ATI Maternal newborn Exam 2
Total Questions : 19
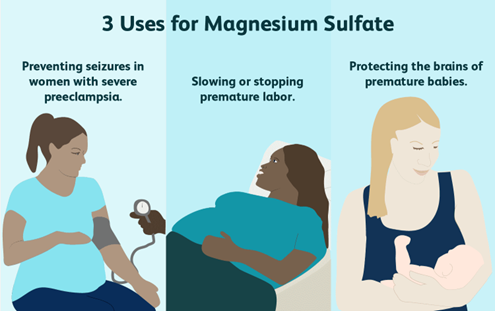
Showing 19 questions, Sign in for moreA nurse is assessing a client who is at 32 weeks of gestation and is receiving magnesium sulphate via continuous IV infusion. Which of the following findings should the nurse report to the provider?
Explanation
Absent deep tendon reflexes are a sign of magnesium toxicity, which can occur with high levels of magnesium in the bloodstream. This can be a serious complication that requires immediate attention from the provider.
Option A, a decrease in the frequency of contractions, is actually a desired effect of magnesium sulfate in the management of preterm labor. It is not a cause for concern.
Option B, a blood pressure reading of 150/100 mm Hg, is high, but it is not necessarily related to the administration of magnesium sulfate. However, it should still be reported to the provider for appropriate management.
Option D, a urinary output of 35 mL/hr, is below the normal range but it may still be within an acceptable range for a client receiving magnesium sulfate. The provider should be notified if urinary output continues to decrease or if it falls below a certain threshold.
Out of the listed findings, the nurse should report c. Absent deep tendon reflexes to the provider immediately.
While the other findings may warrant monitoring or further assessment, they are not immediately concerning in this context:
- a. Decrease in frequency of contractions:This could be a normal response to magnesium sulfate, which is sometimes used to stop preterm labor. However, it's important to monitor the contractions to ensure they don't become too infrequent.
- b. BP 150/100 mm Hg:This is mildly elevated blood pressure, but not severe enough to require immediate intervention in this case. Monitoring blood pressure is still important, though.
- d. Urinary output 35 mL/hr:This is on the lower end of normal, but not concerning enough to require immediate action. Monitoring urine output is important to assess kidney function.
Absent deep tendon reflexes, however, is a sign of magnesium toxicity. Magnesium sulfate is a medication that needs to be closely monitored because high levels can be dangerous. If the nurse detects this finding, they should report it to the provider right away so that magnesium levels can be checked and appropriate action can be taken.
Here are some additional things to keep in mind:
- This is not an exhaustive list of all potential side effects of magnesium sulfate.
- It is important for the nurse to follow the provider's orders and protocols for monitoring clients receiving magnesium sulfate.
- If the nurse has any concerns about the client's condition, they should always err on the side of caution and report them to the provider.
A nurse is teaching a client and her partner about the technique of counterpressure during labor. Which of the following statements by the nurse is appropriate?
Explanation
Counterpressure is a technique that involves applying pressure to specific areas of the body during labor to help alleviate pain and discomfort. This technique is particularly helpful during the active phase of labor when contractions are strong and painful. The most common area to apply counterpressure is the lower back, as this is where many women experience the most intense pain during labor.
Option a, “Your partner will apply pressure to the top of your uterus during contractions” is incorrect as applying pressure to the top of the uterus is not a recommended technique and could be harmful to the mother and the baby.
Option c, “Your partner will apply continuous, firm pressure between your thumb and index finger” is incorrect as this technique is used to alleviate pain and discomfort during contractions in the hand and wrist, not for counterpressure.
Option d, “Your partner will apply upward pressure on your lower abdomen between contractions” is incorrect as this technique is used to help turn a baby who is in a posterior position, not for counterpressure.

A nurse is caring for a client who is at 30 weeks of gestation and receiving magnesium sulfate for preeclampsia. The nurse should recognize which of the following manifestations is an adverse reaction to the medication.
Explanation
Magnesium sulfate is a medication used to prevent seizures in clients with preeclampsia. However, it can cause adverse reactions, including respiratory depression, which can lead to a decrease in the respiratory rate. The normal respiratory rate for adults is between 12-20 breaths per minute, so a respiratory rate of 16 per minute is within normal limits.
Hypertension is a common symptom of preeclampsia, which is why magnesium sulfate is used to control blood pressure in these clients. Hypoglycemia is not a common adverse reaction to magnesium sulfate. Urine output of 20 mL/hr is low and may indicate dehydration or impaired kidney function, but it is not necessarily an adverse reaction to magnesium sulfate. However, the nurse should monitor the client's urine output to ensure adequate kidney function.
A nurse is reviewing the chart of a client who is 2 days postpartum following a vaginal delivery and reports constipation. Which of the following findings should the nurse identify as a contraindication to the use of a suppository?
Explanation
Constipation is a common postpartum issue due to decreased bowel motility, dehydration, and fear of pain during defecation. Suppositories are a common treatment option to help relieve constipation in postpartum clients. However, there are certain contraindications to the use of suppositories.
Option A, abdominal distention, is not a contraindication to the use of a suppository, as it can help relieve the distention and promote bowel movement.
Option C, vaginal candidiasis, is also not a contraindication to the use of a suppository. In fact, antifungal suppositories may be prescribed to treat candidiasis.
Option D, afterpain, is not a contraindication to the use of a suppository, as afterpains are normal
postpartum contractions that occur as the uterus returns to its pre-pregnancy size.
Option B, third-degree perineal laceration, is a contraindication to the use of a suppository. The suppository can cause further trauma to the already injured perineal area and delay the healing process. In this case, alternative treatment options, such as stool softeners or laxatives, should be considered.

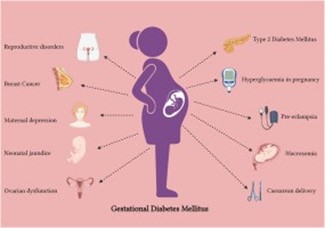
A nurse is caring for a client who is at 32 weeks of gestation and has gestational diabetes mellitus. Which of the following findings should the nurse report to the provider?
Explanation
Fundal height is measured from the top of the pubic bone to the top of the uterus and is used to assess fetal growth. A fundal height measurement that is larger than expected for gestational age may indicate a problem such as macrosomia (a larger than average baby), which can be a complication of gestational diabetes. The nurse should report this finding to the provider for further evaluation.
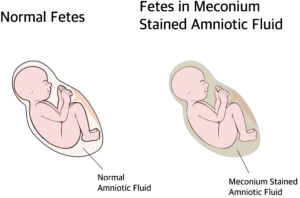
A nurse is reviewing the electronic medical record of a postpartum client. The nurse should identify that which of the following factors places the client at risk for an infection.
Explanation
Meconium is the first stool passed by a newborn and its presence in the amniotic fluid during labor can indicate fetal distress. Meconium can also cause infection in the mother if it enters her bloodstream through the placenta or during delivery.
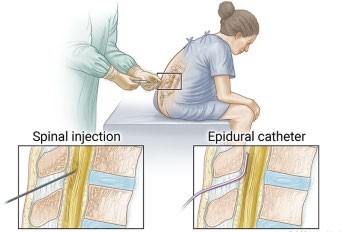
A nurse is caring for a client who is in labor and just received epidural anesthesia. The client’s blood pressure is 90/50 mm Hg. Which of the following actions should the nurse take?
Explanation
A common side effect of epidural anesthesia is a drop in blood pressure. Turning the client onto their side can help improve blood flow to the uterus and baby and may help raise the mother’s blood pressure.
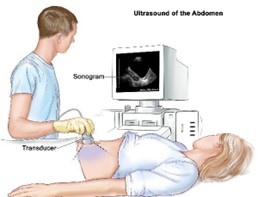
A nurse is providing teaching to a client who is primigravid and is scheduled to have an abdominal ultrasound. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
A full bladder can help improve the quality of an abdominal ultrasound by pushing the intestines out of the way and providing a clearer view of the uterus and baby.
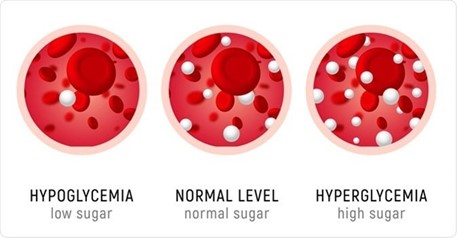
A nurse is caring for a client who has pregestational diabetes mellitus. Which of the following clinical findings should indicate to the nurse that the client has hyperglycemia?
Explanation
Hyperglycemia, or high blood sugar, can cause increased urination as the body tries to remove excess glucose from the blood. This can lead to dehydration and increased thirst.
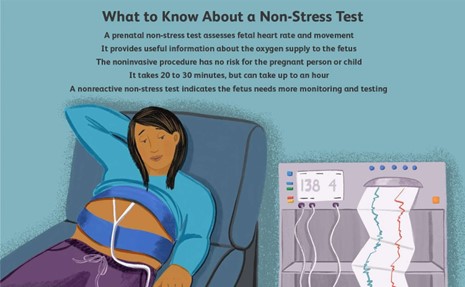
A nurse is assessing the results of a nonstress test for an antepartum client at 35 weeks of gestation. Which of the following findings should indicate to the nurse the need for further diagnostic testing?
Explanation
A nonstress test measures fetal heart rate in response to fetal movement. A reactive nonstress test result is when there are at least two accelerations of the fetal heart rate within a 20-minute period, each lasting at least 15 seconds and peaking at least 15 beats per minute above the baseline. If there are fewer than two accelerations within a 20-minute period, further diagnostic testing may be needed.
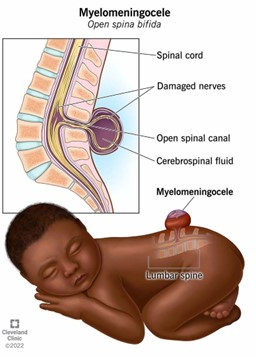
A nurse is planning care immediately following birth for a newborn who has a myelomeningocele that is leaking cerebrospinal fluid. Which of the following actions should the nurse include in the plan of care?
Explanation
A myelomeningocele is a type of spina bifida in which the spinal cord and its protective membranes protrude through an opening in the spine. If the sac is leaking cerebrospinal fluid, it is important to keep the area clean to prevent infection. Povidone-iodine is an antiseptic that can be used to cleanse the area.
A nurse is observing an adolescent client who is offering her newborn a bottle while he is lying in the bassinet. When the nurse offers to pick the newborn up and place him in the client’s arms, the mother states, “No, the baby is too tired to be held.” Which of the following actions should the nurse take?
Explanation
This option respects the mother's wishes of not wanting to hold the newborn while also allowing the nurse to provide education on safe and appropriate feeding positions. It also gives the mother the opportunity to learn and practice holding the newborn in a safe way.
Option a, offering to take the newborn to the nursery, may not be necessary as the mother is already offering the baby a bottle.
Option b, insisting that the mother pick up the newborn, would not be respectful of her wishes and could potentially damage the trust and rapport between the mother and nurse.
Option d, persuading the client to breastfeed, may not be appropriate or feasible in this situation as it may not be the mother's preferred feeding method and may not address the immediate concern of the newborn being too tired to be held.
A nurse is providing teaching to a client who is receiving medroxyprogesterone IM for contraception. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Medroxyprogesterone is a progestin-only contraceptive injection that is administered every 12-13 weeks to prevent pregnancy. The client should return to the clinic for their next injection in 11-13 weeks (or as advised by their healthcare provider) to maintain contraceptive efficacy.
Option b is incorrect because the client only receives one injection each time.
Option c is not directly related to medroxyprogesterone, although it is important for women to have adequate calcium intake to maintain bone health.
Option d is incorrect because spotting is a common side effect of medroxyprogesterone and does not indicate that the medication should be discontinued.
A nurse is planning care for a client who is pregnant and has HIV. Which of the following actions should the nurse include in the plan of care?
Explanation
Pregnant clients with HIV require comprehensive care during pregnancy, delivery, and postpartum periods to prevent transmission of HIV to the newborn. Bathing the newborn before initiating skin-to-skin contact is a recommended action to reduce the risk of HIV transmission from mother to child. This practice helps to remove any maternal blood or other bodily fluids from the newborn's skin, which may contain the virus. Therefore, the nurse should instruct the client to bathe the newborn before initiating skin-to-skin contact.
Antiretroviral medications are usually continued throughout pregnancy and during labor and delivery to decrease the risk of transmission to the newborn. Therefore, the nurse should not instruct the client to stop taking antiretroviral medications at 32 weeks of gestation, as mentioned in option a.
A fetal scalp electrode is a device that attaches to the baby's scalp to monitor the fetal heart rate. This device can cause small cuts or abrasions on the baby's scalp, which may increase the risk of HIV transmission.
Therefore, its use should be avoided in clients with HIV. Therefore, option b is not a recommended action.
Administering pneumococcal immunization to the newborn within 4 hours following birth is not a recommended action in the plan of care for a client who is pregnant and has HIV. Pneumococcal immunization is not indicated for newborns immediately after birth. Therefore, option d is not a recommended action.

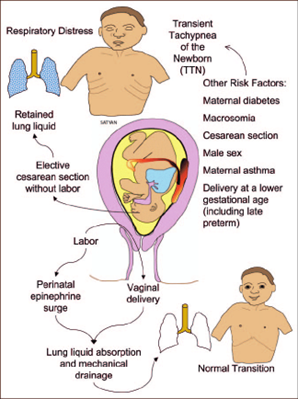
A nurse in a newborn nursery is receiving a change-of-shift report for four newborns. Which of the following newborns should the nurse assess first?
Explanation
New onset tachypnea in a newborn is a concerning symptom and requires immediate assessment by the nurse. Tachypnea is defined as a respiratory rate greater than 60 breaths per minute in a newborn. It can be a sign of respiratory distress or other serious conditions, such as sepsis or cardiac disease.
Option a. A newborn who has a short frenulum and is having difficulty breastfeeding is a common issue that can be addressed by the nurse or lactation consultant. It does not require immediate assessment.
Option b. A newborn who is 24 hr old and has not had a meconium stool may be concerning, but it is not an emergency situation. It may be a sign of bowel obstruction, but it is not an urgent condition.
Option c. A newborn who is 10 hr old and has blood-tinged discharge in her diaper may be a concerning symptom, but it is not an emergency situation. It may be related to maternal hormones and is a common finding in newborns.
Therefore, the correct option is d. A newborn who is 10 hr old and has new onset tachypnea. The nurse should assess the newborn's respiratory status, heart rate, and oxygen saturation and notify the healthcare provider immediately if there are any concerns.
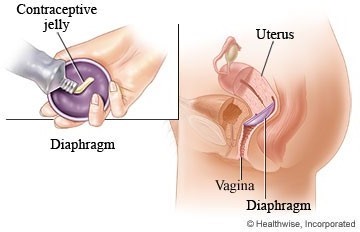
A nurse is providing teaching to a client who is 2 days postpartum and wants to continue using her diaphragm for contraception. Which of the following instructions should the nurse include?
Explanation
After giving birth, a woman's body undergoes many changes, including changes in the size and shape of the vagina. It is essential to have the correct size of the diaphragm to ensure its effectiveness.
Therefore, the nurse should instruct the client to have a provider refit her for a new diaphragm.
Option A is incorrect because the diaphragm should be cleaned with warm water and mild soap, not an oil-based vaginal lubricant.
Option B is incorrect because the diaphragm should be removed no sooner than 6 hours after intercourse but should not be left in place for more than 24 hours.
Option C is incorrect because oil-based vaginal lubricants can damage latex diaphragms, reducing their
effectiveness as a contraceptive method. Water-based lubricants should be used instead.
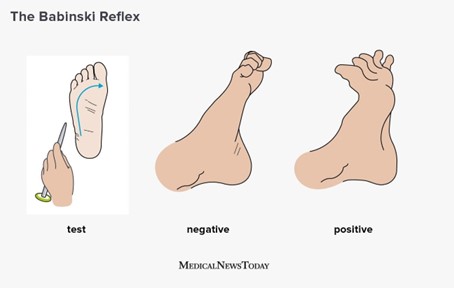
A nurse is performing an assessment of a newborn’s Babinski reflex. Which of the following findings should the nurse expect?
Explanation
The Babinski reflex is a normal reflex present in newborns and infants up to about 2 years old. It is elicited by stroking the lateral aspect of the sole of the foot from the heel toward the toes. A positive Babinski reflex is characterized by dorsiflexion (upward movement) of the big toe and fanning out of the other toes. This is also known as an extensor response.
Therefore, option a, eversion of the great toe, is the expected finding for a positive Babinski reflex. Options b, c, and d are not consistent with a positive Babinski reflex.
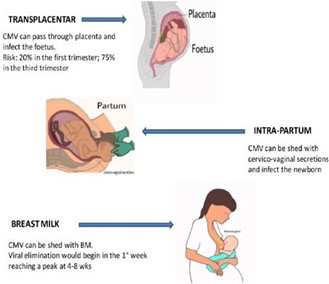
A nurse manager on the labor and delivery unit is teaching a group of newly licensed nurses about maternal cytomegalovirus. Which of the following information should the nurse manager include in the teaching?
Explanation
Transmission can occur through bodily fluids, including urine, saliva, blood, breast milk, and cervical secretions. Therefore, pregnant women can acquire CMV by close contact with young children who are shedding the virus, or by exposure to contaminated body fluids in healthcare settings or through sexual activity.
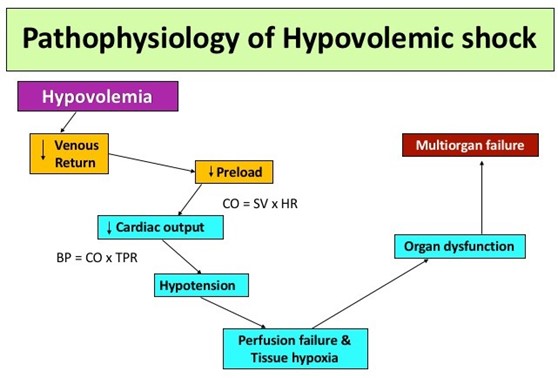
A nurse is caring for a client who is postpartum and experiencing hypovolemic shock. Which of the following findings should the nurse expect?
Explanation
Hypovolemic shock occurs when there is a significant decrease in the circulating blood volume, which can happen after severe bleeding during childbirth. The body tries to compensate for this decrease in blood volume by constricting blood vessels and increasing heart rate. However, these compensatory mechanisms can only last for a certain amount of time before the body starts to show signs of shock.
One of the hallmark signs of hypovolemic shock is cool, clammy skin, which is caused by the body diverting blood flow away from the skin to maintain perfusion to vital organs. Other common signs and symptoms include tachycardia (fast heart rate), hypotension (low blood pressure), tachypnea (fast breathing rate), decreased urine output, and altered mental status.
Sign Up or Login to view all the 19 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now


