ATI LPN Med Surg
Total Questions : 24
Showing 24 questions, Sign in for moreA nurse is planning care for a client who is 1 day postoperative following a partial bowel resection. The client requires a complete dressing change, total parenteral nutrition administration, daily weight and is reporting pain at a level of 6 on a 0 to 10 scale. Which of the following nursing actions should the nurse plan to complete first?
Explanation
Choice A: Obtain the client’s vital signs. This is an important nursing action, but not the priority. The nurse should monitor the client’s vital signs for signs of infection, fluid imbalance, or shock, but these are not as urgent as relieving the client’s pain.
Choice B: Weigh the client. This is a necessary nursing action, but not the priority. The nurse should weigh the client daily to assess their fluid status and nutritional needs, but this can be done after addressing the client’s pain.
Choice C: Administer pain medication. This is the priority nursing action because the nurse should follow the principle of Maslow’s hierarchy of needs and address the client’s physiological needs first. Pain can interfere with the client’s healing process and affect their quality of life.
Choice D: Change the client’s dressing. This is a required nursing action, but not the priority. The nurse should change the client’s dressing to prevent infection and promote wound healing, but this can be done after administering pain medication to make the procedure more comfortable for the client.
A nurse is reinforcing teaching with a client who has diabetes mellitus type 1 about sick-day management. Which of the following is the priority action for the nurse to recommend to the client?
Explanation
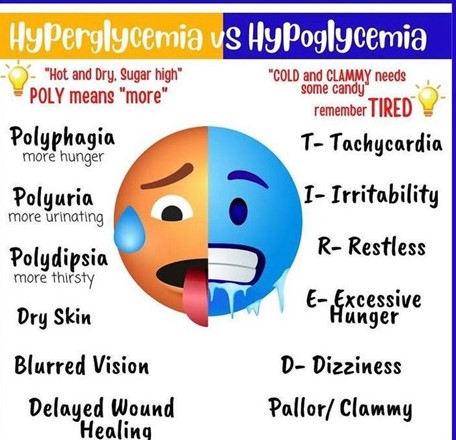
Choice A: “Monitor blood glucose levels every 4 hours.” This is the priority action for the nurse to recommend to the client because it will help them detect and prevent hyperglycemia or hypoglycemia, which can lead to serious complications such as diabetic ketoacidosis or cerebral edema.
Choice B: “Consume 15 grams of carbohydrates every 1 to 2 hours.” This is an important action for the nurse to recommend to the client, but not the priority. The client should consume carbohydrates to prevent hypoglycemia, especially if they have nausea, vomiting, or diarrhea, but this should be done after monitoring their blood glucose levels.
Choice C: “Drink 8 ounces of fluid every hour while awake.” This is a necessary action for the nurse to recommend to the client, but not the priority. The client should drink fluids to prevent dehydration and electrolyte imbalance, which can worsen hyperglycemia, but this should be done after monitoring their blood glucose levels.
Choice D: “Take the usual dosage of insulin.” This is a required action for the nurse to recommend to the client, but not the priority. The client should take their insulin as prescribed to control their blood glucose levels, but this should be done after monitoring their blood glucose levels and adjusting the dosage if needed.
A nurse is collecting data from a client who has gastroesophageal reflux disease (GERD) and reports having heartburn every night. Which of the following actions should the nurse identify as a contributing factor to the client’s heartburn?
Explanation
Choice A: Drinking orange juice regularly. This is a contributing factor to the client’s heartburn because orange juice is acidic and can irritate the esophageal mucosa and lower esophageal sphincter, causing reflux of gastric contents into the esophagus.
Choice B: Eating dinner early in the evening. This is not a contributing factor to the client’s heartburn, but rather a recommended action for the client to prevent heartburn. The client should avoid eating within 3 hours of bedtime to allow for gastric emptying and reduce the risk of reflux.
Choice C: Consuming low-fat meats. This is not a contributing factor to the client’s heartburn, but rather a recommended action for the client to prevent heartburn. The client should avoid high-fat foods, which can delay gastric emptying and increase intra-abdominal pressure, leading to reflux.
Choice D: Sleeping on a large wedge-style pillow. This is not a contributing factor to the client’s heartburn, but rather a recommended action for the client to prevent heartburn. The client should elevate the head of their bed or use a wedge pillow to create an incline that prevents gastric contents from flowing back into the esophagus.
A nurse is assisting with the care of a client who is 1 day postoperative following a thyroidectomy and reports severe muscle spasms of the lower extremities. Which of the following actions should the nurse take?
Explanation
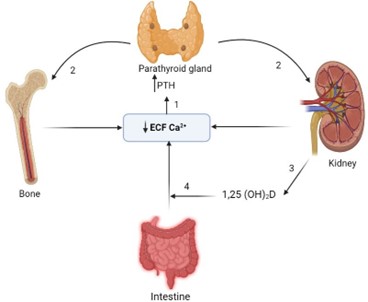
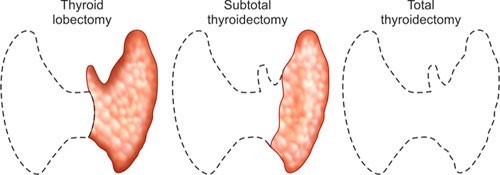
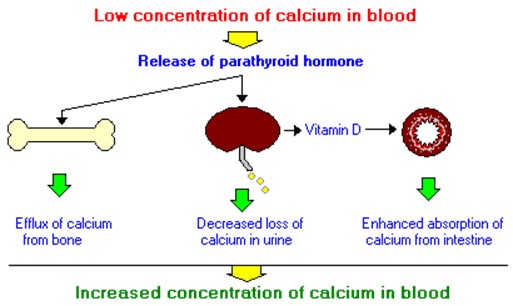
Choice A: Determine the client’s calcium level. This is the priority action for the nurse to take because the client might have hypocalcemia, which is a low level of calcium in the blood. Hypocalcemia can occur after a thyroidectomy due to accidental removal or damage of the parathyroid glands, which regulate calcium levels. Hypocalcemia can cause muscle spasms, tetany, paresthesia, and seizures.
Choice B: Give the client an oral potassium supplement. This is not an appropriate action for the nurse to take because the client might have hyperkalemia, which is a high level of potassium in the blood. Hyperkalemia can also occur after a thyroidectomy due to damage to the adrenal glands, which regulate potassium levels. Hyperkalemia can cause muscle weakness, arrhythmias, and cardiac arrest.
Choice C: Administer intravenous normal saline solution. This is not a necessary action for the nurse to take because the client does not have signs of dehydration or fluid imbalance. Normal saline solution does not affect calcium or potassium levels.
Choice D: Monitor the client’s peripheral pulses. This is an important action for the nurse to take, but not the priority. The nurse should monitor the client’s peripheral pulses for signs of decreased perfusion or ischemia, which can result from hypocalcemia or hyperkalemia affecting the cardiac function. However, this should be done after determining the client’s calcium level and correcting it if needed.
A nurse is reviewing the plan of care for a client experiencing an acute exacerbation of ulcerative colitis. Which of the following treatments should the nurse expect to administer?
Explanation
Choice A: Docusate. This is not a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis. Docusate is a stool softener that can prevent constipation and straining, but it is not indicated for ulcerative colitis.
Choice B: A corticosteroid medication. This is a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis, which is a chronic inflammatory bowel disease that causes ulcers and inflammation in the colon and rectum. A corticosteroid medication, such as prednisone, can reduce inflammation, suppress the immune system, and relieve symptoms such as diarrhea, bleeding, and pain.
Choice C: Aspirin. This is not a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis. Aspirin is a nonsteroidal anti-inflammatory drug (NSAID) that can relieve pain and inflammation, but it can also irritate the gastrointestinal mucosa and worsen ulcerative colitis.
Choice D: A bowel cathartic medication. This is not a treatment that the nurse should expect to administer to a client with an acute exacerbation of ulcerative colitis. A bowel cathartic medication, such as bisacodyl, can stimulate bowel movements and cleanse the colon, but it can also cause dehydration, electrolyte imbalance, and aggravate ulcerative colitis.
A nurse is assisting with the plan of care for a client who is 4 hr postoperative from a subtotal thyroidectomy. Which of the following implementations should the nurse recommend?
Explanation
Choice A: Check for bleeding on the dressing at the back of the client’s neck. This is an implementation that the nurse should recommend for a client who is 4 hr postoperative from a subtotal thyroidectomy, which is a surgical removal of part of the thyroid gland. The nurse should check for bleeding on the dressing at the back of the client’s neck because this is where blood can pool and go unnoticed. Bleeding can cause hematoma, compression of the airway, and respiratory distress.
Choice B: Ensure that acetylcysteine IV is readily available. This is not an implementation that the nurse should recommend for a client who is 4 hr postoperative from a subtotal thyroidectomy. Acetylcysteine IV is an antidote for acetaminophen overdose, which can cause liver damage, but it is not related to thyroid surgery.
Choice C: Place the client in a side-lying position. This is not an implementation that the nurse should recommend for a client who is 4 hr postoperative from a subtotal thyroidectomy. The nurse should place the client in a semi-Fowler’s position, which is a position with the head of the bed elevated to 30 to 45 degrees. This position can facilitate breathing, reduce edema, and prevent aspiration.
Choice D: Check the client for asterixis. This is not an implementation that the nurse should recommend for a client who is 4 hr postoperative from a subtotal thyroidectomy. Asterixis is a sign of hepatic encephalopathy, which is a condition caused by liver failure, but it is not related to thyroid surgery.
A nurse is caring for a client who is scheduled for a colonoscopy. The client asks the nurse if there will be a lot of pain during the procedure. Which of the following responses should the nurse make?
Explanation
Choice A: “You shouldn’t feel any pain since the local area is anaesthetized.” This is not a response that the nurse should make to the client who is scheduled for a colonoscopy. The nurse should not tell the client that they will not feel any pain, as this may create unrealistic expectations and increase anxiety if they do experience discomfort. The nurse should also not tell the client that the local area is anaesthetized, as this is not true. The client does not receive local anesthesia for a colonoscopy, but rather sedation and pain medication.
Choice B: “Don’t worry, you won’t remember anything about the procedure due to the effects of the medication.” This is not a response that the nurse should make to the client who is scheduled for a colonoscopy. The nurse should not tell the client not to worry, as this may sound dismissive and insensitive to their concerns. The nurse should also not tell the client that they will not remember anything about the procedure, as this is not true. The client may receive conscious sedation for a colonoscopy, which means that they are awake but drowsy and relaxed. They may have some memory loss of the procedure, but they are not completely unconscious.
Choice C: “Most clients report more discomfort from the preparation than from the procedure itself.” This is not a response that the nurse should make to the client who is scheduled for a colonoscopy. The nurse should not compare the client’s experience to other clients, as this may minimize their feelings and individual differences. The nurse should also not focus on the preparation, which involves drinking a large amount of liquid laxative to empty the colon, as this may increase anxiety and dread for the client. The nurse should instead focus on providing information and support for both the preparation and the procedure.
Choice D: “You may feel some cramping during the procedure.” This is a response that the nurse should make to the client who is scheduled for a colonoscopy, which is a diagnostic test that uses a flexible tube with a camera to examine the colon and rectum. The nurse should inform the client that they may feel some cramping during the procedure as the tube is inserted and moved through the colon. The nurse should also reassure the client that they will receive sedation and pain medication to make them comfortable and relaxed.

A nurse is assessing a client who has advanced cirrhosis. Which of the following manifestations should the nurse expect to find?
Explanation
Choice A: Weak pulse. This is not a manifestation that the nurse should expect to find in a client who has advanced cirrhosis. A weak pulse may indicate hypovolemia, shock, or cardiac dysfunction, but it is not directly related to liver disease.
Choice B: Dark colored stools. This is not a manifestation that the nurse should expect to find in a client who has advanced cirrhosis. Dark colored stools may indicate bleeding in the upper gastrointestinal tract, such as from esophageal varices or peptic ulcers, but they are not specific to liver disease.
Choice C: Spider angioma. This is a manifestation that the nurse should expect to find in a client who has advanced cirrhosis, which is a chronic liver disease that causes scarring and impaired liver function. Spider angioma is a type of vascular lesion that appears as a red spot with radiating branches on the skin, usually on the face, neck, chest, or upper arms. It is caused by increased estrogen levels due to reduced liver metabolism of hormones.
Choice D: Increased body hair. This is not a manifestation that the nurse should expect to find in a client who has advanced cirrhosis. Increased body hair may indicate hypertrichosis, which is excessive hair growth due to genetic, hormonal, or metabolic factors, but it is not related to liver disease.
A nurse is caring for a client who has developed a Clostridium difficile infection following antibiotic therapy. Which of the following actions should the nurse take?
Explanation
Choice A: Implement neutropenia isolation. This is not an action that the nurse should take for a client who has developed a Clostridium difficile infection. Neutropenia isolation is a type of protective isolation that is used for
clients who have low white blood cell counts and are at risk of infection from others. It is not indicated for clients who have Clostridium difficile infection, which is not transmited through the air.
Choice B: Use alcohol hand sanitizer following client care. This is not an action that the nurse should take for a client who has developed a Clostridium difficile infection. Alcohol hand sanitizer is ineffective against Clostridium difficile spores and can increase the risk of transmission. The nurse should wash their hands with soap and water, which can remove the spores from the skin.
Choice C: Monitor the client for manifestations of fluid overload. This is not an action that the nurse should take for a client who has developed a Clostridium difficile infection. Fluid overload is a condition that occurs when the body retains excess fluid and causes symptoms such as edema, dyspnea, and hypertension. It is not related to Clostridium difficile infection, which can cause fluid loss due to diarrhea and dehydration. The nurse should monitor the client for manifestations of fluid deficit, such as dry mucous membranes, tachycardia, and hypotension.
Choice D: Disinfect equipment with bleach solution. This is an action that the nurse should take for a client who has developed a Clostridium difficile infection, which is a bacterial infection that causes severe diarrhea and inflammation of the colon. Clostridium difficile spores are resistant to most disinfectants and can survive on surfaces for a long time. The nurse should disinfect equipment with bleach solution, which can kill the spores and prevent transmission.
A nurse is collecting data from a client who has obstruction and inflammation of the common bile duct due to cholelithiasis. Which of the following findings is expected for this condition?
Explanation
Choice A: Faty stools. This is a finding that is expected for a client who has obstruction and inflammation of the common bile duct due to cholelithiasis, which is the presence of gallstones in the gallbladder or bile ducts. The common bile duct carries bile from the liver and gallbladder to the duodenum, where it helps digest fats. If the common bile duct is obstructed by a gallstone, bile cannot reach the duodenum and fats cannot be properly absorbed. This results in fatty stools, which are also known as steatorrhea. Fatty stools are pale, bulky, greasy, and foul-smelling.
Choice B: Ecchymosis of the extremities. This is not a finding that is expected for a client who has obstruction and inflammation of the common bile duct due to cholelithiasis. Ecchymosis of the extremities is a sign of bleeding under the skin, which can be caused by trauma, coagulation disorders, or medications. It is not related to bile duct obstruction or gallstones.
Choice C: Straw-colored urine. This is not a finding that is expected for a client who has obstruction and inflammation of the common bile duct due to cholelithiasis. Straw-coloured urine is a normal colour of urine, which indicates adequate hydration and kidney function. It is not affected by bile duct obstruction or gallstones.
Choice D: Tenderness in the left upper abdomen. This is not a finding that is expected for a client who has obstruction and inflammation of the common bile duct due to cholelithiasis. Tenderness in the left upper abdomen is a sign of splenomegaly, which is an enlargement of the spleen due to infection, inflammation, or cancer. It is not related to bile duct obstruction or gallstones.
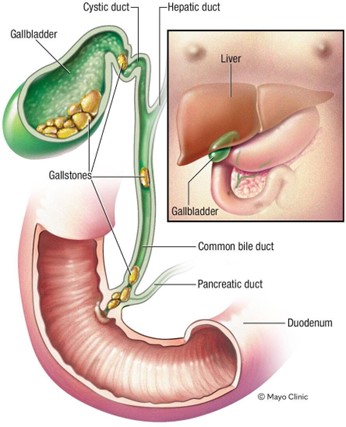
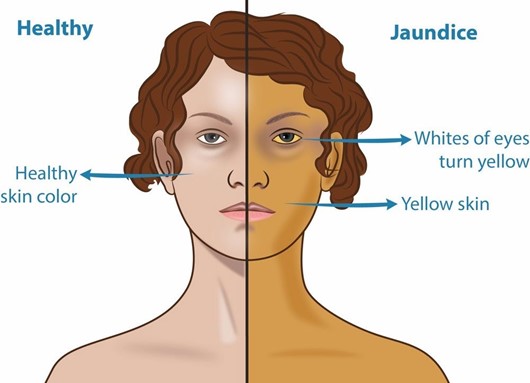
A nurse is collecting data from a client who is African American and has cholecystitis. Which of the following areas should the nurse inspect to monitor for the presence of jaundice?
Explanation
Choice A: Peri-umbilical area. This is not an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis. The peri-umbilical area is the area around the navel, which is part of the skin. The skin can show jaundice, but it may be difficult to detect in clients with dark skin tones.
Choice B: Nail beds. This is not an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis. The nail beds are part of the skin that can show jaundice, but they may also be affected by other factors such as anemia, cyanosis, or nail polish.
Choice C: Webbed areas of the fingers. This is not an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis. The webbed areas of the fingers are part of the skin that can show jaundice, but they may also be influenced by other factors such as temperature, circulation, or pressure.
Choice D: Hard palate. This is an area that the nurse should inspect to monitor for the presence of jaundice in a client who is African American and has cholecystitis, which is an inflammation of the gallbladder. Jaundice is a yellowish discoloration of the skin and mucous membranes due to elevated bilirubin levels in the blood. Bilirubin is a pigment that is produced from the breakdown of red blood cells and is normally excreted in bile. If the gallbladder or bile ducts are inflamed or obstructed, bile cannot flow into the duodenum and bilirubin accumulates in the blood and tissues. The hard palate is a part of the oral mucosa that can show jaundice, especially in clients with dark skin tones.
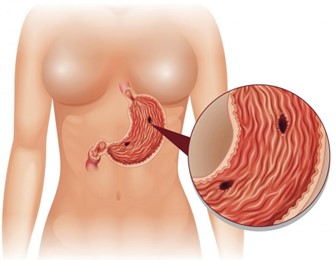
A nurse is collecting data from a client who has peptic ulcer disease. Which of the following findings is a manifestation of gastrointestinal perforation?
Explanation
Choice A: Bradycardia. This is not a manifestation of gastrointestinal perforation, but rather a sign of vagal stimulation, which can occur in response to gastric distension, vomiting, or suctioning. Vagal stimulation can slow down the heart rate and lower the blood pressure.
Choice B: Hyperactive bowel sounds. This is not a manifestation of gastrointestinal perforation, but rather a sign of increased intestinal motility, which can occur in response to inflammation, infection, or irritation of the gastrointestinal tract. Hyperactive bowel sounds are loud, high-pitched, and frequent.
Choice C: Report of epigastric fullness. This is not a manifestation of gastrointestinal perforation, but rather a sign of delayed gastric emptying, which can occur in response to gastric outlet obstruction, gastroparesis, or pyloric stenosis. Epigastric fullness is a feeling of pressure or discomfort in the upper abdomen after eating.
Choice D: Severe upper abdominal pain. This is a manifestation of gastrointestinal perforation, which is a life-threatening complication of peptic ulcer disease. Peptic ulcer disease is a condition that causes erosion and ulceration of the mucosal lining of the stomach or duodenum. If the ulcer penetrates through the wall of the gastrointestinal tract, it can cause perforation, which is a hole that allows gastric contents to leak into the peritoneal cavity. This can cause peritonitis, which is an inflammation and infection of the peritoneum. Peritonitis can cause severe upper abdominal pain, which may radiate to the shoulder or back. The pain may be sudden, sharp, and constant.
A nurse is caring for a client who has type 1 diabetes mellitus. The nurse misread the client’s morning fasting blood glucose level as 210 mg/dL instead of 120 mg/dL and administered the insulin dose appropriate for reading over 200 mg/dL. Which of the following actions should the nurse identify as the priority?
Explanation
Choice A: Notify the nurse manager. This is an important action that the nurse should take, but not a priority. The nurse should notify the nurse manager to report the error and seek guidance on how to proceed. The nurse manager can also provide support and feedback to the nurse and help prevent similar errors in the future.
Choice B: Give the client 15 to 20 g of carbohydrate. This is a necessary action that the nurse should take, but not the priority. The nurse should give the client 15 to 20 g of carbohydrates to raise their blood glucose level and prevent or treat hypoglycemia. The nurse should choose a fast-acting carbohydrate source, such as juice, glucose tablets, or candy.
Choice C: Complete an incident report. This is a required action that the nurse should take, but not the priority. The nurse should complete an incident report to document the error and its consequences. The incident report can help identify the root cause of the error and improve patient safety and quality of care.
Choice D: Check the client’s blood glucose level. This is the priority action that the nurse should identify according to the ABCDE principle, which prioritizes interventions based on airway, breathing, circulation, disability, and exposure. The nurse should check the client’s blood glucose level to confirm the error and assess the risk of hypoglycemia, which is a low level of glucose in the blood. Hypoglycemia can cause symptoms such as sweating, trembling, confusion, and loss of consciousness. It can be life-threatening if not treated promptly.
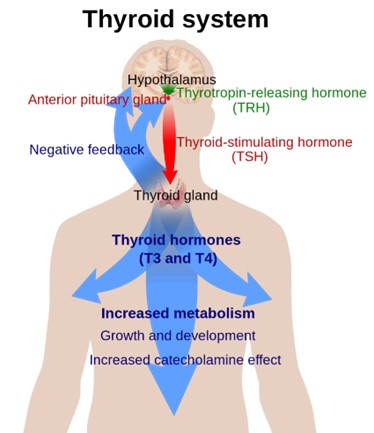
A nurse in a clinic is caring for a client who has a new diagnosis of hypothyroidism. Which of the following findings should the nurse expect?
Explanation
Choice A: Palpitations. This is not a finding that the nurse should expect in a client who has a new diagnosis of hypothyroidism, but rather a sign of hyperthyroidism, which is a condition that occurs when the thyroid gland produces too much thyroid hormone. Hyperthyroidism can cause palpitations due to increased cardiac output and heart rate.
Choice B: Weight gain. This is a finding that the nurse should expect in a client who has a new diagnosis of hypothyroidism, which is a condition that occurs when the thyroid gland does not produce enough thyroid hormone. The thyroid hormone regulates the metabolism of carbohydrates, proteins, and fats, and affects energy expenditure and body temperature. Hypothyroidism can cause weight gain due to decreased metabolic rate and increased fluid retention.
Choice C: Diaphoresis. This is not a finding that the nurse should expect in a client who has a new diagnosis of hypothyroidism, but rather a sign of hyperthyroidism. Hyperthyroidism can cause diaphoresis due to increased heat production and vasodilation.
Choice D: Protruding eyeballs. This is not a finding that the nurse should expect in a client who has a new diagnosis of hypothyroidism, but rather a sign of Graves’ disease, which is an autoimmune disorder that causes hyperthyroidism. Graves’ disease can cause protruding eyeballs due to inflammation and edema of the orbital tissues and muscles.
The nurse is caring for a client who has a bowel obstruction and a new prescription for the insertion of a nasogastric tube. Which of the following interventions should the nurse take when inserting the nasogastric tube?
Explanation
Choice A: Measure the tube for insertion from the tip of the nose to the umbilicus. This is not an intervention that the nurse should take when inserting a nasogastric tube. The nurse should measure the tube for insertion from the tip of the nose to the earlobe and then to the xiphoid process, which is a more accurate way of estimating the length of the tube needed to reach the stomach.
Choice B: Place the client in a supine position. This is not an intervention that the nurse should take when inserting a nasogastric tube. The nurse should place the client in a high-Fowler’s position, which is a position with the head of the bed elevated to 90 degrees. This position can prevent aspiration, promote breathing, and allow gravity to assist with the insertion of the tube.
Choice C: Withdraw the tube if the client gags during insertion. This is not an intervention that the nurse should take when inserting a nasogastric tube. The nurse should not withdraw the tube if the client gags during insertion, as this can cause trauma to the nasal or pharyngeal mucosa and increase discomfort. The nurse should pause and allow the client to rest and breathe until gagging subsides, then resume insertion. The nurse should also provide reassurance and encouragement to the client throughout the procedure.
Choice D: Instruct the client to place his chin to his chest and swallow. This is an intervention that the nurse should take when inserting a nasogastric tube, which is a flexible tube that is inserted through the nose and into the stomach. The nurse should instruct the client to place his chin to his chest and swallow as the tube passes through the pharynx and into the esophagus. This can facilitate the insertion of the tube and prevent it from entering the trachea or causing injury to the nasal or pharyngeal mucosa.
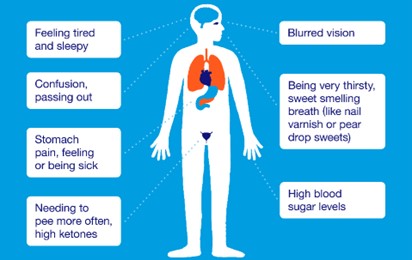
A nurse is collecting data from a client who has diabetes mellitus. Which of the following findings indicates that the client is experiencing DKA?
Explanation
Choice A: Rapid pulse. This is not a finding that indicates that the client is experiencing DKA, but rather a sign of hypoglycemia, which is a low level of glucose in the blood. Hypoglycemia can cause rapid pulse due to increased sympathetic nervous system activity and decreased cardiac output.
Choice B: Clammy skin. This is not a finding that indicates that the client is experiencing DKA, but rather a sign of hypoglycemia. Hypoglycemia can cause clammy skin due to increased sweating and vasoconstriction.
Choice C: Confusion. This is a finding that indicates that the client is experiencing diabetic ketoacidosis (DKA), which is a serious complication of diabetes mellitus that occurs when the body cannot use glucose as a fuel source and breaks down fat instead. This produces ketones, which are acidic byproducts that accumulate in the blood and urine. DKA can cause confusion due to dehydration, electrolyte imbalance, and cerebral edema.
Choice D: Polydipsia. This is not a finding that indicates that the client is experiencing DKA, but rather a sign of hyperglycemia, which is a high level of glucose in the blood. Hyperglycemia can cause polydipsia, which is excessive thirst, due to osmotic diuresis and dehydration.
A nurse is caring for a client who has hyperparathyroidism. Based on this diagnosis, the nurse should monitor the client for which of the following complications?
Explanation
Choice A: Dysphagia. This is not a complication that the nurse should monitor the client for who has hyperparathyroidism. Dysphagia is difficulty swallowing, which can be caused by disorders of the esophagus, throat, or nervous system. It is not related to hyperparathyroidism or calcium and phosphorus levels.
Choice B: Pathologic fractures. This is a complication that the nurse should monitor the client for who has hyperparathyroidism, which is a condition that occurs when the parathyroid glands produce too much parathyroid hormone (PTH). PTH regulates calcium and phosphorus levels in the blood and bones. Hyperparathyroidism can cause hypercalcemia, which is a high level of calcium in the blood, and hypophosphatemia, which is a low level of phosphorus in the blood. These imbalances can lead to bone resorption, which is the breakdown of bone tissue and release of calcium into the blood. Bone resorption can weaken the bones and increase the risk of pathologic fractures, which are fractures that occur due to disease or injury to the bone.
Choice C: Fluid retention. This is not a complication that the nurse should monitor the client for who has hyperparathyroidism. Fluid retention is excess fluid accumulation in the body, which can be caused by disorders of the heart, kidney, liver, or lymphatic system. It is not related to hyperparathyroidism or calcium and phosphorus levels.
Choice D: Impaired skin integrity. This is not a complication that the nurse should monitor the client for who has hyperparathyroidism. Impaired skin integrity is damage or loss of skin tissue, which can be caused by trauma, infection, inflammation, or pressure. It is not related to hyperparathyroidism or calcium and phosphorus levels.
A nurse is caring for a client who is postoperative and has a history of Addison’s disease. For which of the following manifestations should the nurse monitor?
Explanation
Choice A: Hypernatremia. This is not a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease. Hypernatremia is a high level of sodium in the blood, which can be caused by dehydration, excessive sodium intake, or kidney dysfunction. It is not related to Addison’s disease or cortisol and aldosterone levels.
Choice B: Bradycardia. This is not a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease. Bradycardia is a slow heart rate, which can be caused by vagal stimulation, medication side effects, or cardiac disorders. It is not related to Addison’s disease or cortisol and aldosterone levels.
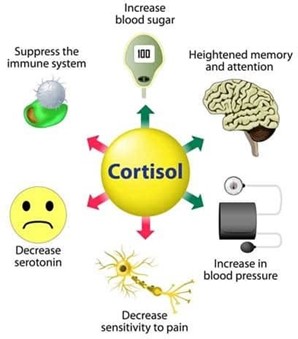
Choice C: Hypotension. This is a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease, which is a condition that occurs when the adrenal glands do not produce enough cortisol and aldosterone. Cortisol is a hormone that regulates the metabolism of carbohydrates, proteins, and fats, and helps the body cope with stress. Aldosterone is a hormone that regulates the balance of sodium and potassium in the blood and fluid volume. Addison’s disease can cause hypotension, which is a low blood pressure, due to decreased aldosterone production and fluid loss.
Choice D: Hypokalemia. This is not a manifestation that the nurse should monitor for in a client who is postoperative and has a history of Addison’s disease. Hypokalemia is a low level of potassium in the blood, which can be caused by diuretics, vomiting, diarrhea, or alkalosis. It is not related to Addison’s disease or cortisol and aldosterone levels.
A nurse is reinforcing teaching of a female client who has a family history of type 2 diabetes mellitus. The nurse should include which of the following risk factors for developing type 2 diabetes mellitus in the teaching?
Explanation
Choice A: Sedentary lifestyle. This is a risk factor for developing type 2 diabetes mellitus, which is a condition that occurs when the body becomes resistant to the action of insulin or does not produce enough insulin to maintain normal blood glucose levels. Insulin is a hormone that helps glucose enter the cells and be used for energy. A sedentary lifestyle can increase the risk of type 2 diabetes mellitus by reducing physical activity, which can improve insulin sensitivity and lower blood glucose levels.
Choice B: Triglyceride level of 100 mg/dL. This is not a risk factor for developing type 2 diabetes mellitus, but rather a normal value. Triglycerides are a type of fat that circulates in the blood and can be used for energy or stored in adipose tissue. A high triglyceride level can indicate an increased risk of cardiovascular disease, but it is not directly related to type 2 diabetes mellitus.
Choice C: Blood glucose of 98 mg/dL. This is not a risk factor for developing type 2 diabetes mellitus, but rather a normal value. Blood glucose is the amount of glucose in the blood, which can vary depending on food intake, physical activity, and hormonal regulation. A high blood glucose level can indicate type 2 diabetes mellitus, but it is not a cause of it.
Choice D: Recent viral infection. This is not a risk factor for developing type 2 diabetes mellitus, but rather a possible trigger for type 1 diabetes mellitus, which is a condition that occurs when the immune system destroys the beta cells of the pancreas that produce insulin. A viral infection can trigger an autoimmune response that attacks the beta cells and causes type 1 diabetes mellitus.
A nurse is collecting data from a client who has acute gastroenteritis. Which of the following data collection findings should the nurse identify as the priority?
Explanation
Choice A: Potassium 2.5 mEq/L. This is the priority data collection finding that the nurse should identify according to the ABCDE principle, which prioritizes interventions based on airway, breathing, circulation, disability, and exposure. The nurse should identify potassium 2.5 mEq/L as the priority because it indicates hypokalemia, which is a low level of potassium in the blood. Potassium is an electrolyte that regulates the electrical activity of the heart and muscles. Hypokalemia can cause cardiac arrhythmias, muscle weakness, and paralysis, which can be life-threatening.
Choice B: Blood glucose 150 mg/dL. This is not the priority data collection finding that the nurse should identify for a client who has acute gastroenteritis. Blood glucose 150 mg/dL indicates hyperglycemia, which is a high level of glucose in the blood. Hyperglycemia can be caused by dehydration, stress, infection, or medication side effects.
Hyperglycemia can cause symptoms such as polyuria, polydipsia, polyphagia, and fatigue. It can also lead to complications such as diabetic ketoacidosis or hyperosmolar hyperglycemic state, which are serious but not as urgent as hypokalemia.
Choice C: Urine specific gravity 1.035. This is not the priority data collection finding that the nurse should identify for a client who has acute gastroenteritis. Urine specific gravity 1.035 indicates concentrated urine, which can be caused by dehydration or fluid loss. Dehydration can result from vomiting and diarrhea, which are common symptoms of acute gastroenteritis. Dehydration can cause symptoms such as dry mucous membranes, tachycardia, hypotension, and oliguria. It can also lead to complications such as shock or kidney failure, which are serious but not as urgent as hypokalemia.
Choice D: Weight loss of 3% of total body weight. This is not the priority data collection finding that the nurse should identify for a client who has acute gastroenteritis. Weight loss of 3% of total body weight indicates mild to moderate dehydration, which can be caused by fluid loss from vomiting and diarrhea. Weight loss can also reflect loss of muscle mass or fat tissue due to malnutrition or inflammation. Weight loss can affect the client’s nutritional status and immune function, but it is not as urgent as hypokalemia.
A nurse is contributing to the plan of care for a client who has cirrhosis and ascites. Which of the following interventions should the nurse recommend for inclusion in the plan of care?
Explanation
Choice A: Increase the client’s sodium intake. This is not an intervention that the nurse should recommend for inclusion in the plan of care for a client who has cirrhosis and ascites. Increasing the client’s sodium intake can worsen fluid retention and exacerbate ascites. The nurse should recommend limiting the client’s sodium intake to less than 2 g per day.
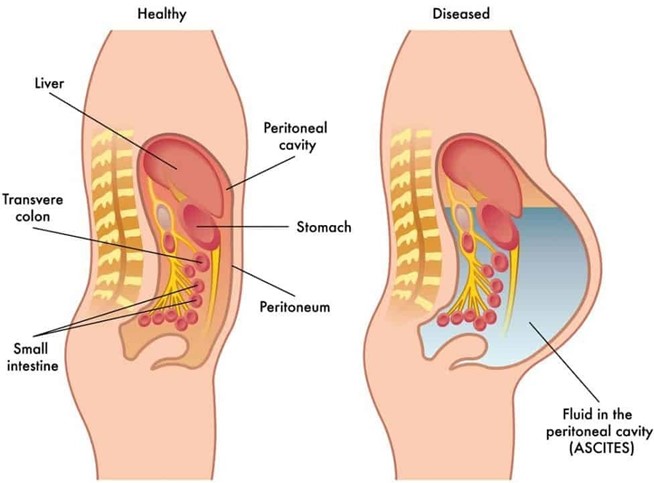
Choice B: Decrease the client’s fluid intake. This is an intervention that the nurse should recommend for inclusion in the plan of care for a client who has cirrhosis and ascites. Cirrhosis is a chronic liver disease that causes scarring and impaired liver function. Ascites is a complication of cirrhosis that involves the accumulation of fluid in the peritoneal cavity. Decreasing the client’s fluid intake can help reduce fluid retention and prevent further distension of the abdomen and pressure on the diaphragm.
Choice C: Increase the client’s saturated fat intake. This is not an intervention that the nurse should recommend for inclusion in the plan of care for a client who has cirrhosis and ascites. Increasing the client’s saturated fat intake can increase the risk of cardiovascular disease, obesity, and faty liver disease. The nurse should recommend a balanced diet that provides adequate protein, calories, vitamins, and minerals.
Choice D: Decrease the client’s carbohydrate intake. This is not an intervention that the nurse should recommend for inclusion in the plan of care for a client who has cirrhosis and ascites. Decreasing the client’s carbohydrate intake can cause ketosis, which is a metabolic state that occurs when the body uses fat as a fuel source instead of glucose.
Ketosis can cause nausea, fatigue, headache, and bad breath. The nurse should recommend a moderate carbohydrate intake that provides enough glucose for energy and prevents ketosis.
A nurse is assisting with the plan of care for a client who has hypothyroidism with myxedema. Which of the following interventions should the nurse include in the plan of care?
Explanation
Choice A: Place the client on bedrest. This is not an intervention that the nurse should include in the plan of care for a client who has hypothyroidism with myxedema. Placing the client on bedrest can increase the risk of complications such as thromboembolism, pressure ulcers, and muscle atrophy. The nurse should encourage the client to perform gentle exercises and change positions frequently.
Choice B: Apply warm blankets. This is an intervention that the nurse should include in the plan of care for a client who has hypothyroidism with myxedema. Hypothyroidism is a condition that occurs when the thyroid gland does not produce enough thyroid hormone. Thyroid hormone regulates the metabolism of carbohydrates, proteins, and fats, and affects the energy expenditure and body temperature. Myxedema is a severe form of hypothyroidism that causes swelling of the skin and tissues due to accumulation of mucopolysaccharides. Applying warm blankets can help maintain the client’s body temperature and prevent hypothermia, which is a low body temperature.
Choice C: Check the client for weight loss. This is not an intervention that the nurse should include in the plan of care for a client who has hypothyroidism with myxedema. Checking the client for weight loss can indicate hyperthyroidism, which is a condition that occurs when the thyroid gland produces too much thyroid hormone.
Hyperthyroidism can cause weight loss due to increased metabolic rate and appetite. The nurse should check the client for weight gain, which can indicate hypothyroidism due to decreased metabolic rate and fluid retention.
Choice D: Limit high-fiber foods. This is not an intervention that the nurse should include in the plan of care for a client who has hypothyroidism with myxedema. Limiting high-fiber foods can cause constipation, which can worsen hypothyroidism symptoms such as bloating, abdominal pain, and fatigue. The nurse should encourage the client to eat high-fiber foods, such as fruits, vegetables, and whole grains, to promote bowel regularity and prevent constipation.
A nurse is collecting data from a client who has diverticular disease. The nurse should expect the client to report abdominal pain in which of the following locations?
Explanation
Choice A: Upper left quadrant. This is not the location where the nurse should expect the client to report abdominal pain who has diverticular disease. The upper left quadrant of the abdomen contains organs such as the stomach, spleen, pancreas, and part of the colon. Abdominal pain in this area can indicate conditions such as gastritis, peptic ulcer, pancreatitis, splenomegaly, or colon cancer.
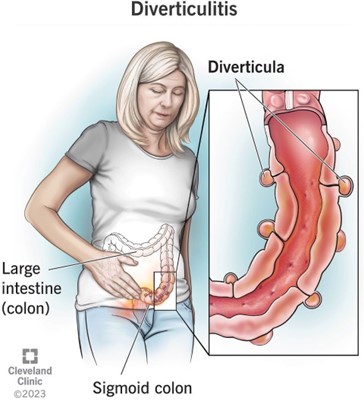
Choice B: Lower left quadrant. This is the location where the nurse should expect the client to report abdominal pain who has diverticular disease, which is a condition that involves the formation of pouches or sacs in the wall of the colon. These pouches or sacs are called diverticula, and they can become inflamed or infected, causing diverticulitis. Diverticulitis can cause abdominal pain, fever, nausea, vomiting, and changes in bowel habits. The most common site of diverticula formation and diverticulitis is the sigmoid colon, which is located in the lower left quadrant of the abdomen.
Choice C: Upper right quadrant. This is not the location where the nurse should expect the client to report abdominal pain who has diverticular disease. The upper right quadrant of the abdomen contains organs such as the liver, gallbladder, duodenum, and part of the colon. Abdominal pain in this area can indicate conditions such as hepatitis, cholecystitis, duodenal ulcer, or colon cancer.
Choice D: Lower right quadrant. This is not the location where the nurse should expect the client to report abdominal pain who has diverticular disease. The lower right quadrant of the abdomen contains organs such as the appendix, cecum, and part of the colon. Abdominal pain in this area can indicate conditions such as appendicitis, Crohn’s disease, or colon cancer.
A nurse is caring for a client who has Cushing’s syndrome. Which of the following clinical manifestations should the nurse expect to observe? (Select all that apply.)
Explanation
Choice A: Purple striations. These are also known as striae, and they are caused by the thinning and weakening of the skin and underlying connective tissue due to cortisol. They appear as purple or red lines on the abdomen, thighs, breasts, or arms.
Choice C: Buffalo hump. This is a term used to describe the accumulation of fat on the upper back and neck due to cortisol. It gives the appearance of a hump or a rounded shape.
Choice E: Moon face. This is a term used to describe the rounding and fullness of the face due to cortisol. It gives the
appearance of a moon-like shape.
Choice B: Tremors. These are not a clinical manifestation of Cushing’s syndrome, but rather a sign of hyperthyroidism, which is a condition caused by excess thyroid hormone production or exposure. Thyroid hormone affects the nervous system and causes increased muscle activity and tremors.
Choice D: Obese extremities. These are not a clinical manifestation of Cushing’s syndrome, but rather a sign of hypothyroidism, which is a condition caused by low thyroid hormone production or exposure. Thyroid hormone affects the metabolism of carbohydrates, proteins, and fats, and causes decreased energy expenditure and weight gain.
Sign Up or Login to view all the 24 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

