ATI Maternal Newborn Exam 3 Fall 2023
Total Questions : 60
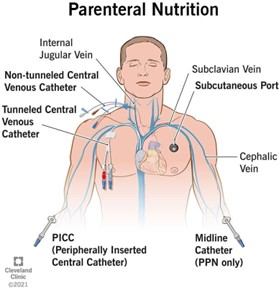
Showing 25 questions, Sign in for moreWhich intervention is most important for the practical nurse (PN) to implement for a client who is receiving total parenteral nutrition (TPN)?
Explanation
a) Collect fingerstick glucose levels.Correct
Collecting fingerstick glucose levels is the most important intervention for the PN to implement for a client who is receiving TPN. TPN is a method of feeding that bypasses the gastrointestinal tract and provides all the nutritional needs of the body through a vein. TPN contains a high concentration of glucose, which can cause hyperglycemia or fluctuations in blood sugar levels. Therefore, it is essential to monitor the client's glucose levels frequently and adjust the infusion rate or insulin administration accordingly.
b) Implement bleeding precautions.
Implementing bleeding precautions is not the most important intervention for the PN to implement for a client who is receiving TPN. Bleeding precautions are measures to prevent or minimize bleeding in clients who have a high risk of hemorrhage due to conditions such as thrombocytopenia, coagulopathy, or anticoagulant therapy. TPN does not directly increase the risk of bleeding, although it may affect the liver function and clotting factors in some cases². Therefore, bleeding precautions are not a priority for a client who is receiving TPN.
c) Obtain daily weights.
Obtaining daily weights is not the most important intervention for the PN to implement for a client who is receiving TPN. Obtaining daily weights is a way to monitor the client's fluid balance, nutritional status, and response to therapy. TPN can cause fluid overload, dehydration, or electrolyte imbalances in some cases²⁵. Therefore, obtaining daily weights is important, but not as important as monitoring glucose levels.
d) Check urine for albumin.
Checking urine for albumin is not the most important intervention for the PN to implement for a client who is receiving TPN. Checking urine for albumin is a way to detect proteinuria, which is an indicator of kidney damage or disease. TPN does not directly cause kidney problems, although it may affect the renal function and urine output in some cases². Therefore, checking urine for albumin is not a priority for a client who is receiving TPN.
 |
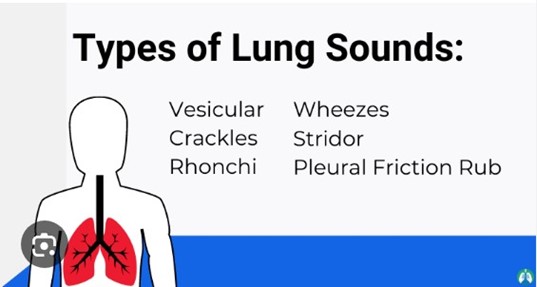
The practical nurse (PN) is assisting with the admission of a client with complications of left-sided heart failure. Which focused assessment should the PN implement first?
Explanation
c) Bilateral lung sounds.
Explanation:
When admitting a client with complications of left-sided heart failure, the practical nurse (PN) should prioritize assessing the client's bilateral lung sounds. Left-sided heart failure can result in the accumulation of fluid in the lungs, leading to pulmonary congestion and impaired gas exchange. By auscultating the client's lung sounds, the PN can assess for the presence of crackles, wheezes, or diminished breath sounds, which are indicative of pulmonary congestion and fluid accumulation. This assessment helps to identify the severity of the client's condition and guides further interventions and treatment.
While assessing heart sounds (option a) is important in evaluating cardiac function, assessing lung sounds takes priority as pulmonary congestion is a common manifestation of left-sided heart failure. Chest pain (option b) is a significant symptom that should be assessed promptly, but in this scenario, the focus is on assessing for signs of pulmonary congestion and impaired gas exchange. Assessing the client's mood and affect (option d) is important for a comprehensive assessment, but it is not the priority when the client is admited with complications of left-sided heart failure.
The other options are considered incorrect because they are not the priority assessments when admitting a client with complications of left-sided heart failure.
Option a) Heart sounds: While assessing heart sounds is important in evaluating cardiac function, the priority in this scenario is to assess for pulmonary congestion and impaired gas exchange. Assessing bilateral lung sounds allows the practical nurse to gather immediate information about the client's respiratory status and the presence of fluid in the lungs.
Option b) Chest pain: Chest pain is a significant symptom that should be assessed promptly, as it could indicate various cardiac or respiratory conditions. However, in this specific scenario, the priority is to assess for signs of pulmonary congestion, which can have a more immediate impact on the client's respiratory function.
Option d) Mood and affect: Assessing the client's mood and affect is important for a comprehensive assessment of their emotional well-being. However, when admitting a client with complications of left- sided heart failure, the priority is to assess their physical condition, particularly the respiratory status, to address any immediate concerns related to pulmonary congestion and impaired gas exchange.
 |
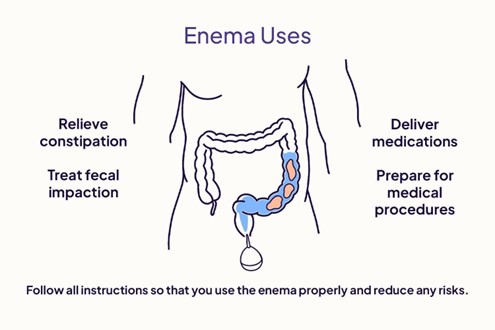
An oil retention enema is prescribed for a hospitalized client. The practical nurse (PN) should administer the enema solution at which temperature?
Explanation
- An oil retention enema is used to soften the stool and lubricate the rectum, making it easier to pass the stool. It is usually oil-based and contains 90-120 ml of solution³.
- The temperature of the enema solution affects the effectiveness and comfort of the procedure. If the solution is too hot or cold, it can cause pain, cramps, or damage to the rectal tissue³. If the solution is too warm, it can also stimulate peristalsis and cause the client to expel the enema before it has time to work⁴.
- The ideal temperature for an enema solution is close to the client’s body temperature, which is around 98°F or 36°C. This temperature ensures that the solution is comfortable and does not cause adverse reactions³⁴.
Option A is incorrect because the client’s comfort level may not reflect the optimal temperature for the
enema.
Option B is incorrect because the temperature of the enema does affect its effectiveness and safety. Option D is incorrect because the temperature is too high and can cause harm to the client.
A male preoperative client who has already signed the informed consent for a surgical procedure confides to the practical nurse (PN) that he is really frightened and unsure about undergoing the surgery. Which priority action should the PN take?
Explanation
d) Notify the charge nurse of the client's concerns about surgery.
Explanation:
When a client expresses fear and uncertainty about undergoing surgery, it is important for the practical nurse (PN) to communicate this information to the charge nurse or the healthcare provider. By notifying the appropriate person, the PN ensures that the client's concerns are addressed and appropriate interventions can be implemented.
Options a) and c) are not the priority actions because documenting the client's concerns or reminding them about the signed consent does not address their emotional needs or provide support.
Option b) may not be the most appropriate response, as simply encouraging the client to continue with the scheduled surgery without addressing their fears and uncertainties may not be sufficient to alleviate their anxiety.
Therefore, the best course of action is to notify the charge nurse or healthcare provider so that they can assess the client's concerns, provide reassurance, and address any questions or fears the client may have prior to the surgery.
A client reports experiencing numbness and ngling in the extremies. Which of the client's serum laboratory values should the praccal nurse (PN) priorize reporng to the healthcare provider?
Explanation
When a client reports experiencing numbness and ngling in the extremies, it is crucial for the praccal nurse (PN) to prioritise reporting the client's electrolyte levels to the healthcare provider. Electrolytes are essential minerals that help maintain the balance of fluids in the body and enable proper nerve and muscle function. Imbalances in electrolyte levels can lead to neurological symptoms, including numbness and ngling.
Opons a, b, and d are not the correct priories to report in this situation:
a) Hematocrit: Hematocrit measures the proportion of red blood cells in the blood. While abnormalies in hematocrit can indicate certain conditions, such as anaemia, it is not directly associated with numbness and ngling in the extremes.
b) Albumin and protein levels: Albumin and protein levels are important for assessing nutritional status and liver function. While low levels of protein can contribute to various health issues, they are not the primary concern when a client experiences numbness and ngling in the extremities.
d) White blood cell count (WBC): WBC count is used to evaluate the immune system's response to infection or inflammation. While infections or inflammatory conditions can cause neurological symptoms, such as ngling, it is not the primary concern in this specific case of numbness and ngling.
Therefore, the most appropriate laboratory value to prioritise reporting in this scenario is the client's electrolyte levels, as imbalances can directly contribute to the reported symptoms and may require prompt intervention.
The practical nurse (PN) is assigning care for a group of clients on the urology medical unit. Which client care interventions should the PN assign to the unlicensed assistive personnel (UAP)? (Select all that apply)
Explanation
The correct answers are:
a) Transport a urine culture sample to the laboratory. Correct
This is a client care intervention that the PN can assign to the UAP. Transporting a urine culture sample to the laboratory is a routine and non-invasive task that does not require clinical judgment or skill. The UAP should follow the standard precautions and protocols for handling and labeling the specimen.
b) Obtain a post-voided residual (PVR) volume.
This is not a client care intervention that the PN can assign to the UAP. Obtaining a post-voided residual (PVR) volume is a procedure that requires clinical judgment and skill, as it involves using a bladder scanner or catheterizing the client to measure the amount of urine left in the bladder after voiding.
The UAP is not trained or authorized to perform this task, and it should be done by the PN or another licensed nurse.
c) Teach the client with fluid restrictions how to measure urine output.
This is not a client care intervention that the PN can assign to the UAP. Teaching the client with fluid restrictions how to measure urine output is an educational activity that requires clinical judgment and skill, as it involves assessing the client's learning needs, providing clear and accurate instructions, and evaluating the client's understanding and compliance. The UAP is not trained or authorized to perform this task, and it should be done by the PN or another licensed nurse.
d) Irrigate an indwelling urinary catheter for a client with bladder suspension.
This is not a client care intervention that the PN can assign to the UAP. Irrigating an indwelling urinary catheter for a client with bladder suspension is a procedure that requires clinical judgment and skill, as it involves inserting sterile fluid into the bladder through the catheter to flush out any clots, debris, or bacteria. The UAP is not trained or authorized to perform this task, and it should be done by the PN or another licensed nurse.
e) Empty bedside drainage unit for a client with indwelling urinary catheter. Correct
This is a client care intervention that the PN can assign to the UAP. Emptying bedside drainage unit for a client with indwelling urinary catheter is a routine and non-invasive task that does not require clinical judgment or skill. The UAP should follow the standard precautions and protocols for emptying, measuring, and recording the urine output.
 |
An older female client who resides in a long-term care facility has a male friend who often visits her in the evenings.
The practical nurse (PN) enters the client's room to administer medications and finds the couple in bed together. What action should the PN take?
Explanation
The correct answer and explanation is:
d) Ask when the nurse should return. Correct
This is the action that the PN should take when entering the client's room and finding the couple in bed together. Asking when the nurse should return respects the client's privacy, dignity, and autonomy, while also ensuring that the client receives the necessary care.
The PN should acknowledge that the client has the right to express her sexuality and intimacy, as long as it is consensual and safe . The PN should also avoid making any judgments or assumptions about the client's relationship or preferences.
a) Request that the man get up and leave.
This is not the action that the PN should take when entering the client's room and finding the couple in bed together. Requesting that the man get up and leave is rude, disrespectful, and intrusive, as it violates the client's privacy, dignity, and autonomy. The PN should not interfere with the client's sexual or intimate activities, unless there is a clear indication of abuse, coercion, or harm.
b) Report the incident to the family.
This is not the action that the PN should take when entering the client's room and finding the couple in bed together. Reporting the incident to the family is inappropriate and unethical, as it breaches the client's confidentiality and autonomy. The PN should not share any information about the client's sexual or intimate activities with anyone without her consent, unless there is a clear indication of abuse, coercion, or harm.
c) Exit the room and quietly close the door.
This is not the action that the PN should take when entering the client's room and finding the couple in bed together. Exiting the room and quietly closing the door is passive and neglectful, as it ignores the client's needs and care.
The PN should not avoid or delay providing care to the client because of her sexual or intimate activities, unless she requests so . The PN should also communicate with the client and her partner in a respectful and professional manner.
In caring for a client who requires seizure precauons, the praccal nurse (PN) should ensure the ready availability of equipment to perform which procedure?
Explanation
Seizure precauons are measures taken to protect a client who is at risk of having a seizure, which is a sudden and abnormal electrical acvity in the brain that can cause changes in behavior, movement, sensaon, or consciousness. Seizure precauons include providing a safe environment, monitoring the client's vital signs and neurological status, administering anconvulsant medicaons, and documenng the onset, duraon, and characteriscs of any seizure acvity³.
One of the potenal complicaons of a seizure is aspiraon, which is the inhalaon of foreign material into the lungs, such as saliva, vomit, or food. Aspiraon can cause choking, pneumonia, or respiratory distress. To prevent or treat aspiraon, the praccal nurse (PN) should ensure the ready availability of equipment to perform suconing of the trachea, which is the tube that connects the mouth and nose to the lungs. Suconing of the trachea involves inserng a catheter through the nose or mouth into the trachea and applying negave pressure to remove any secreons or debris from the airway.
Therefore, opon A is the correct answer, while opons B, C, and D are incorrect.
Opon B is incorrect because inserng a urinary catheter is not related to seizure precauons or aspiraon prevenon.
Opon C is incorrect because applying so restraints may not be necessary or appropriate for a client who requires seizure precauons, as they may interfere with the natural movements of the seizure or cause injury to the client.
Opon D is incorrect because inserng a nasogastric tube is not related to seizure precauons or aspiraon prevenon.
The mother of a school-aged boy tells the praccal nurse (PN) that he fell out of a tree and hurt his arm and shoulder. Which assessment should the praccal nurse (PN) note as the most significant indicator of possible child abuse?
Explanation
- Child abuse is the intentional or neglectful physical, emotional, or sexual harm or injury of a child by a parent, caregiver, or another person who has a relationship of trust or responsibility with the child. Child abuse can have serious and long-lasting consequences for the child's health, development, and well-being.
- The practical nurse (PN) has a legal and ethical duty to identify, report, and prevent child abuse. The PN should be alert for any signs and symptoms of child abuse, such as unexplained or inconsistent injuries, bruises, burns, fractures, or scars; behavioural changes, such as fear, anxiety, aggression, withdrawal, or depression; poor hygiene, nutrition, or growth; lack of supervision, medical care, or education; or sexualized behaviours or knowledge.
- The PN should also conduct a thorough and sensitive assessment of the child and the family situation, using open-ended questions, active listening, and a non-judgmental attitude. The PN should compare the history and physical findings of the child with the expected developmental milestones and normal variations for the child's age and stage. The PN should also document any relevant information in an objective and factual manner.
- When the mother of a school-aged boy tells the PN that he fell out of a tree and hurt his arm and shoulder, the PN should assess the child's injury and compare it with the mother's explanation. The most significant indicator of possible child abuse in this scenario is if the injury description by the mother varies from the child's version. This may suggest that the mother is lying or covering up the true cause of the injury, which may be intentional or accidental harm by herself or someone else. A discrepancy between the mother's and the child's stories may also indicate that the child is afraid or coerced to hide the truth about the abuse.
- Therefore, option D is the correct answer, while options A, B, and C are incorrect.
- Option A is incorrect because the child looking at the floor when answering the nurse's questions may not be a sign of abuse, but rather a sign of shyness, embarrassment, pain, or discomfort.
Option B is incorrect because the mother describing in detail what she did for her injured child may not be a sign of abuse, but rather a sign of concern, care, or guilt.
Option C is incorrect because the abrasions on the child's arms, legs, and chest having healed may not be a sign of abuse, but rather a sign of normal wound healing or previous accidents.
A full-term, 24-hour-old infant in the nursery regurgitates and suddenly turns cyanotic. Which immediate intervention should the practical nurse (PN) implement?
Explanation
In this scenario, the sudden regurgitation and cyanosis in a 24-hour-old infant indicate a potential airway obstruction or compromise. The immediate priority is to clear the airway and ensure adequate ventilation.
Suctioning the oral and nasal passages helps remove any potential obstruction or mucus that may be causing the cyanosis. This intervention aims to restore normal airflow and prevent further respiratory distress in the infant.
Let's briefly evaluate the other options:
a) Turn the infant onto the right side.
Positioning the infant onto the right side does not directly address the potential airway obstruction or cyanosis. While positioning may have some benefit in certain situations, such as facilitating drainage, it is not the most appropriate immediate intervention in this case.
c) Give oxygen by positive pressure.
Administering oxygen by positive pressure may be necessary if the infant's oxygen saturation remains low after suctioning and clearing the airway. However, suctioning should be the initial intervention to address any potential airway obstruction or mucus before considering oxygen administration.
d) Stimulate the infant to cry.
Stimulating the infant to cry is not the appropriate intervention in this case. It does not directly address the potential airway obstruction or cyanosis. Crying requires a patent airway, and if the infant is already cyanotic, it suggests an obstruction or inadequate ventilation. Therefore, suctioning and clearing the airway take precedence over stimulating the infant to cry.
In summary, when a full-term, 24-hour-old infant in the nursery regurgitates and suddenly turns cyanotic, the practical nurse should immediately suction the oral and nasal passages to clear any potential airway obstruction or mucus. This intervention aims to restore normal airflow and ensure adequate ventilation for the infant.
The practical nurse (PN) determines that a client's pupils constrict as they change focus from a far object to a near object. How should the PN document this finding?
Explanation
Accommodation refers to the ability of the eyes to adjust and focus on objects at different distances. When a client's pupils constrict as they change focus from a far object to a near object, it indicates that their pupils are reacting appropriately to accommodate the change in focus.
To document this finding accurately, the practical nurse (PN) should document "Pupils reactive to accommodation." This statement captures the observation that the pupils are constricting in response to the client changing their focus from a far object to a near object. It indicates normal pupillary response and accommodation.
Let's briefly evaluate the other options:
a) Consensual pupillary constriction present.
Consensual pupillary constriction refers to the simultaneous constriction of both pupils when light is shone into one eye. This finding is not directly related to accommodation or the client's change in focus.
Therefore, it is not the appropriate documentation for the given scenario.
b) Nystagmus present with pupillary focus.
Nystagmus refers to involuntary eye movements that can affect the alignment and focus of the eyes. The presence of nystagmus is not mentioned in the scenario, and it is not directly related to the client's change in focus. Therefore, it is not the appropriate documentation for the given scenario.
d) Peripheral vision intact.
Peripheral vision refers to the ability to see objects outside the central visual field. While important for assessing visual function, it is not directly relevant to the observed pupillary response during accommodation. Therefore, it is not the appropriate documentation for the given scenario.
In summary, when a client's pupils constrict as they change focus from a far object to a near object, the practical nurse should document "Pupils reactive to accommodation" to accurately describe the observed pupillary response during the accommodation process.
A 16-year-old client is asking the practical nurse (PN) what can be done about acne. Which recommendation should the PN provide?
Explanation
Acne is a common skin condition that often requires specialized treatment. While general skincare practices can help maintain healthy skin, the most appropriate recommendation for a 16-year-old client seeking treatment for acne is to refer them to a dermatologist.
Acne can have various underlying causes, and effective treatment often involves a tailored approach based on the individual's specific condition. Dermatologists are medical professionals specializing in skin health and are best equipped to assess and provide appropriate treatment options for acne.
Let's briefly evaluate the other options:
a) Wash the hair and skin daily with mild soap and warm water.
While maintaining good hygiene is important for overall skin health, washing the hair and skin alone may not be sufficient to address acne. Acne is a multifactorial condition that requires more comprehensive treatment beyond basic hygiene practices.
b) Omit chocolate, carbonated drinks, and fried foods from the diet.
While diet can play a role in overall skin health, there is limited scientific evidence linking specific foods to the development or worsening of acne. Restricting specific foods may not be the most effective or necessary approach for treating acne. Additionally, dietary changes alone may not address the underlying causes of acne.
c) Express blackheads and follow with an exfoliating scrub.
Squeezing or expressing blackheads can potentially worsen acne and lead to skin damage or infection. It is generally not recommended to atempt self-extraction of blackheads or use aggressive exfoliating scrubs without professional guidance.
In summary, when a 16-year-old client seeks advice for acne, the most appropriate recommendation for the practical nurse (PN) is to refer the client to a dermatologist for prescribed long-term therapy.
Dermatologists have the expertise to evaluate the individual's specific condition and provide appropriate treatment options tailored to their needs.
A client with a compound fracture of the left ankle is being discharged with a below-the-knee cast. Which
instruction should the practical nurse (PN) provide to the client prior to discharge?
Explanation
When providing instructions to a client with a below-the-knee cast for a compound fracture of the left ankle, it is important to prioritize their safety and proper care of the cast. The instruction to never scratch under the cast is crucial for preventing complications and maintaining the integrity of the cast.
Let's evaluate the other options:
a) Apply a cold pack to any "hot spots" on the cast.
Applying a cold pack to any "hot spots" on the cast may help alleviate discomfort or itching, but it is not the highest priority instruction. Preventing scratching under the cast is more important to avoid skin damage or infection.
b) Keep the left leg in a dependent position.
Keeping the left leg in a dependent position (hanging down) is not the appropriate instruction for a client with a below-the-knee cast. It is generally recommended to elevate the injured limb to reduce swelling and promote proper blood flow. Elevating the leg would involve keeping it raised above the level of the heart.
c) Expect some increase in pain.
While it is possible for the client to experience some increase in pain after the application of a cast, this instruction alone is not comprehensive or specific enough for proper discharge education. Providing information about pain management strategies or when to seek medical atention for excessive pain would be more appropriate.
In summary, when discharging a client with a compound fracture of the left ankle and a below-the-knee cast, the practical nurse (PN) should provide the instruction to never scratch under the cast. This helps prevent complications and maintain the integrity of the cast, promoting proper healing of the fracture.

A nurse is reinforcing teaching with a school-age child who has hemophilia about participating in school
sports. Which of the following sports should the nurse recommend for the child? (Select all that apply.)
Explanation
Swimming is the recommended sport for a school-age child with hemophilia. Hemophilia is a bleeding disorder in which the blood lacks certain clotting factors. Engaging in contact sports or activities with a high risk of injury can increase the chances of bleeding episodes and injury for individuals with hemophilia.
Explanation:
Swimming is a low-impact sport that minimizes the risk of injury and joint stress, making it an ideal choice for children with hemophilia. It provides a cardiovascular workout without subjecting the child to excessive physical stress or the risk of trauma that could lead to bleeding. Swimming also promotes muscle strength and coordination without putting significant pressure on the joints.
Now, let's discuss why the other options are not recommended:
Basketball involves physical contact and has a higher risk of falls, collisions, and potential injuries. These factors increase the likelihood of bleeding episodes for individuals with hemophilia.
Gymnastics also carries a high risk of falls, joint stress, and potential injuries. The impact and demanding movements involved in gymnastics can pose a significant risk for children with hemophilia, leading to bleeding complications.
Soccer is a contact sport that involves running, kicking, and potential collisions with other players. The physical demands and unpredictable nature of the game increase the risk of injury and subsequent bleeding for individuals with hemophilia.
In summary, swimming is the most suitable sport fo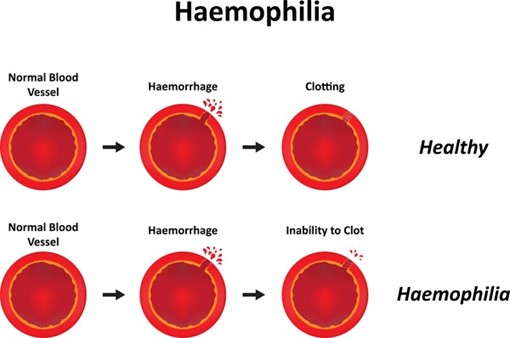 r a school-age child with hemophilia due to its low- impact nature and minimal risk of injury. It promotes physical fitness while minimizing the likelihood of bleeding episodes and joint stress.
r a school-age child with hemophilia due to its low- impact nature and minimal risk of injury. It promotes physical fitness while minimizing the likelihood of bleeding episodes and joint stress.
Explanation
Which of the following interventions should the nurse include in the plan of care?
Explanation
Choice A rationale:
Planning to have the client lay down for 1 hour after meals is not an appropriate intervention for a client with COPD. It may increase the risk of aspiration and worsen their breathing difficulties.
Choice C rationale:
Encouraging the client to use the upper chest for respiration is not the best approach for a client with COPD. Pursed-lip breathing helps improve oxygen exchange and decreases air trapping, which is more effective in managing COPD.
Choice D rationale:
Restricting the client's fluid intake to less than 1 Vday is not a suitable intervention for a client with COPD. Dehydration can lead to thicker mucus, making it harder to breathe
Explanation
Choice A reason: Advances in surgical techniques and procedures have improved the quality of life and survival rates for many patients, but they are not the main factor for the increase in life expectancy in the twentieth century.
Choice B reason: Sanitation and other public health activities, such as vaccination, safe water supply, sewage disposal, and food safety, have reduced the incidence and mortality of infectious diseases, which were the leading causes of death in the past. These activities have had a significant impact on increasing life expectancy in the twentieth century.
Choice C reason: Technology increases in the field of medical laboratory research have enabled better diagnosis and treatment of diseases, but they are not the primary reason for the increase in life expectancy in the twentieth century.
Choice D reason: Use of antibiotics to fight infections has saved many lives and prevented complications from bacterial diseases, but they are not the most important factor for the increase in life expectancy in the twentieth century. Moreover, antibiotics were not widely available until after World War II, which means they did not contribute much to the increase in life expectancy before that perioD.
Explanation
Choice A reason: Completing a survey of the various ethnicities represented in the nurse's community is a good way to learn about the diversity of the population, but it is not the first step in developing cultural competencE. The nurse should first examine their own cultural background and biases before learning about others.
Choice B reason: Studying the beliefs and traditions of persons living in other cultures is a valuable way to gain knowledge and understanding of different worldviews, but it is not the first step in developing cultural competencE. The nurse should first be aware of their own cultural values and assumptions before exploring those of others.
Choice C reason: Considering how the nurse's own personal beliefs and decisions are reflective of their culture is the first step in developing cultural competencE. The nurse should recognize that their culture influences their perception, communication, and behavior, and that they may have prejudices or stereotypes that affect their interactions with clients from different cultures.
Choice D reason: Inviting a family from another culture to join the nurse for an event is a nice gesture to show respect and interest in other cultures, but it is not the first step in developing cultural competencE. The nurse should first develop self-awareness and sensitivity to their own cultural identity before engaging with others.
Explanation
Choice A reason: The integumentary system is a portal of entry for anthrax because the bacteria can enter through cuts or abrasions on the skin, causing cutaneous anthrax, which is the most common and least severe form of the diseasE.
Choice B reason: The endocrine system is not a portal of entry for anthrax because the bacteria do not affect the glands or hormones of the body.
Choice C reason: The central nervous system is a portal of entry for anthrax because the bacteria can invade the brain and spinal cord, causing meningitis, which is a rare but fatal complication of anthrax infection.
Choice D reason: The renal system is not a portal of entry for anthrax because the bacteria do not affect the kidneys or urinary tract.
Choice E reason: The respiratory system is a portal of entry for anthrax because the bacteria can be inhaled into the lungs, causing inhalation anthrax, which is the most deadly and difficult to treat form of the diseasE.
Explanation
Choice A reason: "Diet and exercise are good for you and good for your heart." This response is true, but it does not address the client's concern or provide any specific information about cardiac rehabilitation.
Choice B reason: "It's not unusual to feel that way at first, but once you learn the routine, you'll enjoy it." This response is empathetic, but it does not explain the benefits or goals of cardiac rehabilitation.
Choice C reason: "Cardiac rehabilitation cannot undo the damage to your heart, but it can help you get back to your previous level of activity safely." This response is accurate and informativE. It acknowledges the client's condition and provides realistic expectations about cardiac rehabilitation.
Choice D reason: "Your doctor is the expert here, and I'm sure he would only recommend what is best for you." This response is respectful, but it does not answer the client's question or encourage their participation in cardiac rehabilitation.
A nurse is teaching a client who has a new prescription for sumatriptan (Imitrex) tablets to treat migraine headaches. Which of the following instructions should the nurse include?
Explanation
Choice A reason: "Repeat dose in 1 hour for unrelieved headachE." This instruction is incorrect because sumatriptan should not be taken more than twice in 24 hours.
Choice B reason: "Chew tablet well before swallowinG." This instruction is unnecessary because sumatriptan tablets are meant to be swallowed whole with water.
Choice C reason: "If you experience chest pain, call your physician immediately." This instruction is important because sumatriptan can cause coronary vasospasm, which can lead to angina or myocardial infarction.
Choice D reason: "Take daily to prevent headaches." This instruction is inappropriate because sumatriptan is used to treat acute migraine attacks, not to prevent them.
Explanation
Choice A reason: The AP's ability to complete the task without assistance is not one of the five rights of delegation. The nurse should always supervise and evaluate the AP's performance of delegated tasks.
Choice B reason: The AP's ability to prioritize is not one of the five rights of delegation. The nurse should provide clear and specific instructions and expectations for the delegated tasks.
Choice C reason: The AP's rapport with clients is not one of the five rights of delegation. The nurse should consider the client's preferences, needs, and condition when delegating tasks.
Choice D reason: The AP has the knowledge and skill to perform the task is one of the five rights of delegation. The nurse should delegate tasks that are within the AP's scope of practice, training, and competencE.
Explanation
Choice A reason: Nurses performing duties outside of the nurses' typical job description is not a component of a disaster plan. Nurses should only perform tasks that are within their scope of practice, license, and competencE.
Choice B reason: A plan for comprehensive practice drills is a component of a disaster plan. Nurses should be involved in conducting regular drills to test and improve the preparedness and response of the staff and facility.
Choice C reason: Identification of resources to meet anticipated needs for food, water, and supplies is a component of a disaster plan. Nurses should be involved in assessing and securing the necessary resources to provide adequate care and support for the clients and staff during a disaster.
Choice D reason: An internal and external communication plan is a component of a disaster plan. Nurses should be involved in establishing and maintaining effective communication channels with other health care providers, agencies, authorities, media, and community during a disaster.
Choice E reason: Discharge all surgical clients who are one day or more post-op is not a component of a disaster plan. Nurses should not discharge clients without proper assessment, documentation, education, and follow-up arrangements.
Explanation
Choice A reason: Gradual onset of several hours is not a manifestation of a hemorrhagic strokE. Hemorrhagic strokes occur when a blood vessel bursts in or near the brain, causing rapid bleeding and increased intracranial pressurE.
Choice B reason: Maintains consciousness is not a manifestation of a hemorrhagic strokE. Hemorrhagic strokes often cause loss of consciousness due to compression or damage of brain tissuE.
Choice C reason: Sudden severe headache is a manifestation of a hemorrhagic strokE. Hemorrhagic strokes can cause intense pain in the head due to bleeding and pressure on nerve endings.
Choice D reason: History of neurologic deficits lasting less than 1 hour is not a manifestation of a hemorrhagic strokE. Neurologic deficits lasting less than 1 hour are more indicative of a transient ischemic attack (TIA), which is caused by temporary blockage or narrowing of blood vessels in or leading to the brain.
A nurse who works in health promotion and safety for an automotive plant is functioning in what role?
Explanation
Choice A reason: A public health nurse is a nurse who works to promote and protect the health of populations and communities, not specific workplaces.
Choice B reason: A community nurse specialist is a nurse who has advanced education and training in a specific area of community health, such as mental health, gerontology, or maternal-child healtH.
Choice C reason: A nurse clinician is a nurse who has expertise in a clinical area of nursing practice, such as critical care, oncology, or wound carE.
Choice D reason: An occupational health nurse is a nurse who works to prevent and treat work-related injuries and illnesses, as well as promote the health and safety of workers and the environment.
Sign Up or Login to view all the 60 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

