but they do not provide detailed information about the appendix itself.
Explanation
A) Incorrect. While a physical examination is an important component of the diagnostic process, its primary purpose is to assess for signs and symptoms that may suggest appendicitis. It does not definitively confirm the presence of appendicitis.
B) Correct. One of the main purposes of a physical examination in the diagnostic process for appendicitis is to identify alternative causes of abdominal pain. This helps in ruling out other conditions that may mimic appendicitis.
C) Incorrect. A physical examination does not directly visualize the appendix. Imaging studies like ultrasound or CT scan are used for direct visualization.
D) Incorrect. The primary purpose of a physical examination in the context of appendicitis is to assess for signs and symptoms indicative of the condition, rather than assessing overall gastrointestinal system function.
Explanation
A) Incorrect. Blood tests do not directly visualize the inflamed appendix. They provide information about markers of infection and inflammation in the body.
B) Incorrect. While blood tests can support the diagnosis of appendicitis, they do not confirm it on their own. They provide additional information to aid in the diagnostic process.
C) Correct. Blood tests, specifically white blood cell count and C-reactive protein levels, provide valuable information about infection markers and inflammation in the body. Elevated levels may suggest the presence of an inflammatory process like appendicitis.
D) Incorrect. Blood tests are not primarily used to assess gastrointestinal motility. They are focused on assessing markers of infection and inflammation.
Explanation
A) Incorrect. While ultrasound can provide images of the appendix and surrounding structures, the level of detail may be limited compared to a CT scan.
B) Incorrect. A CT scan is considered the most definitive test for diagnosing appendicitis, not ultrasound.
C) Correct. Ultrasound is particularly effective in obese individuals because it does not rely on radiation and can provide clear images of the appendix in individuals with higher body mass index.
D) Incorrect. Ultrasound does not allow for direct visualization of the inside of the appendix. It provides external images of the appendix and surrounding area.
Explanation
A) Incorrect. A urine test does not directly identify the presence of bacteria in the appendix. It assesses components of urine, not the contents of the appendix.
B) Incorrect. While a urine test can provide information about kidney function and fluid balance, it is not specifically related to the evaluation of appendicitis.
C) Correct. A urine test is relevant in the evaluation of appendicitis because it can help rule out urinary tract infection (UTI) as the cause of abdominal pain. UTI symptoms can sometimes mimic those of appendicitis.
D) Incorrect. A urine test does not directly visualize the appendix. It assesses components of urine, not the anatomy of the abdominal organs.
Explanation
A) Incorrect. While antibiotics may be used in some cases, the primary intervention for appendicitis is surgical removal of the inflamed appendix (appendectomy).
B) Incorrect. Non-pharmacological pain management techniques may provide some relief, but they are not the primary treatment for appendicitis.
C) Correct. Appendectomy is the mainstay of treatment for appendicitis. It involves the surgical removal of the inflamed appendix to prevent complications.
D) Incorrect. Bed rest and observation alone are not sufficient for the treatment of appendicitis. Surgical intervention is typically required.
Explanation
A) Correct. In the immediate post-operative period after an appendectomy, it is crucial to closely monitor the client for signs of infection, such as fever, increased pain, and abnormal wound drainage.
B) Incorrect. While early ambulation is important for preventing complications after surgery, in the immediate post-operative period, monitoring for signs of infection takes precedence.
C) Incorrect. Administering IV antibiotics may be part of the post-operative care plan, but it is not the top priority. Monitoring for signs of infection is more critical.
D) Incorrect. Administering pain medication is important for managing pain, but it is not the top priority in the immediate post-operative period. Monitoring for signs of infection takes precedence.
Explanation
A) Incorrect. Hydrogen peroxide can be too harsh for wound care and may hinder the healing process. It is not recommended for routine use on surgical incisions.
B) Correct. Keeping the incision site clean and dry is essential for preventing infection. The client should also be instructed to promptly report any signs of infection, such as increased redness, swelling, or drainage.
C) Incorrect. Adhesive tape may be used in some cases, but it is not the primary method for wound care. Keeping the incision clean and dry is more important.
D) Incorrect. While antibiotic ointment may be prescribed by the healthcare provider, it should be used as directed and not rubbed onto the incision indiscriminately.
Explanation
A) Incorrect. While some restrictions on physical activity are necessary, avoiding all activity for two weeks is overly restrictive and not typically recommended.
B) Incorrect. Resuming normal activities immediately after surgery is not advisable. There should be a gradual return to regular activities based on the healthcare provider's guidance.
C) Correct. After an appendectomy, clients are generally advised to avoid heavy lifting and strenuous activities for a period of 4-6 weeks to allow for proper healing.
D) Incorrect. Engaging in vigorous exercise immediately after surgery can be detrimental to the healing process and may lead to complications. Gradual return to exercise is advised under healthcare provider guidance.
Explanation
A) Incorrect. Mild tenderness around the incision site is common after surgery. It may not necessarily indicate a complication, especially if it is within a reasonable level of discomfort.
B) Correct. Fever, increased pain, and abnormal wound drainage are potential signs of infection or other complications and should be reported immediately to the healthcare provider.
C) Incorrect. Mild fatigue and drowsiness are common after surgery and do not necessarily indicate a complication. They are typically expected during the recovery period.
D) Incorrect. Temporary loss of appetite can be a normal part of the recovery process and may not necessarily indicate a complication. It is important to focus on overall recovery progress.
Explanation
A) Incorrect. Applying a heating pad directly to the incision site can increase the risk of burns or other complications. It is not recommended for post-operative pain management.
B) Correct. Taking prescribed pain medication as directed by the healthcare provider is an essential component of post-operative pain management. This ensures adequate pain relief and promotes comfort during the recovery period.
C) Incorrect. Avoiding pain medication is not recommended, especially after surgery. Pain management is important for the client's comfort and well-being during the recovery process.
D) Incorrect. While deep breathing exercises can be helpful for relaxation, they are not a substitute for prescribed pain medication, particularly in the immediate post-operative period.
Explanation
A) Correct. Following a clear liquid diet for the first 24 hours after surgery is a common post-operative instruction. This helps prevent nausea and allows the digestive system to gradually return to normal function.
B) Incorrect. Resuming a regular diet immediately after waking up from anesthesia is not advisable. The digestive system needs time to recover after surgery.
C) Incorrect. Avoiding all oral intake for the first 48 hours after surgery can lead to dehydration and is not a standard practice for appendectomy recovery.
D) Incorrect. Starting with solid foods right away can be too harsh on the digestive system after surgery. A clear liquid diet is typically initiated first to allow for a gradual transition.
Explanation
A) Incorrect. Keeping the incision site open to air is not recommended. It should be covered with a clean, dry dressing to prevent infection.
B) Incorrect. Applying hydrogen peroxide to the incision site daily can be too harsh and may hinder the healing process. It is not a standard practice for wound care.
C) Correct. Cleaning the incision site gently with soap and water and then covering it with a clean, dry dressing is the recommended approach for wound care after an appendectomy.
D) Incorrect. It is important for the client to gently clean the incision site as part of wound care. Avoiding touching the site altogether is not necessary, but the hands should be clean when doing so.
Explanation
A) Incorrect. Administering pain medication is important for managing pain, but it is not the top priority in the immediate post-operative period. Monitoring for complications takes precedence.
B) Incorrect. While coughing and deep breathing exercises are important for preventing respiratory complications, they are not the top priority immediately after surgery. Monitoring for other potential complications comes first.
C) Correct. Monitoring for signs of infection or complications is a priority in the immediate post-operative period. Early identification and intervention can prevent further issues.
D) Incorrect. Promoting early ambulation and mobility is important, but it is not the top priority in the immediate post-operative period. Monitoring for complications takes precedence.
Explanation
A) Incorrect. Avoiding handwashing can actually increase the risk of infection. It is important to maintain good hand hygiene to reduce the introduction of germs.
B) Incorrect. Changing the wound dressing with unwashed hands can introduce germs and increase the risk of infection. Hands should be clean before handling the incision site.
C) Correct. Keeping the incision site dry and clean is essential for preventing infection. Additionally, promptly reporting any signs of infection, such as increased redness, swelling, or drainage, allows for early intervention.
D) Incorrect. While some physical activity may need to be limited, avoiding all physical activity is not necessary. It is important to follow healthcare provider guidance on activity restrictions.
Inflammatory bowel disease
Explanation
A) Incorrect. While IBD involves inflammation, it is not primarily an autoimmune condition. The exact cause of IBD is not fully understood, but it is believed to involve a combination of genetic, environmental, and immune factors.
B) Correct. Inflammatory Bowel Disease is a chronic condition that involves inflammation of the gastrointestinal tract. It includes conditions like Crohn's disease and ulcerative colitis.
C) Incorrect. IBD is not caused by a bacterial infection. It is a complex condition with multiple contributing factors.
D) Incorrect. IBD is a chronic condition and does not resolve on its own with time. It requires ongoing management and treatment.
Explanation
A) Correct. Abdominal pain and cramping are common symptoms shared by both Crohn's disease and ulcerative colitis, which are the two main types of Inflammatory Bowel Disease.
B) Incorrect. Rapid weight gain is not a typical symptom of Inflammatory Bowel Disease. In fact, weight loss is often a concern for individuals with IBD.
C) Incorrect. Elevated blood sugar levels are not directly associated with Inflammatory Bowel Disease. This is more relevant to conditions like diabetes.
D) Incorrect. Vision changes and eye pain are not common symptoms of Inflammatory Bowel Disease. They may be indicative of other health issues.
Explanation
A) Incorrect. Kidney stones are not a direct complication of Inflammatory Bowel Disease. They may be associated with certain dietary habits or conditions, but they are not a primary concern in IBD.
B) Correct. Osteoporosis can be a complication of untreated or poorly managed Inflammatory Bowel Disease. This is due, in part, to factors such as malabsorption of nutrients and long-term steroid use, which can lead to bone density loss.
C) Incorrect. Migraine headaches are not a common complication of Inflammatory Bowel Disease. They are separate conditions with different causes.
D) Incorrect. Allergic reactions are not a direct complication of Inflammatory Bowel Disease. They may occur in individuals with allergies but are not specifically related to IBD.
Explanation
A) Incorrect. A high-fiber diet, particularly one rich in fruits and vegetables, can be too rough on the digestive system for individuals with Inflammatory Bowel Disease. It may exacerbate symptoms.
B) Correct. A low-residue diet with limited fiber intake is often recommended for managing symptoms of Inflammatory Bowel Disease. This diet reduces the bulk and frequency of stools, which can help alleviate discomfort.
C) Incorrect. A high-fat diet is not typically recommended for individuals with Inflammatory Bowel Disease. It may lead to additional digestive challenges and is not the primary focus of dietary modifications.
D) Incorrect. While reducing caffeine intake can be beneficial for some individuals with gastrointestinal conditions, it is not the primary diet modification recommended for managing Inflammatory Bowel Disease.
Explanation
A) Incorrect. Surgery is not typically the first-line treatment for Inflammatory Bowel Disease. It is usually reserved for cases where medical management has not been successful or in specific situations where surgery is indicated.
B) Correct. Surgery is rarely the initial approach in managing Inflammatory Bowel Disease. It is considered as a last resort when other treatment options have been exhausted or when specific complications necessitate surgical intervention.
C) Incorrect. Surgery for Inflammatory Bowel Disease is not primarily for cosmetic purposes. It is conducted to address underlying disease processes and complications.
D) Incorrect. Surgery for Inflammatory Bowel Disease is not limited to cases of acute infections. It may be considered for various reasons, including complications related to the disease itself.
Explanation
A) Incorrect. Having a family history of IBD does indeed increase the risk of developing the condition. It is considered a relevant risk factor.
B) Correct. A family history of IBD is associated with a slightly increased risk of developing the condition. While it does elevate the risk, it is not an absolute guarantee that the individual will develop IBD.
C) Incorrect. While a family history of IBD does increase the risk, it does not "significantly" increase the risk in the sense that everyone with a family history will develop the condition.
D) Incorrect. A family history of IBD increases the risk for all immediate family members, including the client.
Explanation
A) Incorrect. Physical inactivity is not considered a specific environmental risk factor for IBD. While a healthy lifestyle is important, it is not a direct cause of the condition.
B) Correct. Exposure to secondhand smoke is a known environmental risk factor for developing Inflammatory Bowel Disease. It has been associated with an increased risk of IBD.
C) Incorrect. A high-fiber diet is not considered an environmental risk factor for IBD. In fact, dietary choices are more relevant to the management of IBD rather than its development.
D) Incorrect. A low-stress lifestyle is not specifically associated with the development of IBD as an environmental risk factor. While stress management is important for overall health, it is not a direct cause of IBD.
Explanation
A) Incorrect. Frequent antibiotic use has been associated with an increased risk of developing Inflammatory Bowel Disease. It is considered a relevant risk factor.
B) Incorrect. Frequent antibiotic use is actually associated with an increased risk, not a decreased risk, of developing IBD.
C) Correct. Frequent antibiotic use has been linked to an increased risk of developing Inflammatory Bowel Disease. This may be due to alterations in gut microbiota and immune function.
D) Incorrect. Frequent antibiotic use can impact the risk of developing IBD in both children and adults, not exclusively in one group.
Explanation
A) Incorrect. Older age (60+) is not typically associated with an increased risk of developing Inflammatory Bowel Disease. IBD can affect individuals of various age groups.
B) Incorrect. In terms of gender, both males and females are susceptible to Inflammatory Bowel Disease. It does not predominantly affect one gender over the other.
C) Correct. Caucasian ethnicity is associated with a higher risk of developing Inflammatory Bowel Disease. It is more commonly diagnosed in individuals of Caucasian descent.
D) Incorrect. While socioeconomic status can impact access to healthcare and management of chronic conditions, it is not a direct demographic factor associated with an increased risk of IBD.
Explanation
A) Incorrect. While having an appendectomy may be associated with a slightly increased risk of developing Inflammatory Bowel Disease, it does not "significantly" increase the risk.
B) Correct. Having an appendectomy has been linked to a slightly increased risk of developing IBD. However, this risk increase is relatively small.
C) Incorrect. Having an appendectomy does have an impact on the risk of developing IBD, albeit a relatively small one. It is not accurate to say it has no impact.
D) Incorrect. Having an appendectomy does not decrease the risk of developing IBD. It may have a slight influence on the risk, but it is not a protective factor against IBD.
Explanation
A) Incorrect. While bacterial infections can play a role in the exacerbation of IBD symptoms, they are not considered the primary cause of the condition.
B) Correct. The exact cause of Inflammatory Bowel Disease is not fully understood, but it is believed to involve a combination of genetic, environmental, and immune factors. An abnormal immune response in the intestines plays a significant role in the development of IBD.
C) Incorrect. While stress and emotional factors can impact the severity of IBD symptoms, they are not the underlying cause of the condition.
D) Incorrect. While there may be a genetic component to IBD, it is not solely a genetic disorder inherited from parents. It involves a complex interplay of genetic and environmental factors.
Explanation
A) Correct. Chronic inflammation in Inflammatory Bowel Disease can lead to the formation of scar tissue (fibrosis) in the intestines. This can result in narrowing of the intestinal lumen and obstruction.
B) Incorrect. While increased production of digestive enzymes may occur in certain digestive disorders, it is not a primary mechanism involved in the tissue damage seen in IBD.
C) Incorrect. In IBD, cell regeneration is often disrupted, and accelerated cell turnover can contribute to inflammation and tissue damage rather than healing.
D) Incorrect. In IBD, the intestinal mucosa may be weakened rather than strengthened due to chronic inflammation and damage.
Explanation
A) Incorrect. Crohn's disease is not limited to the colon and rectum. It can affect any part of the gastrointestinal tract, from the mouth to the anus.
B) Correct. Crohn's disease is known for its potential to affect any segment of the gastrointestinal tract, making it different from ulcerative colitis, which primarily affects the colon and rectum.
C) Incorrect. Crohn's disease can affect both the small and large intestines, but it is not limited to the small intestine alone.
D) Incorrect. Crohn's disease does not primarily affect the stomach and esophagus. It can involve any part of the gastrointestinal tract, but it most commonly affects the small intestine and colon.
Explanation
A) Incorrect. While genetic factors can contribute to the development of IBD, they are not the sole cause. Environmental factors also play a significant role.
B) Incorrect. Having a family history of IBD increases the risk, but it does not guarantee that an individual will develop the condition.
C) Correct. Genetic factors can predispose individuals to IBD, but the condition is believed to result from a complex interplay of genetic, environmental, and immune factors.
D) Incorrect. Genetic factors do have an influence on the development of IBD, but they are not the only contributing factors.
Explanation
Rationale
A) Incorrect. In IBD, the immune system is actually overactive, leading to chronic inflammation rather than being underactive.
B) Correct. In Inflammatory Bowel Disease, the immune system mistakenly identifies the body's own intestinal tissues as foreign invaders and launches an inflammatory response against them. This is known as an autoimmune response.
C) Incorrect. The immune system plays a central role in the development and progression of Inflammatory Bowel Disease. It is not uninvolved.
D) Incorrect. While the immune system is active in Inflammatory Bowel Disease, its focus is not solely on fighting infections. It is also targeting the body's own intestinal tissues due to a misdirected immune response.
Explanation
A) Incorrect. While rectal bleeding can occur in IBD, it is not the most common symptom. Cramping abdominal pain and diarrhea are more characteristic.
B) Incorrect. While alterations in bowel habits can occur in IBD, the primary pattern is often diarrhea rather than alternating constipation and diarrhea.
C) Incorrect. Frequent heartburn and acid reflux are not characteristic symptoms of Inflammatory Bowel Disease. They are more indicative of conditions like gastroesophageal reflux disease (GERD).
D) Correct. Cramping abdominal pain and diarrhea are hallmark symptoms of Inflammatory Bowel Disease. These symptoms are commonly experienced by individuals with IBD.
Explanation
A) Correct. Joint pain and swelling (arthritis) are common extraintestinal manifestations of Inflammatory Bowel Disease. This can occur concurrently with gastrointestinal symptoms.
B) Incorrect. Visual disturbances are not a typical extraintestinal manifestation of IBD. They may be indicative of other health issues.
C) Incorrect. Elevated blood sugar levels are not directly associated with Inflammatory Bowel Disease. This is more relevant to conditions like diabetes.
D) Incorrect. Respiratory distress is not a common extraintestinal manifestation of IBD. It may be indicative of other respiratory conditions.
Explanation
A) Correct. Ulcerative colitis is characterized by inflammation that is limited to the colon and rectum.
B) Incorrect. Ulcerative colitis primarily affects the colon and rectum, not the small intestine.
C) Incorrect. Unlike Crohn's disease, inflammation in ulcerative colitis is continuous and limited to the colon and rectum, rather than patchy and involving different segments of the gastrointestinal tract.
D) Incorrect. Ulcerative colitis is characterized by continuous inflammation in the colon and rectum. It does not skip segments.
Explanation
A) Incorrect. Anemia can be a complication of Inflammatory Bowel Disease, but it is primarily related to factors like chronic inflammation and bleeding, rather than malabsorption.
B) Incorrect. Hypertension is not directly related to malabsorption or a common complication of Crohn's disease.
C) Incorrect. Hyperthyroidism is not a complication commonly associated with Crohn's disease or malabsorption.
D) Correct. Malabsorption in Crohn's disease can lead to nutrient deficiencies, including calcium and vitamin D, which can contribute to osteoporosis.
Explanation
A) Incorrect. While having IBD does increase the risk of colorectal cancer, it is not accurate to say that it does not affect the risk.
B) Correct. Individuals with Inflammatory Bowel Disease, particularly those with long-standing and extensive disease, have a slightly increased risk of developing colorectal cancer.
C) Incorrect. Colorectal cancer is not guaranteed for everyone with IBD. While the risk is increased, it does not mean everyone with IBD will develop colorectal cancer.
D) Incorrect. While the risk of colorectal cancer is elevated in individuals with IBD, it is not accurate to say that it is "significantly" increased for everyone. The level of risk can vary depending on factors such as the extent and duration of the disease.
Explanation
A) Correct. The initial test often performed for suspected IBD is the fecal occult blood test (FOBT). This test checks for the presence of blood in the stool, which can indicate gastrointestinal bleeding.
B) Incorrect. While colonoscopy is an important diagnostic tool for IBD, it is not typically the first test performed. It is usually conducted after initial screenings like the FOBT.
C) Incorrect. A complete blood count (CBC) may be ordered to assess for signs of anemia or other abnormalities, but it is not the initial screening test for IBD.
D) Incorrect. Abdominal ultrasound is not typically used as an initial diagnostic test for IBD. It may be used for specific purposes, but it is not the first-line test.
Explanation
A) Correct. A barium enema is a radiographic procedure that involves the administration of barium sulfate, which coats the lining of the intestines. This allows for direct visualization of the intestinal tract and detection of abnormalities such as strictures or ulcers.
B) Incorrect. A barium enema is not used to assess blood flow in the gastrointestinal tract. It is primarily used for imaging the anatomy and structure of the intestines.
C) Incorrect. A barium enema does not measure pH levels in the intestines. It is a radiographic procedure for visualizing the intestinal tract.
D) Incorrect. A barium enema is not used to assess muscular function of the intestines. It is primarily used for imaging the anatomy and structure of the intestines.
Explanation
A) Incorrect. A sigmoidoscopy allows for visualization of the lower part of the colon and rectum, but it does not provide images of the entire colon.
B) Incorrect. A sigmoidoscopy primarily examines the lower part of the colon and rectum, not the small intestine.
C) Correct. A sigmoidoscopy is an endoscopic procedure used to assess the lower part of the colon and rectum for signs of inflammation, ulcers, and other abnormalities commonly associated with Inflammatory Bowel Disease.
D) Incorrect. A sigmoidoscopy does not measure pH levels in the gastrointestinal tract. It is an endoscopic procedure for visual examination.
Explanation
A) Correct. Computed tomography (CT) scans are valuable in providing detailed images of the intestinal lining, which can help identify strictures (narrowing) and fistulas (abnormal connections between organs).
B) Incorrect. While CT scans can provide valuable information about the gastrointestinal tract, they are not primarily used to assess blood flow.
C) Incorrect. CT scans do not measure pH levels in the intestines. They are used for imaging rather than biochemical analysis.
D) Incorrect. CT scans are not used to
assess muscular function of the intestines. They primarily provide detailed images of the anatomy.
Explanation
A) Correct. An upper endoscopy (also known as esophagogastroduodenoscopy or EGD) allows for direct visualization of the upper part of the gastrointestinal tract, including the stomach and duodenum.
B) Incorrect. An upper endoscopy primarily examines the upper part of the gastrointestinal tract, not the lower part or ileum.
C) Incorrect. An upper endoscopy does not examine the colon and rectum. It is focused on the upper portion of the gastrointestinal tract.
D) Incorrect. An upper endoscopy does not examine the entire length of the small intestine. It primarily focuses on the upper part, including the duodenum.
Explanation
A) Incorrect. While some individuals with IBD may be lactose intolerant, it is not necessary for all to completely avoid all forms of dairy products. A blanket recommendation like this is not appropriate.
B) Correct. A low-fiber diet can help ease gastrointestinal symptoms in individuals with IBD. It reduces the mechanical irritation on the intestines, which can be particularly beneficial during periods of active inflammation.
C) Incorrect. While a diet rich in fruits, vegetables, and whole grains is generally considered healthy, it may exacerbate symptoms in individuals with IBD, especially during flare-ups.
D) Incorrect. Spicy foods can be irritating to the gastrointestinal tract and are not typically recommended for individuals with IBD, as they can exacerbate symptoms.
Explanation
A) Incorrect. Corticosteroids can lead to increased appetite and weight gain, but this is not the primary concern. Weight loss and muscle weakness are more significant potential side effects.
B) Correct. Corticosteroids can lead to weight loss and muscle weakness due to their catabolic effects on tissues.
C) Incorrect. Elevated blood pressure and increased heart rate are not typically associated with corticosteroid use.
D) Incorrect. While mood swings and changes in behavior can be side effects of corticosteroids, they are not the primary concerns mentioned in the question.
Explanation
A) Incorrect. Staying hydrated is important for individuals with IBD, especially during flare-ups when diarrhea can lead to rapid fluid loss and dehydration.
B) Correct. Maintaining adequate hydration is crucial for individuals with IBD, particularly during flare-ups, as diarrhea can lead to significant fluid loss and the risk of dehydration.
C) Incorrect. It is important for individuals with IBD to stay hydrated, and there is no need to unnecessarily limit fluid intake. Dehydration can exacerbate symptoms.
D) Incorrect. Hydration does have a significant impact on IBD symptoms, particularly in preventing dehydration that can result from diarrhea.
Explanation
A) Incorrect. While exercise is beneficial, vigorous exercise may exacerbate symptoms for some individuals with IBD. Moderate exercise is generally recommended.
B) Incorrect. Avoiding all forms of exercise is not recommended for individuals with IBD. Regular, moderate exercise can be beneficial for overall health and well-being.
C) Correct. Engaging in regular, moderate exercise can help improve overall well-being, reduce stress, and may help manage symptoms associated with IBD.
D) Incorrect. Exercise can have a positive impact on Inflammatory Bowel Disease, particularly in terms of overall health and well-being.
Explanation
A) Incorrect. While probiotics may not be suitable for all individuals with IBD, they do have the potential to be beneficial for some by helping restore a healthy balance of gut bacteria.
B) Incorrect. Probiotics have shown promise in some studies for managing IBD, particularly in helping restore a healthy gut microbiome.
C) Correct. Probiotics can potentially be beneficial in managing IBD by helping restore a healthy balance of gut bacteria. However, it's important to note that their effectiveness can vary from person to person.
D) Incorrect. Probiotics are not considered a primary treatment for Inflammatory Bowel Disease, but they may be used as a complementary approach for some individuals. They are not a substitute for other recommended treatments.
Explanation
A) Incorrect. While a high-fiber diet is generally recommended for digestive health, it may exacerbate symptoms in individuals with IBD, especially during flare-ups.
B) Incorrect. While some types of fiber can exacerbate symptoms, not all types of fiber should be avoided. Soluble fiber sources like oats and bananas can be beneficial for managing IBD.
C) Correct. A balanced diet with soluble fiber sources can be beneficial for individuals with IBD. Soluble fiber helps absorb excess liquid in the intestines and can help regulate bowel movements.
D) Incorrect. Spicy foods can be irritating to the gastrointestinal tract and are not typically recommended for individuals with IBD, as they can exacerbate symptoms.
Explanation
A) Incorrect. It is important to be cautious about infections while taking immunosuppressant medications, as they can weaken the immune system.
B) Correct. Individuals taking immunosuppressants, including those with IBD, should take precautions to avoid close contact with individuals who have infections and practice good hand hygiene to reduce the risk of contracting infections.
C) Incorrect. Immunosuppressants do have an impact on the immune system, and individuals taking these medications are at higher risk of infections.
D) Incorrect. Stopping immunosuppressants without medical guidance can have serious consequences and should never be done without consulting a healthcare provider.
Explanation
A) Incorrect. Stress can impact IBD symptoms, and stress management techniques can be beneficial for individuals with IBD.
B) Correct. Managing stress through relaxation techniques and mindfulness has been shown to reduce the frequency and severity of IBD flare-ups. Stress can exacerbate symptoms, so effective stress management is an important aspect of IBD management.
C) Incorrect. Stress management techniques can have a positive impact on both mental well-being and physical health, including managing IBD.
D) Incorrect. While medication is an important component of IBD management, stress management techniques can complement medication in reducing the frequency and severity of flare-ups.
Explanation
A) Incorrect. While high-fiber foods are generally recommended for digestive health, they may exacerbate symptoms, including diarrhea, in individuals with IBD.
B) Correct. Limiting the intake of dairy products, especially for individuals who are lactose intolerant, can help reduce the risk of diarrhea, a common symptom in IBD.
C) Incorrect. Drinking fluids with meals is generally recommended for hydration and digestion. Avoiding this practice is not a standard recommendation for managing diarrhea.
D) Incorrect. Spicy foods can be irritating to the gastrointestinal tract and are not typically recommended for individuals with IBD, especially if they are experiencing diarrhea.
Explanation
A) Incorrect. Avoiding all forms of physical activity is not recommended for individuals with IBD. Regular, moderate exercise can have positive effects on overall well-being.
B) Correct. Engaging in regular, moderate exercise can help improve overall well-being, reduce stress, and may help manage symptoms associated with IBD.
C) Incorrect. While exercise is beneficial, vigorous exercise may exacerbate symptoms for some individuals with IBD. Moderate exercise is generally recommended.
D) Incorrect. Exercise can have a positive impact on Inflammatory Bowel Disease, particularly in terms of overall health and well-being.
Irritable bowel syndrome
Explanation
A) Incorrect. While structural abnormalities can contribute to gastrointestinal disorders, IBS is not primarily caused by such abnormalities.
B) Correct. The exact cause of IBS is unknown, but it is believed to be a multifactorial condition involving abnormal gut motility, heightened visceral sensitivity, and other factors. Psychological and genetic factors may also play a role.
C) Incorrect. While psychological factors can exacerbate symptoms in some individuals with IBS, they are not the sole cause of the condition.
D) Incorrect. While bacterial infections can lead to similar symptoms, IBS is not primarily caused by infections.
Explanation
A) Incorrect. IBS is a chronic condition, but it does not progress to serious complications or structural damage in the intestines.
B) Correct. IBS is a chronic condition characterized by recurrent abdominal pain, along with changes in bowel habits such as diarrhea, constipation, or both. It does not lead to serious structural damage in the intestines.
C) Incorrect. IBS is a chronic condition, and while it can be managed, it does not have a cure.
D) Incorrect. IBS primarily affects the lower gastrointestinal tract, particularly the colon, and does not primarily involve the esophagus.
Explanation
A) Incorrect. Both diet and stress can be significant triggers for IBS symptoms in many individuals.
B) Correct. Dietary factors, including specific foods and beverages, as well as stress, are common triggers for IBS symptoms. Identifying and managing these triggers is an important aspect of IBS management.
C) Incorrect. While physical activity levels can influence IBS symptoms, it is not the only trigger. In fact, moderate exercise is generally recommended for individuals with IBS.
D) Incorrect. While environmental factors can influence health, they are not typically considered primary triggers for IBS symptoms.
Explanation
A) Correct. The main subtypes of IBS are based on predominant bowel habits: diarrhea-predominant, constipation-predominant, and mixed (alternating between diarrhea and constipation).
B) Incorrect. These options refer to different types of gastrointestinal disorders (Ulcerative Colitis, Crohn's Disease, and Diverticular Disease) rather than subtypes of IBS.
C) Incorrect. These options refer to various types of gastrointestinal inflammation (Gastritis, Duodenitis, and Esophagitis) but are not subtypes of IBS.
D) Incorrect. These options refer to different categories of gastrointestinal disorders but are not subtypes of IBS.
Explanation
A) Incorrect. Stress can indeed impact IBS symptoms, often exacerbating them, so managing stress levels is important for individuals with IBS.
B) Correct. Stress can have a significant impact on IBS symptoms. Practicing stress management techniques can help reduce the frequency and severity of flare-ups.
C) Incorrect. Stress can have physical effects on the body, and it can exacerbate symptoms in individuals with IBS.
D) Incorrect. Stress management techniques can be effective in managing IBS symptoms, particularly in reducing the frequency and severity of flare-ups.
Explanation
A) Incorrect. While IBS can affect anyone, there are indeed specific risk factors associated with its development.
B) Correct. There are several known risk factors for developing IBS, including a history of gastrointestinal infections (such as bacterial gastroenteritis) and certain mental health conditions like anxiety and depression.
C) Incorrect. While there may be a genetic component to IBS, it is not exclusively genetic, and other factors play a role in its development.
D) Incorrect. Consuming a high-fiber diet is not considered a primary risk factor for IBS. In fact, dietary factors are more commonly associated with triggering symptoms in individuals who already have IBS.
Explanation
A) Incorrect. There is indeed a known connection between mental health conditions and the development of IBS.
B) Correct. There is a known link between mental health conditions, particularly anxiety and depression, and the development of IBS. The exact mechanism is not fully understood, but it may involve alterations in gut-brain communication.
C) Incorrect. While managing anxiety and depression can potentially help improve symptoms in individuals with IBS, mental health conditions do not directly cause IBS.
D) Incorrect. The link between mental health conditions and IBS is supported by scientific research, and it is not considered coincidental.
Explanation
A) Incorrect. A history of gastrointestinal infections, especially bacterial gastroenteritis, is indeed associated with an increased risk of developing IBS.
B) Correct. Gastrointestinal infections, particularly bacterial gastroenteritis, have been linked to an increased risk of developing IBS. This is a known risk factor.
C) Incorrect. Both viral and bacterial gastrointestinal infections have been associated with an increased risk of developing IBS.
D) Incorrect. There is a known connection between gastrointestinal infections, especially bacterial gastroenteritis, and the development of IBS.
Explanation
A) Incorrect. There appears to be a genetic component to IBS, so family history can be relevant in understanding a client's risk.
B) Correct. While the exact genetic mechanisms are not fully understood, there does appear to be a genetic component to IBS. Having family members with the condition may increase an individual's risk.
C) Incorrect. While environmental factors can influence IBS, there is also a genetic component to consider.
D) Incorrect. While environmental factors can contribute to the development of IBS, there is a known genetic component as well.
Explanation
A) Incorrect. IBS can develop at any age, and it is not primarily associated with older individuals.
B) Correct. While IBS can develop at any age, it is more commonly diagnosed in younger adults. However, it can also occur in older adults.
C) Incorrect. IBS can affect individuals of all ages, including adults.
D) Incorrect. While age is a factor, IBS can develop in individuals of various age groups, not exclusively in one particular demographic.
Explanation
A) Incorrect. While structural abnormalities can contribute to gastrointestinal disorders, IBS is not primarily caused by such abnormalities.
B) Correct. The exact cause of IBS is not fully understood, but it is believed to be a multifactorial condition involving altered gut motility, heightened visceral sensitivity, and dysfunction in the communication between the brain and gut.
C) Incorrect. While bacterial infections can lead to similar symptoms, IBS is not primarily caused by infections.
D) Incorrect. While psychological factors can exacerbate symptoms in some individuals with IBS, they are not the sole cause of the condition.
Explanation
A) Incorrect. While inflammation may be present in some cases, it is not the primary mechanism of IBS.
B) Correct. One of the key aspects of IBS pathophysiology is abnormal gut motility, which can lead to symptoms like abdominal pain and alterations in bowel habits.
C) Incorrect. While bacterial overgrowth may be a factor in some gastrointestinal disorders, it is not the main cause of IBS.
D) Incorrect. While psychological factors can influence symptoms, IBS has a physical basis involving alterations in gut motility and sensitivity.
Explanation
A) Incorrect. Visceral hypersensitivity is not related to an increased susceptibility to bacterial infections.
B) Correct. Visceral hypersensitivity in IBS means that the gut is more sensitive, leading to an increased perception of pain and discomfort from normal gut activities.
C) Incorrect. While inflammation may be present in some cases of IBS, it is not the primary definition of visceral hypersensitivity.
D) Incorrect. IBS has a physical basis, and visceral hypersensitivity is one aspect of its pathophysiology, not solely a psychological condition.
Explanation
A) Incorrect. The brain-gut axis is indeed relevant to IBS and plays a significant role in its pathophysiology.
B) Correct. The brain-gut axis refers to the bidirectional communication between the central nervous system (brain) and the enteric nervous system (gut). In IBS, this interaction is complex and can influence gut motility, sensitivity, and overall symptom experience.
C) Incorrect. While the brain-gut axis is important, its primary impact in IBS is not related to nutrient absorption.
D) Incorrect. The brain-gut axis is relevant in various gastrointestinal disorders, including IBS, and is not limited to severe psychological disorders.
Explanation
A) Incorrect. Psychological factors can indeed impact IBS, playing a role in both symptom exacerbation and, in some cases, the development of the condition.
B) Correct. While IBS has a physical basis, psychological factors can play a significant role in exacerbating symptoms and may contribute to the development of the condition in certain individuals.
C) Incorrect. While psychological factors can contribute to IBS, they are not the sole cause of the condition.
D) Incorrect. IBS has a physical basis, and psychological factors are one aspect of its complex pathophysiology. They are not the exclusive cause of the condition.
Explanation
A) Incorrect. The symptoms listed, including fever and bloody diarrhea, are not typically associated with IBS. These symptoms may suggest a different gastrointestinal condition.
B) Correct. Common symptoms of IBS include abdominal pain or discomfort, bloating, and alterations in bowel habits, such as diarrhea, constipation, or a combination of both.
C) Incorrect. Symptoms like jaundice, nausea, and vomiting are not characteristic of IBS. They may be indicative of other gastrointestinal disorders.
D) Incorrect. Weight loss and a decreased appetite are not primary symptoms of IBS. These may suggest a different underlying condition.
Explanation
A) Incorrect. While abdominal pain is a common symptom of IBS, it is not typically described as severe and constant. Additionally, abdominal pain in IBS may be relieved after a bowel movement.
B) Correct. A characteristic symptom of IBS is that individuals often experience relief from abdominal pain after having a bowel movement.
C) Incorrect. Significant weight loss and malnutrition are not typical features of IBS. These symptoms may suggest a different underlying condition.
D) Incorrect. The presence of blood in the stool is not a characteristic symptom of IBS. This may indicate a different gastrointestinal disorder.
Explanation
A) Incorrect. Abdominal pain in IBS is typically described as crampy or spasmodic, not constant and severe. Additionally, it is not limited to the lower right quadrant.
B) Correct. The abdominal pain associated with IBS is often described as crampy or spasmodic and is usually located in the lower abdomen.
C) Incorrect. IBS-related abdominal pain is not typically described as sharp and stabbing, and it is not usually felt in the upper abdomen.
D) Incorrect. Abdominal pain is indeed a significant symptom of IBS, and it is often described as crampy or spasmodic, not primarily associated with nausea and vomiting.
Explanation
A) Incorrect. Stress can indeed impact IBS symptoms, exacerbating abdominal pain and altering bowel habits.
B) Correct. Stress is known to exacerbate IBS symptoms, leading to increased abdominal pain and changes in bowel habits.
C) Incorrect. While stress can influence IBS symptoms, it is not the sole cause of the condition. IBS has a complex multifactorial etiology.
D) Incorrect. IBS symptoms are influenced by various factors, including stress, but they are not solely related to dietary factors.
Explanation
A) Incorrect. While constipation can be a symptom of IBS (specifically IBS-C, or constipation-predominant IBS), it is not the only presentation. Other forms of IBS may involve loose, watery stools.
B) Correct. IBS can be characterized by loose, watery stools and frequent bowel movements, particularly in cases of diarrhea-predominant IBS (IBS-D).
C) Incorrect. Constipation can be a symptom of IBS, particularly in cases of constipation-predominant IBS (IBS-C).
D) Incorrect. Bloody stools are not a characteristic symptom of IBS. This may suggest a different gastrointestinal condition.
Explanation
A) Incorrect. Imaging studies like CT scans and MRI are not typically used to diagnose IBS. They may be done to rule out other conditions with similar symptoms.
B) Correct. The diagnosis of IBS is primarily based on clinical criteria, including the presence of characteristic symptoms, and a thorough medical history. There are no specific diagnostic tests for IBS.
C) Incorrect. While a colonoscopy may be performed to rule out other gastrointestinal conditions, it is not considered a specific diagnostic test for IBS.
D) Incorrect. Blood tests are not the primary diagnostic tool for IBS. They may be used to rule out other conditions or to check for signs of inflammation.
Explanation
A) Incorrect. Diagnostic tests for IBS do not primarily focus on identifying specific structural abnormalities in the intestines, as IBS is a functional disorder.
B) Correct. There is no specific test that definitively diagnoses IBS. Instead, it relies on clinical criteria, including the presence of characteristic symptoms and a thorough medical history.
C) Incorrect. While blood tests may be used to rule out other conditions, there is no specialized blood test that definitively diagnoses IBS.
D) Incorrect. Specialized imaging studies like PET scans are not typically used in the diagnosis of IBS. They may be performed to rule out other conditions.
Explanation
A) Incorrect. While blood tests may be used to rule out other conditions, there is no specialized blood test that definitively diagnoses IBS.
B) Correct. There is no specific blood test that definitively diagnoses IBS. Diagnosis is based on clinical criteria, including the presence of characteristic symptoms and a thorough medical history.
C) Incorrect. A standard complete blood count (CBC) is a general blood test and is not specific to diagnosing IBS.
D) Incorrect. There is no specific genetic marker blood test for diagnosing IBS. Diagnosis relies on clinical criteria and medical history.
Explanation
A) Incorrect. There is no specialized genetic test for diagnosing IBS.
B) Correct. A colonoscopy is a diagnostic procedure that allows for direct visualization of the intestines, which can help rule out structural abnormalities or other gastrointestinal conditions with similar symptoms.
C) Incorrect. While bacterial infections can lead to similar symptoms, there is no specific test for bacterial infections associated with IBS.
D) Incorrect. While MRI may be used in certain cases to assess intestinal motility, it is not a primary diagnostic test for IBS and may not be performed in all cases.
Explanation
A) Incorrect. Imaging tests like CT scans and MRI are not the primary diagnostic tools for IBS. They may be used to rule out other conditions with similar symptoms.
B) Correct. Diagnostic imaging tests may be used to rule out other conditions that mimic the symptoms of IBS, but they are not specific to diagnosing IBS. Diagnosis of IBS relies on clinical criteria.
C) Incorrect. An ultrasound is not the definitive imaging test for confirming IBS.
D) Incorrect. While specialized endoscopic procedures may be performed to rule out other conditions, they are not required to definitively diagnose IBS. Diagnosis is based on clinical criteria and medical history.
Explanation
A) Incorrect. While certain types of fiber can exacerbate symptoms in some individuals, it is not recommended to completely avoid all types of fiber. Soluble fiber, found in fruits and vegetables, can be beneficial for individuals with IBS.
B) Correct. Maintaining a well-balanced diet with a focus on soluble fiber, fruits, and vegetables can help manage IBS symptoms.
C) Incorrect. While some individuals may find relief from liquid diets, it is not a general recommendation for managing IBS. A well-balanced diet is preferred.
D) Incorrect. Eliminating all carbohydrates from the diet is not a recommended approach for managing IBS. It is important to have a balanced diet.
Explanation
A) Incorrect. Regular physical activity and exercise are generally recommended for individuals with IBS, as they can help improve symptoms.
B) Correct. Stress management techniques, such as deep breathing exercises and mindfulness, can be beneficial in managing IBS symptoms. Stress can exacerbate IBS symptoms, so learning techniques to manage stress can be helpful.
C) Incorrect. Avoiding social interaction and isolating oneself is not a recommended approach for managing IBS. Maintaining social connections can contribute to overall well-being.
D) Incorrect. Skipping meals and intermittent fasting are not recommended strategies for managing IBS. It is important to have regular, balanced meals to support digestive health.
Explanation
A) Incorrect. Probiotics have shown promise in managing IBS symptoms, particularly strains like Bifidobacteria and Lactobacilli. While not every individual may experience benefits, they can be a helpful addition for some.
B) Correct. Probiotics, especially those containing Bifidobacteria and Lactobacilli strains, have been studied for their potential to alleviate some IBS symptoms. While not a universal solution, they can be a beneficial addition for some individuals.
C) Incorrect. Probiotics can be beneficial for various subtypes of IBS, not limited solely to IBS with constipation.
D) Incorrect. High-dose probiotics are not universally recommended for all individuals with IBS. The choice of probiotic and dosage should be individualized based on the specific needs of the client.
Explanation
A) Correct. It is generally recommended to completely avoid caffeine and alcohol, as they can exacerbate symptoms in individuals with IBS.
B) Incorrect. While moderation is key for many aspects of diet, caffeine and alcohol can be particularly problematic for individuals with IBS, and complete avoidance is often recommended.
C) Incorrect. Caffeine should be eliminated from the diet, and complete avoidance of alcohol is generally recommended for managing IBS.
D) Incorrect. While eliminating alcohol is generally recommended for individuals with IBS, complete avoidance of caffeine is also advised, as it can exacerbate symptoms.
Explanation
A) Incorrect. Stress management techniques, such as deep breathing exercises and mindfulness, can be very beneficial in reducing and managing IBS symptoms. Stress can exacerbate IBS symptoms, so learning techniques to manage stress can be helpful.
B) Correct. Stress management techniques can be very beneficial in reducing and managing IBS symptoms. Stress can exacerbate IBS symptoms, so learning techniques to manage stress can be helpful.
C) Incorrect. Stress management techniques are beneficial for individuals with various subtypes of IBS, not limited to IBS-D (diarrhea-predominant).
D) Incorrect. Stress management techniques are an important aspect of managing IBS and should be considered regardless of the effectiveness of dietary modifications. They can complement other strategies for symptom management.
Explanation
A) Incorrect. Increasing stress levels is not a recommended approach for managing IBS symptoms. Instead, stress reduction techniques are advised.
B) Correct. Regular exercise can help improve bowel function and reduce stress, both of which can benefit individuals with IBS. It's important to engage in moderate, regular physical activity.
C) Incorrect. Avoiding all forms of physical activity is not recommended for managing IBS. Regular, moderate exercise can be beneficial.
D) Incorrect. While cardiovascular workouts can be part of a balanced exercise routine, they should not be the sole focus, and other forms of exercise should also be considered.
Explanation
A) Incorrect. Insoluble fiber can exacerbate diarrhea-predominant symptoms in individuals with IBS. Emphasis should be on soluble fiber sources.
B) Correct. Limiting intake of gas-producing foods like beans and cruciferous vegetables can help manage diarrhea in individuals with IBS. These foods can contribute to increased gas and bloating.
C) Incorrect. Consuming large quantities of high-fat foods is not a recommended approach for managing diarrhea-predominant symptoms in individuals with IBS.
D) Incorrect. Increasing caffeine intake is not recommended for managing diarrhea in individuals with IBS, as it can exacerbate symptoms.
Explanation
A) Incorrect. Certain probiotics, particularly those containing Bifidobacteria and Lactobacilli strains, have been studied for their potential to alleviate some IBS symptoms.
B) Correct. Certain probiotics, particularly those containing Bifidobacteria and Lactobacilli strains, have been studied for their potential to alleviate some IBS symptoms. While not a universal solution, they can be a beneficial addition for some individuals.
C) Incorrect. Probiotics can be beneficial for various subtypes of IBS, not limited solely to IBS-C (constipation-predominant).
D) Incorrect. High-dose probiotics are not universally recommended for all individuals with IBS. The choice of probiotic and dosage should be individualized based on the specific needs of the client.
Explanation
A) Correct. It is generally recommended to completely avoid caffeine and alcohol, as they can exacerbate symptoms in individuals with IBS.
B) Incorrect. While moderation is key for many aspects of diet, caffeine and alcohol can be particularly problematic for individuals with IBS, and complete avoidance is often recommended.
C) Incorrect. Caffeine should be eliminated from the diet
, and complete avoidance of alcohol is generally recommended for managing IBS.
D) Incorrect. While eliminating alcohol is generally recommended for individuals with IBS, complete avoidance of caffeine is also advised, as it can exacerbate symptoms.
Explanation
A) Incorrect. Stress management techniques, such as deep breathing exercises and mindfulness, can be very beneficial in reducing and managing IBS symptoms. Stress can exacerbate IBS symptoms, so learning techniques to manage stress can be helpful.
B) Correct. Stress management techniques can be very beneficial in reducing and managing IBS symptoms. Stress can exacerbate IBS symptoms, so learning techniques to manage stress can be helpful.
C) Incorrect. Stress management techniques are beneficial for individuals with various subtypes of IBS, not limited to IBS-D (diarrhea-predominant).
D) Incorrect. Stress management techniques are an important aspect of managing IBS and should be considered regardless of the effectiveness of dietary modifications. They can complement other strategies for symptom management.
Liver Diseases: Hepatitis, Cirrhosis
Explanation
A) Incorrect. This description is more in line with acute hepatitis, rather than cirrhosis.
B) Correct. Cirrhosis is a chronic liver disease characterized by extensive scarring and fibrosis, which leads to loss of normal liver function.
C) Incorrect. This describes a benign liver tumor, not cirrhosis.
D) Incorrect. Cirrhosis is a chronic condition and is not a temporary impairment of liver function.
Explanation
A) Incorrect. While excessive alcohol consumption can contribute to hepatitis, it is not the exclusive cause.
B) Correct. Hepatitis can be caused by viral infections (e.g., Hepatitis A, B, C), autoimmune disorders, and excessive alcohol consumption.
C) Incorrect. Exposure to certain pesticides and industrial chemicals can contribute to liver damage, but they are not the primary causes of hepatitis.
D) Incorrect. While genetic factors can play a role in some forms of hepatitis, it is not the sole cause, and prevention measures can still be taken.
Explanation
A) Incorrect. Hepatitis B is not primarily transmitted through contaminated food and water.
B) Correct. Hepatitis B is primarily transmitted through contact with infected blood, sexual contact, and from mother to newborn during childbirth.
C) Incorrect. Hepatitis B is not primarily transmitted through respiratory droplets.
D) Incorrect. Hepatitis B is not transmitted through casual contact, but rather through specific modes such as blood, sexual contact, and perinatal transmission.
Explanation
A) Incorrect. Practicing good hand hygiene is essential in preventing the spread of viral hepatitis, especially in healthcare settings.
B) Correct. Avoiding sharing needles or personal items that may be contaminated with blood or other bodily fluids is crucial in preventing hepatitis transmission.
C) Incorrect. Vaccination against viral hepatitis is recommended for various populations, not limited solely to healthcare workers.
D) Incorrect. Consuming raw seafood can pose a risk for certain types of foodborne illnesses, but it is not directly related to the prevention of viral hepatitis.
Explanation
A) Correct. Hepatitis C can be treated with a combination of antiviral medications, and there are several effective treatment options available.
B) Incorrect. There are effective treatments available for Hepatitis C, and lifestyle modifications are typically combined with medical treatment.
C) Incorrect. Surgical intervention may be considered in advanced cases of liver disease, but it is not the primary treatment for Hepatitis C.
D) Incorrect. While liver transplantation may be an option for severe cases of Hepatitis C with advanced liver damage, it is not the only treatment option available. Antiviral medications are the first-line treatment.
Explanation
A) Incorrect. While viral infections can contribute to cirrhosis, they are not the sole cause. Excessive alcohol consumption and other factors can also lead to cirrhosis.
B) Correct. Excessive alcohol consumption, chronic viral hepatitis (especially Hepatitis B and C), and nonalcoholic fatty liver disease are common risk factors for cirrhosis.
C) Incorrect. Exposure to environmental toxins can contribute to liver damage, but it is not the primary cause of cirrhosis.
D) Incorrect. Being overweight or obese, especially in the presence of nonalcoholic fatty liver disease, is a risk factor for the development of cirrhosis.
Explanation
A) Incorrect. Viral hepatitis is not primarily transmitted through contaminated food and water.
B) Correct. Sharing needles for drug use and engaging in unprotected sex with multiple partners are common risk factors for the transmission of viral hepatitis, especially Hepatitis B and C.
C) Incorrect. Viral hepatitis is not primarily transmitted through respiratory droplets.
D) Incorrect. Vaccination against viral hepatitis is recommended for various populations, not limited solely to healthcare workers.
Explanation
A) Incorrect. Heavy alcohol consumption is associated with an increased risk of liver disease, particularly alcoholic liver disease.
B) Correct. Heavy alcohol consumption is a well-known risk factor for alcoholic liver disease, which, if not addressed, can progress to cirrhosis over time.
C) Incorrect. Both chronic heavy alcohol consumption and binge drinking pose risks for liver disease.
D) Incorrect. While genetic factors can play a role, heavy alcohol consumption is a significant risk factor for alcoholic liver disease, regardless of genetic predisposition.
Explanation
A) Incorrect. Nonalcoholic fatty liver disease is not primarily associated with alcohol consumption, as the name suggests. It specifically refers to liver fat accumulation in individuals who do not consume excessive alcohol.
B) Correct. Risk factors for nonalcoholic fatty liver disease (NAFLD) include obesity, insulin resistance, and metabolic syndrome. These factors contribute to the accumulation of fat in the liver.
C) Incorrect. NAFLD is not solely caused by viral infections. Lifestyle factors and metabolic conditions play a significant role.
D) Incorrect. Engaging in regular physical activity can help reduce the risk of developing NAFLD, as it contributes to overall metabolic health.
Explanation
A) Incorrect. Chronic viral hepatitis, especially Hepatitis B and C, can lead to cirrhosis over time if not effectively managed.
B) Correct. Chronic viral hepatitis, especially Hepatitis B and C, can lead to cirrhosis over time, especially if not effectively managed.
C) Incorrect. While family history can play a role in some liver conditions, it is not the sole determinant of cirrhosis.
D) Incorrect. Exposure to environmental toxins can contribute to liver damage, but it is not the primary cause of cirrhosis, especially in cases of chronic viral hepatitis.
Explanation
A) Incorrect. This describes alcoholic hepatitis, not viral hepatitis. Viral hepatitis is caused by specific viruses.
B) Incorrect. Autoimmune hepatitis is a separate condition where the immune system attacks liver cells, but it is not the cause of viral hepatitis.
C) Correct. Viral hepatitis is caused by infection with specific viruses (e.g., Hepatitis A, B, C), leading to inflammation and damage to liver cells.
D) Incorrect. Viral hepatitis is primarily caused by viral infections, not genetic factors.
Explanation
A) Incorrect. While exposure to environmental toxins can contribute to liver damage, it is not the primary cause of cirrhosis.
B) Correct. Cirrhosis is the result of chronic, progressive liver damage and scarring, often stemming from various underlying liver diseases, such as chronic viral hepatitis, excessive alcohol consumption, or nonalcoholic fatty liver disease.
C) Incorrect. This describes autoimmune hepatitis, where the immune system attacks liver cells, but it is not the cause of cirrhosis.
D) Incorrect. Cirrhosis is primarily caused by chronic liver damage, not genetic factors.
Explanation
A) Incorrect. While the virus does cause damage to liver cells, it primarily does so by triggering an immune response, rather than directly killing the cells.
B) Correct. Chronic viral hepatitis leads to an overactive immune response, which damages liver cells over time. The immune system's attempt to fight the virus can inadvertently lead to inflammation and damage.
C) Incorrect. This describes autoimmune hepatitis, where the immune system mistakenly attacks liver cells, but it is not the mechanism of damage in chronic viral hepatitis.
D) Incorrect. This statement does not accurately describe the pathophysiology of chronic viral hepatitis.
Explanation
A) Incorrect. Cirrhosis is a chronic condition that develops over an extended period, often years, rather than rapidly within a few weeks.
B) Correct. In cirrhosis, healthy liver tissue is gradually replaced by scar tissue, which impairs liver function. This progressive replacement of functional tissue with fibrous tissue leads to the loss of normal liver function.
C) Incorrect. While cirrhosis can affect the biliary system, it is not the primary mechanism of damage.
D) Incorrect. Cirrhosis is considered an irreversible condition, although early intervention and treatment can help manage symptoms and slow its progression.
Explanation
A) Incorrect. Cirrhosis actually leads to impaired blood flow through the liver, not increased flow.
B) Correct. Cirrhosis impairs blood flow through the liver, leading to increased pressure in the portal vein (portal hypertension) and potential complications such as esophageal varices.
C) Incorrect. Cirrhosis does affect blood flow through the liver, especially due to the development of fibrous tissue that restricts blood flow.
D) Incorrect. Cirrhosis does not cause blood vessels to constrict, but rather the development of fibrous tissue in the liver hinders blood flow.
Explanation
A) Incorrect. While jaundice, abdominal pain, and fatigue can be seen in chronic hepatitis, they are not always present, and the presentation can vary widely among individuals.
B) Incorrect. Chronic hepatitis can present with noticeable symptoms, especially in the early stages, before it progresses to cirrhosis.
C) Incorrect. Chronic hepatitis primarily affects the liver, not the cardiovascular system.
D) Correct. Signs and symptoms of chronic hepatitis can vary widely among individuals, and some individuals may not exhibit noticeable symptoms, especially in the early stages.
Explanation
A) Correct. Spider angiomas (vascular lesions on the skin), jaundice (yellowing of the skin and eyes), and ascites (accumulation of fluid in the abdomen) are indicative of advanced cirrhosis.
B) Incorrect. Mild fatigue and occasional abdominal discomfort may be present in cirrhosis, but they are not specific indicators of advanced disease.
C) Incorrect. Elevated liver enzymes and occasional nausea can be seen in cirrhosis, but they do not specifically indicate advanced stages.
D) Incorrect. Mild splenomegaly (enlarged spleen) and weight loss can occur in cirrhosis, but they are not as indicative of advanced disease as the combination of spider angiomas, jaundice, and ascites.
Explanation
A) Incorrect. Fever, cough, and shortness of breath are not typical initial symptoms of hepatitis.
B) Correct. In the early stages of hepatitis, individuals may experience flu-like symptoms such as fatigue, muscle aches, and fever.
C) Incorrect. Severe abdominal pain and nausea are not typically the initial symptoms of hepatitis.
D) Incorrect. Joint pain and skin rash are not the primary initial symptoms of hepatitis.
Explanation
A) Incorrect. Mild jaundice can occur in liver disease but is not as concerning as easy bruising and bleeding.
B) Correct. Easy bruising and bleeding are indicative of advanced liver disease, as the liver plays a crucial role in producing clotting factors.
C) Incorrect. Occasional fatigue is a common symptom of liver disease, but it is not as concerning as easy bruising and bleeding.
D) Incorrect. Mild abdominal discomfort can occur in liver disease, but it is not as concerning as easy bruising and bleeding.
Explanation
Rationale
A) Incorrect. Cirrhosis primarily affects the liver, not the kidneys, and is not a direct cause of dark urine due to impaired kidney function.
B) Correct. Light-colored urine, particularly pale or clay-colored, can be a common symptom of cirrhosis, especially in the early stages, due to impaired bilirubin processing by the liver.
C) Incorrect. While urine color is not directly related to cirrhosis, changes in color can occur as a result of liver dysfunction.
D) Incorrect. Blood in the urine (hematuria) is not a typical symptom of cirrhosis and would warrant further evaluation.
Explanation
A) Correct. Diagnostic tests for liver disease often involve a combination of blood tests (such as liver function tests), imaging studies (like ultrasound or MRI), and occasionally a liver biopsy for more detailed evaluation.
B) Incorrect. While physical examination and symptom assessment are important components, they alone are not sufficient for a definitive diagnosis of liver disease.
C) Incorrect. While client-reported symptoms are crucial for assessment, they are not the sole basis for diagnosing liver disease. Objective tests are typically needed.
D) Incorrect. The diagnosis of liver disease does require specific tests for accurate evaluation and determination of the type and extent of liver damage.
Explanation
A) Correct. A liver biopsy is an invasive procedure where a small sample of liver tissue is removed for examination under a microscope to assess for signs of liver disease.
B) Incorrect. A liver biopsy is an invasive procedure involving the removal of tissue, and it is not considered non-invasive.
C) Incorrect. The administration of radioactive tracers is not part of a standard liver biopsy procedure.
D) Incorrect. While a liver biopsy can provide information about the liver's condition, it is not primarily used to measure blood flow through the liver.
Explanation
A) Incorrect. Liver function tests do not directly visualize the liver's structure. They assess biochemical markers in the blood related to liver function.
B) Correct. Liver function tests measure specific markers in the blood to evaluate how well the liver is functioning and to identify signs of damage or dysfunction.
C) Incorrect. Liver function tests do not primarily involve measuring blood flow through the liver. They focus on assessing biochemical markers.
D) Incorrect. While liver function tests can provide information about viral infections in the liver, they are not primarily used for this purpose. Specific viral tests would be ordered if infection is suspected.
Explanation
A) Correct. An abdominal ultrasound is a non-invasive imaging test that uses sound waves to create images of the liver's internal structure and blood flow patterns.
B) Incorrect. An abdominal ultrasound does not involve the injection of a contrast dye. This description may be more applicable to other imaging tests.
C) Incorrect. An abdominal ultrasound does not involve the removal of liver tissue. This is more characteristic of a liver biopsy.
D) Incorrect. While an abdominal ultrasound primarily assesses abdominal organs, including the liver, it does not primarily focus on kidney function.
Explanation
A) Incorrect. While a CT scan provides detailed images of the liver, it does not directly visualize blood flow. It uses X-rays to create images.
B) Correct. A CT scan of the abdomen involves using X-rays to create detailed cross-sectional images of the liver and surrounding structures, providing valuable information about liver function and potential abnormalities.
C) Incorrect. A CT scan does not typically involve the injection of a radioactive tracer. This description may be more applicable to nuclear medicine scans.
D) Incorrect. A CT scan is not an invasive procedure that involves removing liver tissue. This description is more characteristic of a liver biopsy.
Explanation
A) Incorrect. Protein restriction is not necessary in cirrhosis. Instead, a balanced diet with adequate protein is recommended.
B) Correct. Clients with cirrhosis should aim for a balanced diet that includes adequate protein. Sodium restriction is also important to manage fluid retention and prevent complications.
C) Incorrect. Carbohydrates are an essential part of a balanced diet. Avoiding them completely is not recommended.
D) Incorrect. Diet plays a crucial role in the management of cirrhosis. Encouraging unrestricted eating without considering dietary modifications can be detrimental to the client's health.
Explanation
A) Incorrect. Avoiding all physical contact with family members is unnecessary. Transmission precautions can be taken without completely isolating oneself.
B) Correct. Using separate utensils and avoiding sharing personal items can help prevent the transmission of hepatitis, as the virus can be present in bodily fluids.
C) Incorrect. While blood-to-blood contact is a significant mode of transmission, hepatitis can also be transmitted through other bodily fluids, so standard precautions are important.
D) Incorrect. Even if a partner has been vaccinated against hepatitis, it's important to take precautions to prevent transmission, as vaccines are not always 100% effective.
Explanation
A) Incorrect. Even moderate alcohol consumption can exacerbate liver damage in individuals with cirrhosis, so complete avoidance is recommended.
B) Correct. Avoiding alcohol is crucial for individuals with cirrhosis, as any amount of alcohol can further harm the already compromised liver.
C) Incorrect. Even occasional social drinking can have detrimental effects on the liver in individuals with cirrhosis. Complete avoidance is recommended.
D) Incorrect. Alcohol consumption has a significant impact on cirrhosis and can worsen liver damage, so continuing as usual is not advisable.
Explanation
A) Correct. Standard precautions, which include practices such as hand hygiene, wearing gloves, and using personal protective equipment, are essential for preventing the spread of hepatitis.
B) Incorrect. Contact precautions are not specifically required for preventing the spread of hepatitis.
C) Incorrect. Airborne precautions are not necessary for preventing the spread of hepatitis, as it is primarily transmitted through blood and other bodily fluids.
D) Incorrect. Droplet precautions are not necessary for preventing the spread of hepatitis, as it is not primarily transmitted through respiratory droplets.
Explanation
A) Incorrect. Not all over-the-counter pain relievers are safe for individuals with cirrhosis. Some, like acetaminophen, can be harmful to the liver.
B) Correct. Over-the-counter pain relievers containing acetaminophen should be avoided in individuals with cirrhosis, as it can lead to further liver damage.
C) Incorrect. While over-the-counter pain relievers can be effective for managing pain, not all of them are safe for individuals with cirrhosis.
D) Incorrect. Aspirin, like other nonsteroidal anti-inflammatory drugs (NSAIDs), can also be harmful to individuals with cirrhosis and should be used with caution or avoided.
Explanation
A) Incorrect. While regular exercise is important for overall health, particularly for individuals with liver disease, high-intensity exercise may not be suitable for those with cirrhosis. Moderate, low-impact activities are often recommended.
B) Correct. Maintaining a low-sodium diet helps manage fluid retention, and avoiding alcohol is crucial to prevent further liver damage and complications in individuals with cirrhosis.
C) Incorrect. Smoking can exacerbate existing health issues, including those related to cirrhosis. It is advisable to quit smoking to support overall health.
D) Incorrect. Herbal supplements can interact with medications and may not be safe for individuals with liver disease. It's important to consult a healthcare provider before using any supplements.
Explanation
A) Incorrect. Over-the-counter pain relievers may not be effective for alleviating fatigue and weakness associated with hepatitis. Moreover, some pain relievers can be harmful to the liver.
B) Correct. Resting and conserving energy are important interventions for clients experiencing fatigue and weakness, which are common symptoms of hepatitis. Adequate rest supports the body's healing process.
C) Incorrect. While exercise is generally beneficial, scheduling vigorous exercise sessions may be too strenuous for a client experiencing fatigue and weakness. Gentle, low-impact activities are more appropriate.
D) Incorrect. Providing caffeinated beverages may not address the underlying cause of the client's fatigue, and excessive caffeine intake can have negative effects on overall health.
Explanation
A) Incorrect. While protein is important, a high-protein diet may not be suitable for all individuals with cirrhosis. It's important to maintain a balanced diet.
B) Correct. Fruits, vegetables, and whole grains provide essential nutrients and fiber that support overall health, including liver function.
C) Incorrect. Limiting fluid intake to an extreme degree can lead to dehydration, which is not recommended. Instead, individuals with cirrhosis should be mindful of their sodium and fluid intake to manage fluid retention.
D) Incorrect. While protein is important, relying solely on red meat is not recommended. A balanced diet with a variety of protein sources is preferable.
Explanation
A) Incorrect. While protein is important, in the case of hepatic encephalopathy, reducing ammonia levels is the priority. A high-protein diet may exacerbate this condition.
B) Correct. Lactulose is a medication used to reduce ammonia levels in clients with hepatic encephalopathy, which is a complication of advanced cirrhosis.
C) Incorrect. Administering sedatives may worsen hepatic encephalopathy. The focus should be on reducing ammonia levels.
D) Incorrect. Administering iron supplements is not a priority in addressing hepatic encephalopathy. The focus should be on managing ammonia levels.
Explanation
A) Incorrect. Avoiding all contact with family members is unnecessary. Transmission precautions can be taken without completely isolating oneself.
B) Correct. Practicing safe sex and avoiding sharing needles or personal items can significantly reduce the risk of transmitting hepatitis C to others.
C) Incorrect. Hepatitis C is primarily transmitted through blood-to-blood contact, but it is still important to take standard precautions to prevent transmission.
D) Incorrect. Even if a partner has been vaccinated against hepatitis C, it's important to take precautions to prevent transmission, as vaccines are not always 100% effective.
Gastrointestinal Cancers
Explanation
A) Incorrect. While a diet rich in fruits and vegetables is generally associated with lower cancer risk, it is not the only significant risk factor for gastrointestinal cancers.
B) Incorrect. While age is a factor, gastrointestinal cancers can occur in individuals of various age groups, not just older adults.
C) Correct. Genetic predisposition, along with lifestyle factors such as smoking, excessive alcohol consumption, and certain dietary choices, can increase the risk of gastrointestinal cancers.
D) Incorrect. While some infectious agents may contribute to certain types of gastrointestinal cancers, they are not the primary cause.
Explanation
A) Correct. Regular screening tests like colonoscopy, endoscopy, and other imaging studies are crucial for early detection and diagnosis of gastrointestinal cancers.
B) Incorrect. There are effective screening methods available, and relying solely on symptoms may lead to delayed diagnosis.
C) Incorrect. While genetic testing and family history may be relevant for some individuals, they are not the primary methods for early detection of gastrointestinal cancers.
D) Incorrect. Biopsy is an important diagnostic tool, but it is not a primary screening method for gastrointestinal cancers.
Explanation
A) Incorrect. While some individuals may choose to explore alternative therapies alongside conventional treatments, it's important not to dismiss the effectiveness of established treatments.
B) Correct. Acknowledging the client's fear and encouraging open communication with the healthcare team empowers the client to make informed decisions about their treatment plan.
C) Incorrect. Gastrointestinal cancer treatment often involves a combination of approaches, including surgery, chemotherapy, radiation, and other modalities, depending on the specific type and stage of the cancer.
D) Incorrect. Experimental treatments are not always the best option, and their success rates may vary. Conventional treatments have been extensively studied and proven effective for many individuals with gastrointestinal cancers.
Explanation
A) Incorrect. Gastrointestinal cancers can present with a wide range of symptoms, and severe abdominal pain is just one possibility. However, not all cases present with such clear signs.
B) Correct. In the early stages, gastrointestinal cancers may not cause noticeable symptoms. Regular screenings, such as colonoscopies and endoscopies
, are crucial for early detection.
C) Incorrect. Gastrointestinal cancers primarily affect the internal organs, and skin changes and rashes on the abdomen are not typical symptoms.
D) Incorrect. While weight loss and loss of appetite can be symptoms of gastrointestinal cancer, they are not the only manifestations. Other symptoms may include changes in bowel habits, blood in stool, abdominal discomfort, and more.
Explanation
A) Incorrect. While genetic factors can play a role, there are proactive steps individuals can take to reduce their risk of gastrointestinal cancer, even with a family history.
B) Correct. Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding tobacco and excessive alcohol consumption, can help reduce the risk of gastrointestinal cancer.
C) Incorrect. While genetic testing may provide valuable information, it is just one component of an overall approach to prevention.
D) Incorrect. The effectiveness and safety of herbal supplements for preventing gastrointestinal cancer have not been conclusively established. Lifestyle factors and regular screenings are more widely accepted preventive measures.
Explanation
A) Incorrect. While a diet rich in fruits and vegetables is generally associated with lower cancer risk, it is not the only significant risk factor for gastrointestinal cancers.
B) Incorrect. While age is a factor, gastrointestinal cancers can occur in individuals of various age groups, not just older adults.
C) Correct. Genetic predisposition, along with lifestyle factors such as smoking, excessive alcohol consumption, and certain dietary choices, can increase the risk of gastrointestinal cancers.
D) Incorrect. While some infectious agents may contribute to certain types of gastrointestinal cancers, they are not the primary cause.
Explanation
A) Correct. Regular screening tests like colonoscopy, endoscopy, and other imaging studies are crucial for early detection and diagnosis of gastrointestinal cancers.
B) Incorrect. There are effective screening methods available, and relying solely on symptoms may lead to delayed diagnosis.
C) Incorrect. While genetic testing and family history may be relevant for some individuals, they are not the primary methods for early detection of gastrointestinal cancers.
D) Incorrect. Biopsy is an important diagnostic tool, but it is not a primary screening method for gastrointestinal cancers.
Explanation
A) Incorrect. While some individuals may choose to explore alternative therapies alongside conventional treatments, it's important not to dismiss the effectiveness of established treatments.
B) Correct. Acknowledging the client's fear and encouraging open communication with the healthcare team empowers the client to make informed decisions about their treatment plan.
C) Incorrect. Gastrointestinal cancer treatment often involves a combination of approaches, including surgery, chemotherapy, radiation, and other modalities, depending on the specific type and stage of the cancer.
D) Incorrect. Experimental treatments are not always the best option, and their success rates may vary. Conventional treatments have been extensively studied and proven effective for many individuals with gastrointestinal cancers.
Explanation
A) Incorrect. Gastrointestinal cancers can present with a wide range of symptoms, and severe abdominal pain is just one possibility. However, not all cases present with such clear signs.
B) Correct. In the early stages, gastrointestinal cancers may not cause noticeable symptoms. Regular screenings, such as colonoscopies and endoscopies, are crucial for early detection.
C) Incorrect. Gastrointestinal cancers primarily affect the internal organs, and skin changes and rashes on the abdomen are not typical symptoms.
D) Incorrect. While weight loss and loss of appetite can be symptoms of gastrointestinal cancer, they are not the only manifestations. Other symptoms may include changes in bowel habits, blood in stool, abdominal discomfort, and more.
Explanation
A) Incorrect. While genetic factors can play a role, there are proactive steps individuals can take to reduce their risk of gastrointestinal cancer, even with a family history.
B) Correct. Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding tobacco and excessive alcohol consumption, can help reduce the risk of gastrointestinal cancer.
C) Incorrect. While genetic testing may provide valuable information, it is just one component of an overall approach to prevention.
D) Incorrect. The effectiveness and safety of herbal supplements for preventing gastrointestinal cancer have not been conclusively established. Lifestyle factors and regular screenings are more widely accepted preventive measures.
Explanation
A) Incorrect. While environmental factors can contribute to the development of cancer, they are not the primary cause. Genetic mutations play a significant role.
B) Correct. Gastrointestinal cancer, like other types of cancer, develops when normal cells in the gastrointestinal tract acquire genetic mutations. These mutations lead to uncontrolled cell growth and the formation of tumors.
C) Incorrect. While there can be a genetic component to some cases of gastrointestinal cancer, it is not exclusively inherited from one's parents.
D) Incorrect. While the exact cause of gastrointestinal cancer may not always be known, significant research has identified genetic mutations and other factors that contribute to its development.
Explanation
A) Incorrect. Metastasis does not refer to the initial formation of cancer, but rather the spread of cancer from its original site to other parts of the body.
B) Correct. Metastasis is the process by which cancer cells break away from the primary tumor in the gastrointestinal tract and travel through the bloodstream or lymphatic system to form new tumors in other organs or tissues.
C) Incorrect. Metastasis is not a surgical procedure; it is the spread of cancer cells.
D) Incorrect. Metastasis is not a diagnostic test but rather a stage in the progression of cancer.
Explanation
A) Incorrect. While lifestyle choices can contribute to the risk of gastrointestinal cancer, genetics also play a significant role.
B) Correct. Certain genetic mutations, particularly those associated with hereditary cancer syndromes, can increase an individual's risk of developing gastrointestinal cancer. This risk is heightened in individuals with a family history of the disease.
C) Incorrect. While inherited genetic abnormalities can be a factor, they are not the sole cause of gastrointestinal cancer.
D) Incorrect. Genetics can play a role in the development of gastrointestinal cancer in both children and adults, especially in cases where there is a family history or known genetic predisposition.
Explanation
A) Incorrect. Tumor suppressor genes have the opposite role; they inhibit the growth of tumors.
B) Correct. Tumor suppressor genes are responsible for regulating cell division and preventing the formation of tumors. When these genes are mutated, they may lose their ability to inhibit tumor growth, increasing the risk of cancer.
C) Incorrect. Tumor suppressor genes are indeed relevant to the development of gastrointestinal cancer.
D) Incorrect. This statement inaccurately describes the role of tumor suppressor genes. They are involved in preventing uncontrolled cell growth and tumor formation.
Explanation
A) Incorrect. Inflammation can be associated with the development of cancer, especially in cases of chronic inflammation.
B) Correct. Chronic inflammation in the gastrointestinal tract can lead to genetic mutations and cellular changes that increase the risk of cancer development.
C) Incorrect. Inflammation can contribute to the development of cancer, but it is not the sole cause.
D) Incorrect. Both acute and chronic inflammation can contribute to the risk of gastrointestinal cancer, but chronic inflammation is particularly relevant in this context.
Explanation
A) Incorrect. While abdominal pain can be a symptom of gastrointestinal cancer, it may not be an early sign. Additionally, tenderness is not always present.
B) Correct. Unexplained weight loss and changes in bowel habits, such as persistent diarrhea or constipation, can be early indicators of gastrointestinal cancer.
C) Incorrect. Skin discoloration and itching are not common early signs of gastrointestinal cancer.
D) Incorrect. Fever and joint pain are not typically associated with the early presentation of gastrointestinal cancer.
Explanation
A) Incorrect. Increased appetite and weight gain are not typical symptoms of advancing gastrointestinal cancer.
B) Correct. As gastrointestinal cancer progresses, it can lead to symptoms like difficulty swallowing (dysphagia) and a sensation of fullness even after consuming small amounts of food.
C) Incorrect. Progressing cancer is more likely to lead to increased fatigue and weakness, not a decrease.
D) Incorrect. Pain and discomfort may actually intensify as the cancer advances due to factors like tumor growth and potential spread.
Explanation
A) Incorrect. Complications of gastrointestinal cancer treatment are more likely to lead to increased fatigue and decreased appetite.
B) Correct. Infection is a potential complication of cancer treatment, as chemotherapy and radiation therapy can suppress the immune system.
C) Incorrect. Treatment can indeed affect blood cell counts and immune function, potentially leading to complications.
D) Incorrect. Nausea and vomiting are common side effects and potential complications of gastrointestinal cancer treatment.
Explanation
A) Incorrect. Severe abdominal pain can indeed be associated with advanced gastrointestinal cancer, particularly if there is tumor growth or complications.
B) Correct. Severe abdominal pain in a client with advanced gastrointestinal cancer warrants further assessment, as it could indicate tumor progression or other complications that require attention.
C) Incorrect. Abdominal pain is not a typical sign of cancer remission, especially in advanced stages.
D) Incorrect. While indigestion can cause abdominal discomfort, severe pain in a client with advanced gastrointestinal cancer should be taken seriously and assessed thoroughly.
Explanation
A) Incorrect. While treatment aims to eliminate or control cancer, there is still a possibility of recurrence, depending on various factors.
B) Correct. The risk of cancer recurrence varies based on factors such as the type and stage of cancer, the effectiveness of treatment, and the individual's overall health. Regular follow-up appointments and monitoring are essential.
C) Incorrect. While a family history of cancer can be a risk factor, it is not the sole determinant of cancer recurrence.
D) Incorrect. Ongoing monitoring and follow-up appointments are crucial after completing treatment for gastrointestinal cancer to detect any signs of recurrence or complications.
Explanation
A) Incorrect. While a biopsy is a crucial diagnostic tool for confirming cancer, it is often performed after initial imaging and endoscopy.
B) Incorrect. Blood tests for cancer markers may be part of the diagnostic process, but they are not typically the initial test.
C) Incorrect. CT scans are valuable for providing detailed images of the gastrointestinal tract, but they may not always be the very first diagnostic test performed.
D) Correct. Endoscopy allows direct visualization of the affected area, which is often the initial step in diagnosing gastrointestinal cancer.
Explanation
A) Correct. A colonoscopy involves the insertion of a flexible tube with a camera through the rectum to visualize the colon and obtain tissue samples for biopsy.
B) Incorrect. The description provided pertains more to an ultrasound or endoscopic ultrasound (EUS) rather than a colonoscopy.
C) Incorrect. Colonoscopy primarily examines the colon, not the esophagus.
D) Incorrect. This description aligns more closely with a capsule endoscopy, where a camera is swallowed to capture images, but it does not allow for biopsy.
Explanation
A) Incorrect. The description provided aligns more closely with a colonoscopy rather than a barium enema.
B) Correct. A barium enema is a radiographic examination that uses X-rays and a contrast material (barium) to provide detailed images of the colon, allowing for the detection of abnormalities.
C) Incorrect. A barium enema primarily examines the colon, not the stomach.
D) Incorrect. This description aligns more closely with a capsule endoscopy, but it does not involve a barium contrast material.
Explanation
A) Incorrect. The description provided aligns more closely with a colonoscopy rather than an upper GI endoscopy.
B) Correct. An upper GI endoscopy involves the insertion of a thin, flexible tube with a camera through the mouth to examine the esophagus, stomach, and duodenum for abnormalities.
C) Incorrect. An upper GI endoscopy primarily focuses on the esophagus, stomach, and duodenum, not the small intestine.
D) Incorrect. This description aligns more closely with a capsule endoscopy, but it does not involve an upper GI endoscopy.
Explanation
A) Incorrect. The description provided aligns more closely with an ultrasound rather than a CT scan.
B) Incorrect. This description aligns more closely with a capsule endoscopy, but it does not involve a CT scan.
C) Correct. A CT scan uses X-rays to create detailed images of the internal organs, helping to identify abnormalities or tumors.
D) Incorrect. CT scans are not primarily used to assess blood flow in the gastrointestinal tract; they provide detailed anatomical images.
Explanation
A) Correct. Surgery, chemotherapy, and radiation therapy are commonly used treatments for gastrointestinal cancer, often used in combination or sequentially.
B) Incorrect. While immunotherapy is an emerging treatment option for some types of cancer, it is not the sole primary treatment for all gastrointestinal cancers.
C) Incorrect. Alternative therapies such as herbal supplements are not considered the preferred or primary approach for treating gastrointestinal cancer.
D) Incorrect. Gastrointestinal cancer treatment often involves a multimodal approach, including surgery, chemotherapy, and sometimes radiation therapy.
Explanation
A) Correct. Common side effects of chemotherapy include nausea, vomiting, fatigue, and hair loss, among others.
B) Incorrect. Chemotherapy affects both cancer cells and normal cells, which can lead to various side effects.
C) Incorrect. It is not accurate to state that a client will not experience any side effects from chemotherapy.
D) Incorrect. While chemotherapy can affect the skin, it has a broader range of potential side effects beyond mild irritation.
Explanation
A) Incorrect. While radiation therapy is an important treatment modality, it is not the exclusive primary treatment for all types of gastrointestinal cancer.
B) Correct. Radiation therapy uses high-energy X-rays or other particles to target and destroy cancer cells.
C) Incorrect. Radiation therapy is an effective treatment option for many types of gastrointestinal cancer.
D) Incorrect. Radiation therapy may be used before or after surgery, depending on the specific circumstances of the case.
Explanation
A) Incorrect. While fiber is important for digestive health, it may need to be adjusted based on individual symptoms and treatment effects.
B) Incorrect. Fruits and vegetables are important sources of essential nutrients. Avoiding them entirely is not recommended.
C) Correct. Protein is crucial for energy levels and tissue repair, which can be especially important during cancer treatment.
D) Incorrect. A strictly liquid diet may not provide all the necessary nutrients for a client undergoing cancer treatment.
Explanation
A) Correct. Targeted therapy is a type of treatment that uses drugs to target specific molecules involved in the growth and spread of cancer cells.
B) Incorrect. Targeted therapy is used in the treatment of various types of cancer, including gastrointestinal cancer, not just breast cancer.
C) Incorrect. While immunotherapy is a different type of treatment that boosts the immune system, it is not synonymous with targeted therapy.
D) Incorrect. Targeted therapy can have a significant impact on cancer outcomes, but its effectiveness may vary depending on the specific type and stage of cancer.
Explanation
A) Incorrect. It is important for clients with gastrointestinal cancer to incorporate a variety of fruits and vegetables into their diet, as they provide essential nutrients.
B) Correct. A balanced diet with a variety of fruits, vegetables, and lean proteins supports overall health and can help the body cope with the demands of cancer treatment.
C) Incorrect. A high-fat, low-fiber diet is not typically recommended for clients with gastrointestinal cancer, as it may exacerbate certain symptoms and is not conducive to overall health.
D) Incorrect. While some clients may have dietary restrictions based on their individual treatment plan, a blanket recommendation for only liquid diets is not appropriate.
Explanation
A) Incorrect. Increasing high-fiber foods can exacerbate diarrhea in clients experiencing gastrointestinal symptoms.
B) Incorrect. While some clients may be lactose intolerant and need to limit dairy, it is not a blanket recommendation for all clients with diarrhea.
C) Correct. Offering foods that are easy to digest and low in fiber can help manage diarrhea and promote comfort for the client.
D) Incorrect. Laxatives may worsen diarrhea and are not the appropriate intervention for this situation.
Explanation
A) Incorrect. While exercise is important, high-intensity exercise may be too strenuous for a client experiencing fatigue.
B) Correct. Taking short, frequent rest breaks can help conserve energy and manage fatigue for clients undergoing cancer treatment.
C) Incorrect. Avoiding all physical activity is not recommended, as some gentle activity can be beneficial for managing fatigue.
D) Incorrect. Consuming large amounts of caffeine may lead to dehydration and worsen fatigue.
Explanation
A) Incorrect. Caffeinated beverages can lead to dehydration and are not the best choice for maintaining hydration.
B) Correct. Monitoring urine color is a practical way for clients to assess their hydration status. Pale yellow urine indicates adequate hydration.
C) Incorrect. Limiting fluid intake is not recommended for clients, especially those undergoing cancer treatment, as it can lead to dehydration.
D) Incorrect. Waiting until extreme thirst sets in is not an effective strategy for maintaining hydration.
A client with gastrointestinal cancer is experiencing pain. The client asks the nurse for advice on pain management. How should the nurse respond?
Explanation
A) Incorrect. Pain should be managed according to the prescribed plan, not just when it reaches severe levels.
B) Correct. Following the prescribed pain management plan and communicating any changes in pain levels to the healthcare provider is crucial for effective pain control.
C) Incorrect. Avoiding pain medication altogether may lead to inadequate pain management, which can negatively impact the client's quality of life.
D) Incorrect. Experimenting with various over-the-counter medications without guidance from a healthcare provider can be unsafe and may not effectively address the client's pain.
Exams on Pathophysiology of the Gastrointestinal System
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Identify the educative, preventive measures and hygiene practices to reduce the incidence of Gastroenteritis.
-
Identify the medications and lifestyle modifications for managing Gastroesophageal Reflux Disease (GERD).
-
Identify ways of increasing public awareness about dietary habits and lifestyle changes to prevent and manage GERD.
-
Identify screening and early detection programs for individuals at risk of Peptic Ulcer Disease.
-
Identify diagnostic methods and treatment options for Gastrointestinal Bleeding.
-
Identify interventions for early detection and management of Appendicitis to prevent complications.
-
Investigate the access to specialized care and medications for individuals with Inflammatory Bowel Disease (IBD).
-
Increase awareness about IBS, including symptom recognition and management strategies.
Gastroenteritis
Introduction to Gastroenteritis
- Definition: Gastroenteritis refers to the inflammation of the gastrointestinal tract, involving the stomach and intestines.
- Commonly known as the stomach flu or food poisoning.
- It can be caused by various infectious agents like bacteria, viruses, or parasites.
Etiology:
- Bacterial Causes:
- E. coli, Salmonella, Campylobacter, Shigella.
- Viral Causes:
- Norovirus, Rotavirus, Adenovirus.
- Parasitic Causes:
- Giardia lamblia, Cryptosporidium.

Pathophysiology
1. Infection Route
- Gastroenteritis is typically contracted by ingesting contaminated food or water that contains infectious agents such as bacteria, viruses, or parasites.
2. Attachment and Invasion
- Once inside the gastrointestinal tract, the infectious agents attach themselves to the lining of the stomach and intestines. They may have specialized structures or proteins that allow them to adhere to the cells.
3. Multiplication and Colonization
- After attachment, the infectious agents start to multiply rapidly. This leads to an increase in their population within the intestines, overwhelming the body's natural defenses.
4. Inflammation and Tissue Damage
- As the infectious agents multiply, they release toxins, enzymes, or other virulence factors. These substances can lead to inflammation of the gastrointestinal mucosa. Inflammatory responses can cause damage to the cells lining the stomach and intestines.
5. Disruption of Absorptive Functions
- The inflammation and damage to the mucosa can impair the normal absorptive functions of the intestines. This can result in malabsorption of nutrients, electrolytes, and water.
6. Activation of Immune Response
- The body recognizes the presence of foreign pathogens and mounts an immune response. Immune cells, such as white blood cells, are mobilized to the site of infection.
7. Release of Cytokines
- The immune response involves the release of signaling molecules called cytokines. These cytokines have various effects, including increasing inflammation, altering the permeability of blood vessels, and stimulating the production of mucus.
8. Symptom Manifestation
- The combined effects of inflammation, altered absorptive functions, and immune response lead to the characteristic symptoms of gastroenteritis, which include diarrhea, nausea, vomiting, abdominal cramps, fever, and sometimes dehydration.
9. Fluid and Electrolyte Imbalance
- The frequent diarrhea and vomiting can lead to significant fluid and electrolyte losses. This can result in dehydration and imbalances in electrolyte levels, which are particularly concerning, especially in vulnerable populations like infants and the elderly.
10. Resolution and Recovery
- With appropriate treatment and supportive care, the body's immune system eventually clears the infectious agents. The gastrointestinal mucosa begins to heal, and normal function is gradually restored.
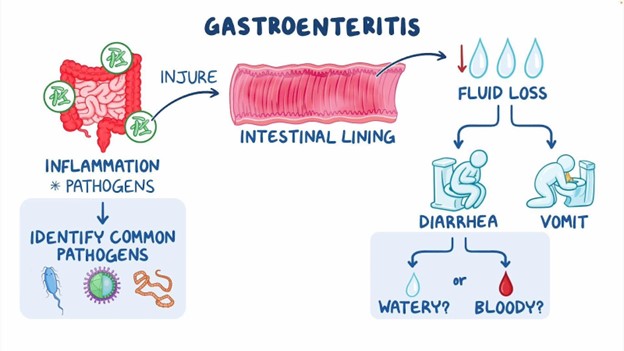
Clinical Presentation
- Diarrhea (loose, watery stools)
- Nausea and the urge to vomit
- Vomiting (forceful expulsion of stomach contents)
- Abdominal cramps and discomfort
- Fever (elevated body temperature)
- Signs of dehydration (e.g., dry mouth, decreased urine output)
- Loss of appetite
- Muscle aches and weakness
- Headache
- Fatigue and low energy levels
- Blood or mucus in stools (in some cases)
- Weight loss (in severe or prolonged cases)
Complications
1. Dehydration:
- Loss of fluids through vomiting and diarrhea can lead to electrolyte imbalance.
2. Malnutrition:
- In severe cases, nutrient absorption may be impaired.
3. Secondary Infections:
- Weakened immune system may lead to opportunistic infections.
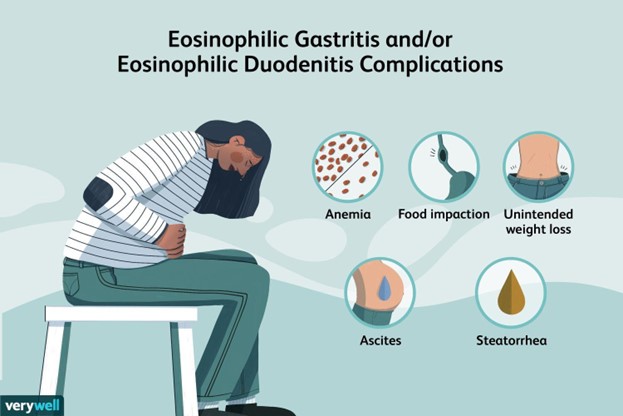
Treatment and Management
- Fluid Replacement: Oral rehydration solutions or, in severe cases, intravenous fluids.
- Dietary Modifications: BRAT diet (Bananas, Rice, Applesauce, Toast) may be recommended.
- Medications: Antibiotics for bacterial infections, antiemetics for vomiting, and antidiarrheal agents.
- Rest and Isolation: Rest to allow the body to recover and prevent spreading the infection.
Prevention and Control
- Frequent handwashing with soap and water.
- Proper handling, cooking, and storage of food.
- Drinking clean, treated water and avoiding swimming in contaminated water sources.
- Vaccines available for certain types of gastroenteritis (e.g., Rotavirus vaccine for infants).
- Isolating infected individuals and practicing good hygiene to prevent spread.
Conclusion
- Gastroenteritis is a common gastrointestinal disorder characterized by inflammation of the stomach and intestines, often caused by infectious agents like bacteria, viruses, or parasites.
- It leads to a range of distressing symptoms including diarrhea, vomiting, abdominal cramps, and fever, which can significantly impact an individual's well-being.
- Dehydration is a significant concern in gastroenteritis, especially in vulnerable populations like infants, the elderly, and those with weakened immune systems.
- Prompt and appropriate treatment is essential to manage symptoms and prevent complications, with interventions including fluid replacement, dietary adjustments, and, in some cases, medications.
- Prevention strategies, such as practicing good hand hygiene, ensuring food safety, and vaccination where applicable, play a crucial role in reducing the incidence and spread of gastroenteritis.
- Timely medical attention is advised in cases of severe dehydration, bloody stools, or prolonged symptoms, particularly in high-risk populations.
- Understanding the pathophysiology, clinical presentation, and management of gastroenteritis empowers individuals to take proactive measures to prevent and address this common gastrointestinal condition.
Summary
- Gastroenteritis is an inflammation of the gastrointestinal tract, caused primarily by viral, bacterial, or parasitic infections.
- Common symptoms include diarrhea, vomiting, abdominal cramps, nausea, and fever, which can lead to dehydration if not managed promptly.
- It spreads through contaminated food, water, or close contact with infected individuals, making proper hygiene and food safety crucial for prevention.
- Treatment focuses on rehydration, dietary adjustments, and in some cases, medications to alleviate symptoms and prevent complications.
- Awareness of the causes, symptoms, and preventive measures empowers individuals to effectively manage and minimize the impact of gastroenteritis on their health.
Gastroesophageal reflux disease
Introduction
- GERD, or Gastroesophageal Reflux Disease, is a chronic condition characterized by the backward flow of stomach acid into the esophagus.
- It is a common gastrointestinal disorder that can lead to discomfort and potential complications if not managed effectively.
- GERD is distinct from occasional heartburn, as it involves persistent and recurrent symptoms.
- The condition can significantly impact an individual's quality of life and may require ongoing treatment and lifestyle modifications.
- Complications of untreated GERD can include esophagitis, Barrett's esophagus, and in severe cases, esophageal cancer.
- Understanding the underlying causes and pathophysiology of GERD is crucial for effective management and prevention of complications.
- Management strategies aim to alleviate symptoms, prevent further damage to the esophagus, and improve overall well-being.
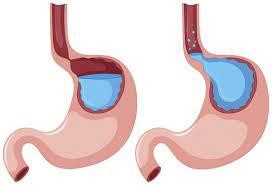
Risk factors
- Obesity and excess body weight increase the pressure on the abdomen, promoting reflux.
- Hiatal hernia, a condition where part of the stomach protrudes into the chest, weakens the lower esophageal sphincter, facilitating reflux.
- Pregnancy leads to increased pressure on the abdomen, potentially causing reflux symptoms.
- Smoking relaxes the lower esophageal sphincter, making it easier for stomach acid to flow into the esophagus.
- Certain foods and beverages, such as citrus fruits, caffeine, alcohol, and fatty or spicy foods, can trigger reflux.
- Medications like Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and calcium channel blockers may relax the LES or irritate the esophagus.
- Conditions like scleroderma and delayed stomach emptying (gastroparesis) can contribute to GERD.
Pathophysiology
- GERD primarily arises from a weakened Lower Esophageal Sphincter (LES), a circular muscle at the junction of the esophagus and stomach.
- The LES normally acts as a barrier, preventing stomach acid from refluxing into the esophagus.
- When the LES weakens, it fails to close properly after food passes into the stomach, allowing acid to flow backward.
- Chronic exposure to stomach acid leads to irritation and inflammation of the esophageal lining.
- This can result in erosions, ulcers, and in severe cases, the development of Barrett's esophagus, a pre-cancerous condition.
- Hiatal hernia, if present, further disrupts the anatomy around the LES, exacerbating reflux symptoms.
- Understanding the pathophysiology is crucial for tailoring interventions and treatments to target the underlying mechanisms.
Clinical Presentation
- Heartburn is the hallmark symptom of GERD, characterized by a burning sensation in the chest, especially after meals or while lying down.
- Regurgitation involves the backflow of acidic or bitter-tasting stomach contents into the mouth or throat.
- Dysphagia, or difficulty swallowing, can occur due to narrowing of the esophagus from chronic inflammation.
- Chest pain, though typically non-cardiac, may be present and can be mistaken for heart-related discomfort.
- Chronic cough, wheezing, or hoarseness may arise from irritation of the respiratory tract by refluxed contents.
- Belching, bloating, and nausea are common, and may be related to increased abdominal pressure.
- Respiratory symptoms, known as silent reflux, can be more pronounced in individuals who do not experience typical GERD symptoms.
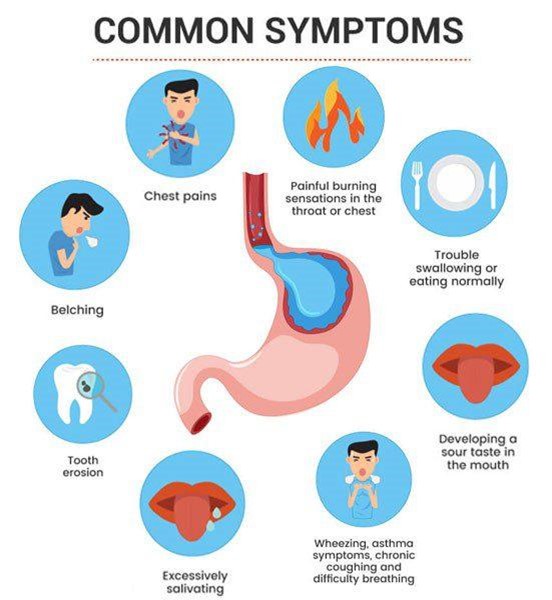
Diagnostic Tests
- Upper Endoscopy (EGD) allows direct visualization of the esophagus and can identify mucosal damage, ulcers, or strictures.
- Barium Swallow involves the ingestion of contrast material to highlight structural abnormalities of the esophagus.
- Esophageal Manometry measures the pressure in the esophagus and evaluates the function of the LES.
- 24-hour pH Monitoring provides data on the acidity levels in the esophagus over an extended period, aiding in diagnosis.
- Esophageal Biopsy may be performed to assess tissue changes and rule out complications like Barrett's esophagus.
- Ambulatory Esophageal pH Testing assesses acid levels over an extended period, providing valuable information on acid exposure.
- Upper GI Series, though less commonly used, can provide additional information about the esophagus and stomach.
Management
Lifestyle Modifications:
- Weight loss, if applicable, can reduce abdominal pressure and improve symptoms.
- Avoiding trigger foods and beverages like caffeine, alcohol, citrus, fatty, and spicy foods can help prevent reflux episodes.
- Eating smaller, more frequent meals can reduce the volume of stomach contents, decreasing the likelihood of reflux.
- Elevating the head of the bed during sleep (using bed risers) can discourage acid from flowing back into the esophagus.
Medications:
- Proton Pump Inhibitors (PPIs) like omeprazole and pantoprazole reduce stomach acid production and are often prescribed as first-line treatment.
- H2 Receptor Antagonists (e.g., ranitidine) block histamine, decreasing acid secretion.
- Antacids provide rapid relief by neutralizing stomach acid, but their effects are short-lived.
Surgery:
- Fundoplication involves wrapping the top of the stomach around the lower esophagus to reinforce the LES.
- LINX device placement involves implanting a ring of magnetic beads around the esophagus to augment the LES.
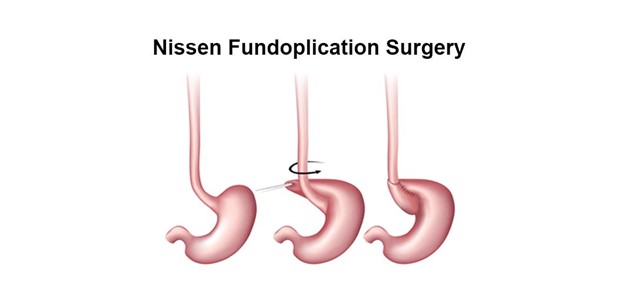
Nursing Care and Interventions
- Educate patients about dietary modifications, lifestyle changes, and medication management to alleviate symptoms.
- Provide information about potential side effects and the importance of adherence to prescribed treatments.
- Regular follow-up appointments and monitoring for signs of complications like Barrett's esophagus are essential.
- Educate patients about symptoms that warrant immediate medical attention, such as severe chest pain or difficulty swallowing.
- Prepare and educate patients about diagnostic tests like upper endoscopy, ensuring they understand the procedure and its purpose.
- Offer emotional support to alleviate any anxiety or concerns about the diagnostic process.
- Monitor for surgical site complications, ensure adequate pain control, and support early ambulation.
- Educate the patient on postoperative restrictions, including diet and activity modifications.
Conclusion
- GERD is a chronic condition characterized by the reflux of stomach acid into the esophagus, leading to a range of symptoms and potential complications.
- Effective management involves a combination of lifestyle modifications, medications, and, in severe cases, surgical interventions.
- Understanding the underlying pathophysiology and risk factors is crucial for tailoring treatment plans to individual patients.
Summary
- GERD is a chronic condition involving the reflux of stomach acid into the esophagus. It necessitates ongoing management to alleviate symptoms and prevent complications.
Nurses play a vital role in educating patients, administering medications, and providing postoperative care for those undergoing surgical interventions.
A thorough understanding of GERD's pathophysiology empowers healthcare professionals to deliver effective care and support to affected individuals.
Peptic ulcer disease
Introduction to peptic ulcer disease
- Peptic ulcer disease (PUD) is a condition that involves the formation of open sores or ulcers in the lining of the stomach or the duodenum, which is the first part of the small intestine.
- PUD can cause abdominal pain, bleeding, and other complications.
- The most common causes of PUD are infection with Helicobacter pylori (H. pylori) bacteria and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
- Peptic ulcers can affect the stomach (gastric ulcers) or the duodenum (duodenal ulcers). Less commonly, they can also occur in the lower esophagus or beyond the duodenum.
- Peptic ulcers are common, affecting about 10% of people in their lifetime.
- Peptic ulcers can cause symptoms such as burning stomach pain, nausea, vomiting, weight loss, and anemia.
- Some people may have no symptoms or only mild discomfort.
- Peptic ulcers can lead to serious complications such as bleeding, perforation, infection, and obstruction. These complications may require emergency treatment or surgery.
- Peptic ulcers can be diagnosed by tests such as blood tests, breath tests, stool tests, endoscopy, upper gastrointestinal series, and biopsy.
- Peptic ulcers can be treated by medications such as antibiotics, proton pump inhibitors, H2 blockers, and antacids. These medications aim to eradicate H. pylori infection, reduce acid production, and promote healing of the ulcers.
Etiology and risk factors
The main causes of peptic ulcers are infection with H. pylori bacteria and long-term use of NSAIDs.
- H. pylori is a spiral-shaped bacterium that colonizes the stomach and duodenum. It can damage the mucosa by producing enzymes, tons, and inflammatory substances. It can also interfere with the production of protective mucus and bicarbonate in the stomach. H. pylori infection is very common, affecting about half of the world's population. It is more prevalent in developing countries, where it is usually acquired in childhood. It can be transmitted from person to person through oral-oral or fecal-oral routes, or through contaminated food or water.
- NSAIDs are a group of drugs that are used to relieve pain, inflammation, and fever. They include aspirin, ibuprofen, naproxen, celecob, and others. NSAIDs can cause peptic ulcers by inhibiting an enzyme called cyclooxygenase (COX), which is involved in the synthesis of prostaglandins. Prostaglandins are substances that protect the mucosa from acid and injury. NSAIDs are widely used for various conditions such as arthritis, headache, menstrual cramps, and sports injuries. They can increase the risk of peptic ulcers by 2 to 4 times, especially if taken at high doses, for long periods, or in combination with other drugs such as steroids or anticoagulants.
Other risk factors for peptic ulcers include:
- Smoking: Smoking can increase acid secretion, reduce blood flow to the mucosa, impair healing of ulcers, and reduce the effectiveness of medications.
- Alcohol: Alcohol can irritate the mucosa, increase acid production, and interfere with the action of prostaglandins.
- Stress: Stress can stimulate acid secretion and impair mucosal defense mechanisms. However, stress alone does not cause peptic ulcers unless there is also H. pylori infection or NSAID use.
- Spicy foods: Spicy foods do not cause peptic ulcers, but they may worsen symptoms in some people who have esting ulcers.
- Genetic factors: Some people may have a genetic predisposition to peptic ulcers due to variations in genes that affect acid secretion, mucosal protection, or immune response to H. pylori.
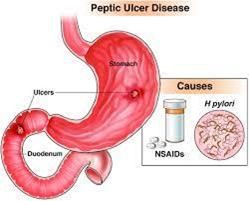
Pathophysiology
- Excessive Acid Production: PUD involves an overproduction of gastric acid, which is normally secreted for digestion but can lead to mucosal damage if in excess.
- Disruption of Mucosal Barrier: Factors like Helicobacter pylori infection, NSAID use, and certain stress-related conditions compromise the protective mechanisms of the gastric and duodenal mucosa.
- Helicobacter pylori Infection: H. pylori is a bacterium that colonizes the stomach lining, leading to inflammation and weakening of the mucosal barrier. It also stimulates increased acid production.
- NSAID-Induced Injury: Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit prostaglandin synthesis, reducing the protective effects on the gastric mucosa. This makes it more susceptible to damage from gastric acid and pepsin.
- Impaired Blood Flow: Conditions that reduce blood flow to the gastric mucosa, such as severe illness or systemic conditions, can lead to ischemic ulcers due to inadequate oxygen and nutrient delivery.
- Genetic Predisposition: Some individuals may be genetically predisposed to PUD, potentially due to variations in mucosal defense mechanisms or response to acid exposure.
- Psychological Stress: While not a direct cause, stress and certain behaviors like smoking or excessive alcohol consumption can exacerbate existing ulcers and hinder the healing process.
Clinical Manifestation and symptoms
The most common symptom of peptic ulcer disease is burning stomach pain that occurs between meals or at night. The pain may last from minutes to hours and may be relieved by eating food or taking antacids. The pain may vary in intensity, frequency, and location depending on the type and location of the ulcer.
- Gastric ulcers tend to cause pain shortly after eating, while duodenal ulcers tend to cause pain 2 to 5 hours after eating.
- Gastric ulcers may also cause loss of appetite, weight loss, and vomiting, while duodenal ulcers may cause increased appetite, weight gain, and bloating.
- Some people with peptic ulcers may have no symptoms or only mild discomfort. This is more common in older adults, who may have less pain receptors or more tolerance to pain. However, asymptomatic ulcers can still lead to complications such as bleeding or perforation.
Other symptoms of peptic ulcer disease may include:
- Nausea and vomiting: Nausea and vomiting may occur due to irritation of the stomach or duodenum by acid or ulcer. Vomiting may also indicate a complication such as bleeding or obstruction. Vomiting blood or material that looks like coffee grounds may indicate a bleeding ulcer, while vomiting undigested food hours after eating may indicate an obstructed ulcer.
- Bleeding: Bleeding is the most common complication of peptic ulcer disease, occurring in about 15% of cases. Bleeding can be mild or severe, acute or chronic. Bleeding can cause hematemesis (vomiting blood), melena (black, tarry stools), or hematochezia (bright red blood in stools). Bleeding can also cause anemia, which can manifest as weakness, fatigue, dizziness, shortness of breath, and pale skin.
- Perforation: Perforation is a life-threatening complication of peptic ulcer disease, occurring in about 5% of cases. Perforation occurs when the ulcer erodes through the entire wall of the stomach or duodenum, creating a hole that allows the contents of the digestive tract to spill into the abdominal cavity. Perforation can cause sudden and severe abdominal pain that radiates to the back or shoulder, fever, nausea, vomiting, shock, and peritonitis (inflammation of the lining of the abdominal cavity).
- Obstruction: Obstruction is a rare complication of peptic ulcer disease, occurring in less than 1% of cases. Obstruction occurs when the ulcer narrows or blocks the passage of food through the stomach or duodenum. Obstruction can cause persistent vomiting, abdominal distension, dehydration, weight loss, and malnutrition.
Diagnostic evaluation
The diagnosis of peptic ulcer disease is based on the history, physical examination, and diagnostic tests.
1. The history should include information about the onset, duration, frequency, location, and characteristics of the pain; any factors that worsen or relieve the pain; any associated symptoms such as nausea, vomiting, bleeding, weight loss; any history of H. pylori infection or NSAID use; any family history of peptic ulcers; and any previous treatments or medications for peptic ulcers.
2. The physical examination should include inspection and palpation of the abdomen for signs of tenderness, distension, masses, or organomegaly; auscultation for bowel sounds; percussion for signs of fluid or air; and rectal examination for signs of bleeding or anemia.
3. The diagnostic tests for peptic ulcer disease include:
- Blood tests: Blood tests can check for anemia due to bleeding; infection by H. pylori using serology (antibody test), antigen test (stool test), or urea breath test; inflammation using erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP); and liver and kidney function using liver enzymes and creatinine.
- Breath test: To check for H. pylori infection by measuring the amount of carbon diode in the breath after swallowing a urea solution.
- Stool test: To check for H. pylori infection by detecting antigens or DNA in the stool sample.
- Endoscopy: Endoscopy is the most accurate test for peptic ulcer disease. It involves inserting a thin fleble tube with a camera and a light source through the mouth into the stomach and duodenum. Endoscopy can visualize the ulcers and their size, location, shape and take biopsies for histological examination and culture.
- Upper gastrointestinal series: To take X-rays of the upper digestive tract after drinking a contrast agent that coats the lining.

Management and treatment of peptic ulcer disease
The main goals of treatment are to heal the ulcers, prevent complications, and eradicate H. pylori infection if present.
The treatment options include:
1. Medication: The most commonly used drugs are:
- proton pump inhibitors (PPIs) such as omeprazole, lansoprazole, rabeprazole, esomeprazole, and pantoprazole. These drugs reduce the production of stomach acid and promote ulcer healing.
- In addition, antibiotics such as amocillin, clarithromycin, metronidazole, tinidazole, tetracycline, and levofloxacin are given to eradicate H. pylori infection.
- Other drugs that may be used are antacids, histamine receptor blockers, sucralfate, and misoprostol.
2. Surgery: Surgery is reserved for cases with severe complications such as bleeding, perforation, obstruction, or cancer.
- The surgical procedures may involve removing part of the stomach (gastrectomy), cutting the nerve that stimulates acid secretion (vagotomy), or creating a new connection between the stomach and the intestine (gastrojejunostomy).
3. Lifestyle changes: Patients are advised to avoid smoking, alcohol, spicy foods, and NSAIDs that can worsen PUD.
- They are also encouraged to eat small and frequent meals, reduce stress, and seek psychological support if needed.

Complications of peptic ulcer disease
PUD can lead to serious complications if left untreated or poorly managed.
These include:
- Bleeding: Ulcers can erode blood vessels and cause hemorrhage that can manifest as vomiting blood (hematemesis), passing black or tarry stools (melena), or having low blood pressure (hypotension) and shock.
- Perforation: Ulcers can penetrate through the wall of the stomach or duodenum and create a hole that allows stomach contents to leak into the abdominal cavity. This can cause severe pain, fever, abdominal rigidity, and peritonitis (inflammation of the lining of the abdomen).
- Obstruction: Ulcers can cause swelling, scarring, or spasm that narrows the opening of the stomach or duodenum and prevents food from passing through. This can result in nausea, vomiting, bloating, weight loss, and malnutrition.
- Cancer: Chronic inflammation and damage to the lining of the stomach or duodenum can increase the risk of developing gastric or duodenal cancer.
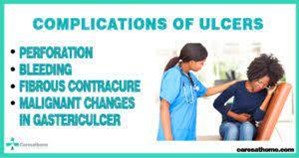
Nursing consideration and intervention
Nurses play a vital role in caring for patients with PUD by providing education, monitoring, and support. Some of the nursing interventions are:
- Assessing the patient's pain level, location, frequency, duration, and aggravating or relieving factors.
- Administering prescribed medications as ordered and observing for their effectiveness and side effects.
- Checking the patient's vital signs, hemoglobin level, stool color and consistency, and signs of bleeding or perforation.
- Encouraging the patient to adhere to the treatment regimen and follow up with regular endoscopy.
- Teaching the patient about PUD causes, symptoms, complications, prevention strategies, and lifestyle modifications.
- Providing emotional support and coping strategies to help the patient deal with stress and anety.
Preventive strategies
PUD can be prevented by avoiding or minimizing the risk factors that contribute to its development. Some of the preventive measures are:
- Testing and treating H. pylori infection if present.
- Limiting or avoiding the use of NSAIDs and taking them with food or antacids if necessary.
- Quitting smoking and reducing alcohol consumption.
- Eating a balanced diet that is rich in vitamin C and low in spicy foods.
- Practicing good hygiene and washing hands frequently.
- Managing stress and seeking professional help if needed.
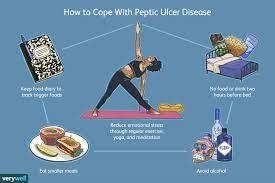
Conclusion
- In conclusion, peptic ulcer disease (PUD) is a common and potentially serious gastrointestinal condition characterized by the formation of ulcers in the lining of the stomach, duodenum, or esophagus.
- This condition can cause various symptoms, ranging from mild discomfort to severe complications, including bleeding and perforation.
- Throughout this study, we have explored the etiology, risk factors, clinical manifestations, diagnosis, and management of peptic ulcer disease.
- One of the primary causes of PUD is the infection with Helicobacter pylori bacteria, which leads to chronic inflammation and ulcer formation.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) and lifestyle factors like smoking and excessive alcohol consumption also contribute significantly to the development of peptic ulcers.
- The clinical presentation of PUD can vary, with common symptoms including burning or gnawing abdominal pain, bloating, nausea, and vomiting.
- In some cases, patients may experience bleeding, leading to dark, tarry stools (melena) or vomiting of blood (hematemesis).
- Recognizing these symptoms early and seeking medical attention promptly is crucial to prevent complications and initiate appropriate treatment.
- Diagnosing peptic ulcer disease involves a combination of patient history, physical examination, and diagnostic tests.
- Endoscopy is a key procedure that allows direct visualization of ulcers and the collection of tissue samples for H. pylori testing. Other tests, such as stool tests, blood tests, and breath tests, can also help identify H. pylori infection.
- The management of peptic ulcer disease aims to alleviate symptoms, promote ulcer healing, eradicate H. pylori infection if present, and prevent complications.
- Treatment may involve a combination of medications, including proton pump inhibitors (PPIs), H2 receptor antagonists, and antibiotics for H. pylori eradication. In cases where NSAID use is necessary, gastroprotective agents may be prescribed to reduce the risk of ulcers.
- Additionally, patient education and lifestyle modifications, such as avoiding smoking, alcohol, and NSAID overuse, can play a vital role in preventing ulcer recurrence and promoting overall gastrointestinal health.
- Preventing complications of PUD, such as bleeding or perforation, requires vigilance in monitoring patients' symptoms and response to treatment.
- In severe cases of bleeding ulcers, endoscopic interventions or surgery may be necessary to stop the bleeding and repair the ulcer.
- In conclusion, peptic ulcer disease remains a prevalent gastrointestinal disorder with significant implications for patient health and quality of life.
- Early diagnosis, appropriate treatment, and lifestyle modifications are crucial in managing the condition effectively.
- Through ongoing research and continued efforts to raise awareness about risk factors and preventive measures, we can strive to reduce the incidence and impact of peptic ulcer disease in the population.
- Timely intervention and comprehensive patient care are essential in achieving successful outcomes and improving the overall well-being of individuals affected by PUD.
Summary
- PUD is a common digestive disorder that affects millions of people worldwide.
- It is characterized by ulcers in the stomach or duodenum that can cause pain, bleeding, infection, and obstruction.
- PUD is mainly caused by H. pylori infection and NSAID use.
- The diagnosis is made by history, physical examination, and laboratory tests.
- The treatment involves medication, surgery, and lifestyle changes.
- The complications of PUD include bleeding, perforation, obstruction, and cancer.
- The nursing care of PUD patients focuses on education, monitoring, and support.
- PUD can be prevented by avoiding or minimizing the risk factors and following preventive strategies.
Gastrointestinal bleeding
Introduction
- Gastrointestinal bleeding refers to any bleeding that occurs in the digestive tract, from the mouth to the rectum.
- It can be caused by various conditions, ranging from minor irritation to severe, life-threatening conditions.
- Gastrointestinal bleeding can present as either overt bleeding (visible in vomit or stool) or occult bleeding (not immediately visible).
- It requires prompt evaluation and intervention to identify the source and prevent complications.
- Understanding the risk factors and underlying pathophysiology is crucial for effective management.
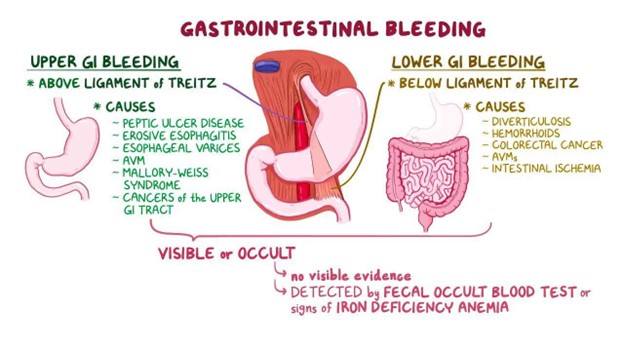
Risk factors
- Peptic ulcers, particularly in the stomach and duodenum.
- Gastroesophageal reflux disease (GERD) and esophagitis.
- Use of nonsteroidal anti-inflammatory drugs (NSAIDs) or anticoagulants.
- Cirrhosis and portal hypertension, which increase pressure in the veins of the digestive tract.
- Esophageal varices, often associated with liver disease.
- Colorectal polyps or cancer.
- Conditions like diverticulosis and Crohn's disease that can lead to gastrointestinal bleeding.
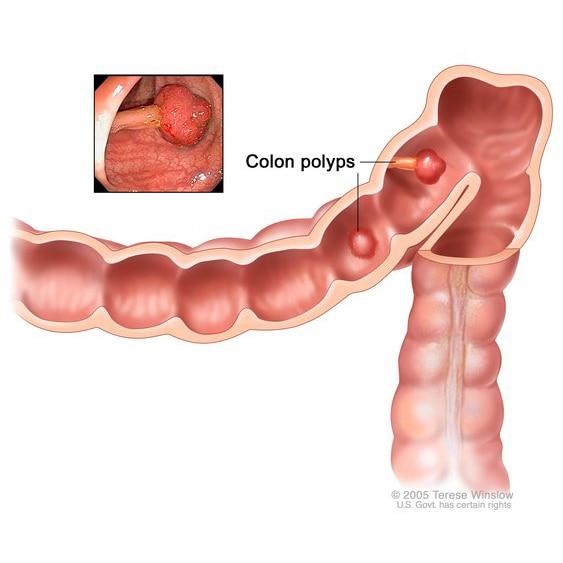
Pathophysiology
- Gastrointestinal bleeding can result from various causes, including erosions, ulcers, varices, tumors, or vascular malformations.
- Peptic ulcers, for example, are often caused by the erosion of the mucosal lining due to excessive acid or H. pylori infection.
- Esophageal varices occur when increased pressure in the portal vein system causes the blood vessels in the esophagus to dilate and rupture.
- Colorectal bleeding can arise from polyps, tumors, or diverticular disease.
- Understanding the underlying cause is crucial for determining appropriate treatment.
Clinical Presentation
- Hematemesis (vomiting blood) or coffee-ground emesis (partially digested blood).
- Melena (black, tarry stools) or hematochezia (bright red or maroon blood in stools).
- Abdominal pain or discomfort, often localized to the area of bleeding.
- Signs of hypovolemic shock in severe cases, including rapid heart rate, low blood pressure, and pale skin.
- Weakness, fatigue, and lightheadedness due to anemia from chronic bleeding.
- Changes in mental status, particularly in cases of significant blood loss.
- Occult bleeding may not have obvious visible signs and is often detected through laboratory tests.
Diagnostic Tests
- Upper Endoscopy (EGD) allows direct visualization of the upper gastrointestinal tract, identifying the source of bleeding.
- Colonoscopy is used to assess the lower gastrointestinal tract, particularly in cases of lower GI bleeding.
- Capsule Endoscopy involves swallowing a small camera capsule that captures images of the entire gastrointestinal tract.
- Barium X-ray studies can help identify structural abnormalities or sources of bleeding.
- Hemoglobin and Hematocrit levels assess for anemia resulting from chronic bleeding.
- Stool Guaiac or Fecal Immunochemical Test (FIT) detect occult blood in the stool.
- Angiography may be used to identify and potentially treat sources of bleeding through the injection of contrast dye.
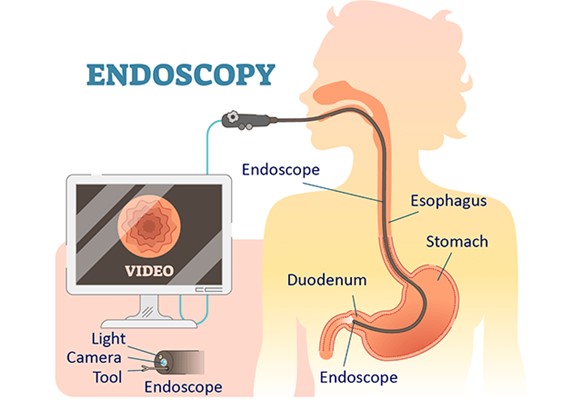
Management
- Acute Bleeding Episodes
- Fluid Resuscitation Intravenous fluids may be administered to restore blood volume.
- Blood Transfusion Packed red blood cells may be given to replace lost blood and correct anemia.
- Hemostasis Interventions like endoscopic therapy or balloon tamponade may be used to stop bleeding.
- Chronic or Recurrent Bleeding
- Medications Proton pump inhibitors (PPIs) or H2 receptor antagonists to reduce stomach acid and promote healing.
- Endoscopic Interventions For example, banding or sclerotherapy for esophageal varices.
- Surgical Intervention In cases where endoscopic therapy is ineffective or not feasible.
- Treatment of Underlying Cause This may include antibiotics for H. pylori infections, discontinuation of NSAIDs, or management of portal hypertension in liver disease.
Nursing Care and Interventions
- Regularly assess vital signs, including blood pressure, heart rate, and respiratory rate.
- Monitor for signs of hypovolemic shock, such as altered mental status and low urine output.
- Evaluate stool and vomitus for color, consistency, and presence of blood.
- Administer IV fluids and blood products as prescribed to maintain hemodynamic stability.
- Monitor for signs of fluid overload or transfusion reactions.
- Administer medications like PPIs or vasoactive drugs as prescribed.
- Educate the patient about the purpose, dosage, and potential side effects of medications.
- Provide education and emotional support to alleviate anxiety about tests like endoscopy or angiography.
- Ensure informed consent is obtained, and the patient understands the procedure.
- Educate about the underlying cause of bleeding, treatment options, and signs of recurrence.
- Emphasize the importance of compliance with medications and follow-up appointments.
Conclusion
- Gastrointestinal bleeding demands prompt evaluation and intervention to prevent life-threatening complications.
- Successful management hinges on identifying the underlying cause and tailoring treatment accordingly.
- Timely fluid resuscitation and blood product administration are critical in acute bleeding episodes.
- Endoscopic interventions and surgical procedures may be necessary for definitive hemostasis.
- Addressing the root cause, such as H. pylori eradication or cessation of NSAID use, is pivotal in preventing recurrence.
- Nursing vigilance, patient education, and interdisciplinary collaboration are vital for comprehensive care.
- Understanding the pathophysiology and treatment options empowers healthcare professionals to deliver effective care.
Summary
- Gastrointestinal bleeding encompasses a range of conditions, from peptic ulcers to varices, necessitating diverse management approaches.
- Risk factors like NSAID use and liver disease amplify the likelihood of bleeding episodes and inform treatment decisions.
- Pathophysiologically, bleeding may arise from erosions, ulcers, varices, or vascular malformations, demanding tailored interventions.
- Clinical presentation varies, encompassing hematemesis, melena, abdominal pain, and signs of hypovolemic shock.
- Diagnostic tests like endoscopy and angiography pinpoint bleeding sources, guiding subsequent management.
- Acute bleeding episodes require immediate intervention, including fluid resuscitation and potentially endoscopic or surgical hemostasis.
- Nurses play a pivotal role in assessment, education, and coordination of care, ensuring optimal patient outcomes in cases of gastrointestinal bleeding.
Pancreatitis
Introduction
- Pancreatitis is the inflammation of the pancreas, a vital digestive organ located behind the stomach.
- It can occur as acute pancreatitis, which is sudden and short-term, or as chronic pancreatitis, which is long-lasting and progressive.
- Acute pancreatitis is characterized by the rapid onset of severe abdominal pain and systemic symptoms.
- Chronic pancreatitis involves the gradual destruction of pancreatic tissue, leading to impaired digestion and absorption of nutrients.
- Understanding the risk factors, pathophysiology, and clinical presentation is crucial for accurate diagnosis and effective management.

Risk Factors
- Gallstones and bile duct obstructions, which can lead to pancreatic enzyme activation within the pancreas.
- Chronic alcohol consumption, which can cause ongoing inflammation and damage to the pancreas.
- Smoking, as it increases the risk of both acute and chronic pancreatitis.
- High levels of triglycerides in the blood (hypertriglyceridemia), which can lead to fat-induced pancreatitis.
- Family history of pancreatitis or genetic mutations associated with the condition.
- Certain medications, such as corticosteroids and some antibiotics, can contribute to pancreatitis.
- Conditions like hypercalcemia, cystic fibrosis, and autoimmune disorders can predispose individuals to pancreatitis.
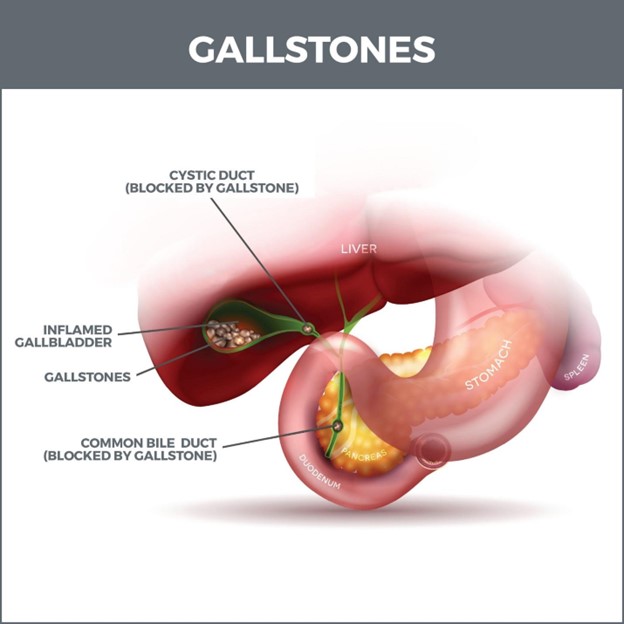
Pathophysiology
- In acute pancreatitis, an initial insult triggers the activation of pancreatic enzymes prematurely within the gland, leading to autodigestion.
- Enzymes like trypsin, lipase, and amylase can cause tissue damage and inflammation, leading to localized or systemic complications.
- In chronic pancreatitis, ongoing inflammation and fibrosis result in the replacement of normal pancreatic tissue with nonfunctional scar tissue.
- This leads to exocrine insufficiency, impairing the secretion of digestive enzymes, and endocrine insufficiency, affecting insulin production.
- In both acute and chronic pancreatitis, complications can include pseudocysts, abscesses, and vascular complications.
- Understanding the underlying pathophysiology is crucial for tailoring treatment and preventing further damage.
Clinical Presentation
- Severe abdominal pain, typically in the upper abdomen, radiating to the back, often described as steady and piercing.
- Nausea and vomiting, often accompanied by anorexia and a distaste for fatty foods.
- Abdominal tenderness and guarding on physical examination, reflecting inflammation of the pancreas.
- Elevated heart rate and blood pressure, reflecting systemic response to inflammation and pain.
- Jaundice in cases where the bile duct is obstructed by inflammation or gallstones.
- Grey-Turner's sign (bruising over the flanks) or Cullen's sign (periumbilical bruising) in severe cases with hemorrhagic complications.
- Hypovolemic shock in severe cases with extensive tissue damage and vascular complications.
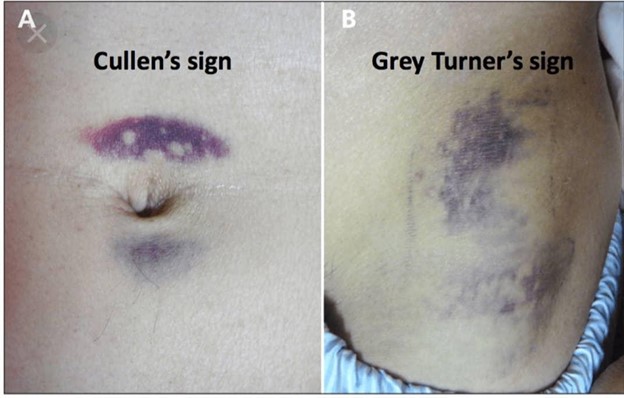
Diagnostic Tests
- Serum Amylase and Lipase levels are elevated in pancreatitis due to the release of these enzymes from damaged pancreatic cells.
- Complete Blood Count (CBC) may show elevated white blood cell count, reflecting inflammation and potential infection.
- Liver Function Tests (LFTs) may be abnormal if there is biliary obstruction or liver involvement.
- Imaging Studies such as abdominal ultrasound, CT scan, or MRI can visualize the pancreas and detect complications like pseudocysts.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) may be used to evaluate the pancreatic and bile ducts.
- Fecal Fat Test may reveal malabsorption in chronic pancreatitis due to impaired enzyme secretion.
- Glucose Tolerance Test can assess for diabetes, which can develop due to endocrine insufficiency.
Management
Acute Pancreatitis
- NPO (Nothing by Mouth) Initially, the patient is kept NPO to rest the pancreas and prevent further stimulation of enzyme secretion.
- IV Fluid Resuscitation Intravenous fluids are administered to maintain hydration and correct any electrolyte imbalances.
- Pain Management Analgesics are given to manage severe pain, with careful consideration to avoid opioids if possible.
- Nutritional Support Enteral nutrition may be initiated once the patient stabilizes to promote healing and prevent malnutrition.
Chronic Pancreatitis
- Pancreatic Enzyme Replacement Enzyme supplements are provided with meals to aid in digestion and prevent malabsorption.
- Nutritional Support A diet low in fat and high in carbohydrates and protein is recommended to reduce stress on the pancreas.
- Pain Management Chronic pain may require a multidisciplinary approach, including medications, lifestyle modifications, and psychological support.
- Management of Complications Interventions such as drainage of pseudocysts or treatment of bile duct strictures may be necessary.
- Surgical Interventions
- Surgical options may include removal of diseased portions of the pancreas (pancreatectomy) or drainage procedures for pseudocysts.
- In severe cases of chronic pancreatitis, pancreaticoduodenectomy (Whipple procedure) may be considered.
- Lifestyle Modifications
- Abstaining from alcohol is crucial in preventing further damage, particularly in cases of alcoholic pancreatitis.
- Smoking cessation is recommended to reduce the risk of recurrent episodes.
- Management of Complications
- Addressing complications like diabetes, bile duct strictures, and pseudocysts is essential in comprehensive care.
Nursing Care and Interventions
- Pain Management:
- Administering analgesics and monitoring pain levels.
- Positioning for comfort and providing relaxation techniques.
- Fluid and Electrolyte Balance:
- Monitoring intake and output, electrolyte levels, and signs of dehydration or fluid overload.
- Administering intravenous fluids as prescribed.
- Nutritional Support:
- Collaborating with dietitians to develop a plan that meets the patient's nutritional needs while minimizing stress on the pancreas.
- Monitoring for signs of malnutrition or complications related to nutritional status.
- Patient and Family Education:
- Providing information about the condition, treatment plan, and lifestyle modifications.
- Educating on signs of complications and when to seek medical attention.
- Emotional Support:
- Offering emotional support and coping strategies to help the patient navigate the physical and emotional challenges of pancreatitis.
- Assessment and Monitoring
- Regularly assessing vital signs, abdominal pain, and signs of complications.
- Monitoring laboratory values such as amylase, lipase, and blood glucose levels.
- Preparation for Procedures:
- Educating the patient about diagnostic tests and surgical procedures, ensuring they understand the purpose and potential outcomes.
- Offering emotional support to alleviate anxiety or concerns about the procedure.
Conclusion
- Pancreatitis, whether acute or chronic, presents significant challenges in diagnosis and management.
- Effective care involves a multidisciplinary approach, including medical, surgical, and nursing interventions.
- Understanding the risk factors, pathophysiology, and treatment options is crucial for providing optimal care.
Summary
- Pancreatitis encompasses acute and chronic inflammation of the pancreas, demanding varied management approaches.
- Risk factors range from gallstones to chronic alcohol consumption, influencing the course and treatment strategies.
- Pathophysiologically, autodigestion due to enzyme activation characterizes acute pancreatitis, while chronic inflammation leads to fibrosis and functional impairment.
- Clinical presentation includes severe abdominal pain, nausea, vomiting, and potential systemic complications.
- Diagnostic tests like serum amylase, imaging studies, and endoscopy pinpoint the diagnosis, guiding subsequent management.
- Care involves pain management, fluid and electrolyte balance, nutritional support, and surgical interventions as needed.
- Nurses play a pivotal role in assessment, education, emotional support, and coordination of care, ensuring optimal patient outcomes in cases of pancreatitis.
Appendicitis
Introduction
- Appendicitis is the inflammation of the appendix, a small pouch-like structure located at the beginning of the large intestine.
- It is considered a surgical emergency and requires prompt intervention to prevent complications like perforation.
- The exact cause of appendicitis is often unclear, but it is believed to involve obstruction of the appendix by fecal material, foreign bodies, or infection.
- Understanding the risk factors, pathophysiology, and clinical presentation is crucial for accurate diagnosis and timely management.
- If left untreated, appendicitis can lead to serious complications such as abscess formation or peritonitis.
Risk Factors
- Age Most common in individuals between 10 and 30 years old.
- Gender Slightly more common in males, although it can occur in both sexes.
- Family History There may be a genetic predisposition to appendicitis.
- Obstruction Fecaliths (hardened pieces of stool), lymphoid hyperplasia, or tumors can obstruct the lumen of the appendix.
- Infections Gastrointestinal infections can lead to inflammation and swelling of the lymphoid tissue in the appendix.
- Gastrointestinal Conditions Conditions like Crohn's disease or ulcerative colitis can increase the risk of appendicitis.
- Prior Abdominal Surgery Previous surgeries may increase the risk of adhesions or blockages in the appendix.
Pathophysiology
- Appendicitis often begins with an obstruction of the appendix, leading to an accumulation of mucus and increased pressure.
- As pressure builds, blood flow to the appendix is compromised, leading to ischemia and tissue necrosis.
- Bacterial overgrowth within the obstructed appendix can further contribute to inflammation and infection.
- If not promptly treated, the appendix may perforate, allowing the contents to spill into the abdominal cavity, potentially leading to peritonitis.
- Abscess formation may occur as the body attempts to wall off the infected area.
- Understanding the pathophysiology is crucial for recognizing the urgency of surgical intervention.
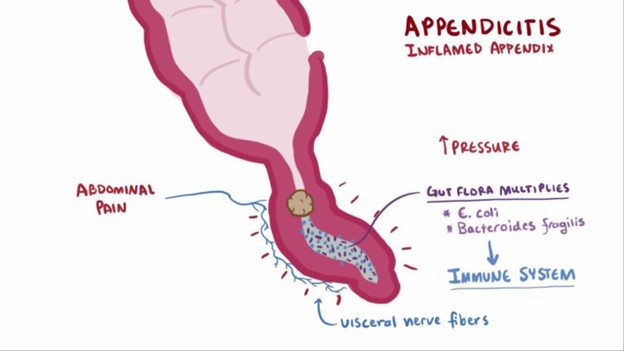
Clinical Presentation
- Periumbilical Pain Initial pain is often diffuse and located near the umbilicus, later migrating to the right lower quadrant (RLQ).
- Anorexia and Nausea Loss of appetite and feelings of nausea may accompany the abdominal pain.
- Vomiting Some individuals may experience vomiting, particularly as the condition progresses.
- Fever and Elevated White Blood Cell Count (WBC) Inflammation and infection lead to systemic signs of infection.
- Localized Tenderness and Guarding in RLQ On physical examination, there is tenderness upon palpation, particularly in McBurney's point (RLQ).
- Rebound Tenderness Pain increases upon the release of pressure after palpation.
- Rovsing's Sign Pain in the RLQ when pressure is applied to the left lower quadrant.
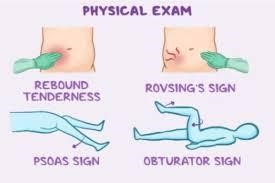
Diagnostic Tests
- Physical Examination Clinical assessment of signs and symptoms, including localized tenderness and guarding.
- Complete Blood Count (CBC) Elevated WBC count indicates an inflammatory response.
- Urinalysis Helps rule out urinary tract infection or kidney stones, which can mimic appendicitis.
- Abdominal Imaging Ultrasound or CT scan may be performed to visualize the appendix and identify signs of inflammation or obstruction.
- Pregnancy Test In female patients of childbearing age, ruling out pregnancy is crucial before undergoing imaging studies.
- Laparoscopy (in some cases) A minimally invasive surgical procedure to directly visualize the appendix for diagnostic and potentially therapeutic purposes.
- Exploratory Laparotomy (in emergencies) If clinical signs suggest acute appendicitis, surgery may be performed without pre-operative imaging.
Management
- Surgical Removal (Appendectomy):
- Appendectomy is the standard treatment for appendicitis and involves the removal of the inflamed appendix.
- It can be performed laparoscopically (minimally invasive) or through an open incision, depending on the severity and surgeon's preference.
- Antibiotics:
- Broad-spectrum antibiotics are administered intravenously before surgery to combat infection and reduce the risk of complications.
- Postoperatively, a course of antibiotics may be prescribed to ensure complete eradication of any residual infection.
- Pain Management:
- Analgesics are provided to alleviate pain and discomfort, both pre- and post-operatively.
- Pain management is crucial for early ambulation and recovery.
- Monitoring for Complications:
- After surgery, close monitoring for signs of infection, wound healing, and bowel function is essential.
- Complications like abscess formation, wound infection, or ileus may require additional intervention.
- Dietary Advancement:
- Initially, the patient is kept NPO (Nothing by Mouth) to rest the digestive tract.
- Diet is gradually advanced as tolerated, starting with clear liquids and progressing to regular meals.
Nursing Care and Interventions
- Regularly assess and document pain levels using a standardized pain scale.
- Administer analgesics as prescribed, monitor for side effects, and evaluate their effectiveness.
- Monitor vital signs, including temperature, heart rate, blood pressure, and respiratory rate, for signs of complications.
- Assess the surgical incision for signs of infection, hematoma, or dehiscence.
- Encourage early ambulation to prevent complications like atelectasis and deep vein thrombosis.
- Collaborate with dietitians to progress the patient's diet as tolerated, ensuring adequate nutrition for healing.
- Provide education on dietary modifications, such as avoiding high-fiber or high-fat foods initially.
- Perform meticulous wound care, ensuring cleanliness and sterile technique to prevent infection.
- Educate the patient on signs of infection and when to seek medical attention.
- Offer emotional support, address concerns, and provide information to alleviate anxiety or fears related to the surgical procedure.
- Provide information about postoperative care, including activity restrictions, diet, wound care, and signs of complications.
- Educate on the importance of follow-up appointments and adherence to prescribed medications.
Conclusion
- Appendicitis is a common surgical emergency characterized by inflammation of the appendix.
- Timely surgical intervention (appendectomy) is the cornerstone of treatment.
- Postoperative care, including pain management, wound care, and monitoring for complications, is crucial for optimal recovery.
Summary
- Appendicitis requires prompt recognition and surgical intervention to prevent complications.
- Risk factors include age, gender, family history, and prior abdominal surgery.
- Pathophysiologically, obstruction of the appendix leads to inflammation, infection, and potential perforation.
- Clinical presentation includes periumbilical pain, anorexia, vomiting, and localized tenderness in the RLQ.
- Diagnostic tests include physical examination, laboratory studies, imaging, and sometimes exploratory surgery.
- Management involves appendectomy, antibiotics, pain management, and postoperative care.
- Nursing care encompasses pain assessment, postoperative monitoring, wound care, patient education, and emotional support.
Inflammatory bowel disease
Introduction
- Inflammatory Bowel Disease (IBD) refers to a group of chronic disorders characterized by inflammation of the gastrointestinal tract.
- The two primary forms of IBD are Crohn's Disease (CD) and Ulcerative Colitis (UC), each with distinct characteristics.
- IBD is a complex condition with a multifactorial etiology, involving genetic, environmental, and immunologic factors.
- It often manifests during adolescence or early adulthood, but can occur at any age.
- Understanding the risk factors, pathophysiology, clinical presentation, and management strategies is crucial for providing comprehensive care.
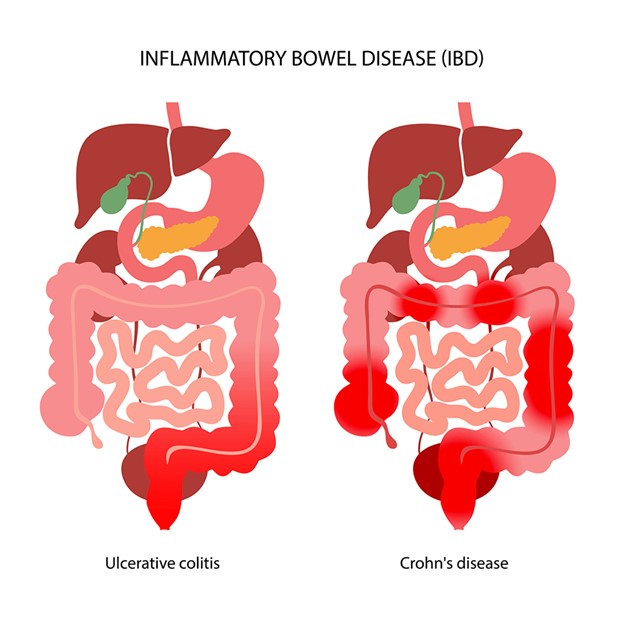
Risk Factors
- Genetic Predisposition Family history of IBD increases the risk of developing the condition.
- Environmental Factors Exposure to certain environmental triggers, such as infections or dietary factors, may play a role.
- Immune System Dysfunction Abnormal immune response in the gastrointestinal tract may contribute to the development of IBD.
- Smoking Smoking is a significant risk factor for the development of Crohn's disease, but paradoxically appears to have a protective effect in ulcerative colitis.
- Age IBD can occur at any age, but is most commonly diagnosed in adolescents and young adults.
- Ethnicity Certain ethnic groups, such as Ashkenazi Jews, have a higher prevalence of IBD.
- Geographical Location IBD is more prevalent in Western industrialized countries, suggesting a potential environmental influence.
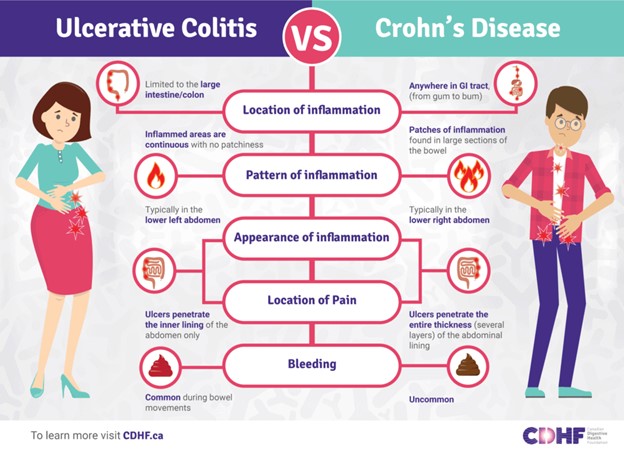
Pathophysiology
- Crohn's Disease (CD):
- Can affect any part of the gastrointestinal tract from mouth to anus, often characterized by skip lesions.
- Transmural inflammation involves all layers of the bowel wall, leading to fibrosis, strictures, and potential fistula formation.
- Inflammation may lead to malabsorption, nutritional deficiencies, and systemic complications.
- Ulcerative Colitis (UC):
- Limited to the colon and rectum, typically starting in the rectum and extending proximally in a continuous fashion.
- Mucosal inflammation primarily involves the inner lining of the colon, leading to friability, ulcers, and bleeding.
- May lead to complications like toxic megacolon and colorectal cancer, particularly in cases of long-standing disease.
- Immunologic Dysregulation Aberrant immune response in IBD involves a combination of genetic predisposition, altered gut microbiota, and environmental triggers.
- Role of Gut Microbiota Dysbiosis, or imbalance in gut microbiota, may contribute to the development and progression of IBD.
Clinical Presentation
- Common Symptoms Shared by CD and UC:
- Diarrhea, often bloody, due to inflammation and ulceration of the intestinal lining.
- Abdominal pain and cramping, varying in location and intensity depending on the subtype and location of the disease.
- Weight loss and malnutrition, resulting from reduced nutrient absorption and increased metabolic demands.
- Fatigue and weakness due to chronic inflammation, anemia, and nutritional deficiencies.
- Extraintestinal Manifestations: IBD can affect other organs, leading to symptoms like joint pain, skin lesions, and eye inflammation.
- Additional Symptoms Specific to CD:
- Perianal Fistulas and Abscesses: Resulting from chronic inflammation and tissue breakdown.
- Strictures and Obstructions: Due to fibrosis and scarring in the bowel wall.
- Additional Symptoms Specific to UC:
- Tenesmus: Frequent, urgent, and painful urges to defecate, often with little stool passed.
- Rectal Bleeding: Common in UC due to mucosal ulcerations.
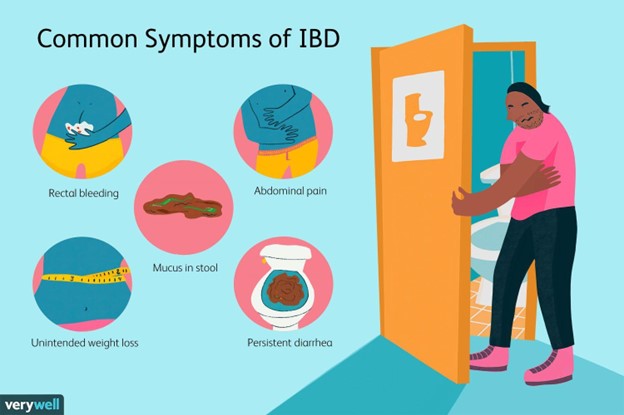
Diagnostic Tests
- Endoscopy and Biopsy:
- Colonoscopy and sigmoidoscopy allow direct visualization of the colon and rectum to assess the extent and severity of inflammation.
- Biopsies are taken during these procedures to confirm the diagnosis and evaluate for dysplasia or malignancy.
- Blood Tests:
- Complete Blood Count (CBC) may reveal anemia, leukocytosis, or thrombocytosis, indicating inflammation or bleeding.
- Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein (CRP) levels are elevated in the presence of inflammation.
- Serum Albumin and Prealbumin levels may be low, indicating malnutrition and inflammation.
- Stool Studies:
- Fecal Calprotectin and Fecal Lactoferrin levels are elevated in IBD, indicating inflammation in the gastrointestinal tract.
- Stool cultures and tests for pathogens are performed to rule out infectious causes of gastrointestinal symptoms.
- Imaging Studies:
- Abdominal CT scan or MRI can provide detailed images of the gastrointestinal tract, assessing for complications like abscesses or strictures.
- Small Bowel Follow-Through or Capsule Endoscopy may be used to evaluate the small intestine in cases of suspected CD.
- Barium Enema or Lower GI Series (for UC):
- This imaging test uses contrast material to visualize the colon and rectum, helping to identify areas of inflammation or strictures.
Management
- Aminosalicylates, Corticosteroids, Immunomodulators, and Biologic Therapies may be prescribed to induce and maintain remission.
- Anti-diarrheal medications and pain relief may also be used to manage symptoms.
- In severe cases or during active flares, enteral or parenteral nutrition may be required to provide adequate nutrition.
- In cases of complications like strictures, fistulas, or toxic megacolon, surgery may be necessary to remove affected portions of the intestine.
- Colectomy may be indicated in cases of refractory UC or if dysplasia/cancer is present.
- Stress reduction, regular exercise, and a balanced diet can help manage symptoms and support overall well-being.
- Regular appointments with healthcare providers are essential for disease management, medication adjustments, and surveillance for complications.
Nursing Care and Interventions
- Provide comprehensive education about IBD, including medication management, dietary recommendations, and symptom recognition.
- Offer emotional support and resources for coping with chronic illness and potential lifestyle changes.
- Collaborate with dietitians to ensure patients receive adequate nutrition, addressing any specific dietary restrictions or needs.
- Monitor for signs of malnutrition and offer guidance on maintaining a balanced diet.
- Administer prescribed medications, educating patients on dosage, timing, and potential side effects.
- Monitor for medication adherence and report any concerns to the healthcare provider.
- Assist in pain relief measures and provide interventions for managing gastrointestinal symptoms.
- Serve as an advocate for the patient, ensuring their needs are communicated and addressed by the healthcare team.
- Collaborate with other healthcare professionals to provide holistic care.
Conclusion
- Inflammatory Bowel Disease encompasses Crohn's Disease and Ulcerative Colitis, chronic disorders requiring lifelong management.
- Effective care involves a combination of pharmacologic interventions, nutritional support, and surgical options in severe cases.
Summary
- Inflammatory Bowel Disease, comprising Crohn's Disease and Ulcerative Colitis, is characterized by chronic inflammation of the gastrointestinal tract.
- Risk factors include genetic predisposition, environmental influences, and immune system dysfunction.
- Pathophysiologically, CD and UC have distinct features, but both involve inflammation and potential complications.
- Clinical presentation includes abdominal pain, diarrhea, weight loss, and various extraintestinal manifestations.
- Diagnostic tests encompass endoscopy, blood work, stool studies, and imaging studies to confirm the diagnosis and assess disease severity.
- Management includes pharmacologic interventions, nutritional support, surgery when necessary, and lifestyle modifications.
- Nursing care involves education, nutritional support, medication administration, symptom management, advocacy, and coordination of care to optimize patient outcomes in IBD.
Irritable bowel syndrome
Introduction
- Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder characterized by chronic abdominal pain and altered bowel habits.
- It is a common condition that affects the large intestine and is associated with a range of symptoms such as bloating, diarrhea, and constipation.
- IBS is considered a diagnosis of exclusion, meaning other conditions with similar symptoms must be ruled out before confirming IBS.
- The exact cause of IBS is unknown, but it is believed to involve a combination of genetic, environmental, and psychosocial factors.
- Understanding the risk factors, pathophysiology, clinical presentation, and management strategies is crucial for providing comprehensive care.
Risk Factors
- Gender IBS is more commonly diagnosed in women than in men.
- Age It can occur at any age, but is most commonly diagnosed in individuals under 50.
- Family History There may be a genetic predisposition to IBS, suggesting a familial link.
- Psychosocial Factors Stress, anxiety, and depression can exacerbate symptoms in individuals with IBS.
- Gastrointestinal Infections Previous bouts of bacterial gastroenteritis may increase the risk of developing IBS.
- Food Intolerances Certain types of carbohydrates (FODMAPs) can trigger or worsen IBS symptoms in some individuals.
- Hormonal Changes Some individuals may experience changes in symptom severity during menstruation.
Pathophysiology
- Altered Gut Motility IBS can involve abnormal contractions of the colon, leading to either accelerated transit (diarrhea-predominant) or slowed transit (constipation-predominant).
- Visceral Hypersensitivity Individuals with IBS may have a heightened sensitivity to normal sensations in the gastrointestinal tract.
- Brain-Gut Interaction Dysregulation of the communication between the brain and gut can lead to abnormal responses to stress and stimuli.
- Microbiota Imbalance Alterations in the gut microbiota composition may play a role in IBS development and symptom exacerbation.
- Low-Grade Inflammation (in some cases) While IBS is primarily considered a functional disorder, some individuals may exhibit low-grade inflammation in the intestine.
- Central Nervous System Sensitization Changes in the central nervous system's processing of pain signals may contribute to the perception of pain in IBS.
- Immune System Activation (in some cases) Immune system activation and low-grade inflammation may contribute to symptom generation in a subset of individuals.
Clinical Presentation
- Abdominal Pain and Discomfort Typically relieved with defecation and associated with changes in stool frequency or form.
- Altered Bowel Habits Can present as diarrhea-predominant, constipation-predominant, or mixed (alternating between diarrhea and constipation).
- Bloating and Distention Many individuals with IBS experience abdominal bloating, often worsening as the day progresses.
- Mucus in Stool Some individuals may notice an increased presence of mucus in their stool.
- Symptom Flares with Stress Stress, anxiety, and emotional triggers can exacerbate IBS symptoms.
- Sensation of Incomplete Evacuation Individuals may feel that they have not fully emptied their bowels after a bowel movement.
- Exacerbation with Certain Foods Some individuals may notice that specific foods or food groups worsen their symptoms.
Diagnostic Tests
- Clinical Evaluation Diagnosis of IBS is primarily based on clinical criteria, including the presence of characteristic symptoms and absence of alarming signs.
- Rome Criteria The Rome IV criteria are widely used for diagnosing IBS, requiring the presence of specific symptoms over a defined period.
- Stool Studies Stool tests may be performed to rule out infectious causes or other gastrointestinal conditions that can mimic IBS.
- Blood Tests Blood work may be done to assess for markers of inflammation or to rule out other conditions.
- Colonoscopy or Sigmoidoscopy (in select cases) These procedures may be performed if there are atypical symptoms or alarming signs to rule out other conditions.
- Imaging Studies (in select cases) Imaging may be used to visualize the gastrointestinal tract and assess for any structural abnormalities.
Management
- Dietary Modifications:
- Some individuals may benefit from dietary adjustments, such as avoiding specific trigger foods or following a low-FODMAP diet.
- Pharmacologic Interventions:
- Medications may be prescribed to manage specific symptoms, such as antispasmodics for abdominal pain or laxatives for constipation.
- Psychological Interventions:
- Cognitive-behavioral therapy, relaxation techniques, and stress management may be beneficial for individuals with IBS.
- Lifestyle Modifications:
- Regular exercise, adequate sleep, and stress reduction techniques can help manage symptoms.
- Probiotics (in some cases) Probiotics may be considered to help restore balance in the gut microbiota.
- Fiber Supplements (in select cases) Soluble fiber supplements may be recommended for individuals with constipation-predominant IBS.
- Biofeedback (in select cases) This technique helps individuals gain control over physiological processes, such as muscle tension in the pelvic floor.
Nursing Care and Interventions
- Provide thorough education about IBS, including its chronic nature, triggers, and symptom management.
- Offer guidance on dietary modifications, stress reduction techniques, and the importance of regular follow-up care.
- Collaborate with dietitians to develop individualized dietary plans, addressing specific trigger foods and promoting balanced nutrition.
- Monitor for signs of malnutrition or nutritional deficiencies.
- Administer prescribed medications, educate patients on dosage, timing, and potential side effects.
- Encourage adherence to prescribed regimens and monitor for medication effectiveness.
- Teach relaxation techniques, such as deep breathing exercises or guided imagery, to help individuals manage stress.
- Offer emotional support, acknowledge the impact of IBS on quality of life, and provide resources for coping and support groups.
- Encourage patients to keep a symptom journal to monitor patterns, triggers, and the effectiveness of interventions.
- Serve as an advocate for the patient, ensuring their needs are communicated and addressed by the healthcare team.
- Collaborate with other healthcare professionals to provide holistic care.
- Irritable Bowel Syndrome is a common functional gastrointestinal disorder characterized by chronic abdominal pain and altered bowel habits.
- Management strategies focus on symptom relief, dietary modifications, stress reduction, and lifestyle adjustments.
Summary
- Irritable Bowel Syndrome (IBS) is a chronic condition characterized by abdominal pain and altered bowel habits.
- Risk factors include gender, age, family history, psychosocial factors, gastrointestinal infections, food intolerances, and hormonal changes.
- Pathophysiologically, IBS involves altered gut motility, visceral hypersensitivity, brain-gut interaction, microbiota imbalance, and potential low-grade inflammation.
- Clinical presentation includes abdominal pain, altered bowel habits, bloating, mucus in stool, symptom flares with stress, sensation of incomplete evacuation, and exacerbation with certain foods.
- Diagnosis is based on clinical evaluation, adherence to Rome Criteria, and ruling out other conditions through stool studies, blood tests, and, in select cases, endoscopy or imaging studies.
- Management includes dietary modifications, pharmacologic interventions, psychological interventions, lifestyle modifications, probiotics, fiber supplements, and biofeedback.
- Nursing care involves education, dietary guidance, medication administration, stress management, supportive care, symptom tracking, advocacy, and coordination of care to optimize patient outcomes in IBS.
Liver Diseases: Hepatitis, Cirrhosis
Introduction
- Liver diseases encompass a range of conditions that affect the liver's structure and function.
- Hepatitis and cirrhosis are two significant categories of liver diseases, each with distinct characteristics and causes.
- Understanding the risk factors, pathophysiology, clinical presentation, and management strategies is crucial for providing comprehensive care to individuals with liver diseases.
Risk Factors
- Hepatitis:
- Hepatitis A Contaminated food or water, close contact with an infected person.
- Hepatitis B Unprotected sex, sharing needles, childbirth from an infected mother, occupational exposure.
- Hepatitis C Sharing needles, receiving contaminated blood products, healthcare worker exposure.
- Hepatitis D Coinfection with hepatitis B.
- Hepatitis E Contaminated food or water, especially in areas with poor sanitation.
- Cirrhosis:
- Chronic Alcohol Abuse Excessive and prolonged alcohol consumption can lead to alcoholic liver disease and cirrhosis.
- Chronic Hepatitis Prolonged inflammation and damage from chronic viral hepatitis (B, C, or D).
- Nonalcoholic Fatty Liver Disease (NAFLD) Associated with obesity, diabetes, and metabolic syndrome.
- Autoimmune Hepatitis The body's immune system mistakenly attacks the liver.
- Hemochromatosis Excessive iron accumulation in the liver.
- Wilson's Disease Inherited disorder leading to copper buildup in the liver.
- Alpha-1 Antitrypsin Deficiency Genetic condition affecting liver and lung function.
Pathophysiology
- Hepatitis
- Hepatitis is characterized by inflammation of the liver tissue, often due to viral infections or other causes.
- Viral hepatitis leads to direct injury to hepatocytes (liver cells) and an immune response.
- In severe cases, ongoing inflammation can lead to fibrosis and cirrhosis.
- Chronic hepatitis can result in long-term liver damage, increasing the risk of cirrhosis and hepatocellular carcinoma.
- Cirrhosis
- Cirrhosis is the end stage of chronic liver disease, characterized by extensive scarring and fibrosis of the liver tissue.
- Ongoing liver damage and inflammation lead to the replacement of normal liver tissue with fibrous scar tissue.
- This disrupts the liver's normal structure and function, impeding blood flow and impairing liver cell regeneration.
- Compensated cirrhosis implies the liver can still perform basic functions, while decompensated cirrhosis indicates significant liver dysfunction.
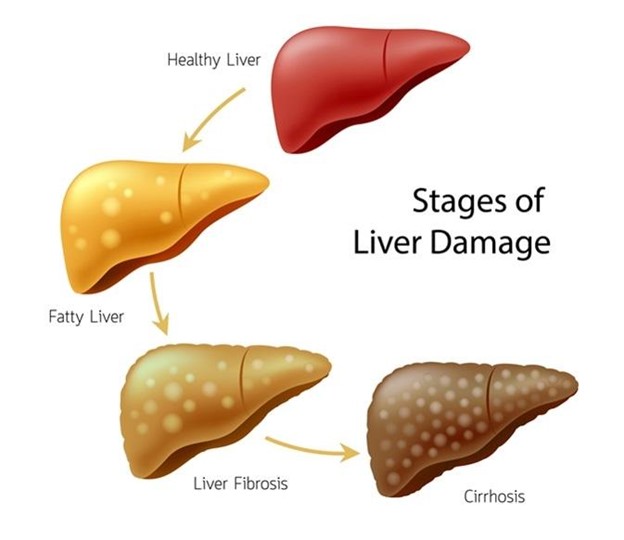
Clinical Presentation
- Hepatitis
- Jaundice Yellowing of the skin and eyes due to elevated bilirubin levels.
- Fatigue Persistent tiredness and weakness.
- Abdominal Pain Discomfort or tenderness in the upper right quadrant of the abdomen.
- Nausea and Vomiting Digestive symptoms often accompanied by loss of appetite.
- Dark Urine and Pale Stools Changes in urine and stool color due to altered bilirubin metabolism.
- Fever and Flu-like Symptoms Common in acute viral hepatitis.
- Enlarged Liver or Spleen (in some cases).
- Cirrhosis
- Fatigue Overwhelming tiredness and weakness.
- Jaundice Yellowing of the skin and eyes due to impaired bilirubin processing.
- Edema and Ascites Fluid retention leading to swelling in the legs (edema) and abdominal swelling (ascites).
- Easy Bruising and Bleeding Reduced production of blood clotting factors and portal hypertension.
- Confusion and Cognitive Impairment Hepatic encephalopathy due to impaired detoxification of ammonia.
- Spider Angiomas and Palmar Erythema Skin changes associated with altered hormone metabolism.
- Gastrointestinal Bleeding (from esophageal varices) in severe cases.
Diagnostic Tests
- Liver Function Tests (LFTs) assess liver enzyme levels, bilirubin, and albumin.
- Viral Hepatitis Serology tests identify specific antibodies or antigens for hepatitis viruses.
- Coagulation Studies evaluate blood clotting factors to assess liver function.
- Ultrasound, CT scan, or MRI can visualize the liver, identify structural changes, and assess for signs of cirrhosis or hepatocellular carcinoma.
- FibroScan or transient elastography measures liver stiffness, providing an estimate of fibrosis.
- A sample of liver tissue is obtained for microscopic examination, providing detailed information about liver structure and function.
- Upper gastrointestinal endoscopy can identify esophageal varices, a complication of cirrhosis.
Management
- Hepatitis
- Supportive Care Rest, hydration, and proper nutrition are essential for recovery in acute cases.
- Antiviral Medications (if applicable) Depending on the type of hepatitis, antiviral drugs may be prescribed to suppress viral replication.
- Vaccination (for Hepatitis A and B) Vaccines are available to prevent future infections.
- Avoidance of Alcohol and Hepatotoxic Substances To prevent further liver damage.
- Cirrhosis
- Lifestyle Modifications Abstinence from alcohol, dietary changes, and sodium restriction to manage fluid retention.
- Management of Complications Addressing complications such as ascites, hepatic encephalopathy, and bleeding varices.
- Medications Depending on specific symptoms or complications, medications may be prescribed (e.g., diuretics, beta-blockers).
- Liver Transplant (in severe cases) Considered for end-stage cirrhosis when liver function is severely compromised.
Nursing Care and Interventions
- Provide comprehensive education about liver disease, including etiology, progression, and symptom management.
- Emphasize the importance of medication adherence, lifestyle modifications, and regular follow-up care.
- Collaborate with dietitians to develop individualized dietary plans, addressing specific dietary restrictions and promoting balanced nutrition.
- Monitor for signs of malnutrition and nutritional deficiencies.
- Administer prescribed medications, educate patients on dosage, timing, and potential side effects.
- Encourage adherence to prescribed regimens and monitor for medication effectiveness.
- Monitor for signs of fluid retention and electrolyte imbalance, particularly in cirrhosis with ascites or edema.
- Administer diuretics or other medications as prescribed.
- Implement bleeding precautions, including avoiding activities that may increase the risk of bleeding.
- Monitor for signs of bleeding, such as petechiae, ecchymosis, or melena.
- Address emotional and psychological aspects of living with liver disease, offering resources for coping and support groups.
- Encourage open communication about fears, concerns, and quality of life.
- Regularly assess for signs of complications such as hepatic encephalopathy, ascites, or bleeding.
- Intervene promptly and communicate findings to the healthcare team.
Conclusion
- Liver diseases, including hepatitis and cirrhosis, can have significant implications for an individual's health and quality of life.
- Timely diagnosis, appropriate management, and supportive care are crucial for optimizing outcomes.
Summary
- Liver diseases encompass a range of conditions affecting the liver's structure and function, including hepatitis and cirrhosis.
- Risk factors for these conditions vary, with viral infections being a common cause of hepatitis and factors like alcohol abuse contributing to cirrhosis.
- Hepatitis involves inflammation of the liver tissue, while cirrhosis is characterized by extensive scarring and fibrosis, leading to impaired liver function.
- Clinical presentations differ based on the type and severity of the liver disease, ranging from jaundice and fatigue to complications like ascites and hepatic encephalopathy.
- Diagnostic tests include blood work, imaging studies, liver biopsy, and endoscopy, providing essential information for diagnosis and management.
- Management strategies involve lifestyle modifications, medication administration, and interventions to address specific complications or symptoms.
- Nursing care focuses on education, nutritional support, medication management, monitoring for complications, and providing psychosocial support to individuals with liver diseases.
Gastrointestinal Cancers
Introduction
- Gastrointestinal (GI) cancers refer to malignancies that develop in various parts of the digestive system, including the esophagus, stomach, intestines, liver, pancreas, and anus.
- They are among the most common types of cancer worldwide, with varying incidence rates based on geographical and demographic factors.
- Understanding the risk factors, pathophysiology, clinical presentation, and management strategies is crucial for providing comprehensive care to individuals with GI cancers.
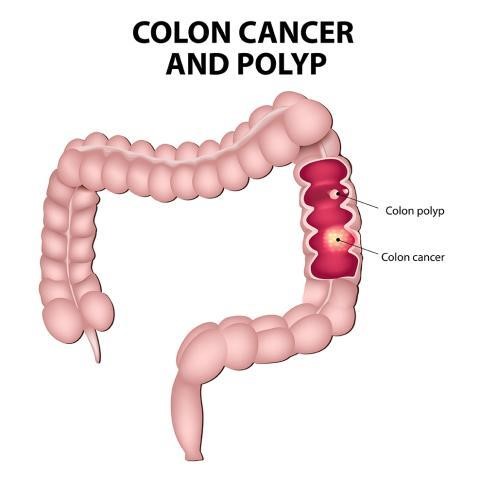
Risk Factors
- Age Incidence of GI cancers increases with age, particularly in individuals over 50.
- Family History Genetic predisposition and certain inherited syndromes can increase the risk.
- Dietary Factors Consumption of processed meats, low-fiber diets, and excessive alcohol intake can contribute.
- Tobacco Use Smoking is a significant risk factor for various GI cancers, including esophageal, stomach, and pancreatic cancer.
- Chronic Inflammation Conditions like Barrett's esophagus, inflammatory bowel disease, and chronic viral hepatitis can elevate risk.
- Obesity is associated with an increased risk of several GI cancers, including esophageal, colorectal, and pancreatic cancer.
- Infectious Agents Infections such as Helicobacter pylori (associated with stomach cancer) and certain viruses (e.g., HPV, hepatitis B and C) can contribute.
Pathophysiology
- Initiation and Promotion of Cancer Cells Genetic mutations or alterations in cell signaling pathways lead to uncontrolled cell growth and division.
- Invasion and Metastasis Cancer cells can invade nearby tissues and, in advanced stages, spread to distant sites via lymphatic or blood vessels.
- Angiogenesis Tumors stimulate the formation of new blood vessels to supply nutrients and oxygen, supporting their growth.
- Immune Evasion Cancer cells can evade the immune system's surveillance mechanisms, allowing them to proliferate unchecked.
- Tumor Microenvironment Factors like inflammation, immune cells, and signaling molecules contribute to tumor growth and progression.
- Metabolic Reprogramming Cancer cells alter their metabolism to support rapid growth and energy demands.
- Genetic and Epigenetic Changes Genetic mutations and epigenetic modifications play a crucial role in the development and progression of GI cancers.
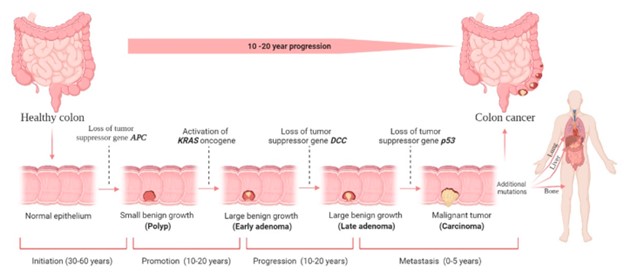
Clinical Presentation
- Esophageal Cancer:
- Dysphagia (difficulty swallowing) is a hallmark symptom, particularly with solid foods.
- Odynophagia (painful swallowing) may also be present.
- Unintentional weight loss and chest pain may occur in advanced stages.
- Gastroesophageal reflux symptoms, such as heartburn, can precede the diagnosis.
- Hoarseness or voice changes may occur with involvement of the recurrent laryngeal nerve.
- Hematemesis (vomiting blood) or melena (black, tarry stools) may indicate bleeding.
- Persistent cough or aspiration pneumonia can occur if the tumor obstructs the airway.
- Stomach (Gastric) Cancer:
- Early stages may be asymptomatic or present with vague symptoms like indigestion, bloating, or mild abdominal discomfort.
- As the tumor advances, symptoms can include persistent abdominal pain, early satiety, and a sense of fullness after eating small amounts.
- Nausea and vomiting, particularly with blood, may occur.
- Weight loss and fatigue are common, often indicating more advanced disease.
- Gastrointestinal bleeding can lead to hematemesis or melena.
- Palpable abdominal mass or lymphadenopathy may be present in advanced cases.
- Signs of metastasis may include jaundice, ascites, or bone pain.
Diagnostic Tests
- Endoscopy and Biopsy:
- Esophagogastroduodenoscopy (EGD) allows direct visualization of the esophagus and stomach, enabling tissue samples (biopsies) to be taken for examination.
- Imaging Studies:
- CT scans, MRI, and PET scans provide detailed images of the gastrointestinal tract, surrounding tissues, and potential metastatic sites.
- Blood Tests:
- Tumor markers like carcinoembryonic antigen (CEA) and CA 19-9 may be elevated in some GI cancers.
- Barium Swallow or Upper GI Series (for esophageal cancer):
- These imaging tests use contrast material to visualize the esophagus and stomach.
- Colonoscopy (for colorectal cancer):
- Allows direct visualization of the colon and rectum, with biopsies taken if suspicious lesions are identified.
- Stool Tests (for colorectal cancer)
- Fecal Occult Blood Test (FOBT) and stool DNA tests can detect traces of blood or genetic alterations associated with cancer.
Management
- Surgery:
- Often the primary treatment for resectable GI cancers, aiming to remove the tumor and any affected surrounding tissues.
- Chemotherapy:
- Systemic medications target rapidly dividing cancer cells throughout the body, often used in combination with other treatments.
- Radiation Therapy:
- High-energy rays target cancer cells and may be used preoperatively, postoperatively, or as a palliative measure.
- Targeted Therapies:
- Drugs that specifically target molecules or pathways involved in cancer growth, often with fewer side effects compared to traditional chemotherapy.
- Immunotherapy:
- Boosts the body's immune system to recognize and attack cancer cells, showing promise in some GI cancers.
- Palliative Care:
- Focuses on symptom management, pain relief, and improving quality of life for individuals with advanced or incurable GI cancers.
Nursing Care and Interventions
- Provide comprehensive education about the type of GI cancer, treatment options, and potential side effects.
- Support patients and families in making informed decisions about their care.
- Monitor and manage symptoms such as pain, nausea, fatigue, and changes in appetite.
- Address emotional and psychological aspects of living with cancer, offering resources for coping and support groups.
- Encourage open communication about fears, concerns, and quality of life.
- Collaborate with dietitians to develop individualized dietary plans, addressing specific dietary restrictions and promoting balanced nutrition.
- Monitor for signs of malnutrition and provide interventions as needed.
- Administer prescribed medications, educate patients on dosage, timing, and potential side effects.
- Encourage adherence to prescribed regimens and monitor for medication effectiveness.
Conclusion
- Gastrointestinal cancers encompass a range of malignancies affecting various parts of the digestive system, each with unique clinical characteristics and management strategies.
- Early detection, appropriate treatment, and supportive care are essential for optimizing outcomes and quality of life for individuals with GI cancers.
Summary
- Gastrointestinal cancers refer to malignancies in the digestive system, including the esophagus, stomach, intestines, liver, pancreas, and anus.
- Risk factors for GI cancers vary based on type and may include age, family history, dietary factors, tobacco use, chronic inflammation, obesity, and infectious agents.
- Pathophysiology involves genetic mutations, invasion, metastasis, angiogenesis, immune evasion, and changes in the tumor microenvironment.
- Clinical presentation varies by location and stage of cancer, with symptoms such as dysphagia, abdominal pain, weight loss, and gastrointestinal bleeding.
- Diagnostic tests encompass endoscopy, imaging studies, biopsies, blood tests, and stool tests, providing essential information for diagnosis and treatment planning.
- Management strategies include surgery, chemotherapy, radiation therapy, targeted therapies, immunotherapy, and palliative care, tailored to the specific type and stage of cancer.
- Nursing care focuses on education, symptom management, psychosocial support, nutritional support, medication management, and advocacy to optimize patient outcomes in GI cancers.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Pathophysiology of the Gastrointestinal System
This filled cannot be empty

