Please set your exam date
Infection Prevention and Control
Study Questions
Introduction
Which type of transmission-based precaution is used for a client with a diagnosis of Clostridium difficile infection?
Explanation
Contact precautions are used for clients with infections that can be transmitted through direct or indirect contact with the client or their environment. Clostridium difficile infection is primarily transmitted through contact with contaminated surfaces, requiring the use of gloves and gowns.
Incorrect choices:
a. Airborne precautions are used for diseases that are transmitted through small airborne particles.
b. Droplet precautions are used for diseases that are transmitted through large droplets produced by an infected individual.
d. Standard precautions should always be followed, but additional precautions specific to the mode of transmission (in this case, contact precautions) are necessary for effective infection control.
Which precaution is appropriate for a client with pulmonary tuberculosis?
Explanation
Pulmonary tuberculosis is primarily transmitted through airborne particles containing the Mycobacterium tuberculosis bacteria. Airborne precautions, including the use of specialized respiratory protection and negative pressure isolation rooms, are necessary to prevent its transmission.
Incorrect choices:
b. Droplet precautions are not sufficient for tuberculosis as it can be transmitted through smaller airborne particles.
c. Contact precautions are not necessary unless there are additional skin lesions or draining wounds associated with tuberculosis.
d. Standard precautions should always be followed, but additional precautions specific to the mode of transmission (in this case, airborne precautions) are required for effective infection control.
Which type of transmission-based precaution is used for a client with influenza?
Explanation
Influenza is primarily transmitted through respiratory droplets generated when an infected person coughs, sneezes, or talks. Droplet precautions, including the use of masks and maintaining a safe distance, are necessary to prevent its spread.
Incorrect choices:
a. Airborne precautions are not necessary for influenza, as it is primarily transmitted through larger respiratory droplets rather than small airborne particles.
c. Contact precautions are not required for influenza unless the client has additional conditions or infections that warrant contact precautions.
d. Standard precautions should always be followed, but additional precautions specific to the mode of transmission (in this case, droplet precautions) are required for effective infection control.
Which precaution is used for a client with chickenpox (varicella)?
Explanation
Chickenpox is highly contagious and primarily transmitted through airborne particles containing the varicella-zoster virus. Airborne precautions, including the use of specialized respiratory protection and negative pressure isolation rooms, are necessary to prevent its transmission.
Incorrect choices:
b. Droplet precautions are not sufficient for chickenpox as it can be transmitted through smaller airborne particles.
c. Contact precautions are not necessary unless there are additional skin lesions or the client has conditions that warrant contact precautions.
d. Standard precautions should always be followed, but additional precautions specific to the mode of transmission (in this case, airborne precautions) are required for effective infection control.
Transmission-Based Precautions:
Which type of transmission-based precaution is used for a client with tuberculosis?
Explanation
Airborne precautions are used for clients with infectious diseases that are spread through small airborne particles, such as tuberculosis. It involves the use of specialized respiratory protection and negative pressure isolation rooms.
Incorrect choices:
a. Contact precautions are used for diseases that can be transmitted through direct or indirect contact with the client or their environment.
b. Droplet precautions are used for diseases that are transmitted through large droplets produced when an infected person coughs, sneezes, or talks.
d. Standard precautions are the basic level of infection prevention and control measures that should be followed for all clients, regardless of their specific infectious status.
Which of the following is an example of a condition requiring contact precautions?
Explanation
Methicillin-resistant Staphylococcus aureus (MRSA) infection Explanation: MRSA is a multidrug-resistant bacterium that can be spread through direct contact with an infected individual or contaminated objects. Contact precautions, including the use of gloves and gowns, are necessary to prevent its transmission.
Incorrect choices:
a. Influenza is primarily spread through respiratory droplets and requires droplet precautions.
c. Pertussis (whooping cough) is also spread through respiratory droplets and requires droplet precautions.
d. Tuberculosis requires airborne precautions due to the risk of transmission through airborne particles.
Which precaution is appropriate for a client with a respiratory infection caused by the influenza virus?
Explanation
Droplet precautions Explanation: Influenza is primarily transmitted through respiratory droplets generated when an infected person coughs, sneezes, or talks. Droplet precautions, including wearing a mask and maintaining a safe distance, are necessary to prevent its spread.
Incorrect choices:
a. Contact precautions are not required for influenza unless the client also has additional conditions or infections that warrant contact precautions.
c. Airborne precautions are not necessary for influenza, as it is primarily transmitted through droplets rather than airborne particles.
d. Standard precautions should always be followed, but additional precautions specific to the mode of transmission (in this case, droplet precautions) are required for effective infection control.
Which precaution is used for a client with a draining wound infection?
Explanation
Contact precautions are used for clients with infections or conditions that are transmitted through direct or indirect contact with the client or their environment. A draining wound infection can potentially spread infectious material to others, requiring contact precautions, including the use of gloves and gowns.
Incorrect choices:
b. Droplet precautions are not necessary for a draining wound infection unless there is evidence of concurrent respiratory infection or the wound is contaminated with respiratory secretions.
c. Airborne precautions are not needed for a draining wound infection unless there is evidence of airborne pathogens present in the wound.
d. Standard precautions should always be followed, but additional precautions specific to the mode of transmission (in this case, contact precautions) are necessary when dealing with infectious wounds.
Hand Hygiene
When should healthcare providers perform hand hygiene?
Explanation
Hand hygiene should be performed before and after every patient contact or care activity to prevent the transmission of microorganisms.
Incorrect choices:
a. Hand hygiene should be performed before and after every patient contact or care activity, not limited to direct contact with bodily fluids.
b. Hand hygiene should be performed both before and after patient care tasks, not only after completing all tasks.
d. Hand hygiene should be performed regardless of visible dirt or contamination, as microorganisms may be present even if not visible.
What is the recommended duration for performing hand hygiene using an alcohol-based hand rub?
Explanation
The recommended duration for using an alcohol-based hand rub is approximately 15 seconds, ensuring all surfaces of the hands are thoroughly covered and rubbed until dry.
Incorrect choices:
a. 5 seconds is insufficient for proper hand hygiene using an alcohol-based hand rub.
c. 30 seconds and
d. 60 seconds are longer than necessary for using an alcohol-based hand rub and can lead to wastage of the product.
Which of the following is true regarding hand hygiene with soap and water?
Explanation
If alcohol-based hand rubs are not readily available, hand hygiene with soap and water can be used as an effective alternative.
Incorrect choices:
b. Hand hygiene with soap and water is equally effective as using hand rubs, as long as proper technique and sufficient duration are followed.
c. Hand hygiene with soap and water requires friction and rubbing to effectively remove microorganisms.
d. Hand hygiene with soap and water should be performed even if gloves were worn during patient care, as gloves may have microscopic defects or contamination.
Which of the following is an appropriate method for drying hands after hand hygiene?
Explanation
Using a paper towel for drying hands and turning off the faucet is an appropriate method to maintain hand hygiene after the handwashing process.
Incorrect choices:
b. Shaking hands vigorously can increase the risk of cross-contamination and should be avoided.
c. Wiping hands on a disposable gown or apron can lead to contamination of the gown and should not be done.
d. Using a shared hand towel with other healthcare providers can promote the spread of microorganisms and is not recommended.
Personal Protective Equipment (PPE)
Which of the following is an example of appropriate use of personal protective equipment (PPE)?
Explanation
Wearing a surgical mask in place of a respirator when caring for a patient with tuberculosis Explanation: When caring for a patient with tuberculosis, the appropriate use of PPE includes wearing a respirator to protect against airborne transmission of the infectious agent.
Incorrect choices:
a. Wearing gloves when handling non-infectious materials is unnecessary and does not align with appropriate PPE use.
b. Reusing a disposable gown after disinfection is not recommended as disposable gowns are meant for single-use to prevent cross-contamination.
d. Wearing goggles only when there is a risk of splashing does not provide adequate eye protection in all situations where eye exposure may occur.
Which of the following is true regarding the order of donning and removing PPE?
Explanation
The gown should be removed before the gloves. Explanation: When removing PPE, the gown should be removed before the gloves to prevent contamination of the hands during the process.
Incorrect choices: a. Gloves should be removed last after removing the gown to minimize the risk of contaminating the hands.
b. The mask should be donned before wearing gloves to ensure proper respiratory protection.
d. The mask should be removed after removing the goggles or face shield to maintain a barrier against respiratory droplets.
Which of the following is an example of appropriate glove use?
Explanation
Touching clean surfaces with gloved hands
Explanation: Gloves should not be considered a substitute for hand hygiene. Touching clean surfaces with gloved hands can contaminate those surfaces, and proper hand hygiene should be performed after glove removal.
Incorrect choices: a. Wearing the same pair of gloves for multiple patient care tasks increases the risk of cross-contamination and is not recommended.
c. Gloves should be removed after completing all necessary patient care tasks and hand hygiene should be performed immediately.
d. Gloves should be removed and hand hygiene performed before touching clean surfaces.
When should a healthcare provider wear a gown as part of their PPE?
Explanation
When providing oral care to an unconscious patient, a gown should be worn to protect against potential contact with bodily fluids or contaminants.
Incorrect choices:
a. Wearing a gown during routine hand hygiene is unnecessary and not recommended.
c. Wearing a gown while transporting a stable patient within the facility is unnecessary unless there is a risk of contact with potentially infectious materials.
d. Wearing a gown when administering oral medication to a non-isolated patient is not typically required unless there is a risk of splashing or exposure to bodily fluids.
Which of the following is true regarding the use of N95 respirators?
Explanation
N95 respirators should be fit-tested to ensure a proper seal and provide adequate respiratory protection.
Incorrect choices:
a. N95 respirators should only be used when there is a risk of airborne transmission, such as caring for patients with airborne infections.
b. N95 respirators are not designed for multiple reuse and should be disposed of properly after use to prevent contamination and maintain effectiveness.
Respiratory Hygiene/Cough Etiquette:
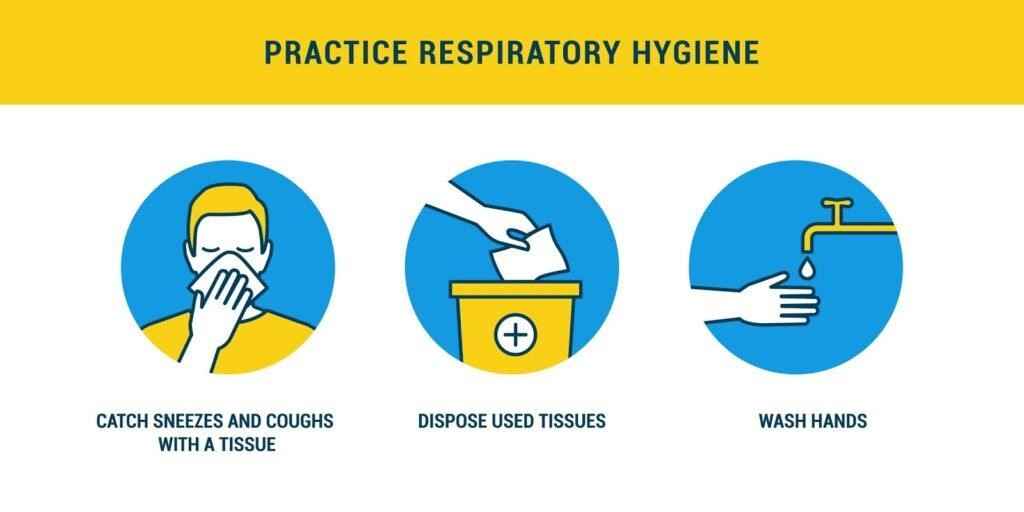
Which of the following actions is recommended as part of respiratory hygiene practices?
Explanation
Using a tissue to cover the mouth and nose when coughing or sneezing Explanation: Using a tissue to cover the mouth and nose when coughing or sneezing helps contain respiratory droplets and reduces the risk of spreading infectious respiratory illnesses.
Incorrect choices: a. Coughing or sneezing into hands can lead to the spread of germs through direct contact with surfaces or other individuals.
c. Blowing the nose without using a tissue can result in the release of respiratory droplets and should be avoided.
d. Discarding used tissues on the floor is unsanitary and can contribute to the transmission of infections.
How often should healthcare providers perform hand hygiene after assisting with respiratory procedures, such as suctioning or providing nebulizer treatments?
Explanation
Healthcare providers should perform hand hygiene before and after each patient contact, including after assisting with respiratory procedures. This helps prevent the spread of pathogens to other patients and healthcare personnel.
Incorrect choices:
a. Performing hand hygiene only if visible soiling is present is insufficient, as pathogens may be present even when hands appear clean.
b. Performing hand hygiene every hour may not be frequent enough to maintain proper infection prevention and control.
d. Performing hand hygiene only once at the end of the shift does not ensure continuous protection throughout patient care interactions.
Which of the following actions promotes respiratory hygiene in the healthcare setting?
Explanation
Providing masks to patients who are coughing or sneezing helps contain respiratory droplets and reduce the risk of spreading infections within the healthcare setting.
Incorrect choices: a. Encouraging visitors to wear masks only if they have symptoms does not account for asymptomatic individuals who may be carriers of respiratory infections.
c. Allowing healthcare personnel to cough or sneeze freely in patient care areas is unhygienic and can contribute to the spread of infections.
d. Reusing masks throughout the day to conserve supplies increases the risk of contamination and compromises respiratory hygiene practices.
What is the appropriate distance for maintaining respiratory etiquette when interacting with someone who is coughing or sneezing?
Explanation
Maintaining a distance of 6 feet (2 meters) from someone who is coughing or sneezing helps reduce the risk of inhaling respiratory droplets and potential pathogen transmission.
Incorrect choices:
a. 1 foot (30 centimeters) may not provide sufficient distance to minimize the risk of inhaling respiratory droplets.
b. 3 feet (1 meter) is closer than the recommended distance and may not effectively reduce exposure to respiratory droplets.
d. 10 feet (3 meters) is farther than necessary for routine respiratory etiquette and may not be practical in most healthcare settings.
What is the appropriate method for disposing of used masks or tissues contaminated with respiratory secretions?
Explanation
Used masks or tissues contaminated with respiratory secretions should be disposed of in a biohazard container to minimize the risk of exposure to infectious agents.
Incorrect choices: a. Placing them in a regular waste bin increases the risk of contamination and potential spread of infections.
b. Flushing them down the toilet can cause plumbing issues and is not an appropriate method of disposal.
d. Leaving them on a clean surface for someone else to handle is unhygienic and may lead to cross-contamination.
Safe Injection Practices
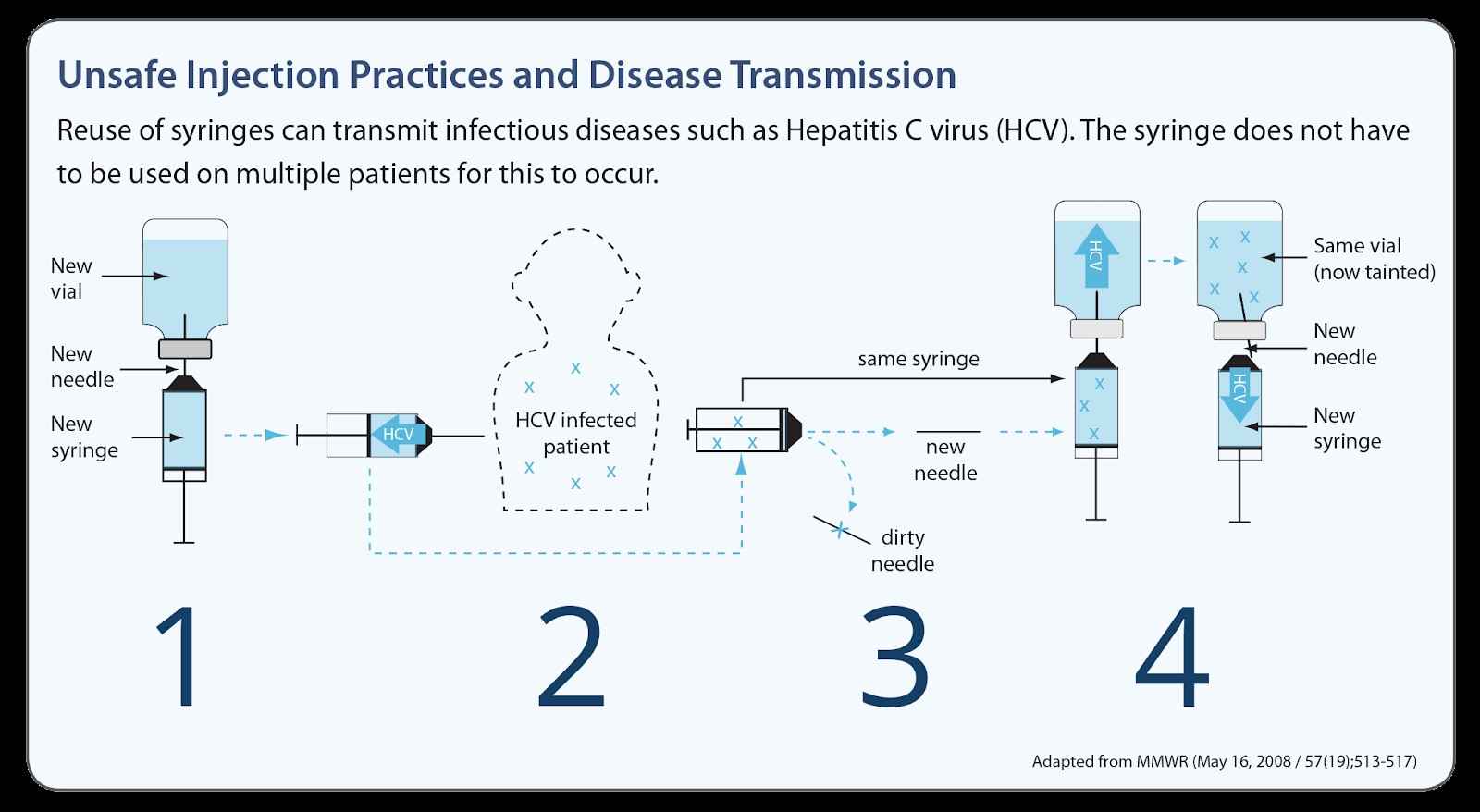
Which of the following actions is an essential component of safe injection practices?
Explanation
Using single-use syringes and needles for each injection is an essential component of safe injection practices. It helps prevent the transmission of infectious agents between patients.
Incorrect choices:
a. Reusing needles on the same patient is not a safe practice as it can lead to contamination and infection.
b. Recapitulating needles increases the risk of accidental needlestick injuries and should be avoided.
c. Administering medication from a multidose vial to multiple patients can introduce contamination and increase the risk of infection.
What is the recommended method for disposing of used needles and syringes after an injection?
Explanation
Disposing of used needles and syringes in a biohazard sharps container is the recommended method. It ensures safe containment and proper disposal of sharps to minimize the risk of needlestick injuries and transmission of infections.
Incorrect choices: a. Placing used needles and syringes in a regular trash bin is unsafe and can lead to accidental injuries for waste handlers.
b. Recapitulating needles is not recommended due to the increased risk of needlestick injuries.
d. Leaving used needles and syringes on the patient's bedside table is unsafe and can pose a risk to the patient and healthcare providers.
What should a healthcare provider do if a needlestick injury occurs during an injection?
Explanation
If a needlestick injury occurs during an injection, the healthcare provider should follow the facility's protocol for reporting the incident and receiving appropriate post-exposure prophylaxis (PEP) to minimize the risk of infection transmission.
Incorrect choices:
a. Continuing with the injection procedure without reporting the needlestick injury is unsafe and can lead to further complications.
b. Washing the affected area with soap and water is a general first aid measure, but it is not sufficient in the case of a needlestick injury.
c. Discarding the used needle in a regular trash bin is inappropriate as it does not ensure proper handling and disposal of the contaminated needle.
Which of the following statements is true regarding the preparation of medication for injection?
Explanation
It is unnecessary to clean the rubber stopper on a medication vial before withdrawing medication, as long as proper aseptic technique is used during the preparation process.
Incorrect choices:
a. Sharing medication vials among multiple patients, even with needle changes, can lead to contamination and should be avoided.
b. Drawing medication from a vial using the same syringe for multiple injections increases the risk of contamination and infection.
d. Ampules should be broken open using a sterile device or ampule breaker to ensure a clean break and prevent injuries.
What is the recommended duration for hand hygiene before and after administering injections?
Explanation
The recommended duration for hand hygiene before and after administering injections is typically 15 seconds. This allows sufficient time to effectively clean the hands and reduce the risk of infection transmission.
Incorrect choices:
a. 5 seconds may not be enough to adequately clean the hands and remove potential pathogens.
c. 30 seconds and d. 60 seconds are longer than necessary for routine hand hygiene before and after administering injections.
Environmental Control
What is the primary goal of environmental control in infection prevention?
Explanation
The primary goal of environmental control in infection prevention is to minimize the risk of infection transmission by implementing strategies to eliminate or reduce the presence of infectious agents in the healthcare environment.
Incorrect choices:
a. Enhancing the aesthetic appeal of the healthcare facility is not the primary goal of environmental control in infection prevention, although it may be considered as part of overall facility management.
b. While environmental control measures can help reduce healthcare costs indirectly by preventing healthcare-associated infections, cost reduction is not the primary goal.
d. Increasing patient satisfaction scores is important but not the primary goal of environmental control in infection prevention.
Which of the following is an example of a physical barrier used for environmental control in infection prevention?
Explanation
Isolation gowns are an example of a physical barrier used for environmental control in infection prevention. They create a barrier between healthcare workers and patients, preventing the transfer of microorganisms.
Incorrect choices:
a. Hand hygiene stations are not physical barriers but rather a measure to promote hand hygiene.
b. Antimicrobial cleaners are chemical agents used for cleaning and disinfection, not physical barriers.
d. Air filtration systems are designed to control airborne contaminants but do not act as physical barriers themselves.
Why is proper ventilation important for environmental control in infection prevention?
Explanation
Proper ventilation is important in environmental control to minimize the concentration of airborne pathogens and maintain air quality within healthcare facilities.
Incorrect choices:
a. Maintaining a pleasant odor is a secondary consideration compared to infection prevention.
b. While energy conservation is important, it is not the primary purpose of proper ventilation in infection prevention.
c. Controlling temperature and humidity levels contribute to comfort but are not directly related to infection prevention through ventilation.
Which of the following is an example of routine cleaning in environmental control?
Explanation
Disinfection of high-touch surfaces is an example of routine cleaning in environmental control. It involves regularly cleaning and disinfecting surfaces that are frequently touched by healthcare workers, patients, and visitors.
Incorrect choices:
a. Terminal disinfection after patient discharge is not considered routine cleaning but rather a more thorough cleaning process.
c. Sterilization of surgical instruments is a specialized process for eliminating all microorganisms, not routine cleaning.
d. Fumigation of patient rooms is a more extreme measure typically used for specific situations, such as outbreaks, and is not part of routine cleaning.
What is the purpose of implementing aseptic techniques in environmental control?
Explanation
Aseptic techniques are used in environmental control to prevent the spread of infections in sterile areas, such as operating rooms or invasive procedure areas.
Incorrect choices:
a. Reducing energy consumption is not the primary purpose of implementing aseptic techniques.
b. While patient comfort is important, it is not the primary goal of aseptic techniques.
d. Maintaining a pleasant scent is not the primary purpose of aseptic techniques but can be achieved through other means unrelated to infection prevention.
Staff Health and Immunizations
Which of the following is an important consideration for staff health and immunization?
Explanation
Regular hand hygiene practices are essential for staff health and infection prevention. It helps reduce the risk of transmitting pathogens and maintaining a safe working environment.
Incorrect choices:
a. Compliance with personal phone usage policies is unrelated to staff health and immunization.
b. Adequate supply of office stationery is important for daily operations but not directly related to staff health and immunization.
d. Attending team-building activities is beneficial for team dynamics but not directly related to staff health and immunization.
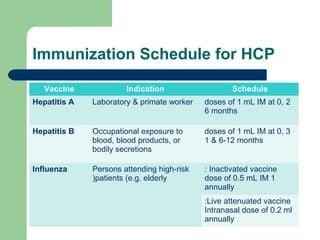
Why is it important for healthcare staff to receive immunizations?
Explanation
Healthcare staff receiving immunizations helps prevent the transmission of infectious diseases to vulnerable patients and also protects themselves from contracting vaccine-preventable infections.
Incorrect choices:
a. Reducing the cost of healthcare services is not the primary reason for healthcare staff to receive immunizations.
b. Enhancing physical fitness levels is unrelated to the purpose of immunizations for infection prevention.
c. Compliance with organizational dress code policies does not address the importance of immunizations.
What should be done if a healthcare staff member has a known contraindication to a specific vaccine?
Explanation
If a healthcare staff member has a known contraindication to a specific vaccine, it is important to refer them to occupational health services for further assessment and guidance regarding alternative options or accommodations.
Incorrect choices:
a. Ignoring the contraindication and administering the vaccine can jeopardize the staff member's health and well-being.
b. Consulting a coworker may not provide the appropriate expertise to address contraindications.
d. Delaying vaccination until the contraindication resolves may not be appropriate, as some contraindications may be permanent.
Which of the following is a common vaccine recommended for healthcare staff?
Explanation
The influenza vaccine is a common vaccine recommended for healthcare staff to protect themselves and prevent the spread of influenza to patients and coworkers.
Incorrect choices:
a. Meningococcal vaccine is typically recommended for individuals at high risk or traveling to certain areas but may not be a common recommendation for healthcare staff.
b. Varicella vaccine is typically recommended for individuals who are not immune to chickenpox but may not be a primary recommendation for healthcare staff.
c. Pneumococcal vaccine is typically recommended for individuals at high risk or older adults but may not be a primary recommendation for all healthcare staff.
What is the purpose of staff health programs in infection prevention and control?
Explanation
Staff health programs aim to promote and maintain the health and well-being of staff members, including measures such as immunizations, health screenings, and education on infection prevention and control.
Incorrect choices:
a. Providing extra breaks and time off is not the primary purpose of staff health programs.
b. Increasing the workload is counterproductive to promoting staff health and well-being.
d. Enforcing strict dress code policies is unrelated to the primary purpose of staff health programs.
Education and Training
What is the purpose of surveillance in infection prevention and control?
Explanation
Surveillance in infection prevention and control is performed to identify and control the spread of infections within healthcare settings.
Incorrect choices:
a. Tracking the movement of healthcare providers is not the primary purpose of surveillance.
b. Monitoring patient satisfaction is important but not the primary purpose of surveillance in infection prevention and control.
d. Ensuring compliance with documentation requirements is important but not the primary purpose of surveillance.
Which of the following is an example of a healthcare-associated infection (HAI) that should be reported?
Explanation
Healthcare-associated infections (HAIs) that occur within healthcare facilities, such as surgical site infections, should be reported for surveillance and appropriate management.
Incorrect choices:
a. Common colds acquired outside the healthcare facility are not considered HAIs and do not require reporting.
c. Self-limiting gastrointestinal infections are not typically considered HAIs and may not require reporting.
d. Mild respiratory infections in healthcare providers may not necessarily be considered HAIs and may not require reporting.
What is the purpose of reporting infections in healthcare facilities?
Explanation
Reporting infections in healthcare facilities allows for the monitoring of trends and patterns, which helps in the identification of potential outbreaks and implementation of appropriate preventive measures.
Incorrect choices:
a. Identifying the responsible healthcare provider is not the primary purpose of infection reporting.
b. Allocating additional funding for infection control may be a potential outcome of infection reporting but is not the primary purpose.
d. Assigning blame for the occurrence of infections is not the primary purpose of infection reporting.
Which of the following is an important component of effective infection surveillance?
Explanation
Effective infection surveillance requires the collection and analysis of accurate and timely data to identify trends, patterns, and potential areas for improvement.
Incorrect choices:
a. Conducting patient satisfaction surveys is important but is not directly related to infection surveillance.
b. Inspecting the physical environment is important for infection control but is not the primary component of infection surveillance.
c. Implementing staff disciplinary actions is not directly related to infection surveillance and may be more focused on individual incidents rather than overall surveillance.
Which of the following is an example of a healthcare-associated infection that should be reported to the appropriate regulatory agencies?
Explanation
Central line-associated bloodstream infections are considered serious healthcare-associated infections and should be reported to the appropriate regulatory agencies for surveillance and intervention.
Incorrect choices:
a. Minor skin abrasions are not typically considered reportable healthcare-associated infections.
b. Asymptomatic urinary tract infections in non-catheterized patients may not necessarily require reporting.
d. Self-limiting viral upper respiratory infections are not typically considered reportable healthcare-associated infections.
What is the purpose of analyzing infection surveillance data?
Explanation
Analyzing infection surveillance data allows for the identification of trends and patterns, which can help in the implementation of targeted interventions and preventive measures.
Incorrect choices:
a. Identifying the individual responsible for the infection is not the primary purpose of analyzing surveillance data.
b. Determining the cost of treating infections may be a potential outcome of data analysis but is not the primary purpose.
d. Assigning blame for the occurrence of infections is not the primary purpose of analyzing surveillance data.
Which of the following is a common method used for reporting infections in healthcare facilities?
Explanation
Submitting electronic reports to public health agencies is a common method used for reporting infections in healthcare facilities, ensuring appropriate surveillance and monitoring.
Incorrect choices:
a. Posting infection-related data on social media platforms is not a recommended method for reporting infections in healthcare facilities.
b. Sending individual emails may not be practical for reporting infections on a larger scale.
d. Publishing infection reports in local newspapers is not a standard method for reporting infections in healthcare facilities.
More Questions
Which of the following is an example of a healthcare-associated infection (HAI)?
Explanation
Healthcare-associated infections are infections that occur as a result of receiving healthcare, such as in hospitals or other healthcare settings.
Incorrect choices:
a. A cold contracted from a family member is not an example of a healthcare-associated infection.
c. Food poisoning from contaminated food is not an example of a healthcare-associated infection.
d. Athlete's foot from a public swimming pool is not an example of a healthcare-associated infection.
What is the most effective way to prevent the transmission of healthcare-associated infections?
Explanation
Hand hygiene is considered the most effective way to prevent the transmission of healthcare-associated infections. It includes washing hands with soap and water or using alcohol-based hand sanitizers.
Incorrect choices:
a. Wearing gloves during patient care is important but not as effective as hand hygiene in preventing infection transmission.
c. Disinfecting surfaces regularly is important for infection control, but hand hygiene is the most effective measure.
d. Administering prophylactic antibiotics is not a preventive measure for healthcare-associated infections but rather a treatment option in certain cases.
Which of the following is an example of a standard precaution for infection control?
Explanation
Respiratory hygiene/cough etiquette is a standard precaution that involves covering the mouth and nose when coughing or sneezing and using tissues or elbow to prevent the spread of respiratory droplets.
Incorrect choices:
a. Wearing a gown and gloves during a sterile procedure is an example of contact precautions, not standard precautions.
c. Placing a patient in airborne isolation is an example of airborne precautions, not standard precautions.
d. Using dedicated equipment for each patient is an example of transmission-based precautions, not standard precautions.
What is the recommended duration for performing hand hygiene with alcohol-based hand sanitizers?
Explanation
The recommended duration for performing hand hygiene with alcohol-based hand sanitizers is approximately 15 seconds, ensuring all surfaces of the hands are covered and allowed to dry.
Incorrect choices:
a. 5 seconds is not a sufficient duration for effective hand hygiene with alcohol-based hand sanitizers.
c. 30 seconds and d. 60 seconds are longer durations than necessary for alcohol-based hand sanitizers.
Which personal protective equipment (PPE) should be worn when entering the room of a patient with tuberculosis?
Explanation
When entering the room of a patient with tuberculosis, healthcare workers should wear a fitted N95 respirator mask to protect against airborne transmission.
Incorrect choices:
a. Gloves and gown are necessary for contact precautions, but the primary concern with tuberculosis is airborne transmission.
b. Mask and goggles are not sufficient for protecting against airborne transmission of tuberculosis.
d. Face shield and gloves are not the recommended combination of PPE for tuberculosis precautions.
What is the appropriate technique for removing personal protective equipment (PPE) after caring for a patient with a highly contagious infection?
Explanation
he appropriate technique for removing PPE after caring for a patient with a highly contagious infection is to remove the gown first, followed by the gloves, mask, and goggles, in order to minimize the risk of self-contamination.
Incorrect choices:
a. Removing gloves first can lead to contamination of the hands when removing the gown. The correct order is to remove the gown first.
c. Removing the goggles first can potentially expose the eyes to contamination. The correct order is to remove the gown first.
d. Removing the mask first can potentially e
When should sterile gloves be worn?
Explanation
Sterile gloves should be worn when performing invasive procedures, such as administering intravenous medication, to maintain a sterile field and prevent infection.
Incorrect choices: a. Oral hygiene does not require sterile gloves. Non-sterile gloves should be used.
b. Emptying a urinary drainage bag does not require sterile gloves. Non-sterile gloves should be used.
d. Assisting a patient with ambulation does not require sterile gloves. Non-sterile gloves should be used.
What is the appropriate technique for cleaning a contaminated surface?
Explanation
The appropriate technique for cleaning a contaminated surface is to use a detergent or disinfectant to effectively remove or kill microorganisms present on the surface.
Incorrect choices: a. Wiping the surface with a dry cloth does not effectively remove microorganisms. Cleaning agents should be used.
b. Spraying the surface with water alone does not effectively kill microorganisms. Detergent or disinfectant is required.
d. Blowing air over the surface does not effectively clean or disinfect it. Cleaning agents should be used.
Which of the following is an example of a healthcare-associated infection prevention measure?
Explanation
Practicing proper hand hygiene is an important infection prevention measure in healthcare settings and can help reduce the risk of healthcare-associated infections.
Incorrect choices:
a. Using sterile technique during surgical procedures is a specific practice for maintaining a sterile field but does not address overall infection prevention.
c. Administering prophylactic antibiotics before surgery is a strategy to prevent surgical site infections but does not encompass all healthcare-associated infections.
What is the primary purpose of using isolation precautions in healthcare settings?
Explanation
The primary purpose of using isolation precautions is to protect patients from getting infections and to prevent the spread of infectious agents within healthcare settings.
Incorrect choices:
a. Protecting healthcare providers from getting infections is important but not the primary purpose of isolation precautions.
c. Restricting visitors' access to healthcare facilities may be a component of infection control but is not the primary purpose of isolation precautions.
d. Reducing healthcare costs associated with infections is a potential benefit of effective infection prevention and control, but it is not the primary purpose of isolation precautions.
Exams on Infection Prevention and Control
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Nursingprepexams
Just Now
Nursingprepexams
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Demonstrate proper hand hygiene techniques and explain the rationale for its importance in preventing the transmission of infections.
- Identify and apply appropriate personal protective equipment (PPE) based on the type of anticipated exposure or isolation precautions.
- Describe the principles and techniques of safe injection practices to minimize the risk of infection transmission.
- Explain the importance of environmental control measures, such as maintaining cleanliness and implementing proper disinfection protocols, in preventing the spread of infections.
- Differentiate between standard precautions and transmission-based precautions, and apply the appropriate precautions based on the specific infectious agent or mode of transmission.
Introduction
Infection prevention and control play a crucial role in healthcare settings to minimize the transmission of infectious diseases and ensure the safety of patients, healthcare professionals, and visitors. The ATI/HESI curriculum emphasizes the importance of infection control practices, which are based on evidence-based guidelines and regulations established by healthcare organizations such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
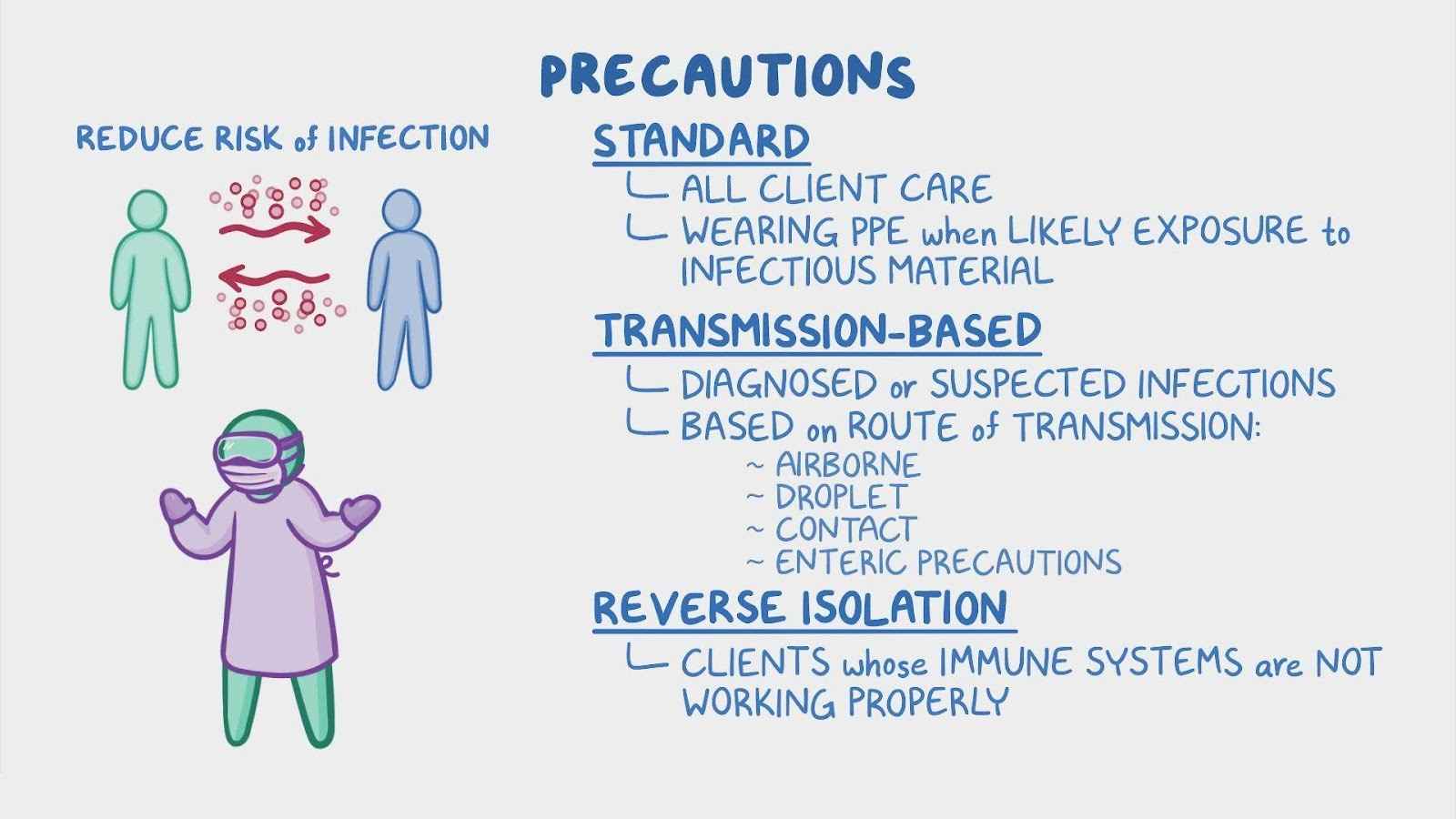
Standard Precautions:
Standard precautions are the foundation of infection prevention and control and should be applied to all patients regardless of their diagnosis or infection status.
They include hand hygiene, use of personal protective equipment (PPE), respiratory hygiene/cough etiquette, safe injection practices, safe handling of potentially contaminated equipment or surfaces, and safe handling of linen.
Hand hygiene is the single most important measure for preventing the transmission of healthcare-associated infections. It can be performed using soap and water or an alcohol-based hand sanitizer.
PPE includes gloves, gowns, masks, and eye protection, and should be worn when there is a risk of exposure to blood, bodily fluids, secretions, or excretions.
Transmission-Based Precautions:
Transmission-based precautions are used in addition to standard precautions for patients with known or suspected infections that are spread through specific routes, including contact, droplet, or airborne transmission.
Contact precautions: Used for infections spread through direct or indirect contact with the patient or their environment. Examples include methicillin-resistant Staphylococcus aureus (MRSA), Clostridium difficile (C. diff), and vancomycin-resistant enterococci (VRE).
Droplet precautions: Used for infections spread through respiratory droplets generated by coughing, sneezing, or talking. Examples include influenza, pertussis, and meningococcal meningitis.
Airborne precautions: Used for infections spread through small droplet nuclei that remain suspended in the air for long periods. Examples include tuberculosis (TB), measles, and varicella (chickenpox).
Hand Hygiene
Hand hygiene is a critical component of infection prevention and control.
Hands should be washed with soap and water for at least 20 seconds when they are visibly soiled or contaminated with blood or body fluids.
Alcohol-based hand sanitizers containing at least 60% alcohol can be used when hands are not visibly soiled.

Personal Protective Equipment (PPE)
PPE should be used based on the anticipated exposure to blood, bodily fluids, secretions, or excretions.
Gloves should be worn when touching blood, body fluids, or contaminated surfaces, and they should be changed between patient contacts.
Gowns should be worn during procedures and patient care activities that may generate splashes or sprays of blood, body fluids, secretions, or excretions.
Masks and eye protection should be used when there is a risk of droplet or airborne transmission.

Respiratory Hygiene/Cough Etiquette:
Respiratory hygiene and cough etiquette aim to prevent the transmission of respiratory infections.
Patients and visitors with respiratory symptoms should be provided with tissues and instructed to cover their mouth and nose when coughing or sneezing.
They should be encouraged to perform hand hygiene after coughing, sneezing, or using tissues.
Safe Injection Practices
Safe injection practices are essential to prevent the transmission of bloodborne infections.
Needles, syringes, and other injection equipment should be used for a single patient and should not be reused.
Multi-dose vials should be dedicated to a single patient whenever possible, and if used for multiple patients, they should be accessed with a new needle and new syringe.
Environmental Control
Proper cleaning and disinfection of patient care equipment and the healthcare environment are crucial to prevent healthcare-associated infections.
Surfaces should be cleaned regularly with appropriate disinfectants, paying particular attention to high-touch surfaces.
Single-use items should be properly disposed of, and reusable items should be appropriately cleaned and sterilized or high-level disinfected.
Staff Health and Immunizations
Healthcare professionals should comply with immunization requirements to prevent the transmission of vaccine-preventable diseases.
Routine immunizations recommended for healthcare professionals include influenza, hepatitis B, and measles, mumps, and rubella (MMR).
Healthcare professionals should monitor their health and report any signs or symptoms of infectious diseases. They should not work when they are ill and potentially infectious.
Education and Training
Ongoing education and training programs should be implemented to ensure that healthcare professionals are knowledgeable about infection prevention and control practices.
Training should cover topics such as hand hygiene, proper use of PPE, respiratory hygiene/cough etiquette, safe injection practices, and environmental control measures.
Healthcare professionals should stay updated with the latest evidence-based guidelines and recommendations related to infection prevention and control.
Surveillance and Reporting:
Surveillance systems should be in place to monitor healthcare-associated infections and identify trends or outbreaks.
Infections should be reported to the appropriate authorities and infection prevention and control committee or department.
Timely reporting of infections allows for prompt investigation, implementation of control measures, and prevention of further transmission.
Nursingprepexams
Videos
Login to View Video
Click here to loginTake Notes on Infection Prevention and Control
This filled cannot be empty

