Ati lpn fundamentals exam
Total Questions : 39
Showing 25 questions, Sign in for moreA nurse is caring for a client with pneumonia whose oxygen saturation is 88%. Which of the following actions should the nurse take first?
Explanation
Choice A reason: Initiating humidification therapy can be beneficial for a client with pneumonia. Humidified air can help loosen respiratory secretions, making them easier to expectorate. However, while this intervention is helpful, it is not typically the first action a nurse should take. The priority is to address the client's immediate need for adequate oxygenation and ventilation.
Choice B reason: Encouraging the client to cough and perform deep breathing exercises is an essential part of care for patients with pneumonia. These actions help to clear mucus from the lungs and improve ventilation. Deep breathing helps to fully expand the alveoli, which can be compromised in pneumonia, and coughing helps to expel secretions that may be blocking the airways. However, this is not the most immediate action when the oxygen saturation is borderline normal.
Choice C reason: Increasing the client's oral fluid intake is important in the management of pneumonia. Adequate hydration thins respiratory secretions, making them easier to clear. It also supports overall bodily functions, which can be taxed during illness. Nonetheless, this intervention is not the most critical initial step in managing a client's immediate respiratory needs.
Choice D reason: Raising the head of the bed is the correct and immediate action to take for a client with pneumonia and an oxygen saturation of 88%. This position helps to improve chest expansion, promotes better lung aeration, and facilitates easier breathing. It also reduces the risk of aspiration, which is particularly important in clients with pneumonia. Elevating the head of the bed is a simple yet effective way to enhance oxygenation and should be the first step taken.

A client reports difficulty sleeping through the night since being admitted three days ago. Which of the following factors is most likely to disrupt the patient's sleep patterns?
Explanation
Choice A reason: Moderate fatigue typically encourages sleep as the body naturally seeks rest to recover. However, if fatigue is excessive, it might lead to an overtired state where the patient finds it difficult to relax and fall asleep. Normal ranges of physical activity and resulting fatigue can actually promote better sleep patterns by helping to regulate the body's natural sleep-wake cycle.
Choice B reason: The ability to talk about the day's events can be therapeutic and help in reducing stress levels. It allows the patient to process emotions and experiences, potentially leading to a calmer state of mind which is conducive to sleep. This is particularly true if the conversation is positive or neutral rather than rehashing stressful or traumatic events.
Choice C reason: The presence of pain is a significant factor that can disrupt sleep. Pain can make it difficult for a person to find a comfortable position for sleep, and it can cause frequent awakenings or prevent the patient from falling asleep altogether. Pain management should be a priority in patient care, especially at night, to facilitate better sleep. For instance, arthritis pain can be particularly disruptive due to joint discomfort, and addressing this with appropriate pain relief can greatly improve sleep quality.
Choice D reason: While unfamiliar stimuli can disrupt sleep, their absence is not typically a factor that would negatively affect sleep patterns. In fact, a lack of unfamiliar stimuli, meaning a quiet and consistent environment, is generally beneficial for sleep as it reduces the chances of disturbances.
A patient has a high temperature. The nurse assesses the patient and notes that the skin is flushed and very warm. The patient is oriented to person, place, time, and situation, and reports severe fatigue. The most appropriate nursing action at this time would be to:
Explanation
Choice A reason: When a patient has an elevated temperature, the body is attempting to cool down through vasodilation, which is why the skin may appear flushed and feel warm. Removing excess blankets can help facilitate the body's natural cooling process. Offering fluids is also crucial as fever can lead to dehydration, especially if there is sweating. Adequate hydration helps regulate body temperature and replaces fluids lost through sweating. The normal body temperature range is typically between 36.5°C to 37.5°C (97.7°F to 99.5°F). When the body temperature rises above this range, interventions such as removing blankets and providing fluids can be effective in reducing fever.
Choice B reason: Increasing the patient's activity is not advisable when they have an elevated temperature and are experiencing severe fatigue. Activity generates heat and can raise body temperature further, exacerbating the fever. Rest is recommended to conserve energy and reduce metabolic demand, which can help lower the body temperature.
Choice C reason: The use of ice bags can be a rapid cooling measure but must be used with caution. Direct application of ice to the skin can cause vasoconstriction and shivering, which can actually increase the body's core temperature. It is generally reserved for hyperthermia or heatstroke when immediate cooling is necessary. For a simple fever, less aggressive cooling measures are usually preferred.
Choice D reason: Decreasing the patient's intake is not appropriate unless there is a specific contraindication, such as vomiting or risk of aspiration. Adequate nutrition supports the immune system and provides the energy needed for the body to combat the underlying cause of the fever.
A nurse is caring for a client who reports escalating anxiety, along with difficulty sleeping and concentrating. Which of the following is an appropriate response from the nurse?
Explanation
Choice A reason: This response demonstrates empathy and active listening. It acknowledges the client's feelings without judgment and opens the door for further discussion about their concerns. It is a therapeutic communication technique that helps build rapport and trust between the nurse and the client. When a client feels understood, it can reduce their anxiety and promote a sense of safety, which may improve their ability to sleep and concentrate.
Choice B reason: While it is important for clients to communicate with their healthcare providers, this response might make the client feel dismissed or that their immediate concerns are not being addressed by the nurse. It could be perceived as deflecting the responsibility to someone else, rather than the nurse providing support at that moment.
Choice C reason: Asking the client to self-reflect on the reasons for their anxiety could be helpful, but it might also be overwhelming for them if they are already in a heightened state of anxiety. This question should be asked with caution and at an appropriate time when the client is more likely to engage in productive self-reflection.
Choice D reason: This statement minimizes the client's experience by suggesting that their problem is common and insignificant. It fails to acknowledge the severity of the client's distress and does not offer any comfort or assistance. It is not a therapeutic response because it does not validate the client's feelings or encourage further communication.
When a nurse records an unusually low blood pressure for a client who typically has elevated readings, she considers the possibility of a technique issue. Which of the following sources of error should she consider as a potential cause of the low reading?
Explanation
Choice A reason: Wrapping the cuff too loosely can lead to inaccurately low blood pressure readings. The cuff must be snug but not too tight, ensuring that it can fully compress the artery. A loose cuff fails to provide the necessary pressure, resulting in a reading that does not accurately reflect the client's blood pressure.
Choice B reason: Measuring blood pressure right after a meal can sometimes affect the reading, but it typically does not cause a low reading. Postprandial hypotension, a drop in blood pressure after eating, is more common in older adults and those with certain health conditions, but it is not a widespread cause of low readings in the general population.
Choice C reason: Positioning the client's arm above heart level can actually result in a reading that is falsely low. The heart level is the reference point for accurate blood pressure measurement because it is the level of the right atrium, where central venous pressure is measured.
Choice D reason: Deflating the cuff too slowly can lead to inaccuracies, but it typically results in a higher diastolic reading, not a lower overall reading. A slow deflation rate can cause the nurse to miss the first Korotkoff sounds, which indicate the systolic pressure.
A nurse is assessing the apical pulse of a client who is on multiple cardiovascular medications. Which of the following actions should the nurse take?
Explanation
Choice A reason: The diaphragm of the stethoscope is used for high-pitched sounds such as breath sounds, bowel, and normal heart sounds. For the apical pulse, which involves listening to the heart's sounds, the bell of the stethoscope is often recommended, especially for lower-pitched sounds like murmurs.
Choice B reason: Counting the apical pulsations for a full minute is the correct action when assessing the apical pulse, particularly for clients on cardiovascular medications. This ensures accuracy in detecting any irregularities or changes in the heart rate that could be affected by the medications.
Choice C reason: The stethoscope should be placed gently against the client's skin. Pressing too firmly can distort the heart sounds, making it difficult to accurately assess the apical pulse.
Choice D reason: A Doppler device is not typically used for routine assessment of the apical pulse. It is more commonly used when pulses are difficult to palpate or auscultate, such as in cases of peripheral arterial disease.
A nurse is gathering information from a client with insomnia. The nurse needs to determine which of the following is most likely to interfere with sleep.
Explanation
Choice A reason: Regular morning exercise can actually promote better sleep. It helps to regulate the body's clock and can lead to deeper, more restful sleep. However, exercising too close to bedtime may have the opposite effect.
Choice B reason: Going to bed at the same time every evening can help establish a consistent sleep-wake cycle, which is beneficial for people who have insomnia. This regularity can make it easier to fall asleep and wake up naturally.
Choice C reason: Alcohol consumption before bedtime can disrupt sleep patterns. While it may initially help someone fall asleep, it often leads to poorer quality of sleep and can cause awakenings throughout the night.
Choice D reason: If unable to sleep, getting out of bed can be a good strategy. It's part of stimulus control therapy for insomnia, which advises leaving the bed if you can't sleep, so you don't associate the bed with wakefulness.
A nurse is emphasizing hand hygiene with a group of assistive personnel (AP). Which of the following statements from an AP should indicate to the nurse that additional instruction is needed?
Explanation
Choice A reason: Not wearing artificial nails during client care is a recommended practice to prevent the spread of infection, as artificial nails can harbor bacteria.
Choice B reason: Washing hands when they are visibly dirty is correct, but hand hygiene should also be performed at other times, such as before and after patient contact, regardless of the appearance of cleanliness.
Choice C reason: Changing gloves is not a substitute for hand washing. Hand hygiene is necessary before donning gloves and after removing them to prevent the transmission of pathogens.
Choice D reason: Using alcohol-based hand products is a standard practice in healthcare settings and is effective in killing most bacteria and viruses when the hands are not visibly soiled.
After completing a care procedure for a client in isolation, which piece of personal protective equipment (PPE) should the nurse take off last?
Explanation
Choice A reason: Gloves are typically removed first because they are likely to be the most contaminated. They should be removed carefully to avoid contaminating the hands, using the glove-in-glove or beak method.
Choice B reason: The gown should be removed after the gloves because it may also be contaminated. The nurse should reach up to the shoulders and carefully pull the gown forward and away from the body, touching only the inside of the gown.
Choice C reason: Eyewear is removed after the gown. The nurse should handle the eyewear by the arms, avoiding touching the front part that has been exposed to contaminants.
Choice D reason: The mask should be removed last because it protects the mucous membranes of the mouth and nose from infectious droplets. It should be taken off by handling the ties or elastic bands from behind the head and pulling it away from the face without touching the front of the mask.
While changing a client's wound dressing, the nurse should identify which of the following signs as an indication of a wound infection?
Explanation
Choice A reason: Edema, or swelling, can be a normal response to injury as part of the inflammatory process. However, it can also be a sign of infection, especially if it is excessive or increasing. In the context of wound healing, edema should decrease over time, and persistent or worsening edema may suggest an infection.
Choice B reason: Petechiae are small, pinpoint, red spots that are not usually associated with wound infections. They are more commonly related to blood or vascular disorders, allergic reactions, or causes of increased venous pressure.
Choice C reason: Urticaria, also known as hives, is typically a sign of an allergic reaction and not an infection. It presents as raised, itchy welts on the skin and is usually related to an immune response to a substance or allergen, rather than an infectious process.
Choice D reason: Crusting over granulated tissue can indicate a wound infection. Granulation tissue is new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process. It is normally red or pink and does not have a crust. If a crust forms over it, especially if it is yellow or green, it may be composed of dried pus and is a sign of infection.

While caring for a group of clients, for which tasks should the nurse plan to use protective eye equipment? (Select all that apply)
Explanation
Choice A reason: While providing a newborn's first bath, there is minimal risk of exposure to infectious fluids that would necessitate eye protection. However, standard precautions should always be followed.
Choice B reason: When giving personal care to an infant who is HIV-positive, standard precautions should be followed, which includes wearing gloves. Eye protection is not typically required unless there is a risk of splashing bodily fluids.
Choice C reason: Suctioning secretions from a child's newly placed tracheostomy tube requires eye protection because there is a high risk of secretions being expelled forcefully, which could contact the mucous membranes of the eyes.
Choice D reason: Withdrawing cord blood from a neonate generally does not require eye protection unless there is a risk of blood splatter. Standard precautions, including the use of gloves, should be sufficient.
Choice E reason: Transporting a cerebrospinal fluid specimen to the laboratory does not require the nurse to wear eye protection. However, the nurse should ensure that the specimen is sealed properly to prevent any leaks.
For a client with obstructive sleep apnea (OSA), the nurse should anticipate the following findings:
Explanation
Choice A reason: Decreased energy is a common symptom of OSA due to disrupted sleep patterns and the body's struggle to maintain adequate oxygen levels during apneic episodes. This can lead to excessive daytime sleepiness and fatigue.
Choice B reason: While thyroid disease can be associated with sleep disorders, it is not a direct finding of OSA. However, hypothyroidism can contribute to the development of OSA due to myxedematous changes leading to airway obstruction.
Choice C reason: Pneumonia is not a direct finding of OSA. However, individuals with OSA may be at increased risk for respiratory infections due to repeated episodes of upper airway collapse during sleep, which can lead to aspiration.
Choice D reason: Hypotension is generally not associated with OSA. In fact, OSA is more commonly linked with hypertension due to the sympathetic nervous system activation that occurs with each apneic episode.
When evaluating a client's abdomen, especially for "stomach pain," the nurse should:
Explanation
Choice A reason: Inspection should be performed first to observe for any visible abnormalities, distention, or movements that could indicate underlying conditions.
Choice B reason: Percussion is used after auscultation to assess the presence of fluid, gas, and to estimate the size of the organs within the abdomen.
Choice C reason: Palpation is typically performed last because it can alter the natural state of the abdomen, potentially causing discomfort and affecting the bowel sounds that are assessed during auscultation.
Choice D reason: Auscultation should be performed before palpation and percussion to avoid altering bowel sounds. It allows the nurse to listen to the natural state of bowel motility and vascular sounds without interference.
A nurse is reviewing the use of personal protective equipment (PPE) with an assistive personnel (AP) during client care. Which of the following statements should indicate to the nurse that the AP comprehends the instructions?
Explanation
Choice A reason: Wearing gloves when measuring a client's blood pressure is not typically necessary unless there is a risk of exposure to bodily fluids or if the client has an infectious disease. The use of gloves is based on the type of contact and potential for exposure, not routine tasks like BP measurement.
Choice B reason: Wearing gloves for all client contact is not necessary and is not consistent with standard precautions. Gloves should be used when there is potential contact with blood, body fluids, secretions, excretions, contaminated items, or mucous membranes.
Choice C reason: Gloves are not a substitute for hand hygiene. The primary reason for wearing gloves is to provide a barrier against infection, not to reduce handwashing. Hand hygiene is still required before donning gloves and after removing them, regardless of whether the gloves are soiled or not.
Choice D reason: Wearing gloves and a gown when bathing a client with open skin lesions is correct because it protects both the healthcare worker and the client from the risk of infection. Open skin lesions can be a source of infection, and PPE is necessary to prevent the transmission of pathogens.
For a client who reports pain, the nurse should regard the following as the most dependable indicator of pain:
Explanation
Choice A reason: The severity of the condition may not always correlate with the level of pain experienced by the client. Pain is a subjective experience, and two individuals with the same condition may report different levels of pain.
Choice B reason: Vital signs can be indicators of pain but are not always reliable. For example, some clients may exhibit increased heart rate or blood pressure when in pain, while others may not show significant changes in vital signs despite severe pain.
Choice C reason: Nonverbal behavior can be an indicator of pain, especially in clients who are unable to communicate verbally. However, it is still considered less reliable than self-report because it is subject to interpretation by the observer.
Choice D reason: Self-report of pain is considered the most reliable indicator of a patient's pain experience. It is a direct expression of the client's experience and should be the primary source of assessment whenever possible.
For documenting vital signs, the following entries made by the nurse demonstrate an understanding of the teaching:
Explanation
Choice A reason: This documentation is correct as it includes the pulse rate and the client's position when the measurement was taken, which can affect the reading.
Choice B reason: The temperature is documented with the correct unit of measurement, but it does not specify the method of measurement (oral, axillary, tympanic, etc.), which is important for accurate interpretation.
Choice C reason: Respirations should be observed, not auscultated, and the documentation should include the client's position. The term 'even' is unnecessary and could be confusing.
Choice D reason: The blood pressure reading is correctly documented with both systolic and diastolic values. However, it should also include the client's position and the arm in which the measurement was taken for clarity.
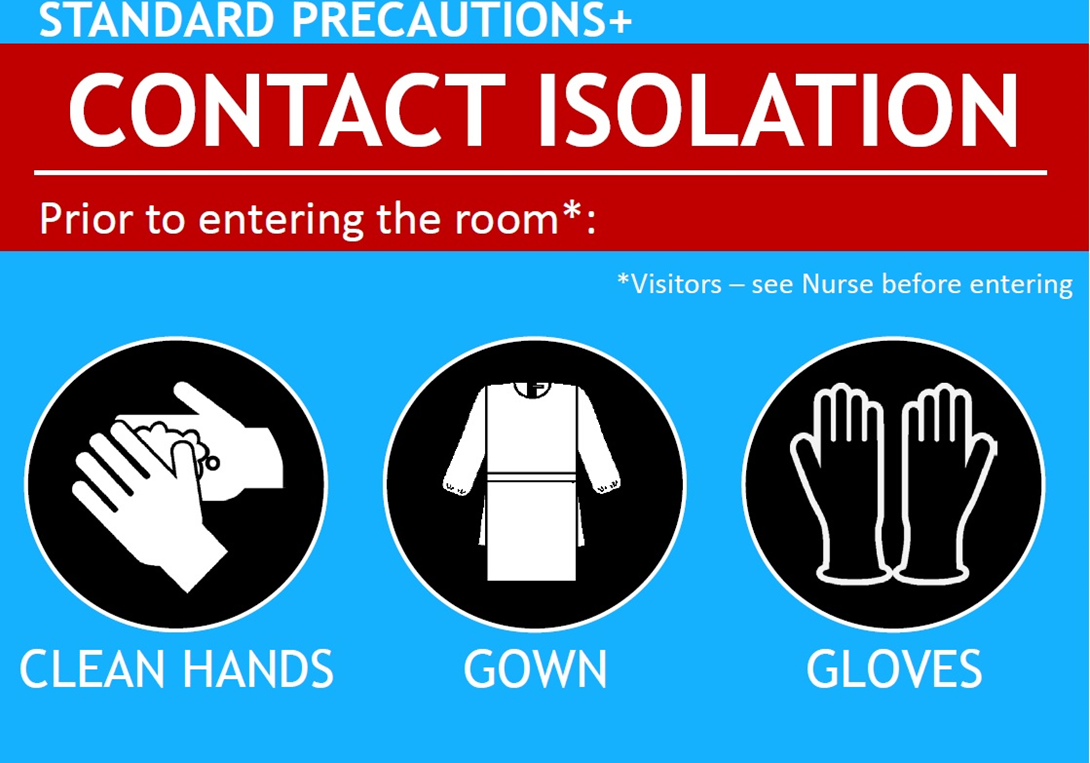
A nurse is caring for a client with a wound infection caused by vancomycin-resistant Enterococcus (VRE). What type of precautions should the nurse plan to use while caring for this client?
Explanation
Choice A reason: Airborne precautions are used for diseases that are spread through the air over long distances, such as tuberculosis, measles, or chickenpox. VRE is not typically spread through the air.
Choice B reason: Droplet precautions are used for diseases that are spread through large droplets in the air, such as influenza or pertussis. VRE is not spread through droplets but through contact with contaminated surfaces or equipment.
Choice C reason: A protective environment is designed to protect immunocompromised patients from infection and is not typically used for patients with VRE. This type of precaution includes the use of HEPA filters, laminar air flow, and other strategies to maintain a sterile environment.
Choice D reason: Contact precautions are the appropriate measures for a patient with a VRE infection. VRE can be spread from one person to another through contact with contaminated surfaces or equipment or through person-to-person spread, often via contaminated hands. It is not spread through the air by coughing or sneezing. Therefore, contact precautions, including the use of gloves and gowns, are necessary when caring for patients with VRE to prevent the spread of the bacteria.
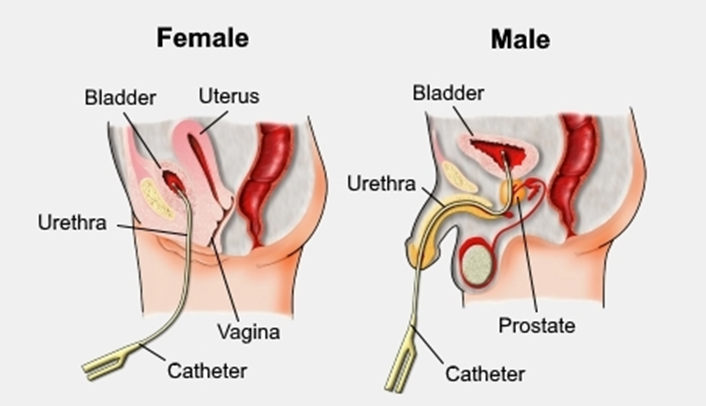
A nurse is preparing an in-service presentation on preventing healthcare-associated infections (HAIs). Which of the following should the nurse include as a common cause of these infections?
Explanation
Choice A reason: Urinary catheterization is a well-known risk factor for HAIs, particularly catheter-associated urinary tract infections (CAUTIs). The use of indwelling urinary catheters can introduce bacteria into the urinary tract and is associated with a significant proportion of HAIs.
Choice B reason: While malnutrition can affect the immune system and increase the risk of infections, it is not a direct cause of HAIs. Good nutritional status is important for wound healing and infection prevention, but it does not cause HAIs by itself.
Choice C reason: Having multiple caregivers can increase the risk of transmitting infections, especially if hand hygiene and other infection control practices are not consistently followed. However, it is not considered a direct cause of HAIs like urinary catheterization is.
Choice D reason: Chlorhexidine washes are actually used as a preventive measure against HAIs, particularly in reducing the risk of surgical site infections. They are not a cause of HAIs but rather part of the solution to prevent them.
A nurse is reviewing healthful sleep habits with a client. Which of the following statements should the nurse recognize as a sign that the client requires additional instruction?
Explanation
Choice A reason: Going to bed and waking up at the same times each day is a recommended practice for good sleep hygiene. It helps to regulate the body's internal clock and can improve sleep quality.
Choice B reason: Watching television until falling asleep is not recommended for healthful sleep habits. The light emitted from screens can interfere with the body's production of melatonin, the hormone that regulates sleep, and can make it more difficult to fall asleep.
Choice C reason: Avoiding naps, especially in the afternoon or evening, can help ensure that a person is sufficiently tired at bedtime, which can improve the ability to fall asleep and maintain sleep throughout the night.
Choice D reason: Having a small snack and taking a bath before bed can be part of a relaxing bedtime routine. A light snack can prevent hunger from disrupting sleep, and a warm bath can help to relax the body and signal that it's time to wind down.
A nurse inserts an indwelling urinary catheter for a preoperative client. Three days later, the client develops a urinary tract infection. The nurse should determine that the client has which type of infection?
Explanation
Choice A reason: A systemic infection would affect the entire body or multiple systems, not just the urinary tract. While a urinary tract infection can become systemic if it leads to sepsis, the scenario provided does not specify such progression.
Choice B reason: A health care-associated infection (HAI) is an infection that a patient acquires while receiving treatment for another condition within a healthcare setting. Since the infection occurred after the insertion of a urinary catheter in a hospital, it is considered an HAI.
Choice C reason: An endogenous infection originates from the host's own microbial flora. The scenario does not provide enough information to determine if the infection was caused by the client's own flora or by external sources.
Choice D reason: An exogenous infection comes from outside the body. While the urinary tract infection could be exogenous, the scenario suggests it is more likely to be health care-associated due to the timing and context of the catheter insertion.
A nurse accidentally punctures his finger with a needle used for an IM injection on a client. What action should the nurse take?
Explanation
Choice A reason: The first step after a needlestick injury is to wash the wound with soap and water to reduce the risk of infection. This helps to remove any pathogens that may have been introduced into the puncture site.
Choice B reason: Squeezing the puncture site is not recommended because it can cause further injury to the tissue and does not effectively reduce the risk of bloodborne pathogen transmission.
Choice C reason: Flushing the puncture site with water is a good practice, but it should be done immediately, not just for 5 minutes. The initial washing is more critical.
Choice D reason: Postexposure prophylaxis (PEP) should be started as soon as possible, ideally within hours and no later than 72 hours after potential exposure to HIV. Waiting until the following day could decrease the effectiveness of PEP.
A nurse is caring for a postoperative client. What action should the nurse take to help prevent an incisional infection?
Explanation
Choice A reason: Cleaning the incision with soap and water is not typically recommended as it can disrupt the healing process and may lead to irritation or infection. The incision should be kept clean and dry, and any cleaning should be done according to the surgeon's instructions.
Choice B reason: Performing hand hygiene before dressing changes is essential in preventing incisional infections. Hand hygiene is one of the most effective ways to prevent the spread of infections, including those at surgical sites.
Choice C reason: Protective isolation is used for immunocompromised patients to protect them from infections, not typically for postoperative patients unless they are at high risk for infection due to other conditions.
Choice D reason: Allowing the wound to air can be part of the healing process, but it must be done carefully and under the guidance of healthcare professionals to ensure that the wound is protected from contamination.
A nurse is gathering information about a client's circulatory system. Which of the following pulse sites should the nurse avoid checking on both sides simultaneously?
Explanation
Choice A reason: The first and immediate action after a needlestick injury is to wash the puncture site with soap and water. This helps to remove any pathogens that may have been introduced into the puncture site.
Choice B reason: Squeezing the puncture site is not recommended because it can cause further injury to the tissue and does not effectively reduce the risk of bloodborne pathogen transmission.
Choice C reason: Flushing the puncture site with water is a good practice, but it should be done immediately, not just for 5 minutes. The initial washing is more critical.
Choice D reason: Postexposure prophylaxis (PEP) should be started as soon as possible, ideally within hours and no later than 72 hours after potential exposure to HIV. Waiting until the following day could decrease the effectiveness of PEP.
A nurse is helping with the admission of a client who has meningococcal pneumonia. Which isolation precautions should the nurse implement?
Explanation
Choice A reason: Protective precautions are used to shield immunocompromised patients from infections, not typically for patients with meningococcal pneumonia.
Choice B reason: Contact precautions are used for infections that are spread by direct contact with the patient or the patient's environment. Meningococcal pneumonia is not primarily spread this way.
Choice C reason: Airborne precautions are for diseases that are spread through the air over long distances, such as tuberculosis. Meningococcal pneumonia is not spread in this manner.
Choice D reason: Droplet precautions are recommended for meningococcal pneumonia. This infection can be spread through droplets from the respiratory tract when the infected person coughs or sneezes. Therefore, droplet precautions, including the use of masks, are necessary to prevent the spread of this infection.
Before taking the health history, what should the nurse do first?
Explanation
Choice A reason: Offering a beverage is a hospitable gesture but not the first step in taking a health history. The priority is to establish communication and trust.
Choice B reason: Confirming insurance coverage is important but not the initial step in the health history process. The focus should first be on the patient's immediate needs and concerns.
Choice C reason: Establishing a rapport with the patient is the first and most crucial step in taking a health history. It involves creating a comfortable and trusting environment for the patient to share personal health information.
Choice D reason: Asking the patient to disrobe and put on a gown may be necessary for a physical examination but is not the first step in taking a health history. The nurse should first establish a rapport with the patient.
Sign Up or Login to view all the 39 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

