ATI MATERNAL NEWBORN 2019 EXAM 3
Total Questions : 39
Showing 25 questions, Sign in for moreA nurse is teaching a client and her partner about the technique of counter pressure during labor. Which of the following statements by the nurse is appropriate?
Explanation
Counter pressure is a technique used to help alleviate the pain and discomfort of contractions during labor. It involves applying pressure to certain areas of the body to help relieve pain and tension. One of the most common areas for counter pressure is the lower back, as this area often experiences significant pain and discomfort during contractions.
Option A is incorrect because the top of the uterus is not an appropriate area for counter pressure during labor.
Option C is also incorrect as applying pressure between the thumb and index finger is a technique used to relieve headache pain, not labor pain.
Option D is incorrect because upward pressure on the lower abdomen is not an effective way to relieve the pain of contractions.
A nurse is assessing a client who is at 32 weeks of gestation and is receiving magnesium sulfate via continuous IV infusion. Which of the following findings should the nurse report to the provider?
Explanation
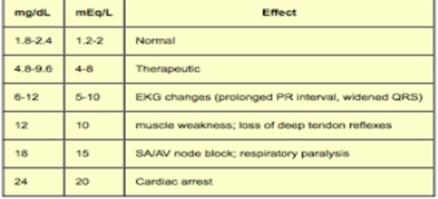
Magnesium sulfate is a medication used to prevent and treat seizures in clients with preeclampsia and eclampsia. It is also used to stop preterm labor. However, magnesium sulfate can cause a variety of side effects, including decreased reflexes, which can be a sign of magnesium toxicity. Therefore, it is important for the nurse to monitor the client for signs of toxicity.
Option A is incorrect because a decrease in the frequency of contractions is a desired effect of magnesium sulfate when it is used to stop preterm labor.
Option B is also incorrect because although a blood pressure of 150/100 mm Hg is elevated, it is not an unexpected finding in a client with preeclampsia, and it may actually be considered an improvement if the client's blood pressure was previously higher.
Option D is incorrect because a urinary output of 35 mL/hr is within the normal range for an adult.
A nurse is caring for a client who is at 32 weeks of gestation and has gestational diabetes mellitus. Which of the following findings should the nurse report to the provider?
Explanation
Gestational diabetes mellitus (GDM) is a condition in which a pregnant woman develops high blood sugar levels during pregnancy. Complications of GDM can include macrosomia (a larger-than-average baby), polyhydramnios (an excessive amount of amniotic fluid), and preterm labor. One of the ways to monitor for these complications is through regular fundal height measurements. A fundal height measurement that is significantly larger than expected can indicate macrosomia or polyhydramnios, which can lead to complications during delivery.
Option B is incorrect because a fasting blood glucose of 90 mg/dL is within the normal range for a non-pregnant individual, and it is lower than the target range for a pregnant woman with GDM.
Option C is also incorrect because a fetal movement count of 12 in 1 hour is within the normal range.
Option D is incorrect because non-pitting pedal edema is a common finding in pregnancy and is not typically a cause for concern.
A nurse is reviewing the chart of a client who is 2 days postpartum following a vaginal delivery and reports constipation. Which of the following findings should the nurse identify as a contraindication to the use of a suppository?
Explanation
Constipation is a common problem for clients who have recently given birth, and suppositories are a common treatment option for constipation. However, suppositories are not appropriate for all clients. Certain conditions can be a contraindication to the use of suppositories, and the nurse should be aware of these conditions.
The nurse should identify that a third-degree perineal laceration is a contraindication to the use of a suppository, as it may cause further trauma to the already injured area. In this case, alternative treatments such as stool softeners or oral laxatives may be more appropriate for the client.
Option A is incorrect because although abdominal distention can be a sign of constipation, it is not a contraindication to the use of a suppository.
Option C is also incorrect because vaginal candidiasis is not a contraindication to the use of a suppository. In fact, suppositories are sometimes used to treat vaginal candidiasis.
Option D is also incorrect because afterpains are not a contraindication to the use of a suppository.
A nurse is caring for a client who is at 30 weeks of gestation and receiving magnesium sulfate for preeclampsia. The nurse should recognize which of the following manifestations as an adverse reaction to the medication?
Explanation
Magnesium sulfate is a medication commonly used to treat preeclampsia, a pregnancy-related condition characterized by high blood pressure and damage to other organ systems, such as the kidneys. However, magnesium sulfate can also cause adverse reactions, and the nurse should be aware of these reactions.
The nurse should recognize that a urine output of 20 mL/hr is a manifestation of an adverse reaction to magnesium sulfate, as magnesium sulfate can cause decreased urine output, which can lead to dehydration and electrolyte imbalances. The nurse should promptly report this finding to the provider, as it may require immediate intervention.
Option A is incorrect because hypertension is a symptom of preeclampsia, not an adverse reaction to magnesium sulfate.
Option B is also incorrect because hyperglycemia is not an adverse reaction to magnesium sulfate.
Option C is also incorrect because a respiratory rate of 16/min is within the normal range.
A nurse is providing teaching to a client who is primigravid and is scheduled to have an abdominal ultrasound. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Abdominal ultrasounds are noninvasive imaging tests that use high-frequency sound waves to create images of the internal organs. When an abdominal ultrasound is performed, the client is typically asked to drink water before the test and to hold the urine to ensure that the bladder is full. This full bladder helps to create a clear image of the uterus and the developing fetus.
Option A is incorrect because applying perfumed lotion to the abdomen can interfere with the ultrasound waves and may affect the quality of the images.
Option B is also incorrect because having an empty stomach is not necessary for an abdominal ultrasound.
Option C is also incorrect because a stool softener is not necessary for an abdominal ultrasound.
A nurse is reviewing the electronic medical record of a postpartum client. The nurse should identify which of the following factors places the client at risk for an infection?
Explanation
An episiotomy is a surgical incision made in the perineum to enlarge the vaginal opening during delivery. A midline episiotomy is an incision made in the midline of the perineum, which has been associated with a higher risk of infection than a mediolateral episiotomy.
Option B is incorrect because meconium-stained fluid does not necessarily place the postpartum client at increased risk for infection. However, it can indicate that the fetus was stressed during delivery and may require additional monitoring after birth.
Option C is also incorrect because gestational hypertension, while it can lead to complications during pregnancy and delivery, does not necessarily place the postpartum client at increased risk for infection.
Option D is also incorrect because placenta previa is a condition in which the placenta is low-lying and can partially or completely cover the cervix. It can cause bleeding during pregnancy and delivery but does not necessarily place the postpartum client at increased risk for infection.
A nurse is caring for a client who is in labor and just received epidural anesthesia. The client's blood pressure is 90/50 mm Hg. Which of the following actions should the nurse take?
Explanation
Epidural anesthesia can cause hypotension in the mother, which can decrease blood flow to the fetus. Turning the client onto their side can help to improve blood flow to the fetus by reducing the pressure of the uterus on the vena cava and increasing venous return to the heart.
Option B is incorrect because an amnio-infusion is not indicated for hypotension related to epidural anesthesia.
Option C is also incorrect because naloxone is a medication used to reverse the effects of opioid medications and would not be appropriate for treating hypotension related to epidural anesthesia.
Option D is partially correct but does not address the immediate need to improve blood flow to the fetus. The nurse should monitor the client's blood pressure regularly but should also take immediate action to turn the client onto their side to improve blood flow.
A nurse is caring for a client who has pre-gestational diabetes mellitus. Which of the following clinical findings should indicate to the nurse the client has hyperglycemia?
Explanation
Increased urination, or polyuria, is a common clinical finding in clients with hyperglycemia. High levels of glucose in the blood can cause the kidneys to work harder to filter out the excess glucose, resulting in increased urine output.
Option A, dizziness, is a nonspecific symptom and can occur for a variety of reasons, including hypoglycemia, hyperglycemia, or dehydration.
Option C, sweating, is also a nonspecific symptom and can occur for a variety of reasons, including hypoglycemia, hyperglycemia, or anxiety.
Option D, double vision, is a symptom that can occur in severe cases of hyperglycemia or diabetic ketoacidosis. However, it is not a common or early symptom of hyperglycemia.
A nurse is assessing the results of a nonstress test for an antepartal client at 35 weeks of gestation. Which of the following findings should indicate to the nurse the need for further diagnostic testing?
Explanation
The nonstress test is a screening tool that assesses fetal well-being. It is performed by monitoring the fetal heart rate (FHR) and uterine contractions (UC) while the client is at rest. The test is considered reactive if there are two or more accelerations of the FHR that reach a certain level above the baseline and last for at least 15 seconds over a 20-min period.
The presence of irregular contractions that are not felt by the client is a finding that is concerning because it could be a sign of uterine hyperstimulation, which can lead to fetal distress. Further diagnostic testing may be needed to assess fetal well-being in this situation.
Option A indicates that the client felt fetal movements during the testing period. This is a reassuring finding because fetal movements are a sign of fetal well-being.
Option B indicates that there were no late decelerations in the FHR with uterine contractions. This is a reassuring finding because late decelerations are a sign of fetal compromise.
Option C indicates that there was an acceleration of the FHR in response to fetal movement. This is a reassuring finding because it indicates that the fetus is capable of responding to stimuli.
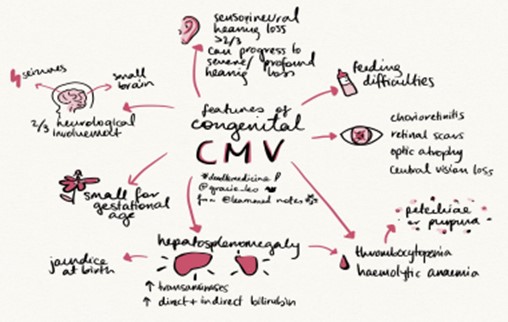
A nurse is assessing a newborn whose mother had a primary cytomegalovirus (CMV) infection during pregnancy. The newborn acquired CMV transplacentally. Which of the following findings should the nurse expect the newborn to exhibit?
Explanation
Cytomegalovirus (CMV) is a viral infection that can cause serious health problems for newborns if acquired in utero. Some newborns may appear asymptomatic at birth but later develop complications such as hearing loss, intellectual disability, and vision problems. The virus can be transmitted through bodily fluids such as saliva, urine, and breast milk, and can be especially dangerous for premature infants or those with weakened immune systems. While macrosomia (large body size) and urinary tract infections are possible complications in newborns, they are not typically associated with CMV. Cataracts may also occur in infants with congenital CMV, but hearing loss is a more common complication.
A nurse is caring for a client who is postpartum and experiencing hypovolemic shock. Which of the following findings should the nurse expect?
Explanation
Hypovolemic shock is caused by a significant loss of blood or fluids, resulting in decreased tissue perfusion and oxygenation. Cool, clammy skin is a classic symptom of hypovolemic shock, indicating that the body is redirecting blood flow to vital organs. A respiratory rate of18/min is within normal limits. Bounding pulses are associated with conditions such as hyperthyroidism or aortic regurgitation. A urinary output of 30 mL/hr is low, but it is not necessarily indicative of hypovolemic shock on its own.
A nurse is providing teaching to a client who is 2 days postpartum and wants to continue using her diaphragm for contraception. Which of the following instructions should the nurse include?
Explanation
The size and shape of the cervix and vagina can change after childbirth, which can affect the fit and effectiveness of the diaphragm. The nurse should instruct the client to see her healthcare provider to be refitted for a new diaphragm.
Option A is incorrect because storing the diaphragm in sterile water is not necessary or recommended. The diaphragm should be cleaned with soap and water and allowed to air dry.
Option B is incorrect because the diaphragm should be removed no sooner than 6 hours after intercourse and can be left in place for up to 24 hours.
Option C is incorrect because oil-based vaginal lubricants can damage latex diaphragms, so water-based lubricants should be used instead.
A nurse is discussing risk factors of postpartum hemorrhage with a newly licensed nurse. Which of the following conditions is a risk factor for postpartum hemorrhage that the nurse should include in the teaching?
Explanation
Retained placental fragments is a risk factor for postpartum hemorrhage. When placental fragments remain in the uterus, they prevent the uterus from contracting down and can cause significant bleeding. Pregnancy-induced hypertension, oligohydramnios, and meconium-stained fluid are not considered risk factors for postpartum hemorrhage.

A nurse in a newborn nursery is receiving a change-of-shift report for four newborns. Which of the following newborns should the nurse assess first?
Explanation
The newborn who is 10 hr old and has new onset tachypnea should be assessed first as this could indicate a respiratory distress, which requires immediate intervention. The other options are concerning but not as urgent as respiratory distress.
A newborn with a short frenulum and difficulty breastfeeding can be assessed after the respiratory distress is addressed.
A newborn who is 24 hr old and has not had a meconium stool should be assessed for bowel sounds and abdominal distension, but it is not as urgent as respiratory distress. A newborn who is 30 hr old and has blood-tinged discharge in her diaper can be assessed after the respiratory distress is addressed. The blood-tinged discharge could be due to the infant's mother passing her own vaginal blood to the infant or a minor vaginal laceration during delivery.
A nurse in a newborn nursery is receiving a change-of-shift report for four newborns. Which of the following newborns should the nurse assess first?
Explanation
The newborn who is 10 hr old and has new onset tachypnea should be assessed first as this could indicate a respiratory distress, which requires immediate intervention. The other options are concerning but not as urgent as respiratory distress.
A newborn with a short frenulum and difficulty breastfeeding can be assessed after the respiratory distress is addressed.
A newborn who is 24 hr old and has not had a meconium stool should be assessed for bowel sounds and abdominal distension, but it is not as urgent as respiratory distress. A newborn who is 30 hr old and has blood-tinged discharge in her diaper can be assessed after the respiratory distress is addressed. The blood-tinged discharge could be due to the infant's mother passing her own vaginal blood to the infant or a minor vaginal laceration during delivery.
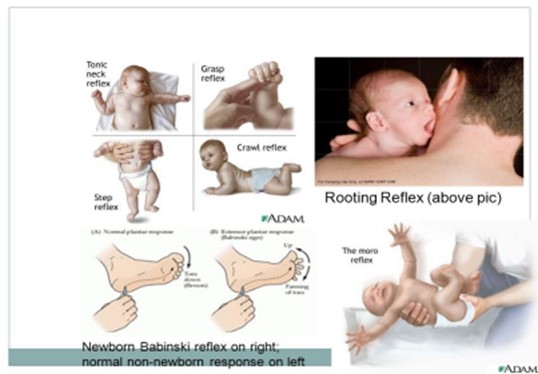
A nurse is performing an assessment of a newborn's Babinski reflex. Which of the following findings should the nurse expect?
Explanation
Dorsiflexion of the great toe is the expected finding for the Babinski reflex in a newborn. Babinski is positive in newborns up to the age of 2 years.
A nurse is observing an adolescent client who is offering her newborn a bottle while he is lying in the bassinet. When the nurse offers to pick the newborn up and place him in the client's arms, the mother states, "No, the baby is too tired to be held." Which of the following actions should the nurse take?
Explanation
It is important to ensure the safety of the newborn, and in this situation, the adolescent mother is putting the newborn at risk by leaving him unattended while feeding. Offering to take the newborn to the nursery allows him to finish feeding in a safe environment while also allowing the nurse to assess his feeding and ensure he is receiving adequate nutrition. It is important to provide education to the mother on safe feeding practices, but at this moment, ensuring the safety of the newborn is the priority.
A nurse is planning care for a client who is pregnant and has HIV. Which of the following actions should the nurse include in the plan of care?
Explanation
The purpose of bathing the newborn before initiating skin-to-skin contact is to decrease the risk of transmission of the virus from the mother to the newborn. Instructing the client to stop taking the antiretroviral medications at 32 weeks of gestation is incorrect as these medications should be taken throughout pregnancy to decrease the risk of transmission to the fetus.
Using a fetalscalp electrode during labor and delivery is also not an appropriate action as it increases the risk of transmission of the virus to the newborn. Administering a pneumococcal immunization to the newborn within 4 hours following birth is not specific to HIV positive newborns and is not related to preventing transmission of the virus.
A nurse is providing teaching to a client who is receiving medroxyprogesterone IM for contraception. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Medroxyprogesterone is an injectable form of contraception that is given every 12 to 13 weeks. Therefore, the correct statement is that the client will need to return to the clinic in 8 weeks for her next injection.
Option B is incorrect because the client receives only one shot each time she receives this medication.
Option C is incorrect because medroxyprogesterone can decrease bone density, so the client should increase calcium intake.
Option D is incorrect because spotting is a common side effect of medroxyprogesterone, and the client should not discontinue the medication unless advised to do so by her healthcare provider.
A nurse is planning care immediately following birth for a newborn who has a myelomeningocele that is leaking cerebrospinal fluid. Which of the following actions should the nurse include in the plan of care?
Explanation
The priority action in this scenario is to prevent infection. Cleansing the site with povidone-iodine can help reduce the risk of infection. Rectal temperature monitoring and administration of antibiotics may be necessary if infection is suspected, but preventing infection is the priority. Surgical closure may be necessary, but this is not an immediate concern.
A nurse is caring for a client who is in the latent phase of the first stage of labor and is in pain. Which of the following nursing interventions are appropriate to reduce pain? (Select all that apply.)
Explanation
Administering 70% nitrous oxide mixed with oxygen is a common pain management option for laboring clients.
Applying counterpressure to the sacral area can help alleviate back pain during labor. Sitting in a tub of warm water, also known as hydrotherapy, can help reduce pain and promote relaxation during labor.
Ambulating the client may not be feasible or safe during the latent phase of labor when contractions are less frequent and intense.
Performing Leopold maneuvers, which involve palpating the mother's abdomen to determine the position of the fetus, does not directly address pain management.
A nurse is providing teaching about the expected effects of magnesium sulfate to a client who is at 28 weeks of gestation and has preeclampsia. Which of the following responses by the nurse is appropriate?
Explanation
Magnesium sulfate is used to prevent seizures in clients with preeclampsia. It works by relaxing the smooth muscles and blocking neuromuscular transmission. While magnesium sulfate can indirectly improve fetal heart rate and tissue perfusion by preventing seizures, it does not directly stabilize the fetal heart rate or increase cardiac output.
A nurse is caring for a client who has hyperemesis gravidarum. Which of the following laboratory tests should the nurse anticipate?
Explanation
The nurse should anticipate a urine ketones test for a client who has hyperemesis gravidarum. This test is used to monitor the client's ketone levels, which can increase as a result of excessive vomiting and nausea that can cause dehydration and malnutrition. The other tests mentioned are not typically associated with hyperemesis gravidarum.
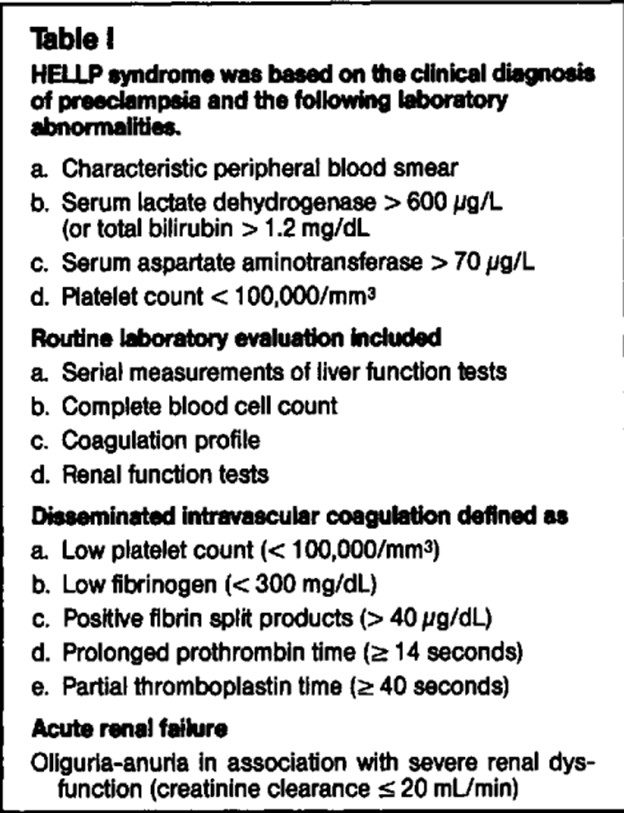
A nurse is reviewing the laboratory results of a newborn. Which of the following findings should the nurse report to the provider?
Explanation
The nurse should report a platelet count of 60,000/mm to the provider as this value is below the normal range and can indicate severe preeclampsia or HELLP syndrome, both of which are serious conditions that require immediate medical intervention. The other values are within normal range for pregnancy.
Sign Up or Login to view all the 39 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

