ATI Custom maternity exam #2 2024
Total Questions : 57
Showing 25 questions, Sign in for more
A nurse is collecting data from a postpartum client.
Which of the following findings should alert the nurse to the possibility of a postpartum complication?
Explanation
Choice A rationale:
The fundus at the umbilicus level is a normal finding in the immediate postpartum period. After delivery, the top of the uterus
(known as the fundus) is typically at the level of the umbilicus. In the days following delivery, the uterus begins to shrink and
descend into the pelvic cavity, guided by the process known as involution.
Choice B rationale:
A urinary output of 3,000 mL is unusually high and could indicate a postpartum complication. Postpartum diuresis is common
as the body eliminates excess fluid accumulated during pregnancy. However, excessive urinary output could be a sign of
postpartum complications such as postpartum preeclampsia, which can occur after the birth of the baby and is characterized
by high blood pressure and signs of damage to another organ system, often the kidneys.
Choice C rationale:
A temperature of 100.4 F for two days postpartum can be a normal finding. It’s not uncommon for women to experience a
slight elevation in temperature in the first 24 hours after delivery due to the exertion of labor. However, a temperature above100.4 F beyond the first 24 hours could indicate an infection and should be evaluated.
Choice D rationale:
A cesarean section shortly following delivery is not typically a sign of a postpartum complication. It’s a surgical procedure used to deliver the baby and can be planned or unplanned due to various reasons such as the baby’s position, multiple pregnancies, or complications during labor. However, like any surgery, a cesarean section does carry risks and can increase the likelihood of certain postpartum complications such as infection or blood clots.
A nurse is assisting with the care of a client who is in labor and has the urge to push.
Which of the following instructions should the nurse give the client?
Explanation
Choice A rationale:
Pushing continuously throughout the entire contraction can lead to maternal exhaustion and may not be the most effective way to progress labor. It’s important for the mother to conserve her energy and work with her body’s natural rhythms.
Choice B rationale:
Taking a deep, cleansing breath before and after each contraction can help the mother manage pain and keep her energy up.
This technique is often recommended because it allows the mother to rest briefly and gather strength for the next contraction.

Choice C rationale:
While it’s important for the nurse to monitor contractions and provide guidance, the urge to push is a natural response that
can vary among individuals. Telling the mother when to push according to contractions may not align with her body’s natural
instincts.
Choice D rationale:
Holding one’s breath and pushing while someone counts to ten is an outdated practice. This method can cause unnecessary
strain and doesn’t take into account the individual rhythms and responses of the mother’s body.
Which of the following findings should the nurse monitor to evaluate the effectiveness of this medication?
Explanation
Choice A rationale:
Oxytocin is a hormone that causes the uterus to contract. It is often given to women after childbirth to help the uterus return
to its normal size and to prevent heavy bleeding. Therefore, monitoring the consistency of the fundus (the upper part of the
uterus) is an effective way to evaluate the effectiveness of this medication.
Choice B rationale:
While urinary output is an important vital sign to monitor in all patients, it is not directly related to the effectiveness of
Oxytocin. Oxytocin does not have a significant effect on urinary output.
Choice C rationale:
Blood pressure is another vital sign that should be monitored in all patients. However, it is not the primary indicator of
Oxytocin’s effectiveness. While Oxytocin can cause blood pressure changes, these are usually transient and not the primary
intended effect of the medication.
Choice D rationale:
Heart rate, like blood pressure and urinary output, is an important vital sign to monitor in all patients. However, it is not the
primary indicator of Oxytocin’s effectiveness. Oxytocin does not have a significant direct effect on heart rate.
A nurse is assisting with the care of a client who is in labor.
The client's labor is difficult and prolonged and she reports a severe backache.
Which of the following factors is a contributing cause of difficult, prolonged labor?
Explanation
Choice A rationale:
Fetal attitude in general flexion is not a contributing factor to difficult, prolonged labor. In fact, it is the normal fetal attitude
during labor. The fetus is typically in a position of general flexion, where the head is flexed forward, chin to chest, and the arms
and legs are flexed, with the arms crossed over the chest and the legs bent at the knees.
Choice B rationale:
Fetal lie being longitudinal is the normal and most common fetal lie during labor. In a longitudinal lie, the long axis of the fetus
is parallel with the long axis of the mother. This is the ideal and most common position for labor and delivery.
Choice C rationale:
A gynecoid pelvis is the most common type of female pelvis and is the most favorable for childbirth. It has a round shape with
a wide pubic arch, which allows for easier passage of the baby during delivery.
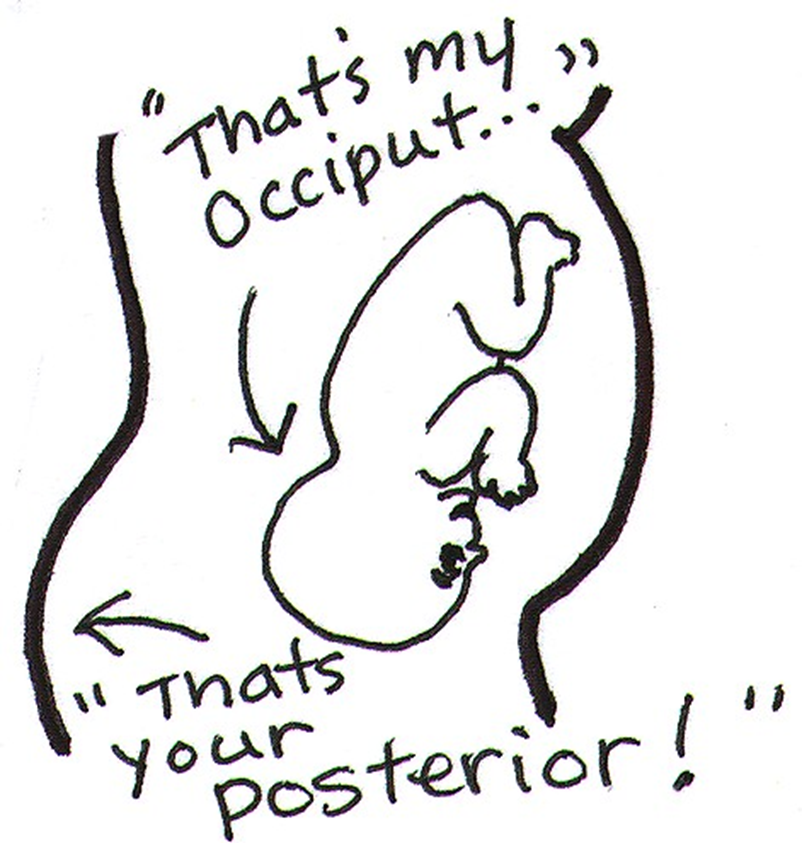
Choice D rationale:
A persistent occiput posterior (OP) position can indeed contribute to difficult, prolonged labor. In an OP position, the baby’s
occipital bone is towards the mother’s posterior side. This position can cause labor to be more painful and last longer because the baby’s head diameter that presents to the birth canal is larger. It can also cause back pain during labor, often referred to as "back labor"1.
Which of the following actions should the nurse take first?
Explanation
Choice A rationale:
Checking the client’s blood pressure is important, but it is not the first action the nurse should take. Hypotension could
indicate hemorrhage, but the nurse needs to address the immediate risk of excessive bleeding.
Choice B rationale:
The nurse should first massage the client’s fundus. A saturated perineal pad could indicate a postpartum hemorrhage.
Massaging the fundus helps the uterus contract and may stop the bleeding.
Choice C rationale:
Observing for pooling of blood under the buttocks is a way to assess for bleeding. However, this is not the first action because
it does not address the cause of the bleeding.
Choice D rationale:
Administering oxytocin can help the uterus contract and reduce bleeding. However, this is not the first action because it
requires a physician’s order.
breastfeeding her newborn.
Which of the following client statements indicates an understanding of the teaching?
Explanation
Choice A rationale:
Stopping breastfeeding until the antibiotics are done is not a recommended practice. Most antibiotics are safe to use while
breastfeeding. Moreover, stopping breastfeeding can lead to engorgement.
Choice B rationale:
Applying cold compresses 20 minutes before each feeding is not a recommended practice. Cold compresses are usually
recommended after breastfeeding to help reduce swelling. Warm compresses or taking a warm shower before breastfeeding
can help increase milk flow and promote the letdown reflex.
Choice C rationale:
Feeding the baby every 2 hours is a good practice to prevent breast engorgement. Frequent feeding helps to empty the breasts,
which can prevent them from becoming overly full and engorged.
Choice D rationale:
Not wearing a bra during the daytime is not a recommended practice. Wearing a well-fitted bra can provide support and help
reduce discomfort associated with breast engorgement.
The nurse observes the umbilical cord protruding from the vagina.
Which of the following actions should the nurse take first?
Explanation
Choice A rationale:
Preparing the client for an emergency cesarean birth is an important step, but it is not the first action the nurse should take.
The immediate priority is to relieve pressure on the cord to prevent or alleviate cord compression.
Choice B rationale:
Covering the cord with a sterile, moist saline dressing is done to prevent drying of the cord and to maintain blood flow.
However, this is not the first action to take. The priority is to relieve cord compression by changing the client’s position.
Choice C rationale:
While it is important to explain to the client what is happening, this should not be the first action. The nurse’s priority is to
ensure the safety of the mother and baby, which involves immediate interventions to relieve cord compression.
Choice D rationale:
Placing the client in a knee-chest or Trendelenburg position is the first action the nurse should take. This position helps to
reduce pressure on the cord, which can improve blood flow to the fetus. It is a critical intervention that can prevent serious
complications such as fetal hypoxia.
The nurse finds a small amount of lochia rubra on the client's perineal pad, and the fundus is midline and firm at the
umbilicus.
Which of the following actions should the nurse take?
Explanation
Choice A rationale:
Assisting the client to ambulate is not the immediate action required in this scenario. The nurse has found a small amount of
lochia rubra on the client’s perineal pad, and the fundus is midline and firm at the umbilicus. These are normal findings for a
client who is 4 hours postpartum. However, the nurse should ensure that there is no excessive bleeding, which could be a sign
of postpartum hemorrhage.
Choice B rationale:
Performing a fundal massage is not necessary in this case. Fundal massage is usually performed when the uterus is boggy or
soft, which could indicate uterine atony, a leading cause of postpartum hemorrhage. In this scenario, the fundus is firm and at
the level of the umbilicus, which is a normal finding 4 hours postpartum.
Choice C rationale:
Increasing the rate of IV fluids is not the immediate action required in this scenario. IV fluids are usually increased to expand
intravascular volume in cases of postpartum hemorrhage. In this case, the nurse has found a small amount of lochia rubra on
the client’s perineal pad, which is a normal finding 4 hours postpartum.
Choice D rationale:
Checking for blood under the client’s buttocks is the correct action for the nurse to take in this scenario. This is to ensure that
there is no excessive bleeding, which could be hidden under the client’s buttocks. Excessive bleeding could be a sign of
postpartum hemorrhage, a potentially life-threatening complication.
A nurse is assisting in the care of a client who is in the second stage of labor.
Which of the following findings should the nurse report to the provider?
Explanation
Choice A rationale:
The presence of a “bloody show” from the vagina is a normal part of labor. It’s caused by the expulsion of the mucus plug that
has sealed the cervix during pregnancy. This is a common occurrence and does not need to be reported to the provider.
Choice B rationale:
Early decelerations in the Fetal Heart Rate (FHR) are usually not a cause for concern. They are often a sign of head
compression, which is a normal occurrence during labor. Therefore, this finding does not need to be reported to the provider.
Choice C rationale:
Uterine contractions lasting 2 minutes could be a sign of a complication known as “uterine tachysystole” or “hyperstimulation”. This condition can reduce oxygen supply to the baby and may require medical intervention. Therefore, this finding should be reported to the provider.
Choice D rationale:
Feeling pelvic pressure with contractions is a normal part of the second stage of labor. This pressure is due to the baby moving
down into the birth canal. Therefore, this finding does not need to be reported to the provider.
A nurse is assisting a client who is postpartum with her first breastfeeding experience.
When the client asks how much of the nipple she should put into the baby's mouth, which of the following responses
by the nurse is appropriate?
Explanation
Choice A rationale:
When breastfeeding, it’s important for the baby to latch onto not just the nipple, but also some of the areola, which is the
darker circle of skin around the nipple. This allows the baby to get a deep latch, which is necessary for effective breastfeeding.
The baby’s chin should be firmly touching the breast, and their mouth should be wide open. When they attach, you should see
much more of the darker nipple skin above the baby’s top lip than below their bottom lip.
Choice B rationale:
While it’s true that babies have certain instincts when it comes to breastfeeding, they still need guidance and proper
positioning to latch correctly. Simply relying on the baby’s instincts may not ensure a proper latch, which could lead to
ineffective breastfeeding and potential discomfort for the mother.
Choice C rationale:
The size of the baby’s mouth does not determine how much of the nipple they should take in. Regardless of the size of the
baby’s mouth, they should still latch onto the nipple and some of the areola for effective breastfeeding. Taking only part of the
nipple could lead to a shallow latch, which can cause nipple pain and may not allow the baby to get enough milk.
Choice D rationale:
While it’s important for the baby to take in a good amount of the breast tissue, including the nipple and areola, during
breastfeeding, suggesting to include some breast tissue beyond the areola might be excessive. The key is to ensure a deep
latch, which typically involves the nipple and some of the areola, rather than the entire areola and additional breast tissue.
A nurse is reinforcing teaching about reducing the risk of perineal infection with a client who had a vaginal birth.
Which of the following information should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A rationale:
Performing hand hygiene before and after voiding is crucial in preventing perineal infection. Hand hygiene is the most
effective way to prevent the spread of infections, including those that can infect the perineum.
Choice B rationale:
Cleaning the perineal area from front to back is a standard recommendation to prevent infection. This method ensures that
bacteria from the anal area are not spread to the vagina and urethra, which can cause urinary tract infections.
Choice C rationale:
Sitting on an inflatable donut is not typically recommended for the prevention of perineal infection. While it can provide
comfort for those with perineal pain, especially after childbirth, it does not directly contribute to the prevention of infection.
Choice D rationale:
Applying ice packs to the perineal area several times daily can help reduce swelling and provide pain relief, especially after a
vaginal birth. While it does not directly prevent infection, it can promote healing and comfort, which can indirectly help
prevent infection.
Choice E rationale:
Blotting the perineal area dry after voiding is another important step in preventing perineal infection. Keeping the area dry
prevents the growth of bacteria and other microbes that thrive in moist environments.
The client's blood pressure is 80/40 mm Hg and the fetal heart recording is 140/min.
Which of the following actions should the nurse take first?
Explanation
Rationale for Choice A: Increase IV fluid rate
While hypotension is a potential complication of epidural anesthesia, increasing the IV fluid rate is not the first-line
intervention in this scenario. While fluid resuscitation may be necessary in some cases, it has the potential to further decrease
the client's blood pressure and exacerbate the situation. Additionally, the cause of the hypotension is not yet fully determined,
and increasing fluids without addressing the underlying cause could mask or worsen the problem.
Rationale for Choice B: Place the client in a lateral position
Supine hypotension, a sudden drop in blood pressure upon assuming a supine position, is a common complication of epidural
anesthesia. This occurs due to aortocaval compression, where the enlarged uterus compresses the major blood vessels
supplying the lower body and returning blood to the heart. Placing the client in a lateral position, preferably tilted slightly to
the left, alleviates this compression, allowing blood to flow more freely and improving blood pressure. This intervention is
simple, non-invasive, and has the potential to quickly resolve the hypotension without further interventions.
Rationale for Choice C: Notify the provider
While notifying the provider is certainly warranted in this situation, it should not be the first action taken. The client's vital
signs indicate a potentially serious situation requiring immediate intervention. Delaying action while waiting for the provider
could have negative consequences for both the client and the fetus. Therefore, placing the client in a lateral position should be
the immediate priority followed by notifying the provider to discuss further management.
Rationale for Choice D: Elevate the legs
Elevating the legs is a standard intervention for managing orthostatic hypotension, which is characterized by dizziness or
lightheadedness upon standing. However, in this case, the client is already supine and experiencing supine hypotension, not
orthostatic hypotension. Elevating the legs would not address the aortocaval compression and may even worsen the venous
return, further decreasing blood pressure.
Additional Notes:
Other interventions that may be considered depending on the client's response and provider's assessment include
administering vasopressors to increase blood pressure and administering oxygen to improve fetal oxygenation.
Continuous monitoring of the client's vital signs and fetal heart rate is crucial to assess the effectiveness of interventions and
identify any further deterioration.
Prompt communication with the provider is essential to ensure timely and appropriate management of the situation.
Her lochia rubra is moderate, and her breasts feel hard and warm.
Which of the following recommendations should the nurse give the client?
Explanation
Rationale for Choice A:
Nipple shields are typically recommended for breastfeeding mothers experiencing nipple pain or thrush. While the client may
be experiencing some breast engorgement due to the hard and warm feeling, there is no indication of nipple pain or thrush.
Therefore, using a nipple shield is not the most appropriate recommendation in this case.
Rationale for Choice B:
Obtaining a prescription for an antibiotic is not warranted at this time. While mastitis, a breast infection, can occur
postpartum, the client's symptoms of moderate lochia rubra and firm, warm breasts are not specific enough to indicate
mastitis. Additionally, unnecessary antibiotic use should be avoided as it can contribute to antibiotic resistance.
Rationale for Choice C:
Applying a heating pad to the breasts may initially provide some comfort, but it can worsen engorgement and inflammation.
Heat stimulates milk production, which can further contribute to the client's discomfort. Applying cold compresses or ice
packs would be a more appropriate intervention for reducing inflammation and breast engorgement.
Rationale for Choice D:
Expressing milk from both breasts is the most appropriate recommendation for the client experiencing breast engorgement.
Regular milk removal helps to reduce milk build-up, alleviate engorgement, and decrease the risk of mastitis. The nurse can
teach the client proper handwashing techniques and breast massage strategies to facilitate effective milk expression.
Additionally, the nurse can encourage the client to breastfeed frequently, as this is the most efficient way to remove milk and
prevent engorgement.
Additional Notes:
The client's postpartum day (3 days) is a significant factor in considering the cause of her symptoms. Breast engorgement is
common during the first few days postpartum as milk production becomes established.
The nurse should assess the client's breastfeeding technique and ensure proper latching to prevent nipple trauma and
encourage effective milk removal.
Monitoring the client's temperature and other vital signs is crucial for identifying potential signs of infection, such as mastitis.
Providing the client with supportive measures such as comfortable bras and pain relief medications can also contribute to her
comfort and well-being.
By addressing the underlying cause of breast engorgement (milk build-up) through milk expression, the nurse can effectively
manage the client's symptoms and prevent potential complications like mastitis.
The client becomes frightened when she passes a large amount of lochia.
Which of the following responses should the nurse make?
Explanation
Choice A rationale:
Lochia pooling: When a woman lies in bed, gravity causes lochia to pool in the vagina. This can result in a larger amount of
lochia being expelled when she stands up or moves around.
Reassurance: Explaining this physiological process to the client can help to reassure her that the sudden increase in lochia is
normal and not a cause for alarm.
Validation: The nurse should validate the client's feelings of concern, as it is understandable for a new mother to be anxious
about any changes in her body after childbirth.
Education: The nurse should also provide education about lochia, including its typical characteristics, duration, and expected
changes. This can help the client to anticipate and understand her postpartum experience.
Choice B rationale:
Retained placenta: While retained fragments of the placenta can cause increased lochia, this is not the most common
this possibility, especially before further assessment.
Assessment and intervention: If there is a concern for retained placenta, the nurse would conduct a thorough assessment,
including fundal height, uterine tone, and lochia characteristics. Further interventions, such as ultrasound or manual
exploration of the uterus, may be necessary.
Choice C rationale:
Urinary tract infections (UTIs): UTIs can sometimes cause an increase in lochia, but they are not typically associated with a
sudden, large gush of lochia upon standing. Other symptoms of a UTI, such as burning with urination, urgency, or frequency,
would likely be present as well.
Assessment and intervention: If a UTI is suspected, the nurse would assess for urinary symptoms and collect a urine sample
for analysis. Antibiotic treatment would be initiated if a UTI is confirmed.
Choice D rationale:
Lochia progression: The amount of lochia generally decreases over time during the postpartum period. It is heaviest in the first
few days after delivery and gradually tapers off over the course of several weeks.
Inconsistency with presentation: While this statement is true, it does not directly address the client's concern about a sudden
labor pattern has been established.
Which of the following explanations should the nurse include?
Explanation
Choice A rationale:
There is no evidence to suggest that epidural anesthesia delays the rupture of fetal membranes. The timing of rupture of fetal
membranes is influenced by various factors, including the strength of uterine contractions, the position of the baby, and the
elasticity of the amniotic sac. Epidural anesthesia does not directly affect these factors.
Choice B rationale:
Epidural anesthesia can prolong labor by interfering with the natural process of labor. It can weaken uterine contractions,
slow down cervical dilation, and potentially lead to a prolonged second stage of labor. This is because the anesthesia blocks the
nerve signals that control the muscles of the uterus. When these signals are blocked, the contractions may become less
frequent and less intense. This can delay the progress of labor and increase the risk of interventions such as forceps delivery
or cesarean section.
Choice C rationale:
While epidural anesthesia can have some effects on the baby, it is not a primary cause of fetal depression. Fetal depression is
typically caused by other factors, such as decreased oxygen supply to the baby, maternal infection, or placental problems.
Epidural anesthesia can sometimes lead to a temporary decrease in the baby's heart rate, but this is usually well-managed by
the healthcare team and does not typically lead to significant fetal depression.
Choice D rationale:
Epidural anesthesia does not typically cause maternal hypertension. In fact, it can sometimes have the opposite effect and
cause a slight decrease in blood pressure. This is because the anesthesia can relax the blood vessels, which can lead to a drop
in blood pressure. However, this is usually not a significant concern and is easily managed by the healthcare team.
The nurse should identify that which of the following findings places the client at risk for a postpartum hemorrhage?
Explanation
Choice A rationale:
Gestational hypertension is a condition characterized by elevated blood pressure during pregnancy. While it can increase the
risk of certain complications, it is not directly associated with an increased risk of postpartum hemorrhage. This is because
gestational hypertension primarily affects the vascular system, not the uterine muscle function, which is responsible for
controlling postpartum bleeding.
Choice B rationale:
A small for gestational age newborn (SGA) is a baby who is smaller than expected for their gestational age. While SGA can be
associated with some pregnancy complications, it is not a direct risk factor for postpartum hemorrhage. The size of the baby
does not have a significant impact on the ability of the uterus to contract and prevent excessive bleeding after delivery.
Choice C rationale:
Precipitous birth is defined as a labor that progresses very rapidly, with delivery occurring within three hours or less of the
onset of regular contractions. This rapid progression of labor can lead to postpartum hemorrhage for several reasons:
Uterine atony: The uterus may not have enough time to contract effectively after a rapid delivery, leading to increased
bleeding.
Lacerations and trauma: The rapid passage of the baby through the birth canal can increase the risk of tearing of the cervix,
vagina, or perineum, which can contribute to blood loss.
Retained placenta: The placenta may not separate from the uterine wall as easily after a precipitous birth, increasing the risk
of hemorrhage.
Choice D rationale:
A two-vessel umbilical cord is a variation in which the umbilical cord contains only two blood vessels (one vein and one
artery) instead of the usual three (one vein and two arteries). While this can be associated with certain fetal anomalies, it is not
a direct risk factor for postpartum hemorrhage. The number of blood vessels in the umbilical cord does not significantly
impact the ability of the uterus to contract and prevent bleeding after delivery.
Which of the following actions should the nurse take?
Explanation
Choice A rationale:
Evaluating the side effects of analgesia is not the priority action in this situation. While it's important to assess for potential
side effects, the client's immediate need to use the bathroom takes precedence.
Analgesia might contribute to urinary retention in some cases, but it's not the most likely reason for the client's request.
Promptly addressing the client's need to void helps prevent bladder distention, discomfort, and potential urinary tract
infections.
Choice B rationale:
Using a wheelchair is not necessary in most cases after a vaginal birth.
Early ambulation is generally encouraged to promote circulation, prevent blood clots, and aid in recovery.
Requiring a wheelchair could delay the client's ability to void and might make her feel less independent.
Choice C rationale:
Advising the client to remain in bed is not recommended practice after a vaginal birth.
Prolonged bed rest can increase the risk of complications, such as blood clots, muscle weakness, and delayed bowel function.
Early ambulation, as tolerated, is crucial for promoting physical recovery and preventing postpartum complications.
Which of the following statements should the nurse include?
Explanation
Choice A rationale:
Urinary retention is not a common sign of impending labor. In fact, it's more likely to occur in the early stages of pregnancy
due to hormonal changes and the pressure of the growing uterus on the bladder. As labor approaches, the baby's head often
descends into the pelvis, which can relieve some of the pressure on the bladder and make urination more frequent, not less
frequent.
Urinary retention can be a sign of other medical concerns, such as a urinary tract infection or problems with bladder function.
It's important to report any difficulty urinating to a healthcare provider for proper evaluation and treatment.
Choice B rationale:
A decrease in vaginal discharge is not typically associated with impending labor. On the contrary, many women notice an
increase in vaginal discharge, often referred to as "bloody show," as labor approaches. This discharge is typically pink or
brownish in color and may contain streaks of blood. It's caused by the release of the mucus plug that seals the cervix during
pregnancy.
A decrease in vaginal discharge could be a sign of other issues, such as a decrease in amniotic fluid or a yeast infection. It's
important to report any changes in vaginal discharge to a healthcare provider for assessment.
Choice D rationale:
A weight gain of 0.5 to 1.5 kilograms (1 to 3 pounds) is not a reliable sign of impending labor. Weight fluctuations are common
in late pregnancy due to factors such as fluid retention and changes in blood volume. Some women may even lose a small
amount of weight in the days leading up to labor.
While significant weight gain (more than 2 kilograms or 4 pounds in a week) could indicate a potential issue like preeclampsia,
a small weight gain or loss is not typically a cause for concern in terms of labor onset.
Choice C rationale:
A surge of energy, often referred to as "nesting instinct," is a common sign that labor may be approaching. This sudden burst of
energy can manifest as a strong urge to clean, organize, and prepare the home for the baby's arrival. It's thought to be caused
by a combination of hormonal changes and the body's natural instincts to prepare for childbirth.
While the exact timing of labor is unpredictable, experiencing a surge of energy, especially in conjunction with other signs like
increased Braxton Hicks contractions, lower back pain, or pelvic pressure, may suggest that labor is likely to start within the
next few days or weeks.
A nurse is preparing to administer dinoprostone gel to a client who is pregnant.
The client asks the nurse about the purpose of the medication.
Which of the following responses should the nurse make?
Explanation
Choice A rationale:
Dinoprostone can be used to induce labor or terminate a pregnancy, but it is not accurate to say that it universally "assists with
ending the pregnancy."
Its primary action is to ripen the cervix, making it softer and more open, which can then lead to labor or facilitate other
medical interventions.
However, it's important to provide a more precise and informative response to the client's query.
Choice B rationale:
While dinoprostone can stimulate uterine contractions, this is not its primary purpose when used to prepare the cervix for
labor or other procedures.
Focusing solely on uterine contractions might lead to misunderstanding or undue concern for the client.
It's essential to emphasize the cervical ripening aspect of the medication.
Choice C rationale:
Dinoprostone does not relax uterine contractions. In fact, it can potentially increase the frequency and intensity of
contractions.
Stating that it relaxes contractions would be factually incorrect and could mislead the client about the medication's expected
effects.
Choice D rationale:
This is the most accurate and comprehensive response to the client's question.
Dinoprostone primarily functions to soften and efface the cervix, which is a crucial step in preparing for labor or certain
medical procedures related to pregnancy.
By promoting cervical ripening, dinoprostone can help facilitate a smoother and potentially less complicated labor process.
It's essential to provide the client with clear and accurate information about the medication's intended purpose.
that she thinks she is in labor.
Which of the following findings confirm that the client is in labor?
Explanation
Choice A rationale:
Amniotic fluid in the vaginal vault may indicate that the client's membranes have ruptured, but it does not necessarily mean
that labor has begun. Some women experience rupture of membranes before labor starts, while others do not experience it
until labor is well underway.
Additionally, it is not always possible to visually confirm the presence of amniotic fluid, as it may be mixed with other fluids or
present in small amounts.
Therefore, the presence of amniotic fluid alone is not a definitive sign of labor.
Choice B rationale:
Contractions are a common sign of labor, but they can also occur for other reasons, such as Braxton Hicks contractions or a
urinary tract infection.
To be considered a sign of true labor, contractions should be regular, becoming progressively stronger, longer, and closer
together.
A frequency of every 3 to 4 minutes is often suggestive of labor, but it is not always definitive.
Some women may experience contractions that are less frequent or more irregular and still be in labor.
Choice C rationale:
Cervical dilation is the most reliable sign of labor.
During labor, the cervix gradually opens to allow the baby to pass through the birth canal.
Cervical dilation is typically measured in centimeters, with 10 centimeters being considered full dilation.
Once the cervix has dilated to 3-4 centimeters, it is generally considered to be active labor.
This is because dilation of this degree usually indicates that the contractions are strong enough to effectively move the baby
through the birth canal.
Choice D rationale:
Pain just above the navel, also known as suprapubic pain, can be a sign of labor, but it is not a definitive one.
This type of pain can also be caused by other factors, such as bladder fullness or indigestion.
Additionally, not all women experience pain in this area during labor.
Which of the following findings should the nurse report to the provider?
Explanation
Choice A rationale:
Contraction duration: Contractions that last longer than 75 seconds are considered abnormal and should be reported to the
provider. This is because prolonged contractions can decrease oxygen supply to the fetus, leading to fetal distress.
Risk of uterine rupture: Excessively long contractions can also increase the risk of uterine rupture, a serious complication that
can endanger both the mother and the fetus.
Signs of fetal distress: The nurse should closely monitor the fetal heart rate for any signs of distress, such as late decelerations,
decreased variability, or bradycardia.
Need for intervention: If the contractions remain prolonged or if fetal distress is detected, the provider may need to intervene
to ensure the safety of both the mother and the fetus. This could involve measures such as administering medications to stop
or slow down labor, or performing a cesarean delivery.
Choice B rationale:
Contraction resting period: A contraction resting period of 35 seconds is within the normal range. Ideally, the resting period
between contractions should be at least 60 seconds, but it can vary. However, a resting period shorter than 30 seconds could
be a sign of tachysystole (excessively frequent contractions), which may also require intervention.
Choice C rationale:
Maternal heart rate: A maternal heart rate of 100 beats per minute is considered normal during labor. Heart rate can increase
with exertion, pain, and anxiety, which are common during labor. However, it's important to monitor for significant
tachycardia (heart rate over 120 beats per minute), which could indicate underlying issues such as dehydration or infection.
Choice D rationale:
Contraction frequency: One contraction in a 10-minute period is not indicative of active labor. Labor is typically defined as
having regular contractions that are 5 minutes apart or less, lasting for 45-60 seconds each, and causing progressive cervical
change. In early labor, contractions may be more sporadic and less intense.
Which of the following findings should the nurse report to the provider?
Explanation
Choice A rationale:
Umbilical cord compression is a serious condition that can deprive the fetus of oxygen and nutrients. It can occur during labor
due to various factors, such as excessive fetal movement, a long umbilical cord, or decreased amniotic fluid.
Key signs of umbilical cord compression include:
Variable decelerations: These are abrupt decreases in the fetal heart rate (FHR) that vary in duration, depth, and timing. They
are often caused by cord compression, as the compression temporarily reduces blood flow to the fetus.
Late decelerations: These are delayed decreases in the FHR that occur after the peak of a uterine contraction. They can also be
a sign of cord compression, as the compression can impair placental blood flow.
Loss of FHR variability: This refers to a decrease in the normal fluctuations of the FHR. It can be a sign of fetal distress,
including cord compression.
Immediate action is crucial when umbilical cord compression is suspected. The nurse should:
Notify the provider immediately.
Change the mother's position: This can help relieve pressure on the cord. Common positions include:
Lateral positioning (lying on the side)
Trendelenburg position (lying on the back with the head tilted down)
Knee-chest position (kneeling with the chest on the bed)
Administer oxygen to the mother: This can increase fetal oxygenation.
Prepare for possible interventions: These may include amnioinfusion (infusing fluid into the amniotic sac to increase fluid
volume), internal fetal monitoring, or cesarean delivery.
Choice B rationale:
Head compression is a common occurrence during labor as the fetal head descends through the birth canal. It usually does not
require intervention unless it causes significant changes in the FHR or other signs of fetal distress.
Choice C rationale:
Maternal opioid administration can affect the FHR, but it is not typically a cause for immediate concern unless there are
significant changes in the FHR or other signs of fetal distress. The nurse should continue to monitor the FHR closely and report
any concerns to the provider.
Choice D rationale:
Lateral decelerations are not a recognized pattern of fetal heart rate decelerations. The correct term for decelerations that
occur after the peak of a contraction is "late decelerations."
A nurse is caring for a group of clients on a postpartum unit.
Which of the following findings should be reported to the RN immediately?
Explanation
Choice A rationale:
2+ patellar reflex: A hyperactive patellar reflex (also known as a knee-jerk reflex) is a sign of hyperreflexia, which can be a neurological symptom of preeclampsia. Hyperreflexia results from heightened nerve excitability and can manifest as exaggerated reflexes. In preeclampsia, it stems from central nervous system irritability due to cerebral edema or other neurological disturbances.
2+ proteinuria: Proteinuria, defined as the presence of excessive protein in the urine, is a hallmark sign of preeclampsia. It indicates glomerular damage in the kidneys, leading to protein leakage into the urine. The degree of proteinuria is graded on a scale of 1+ to 4+, with 2+ representing a significant level that warrants immediate attention.
Choice B rationale:
24 weeks of gestation: While 24 weeks of gestation is considered early preterm birth, it is not inherently a finding that requires immediate reporting to the RN in the context of postpartum care. The focus on the postpartum unit is primarily on the health of the mother and newborn after delivery, rather than managing ongoing pregnancies.
Choice C rationale:
Preeclampsia: While preeclampsia is a serious condition that necessitates close monitoring and management, the mere diagnosis of preeclampsia without additional concerning findings does not automatically require immediate reporting to the RN. It's essential to assess for specific signs and symptoms that indicate worsening or complications of preeclampsia, such as those mentioned in Choice A.
Choice D rationale:
Heart rate of 100/min: A heart rate of 100 beats per minute is within the normal range for adults, even postpartum. Mild tachycardia (increased heart rate) can be a physiological response to various factors such as pain, anxiety, or exertion, and it does not always signify a serious problem. However, if the heart rate is persistently elevated or accompanied by other concerning symptoms, it would warrant further evaluation.
labor.
The client informs the nurse that she needs to push.
Which of the following is the appropriate action for the nurse to take?
Explanation
Rationale for Choice A:
Having the client pant during the next few contractions is not appropriate at this time. While panting can be a helpful
breathing technique during earlier stages of labor, it is not recommended when the client feels the urge to push.
Panting can actually delay the progress of labor by preventing the client from bearing down effectively.
It is important to allow the client to push when she feels the urge, as this will help to facilitate the descent of the fetal head and
progress labor.
Rationale for Choice B:
Helping the client to the bathroom to empty her bladder is not the priority action at this time. While a full bladder can
sometimes interfere with labor progress, it is more important to assess the perineum for signs of crowning before taking the
client to the bathroom.
If the fetal head is crowning, it is crucial to avoid any unnecessary delays in delivery.
Rationale for Choice C:
Assisting the client into a comfortable position is important for labor progress, but it is not the priority action at this time.
Assessment of the perineum for signs of crowning takes precedence, as it will guide the nurse's subsequent actions.
Once crowning is confirmed, the nurse can then help the client into a position that facilitates pushing, such as squatting, semi-
sitting, or side-lying.
Rationale for Choice D:
Assessing the perineum for signs of crowning is the most appropriate action for the nurse to take in this situation.
Crowning is the term used to describe the appearance of the fetal head at the vaginal opening.
It is a definitive sign that the client is in the second stage of labor and that delivery is imminent.
By assessing for crowning, the nurse can confirm the progress of labor and prepare for the delivery of the baby.
client’s perineal pad.
Which of the following actions should the nurse take first?
Explanation
Rationale for Choice A:
Checking the client's fundus is an important assessment in the postpartum period, but it is not the most immediate action
when a large amount of lochia rubra with clots is present. A boggy or displaced fundus could indicate subinvolution or
hemorrhage, but these are not the most likely causes of the presenting symptoms.
Rationale for Choice B:
Performing a vaginal examination is the most appropriate first action in this situation. This will allow the nurse to directly
assess the source and amount of bleeding, as well as to check for any retained placental fragments or cervical lacerations.
These findings could be the cause of the lochia rubra and clots, and prompt intervention may be necessary.
Rationale for Choice C:
While measuring the client's vital signs is an important part of the postpartum assessment, it is not the most immediate action
when there is evidence of active bleeding. Taking vital signs can be delayed while the nurse performs a vaginal examination to
assess the source and severity of the bleeding.
Rationale for Choice D:
Checking for a full bladder is not the most relevant action in this situation. A full bladder can contribute to postpartum
discomfort, but it is not likely to be the cause of the lochia rubra and clots. Addressing the bleeding should be the priority.
Sign Up or Login to view all the 57 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

