ATI Custom MS Nurse
Total Questions : 47
Showing 25 questions, Sign in for moreWhile collecting data from a client who has a cast on his right leg, a nurse locates an area on the cast that feels warm to the touch. Which of the following findings should the nurse identify as a complication to the client's condition?
Explanation
The nurse should identify infection as a complication to the client's condition. A warm area on the cast could indicate the presence of an underlying infection. The warmth could be due to an increase in blood flow to the area as the body tries to fight off the infection.
Uneven cast drying, pressure from the cast, and poor circulation are not complications that would cause a warm area on the cast. Uneven cast drying could cause discomfort but would not result in warmth. Pressure from the cast could cause skin breakdown but would not result in warmth. Poor circulation could cause coolness or pallor but would not result in warmth.
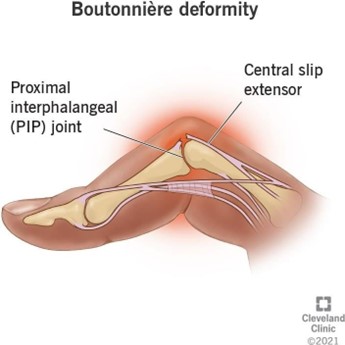
A nurse is collecting data from a client who has rheumatoid arthritis. Which of the following is an expected finding for this client?
Explanation
Boutonniere deformity is an expected finding for a client who has rheumatoid arthritis. It is a type of hand deformity that can occur in people with rheumatoid arthritis. It is characterized by a bent middle finger joint and a hyperextended fingertip.
Tophi, osteoma, and Heberden's nodules are not expected findings for a client who has rheumatoid arthritis. Tophi are deposits of uric acid crystals that can occur in people with gout. Osteoma is a benign bone tumour. Heberden's nodules are bony growths that can occur in people with osteoarthritis.
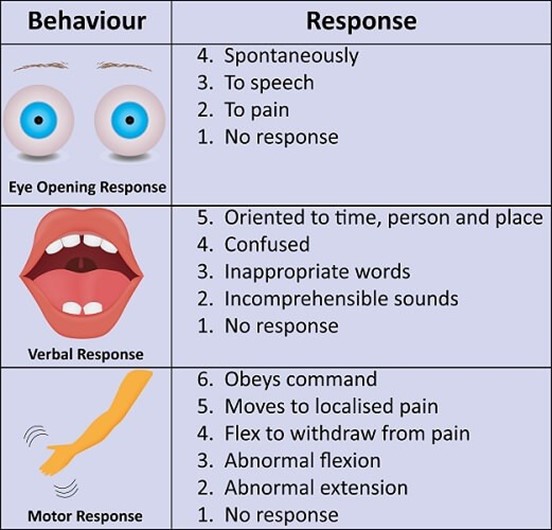
A nurse is receiving a transfer report for a client who has a head injury. The client has a Glasgow Coma Scale (GCS) score of 3 for eye opening, 5 for best verbal response, and 5 for best motor response. Which of the following is an appropriate conclusion based on this data?
Explanation
An appropriate conclusion based on this data is that the client opens his eyes when spoken to. A GCS score of 3 for eye opening indicates that the client opens his eyes in response to voice.
The client is not unconscious, as a GCS score of 3 for eye opening indicates that the client is able to open his eyes in response to voice. The client is not unable to make vocal sound, as a GCS score of 5 for best verbal response indicates that the client is able to make vocal sounds. The client may or may not be able to follow simple motor commands, as a GCS score of 5 for best motor response indicates that the client is able to localize pain.
A nurse is assisting a client who is postoperative following a total hip arthroplasty into a supine position. Which of the following actions is appropriate to prevent hip dislocation?
Explanation
An appropriate action to prevent hip dislocation in a client who is postoperative following a total hip arthroplasty is to place a wedge pillow between the legs. This helps to maintain proper alignment and prevent the legs from crossing or adducting, which can cause hip dislocation.
Placing a trochanter roll against the thigh, placing a sandbag on the lateral calf, and placing a footboard on the bed are not appropriate actions to prevent hip dislocation in this situation. A trochanter roll is used to prevent the external rotation of the hip. A sandbag to the lateral calf can help prevent foot drop. A footboard can help prevent plantar flexion contractures.
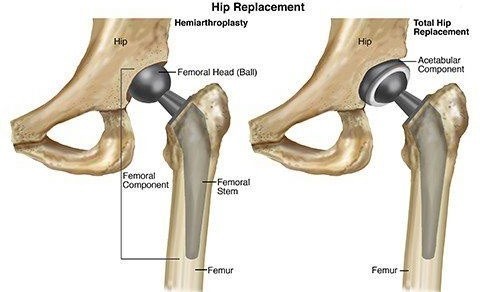
A nurse is caring for a client who is postoperative following a right total hip arthroplasty. In which of the following positions should the nurse place the client's right leg?
Explanation
The nurse should place the client's right leg in abduction following a right total hip arthroplasty. Abduction means moving the leg away from the midline of the body. This position helps to prevent hip dislocation by keeping the hip joint in proper alignment.
Internal rotation, adduction, and external rotation are not appropriate positions for the client's right leg following a right total hip arthroplasty. Internal rotation means turning the leg inward towards the midline of the body. Adduction means moving the leg towards the midline of the body. External rotation means turning the leg outward away from the midline of the body. These positions can increase the risk of hip dislocation.
A nurse in a long-term care facility finds an older adult client lying on the floor next to the bed. Which of the following actions should the nurse take?
Explanation
The first action the nurse should take is to check the client for injuries. The nurse should assess the client for any signs of injury or trauma and provide appropriate care as needed.
Obtaining a prescription for medication to sedate the client, calling the family and asking them to make arrangements for someone to sit with the client, and assisting the client back into bed and applying restraints are not appropriate initial actions for the nurse to take in this situation. These actions may be considered after the client has been assessed for injuries and their immediate needs have been addressed.
A nurse is shopping and finds a woman who has collapsed with right-sided weakness and slurred speech.
Which of the following actions should the nurse take?
Explanation
The nurse should call emergency medical services if they find a woman who has collapsed with right-sided weakness and slurred speech. These symptoms could indicate a stroke or other serious medical condition that requires immediate medical attention.
Finding a location for the client to sit, driving the client to the nearest emergency room, and obtaining the number of the client's provider are not appropriate initial actions for the nurse to take in this situation. The priority is to get the client immediate medical attention by calling emergency medical services.
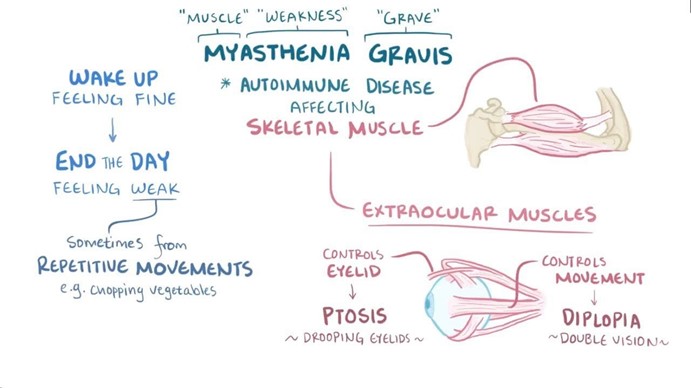
A nurse in the emergency department is assisting with the care of a client who has myasthenia gravis and is in crisis. The nurse should identify that which of the following factors can cause a myasthenic crisis?
Explanation
The nurse should identify that developing a respiratory infection can cause a myasthenic crisis in a client who has myasthenia gravis. A myasthenic crisis is a sudden worsening of myasthenia gravis symptoms, which can include difficulty breathing and swallowing. Respiratory infections can exacerbate these symptoms and trigger a myasthenic crisis.
Taking too much-prescribed medication, insufficient exercise, and insufficient sleep are not factors that can cause a myasthenic crisis. Taking too much-prescribed medication can cause side effects but would not directly cause a myasthenic crisis. Insufficient exercise and insufficient sleep can worsen overall health but would not directly cause a myasthenic crisis.
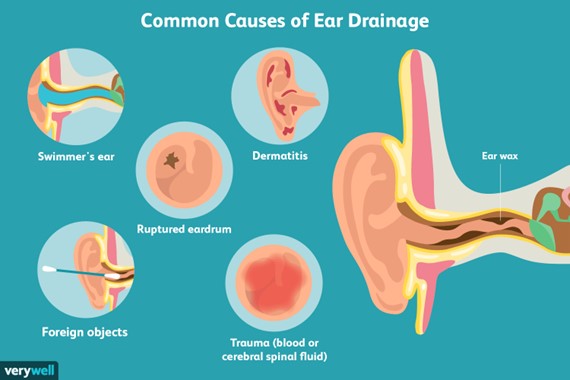
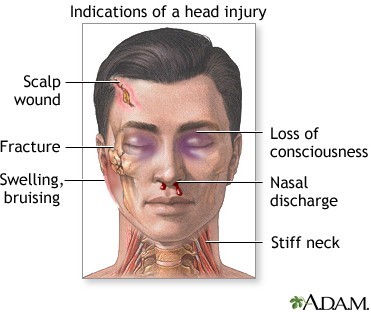
A nurse is collecting data from a client who fell at home and reported a brief loss of consciousness. Which of the following findings should the nurse immediately report to the charge nurse?
Explanation
The nurse should immediately report small drops of clear fluid in the left ear to the charge nurse. This finding could indicate a cerebrospinal fluid (CSF) leak, which can occur as a result of a head injury. A CSF leak can be a serious medical condition that requires immediate attention.
An edematous bruise on the forehead, client disorientation to place, and a heart rate of 110/min and regular are also important findings that the nurse should report to the charge nurse. However, these findings are not as urgent as the presence of small drops of clear fluid in the left ear.
A nurse is reviewing discharge instructions with the family of a client who sustained a minor head injury earlier in the day. Which of the following instructions should the nurse include?
Explanation
The nurse should instruct the family to not let the client engage in strenuous activities for 1 week following a minor head injury. This can help prevent further injury and allow the client to rest and recover.
Applying heat to the area of swelling for the first 48 hr, repeatedly asking the client questions to check for orientation, and encouraging the client to sleep for the first 24 hr are not appropriate instructions for the nurse to include in this situation. Applying heat can increase swelling and inflammation. Repeatedly asking the client questions can be disorienting and confusing. Encouraging the client to sleep for the first 24 hr is not necessary and could interfere with monitoring the client's condition.
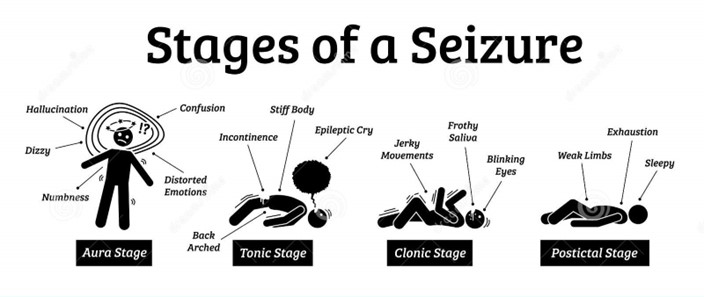
A nurse enters a client's room and finds the client on the floor in the clonic phase of a tonic-clonic seizure. Which of the following interventions should the nurse take?
Explanation
The nurse should place a pillow under the client's head if the client is on the floor in the clonic phase of a tonic-clonic seizure. This can help protect the client's head from injury during the seizure.
Inserting a padded tongue blade into the client's mouth, keeping the client in a supine position, and gently restraining the client's extremities are not appropriate interventions for the nurse to take in this situation. Inserting a padded tongue blade into the client's mouth can cause injury to the teeth and gums. Keeping the client in a supine position can increase the risk of aspiration. Gently restraining the client's extremities can cause injury and is not recommended during a seizure.

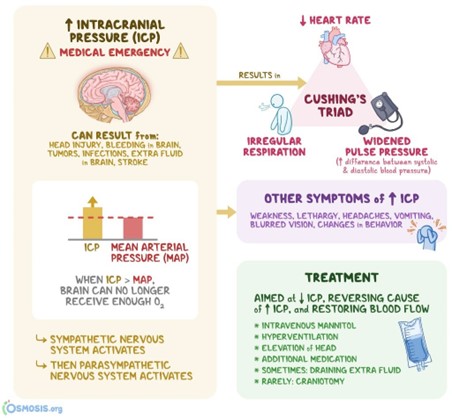
A nurse is assisting in the planning of preventative care for a client who is restless following a traumatic brain injury with increased intracranial pressure. Which of the following is an appropriate nursing action?
Explanation
An appropriate nursing action for a client who is restless following a traumatic brain injury with increased intracranial pressure is to reduce stimuli. This can help calm the client and prevent further increases in intracranial pressure. The nurse can reduce stimuli by minimizing noise and light in the client's environment and limiting the number of visitors.
Administering opioids, applying restraints, and blackening the room are not appropriate nursing actions for this situation. Administering opioids can cause respiratory depression and is not recommended for clients with increased intracranial pressure. Applying restraints can increase agitation and is not recommended for clients who are restless. Blackening the room can disorient the client and is not recommended.
A nurse is caring for a client who is difficult to arouse and very sleepy for several hours following a generalized tonic-clonic seizure. Which of the following descriptions should the nurse use when documenting this finding in the medical record?
Explanation
The nurse should use the term "postictal phase" when documenting the client's difficulty arousing and sleepiness for several hours following a generalized tonic-clonic seizure. The postictal phase is the period of time immediately following a seizure during which the client may be difficult to arouse and very sleepy.
Presence of absence seizures, presence of automatisms, and aura phase are not appropriate descriptions for the nurse to use when documenting this finding in the medical record. Absence seizures are a type of seizure characterized by brief episodes of staring and unresponsiveness. Automatisms are repetitive, unconscious movements that can occur during a seizure. The aura phase is a warning sign that can occur before a seizure.
A nurse is caring for a client who is unconscious following a stroke. Which of the following nursing interventions is of highest priority?
Explanation
The highest priority nursing intervention for a client who is unconscious following a stroke is to suction saliva from the client's mouth. This can help prevent aspiration and maintain a patent airway, which is essential for the client's survival.
Performing passive range of motion on each extremity, recording the client's intake and output, and monitoring the client's electrolyte levels are also important nursing interventions for this client. However, these interventions are not as high of a priority as maintaining a patent airway.

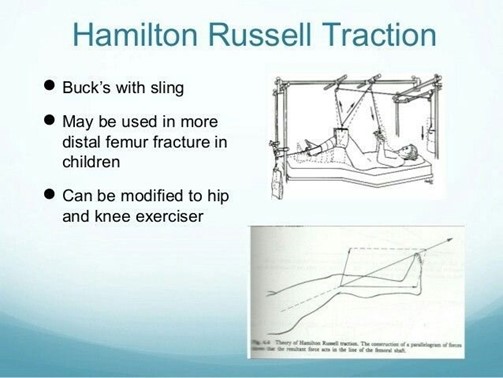
A nurse is reinforcing teaching about Russell's traction with a newly licensed nurse. Which of the following statements should the nurse make?
Explanation
The nurse should tell the newly licensed nurse that Russell's traction uses a sling under the knee to treat a fracture of the femur. Russell's traction is a type of skin traction that is used to immobilize and align a fractured femur. It involves placing a sling under the knee and applying weights to the affected leg to provide continuous traction.
Russell's traction does not use a cervical halter, skeletal pins, or a pelvic girdle belt. A cervical halter is used to treat neck injuries. Skeletal pins are used in skeletal traction to stabilize fractures. A pelvic girdle belt is used to treat lower back pain.
A nurse is collecting data from a client who has a traumatic head injury. Which of the following findings should the nurse report to the provider immediately?
Explanation
The nurse should report sudden sleepiness to the provider immediately if the client has a traumatic head injury. Sudden sleepiness can indicate an increase in intracranial pressure, which can be a life-threatening complication of a head injury.
Headache, diplopia, and slight ataxia are also important findings that the nurse should report to the provider. However, these findings are not as urgent as sudden sleepiness. Headache can be a common symptom following a head injury. Diplopia is double vision and can indicate cranial nerve damage. Slight ataxia is unsteadiness or lack of coordination and can indicate neurological damage.
A nurse is collecting data from a client who has a score of 8 using the Glasgow Coma Scale. Which of the following findings should the nurse expect?
Explanation
The Glasgow Coma Scale (GCS) is a clinical scale used to reliably measure a person's level of consciousness after a brain injury³. The GCS assesses a person based on their ability to perform eye movements, speak, and move their body³. A score of & on the GCS indicates that the client is in a deep coma.
a. The client requiring total nursing care is not necessarily indicated by a score of & on the GCS.
b. The client having a stable neurological status is not necessarily indicated by a score of & on the GCS.
c. The client being alert and oriented is not indicated by a score of & on the GCS.
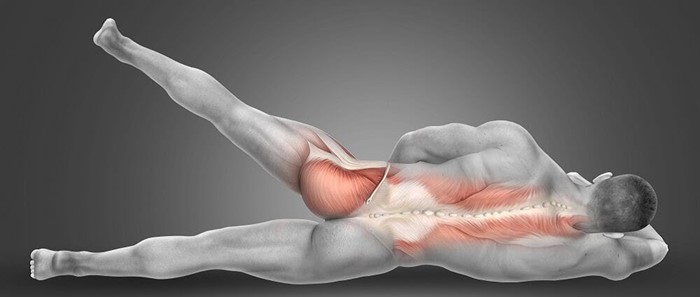
A nurse is caring for a client who is 2 days postoperative following an above-the-knee amputation. Which of the following is an appropriate nursing intervention for the client at this time?
Explanation
Having the client lie prone several times each day is an appropriate nursing intervention for a client who is 2 days postoperative following an above-the-knee amputation. Lying prone can help prevent hip flexion contractures, which can occur after an above-the-knee amputation².
a. Elevating the foot of the bed is not an appropriate intervention for a client who is 2 days postoperative following an above-the-knee amputation.
b. Encouraging sitting up as much as possible is not an appropriate intervention for a client who is 2 days postoperative following an above-the-knee amputation.
c. Elevating the stump on a pillow is not an appropriate intervention for a client who is 2 days postoperative following an above-the-knee amputation.
A nurse is caring for a client who sustained a basal skull fracture. When performing morning hygiene care, the nurse notices a thin stream of clear drainage coming from out of the client's right nostril. Which of the following actions should the nurse take first?
Explanation
The first action the nurse should take is to test the drainage for glucose. Clear drainage from the nose following a basal skull fracture could indicate a cerebrospinal fluid (CSF) leak. CSF contains glucose, so testing the drainage for glucose can help determine if it is CSF.
b. Taking the client's temperature is not the first action the nurse should take.
c. Notifying the charge nurse is important but not the first action the nurse should take.
d. Placing a dressing under the client's nose is not the first action the nurse should take.
A nurse is assisting with caring for a client who has a new concussion following a motor-vehicle crash. The nurse should monitor the client for which of the following manifestations of increased intracranial pressure?
Explanation
The nurse should monitor the client for lethargy as a manifestation of increased intracranial pressure. Increased intracranial pressure (ICP) is a rise in pressure around the brain that can occur due to various reasons such as brain injury, bleeding into the brain, swelling in the brain, or an increase in cerebrospinal fluid. Lethargy (feeling less alert than usual) is a common symptom of increased ICP.
a. Nuchal rigidity is not a common symptom of increased ICP.
b. Batle's sign is not a common symptom of increased ICP.
c. Polyuria is not a common symptom of increased ICP.

A nurse is discussing skeletal and skin traction with a newly licensed nurse. Which of the following statements should the nurse identify as an indication that the newly licensed nurse understands these therapies?
Explanation
The statement that clients in skin traction have more mobility than those in skeletal traction indicates that the newly licensed nurse understands these therapies. Skin traction is applied directly to the skin using splints, bandages, or adhesive tapes and is less invasive than skeletal traction³. Skeletal traction involves placing a pin, wire, or screw in the fractured bone and ataching weights to it to pull the bone into the correct position¹. Because skin traction is less invasive and does not involve inserting a pin into the bone, clients in skin traction have more mobility than those in skeletal traction.
a. Skeletal traction being beter than skin traction for reducing a fracture is not necessarily true.
c. Skeletal traction having less risk for infection than skin traction is not true.
d. Clients in skin traction having more discomfort than those in skeletal traction is not necessarily true.
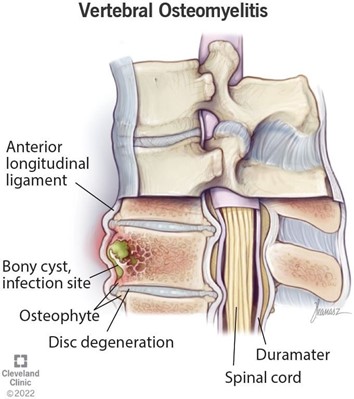
A nurse is assisting with the care of a newly-admited client who has acute osteomyelitis. Which of the following interventions is the priority for the nurse to implement?
Explanation
The priority intervention for the nurse to implement for a newly-admitted client who has acute osteomyelitis is antibiotic therapy. Osteomyelitis is an inflammatory condition of bone secondary to an infectious process¹. Antibiotics are the primary treatment option and should be tailored based on culture results and individual patient factors.
a. Optimal nutrition and hydration is important but not the priority intervention.
b. Surgical debridement of necrotic tissue may be necessary but is not the priority intervention.
d. Antipyretic therapy may be necessary but is not the priority intervention.
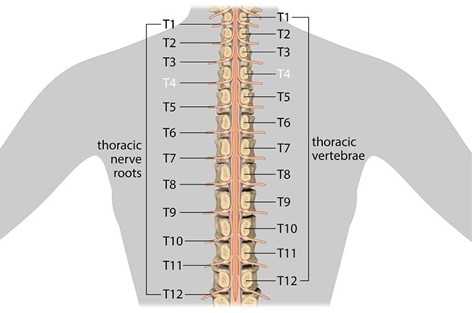
A nurse is caring for a client who has a spinal cord injury at T-4. The nurse should recognize that the client is at risk for autonomic dysreflexia. Which of the following interventions should the nurse take to prevent autonomic dysreflexia?
Explanation
To prevent autonomic dysreflexia, the nurse should take the intervention of preventing bladder distention. Autonomic dysreflexia is a serious medical problem that can happen if a person has injured the spinal cord in their upper back¹. It makes their blood pressure dangerously high and can lead to a stroke, seizure, or cardiac arrest¹. One way to lower the chance of complications is to use the bathroom on a regular schedule and keep the bladder and bowels from becoming too full.
a. Monitoring for elevated blood pressure is important but not an intervention to prevent autonomic dysreflexia.
b. Providing analgesia for headaches is important but not an intervention to prevent autonomic dysreflexia.
d. Elevating the client's head is important but not an intervention to prevent autonomic dysreflexia.
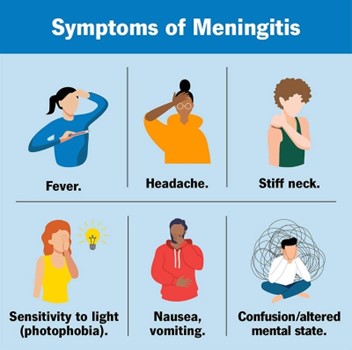
A nurse at a community health clinic is caring for a client who reports a headache and stiff neck. Which of the following actions should the nurse perform first?
Explanation
The first action the nurse should perform is to check the client's temperature. A headache and stiff neck can be symptoms of meningitis, which is an inflammation of the membranes surrounding the brain and spinal cord. Meningitis can be caused by a bacterial or viral infection and is often accompanied by a fever. Checking the client's temperature can help determine if the client has a fever and if further evaluation for meningitis is necessary.
a. Obtaining a throat culture specimen is not the first action the nurse should take.
b. Performing a complete blood count is not the first action the nurse should take.
d. Administering an oral analgesic is not the first action the nurse should take.
A nurse is caring for a client who has osteoporosis and is taking calcium carbonate. The nurse should monitor the client for which of the following adverse effects?
Explanation
The nurse should monitor the client for flank pain as an adverse effect of taking calcium carbonate. Calcium carbonate is a calcium supplement used to prevent or treat a calcium deficiency¹. One of the side effects of calcium carbonate is the formation of kidney stones, which can cause flank pain².
a. Urinary retention is not a common adverse effect of calcium carbonate.
b. Tinnitus is not a common adverse effect of calcium carbonate.
d. Bradycardia is not a common adverse effect of calcium carbonate.
Sign Up or Login to view all the 47 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

