Ati Lpn maternal exam 1
Total Questions : 49
Showing 25 questions, Sign in for moreA nurse in the antepartum unit is assisting with the care of a client who is at 36 weeks of gestation and reports continuous abdominal pain and vaginal bleeding.
The nurse should identify that the client is likely experiencing which of the following complications?
Explanation
Choice A rationale:
Prolapsed cord is a serious obstetric emergency that occurs when the umbilical cord descends into the vagina ahead of the baby. It typically happens after the rupture of membranes, not before.
Key signs of a prolapsed cord include:
A visible or palpable cord in the vagina Sudden fetal heart rate decelerations
Vaginal bleeding (may or may not be present)
The client in this scenario does not present with these characteristic signs, making prolapsed cord less likely.
Choice B rationale:
Premature rupture of membranes (PROM) refers to the breaking of the amniotic sac before the onset of labor. It can lead to vaginal leaking of clear or straw-colored fluid, but not typically continuous bleeding.
While PROM is possible, the presence of continuous abdominal pain makes abruptio placentae more likely.
Choice C rationale:
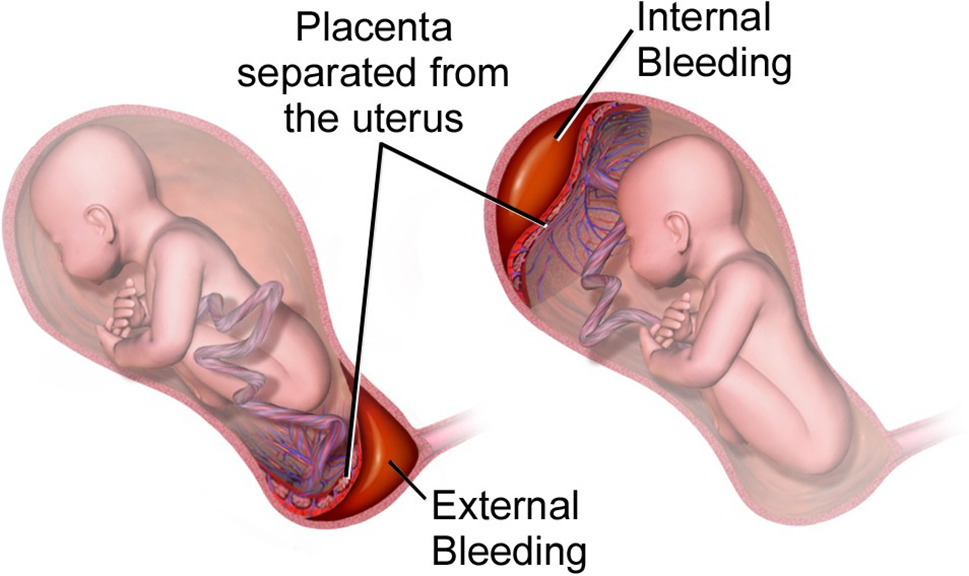
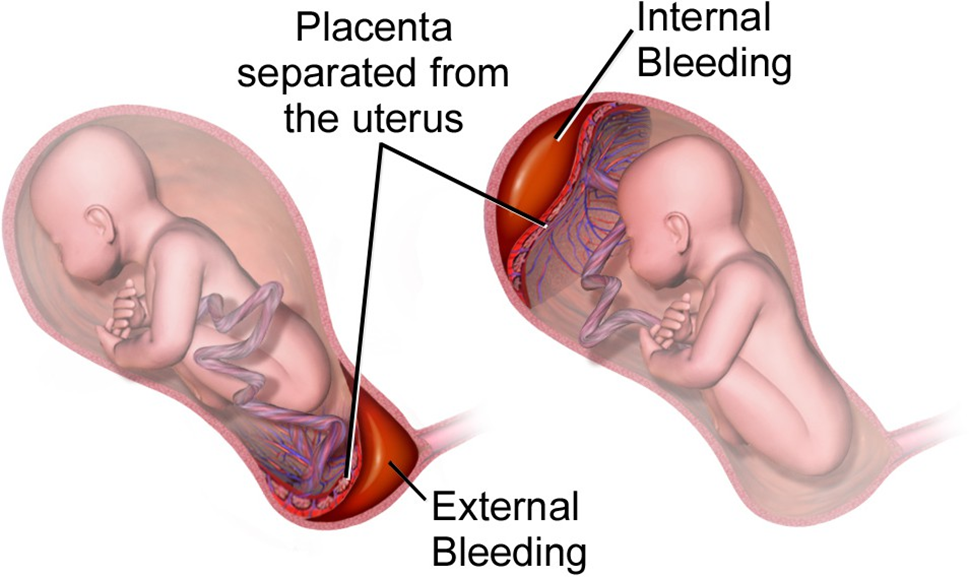
Abruptio placentae is the premature separation of the placenta from the uterine wall, a serious condition that can endanger both the mother and the fetus.
It often presents with the following symptoms: Sudden onset of severe abdominal pain
Vaginal bleeding (may be bright red or dark brown) Uterine tenderness
Fetal distress (indicated by abnormal heart rate patterns)
The client in this scenario exhibits the classic signs of abruptio placentae, making it the most likely diagnosis.
A nurse should include which of the following information?
Explanation
Rationale for Choice A:
Quickening does not start soon after implantation. Implantation typically occurs 6-12 days after ovulation, while quickening is usually first felt between 16-22 weeks of gestation.
During implantation, the embryo is still very small and developing, and its movements are not yet strong enough to be felt by the mother.
It's important to clarify this misconception to ensure pregnant women have accurate expectations about the timeline of fetal development and sensations.
Rationale for Choice B:
Quickening is the term used to describe the first time a pregnant woman feels her baby move inside her womb. It is a significant milestone in pregnancy and is often a very exciting moment for expectant mothers.
It typically occurs between the fourth and fifth months of pregnancy, which corresponds to 16-22 weeks of gestation. At this stage, the fetus is large enough and its movements are strong enough to be felt by the mother.
The initial sensations of quickening may be subtle, like flutters or butterflies, but they will become more distinct and frequent as the pregnancy progresses.
Rationale for Choice C:
Quickening does not start during the last trimester of pregnancy. By the third trimester, the fetus is much larger and its movements are much more pronounced, often visible through the abdomen.
Women typically feel quickening well before this stage.
Rationale for Choice D:
Quickening does not typically occur between the second and third month of pregnancy. While it's possible for some women to feel very early fetal movements, especially those who have been pregnant before, it's more common for quickening to be experienced around the fourth or fifth month.
A nurse is caring for a client who is pregnant in a provider’s office.
Relevant vital signs to help answer the questions are as follows: Medical History: 0830 Gravida 3 Para 2, 32 weeks of gestation, Allergies: Penicillin, Height: 163 cm, Weight: 78 kg, BMI: 30.6, 6 lb weight gain over the last 2 weeks.
The client reports “I have had a headache for 5 days, blurred vision, and dizziness. Tylenol does not relieve it.” The client reports swelling of their feet and fingers.
2+ pitting edema of the lower extremities noted bilaterally. Swelling of the fingers and hands noted.
Deep tendon reflexes 3+, absent clonus.
Fetal heart tones (FHT) 1. Which of the following findings should the nurse report to the provider? Select all that apply.
Explanation
Rationale for Choice A: Visual disturbances
Preeclampsia: Visual disturbances, such as blurred vision or seeing spots, can be a sign of preeclampsia, a serious pregnancy complication characterized by high blood pressure and protein in the urine. It typically develops after 20 weeks of gestation and can progress rapidly.
Potential complications: If left untreated, preeclampsia can lead to seizures (eclampsia), stroke, liver and kidney failure, premature birth, and even death of the mother or baby.
Prompt reporting: Early recognition and management of preeclampsia are crucial for preventing adverse outcomes. Therefore, visual disturbances should be reported to the provider immediately to initiate further assessment and potential interventions.
Rationale for Choice B: Fetal heart rate
No indication for reporting: While monitoring fetal heart rate is essential during pregnancy, the promptness of reporting it to the provider depends on specific concerns. In this case, the fetal heart tones are documented as 1, suggesting a normal rate and rhythm. There's no immediate indication for reporting it as a concerning finding.
Rationale for Choice C: Blood pressure
Hypertension: High blood pressure is a key feature of preeclampsia. Although blood pressure readings are not provided in the scenario, the nurse should measure and report them to the provider, as hypertension is a critical finding that could necessitate further evaluation and treatment.
Rationale for Choice D: Deep tendon reflexes
Hyperreflexia: The client's deep tendon reflexes are 3+, which is considered hyperreflexia. Hyperreflexia can be a neurological sign of preeclampsia, indicating increased excitability of the nervous system. It's important to report this finding to the provider for further assessment and monitoring.
A nurse is reinforcing nutrition teaching with a client during the first prenatal visit. Which of the following statements by the client indicates understanding of the teaching?
Explanation
Choice A rationale:
Consuming any amount of alcohol during pregnancy is not recommended. Alcohol can cross the placenta and harm the developing fetus, potentially leading to fetal alcohol spectrum disorders (FASDs). FASDs can cause a range of physical, mental, and behavioral problems, including intellectual disabilities, learning disabilities, and physical abnormalities. Even small amounts of alcohol can increase the risk of FASDs, and there is no known safe amount of alcohol to consume during pregnancy.
Choice B rationale:
Switching to whole milk during pregnancy can be a beneficial choice for several reasons:
Increased calcium and vitamin D: Whole milk is a rich source of calcium and vitamin D, which are essential for the development of the baby's bones, teeth, and muscles. Calcium also supports the mother's bone health and helps prevent pregnancy-related osteoporosis.
Healthy fats: Whole milk contains healthy fats that are important for fetal brain development and the mother's overall health. These fats also contribute to satiety and can help manage weight gain during pregnancy.
Essential nutrients: Whole milk provides a variety of other essential nutrients, including protein, vitamins A and B12, riboflavin, and zinc. These nutrients support overall health and well-being during pregnancy.
Choice C rationale:
Weight loss during pregnancy is generally not recommended unless specifically advised by a healthcare provider. Pregnancy is a time for growth and nourishment of the baby, and restricting calories or attempting to lose weight can potentially harm the developing fetus. It's important to focus on consuming a healthy, balanced diet and gaining a healthy amount of weight during pregnancy.
Choice D rationale:
Consuming high amounts of caffeine during pregnancy is not recommended. Caffeine can cross the placenta and potentially affect the baby's heart rate and sleep patterns. It's generally advised to limit caffeine intake to less than 200 milligrams per day during pregnancy.
A nurse is assisting with a community program to educate adolescents about contraception. After the class, a 15-year-old girl asks the nurse which method is best for her to use.
Which of the following statements is an appropriate nursing response?
Explanation
Rationale for Choice A:
Judgmental and shaming: The statement "You are so young. Are you sure you are ready for the responsibilities of a sexual relationship?" conveys judgment and may make the adolescent feel ashamed or embarrassed. This can create a barrier to open communication and discourage the teen from seeking further guidance.
Dismisses the teen's concerns: It does not directly address the teen's question about contraception, suggesting that her concerns are not valid or important.
Does not provide helpful information: It does not offer any guidance or education about contraception, leaving the teen without the information she needs to make informed decisions about her sexual health.
Rationale for Choice B:
Erects barriers to access: Requiring parental consent for an examination can delay or prevent the teen from obtaining contraception, even if she is legally allowed to do so without parental consent.
Discourages open communication: It may make the teen feel like she cannot trust the nurse or that her privacy will not be respected, leading her to withhold information or avoid seeking further help.
Rationale for Choice C:
Defers responsibility: It shifts the responsibility for providing contraception counseling to the doctor, potentially delaying the teen's access to information and services.
May not be necessary: A physical examination is not always required before prescribing contraception, and in some cases, a nurse practitioner or other qualified health professional can provide this service.
Rationale for Choice D:
Open and non-judgmental: It invites the teen to share information about her sexual activity without judgment or pressure. Gathers essential information: It allows the nurse to assess the teen's individual needs and preferences, which is crucial for recommending the most appropriate contraceptive method.
Promotes informed decision-making: It empowers the teen to make informed choices about her sexual health by providing her with accurate and comprehensive information about contraception.
A nurse is caring for a 22-year-old female client who is experiencing lower abdominal pelvic pain. The client is at risk of developing a condition due to a finding.
Explanation
Choice A rationale:
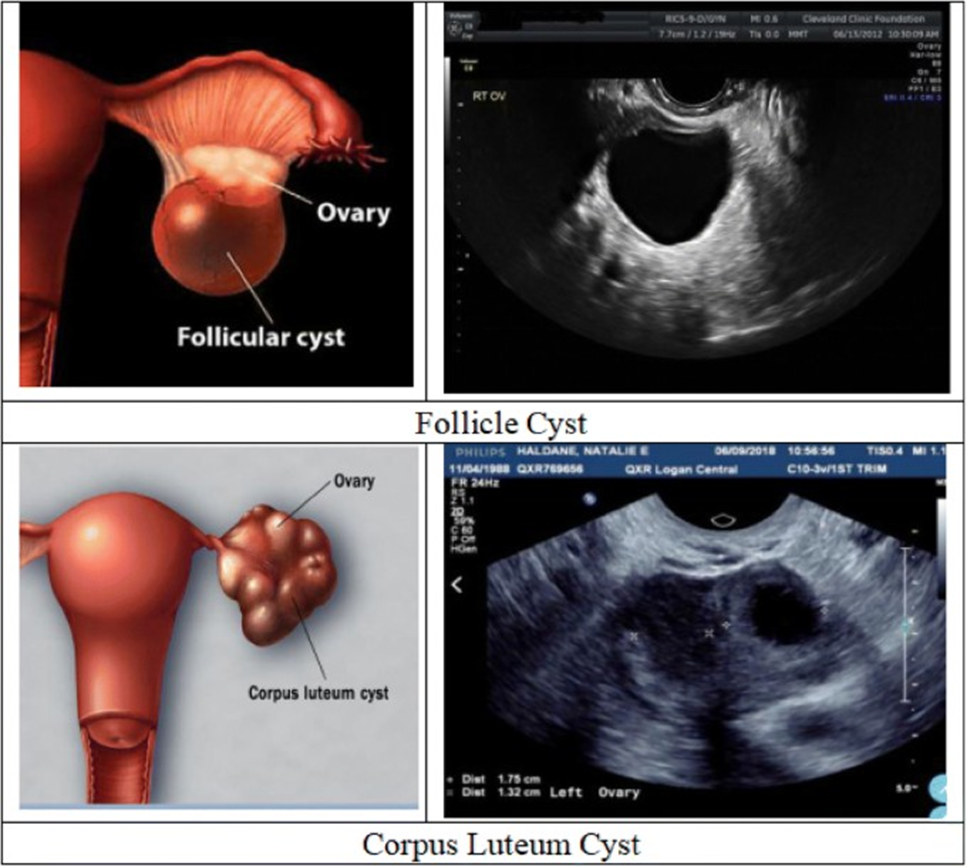
Ovarian cysts are fluid-filled sacs that form on or within an ovary. They are a common condition, affecting up to 1 in 5 women at some point in their lives. While most ovarian cysts are benign (non-cancerous), they can sometimes cause symptoms, including pelvic pain.
Ultrasound is a common imaging test that uses sound waves to create pictures of internal organs. It can be used to detect ovarian cysts, which often appear as fluid-filled sacs on the ovary.
The presence of an ovarian cyst on ultrasound, combined with the patient's symptoms of lower abdominal pelvic pain, suggests that the patient is at risk of developing complications from the cyst. These complications can include: Rupture: A ruptured ovarian cyst can cause sudden, severe pain and bleeding.
Torsion: This is when a cyst twists on its stalk, cutting off its blood supply. Torsion can also cause severe pain and may require emergency surgery.
Choice B rationale:
Appendicitis is an inflammation of the appendix, a small, finger-shaped organ located in the lower right abdomen. It is a common cause of abdominal pain, especially in young adults.
However, the patient in this scenario is experiencing pain in the lower abdominal pelvic region, not specifically in the lower right quadrant. This makes appendicitis less likely.
Additionally, the patient does not have any other symptoms that are typically associated with appendicitis, such as fever, nausea, or vomiting.
Choice C rationale:
Endometriosis is a condition in which tissue that normally lines the uterus grows outside of the uterus. It can cause pain, especially during menstruation.
However, the patient in this scenario does not report cyclical pain, which is a hallmark symptom of endometriosis. Additionally, endometriosis is not typically associated with the presence of fluid-filled sacs on the ovaries.
Choice D rationale:
Pelvic inflammatory disease (PID) is an infection of the upper genital tract, including the uterus, fallopian tubes, and ovaries. It is often caused by sexually transmitted infections (STIs).
PID can cause pelvic pain, but it is also typically associated with other symptoms, such as fever, vaginal discharge, and irregular bleeding.
The patient in this scenario does not have any of these other symptoms, and her white blood cell count is not elevated, which makes PID less likely.
A nurse is admitting a client who is at 36 weeks gestation and has pain, bright red vaginal bleeding. The nurse recognizes this finding as an indication of which of the following conditions? Choice Options:
Explanation
Choice A Rationale:
Threatened abortion is a condition characterized by vaginal bleeding during pregnancy, typically in the first 20 weeks. It does not usually involve pain or bright red bleeding.
In this case, the client is at 36 weeks gestation, which is beyond the typical timeframe for threatened abortion. Moreover, the presence of pain and bright red bleeding is more suggestive of abruptio placentae than threatened abortion.
Choice B Rationale:
Placenta previa is a condition where the placenta covers part or all of the cervix. It can cause painless, bright red vaginal bleeding, but it typically occurs in the later stages of pregnancy, often after 32 weeks.
However, pain is not a common symptom of placenta previa, and its presence in this case makes abruptio placentae more likely.
Choice C Rationale:
Preterm labor is defined as labor that starts before 37 weeks of pregnancy. It can be accompanied by vaginal bleeding, but it is often accompanied by other signs like contractions, back pain, and pressure in the pelvis.
In this scenario, the client is experiencing pain and bright red bleeding, but there is no mention of contractions or other typical symptoms of preterm labor.
Choice D Rationale:
Abruptio placentae is a serious condition in which the placenta separates from the uterine wall prematurely. It can occur at any time during pregnancy, but it is more common in the third trimester.
The classic symptoms of abruptio placentae are pain, bright red vaginal bleeding, and a rigid or tender uterus. These symptoms align with the client's presentation, making abruptio placentae the most likely diagnosis.
A nurse is teaching a client who is scheduled for a non-stress test. Which of the following information should the nurse include? Choice Options:
Explanation
Rationale for Choice A:
An IV is not routinely initiated prior to a non-stress test. It may be started if a biophysical profile (BPP), which includes an ultrasound, is also being performed, or if there is a risk of complications that may necessitate immediate intervention. However, it is not a standard part of the non-stress test itself.
Rationale for Choice B:
Nipple stimulation is not a standard component of a non-stress test. It may be used in some cases to try to induce fetal movement if the fetus is not moving actively enough during the test. However, it is not a routine part of the procedure.
Rationale for Choice C:
An ultrasound is not typically performed prior to a non-stress test. It may be done as part of a BPP, but it is not necessary for the non-stress test itself.
Rationale for Choice D:
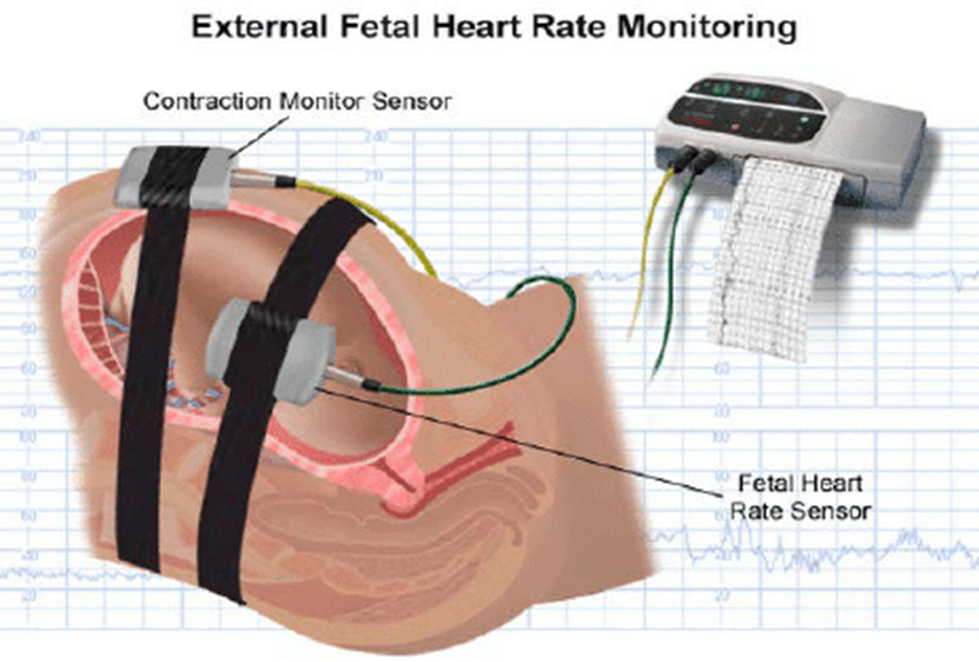
An external fetal monitor is essential for conducting a non-stress test. This monitor uses two belts that are placed around the mother's abdomen. One belt measures the fetal heart rate, and the other belt measures uterine contractions. The monitor records the fetal heart rate and any contractions for a period of 20 to 40 minutes. The test is considered reactive (normal) if the fetal heart rate increases by at least 15 beats per minute for at least 15 seconds twice during the test. This acceleration in heart rate is typically in response to fetal movement.
A nurse in a provider’s office is reinforcing teaching about home care to a client who has mild preeclampsia. Which of the following information should the nurse include in the teaching? Choice Options:
Explanation
Choice A rationale:
Fetal movement counts are a simple yet effective tool to monitor fetal well-being in women with preeclampsia. They provide valuable insights into the baby's activity level and can alert the healthcare team to potential concerns early on.
Preeclampsia can compromise placental blood flow, which can lead to decreased fetal movement. By tracking fetal movements daily, the mother can detect any significant changes or reductions in activity, prompting further assessment and intervention if necessary.
Research has shown that regular fetal movement counts can reduce the risk of stillbirth in women with preeclampsia. This is because prompt recognition of decreased fetal movements allows for timely interventions, such as closer monitoring, induction of labor, or delivery, to prevent adverse outcomes.
Daily fetal movement counts empower women to take an active role in their pregnancy care and contribute to a sense of control in a condition that can often feel unpredictable. This increased involvement can promote maternal-fetal bonding and reduce anxiety.
Choice B rationale:
While fluid restriction has been a traditional recommendation for preeclampsia, current evidence does not support limiting fluid intake to 1,000 ml/day. In fact, excessive fluid restriction can lead to dehydration, which can worsen placental perfusion and compromise fetal well-being.
It's essential for women with preeclampsia to maintain adequate hydration to support essential bodily functions and fetal growth. Adequate fluid intake also helps to prevent urinary tract infections, which are more common in women with preeclampsia.
Choice C rationale:
Although reducing sodium intake can be beneficial for overall blood pressure control, there's insufficient evidence to support a strict sodium restriction of 2,000 mg/day specifically for managing mild preeclampsia. Individual needs may vary, and a more moderate approach to sodium reduction is often recommended.
Focusing on a balanced, healthy diet with appropriate sodium intake is generally more effective than strict limitations. This approach promotes overall well-being and supports healthy blood pressure levels without compromising nutritional needs. Choice D rationale:
Rest is often recommended for women with preeclampsia to reduce stress on the cardiovascular system and promote placental blood flow. However, the supine position (lying on the back) is not ideal, as it can further compress the large blood vessels in the abdomen and potentially reduce blood flow to the placenta.
Side-lying positions, particularly the left lateral position, are preferred for women with preeclampsia. These positions help to alleviate pressure on the major blood vessels, enhance blood flow, and improve uteroplacental circulation, which benefits both the mother and the baby.
The nurse is caring for a client who might have a hydatidiform mole. The nurse should monitor the client for which of the following findings? Choice Options:
Explanation
Rationale for Choice A: Whitish vaginal discharge
While whitish vaginal discharge can occur in some cases of hydatidiform mole, it's not a specific or sensitive finding for this condition.
It can also be present in various other gynecological conditions, including normal pregnancy, infections, and hormonal imbalances.
Therefore, relying on whitish vaginal discharge alone for monitoring a potential hydatidiform mole could lead to misdiagnosis or delayed diagnosis.
Rationale for Choice B: Excessive uterine enlargement
Excessive uterine enlargement is a common sign of hydatidiform mole, but it's not always present and might not be detected early in the condition.
The uterus might not be significantly enlarged in early stages, and other factors like multiple pregnancies or uterine fibroids could also contribute to uterine enlargement.
Solely relying on uterine enlargement could miss cases of hydatidiform mole that haven't progressed to a noticeable degree.
Rationale for Choice C: Fetal heart rate irregularities
Fetal heart rate irregularities are not relevant in hydatidiform mole because there is no viable fetus present. Hydatidiform moles are characterized by abnormal growth of placental tissue without a normal fetus developing. Monitoring for fetal heart rate would be inappropriate and misleading in this context.
Rationale for Choice D: Rapidly changing hCG levels
This is the most accurate and reliable finding to monitor for in a suspected hydatidiform mole.
hCG is a hormone produced by the placenta, and it's typically elevated in pregnancy. However, in hydatidiform mole, hCG levels are often abnormally high and rise rapidly.
Serial hCG measurements can accurately detect and track the progression of a hydatidiform mole, even in its early stages. It's considered the gold standard for diagnosis and monitoring of this condition.
A nurse is reinforcing teaching with a newly licensed nurse. Which of the following complications should the nurse include?
Explanation
Choice A rationale:
Placenta previa is a condition in which the placenta covers all or part of the cervix. It's a serious complication that can cause heavy bleeding during pregnancy and childbirth. However, it's not a direct complication of maternal gestational diabetes.
Choice B rationale:
Newborn hypoglycemia is a condition in which a newborn's blood sugar levels are too low. It can occur in infants of mothers with gestational diabetes, but it's not the most common or significant complication associated with the condition.
Choice C rationale:
Oligohydramnios is a condition characterized by a low amount of amniotic fluid around the baby. It can be associated with maternal gestational diabetes, but it's not as common as other complications, such as macrosomia (large for gestational age baby).
Choice D rationale:
Small for gestational age (SGA) newborn refers to a baby who is smaller than expected for their gestational age. It can be caused by several factors, including restricted intrauterine growth, which can be associated with maternal gestational diabetes. However, it's not the most direct or common complication of the condition.
Choice E rationale:
Maternal gestational diabetes is a condition in which a woman develops high blood sugar levels during pregnancy. It's the most common metabolic complication of pregnancy and can lead to several serious health risks for both the mother and baby. These risks include:
Macrosomia (large for gestational age baby): High blood sugar levels in the mother can cause the baby to grow excessively large, leading to complications during labor and delivery, such as shoulder dystocia, birth injuries, and cesarean delivery. Preeclampsia: Gestational diabetes increases the risk of preeclampsia, a serious condition characterized by high blood pressure and protein in the urine. It can affect multiple organs, including the liver and kidneys, and can be life-threatening for both mother and baby.
Premature birth: Women with gestational diabetes are more likely to deliver their babies prematurely, which can lead to health problems for the baby, such as respiratory distress syndrome, feeding difficulties, and developmental delays.
Neonatal hypoglycemia: Newborns of mothers with gestational diabetes are at increased risk of hypoglycemia (low blood sugar) after birth due to the sudden withdrawal of maternal glucose supply. This can cause seizures, brain damage, and even death if not promptly treated.
Type 2 diabetes later in life: Both mother and child are at increased risk of developing type 2 diabetes later in life.
A nurse is caring for a client who is pregnant and has suspected placenta previa. Which of the following should the nurse monitor the client for?
Explanation
Choice A rationale:
Large amount of bright red vaginal bleeding is the cardinal sign of placenta previa. This is because the placenta is abnormally positioned low in the uterus, covering the cervix partially or completely. When the cervix starts to dilate in preparation for labor, it can detach from the uterine wall, leading to significant bleeding. The blood is typically bright red, indicating fresh bleeding, and can be painless.
Severity of bleeding: The amount of bleeding can vary from spotting to massive hemorrhage, and it may start suddenly or gradually. Even a small amount of bleeding can be a sign of placenta previa and should not be ignored.
Risks of hemorrhage: Prompt recognition and management of bleeding are crucial to prevent potentially life-threatening hemorrhage for both the mother and the fetus.
Choice B rationale:
Severe pain with no bleeding is not a typical presentation of placenta previa. While some women with placenta previa may experience mild abdominal pain or cramping, severe pain without bleeding is more suggestive of placental abruption, a condition where the placenta prematurely separates from the uterine wall.
Choice C rationale:
High-grade fever is not a direct symptom of placenta previa. However, if a woman with placenta previa develops a fever, it could indicate an infection, which can further complicate the condition and require immediate medical attention.
Choice D rationale:
Sudden sharp pain in the lower abdomen can be a sign of placental abruption but is not characteristic of placenta previa.
A nurse is reinforcing teaching with a client who is at weeks of gestation and scheduled for a non-stress test (NST). Which of the following statements by the client indicates a need for further teaching?
Explanation
Rationale for Choice A:
It is accurate that scheduling the NST when the baby is usually active is beneficial. This is because fetal movement is expected to cause accelerations in the fetal heart rate, which is a positive sign of fetal well-being.
By scheduling the test during a time of typical fetal activity, the chances of obtaining a reactive NST (a normal result) are increased.
Therefore, this statement does not indicate a need for further teaching.
Rationale for Choice B:
Lying on the back during the NST is not recommended.
This position can cause the weight of the uterus to compress the major blood vessels (the inferior vena cava and aorta), potentially reducing blood flow to the placenta and fetus.
Reduced blood flow can, in turn, lead to a decrease in fetal heart rate and movement.
To avoid this, the recommended position for NST is a semi-Fowler's position, which involves being partially reclined with the head and upper body elevated.
This position helps to promote uterine perfusion and prevent supine hypotension.
Rationale for Choice C:
It is accurate that the baby's heart rate will be monitored during the NST.
This is the primary purpose of the test: to assess the fetal heart rate response to fetal movement. Therefore, this statement does not indicate a need for further teaching.
Rationale for Choice D:
It is accurate that the client will be able to go to the bathroom during the NST if necessary. The test is noninvasive and does not require strict immobility.
The client can move around and use the bathroom as needed, as long as the fetal heart rate monitor is not disconnected.
Therefore, this statement does not indicate a need for further teaching.
A nurse is caring for a female client scheduled to have a pelvic exam. The client tells the nurse, “I’m really nervous.
I’ve never had a pelvic exam before.” Which of the following is an appropriate therapeutic response by the nurse?
Explanation
Rationale for Choice A:
A pelvic exam is required if you want birth control pills. This response is not therapeutic because it dismisses the client's feelings and does not address her concerns. It focuses on the policy or requirement rather than the client's emotional needs. It could make the client feel like her anxiety is not justified or that she has no choice in the matter.
Rationale for Choice B:
Don't worry, I will stay in there with you for the exam. While this response may be intended to provide reassurance, it does not fully address the client's underlying concerns. It offers a solution without first exploring the specific reasons for the client's anxiety. It could also make the client feel dependent on the nurse's presence for comfort, rather than empowering her to manage her own anxiety.
Rationale for Choice C:
All you need to do is relax during the exam. This response is not therapeutic because it minimizes the client's feelings and suggests that she can simply control her anxiety by relaxing. It does not acknowledge the validity of her concerns or provide any guidance on how to manage those concerns. It could make the client feel like her anxiety is her fault or that she is not coping well.
Rationale for Choice D:
Tell me more about your concerns. This is the most therapeutic response because it encourages the client to express her feelings and concerns openly. It validates the client's experience and demonstrates active listening and empathy. It provides an opportunity for the nurse to gather more information about the specific reasons for the client's anxiety and to tailor interventions accordingly. It also empowers the client by allowing her to share her thoughts and take control of the conversation.
A nurse is reinforcing teaching about fetal development with a group of women who are pregnant. Which of the following statements should the nurse include in the teaching?
Explanation
Choice A:
It is incorrect to state that all women will start to feel the baby move at 24 weeks. While this is a common timeframe, the exact timing of when a woman first feels fetal movements, known as quickening, can vary. Some women may feel movement as early as 16 weeks, while others may not feel it until closer to 25 weeks. Factors such as the position of the placenta, the woman's body size, and whether it is her first pregnancy can influence when she first perceives movement.
Choice B:
While the baby's sex is genetically determined at conception, it is not typically visible on ultrasound until around 18-20 weeks of gestation. This is due to the development of the external genitalia, which occurs between 11 and 14 weeks. It is not accurate to state that the sex is always definitively determined by week 8.
Choice D:
Lanugo, the fine hair that covers a fetus's body, is typically present between 14 and 20 weeks of gestation. It starts to disappear around 32-36 weeks, and most babies are born without it. Therefore, it is incorrect to say that lanugo covers the entire body at 36 weeks.
Choice C:
The fetal heartbeat can be detected by a Doppler stethoscope as early as 10-12 weeks of gestation. This is often a reassuring milestone for pregnant women, as it provides audible confirmation of the baby's presence and well-being. It is a common practice for healthcare providers to use a Doppler stethoscope during prenatal visits to assess the fetal heart rate and monitor fetal development.
A nurse is caring for a client who is at 34 weeks of gestation and has a suspected placenta previa. Which of the following actions should the nurse take?
Explanation
Choice A:
Applying ice to the perineal area is not a recommended intervention for suspected placenta previa. While ice can help reduce swelling and pain in some cases, it does not address the underlying concern of potential placental bleeding.
Focusing on external monitoring for fetal well-being and avoiding any actions that could disrupt the placenta are the priorities in this situation.
Choice C:
Completing a vaginal exam is contraindicated in suspected placenta previa. Inserting fingers into the vagina can disrupt the placenta and potentially cause heavy bleeding, increasing the risk of preterm labor, fetal distress, or maternal hemorrhage. Non-invasive assessment methods are crucial to protect the placenta and prevent complications.
Choice D:
Performing a rectal exam is also not indicated for suspected placenta previa. It does not provide information about the placental position and could potentially stimulate contractions, which are undesirable in this situation.
External fetal monitoring is a safer and more informative approach.
Choice B:
Applying an external fetal monitor is the most appropriate action for a nurse caring for a client with suspected placenta previa. It allows for continuous assessment of fetal heart rate and activity, which can help detect any signs of fetal distress or placental abruption.
It is a non-invasive method that does not carry the risks associated with vaginal or rectal exams.
Early identification of any fetal compromise can lead to prompt interventions to ensure the best possible outcomes for both mother and baby.
A nurse is caring for a client who has consented to an amniocentesis for genetic cell analysis. The client asks why she can’t have the test before 14 weeks of gestation.
Which of the following responses should the nurse make?
Explanation
Choice A:
While fetal maturity is a factor in the timing of amniocentesis, it's not the primary reason for waiting until 14 weeks.
Earlier in pregnancy, fetal cells are less abundant in the amniotic fluid, making it more challenging to obtain a sufficient sample for accurate testing.
Additionally, the procedure carries a slightly higher risk of miscarriage before 14 weeks.
Choice B:
The audibility of the fetal heartbeat is not directly related to the timing of amniocentesis.
It's typically possible to hear the heartbeat by Doppler ultrasound around 10-12 weeks, but this doesn't mean there's enough amniotic fluid for amniocentesis.
Choice D:
The accuracy of genetic results is not dependent on the timing of amniocentesis after 14 weeks.
As long as a sufficient sample of amniotic fluid is obtained, the accuracy of the results is not affected by gestational age.
Choice C:
The most accurate explanation for why amniocentesis is not performed before 14 weeks is the amount of amniotic fluid. Before 14 weeks, there's typically not enough amniotic fluid to safely extract a sample without potentially harming the fetus or the placenta.
By 14 weeks, there's usually enough fluid to adequately cushion the fetus and the needle during the procedure, reducing the risks involved.
A nurse is assisting with the admission of a client who is at 38 weeks of gestation and has severe preeclampsia. When collecting data from the client, the nurse should expect which of the following findings?
Explanation
Choice A rationale:
Tachycardia, or a fast heart rate, is not a common finding in severe preeclampsia. While some women with preeclampsia may experience a slight increase in heart rate, it is not typically a significant or defining feature of the condition. In fact, some women with severe preeclampsia may even experience a slightly decreased heart rate due to increased vagal tone.
Choice B rationale:
Hypotension, or low blood pressure, is also not a typical finding in severe preeclampsia. Blood pressure is often elevated in preeclampsia, and it is one of the key diagnostic criteria. Hypotension would be a concerning finding in a woman with preeclampsia, as it could indicate a serious complication such as placental abruption or HELLP syndrome (Hemolysis, Elevated Liver enzymes, and Low Platelet count).
Choice C rationale:
Polyuria, or excessive urination, is not a characteristic finding of severe preeclampsia. In fact, many women with preeclampsia experience oliguria, or decreased urine output, due to decreased kidney function. This is because preeclampsia can cause damage to the blood vessels in the kidneys, impairing their ability to filter blood and produce urine.
Choice D rationale:
Headache is a common and often severe symptom of severe preeclampsia. It is thought to be caused by increased pressure within the brain due to swelling and vasoconstriction of the blood vessels. Headaches in preeclampsia can be very intense and may be accompanied by other symptoms such as blurred vision, nausea, and vomiting. They are often a sign that the preeclampsia is worsening and that delivery may be necessary.
A nurse is assisting with the admission of a client who is at 10 weeks of gestation and reports abdominal pain and moderate vaginal bleeding.
Incomplete abortion is the initial diagnosis.
Which of the following actions should the nurse contribute to the client’s plan of care?
No explanation
A nurse is caring for a client who has just learned that she is pregnant.
The nurse should reinforce with the client to call her provider if she experiences which of the following manifestations?
Explanation
Choice A:
Mood swings are a common and expected symptom of early pregnancy due to hormonal changes. They typically do not require medical attention unless they become severe or interfere with daily life.
While it's important to discuss mood swings with a healthcare provider, they are not considered a critical symptom that necessitates immediate action.
Choice C:
Urinary frequency, or the need to urinate more often, is also a common symptom of early pregnancy. It's caused by hormonal changes and the growing uterus putting pressure on the bladder.
While it can be inconvenient, it's typically not a cause for concern unless accompanied by other symptoms, such as pain or burning during urination.
Choice D:
Decreased energy, or fatigue, is another common and expected symptom of early pregnancy.
It's often caused by hormonal changes and the body's increased workload to support the growing fetus.
While it can be frustrating, it's typically not a cause for concern unless it becomes severe or interferes with daily life.
Choice B:
Facial edema, or swelling of the face, is not a common symptom of early pregnancy.
It can be a sign of preeclampsia, a serious pregnancy complication characterized by high blood pressure and protein in the urine.
Preeclampsia can develop suddenly and progress quickly, so it's important to seek medical attention right away if facial edema occurs.
Key Points:
Facial edema is a potential sign of preeclampsia, a serious pregnancy complication.
Mood swings, urinary frequency, and decreased energy are common and expected symptoms of early pregnancy that typically do not require immediate medical attention.
It's important for pregnant women to be aware of potential warning signs and to seek medical advice promptly if they experience any concerning symptoms.
A nurse is reinforcing teaching with a client who is 15 weeks pregnant about to undergo amniocentesis. This test can identify which traits or problems? Select all that apply.
Explanation
Choice A:
Rh incompatibility is not directly identified through amniocentesis. Instead, it's typically assessed through blood tests that determine a woman's Rh factor and screen for Rh antibodies.
However, amniocentesis can provide information that might be relevant to Rh incompatibility, such as the fetal Rh type. If the mother is Rh-negative and the fetus is Rh-positive, there's a risk of Rh incompatibility.
Choice B:
Amniocentesis can detect neural tube defects (NTDs) like spina bifida and anencephaly.
It does this by measuring the levels of alpha-fetoprotein (AFP) in the amniotic fluid. AFP is a protein produced by the fetal liver, and elevated levels in the amniotic fluid can indicate an NTD.
Choice C:
Amniocentesis can accurately determine the fetal gender by examining the sex chromosomes present in the cells of the amniotic fluid.
Choice D:
Cephalopelvic disproportion (CPD) is a condition where the baby's head is too large to fit through the mother's pelvis. It's not diagnosed through amniocentesis.
CPD is usually suspected based on clinical findings like a slow progression of labor or a high fetal station, and it might be confirmed with imaging techniques like X-ray or ultrasound.
Choice E:
Amniocentesis is a valuable tool for diagnosing chromosomal defects, such as Down syndrome, Trisomy 18, and Trisomy 13. It does this by analyzing the chromosomes of the fetal cells present in the amniotic fluid.
A nurse is collecting data from a client who is at 35 weeks of gestation. Which of the following findings should the nurse report to the provider?
Explanation
Choice A rationale:
Constipation is a common complaint during pregnancy, especially in the later stages. It is caused by hormonal changes that relax the muscles of the intestines, as well as the pressure of the growing uterus on the rectum.
It is generally not a cause for concern, and can be managed with dietary changes, increased fluid intake, and exercise. However, if constipation is severe or persistent, it is important to rule out other potential causes, such as intestinal obstruction or hypothyroidism.
Choice C rationale:
Leukorrhea is a white, milky discharge that is common during pregnancy. It is caused by increased production of cervical mucus, and is generally harmless.
However, if leukorrhea is accompanied by other symptoms, such as itching, burning, or a foul odor, it may be a sign of an infection and should be evaluated by a healthcare provider.
Choice D rationale:
Blurred vision can be a symptom of several different conditions, including preeclampsia, gestational diabetes, and migraines. It is important to report any changes in vision to a healthcare provider so that the underlying cause can be identified and treated.
Choice B rationale:
Low back pain is a common complaint during pregnancy, especially in the later stages. It is caused by a number of factors, including:
The weight of the growing uterus, which puts strain on the muscles and ligaments of the back. The relaxation of the joints and ligaments in the pelvis in preparation for childbirth.
Changes in posture to accommodate the growing belly.
While low back pain is often a normal part of pregnancy, it can sometimes be a sign of a more serious problem, such as preterm labor or placental abruption.
Therefore, it is important to report any new or worsening back pain to a healthcare provider.
A nurse is caring for a client at 34 weeks gestation.
Medical History: The client has a history of gestational diabetes and mild hypertension. Diagnostic Results: The latest ultrasound shows normal fetal growth and development. Blood sugar levels have been slightly elevated in the past week.
Vital Signs: Blood pressure has been steadily increasing over the past few hours. Heart rate and temperature remain within normal limits.
Complete the diagram by selecting the condition the client is most likely experiencing? Two actions the nurse should take to address that condition and two parameters the nurse should monitor to assess the client’s progress.
Explanation
Choice A rationale:
Preeclampsia is a pregnancy complication characterized by high blood pressure and signs of damage to other organ systems, often the kidneys. It typically develops after 20 weeks of gestation and can progress to severe preeclampsia or eclampsia, which can be life-threatening for both the mother and the baby.
The client's history of gestational diabetes and mild hypertension, along with the recent elevation in blood pressure, is strongly suggestive of preeclampsia. Gestational diabetes is a known risk factor for preeclampsia.
The ultrasound showing normal fetal growth and development does not rule out preeclampsia. Preeclampsia can occur even in pregnancies where the baby is growing normally.
The elevated blood sugar levels in the past week could be a sign of worsening preeclampsia, as it can affect the body's ability to regulate blood sugar.
Choice B rationale:
Antihypertensive medication is a key component of managing preeclampsia. It helps to lower blood pressure and reduce the risk of complications such as stroke and organ damage.
The specific medication and dosage will be determined by the healthcare provider based on the severity of the preeclampsia and the client's individual needs.
Choice C rationale:
Regular monitoring of blood pressure and urine protein levels is essential for assessing the progression of preeclampsia and guiding treatment decisions.
Blood pressure readings can indicate whether the preeclampsia is worsening or responding to treatment. Urine protein levels can reveal kidney damage, which is a common complication of preeclampsia.
Choice D rationale:
Blood pressure readings are a direct measure of the severity of preeclampsia.
Elevated blood pressure can strain the heart, kidneys, and other organs, leading to serious complications.
Choice E rationale:
Protein in the urine (proteinuria) is a sign of kidney damage, which can be a complication of preeclampsia.
The level of protein in the urine can help to assess the severity of the kidney damage and guide treatment decisions.
A nurse is reinforcing teaching with a newly licensed nurse about a biophysical profile. Which of the following information should the nurse include in the teaching?
Explanation
Choice A:
Purpose of the Biophysical Profile (BPP): The BPP is a non-invasive test that combines ultrasound and fetal heart rate monitoring to assess fetal well-being, specifically in the third trimester of pregnancy. It evaluates five parameters: fetal breathing movements, fetal body movements, fetal tone, amniotic fluid volume, and fetal heart rate reactivity. Each parameter is assigned a score of 0 or 2, resulting in a total score of 0 to 10. A score of 8 or 10 is generally considered reassuring of fetal well-being, while a score of 6 or below may warrant further evaluation or intervention.
Timing of BPP: It's typically performed in the third trimester, often after 32 weeks of gestation, when the fetus has developed regular sleep-wake cycles and breathing movements.
Risk Assessment: It's often recommended for pregnancies considered high-risk, such as those with: Maternal diabetes
Preeclampsia
Decreased fetal movement Past stillbirth
Multiple gestation
Oligohydramnios (low amniotic fluid) Post-term pregnancy (over 42 weeks)
Choice B:
IV initiation is not a routine part of BPP: Intravenous (IV) access is not typically required for a BPP. The test involves external monitoring of fetal heart rate and ultrasound imaging, which do not necessitate IV access.
Choice C:
NPO status is not necessary: The client does not need to be NPO (nothing by mouth) for a BPP. There are no dietary restrictions or fasting requirements for this test.
Choice D:
BPP does not determine the estimated date of birth: The primary purpose of the BPP is to assess fetal well-being, not to determine the estimated date of delivery (EDD). The EDD is typically established based on the last menstrual period or early ultrasound measurements.
A nurse is assisting with the admission of a client who is at 8 weeks of gestation and has heavy vaginal bleeding. Which of the following actions should the nurse take?
Explanation
Choice A:
Magnesium sulfate is a medication primarily used to prevent or manage seizures in women with preeclampsia or eclampsia, conditions characterized by high blood pressure and protein in the urine during pregnancy. It is not indicated for heavy vaginal bleeding in early pregnancy.
Administration of magnesium sulfate without a clear indication could potentially lead to adverse effects such as respiratory depression, decreased deep tendon reflexes, and cardiac arrhythmias.
Choice B:
Antibiotics are used to treat bacterial infections. While heavy vaginal bleeding can sometimes be a sign of infection, it is not the primary cause of bleeding in early pregnancy.
Indiscriminate use of antibiotics without a confirmed bacterial infection can contribute to antibiotic resistance and potentially mask the underlying cause of the bleeding.
Choice D:
Cesarean birth is a major surgical procedure that is typically reserved for situations where there is a risk to the mother or fetus, such as fetal distress, failure to progress in labor, or placental abruption.
It is not indicated as the first-line intervention for heavy vaginal bleeding in early pregnancy, as there are other less invasive diagnostic and management options available.
Choice C:
A cervical examination allows the healthcare provider to assess the condition of the cervix, including its dilation and effacement, as well as to potentially identify any sources of bleeding, such as cervical polyps or lesions.
This information is crucial in determining the appropriate course of management for the patient.
It can help differentiate between potential causes of bleeding, such as threatened miscarriage, inevitable miscarriage, or ectopic pregnancy.
Sign Up or Login to view all the 49 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

