ATI Maternal Newborn
Total Questions : 82
Showing 25 questions, Sign in for moreA nurse is reviewing a client's medical record and notes that the client is taking tamoxifen.
The nurse should identify that tamoxifen is used to treat which of the following conditions?
Explanation
Choice A rationale:
Tamoxifen is not used to treat Non-Hodgkin's lymphoma. Tamoxifen is a selective estrogen
receptor modulator (SERM) and is primarily used in breast cancer treatment. It functions by
binding to estrogen receptors, blocking estrogen's effects, and inhibiting the growth of
hormone-sensitive breast cancer cells.
Choice B rationale:
Tamoxifen is not used to treat endometriosis. Endometriosis is a condition in which tissue
similar to the lining of the uterus grows outside the uterus, and it is typically managed with
hormonal therapies, pain medications, or surgical interventions, but not tamoxifen.
Choice C rationale:

This is the correct choice. Tamoxifen is widely used in the treatment of breast cancer,
especially in cases of estrogen receptor-positive breast cancer. It helps prevent cancer
recurrence and is often prescribed for both early-stage and advanced breast cancer patients.
Choice D rationale:
Tamoxifen is not used to treat polycystic ovary syndrome (PCOS). PCOS is a hormonal
disorder characterized by enlarged ovaries with small cysts, and it is typically managed with
lifestyle changes, hormonal contraceptives, and medications to regulate menstrual cycles and
manage symptoms like hirsutism and acne.
A nurse is caring for a client who has placenta previa. Which of the following interventions should the nurse implement for this client? (Select all that apply.)
Explanation
Choice A rationale:
Performing a vaginal exam is contraindicated in a client with placenta previa. Placing anything in the vagina can disrupt the placenta and lead to significant bleeding due to the placenta's low implantation in the uterus.
Choice B rationale:
Monitoring fetal heart rate with an internal fetal monitor is appropriate for a client with placenta previa. Since placenta previa can cause bleeding during labor, an internal fetal monitor provides a more accurate and continuous assessment of the baby's well-being, especially if external monitoring is difficult due to bleeding or maternal movement.
Choice C rationale:
Frequently assessing maternal heart rate is essential in a client with placenta previa. Excessive maternal heart rate may indicate bleeding or hypovolemic shock, which can be life- threatening for both the mother and the baby.
Choice D rationale:
Initiating bed rest with bathroom privileges is a standard intervention for a client with placenta previa. Bed rest helps to reduce physical activity, decreasing the risk of bleeding episodes. However, bathroom privileges are allowed to maintain the client's comfort and prevent complications associated with immobility.
Choice E rationale:
Having oxygen equipment available is crucial for a client with placenta previa. In cases of severe bleeding, the client may experience hypoxia due to blood loss. Oxygen administration can help improve tissue oxygenation until other interventions, such as blood transfusions or emergency delivery, can be performed.
A nurse is providing teaching to a client who is at 34 weeks of gestation and is scheduled for a nonstress test. Which of the following statements should the nurse plan to make?
Explanation
Choice A rationale:
This statement is incorrect. A nonstress test does not involve receiving medication through an
IV. It is a simple and non-invasive test that monitors the baby's heart rate in response to its movements.
Choice B rationale:
This is the correct choice. A nonstress test typically takes about 30 minutes to complete. During the test, the client will have a fetal heart rate monitor placed on her abdomen to measure the baby's heart rate while it is moving.
Choice C rationale:
This statement is incorrect. There is no requirement for the client to fast or restrict food and drink before a nonstress test. The client can eat and drink as usual before the procedure.
Choice D rationale:
This statement is incorrect. A nonstress test is not used to determine if the baby's lungs are mature. Instead, it assesses the baby's heart rate patterns in response to its own movements, which helps evaluate the baby's overall well-being in the third trimester of pregnancy.
A nurse is teaching a client about using an intrauterine device (IUD) for contraception. Which of the following client statements indicates an understanding of the teaching?
Explanation
Choice A rationale:
The client's statement about needing to have the IUD replaced each year is incorrect. The lifespan of most IUDs is longer than a year. Copper IUDs can last up to 10 years, and hormonal IUDs can last between 3 to 7 years, depending on the brand.
Choice B rationale:
The client's statement about needing to apply a spermicide prior to intercourse is unrelated to the correct use of an intrauterine device (IUD) for contraception. Spermicides are not required when using an IUD.
Choice C rationale:
The client's statement about expecting periods to stop while having the IUD is incorrect. Hormonal IUDs can often lead to lighter periods, and in some cases, periods may stop altogether. However, with a copper IUD, periods usually remain the same.
Choice D rationale:

This is the correct choice. The client's statement indicates an understanding of the teaching. Checking for the string each month after menstruation is crucial because it confirms that the IUD is still in place, reducing the risk of unintended pregnancy.
A nurse is teaching the parent of a newborn about car seat safety. Which of the following statements should the nurse make?
Explanation
Choice A rationale:
This is the correct choice. The American Academy of Pediatrics (AAP) recommends keeping children in a rear-facing car seat until they reach the age of 2 or until they reach the maximum weight and height allowed by the car seat's manufacturer. This is because rear- facing seats provide better support for a baby's head, neck, and spine during a crash, reducing the risk of injury.
Choice B rationale:
Placing the retainer clip over the upper part of the baby's abdomen is incorrect and potentially dangerous. The retainer clip should be positioned at armpit level to secure the harness straps properly.
Choice C rationale:
Placing the baby in the car seat at a 90-degree angle is not necessary. The car seat should be installed according to the manufacturer's instructions, and the angle will vary based on the specific car seat model.
Choice D rationale:
Placing the shoulder harness straps in the slots an inch above the baby's shoulders is incorrect. The straps should be positioned at or below the baby's shoulders for rear-facing car seats and at or above the shoulders for forward-facing seats.
A nurse is assessing a newborn who is 10 hr old. Which of the following findings should the nurse report to the provider?
Explanation
Choice A rationale:
An axillary temperature of 36.5°C (97.7°F) is within the normal range for a newborn. Normal axillary temperature for a newborn is typically between 36.5°C to 37.5°C (97.7°F to 99.5°F).
Choice B rationale:
This is the correct choice. Nasal flaring in a newborn is a concerning sign and may indicate respiratory distress. It suggests that the baby is having difficulty breathing and should be reported to the provider for further evaluation.
Choice C rationale:
A heart rate of 158/min is within the normal range for a newborn. The normal heart rate for a newborn can range from 100 to 160 beats per minute.
Choice D rationale:
Having one void since birth is not a concerning finding for a 10-hour-old newborn. In the early hours of life, the frequency of voids may vary, but the baby should have an increasing number of wet diapers in the following days.
A nurse is caring for a client who gave birth 4 hr ago and is experiencing excessive vaginal bleeding. Which of the following actions should the nurse plan to take first?
Explanation
Choice C rationale:
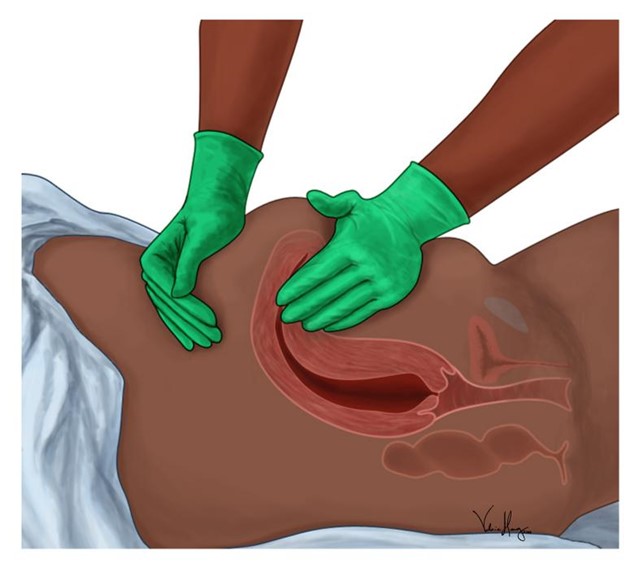
The nurse should first massage the client's fundus to address the excessive vaginal bleeding. Massaging the fundus helps the uterus contract and prevents further bleeding. Excessive postpartum bleeding may indicate uterine atony, which is a leading cause of postpartum hemorrhage. The nurse should apply gentle pressure to the fundus to promote uterine contractions and reduce bleeding.
Choice A rationale:
Elevating the client's legs to a 30° angle (Trendelenburg position) is not the priority action in this situation. Fundal massage takes precedence because it directly addresses the cause of the excessive bleeding. While Trendelenburg position might be used in some situations to increase blood flow to vital organs, it is not the first-line intervention for postpartum bleeding.
Choice B rationale:
Inserting an indwelling urinary catheter is not the priority action for excessive vaginal bleeding. While monitoring urine output is essential, the immediate concern is controlling the bleeding by massaging the fundus.
Choice D rationale:
Initiating an infusion of oxytocin may be indicated if fundal massage alone is insufficient to control bleeding. However, massaging the fundus should be the first action taken to promote uterine contractions. Oxytocin can be administered afterward, if needed, under the direction of a healthcare provider.
A nurse is caring for a client who is in the transition phase of labor. Which of the following actions should the nurse take?
Explanation
Choice D rationale:
During the transition phase of labor, the nurse should encourage the client to use a pant- blow breathing pattern. The transition phase is intense, and pant-blow breathing (a form of controlled breathing) can help the client manage the pain and reduce anxiety. Panting during contractions allows the client to focus on short, shallow breaths, which can be more effective than deep breathing during this stage.
Choice A rationale:
Assisting the client to void every 3 hours is important during labor, but it is not specific to the transition phase. The nurse should encourage the client to void regularly during the entire labor process to prevent bladder distension and facilitate the descent of the baby. However, during the transition phase, the client may be more focused on contractions and may not need reminders to void every 3 hours.
Choice B rationale:
Monitoring contractions every 30 minutes is not appropriate during the transition phase of labor. The transition phase is characterized by frequent and strong contractions, and continuous monitoring of contractions is usually required during this phase to ensure fetal well-being and progress in labor.
Choice C rationale:
Placing the client into a lithotomy position is not appropriate during the transition phase of labor. The lithotomy position, where the client lies on their back with legs raised and supported in stirrups, is often used during the pushing phase. During the transition phase, it is more common for the client to be in an upright or semi-reclining position to facilitate the descent of the baby through the birth canal.
A nurse is providing teaching about newborn safety to a client who is being admitted for induction of labor. Which of the following client statements indicates an understanding of the teaching?
Explanation
Choice A rationale:
The client's statement, "I will check the identification badge of anyone who removes my baby from our room,” indicates an understanding of newborn safety. This statement shows the client's awareness of the importance of verifying the identity of anyone handling their baby before allowing them to be taken out of the room. Checking identification badges helps ensure that only authorized personnel, such as nurses or hospital staff, are allowed to handle the newborn, reducing the risk of unauthorized individuals taking the baby.
Choice B rationale:
This statement is incorrect and does not demonstrate an understanding of newborn safety. Including a photo of the baby along with public birth announcements to social media can compromise the baby's security and privacy. It may expose sensitive information about the baby's location and identity, making the baby vulnerable to potential risks.
Choice C rationale:
This statement is incorrect as it poses a safety risk to the newborn. Allowing the baby to sleep on the bed when the client is in the shower increases the risk of falls or suffocation. The baby should always be placed in a safe sleep environment, such as a crib or bassinet, to minimize the risk of accidents.
Choice D rationale:
This statement is incorrect and does not reflect an understanding of newborn safety. Nurses should not carry the baby in their arms to the nursery. Instead, they should use a crib or an infant carrier to transport the baby safely.
A nurse is teaching a pregnant client who is Rh-negative about Rh(D) immune globulin. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A rationale:
This statement is incorrect. The client should receive Rh(D) immune globulin (RhoGAM) if they are Rh-negative and their partner's Rh status is unknown or Rh-positive. This prevents the development of Rh antibodies in the mother's blood, which could be harmful in future pregnancies if the baby is Rh-positive.
Choice B rationale:
This statement is incorrect. Rh(D) immune globulin is administered to an Rh-negative mother within 72 hours after delivery if the baby is Rh-positive. This is done to prevent the mother from developing Rh antibodies that could affect subsequent pregnancies.
Choice C rationale:
This statement is incorrect. There is no restriction on receiving other immunizations after receiving Rh(D) immune globulin. The shot only protects against Rh incompatibility and does not interfere with other immunizations.
Choice D rationale:

This statement is correct. Rh(D) immune globulin can be given after birth to an Rh-negative mother with an Rh-positive baby. This helps protect the mother's future pregnancies from the potential harmful effects of Rh incompatibility.
A nurse is caring for a client who has a prescription for ibuprofen to treat postpartum cramping. Which of the following questions should the nurse ask prior to administering the medication? (Select all that apply.)
Explanation
Choice A rationale:
The nurse should ask the client if they are taking over-the-counter medications because ibuprofen is also available over-the-counter. It is important to know if the client is already taking ibuprofen or any other non-prescription pain relievers to avoid potential drug interactions or overdosing.
Choice B rationale:
The nurse should inquire about the client's history of gastric problems because ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can cause gastrointestinal irritation and bleeding. If the client has a history of gastric ulcers or other gastric issues, the nurse may need to consider an alternative pain relief option.
Choice C rationale:
The question about contraception is not directly related to administering ibuprofen for postpartum cramping. It is essential to provide adequate pain relief, but the method of contraception the client plans to use is not relevant to the administration of the medication.
Choice D rationale:
Although high blood pressure is a concern with certain medications, ibuprofen is not contraindicated for clients with hypertension. However, it is always good practice to monitor blood pressure when administering any new medication, especially in the postpartum period.
Choice E rationale:
The presence of cataracts is not relevant to the administration of ibuprofen for postpartum cramping. Cataracts are a concern with eye health and are not associated with taking this pain medication.
A nurse is caring for a client who is receiving oxytocin to augment labor. The nurse notes recurrent variable decelerations of the FHR. Which of the following actions should the nurse take first?
Explanation
Choice A rationale:
This action is not the first priority. Recurrent variable decelerations of the fetal heart rate (FHR) indicate umbilical cord compression, and initiating an amnioinfusion may be necessary to relieve the compression. However, before taking this step, the nurse should address the immediate needs of the baby.
Choice B rationale:
This is the correct first action. Administering oxygen at 10 L/min via a nonrebreather face mask is a priority intervention to improve fetal oxygenation. The variable decelerations may be caused by temporary decreases in oxygen supply to the baby, and providing supplemental oxygen to the mother can increase oxygenation to the fetus.
Choice C rationale:
Discontinuing the oxytocin infusion is an appropriate intervention but not the first action. The nurse should first address the fetal well-being by administering oxygen and assessing the response before considering discontinuation of oxytocin.
Choice D rationale:
Placing the client in a left lateral position is a helpful measure to improve blood flow to the placenta and fetal oxygenation. However, it is not the first action to take in this situation. Administering oxygen is more critical, and the left lateral position can be considered after oxygenation has been addressed.
A nurse is providing teaching to a group of women about risk factors for ovarian cancer. Which of the following risk factors should the nurse include? (Select all that apply.)
Explanation
Choice A rationale:
Nulliparity (never having given birth) is a known risk factor for ovarian cancer. Women who have never had children have a higher risk compared to those who have. This is believed to be associated with the number of ovulatory cycles a woman experiences throughout her lifetime.
Choice B rationale:
History of breastfeeding does not have a direct link to ovarian cancer risk. In fact, breastfeeding is associated with a reduced risk of both breast and ovarian cancer due to hormonal changes that occur during lactation.
Choice C rationale:
Previous use of oral contraceptives is associated with a decreased risk of ovarian cancer. Women who have used birth control pills have a lower risk compared to those who have never used them. The protective effect is believed to be due to the suppression of ovulation.
Choice D rationale:
History of breast cancer is not a risk factor for ovarian cancer. Although both cancers are related to the reproductive system, they have distinct risk factors and characteristics.
Choice E rationale:
Hormone replacement therapy (HRT) is a potential risk factor for ovarian cancer, especially long-term use. The hormones used in HRT can affect hormone levels and may increase the risk of ovarian cancer.
A nurse is caring for a client who is experiencing preterm labor and has a new prescription for terbutaline. Which of the following findings is a contraindication for the administration of this medication?
Explanation
Choice A rationale:
Terbutaline is a medication commonly used to stop preterm labor by relaxing the uterine muscles. However, it is contraindicated in clients with heart disease or certain cardiac conditions, as it can cause cardiovascular side effects such as increased heart rate, palpitations, and potential arrhythmias.
Choice B rationale:
Cervical dilation of 2 cm is a typical sign of preterm labor, and the prescription for terbutaline is appropriate to prevent further cervical dilation and delay delivery.
Choice C rationale:
A gestational age of 34 weeks indicates preterm labor, which is precisely the scenario where terbutaline would be administered to halt labor progression and extend the pregnancy.
Choice D rationale:
Allergy to penicillin is unrelated to the administration of terbutaline, as they are different medications with distinct mechanisms of action and side effects.
A nurse is providing teaching to a client who has fibrocystic breast changes and is experiencing breast discomfort during menstruation. Which of the following instructions should the nurse include?
Explanation
Choice A rationale:
Increasing potassium intake is not specifically associated with relieving breast discomfort during menstruation. There is no established link between potassium intake and fibrocystic breast changes.
Choice B rationale:
Increasing fluid intake is generally beneficial for overall health, but it is not a specific recommendation for managing breast discomfort during menstruation. It may not have a direct impact on fibrocystic breast changes.
Choice C rationale:
Decreasing sodium intake before menstruation is a relevant instruction for managing breast discomfort associated with fibrocystic breast changes. High sodium intake can lead to water retention and breast swelling, exacerbating discomfort.
Choice D rationale:
Daily fiber intake is important for bowel health but is not directly related to managing breast discomfort during menstruation or fibrocystic breast changes.
A nurse is caring for a client who is postpartum, has a deep-vein thrombosis, and is receiving heparin therapy via subcutaneous injections. Which of the following actions should the nurse take?
Explanation
Choice A rationale:
The nurse should not request a prescription for PRN aspirin from the provider. Heparin is an anticoagulant medication, and adding aspirin can increase the risk of bleeding complications.
Choice B rationale:
The nurse should not massage the injection site thoroughly following administration. Massaging the injection site can cause bruising and irritation, increasing the risk of bleeding.
Choice C rationale:
This is the correct choice. Heparin is contraindicated during breastfeeding due to its potential to pass into breast milk and cause bleeding in the newborn.
Choice D rationale:
The nurse should not administer the injection in the client's abdomen. Subcutaneous heparin injections are typically given in areas with a layer of fat, such as the back of the arms or abdomen. However, the abdomen is avoided during the postpartum period because of the risk of hematoma formation at the site of injection.
A nurse is caring for a client who is in labor and has an epidural for pain control. Which of the following clinical manifestations is an adverse effect of epidural anesthesia?
Explanation
Choice A rationale:
Polyuria is not an adverse effect of epidural anesthesia. It is unrelated to this type of pain control.
Choice B rationale:
Hypertension is not an adverse effect of epidural anesthesia. Epidurals can actually cause a decrease in blood pressure due to vasodilation.
Choice C rationale:
This is the correct choice. Pruritus, or itching, is a common adverse effect of epidural anesthesia caused by the release of histamines from local anesthetics.
Choice D rationale:
Dry mouth is not an adverse effect of epidural anesthesia. Dry mouth is more commonly associated with general anesthesia or medications with anticholinergic effects.
A nurse is caring for a newborn whose father voices concerns about his ability to bond with his baby. Which of the following actions should the nurse take to facilitate bonding? (Select all that apply.)
Explanation
Choice A rationale:
Pointing out to the father that the newborn turns toward his voice helps him understand that the baby is already responding to him, promoting bonding.
Choice B rationale:
Asking the father why he is concerned about bonding with the newborn allows the nurse to address specific fears or misconceptions and provide appropriate support.
Choice C rationale:
Encouraging the father to touch and stroke the newborn's skin promotes physical contact and enhances the bonding process.
Choice D rationale:
Demonstrating diapering and swaddling techniques for the father helps him feel more confident in caring for his baby and fosters bonding through caregiving activities.
Choice E rationale:
Encouraging the father to lay the newborn beside him while both are sleeping promotes skin- to-skin contact and allows for bonding during restful moments. However, the nurse should ensure that safety measures are followed to prevent accidental suffocation. By following these actions, the nurse can support the father's bonding with his newborn and facilitate a positive and nurturing parent-infant relationship.
A nurse is assessing a newborn who was born vaginally with vacuum extractor assistance. The nurse notes swelling over the newborn's head that crosses the suture line. The nurse should identify the swelling as which of the following findings?
Explanation
Choice A rationale:
Nevus flammeus, also known as a "port-wine stain,” is a type of birthmark characterized by a flat, pink, or reddish-purple patch on the skin. It does not involve swelling over the head.
Choice B rationale:
Caput succedaneum is a common condition in newborns born vaginally, especially with vacuum extraction. It presents as diffuse scalp swelling due to fluid accumulation beneath the scalp's skin. However, caput succedaneum does not cross the suture line, which differentiates it from the swelling described in the question.
Choice C rationale:
Cephalohematoma is a collection of blood between the periosteum and the skull bone. It typically appears as a localized swelling over the newborn's head, often crossing the suture lines. The bleeding results from the rupture of blood vessels during birth trauma.

Cephalohematoma usually resolves spontaneously over several weeks to months.
Choice D rationale:
Erythema toxicum is a common rash seen in newborns. It appears as small, yellow or white papules surrounded by a reddened base. It is a benign and self-limiting condition and is not related to the described swelling over the head.
A nurse is discussing recommendations for daily nutrient intake during pregnancy with a client who is at 10 weeks of gestation. For which of the following nutrients should the nurse instruct the client to increase intake during pregnancy?
Explanation
Choice A rationale:
Vitamin E is essential for cell function and acts as an antioxidant. While vitamin E is important during pregnancy, there is no specific recommendation to increase its intake during gestation. The recommended daily allowance (RDA) for vitamin E during pregnancy is 15 mg.
Choice B rationale:
Vitamin D is crucial for calcium absorption and bone health. However, it is not explicitly advised to increase vitamin D intake during pregnancy, and it largely depends on the individual's baseline vitamin D levels. The RDA for vitamin D during pregnancy is 600 IU.
Choice C rationale:
Fiber is important for maintaining bowel regularity, but there is no need to significantly increase its intake during pregnancy. Pregnant individuals are advised to consume a well- balanced diet with sufficient fiber. The RDA for fiber during pregnancy is 28 grams.
Choice D rationale:
Calcium is vital for the development of the fetal skeleton and is necessary for the proper functioning of muscles and nerves. During pregnancy, the recommended intake of calcium increases to support the growing baby's needs. The RDA for calcium during pregnancy is 1000 mg.
A nurse is caring for a client who is at 14 weeks of gestation and has hyperemesis gravidarum. Which of the following medications should the nurse plan to administer?
Explanation
Choice A rationale:
Digoxin is a cardiac glycoside and is primarily used in the management of certain heart conditions, such as heart failure and atrial fibrillation. It is not indicated for hyperemesis gravidarum, which is severe and persistent vomiting during pregnancy.
Choice B rationale:
Calcium gluconate is a mineral supplement used to treat calcium deficiencies. It is not a standard treatment for hyperemesis gravidarum.
Choice C rationale:
Vitamin Bs (B6 and B12) are commonly used to manage hyperemesis gravidarum. Vitamin B6, also known as pyridoxine, has been shown to alleviate nausea and vomiting during pregnancy. Vitamin B12 may also be administered to help manage symptoms. Both vitamins are safe to use during pregnancy.
Choice D rationale:
Propranolol is a beta-blocker used to treat high blood pressure, heart conditions, and migraines. It is not recommended for managing hyperemesis gravidarum and is generally avoided during pregnancy due to potential risks to the developing fetus.
A nurse is developing a plan of care for a newborn who has hyperbilirubinemia and a prescription for phototherapy. Which of the following interventions should the nurse include?
Explanation
Choice A rationale:
Checking the newborn's temperature every 8 hours is not directly related to managing hyperbilirubinemia or phototherapy. Monitoring the newborn's temperature is important, but it should be done more frequently, especially during phototherapy, as infants are at risk of developing hypothermia.
Choice B rationale:
Applying moisturizing lotion to the newborn's skin every 4 hours is not a necessary intervention for hyperbilirubinemia or phototherapy. While skin care is important for all newborns, it is not a specific intervention for this condition.
Choice C rationale:
Giving the newborn 1 oz of glucose water every 4 hours is not an appropriate intervention for hyperbilirubinemia. Glucose water is not a recommended treatment for this condition.
Instead, phototherapy helps break down the bilirubin and promote its elimination from the body.
Choice D rationale:
Repositioning the newborn every 2 to 3 hours is the correct intervention. Repositioning helps ensure even exposure of the baby's skin to the phototherapy lights, maximizing its effectiveness in reducing bilirubin levels. Additionally, repositioning prevents pressure ulcers and promotes comfort for the infant during treatment.
A nurse is assessing a client who is at 31 weeks of gestation. Which of the following findings should the nurse identify as an indication of a potential prenatal complication?
Explanation
Choice A rationale:
Periodic tingling of fingers is a common symptom during pregnancy and is often related to hormonal changes and increased fluid retention. While it can be uncomfortable, it is not necessarily an indication of a potential prenatal complication.
Choice B rationale:
Absence of clonus is not an abnormal finding during pregnancy. Clonus is a series of involuntary muscle contractions and relaxations and is generally not expected during a routine assessment.
Choice C rationale:
Leg cramps are a common complaint during pregnancy and are usually caused by changes in calcium and magnesium levels. While they can be uncomfortable, they are not typically considered an indication of a potential prenatal complication.
Choice D rationale:
Blurred vision can be an indication of preeclampsia, a serious condition that can occur during pregnancy. Preeclampsia is characterized by high blood pressure and damage to organs, often affecting the eyes, kidneys, and liver. It is crucial for the nurse to recognize this symptom and promptly inform the healthcare provider for further evaluation and management.
A nurse is caring for a client who is at 38 weeks of gestation and is experiencing continuous abdominal pain and vaginal bleeding. The client has a history of cocaine use. The nurse should identify that the client is likely experiencing which of the following complications?
Explanation
Choice A rationale:
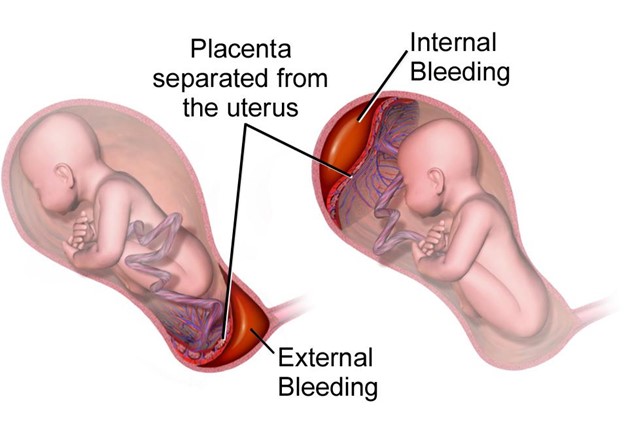
Continuous abdominal pain and vaginal bleeding in a client with a history of cocaine use are indicative of abruptio placentae. Abruptio placentae is a medical emergency where the placenta detaches from the uterine wall before delivery, leading to severe bleeding and abdominal pain. Immediate medical intervention is necessary to prevent complications for both the mother and the baby.
Choice B rationale:
Hydatidiform mole is a gestational trophoblastic disease that occurs due to an abnormal pregnancy. It is not associated with continuous abdominal pain and vaginal bleeding. Instead, clients with this condition often present with vaginal bleeding and a grape-like cluster of cysts in the uterus.
Choice C rationale:
Preterm labor involves regular uterine contractions and cervical changes before 37 weeks of gestation. While preterm labor can cause abdominal discomfort, it is not usually described as continuous abdominal pain. Vaginal bleeding is not a typical symptom of preterm labor.
Choice D rationale:
Placenta previa is a condition where the placenta covers the opening of the cervix. It can cause painless vaginal bleeding, but it is not usually associated with continuous abdominal pain. Clients with placenta previa often experience sudden, painless bleeding later in pregnancy.
A nurse is caring for a client who is at 38 weeks of gestation and is experiencing continuous abdominal pain and vaginal bleeding. The client has a history of cocaine use. The nurse should identify that the client is likely experiencing which of the following complications?
Explanation
Choice A rationale:
The client is experiencing continuous abdominal pain and vaginal bleeding, which are key signs of abruptio placentae. This condition occurs when the placenta prematurely separates from the uterine wall before the baby is born, leading to bleeding and potential fetal distress. The history of cocaine use can be a risk factor for abruptio placentae, as cocaine use may lead to vasoconstriction and reduced blood flow to the placenta.
Choice B rationale:
Hydatidiform mole is not likely in this case because it presents with symptoms such as vaginal bleeding and a "grape-like” mass on ultrasound. The continuous abdominal pain is not typical for a hydatidiform mole.
Choice C rationale:
Preterm labor is not the likely complication in this scenario because the client is at 38 weeks of gestation, which is considered full term. Preterm labor refers to labor that occurs before 37 weeks of gestation.
Choice D rationale:
Placenta previa is not the likely complication as it presents with painless vaginal bleeding in the third trimester, and the abdominal pain described in the question suggests a different condition.
Sign Up or Login to view all the 82 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

