Ati Maternal Newborn 4
Total Questions : 49
Showing 25 questions, Sign in for moreA nurse suspects that a pregnant client may be experiencing placenta abruption based on assessment of which finding? Select all that apply.
Explanation
Choice A: Absence of pain is not a sign of abruptio placenta. Abruptio placenta is a condition where the placenta separates from the uterine wall before delivery, causing bleeding and pain. The pain is usually severe and constant.
Choice B: Insidious onset is not a sign of abruptio placenta. Abruptio placenta is usually a sudden and acute event that occurs in the third trimester or during labor.
Choice C: Dark red vaginal bleeding is a sign of abruptio placenta. The bleeding is caused by the rupture of blood vessels between the placenta and the uterus. The blood may be dark red because it is old or clotted.
Choice D: Rigid uterus is a sign of abruptio placenta. The uterus becomes hard and tense as a result of the bleeding and contraction of the uterine muscles. This can impair the blood flow to the fetus and cause fetal distress.
Choice E: Absent fetal heart tones is a sign of abruptio placenta. The loss of blood and oxygen to the fetus can cause fetal death or stillbirth. Fetal heart tones can be detected by using a Doppler device or a fetoscope.
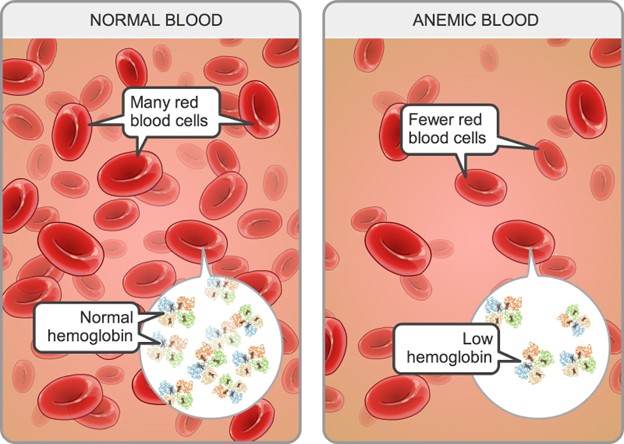
A pregnant client in her second trimester has a hemoglobin level of 11 g/dL. The nurse interprets this as indicating
Explanation
Choice A: Hemodilution of pregnancy is a normal physiological phenomenon that occurs when the plasma volume increases more than the red blood cell mass, resulting in a lower hemoglobin concentration. The normal hemoglobin range for pregnant women in the second trimester is 10.5 to 14 g/dL.
Choice B: A multiple gestation pregnancy may cause a higher hemoglobin level due to increased erythropoietin production by the placenta. The normal hemoglobin range for pregnant women with twins in the second trimester is 12 to 16 g/dL.
Choice C: Greater-than-expected weight gain is not related to hemoglobin level. Weight gain during pregnancy depends on various factors such as pre-pregnancy weight, nutrition, activity level, and fetal growth.
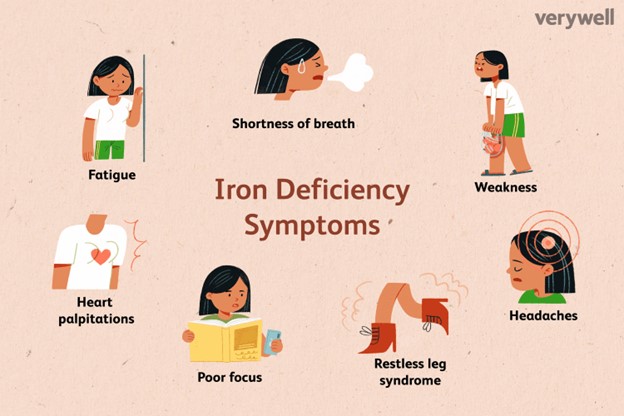
Choice D: Iron-deficiency anemia is a condition where the hemoglobin level is below the normal range due to inadequate iron intake or absorption, blood loss, or increased iron demand. The signs and symptoms of iron-deficiency anemia include fatigue, pallor, weakness, shortness of breath, and pica.
A pregnant client in her second trimester has a hemoglobin level of 11 g/dL. The nurse interprets this as indicating
Explanation
Choice A: Hemodilution of pregnancy is a normal physiological phenomenon that occurs when the plasma volume increases more than the red blood cell mass, resulting in a lower hemoglobin concentration. The normal hemoglobin range for pregnant women in the second trimester is 10.5 to 14 g/dL.
Choice B: A multiple gestation pregnancy may cause a higher hemoglobin level due to increased erythropoietin production by the placenta. The normal hemoglobin range for pregnant women with twins in the second trimester is 12 to 16 g/dL.
Choice C: Greater-than-expected weight gain is not related to hemoglobin level. Weight gain during pregnancy depends on various factors such as pre-pregnancy weight, nutrition, activity level, and fetal growth.
Choice D: Iron-deficiency anemia is a condition where the hemoglobin level is below the normal range due to inadequate iron intake or absorption, blood loss, or increased iron demand. The signs and symptoms of iron-deficiency anemia include fatigue, pallor, weakness, shortness of breath, and pica.
A nurse is providing prenatal care to a pregnant client. At which time would the nurse expect to screen the client for group B streptococcus infection?
Explanation
Choice A: 28 weeks' gestation is too early to screen for group B streptococcus infection. Group B streptococcus (GBS) is a type of bacteria that can cause serious infections in newborns if transmitted from the mother during labor and delivery. The optimal time to screen for GBS is between 35 and 37 weeks' gestation.
Choice B: 32 weeks' gestation is also too early to screen for GBS infection. Screening at this time may not reflect the true colonization status of the mother at the time of delivery, as GBS can be transient or intermittent.
Choice C: 16 weeks' gestation is much too early to screen for GBS infection. Screening at this time has no clinical value, as GBS colonization can change throughout pregnancy.
Choice D: 36 weeks' gestation is the appropriate time to screen for GBS infection. Screening at this time can identify mothers who are colonized with GBS and who need intrapartum antibiotic prophylaxis to prevent neonatal sepsis, pneumonia, and meningitis.
A nurse is providing teaching about nutrition to a client at her first prenatal visit. Which of the following statements by the nurse should be included in the teaching?
Explanation
Choice A: Vitamin E requirements do not decrease during pregnancy due to the increase in body fat. Vitamin E is a fat-soluble vitamin that acts as an antioxidant and protects cell membranes from oxidative damage. The recommended dietary allowance (RDA) for vitamin E during pregnancy is 15 mg/day, which is the same as for non-pregnant women.
Choice B: Prenatal vitamins will meet your need for increased folic acid during pregnancy. Folic acid is a water-soluble vitamin that is essential for DNA synthesis and cell division. Folic acid deficiency can cause neural tube defects in the fetus, such as spina bifida and anencephaly. The RDA for folic acid during pregnancy is 600 mcg/day, which can be obtained from prenatal vitamins and fortified foods.
Choice C: You will not need to double your intake of protein during pregnancy. Protein is a macronutrient that provides amino acids for tissue growth and repair. The RDA for protein during pregnancy is 1.1 g/kg/day, which is only slightly higher than for non-pregnant women (0.8 g/kg/day).
Choice D: You will not need to increase your intake of calcium during pregnancy. Calcium is a mineral that is important for bone health and muscle contraction. Calcium absorption and retention are enhanced during pregnancy, so there is no need to increase the intake above the RDA of 1000 mg/day for women aged 19 to 50 years.
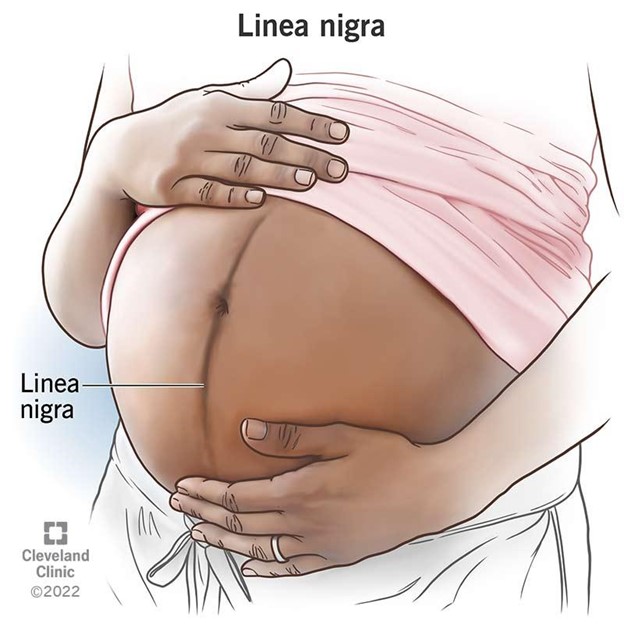
Assessment of a pregnant woman reveals a pigmented line down the middle of her abdomen. The nurse documents this as which finding?
Explanation
Choice A: Striae gravidarum are stretch marks that appear on the abdomen, breasts, or thighs during pregnancy. They are caused by the tearing of the connective tissue in the dermis due to rapid growth or weight gain.
Choice B: Linea nigra is a dark vertical line that runs from the umbilicus to the pubic area. It is caused by increased melanin production due to hormonal changes during pregnancy. This is the correct choice because it matches the description in the question.
Choice C: Vascular spiders are dilated blood vessels that appear on the skin as red or purple spider-like lesions. They are caused by increased estrogen levels and blood volume during pregnancy. They are usually found on the face, neck, chest, or arms.
Choice D: Melasma is a condition that causes brown or gray patches on the face, especially on the forehead, cheeks, nose, or upper lip. It is caused by increased melanin production due to sun exposure and hormonal changes during pregnancy. It is also known as chloasma or the mask of pregnancy.
A client with hyperemesis gravidarum is admitted to the facility after being cared for at home without success. What would the nurse expect to include in the client's plan of care?
Explanation
Choice A: A clear liquid diet is not appropriate for a client with hyperemesis gravidarum, which is a severe form of nausea and vomiting during pregnancy that can lead to dehydration, electrolyte imbalance, and weight loss. A clear liquid diet does not provide adequate calories, protein, vitamins, or minerals for the client and the fetus.
Choice B: Administration of diethylstilbestrol is not indicated for a client with hyperemesis gravidarum. Diethylstilbestrol is a synthetic estrogen that was used in the past to prevent miscarriage and premature birth, but it was found to cause serious adverse effects such as vaginal cancer, infertility, and birth defects in the offspring.
Choice C: Total parenteral nutrition is the correct choice because it provides a complete and balanced source of nutrients through a central venous catheter. It is used for clients who cannot tolerate oral or enteral feeding due to severe gastrointestinal disorders such as hyperemesis gravidarum. It helps to prevent malnutrition, dehydration, and ketosis in the client and the fetus.
Choice D: Nothing by mouth is not a suitable option for a client with hyperemesis gravidarum. It can worsen the condition by causing starvation, acidosis, and ketosis. It can also increase the risk of aspiration pneumonia if the client vomits.
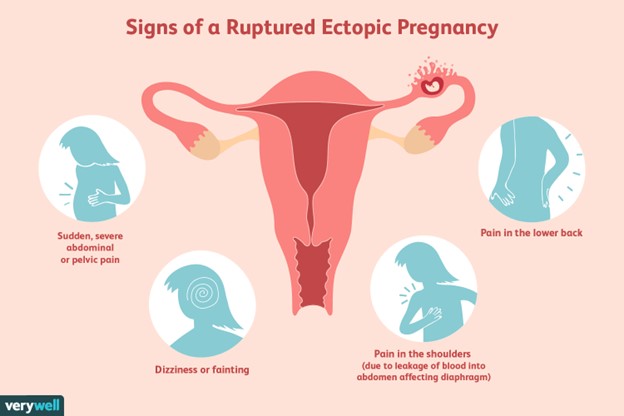
A client is suspected of having a ruptured ectopic pregnancy. Which assessment would the nurse identify as the priority?
Explanation
Choice A reason: Hemorrhage is the most life-threatening complication of a ruptured ectopic pregnancy, as it can lead to hypovolemic shock and death. The nurse should monitor the client's vital signs, blood loss, and level of consciousness, and administer fluids and blood products as ordered.
Choice B reason: Edema is not a common sign of a ruptured ectopic pregnancy, and it is not a priority over hemorrhage. Edema may be caused by other conditions, such as heart failure, kidney disease, or venous insufficiency.
Choice C reason: Infection is a possible complication of a ruptured ectopic pregnancy, but it is not as urgent as hemorrhage. Infection may manifest as fever, chills, malaise, or foul-smelling vaginal discharge. The nurse should administer antibiotics as ordered and monitor the client's temperature and white blood cell count.
Choice D reason: Jaundice is not a typical symptom of a ruptured ectopic pregnancy, and it is not a priority over hemorrhage. Jaundice may indicate liver dysfunction or hemolytic anemia, which are unrelated to ectopic pregnancy. The nurse should assess the client's skin and sclera color, and check the liver enzymes and bilirubin levels.
Upon entering the room of a client who has had a spontaneous abortion, the nurse observes the client crying. Which response by the nurse would be most appropriate?
Explanation
Choice A Reason: This is the correct answer because it is an empathetic and supportive response that acknowledges the client's loss and grief. This is an empathetic and supportive response that acknowledges the client's loss and grief. The other choices are inappropriate because they are insensitive, dismissive, or inaccurate.
Choice B Reason: This is an inappropriate answer because it implies that the nurse does not understand or care about the client's emotional state. It also suggests that the client has no Reason to cry, which is invalidating and hurtful.
Choice C Reason: This is an inappropriate answer because it focuses on the physical pain rather than the emotional pain of the client. It also implies that the nurse wants to avoid dealing with the client's feelings and just give them a medication to make them stop crying.
Choice D Reason: This is an inappropriate answer because it is inaccurate and misleading. A spontaneous abortion, also known as a miscarriage, occurs when a pregnancy ends before 20 weeks of gestation. At this stage, the baby is already formed and has a heartbeat, organs, and limbs. Saying that a baby still wasn't formed in the womb is false and insensitive to the client's loss.
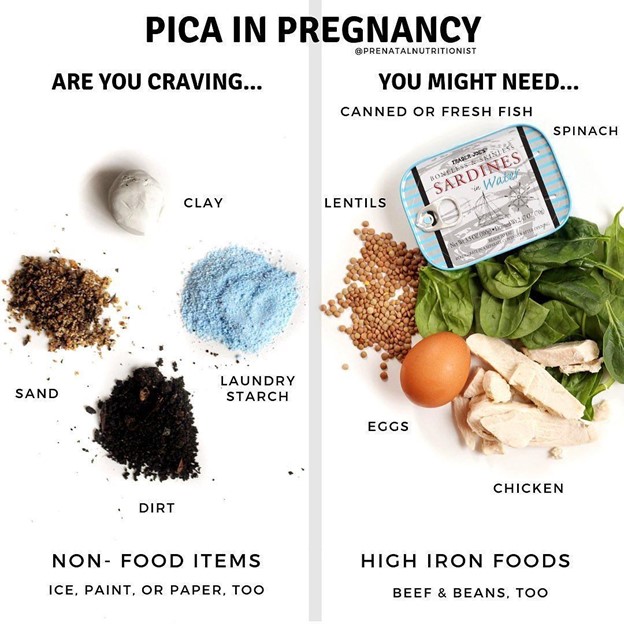
Assessment of a pregnant woman reveals that she compulsively craves ice. The nurse documents this finding as
Explanation
Choice A Reason: Linea nigra is a dark vertical line that appears on the abdomen of some pregnant women. It is caused by increased melanin production and usually fades after delivery.
Choice B Reason: Pica is a condition in which a person has an abnormal desire to eat substances that are not food, such as ice, clay, dirt, or chalk. It is more common in pregnant women and may indicate a deficiency in iron or other nutrients.
Choice C Reason: Ballottement is a technique of palpating a floating structure by bouncing it gently and feeling it rebound. In obstetrics, it can be used to detect the presence of the fetus by feeling its head move when the cervix is tapped.
Choice D Reason: Quickening is the first perception of fetal movements by the pregnant woman. It usually occurs between 16 and 20 weeks of gestation.
Assessment of a pregnant woman reveals that she compulsively craves ice. The nurse documents this finding as
Explanation
Choice A Reason: Linea nigra is a dark vertical line that appears on the abdomen of some pregnant women. It is caused by increased melanin production and usually fades after delivery.
Choice B Reason: Pica is a condition in which a person has an abnormal desire to eat substances that are not food, such as ice, clay, dirt, or chalk. It is more common in pregnant women and may indicate a deficiency in iron or other nutrients.
Choice C Reason: Ballottement is a technique of palpating a floating structure by bouncing it gently and feeling it rebound. In obstetrics, it can be used to detect the presence of the fetus by feeling its head move when the cervix is tapped.
Choice D Reason: Quickening is the first perception of fetal movements by the pregnant woman. It usually occurs between 16 and 20 weeks of gestation.
Complete the following sentence by using the best option: The client is at great risk for __________ evidenced by the client's serum __________.
Explanation
Choice A Reason: Preeclampsia is a condition in which a pregnant woman develops high blood pressure and proteinuria (protein in the urine). It can lead to serious complications such as eclampsia, which is seizures caused by preeclampsia, and HELLP syndrome, which is hemolysis, elevated liver enzymes, and low platelets. The main risk factor for preeclampsia is chronic hypertension, which means high blood pressure before pregnancy or before 20 weeks of gestation. Preeclampsia can be detected by measuring the blood pressure and urine protein level. Uric acid is not a reliable indicator of preeclampsia.
Choice B Reason: Gestational diabetes is the correct answer as explained above.
Choice C Reason: Eclampsia is a severe complication of preeclampsia that causes seizures and can be fatal for both the mother and the baby. It usually occurs after 20 weeks of gestation or during labor or postpartum. The main risk factor for eclampsia is preeclampsia, which means high blood pressure and proteinuria during pregnancy. Eclampsia can be prevented by treating preeclampsia with antihypertensive drugs and magnesium sulfate, which is a medication that prevents seizures. Magnesium sulfate can also lower the serum magnesium level, which is the amount of magnesium in the blood. However, magnesium level is not a diagnostic criterion for eclampsia.
Choice D Reason: Placenta previa is a condition in which the placenta covers part or all of the opening of the cervix. It can cause bleeding during pregnancy or delivery and can endanger both the mother and the baby. The main risk factor for placenta previa is previous cesarean section or other uterine surgery, which can cause scarring or damage to the uterine wall. Placenta previa can be detected by ultrasound, which is an imaging test that uses sound waves to create pictures of the uterus and placenta. Hemoglobin is not a relevant factor for placenta previa. Gestational diabetes is a condition in which a woman develops high blood sugar levels during pregnancy. It can cause complications for both the mother and the baby, such as macrosomia, hypoglycemia, and birth trauma. The main risk factor for gestational diabetes is glucose intolerance, which means the body cannot use glucose effectively. Glucose intolerance can be detected by measuring the serum glucose level, which is the amount of glucose in the blood.
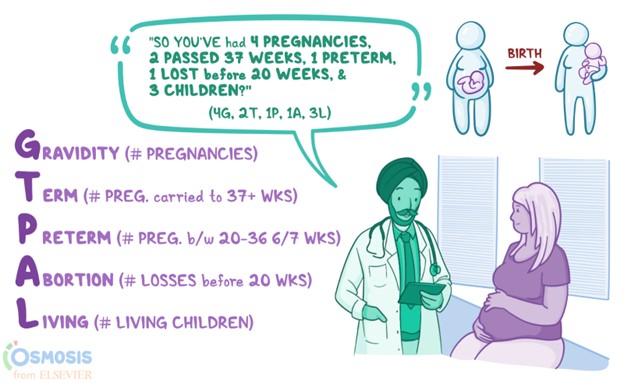
A client who is 4 months pregnant is at the prenatal clinic for her initial visit. Her history reveals she has 7-year-old twins who were born at 34 weeks gestation, a 2-year-old son born at 39 weeks gestation, and a spontaneous abortion 1 year ago at 6 weeks gestation. Using the GTPAL method, the nurse would document her obstetric history as:
Explanation
Choice A Reason: This option is incorrect because it underestimates the number of pregnancies (gravida) and overestimates the number of preterm births (preterm). The client has had four pregnancies (twins count as one pregnancy), not three. The client has had one preterm birth (the twins), not two.
Choice B Reason: This option is correct because it accurately reflects the client's obstetric history. GTPAL stands for Gravida, Term, Preterm, Abortions, and Living children. Gravida is the number of pregnancies a woman has had, regardless of outcome. Term is the number of pregnancies that ended at or beyond 37 weeks gestation. Preterm is the number of pregnancies that ended between 20 and 36 weeks gestation. Abortions are the number of pregnancies that ended before 20 weeks gestation, either spontaneously or induced. Living children are the number of children who are alive at present.
The client has had four pregnancies (gravida), one term birth (the son), one preterm birth (the twins), one abortion (the miscarriage), and three living children (the twins and the son).
Choice C Reason: This option is incorrect because it overestimates the number of preterm births (preterm) and underestimates the number of living children (living). The client has had one preterm birth (the twins), not two. The client has three living children (the twins and the son), not one.
Choice D Reason: This option is incorrect because it underestimates the number of pregnancies (gravida) and overestimates the number of abortions (abortions) and preterm births (preterm). The client has had four pregnancies (twins count as one pregnancy), not three. The client has had one abortion (the miscarriage), not two. The client has had one preterm birth (the twins), not two.
A nurse is preparing to infuse 1 liter of 0.9% sodium chloride IV over 8 hr with a tubing set that delivers 15 gtts/mL. The nurse should set the manual IV infusion to deliver how many drops/min? Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.
Explanation
The correct answer is 31 gtts/min. To calculate the infusion rate, the nurse should use the following formula:
Infusion rate (gtts/min) = Volume (mL) x Drop factor (gtts/mL) / Time (min)
Plugging in the given values, we get:
Infusion rate (gtts/min) = 1000 mL x 15 gtts/mL / 480 min
Infusion rate (gtts/min) = 31.25 gtts/min
Rounding to the nearest whole number, we get 31 gtts/min.
A nurse is preparing to administer penicillin G benzathine 1.2 million units IM now. The amount available is penicillin G benzathine 600,000 units/mL. How many mL should the nurse administer? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
The correct answer is 2 mL. To calculate the volume to administer, the nurse should use the following formula:
Volume (mL) = Dose (units) / Concentration (units/mL)
Plugging in the given values, we get:
Volume (mL) = 1,200,000 units / 600,000 units/mL
Volume (mL) = 2 mL
Rounding to the nearest whole number, we get 2 mL.

When describing perinatal education to a pregnant woman and her partner, the nurse emphasizes which goal as the primary one?
Explanation
Choice A Reason: This option is incorrect because it is unrealistic and impractical to eliminate anxiety completely. Anxiety is a normal and natural response to pregnancy and childbirth, and it can have both positive and negative effects on the outcome. Anxiety can motivate women and their partners to seek information and care, but it can also interfere with their ability to relax and cope with pain. Perinatal education can help them manage their anxiety by providing accurate information, reassurance, and coping strategies.
Choice B Reason: This option is incorrect because it implies that the couple has no control over their pregnancy and birth unless they are empowered by perinatal education. While perinatal education can enhance their sense of control and autonomy, it is not the only factor that influences their experience. Pregnancy and birth are complex and dynamic processes that involve many factors beyond their control, such as biological, environmental, social, and cultural factors. Perinatal education can help them adapt to these factors and collaborate with their health care providers.
Choice C Reason: Perinatal education is a process of providing information and support to pregnant women and their partners before, during, and after childbirth. The main goal of perinatal education is to help them prepare for a positive birth experience, which can have lasting benefits for their physical and emotional health, as well as their relationship with their baby. Perinatal education can also help them make informed decisions about their care and preferences, and cope with any challenges or complications that may arise.
Choice D Reason: This option is incorrect because it is too narrow and limited in scope. Providing knowledge and skills that will help them cope with labor is an important aspect of perinatal education, but it is not the primary goal. Labor is only one stage of childbirth, and perinatal education covers a broader range of topics that are relevant for pregnancy, birth, and postpartum. Moreover, coping with labor is not the only outcome that matters for a positive birth experience. Perinatal education can also help them achieve other outcomes, such as satisfaction, empowerment, bonding, and well-being.
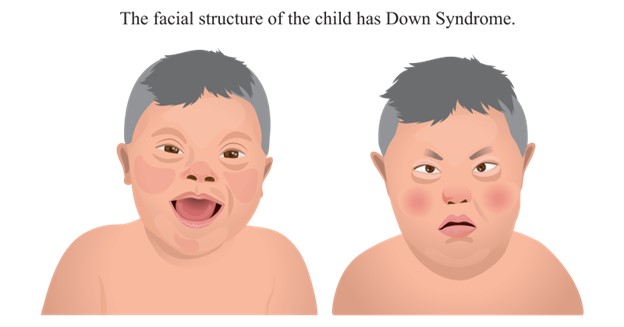
While talking with a pregnant woman who has undergone genetic testing, the woman informs the nurse that her baby will be born with Down syndrome. The nurse understands that Down syndrome is an example of:
Explanation
Choice A Reason: Trisomy numeric abnormality. Down syndrome is a genetic disorder that occurs when a person has three copies of chromosome 21 instead of two. This extra chromosome causes various physical and mental features that vary from person to person. Down syndrome is also called trisomy 21 because it involves three copies of chromosome 21.
Choice B Reason: Multifactorial inheritance is incorrect because it refers to a type of genetic disorder that results from the interaction of multiple genes and environmental factors. Examples of multifactorial disorders include cleft lip or palate, neural tube defects, diabetes, hypertension, and some types of cancer.
Choice C Reason: X-linked recessive inheritance is incorrect because it refers to a type of genetic disorder that affects males more than females because it is caused by a mutation on the X chromosome. Females have two X chromosomes, so they can be carriers or affected depending on whether they inherit one or two copies of the mutated gene. Males have one X chromosome and one Y chromosome, so they are always affected if they inherit the mutated gene from their mother. Examples of X-linked recessive disorders include hemophilia, color blindness, and Duchenne muscular dystrophy.
Choice D Reason: Chromosomal deletion is incorrect because it refers to a type of genetic disorder that occurs when a part of a chromosome is missing or deleted. This can cause various physical and mental problems depending on the size and location of the deletion. Examples of chromosomal deletion
A 22-year-old homeless woman arrives at a walk-in clinic seeking pregnancy confirmation. The nurse notes on assessment a 12-week gestational uterus, a BP of 110/70, a BMI of 17.5. The client admits to using cocaine a few times. She has been pregnant before and indicates she "loses them early." What characteristics place the client in the high-risk pregnancy category? Select all that apply.
Explanation
Choice A Reason: Homelessness is a risk factor for high-risk pregnancy because it exposes the woman to various challenges and stressors that can affect her health and well-being. Homeless women may face difficulties in accessing adequate nutrition, hygiene, safety, shelter, transportation, and health care. They may also experience higher levels of violence, substance abuse, mental illness, and social isolation. These factors can increase the risk of infections, complications, preterm birth, low birth weight, and infant mortality.
Choice B Reason: Age is not a risk factor for high-risk pregnancy in this case because the woman is 22 years old, which is within the optimal age range for childbearing. The optimal age range is considered to be between 20 and 35 years old, as women in this age group tend to have fewer complications and better outcomes than women who are younger or older. Women who are younger than 20 or older than 35 are considered to have advanced maternal age or adolescent pregnancy, respectively, which are risk factors for high-risk pregnancy.
Choice C Reason: BP 110/70 is not a risk factor for high-risk pregnancy because it is within the normal range for blood pressure. The normal range for blood pressure is considered to be between 90/60 and 120/80 mmHg. Blood pressure that is too high or too low can indicate problems such as preeclampsia, eclampsia, or hypotension, which are risk factors for high-risk pregnancy.
Choice D Reason: BMI 17.5 is a risk factor for high-risk pregnancy because it indicates that the woman is underweight. BMI stands for body mass index, which is a measure of body fat based on height and weight. The normal range for BMI is considered to be between 18.5 and 24.9 kg/m2. BMI that is too low or too high can indicate problems such as malnutrition, obesity, or gestational diabetes, which are risk factors for high-risk pregnancy.
Choice E Reason: Prenatal care is a risk factor for high-risk pregnancy because it indicates that the woman has not received adequate medical attention and support during her pregnancy. Prenatal care is essential for ensuring the health and well-being of both the mother and the baby. Prenatal care involves regular visits to a health care provider who can monitor the progress of the pregnancy, screen for any complications or infections, provide education and counseling, and prescribe any necessary medications or interventions. Lack of prenatal care can increase the risk of maternal mortality, morbidity, preterm birth, low birth weight, congenital anomalies, and infant mortality.
Choice F Reason: Prenatal history is a risk factor for high-risk pregnancy because it indicates that the woman has had previous pregnancies that ended in miscarriage or stillbirth. Prenatal history can provide important information about the woman's reproductive health and potential complications that may recur or affect her current pregnancy. Previous pregnancy losses can indicate problems such as genetic abnormalities, chromosomal disorders, infections, immunological factors, hormonal imbalances, uterine abnormalities, or placental issues. These factors can increase the risk of spontaneous abortion, fetal demise, preterm birth, intrauterine growth restriction (IUGR), or placenta previa.
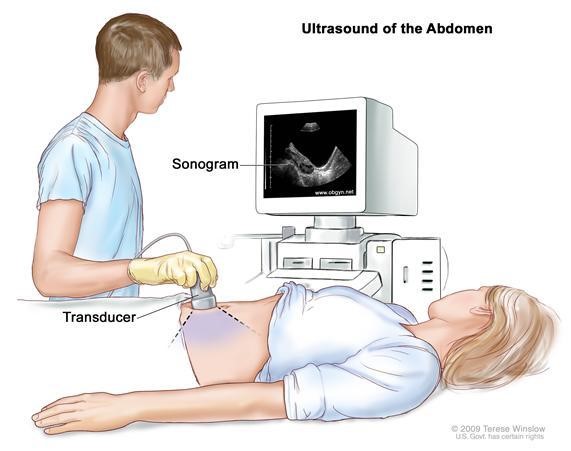
A client comes to the prenatal clinic for her first visit. When determining the client's estimated due date, the nurse understands that which method is the most accurate?
Explanation
Choice A Reason: Nagele's rule is a formula that estimates the due date by subtracting three months from the first day of the last menstrual period and adding seven days. However, this method assumes a regular 28-day cycle and may not be accurate for women with irregular cycles or who are unsure of their last menstrual period.
Choice B Reason: Ultrasound is the most accurate method of determining the estimated due date, especially in the first trimester. Ultrasound uses sound waves to create an image of the fetus and measure its size and development. Ultrasound can also detect any abnormalities or complications that may affect the pregnancy.
Choice C Reason: Gestation wheel is a circular calendar that estimates the due date by aligning the first day of the last menstrual period with a corresponding date on the wheel. However, this method also assumes a regular 28-day cycle and may not account for variations in ovulation or implantation.
Choice D Reason: Birth calculator is an online tool that estimates the due date based on various factors such as the last menstrual period, cycle length, ovulation date, conception date, or ultrasound date. However, this method may not be reliable as it depends on the accuracy of the input data and the algorithm used by the calculator.
A client's last menstrual period was April 11. Using Nägele's rule, her estimated date of birth (EDB) would be:
Explanation
Choice A Reason: This is incorrect because it adds 10 months and 7 days to the last menstrual period, which is not Nägele's rule.
Choice B Reason: This is incorrect because it adds 9 months and 7 days to the last menstrual period, which is not Nägele's rule.
Choice C Reason: This is correct because it follows Nägele's rule, which is to subtract 3 months and add 7 days to the last menstrual period.
Choice D Reason: This is incorrect because it subtracts 4 months and adds 7 days to the last menstrual period, which is not Nägele's rule.
Choice E Reason: This is incorrect because it subtracts 4 months and adds 17 days to the last menstrual period, which is not Nägele's rule.
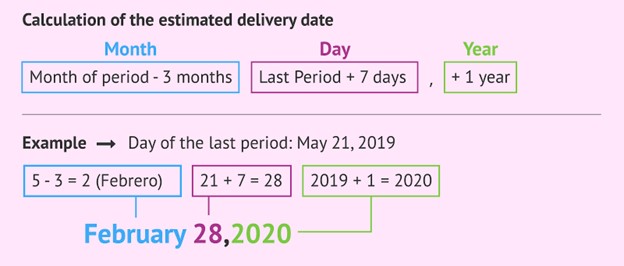
A client's last menstrual period was April 11. Using Naegele's rule, her estimated date of birth (EDB) would be:
Explanation
Choice A Reason: This is incorrect because it is too early. Naegele's rule is a formula that estimates the date of birth by adding one year, subtracting three months, and adding seven days to the date of the last menstrual period. Applying this rule to April 11 gives February 18, not February 24.
Choice B Reason: This is incorrect because it is too early. Naegele's rule gives February 18, not January 18.
Choice C Reason: This is incorrect because it is too early. Naegele's rule gives February 18, not January 25.
Choice D Reason: This is correct because it follows Naegele's rule. Adding one year, subtracting three months, and adding seven days to April 11 gives February 18.
A nurse is assessing a client who may be pregnant. The nurse reviews the client's history for presumptive signs. Which signs would the nurse most likely note? Select all that apply.
Explanation
Choice A Reason: Nausea is a common presumptive sign of pregnancy, especially in the first trimester. It is caused by hormonal changes and may be accompanied by vomiting.
Choice B Reason: Abdominal enlargement is another presumptive sign of pregnancy, as the uterus grows to accommodate the developing fetus. It may be noticeable as early as 12 weeks of gestation.
Choice C Reason: A positive pregnancy test is a presumptive sign of pregnancy, as it detects the presence of human chorionic gonadotropin (hCG), a hormone produced by the placenta. However, it is not a definitive sign, as it may be affected by other factors such as medications, tumors, or false positives.
Choice D Reason: Braxton Hicks contractions are not a presumptive sign of pregnancy, but a probable sign. They are irregular and painless contractions of the uterus that occur throughout pregnancy, but become more frequent and noticeable in the third trimester. They are also known as false labor contractions.
Choice E Reason: Amenorrhea, or the absence of menstrual periods, is a presumptive sign of pregnancy, as it indicates that ovulation has ceased. However, it is not a definitive sign, as it may be caused by other factors such as stress, illness, or hormonal imbalances.
A pregnant client in her second trimester has a hemoglobin level of 11 g/dL. The nurse interprets this as indicating:
Explanation
Choice A Reason: This is incorrect because hemoconcentration by hypertension is a condition where the blood volume decreases and the blood pressure increases, leading to a higher hemoglobin level. A normal hemoglobin level for a pregnant woman in her second trimester is 10.5 to 14 g/dL. A hemoglobin level of 11 g/dL is within the normal range, not indicative of hemoconcentration.
Choice B Reason: This is incorrect because a multiple gestation pregnancy is a pregnancy with more than one fetus, such as twins or triplets. A multiple gestation pregnancy can cause a lower hemoglobin level due to increased blood volume and increased demand for iron. A hemoglobin level of 11 g/dL is not suggestive of a multiple gestation pregnancy.
Choice C Reason: This is incorrect because greater-than-expected weight gain is not directly related to the hemoglobin level. Weight gain during pregnancy depends on various factors such as pre-pregnancy weight, nutrition, physical activity, and genetics. A hemoglobin level of 11 g/dL does not reflect the weight status of the pregnant client.
Choice D Reason: This is correct because iron-deficiency anemia is a common type of anemia that occurs when the body does not have enough iron to produce enough red blood cells. Iron-deficiency anemia can cause a low hemoglobin level and affect the oxygen delivery to the tissues and the fetus. A hemoglobin level of 11 g/dL may indicate iron-deficiency anemia, especially if the client has other symptoms such as fatigue, weakness, pale skin, or cravings for non-food items. The nurse should confirm the diagnosis with further tests and recommend iron supplements and dietary changes to treat the condition.
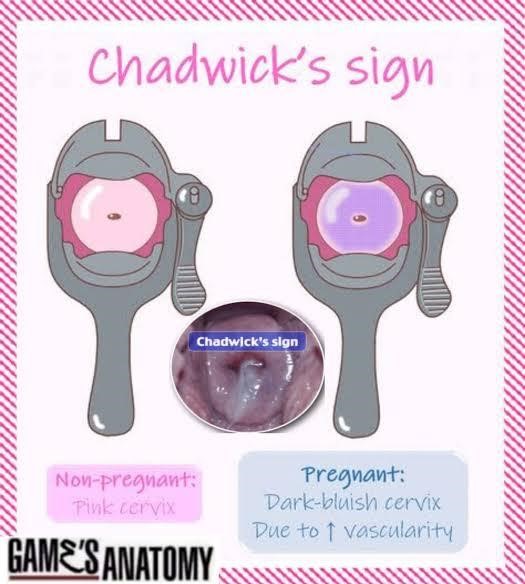
On the first prenatal visit, examination of the woman's internal genitalia reveals a bluish coloration of the cervix and vaginal mucosa. The nurse documents this finding as:
Explanation
Choice A Reason: This is correct because Chadwick's sign is a bluish or purplish discoloration of the cervix, vagina, and vulva caused by increased blood flow to the pelvic area during pregnancy. It is one of the earliest signs of pregnancy and can be observed as early as six to eight weeks of gestation.
Choice B Reason: This is incorrect because Goodell's sign is a softening of the cervix due to increased vascularity and edema during pregnancy. It is another early sign of pregnancy and can be detected by palpation around six to eight weeks of gestation.
Choice C Reason: This is incorrect because Hegar's sign is a softening of the lower uterine segment or isthmus during pregnancy. It is also an early sign of pregnancy and can be felt by bimanual examination around six to twelve weeks of gestation.
Choice D Reason: This is incorrect because Homan's sign is a pain in the calf or popliteal region when the foot is dorsiflexed. It is a sign of deep vein thrombosis, which is a potential complication of pregnancy, but not a normal finding.
A pregnant woman undergoes a triple/quadruple screen at 16 to 18 weeks' gestation. What would the nurse suspect if the woman's alpha-fetoprotein (AFP) level is decreased?
Explanation
Choice A Reason: This is incorrect because sickle-cell anemia is a genetic disorder that affects the shape and function of the red blood cells. It is not related to the AFP level, which is a protein produced by the fetal liver and yolk sac.
Choice B Reason: This is incorrect because cardiac defects are abnormalities in the structure or function of the heart. They are not related to the AFP level, which is a marker of neural tube defects and abdominal wall defects.
Choice C Reason: This is correct because Down syndrome is a chromosomal disorder that results from an extra copy of chromosome 21. It is associated with a decreased AFP level, as well as increased levels of human chorionic gonadotropin (hCG) and unconjugated estriol (uE3).
Choice D Reason: This is incorrect because respiratory disorders are problems that affect the lungs and breathing. They are not related to the AFP level, which reflects the fetal development and integrity.
Sign Up or Login to view all the 49 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

