ATI Custom Maternity Final 23D
Total Questions : 69
Showing 25 questions, Sign in for moreWhich of these is a characteristic of a preterm infant?
Explanation
Choice A reason:
Hypertonia is not a characteristic of a preterm infant, but rather of a post-term infant. Hypertonia means increased muscle tone or stiffness, which is more common in infants who are overdue. Preterm infants have poor muscle tone and less subcutaneous fat.
Choice B reason:
Long toenails are also not a characteristic of a preterm infant but of a post-term infant. Long toenails indicate that the infant has grown beyond the expected gestational age. Preterm infants have short and brittle nails.
Choice C reason:
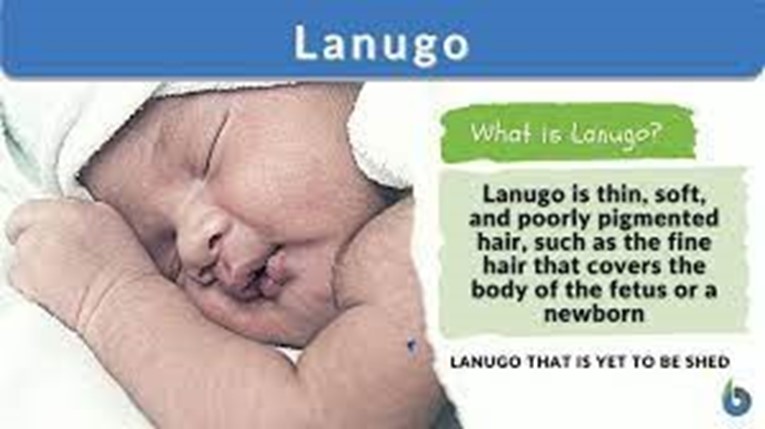
Lanugo is a characteristic of a preterm infant. Lanugo is fine, downy hair that covers the body of the fetus. It usually disappears by the 36th week of gestation, but preterm infants may still have it at birth.
Choice D reason:
Dry skin is not a characteristic of a preterm infant but of a post-term infant. Dry skin indicates that the infant has lost moisture and subcutaneous fat due to prolonged exposure to the amniotic fluid. Preterm infants have thin and transparent skin that may be covered by vernix caseosa, a white, cheesy substance that protects the skin from the amniotic fluid.
What are the signs and symptoms of Thalassemia? Select all that apply.
Explanation
Choice A reason:
Slow growth is a common symptom of thalassemia, especially in children. It is caused by the reduced production of hemoglobin and red blood cells, which leads to anemia and poor oxygen delivery to the tissues. Slow growth can also affect the development of facial bones and cause deformities.
Choice B reason:
Fatigue is another common symptom of thalassemia, also related to anemia and low oxygen levels in the body. People with thalassemia may feel tired, weak, and short of breath even after mild physical activity. Fatigue can also affect their mood, concentration, and quality of life.
Choice C reason:
Hematoma is not a typical symptom of thalassemia. Hematoma is a collection of blood under the skin or in an organ, usually caused by trauma, injury, or bleeding disorders. People with thalassemia may have a higher risk of bleeding due to low platelet counts or frequent blood transfusions, but this does not necessarily result in hematoma.
Choice D reason:
Pruritus is not a typical symptom of thalassemia. Pruritus is a sensation of itching that can affect any part of the body. It can have many causes, such as dry skin, allergies, infections, or liver problems. People with thalassemia may experience pruritus as a side effect of iron overload or iron chelation therapy, but it is not a direct consequence of the condition.
Choice E reason:
Ecchymoses are not typical symptoms of thalassemia. Ecchymoses are large bruises that appear on the skin due to bleeding under the surface. They can be caused by trauma, injury, or bleeding disorders. People with thalassemia may have a higher risk of bleeding due to low platelet counts or frequent blood transfusions, but this does not necessarily result in ecchymoses.
A nurse is caring for a newborn immediately following delivery. After assuring a patent airway, which of the following actions should be the nurse's priority?
Explanation
Choice A reason:

Drying the newborn's skin thoroughly is the nurse's priority after assuring a patent airway because it reduces evaporative heat loss by the newborn and prevents cold stress. Cold stress can lead to hypoxia, hypoglycemia, acidosis, and increased bilirubin levels. Drying the newborn also stimulates breathing and crying, which are signs of a healthy newborn.
Choice B reason:
Administering phytonadione IM is not the nurse's priority because it is not an immediate life-saving intervention. Phytonadione is given to prevent hemorrhagic disease of the newborn, which is caused by vitamin K deficiency. However, this condition usually occurs after the first day of life, so administering phytonadione can be delayed until after the initial assessment and stabilization of the newborn.
Choice C reason:
Documenting the Apgar score is not the nurse's priority because it is not an action that directly affects the newborn's well-being. The Apgar score is a tool to assess the newborn's condition at 1 and 5 minutes after birth based on five criteria: heart rate, respiratory effort, muscle tone, reflex irritability, and color. The Apgar score can help guide the nurse's interventions, but it is not more important than providing care to the newborn.
Choice D reason:
Applying identification bands is not the nurse's priority because it is not an urgent or essential action. Identification bands are used to ensure the safety and security of the newborn and prevent errors or mix-ups. However, applying identification bands can be done after the newborn is dried, warmed, and assessed for any problems.
A nurse is collecting data from a newborn who has respiratory distress syndrome and is experiencing respiratory acidosis. Which of the following risk factors predisposes the newborn to respiratory difficulties?
Explanation
Choice A reason:
Small for gestational age (SGA) newborns are at risk for respiratory distress syndrome (RDS) and respiratory acidosis because they have immature lungs that produce less surfactant, which is needed to keep the alveoli open and prevent atelectasis. SGA newborns also have less glycogen stores, which can lead to hypoglycemia and impaired oxygen delivery to the tissues.
Choice B reason:
Maternal history of asthma is not a risk factor for RDS or respiratory acidosis in the newborn. Asthma is a chronic inflammatory disorder of the airways that affects the mother, not the fetus. Maternal asthma can cause complications such as preterm labor, preeclampsia, or intrauterine growth restriction, but it does not directly affect the fetal lung development or function.
Choice C reason:
Ventricular septal defect (VSD) is a congenital heart defect that causes a hole in the wall between the ventricles of the heart. This can result in increased pulmonary blood flow and pressure, which can lead to pulmonary edema and heart failure in the newborn. However, VSD does not cause RDS or respiratory acidosis, which are related to lung maturity and surfactant production.
Choice D reason:
Cesarean birth is not a risk factor for RDS or respiratory acidosis in the newborn. Cesarean birth can increase the risk of transient tachypnea of the newborn (TTN), which is caused by delayed absorption of fetal lung fluid. TTN usually resolves within 24 to 48 hours and does not cause a significant acid-base imbalance in the newborn.
A nurse is caring for a client who is postpartum. The nurse should recognize which of the following statements by the client as a possible indicator of inhibition of parental attachment?
Explanation
Choice A reason:
This statement does not indicate inhibition of parental attachment. The client may have prior experience or knowledge of bathing a newborn and may not need the demonstration. The nurse should respect the client's autonomy and confidence in this skill.
Choice B reason:
This statement does not indicate inhibition of parental attachment. The client may be exhausted from the labor and delivery process and may need some rest to recover. The nurse should support the client's request and ensure that the newborn is well cared for in the nursery.
Choice C reason:
This statement indicates inhibition of parental attachment. The client expresses dissatisfaction with the newborn's appearance and implies that the newborn is not attractive enough. The nurse should explore the client's feelings and expectations about the newborn and provide reassurance and education about normal variations in newborn features.
Choice D reason:
This statement does not indicate inhibition of parental attachment. The client recognizes a family resemblance in the newborn and expresses a positive connection with the newborn and the partner. The nurse should acknowledge the client's observation and encourage further bonding with the newborn.
What is the most significant risk factor for clubfoot?
Explanation
Choice A reason:

Smoking is the most significant risk factor for clubfoot, according to several studies that have found a strong association between maternal smoking during pregnancy and the occurrence of clubfoot in the offspring. Smoking may affect the development of the muscles and tendons in the fetus, leading to abnormal positioning of the foot.
Choice B reason:
Trauma during pregnancy is not a significant risk factor for clubfoot, as there is no evidence that physical injury to the mother or the fetus can cause this deformity. Clubfoot is a congenital condition that is present at birth and usually detected by prenatal ultrasound.
Choice C reason:
Hypertension is not a significant risk factor for clubfoot, as there is no evidence that high blood pressure in the mother or the fetus can cause this deformity. Clubfoot is a congenital condition that is present at birth and usually detected by prenatal ultrasound.
Choice D reason:
Decreased circulation is not a significant risk factor for clubfoot, as there is no evidence that poor blood flow to the mother or the fetus can cause this deformity. Clubfoot is a congenital condition that is present at birth and usually detected by prenatal ultrasound.
A nurse is assisting in the care of a newborn who is 72 hr old and is receiving treatment for neonatal abstinence syndrome. Vital Signs Medical History Nurses Notes Physical Examination NAS Scoring System Newborn has a continuous high-pitched cry = 3 Sleeps less than 1 hr = 3 Hyperactive Moro reflex = 2 Moderate to severe tremors disturbed = 2 Increased muscle tone = 2 Excessive sucking = 1 Frequent yawning = 1 Projectile vomiting = 3 Watery stools = 3 Respirations greater than 60 with retractions = 2 NAS Score 22 Physical Examination Which of the following data collection findings should the nurse identify as requiring immediate follow- up? (Select all that apply.).
Explanation
Choice A reason:
Blood pressure is not a priority finding for a newborn with neonatal abstinence syndrome (NAS). Blood pressure may be slightly elevated due to increased muscle tone, but it is not a sign of severe withdrawal or a life-threatening complication.
Choice B reason:
Gastrointestinal disturbances are a common and serious symptom of NAS. They include poor feeding, excessive sucking, vomiting, diarrhea, and dehydration. These can lead to weight loss, electrolyte imbalance, and failure to thrive. Gastrointestinal disturbances require immediate follow-up and intervention to prevent further complications.
Choice C reason:
Skin color is not a priority finding for a newborn with NAS. Skin color may be slightly pale or mottled due to poor perfusion, but it is not a sign of severe withdrawal or a life-threatening complication.
Choice D reason:
NAS score is an important tool to assess the severity of withdrawal symptoms and the need for pharmacological treatment. However, it is not a data collection finding that requires
immediate follow-up. It is a cumulative score based on multiple findings that are evaluated over time.
Choice E reason:
Temperature is not a priority finding for a newborn with NAS. Temperature may be slightly elevated due to increased metabolic rate, but it is not a sign of severe withdrawal or a life-threatening
cry, hyperactive reflexes, increased muscle tone and seizures. These can lead to intracranial complications.
Choice F reason:
Oxygen saturation is a priority finding for a newborn with NAS. Respiratory distress is a common and serious symptom of NAS. It includes tachypnea, nasal flaring, retractions, grunting, and cyanosis. These can lead to hypoxia, acidosis, and respiratory failure. Oxygen saturation requires immediate follow-up and intervention to prevent further complications.
Choice G reason:
Central nervous system disturbances are a priority finding for a newborn with NAS. They include tremors, irritability, high-pitched hemorrhage, brain damage, and death. Central nervous system disturbances require immediate follow-up and intervention to prevent further complications.
Choice H reason:
Respiratory rate is not a priority finding for a newborn with NAS. Respiratory rate may be slightly increased due to increased metabolic rate, but it is not a sign of severe withdrawal or a life-threatening complication.
A nurse is assisting in the care of a newborn who is 72 hr old and is receiving treatment for neonatal abstinence syndrome. Vital Signs Medical History Nurses Notes Physical Examination The newborn has acrocyanosis, tachypnea with retractions, increased muscle tone, Newborn has a continuous high-pitch cry, and has slept less than 1 hr, Moderate to severe tremors noted when the newborn is disturbed, Newborn projectile vomited large amount of undigested formula, Newborn is consoled by rocking, Lights dimmed to decrease environmental stimuli, Which of the following data collection findings should the nurse identify as requiring immediate follow-up? (Select all that apply.).
Explanation
Choice A reason:
Blood pressure is not a priority finding for a newborn with neonatal abstinence syndrome (NAS). Blood pressure is usually normal or slightly elevated in NAS, and it is not a reliable indicator of the severity of withdrawal symptoms.
Choice B reason:
Gastrointestinal disturbances are a common and serious finding for a newborn with NAS. Vomiting and diarrhea can lead to dehydration, electrolyte imbalance, and poor weight gain. Projectile vomiting can also increase the risk of aspiration. This finding requires immediate follow-up and intervention.
Choice C reason:
Skin color is not a priority finding for a newborn with NAS. Acrocyanosis (bluish color of the hands and feet) is a normal finding in newborns and does not indicate hypoxia or poor circulation. It usually resolves within the first few days of life.
Choice D reason:
NAS score is not a priority finding for a newborn with NAS. NAS score is a tool used to assess the severity of withdrawal symptoms and the need for pharmacological treatment. It is based on a set of clinical signs and symptoms that are scored at regular intervals. However, it is not a substitute for clinical judgment and individualized care. The NAS score alone does not determine the urgency of follow-up.
Choice E reason:
Temperature is not a priority finding for a newborn with NAS. The temperature may be slightly elevated or normal in NAS, and it is not a specific sign of infection or withdrawal. Temperature regulation is important for newborns, but it is not an immediate concern in this case.
Choice F reason:
Oxygen saturation is a priority finding for a newborn with NAS. Tachypnea (rapid breathing) and retractions (inward movement of the chest wall) are signs of respiratory distress, which can compromise oxygen delivery to the tissues and organs. Hypoxia (low oxygen level) can cause brain damage, organ failure, and death if not corrected promptly. This finding requires immediate follow-up and intervention.
Choice G reason:
Central nervous system disturbances are a priority finding for a newborn with NAS. Increased muscle tone, tremors, high-pitched cries, and seizures are signs of neurological dysfunction, which can indicate brain injury, bleeding, or infection. Seizures can also worsen hypoxia and metabolic acidosis. This finding requires immediate follow-up and intervention.
Choice H reason:
Respiratory rate is not a priority finding for a newborn with NAS. Respiratory rate may be increased or normal in NAS, and it is not a specific sign of respiratory distress or infection. Respiratory rate should be monitored along with other vital signs, but.
A nurse is assisting in the care of a newborn who is 72 hours old and is receiving treatment for neonatal abstinence syndrome. Vital Sign. Medical History Nurses Notes. Medical History. A newborn who is 39 weeks of gestation is admitted to the newborn nursery following a spontaneous vaginal birth. Maternal history of opioid use during pregnancy and no prenatal care. Maternal positive drug screen for opioids. Newborn with a positive drug screen for opioids. Physical Examination. Which of the following data collection findings should the nurse identify as requiring immediate follow-up? (Select all that apply.).
Explanation
Choice A:
Blood pressure is not a priority finding for a newborn with neonatal abstinence syndrome (NAS). Blood pressure may be slightly elevated or normal in NAS, but it is not a sign of severe withdrawal or a risk for complications. •
Choice B:
Gastrointestinal disturbances are common and serious symptoms of NAS. They include poor feeding, vomiting, diarrhea, dehydration and poor weight gain. These can lead to electrolyte imbalance, malnutrition and failure to thrive. This choice requires immediate follow-up. •
Choice C:
Skin color is not a priority finding for a newborn with NAS. Skin color may be normal or slightly pale in NAS, but it is not a sign of severe withdrawal or risk for complications. •
Choice D:
NAS score is a priority finding for a newborn with NAS. NAS score is a tool used to assess the severity of withdrawal symptoms and the need for pharmacological treatment. A high NAS score indicates that the newborn needs medication to manage the withdrawal and prevent complications such as seizures. This choice requires immediate follow-up. •
Choice E:
Temperature is not a priority finding for a newborn with NAS. The temperature may be slightly elevated or normal in NAS, but it is not a sign of severe withdrawal or risk for complications. •
Choice F:
Oxygen saturation is a priority finding for a newborn with NAS. Oxygen saturation measures the amount of oxygen in the blood. Low oxygen saturation can indicate respiratory distress, which is a common and serious symptom of NAS. Respiratory distress can lead to hypoxia, acidosis, and brain damage. This choice requires immediate follow-up. •
Choice G:
Central nervous system disturbances are common and serious symptoms of NAS. They include tremors, irritability, excessive crying, hyperactivity, increased muscle tone, seizures, and sleep problems. These can indicate severe withdrawal and risk for neurological damage. This choice requires immediate follow-up.
Choice H:
Respiratory rate is a priority finding for a newborn with NAS. The respiratory rate measures the number of breaths per minute. A high respiratory rate can indicate respiratory distress, which is a common and serious symptom of NAS. Respiratory distress can lead to hypoxia, acidosis, and brain damage. This choice requires immediate follow-up.
A nurse is assisting in the care of a newborn who is 72 hours old and is receiving treatment for neonatal abstinence syndrome. Vital Signs Medical History. Vital Signs: Heart rate 160/min, Blood pressure: 78/42 mm Hg, Respiratory rate: 92/min, Temperature 38.1°C (100.6°F), Oxygen saturation 96%. PREVIOUS: Please Make a note during your proctored assessment. Physical Examination: Which of the following data collection findings should the nurse identify as requiring immediate follow-up? (Select all that apply.).
Explanation
Choice A:
Blood pressure. The normal blood pressure range for a newborn is 60 to 80 mm Hg systolic and 40 to 50 mm Hg diastolic. The baby's blood pressure is low, which could indicate shock, dehydration, infection, or heart failure. This requires immediate follow-up to identify and treat the cause.
Choice B:
Gastrointestinal disturbances. Gastrointestinal disturbances such as vomiting and diarrhea are common symptoms of neonatal abstinence syndrome (NAS), which is a withdrawal syndrome of infants after birth caused by in-utero exposure to drugs of dependence, most commonly opioids. These symptoms are not life-threatening and can be managed with supportive care such as hydration, nutrition, and comfort measures.
Choice C:
Skin color. Skin color is not a reliable indicator of NAS, as it can vary depending on the baby's ethnicity, temperature, oxygenation, and circulation. Skin color alone does not require immediate follow-up unless it is accompanied by other signs of distress such as cyanosis, pallor, or jaundice.
Choice D:
NAS score. NAS score is a tool used to assess the severity of withdrawal symptoms in infants with NAS. It includes items such as tremors, irritability, sleep problems, muscle tone, reflexes, seizures, yawning, sneezing, feeding, vomiting, stooling and temperature. A high NAS score indicates that the baby needs more intensive treatment such as medication to ease the withdrawal process. A low NAS score indicates that the baby is coping well and may not need medication. The NAS score should be monitored frequently and adjusted according to the baby's response.
Choice E:
Temperature. The normal temperature range for a newborn is 36.5 to 37.5°C (97.7 to 99.5°F). The baby's temperature is high, which could indicate infection, dehydration or hyperthermia. This requires immediate follow-up to identify and treat the cause.
Choice F:
Oxygen saturation. The normal oxygen saturation range for a newborn is 95 to 100%. The baby's oxygen saturation is within the normal range and does not require immediate follow- up unless it drops below 90% or rises above 100%, which could indicate hypoxia or hyperoxia respectively.
Choice G:
Central nervous system disturbances. Central nervous system disturbances such as seizures, tremors, irritability, and overactive reflexes are common symptoms of NAS. These symptoms are not life-threatening and can be managed with supportive care such as swaddling, rocking, dimming lights, and reducing noise.
Choice H:
Respiratory rate. The normal respiratory rate range for a newborn is 40 to 60 breaths per minute. The baby's respiratory rate is high, which could indicate respiratory distress, infection, pain, or anxiety. This requires immediate follow-up to identify and treat the cause.
A newborn is most interested in eating in which wake and sleep state?
Explanation
Choice A reason:
Drowsy. This is not the best state for feeding a newborn, because the baby may fall asleep before finishing the feed or may not latch on well. A drowsy baby may also have trouble swallowing or coordinating sucking and breathing. •
Choice B reason:
Crying. This is also not a good state for feeding a newborn, because crying is a late sign of hunger and indicates that the baby is already distressed. A crying baby may have difficulty calming down enough to feed or may gulp air and become gassy. •
Choice C reason:
Active alert. This is a possible state for feeding a newborn, but not the most optimal one. An active alert baby may be easily distracted by noises or movements around them or may become fussy or overstimulated if they are not fed quickly enough. •
Choice D reason:
Alert. This is the best state for feeding a newborn because the baby is awake, calm, and attentive to their surroundings. An alert baby will show signs of hunger such as rooting, smacking their lips, or sucking their fingers, and will be ready to latch on and feed well.
A nurse is reinforcing teaching about appropriate exercises during pregnancy with a client who is at 24 weeks of gestation. Which of the following statements indicates a need for additional teaching?
Explanation
Choice A reason:
Swimming is one of the best and safest exercises for pregnant women. It exercises your large muscle groups, provides cardiovascular benefits, reduces swelling, and allows you to feel weightless. Swimming is also a low-impact exercise that does not put too much stress on your joints and muscles. Therefore, this statement does not indicate a need for additional teaching.
Choice B reason:
Racquetball is not an appropriate exercise during pregnancy. It is a high-impact sport that involves sudden changes of direction, quick movements, and the risk of falling or getting hit by the ball or the racquet. These factors can increase the chance of injury, bleeding, or premature labor. Therefore, this statement indicates a need for additional teaching.
Choice C reason:
Cycling on a stationary bike is a safe exercise during pregnancy. It provides moderate aerobic conditioning and relieves stress and tension in your joints and muscles. Cycling on a stationary bike also reduces the risk of falling or losing balance compared to cycling on a regular bike. Therefore, this statement does not indicate a need for additional teaching.
Choice D reason:
Yoga is a beneficial exercise during pregnancy. It can help you relax, improve your flexibility, strengthen your muscles, and prepare your body for labor and delivery. Yoga can also help you cope with symptoms of depression and anxiety during pregnancy. However, you should avoid hot yoga or poses that involve lying flat on your back, twisting your abdomen, or compressing your belly. Therefore, this statement does not indicate a need for additional teaching.
A nurse is caring for a postpartum client following a vaginal birth of a newborn weighing 4252 g (9 lb 6 oz). The nurse should identify that this client is at risk for which of the following postpartum complications?
Explanation
Choice A reason:
Uterine atony is the failure of the uterus to contract and retract after delivery, which can lead to excessive bleeding and hemorrhage. It is the most common cause of postpartum hemorrhage, accounting for up to 80 percent of cases. Risk factors for uterine atony include large or multiple babies, prolonged or rapid labor, overdistended uterus, use of oxytocin or magnesium sulfate during labor, and previous history of uterine atony.
Choice B reason:
Puerperal infection is an infection of the reproductive tract that occurs within six weeks after delivery. It can affect the uterus (endometritis), the bladder (cystitis), the kidneys (pyelonephritis), the breast (mastitis), or the wound (cesarean section or episiotomy).
Symptoms include fever, chills, malaise, foul-smelling lochia, pelvic pain, and wound redness or drainage. Risk factors for puerperal infection include cesarean delivery, prolonged rupture of membranes, prolonged labor, multiple vaginal examinations, retained placental fragments, and poor hygiene.
Choice C reason:
Retained placental fragments are pieces of the placenta that remain in the uterus after delivery. They can cause postpartum hemorrhage, infection, or delayed involution of the uterus. Symptoms include heavy or prolonged bleeding, fever, abdominal pain, and an enlarged uterus. Risk factors for retained placental fragments include placenta previa, placenta accrete, manual removal of the placenta, and incomplete examination of the placenta after delivery.
Choice D reason:
Thrombophlebitis is the inflammation and clotting of a vein, usually in the legs or pelvis. It can cause pain, swelling, redness, and warmth in the affected area. It can also lead to pulmonary embolism if the clot breaks off and travels to the lungs. Risk factors for thrombophlebitis include pregnancy and the postpartum period, cesarean delivery, obesity, smoking, dehydration, immobility, varicose veins, and inherited or acquired clotting disorders.
Exhibit 1. What are the risk factors for neonatal sepsis? Select all that apply. (Select All that Apply.).
Explanation
Choice A reason:
Preterm birth is a major risk factor for neonatal sepsis, especially early-onset sepsis. Preterm babies have immature immune systems and lack antibodies to protect them against certain bacteria.
Choice B reason:
Cesarean birth is not a risk factor for neonatal sepsis by itself, unless it is associated with other factors such as prolonged rupture of membranes, maternal infection or chorioamnionitis.
Choice C reason:
Precipitous delivery is a risk factor for neonatal sepsis, especially early-onset sepsis. Precipitous delivery can cause fetal distress, hypoxia, acidosis and increased susceptibility to infection.
Choice D reason:
Frequent vaginal exams are a risk factor for neonatal sepsis, especially early-onset sepsis. Frequent vaginal exams can introduce bacteria into the amniotic fluid and increase the risk of ascending infection.
Choice E reason:
Mother has GBS infection is a risk factor for neonatal sepsis, especially early-onset sepsis. GBS (group B streptococcus) is the most common cause of early-onset neonatal sepsis and can be transmitted from the mother to the baby during labor and delivery.
Which of the following are contraindications for VBAC? (Select All that Apply.).
Explanation
Choice A reason:
A prior vaginal delivery is not a contraindication for VBAC. In fact, it is a positive predictor of success for VBAC, as it indicates that the woman has a proven pelvis and can tolerate labor.
Choice B reason:
The gestation of 42 weeks is not a contraindication for VBAC. However, it is associated with an increased risk of stillbirth while awaiting spontaneous labor, which should be balanced against the risks of induction of labor or elective repeat cesarean.
Choice C reason:
Maternal obesity is a relative contraindication for VBAC. It is associated with a lower success rate of VBAC, a higher risk of uterine rupture, and a higher risk of maternal and neonatal complications. The decision to attempt VBAC in obese women should be made on a case-by-case basis by a senior obstetrician.
Choice D reason:
One prior cesarean delivery is not a contraindication for VBAC. Most women who have had one prior lower segment cesarean delivery are eligible for VBAC, as the risk of uterine rupture is low (0.5%) and the success rate is high (72-75%).
Choice E reason:
A macrosomic fetus is a relative contraindication for VBAC. It is associated with a lower success rate of VBAC, a higher risk of uterine rupture, and a higher risk of shoulder dystocia and birth trauma. The decision to attempt VBAC in women with suspected macrosomia should be made on a case-by-case basis by a senior obstetrician.
A nurse is contributing to the plan of care for a preterm newborn. To help the newborn conserve energy, which of the following actions should the nurse recommend?
Explanation
Choice A reason:
Allowing opportunities for newborn massage is not recommended for preterm newborns, as it can increase their oxygen consumption and energy expenditure. Massage can also cause stress responses, such as increased heart rate, blood pressure, and cortisol levels.
Choice B reason:
Clustering the newborn's care activities is the best way to help the newborn conserve energy, as it minimizes the frequency of handling and stimulation. Clustering care also allows for longer periods of uninterrupted sleep, which is essential for growth and development.
Choice C reason:
Changing the newborn's position every 2 hours is not necessary for preterm newborns, as it can disrupt their sleep and cause them to lose heat. Preterm newborns have limited ability to regulate their body temperature, and frequent position changes can expose them to cold stress.
Choice D reason:
Placing elbow restraints on the newborn is not indicated for preterm newborns, unless they have a specific condition that requires them, such as a cleft lip or palate repair. Elbow restraints can restrict the newborn's movement and cause skin irritation or injury.
A nurse is caring for a client who might have a hydatidiform mole. The nurse should monitor the client for which of the following findings?
Explanation
Choice A reason:
Fetal heart rate irregularities are not a sign of hydatidiform mole, as this condition involves an abnormal fertilization of the egg that results in an abnormal or absent fetus.
Choice B reason:
Whitish vaginal discharge is a possible sign of hydatidiform mole, as this may indicate the presence of molar tissue in the uterus This is the correct answer.
Choice C reason:
Rapidly dropping human chorionic gonadotropin (hCG) levels are not a sign of hydatidiform mole, as this condition causes very high levels of hCG due to the overgrowth of the placental tissue.
Choice D reason:
Excessive uterine enlargement is a possible sign of hydatidiform mole, as this may indicate the presence of molar tissue in the uterus However, this is not as specific as whitish vaginal discharge, which is more characteristic of this condition.
A nurse is reinforcing teaching with a new mother about the purpose of administering vitamin K to her newborn following delivery. The nurse should explain that the purpose of administering vitamin K is to prevent which of the following complications?
Explanation
Choice A reason:
Infection is not prevented by vitamin K administration. Vitamin K is needed for blood clotting, not for fighting infections. Newborns are given vitamin K injections to prevent a serious disease called hemorrhagic disease of the newborn (HDN), which is caused by bleeding in the brain or other organs.
Choice B reason:
Hyperbilirubinemia is not prevented by vitamin K administration. Hyperbilirubinemia is a condition in which there is too much bilirubin in the blood, causing jaundice. Bilirubin is a yellow pigment that is produced when red blood cells break down. Vitamin K does not affect the production or breakdown of bilirubin.
Choice C reason:
Bleeding is prevented by vitamin K administration. Vitamin K is needed for the synthesis of several clotting factors that help stop bleeding when there is an injury. Newborns have very low levels of vitamin K in their bodies because they do not get enough from the placenta or breast milk, and they do not have enough bacteria in their intestines to produce it. This puts them at risk for VKDB, which can cause life-threatening bleeding in the brain or other organs.
Choice D reason:
Potassium deficiency is not prevented by vitamin K administration. Potassium is an electrolyte that is important for nerve and muscle function, as well as fluid balance. Vitamin K does not affect the absorption or excretion of potassium.
What is true regarding FAS and NAS?
Explanation
Choice A reason:
FAS is caused by alcohol, and NAS is caused by opioids. This is the correct answer because FAS stands for fetal alcohol syndrome, which is a condition that affects the development of a baby when the mother drinks alcohol during pregnancy. NAS stands for neonatal abstinence syndrome, which is a group of problems that can happen when a baby is exposed to opioid drugs for a length of time while in their mother's womb.
Choice B reason:
FAS and NAS are both incurable. This is incorrect because FAS and NAS are not diseases, but conditions that result from prenatal exposure to substances. FAS and NAS can cause various physical, mental, and behavioral problems in the baby, some of which may be permanent, but others may be improved with early intervention and treatment.
Choice C reason:
FAS is caused by analgesics and NAS is caused by NSAIDs. This is incorrect because analgesics are painkillers, and NSAIDs are nonsteroidal anti-inflammatory drugs. Neither of these types of drugs is known to cause FAS or NAS. However, some analgesics, such as codeine and oxycodone, are opioids and can cause NAS if used by pregnant women.
Choice D reason:
FAS and NAS are both curable. This is incorrect because FAS and NAS are not diseases, but conditions that result from prenatal exposure to substances. FAS and NAS can cause various physical, mental, and behavioral problems in the baby, some of which may be permanent, but others may be improved with early intervention and treatment. However, there is no cure for FAS or NAS.
A nurse is collecting data from a client who gave birth 12 hours ago. The nurse notes the fundus is deviated to the right, boggy, and 2 cm above the umbilicus. Which of the following actions should the nurse take first?
Explanation
Choice A reason:
Administering methylergometrine to the client is not the first action the nurse should take. Methylergometrine is a medication that stimulates uterine contractions and can help reduce postpartum bleeding. However, it can also cause hypertension and should be used with caution in clients with high blood pressure. Furthermore, the nurse should first identify and address the cause of the boggy and deviated fundus before giving any medication.
Choice B reason:
Assisting the client to void is the first action the nurse should take. A full bladder can displace the uterus and prevent it from contracting properly, leading to uterine atony and bleeding.
The nurse should help the client empty her bladder by encouraging her to use the bathroom, providing privacy, running water, or using a bedpan. This can help the uterus return to its normal position and tone.
Choice C reason:
Inserting an indwelling urinary catheter is not the first action the nurse should take. A urinary catheter can be used to drain the bladder if the client is unable to void or has a large amount of residual urine. However, it can also increase the risk of infection and trauma to the urethra
and bladder. The nurse should first try noninvasive methods to help the client void, such as those mentioned in choice B.
Choice D reason:
Obtaining a stat hemoglobin level is not the first action the nurse should take. A hemoglobin level can indicate the extent of blood loss and the need for transfusion or other interventions. However, it is not a priority over restoring uterine tone and preventing further bleeding. The nurse should first assist the client to void and then massage the fundus if it remains boggy.
Exhibit 1. What are possible complications of prematurity? Select all that apply. (Select All that Apply.).
Explanation
Choice A reason:
Cerebral palsy is a disorder that affects movement, posture, and muscle tone. It can be caused by brain damage that occurs before, during, or after birth. Premature babies are at a higher risk of developing cerebral palsy because they are more likely to have bleeding in the brain, lack of oxygen to the brain, infections or other complications that can damage the brain.
Choice B reason:
Color blindness is a condition that affects the ability to see colors or differences in colors. It is usually inherited and not related to prematurity. However, some premature babies may develop retinopathy of prematurity, which can affect their vision in other ways.
Choice C reason:
Learning disabilities are problems that affect the ability to learn, read, write, speak or do math. They can be caused by genetic factors, environmental factors or brain injuries.
Premature babies are more likely to have learning disabilities because they are more likely to have brain damage, low birth weight, infections or other complications that can affect their brain development.
Choice D reason:
Retinopathy is a disease that affects the blood vessels in the retina, the light-sensitive layer of tissue at the back of the eye. Retinopathy of prematurity is a condition that occurs when the blood vessels in the retina grow abnormally in premature babies. This can cause bleeding, scarring or detachment of the retina, which can lead to vision loss or blindness.
Choice E reason:
Apnea is a condition that causes pauses in breathing during sleep. Apnea of prematurity is a condition that affects premature babies who have not fully developed their nervous system and respiratory system. This can cause them to stop breathing for more than 20 seconds at a time, which can lower their oxygen levels and heart rate.
Exhibit 1. The names of the newborn reflexes are? Select all that apply. (Select All that Apply.)
Explanation
Choice A reason:
Moro is a newborn reflex that occurs when the baby is startled by a loud sound or movement. The baby will cry, throw back his or her head, and then pull his or her limbs into the body. This reflex lasts until the baby is about 2 months old.
Choice B reason:
Rooting is a newborn reflex that starts when the corner of the baby's mouth is stroked or touched. The baby will turn his or her head and open his or her mouth to follow and root in the direction of the stroking. This helps the baby find the breast or bottle to start feeding. This reflex lasts about 4 months.
Choice C reason:
Gag is a newborn reflex that prevents the baby from choking on foreign objects. The baby will cough, gag or spit out anything that touches the back of the throat or the roof of the mouth. This reflex is present throughout life.
Choice D reason:
Running is not a newborn reflex. It is a voluntary movement that develops later in childhood. Choice E reason:
Babinski is a newborn reflex that occurs when the sole of the foot is stroked from heel to toe. The baby will fan out and curl up the toes and twist the foot inward. This reflex lasts until the baby is about 12 months old.
Choice F reason:
Stepping is a newborn reflex that occurs when the baby is held upright with his or her feet touching a solid surface. The baby will appear to take steps or dance. This reflex lasts about 2 months.
A nurse is caring for a client who is at 36 weeks of gestation and has suspected placenta previa. For which of the following findings should the nurse monitor the client?
Explanation
Choice A reason:
Intermittent abdominal pain following passage of bloody mucus is not a sign of placenta previa, but rather of bloody show, which is a normal occurrence in late pregnancy as the cervix begins to dilate and efface.
Choice B reason:
Abdominal pain with minimal red vaginal bleeding is not a sign of placenta previa, but rather of abruptio placentae, which is a serious complication where the placenta detaches from the uterine wall before delivery.
Choice C reason:
A large amount of bright red vaginal bleeding without pain is a sign of placenta previa, which is a condition where the placenta covers part or all of the cervical opening. This can cause bleeding when the cervix dilates or contracts, especially in the third trimester. This is a medical emergency that requires immediate attention.
Choice D reason:
Severe abdominal pain with increasing fundal height is not a sign of placenta previa, but rather of uterine rupture, which is a rare but life-threatening complication where the uterus tears open along the scar line from a previous cesarean delivery or other uterine surgery. This can cause severe bleeding, fetal distress, and shock.
A patient diagnosed with Iron deficiency has been instructed to eat iron-rich food, what statement indicates understanding by the patient?
Explanation
Choice A reason:
Eating leafy green vegetables is a good way to increase iron intake, as they are rich in iron and other nutrients. Iron is needed to produce hemoglobin, the protein that carries oxygen in red blood cells. Iron deficiency anemia occurs when there is not enough iron to make hemoglobin, resulting in low red blood cell count and low oxygen delivery to the tissues.
Leafy green vegetables such as broccoli, kale, turnip greens, and collard greens are among the best sources of iron from plants.
Choice B reason:
Taking calcium supplements is not helpful for iron deficiency anemia, as calcium can interfere with iron absorption. Calcium binds to iron in the intestine and prevents it from being absorbed into the bloodstream. Therefore, calcium supplements should not be taken at the same time as iron supplements or iron-rich foods. Calcium is important for bone health, but it does not affect hemoglobin production or red blood cell count.
Choice C reason:
Consuming two glasses of prune juice daily is not advisable for iron deficiency anemia, as prune juice has a laxative effect and can cause diarrhea. Diarrhea can lead to dehydration and loss of nutrients, including iron. Prune juice also contains oxalates, which are compounds that can reduce iron absorption by forming insoluble complexes with iron in the intestine. Prune juice does contain some iron, but not enough to compensate for its negative effects on iron status.
Choice D reason:
Consuming raw sushi is not recommended for iron deficiency anemia, as raw fish can contain parasites or bacteria that can cause infections. Infections can increase inflammation and blood loss, which can worsen iron deficiency anemia. Raw fish also contains phytates, which are substances that can inhibit iron absorption by binding to iron in the intestine. Raw fish does provide some iron, but it is not a reliable or safe source of iron for people with iron deficiency anemia. : Iron deficiency anemia - Diagnosis & treatment - Mayo Clinic. : Iron- Deficiency Anemia - Hematology.org.
A nurse is caring for a newborn who was delivered by vacuum extraction and has swelling on his head that crosses the suture line. The newborn's mother asks about the swelling on her newborn's head. Which of the following responses should the nurse make?
Explanation
Choice A reason:
This is a caput succedaneum, which is a collection of fluid from pressure of the vacuum extractor. This is the correct answer because caput succedaneum is a swelling of the scalp that crosses the suture line and is caused by prolonged pressure on the baby's head during delivery. It can also result from the use of vacuum extraction or forceps. Caput succedaneum is harmless and usually resolves on its own within a few days.
Choice B reason:
This is erythema toxicum, which is a transient allergic reaction that causes edema in the skin. This is incorrect because erythema toxicum is a common rash that affects newborns, but it does not cause swelling of the scalp or cross the suture line. It appears as red blotches with small white or yellow bumps that can occur anywhere on the body. Erythema toxicum is also harmless and usually disappears within a week.
Choice C reason:
This is a cephalhematoma, which will resolve on its own in 3 to 5 days. This is incorrect because cephalhematoma is bleeding under the scalp that does not cross the suture line and is caused by ruptured blood vessels in the scalp. It can also result from the use of vacuum extraction or forceps. Cephalhematoma may take weeks or months to resolve and can increase the risk of jaundice.
Choice D reason:
This is a Mongolian spot, which is found on many newborns. This is incorrect because Mongolian spots are bluish-gray patches of skin that are present at birth and are caused by melanocytes (pigment-producing cells) that are trapped in the deeper layers of the skin. They are not related to swelling or pressure on the head and usually fade by age 5.
Sign Up or Login to view all the 69 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

